C9orf72 G(4)C(2) repeat expansions in Alzheimer's disease and mild cognitive impairment
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of C9orf72 G(4)C(2) repeat expansions in Alzheimer's disease and mild cognitive impairment
at SciVerse ScienceDirect
Neurobiology of Aging 34 (2013) 1712.e1e1712.e7
Contents lists available
Neurobiology of Aging
journal homepage: www.elsevier .com/locate/neuaging
C9orf72 G4C2 repeat expansions in Alzheimer’s disease and mild cognitiveimpairment
Rita Cacace a,b,1, Caroline Van Cauwenberghe a,b,1, Karolien Bettens a,b, Ilse Gijselinck a,b,Julie van der Zee a,b, Sebastiaan Engelborghs b,c, Mathieu Vandenbulcke d, Jasper Van Dongen a,b,Veerle Bäumer a,b, Lubina Dillen a,b, Maria Mattheijssens a,b, Karin Peeters a,b, Marc Cruts a,b,Rik Vandenberghe e, Peter P. De Deyn b,c,f, Christine Van Broeckhoven a,b, Kristel Sleegers a,b,*
aDepartment of Molecular Genetics, VIB, Antwerp, Belgiumb Institute Born-Bunge, University of Antwerp, Antwerp, BelgiumcDepartment of Neurology and Memory Clinic, Hospital Network Antwerp, Middelheim and Hoge Beuken, Antwerp, BelgiumdDepartment of Psychiatry and Memory Clinic, University of Leuven and University Hospitals Leuven Gasthuisberg, Leuven, Belgiume Laboratory for Cognitive Neurology, Department of Neurology, University of Leuven and University Hospitals Leuven Gasthuisberg, Leuven, BelgiumfDepartment of Neurology and Alzheimer Research Center, University Medical Center Groningen, Groningen, the Netherlands
a r t i c l e i n f o
Article history:Received 19 December 2012Accepted 23 December 2012Available online 24 January 2013
Keywords:ADMCIC9orf72G4C2 repeat expansionGenetic association study
* Corresponding author at: NeurodegenerativeDepartment of Molecular Genetics, University of Antw1, B-2610 Antwerp, Belgium. Tel.: þ32 3 265 1032; fax
E-mail address: [email protected] These authors contributed equally to this work.
0197-4580/$ e see front matter � 2013 Elsevier Inc. Ahttp://dx.doi.org/10.1016/j.neurobiolaging.2012.12.019
a b s t r a c t
C9orf72 G4C2 repeat expansion is a major cause of amyotrophic lateral sclerosis and frontotemporal lobardegeneration. Its role in Alzheimer’s disease (AD) is less clear. We assessed the prevalence of G4C2
pathogenic repeat expansions in Flanders-Belgian patients with clinical AD or mild cognitive impairment(MCI). In addition, we studied the effect of non-pathogenic G4C2 repeat length variability on suscepti-bility to AD, and on AD cerebrospinal fluid (CSF) biomarker levels. A pathogenic repeat expansion wasidentified in 5 of 1217 AD patients (frequency <1%). No pathogenic expansions were observed in patientswith MCI (n ¼ 200) or control individuals (n ¼ 1119). Nonpathogenic repeat length variability was notassociated with AD, risk of conversion to AD in MCI individuals, or CSF biomarker levels. We concludethat pathogenic C9orf72 G4C2 repeat expansions can be detected in clinical AD patients and could act asa contributor to AD pathogenesis. Non-pathogenic repeat length variability did not affect risk of AD orMCI, nor AD biomarker levels in CSF, indicating that C9orf72 is not a direct AD risk factor.
� 2013 Elsevier Inc. All rights reserved.
1. Introduction
A pathogenic expansion of a hexanucleotide (G4C2) repeat in theregulatory region of C9orf72 (Fig. 1) was recently identified asa major cause of disease in the amyotrophic lateral sclerosis (ALS)efrontotemporal lobar degeneration (FTLD) spectrum of neuro-degeneration (DeJesus-Hernandez et al., 2011; Gijselinck et al.,2012; Renton et al., 2011). C9orf72 repeat expansions exceeding30 G4C2 units have been suggested to be pathological (Renton et al.,2011), although a much higher number of G4C2 repeats have beendetected, depending on the sensitivity of the molecular geneticstechnology used to size the G4C2 repeat itself (i.e. fluorescence insitu hybridization [FISH] and Southern blot assay) (DeJesus-Hernandez et al., 2011; Renton et al., 2011). A heterozygous
Brain Diseases Group, VIBerp e CDE, Universiteitsplein: þ32 3 265 1112.(K. Sleegers).
ll rights reserved.
pathogenic G4C2 repeat expansion in C9orf72 explains 4% to 8% ofpatients with isolated ALS or FTLD, and 25% to 40% of familial ALS orFTLD worldwide (Majounie et al., 2012b), but is particularlycommon in patients or families with a mixed phenotype of bothFTLD and ALS, explaining up to 85% of the occurrence of disease(Gijselinck et al., 2012). In line with this, detailed clinical investi-gations on cohorts of pathogenic repeat expansion carriersdemonstrate a relatively high prevalence of cognitive dysfunctionand frontal symptoms in mutation carriers with ALS, and of motorneuron disease in mutation carriers with FTLD (Chio et al., 2012;Mahoney et al., 2012). Nevertheless, substantial clinical heteroge-neity is observed between mutation carriers and within families,providing evidence for a wider phenotypic spectrum associatedwith this genetic defect (Mahoney et al., 2012; Stewart et al., 2012).Psychosis or other psychiatric symptoms appear to be prominentfeatures (Arighi et al., 2012; Mahoney et al., 2012; Snowden et al.,2012). Pathogenic repeat expansions have been identified inpatients with atypical clinical presentation, i.e. clinically diagnosedwith olivopontocerebellar degeneration, atypical Parkinsonian
Fig. 1. Schematic representation of C9orf72 gene and genotyping techniques. Schematic representation of the location of the 2 major isoforms of C9orf72 gene (coding regions arerepresented in black and noncoding regions in gray) and of rs2814707 on chromosome 9p21 (green). In orange, the position of the G4C2 repeat within the regulatory region (blue) isdepicted, and the orange sequence presents 3 complete G4C2 repeat units. The letter “n” indicates a variable G4C2 repeat length, with number of units ranging from 2 to w30 incontrol individuals, and more than 30 in patients. The first 2 exons of the isoform a (NM_018325.2) are enhanced to show the location of the primer pairs used for RP-PCR (theprimer anchor sequence is represented in gray) and STR-PCR to genotype the G4C2 repeats in the AD and MCI cohorts. The two C9orf72 gene isoforms, rs2814707, G4C2 repeat andprimer pairs for the genotyping have been represented on the reverse complement strand relative to their original position on the reference genome (NCBIbuild37 - hg19).
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e7 1712.e2
syndrome, corticobasal syndrome (Lindquist et al., 2012) or slowlyprogressive behavioral variant FTD (Khan et al., 2012). Also,a family-based study detected a pathogenic repeat expansion in 6patients clinically diagnosed with probable AD in 3 of 342 families(Majounie et al., 2012a). In a second series of 114 AD patients withearly age at onset and cerebrospinal fluid (CSF) biomarker profiletypical of AD, 3 carried a G4C2 expansion (Wallon et al., 2012). In 2additional series of 568 and 424 AD patients, no pathogenic repeatexpansions were detected (Rollinson et al., 2012; Xi et al., 2012). Anadditional cohort of 1184 AD patients was recently investigated byKohli et al. and resulted in the identification of 9 patients carryingthe G4C2 expansion of which 3 were autopsy confirmed (Kohli et al.,2012). These studies suggest that, albeit rare, C9orf72 repeatexpansions may underlie a spectrum of neurodegenerative braindisease phenotypes, such as Alzheimer’s disease (AD), with repercus-sions for clinical decisionmaking. A general role of C9orf72 in differentneurodegenerative diseaseswas recently proposed (Satoh et al., 2012),because of co-expression of C9orf72 and UBQLN1 in dystrophic neu-rites distributed in the CA1 region and the molecular layer in thehippocampus of AD and non-AD brains, suggesting that C9orf72 indystrophic neurites is involved in the homeostasis of protein degra-dation by acting together with UBQLN1 (Satoh et al., 2012).
In this study, we assess the prevalence of pathogenic C9orf72repeat expansions in a large prospective cohort of Flanders-Belgianpatients with clinical diagnosis of AD (n ¼ 1217) or mild cognitiveimpairment (MCI; n ¼ 200), an intermediate stage of cognitivedecline that may convert to AD. We extend these analyses toexplore whether repeat expansions of intermediate length mightconvey risk to develop AD and/or could influence the CSF biomarkerlevels of amyloid-b peptide (Ab1-42), total tau (T-tau), and tauphosphorylated at threonine 181 (P-tau181P).
2. Material and methods
2.1. Patient/control cohort
The Flanders-Belgian study cohort consisted of 1417 patients,1217 AD patients (mean age at onset, 74.5 � 8.9 years; 65.2%
women) and 200 MCI individuals (mean age at onset, 72.4 � 8.8years; 50.7% women), and another group of 1119 healthy controlindividuals (mean age at inclusion, 65.1 � 13.6 years; 56.5%women).
The majority of the AD and MCI cohort was ascertained at theMemory Clinic of the ZNA Middelheim and Hoge Beuken, Ant-werp, Belgium (P.P.D.D. and S.E.) as part of a prospective study ofneurodegenerative and vascular dementia in Flanders, the Dutch-speaking region of Belgium (Engelborghs et al., 2003;Engelborghs et al., 2006). Consensus diagnosis of possible andprobable AD was given by at least 2 neurologists based on theNational Institute of Neurological and Communication Disordersand StrokeeAlzheimer’s Disease and Related Disorders Associa-tion (NINCDS-ADRDA) criteria (McKhann et al., 1984). Anothersubset of patients was collected at the Memory Clinic of theUniversity Hospitals of Leuven, Gasthuisberg, Leuven, Belgium(R.V. and M.V.) as part of a prospective study on the moleculargenetics of cognitive impairment (Bettens et al., 2010) using thesame clinical assessments and biosampling schemes. Each ADpatient underwent a neuropsychological examination, includingMini-Mental State Examination (MMSE) (Folstein et al., 1975),and structural and/or functional neuroimaging (Bettens et al.,2010). For a subset of patients (n ¼ 292; mean age at onset,76.7 � 8.2 years; 62.3% women), CSF levels of Ab1-42, T-tau, andP-tau181P were available as part of the diagnostic work-up,determined with commercially available single parameterenzyme-linked immunosorbent assay (ELISA) kits (Innogenetics,Ghent, Belgium). Previous mutation screening revealed 1 patientwith a known pathogenic APP mutation, 6 patients with a PSEN1,and 3 patients with a GRN known pathogenic mutation, respec-tively. Diagnosis of MCI was based on Petersen’s diagnosticcriteria (Petersen 2004). During follow-up, 62 of the MCI patients(31%) converted to AD.
The control cohort consisted of unrelated individuals, withoutneurological or psychiatric antecedents or neurologicalcomplaints or without organic disease involving the centralnervous system, examined at the Memory Clinic of ZNA Mid-delheim and Hoge Beuken, Antwerp, Belgium (P.P.D.D. and S.E.)
Fig. 2. Distribution of C9orf72 G4C2 repeat units in AD patients and control individuals.The blue line indicates AD patients and the green line healthy control individuals. Theshortest allele (2 units) contains one unit less than the reference genome (NCBIbuild37- hg19). The cut-off between short and intermediate C9orf72 allele repeat units,determined as previously described (van der Zee et al., 2012), is indicated witha dashed line.
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e71712.e3
and the memory clinic at the University Hospitals of Leuven,Gasthuisberg, Leuven, Belgium. Additional community controlindividuals were included after interview concerning medicaland family history and Mini Mental State Examination (MMSE >
24) (Folstein et al., 1975).
2.2. Ethical assurances
All participants and/or their legal guard gave written informedconsent for participation in clinical and genetic studies. Clinicalstudy protocol and the informed consent forms for patient ascer-tainment were approved by the Ethics Committee of the respectivehospitals at the cohort sampling sites in Flanders-Belgium. Thegenetic study protocols and informed consent formswere approvedby the Ethics Committees of the University of Antwerp and theUniversity Hospital of Antwerp, Belgium.
2.3. Procedures
To screen the Flanders-Belgian AD and MCI cohorts for thepathological C9orf72 repeat expansion, G4C2 repeat-primed poly-merase chain reaction (RP-PCR) (Fig. 1) was performed as previ-ously described (Gijselinck et al., 2012; van der Zee et al., 2012).Briefly, we used a locus specific 6-carboxyfluorescein (FAM) labeledreverse primer, a first forward primer consisting of 4 GGGGCC unitsand an anchor sequence and a second forward primer consisting ofthe anchor sequence only. The amplification was performed usingthe Expand Long Template PCR System (Roche Diagnostic GmbH,Mannheim, Germany) with an annealing temperature of 53 �C. Theamplification product was separated on an ABI 3730 automaticsequencer (Applied Biosystems, Foster City, CA) and analyzed usingin house developed TracI genotyping software (http://www.vibgeneticservicefacility.be).
The RP-PCR is able to detect a maximum of w60 units of G4C2
repeat expansion. This detection limit is sufficient to discriminatesamples carrying a pathological repeat expansion (>30 units) fromthose that are not pathological, and to estimate the size of thelongest allele in non-expansion carriers. To accurately size therepeat length of the nonpathologically expanded alleles (<30repeat units) in the Flanders-Belgian AD and MCI cohorts, we alsoperformed an STR genotyping assay (STR-PCR) (Fig. 1) usinga primer pair flanking the repeat (primers available upon request)(van der Zee et al., 2012), which allows deducing the number ofG4C2 units from the PCR fragment length. The STR-PCR was per-formed using the KAPA HiFi HotStart DNA Polymerase with dNTPskit (KAPA Biosystems, Boston, MA) with an annealing temperatureof 59 �C and optimized for high GC content. The amplificationproduct was size separated on an ABI 3730 automatic sequencer(Applied Biosystems) using GeneScan-600 LIZ (Applied Biosystems)as internal size standard. Data analysis was performed using theTracI genotyping software.
In addition, rs2814707, located 10 kb downstream of C9orf 72 onchromosome 9p21 (Fig. 1) and tagging the chromosome 9 riskhaplotype, was genotyped in the Flanders-Belgian AD and MCIcohorts. Specific PCR primers were amplified using Titanium TaqDNA Polymerase (Clontech Laboratories, Takara Bio Company,Mountain View, CA) in a 2-step combined annealing/extensionprotocol at 68 �C. The resulting amplicons were purified with 10Uexonuclease I (USB Corporation, Cleveland, OH) and 2U shrimpalkaline phosphatase (USB Corporation). Purified amplicons weresequenced using the BigDye Terminator Cycle Sequencing kit v3.1(Applied Biosystems) and analyzed on an ABI 3730 DNA Analyzer(Applied Biosystems). Sequence analysis was performed using bothSeqManII (DNASTAR, Madison, WI) and novoSNP (Weckx et al.,2005) (http://www.molgen.ua.ac.be/bioinfo/novosnp).
2.4. Statistical analysis
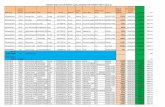
Allelic and genotypic frequencies of short (2e6 units) andintermediate (7e25 units) (nonpathogenic) normal repeat alleleswere compared between AD patients and control individuals. Inaddition, allele and genotype frequencies were compared betweenMCI and control individuals, as well as between MCI and ADpatients. The repeat length cut-off of 7 units was determined aspreviously described (van der Zee et al., 2012). Briefly, the alleledistribution shows a multimodal pattern (Fig. 2). Three groupscould be defined using the MCLUST package in R, of which the thirdgroup, determined by a cutoff at 7 units, correlates with rs2814707tagging the chromosome 9 risk haplotype. Pathogenic repeatexpansion carriers were excluded from the association analyses.Odds ratios (ORs) and 95% confidence interval (CIs) were calculatedin a logistic regression model, adjusted for gender and age at onset(age at inclusion for control individuals). Deviation from Hardy-Weinberg equilibrium (HWE) of the genotyped SNP rs2814707was assessed using an exact HWE test (www.pharmgat.org/IIPGA2/Bioinformatics/exacthweform).
Differences in genotypic frequencies for rs2814707 between ADpatients and control individuals were tested using c2 statistics. Todetermine the effect of rs2814707 on AD risk, ORs and 95% CIs werecalculated in a logistic regression model, adjusted for gender andage at onset (age at inclusion for control individuals). To assess theinfluence of repeat length on conversion from MCI to AD, we esti-mated hazard ratios using Cox proportional hazard models. Toestablish the effect of the nonpathogenic longer allele in influencingCSF biomarker levels of Ab1-42, T-tau and P-tau181P, possible cova-riates affecting CSF biomarker levels (age and disease duration atlumbar puncture, APOE ε4 genotype and gender) were evaluatedand retained in the analysis. For Ab1-42, and P-tau181P, APOE ε4significantly affected the model. T-tau and P-tau181P were log10transformed to approximate normality before analysis of variance.All statistical analyses were performed using SPSS18.0 Version forWindows (SPSS Inc., Chicago, IL). A 2-sided p value of .05 wasconsidered statistically significant.
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e7 1712.e4
3. Results
3.1. C9orf72 pathogenic G4C2 repeat expansions
In the AD cohort of Flanders-Belgian origin we detected a path-ological G4C2 repeat expansion in 5 out of 1217 patients, hencea mutation frequency of 0.41%. All pathogenic G4C2 expansioncarriers had an expansion of >60 units. In the MCI cohort, no path-ological G4C2 repeat expansions were observed. The age at diseaseonset of the 5 pathogenic G4C2 expansion carriers ranged from 56 to80 years (Table 1). The 5 patients were clinically diagnosed withAD. Patient DR212.1 showed signs of frontal dysfunction (lossof decorum, inhibition) and paranoid delusions, but neuro-psychological test results were most compatible with a diagnosis ofAD. For 1 patient (DR740.1), a rapid secondary deterioration wasnotable. This patient presented initially with a classical amnesticMCI with encoding and retrieval deficit and only subtle changes inexecutive function, without any language, personality, or comport-mental disturbances. She converted from amnestic MCI to clinicallyprobable AD 1 year after the initial presentation. Approximately 2.5years after the initial presentation, a faster decline was noted, withthe appearance of comportmental changes. None of the patients hada clinical diagnosis of motor neuron dysfunction (MND). Structuralneuroimaging showed generalized corticoesubcortical atrophy in 4patients (computed tomography [CT]) and bilateral hippocampalatrophy in 1 patient (DR 740.1; magnetic resonance imaging [MRI]),and functional neuroimaging (perfusion single-photon emissioncomputed tomography [SPECT]), performed in 3 patients, showedrelative hypoperfusion of the frontal, parietal, and temporal regions.A CSF biomarker profile had been determined for 1 patient, whichwas compatible with a diagnosis of AD (Table 1). Among the path-ological expansion carriers, 4 patients had a documented positivefamily history of cognitive deterioration. For patient DR212.1, DNAof3 relatives was available for segregation analyses. We detecteda pathological G4C2 repeat expansion in a sibling (DR212.4; Table 1)who presented to the memory clinic at age 65 years with cognitiveimpairment and reduced ability to live independently. At that time,CSF biomarker profile was within the normal range, and CT imagingshowed a physiological degree of atrophy in the presence of whitematter lesions (WML), but the neuropsychological examinationrevealed general cognitive deterioration with predominant frontaland temporal dysfunction.
Table 1Clinical characteristics of the C9orf72 G4C2 repeat expansion carriers
PatientID
Gender(M/F)
Clinicaldementiadiagnosis
Clinicaldiagnosisof MND
Onsetage
Age at death Fam
DR738.1 F Probable AD No 56 72 þ (t
DR212.1 M Probable AD No 68 72 þ
DR212.4a F Dementia NOS No 65 ? þ
DR739.1 F Probable AD No 80 ?
DR452.1 F Probable AD No 73 80 þ (fons
DR740.1 F AD No 73 79 þ (f65 ydem
Key: CSF, cerebrospinal fluid; CT, computed tomography; F, female; ID, patient identifier;specified; SPECT, single-photon emission computed tomography; WML, white matter le
a sibling of DR212.1.
3.2. C9orf72 nonpathogenic G4C2 repeats and risk of AD and effecton CSF biomarker levels of Ab1-42, T-tau and P-tau181P
To analyze whether variability in nonpathogenic G4C2 repeatlength is associated with AD or MCI, we sized the length (i.e. thenumber of G4C2 units) of nonpathogenic G4C2 alleles with an STR-PCR in the study population. After exclusion of the 5 pathologicalexpansion carriers (>60 G4C2 units), the number of G4C2 repeatunits in the AD cohort ranged from 2 to 25, and in the MCI cohortfrom 2 to 24, as found in control individuals (van der Zee et al.,2012) (Fig. 2). No significant difference in frequencies of short andintermediate C9orf72 repeats (short alleles <7 repeat units; inter-mediate alleles �7 repeat units) could be identified between ADpatients and control individuals (Table 2). Furthermore, weobserved no significant difference in repeat length distributionbetween MCI individuals and AD patients (p ¼ .4), or between MCIand control individuals (p ¼ .6). MCI individuals with an interme-diate repeat length were not at greater risk for developing AD thanthose not carrying an intermediate length repeat (hazard ratio[HR]¼ 0.83, 95% CI¼ 0.50e1.40, p¼ .5). In addition, the effect of theintermediate repeat length on cerebrospinal fluid biomarkers wasexamined considering CSF levels of T-tau (mean difference ¼ 0.03;standard error (SE) ¼ 0.02; p ¼ .91; 95% CI for difference ¼ �0.04 to0.05), Ab1-42 (mean difference ¼ 13.51; SE ¼ 17.48; p ¼ .44; 95% CIfor difference ¼ �47.85 to 20.82) and P-tau181P (mean difference ¼0.015; SE ¼ 0.020; p ¼ .46; 95% CI for difference ¼ �0.024 to 0.053),but no association of the intermediate allele was observed.
3.3. Association analysis of rs2814707
SNP genotyping was performed of rs2814707, a SNP that reachedgenome-wide significant association of the T-allelewith ALS and tagsthe chromosome 9p21 risk haplotype harboring the C9orf72 patho-genic G4C2 repeat expansion (Gijselinck et al., 2012; Laaksovirta et al.,2010; Shatunov et al., 2010; van Es et al., 2009). It was previouslyshownthat the riskassociationof theT-allelewithdiseasewasmainlydriven by the carriers of a pathological expansion (DeJesus-Hernandez et al., 2011; Gijselinck et al., 2012). We also demon-strated anallelic association between thepresence of an intermediateG4C2 repeat and the T-allele at rs2814707 (van der Zee et al., 2012).
In our cohorts, all pathological G4C2 repeat expansion carrierscarry the T-allele at rs2814707 in a homozygous or heterozygous
ily history Neuroimaging CSF biomarker profile
win sister) Generalized corticosubcorticalatrophy (CT), relative frontoparieto-temporal hypo-perfusion (SPECT)
ND
Generalized corticosubcorticalatrophy (CT), relative frontoparieto-temporal hypo-perfusion (SPECT)
ND
Physiological atrophy, WML (CT) Normal (T-tau: 316 pg/ml;Abeta1-42: 1052 pg/ml;P-tau181P: 47 pg/ml)
Generalized corticosubcorticalatrophy (CT)
ND
ather, lateet dementia)
Generalized corticosubcorticalatrophy (CT), relative frontoparieto-temporal hypo-perfusion (SPECT)
Typical for AD (T-tau: 746pg/ml; Abeta1-42: 707 pg/ml; P-tau181P: 86 pg/ml)
ather died atears withentia)
MRI: bilateral hippocampal atrophy ND
M, male; MND, motor neuron dysfunction; ND, not determined; NOS, not otherwisesion.
Table 2Association of C9orf72 G4C2 repeat and rs2814707 in Flanders-Belgian Alzheimer’sdisease, mild cognitive impairment, and control cohorts
Genotype AD patients Controls Logistic regression
N % N % OR (95% CI) pvalue
G4C2repeat
S/S 540 59.7 596 59.3 .73S/I 322 35.6 364 36.2 0.92 (0.75e1.13) .43I/I 42 4.7 45 4.5 0.94 (0.58e1.51) .80
S 1402 77.5 1556 77.4I 406 22.5 454 22.6 0.94 (0.80e1.11) .48
rs2814707 CC 527 59.3 559 58.3 .67CT 322 36.2 356 37.1 0.92 (0.75e1.13) .43TT 40 4.5 44 4.6 0.87 (0.54e1.41) .57
C 1376 77.4 1474 76.9T 402 22.6 444 23.1 0.93 (0.79e1.10) .38
Genotype MCI AD patients Logistic regression
N % N % OR (95% CI) pvalue
G4C2repeat
S/S 87 55.4 540 59.7 .40S/I 64 40.8 322 35.6 1.27 (0.89e1.81) .19I/I 6 3.8 42 4.7 0.93 (0.38e2.27) .87
S 238 75.8 1402 77.5I 76 24.2 406 22.5 1.13 (0.85e1.50) .40
rs2814707 CC 92 55.4 527 57.8 .43CT 64 38.6 322 35.3 1.16 (0.82e1.65) .40TT 10 6.0 63 6.9 1.53 (0.73e3.19) .26
C 248 74.7 1376 77.4T 84 25.3 402 22.6 1.19 (0.90e1.56) .22
Genotype MCI Controls Logistic regression
N % N % OR (95%CI) pvalue
G4C2repeat
S/S 87 55.4 596 59.3 .68S/I 64 40.8 364 36.2 1.16 (0.82e1.66) .41I/I 6 3.8 45 4.5 0.93 (0.38e2.26) .87
S 238 75.8 1556 77.4I 76 24.2 454 22.6 1.08 (0.81e1.43) .62
rs2814707 CC 92 55.4 559 58.3 .76CT 64 38.6 356 37.1 1.05 (0.74e1.49) .79TT 10 6.0 44 4.6 1.32 (0.63e2.75) .46
C 248 74.7 1474 76.9T 84 25.3 444 23.1 1.09 (0.83e1.43) .54
Key: AD, Alzheimer’s disease; 95% CI, 95% confidence interval; I, intermediate repeatalleles with�7 repeat units; MCI, mild cognitive impairment; OR, odds ratio; S, shortrepeat alleles with <7 repeat units.Patients with a pathological C9orf72 G4C2 expansion carriers were excluded from allassociation analyses.p Values were calculated using logistic regression analysis and were corrected forage at onset (AAO)/ age at inclusion (AAI) for control individuals and gender.
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e71712.e5
state; however, in line with the results of the association analysiswith G4C2 repeat length, we did not identify a significant associa-tion of rs2814707 with AD (p ¼ .4) (Table 2). Furthermore, we werenot able to identify a significant association of rs2814707 betweenMCI and AD patients on one hand (p¼ .2) and control individuals onthe other hand (p ¼ .5) (Table 2).
4. Discussion
C9orf72 hexanucleotide repeat expansion has recently beenidentified as a major cause of FTLD and ALS (DeJesus-Hernandezet al., 2011; Gijselinck et al., 2012; Renton et al., 2011). In thepresent study we investigated the frequency of the pathologicalC9orf72 G4C2 expansion in a prospective Flanders-Belgian cohort of
patients with a clinical diagnosis of AD (n¼ 1217) or MCI (n ¼ 200),and we assessed the potential role of intermediate C9orf72 repeatexpansion in conferring risk for developing AD and/or for influ-encing the CSF biomarker levels of T-tau, Ab1-42, and P-tau181P.
The screening of C9orf72 G4C2 repeat expansion in our cohortsresulted in the identification of 5 AD patients (<1%) carryinga pathological expansion, and none in individuals with MCI.Notably, the frequency of G4C2 repeat expansion in our study cohortis comparable to a cohort investigated previously (<1%) (Kohli et al.,2012). This confirms that C9orf72 G4C2 repeat expansion is nota common cause of AD, but that it could nevertheless underliea neurodegenerative process presenting with a clinical phenotypecompatible with AD (Majounie et al., 2012a). Mutations in genesinvolved in other neurodegenerative brain diseases have beenobserved before in patients with clinical AD (i.e. in MAPT(Rademakers et al., 2003), GRN (Brouwers et al., 2007)), under-scoring the need for a broader molecular diagnostic screening. Inthis study, we identified 1 mutation carrier with a CSF biomarkerprofile typical for AD in addition to G4C2 repeat expansion carrierswith atypical clinical presentation. Furthermore, a recent studyidentified G4C2 expansion carriers with a pathologically confirmedAD diagnosis (Kohli et al., 2012).
This implies that even in patients with a biochemically orpathologically supported diagnosis of AD, diagnostic screening ofgenes outside the amyloid pathway is warranted when initialscreening of APP, PSEN1, or PSEN2 is negative. In our series of 5mutation-carrying AD patients and 1 sibling with dementia NOS, noclear phenotypic characteristics can be defined that point towardthe underlying mutation. One C9orf72 mutation carrier in ourcohort had paranoid delusions. A recent study suggests that thismay be a prominent feature of C9orf72erelated disease (Snowdenet al., 2012). Rapid deterioration after initially slowly progressivedisease was remarkable for 1 patient, although we cannot excludethat this was due to external factors. The onset age varied widely, ashas been reported before for C9orf72mutation carriers (Boeve et al.,2012; Mahoney et al., 2012), but also for mutations in other genes.The average onset age of patients in our series (69.2 years), and inthe study of Kohli et al. (77.8 years) (Kohli et al., 2012), was higherthan reported for FTLD and ALS cohorts, as reviewed by Ferrari andcolleagues (Ferrari et al., 2012). In fact, in our study, 3 of the 6patients had a disease onset after age 70 years. In line with this, inan autopsy series of C9orf72 carriers, mutation carriers with aninitial clinical diagnosis of AD, sometimes preceded by amnesticMCI, were older, at least at death, than those presenting with anFTLD or MND phenotype (Murray et al., 2011). This suggests thatmodifying factors are at play that bring about a predominantlyamnestic dementia with later onset in C9orf72 mutation carrierswith clinical AD. It should be noted that for none of the mutationcarriers in this study an autopsy has been performed, and a CSFbiomarker profile had been determined for only 1 of the ADpatients. In the autopsy series described by Murray and colleagues,the majority of the C9orf72 mutation carriers presenting withsymptoms of amnestic MCI or AD had hippocampal sclerosis, andonly 1 had AD-type pathology sufficient to diagnose AD (Murrayet al., 2011). Accordingly, in our study, DR740.1 presented witha typical amnestic MCI and had clear bilateral hippocampal volumeloss on MRI. The hippocampal sclerosis may mimic the clinicalaspects of AD through an impact on memory dysfunction, resultingin a primary diagnosis of AD. Most likely the AD-type pathologyobserved in the autopsy series, and the CSF AD biomarker profile ofDR452.1 in our study and 3 patients with early-onset dementiadescribed elsewhere (Wallon et al., 2012) reflect concomitant AD.Brain autopsy confirming definite AD diagnoses in patients carryingthe G4C2 repeat expansion (Kohli et al., 2012) gives further proofthat the presence of the C9orf72 G4C2 repeat expansions in cohorts
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e7 1712.e6
of AD patients cannot be fully explained by misdiagnosed FTLDpatients. In addition, we investigated the role of normal variabilityof C9orf72 G4C2 repeat length in AD susceptibility and/or in influ-encing CSF biomarker levels of T-tau, Ab1-42, and P-tau181P, and weassessed association between AD and rs2814707, which showsgenome-wide significant association with ALS and tags the chro-mosome 9p21 risk haplotype harboring the C9orf72 pathogenicG4C2 repeat expansion (Gijselinck et al., 2012; Laaksovirta et al.,2010; Shatunov et al., 2010; van Es et al., 2009). Neitherrs2814707 nor longer C9orf72 G4C2 repeat length were associatedwith AD orMCI, and longer repeat length did not predict conversionto AD in MCI individuals or affect CSF biomarker levels of T-tau,Ab1-42, and P-tau181P. This implies that C9orf72 is not a direct riskfactor for AD or for the conversion of MCI to AD.
5. Conclusion
In conclusion, our data underscore that C9orf72 G4C2 expansioncould lead to a spectrum of neurodegenerative brain diseasephenotypes and, in a small percentage of cases, could act asa contributor to AD pathogenesis. The genetic screening of C9orf72G4C2 expansion in AD patients, both with typical clinical presen-tation and differential diagnosis with atypical symptoms (i.e.,frontal dysfunction, paranoid delusion), could be an additional toolto establish an evenmore cautious clinical diagnosis and could havean influence on patient care management.
Disclosure statement
The authors declare that they have no conflicts of interest.
Acknowledgements
The authors acknowledge the important participation ofpatients and their relatives as well as control individuals. Researchin the authors’ group is funded in part by the InteruniversityAttraction Poles program P7/16 of the Belgian Science Policy Office(BELSPO, http://www.belspo.be/), the Foundation for AlzheimerResearch (SAO/FRMA, http://alzh.org/), the Europe Initiative onCenters of Excellence in Neurodegeneration (CoEN), a MethusalemExcellence Grant of the Flemish Government (EWI, http://www.ewi-vlaanderen.be/), the Research Foundation Flanders (FWO,http://www.fwo.be/), the University Research Fund of the Univer-sity of Antwerp (UA, http://www.ua.ac.be/), the Medical ResearchFoundation Antwerp, Belgium, and the MetLife Foundation Awardto C.V.B. K.B., I.G., and J.vdZ. are postdoctoral fellows of the FWO;R.V. is a senior clinical investigator of the FWO.
References
Arighi, A., Fumagalli, G.G., Jacini, F., Fenoglio, C., Ghezzi, L., Pietroboni, A.M., DeRiz, M., Serpente, M., Ridolfi, E., Bonsi, R., Bresolin, N., Scarpini, E., Galimberti, D.,2012. Early onset behavioral variant frontotemporal dementia due to theC9ORF72 hexanucleotide repeat expansion: Psychiatric clinical presentations.J. Alzheimers Dis. 31, 447e452.
Bettens, K., Brouwers, N., Van Miegroet, H., Gil, A., Engelborghs, S., De Deyn, P.P.,Vandenberghe, R., Van Broeckhoven, C., Sleegers, K., 2010. Follow-up study ofsusceptibility loci for Alzheimer’s disease and onset age identified by genome-wide association. J. Alzheimers Dis. 19, 1169e1175.
Boeve, B.F., Boylan, K.B., Graff-Radford, N.R., DeJesus-Hernandez, M., Knopman, D.S.,Pedraza, O., Vemuri, P., Jones, D., Lowe, V., Murray, M.E., Dickson, D.W.,Josephs, K.A., Rush, B.K., Machulda, M.M., Fields, J.A., Ferman, T.J., Baker, M.,Rutherford, N.J., Adamson, J., Wszolek, Z.K., Adeli, A., Savica, R., Boot, B.,Kuntz, K.M., Gavrilova, R., Reeves, A., Whitwell, J., Kantarci, K., Jack Jr., C.R.,Parisi, J.E., Lucas, J.A., Petersen, R.C., Rademakers, R., 2012. Characterization offrontotemporal dementia and/or amyotrophic lateral sclerosis associated withthe GGGGCC repeat expansion in C9ORF72. Brain 135, 765e783.
Brouwers, N., Nuytemans, K., van der Zee, J., Gijselinck, I., Engelborghs, S., Theuns, J.,Kumar-Singh, S., Pickut, B.A., Pals, P., Dermaut, B., Bogaerts, V., De Pooter, T.,
Serneels, S., Van den Broeck, M., Cuijt, I., Mattheijssens, M., Peeters, K., Sciot, R.,Martin, J.J., Cras, P., Santens, P., Vandenberghe, R., De Deyn, P.P., Cruts, M., VanBroeckhoven, C., Sleegers, K., 2007. Alzheimer and Parkinson diagnoses inprogranulin null mutation carriers in an extended founder family. Arch. Neurol.64, 1436e1446.
Chio, A., Borghero, G., Restagno, G., Mora, G., Drepper, C., Traynor, B.J., Sendtner, M.,Brunetti, M., Ossola, I., Calvo, A., Pugliatti, M., Sotgiu, M.A., Murru, M.R.,Marrosu, M.G., Marrosu, F., Marinou, K., Mandrioli, J., Sola, P., Caponnetto, C.,Mancardi, G., Mandich, P., La Bella, V., Spataro, R., Conte, A., Monsurro, M.R.,Tedeschi, G., Pisano, F., Bartolomei, I., Salvi, F., Lauria Pinter, G., Simone, I.,Logroscino, G., Gambardella, A., Quattrone, A., Lunetta, C., Volanti, P., Zollino, M.,Penco, S., Battistini, S., Renton, A.E., Majounie, E., Abramzon, Y., Conforti, F.L.,Giannini, F., Corbo, M., Sabatelli, M., 2012. Clinical characteristics of patientswith familial amyotrophic lateral sclerosis carrying the pathogenic GGGGCChexanucleotide repeat expansion of C9ORF72. Brain 135, 784e793.
DeJesus-Hernandez, M., Mackenzie, I.R., Boeve, B.F., Boxer, A.L., Baker, M.,Rutherford, N.J., Nicholson, A.M., Finch, N.A., Flynn, H., Adamson, J., Kouri, N.,Wojtas, A., Sengdy, P., Hsiung, G.Y., Karydas, A., Seeley, W.W., Josephs, K.A.,Coppola, G., Geschwind, D.H., Wszolek, Z.K., Feldman, H., Knopman, D.S.,Petersen, R.C., Miller, B.L., Dickson, D.W., Boylan, K.B., Graff-Radford, N.R.,Rademakers, R., 2011. Expanded GGGGCC hexanucleotide repeat in noncodingregion of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron 72,245e256.
Engelborghs, S., Dermaut, B., Goeman, J., Saerens, J., Marien, P., Pickut, B.A., Van denBroeck, M., Serneels, S., Cruts, M., Van Broeckhoven, C., De Deyn, P.P., 2003.Prospective Belgian study of neurodegenerative and vascular dementia: APOEgenotype effects. J. Neurol. Neurosurg. Psychiatry 74, 1148e1151.
Engelborghs, S., Dermaut, B., Marien, P., Symons, A., Vloeberghs, E., Maertens, K.,Somers, N., Goeman, J., Rademakers, R., Van den Broeck, M., Pickut, B., Cruts, M.,Van Broeckhoven, C., De Deyn, P.P., 2006. Dose dependent effect of APOEepsilon4 on behavioral symptoms in frontal lobe dementia. Neurobiol. Aging 27,285e292.
Ferrari, R., Mok, K., Moreno, J.H., Cosentino, S., Goldman, J., Pietrini, P., Mayeux, R.,Tierney, M.C., Kapogiannis, D., Jicha, G.A., Murrell, J.R., Ghetti, B.,Wassermann, E.M., Grafman, J., Hardy, J., Huey, E.D., Momeni, P., 2012. Screeningfor C9ORF72 repeat expansion in FTLD. Neurobiol. Aging 33, 1850.e1e11.
Folstein, M.F., Folstein, S.E., McHugh, P.R., 1975. "Mini-Mental State". A practicalmethod for grading the cognitive state of patients for the clinician. J. Psychiatr.Res. 12, 189e198.
Gijselinck, I., Van Langenhove, T., van der Zee, J., Sleegers, K., Philtjens, S.,Kleinberger, G., Janssens, J., Bettens, K., Van Cauwenberghe, C., Pereson, S.,Engelborghs, S., Sieben, A., De Jonghe, P., Vandenberghe, R., Santens, P., DeBleecker, J., Maes, G., Baumer, V., Dillen, L., Joris, G., Cuijt, I., Corsmit, E., Elinck, E.,Van Dongen, J., Vermeulen, S., Van den Broeck, M., Vaerenberg, C.,Mattheijssens, M., Peeters, K., Robberecht, W., Cras, P., Martin, J.J., De Deyn, P.P.,Cruts, M., Van Broeckhoven, C., 2012. A C9orf72 promoter repeat expansion ina Flanders-Belgian cohort with disorders of the frontotemporal lobardegeneration-amyotrophic lateral sclerosis spectrum: a gene identificationstudy. Lancet Neurol. 11, 54e65.
Khan, B.K., Yokoyama, J.S., Takada, L.T., Sha, S.J., Rutherford, N.J., Fong, J.C.,Karydas, A.M., Wu, T., Ketelle, R.S., Baker, M.C., Hernandez, M.D., Coppola, G.,Geschwind, D.H., Rademakers, R., Lee, S.E., Rosen, H.J., Rabinovici, G.D.,Seeley, W.W., Rankin, K.P., Boxer, A.L., Miller, B.L., 2012. Atypical, slowlyprogressive behavioural variant frontotemporal dementia associated withC9ORF72 hexanucleotide expansion. J. Neurol. Neurosurg. Psychiatry 83,358e364.
Kohli, M.A., John-Williams, K., Rajbhandary, R., Naj, A., Whitehead, P., Hamilton, K.,Carney, R.M., Wright, C., Crocco, E., Gwirtzman, H.E., Lang, R., Beecham, G.,Martin, E.R., Gilbert, J., Benatar, M., Small, G.W., Mash, D., Byrd, G., Haines, J.L.,Pericak-Vance, M.A., Zuchner, S. 2012. Repeat expansions in the C9ORF72 genecontribute to Alzheimer’s disease in Caucasians. Neurobiol. Aging. http://dx.doi.org/10.1016/j.neurobiolaging.2012.10.003.
Laaksovirta, H., Peuralinna, T., Schymick, J.C., Scholz, S.W., Lai, S.L., Myllykangas, L.,Sulkava, R., Jansson, L., Hernandez, D.G., Gibbs, J.R., Nalls, M.A., Heckerman, D.,Tienari, P.J., Traynor, B.J., 2010. Chromosome 9p21 in amyotrophic lateral scle-rosis in Finland: a genome-wide association study. Lancet Neurol. 9, 978e985.
Lindquist, S., Duno, M., Batbayli, M., Puschmann, A., Braendgaard, H., Mardosiene, S.,Svenstrup, K., Pinborg, L., Vestergaard, K., Hjermind, L., Stokholm, J., Andersen,B., Johannsen, P., Nielsen, J. 2012. Corticobasal and ataxia syndromes widen thespectrum of C9ORF72 hexanucleotide expansion disease. Clin. Genet. 9999,http://dx.doi.org/10.1111/j.1399-0004.2012.01903.x.
Mahoney, C.J., Beck, J., Rohrer, J.D., Lashley, T., Mok, K., Shakespeare, T., Yeatman, T.,Warrington, E.K., Schott, J.M., Fox, N.C., Rossor, M.N., Hardy, J., Collinge, J.,Revesz, T., Mead, S., Warren, J.D., 2012. Frontotemporal dementia with theC9ORF72 hexanucleotide repeat expansion: clinical, neuroanatomical andneuropathological features. Brain 135, 736e750.
Majounie, E., Abramzon, Y., Renton, A.E., Perry, R., Bassett, S.S., Pletnikova, O.,Troncoso, J.C., Hardy, J., Singleton, A.B., Traynor, B.J., 2012a. Repeat expansion inC9ORF72 in Alzheimer’s disease. N. Engl. J. Med. 366, 283e284.
Majounie, E., Renton, A.E., Mok, K., Dopper, E.G., Waite, A., Rollinson, S., Chio, A.,Restagno, G., Nicolaou, N., Simon-Sanchez, J., van Swieten, J.C., Abramzon, Y.,Johnson, J.O., Sendtner, M., Pamphlett, R., Orrell, R.W., Mead, S., Sidle, K.C.,Houlden, H., Rohrer, J.D., Morrison, K.E., Pall, H., Talbot, K., Ansorge, O.,Hernandez, D.G., Arepalli, S., Sabatelli, M., Mora, G., Corbo, M., Giannini, F.,Calvo, A., Englund, E., Borghero, G., Floris, G.L., Remes, A.M., Laaksovirta, H.,
R. Cacace et al. / Neurobiology of Aging 34 (2013) 1712.e1e1712.e71712.e7
McCluskey, L., Trojanowski, J.Q., Van Deerlin, V.M., Schellenberg, G.D.,Nalls, M.A., Drory, V.E., Lu, C.S., Yeh, T.H., Ishiura, H., Takahashi, Y., Tsuji, S.,Le Ber, I., Brice, A., Drepper, C., Williams, N., Kirby, J., Shaw, P., Hardy, J.,Tienari, P.J., Heutink, P., Morris, H.R., Pickering-Brown, S., Traynor, B.J., 2012b.Frequency of the C9orf72 hexanucleotide repeat expansion in patients withamyotrophic lateral sclerosis and frontotemporal dementia: a cross-sectionalstudy. Lancet Neurol. 11, 323e330.
McKhann, G., Drachman, D., Folstein, M., Katzman, R., Price, D., Stadlan, E.M., 1984.Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA WorkGroup under the auspices of Department of Health and Human Services TaskForce on Alzheimer’s Disease. Neurology 34, 939e944.
Murray, M.E., DeJesus-Hernandez, M., Rutherford, N.J., Baker, M., Duara, R., Graff-Radford, N.R., Wszolek, Z.K., Ferman, T.J., Josephs, K.A., Boylan, K.B.,Rademakers, R., Dickson, D.W., 2011. Clinical and neuropathologic heterogeneityof c9FTD/ALS associated with hexanucleotide repeat expansion in C9ORF72.Acta Neuropathol. 122, 673e690.
Petersen, R.C., 2004. Mild cognitive impairment as a diagnostic entity. J. Intern. Med.256, 183e194.
Rademakers, R., Dermaut, B., Peeters, K., Cruts, M., Heutink, P., Goate, A., VanBroeckhoven, C., 2003. Tau (MAPT) mutation Arg406Trp presenting clinicallywith Alzheimer disease does not share a common founder in Western Europe.Hum. Mutat. 22, 409e411.
Renton, A.E., Majounie, E., Waite, A., Simon-Sanchez, J., Rollinson, S., Gibbs, J.R.,Schymick, J.C., Laaksovirta, H., van Swieten, J.C., Myllykangas, L., Kalimo, H.,Paetau, A., Abramzon, Y., Remes, A.M., Kaganovich, A., Scholz, S.W.,Duckworth, J., Ding, J., Harmer, D.W., Hernandez, D.G., Johnson, J.O., Mok, K.,Ryten, M., Trabzuni, D., Guerreiro, R.J., Orrell, R.W., Neal, J., Murray, A.,Pearson, J., Jansen, I.E., Sondervan, D., Seelaar, H., Blake, D., Young, K.,Halliwell, N., Callister, J.B., Toulson, G., Richardson, A., Gerhard, A., Snowden, J.,Mann, D., Neary, D., Nalls, M.A., Peuralinna, T., Jansson, L., Isoviita, V.M.,Kaivorinne, A.L., Holtta-Vuori, M., Ikonen, E., Sulkava, R., Benatar, M., Wuu, J.,Chio, A., Restagno, G., Borghero, G., Sabatelli, M., Heckerman, D., Rogaeva, E.,Zinman, L., Rothstein, J.D., Sendtner, M., Drepper, C., Eichler, E.E., Alkan, C.,Abdullaev, Z., Pack, S.D., Dutra, A., Pak, E., Hardy, J., Singleton, A., Williams, N.M.,Heutink, P., Pickering-Brown, S., Morris, H.R., Tienari, P.J., Traynor, B.J., 2011.A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome9p21-linked ALS-FTD. Neuron 72, 257e268.
Rollinson, S., Halliwell, N., Young, K., Callister, J.B., Toulson, G., Gibbons, L.,Davidson, Y.S., Robinson, A.C., Gerhard, A., Richardson, A., Neary, D., Snowden, J.,Mann, D.M., Pickering-Brown, S.M., 2012. Analysis of the hexanucleotide repeatin C9ORF72 in Alzheimer’s disease. Neurobiol. Aging 33, 1846.e5e6.
Satoh, J.I., Tabunoki, H., Ishida, T., Saito, Y., Arima, K., 2012. Dystrophic neuritesexpress C9orf72 in Alzheimer’s disease brains. Alzheimers Res. Ther. 4, 33.
Shatunov, A., Mok, K., Newhouse, S., Weale, M.E., Smith, B., Vance, C., Johnson, L.,Veldink, J.H., van Es, M.A., van den Berg, L.H., Robberecht, W., Van, D.P.,Hardiman, O., Farmer, A.E., Lewis, C.M., Butler, A.W., Abel, O., Andersen, P.M.,Fogh, I., Silani, V., Chio, A., Traynor, B.J., Melki, J., Meininger, V., Landers, J.E.,McGuffin, P., Glass, J.D., Pall, H., Leigh, P.N., Hardy, J., Brown Jr., R.H., Powell, J.F.,Orrell, R.W., Morrison, K.E., Shaw, P.J., Shaw, C.E., Al-Chalabi, A., 2010. Chro-mosome 9p21 in sporadic amyotrophic lateral sclerosis in the UK and sevenother countries: a genome-wide association study. Lancet Neurol. 9, 986e994.
Snowden, J.S., Rollinson, S., Thompson, J.C., Harris, J.M., Stopford, C.L.,Richardson, A.M., Jones, M., Gerhard, A., Davidson, Y.S., Robinson, A., Gibbons, L.,Hu, Q., DuPlessis, D., Neary, D., Mann, D.M., Pickering-Brown, S.M., 2012.Distinct clinical and pathological characteristics of frontotemporal dementiaassociated with C9ORF72 mutations. Brain 135, 693e708.
Stewart, H., Rutherford, N.J., Briemberg, H., Krieger, C., Cashman, N., Fabros, M.,Baker, M., Fok, A., DeJesus-Hernandez, M., Eisen, A., Rademakers, R.,Mackenzie, I.R., 2012. Clinical and pathological features of amyotrophic lateralsclerosis caused by mutation in the C9ORF72 gene on chromosome 9p. ActaNeuropathol. 123, 409e417.
van der Zee, J., Gijselinck, I., Dillen, L., Van Langenhove, T., Theuns, J., Engelborghs, S.,Philtjens, S., Vandenbulcke, M., Sleegers, K., Sieben, A., Baumer, V., Maes, G.,Corsmit, E., Borroni, B., Padovani, A., Archetti, S., Perneczky, R., Diehl-Schmid, J.,de, M.A., Miltenberger-Miltenyi, G., Pereira, S., Pimentel, J., Nacmias, B., Bagnoli,S., Sorbi, S., Graff, C., Chiang, H.H., Westerlund, M., Sanchez-Valle, R., Llado, A.,Gelpi, E., Santana, I., Almeida, M.R., Santiago, B., Frisoni, G., Zanetti, O., Bonvicini,C., Synofzik, M., Maetzler, W., vom Hagen, J.M., Schols, L., Heneka, M.T., Jessen, F.,Matej, R., Parobkova, E., Kovacs, G.G., Strobel, T., Sarafov, S., Tournev, I., Jorda-nova, A., Danek, A., Arzberger, T., Fabrizi, G.M., Testi, S., Salmon, E., Santens, P.,Martin, J.J., Cras, P., Vandenberghe, R., De Deyn, P.P., Cruts, M., Van BroeckhovenC. 2012. A Pan-European study of the C9orf72 Repeat Associated with FTLD:Geographic Prevalence, Genomic Instability and Intermediate Repeats. Hum.Mutat, http://dx.doi.org/10.1002/humu.22244.
van Es, M.A., Veldink, J.H., Saris, C.G., Blauw, H.M., van Vught, P.W., Birve, A.,Lemmens, R., Schelhaas, H.J., Groen, E.J., Huisman, M.H., van der Kooi, A.J.,de, V.M., Dahlberg, C., Estrada, K., Rivadeneira, F., Hofman, A., Zwarts, M.J., vanDoormaal, P.T., Rujescu, D., Strengman, E., Giegling, I., Muglia, P., Tomik, B.,Slowik, A., Uitterlinden, A.G., Hendrich, C., Waibel, S., Meyer, T., Ludolph, A.C.,Glass, J.D., Purcell, S., Cichon, S., Nothen, M.M., Wichmann, H.E., Schreiber, S.,Vermeulen, S.H., Kiemeney, L.A., Wokke, J.H., Cronin, S., McLaughlin, R.L.,Hardiman, O., Fumoto, K., Pasterkamp, R.J., Meininger, V., Melki, J., Leigh, P.N.,Shaw, C.E., Landers, J.E., Al-Chalabi, A., Brown Jr., R.H., Robberecht, W.,Andersen, P.M., Ophoff, R.A., van den Berg, L.H., 2009. Genome-wide associationstudy identifies 19p13.3 (UNC13A) and 9p21.2 as susceptibility loci for sporadicamyotrophic lateral sclerosis. Nat. Genet. 41, 1083e1087.
Wallon, D., Rovelet-Lecrux, A., Deramecourt, V., Pariente, J., Auriacombe, S., Le Ber, I.,Schraen, S., Pasquier, F., Campion, D., Hannequin, D., 2012. Definite behavioralvariant of frontotemporal dementia with C9ORF72 expansions despite positiveAlzheimer’s disease cerebrospinal fluid biomarkers. J. Alzheimers Dis. 32,19e22.
Weckx, S., Del Favero, J., Rademakers, R., Claes, L., Cruts, M., De Jonghe, P., VanBroeckhoven, C., De Rijk, P., 2005. novoSNP, a novel computational tool forsequence variation discovery. Genome Res. 15, 436e442.
Xi, Z., Zinman, L., Grinberg, Y., Moreno, D., Sato, C., Bilbao, J.M., Ghani, M.,Hernandez, I., Ruiz, A., Boada, M., Moron, F.J., Lang, A.E., Marras, C., Bruni, A.,Colao, R., Maletta, R.G., Puccio, G., Rainero, I., Pinessi, L., Galimberti, D.,Morrison, K.E., Moorby, C., Stockton, J.D., Masellis, M., Black, S.E., Hazrati, L.N.,Liang, Y., van Haersma de, W.J., Fornazzari, L., Villagra, R., Rojas-Garcia, R.,Clarimon, J., Mayeux, R., Robertson, J., St George-Hyslop, P., Rogaeva, E., 2012.Investigation of C9orf72 in 4 Neurodegenerative Disorders. Arch. Neurol. 69,1583e1590.