Epigenetic Inheritance and the Intergenerational Transfer of ...
Autosomal Dominant Inheritance of Centrotemporal Sharp Waves in Rolandic Epilepsy Families
Transcript of Autosomal Dominant Inheritance of Centrotemporal Sharp Waves in Rolandic Epilepsy Families
Autosomal Dominant Inheritance of Centrotemporal Sharp Wavesin Rolandic Epilepsy Families
Bhavna Bali*, Lewis L. Kull†, Lisa J. Strug‡, Tara Clarke*, Peregrine L. Murphy*, Cigdem I.Akman†, David A. Greenberg‡,§, and Deb K. Pal*,‡,§
*Department of Epidemiology, Columbia University, New York, New York, U.S.A.
†Department of Neurology, Columbia University, New York, New York, U.S.A.
§Department of Psychiatry, Columbia University, New York, New York, U.S.A.
‡Department of Division of Statistical Genetics, Columbia University, New York, New York, U.S.A.
SUMMARYPurpose: Centrotemporal sharp (CTS) waves, the electroencephalogram (EEG) hallmark ofrolandic epilepsy, are found in approximately 4% of the childhood population. The inheritance ofCTS is presumed autosomal dominant but this is controversial. Previous studies have variedconsiderably in methodology, especially in the control of bias and confounding. We aimed to testthe hypothesis of autosomal dominant inheritance of CTS in a well-designed family segregationanalysis study.
Methods: Probands with rolandic epilepsy were collected through unambiguous singleascertainment. Siblings in the age range 4–16 years underwent sleep-deprived EEG; observationsfrom those who remained awake were omitted. CTS were rated as present or absent by two indepen-dent observers blinded to the study hypothesis and subject identities. We computed the segregationratio of CTS, corrected for ascertainment. We tested the segregation ratio estimate for consistencywith dominant and recessive modes of inheritance, and compared the observed sex ratio of thoseaffected with CTS for consistency with sex linkage.
Results: Thirty siblings from 23 families under-went EEG examination. Twenty-three showedevidence of sleep in their EEG recordings. Eleven of 23 recordings demonstrated CTS, yielding acorrected segregation ratio of 0.48 (95% CI: 0.27–0.69). The male to female ratio of CTS affectednesswas approximately equal.
Conclusions: The segregation ratio of CTS in rolandic epilepsy families is consistent with a highlypenetrant autosomal dominant inheritance, with equal sex ratio. Autosomal recessive and X-linkedinheritance are rejected. The CTS locus might act in combination with one or more loci to producethe phenotype of rolandic epilepsy.
KeywordsCentrotemporal; Rolandic; Focal sharp wave; Epilepsy; Genetic; Family; EEG; Segregation
Address correspondence and reprint requests to Dr. Deb K. Pal, Mailman School of Public Health, Columbia University, 722 West 168thStreet, Sixth floor, New York, NY 10032. E-mail: [email protected] authors declare that they have no competing financial interests. The study was conceived and designed by DKP. Data collection andprocessing was performed by BB, TC, LLK, and CIA. BB, LS, TC, DKP conducted the analysis. BB wrote the first draft. All authorstook part in revising the manuscript for the final draft.
NIH Public AccessAuthor ManuscriptEpilepsia. Author manuscript; available in PMC 2007 December 20.
Published in final edited form as:Epilepsia. 2007 December ; 48(12): 2266–2272.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Focal sharp waves (FSWs) on the surface electroencephalogram (EEG) are a common (1.6–3.5%) finding in early to mid-childhood (Eeg-Olofsson et al., 1971; Okubo et al., 1994).Although they can be found in asymptomatic children, they are particularly associated withidiopathic focal epilepsy syndromes and have been noted in other epileptic encephalopathiesincluding Landau-Kleffner syndrome (Doose et al., 1996). FSWs are inconstant: they maydisappear from one location or other in serial EEGs, and appear to migrate from posterior toanterior regions with maturation (Gibbs et al., 1954). They may occur only in non-rapid eyemovement (NREM) sleep, not in a waking state or in rapid eye movement (REM) sleep, but,if FSW are present awake, they are also dramatically increased in Stage II sleep (Kellaway,1985; Nobili et al., 1999).
The discovery of FSW in the centrotemporal region in 4–16-year-old children, a finding sanssignificance focale, was the first milestone in the history of rolandic epilepsy (Gastaut, 1952).A few years later, focal seizures were described in association with these “centrotemporal sharpwaves” (CTS). This was the origin of the electro-clinical syndrome of rolandic epilepsy orbenign epilepsy with centrotemporal spikes (BECTS) (Nayrac and Beaus-sart, 1958). Manyauthors have noted the presence of CTS in siblings of children with rolandic epilepsy,suggesting a genetic cause, but the precise mode of inheritance of CTS is debated, as is thegenetic basis of rolandic epilepsy (Ottman, 1989; Vadlamudi et al., 2004; Bali et al., 2005;Vadlamudi et al., 2006). The debate largely stems from the difficulty in evaluating andcomparing studies that have used different methods of case selection, varying protocols forEEG measurement, and different analytical approaches for assessing mode of inheritance(Rodin and Whelan, 1960; Bray and Wiser, 1964, 1965a, 1965b; Rodin and Gonzalez, 1966;Heijbel et al., 1975; Doose et al., 1977; 2001; Gerken et al., 1977).
The aim of this study was to test the hypothesis of an autosomal dominant mode of inheritancefor CTS in siblings of children with stringently defined rolandic epilepsy. Determining thelikely mode of inheritance of CTS in families of rolandic epilepsy probands will be invaluablefor (1) detecting susceptibility loci by genetic linkage analysis; (2) estimating the exact geneticparameters of susceptibility gene(s) for CTS; as well as for (3) investigating the etiology ofother CTS-associated syndromes.
MethodsAscertainment
Subjects with a probable diagnosis of rolandic epilepsy were recruited from pediatric neurologycenters in the northeastern United States. Subjects and their biological relatives were eligibleto take part in a genetic linkage study, providing that the proband satisfied strict diagnosticcriteria (below). Both parents were required to be available. Ascertainment was strictly single,i.e., all families were identified only once and through a single affected offspring (the proband).
Operational definitionsThe definition of rolandic epilepsy was based on international criteria described by theInternational League Against Epilepsy (Commission on Classification and Terminology of theInternational League Against Epilepsy, 1989), with age of onset between 3 and 12 years. Forthe purposes of genetic study, we required both a typical history of focal, orofacial seizures,and an interictal EEG showing centrotemporal sharp or spike waves in standard leads C3, C4,T3, or T4. Hence children with only a history of a secondary generalized seizure, even withsuggestive EEG features, were not eligible. Neuroimaging had to exclude a structural,inflammatory, or metabolic cause for the seizures.
Bali et al. Page 2
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Data collectionCharts of potentially eligible subjects were first screened by a pediatric neurologist (DKP).The parents of eligible subjects, and the children when age-appropriate, were then interviewedat home by one of the authors (BB, TC, DKP) for a detailed seizure, perinatal, developmental,medical, and family history, using a 125-item questionnaire designed for the study. Siblingsin the age range 4–16 years unaffected by seizures were invited to undergo sleep deprived EEGrecording as part of the study. EEG results were not routinely shared with parents. All subjectsgave written informed consent or assent. The study was approved by the institutional reviewboard of New York State Psychiatric Institute, Columbia University Medical Center and allparticipating centers.
SampleTwenty-three families had at least one sibling in the age range 4–16 years. None of the parentswere consanguineous. The 23 probands comprised 17 boys and six girls. There were 40 siblingsin these 23 families, of which 30 were in the age range 4–16 years. These 30 siblings wereasked to undergo sleep deprived EEG recordings as described below.
EEG recordingSiblings between the ages of 4 and 16 years had sleep-deprived EEGs according to thefollowing protocol: (1) 4 h or less sleep the night before; (2) a 60-min digital recordingincluding awake and sleep segments; (3) international 10–20 system electrode placement; (4)activation procedures including hyperventilation, eye closure, and photic stimulation.Recordings were performed by trained technologists in pediatric EEG laboratories.
EEG classificationAll study EEGs were saved onto disk and reviewed firstly by a senior electroencephalographer(LLK), and secondly by a pediatric epileptologist board certified in clinical neurophysiology(CIA). Both observers were blind to subject identity, diagnosis, proband or sibling status, andstudy hypothesis. Age and sex information were available to allow assessment of maturationalfeatures. EEGs were classified according to the appropriateness of background features forage; presence of features indicating sleep state (spindles, etc); response to activationprocedures; presence of focal discharges by morphology, distribution and duration; andadditional features associated with generalized seizures such as 3 Hz or generalized spike-and-wave (GSW).
Statistical analysisSiblings' EEG classifications were dichotomized according to the presence or absence of CTS.Observations from siblings who did not fall asleep were omitted. We calculated the segregationratio (in this case, the proportion of offspring in the families with CTS in the age range 4–16years), applying the Weinberg correction for ascertainment bias under single selection (whichexcludes the probands) (Weinberg, 1912). This proportion represents a point estimate of thesegregation ratio for the CTS trait, around which we computed 95% confidence intervals. Wealso examined sex ratios among siblings to test hypotheses about sex-linked inheritance.
ResultsThirty siblings underwent EEG examinations: 14 boys and 16 girls of median age 10.3 years,range 4.5–15.6 years. Seven siblings were fully awake during their EEG recording, despitesleep deprivation; 16 fell into Stage I or II sleep during their EEG; and seven showed EEGevidence of Stage III or IV sleep in their recordings (Table 1). All EEG classifications werecompletely concordant between the two observers.
Bali et al. Page 3
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
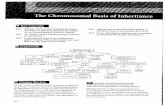
Seizures and EEG abnormalitiesThirteen of the 30 siblings showed CTS. Two of these 13 siblings developed rolandic epilepsyduring the period of the study, one boy and one girl. The other 11 siblings, five boys and sixgirls, showed CTS of typical morphology (Kellaway, 2000) in the EEG record (Fig. 1). Theobservation of CTS as a function of the deepest sleep stage achieved is shown in Table 1. Threeof the 13 CTS positive siblings only showed CTS in sleep stages III/IV. CTS showedpredominantly left-sided distribution in 7 siblings and right-sided in 6 siblings. Threeindividuals showed FSW in temporal and extratemporal areas in addition to CTS. Two siblingsshowed GSW bursts in addition to CTS, but none had GSW alone. Seventeen siblings showedneither CTS nor GSW on EEG.
Segregation ratioIn total, 13 of 30 siblings exhibited FSWs, all of them centrotemporal, on their EEG recordings.We omitted, from the calculation of the segregation ratio, the observations of seven subjectswho did not fall asleep, two of whom showed CTS. Thus we estimated a segregation ratio forCTS of 11/23 or 0.48, with a 95% confidence interval of 0.27–0.69.
DiscussionOur results confirm the strong familial aggregation of CTS in siblings of rolandic epilepsyprobands. Our estimated segregation ratio of 0.48 is consistent with a monogenic autosomaldominant inheritance with high penetrance, and is inconsistent with autosomal recessiveinheritance. The approximately equal sex ratio of CTS affectedness among siblings makes acompletely sex-linked mode of inheritance unlikely. The inheritance of CTS is clearly notidentical to the inheritance of rolandic epilepsy, although an autosomal dominant CTS locuswould necessarily comprise a part of the etiology of rolandic epilepsy.
This is the first study of CTS inheritance, which provides strict consideration of confounders,and methodological issues such as phenotype definition, ascertainment bias, and measurementerror. We adopted a stringent and consistently homogeneous proband definition for rolandicepilepsy, which included orofacial sensorimotor features and excluded secondarily generalizedseizures. We recruited only those patients with rolandic epilepsy who satisfied our stringenteligibility criteria for genetic study. The reason for this is to limit the possibility of geneticheterogeneity in the sample. Thus, requiring a witnessed history of an orofacial seizure meansthat we rejected 75% of referred patients who only had a history of secondary generalizationor could not provide a clear-cut description of the typical orofacial progression. Ascertainmentwas based on the occurrence of rolandic epilepsy only in the proband, regardless of the familyconfiguration or number of affected members in the family. Our ascertainment scheme wastherefore not biased in favor of densely affected pedigrees, a strategy that biases towardcollection of pedigrees expressing autosomal dominant disease forms (Durner et al., 1992; Paland Greenberg, 2002). We used the method for correcting ascertainment bias under singleascertainment that excludes the probands. Ascertainment bias occurs when at-risk families canonly be identified through affected offspring. Thus at-risk families without affected offspringcannot be ascertained, and that censoring must be corrected. We also excluded from the studythose siblings who, because of their age, would have a low probability of having CTS detectableon brief, extracranial EEG. Lastly, we excluded the observations of siblings who did not showsigns of sleep on the EEG in order to control the main confounding variable, arousal stateduring EEG. Our estimate of segregation ratio is therefore the most robust to date. Theenormous methodological variation in previous studies makes it difficult to make comparisons,or to pool data for meta-analysis. Below, we discuss some of the methodological issues thathave biased or confounded prior estimates of the CTS segregation ratio.
Bali et al. Page 4
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
The fundamental variable in studying the segregation of CTS in RE is the definition of theproband. Although CTS occurs in various clinical scenarios including developmentaldisorders, epilepsies and in asymptomatic children, one cannot assume that the inheritance ofCTS is identical in each scenario, especially because the morphology of CTS differs for eachsyndrome. Thus, there needs to be strict homogeneity in the ascertainment criteria for probandsto obtain an accurate estimate of CTS segregation. This has not generally been the case (Table2). For example, some authors have included children with headache, abdominal pain, learning,and behavioral problems (Bray and Wiser, 1964;Degen and Degen, 1992;Doose et al., 1997).Others have included various types of epilepsy or seizure types: generalized seizures (Brayand Wiser, 1964;Heijbel et al., 1975;Degen and Degen, 1992), with a high prevalence of GSWabnormality in the siblings (Degen and Degen, 1992); temporal lobe epilepsy (Gerken et al.,1977); atypical benign partial epilepsy (Doose et al., 2001); or nonspecific seizures (Doose etal., 1997). Segregation estimates may also have been heavily influenced by well-knownconfounding factors such as the sleep stage of the EEG, and age.
Sleep profoundly influences the sensitivity of the EEG for detecting FSWs (Kellaway, 1985;Nobili et al., 1999). Sleep doubles the detection of FSWs in the EEG (Gibbs and Gibbs,1947; Blom and Heijbel, 1975; Degen and Degen, 1992) and increases the discharge rate byone or two orders of magnitude (Kellaway, 2000). By not performing sleep studies, or by notreporting the sleep stage reached in EEG recordings, the extent of confounding by sleep stagecannot be judged (Table 2). It is notable that the two of the lowest estimates of CTS prevalencein siblings comes from studies in which awake only EEG recordings were performed (Okuboet al., 1994; Doose et al., 1997). Confounding by sleep stage can be dealt with most easily byomitting the observations of subjects who did not fall asleep.
Age is another important confounder, but its effect is not linear. CTS begin to appear in theEEG at about three years of age, peaking between 5 and 10 years, almost disappearing afterpuberty (Beaussart, 1972; Degen and Degen, 1990). Hence, EEGs recorded before the age ofthree or after the age of 16 have low sensitivity for detecting CTS, even if subjects truly carrythe CTS trait. Subjects outside the peak age range who are included in the calculation ofsegregation serve to falsely reduce the segregation ratio (Table 2). Age confounding is bestdealt with at the study design stage, by excluding subjects out of age range for FSW.
The calculation of the segregation ratio is not straight-forward, because of confusion aboutappropriate methods for ascertainment adjustment, depending on the different samplingschemes (Nicholas, 1982). In one of the earliest attempts to define the transmission of CTS, asegregation ratio was calculated using only those families in which a sibling showed CTS, andexcluding families in which siblings did not show CTS (Bray and Wiser, 1964, 1965a). Laterattempts (Heijbel et al., 1975) used adjustment methods for complete ascertainment (Bernstein,1925) (when all affected people in the population are included for study) when data had beencollected by single ascertainment (Weinberg, 1912).
Despite the enormous variation in experimental methods, our results are not inconsistent withprevious studies of CTS inheritance in rolandic epilepsy families. Our results support thetransmission of CTS as an autosomal dominant trait with high penetrance and strongly suggestsa major genetic influence on the CTS component of RE (Vadlamudi et al., 2004). AlthoughCTS is a necessary feature of rolandic epilepsy, it is clear that rolandic epilepsy is notgenetically identical to CTS. Instead, it is likely that rolandic epilepsy has a complex geneticinheritance, with the CTS locus as one of the mandatory contributing genes. This idea issupported by familial studies, unequal sex ratio, and comorbidity with other traits. First, asibling RE prevalence of 10% or so is obviously inconsistent with a fully penetrant autosomaldominant inheritance for RE. However, it could be consistent with a reduced penetrance
Bali et al. Page 5
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
autosomal dominant gene, with the reduced penetrance explained by interaction with othergene(s).
Second, RE shows a consistent male excess of 3:2 (studies summarized in (Luders et al.,1987), page 309), which contrasts with an equal population sex ratio of CTS (Eeg-Olofsson etal., 1971; Okubo et al., 1994). To produce a male excess, there must be a hypotheticalinteracting locus, which itself or via its effects, may be sex-linked, sex-limited, or demonstratesome other mechanism of preponderant male expression.
Last, hypothetical interacting loci are further suggested by the comorbidity of rolandic epilepsywith reading disability (Staden et al., 1998; Carlsson et al., 2000; Lindgren et al., 2004;Northcott et al., 2005; Clarke et al., 2006; Pinton et al., 2006), and the less well-knowncomorbidity with speech sound disorder (Bladin, 1987; Doose, 1989; Clarke et al., 2006). Allthree traits exhibit a male bias, may be genetically transmitted, and are anatomically colocalizedto the perisylvian region. These interesting hypotheses about the inheritance of the CTS locusand of possible interacting loci will be tested by linkage analysis.
Acknowledgments
Our thanks to the families participating in the IRELAND study (http://www.rolandic.com) and to the IRELAND StudyConsortium who referred patients to the study: William D. Brown, MD, John Gaitanis, MD, Karameh Hawash, MD,Steven L. Kugler, MD, Linda Leary, MD, David E. Mandelbaum, MD, PhD, Steven M. Wolf, MD, Maria Younes,MD. We are grateful to Lynne Capuano, Somaria Persaud, and other technicians who recorded sleep EEGs. Our thanksalso to Joshua Cappell, MD, for reviewing and selecting EEG records for publication. This study was supported bymembers of the Partnership for Pediatric Epilepsy Research, which includes the American Epilepsy Society, theEpilepsy Foundation, Anna and Jim Fantaci, Fight Against Childhood Epilepsy and Seizures (FACES), NeurotherapyVentures Charitable Research Fund, and Parents Against Childhood Epilepsy (PACE) (DKP); the Epilepsy Foundationthrough the generous support of the Charles L. Shor Foundation for Epilepsy Research, Inc (DKP); National Institutesof Health grants NS047530 (DKP), NS27941 (DAG), MH48858 (DAG), DK31775 (DAG).
ReferencesBali B, Kugler SL, Pal DK. Genetic influence on Rolandic epilepsy. Ann Neurol 2005;57:464–465.
[PubMed: 15732105]Beaussart M. Benign epilepsy of children with Rolandic (centro-temporal) paroxysmal foci: a clinical
entity. Study of 221 cases. Epilepsia 1972;13:795–811. [PubMed: 4509173]Bernstein F. Zusammenfassende Betrachtungen uber die erblichen und Blutstrukturen des Menschen. Z
indukt Abstamm u VerebLehre 1925;37:237–270.Bladin, PF. The association of benign rolandic epilepsy with migraine. In: Andermann, F.; Lugharesi,
E., editors. Migraine and Epilepsy. Butterworths; Boston: 1987.Blom S, Heijbel J. Benign epilepsy of children with centro-temporal EEG foci. Discharge rate during
sleep. Epilepsia 1975;16:133–140. [PubMed: 1122897]Bray P, Wiser WC. Evidence for a genetic etiology of temporal central abnormalities in focal epilepsy.
N Eng J Med 1964;271:926.Bray PF, Wiser WC. Hereditary characteristics of familial temporal-central focal epilepsy. Pediatrics
1965a;36:207–211. [PubMed: 14320029]Bray PF, Wiser WC. The relation of focal to diffuse epileptiform EEG discharges in genetic epilepsy.
Arch Neurol 1965b;13:223–237. [PubMed: 5832260]Carlsson G, Igelbrink-Schulze N, Neubauer BA, Stephani U. Neuropsychological long-term outcome of
rolandic EEG traits. Epileptic Disord 2000;2:S63–S66. [PubMed: 11231228]Choy, YS.; Tan, CT.; Omar, A. Families with benign childhood epilepsy with centro-temporal spikes.
In: Berkovic, SF.; Genton, P.; Hirsch, E.; Picard, F., editors. Genetics of focal epilepsies: clinicalaspects and molecular biology. John Libbey and Company Limited; 1999.
Clarke T, Bali B, Carvalho J, Foster S, Tremont G, Hawash K, Strug L, Murphy PL, Dorta N, Pal DK.Speech and language disorders aggregate in Rolandic epilepsy families. Neuropediatrics 2006;37:60.
Bali et al. Page 6
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Commission on Classification and Terminology of The International League Against. Proposal forrevised classification of epilepsies and epileptic syndromes. Epilepsia 1989;30:389–399. [PubMed:2502382]
Degen R, Degen HE. Some genetic aspects of rolandic epilepsy: waking and sleep EEGs in siblings.Epilepsia 1990;31:795–801. [PubMed: 2123156]
Degen, R.; Degen, HE. Contribution to the genetics of Rolandic epilepsy: waking and sleep EEGs insiblings. In: Degen, R.; Dreifuss, FE., editors. Benign localized and generalized epilepsies of earlychildhood. Elsevier Science; New York: 1992.
Doose H. Symptomatology in children with focal sharp waves of genetic origin. Eur J Pediatr1989;149:210–215. [PubMed: 2482185]
Doose H, Gerken H, Kiefer R, Volkze E. Genetic factors in childhood epilepsy with focal sharp waves.II. EEG findings in patients and siblings. Neuropadiatrie 1977;8:10–20. [PubMed: 403481]
Doose H, Neubauer B, Carlsson G. Children with benign focal sharp waves in the EEG—developmentaldisorders and epilepsy. Neuropediatrics 1996;27:227–241. [PubMed: 8971743]
Doose H, Brigger-Heuer B, Neubauer B. Children with focal sharp waves: clinical and genetic aspects.Epilepsia 1997;38:788–796. [PubMed: 9579906]
Doose H, Hahn A, Neubauer BA, Pistohl J, Stephani U. Atypical “benign” partial epilepsy of childhoodor pseudo-lennox syndrome. Part II: family study. Neuropediatrics 2001;32:9–13. [PubMed:11315204]
Durner M, Greenberg DA, Hodge SE. Inter- and intrafamilial heterogeneity: effective sampling strategiesand comparison of analysis methods. Am J Hum Genet 1992;51:859–870. [PubMed: 1415227]
Eeg-Olofsson O, Petersen I, Sellden U. The development of the electroencephalogram in normal childrenfrom the age of 1 through 15 years. Paroxysmal activity. Neuropadiatrie 1971;2:375–404. [PubMed:5171489]
Gastaut Y. Un element deroutant de la semeiologie electroencephalographique: les pointes prerolandiquessans signification focale. Rev Neurol 1952;99:489–490.
Gerken H, Kiefer R, Doose H, Volkze E. Genetic factors in childhood epilepsy with focal sharp waves.1 Clinical data and familial morbidity for seizures. Neuropadiatrie 1977;8:3–9. [PubMed: 403482]
Gibbs EL, Gibbs FA. Diagnostic and localizing value of electroencephalographic studies in sleep. ResPubl Assoc Res Nerv Ment Dis 1947;26:366–376.
Gibbs EL, Gillen HW, Gibbs FA. Disappearance and migration of epileptic foci in childhood. Am J DisChild 1954;88:596–603.
Heijbel J, Blom S, Rasmuson M. Benign epilepsy of childhood with centrotemporal EEG foci: a geneticstudy. Epilepsia 1975;16:285–293. [PubMed: 807473]
Kellaway P. Sleep and epilepsy. Epilepsia 1985;26(Suppl 1):S15–S30. [PubMed: 3922748]Kellaway P. The electroencephalographic features of benign centrotemporal (Rolandic) epilepsy of
childhood. Epilepsia 2000;41:1053–1056. [PubMed: 10961638]Lindgren S, Kihlgren M, Melin L, Croona C, Lundberg S, Eeg-Olofsson O. Development of cognitive
functions in children with rolandic epilepsy. Epilepsy Behav 2004;5:903–910. [PubMed: 15582839]Luders, HO.; Lesser, RP.; Dinner, RS.; Morris, HH. Benign focal epilepsy of childhood. In: Luders, HO.;
Lesser, RP., editors. Epilepsy: electroclinical syndromes. Springer; Berlin: 1987.Nayrac P, Beaussart M. Pre-rolandic spike-waves: a very peculiar EEG reading; electroclinical study of
21 cases. Rev Neurol (Paris) 1958;99:201–206. [PubMed: 13624406]Nicholas FW. Simple segregation analysis: a review of its history and terminology. J Hered 1982;73:444–
450. [PubMed: 7153496]Nobili L, Baglietto MG, Beelke M, De Carli F, De Negri E, Rosadini G, De Negri M, Ferrillo F.
Modulation of sleep interictal epileptiform discharges in partial epilepsy of childhood. ClinNeurophysiol 1999;110:839–845. [PubMed: 10400197]
Northcott E, Connolly AM, Berroya A, Sabaz M, Mcintyre J, Christie J, Taylor A, Batchelor J, BleaselAF, Lawson JA, Bye AM. The neuropsychological and language profile of children with benignrolandic epilepsy. Epilepsia 2005;46:924–930. [PubMed: 15946332]
Bali et al. Page 7
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Okubo Y, Matsuura M, Asai T, Asai K, Kato M, Kojima T, Toru M. Epileptiform EEG discharges inhealthy children: prevalence, emotional and behavioral correlates, and genetic influences. Epilepsia1994;35:832–841. [PubMed: 8082631]
Ottman R. Genetics of the partial epilepsies: a review. Epilepsia 1989;30:107–111. [PubMed: 2492220]Pal DK, Greenberg DA. Evaluating genetic heterogeneity in complex disorders. Hum Hered
2002;53:216–226. [PubMed: 12435885]Pinton F, Ducot B, Motte J, Arbues AS, Barondiot C, Barthez MA, Chaix Y, Cheminal R, Livet MO,
Penniello MJ, Peudenier S, De Saint-Martin A, Billard C. Cognitive functions in children with benignchildhood epilepsy with centrotemporal spikes (BECTS). Epileptic Disord 2006;8:11–23. [PubMed:16567321]
Rodin EA, Gonzalez S. Hereditary components in epileptic patients. JAMA 1966;198:221–225.[PubMed: 5952917]
Rodin EA, Whelan JL. Familial occurrence of focal temporal electroencephalographic abnormalities.Neurology 1960;10:542–545. [PubMed: 14438168]
Staden U, Isaacs E, Boyd SG, Brandl U, Neville BG. Language dysfunction in children with Rolandicepilepsy. Neuropediatrics 1998;29:242–248. [PubMed: 9810559]
Vadlamudi L, Harvey AS, Connellan MM, Milne RL, Hopper JL, Scheffer IE, Berkovic SF. Is benignrolandic epilepsy genetically determined? Ann Neurol 2004;56:129–132. [PubMed: 15236411]
Vadlamudi L, Kjeldsen MJ, Corey LA, Solaas MH, Friis ML, Pellock JM, Nakken KO, Milne RL,Scheffer IE, Harvey AS, Hopper JL, Berkovic SF. Analyzing the etiology of benign rolandic epilepsy:a multicenter twin collaboration. Epilepsia 2006;47:550–555. [PubMed: 16529620]
Weinberg W. Methode und Fehlerquellen der Untersuchung auf Mendelschen Zahlen beim Menschen.Arch Rass Ges Biol 1912;9:165–174.
Bali et al. Page 8
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Figure 1.EEG of 9-year-old male sibling showing runs of focal sharp waves on right side, bipolarmontage. Epilepsia C ILAE
Bali et al. Page 9
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Bali et al. Page 10
Table 1Centrotemporal sharp waves and sleep stage during EEG in 30 siblings, aged 4–16 years, of 23 rolandic epilepsyprobands
CTS
Deepest sleepstage achieved Not observed Observed TotalAwake only 5 2 7Sleep: stage I/II 8 8 16Sleep: stage III/IV 4 3 7Total 17 13 30
Epilepsia. Author manuscript; available in PMC 2007 December 20.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Bali et al. Page 11Ta
ble
2Fa
mily
stud
ies o
f the
cen
trote
mpo
ral s
pike
wav
e tra
it
Aut
hors
Seiz
ure
defin
ition
EE
Gde
finiti
onN
o.pr
oban
ds,
age,
sex
Typ
e of
rela
tives
Seiz
ures
inre
lativ
esC
TS/
FSW
inre
lativ
esSz
/CT
S in
rela
tives
GSW
a or
othe
rin
rel
ativ
es
Slee
pE
EG
,N
o. o
fE
EG
s
(Bra
yan
dW
iser
,19
64,
1965
a,19
65b)
“Reg
ardl
ess o
f the
natu
re o
f clin
ical
seiz
ure,
mos
tge
nera
lized
, a fe
wps
ycho
mot
or (n
5)
,fo
cal a
nd h
eada
che
or a
bdom
inal
pai
n,an
d 1
patie
nt h
ad‘a
bsen
ce’ e
piso
des”
40 c
ontro
ls h
ad n
one
urol
ogic
alco
mpl
aint
s and
wer
em
atch
ed to
inde
xca
ses b
y ag
e, se
x an
dso
cioe
cono
mic
stat
us
Shar
p w
aves
or s
pike
s in
the
vici
nity
of T
3 or
T4
n 4
0 A
ge,
sex
not
repo
rted,
mix
ture
of
child
ren
and
adul
tsn
40
cont
rols
53 si
blin
gsan
dof
fspr
ing;
21 p
aren
tsof pr
oban
ds15
1si
blin
gsan
dof
fspr
ing
of c
ontro
ls51
par
ents
of c
ontro
ls
Not
repo
rted
19 (3
6%) 4
(19%
) 3 (2
%)
1 (2
%)
19 (
36%
) 4(
19%
) 3 (
2%) 1
( 2%
)
13
%si
blin
gs a
ndof
fspr
ing.
16%
par
ents
.1%
sibl
ings
and
offs
prin
g.2%
par
ents
.
A
wak
ean
d as
leep
seria
l (2–
3)EE
Gs f
orpr
oban
dan
dre
lativ
es.
One
aw
ake
and
asle
epEE
G fo
rco
ntro
ls.
EEG
sin
terp
rete
dbl
ind
toca
se/
cont
rol
stat
us.
(Hei
jbel
et a
l.,19
75)
Parti
al se
izur
es (n
6)
onl
y; a
ndge
nera
lized
seiz
ures
only
(n
13) n
otfu
rther
des
crib
ed
“Rol
andi
c di
scha
rges
”n
19
5–16
yrs 1
0 M
9F
34 si
blin
gsof pr
oban
ds:
6 m
o–18
yrs 3
8pa
rent
s of
prob
ands
5/34
(15%
)al
l RE
4/38
(11%
)
11/3
2 (3
4%) 1
(3%
)11
/34
(32%
)5/
38 (1
3%)
Not
repo
rted
One
aw
ake
and
asle
epEE
G.
(Deg
enan
dD
egen
,19
92)
“Rol
andi
cep
ileps
y” (n
36
:14
“loc
aliz
ed,”
22
only
seco
ndar
yge
nera
lized
);he
adac
hes,
lear
ning
prob
lem
s (n
7)
Cen
trote
mpo
ral s
pike
focu
sn
43
5–18
yrs s
ex n
otre
porte
d
69 sibl
ings
:1–
24 y
rs
5/69
(7%
)no
ne R
E4/
69 (6
%)
7/69
(10%
)21
/69
(30%
)
One
awak
e an
das
leep
EEG
.
(Oku
boet
al.,
1994
)
Hea
lthy
scho
olch
ildre
n ag
ed6–
12 y
rs
Cen
trote
mpo
ral s
harp
wav
esn
37
6–12
yrs 2
6 M
11 F
38 si
blin
gs5/
38 (1
3%)
2/38
(5%
)5/
38 (1
3%)
Not
repo
rted
O
neaw
ake
EEG
onl
y.(D
oose
et a
l.,19
97)
Rol
andi
c se
izur
es(p
eri-o
ral)
(n
32);
othe
r sei
zure
type
s(n
102)
;de
velo
pmen
tal o
rbe
havi
oral
pro
blem
s(n
13)
“Wel
l-stru
ctur
ed sh
arp
wav
es”
in te
mpo
ral,
parie
tal
or o
ccip
ital r
egio
ns
n 1
47 a
geno
tre
porte
d;79
M 5
5 F
242
sibl
ings
145
M 9
7 F
18/2
42 (7
%)
4/44
(9%
) in
RE
sibs
; 0 in
sibs
of s
zfr
eepr
oban
ds
21/1
88 (1
1%)
11
% ?
43/1
88 (2
3%)
Se
rial
(<14
)EE
Gs f
orpr
oban
ds.
One
aw
ake
EEG
onl
yfo
r sib
s.(C
hoy
etal
.,19
99)
Parti
al o
rge
nera
lized
toni
c–cl
onic
seiz
ures
Foca
l mon
omor
phic
, di-,
or
tri-p
hasi
c ro
land
ic sp
ikes
at
T3, T
4, C
3 or
C4
n 3
1 ag
e,se
x no
tre
porte
d
44 sibl
ings
:1–
22 y
rs 2
5M
19
F
6/44
(14%
)5/
43 (1
1%)
CTS
14/
44(3
2%) C
TS/
FSW
15/4
4 (3
4%)
4/44
(9%
)O
ne a
wak
ean
d on
esl
eep
EEG
for s
ibs.
(Doo
seet
al.,
2001
)
Aty
pica
l ben
ign
parti
al e
pile
psy
ofch
ildho
od
Mul
tifoc
al sh
arp
wav
es a
s in
RE
n 4
3 23
M20
F41
sibl
ings
22 M
19
F5/
56 (9
%)
12/4
1 (2
9%)
29
% ?
26%
Aro
usal
stat
e no
tre
porte
d.
CTS
, cen
trote
mpo
ral s
harp
wav
es; E
EG, e
lect
roen
ceph
alog
raph
; FSW
, foc
al sh
arp
wav
es; R
E, ro
land
ic e
pile
psy;
Sz,
seiz
ures
; M, m
ale;
F, f
emal
e.
Epilepsia. Author manuscript; available in PMC 2007 December 20.