Using the ancient past for establishing current threat in poorly inventoried regions
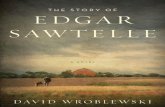
A case series of patients with poorly-tolerated arrhythmias related to a preexcitation syndrome and...
-
Upload
univ-lorraine -
Category
Documents
-
view
4 -
download
0
Transcript of A case series of patients with poorly-tolerated arrhythmias related to a preexcitation syndrome and...
International Journal of Cardiology 174 (2014) 348–354
Contents lists available at ScienceDirect
International Journal of Cardiology
j ourna l homepage: www.e lsev ie r .com/ locate / i j ca rd
A case series of patients with poorly-tolerated arrhythmias relatedto a preexcitation syndrome and presenting with atypical ECG
Béatrice Brembilla-Perrot 1, Jean Marc Sellal, Arnaud Olivier, Vladimir Manenti, Daniel Beurrier,Bassam Al Jouma, Marius Andronache, Christian de Chillou, Nicolas Girerd, Thibaut VilleminDepartment of Cardiology, University Hospital of Brabois, Vandoeuvre Les Nancy, France
E-mail address: [email protected] (B. B1 Cardiology, University Hospital of Brabois, 54500 V
Tel.: +33 3 83 15 32 56; fax: +33 3 83 15 42 26.
http://dx.doi.org/10.1016/j.ijcard.2014.04.1140167-5273/© 2014 Elsevier Ireland Ltd. All rights reserved
a b s t r a c t
a r t i c l e i n f oArticle history:Received 18 February 2014Received in revised form 25 March 2014Accepted 9 April 2014Available online 18 April 2014
Keywords:Wolff–Parkinson–White syndromeECGElectrophysiologic study
The aim of study was to report different and unusual patterns of preexcitation syndrome (PS) noted in patientsreferred for studied for poorly-tolerated arrhythmias and their frequency. Electrophysiologic study (EPS) is aneasy means to identify a patient with PS at risk of serious events. However the main basis for this diagnosis isthe ECG which associates short PR interval and widening of QRS complex with a delta wave.Methods: ECGs of 861patients inwhomPS related to an atrioventricular accessory pathway (AP)was identified atelectrophysiological study (EPS), were studied.Results: Themost frequent unusual presentation (9.6%)was the PS presentingwith a normal or near normal ECG,noted preferentially for left lateral AP and rarely for posteroseptal or right lateral location. More exceptional(0.1%) was the presence of a long PR interval, which did not exclude a rapid conduction over AP. The associationof a complete AV blockwith symptomatic tachycardias was exceptional (0.3%) andwas shown related to a rapidconduction over AP after isoproterenol. Most of the presented patients were at high-risk at EPS.Conclusion: The diagnosis of PS is not always evident and symptoms should draw attention to minor abnormal-ities and lead to enlarge indications of EPS, only means to confirm or not PS.
© 2014 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Wolff–Parkinson–White syndrome (WPW) is diagnosed by thesurface ECG in sinus rhythm with a typical pattern associating a shortPR interval (b0.12 s in adults) and a widening of QRS complex with adelta wave [1], called the preexcitation syndrome (PS). The pattern isassociatedwith history of tachycardia. Patients with a PS can be asymp-tomatic. Some of these patients and patients with aWPW syndrome areknown to be at risk of sudden death. The risk is low [2–6] and estimatedto be of 0.02% per patient per year [4]. These studies have shown thatventricular fibrillation may be the first event. This low risk of arrhyth-mias associatedwith adverse presentation needs to be detected becausethe events frequently occur in youngpeoplewithout heart disease and apreventive treatment is possible. The main means of diagnosis is theinitial ECG.
A pattern of PS is noted among 0.1 to 0.5% of the population [7]. Thepattern is dependent on the location of accessory pathway (AP), but alsoon the properties of atrioventricular (AV) node and His Purkinje systemand there is a wide spectrum of ECG types encountered. Spontaneousnormalization of ECG with intermittent preexcitation is reported in 20
rembilla-Perrot).andoeuvre Les Nancy, France.
.
to 30% of WPW [8,9]; dynamic QRS variations in WPW syndromewere noted several years ago [10,11].
The purpose of study was to report unusual patterns of PS, theelectrophysiological data of these patients and the prevalence of theseatypical patterns in subjects with antegrade conduction through an AP.
2. Methods
2.1. Population
The present cases were issued from a consecutive series of 861 patients in whom aPS related to an atrioventricular AP was identified at EPS. There were 528 males and 333females, aged from 5 to 85 years (mean 34 ± 17). The subjects were consecutivelyexamined in our department between 1990 and May 2013.
The initial clinical presentation of the total population was as follows:
Three hundredfifty nine patients had a knownhistory of orthodromicAV reciprocatingtachycardia.Three hundred five patients were asymptomatic: ventricular PS was discoveredduring a systematic assessment before anesthesia, before sporting license, prior toemployment in certain occupations at risk or on an ECG performed in the preventivemedicine.One hundred five patients presented with unexplained syncope without documenta-tion of any arrhythmia, event that was generally the initial cause leading to indicateEPS.Twenty eight patients presented with a documented well-tolerated spontaneousatrial fibrillation (AF).Sixty four patients had an adverse presentation defined as a documented life-threatening hemodynamically poorly-tolerated arrhythmia.
349B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
2.2. Methods
The data of ECG at the time of EPS and the data of EPS were retrospectively collectedand studied.
1. Clinical data and the ECG in sinus rhythm were collected.2. EPS was performed either by intracardiac route in symptomatic
patients or first by the transesophageal route in out-patient clinicwhen these patients were asymptomatic or had unexplained syncope.Our protocol was previously reported [12]. Atrial pacing andprogrammed atrial stimulation were performed in the basal stateand generally after isoproterenol.
3. Definitions.AP location was determined with the 12-lead ECG recorded in maxi-mal preexcitation. The diagnosis of multiple pathways was retainedonly if ECGs in maximal preexcitation were clearly different or ifthe sites of ablation were also clearly different. The exact locationgenerally was confirmed by the disappearance of AP at the presumedsite during ablation.Unapparent preexcitation syndrome was defined as a normal ECG atthe time at electrophysiology which can be related to a maskedpreexcitation or an intermittent preexcitation. Masked preexcitationwas defined as overt antegrade conduction over AP masked by thenormal AV conduction. These patients have a minimal preexcitationon the ECG. The signs of the conduction over an AP could be retro-spectively detected by the appearance of minor changes of ECGafter AP ablation. Intermittent preexcitation was defined as a normalECG related to a normal AV conduction recorded amongpatientswhopresented overt preexcitation on another ECG.PS was considered as at high-risk at EPS when the following associa-tion was observed: the maximal heart rate with a 1 to 1 conductionover the AP was more than 240 bpm in control state or more than290 bpm after isoproterenol infusion [13] during induced sustainedAF.
3. Results
Seven unusual ECGs are presented. The data are summarized inTable 1.
3.1. Masked PS associated with poorly-tolerated arrhythmias was the mostfrequent unusual presentation
The ECGs were recorded in patients complaining of tachycardia orsyncope. Atrial pacing and EPS revealed the presence of a malignantform of PS.
The AP conducted in the anterograde conduction was frequentlyleft-lateral sided. Minor changes of ECG were noted after AP successfulablation, but were variable:
In case 1, aman aged 46 years (Fig. 1), only r′ in V1 disappeared afterablation.
Table 1Presentation of the case series.Gender: M = male, ECG: N = normal; 1 AVB = first d AV block, PS: preexcitation syndromtachycardia, PT AF = poorly-toleratedAF, HF: stage 3 or 4 heart failure; AP loc = AP location, LLrate base:maximal heat rate conducted over AP in basal state (bpm); rate iso = maximal heat rATD antidromic tachycardia, AVRT: AV re-entrant tachycardia, AF: atrial fibrillation.
Case Age Gender ECG Symptoms
1 46 M N PT T2 43 M N PT AF3 25 M N PT AF4 57 M N PT AF5 25 M N PT AF6 64 M 1AVB PT AF7 58 M 3rd d AVB HF
In case 2, a man aged 43 years (Fig. 2), the size of R wave decreasedin precordial leads from V1 to V5 after ablation with a change of apattern R/s to r/S in leads V2 and V3.In case 3, a man aged 25 years (Figs. 3 and 4), the size of R wave inlead V2 decreased after ablation.
Less frequently, PS was related to a posteroseptal AP (Fig. 5). Theman aged of 57 years had presented a poorly-tolerated AF requiringemergent electrical shock. ECG in sinus rhythm was normal. Afterablation of the left posteroseptal AP, a small decrease of the size ofventriculograms in frontal leads was noted. Precordial leads wereunchanged.
Rarely preexcitation syndrome can be related to a right lateral AP(Fig. 6). In this last case, patient of 25 years complaining of tachycardias,the ECG was normal. At EPS, antidromic tachycardia and then atrialfibrillation using a right lateral AP were induced. Ablation was per-formed in sinus rhythm because at the site of right lateral AP therewas a direct activation of ventricles by atrial activity despite a normalECG. After ablation, ECG was unchanged despite increasing delaybetween atrial electrogram and ventriculogram at the site of ablation.
These unapparent PSs were noted in 83 patients of our population(9.6%) and 12% of them had a high-risk PS; 46 other patients had inter-mittent PS.
3.2. Delta waves and long PR interval
Fig. 7 was recorded in a man aged 64 years, who had presented apoorly-tolerated AF requiring electrical chock in emergency. Therewas a deltawave but PR intervalwas prolonged (220ms). After ablationof a left lateral sided AP, PR interval was 240ms in relationship with AVnode conduction abnormalities (AH interval 140 ms). Despite poorconduction in normal AV system, the rate in AF conducted by AP wasrapid. This ECG remains exceptional and was noted only in one patientof our population (0.1%).
3.3. Complete AV block and preexcitation syndrome
Fig. 8 reports the case of a 58 year old man complaining of poorly-tolerated tachycardias associated with supraventricular tachycardia-related tachycardiomyopathy and heart failure. This last complicationwas facilitated by the presence of left ventricular noncompaction.Three years earlier, ablation of a right posteroseptal sidedAP responsiblefor orthodromic re-entrant tachycardia was complicated by the occur-rence of a complete AV block. A pace-makerwas implanted. Left ventric-ular ejection fractionwas preserved. Later the patient still complained oftachycardia and was admitted for heart failure. Frequent episodes oftachycardias with wide QRS complexes were recorded on a Holtermonitor. Therefore a second EPS was performed. At control state,there were no anterograde and retrograde conductions over normalAV conduction system or over AP. After isoproterenol infusion, the
e, 3rd D AVB: 3rd degree AV; symptoms: S syncope, PT T: poorly-tolerated documentedleft lateral, LPS left posteroseptal, R PS right posteroseptal, AS anteroseptal, RL right lateral;ate conducted over AP during isoproterenol infusion (bpm); ind T = induced tachycardia:
AP loc Rate base Rate iso Ind T
LL 220 280 AF + AVRTLL 240 290 AFLL 230 300 AF + ATDLPS 260 AF + AVRTRL 220 290 AF + AVRT + ATDLL 220 290 AFRPS 0 280 AF
Fig. 1. (Patient no. 1): On the left panel: induced sustained AF; AF was conducted over AP at high rate (N240 bpm). On the right panel: ECG recorded during AP ablation (arrow); beforeablation the ECG was near normal. We note a transitory maximal conduction over AP (or radiofrequency-induced automaticity at AP) and then a disappearance of the r′ wave in V1probably related to the conduction over AP.
350 B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
right posteroseptal AP was capable of rapid anterograde AV conductionuntil 280 bpm reproducing the symptoms. After AP ablation, the patientwas in complete AV block with QRS complexes of normal duration(0.10 s) (suprahisian AV block) and was dependent on its pacemaker.He became asymptomatic. Two other cases of complete AV blockassociated with PS were noted in our population: another iatrogenicAV block occurred in a patient with a concealed conduction over a leftposteroseptal AP during the attempt of AP ablation; it was related toan inadvertent normal AV conduction ablation; an anterograde conduc-tion over the AP reappeared later and the patient still presented re-entrant tachycardias despite the completeAV block. A second procedurewas required to ablate the AP. One natural paroxysmal AV block wasnoted in a patient complaining of syncope (0.3%). Pacemaker implanta-tion suppressed syncope and ablation of the AP was not required.
4. Discussion
Wehave reported some ECGs considered as normal, or with atypicalpresentation, that are considered as rare in PS. These patients were
Fig. 2. (Patient no. 2): On the left panel: spontaneousmalignant form in a patientwith a left latersize of Rwave decreased in precordial leads fromV1 to V5 after ablation (right ECG). Therewassite of ablation (left lateral). This figure was previously reported [14].
studied because they complained of tachycardia or unexplaineddizziness/syncope. Similar findings could be expected in apparentlyasymptomatic subjects; systematic ECG in subjects at risk of arrhyth-mias as athletes is probably not sufficient to eliminate the presence ofa masked electrical abnormality as a PS sometimes at risk of seriousevents. The interpretation of symptoms by patient is variable andsome patients with overt PS are presented as asymptomatic but afterinterrogatory, dyspnea, chest pain or transitory anxiousness are fre-quently noted in patients with induced tachycardia.
The most frequent unusual ECG of PS was the masked pattern of PS,associated with minor signs of preexcitation retrospectively visiblewhen ECG became slightly different after AP ablation. The reportedcases had amasked preexcitation, defined as overt anterograde conduc-tion through the AP masked by the normal AV conduction. Thesepatients have a minimal preexcitation on the ECG that may becomeapparent when this ECG differed after ablation. These cases differedfrom patients with intermittent preexcitation defined as a normal ECGrelated to a normal AV conduction recorded among patients whopresented overt preexcitation on another ECG.
al AP; On themiddle panel: ECGbefore ablation. On the right panel: ECG after ablation: Thea new appearance of Twave inversion in III and aVF just after ablation not explained by the
Fig. 3. (Patient no. 3): On the left panel: induced atrial fibrillation conducted at 300 bpm over AP in a patient with a left-lateral sided AP complaining of tachycardia. On the right panel:disappearance of conduction over AP only visible on the distal coronary sinus recording with an abrupt increase of AV interval.
351B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
We previously reported that the frequency of a normal or nearnormal ECG in patients who had a preexcitation syndrome proved byelectrophysiologic study represented 11% of our population withanterograde conduction through an AP; this prevalence could beunderestimated [14,15]. This prevalence included the patients withintermittent PS and the patients with masked PS. The risk to have anelectrophysiological malignant formwas reported as similar to patientswith permanently overt preexcitation syndrome in sinus rhythm.
The importance of ventricular preexcitation on ECG in sinus rhythmdepends on the quality of the nodohisian conduction and the distancebetween the AP and the normal conduction system [9]. More AP islocated away from the sinus node and the normal atrioventricular sys-tem, less ventricular preexcitation is visible. Concealed conduction in
Fig. 4. (Patient no. 3): ECGs recorded just before ablation and after successful ablation (patient osurface ECG is near similar before and after ablation. Only the size of R wave in leads V2 and V3
anomalous AV bypass tracts can be demonstrated in both anterogradeand retrograde directions in most patients with WPW syndrome andis an important factor in the clinical expression of their arrhythmias[16,17]. Changes in atrioventricular conduction may account for thevariability of the QRS pattern in patients with a PS [18–20]. Most ofour patients had a left lateral AP, but some of them had septal or rightAPs and we have no explanation for the absence of clear sign ofpreexcitation in sinus rhythm, except a preferential conduction overnormal AV system.
Exceptionally, the PR interval is greater than 0.12 s [16], the QRScomplex is more or less wide and there is a delta wave. This form ofpre-excitation is more common in left AP than in right APs. It is due toa disorder of intra-atrial conduction or a first degree block in the AP
f Fig. 3). On the left panel: ECG before ablation; On the right panel: ECG after ablation; thedecreased after ablation (right ECG) with a change of a pattern of R/s to r/S after ablation.
Fig. 5. (Patient no. 4): On the left panel: poorly-tolerated atrial fibrillation conducted over a septal AP (QS pattern in leads II, III, VF) requiring emergent electrical shock and occurring in apatientwith a preexcitation syndrome related to a left posteroseptal AP. On the right panel: ECG during ablation of the left posteroseptal AP indicated by the arrow; a small decrease of thesize of ventriculograms in frontal leads was noted corresponding to the disappearance of anterograde conduction over AP. Precordial leads were unchanged.
352 B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
[21]. In our case nodal AV conduction was abnormal. It was reported inless than 1/1000 patients with a PS. The long PR interval does notexclude a rapid conduction over AP in the case of AF as in our patient.
Fig. 6. (Patient no. 5): On the left panel: only short PR interval on the ECGbefore ablation.On theright panel: ECGduring ablation; on the right lateral atrium therewas a sitewith a fusion of atriaof radiofrequency energy at this site increased immediately the interval between atrial and ventsame short PR interval despite increasing delay between atrial electrogram and ventriculogram
At least, disorders of conduction occurring simultaneously in bothnormal and AP's of patients with a PS have only rarely been observed[22]. Impaired conduction in both pathways in PS has been noted in
middle panel: AF using initially normal AV conduction systemand a right lateral AP. On thel and ventricular electrograms. The arrow on the lead of ablation indicated that applicationricular electrograms. After ablation, ECGwas unchanged (leadsD1, D2, VF, V1, V6)with theat the site of ablation visible on the third beat of the right panel.
Fig. 7. (Patient no. 6): On the left panel: spontaneousmalignant form in a patient with a left lateral AP. On the right panel: ECG during ablation; there is a long PR interval before ablationdespite a presentation with a malignant form. After AP ablation, the PR interval was slightly longer.
353B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
patient with mitral annulus calcification [23]. Infrahisian conductionabnormalities were previously reported by our group in one patientwith syncope [24]. One-to-one conduction through the AP occurredonly at a distinct range of cycle lengths, at lower frequencies the acces-sory tractswere refractory and a 2nd or a 3rd degree A-V blockoccurred.In our case, the patient had adrenergic tachycardia rapidly conductedover AP and developed tachycardia-induced cardiomyopathy. Isopro-terenol infusion frequently used to enhance conduction over AP iscapable to demonstrate an anterograde rapid conduction over AP [25,26]. Vagal stimulation was used several years ago to provoke the reap-pearance of ventricular preexcitation [27].
The clinical implications are important. Apparently normal ECG doesnot exclude the presence of an accessory pathway. Therefore systematic
Fig. 8. (Patient no. 7): On the left panel: intermittent conduction over a right posteroseptal Acomplexes are stimulated electrograms. On the middle panel: after isoproterenol infusion, 1/with a normal duration.
ECG is probably not sufficient in asymptomatic subjects at high of ar-rhythmias as competitive athletes ormilitary or police to exclude the di-agnosis. We must be especially vigilant in symptomatic patientscomplaining of tachycardia associated or not with syncope. ECG shouldbe repeated and non-invasive studies as exercise testing and ECGHoltermonitoring are indicated to look for small variations of QRSmorphology.If it is done locally, transesophageal atrial pacing is an easyway to reveala preexcitation syndrome.
The limitation of the study is the lack of repetition of ECG in sinusrhythm, of systematic exercise testing and vagal maneuvers to evaluatepossible changes of ECG that have oriented the diagnosis.
In conclusion preexcitation syndromes may present with severalunusual patterns on ECG. Classical pattern of PS is not always present
P (first and last complexes) in a patient with complete AV block; the other enlarged QRS1 conduction over AP. On the right panel: after AP ablation, complete AV block and QRS
354 B. Brembilla-Perrot et al. / International Journal of Cardiology 174 (2014) 348–354
and in symptomatic patients minor signs of PS should be sought. Alllocations of AP's can be encountered, but left lateral location is themore frequent location presenting with a near normal ECG.
References
[1] Anderson RH, Becker AE, Brechenmacher C, Davies MJ, Rossi L. Ventricularpreexcitation. A proposed nomenclature for its substrates. Eur J Cardiol 1975;3:27–36.
[2] Klein GJ, Bashore TM, Sellers TD, Pritchett ELC, Smith WM, Gallagher JS. Ventricularfibrillation in theWolff–Parkinson–White syndrome.N Engl JMed1979;301:1080–5.
[3] Brembilla-Perrot B, Aliot E, Louis P, et al. Devenir de 195 patients atteints desyndrome de Wolff–Parkinson–White. Arch Mal Coeur 1987;80:271–7.
[4] Fitzsimmons PJ, Mc Whirter PD, Peterson DW, Kruyer WB. The natural history ofWolff–Parkinson–White syndrome in 228 military aviators: a long-term follow-upof 22 years. Am Heart J 2001;142:530–6.
[5] Timmermanns C, Smeets JL, Rodriguez LM, Vrouchos G, Van den Dool A, Wellens HJ.Aborted sudden death in the Wolff–Parkinson–White syndrome. Am J Cardiol1995;76:492–4.
[6] Montoya P, Brugada P, Smeets J, et al. Ventricular fibrillation in the Wolff–Parkinson–White syndrome. Eur Heart J 1991;12:144–50.
[7] Pelliccia A, Culasso F, Di Paolo FM, et al. Prevalence of abnormal electrocardiogramsin a large, unselected population undergoing pre-participation cardiovascularscreening. Eur Heart J 2007;28:2006–10.
[8] Klein GJ, Gulamhusein SS. Intermittent preexcitation in the Wolff–Parkinson–Whitesyndrome. Am J Cardiol 1983;52:292–6.
[9] Garcia OL, Castellanos A, Vagueiro MC, Myerburg RJ, Gelband H. Arrival of excitationat the left ventricular apical endocardium in W.P.W. syndrome type B. JElectrocardiol 1982;15:165–72.
[10] Hindman MC, Last JH, Rosen KM. W.P.W. syndrome observed by portable monitor-ing. Ann Intern Med 1973;79:654–63.
[11] Khair GZ, Tristami FE, Bamrath VS. Dynamic QRS variations in Wolff–Parkinson–White syndrome: electrocardiographic and clinical observations. Am Heart J1983;105:878–82.
[12] Brembilla-Perrot B, Chometon F, Groben L, et al. Interest of non-invasive and semi-invasive testings in asymptomatic children with pre-excitation syndrome. Europace2007;9:837–43.
[13] Brembilla-Perrot B, Tatar C, Suty-Selton C. Risk factors of adverse presentation as thefirst arrhythmia in Wolff–Parkinson–White syndrome. Pacing Clin Electrophysiol2010;33:1074–81.
[14] Brembilla-Perrot B, Brembilla-Perrot B, Valizadeh Moejezi R, et al. Missing diagnosisof preexcitation syndrome on ECG. Clinical and electrophysiological significance. IntJ Cardiol 2013;163:288–93.
[15] Brembilla-Perrot B, Moulin-Zinsch A, Sellal JM, et al. Impact of transesophageal EPstudy to elucidate the mechanism of arrhythmia in children with SVT and nopreexcitation. Pediatr Cardiol 2013;34:1695–702.
[16] Klein GJ, Yee R, Sharma AD. Concealed conduction in accessory atrioventricularpathways: an important determinant of the expression of arrhythmias in patientswith Wolff–Parkinson–White syndrome. Circulation 1984;70:402–11.
[17] Svinarich JT, Tai DY,Mickelson J, Keung EC, Sung RJ. Electrophysiologic demonstrationof concealed conduction in anomalous atrioventricular bypass tracts. J AmColl Cardiol1985;5:898–903.
[18] Parameswaran R, Ohe T, Nakhjavan FK, Goldberg H. Spontaneous variations inatrioventricular conduction in pre-excitation. Br Heart J 1976;38:427–30.
[19] TeoWS, Klein GJ, Yee R, Leitch JW,Murdock CJ. Significance of minimal preexcitationin W.P.W. syndrome. Am J Cardiol 1991;67:205–7.
[20] Fujiki A, Yoshida S, Tani M, Mizumaki K, Tsuji H, Sasayama S. Phase 3 and phase 4block in the accessory pathway. J Cardiol 1990;20:217–25.
[21] Guérot C, Valere P-E, Castillo-Fenoy A, Rl Tricot. Syndrome de W.P.W. et espace P Rlong. A propos d'une observation associant une double voie de préexcitation et untrouble de conduction intra-auriculaire. Ann Cardiol Angeiol 1975;24:51–7.
[22] Seipel L, Mäurer W, Zebe H. Severe atrioventricular block in 2 cases withpreexcitation syndrome. Z Kardiol 1976;65:616–23.
[23] Kriwisky M, Goldstein J, Gotsman MS. Accessory atrioventricular pathway, supra-,and infrahisian conduction impaired due to mitral annulus calcification. Clin Cardiol1987;10:818–20.
[24] Brembilla-Perrot B, Chometon F, Groben L, et al. Are the results of electrophysiolog-ical study different in patients with a pre-excitation syndrome, with and withoutsyncope? Europace 2008;10:175–80.
[25] Easley Jr AR, Sensecqua JE, Mann DE, Reiter MJ. Intermittent preexcitation: markedenhancement of anterograde conduction in the atrioventricular accessory pathwaywith isoproterenol. Pacing Clin Electrophysiol 1988;11:349–54.
[26] Yamamoto T, Yeh SJ, Lin FC, Wu DL. Effects of isoproterenol on accessory pathwayconduction in intermittent or concealed Wolff–Parkinson–White syndrome. Am JCardiol 1990;65:1438–42.
[27] Przybylski J, Chiale PA, Halpern MS, Nau GJ, Elizari MV, Rosenbaum MB. Unmaskingof ventricular preexcitation by vagal stimulation or isoproterenol administration.Circulation 1980;61:1030–7.