36. Transplantation Review 2004
Transcript of 36. Transplantation Review 2004
SIS
A
t
t
T
r
p
i
r
d
t
R
d
e
t
p
©
DdtustvSs(cte(tve
aU
tMW
ynbiotic Control of Inflammation andnfection in Transplantationtig Bengmark
part from rejection, infection and inflammation are the most common threat to success in organ
ransplantation. The incidence of infection is high while patients are on the waiting list for transplan-
ation and in the immediate postoperative period, as well as during several years after transplantation.
he majority of immune cells are found in the gut, and insufficient gut immune functions and exuberant
elease of proinflammatory mediators such as cytokines are seen in combination with translocation of
otentially pathogenic microorganisms (PPMs) in these patients. Specific lactic acid bacteria (probiot-
cs) and specific plant fibers (probiotics), often in combination (synbiotics), have proven effective to
educe inflammation and infection in these patients. The supply of synbiotics to these patients is a
ocumented effective tool to reduce the PPM flora, eliminate potential toxins and mutagens, provide
hrough fermentation numerous antioxidants and nutrients, and stimulate the innate immune system.
ecent studies suggest that inflammation can effectively be reduced in patients with chronic liver
isease and inflammation and infection almost abolished just by uninterrupted—continuous—periop-
rative supplementation of synbiotics in connection with transplantation. A special feeding tube
echnology has been developed to optimize uninterrupted enteral nutrition with synbiotics in the
erioperative period.
2004 Elsevier Inc. All rights reserved.
$S
ST
Bcdsotiicttqdth
Bilwmt
espite obvious progress in medicopharmaceuti-cal and surgical treatments during the last few
ecades, morbidity and mortality in severely ill pa-ients, such as transplant patients, remain at annacceptably high level. This is especially true foreptic morbidity. The high incidence of sepsis hashus far remained relatively resistant to most pre-entive and treatment efforts. Only in the Unitedtates does severe sepsis annually affect 751,000 per-ons, which results in death of the patients in 29%215,000 patients). Sepsis is currently the tenth mostommon cause of death in the country. Furthermore,he incidence of critical illness is rising by about 1.5%ach year. More than half of critically ill patients51%) or 383,000 are treated in special intensiveherapy units (ITUs), and an additional 130,000 areentilated in some intermediary-type care units. Thextra treatment cost for each case is estimated to be
From the Institute of Hepatology and Department of Surgery, Royal Freend University College Medical School, University College London, London,nited Kingdom.Address reprint requests to Stig Bengmark, MD, PhD, Institute of Hepa-
ology and Department of Surgery, Royal Free and University Collegeedical School, University College London, 69-75 Chenies Mews, LondonC1E 6HX, United Kingdom.0955-470X/$ - see front matter© 2004 Elsevier Inc. All rights reserved.doi:10.1016/j.trre.2004.01.001
38 Transplantation Reviews, Vol 18, No
22,100 and the total annual cost in the Unitedtates is about $17 billion.
epsis: A Major Problem inransplantation
one marrow, liver, lung, and intestines are espe-ially central to immune defense and resistance toisease. Both the function and the immunologictrength of these organs in transplant patients areften considerably reduced by disease even beforehe transplant and are further handicapped by thenstituted treatments, especially by the supply ofmmunosuppressive agents and other pharmaceuti-als, including antibiotics. There is a strong associa-ion between the dose of immunosuppressants giveno the patient and the rate of infections. As a conse-uence, the incidence of infections is especially highuring the first 2 to 4 weeks after transplanta-ion, when the supply of immunosuppressants is theighest.
Bone Marrow (Stem Cell) Transplantationone marrow transplantation constitutes a unique
mmunological situation because of the induced totalack of lymphocytes. It is estimated that each yearorldwide more than 50,000 patients undergo bonearrow–stem cell transplantation, and manifesta-
ions of sepsis will develop in more than 25,000 of
1 (January), 2004: pp 38-53
tbsow
Ipoemilcfaappop
Ihmrttt.cttttiaiip2e
Imdfd
r3ptqrorosthasrc
Mpicptismrrwbttwiclgw
Ft
St
Ab(a
Synbiotic Control of Inflammation 39
hem within the first 2 to 4 weeks.1,2 The conditionecomes very serious in patients who require inva-ive mechanical ventilation, need inotrope support,r experience development of organ dysfunction,ith a reported mortality of �80%.3,4
Lung Transplantationnfection is also a major problem in lung transplantatients. As with transplantation of other organs, usef immunosuppressants is responsible for a consid-rable suppression of humoral and cell-mediated im-unity and subsequent infections. However, it is
mportant to recognize that the function of the newung is quite impaired and the cough blunted be-ause of postoperative pain but also because of theact that the new lung is without nerve supply. Inddition, the lymphatic drainage is almost totallybsent and the mucociliary clearance severely im-aired. All of this explains why approximately 80% ofostoperative infections in lung transplant patientsccur within the chest, lung, mediastinum, andleura.5
Heart Transplantationnfectious complications are also commonly seen ineart transplantation and are the major reason fororbidity and mortality. They are second only to
ejection as the cause of early deaths and are, in fact,he dominant cause of late deaths.6 Among the iden-ified risk factors for early infections are older age ofhe recipient (P �.0001), race of the donor (P �0007), and positive donor serologic test results forytomegalovirus (P � .0007).7 Various supportiveechnologies such as ventilator support at the time ofransplant (P �0.0001), ventricular assist device athe time of transplant (P � .02), and OKT3 induc-ion therapy (P �.0001) add considerably to morbid-ty and mortality.7 Use of various types of ventricularssist systems (VAS) will significantly increase thencidence of severe morbidity and mortality; severenfections are reported to occur in at least 50% of theatients supported by an implantable VAS and in8% of the patients supported by short-term andxternally applied VAS.8
Liver, Intestinal, and MultivisceralTransplantation
n the majority of patients subjected to intestinal andultivisceral transplantation, sepsis will develop
uring the first postoperative month.9 Recent studiesrom clinical liver transplantation report infectionsuring the first 30 days in about half of patients; the
eported incidence in the literature varies between0% and 86%. The highest incidence, 86%, was re-orted in a recent study in which selective digestiveract decontamination (SDD) was used. One mightuestion whether SDD did not, in fact, add to theisk of sepsis instead of preventing it. The occurrencef surgical infections in liver transplantation has se-ious economic implications, in addition to its impactn morbidity, mortality, and quality of life. A recenttudy suggests that surgical site infections after liverransplantation incur approximately 24 additionalospital days per patient, $159,967 in excess charges,nd a 10% increase in mortality. Strong evidenceuggests that postoperative infections and antibacte-ial treatments are also associated with a signifi-antly higher incidence of graft loss.10
An Infection-Rejection-ImmunosuppressionConnection
ore than half of the early infections after trans-lantation are of bacterial origin. Viral and fungalnfections are also frequent. There is a strong asso-iation between the dose and type of immunosup-ressive agents administered and subsequent infec-ion and rejection episodes. That the occurrence ofnfection also increases the rate of rejection wasuggested by Simmons et al11 in 1970. These authorsade the observation that mild fever often preceded
ejection, later accompanied by renal function dete-ioration, consistent with allograft rejection. Theyere especially able to show a clear-cut associationetween rejection episodes and herpesvirus infec-ions.12 The cause-and-effect relation between infec-ion was recently reviewed by Cainelli and Vento,10
ho proposed that it is especially cytomegalovirusnfections which up-regulate various adhesion mole-ules, cytokines, and coagulation factors, activate Tymphocytes, and damage human lymphocyte anti-en (HLA)–DR expressing allograft blood vessels,hich triggers rejection.
actors Known to Decrease Resistanceo Infection
everal factors are known to contribute to the sensi-ivity of infection.
Pre-existing Morbidityn increasing part of the patient population treatedy organ transplantation has metabolic syndromeMS), prediabetes, manifest diabetes, or other MS-ssociated conditions known to be associated with
dtwial
Moblmapiaitsis
Tifraatcsdbaiatoc
Tandmiiti
oamisfIcta
SC
Idewlir1pttcmwetar(stlofd
ahppoaSpotoa
40 Stig Bengmark
epressed immune function and depressed resis-ance to disease. An exaggerated immune responseith increased release of proinflammatory cytokines
s often seen in these patients. They also often haven increased incidence of septic morbidity (seeater).
Extensive Use of Pharmaceuticalsost transplant patients, if not all, are on a regimen
f short-term or long-term drug treatment. It shoulde recognized that many more drugs than thoseabeled as immunosuppressive have significant im-
unodepressive effects. Among such drugs are mostntibiotics. Furthermore, a large number of otherharmaceuticals that are commonly used inhibit sal-vation and gastrointestinal (GI) secretions, whichre necessary for luminal release of important anti-nflammatory, anti-infectious, and growth-stimula-ory factors normally provided with saliva and GIecretions.13,14 Such unwanted effects are an increas-ng problem with increased use of modern and con-iderably more effective drugs.
Too Much Focus on Antibioticshe process that leads to fulminant and severe sepsis
s extremely complex and still in many aspects notully understood. It has taken too long for us toealize that this process cannot be controlled withntibiotics and, as it appears now, also not withntagonists or inhibitors of individual proinflamma-ory cytokines. Even if prompt antibiotic therapy,ompared with treatment instituted later, seems tolightly reduce the mortality in sepsis (10%-15%), itoes not significantly reduce the unacceptably highurden of mortality in these groups of patients. Afterlmost 30 years of efforts and more than 30 random-zed clinical trials, it now seems clear that SDD is notn effective tool to prevent and combat sepsis. Al-hough these treatments will decrease the incidencef chest infections, they will not influence outcome inritically ill patients.15
Late Institution of Preventive Measureshe therapeutic window for institution of effectiventi-inflammatory and anti-infectious measures isarrower than earlier thought. From the onset ofisease or trauma or the beginning of surgery, it isost likely not much more than 24 to 36 hours. If
nstituted later, it will have no or little effect on thenflammatory cascade that precedes sepsis, a cascadehat, if “exuberant” (overwhelming and prolonged),s regarded as a key event in the subsequent devel-
pment of multiorgan failure. The need for early andggressive treatment is often neglected. One reasonight be that early preventive measures are often
nstituted by several medical and surgical specialists,ome of whom seem to have no knowledge or feelingor the urgency of immediate aggressive treatment.n addition, the power of early signs of sepsis variesonsiderably, and these are often occult and difficulto identify, which also explains why septic conditionsre sometimes overlooked in the early stages.
uperinflammation and Infectiousomplications
ndividuals affected by MS, diabetes, or other chroniciseases will most often respond to stress with anxuberant acute or chronic superinflammation,hich is manifested by an exaggerated and pro-
onged release of proinflammatory cytokines such asnterleukin (IL) 6, acute-phase proteins such as C-eactive protein, and plasminogen activator inhibitor
(PAI-1).16 Both IL-6 and PAI-1 are regarded asrognosticators of outcome in conditions such ashose after operation or trauma, myocardial infarc-ion, and pancreatitis but also in semichronic orhronic inflammatory conditions, such as arthritis,ental depression, or Alzheimer’s disease. An over-helming IL-6 response (eg, prolonged or extremelevations of circulating IL-6) in patients with condi-ions like infection, burns, or trauma is significantlyssociated with adverse clinical events such as acuteespiratory distress and multiple-organ failureMOF). The effect of overwhelming acute-phase re-ponse on outcome has been well shown by a liverransplantation study; in all patients who during theater phase of operation already had signs of a 6-foldr larger increase in the cytokines tumor necrosisactor � (TNF-�)and IL-6, clinical sepsis did developuring subsequent postoperative days.
Among the changes observed in an overexuberantcute-phase response are augmented endothelial ad-esion of polymorphonuclear (PMN) cells, increasedroduction of intracellular adhesion molecule 1,riming of the PMNs for an oxidative burst, releasef proinflammatory platelet-activating factor, and,ssociated with this, a delay in PMN apoptosis.ymptoms such as fatigue, somnolence, mental de-ression, anorexia, and daytime sleepiness are alsoften associated with the condition. In stress situa-ions visceral adipocytes, compared with subcutane-us fat cells, do secrete much more free fatty acidsnd, most interestingly, per gram of tissue compared
woPoctfops
A
Tstkpgpsmaataldsaitascttttaauws
a(aiCwa
lcesoadgktfrtpmdi
gwimMisa(awtrfdrttd
IT
Tapmtiated
Synbiotic Control of Inflammation 41
ith subcutaneous fat, greater than 3 times as muchf the proinflammatory molecules such as IL-6 andAI-1, which well explains the observation of thebserved higher risk of disease in patients with vis-eral obesity. This is further elucidated by the facthat the amount of fat in the abdomen varies from aew milliliters to about 6 L in persons with grossbesity. The load of free fatty acids and these otherowerful molecules on the liver can, thus, in stressfulituations vary up to a thousand times.17
Failing Innate Immune System
he disease-related changes in physical activity,leep, and mood, age, gender, circadian rhythm, bodyemperature, drugs consumed, and food eaten are allnown to influence important functions such as lym-hocyte function, hemostasis, endothelial function,lucose and fat metabolism, capillary permeability,roduction of immunoglobulins (Ig), and general re-istance to disease. The gut plays a leading role inost of these functions. It is not always realized that
bout 80% of the total Ig-producing cells of the bodyre localized in the lamina propria of the gut andhat, under normal conditions each day, largemounts of Ig, especially IgA, are released to the gutumen. Endemic chronic diseases, particularly type 2iabetes mellitus, but also acute conditions such asevere sepsis and MOF are increasingly recognizeds associated with, or caused by, a failing innatemmune system. The innate or natural immune sys-em, phylogenetically much older than adaptive orcquired immunity, constitutes a first-line defenseystem, identical to or closely associated with what isalled acute phase response (APR). The relationship be-ween chronic diseases and various acute complica-ions is of great interest because it has been observedhat the great majority of posttreatment and post-rauma morbidity does occur in patients with MSnd associated conditions such as diabetes, obesity,nd hypertension. Patients with chronic diseases arender the influence of a chronically elevated APR,hich is better expressed as a “chronic”-phase re-
ponse.16
The main function of the innate immune systemnd the APR is to instantly neutralize the stressorstissue injury, malignancy, inflammation, infection,nd so on) and restore homeostasis. The main toolsn this process are so-called acute-phase proteins, such as-reactive protein and fibrinogen, the production ofhich is stimulated through release of cytokines suchs IL-1, IL-6, and TNF-�. These molecules are re-
eased from endothelium, macrophages, and mono-ytes but, to a large extent, also from adipocytes,specially within the abdomen. It is not fully under-tood why in some patients this process becomesverwhelming (exuberant) and leads to induction ofsystemic inflammatory response syndrome and to
istant organ injuries. Central to this process is theut, which more or less suddenly turns into a “cyto-ine-generating” organ.18 Deitch18 recently showedhat cytokines, endotoxins, pathogens originatingrom the intestines, and other unidentified gut-de-ived factors are delivered into the general circula-ion through the lymphatic system rather than theortal vein. The lack of the filtering function nor-ally provided by the liver makes these compounds
eleterious to distant organs and especially damag-ng to the lung.
Ancient Egyptian and, later, Greek medicine sug-ested that noxious agents, associated with feces,ere the cause of disease. The concept of autointox-
cation was central to 18th and 19th century Westernedicine. The immunologist and Nobel laureateetchnikov suggested in the early 20th century that
ntestinal toxins induce disease and shorten lifepan; he believed these processes could be counter-cted by regular consumption of lactic acid bacteriaLAB). In the early 20th century several surgeons,mong them, Sir W. A. Lane, performed colectomyith the aim to prevent and cure intestinal autoin-
oxication. History repeats itself, and evidence is cur-ently accumulating that translocated gut-associatedactors cause acute or chronic inflammation and pro-uce “autodestruction” as in systemic inflammatoryesponse syndrome and MOF. They also contributeo the development of thrombosis, adhesion forma-ion, and sepsis and most likely play a role in theevelopment of chronic diseases.
nstant APR Requires Instantreatment
he inflammatory cascade is instant and the “ther-peutic window” for preventive measures narrow,robably not much more than 24 hours. Measures toodulate the inflammatory cascade, for example,
hrough early enteral nutrition, should be instituted,f possible, before surgery and be continued duringnd immediately after surgery. Because pretraumareatment is not possible in trauma and medicalmergencies, it should at least be instituted imme-iately on arrival to the hospital.19,20
otiietocniaaioiTgtbvpibpcw
tliahbdapkc
udepislbswomatp
42 Stig Bengmark
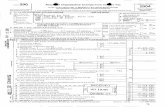
Recognition of the importance of aggressive peri-perative nutrition was the reason why I inventedhe autopositioning and regurgitation-resistant feed-ng tube, developed only for the purpose of beingntroduced before surgery and making immediatenteral nutrition possible.21 A coil was constructed ashe head (tip) of the tube (Fig 1) instead of a balloonr a weight, which is more commonly used. It isonstructed to maximally absorb gastric and duode-al motility and use it for its transportation down
nto the region of the ligament of Treitz. Its ability tobsorb motility has been further increased with thedaptation of thin flexible fins on the outside andnside of the tube and by making the exterior surfacef the coil “frosty” or “hairy,” measures aimed toncrease the adherence to the mucosa of the coil.22
he coil is placed in the stomach with the aid of auide wire and allowed to expand in the lower part ofhe stomach. Gastroduodenal motility is stimulatedy a small meal (sandwich, pizza, spaghetti, or aegetable juice, such as V8 [Campbell Soup Com-any, Camden, NJ]). The head of the tube (the coil)s in most cases within minutes, together with theolus of the food, transported to its final and optimalosition around the ligament of Treitz (Fig 2). Theonstruction of the tube also makes it self-anchoring,hich is important to prevent spontaneous regurgi-
Figure 1. Autopositioning reg
ation. Experience has shown that the rate of dis-odgement compared with that of conventional tubess much less. It is an advantage of this tube that nottempts are needed to verify the position of theead before the supply of nutrition is started. It hasecome increasingly common to start feeding imme-iately after the tube has been placed in the stom-ch, without waiting for the coil to move to its finalosition. The tube is available on the European mar-et (Bengmark Flo-Care tube; Royal Numico-Nutri-ia Group, Zoetermeer, The Netherlands).
Although the tube was intended as a tool to besed only in patients with intact motility (eg, intro-uced before surgery and used in connection withlective surgery), it has increasingly been tried inatients with reduced motility and here in Europentroduced both with and without pharmacologictimulation of motility. Gastric acidity stimulates re-ease of nitric oxide from donor molecules, prefera-ly nitrate or nitrite. This is why vegetable extractsuch as rhubarb decoction and V8 vegetable juice,hich are fluids that are known to stimulate releasef nitric oxide and motility, are used to promoteotility when necessary. Successful intubation has
lso been reported with use in critically ill patientsreated in intensive care units. One such study re-orted successful intubation in 10 of 10 patients with
tation-resistant feeding tube.
urgiaistertttsnsprs
Q
Sa
ctawcetotcm
Iaitasc
F(
Synbiotic Control of Inflammation 43
cute pancreatitis and in 6 of 6 patients with abdom-nal sepsis.23 Although all the patients in this studyhowed significantly reduced GI motility, the head ofhe tube reached its optimal position within an av-rage of 5.2 hours and always within 24 hours. Aecent prospective study reported successful intuba-ion in 49% of the intended intensive care unit pa-ients, reducing the need for endoscopic placemento half,24 and another recent randomized controlledtudy reported successful placement in patients withormal gastric emptying after 24 hours in 78% ver-us 14% with a straight standard tube (P � .041). Inatients with impaired gastric emptying, the successates after 24 hours were 57% versus 0% with atraight standard tube (P � .07).25
uestionable Practices Commonly Used
everal measures commonly used in perioperativend intensive care unit management and often in
igure 2. Feeding tube placed in ideal position with headPhotograph by Gerardo Mangiante, Verona, Italy.)
onnection with transplantation need reconsidera-ion. These treatments, often adapted long ago andt a time when the demand for scientific evidenceas not as strict as it is today, cannot with modernriteria be regarded as evidence-based. Even if ben-ficial effects can sometimes be shown with the prac-ice of some of these methods, they seem to havebvious negative consequences, which might exceedheir positive value. Common to all methods dis-ussed later is that they negatively influence im-une function and resistance to infection.
Extensive Use of Antibioticst was shown 50 years ago that administration ofntibiotics increases the susceptibility to acquire newnfections.26 Later it was proven that the administra-ion of antibiotics suppresses macrophage functions,s documented by studies of chemiluminescence re-ponse, chemotactic motility, and bactericidal andytostatic ability.27,28 Appropriately timed short-term
ube in small intestine just beyond the ligament of Treitz.
of t(eiodktacg
Ads((rskeibifcmppscabgtpgmstdv
Ptsotdh
tbttiaobmtnottm
AnmtvtwroTtltStaisrqqnusfvp3dspfim
44 Stig Bengmark
most often used as a “single-shot”) prophylaxis is anffective tool to prevent wound infections that seem-ngly does not have the same negative consequencesn the immune system as are seen with multiple-ose prophylaxis. Although these facts are wellnown, it has proven very difficult, even when thehreat of microbial resistance is considered, to actu-lly change clinical policy. Prophylactic antibioticsontinue to be heavily overprescribed,58 both in sur-ery and in intensive care units.
Inhibition of Salivationn adult individual secretes as much as 10 L eachay of GI secretions, as follows: saliva (2.5 L), gastricecretion (2.5 L), bile (0.5 L), pancreatic secretion1.5 L), and small intestinal and colonic secretionsbetween 1.0 and 5.0 L). In children, secretion iselated to body weight, and the production of GIecretions is even larger; 5-year-old children arenown to secrete about 5 L a day. GI secretions arextremely rich in immunosupportive factors such asmmunoglobulins, lactoferrin, lysozyme, and fi-ronectin but also in mucus, which is of utmostmportance for mucosa protection. It must, there-ore, always be remembered that these secretionsonstitute a main defense system against invadingicroorganisms and that their maintenance is im-
ortant. Mucus is also an important matrix trans-ort vehicle for ingested bacteria and an importantubstrate for nutrition of the commensal flora, espe-ially when inadequate amounts of nutritional fibersre supplied. Saliva is one of the main sources in theody of important growth factors such as epidermalrowth factor. Surgical or pharmaceutical removal ofhe salivary glands is accompanied by GI ulcerations,oor wound healing, and a poor regeneration of or-ans such as the liver. If possible, attempts should beade in postoperative patients and those in inten-
ive care units to maintain and even to stimulatehese secretions.16,19,29 It is unfortunate that mostrugs commonly used in intensive care units haveery pronounced antisecretory effects.29
Inhibition of GI Secretionsroduction of gastric nitric oxide is of utmost impor-ance for maintenance of GI motility, mucosal andplanchnic blood flow, and prevention of gastric col-nization with pathogens. Maintenance of low gas-ric pH is a prerequisite for gastric nitric oxide pro-uction, a function that is totally eliminated withistamine blockers and proton pump inhibitors. Fur-
hermore, in the absence of acidity, the stomach willecome a reservoir for pathogens, from which bac-eria for chest infections are recruited and regurgi-ated into the lungs. Normal gastric acid productions also essential for absorption of several vitaminsnd antioxidants, including vitamin C and glutathi-ne. Prevention of peptic ulcers by use of histaminelockers or proton pump inhibitors or similar drugsight be a priority issue when total parenteral nu-
rition is used but with aggressive enteral nutrition iso longer needed. Routine use of histamine blockersr proton pump inhibitors in partially or totally en-erally fed postoperative and intensive care unit pa-ients can no longer be regarded as evidence-basededicine.30
Prophylactic Nasogastric Decompression
bout 70 years ago, Mayo introduced postoperativeasogastric decompression with the idea that itight prevent nausea, vomiting, and abdominal dis-
ension but also decrease postoperative ileus, pre-ent wound complications, and protect enteric anas-omoses. This treatment modality was introducedithout any scientific background, and the wisdom of
outine gastric decompression was questioned earlyn and has continued to be questioned ever since.oday, there is accumulating evidence that this
reatment is counterproductive and might both de-ay the return of adequate bowel function and con-ribute to an increased rate of septic complications.everal recent studies confirm that omission of rou-ine nasogastric decompression is not associated withny obvious increase in morbidity or mortality. Evenf a slight gastric distention occurs, no active mea-ures should be needed because the distention willesolve spontaneously with no negative conse-uences and insertion of a tube is not usually re-uired. As a matter of fact, gastric distention shouldot be regarded as a contraindication to the contin-ation of enteral feeding and high residual volumeshould not automatically lead to cessation of tubeeeding; if tube feeding is continued, the residualolume will most often soon decrease and disap-ear.31 A meta-analysis based on 26 trials (a total of964 patients) concluded that routine nasogastricecompression is not supported in the literature bycientific evidence.32 Instead, fever, atelectasis, andneumonia are significantly less common and days torst oral intake are significantly fewer in patientsanaged without nasogastric tubes.30
RtcelcclunSdsbUcigibi
Artodfloaapmfmteafiffp
moctEb
sbaabcltctc
Ismccaamrv
gasfqosbstocbttwbsi1tsi
cati
Synbiotic Control of Inflammation 45
Postoperative Drainage of Body Cavitiesoutine use of postoperative drainage of body cavi-
ies is also not based on scientific evidence. In mostases drainage tubes serve more effectively as anntrance for microbes than as an outlet of accumu-ated fluids. Furthermore, most body cavities, espe-ially the abdomen, have an extraordinarily goodapacity to reabsorb leaked fluids, including blood, ateast if not infected or mixed with body fluids such asrine and bile. Most studies suggest that there is noeed for abdominal drainage in gastric surgery.ome controlled studies suggest no advantages of arainage policy in liver and pancreatic surgery, andeveral randomized trials have documented clearenefits of a no-drainage policy in colonic surgery.se of drains is often shown to increase the rate of
omplications, especially adhesions and mechanicalleus, in appendicitis-related operations. As sug-ested in a recent excellent review, high-quality clin-cal studies are necessary for solid and evidence-ased recommendations re use of drainages, at leastn visceral surgery.33
Preoperative Bowel Preparationvailability of flora is an absolute requirement for
elease from consumed plant fibers and utilization inhe body of various nutrients such as amino acids,ther fatty acids, polyamines, vitamins and antioxi-ants, and coagulation and growth factors. Intestinalora and gut immune cells are also powerful sourcesf proinflammatory and anti-inflammatory cytokinesnd are deeply involved in prevention of infection,nastomotic leakage, and formation of extensiveeritoneal adhesions. Healing of intestinal anasto-oses depends on luminal production of short-chain
atty acids, especially butyrate, which is released byicrobial fermentation of plant fibers in the intes-
ine. These important processes are negatively influ-nced by lavage or bowel preparation, as well as bydministration of antibiotics. Bowel preparation andber-free enteral feeding also have detrimental ef-ects on the release of important intestinal healingactors such as transforming growth factor-�1 andro-collagen type I.
It was recently claimed that no obvious improve-ent in outcome after surgery for bowel cancer has
ccurred in recent decades. In addition, the unac-eptably high postoperative infection rate also seemso have remained unchanged during several decades.ven if bowel preparation does not enhance micro-ial translocation, as was concluded in a recent
tudy, several other reasons suggest that routineowel preparation before surgery should be omittednd several studies in recent years have producedctive support of the omission of bowel preparationefore surgery. A recently published meta-analysisould not document any reduction in anastomoticeaks or other complications with the routine prac-ice of preoperative bowel preparation. Instead, in-reasing experimental and clinical evidence suggestshat reduced morbidity and considerable cost savingsan be obtained by omission of bowel preparation.34
Transfusion With Stored Bloodmmunosuppression is increasingly recognized as aerious consequence of transfusion of allogeneic (ho-ologous) blood in humans, including both in-
reased recurrence rates after potentially curativeancer surgery and increased frequency of postoper-tive bacterial infections. We observed some 35 yearsgo that intraportal and intravenous infusion of he-olyzed blood to experimental animals resulted in
ather immediate and extensive disseminated intra-ascular coagulation and fibrinolysis.35-37
Similar changes were obtained after induced or-an hypoxia, such as intestinal or liver ischemia,38
nd after infusion of alcohol.39 Several recent studiesuggest that blood transfusion is a major risk factoror postinjury MOF.40-42 Traumatic injuries fre-uently occur in alcohol-intoxicated individuals, whoften also have severe shock and poor organ perfu-ion, and, in addition, are the objects of extensivelood transfusions. Recent studies document atrong association between the number of unitsransfused during the first 6 hours after trauma, agef the stored blood transfused, and outcome.43 It isonsequently recommended that, if possible, freshlood should also be used in initial resuscitation ofrauma patients. Removal of old blood cells and res-oration of tissues in organs damaged by ischemia, asell as alcohol intoxication, constitute an enormousurden on the reticuloendothelial system, which re-ults in immunoparalysis and increased sensitivity tonfections. A meta-analysis based on more than3,000 patients provided overwhelming evidencehat autologous blood transfusion is associated with aignificantly higher risk of postoperative bacterialnfection.44
The phagocytic functions of neutrophils, mono-ytes, and macrophages are essential for protectiongainst both chronic diseases and severe acute infec-ions, a function considerably reduced with alcohol-sm, diabetes, and other chronic diseases. These
fpoat(dln
Iliwmwoqonincdmrniiislfid
lsvliwpsb
O
Mf
rsmanioifaa
Amtspctontrmddsenmpt
Hcoctgriaergemda4
46 Stig Bengmark
unctions are all significantly impaired, especially inatients with acute tissue injuries such as burns orrgan ischemia.45 It is suggested that the increasedmounts of lysophosphatidylcholine and platelet-ac-ivating factor in the stored blood induce neutrophilPMN) priming for reactive oxygen metabolite pro-uction and induce endothelial cell damage, capil-ary leakage, and degranulation, which often culmi-ate with end-organ injury and MOF.46
Overload With Nutrients OrHyperalimentation
t was not long ago that hyperalimentation (eg, over-oad with nutrients) was regarded as a key to successn the care of the critically ill. Today, overfeedingith macronutrients is known to be regarded asuch more dangerous than underfeeding, especiallyhen applied during the first 1 or 2 weeks afterperation. A series of negative metabolic conse-uences have been shown to be a consequence ofverfeeding.47 In intensive care unit patients, a sig-ificant association between degree of impairment
n glucose and lipid metabolism and severity of ill-ess and outcome has been documented.48 The in-reased amounts of free fatty acids especially have aocumented strong depressive effect on innate im-une functions. The endothelial cells, which are
esponsible for transport to the underlying cells ofutrients such as free fatty acids and glucose, play an
mportant role, and endothelial function is severelympaired by the inflammatory response, various tox-ns, and microbes.49,50 One consequence of elevatederum free fatty acid levels is that they inhibit T-ymphocyte signaling.51 However, the neutrophilunction is reported to be considerably improved bynfusion of insulin, as has been especially shown iniabetic patients after cardiac surgery.52
We observed some 35 years ago that high serumevels of fat and the presence of liver steatosis con-titute poor risks in liver resection.53,54 Similar obser-ations were more recently shown in connection withiver transplantation.55 The negative effect of dyslip-demia and steatosis is most likely independent ofhether it is induced by lifestyle and constituting aart of MS, induced by the overloading of calories,uch as seen in total parenteral nutrition, or causedy an exaggerated APR.
ften-Neglected Measures
aximizing the function of the immune system, en-orcing the innate immune functions, and improving
esistance to diseases through enteral nutrition withpecific nutrients is currently regarded to be of ut-ost importance. We are increasingly becoming
ware that proper supply of a variety of food compo-ents is important for a satisfactory outcome in crit-
cally ill patients and those who have undergoneperation and also as a measure to prevent chronicllnesses. Some important components, especially inresh food but also in live microorganisms, have thebility to preserve and augment cellular immunitynd modify production of inflammatory mediators.56
Aggressive Perioperative Enteral Nutritions already stated, all attempts to control the APRust be instituted early because the reaction to
rauma is instant. It is well supported by scientifictudies that immediate postoperative feeding is safe,revents an increased gut mucosal permeability,ontributes to a positive nitrogen balance, reduceshe incidence of septic complications, reduces post-perative ileus, and accelerates restitution of pulmo-ary physical performance.57-59 Delaying the institu-ion of enteral nutrition for a few hours is shown toesult in increased intestinal permeability; increasedicrobial translocation; and, compared with imme-
iate enteral nutrition, a significantly higher inci-ence of MOF.60 An intensive and uninterruptedupply through feeding tubes of enteral nutrition,specially when it contains plant fibers, during theight before surgery, during the operation, and im-ediately thereafter will most likely significantly im-
rove immune functions and increase the resistanceo complications.19,30,61,62
Tight Control of Blood Glucose Levelsyperglycemia is known to predispose to infectious
omplications63 and serve as an independent markerf in-hospital mortality,64 as well as to predict myo-ardial infarction in patients on a regimen of hyper-ensive treatment.65 Even though the value of strictlucose control has been known for some time toeduce the incidence of wound infection in surgery,66
t was not until recently that such control had beendapted in modern intensive care units and postop-rative care. The state of the art was until ratherecently to tolerate, in fed critically ill patients, bloodlucose levels up to 12 mmol/L (220 mg/dL). How-ver, maintaining the blood glucose level below 6.1mol/L led to significant improvements such as a
ecrease in bloodstream infections (by 46%), incute renal failure with a need of hemofiltration (by1%), in critical illness polyneuropathy (by 44%), in
rabgcTia
TaalvofrisTgpiaTottoomtstapicil
Pmtstimo(
i5vi
Aedbtawaacmdbdaaaapjwig
S
Tvofiibaitbaih
sc
1
Synbiotic Control of Inflammation 47
equirement for red blood cell transfusions (by 50%),nd in mortality (by 34%).67,68 Small elevations oflood glucose (to 8-10 mmol/L) are know to impairut motility and function,69 and such impairmentontributes to induction and prolongation of ileus.hus a stricter glucose control after operation and in
ntensive care units might also promote gut motilitynd GI function.
Supply of Antioxidantshe tissue and blood concentrations of pro-oxidantsre almost invariably high and the levels of variousntioxidants and micronutrients low or extremelyow in critically ill patients. As an example, totalitamin C and ascorbic acid are reported to be �25%f normal values in these patients.70 A study per-ormed mainly in trauma patients reported a 19%eduction in pulmonary morbidity and a 57% lowerncidence of MOF in a group of patients receivingupplementation with �-tocopherol and ascorbate.71
he benefit of antioxidant supplementation in sur-ical and intensive care unit patients is also sup-orted by several other studies.72 Glutathione is anmportant antioxidant, both synthesized by the bodynd supplied by foods, mainly fruits and vegetables.his antioxidant is significantly decreased both post-peratively and in critically ill patients, a decreasehat is associated with impaired lymphocyte and neu-rophil function. Glutamine is an important sourcef fuel for the enterocytes of the small bowel andther rapidly dividing cells such as leukocytes andacrophages and an important substrate for produc-
ion of glutathione.73 Supplying glutamine has beenhown in various experimental studies to reduce cy-okine release, organ damage, and mortality74 andlso to revert the depletion of glutathione and lym-hocytes in Peyer’s patches.75 Several controlled clin-cal studies performed in recent years show signifi-ant benefits from supplementation of glutamine,ncluding reductions in morbidity, mortality, andength of stay in critically ill patients.76
Supply of Plant Fiberslant fibers are favored substrates for microbial fer-entation in the lower digestive tract. They also have
heir own strong bioactivities. Unfortunately, too fewtudies on the effects of supplying various plant fiberso surgical and intensive care unit patients are foundn the medical literature. A controlled study worth
entioning reported a significant reduction in post-perative morbidity after the administration of glucanbeta 1,3-polyglucose) with reduction in nosocomial
nfections from 65% to 14% and mortality from 30% to%.77 There is certainly a need to explore the effects ofarious plant fibers when supplied to postsurgical andntensive care unit patients.
Supplementing Florasignificant reduction of the commensal flora occurs
arly in the disease process and is caused both by theisease and by the pharmaceutical treatment. It haseen observed in experimental pancreatitis that af-er the induction of disease the anaerobic bacteriand particularly the LAB are significantly reducedithin 6 to 12 hours both in the distal small bowelnd in the colon. The reduction in preventive flora islmost instantly accompanied by significant in-reases in the numbers of potentially pathogenicicroorganisms (PPMs) such as Escherichia coli and in
ramatic increases in the permeability (lumen tolood) of the mucosal barrier, as well as in the en-othelial (blood to tissue) permeability,78,79 changesssociated with increased microbial translocationnd microbial growth in mesenteric lymph nodesnd, in the case of acute pancreatitis, in the pancre-tic tissue.80 One can take for granted that everyatient who undergoes a major operation is the ob-ect of significant trauma or every patient treatedith modern antibiotics has a considerable reduction
n the beneficial flora often combined with an over-rowth of PPMs.
ynbiotics: A Promising New Tool
here is genetically a very large difference amongarious bacteria called LAB; the difference betweenne LAB and another can be greater than between ash and a human. Most of the LAB used by food
ndustry have no or limited ability to ferment strongioactive fibers such as inulin or phlein; have nobility to adhere to human mucus; have low antiox-dant capacity; and, most important, do not survivehe acidity of stomach and bile acid content. Strongioactivity cannot often be expected from LAB suchs yogurt bacteria, chosen mainly for their palatabil-ty. Most of the LAB currently used in sick patientsave originally been identified on plants.
My personal experience during the last 15 yearstems from studies using 2 different symbiotics—ombinations of prebiotics and probiotics, as follows:
. A 1 LAB/1-fiber composition, produced by fer-mentation of oatmeal with Lactobacillus plantarumstrain 299.81 The formula was produced for ourstudies by Probi AB, Lund, Sweden.
2
CA
PdtpdfitwiohrkaLvLstlsda
TsTltchett
ii�nntbmthtcmw8TfvdsgtCc
ALtw31ehnpb1l1iSppc1HKnSeT
48 Stig Bengmark
. A 4 LAB/4 fiber composition, called Synbiotic2000, consisting of a mixture of 1010 (and morerecently a Synbiotic FORTE with 1011) of each of4 LAB—Pediacoccus pentosaceus 5-33:3, Leuconostocmesenteroides 32-77:1, Lactobacillus paracasei subspparacasei 19, and L plantarum 2362)—and 2.5 g ofeach of the 4 fermentable fibers (prebiotics)—betaglucan, inulin, pectin, and resistant starch.82,83
The formula is produced for our studies byMedipharm AB, Kågerod, Sweden, and DesMoines, Iowa.
linical Experience With Synbiotics incute Conditions
Acute Pancreatitisatients with severe acute pancreatitis were ran-omized to receive daily during the first 7 dayshrough a nasojejunal tube either a freeze-driedreparation containing live Lb plantarum 299 in aose of 109 together with a substrate of 10 g of oatber or the same preparation after heat inactiva-ion.84 The study was designed to be interruptedhen on repeat statistical analysis statistically signif-
cant differences in favor of 1 of the 2 groups werebtained, which occurred when a total of 45 patientsad entered the study. At that time, 22 patients hadeceived treatment with live and 23 with the heat-illed Lb plantarum 299. Infected pancreatic necrosisnd abscesses were seen in 1 of 22 (4.5%) in the liveAB group versus 7 of 23 (30%) in the heat-inacti-ated group (P � .023). The only patient in the liveAB group with development of an infection hadigns of urinary infection on the 15th day (eg, at aime when he had not received treatment during theast 8 days). The length of stay was considerablyhorter in the live LAB group (13.7 days vs 21.4ays), but the limited size of the material did notllow statistical significance to be reached.
Abdominal Surgeryhe same 1 LAB/1 fiber composition was used in a
tudy in extensive abdominal surgical operations.he patients consisted mainly of those undergoing
iver, pancreatic, and gastric resections, equally dis-ributed among the 3 groups. Three groups wereompared, as follows: (1) live LAB and oat fiber, (2)eat-inactivated LAB and oat fiber, and (3) standardnteral nutrition.85 Each group consisted of 30 pa-ients. The 30-day sepsis rate was 10% (3/30 pa-ients) in the 2 groups receiving either live or heat-
nactivated LAB, compared with 30% (9/30 patients)n the group receiving standard enteral nutrition (P
.01). The biggest differences were observed in theumbers of cases of pneumonia, as follows: enteralutrition only, 6 patients; live LAB and fiber, 2 pa-ients; and heat-killed LAB and fiber, 1 patient. Theeneficial effects of synbiotic treatment seemed to beost pronounced in gastric and pancreatic resec-
ions with a sepsis rate of 7% with live LAB, 17% witheat-inactivated LAB, and 50% with standard en-eral nutrition. The live LAB-treated patients re-eived significantly less antibiotics (P � .04); theean length of antibiotic treatment was 4 � 3.7 daysith live LAB, 7 � 5.2 days with heat-killed LAB, and� 6.5 days with only standard enteral nutrition.he incidence of noninfectious complications was as
ollows: enteral nutrition, 30% (9/30); heat-inacti-ated LAB, 17% (5/30); and live LAB, 13% (4/30). Noifferences were observed in the length of hospitaltay. No significant changes were observed in hemo-lobin; leukocytes; C-reactive protein; blood urea ni-rogen; bilirubin; albumin; total lymphocyte count inD45 RA, CD45 RO, CD4, CD8, or natural killer
ells; or CD4/CD8 ratio.
Liver Transplantationprospective randomized study with the same 1
AB/1 fiber preparation was performed in 95 liverransplant patients,86 and the following 3 groupsere studied: (1) SDD 4 times daily for 6 weeks (n �2), (2) Lb plantarum 299 (LLP) in a dose of 109 plus0 g of oat and inulin fibers (n � 31) for 12 postop-rative days, and (3) identical to group 2 but witheat-killed Lb plantarum 299 (HLP) (n � 32). Enteralutrition was supplied to all patients from the secondostoperative day. There were no deaths. The num-ers of postoperative infections were SDD, 23; HLP,7; and LLP, 4. Signs of infections occurred as fol-ows: SDD, 48% (15/32); HLP, 34% (11/32); and LLP,3% (4/31) (P � .017, respectively). The most dom-nating infections were cholangitis, occurring in 10DD, 8 HLP, and 2 LLP patients, respectively, andneumonia, occurring in 6 SDD, 4 HLP, and 1 LLPatient, respectively. The most often isolated mi-robes were Enterococci, found in 8 SDD, 8 HLP, andLLP patient, and Staphylococci, found in 6 SDD, 3LP, and 1 LLP patient, respectively. No E coli orlebsiella infections were seen in the LLP group. Theumbers of patients requiring hemodialysis were 8DD, 4 HLP, and 2 LLP, and the numbers of reop-rations were 6 SDD, 2 HLP, and 4 LLP, respectively.he CD4/CD8 ratio was higher in the LLP group
cits
awbbs4sustpts
CC
Tscsl
Twokeiwasstgslaatiplrs
aibTcSmptpttetepal
ApemmGstp1sLitSnidc�(cam
Rgt
Synbiotic Control of Inflammation 49
ompared with the other 2 groups (P � .06), and thentensive care unit stay, hospital stay, and length ofime on a regimen of antibiotic therapy were alsohorter, none of them reaching statistical significance.
The same investigators did continue their effortsnd try to further reduce the morbidity in connectionith liver transplantation87; this time with the com-ination of 4 LAB and 4 fibers.82,83 In this double-lind randomized study, 33 patients were suppliedynbiotics and another 33 patients received only thefibers in the synbiotic composition. The treatment
tarted on the day before surgery and continuedntil the 14th day after surgery. Only 1 patient in theynbiotic-treated group (3%) showed signs of infec-ion (urinary infection) during the first month com-ared with 17 of 33 (51%) in the patients suppliedhe 4 fibers only. The use of antibiotics was alsoignificantly shorter in the synbiotic-treated group.
linical Experience With Synbiotics inhronic Conditions
here are good reasons to expect beneficial effects ofynbiotic treatment in chronic conditions such asancer, kidney disease, lung disease, and so on, butystematic studies so far have been limited to chroniciver disease.
Chronic Liver Disease: Effect onInflammation
he grade of nonalcoholic steatohepatitis correlatesell with the extent of obesity, especially visceralbesity. Fat cells, especially visceral adipocytes, arenown to have an increased expression of cytokines,specially TNF-�. The amount of fat in the abdomens known to vary from a few milliliters to 6 L, whichell explains the increased exposure of TNF-� indipose individuals, which together with overexpres-ion of �-interferon and underexpression of IL-10ensitizes the liver both to endotoxins and to theoxic effects of TNF-�. Activation of macrophages byut-derived endotoxin has been assumed to be re-ponsible for the raised levels of TNF-� and is mostikely a key factor behind the progressive liver dam-ge seen in patients with liver cirrhosis. Probioticsnd prebiotics (synbiotics) have the ability to reducehe production and absorption of endotoxin in thentestine and also to down-regulate the production ofroinflammatory cytokines, including TNF-�. Aong-term supply of synbiotics can be expected toeduce the inflammation of the liver and lessen theteatosis. Expression of Toll-like receptors (TLR 4
nd TLR2) is critically involved in TNF-� productionn response to endotoxin and gram-positive micro-ial stimuli. It was recently observed that in vitroNF-� production by peripheral blood mononuclearells in response to stimulation by endotoxin ortaphylococcus aureus enterotoxin B was reduced by aedian of 46% (range, 8%-67%) in comparison with
resupplementation levels in 8 of 11 (72.7%) pa-ients with cirrhosis who received the synbiotic com-osition.88 The administration of synbiotics to pa-ients with advanced chronic liver disease is wellolerated, and no adverse events or changes in gen-ral clinical state have been observed. If administra-ion of synbiotics is capable of down-regulating thexpression of Toll-like receptors and reducing theroduction of TNF-�, synbiotics could well constitutecheap and powerful tool with no side effects for
ong-term treatment of patients with liver disease.
Chronic Liver Disease: Effect on GutColonization, Liver Function, andEncephalopathy
mong a group of 97 patients with liver cirrhosis, 58atients were found to have signs of so-called minimalncephalopathy. They were randomized into 3 treat-
ent groups and studied when synbiotics were ad-inistered during a 1-month period, as follows:roup 1 received the 4 LAB/4 fiber synbiotic compo-
ition (n � 20), group 2 received only the fibers inhe composition (n � 20), and group 3 received alacebo (nonfermentable, nonabsorbable fiber) (n �5).89 A 1-month supply was shown to lead to aignificant increase in the intestinal LAB flora in theAB-supplied group but not the other 2 groups. The
ntestinal pH was significantly reduced in both thereatment groups. Significant decreases in E coli,taphylococcus, and Fusobacterium, as well as in ammo-ia, were seen, but such decreases were not observed
n Pseudomonas and Enterococcus and the levels of en-otoxin fell significantly. The levels of ALT de-reased significantly from 252 � 182 to 84 � 65 (P.01) in the synbiotic-treated group and to 110 � 86
P �.05) in the fiber-only group but not in the pla-ebo group. The improvements in liver function wereccompanied by significant improvements in psycho-etric tests and in the degree of encephalopathy.
Chronic Liver Disease: Effect on Liver BloodFlow and Indocyanine Green Clearance
educing intestinal levels of endotoxin-containingram-negative bacteria is reported to improve sys-emic hemodynamic disturbance in liver cirrhosis.
Sct111ml
C
Igaapuaocoadprmdreubdtpw4ttatattcchmiicBa
gitctmes
em1watutpiaasesami
F
SmfwseFrtwndrcibgytoca
50 Stig Bengmark
upplementation with the 4 LAB/4 fiber synbioticomposition was associated with a significant reduc-ion in indocyanine green clearance by a median of7.5% (range, 1.4%-65%) of baseline values in 14 of5 (93%) patients with cirrhosis and was increased inpatient by 4.1%.90 The observed improvement wasost likely a result of a reduced swelling of endothe-
ial and sinusoidal cells and reduced resistance to flow.
hoice of Synbiotic Composition
t is important to recognize that no conclusions re-arding bioactivities can be drawn from one LAB tonother because they are all different in functionnd genetically unrelated. Producers of probioticroducts often claim health benefits from their prod-cts; in most cases these claims are unsubstantiatednd not true. The truth is that only a small minorityf LAB have the health potentials needed for use inritical medicine. Most of the probiotic bacteria soldn the market do not survive the acidity of the stom-ch or the bile acid content of the small intestine, noro they adhere to the colonic mucosa or even tem-orarily colonize the stomach or intestine. It hasecently become increasingly common that milk-fer-enting LAB, such as yogurt bacteria and Lb aci-
ophilus, are used in clinical medicine. Yogurt bacte-ia have, like most other LAB, a low survival in annvironment with acidity and bile acids such as thepper GI tract and generally have only limited or noiologic influence on the immune system. The greatifferences in the ability of some LAB to survive andheir ability to influence cytokine production afterassage through the stomach and small intestineere well shown in a study comparing the followingdifferent LAB species: L plantarum, L paracasei, Lac-
obacillus rhamnosus, and Bifidobacter animalis.91 Afterhe administration of 108 cells/mL of each LAB andfter passage through the stomach and small intes-ine, there remained only between 107 (L plantarum)nd 102 (L rhamnosus) bacterial cells. After passagehrough the small intestine, most of the strainsested showed a significantly reduced or weak (espe-ially L rhamnosus) ability to influence, for example,ytokine production. If LAB such as yogurt bacteriaad been studied, an even smaller survival wouldost likely have been expected. The absence of clin-
cal efficacy of yogurt bacteria when used in severelyll patients was recently shown. A standard commer-ial product containing Lactobacillus acidophilus LA5,ifidobacterium lactis BP12, Streptococcus thermophilus,nd Lactobacillus bulgaricus was mixed with 7.5 g oli-
ofructose and supplied in a controlled study to crit-cally ill patients.92 Although significant reductions inhe number of potentially pathogenic organismsould be observed in the contents of the stomach ofhe treated patients, no influence on intestinal per-eability could be demonstrated and no clinical ben-
fits could be shown when this particular formula wasupplied to a mixed group of critically ill patients.93
The LAB used in the synbiotic studies mentionedarlier were all selected after extensive studies ofore than 350 human fecal bacteria and more than
80 bacteria harvested from fresh-growing rye. Theyere chosen because of their unique and superiorbilities to survive in the low pH of the stomach and inhe high bile acid content of the small intestine, theirnique ability to attach to colonic mucosa and toemporary colonize the large intestine, their high ca-acity to ferment various types of plant fibers includ-ng rather fermentation-resistant fibers such as inulin,
balanced production of both proinflammatory andnti-inflammatory molecules such as cytokines, atrong ability to produce several bioactive molecules,specially heat shock proteins, and the production ofignificant amounts of antioxidants. Similarly, thedded fibers were chosen because of their docu-ented bioactivities. These simultaneous fibers signif-
cantly improved the previously described functions.
uture Aspects
ynbiotic treatment as a new and promising treat-ent is still in its infancy. There is an urgent need
or synbiotic studies to be given priority. Patientsho are to undergo transplantation are affected by a
ignificantly elevated risk of sometimes life-threat-ning infections long before the actual treatment.urthermore, they continue to be at risk for bacte-ial, viral, and fungal infections for many years afterhe replacement of organ(s). One of the real benefitsith synbiotics is that they can be used for years witho negative effects because their supplementationoes not cause any side effects nor do they causeesistance. The promising effects from the studies inhronic liver disease suggest that patients on a wait-ng list for operation could well benefit from a syn-iotic umbrella. Similarly, there are reasons to sug-est that a synbiotic umbrella during the first fewears after transplantation could offer good protec-ion against various infectious complications. An-ther important group to study is patients withhronic kidney disease, especially those on hemodi-lysis or peritoneal dialysis. These patients, espe-
caidTpfd
tititbobatmchmca
A
H
R
1
1
1
11
1
1
1
1
1
2
2
2
2
2
2
2
2
2
2
Synbiotic Control of Inflammation 51
ially those on continuous ambulatory peritoneal di-lysis, have a high risk of infections. In addition, thencidence of chronic diseases such as coronary heartisease and diabetes is high in this patient group.here is good reason to suggest that long-term sup-lementation with synbiotics could help control in-ections and eventually also reduce the threat ofevelopment of other chronic diseases.
Thus far, most attempts to administer synbioticreatment have been through the oral route. Prelim-nary studies suggest excellent results when triedopically on skin and wounds to prevent and curenfections. When applied around tracheostomies andhe entrance sites of tubes and lines, the eventualiofilm is dissolved and removed and protection isffered against infections. Excellent results have alsoeen obtained in preliminary studies with topicalpplication in burns. Although a daily supply of bac-eria and fiber is important, a whole series of othereasures must be considered for optimal care of
ritically ill patients. Re-evaluation of practices thatave been used for decades is also urgent. There isuch to gain from bringing the management of
ritically ill patients in line with modern bioecologicnd evidence-based principles.
cknowledgmentI thank Dr Nada Rayes and her team at Charite University
ospital in Berlin, Germany.
eferences
1. Sparrelid E, Hagglund H, Remberger M, et al: Bacteraemiaduring the aplastic phase after allogeneic bone marrow trans-plantation is associated with early death from invasive fungalinfection. Bone Marrow Transplant 1998, 22:795
2. Faber-Langendoen K, Caplan AL, McGlave PB: Survival ofadult bone marrow transplant patients receiving mechanicalventilation: A case for restricted use. Bone Marrow Trans-plant 1993, 12:501
3. Kress JP, Christenson J, Pohlman AS, et al: Outcomes ofcritically ill patients in a university hospital setting. Am JRespir Crit Care Med 1999, 160:1957
4. Huaringa AR, Shaw PJ, Rowell F, et al: Outcome of bonemarrow transplantation patients requiring mechanical venti-lation. Crit Care Med 2000, 28:1014
5. Alexander BD, Tapson VF: Infectious complications of lungtransplantation. Transplant Infect Dis 2001, 3:128
6. Montoya JG, Giraldo LF, Efron B, et al: Infectious complica-tions among 620 consecutive heart transplant patients atStanford University Medical Center. Clin Infect Dis 2001,33:629
7. Smart FW, Naftel DC, Costanzo MR, et al: Risk factors forearly, cumulative, and fatal infections after heart transplan-
tation: A multi-institutional study. J Heart Lung Transplant1996, 15:329
8. Myers TJ, Khan T, Frazier OH: Infectious complications as-sociated with ventricular assist systems. ASAIO J 2000, 46:28
9. Kato T, Ruiz P, Thompson JF, et al: Intestinal and multivis-ceral transplantation. World J Surg 2002, 26:226
0. Cainelli F, Vento S: Infections and solid organ transplantrejection: A cause-and-effect relationship? Lancet Infect Dis2002, 2:539
1. Simmons RL, Weil R, Tallent MB, et al: Do mild infectionstrigger the rejection of renal allografts. Transplant Proc 1970,2:419
2. Lopez C, Simmons RL, Mauer SM, et al: Association of renalallograft rejection with virus infections. Ann J Med 1974,56:280
3. Mandel ID: The function of saliva. J Dent Res 1987, 66:6234. Sreebny LM, Banoczy J, Baum BJ, et al: Saliva: Its role in
health and disease. Int Dent J 1992, 42:2915. van Nieuwenhoven CA, Buskens E, van Tiel FH, et al: Rela-
tionship between methodological trial quality and the effectsof selective digestive decontamination on pneumonia andmortality in critically ill patients. JAMA 2001, 286:335
6. Bengmark S: Nutritional modulation of acute and “chronic”phase response. Nutrition 2001, 17:489
7. Bengmark S, Andersson R, Mangiante G: Uninterrupted peri-operative enteral nutrition. Clin Nutr 2001, 20:11
8. Deitch E: Role of the gut lymphatic system in multiple organfailure. Curr Opin Crit Care 2001, 7:92
9. Bengmark S: Aggressive peri- and intraoperative enteral nu-trition—Strategy for the future, in Shikora SA, MartindaleRG, Schwaitzberg SD (eds): Nutritional Considerations in theIntensive Care Unit—Science, Rationale and Practice. Dubu-que, IA, Kendall/Hunt Publ Co, 2002, p 365
0. Bengmark S: Enteral nutrition in HPB surgery—Past andfuture. J Hepatobiliary Pancreat Surg 2002, 9:448
1. Bengmark S: Swedish patent 8700582, PTC patent 0278937,US patent 4887996
2. Bengmark S: Swedish patent 507786, Int patent applicationSE 98/00145
3. Mangiante G, Colucci G, Marinello P, et al: Bengmark’sselfpropelling naso-jejunal tube: A new useful device for in-tensive enteral nutrition (abstr). Intensive Care Med 1998,24:330
4. Berger MM, Bollmann MD, Revelly JP: Progression rate ofselfpropelling feeding tubes in critically ill patients. IntensiveCare Med 2002, 28:1768
5. Lai CWY, Barlow R, Barnes M, et al: Bedside placement ofnasojejunal tubes: A randomized-controlled trial of spiral- vsstraight-ended tubes. Clin Nutr 2003, 22:267
6. Freter R: The fatal enteric cholera infection in guinea pigachieved by inhibition of normal enteric flora. J Infect Dis1995, 97:57
7. Roszkowski K, Ko KL, Beuth J, et al: Intestinal microflora ofBALB/c-mice and function of local immune cells. Z BakteriolHyg 1988, 270:270
8. Pulverer G, Ko HL, Roszkowski W, et al: Digestive tractmicroflora liberates low molecular weight peptides with im-munotriggering activity. Zentralbl Bakteriol 1990, 272:318
9. Bengmark S: Gut and the immune system: enteral nutritionand immunonutrients, in Baue AE, Faist E (eds): SIRS,MODS and MOF—Systemic Inflammatory Response Syn-drome, Multiple Organ Dysfunction Syndrome, Multiple Or-
3
3
3
3
3
3
3
3
3
3
4
4
4
4
4
4
4
4
4
4
5
5
5
5
5
5
55
5
5
6
6
6
6
6
6
6
6
6
6
7
52 Stig Bengmark
gan Failure—Pathophysiology, Prevention and Therapy. NewYork, NY, Fry Springer, 2000, p 420
0. Savassi-Rocha PR, Conceicao SA, Ferreira JT, et al: Evalua-tion of the routine use of the nasogastric tube in digestiveoperation by a prospective controlled study. Surg GynecolObstet 1992, 174:317
1. Cook DJ, Fuller HD, Guyatt GH, et al: Gastrointestinal bleed-ing in the critically ill: Stress ulcer prophylaxis is not foreveryone. N Engl J Med 1994, 330:377
2. Cheatham ML, Chapman WC, Key SP, et al: A meta-analysisof selective versus routine nasogastric decompression afterelective laparotomy. Ann Surg 1995, 221:469
3. Dominguez Fernandez E, Post S: Abdominal drainages (Ger-man). Chirurg 2003, 74:91
4. Bengmark S: Bio-ecological control of perioperative and ITUmorbidity. Langenbecks Arch Surg 2003, Nov 7 (Epub aheadof print)
5. Bengmark S, Hafstrom L, Korsan-Bengtsen K: A trial toproduce intravascular coagulation by infusion of connective-tissue homogenate and erythrocyte haemolysate–A compara-tive study. Br J Surg 1969, 56:619
6. Bengmark S, Hafstrom L, Korsan-Bengtsen K: A trial toproduce disseminated intravascular coagulation with intrave-nous infusion of homologous haemolysate and serum in cats.Acta Chir Scand 1972, 138:453
7. Bengmark S, Hafstrom L, Korsan-Bengtsen K: Effects ofintraportal infusion of autologous hemolysate on blood coag-ulation factors and fibrinolysis in the cat. Am J Surg 1972,124:647
8. Hafstrom L, Korsan-Bengtsen K, Bengmark S: Changes inblood clotting and fibrinolysis after liver ischemia in pigs.Am J Surg 1974, 127:300
9. Zoucas E, Bergqvist D, Goransson G, et al: Effect of acuteethanol intoxication on primary haemostasis, coagulation fac-tors and fibrinolytic activity. Eur Surg Res 1982, 14:33
0. Sauaia A, Moore FA, Moore EE, et al: Early predictors ofpostinjury multiple organ failure. Arch Surg 1994, 129:39
1. Moore FA, Moore EE, Sauaia A: Blood transfusion. An inde-pendent risk factor for postinjury multiple organ failure. ArchSurg 1997, 132:620
2. Sauaia A, Moore FA, Moore EE, et al: Multiple organ failurecan be predicted as early as 12 hours after injury. J Trauma1998, 45:291
3. Zallen G, Offner PJ, Moore EE, et al: Age of transfused bloodis an independent risk factor for postinjury failure. Am J Surg1999, 178:570
4. Hill GE, Frawley WH, Griffith KE, et al: Allogeneic bloodtransfusion increases the risk of postoperative bacterial infec-tion: A meta-analysis. J Trauma 2003, 54:908
5. Engelich G, Wright DG, Hartshorn KL: Acquired disorders ofphagocyte function complicating medical and surgical ill-nesses. Clin Infect Dis 2001, 33:2040
6. Aibochi J, Moore EE, Ciesla DJ, et al: Blood transfusion andthe two-insult model pf post-injury multiple organ failure.Shock 2001, 15:302
7. Klein CJ, Stanek GS, Wiles CE: Overfeeding macronutrientsto critically ill adults: Metabolic complications. J Am DietAssoc 1998, 98:795
8. Lind L, Lithell H: Imparied glucose and lipid metabolism seenin intensive care patients is related to severity of illness andsurvival. Clin Intensive Care 1994, 5:100
9. Steinberg HO, Tarshoby M, Monestel R, et al: Elevated cir-
culating free fatty acid levels impair endothelium-dependentvasodilation. J Clin Invest 1997, 100:1230
0. Pleiner J, Schaller G, Mittermayer F, et al: FFA-inducedendothelial dysfunction can be corrected by vitamin C. J ClinEndocrinol Metab 2002, 87:2913
1. Stulnig TM, Berger M, Roden M, et al: Elevated free fattyacid concentrations inhibit T lymphocyte signaling. FASEB J2000, 14:939
2. Rassias AJ, Marrin CAS, Arruda J, et al: Insulin infusionimproves neutrophil function in diabetic cardiac surgery pa-tients. Anesth Analg 1999, 88:1011
3. Almersjo O, Bengmark S, Engevik L, et al: Serum lipids afterextensive liver resection in man. Acta Hepatosplenol 1968,15:1
4. Bengmark S: Liver steatosis and liver resection. Digestion1968, 2:304
5. Marchesini G, Forlani G: NASH: From liver disease to met-abolic disorders and back to clinical hepatology. Hepatology2002, 35:497
6. Calder PC: Immunonutrition. BMJ 2003, 327:1177. Bisgaard T, Kehlet H: Early oral feeding after elective ab-
dominal surgery—What are the issues? Nutrition 2002, 18:944
8. Basse L, Raskov HH, Hjort Jakobsen D, et al: Acceleratedpostoperative recovery programme after colonic resection im-proves physical performance, pulmonary function and bodycomposition. Br J Surg 2002, 89:446
9. Kehlet H, Holte K: Review of postoperative ileus. Am J Surg2001, 182(Suppl):S3
0. Kompan L, Kremzar B, Gadzijev E, et al: Effects of earlyenteral nutrition on intestinal permeability and the develop-ment of multiple organ failure after multiple injury. IntensiveCare Med 1999, 25:129
1. Bengmark S: Progress in perioperative enteral tube feeding.Clin Nutr 1998, 17:145
2. Bengmark S: Use of some pre-, pro-, and synbiotics in criti-cally ill patients. Probiotics in gastroenterology. Best PractRes Clin Gastroenterol 2003, 17:833
3. McCowen KC, Malhotra A, Bistrian BR: Stress-induced hy-perglycemia. Crit Care Clin 2001, 17:107
4. Umpierrez GE, Isaacs SD, Bazargan N, et al: Hyperglycemia:An independent marker of in-hospital mortality in patientswith undiagnosed diabetes. J Clin Endocrinol Metab 2002,87:978
5. Dunder K, Lind L, Zethelius B, et al: Increase in blood glucoseconcentration during hypertensive treatment as a predictor ofmyocardial infarction: Population based cohort study. BMJ2003, 326:681
6. Zerr KJ, Furnary AP, Grunkemeier GL, et al: Glucose controllowers the risk of wound infection in diabetes after open heartoperations. Ann Thorac Surg 1997, 63:356
7. Van den Berghe G, Wouters P, Weekers F, et al: Intensiveinsulin therapy in critically ill patients. N Engl J Med 2001,345:1359
8. Mesotten D, Van den Berghe G: Clinical potential of insulintherapy in critically ill patients. Drugs 2003, 63:625
9. Rayner CK, Jones KL, Samsom N, et al: Relationship of uppergastrointestinal motor and sensory function with glycemiccontrol. Diabetes Care 2001, 24:371
0. Schorah CJ, Downing C, Piripitsi A, et al: Total vitamin C,ascorbic acid, and dehydroascorbic acid concentrations inplasma of critically ill. Am J Clin Nutr 1996, 63:760
7
7
7
7
7
7
7
7
7
8
8
8
8
8
8
8
8
8
8
9
9
9
9
Synbiotic Control of Inflammation 53
1. Nathens AB, Neff MJ, Jurkovich GJ, et al: Randomized, pro-spective trial of antioxidant supplementation in critically illsurgical patients. Ann Surg 2002, 236:814
2. Baines M, Shenkin A: Use of antioxidants in surgery: a mea-sure to reduce postoperative complications. Curr Opin NutrMetab 2002, 5:665
3. Cao Y, Feng F, Hoos A, et al: Glutamine enhances gut glu-tathione production. J Parenteral Enteral Nutr 1998, 22:224
4. Wischmeyer PE, Kahana M, Wolfson R, et al: Glutaminereduces cytokine release, organ damage, and mortality in arat model of endotoxemia. Shock 2001, 16:398
5. Manhart N, Vierlinger K, Spittler A, et al: Oral feeding withglutamine prevents lymphocyte and glutathione depletion ofPeyer’s patches in endotoxemic mice. Ann Surg 2001, 234:92
6. Kelly D, Wischmeyer PE: Role of L-glutamine in criticalillness: New insights. Curr Opin Nutr Metab 2003, 6:217
7. de Fellippe J, da Rocha e Silva M, Maciel FMB, et al: Infectionprevention in patients with severe multiple trauma with theimmunomodulator beta 1-3 polyglucose (glucan). Surg Gy-necol Obstet 1993, 177:383
8. Andersson R, Wang X, Ihse I: The influence of abdominalsepsis on acute pancreatitis in rats: A study on mortality,permeability, arterial blood pressure and intestinal blood flow.Pancreas 1995, 11:365
9. Leveau P, Wang X, Soltesz V, et al: Alterations in intestinalpermeability and microflora in experimental acute pancreati-tis. Int J Pancreatol 1996, 20:119
0. De Souza LJ, Sampietre SN, Figueiredo S, et al: Bacterialtranslocation during acute pancreatitis in rats (in Portuguese,with English summary). Rev Hosp Clin Fac Med Sao Paolo1996, 51:116
1. Johansson ML, Molin G, Jeppsson B, et al: Administration ofdifferent lactobacillus strains in fermented oatmeal soup: Invivo colonization of human intestinal mucosa and effect onthe indigenous flora. Appl Environ Microbiol 1993, 59:15
2. Kruszewska K, Lan J, Lorca G, et al: Selection of lactic acidbacteria as probiotic strains by in vitro tests. Microecol Ther2002, 29:37
3. Ljungh Å, Lan J-G, Yamagisawa N: Isolation, selection and
characteristics of Lactobacillus paracasei ssp paracasei isolateF19. Microb Ecol Health Dis 2002, 3(Suppl):4
4. Olah A, Belagyi T, Issekutz A, et al: Early enteral nutritionwith specific lactobacillus and fibre reduces sepsis in severeacute pancreatitis. Br J Surg 2002, 89:1103
5. Rayes N, Hansen S, Boucsein K, et al: Early enteral supply offibre and lactobacilli vs parenteral nutrition—A controlledtrial in major abdominal surgery patients. Nutrition 2002,18:609
6. Rayes N, Hansen S, Seehofer D, et al: Early enteral supply ofLactobacillus and fibre vs selective bowel decontamination(SBD)—A controlled trial in liver transplant recipients.Transplantation 2002, 74:123
7. Rayes N, Seehofer D, Theruvath T, et al: Combined periop-erative enteral supply of bioactive pre- and probiotics abol-ishes postoperative bacterial infections in human liver trans-plantation—A randomised, double blind clinical trial. In press2004
8. Riordan SM, Skinner N, Nagree A, et al: Peripheral bloodmononuclear cell expression of Toll-like receptors and rela-tion to cytokine levels in cirrhosis. Hepatology 2003, 37:1154
9. Qing L, Zhong PD, Da Kang H, et al: Synbiotic modulation ofgut flora: Effect on minimal hepatic encephalopathy in pa-tients with liver cirrhosis. Hepatology. In press 2004
0. Kurtovic J, Ruettimann U, Adamson H, et al: Improvement inindocyanine green clearance following synbiotic treatment incirrhosis (abstr). Ear Nose Throat J 2003, 52(Suppl 3)
1. Miettinen M, Alander M, von Wright A, et al: The survival ofand cytokine induction by lactic acid bacteria after passagethrough a gastrointestinal model. Microb Ecol Health Dis1998, 10:41
2. Jain PK, McNaught CE, Anderson ADG, et al: Influence ofsynbiotic containing Lactobacillus acidophilus LA5, Bifidobac-terium lactis BP12, Streptococcus thermophilus, Lactobacillusbulgaricus and oligofructose on gut barrier function and sepsisin critically ill patients: A randomized controlled trial. ClinNutr. In press 2004
3. Bengmark S: Synbiotics to strengthen gut barrier functionand reduce morbidity in critically ill patients. Clin Nutr. In
press 2004