Dengue liza
-
Upload
dr-liza-bulsara -
Category
Health & Medicine
-
view
252 -
download
1
Transcript of Dengue liza

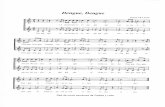
Dengue
ByDr. Liza Bulsara

l Benign Syndromel Causative Agent : Arthopod borne virus l Clinical Features: l Biphasic Feverl Myalgia\arthalgia.l Rash l Luekopenial Lymphadenopathy
l Dengue Haemorrhagic Fever: Severe, Fatal, febrile diseases caused by 1 out of 4 dengue virus.
l Clinical Features: l Capillary Permeabilityl Abnormalities of Haemostatsisl Protein losing shock syndrome (Dengue shock syndrome)

The Dengue Virusl Single stranded RNA virus l Positive sensel 40 to 50 nanometersl Flavivirus l Four sero-sub typesl Type 1 to 4
l Arthropod borne (zoonotic)l Man is accidentally infectedl Other vertebrates are reservoirs


Etiologyl 4 Distinct antigenic types of flavivirus.l Dengue 1l Dengue 2l Dengue 3l Dengue 4l Members of Family Flaviviridae.l Dengue like illness are caused by arthropod borne virus l Togavirus : Chikungunya (Africa, India, Southeast Asia, USA)l Togavirus : O'nyong-nyong (East Africa)l Flavivirus : West Nile Fever (Europe, Africa, Middle east, India)

Epidemiologyl Dengue virus are transmitted by mosquitoes “STEGOMYIA” family, AEDES AGEYTI, a day time biting mosquito, is the principal vector.
l A. Aegyti, is highly urbanised , breeding in water stored for drinking or bathing and in rainwater collected in any container .
l More than 390 million dengue infections occur annually, 96 million have clincial diseases,
l A. Aegyti has limited flight range, spread of epidemic occcurs mainly through viremic human beings and follows the main line of transportation, nearly simultaneous secondary infection give the appearance of a contagious disease.


Transmission Cycle
Intrinsic Incubation Period: 3-14 days
Viraemia & Fever: 5-7 days
VectorHumidity: Rainfall & Temp.
Susceptible hosts,(population)
Source patients
ExtrinsicIncubation Period: 8-10 days


Dengue Haemorrhagic feverl Endemic in asia and tropical america, wgere warm temperatures and the practise of water storage in homes plus outdoor breeding sites result in large, permanent populations of A.Aegypti.
l Primary Infection : First Infection .l Secondary Infection: It is followed by Primary infection with different dengue virus.

Pathogenesis l The virus is taken up by dendritic cells, and after antigenic processing, presents it to T- Cell, leading to immune activation and release cascade of cytokines that are believed to mdiate systemic effect of plasma leakeage and circulatory insufficiency.
l Thrombocytopenia develops due to the presence of cross-reacting antibodies to platelets and is responsible for bleeding diathesis.
l The original phenomeon of “Original antigenic shift” explains the increased severuty of the illness suring secondary infection, due to presence of antibodies to the previously infecting serotype.it leads to immune enhacement and causing severe haemorrhagic fever.
l Increased apoptosis and endothelial cell dysfunction.
l The major pathophysiologiuc change that determine the severity of disease and differentiate it from dengue infection are plasma leakage into third space and abnormal hemostasis ;leading to rising hemocit value and mod-marked thrombocytopenia along with varying degree of bleeding manisfestation.


Clinical Features Febrile Phase Critical Phase Recovery Phase Sudden onset fever Last for 2-7 days.
3-7 day of onset of fever After 24-48 hr of critical phase, a gradual reabsorption of extravasted fluid takes place takes place in 48-72 hours.
Facial Flushing Skin Ertheyema
Bleeding manisfestation and shock with fall in platelet count and increased in PCV
General well being improves, Apetite returns, GIT symptoms abate, haemodynamic status Stabilises
Generalised Body Ache Capillary Leakage In form of puffiness, ascites, edema and pleural effusion (Right side)
Skin rash “ isles of white in sea of red”
Myalgia/ Arthralgias/ backache Profound leakage of plasma Marked itching of extremitiesHeadache /Pain in eyes Hypovolamia—shock related
symptomsRespiratoey distress—pul edema
anorexia Restlessness/ cold extremities PCV Stabilies or becomes lowNausea/ vommitting Rapid thready pulse, low BP TLC NORMALSorethroat/ infected pharynx Delayed capillary refill filing PC rises slowlyBradycardia oliguria
ECG changes Organ dysfunction : hepatitis
Torniquet test: Positive Myocarditis,encephalitis
Pretechial, Mucosal bleeeding Severe bleeding without pl leakage
Hepatomegaly. Tender after2-5 daysDecrease in TLC , PC

C linical Manisfestation

l Incubation period: 4-10 days
l Clinical criterial high grade feverl hemorrhgic manifestation (a positive torniquet test)
l Tender hepatomegalyl Effusion in body cavities and shock.
l Laboratory criterial Thrombocytopenia l Rising hametocrit

Tourniquet Test
Inflate blood pressure cuff to a point midway between systolic and diastolic pressure for 5 min
Positive test: 20 or more petechiae / inch2 (6.25 cm2)
In an epidemic situation, the test is positive in 50% on the 1st day, and in 80% by the end of the febrile phase.

WHO classification of dengue infections and grading of severity of DHF


Differential Diagnosisl Influenzal Malarial Enteric feverl Leptospirosisl Flul Ricketessial feverl Chikungunya fever

Laboratory investigation l Hametological studies:l Gradual increase in PCVl Decrease in Platelet, leukocyte count.l Increase in lymphocytel Rising hematocrit or single hamatocrit more than 40% S/o capillary hemoconc. Due to capillary leakage
l low WBC with febrile illness in endemic season is a pointer towards possible dengue infection
l peripheral smear shows transformed lymphocytes
l shock reveals DIC

l Blood collection in tubes or vials
l The following are the steps for blood collection in tubes or vials:l Collect 2 ml–10 ml of venous blood with aseptic precautions.l Use adhesive tape marked with pencil, indelible ink, or a typewritten/printed self-adhesive
label to identify the container. The name of the patient, identification number and date of collection must be indicated on the label.
l Use vacuum tubes or sterile vials with screw caps and gasket, if possible, for collection. l Secure the cap with adhesive tape, wax or other sealing material to prevent leakage during l transport.l In case of an anticipated delay of more than 24 hours before specimens can be submitted to
the laboratory, separate the serum from the red blood cells and store frozen. Do not freeze
whole blood as haemolysis may interfere with serology test results.l Ship specimens to the laboratory on wet ice (blood) or dry ice (serum) as soon as possible. l The shipment should adhere to national/international guidelines on shipment of infectious
material

Biochemistry
l Decrese in total protein & albuminl Transaminases raisedl Increase in SGOT than SGPT s/o dengue infection
l Severe Cases: Hyponateremia & Acidosis. Increase in BUN and creatinine.

l Skiagram & Ultrasonography: Pleural effusion (Right side)
l Ultrasonography: Ascites & enlarged gall bladder due to wall edema
l Abnormal ECG & mycordial dysfunctionon ECGl Decrease in cardiac output l Decrease preloadl Decrease in left ventricularl Activation of complement system leads to profound depression of C3 AND C5 level.

Confirmatory test
l Antibody detection l Hemagglutination Inhibition (HAI)l ELISA (IgG/IgM) l Rapid test (IgG/IgM)l Antigen detection l NS1 & E/M antigenl RNA detection l PCRl Viral isolation

l Primary Infection
l NS1 antigen : Day 1 after onset of fever and up to day 9
l IgM antibody : Day 5 of infection, sometimes as early as Day 3
l IgM levels : peak in 2 weeks, followed by a 2 week rapid decay
l Undetectable 2 to 3 months after infectionl Low levels of IgG are detected in the early convalescent phase, not during the acute phase

l Secondary Infection
l NS1 antigen : day 1 after onset of fever and up to day 9IgM response is more varied
l Usually preceded by IgG and appears quite late during the febrile phase
l Minority of patients will show no detectable levels of IgM
l May not be produced until 20 days after onset of infection●
l High levels of IgG are detectable during the acute phase Persist for 30-40 days then decline to levels found in primary or past infection.


Approximate timeline of primary and secondary dengue virus infections and the diagnostic methods that can be used to detect infection

Treatment

DENGUE FEVERNo specific therapy – only symptomatic
Rest and Plenty of oral fluids
Use ParacetamolAvoid Aspirin and NSAIDs
Follow up preferably everyday - from the 3rd day until afebrile for 24-48 hours

General measuresFrequent monitoring of vitals.
Essential nursing care.
Stop bleeding with proper techniques e.g. anterior nasal packing for massive epistaxis.
Avoid blind invasive procedures e.g. no nasogastric tube insertion, no gastric lavage.
Soft, balanced, nutritious diet, juice and electrolyte solution – plain water is not adequate.
Avoid black- or red-colored food or drinks (may be mistaken for bleeding

Sedation is needed in some cases to restrain agitated child.
Chloral hydrate(12.5-50 mg/kg), orally or rectally recommended.Avoid Long-acting sedatives.
NCPAP should be preferred if there is Acute respiratory failure associated with DSS.
Oxygen via face mask/nasal cannula
in case of shock/impending shock.

H2-blockers (ranitidine)Recommended in case of gastrointestinal bleeding
Domperidone 1 mg/kg/day in three divided doses in case of severe vomiting for 1-2 days. One single dose may be adequate
Antibiotic Not necessary; it may lead to complications




FLUID MANAGEMENT
l In young infants without shock-l N/2 saline in 5% dextrose
l In patients who already have volume overload, i.e., massive pleural effusionl colloid solutions
l Hydroxyethyl starch at 6% may be preferred in children with severe shock; the use of dextran is associated with various adverse reactions

In case of no response to IV fluids:May have myocardial dysfunction and decreased LV performance, which may be easily detected by echocardiography.
Consider and correct
Massive plasma leakageConcealed internal bleeding – decrease in HctHypoglycemia – Blood sugar < 60 mg%Hyponatremia, hypocalcemia – electrolytesAcidosis – indicates metabolic acidosis in blood gas analysis

Blood and platelet transfusion
Platelet Transfusion: Thrombocytopenia with significant bleeding.Platelet count < 10,000/mm3 DOSE: 10-20 mL/kg

Platelets or blood should NOT be transfused based upon platelet count alone.
Low platelet count may not be predictive of bleeding.
Only 0.4% of DHF pts need platelet transfusion.
Mild reductions in platelet counts are usually not associated with significant bleeding.
In children with severe thrombocytopenia in absence of significant bleeding, platelet infusion does not alter the outcome.
Platelets return to normal within 7-9 days.

Fresh Whole blood / Packed red cell transfusion
Significant blood loss > 10% (6-8 mL/kg)Concealed internal bleedingHemolysis
DOSE
Fresh whole blood 10 mL/kg/dose Packed red cells 5 mL/kg/dose

Complications of DF/DSS
DICMyocardial dysfunction incl. CardiomyopathyHepatitisReye-like syndromeEncephalitisARDSGlomerulonephritis

Treatment of complications
Fluid overload AVOID
Early IV fluid therapy- in the febrile phaseExcessive use of hypotonic solutionsNon-reduction in the rate of IV fluid after initial resuscitationBlood loss replaced with fluids in cases with occult bleeding
Treatment
Judicious fluid removal colloids with controlled diuresis (furosemide 1 mg/kg infusion over 4 hours) or dialysis

Electrolyte imbalance
HyponatremiaHypocalcemia – 10% Ca gluconate 1 mL/kg/dose, slow IV push every 6 hour.
Large pleural effusions, ascites
Careful titration of intravenous fluids. Avoid insertion of intercostal drains and tracheal intubation. Large pleural effusions during recovery phase after 48 hoursfurosemide (0.25-0.5 mg/kg at 6 hours’ interval for 1 to 2 doses).

Disseminated intravascular coagulation
Frequent Clinical assessment
Regular Coagulation profile
PT, aPTT, fibrinogen, platelet and FDP mandatory, as indicated.
Seriously sick patients with bleeding & DIC have benefited from :
Platelets (4 units/m2 or 10-20 mL/kg) within 1 hr and Fresh frozen plasma (FFP 10-20 mL/kg).

Prognosis
DF is a very incapacitating disease; however, its prognosis is favorable.Significant morbidity and mortality can result if early recognition and monitoring of severe forms are not done.
If left untreated, the mortality of DHF or DSS patients may be as high as 40-50%.
Early recognition of illness, careful monitoring and adequate and appropriate fluid therapy have decreased mortality to 1%.
If shock is identified when pulse pressure starts to drop and intravenous fluids are administered, the outcome will be excellent.

Recovery is fast and most patients recover in 24-48 hours without any sequelae.
The outcome may not be so good if the patient develops cold extremities.
Most deaths from DHF/DSS are caused by
prolonged shock massive bleedingfluid overload and acute liver failure with encephalopathy.
Severe refractory shock, DIC, ARDS, liver failure and neurological manifestations singly or in combination were the commonest causes of death in a recent series.
The case fatality rate is high with shortage of experienced medical teams..

Criteria for Discharge of patients
l Visible clinical improvement with return of appetitel Stable pulse, blood pressure and respiratory ratel Afebrile for 24 hours (without anti-fever therapy)l Minimum of 3 days after recovery from shockl Good urinary output and stable haematocrit levelsl Platelet count > 100,000/mm3l No respiratory distress /pleural effusion /ascitesl No evidence of external or internal bleedingl Convalescent confluent petechial rash


VECTOR CONTROL
The control is primarily dependent on eradicating mosquito.Public spraying for mosquitoes is the most important aspect of this approach.
PERSONAL PROTECTION
Avoiding endemic areasCover exposed skin Mosquito nets, repellents Use of DEET-impregnated bed nets

Immunopathogenic l Cascade of DHF/DSS
l Macrophage – monocyte infection l Previous infection with heterologous
Dengue serotype results in production
of non protective antiviral antibodiesl These Ab bind to the virion’s surface
Fc receptor and focus the Dengue virus
on to the target cells – macro/monocytesl T cell - cytokines, interferon, TNF alpha