Cardiac Physical Examination
-
Upload
niken-widayanti -
Category
Documents
-
view
224 -
download
0
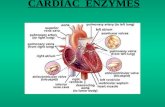
Transcript of Cardiac Physical Examination
-
7/28/2019 Cardiac Physical Examination
1/72
Bayu Laksono
Kartika Kristianto
Gloria Tanjung
Cardiac Physical Examination
-
7/28/2019 Cardiac Physical Examination
2/72
A. Inspeksi jantung
Tanda-tanda yang diamati :
(1) bentuk prekordium
(2) Denyut pada apeks jantung
(3) Denyut nadi pada dada
(4) Denyut vena
-
7/28/2019 Cardiac Physical Examination
3/72
bentuk prekordium
Pada umumnya kedua belah dada adalah simetris
Prekordium yang cekung dapat terjadi akibat
perikarditis menahun, fibrosis atau atelektasis
paru, scoliosis atau kifoskoliosis
Prekordium yang gembung dapat terjadi akibat daripembesaran jantung, efusi epikardium, efusi
pleura, tumor paru, tumor mediastinum
-
7/28/2019 Cardiac Physical Examination
4/72
sternotomy pada garis tengah menunjukkanbypass sebelumnya, torakotomi lateral
menunjukkan operasi bypass minimal invasif (left
internal mammary artery to left anterior
descending coronary artery) atau katup mitralsebelumnya
-
7/28/2019 Cardiac Physical Examination
5/72
Denyut apeks jantung (iktus kordis)
Dalam keadaaan normal, dengan sikap duduk, tidur terlentangatau berdiri iktus terlihat didalam ruangan interkostal V sisi kiriagak medial dari linea midclavicularis sinistra
Pada anak-anak iktus tampak pada ruang interkostal IV
Sifat iktus :
Pada keadaan normal, iktus hanya merupakan tonjolan kecil, yangsifatnya local. Pada pembesaran yang sangat pada bilik kiri, iktusakan meluas.
Iktus hanya terjadi selama systole.Oleh karena itu, untuk memeriksaiktus, kita adakan juga palpasi pada a. carotis comunis untukmerasakan adanya gelombang yang asalnya dari systole.
-
7/28/2019 Cardiac Physical Examination
6/72
Denyutan nadiApabila di dada bagian atas terdapat denyutan
maka harus curiga adanya kelainan pada aorta
Aneurisma aorta ascenden dapat menimbulkandenyutan di ruang interkostal II kanan,
sedangkan denyutan dada di daerah ruanginterkostal II kiri menunjukkan adanya dilatasi a.pulmonalis dan aneurisma aorta descenden
-
7/28/2019 Cardiac Physical Examination
7/72
Carotid pulse Diperiksa amplitudo, kontur, variasi, waktu carotid
upstroke berhubung S1 dan S2
Penyebab menurun pulsasi termasuk penurunan
stroke volume dan faktor di arteri seperti penyempitan
atherosclerotic atau penyumbatan Pulsus alternans, bigeminal pulse (beat-to-beat
variation); paradoxical pulse (respiratory variation)
Delayed carotid upstroke in aorticstenosis
-
7/28/2019 Cardiac Physical Examination
8/72
-
7/28/2019 Cardiac Physical Examination
9/72
Denyutan vena
Vena yang tampak pada dada dan punggungtidak menunjukkan denyutan
Vena yang menunjukkan denyutan hanyalah
vena jugularis interna dan eksterna
-
7/28/2019 Cardiac Physical Examination
10/72
JVP
Peningkatan tekanan menandakan CHF,constrictive pericarditis, tricuspid stenosis, or SVC
obstruction
98% spesifik untuk peningkatan ventrikel kiri dan
rendahnya fraksi ejeksi ventrikel kiri dan ini
meningkatkan resiko kematian dari gagal jantung
-
7/28/2019 Cardiac Physical Examination
11/72
Palpasi jantung
Urutan palpasi dalam rangka pemeriksaanjantung adalah sebagai berikut :
Pemeriksaan iktus cordis
Pemeriksaan getaran / thrill
Pemeriksaan gerakan trachea
-
7/28/2019 Cardiac Physical Examination
12/72
Pemeriksaan iktus cordis
Hal yang dinilai adalah lokasi, diameter, terabatidaknya iktus, dan apabila teraba dinilai kuat
angkat atau tidak, dan durasi.
Kadang-kadang kita tidak dapat melihat, tetapi
dapat meraba iktus
Pada keadaan normal iktus cordis dapat teraba
pada ruang interkostal kiri V, agak ke medial (2
cm) dari linea midklavikularis kiri.
-
7/28/2019 Cardiac Physical Examination
13/72
The apical impulse may be displaced upward andto the left by pregnancy or a high left diaphragm.
Lateral displacement from cardiac enlargement in
congestive heart failure, cardiomyopathy,
ischemic heart disease. Displacement in
deformities of the thorax and mediastinal shift.
-
7/28/2019 Cardiac Physical Examination
14/72
Pemeriksaan getaran / thrill Adanya getaran seringkali menunjukkan adanya
kelainan katub bawaan atau penyakit jantungcongenital.
Disini harus diperhatikan : Lokalisasi dari getaran
Terjadinya getaran : saat systole atau diastole
Getaran yang lemah akan lebih mudah dipalpasi apabilaorang tersebut melakukan pekerjaan fisik karena frekuensi
jantung dan darah akan mengalir lebih cepat.
Dengan terabanya getaran maka pada auskultasi nantinya
akan terdengar bising jantung
-
7/28/2019 Cardiac Physical Examination
15/72
Thrills dapat menyertai keras, keras, ataugemuruh murmur sebagai pada stenosis aorta,
patent ductus arteriosus, defek septum ventrikel,
dan stenosis, mitral
-
7/28/2019 Cardiac Physical Examination
16/72
Pemeriksaan gerakan trachea
Pada pemeriksaan jantung, trachea harus jugadiperhatikan karena anatomi trachea
berhubungan dengan arkus aorta
Pada aneurisma aorta denyutan aorta menjalar
ke trachea dan denyutan ini dapat teraba
-
7/28/2019 Cardiac Physical Examination
17/72
Pemeriksaan arteri perifer Palpate the radial pulse with the pads of your fingers on the
flexor surface of the wrist laterally. Partially flexing the patients
wrist may help you feel this pulse. Compare the pulses in both
arms.
-Prominent veins in an edematous arm suggest venous
obstruction brachial pulse. Flex the patients elbow slightly, and with the
thumb of your opposite hand palpate the artery just medial to the
biceps tendon at the antecubital crease
- check arterial insuffieciency
-
7/28/2019 Cardiac Physical Examination
18/72
femoral feel at the midinguinal point (midway between thesymphysis pubis and the anterior superior iliac spine, just inferior
to the inguinal ligament)
popliteal feel deep in the center of the popliteal fossa with thepatient lying on their back with their knees bent
- widened femoral and popliteal pulse suggests an aneurysm of
the popliteal artery. Neither popliteal nor femoral aneurysms are
common. They are usually due to atherosclerosis, and occur
primarily in men over age 50.
-
7/28/2019 Cardiac Physical Examination
19/72
posterior tibial feel behind the medial malleolus
dorsalis pedis feel over the second metatarsalbone just lateral to the extensor hallucis tendon
-
7/28/2019 Cardiac Physical Examination
20/72
The dorsalis pedis artery may be congenitally absent or maybranch higher in the ankle. Search for a pulse more laterally.
Decreased or absent foot pulses (assuming a warm
environment) with normal femoral and popliteal pulses suggest
occlusive disease in the lower popliteal artery or its branches a
pattern often associated with diabetes mellitus. Sudden arterial occlusion, as by embolism or thrombosis, causes
pain and numbness or tingling. The limb distal to the occlusion
becomes cold, pale, and pulseless. Emergency treatment is
required. If collateral circulation is good, only numbness and
coolness may result.
-
7/28/2019 Cardiac Physical Examination
21/72
Percussion
-
7/28/2019 Cardiac Physical Examination
22/72
Percussion
Careful percussion will usually reveal
whether the heart is normal in size or
whether it is definitely marked
enlarged.
One should use the lightest percussion
possible and, with experience, rely
more and more upon the vibratory
-
7/28/2019 Cardiac Physical Examination
23/72
To determine the left border of the heart,percussion should begin at the lateral side and
percuss toward the sternum. The dullness usually
reveal along mid clavicular line.
-
7/28/2019 Cardiac Physical Examination
24/72
To determine the left border of the heart percussfrom left lateral toward medial.
The left border : the anterior axillary line.
The right border : the right sternal line.
the upper border (base of the heart): 2nd left
interspace.
-
7/28/2019 Cardiac Physical Examination
25/72
Physiologic changes in the area of
cardiac dullness
The position of the heart, and with it the area ofcardiac dullness, is influenced by the level of the
diaphragm.
In deep inspiration the diaphragm descends,producing a decrease in cardiac dullness, while in
forced expiration the diaphragm rises and produces
an increase in the cardiac dullness.
-
7/28/2019 Cardiac Physical Examination
26/72
In the later months of pregnancy thediaphragm is pushed upward, causing the
heart to lie more horizontally and closer to the
chest wall, thus increasing the area of cardiac
dullness.
-
7/28/2019 Cardiac Physical Examination
27/72
Cardiac dullness in
abdominal distention
A variety of pathologic conditions such asascites, an ovarian cyst, or peritonitis may
cause an elevation of the diaphragm with an
increase in the area of cardiac dullness.
-
7/28/2019 Cardiac Physical Examination
28/72
Changes in position of
cardiac dullness
A left-sided pleural effusion will push the heart
to the right, and increase the cardiac dullness
to the right of sternum, the left border in suchcases can usually not be made out. A right-
sided pleural effusion increase the cardiac
dullness on left side.
-
7/28/2019 Cardiac Physical Examination
29/72
In pneumothorax the heart is displaced toward
the normal side, but in massive collapse of the
lung the heart is displaced toward the affected
side.
Pleural adhesions may pull the heart to the
affected side with resulting changes in
cardiac dullness similar to those produced bycollapse of the lung.
-
7/28/2019 Cardiac Physical Examination
30/72
Decrease in the area of
cardiac dullness
A decrease in the relative cardiacdullness may occur in pulmonary
emphysema. The absolute cardiac
dullness is usually decreased insuch cases, since the lung is
increased in size and covers a
greater area of the heart than
normal.
-
7/28/2019 Cardiac Physical Examination
31/72
Increase in the area of
cardiac dullness
An increase in the area of cardiac dullness is
most strikingly seen in patients with cardiac
disease. we cannot detect by percussion an
appreciable increase of the cardiac dullness inhypertrophy of the heart unless there is an
accompanying dilatation.
-
7/28/2019 Cardiac Physical Examination
32/72
Cardiac enlargement
Enlargement of the left ventricle produces anincrease in the relative cardiac dullness to the
left and often downward on this side.
The heart silhouette looks like a shoe
-
7/28/2019 Cardiac Physical Examination
33/72
Enlargement of the left ventricle appears inaortic insufficiency, in aortic stenosis, in mitral
insufficiency, in longstanding hypertension
and in chronic nephritis. It is called aortic
heart.
Right ventricular enlargement, the cardiac
dullness will extended to left and upward. Ifthe right ventricular is severely enlarged, the
right border of the heart will extend to the right.
It is seen in cor pulmonale, in mitral stenosis,
in tricuspid insufficiency etc.
-
7/28/2019 Cardiac Physical Examination
34/72
Both the left atrium and pulmonary arteryenlarged, the pulmonary artery will be
exaggerated to leftward. The cardiac
silhouette is like a pear and called mitral heart,
it is frequently seen in mitral valve stenosis.
The heart silhouette is like a
ear
-
7/28/2019 Cardiac Physical Examination
35/72
Aortic dilation, aneurysm of aorta, pericardialeffusion, all those diseases may cause thebase border of heart enlargement, so that thebase border of the heart will be widened.
Congestive heart failure, severe myocarditis,Keshan disease, dilated myocardiopathy maycause the heart silhouette extending both to
right and left.
-
7/28/2019 Cardiac Physical Examination
36/72
Pericardial effusion
The cardiac dullness is increased in alldirections and assumes the form of a triangle
with the apex at the level of the first or second
intercostal space or a general globular
enlargement.
The heart silhouette is like
a flask
The heart silhouette is like a globe
-
7/28/2019 Cardiac Physical Examination
37/72
Adhesive pericarditis
The degree of enlargementdepends on the extent of the
adhesive process. The relative, and
especially the absolute, cardiacdullness are both markedly
increased to left and to the right.
-
7/28/2019 Cardiac Physical Examination
38/72
Increase in the absolute
cardiac dullness
Increase in the absolute cardiac dullnesswithout demonstrable cardiac enlargement
occurs when the left lung is retracted and a
larger area of the ventricle is exposed.
It also occurs in mediastinal tumors when the
heart is pushed up against the chest wall and
a large area of the ventricle comes into directcontact with the anterior surface of the chest.
-
7/28/2019 Cardiac Physical Examination
39/72
AUSCULTATION
-
7/28/2019 Cardiac Physical Examination
40/72
-
7/28/2019 Cardiac Physical Examination
41/72
-
7/28/2019 Cardiac Physical Examination
42/72
First Heart Sounds S1 is produced by closure of the mitral and tricuspid
valves in early systole
is loudest near the apex of the heart
it is high-frequency sound best heard with
diaphragm of stethoscope
mitral closure usually precedes tricuspid closure
they are separated by only about 0.01 sec
so,, human ear appreciates only a single sound
if right bundle branch is blocked mitral &
tricuspid may be audible split due to delayed
closure of tricuspid valve
F d i h i i f
-
7/28/2019 Cardiac Physical Examination
43/72
Factor determinate the intensity of
S1
the distance separating the leaflets of the openvalves at the onset ventricular contraction
relates to PR interval
the mobility of the leaflets (normal or rigid due to
stenosis)
the rate of rise of ventricular pressure
-
7/28/2019 Cardiac Physical Examination
44/72
Altered Intensity of S1
accentuated S1 shortened PR interval
mild mitral stenosis
high cardiac output states or tachycardia (eg.
exercise or anemia)
diminished S1
lengthened PR interval: first-degree AV nodal block
mitral regurgitation
severe mitral stenosis
stiff left ventricle (eg. systemic hypertension)
-
7/28/2019 Cardiac Physical Examination
45/72
Second Heart Sounds S2 results from the closure of the SL valves has 2 components:
aortic (A2)
pulmonic (P2)
Components of S2 are heard varying sounds with
respiratory cycle: (this situation is termed normal
or physiologic splitting)
theyre normally fused as one sound during
expiration
theyre audibly separated during inspiration
-
7/28/2019 Cardiac Physical Examination
46/72
during inspiration expansion of the chest intrathoracic pressure more negative
capacitance ( impedance) of the intrathoracic
pulmonary vessels temporary delay in the
diastolic backpressure of the pulmonary artery P2 is delayed (occurs later during inspiration
than during expiration)
-
7/28/2019 Cardiac Physical Examination
47/72
-
7/28/2019 Cardiac Physical Examination
48/72
Abnormalities of S2
alteration of its intensity changes in the pattern of splitting
-
7/28/2019 Cardiac Physical Examination
49/72
Alterations of its intensity of S2
Depends on: velocity of blood coursing back toward the valves
from the aorta and pulmonary artery after the
completion of ventricular contraction
the suddenness with which that motion is arrestedby the closing valves
In systemic of pulmonary artery hypertension
diastol pressure in respective great artery
velocity of blood surging toward the valve S2 Severe aortic and pulmonary stenosis
the valve commisure are nearly fixed in position
S2
-
7/28/2019 Cardiac Physical Examination
50/72
Changes in splitting in pattern
Widened splitting refers to in the time interval between A2 and P2
the 2 components are audibly separated even
during expiration and become more widely
separated in inspiration
result from delayed closure of the pulmonic valve
(eg. right bundle branch block, pulmonic valve
stenosis)
-
7/28/2019 Cardiac Physical Examination
51/72
Changes in splitting in pattern
Fixed splitting refers to abnormally widened interval between A2
and P2 that persist unchanged through the
respiratory cycle
results fromASD (ASD chronic volume
overload of right-sided circulation
capacitance, resistance pulmonary pressure
delay the backpressure responsible from
closure of pulmonary valve P2 delayed thannormal)
-
7/28/2019 Cardiac Physical Examination
52/72
Changes in splitting in pattern
Paradoxical splitting = Reverse splitting opposite of the normal situation
refers to audible separation of A2 and P2 duringexpiration that disappears on inspiration
the most common cause is Left Bundle BranchBlock (LBBB)
LBBB electrical activity within LV impaired delayed ventricular contraction late closure
aortic valve A2 followed P2 when inspiration, normally P2 occur later and A2
earlier but in LBBB due to A2 delayed P2 andA2 are heard as one sound.
-
7/28/2019 Cardiac Physical Examination
53/72
Extra Systolic Heart Sounds
May occur in early, mid-, or late systole
1. Early Extra Systole Heart Sounds = ejection
clicks
occur shirtly after S1 and coincide with the opening
of the aortic or pulmonic valves
have a sharp, high pitched quality heard best
with the diaphragm of stethoscope, placed over the
aortic and pulmonary areas
-
7/28/2019 Cardiac Physical Examination
54/72
Extra Systolic Heart Sounds
indicate: Aortic or Pulmonic valve stenosis: sound occurs as
the leaflets reach their maximal level of ascent intothe great artery, just prior to blood ejection
Dilatation of the Pulmonary artery or Aorta: sound isassociated with sudden tensing of the aortic orpulmonic root with the onset of blood flow into thevessel aortic ejection click:
Is heard at both base and apex Doesnt vary with respiration
pulmonic Ejection Click: Is heard only at the base
Intensity during inspiration
-
7/28/2019 Cardiac Physical Examination
55/72
Extra Systolic Heart Sounds
2. Mid
or Late Extra Systolic Heart Sounds result of systolic prolapse of the mitral or tricuspid
vein
leaflets bulge abnormally into the atrium during
ventricular contraction.
often accompanied by valvular regurgitation
mitral louder than tricuspid
-
7/28/2019 Cardiac Physical Examination
56/72
Extra Diastolic Heart Sounds
opening snap(OS)
the third heartsound (S3)
the fourth heartsound (S4)
QuadrubpleRythm or
SummationGallop
the pericardial
knock
-
7/28/2019 Cardiac Physical Examination
57/72
Opening Snap
refers to sound that are produced by the mitral ortricuspid valvular stenosis when they open
a sharp, highpitched sound, and timing doesnt
vary significantly with respiration
OS is heard best between apex & left sternalborder, just after the aortic closure sound (A2)
The severity of stenosis can be approximated by
the time interval between A2 and OS :
advanced stenosis interval A2 OS
In mild interval A2 OS
-
7/28/2019 Cardiac Physical Examination
58/72
Third heart sound after S2
result from tensing of the chordae tendinae duringrapid filling and expansion of the ventricle
occurs in early diastole, following the opening of theAV valves during the ventricular rapid filling phase
a dull, low pitched sound best heard with the bell of
the stethoscope S3 normal in children and young adults
implies the presence of a supple ventricle capable ofnormal rapid expansion in early diastole
S3 sign of disease in mid age or older adults
indicating volume overload due to CHF, ortransvalvular flow that accompanies advanced mitral ortricuspid regurgitation
Pathologic S3 Ventricular Gallop
Fourth Heart Sound before
-
7/28/2019 Cardiac Physical Examination
59/72
Fourth Heart Sound beforeS1
is generated by the L or R atrium vigorouslycontracting against the stiffened ventricle
occurs in late diastole and coincides withcontraction of the atria
usually indicates the presence of cardiac disease spesifically ventricular compliance typicallyresult from ventricular hypertrophy or myocardialischemia.
a dull, low pitched sound best heard with thebell
loudest at the apes when patient lying in the L.Lateral decubitus position
S4 atrial gallop
-
7/28/2019 Cardiac Physical Examination
60/72
Quadrubple Rythm or Summation
-
7/28/2019 Cardiac Physical Examination
61/72
Quadrubple Rythm or Summation
Gallop
in patient with S3 and S4 in conjunction with S1and S2 quadrupic beat
if this patient develops tachycardia duration of
diastole S3 and S4 coalesce summation
gallop (heard as as long mid diastolic, low-pitchedsound, often louder than S1 and S2)
-
7/28/2019 Cardiac Physical Examination
62/72
Pericardial Knock
results from the abrupt cessation of ventricularfilling in early diastole
appears early in diastole soon after S2 ; but
slightly later than OS and is louder ; and earlier
than ventricular gallop uncommon, high pitched sound
hall mark of constrictive pericarditis
-
7/28/2019 Cardiac Physical Examination
63/72
Murmurs
the sound generated by turbulent blood flow the mechanisms which produce murmus:
flow across a partial obstruction (eg. Aortic stenosis)
flow through normal structures (eg. Aortic systolic
murmur associated with high output state, anemia) ejection into a dilated chamber (eg. Aortic SM
associated with aneurysmal dilatation of the aorta)
regurgitant flow across an incopetent valve (eg.
Mitral reg) abnormal shunting of blood from 1 vascular
chamber to a lower pressure chamber (eg.
Ventricular septal defect)
-
7/28/2019 Cardiac Physical Examination
64/72
Description of Murmur
1. timing whether murmur occurs during systole,diastole, or continous
2. intensity is typically quantified by a grading systemsystolic murmurs
systo l ic mu rmurs grade 1/6 (or I/VI) : barely audible (eg. medical students may not
hear it) grade 2/6 (or II/VI) : faint but immediately audible grade 3/6 (or III/VI) : easily heard grade 4/6 (or IV/VI) : easily heard and associated with a palpable thrill
grade 5/6 (or V/VI) : very loud; heard with a stethoscope lightly on thechest
grade 6/6 (or VI/VI) :audible without the stethoscope directly on thechest wall
dias to l ic m urmu rs grade 1/4 (or I/IV): barely audible
grade 2/4 (or II/IV): faint but immediately audible
grade 3/4 (or III/IV): easily heard
grade 4/4 (or IV/IV): very loud
-
7/28/2019 Cardiac Physical Examination
65/72
-
7/28/2019 Cardiac Physical Examination
66/72
-
7/28/2019 Cardiac Physical Examination
67/72
3. pitch frequency of the murmur High are caused by large pressure gradients
between chambers (eg. Aortic stenosis)
Low smaller pressure gradient (eg. Mitral
stenosis)4. shape how the murmur changes in intensity
from its onset to its completion.
CresendoDecresendo (diamond shaped)
Decresendo Uniform (intensity doesnt change shape)
-
7/28/2019 Cardiac Physical Examination
68/72
5. location the murmurs region of maximalintensity
6. radiation murmurs are often heard to radiate
to other areas of the chest from their primary
location7. response to maneuvers maneuvers can alters
the hearts loading conditions and can affect the
intensity of many murmurs.
maneuvers: standing upright, Valsava (forceful
expiration against a closed airway), clenching of
the fist
-
7/28/2019 Cardiac Physical Examination
69/72
-
7/28/2019 Cardiac Physical Examination
70/72
-
7/28/2019 Cardiac Physical Examination
71/72
-
7/28/2019 Cardiac Physical Examination
72/72
Thank you