Predictors of withdrawal: Possible precursors of avoidant personality disorder
The manualization of a treatment programme for personality disorder
-
Upload
nottingham -
Category
Documents
-
view
0 -
download
0
Transcript of The manualization of a treatment programme for personality disorder
The manualization of a treatmentprogramme for personality disorder
MARY MCMURRAN1 AND CONOR DUGGAN2, 1School of Psychology,Cardiff University, Cardiff, UK; 2Division of Psychiatry, University ofNottingham, Nottingham, UK
ABSTRACTBackground The advantages of manualized psychological treatments include: thepromotion of evidence-based practice, the enhancement of treatment integrity, thefacilitation of staff training, and the potential replicability of treatment.Argument The manualization of a multi-component, multidisciplinary treatmentprogramme for male personality-disordered offenders is described. The backgroundto this development is explained and the treatment setting is described briefly,followed by a description of the eight treatment manuals: (1) the treatmentoverview, (2) Psychoeducation focusing on personality disorder diagnosis and corebeliefs, (3) Trust and Self-awareness group exercises, (4) Stop & Think! - a socialproblem-solving intervention, (5) Controlling Angry Aggression, (6) ControllingSubstance Use, (7) Criminal Thinking/Belief Therapy, and (8) Skills for Living - asocial skills manual.Conclusions In addition to the original aims of manualization, this exercise hasclarified the treatment programme, included less highly trained staff in the delivery oftherapy and permitted the evaluation of treatment modules, thus contributing to theincremental evaluation of the overall programme. These manuals may usefully beshared with other practitioners in the field.
Introduction
Treatment manuals that guide the practitioner in the application of psycho-logical therapies have three principal advantages. One is that they enhancetreatment integrity, the second is that they facilitate staff training, and the thirdis that they permit treatments to be replicated. There are also perceived disad-vantages with manualized treatments: they may be seen as prescriptive, rigid andsterile. In this paper, we elaborate on the potential advantages of treatment
Criminal Behaviour and Mental Health, 15, 17–27 2005 © Whurr Publishers Ltd 17
CBMH 15.1 2nd 4/8/05 12:28 PM Page 17
manuals, address the potential disadvantages, and describe the manualization ofa multi-component treatment programme for personality-disordered offenders.
The development of treatments for this group of patients is of particularimportance, since the NHS National Institute for Mental Health in England(NIMHE) issued guidance in a report whose title summarizes the directionmental health services are expected to take: Personality Disorder: No Longer aDiagnosis of Exclusion (NIMHE, 2003a). The development of services for peoplewith personality disorders has turned attention to the capabilities of theworkforce in treating people with personality disorders (NIME, 2003b).Manualized treatments may help in building up a skilled workforce in mentalhealth services, as has been evident with the implementation of structuredprogrammes in prison and probation services in the UK and elsewhere(McGuire, 2001).
Advantages of treatment manuals
Effective treatment is theory-driven and evidence-based. Once a treatmentprogramme has been designed according to theory and evidence, adherence tothese principles in practice is important. This is the concept of ‘treatmentintegrity’ defined by Hollin (1995) as meaning ‘that the programme isconducted in practice as intended in theory and design’ (p. 196). Fundamentalto programme integrity is a clear statement of what is to be done in treatmentand how. Manuals do this to a greater or lesser degree. There are different typesof treatment manual – those that are prescriptive, detailed, session-by-sessionrecipes for treatment, or those that are more conceptual, emphasizing anindividual case approach (Addis and Krasnow, 2000).
Treatment integrity also requires that staff are adequately trained in theprinciples and practice of treatment, and thereafter are monitored and super-vised so that their practice develops appropriately, preventing drift from theoriginal principles. Treatment manuals provide a focus for these activities. Theycan provide the basis for training experienced clinicians in new treatments and,in an ongoing treatment programme, they offer an effective basis for trainingnew members of staff, so minimizing the threat to treatment integrity posed bystaff turnover.
Treatment manuals have a particularly important role in providing supportand structure to less experienced practitioners. Crits-Cristoph et al. (1991), in ameta-analysis of psychotherapy outcome, found that the use of treatmentmanuals reduced variability in treatment outcome across therapists. This effectwas particularly important with inexperienced therapists, where the variabilitywas wide. Therefore, although manuals may reduce the effectiveness of the verybest experienced therapists, adherence to manuals offers a minimum qualityassurance. Crits-Cristoph et al. (1991) found the variability in treatmentoutcome among experienced therapists to be small, and so structured manuals
18 McMurran, Duggan
CBMH 15.1 2nd 4/8/05 12:28 PM Page 18
may be less important in guarding against poor outcomes with this group.Nevertheless, even experienced therapists need to adhere to what is evidence-based in treatment, and it is with this group that more conceptual manuals mayhave a place.
As for other treatments, continued support and supervision are vital toensure the integrity of manualized treatments: just because a treatment ismanualized does not mean that it is simple (Castonguay et al., 1999). Wilson(1996) argues that having the content of treatment manualized enables super-vision to focus less on techniques and more on the process aspects ofimplementation.
As well as enabling the use of treatments that have an evidence base,manuals have a role in contributing to the build-up of that evidence base.Evidence-based practice is the guiding principle for healthcare in today’s NHS,and this raises questions as to what is an acceptable as an evidence base. Beutler(2000) pointed out that the US Food and Drug Administration requires aminimum standard of two, independent, controlled studies that show statisticalsignificance of a drug effect over no treatment or a placebo, and he suggests thatpsychological therapies should be subject to the same standards. The key to thisis the ability to replicate a treatment, and manuals assist with this.
Treatment manuals offer a number of advantages in the promotion anddevelopment of evidence-based practice, the facilitation of treatment integrity,and staff training and supervision; however, there are criticisms of manualizedtreatments.
Disadvantages of treatment manuals
One major criticism of treatment manuals is that all clients are treated with astandardized approach that does not permit the use of clinical judgement. Thereis no individual case formulation that would reveal the particular factors impli-cated in the development and maintenance of a client’s problem. Wilson (1996)counters the clinical judgement argument by querying the validity of case formu-lation. In clinical case formulation a vast quantity of complex information has tobe processed by the therapist, who has to choose from a large number of theoriesin which to frame the information, and is prone to an element of cognitive biasbased on personal perspectives. Consequently, the validity of case formulation issuspect. Wilson (1996) suggests that, since clinical judgement may be inaccurateand could lead to inferior results compared with standardized treatment, anactuarial approach to treatment is ethically defensible. Application of the mosteffective approach known for a particular problem has a good chance of beingeffective, particularly in multi-component programmes, although the effec-tiveness of using this simple decision rule requires empirical testing.
Another concern is that the manualized treatments reduce the ‘art’ oftherapy. This has led to attempts to define the nature of the art in therapy and
Manualization of a treatment programme for PD 19
CBMH 15.1 2nd 4/8/05 12:28 PM Page 19
an assessment of whether or not this really is curtailed by manualized treat-ments. If the art is flexibility in terms of hypothesis testing as treatmentprogresses, then allowing no scope for changing therapeutic tack according tothe client’s response is removed in the more rigid manuals. However, the use offlexible hypothesis testing in therapy is not entirely supported by evidence:clinicians often form opinions early on and these opinions are subject to confir-matory bias, exacerbated by dispositional theories of human behaviour (Wilson,1998). Alternatively, if the art is taken to mean building rapport, engaging theclient and developing a therapeutic relationship, then manualization does notremove the need for these clinical skills (Wilson, 1996). When training to use amanualized treatment, therapists are often initially thrown by the apparentemphasis on technique over process, but the techniques cannot work in theabsence of a therapeutic alliance. Clinical competence is crucial to the effectiveuse of manualized treatments.
The standardized approach of manualized treatments may not, therefore, bedoing the client a disservice. Furthermore, they may be seen as the first line in astepped care approach, where individualized treatments by experienced thera-pists may be a next step if the manualized treatment fails.
A different response to the one-size-fits-all criticism is to increase the flexi-bility of manuals (Henin et al., 2001). Within the context of decision rulesthat guard treatment replication, flexibility can be increased by using amodular approach, fitting people to the aspects of treatment that meet theirneeds. Another method of increasing flexibility is to specify the sessionformat, but allow the session content to be guided by the patient’s currentproblems.
Indeed, it is likely that there is a client x therapist x therapy x manualinteraction in achieving successful therapeutic outcome. In psychodynamicpsychotherapy training there is some evidence that manualization makessome therapists worse (Vacoch and Strupp, 2000). In the Vanderbilt II study,Henry et al. (1993a, 1993b) compared the effectiveness of therapists beforeand after they had been trained using a manualized form of psychodynamictherapy. Although the therapists were found to follow the manual, they werealso found to display more negative processes in therapy, with therapists whowere most controlling and self-blaming being the most likely to adhere to thetreatment manual. In one respect, this is not fair evaluation of manualizationin that, as the authors admit, all of the therapists who were trained to use themanuals were already experienced therapists . A more informativecomparison would have been a before-and-after design with inexperiencedtherapists as this would be the situation that would more usually apply inpractice. What this does point to, however, is that there is variability amongtherapists in their performance with manualized therapies, and this requiresfurther investigation, both for good clinical practice and as a variable inclinical research.
20 McMurran, Duggan
CBMH 15.1 2nd 4/8/05 12:28 PM Page 20
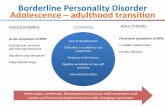
Arnold Lodge Personality Disorder Unit
We turn now to the manualization of a multi-component treatment programmefor people with personality disorder. This was developed at Arnold Lodge, asecure forensic mental health unit in Leicester, UK, which was commissioned in1998 to provide a service for men with personality disorder. As a result, a 10-bedded (later increased to 12-bedded) Personality Disorder Unit (PDU) wasopened in 1999. The PDU treatment programme aims to develop and maintaintherapeutic relationships, to teach people skills for appropriate containment oftheir behavioural disturbance, and to address some of the interpersonal diffi-culties that are at the core of personality disturbance. These therapeutic tasksare addressed in the all stages of assessment and treatment (post-admissionassessment, treatment and pre-discharge), by all disciplines, and in various ways,including a therapeutic milieu, structured individual work, structured grouptreatment, and a range of individual therapies. The components of the PDUprogramme are shown in Figure 1.
Although admission depends on a psychiatric diagnosis, people diagnosed assuffering from personality disorder need not be treated according to theirdiagnostic category, but rather treated according to the problems they typicallyexperience. This is not to suggest that underlying factors are ignored but ratherthat they are addressed within a problem-focused approach. Castonguay et al.
Manualization of a treatment programme for PD 21
Therapeutic milieu
Assessment
Stop & Think!Controlling
angry aggressionControlling substance
use
Trust & Self-awareness
Social and life skills
Criminal beliefs therapy
Integrating therapies
Psychoeducation
Figure 1. The Arnold Lodge PDU treatment programme.
CBMH 15.1 2nd 4/8/05 12:28 PM Page 21
(1999) point out that, because of the complexity of Axis II disorders, treatmentfor these clients cannot focus on a single diagnosis, but should instead be broad-based. This leads to a multi-component treatment, which Henin et al. (2001)noted as one way to increase the flexibility of manualized treatments to meetthe individual’s needs. The multidisciplinary input means that the theoreticalperspectives of the treatment components may differ, although most compo-nents are cognitive-behavioural. This is in line with manualization oftreatments generally: although psychodynamic and interpersonal psychother-apies have been manualized, most manualized treatments arecognitive-behavioural (Scaturo, 2001).
The treatment manuals
Originally only two components of the PDU treatment programme weremanualized: Controlling Angry Aggression and Controlling Substance Use. Thesewere structured, cognitive-behavioural programmes, designed by a psychol-ogist, which is unsurprising since cognitive-behavioural psychologists arethose who most favour the use of manuals in treatment (Addis and Krasnow,2000). In 2000, the PDU gained Beacon status as a site of good practice in thetreatment of personality disorder. The NHS Beacon programme was launchedin 1999 to identify services that make significant contributions to modern-izing the NHS. In acquiring Beacon status, a service was obliged to share goodpractice with others. As a Beacon service, the PDU held a number ofsuccessful open days, when professionals would visit and learn about the PDUtreatment programme. It became clear that the level of interest in thetreatment was high, and other services were keen to implement some, if notall, aspects of the PDU treatment programme. The existing treatment manualsclearly facilitated the sharing of practice, and so a decision was eventuallymade to attempt to capture the entire treatment programme in a set ofmanuals. Funding for the task was obtained from Nottinghamshire HealthcareNHS Trust.
The project was a collaborative effort by representatives of all disciplinesinvolved in the design, development and application of treatments. Managedby a psychologist with the help of an assistant psychologist, the programmedirector, psychiatrists, nurses, psychologists, an occupational therapist andresearchers all contributed to the manualization of the treatment programme.Quarterly project meetings were held with the PDU team, and the productionof most of the manuals occurred off-site. The process took 15 months in all.
The PDU treatment programme has been captured in eight manuals – anoverview plus seven treatment manuals:
(1) The Personality Disorder Unit: A research treatment programme forpersonality-disordered offenders;
22 McMurran, Duggan
CBMH 15.1 2nd 4/8/05 12:28 PM Page 22
(2) Psychoeducation;(3) Trust and self-awareness;(4) Stop & Think!;(5) Controlling angry aggression;(6) Controlling substance use;(7) Criminal thinking/belief therapy;(8) Skills for living.
The PDU overview is a comprehensive document, containing information onthe theory behind the treatment programme, selection criteria, assessmentinstruments, the operational running of the unit, audit procedures, staffselection and training, and the research agenda. Guided by this document, thetreatment infrastructure can be replicated.
Psychoeducation consists of eight individual sessions, focusing first on clari-fying the patient’s diagnosis and then on identifying core schema related to thepatient’s problems. This component developed from information that fewpatients understood their diagnosis, and that those who did had picked up theinformation from reports rather than having been informed by a clinician(D’Silva and Duggan, 2002). This component is intermediate in structure, withthe procedure used to discuss personality disorder specified, but methods ofaddressing concerns and raising core beliefs requiring clinical expertise.Discussing personality disorder diagnosis, traits and schema in a collaborativedialogue not only informs the patient but also builds a therapeutic alliance.
Trust and Self-Awareness is a 20-session group programme consisting ofexercises aimed broadly at improving group cohesion and building an atmos-phere of trust to ease communication among group members. Developed andimplemented by nurses, this programme is based on experiential therapyapproaches.
Criminal Thinking/Belief Therapy is a 12-session structured group aimed atcorrecting criminal thinking styles, as identified by Walters (1995).Maladaptive thinking styles, such as rationalization, entitlement and incon-gruity, are identified and challenged, thus opening up a person’s life choices.
Stop & Think! is a social problem-solving intervention based on the work ofD’Zurilla and Goldfried (1971). This manual differs from the others in that it isa conceptual manual rather than a structured session-by-session account oftreatment. Social problem-solving is a core aspect of treatment and all patientsattend this rolling group. The process of problem-solving is invariant but theproblems addressed in any session are those that are of current concern to thepatients. This counterbalances the high structure of other treatment compo-nents, and adds to the flexibility of the treatment to meet the individual’s needs(Henin et al., 2001). In addition to groups, the problem-solving process isreinforced in individual work with patients. McMurran et al. (1999) piloted theStop & Think! group with a mix of stable mentally ill and personality-disordered
Manualization of a treatment programme for PD 23
CBMH 15.1 2nd 4/8/05 12:28 PM Page 23
patients, leading to significant improvements on the Social Problem SolvingInventory – Revised (SPSI-R; D’Zurilla et al., 2002). It has since been evaluatedwith PDU patients, finding significant improvements on the SPSI-R over thefirst six months of treatment, an effect maintained at nine months (McMurran,Fyffe, et al., 2001).
Controlling Angry Aggression is a 15-session structured group treatmentprogramme offered only to those who need this treatment, as identified byclinical judgement and psychometric testing. It is based on Robins and Novaco’s(1999) system approach to anger and aggression and using a ‘personal scientist’approach to teach participants methods of self-control (Mahoney andThoresen, 1974). There are two Stop & Think! sessions within the programme toillustrate to patients that the problem-solving approach is applicable to angerproblems, as well as the more specific cognitive-behavioural techniques taughton the programme. Controlling Angry Aggression has been piloted with only fourpatients, three of whom did better on psychometric measures of anger andaggression after treatment (McMurran, Charlesworth et al., 2001). Important tonote was that ongoing self-monitoring indicated fluctuations in anger experi-ences but behaviour was stable over that same period. This was a good learningexperience: even though external constraints may have played a major role, theevidence was that anger can be controlled.
Controlling Substance Use is similar in structure to Controlling AngryAggression. It is a 15-session structured group treatment programme offered onlyto those with substance-related problems, as identified by clinical judgementand psychometric testing. Again, it uses a ‘personal scientist’ approach to self-control, and it contains two Stop & Think! sessions to illustrate to patients thatthe problem-solving approach is applicable to problems relating to drugs andalcohol.
Skills for Living is a 17-session structured social skills training group,developed by the occupational therapist, and covering a range of personal andinterpersonal skills, such as positive thinking, communication, negotiation andstress management.
The suite of manuals permits a degree of tailoring to meet clients’ needs.While there are components in which every patient is expected to participate(e.g. Psychoeducation and Stop & Think!), there are others that are optional,depending on need (e.g. Controlling Angry Aggression and Controlling SubstanceUse). These needs are assessed by the clinical team prior to admission to ensurethat the needs of the patient can be met by the PDU treatment programme, andthroughout the patient’s stay in the PDU, to respond to identified changes inneed. The treatment is a mix of structured and conceptual approaches, anddifferent manuals will appeal to different practitioners: less experienced practi-tioners may prefer the highly structured manuals, and experienced practitionersmay prefer the conceptual manuals (Addis and Krasnow, 2000).
24 McMurran, Duggan
CBMH 15.1 2nd 4/8/05 12:28 PM Page 24
Conclusion
The process of constructing these manuals has itself contributed to theevolution of the PDU treatment programme. First, the documentation oftreatment creates the need for clinicians to specify their treatments and clarifythe rationale behind them, thus advancing their thinking. Second, externalassistance in compiling the manuals contributes a refereeing and reviewingaspect. Third, the availability of the manuals allows for peer reviewing amongmembers of the clinical team, creating the opportunity for reflexive devel-opment of all aspects of the treatment programme so that they fit better witheach other. There is, therefore, a valuable iterative process in the constructionof manuals.
Structured manuals are important when less highly trained and less experi-enced personnel are involved in therapy, and in this case the manuals allowedfor the training of selected healthcare assistants in the delivery of therapy. Thisgroup of workers arguably spend most time with inpatients yet often they are nottrained in the therapies used in a ward or unit. Having more staff trained in thetherapy components means fewer logistical problems in providing therapyconsistently, and also enhances the integrity of approach overall.
Another advantage was that formally specifying treatment componentsemphasized the opportunity of evaluating each part of the treatment programmeseparately, checking to see whether clinical targets have been met. This incre-mental and intermediate approach to the evaluation of treatment is particularlyimportant for units like the PDU where the treatment is lengthy (average 18months) and the final outcomes are available only after a considerable follow-upperiod. Also, if patients in general are not responding to a particular componentof treatment, it may be revisited and the manual revised as necessary.
The value of manuals in promoting the development of treatments hasbeen recognized by Carroll and Nuro (2002). They suggest evolutionary stagesin the role of manuals in clinical trials. The first stage is defining thetreatment for preliminary evaluation; the second is training therapists andreducing differences between therapists in clinical trials; and the third isrolling out the treatment in clinical practice. The PDU manuals have passedthe first stage in this scheme, in that the treatment has been specified andpilot evaluations of specific components have been enabled (e.g. McMurran,Charlesworth, et al., 2001; McMurran, Fyffe, et al., 2001). To fulfil stage twocriteria, further attention needs to be paid to developing staff training andmethods of monitoring adherence to the programme. At this stage, theefficacy of the manualized treatment should be examined, preferably in arandomized control trial. According to Carroll and Nuro (2002) stage threerequires inclusion of information, based on clinical trials, on how to apply theprogramme with different clients and in a variety of settings. This permits
Manualization of a treatment programme for PD 25
CBMH 15.1 2nd 4/8/05 12:28 PM Page 25
testing of the effectiveness of the treatment in clinical practice, as opposed toits efficacy in clinical trials.
Acknowledgements
Support was provided through funding from the NHS National Programme onForensic Mental Health R&D (McMurran). Nottinghamshire Healthcare NHSTrust provided the funding for the production of the manuals. However, theviews expressed in this publication are those of the authors and not necessarilythose of the Programme, the Department of Health, or the Trust.
References
Addis ME, Krasnow AD (2000) A national survey of practising psychologists’ attitudes towardpsychotherapy treatment manuals. Journal of Consulting and Clinical Psychology 68: 331–339.
Beutler LE (2000) David and Goliath: when empirical and clinical standards of practice meet.American Psychologist 55: 997–1007.
Carroll KM, Nuro KF (2002) One size cannot fit all: a stage model for psychotherapy manualdevelopment. Clinical Psychology: Science and Practice 9: 396–406.
Castonguay LG, Schut AJ, Constantino MJ, Halperin GS (1999) Assessing the role of treatmentmanuals: have they become necessary but nonsufficient ingredients of change? ClinicalPsychology: Science and Practice 6: 449–455.
Crits-Cristoph P, Carroll K, Perry K, Luborsky L, McLellan AT, Woody GE, Thompson L,Gallagher D, Zitrin C (1991) Meta-analysis of therapist effects in psychotherapy outcomestudies. Psychotherapy Research 1: 81–91.
D’Silva K, Duggan C (2002) The development of a psycho-educational programme for personalitydisordered patients. Psychiatric Bulletin 26: 268–271.
D’Zurilla TJ, Goldfried MR (1971) Problem solving and behaviour modification. Journal ofAbnormal Psychology 78: 107–126.
D’Zurilla TJ, Nezu AM, Maydeu-Olivares A (2002) Manual for the Social Problem Solving Inventory- Revised. North Tonawanda, NY: Multi-Health Systems, Inc.
Henin A, Otto MW, Reilly-Harrington NA (2001) Introducing flexibility in manualized treat-ments: application of recommended strategies to the cognitive-behavioral treatment ofbipolar disorder. Cognitive and Behavioral Practice 8: 317–328.
Henry WP, Schacht TE, Strupp HH, Butler SF, Binder JL (1993a) Effects of training in time-limited dynamic psychotherapy: mediators of therapists’ responses to training. Journal ofConsulting and Clinical Psychology 61: 441–447.
Henry WP, Strupp HH, Butler SF, Schacht TE, Binder JL (1993b) Effect of training in time-limited dynamic psychotherapy: changes in therapist behaviour. Journal of Consulting andClinical Psychology 61: 434–440
Hollin CR (1995) The meaning and implications of ‘programme integrity’. In McGuire J, ed.What Works: Reducing Reoffending. Chichester: Wiley, pp. 195–208.
Mahoney MJ, Thoresen CE (1974) Self-control: Power to the Person. Monterey, CA: Brookes/Cole.McGuire J (2001) What works in correctional intervention? Evidence and practical implications.
In Bernfeld GA, Farrington DP, Leschied AW, eds. Offender Rehabilitation in Practice.Chichester: Wiley, pp. 25–43.
McMurran M, Charlesworth P, Duggan C, McCarthy L (2001) Controlling angry aggression: Apilot group intervention with personality disordered offenders. Behavioural and CognitivePsychotherapy 29, 473–483.
26 McMurran, Duggan
CBMH 15.1 2nd 4/8/05 12:28 PM Page 26
McMurran M, Egan V, Richardson C, Ahmadi S (1999) Social problem-solving in mentallydisordered offenders: a brief report. Criminal Behaviour and Mental Health 9: 315–322.
McMurran M, Fyffe S, McCarthy L, Duggan C, Latham A (2001) ‘Stop Think!’: social problem-solving therapy with personality disordered offenders. Criminal Behaviour and Mental Health11: 273–285.
National Institute for Mental Health in England (2003a) Personality Disorder: No Longer aDiagnosis of Exclusion. London: NHS.
National Institute for Mental Health in England (2003b) The Personality Disorder CapabilitiesFramework. London: NHS.
Robins S, Novaco RW (1999) Systems conceptualization and treatment of anger. Journal ofClinical Psychology – In Session: Psychotherapy in Practice 55: 325–337.
Scaturo DJ (2001) The evolution of psychotherapy and the concept of manualizaton: anintegrative perspective. Professional Psychology: Research and Practice 32: 522–530.
Vacoch D, Strupp HH (2000) The evolution of psychotherapy training: reflections on manual-based learning and future alternatives. Journal of Clinical Psychology 56: 309–318.
Walters GD (1995) The Psychological Inventory of Criminal Thinking Styles, Part I: Reliabilityand preliminary validity. Criminal Justice and Behavior 22: 307–325.
Wilson GT (1996) Manual-based treatments: the clinical application of research findings.Behaviour Research and Therapy 34: 295–314.
Wilson GT (1998) Manual-based treatment and clinical practice. Clinical Psychology: Science andPractice 5: 363–375.
Address correspondence to: Mary McMurran, School of Psychology, CardiffUniversity, Park Place, Cardiff CF10 3AT, UK. Email: [email protected]
Manualization of a treatment programme for PD 27
CBMH 15.1 2nd 4/8/05 12:28 PM Page 27