Susceptibility of Plasmato Ferrous Iron/Hydrogen Peroxide-Mediated Oxidation: Demonstrationof a...
-
Upload
independent -
Category
Documents
-
view
3 -
download
0
Transcript of Susceptibility of Plasmato Ferrous Iron/Hydrogen Peroxide-Mediated Oxidation: Demonstrationof a...
CLIN. CHEM. 41/2, 220-225 (1995) #{149}Lipids and Lipoproteins
flO CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995
Susceptibility of Plasma to Ferrous Iron/Hydrogen Peroxide-Mediated Oxidation:Demonstration of a Possible Fenton ReactionAhmad Agil,’ Cindy J. Fuller, and Ishwarlal Jialal2
The aim of our study was to evaluate a model system byusing iron in the peroxidation of plasma. Lipid peroxida-tion was monitored by fluorometric measurement of lipidperoxides (LPO). Plasma coincubated with Fe2 andH202 had a 268% increase in plasma LPO after 1 h. Theoptimum concentrations were 0.42 mmol/L Fe2 and0.73 moVL H202. Coincubation of plasma with theseconcentrations of Fe2 and H202 separately resulted inno increase in plasma LPO. The increase in plasma LPOafter oxidation with Fe2/H2O2 was paralleled by a de-crease in plasma polyunsaturated fatty acids, an increasein the relative electrophoretic mobility of low-densitylipoprotein (LDL), and decreases in apolipoprotein (apo)B-i 00 and apo A-I immunoreactivity. In vitro oxidation ofLDL and high-density lipoprotein separately with thissystem produced increases of LPO of 246% and 128%,respectively. LPO formation in plasma was inhibited bycatalase, desfemoxamine, and mannitol, but not by su-peroxide dismutase. Hydroxyl radical generation withFe2/H2O2 was evidenced by fragmentation of deoxyri-bose. We conclude that the Fe2/H2O2 system, possiblyby a Fenton reaction mechanism, resulted in significantplasma oxidation. This model system may be useful forexamining lipid peroxidation in clinical investigations.
Indexing Terms: lipid peroxidation/hydroxyl radicals/atherosclero-sis/antioxidants
Lipid peroxidation appears to play a key role in
various degenerative diseases (1). Patients with car-diovascular disease have increased plasma lipid perox-ides (LPO) (2 )3 In addition, oxidation-specific epitopeson proteins have been found in carefully extractedmaterial from atherosclerotic plaques (3, 4).
Previous studies have reported that oxidation of
low-density lipoprotein (LDL) promotes the develop-ment of fatty streaks by increasing the uptake ofoxidized LDL by the macrophage scavenger receptor,which may be a key early step in the development ofatherosclerosis (5, 6). These studies specifically looked
Laboratory of Molecular Pathology & Center for Human Nutri-tion, Departments of Pathology and Internal Medicine, Univer-sity of Texas Southwestern Medical Center at Dallas.
1 Visiting scientist from Department of Pharmacology, Univer-sity of Granada (Spain).
Address correspondence to this author at: University of TexasSouthwestern Medical Center, 5323 Harry Hines Blvd., Dallas,TX 75235-9052. Fax 214-590-2785.
3Nonstandard abbreviations: LPO, lipid peroxides; PUFA,polyunsaturated fatty acids; LDL, low-density lipoprotein; HDL,high-density lipoprotein; apo, apolipoprotein; SOD, superoxidedismutase; DFO, desferrioxamine; TBA, thiobarbituric acid; andREM, relative electrophoretic mobility.
Received April 26, 1994; accepted October 19, 1994.
at isolated LDL oxidation and failed to evaluate theprooxidant and antioxidant factors present in wholeplasma, the balance of which could be crucial in deter-mining the susceptibility to lipid peroxidation. Plasmaoxidation may be more biologically relevant than LDLoxidation since water-soluble antioxidants such as
ascorbate, uric acid, and other plasma constituentswould also be taken into account (7, 8). These antioxi-
dants would presumably be lost during the isolation of
LDL from plasma.Iron may be an important modulator of lipid peroxi-
dation. Although virtually all of the circulating iron is
bound to proteins such as transferrin and ferritin
under normal conditions, iron release from stores canoccur from injured cells in conditions such as inflam-
mation, and may stimulate peroxidation (9, 10). In-creased iron concentrations in plasma have been asso-ciated with increased lipid peroxidation, decreasedascorbate concentrations, and reduced superoxide dis-mutase (SOD; EC 1.15.1.1) activity in aortic occlusiveand aneurysmal diseases (11).
Iron may also be an important promoter of athero-
sclerosis (12). Salonen et al. (13) reported that excessstored iron (measured as serum ferritin concentration)
and high dietary iron intake are associated with anincreased risk of acute myocardial infarction in middle-aged men. Also, Smith et al. (14) demonstrated thatmaterial isolated from atherosclerotic lesions con-
tained catalytic iron detectable by the bleomycin assay
and stimulated the peroxidation of rat liver micro-somes. The presence of iron in atherosclerotic plaqueshas also been documented previously (11). The resultsof these studies indicate that further investigation isneeded into the role of iron in atherogenesis (12, 13).
Lipid peroxidation in vitro occurs with irradiation(either ultraviolet or ionizing), in the presence of tran-sition metals such as iron or coincubation with afree-radical initiator. Iron may stimulate peroxidationby hydroxyl radical (HO) formation (10) and may
promote decomposition of hydroperoxides (9, 10). Fe2and H202 can generate H0 by means of the Fentonreaction:
H202 + Fe2 -Fe3 + OW+HO’
Fenton (15, 16) described the powerful oxidizingproperties of the mixture of hydrogen peroxide andferrous salts. Haber and Weiss subsequently estab-
lished the oxidizing species as H0 (17). The hydroxylradical formed by the Fenton reaction can abstract ahydrogen atom from the methylene group of a noncon-jugated polyunsaturated fatty acid (PUFA) to yield acarbon-centered radical (RC). The PUFA undergoes
CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995 1
molecular rearrangement to a conjugated double-bond
system to partially stabilize RC. The RC can thenreact with 02 to form a peroxy radical (R00), whichcan attack an adjacent PUFA to form hydroperoxides(LOOH) (9, 18) and a new RC. In addition to initiatinglipid peroxidation in plasma, ferrous ions may alsomediate decomposition of LOOH to peroxyl and alkoxylradicals, aldehydes, and other reactive products (18,19). Since data suggest a relation between increasingiron status and atherosclerosis (12, 13), and Fe2appears to be involved in the Fenton reaction resultingin the production of the highly reactive hydroxyl radi-cals, we sought to investigate the susceptibility ofwhole plasma to iron-catalyzed lipid peroxidation byusing a Fe2fH202 model system. Iron was chosen asthe transition metal instead of copper since moreinformation supports the role of iron in atherogenesisand the Fenton reaction.
Materials and Methods
Reagents
1,1’,3,3 ‘-Tetramethoxypropane was obtained fromKodak (Rochester, NY), and 1-butanol from FisherScientific (Fair Lawn, NJ). All other reagents wereobtained from Sigma Chemical Co. (St. Louis, MO).
Plasma
Blood samples from healthy normolipidemic volun-teers between ages 20 and 50 years were collected afteran overnight fast into EDTA (1.5 g/L)-containing tubes.Plasma was separated by centrifugation at 4#{176}Cat2000g for 20 mm.
Plasma Oxidation Systems
Lipid peroxidation was initiated by incubatingplasma (500 L) with 50 L of various concentrationsof ferrous sulfate (0.21-1.67 mmoIIL), with or without50 p.L of various concentrations of H202 (0.18-0.73mol/L). The samples were incubated for 1 h at 37#{176}C.The length of incubation corresponded to the steadystate of maximum plasma oxidation, as determined inpreliminary time-course experiments (data not shown).In some experiments, oxidation was performed in thepresence or absence of catalase (EC 1.11.1.6; 50 and100 mgfL) to determine the importance of H202; SOD(50 and 100 mg/L), to determine whether 02. is in-volved in plasma oxidation; desferrioxamine (DFO, 1and 2 mmoIJL), to investigate the importance of iron inoxidation; and mannitol (100 and 200 mmol/L), todetermine the role of H0. All of the inhibitors wereadded before the addition of Fe2 and H202 to test forinhibition of oxidation. All experimental points wereperformed in triplicate. Oxidation was stopped by ad-dition of 40 prnol/L butylated hydroxytoluene and re-frigeration.
Lipoprotein Preparation
Plasma for LDL and high-density lipoprotein (HDL)were collected from healthy fasting human volunteers
into tubes containing EDTA (1 g/L). LDL (d = 1.019-1.063 kgfL) and HDL (d = 1.063-1.21 kgfL) wereisolated by sequential ultracentrifugation, as previ-ously described (20). The isolated LDL and HDL weredialyzed against 150 mmol/L NaC1 and 1 mmol/L
EDTA (pH 7.4), filtered through a 0.45-sm filter, andstored at 4#{176}Cunder N2. Protein was measured by themethod of Lowry et al. (21), with bovine serum albu-min as calibrator.
Oxidation of Lipoproteins
LDL and HDL were dialyzed against 1 L of phos-phate-buffered saline (0.01 mol/L phosphate, 0.15mol/L NaC1, pH 7.4) at 4#{176}Cin the dark. LDL and HDL(200 mg/L protein) were then incubated with 0.42mmol/L Fe2 and 0.73 mol/L H2O2 in the buffer in atotal volume of 1 mL for 1 h at 37#{176}C.Oxidation wasstopped with butylated hydroxytoluene and refrigera-tion as in plasma experiments.
Analysis of Oxidation
Plasma LPO formed after Fe2/H2O2 oxidation wasassayed by a modification of the thiobarbituric acid(TBA)-reactive substances method of Yagi (22). Briefly,three modifications were made to improve the specific-
ity of the plasma LPO measurement. First, water-soluble substances, which also react with TBA to yieldthe same product as LPO, were removed by including a
phosphotungstic acid (0.1 gfL)-sulfl.iric acid (35mmol/L) step to precipitate lipids with the proteins.The supernate was discarded. Second, interferencefrom bilirubin was prevented by reading the fluores-cence at 553 nm rather than at 532 nm. Finally, sialicacid interference was eliminated by adding acetic acidin the TBA reagent to adjust the reaction mixture pHto 3.0. The fluorescence was read at 553 nm with 515nm excitation with a Perkin-Elmer (Norwalk, CT)LM-5 spectrofluorometer. The amount of LPO wasexpressed in terms of malondialdehyde equivalents(moI/L of plasma), as calibrated with freshly diluted1,1’,3,3’-tetramethoxypropane. The intra- and interas-say CVs of this assay were 4.2% and 4.0%, respectively,and the results correlated highly with LPO analysis by
HPLC (23). LPO concentrations of LDL and HDL weremeasured as described above for plasma, except thatpretreatment with phosphotungstic acid/sulfuric acidwas eliminated and the TBA reaction was carried outdirectly on 50 L of sample mixed with 0.1 gIL phos-photungstic acid and 3.5 mL of water (24).
The fatty acid composition before and after plasmaoxidation was analyzed by the direct transesterifica-tion method of Lepage and Roy (25). Plasma (100 FL),pre- and postoxidation, was extracted with methanol:benzene (4:1 by vol) and transesterified with 200 L ofacetyl chloride for 1 h at 100#{176}C.The sample was thenneutralized with 5 mL of K2CO3, and 2 1.iL of thebenzene phase was injected into the GC.100A(Hewlett-Packard, Avondale, PA) 5880A gas chromato-graph with a 30 m X 0.75 mm (i.d.) SP-2330 capillarycolumn (0.2-nm film thickness; Supelco, Bellefont, PA)
1.67Plasma 2
+ H202, mol/L
0.18
2.57 ± 0.224.40 ± 0d
8.00 ± 052d
2.28 ± 0.18
0.42
0.84
1.67
222 CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995
for fatty acid analysis. The chromatographic conditionswere: injector temperature, 225#{176}C;detector tempera-ture, 230#{176}C.The column temperature program was asfollows: initial oven temperature 150#{176}Cfor 5 mm,increasing by 8#{176}C/mmto a final temperature of 220#{176}C,held for 15 mm. The carrier gas was nitrogen, at a flowrate of 30 mL/min. The fatty acid calibrator was ob-tained from Nuchek Prep (Elysian, MN). The fatty acid
was expressed as a percentage: fatty acid area/totalfatty acid area (unsaturated and saturated). Seven
fatty acids were incorporated in the total fatty acids:14:0, 16:0, 18:0, 18:1, 18:2, 18:3, and 20:4.
Plasma lipoprotein electrophoresis was performed atpH 8.6 in 0.05 mol/L barbital buffer on 0.05% agarosegels as described previously (26). Relative electro-phoretic mobility (REM) was measured by comparingthe mobility of LDL in oxidized plasma with that forLDL from untreated plasma. Similar experiments wereconducted with LDL and HDL in vitro.
Apolipoprotein (apo) A-I and apo B immunoreactivity
before and after plasma oxidation were measured byiminunonephelometry (Behring Diagnostics, Somer-ville, NJ).
Hydroxyl Radical Generation (Fenton Reaction)
The presence of H0 radicals in the Fe2t’H202 sys-tem was assessed by the degradation of deoxyribose asdescribed by Gutteridge (27). Reaction tubes contained0.73 molJL H2O2 and 0.8 mmol/L deoxyribose in 10
mmol/L phosphate buffer, pH 7.4. The final volume was1.0 mL. The reaction was initiated by adding 0.42mmol of FeSO4, and the mixture was incubated for 10mm at 37#{176}C.The reaction was carried out in triplicate.Solutions of iron and deoxyribose were made up just
before use. Deoxyribose degradation by generated hy-droxyl radical in the presence or absence of mannitol(100 mmolJL) was measured by the TBA-reactive sub-
stances assay (28). The samples were heated for 10 mmat 100#{176}C,cooled in ice, and mixed with catalase (15 gIL)to prevent the effect of H2O2 in the TBA reaction (29).The absorbance was read in a spectrophotometer at532 nm against a blank (deoxyribose in phosphate
buffer).
Statistics
Data are expressed as mean ± SEM of at least threeseparate experiments. Student’s t-tests were used todetermine differences. The Bonferroni method wasused to correct for multiple comparisons.
Results
Table 1 shows the dose effects of Fe2 on LPO
formation after 1 h of incubation. The basal concentra-tion of LPOs was 2.08 ± 0.06 mo1/L. Fe2 produced noincrease in the formation of LPOs in concentrations
ranging from 0.21 to 1.67 mmoltL. Also, incubation ofplasma with H202 alone at concentrations rangingfrom 0.18 to 0.73 mol/L showed no significant differ-ences in LPOs. Table 2 shows that Fe2 (0.42 mmol/L)coincubation with different concentrations of H202
Table 1. Effect of Fe2 or H202 on plasma oxidation.Incubation conditlonV LPO, gAmoUL”
Plasma 1 2.08 ± 0.06
+ Fe504, mmoVL
0.210.420.83
2.11 ± 0.072.12 ± 0.02
2.16 ± 0.082.60 ± 0.202.75 ± 0.24
2.88 ± 0.340.37 2.67 ± 0.150.73 2.76 ± 0.28
500 L of plasma was incubated at 37’C for I h in the presence orabsence of 50 p1 of FeSO4 or H202 at venous concentrations.
#{176}Mean ± SEM of three separate experiments.
Table 2. Effect of coincubation with both Fe2’ andH202 on plasma LPO.
incubation condltlonV LPO, pmol/IP
FeSO4 (0.42 mmoVL) + plasma A 2.22 ± 0.18
+ H202, moVL
0.180.370.73
H202 (0.73 moVL) + plasma B+ Fe2, mmoVL
0.21 4.44 ± 0.21
8.38 ± O.26c79.56 ± 137d
162.92 ± 3.02c
Plasma (500 p1) was incubated at 37CC for 1 h in the presence of 50 p1of various concentrations of FeSO4 and H202.
Mean ± SEM of three separate experiments.
Thresholdsfor statistical significance, using the Bonferroni correction: P =
0.0167; P = 0.0125 (‘P <0.005, ‘p <0.001).
promoted increased formation of LPOs in plasma,which were significantly different from baseline only atH202 concentrations of 0.37 and 0.73 mol/L (P <0.001).Table 2 also shows that H202 (0.73 mol/L) coincubatedwith different concentrations of Fe2 significantly in-
creased lipid peroxidation at concentrations �0.42mmoIJL.
We also investigated the effect of copper on theoxidizability of plasma in this model system (data notshown). Copper (0.42 mmol/L) plus H202 failed tosignificantly oxidize plasma, possibly because of chela-
tion by the EDTA in the plasma. With heparinizedplasma, copper significantly increased plasma oxidiz-
ability over baseline (2.8 ± 0.6 vs 9.2 ± 2.2 mo1fL,respectively, P <0.001). However, the oxidizability of
heparinized plasma by copper (0.42 mmol/L)-H202 wassimilar to that of EDTA plasma by iron-H2O2 (9.2 ±
2.2 vs 9.5 ± 1.8 respectively, P = 0.90) in five subjects.The oxidation of plasma by the Fe2/H2O2 system
was tested in the presence of several inhibitors. Table3 shows that catalase (50 and 100 mgfL) inhibited lipid
peroxidatiom by 52.1% and 71.0%, respectively (both P<0.001). Heat-denaturation of catalase (100#{176}Cfor 10
A
52.1”
B
0 5 10 15 20
CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995 223
Table 3. Effect of inhibitors on Fe2t/H202 LPOformation in plasma.
inhibitor added LPO, % inhibltlofl”
Catalase, mg/L50
100 710d
SOD, mg/L50 00.0
100 00.0DFO, mmoVL
1 45.2#{176}
2 56.0”Mannitol, mmoVL
100 41.6”200 51.5”
Plasma (500 p1) was incubated at 37#{176}Cfor 1 h alone and with 0.42mmoL/L Fe2 and 0.73 moVL H202 in the presence and absence of inhibitors.
b Mean ± SEM of three separate experiments.C Significant at P <0.01. d P <0.005.
mm) abolished its inhibitory effect. SOD (50 and 100mgfL), in contrast, had no inhibitory effect. In addition,LPO formation was inhibited 45.2% (P <0.005) and56.0% (P <0.001) by DFO (1 and 2 mmol/L, respective-ly). Catalase and DFO combined (100 mg/L and 2mmol/L, respectively) totally inhibited lipid peroxida-tion (data not shown). Mannitol (100 and 200 mmol/L)also inhibited LPO formation by 41.6% and 51.5% (bothP <0.001), respectively.
The addition of Fe2 at 0.42 mmol/L and H202 at0.73 mol/L to deoxyribose solutions in phosphate bufferat pH 7.4 caused a rapid degradation of the sugar(absorbance of TBA-reactive substances relative tocontrol 0.17 ± 0.02, mean ± SE of three experiments).The hydroxyl radical scavenger mannitol (100 mmol/L)
inhibited deoxyribose degradation by Fe2/H2O2 by67.9% (0.05 ± 0.01, relative to control).
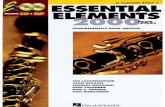
Figure 1 depicts the fatty acids in plasma before andafter oxidation with the Fe2iH2O2 system. The per-centages of unsaturated fatty acids (18:1, 18:2, 18:3,and 20:4) originally present in the plasma were 24.3%± 2.4%, 36.5% ± 1.7%, 0.6% ± 0.1%, and 10.9% ± 2.8%(mean ± SE of three experiments), respectively; thesewere undetectable after oxidation.
The REM of LDL during plasma oxidation with Fe2and H202, separately and combined, was measured.Neither Fe2 (0.42 mmol/L) alone nor H2O2 (0.73mol/’L) alone affected the REM; however, coincubationresulted in an increase in the REM (2.59 ± 0.23, mean± SE of three experiments).
Plasma concentrations of apo B-100 and apo A-I weremeasured by immunonephelometry before and afteroxidation by the Fe2/H2O2 system. Apo A-I decreased30.3% after oxidation, from 1263 ± 26 to 881 ± 5.0mg/L. Similarly, apo B-100 decreased 19.8% after oxi-dation (1030 ± 6.0 vs 826 ± 14 mg/L).
Also, the effect of this model system on the oxidiz-ability of isolated LDL and HDL was tested. The meanpercent increase in LDL LPO was 246.1% (n = 5); inHDL, 128.2% (n = 5, done in triplicate). Coincubation
Time,Minutes
Fig. 1. Gas-liquid chromato9raphic analysis of fatty acids fromwhole human plasma before (A) and after oxidation (B) withFe2/H2O2.
of LDL with the Fe2fH2O2 system (0.42 mmol/L and0.73 mol/L) resulted in an increase of REM (1.51 ±
0.05, mean ± SE of three experiments); however, theREM of HDL was not changed by coincubation.
Discussion
In this study the susceptibility of plasma to iron-mediated oxidation was tested by using a Fe2fH2O2model system. Although this modified Yagi assay is notthe ideal assay to monitor lipid peroxidation as com-pared with more sophisticated methodologies such asmeasurement of oxysterols (e.g., 7-ketocholesterol) andother aldehydes (e.g., 4-hydroxynonenal), it is rapidand simple. Also, its results correlate strongly (r =
0.85) with HPLC analysis of LPO (23). The Fe2fH2O2system produced extensive lipid peroxidation ofplasma, whereas Fe2 and H2O2 separately did not.This supports the role of H0 production, as evidencedby the inhibition of plasma LPO formation by the H0scavenger mannitol. The production of H0 by theFe2 /H2O2 system was confirmed by deoxyribose frag-mentation and by the inhibition of deoxyribose degra-dation by mannitol. Our results are in agreement withMinotti and Aust (30), who reported that matmitol
224 CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995
inhibited the oxidation of liposomes by FeCl2 (0.2mmol/L) and H202 (0.1 mmoIJL) as measured by thedisappearance of 1,10-phenanthroline-chelatable Fe2and the inhibition of malondialdehyde production. Theinhibition of LPO production by Fe2/H2O2 in thepresence of other inhibitors was also shown. The ironchelator DFO partially inhibited lipid peroxidation bypreventing the interaction of Fe2 and H2O2 to produceHo’ radicals. Lipid peroxidatiom was also prevented bycatalase, which removes H2O2, thus preventing Ho’formation. The inability of SOD to inhibit lipid peroxi-dation supports the lack of 02 generation in thissystem (28). Arshad et al. (31) demonstrated that thecombination of cupric acetate and H2O2 inducedplasma lipid peroxidation; however, they did not elab-orate on the mechanism by which the peroxidation wasmediated nor did they confirm lipoprotein oxidation.When we compared plasma oxidizability involving cop-per and iron, we found that they resulted in a similarextent of lipid peroxidation.
An earlier experiment showed that xanthine andxanthine oxidase (0.33 mmoIIL and 40 U/LI, respective-ly), in combination with the Fe3:adenosine diphos-phate chelate (0.2 mmol/L:2 mmol/L, respectively), didnot increase plasma LPO (32). In addition, the Fe2/H2O2 system was compared with the water-solubleradical initiator 2,2’-azobis-2-amidinopropane hydro-chloride (50 mmol/L). The oxidation of plasma withFe2 VH2O2 system resulted in greater generation of
LPO: 8.7 ± 0.1 vs 4.41 ± 0.1 moIJL, respectively (n =
5 experiments). Thus the Fe2/H2O2 system appears to
result in greater lipid peroxidation.
Several lines of evidence in the present report sug-gest that this model system accounts for lipoproteinoxidation. The accumulation of LPO was paralleled bydisappearance of the unsaturated fatty acids 18:1, 18:2,18:3, and 20:4 from plasma after oxidation, supportingthe notion that lipid peroxidation occurred. Followingplasma oxidation, PUFAs were virtually absent fromthe gas chromatograph. Interestingly, oleic acid was
also reduced after treatment with Fe2/H2O2. Onepossible explanation for this may be secondary oxida-tion of oleic acid by products of oxidation after PUFAoxidation. Agarose gel electrophoresis of plasma after
oxidation with Fe2fH2O2 showed an increase in theREM of LDL-additional proof that lipid peroxidation(including LDL oxidation) occurred. When LDL is oxi-dized, aldehydes from the breakdown of LPO derivatizethe lysmne residues of apo B and increase its negativecharge (33). The reduction in apo A-I and apo Bimmunoreactivity is further evidence that the Fe2/H202 system resulted in oxidation of lipoproteins.
The addition of Fe2 and H2O2 at 0.42 mmol/L and0.73 mol/L, respectively, to LDL and HDL in vitroshowed an increase in the LPO. The in vitro oxidationof LDL (LPO) was twice that of HDL, which could beexplained by the higher percentage of lipid in LDL thanin HDL. We have shown higher concentrations of LPOin plasma than in HDL and LDL, possibly due to the
greater concentrations of lipoproteins in plasma thanin the studies with isolated LDL and HDL.
Plasma lipid peroxidation may provide a more com-plete picture of the situation in vivo than the oxidationof isolated LDL in vitro. LDL circulates through thebody in a medium containing numerous aqueous anti-oxidants. Isolation of LDL removes the aqueous-phaseantioxidants, leaving behind the lipophilic antioxi-dants such as a-tocopherol. Plasma lipid peroxidationwith Fe2/H2O2 would be useful in clinical trials withantioxidants used to decrease lipoprotein oxidation,especially in trials using water-soluble antioxidants. Itwould also provide a faster, less labor-intensive meansto study lipoprotein oxidation than LDL isolation fromplasma, especially if the system can be modified todetermine oxidation kinetics.
This plasma lipid peroxidation method, being rapidand simple, could prove useful in clinical investigationsand studies with antioxidant supplementation. Fur-
thermore it can be easily adapted to a clinical chemis-
try laboratory. Hence, plasma lipid peroxidation wouldgive a more complete picture of both antioxidant re-serve and oxidative stress than does the peroxidation ofisolated lipoproteins (e.g., LDL). Although increasedplasma LPOs have been reported in diabetics, theinterpretation of these findings is confounded by thepresence of vascular disease in most studies (34).Studies are now underway in this laboratory examin-
ing the oxidizability of both LDL and HDL and plasmain diabetics free of vascular disease. The data fromthese studies could further validate this assay ofplasma oxidizability.
We thank Anh Nguyen for technical assistance with the gaschromatography and Beverely Adams Huet for statistical exper-tise.
References1. Halliwell B, Gutteridge JMC. Free radicals, ageing, and dis-ease. In: Halliwell B, Gutteridge JMC, eds. Free radicals inbiology and medicine. New York: Oxford University Press, 1993:416-93.2. Yagi K. Lipid peroxidation and human diseases. Chem PhysLipids 1979;45:337-51.3. Yla-Herttuala S, Palinski W, Rosenfeld ME, Parthasarathy 8,Carew TE, ButlerS, et al. Evidence for the presence of oxidativelymodified low density lipoprotein in atherosclerotic lesions ofrabbit and man. J Clin Invest 1989;84:1086-95.4. Palinski W, Rosenfeld ME, Yla-Herttuala S, Gurtner GC,Socher SS, Butler S, et al. Low density lipoprotein undergoesoxidative modification in vivo. Proc NatI Acad Sci USA 1989;86:1372-6.5. Jurgens G, Hoff HE, Chisoim GM, Esterbauer H. Modificationof human low density lipoproteins by oxidation. Characterizationand pathophysiological implications. Chem Phys Lipids 1987;45:315-36.6. Heinecke JW, Rosen H, Chait A. Iron and copper promotemodification of low density lipoprotein by human arterial smoothmuscle cells in culture. J Clin Invest 1984;74:1890-4.7. Frei B, Stocker R, Ames BN. Antioxidant defenses and lipidperoxidation in human blood plasma. Proc Natl Acad Sci USA1988;84:9748-52.8. Esterbauer H, Striegi G, Puhi H, Rotheneder M. Continuousmonitoring of in vitro oxidation of human low density lipoprotein.Free Radic Res Commun 1989;6:67-75.9. Gutteridge JMC, Halliwell B. The measurement and mecha-
CLINICAL CHEMISTRY, Vol. 41, No. 2, 1995 225
nism of lipid peroxidation in biological systems. Trends BiochemSci 1990;15:129-35.10. Halliwell B, Gutteridge JMC. Iron and free radical reactions:two aspects of antioxidant protection. Trends Biochem Sci 1986;11:372-S.11. Piotrowski JJ, Hunter GC, Eskelon CD, Dubick MA, Bern-hard VM. Evidence for lipid peroxidation in atherosclerosis. LifeSci 1990;46:715-21.12. Sullivan JL. The iron paradigm of ischemic heart disease. AmHeart J 1989;117:1177-88.
13. Salonen JT, Nyssonen K, Korpela H, Toumilethto J, Sep.panen R, Salonen R. High stored iron levels are associated withexcess risk of myocardial infarction in Eastern Finnish men.Circulation 1992;86:803-11.14. Smith CH, Mitchinson MJ, Aruoma 0, Halliwell B. Stimula-tion of lipid peroxidation and hydroxyl-radical generation by thecontents of human atherosclerotic lesions. Biochem J 1992;286:901-5.15. Fenton HJH. Oxidation of tartaric acid in the presence ofiron. J Chem Soc 1894;65:899.16. Fenton HJH. Oxidation of certain organic acids in the pres-ence of ferrous salts. Proc Chem Soc 1899;15:224.17. Haber F, Weiss J. The catalytic decomposition of hydrogenperoxide by iron salts. Proc R Soc A 1934;147:332.18. Kappus H. Lipid peroxidation: mechanism, analysis, enzy-mology and biological relevance. In: Sies H, ed. Oxidative stress.London: Academic Press, 1985:273-310.19. Halliwell B. Curcent status review: free radicals, reactive oxy-gen species and human disease. A critical evaluation with specialreference to atherosclerosis. Br J Exp Pathol 1989;70:737-57.20. Lindgren FJ, Jensen LC, Hatch Yr. The isolation and quan-titative analysis of serum lipoproteins. In: Nelson GS, ed. Bloodlipids and lipoproteins: quantitation, composition and metabo-lism. New York: Wiley Interscience, 1972:181-274.21. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Proteinmeasurement with Folin phenol agent. J Biol Chem 195 1;193:265-75.22. Yagi K Assay for blood plasma or serum. Methods Enzymol1984;105:328-31.
23. Therasse J, Lemonnier F. Determination of plasma lipoper-oxides by high-performance liquid chromatography. J Chro-matogr 1987;413:237-41.24. Maseki M, Nishigaki I, Hagihara M, Tomoda Y, Yagi K Lipidperoxide levels and content of serum lipoprotein fractions ofpregnant subjects with or without pre-eclampsia. Clin Chim Acta1981;115:155-61.25. Lepage G, Roy CC. Direct transesterification of all classes oflipids in a one-step reaction. J Lipid Res 1986;27:114-20.26. Jialal I, Grundy SM. Preservation of the endogenous antioxi-dants in low density lipoprotein by ascorbate but not probucolduring oxidative modification. J Clin Invest 1991;87:597-601.27. Gutteridge JM. Thiobarbituric acid-reactivity following iron-dependent free-radical damage to amino acids and carbohydrates.FEBS Lett 1981;128:343-6.28. Halliwell B, Gutteridge JMC. Formation of a thiobarbituric-acid-reactive substance from deoxyribose in the presence of ironsalts. The role of superoxide and hydroxyl radical. FEBS Lett1981;128:347-52.29. Montgomery R, Nathan CF, Cohn ZA. Effects of the reagentand cell-generated hydrogen peroxide on the properties of lowdensity lipoprotein. Proc Nati Acad Sci USA 1986;83:6631-5.30. Minotti G, Aust SD. The role of iron in the initiation of lipidperoxidation. Chem Phys Lipids 1987;44:191-208.31. Arshad MAQ, Bhadra S, Cohen RM, Subbiah MTh. Plasmalipoprotein peroxidation potential: a test to evaluate individualsusceptibility to peroxidation. Cliii Chem 1991;6:67-75.32. Jialal I, Agil MA, Fuller CJ. The susceptibility of plasma toiron mediated oxidation: an evaluation of two model systems[Abstract]. Clin Chem 1994;40:1101.33. Brown MS, Basu SP, Falck JR, Ho YR, Goldstein JL. Thescavenger pathway for lipoproteun degradation: specificity of thebinding site that mediates uptake of negatively charged LDL bymacrophages. J Supramol Struct 1980;13:67-81.34. Sato Y, Hatta N, Sakamoto N, Matsuoka 5, Yagi S. Lipid
peroxide levels in plasma of diabetic subjects. Biochem Med1979;21:104-7.