Subpopulations of marrow stromal cells share a variety of osteoblastic markers
-
Upload
independent -
Category
Documents
-
view
3 -
download
0
Transcript of Subpopulations of marrow stromal cells share a variety of osteoblastic markers
Calcif Tissue Int (1991) 49:202-207 Calcified Tissue International �9 1991 Springer-Verlag New York Inc.
Subpopulations of Marrow Stromal Cells Share a Variety of Osteoblastic Markers
Dafna Benayahu, 1 Adina Fried, 1 Dov Zipori , 2 and Sh iomo Wientroub 1'3
1Department of Histology and Cell Biology, Sackler Faculty of Medicine, Tel-Aviv University, Ramat Aviv 69-978, Tel-Aviv; 2Department of Cell Biology, Weizmann Institute of Science, Rehovot; and 3Department of Orthopaedics, Tel-Aviv Medical Center, Tel-Aviv, Israel
Received April 6, 1990, and in revised form July 5, 1990
Summary. A series of stromal cell lines derived from mouse bone marrow, representing subpopulations of putative stro- mal cell types, were examined for the expression of osteo- blastic properties. The effects of dexamethasone and spe- cific inhibitors on alkaline phosphatase activity, cAMP re- sponse to bone- seek ing hormones , and the abi l i ty to mineralize extracellular matrix in vitro as well as collagen typing were used as osteoblastic markers. We found that all stromal cell types examined possess some osteoblastic fea- tures but differ in the degree of expression. The data provide support to the hypothesis of a common stem cell for marrow stromal cells.
Key words: Marrow stromal cells - Osteoblast - Osteoblas- tic markers - Stromal cell lines.
In the stromal compartment of mammalian bone marrow, blood cells develop within a complex of humoral, cellular, and extracellular matrix factors. Stem cells and progenitors are mostly found in discrete sites, tightly packed in an orga- nized tissue. The marrow stromal tissue is a heterogenous collection of cell types. It has been recognized by many investigators that the adherent cell layer emerging from pri- mary marrow cultures is composed of different cell popula- tions. These include fibroblasts, fat cells, reticular cells, en- dothelial cells, macrophages, and bone-forming cells [1-3]. Although it has been suggested that stromal cells may share a common precursor with blood ceils [4], it remains to be demonstrated what pathways they follow in differentiation.
An attractive hypothesis for differentiation in the marrow stromal compartment is a scheme analogous to that in the hemopoietic compartment, where stem cells give rise to committed progenitors for different stromal cell lineages [5]. The main indications for a possible existence of stromal stem cells come from in vivo assays. Single cell suspension of bone marrow cells forms fibrous and osteogenic tissue when incubated within diffusion chambers in vivo [6], indicating that precursor cells determined to the osteogenic direction are present in the marrow stroma. When an intact piece of marrow is transplanted under the renal capsule or subcuta- neously, bony tissue is formed and than populated by he- mopoietic cells [7, 8]. The marrow stromal cells of this
Offprint requests to: S. Wientroub at the Sackler Faculty of Medi- cine.
newly formed organ are derived from the donor and the he- mopoietic tissue is derived from the host [9].
The clonal origin of fibroblastic colonies that form when dispersed marrow cells are cultured in vitro has been dem- onstrated [10, 11]. The potential for differentiation of single fibroblastic clones grown in vitro was studied in open trans- plants grafted under the renal capsule of syngeneic recipients [12] or in diffusion chambers [10]. It was demonstrated that some colony-forming units-fibroblasts (CFU-F) have a high ability for self-renewal and multipotentiality whereas some have more limited potential. The heterogeneity of the colo- nies formed with regard to their alkaline phosphatase expres- sion is consistent with their derivation from a population of stem and progenitor cells at different stages of tissue devel- opment [13].
Based on morphological and functional evidence, it is now well established that fibroblasts, reticular cells, adipo- cytes, endothelial cells, and osteoblasts are members of the stromal cell system. A variety of cell clones from mouse bone marrow stroma (MBA series) has been classified ac- cording to their properties. MBA-1 is a fibroblast cell line, MBA-2 exhibits some properties of endothelial cells, MBA- 13 shares properties with both fibroblasts and endothelial cells, 14F1.1 are cloned preadipocytes, and MBA-15 has os- teoblastic features in vitro and osteogenic potential in vivo [3, 5, 14, 15]. There is neither standard terminology nor a defined set of markers for the different cell types comparable to that described for the osteogenic cells [3].
In this study we examined the extent that various stromal cell types share osteoblastic features. It may point to a pre- sumed single ancestry.
Material and Methods
Marrow Stromal Cell Lines
The following stromal cell lines or their clones derived from mouse bone marrow previously described as having varied phenotypes were included in this study: MBA-I fibroblasts, MBA-2 endothelial- like, MBA-13 fibroendothelial cells, 14Fl.1 cloned preadipocytes, and MBA-15 osteoblastic cells [3, 14, 16].
The stromal cell lines were seeded in tissue culture plates (Nunc) in DMEM containing 4.5 g glucose/liter supplemented with 10% FCS. Cells were passaged once weekly by removal with a rubber policeman and dispersion in fresh medium. All cultures were incu- bated at 37~ in a humidified atmosphere of 10% CO2 in air.
Alkaline Phosphatase Activity
Cytochemical staining of alkaline phosphatase was performed on
D. Benayahu et al.: Marrow Stromal Cells
,.o] #
r
" 2 . 0 - o Q.
? 1.5-
c
-~ i . o -
- t
0 5 -
14 F I.I M B A ' - I M B A - 2
and Osteoblastic Markers
.,...........
iiiiiii
iiiii :::::::::::::
iiiii ,i,!i!i!i!ii iiiiiiiiiiiii ............,
M B A - 1 3 M B A-15
Fig. 1. Alkaline phosphatase activity of marrow stromal cell lines. Values are mean -+ SD of duplicate determinations on four separate dishes.
260 -
2 4 0 -
3 22o-
- 200-
--~ 180 -
~ [ 6 0 - 2
~, 140-
~ L20-
I00 14F1.1 MBA-2 MBA'I5 MBA-i5
Fig. 2. Dexamethasone effect on alkaline phosphatase activity of marrow stromal cell lines. Experiments performed as described in Materials and Methods. Values represent the mean of duplicate de- terminations of four separate dishes.
ceils grown to confluence. The cultures were fixed in 10% formalin in methanol for 60 seconds at room temperature, washed briefly in water, and reacted with naphthol AS-MX (Sigma, St. Louis, MO, kit 85L-1).
Biochemical determination of alkaline phosphatase was done on cells seeded at 5 • 104/ml in 35 mm plates incubated for 24 hours. In some experiments cultures were exposed to 100 nM dexamethasone sodium phosphate (Dexacort IKAPHARM, Tel-Aviv, Israel). On day 4, cultures were fed either with medium containing the hormone or hormone-free medium. On day 7, cultures were rinsed twice with phosphate-buffered saline (PBS), removed with a teflon spatula, transferred to 0.25 M sucrose, sonicated on ice for 30 seconds at high speed, and assayed for enzyme activity and protein content. Alkaline phosphatase activity was determined at 37~ as described
203
-6
g
>
<~
o
o
1 :
E
o
100-
8 0 -
o
6 0 -
4 0 -
2 0 - i , i , i i i ,6 3b so ro 90 Levo misole ( ~ m )
,;o
100-
8 0 -
60
4 0
2 0 -
6 2b 4b H o m o a r g i n i n e ( r a M )
6b
8 0
60
40 - O - M B ~ - 1 3
t - I 4 F I.I
2 0 A - M B A - 1 5
0 , �9 1 v , i i , , i , , i , , , IO 3 0 50 7 0 9 0 tK) 130 ~50
Phenyiolonme ( m M )
Fig. 3. Inhibition of alkaline phosphatase activity by specific inhib- itors readily distinguish the various enzyme forms. Each point is the mean +- SD of duplicate determinations of four separate dishes.
by Majeska and Rodan [17]. Protein was measured by the method of Lowry et al. [18], with human serum albumin used as a standard.
Inhibition of alkaline phosphatase activity was tested in the pres- ence of levamisole, L-phenylalanine, or homoarginine (Sigma). The enzyme activity was assayed in a particulate preparation of assay mixture containing different concentrations of inhibitor.
cAMP Determination
Cells were seeded at 5 x 104/ml in 35 mm plates and were grown for 4 days. The medium was then removed and the cultures were pre- incubated with fresh medium containing 0.5% BSA and 5 • 10 4 M isobutylmethylxanthine (IBMX) (Sigma) at 37~ for 15 minutes. The cells were then challenged with fresh medium containing either 100 ng/ml of 1-34 human parathyroid hormone (hPTH) (Sigma) for 5 minutes or 500 ng/ml prostaglandin Ez (PGE2) (Sigma) for 10 min- utes. After incubation, cells were rinsed with PBS, scraped off and suspended in 40 mM Na-acetate containing 4 mM EDTA (pH 4.2), sonicated on ice for 30 seconds, then heated for 2 minutes in boiling water. After centrifugation, the supernatant was removed, lyophi- lized, reconstituted in Tris-buffer, and assayed with the [3HI-cAMP assay kit (KAPH2, Diagnostic Products Corporation, Los Angeles, Ca).
hPTH was dissolved in 1% sodium acetate (pH 4.0) containing 0.1% bovine serum albumin. PGE2 was dissolved in 0.4% ethanol. Aliquots of all hormone stock solutions were frozen and dilutions were prepared fresh in serum-free medium immediately before use.
Mineralization In Vitro
Cells were seeded at 5 • 104/ml in 35 mm plates and grown for 7 days. At confluency, cultures were fed daily with fresh medium
204
4 -
r-]-Corffrol
~ - PTH
Q .
o
I ~ 4 r H MsA-~ MSA-Z MSa-f3 MSA-~5
Fig. 4. Effect of PTH exposure on intracellular cAMP accumulation in marrow stromal cell lines. The values of representative experi- ments are log of the mean -+ SEM of duplicate determination of four separate dishes.
D. Benayahu et al.: Marrow Stromal Cells and Osteohlastic Markers
Q .
a
D - C o n l t o t
~-PGE 2
5-
2-
! i i i i
i::ii:~il
14vu Maa-1 MSA-Z usa-13 USA-f5 Fig. 5. Effect of PGE 2 exposure on intraceUular cAMP accumula- tion in marrow stromal cell lines. The values of representative ex- periments are log of the mean -+ SEM of duplicate determination of four separate dishes.
supplemented with 50 wg/ml ascorbic acid and 10 mM 13-glycero- phosphate (~-GP) [19]. In some cultures, dexamethasone (100 nM) was added as well. Eight days later the culture dishes were fixed with 4% phosphate-buffer formalin with 1 mM CaCI2 for 2 hours at room temperature and then stained with silver gelatin-modified Von Kossa procedure [20].
X-ray Diffraction
Cells were grown on cover slips under the conditions described for mineralization in vitro. On day 8, the cover slips were rinsed with PBS and air dried. The resulting powder was photographed in a Chesley X-ray diffraction microcamera at a 15 mm specimen-to-film distance, with Ni-filtered Copper Ks radiation.
Results
Alkaline Phosphatase
A group of cell lines derived from bone marrow, represent- ing putative subpopulations of stromal cells, were studied. Clones of these cell lines were tested and similar results were obtained.
Histochemical staining for alkaline phosphatase revealed marked differences between the cell lines. Over 80% of the cells in the lines MBA-1, MBA-13, and MBA-15 were posi- tive, whereas only occasional cells showed detectable activ- ity in the MBA-2 cell line and occasional cells demonstrated very strong staining in 14FI. 1.
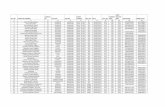
Biochemical quantification of the enzyme-specific activ- ity showed high activity in the fibro-endothelial cell line MBA-13 (Fig. 1), in the range of 4-5 txmol/min/mg protein. All other cell lines, although positive, were in the range of 0.2-0.7 0.mol/min/mg protein (Fig. 1). Dexamethasone sig- nificantly increased alkaline phosphatase activity in all cell lines included in this study (Fig. 2). The osteoblastic cell line (MBA-15) showed a 2.5-fold increase in the enzyme activity when exposed to 100 nM of the steroid. In all other cell lines
the activity rose 30-80% over nontreated control cultures in the presence of dexamethasone (Fig. 2). Both activities, i.e., alkaline phosphatase and its response to dexamethasone stimulation, were retained through more than 20 passages of the cell lines.
Alkaline phosphatase was further characterized using specific inhibitors that readily distinguish the various en- zyme forms. Levamisole, L-homoarginine, and L-phenylal- anine were used at different concentrations (Fig. 3). The enzyme activity in the presence of the inhibitors was assayed in MBA-15, the osteoblastic cell line, 14Fl.I , the cloned preadipocytes, and the fibroendothelial line MBA-13. Alka- line phosphatase was inhibited to the same extent in the different cell lines (Fig. 3) suggesting that the cells contained the same isoenzyme of alkaline phosphatase.
cAMP Response to Bone-Seeking Hormones
Confluent cultures of the various cell lines were exposed to either 1-34 hPTH (Fig. 4) or to PGE 2 (Fig. 5). As expected, the osteoblastic cell line, MBA-15, demonstrated the highest increase (2900 -+ 120 pmol/mg protein), i.e., up to 50-fold over control levels (55 -+ 6 pmol/mg protein) with hPTH and 30-fold with PGE2 (1620 -+ 70 pmol/mg protein). Much lower response, but still significant, was observed when MBA-13 was exposed to the hormones. PGE2 caused up to 5-fold and hPTH only 2-fold increase. The preadipocyte cloned line, 14Fl.1, responded to PGE 2 stimulus by up to 13-fold in- crease in cAMP, but no significant effect was demonstrated with hPTH. The other cell lines were not stimulated by ei- ther of the hormones.
Mineralization In Vitro
Confluent MBA-15 cultures grown in the presence of an or- ganic phosphate source and ascorbic acid showed massive macroscopic Von Kossa-positive solid deposits (Fig. 6).
D. Benayahu et al.: Marrow Stromal Cells and Osteoblastic Markers
Fig. 6. Von Kossa-stained control and dexamethasone-treated con- fluent cultures of marrow stromal cell lines. Cultures were supple- mented with ascorbic acid and 13-glycerophosphate. Note the highly mineralized extracellular matrix in MBA-15 and the spotty deposits in MBA-13. •
MBA-13 and 14F1.1 showed small, mainly microscopic Von Kossa-posit ive nodules. Those in 14Fl . I culture were asso- ciated with the fat laden cells. There was no Von Kossa- positive material in other cell types. Addition of 100 nM dexamethasone to mineralizing cultures caused a significant increase of the surface area and the intensity of the staining only in MBA-15 and MBA-13 (Fig. 6). X-ray diffraction anal- ysis confirmed the stained mineral in MBA-15 and MBA-13 as hydroxyapati te (Fig. 7).
Discussion
All osteoblastic cells, defined either by their origin or their ability to produce mineralized matrix, share a few common properties [21]. The cells are identified by their ability to produce type I collagen in vitro and in vivo [22, 23], in- creased alkaline phosphatase activity [24] and parathyroid hormone-stimulated adenylate cyclase [25]. The fact that isolated cells were capable of making mineralized matrix in vitro and in vivo in diffusion chambers [3] helped to establish those features as characteristic of the osteoblastic pheno- type. Other features, such as osteocalcin and prostaglandin E production and the response to prostaglandin E, are only selectively expressed by certain cell types [21].
Stromal cell lines from the bone marrow were previously described as having heterogeneous morphology [3, 14, 16].
205
MBA-I , MBA-13, and MBA-15 cells had a flattened fibro- b las to id appea rance and MBA-2 were sp ind le - shaped whereas 14F1.1 had a polygonal appearance in young cul- tures followed by adipocyte morphology. All cell lines stud- ied were shown to synthesize extracellular matrix compo- nents in culture [3, 14, 15]. The cell line differed in both the distribution and the quantity of extracellular matrix glyco- proteins. MBA-15 produced only type I collagen; MBA-1 produced primarily type I and to a lesser extent, type III collagen; MBA-2 cells produced collagens type I, IV, and V; MBA-13 cells produced mostly type I collagen with small amounts of types III and IV; 14F1.1 produced types I and IV collagen. From these different combinations of the matrix macromolecules, one can see that type I collagen is present in all marrow stromal cell types involved in this study.
Alkaline phosphatase has long been correlated with os- teoblast differentiation. Activity of this enzyme serves as an early indicator of developing osteogenic tissue. The level of the enzyme expression varied between cell types, but none of the stromal cell lines studied was entirely negative. Dexa- methasone had a profound effect on the enzyme, causing a significant increase in activity of all the lines. Alkaline phos- phatase isoenzymes can be distinguished by sensitivity to inbibitors, heat stability, and electrophoretic mobility [17, 26]. Inhibition studies were done with L-homoarginine, le- vamisole, and L-phenylalanine. These inhibitors provide a clear discrimination between the liver/kidney/bone form and the intestinal form of the enzyme. The results suggest that mouse marrow stromal cell lines included in this study con- tain the liver/kidney/bone isoenzyme.
Osteoblasts cultured in the presence of an organic phos- phate source and ascorbic acid form three-dimensional nod- ules in vitro having morphological and immunohistochemical characteristics of bone [19, 27, 28]. Two stromal cell lines (MBA-15, MBA-13) formed discrete mineralized nodules containing hydroxyapati te. Mineralizing cultures exposed to dexamethasone showed significant increase in the number and intensity of mineralized regions. The mineralization pat- tern and the effects of dexamethasone on both cell lines may suggest that they varied in the number of osteoprogenitor cells present. The steroid affect the ability of these cells to express the osteoblastic phenotype [29]. An attractive alter- nate explanation is that these lines differ in their stage of osteoblastic maturation.
Our studies on the cell line MBA-15 [3] demonstrated the reproducibility of the expression of full osteoblastic pheno- typic activity in defined culture condition as well as their ability to form mineralized osteogenic tissue when implanted in vivo within diffusion chambers. This work can be regarded as a definite proof of osteogenic commitment of a stromal- derived cell population. According to the stem cell hypoth- esis the precursors of the different stromal cell types are believed to be derived from stem ceils within the bone mar- row stroma [30].
This study summarizes extensive characterization of dif- ferent marrow stromal cell lines, previously described as having varied phenotypes [3, 14, 16], for their putative os- teoblastic properties. It provides evidence that may support the hypothesis that there are stem cells present within the marrow stroma giving rise to a variety of mature cell lineages necessary to establish the hemopoietic microenvironment [5]. The assumption is that these pluripotential cells can be considered stromal stem ceils rather than osteogenic stem cells only. It is possible that the marrow stromal cell system is part of a wider stromal cell system of the organism [30]. In each organ, pluripotent and restricted stem cells will gener- ate the cell types of the particular organ concerned. It is well
206 D. Benayahu et al.: Marrow Stromal Cells and Osteoblastic Markers
ous proof is needed. At present, the identification of irre- versible committed progenitors for all various cell types and information on the hierarchy of the different cell lines is not available. These are the goals of future studies.
A critical question raised is whether the functions of stro- mal cells, as observed under culture conditions, are a true representation of events that occur in vivo. One interpreta- tion of the results may be that upon culture, cells tend to lose their tissue-specific functions. Instead, they may express an array of common functions, similar to those expressed by embryo fibroblasts; it is their specific localization in vivo that triggers the correct gene expression. The alternative is that the cell clones that we studied in vitro genuinely reflect the existence of corresponding populations forming the micro- environment in vivo.
Acknowledgments. We gratefully acknowledge the help of Professor W. Traub from The Weizmann Institute of Science, Israel with the X-ray diffraction. This work was supported in part by grants to S.W. from The Basic Research Foundation, The Israel Academy of Sci- ence and Humanities and The Israel Cancer Association, Kesler Foundation. This work is part of the Ph.D. thesis of D.B., carried out at the Department of Histology and Cell Biology, Sackler Fad- ulty of Medicine, Tel-Aviv University.
Fig. 7. Von Kossa-stained MBA-15 (A) and MBA-13 (B) cultures supplemented with ascorbic acid and 13-glycerophosphate. Note the extensive mineralization in MBA-15 cultures (A, x 125) and the nod- ules of mineralized extracellular matrix observed in MBA-13 (B, x 125). C-electron diffraction pattern of crystals deposited by MBA- 13 cells in culture, showing intense reflections of hydroxyapatite.
known that induction of osteogenesis can occur in many tissues outside of the skeleton [31] by factors extracted from bone or transitional uroepithelium [32-35].
The evidence supporting the existence of a stromal stem cell in the postnatal organism is suggestive, but more rigor-
References
1. Zipori D (1988) Hemopoietic microenvironment. In: Testa NG, Gale RP (eds) Hematopoiesis. Long-term effects of chemother- apy and radiation. Marcel Dekker, Inc, New York and Basel, pp 27-62
2. Zipori D, Tamir M (1989) Stromal cell of hemopoietic origin. Int J Cell Clon 7:281-300
3. Benayahu D, Kletter Y, Zipori D, Wientroub S (1989) Bone marrow-derived stromal cell line expressing osteoblastic pheno- type in-vitro and osteogenic capacity in-vivo. J Cell Physiol 140:1-7
4. Singer JW, Charbord P, Keating A, Nemunaitis J, Raugi G, Wight TN, Lopez JA, Roth GJ, Dow LW, Fialkow PJ (1987) Simian virus 40- transformed adherent cells from human long- term marrow cultures: cloned cell lines produce cells with stro- mal and hematopoietic characteristics. Blood 70:464--474
5. Owen ME (1985) Lineage of osteogenic cells and their relation- ship to the stromal system. In: Peck WA (ed) Bone and mineral research, Vol. 3. Amsterdam, New York, Oxford, Elsevier, pp 1-25
6. Friedenstein AJ (1973) Determined and inducible osteogenic precursor cells. In: Hard tissue growth, repair and remineral- ization. Ciba Fdn. Symp. Vol. II. North-Holland, Amsterdam, Elsevier-Excerpta Medica, pp 169-185
7. Tavassoli M, Crosby WH (1968) Transplantation of marrow to extramedullary sites. Science 161:54--56
8. Friedenstein AJ (1976) Precursor cells of mechanocytes. Int Rev Cytol 47:327-355
9. Friedenstein AJ, Ivanov-Smolenski AA, Chajlakjan RK, Gor- skaya UF, Kuralesova AI, Latzinik NW, Gerasimow UW (1978) Origin of bone marrow stromal mechanocytes in radio- chimeras and heterotopic transplants. Exp Hematol 6:440--444
10. Friedenstein AJ, Chailakhyan RK, Gerasimov UV (1987) Bone marrow osteogenic stem cells: in vitro cultivation and transplan- tation in diffusion chambers. Cell Tissue Kinet 20:263-272
11. Latsinik NV, Grosheva AG, Narovlyanskii AN, Pavlenko RG, Friedenstein AJ (1987) Clonal nature of fibroblast colonies formed by bone marrow stromal cells in culture. Bull Exp Biol Med 103:356-358
12. Friedenstein AJ (1980) Stromal mechanisms of bone marrow: cloning in vitro and retransplantation in-vivo. In: Thienfelder S (ed) Immunobiology of bone marrow transplantation. Springer- Verlag, Berlin, pp 19-29
D. Benayahu et al.: Marrow Stromal Cells and Osteoblastic Markers
13. Owen M, Friedenstein AJ (1988) Stromal stem cells: marrow- derived osteogenic precursors. In: Evered D, Harnett S (eds) Cell and molecular biology of vertebrate hard tissue. Ciba Fdn. Symp. 136. John Wiley & Sons, New York, pp 42-60
14. Zipori D, Duksin D, Tamir M, Argaman A, Toledo J, Malik Z (1985a) Cultured mouse marrow stromal cell lines. II. Distinct subtypes differing in morphology, collagen types, myelopoietic factors and leukemic cell growth modulating activities. J Cell Physiol 122:81-90
15. Zipori D, Toledo J, von der Mark K (1985b) Phenotypic heter- ogeneity among stromal cell lines from mouse bone marrow disclosed in their extracellular matrix composition and interac- tion with normal and leukemic cells. Blood 66:447-455
16. Zipori D, Friedman A, Tamir M, Silverberg D, Malik Z (1984) Cultured mouse marrow cell lines: interaction between fibro- blastoid cells and monocytes. J Cell Physiol 118:143-152
17. Majeska RJ, Rodan GA (1982) Alkaline phosphatase inhibition by parathyroid hormone and isoproterenol in a clonal rat os- teosarcoma cell line. Possible mediation by cyclic AMP. Calcif Tissue Int 34:59-66
18. Lowry OH, Rosenbrough NJ, Farr AL, Randall RJ (1951) Pro- tein measurement with Folin phenol reagent. J Biol Chem 193:265-275
19. Bellows CG, Aubin JE, Heersche JNM, Antosz ME (1986) Min- eralized bone nodules formed in vitro from enzymatically re- leased rat calvaria cell population. Calcif Tissue Int 38:143-154
20. Rosenquist TH, Slavin BG, Bernick S (1971) The Pearson sil- ver-gelatin method for light microscopy of 0.5-2 ix plastic sec- tion. Stain Technol 46:253-257
21. Rodan GA, Heath JK, Yoon K, Noda M, Rodan SB (1988) Diversity of the osteohlastic phenotype. In: Evered D, Harnett S (eds) Cell and molecular biology of vertebrate hard tissues. Ciba Fdn. Symp. 136. John Wiley & Sons, New York, pp 78-91
22. Sandberg M, Vuorio E (1987) Localization of types I, II and III collagen mRNAs in developing human skeletal tissues by in situ hybridization. J Cell Biol 104:1077-1084
23. Sandberg M, Autio-Harmainen H, Vuorio E (1988) Localization of the expression of types I, III and IV collagen, TGF-[31 and C-fos genes in developing human calvarial bones. Dev Biol 130:324-334
207
24. Parfitt AM (1976) The actions of parathyroid hormone on bone: relation to bone remodeling and turnover, calcium homeostasis and metabolic bone diseases. II. PTH and bone cells: bone turn- over and plasma calcium regulation. Metabolism 25:909-955
25. Rodan GA, Rodan SB (1984) Expression of the osteoblastic phenotype. In: Peck WA (ed) Bone and mineral research, Vol. 2. Elsevier, Amsterdam, pp 244-285
26. Majeska RJ, Nair BC, Rodan GA (1985) Glucocorticoid regula- tion of alkaline phosphatase in the osteoblastic osteosarcoma cell line ROS 17/2.8. Endocrinology 116:170-179
27. Bhargava U, Bar-Lev M, Bellows CG, Aubin JE (1988) Ultra- structural analysis of bone nodules formed in vitro by isolated fetal rat calvaria cells. Bone 9:155-163
28. Ecarot-Charrier B, Shepard N, Charette G, Grynpas M, Glo- rieux FH (1988) Mineralization in osteoblast cultures: a light and electron microscopic study. Bone 9:147-154
29. Bellows CG, Aubin JE (1989) Determination of numbers of os- teoprogenitors present in isolated fetal rat calvaria cells in-vitro. Dev Biol 133:8-13
30. Owen M (1988) Marrow stromal stem cells. J Cell Sci (suppl) 10:63-76
31. Reddi AH, Anderson WA (1976) Collagenous bone matrix in- duced endochondral ossification and hemopoiesis. J Cell Biol 69:557-572
32. Luyten FP, Cunningham NS, Ma S Muthukumaran N, Ham- monds RG, Nevins WB, Wood WI, Reddi AH (1989) Purifica- tion and partial amino acid sequence of osteogenin, a protein initiating bone differentiation. J Biol Chem 264:13377-13380
33. Wozney JM, Rosen V, Celeste AJ, Mitsock LM, Whitters MJ, Kriz RW, Hewick RM, Wang EA (1988) Novel regulators of bone formation: molecular clones and activities. Science 242:1528-1534
34. Wang EA, Rosen V, Cordes P, Hewick RM, Kriz MJ, Luxen- berg DP, Sibley BS, Wozney JM (1988) Purification and char- acterization of other distinct bone-inducing factors. Proc Natl Acad Sci USA 85:9484-9488
35. Huggins C (1931) The formation of bone under the influence of epithelium of the urinary tract. Arch Surg 22:377-408