Proefschrift versie 01-03-2020
-
Upload
khangminh22 -
Category
Documents
-
view
11 -
download
0
Transcript of Proefschrift versie 01-03-2020
University of Groningen
Transplantation of Suboptimal Donor Livers: Exploring the Boundariesvan Leeuwen, Otto
DOI:10.33612/diss.132816502
IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite fromit. Please check the document version below.
Document VersionPublisher's PDF, also known as Version of record
Publication date:2020
Link to publication in University of Groningen/UMCG research database
Citation for published version (APA):van Leeuwen, O. (2020). Transplantation of Suboptimal Donor Livers: Exploring the Boundaries. Universityof Groningen. https://doi.org/10.33612/diss.132816502
CopyrightOther than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of theauthor(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons).
The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license.More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne-amendment.
Take-down policyIf you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediatelyand investigate your claim.
Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons thenumber of authors shown on this cover page is limited to 10 maximum.
Download date: 12-02-2022
Fortheprintingofthisthesis,financialsupportofthefollowinginstitutionsandcompaniesisgratefullyacknowledged:UniversityofGroningenResearchInstituteGUIDENederlandseTransplantatieVerenigingOrganAssistBridgetoLife
©Copyright2020O.B.vanLeeuwen,Groningen.Allrightsreserved.Nopartofthisthesismaybereproduced,storedinaretrievalsystem,ortransmittedinanyformorbyanymeans,withoutpriorpermissionoftheauthor.Layoutandcover:EvelienJagtman–evelienjagtman.comPrinting:Ridderprint–www.ridderprint.nlISBN:978-94-034-2539-9(Book)ISBN:978-94-034-2538-2(Epub)
Transplantation of Suboptimal Donor Livers: Exploring the
Boundaries
Proefschrift
ter verkrijging van de graad van doctor aan de Rijksuniversiteit Groningen
op gezag van de rector magnificus prof. dr. C. Wijmenga
en volgens besluit van het College voor Promoties.
De openbare verdediging zal plaatsvinden op
woensdag 04 november 2020 om 14.30 uur
door
OttoBoudewijnvanLeeuwen
geboren op 15 november 1995 te Apeldoorn
Promotores
Prof.dr.R.J.Porte
Prof.dr.J.A.Lisman
Copromotor
Dr.V.E.deMeijer
Beoordelingscommissie
Prof.dr.H.G.D.Leuvenink
Prof.dr.D.Monbaliu
Prof.dr.J.K.G.Wietasch
Tableofcontents
Chapter1 Generalintroductionandoutlineofthisthesis 11
PartI:Transplantationofsuboptimaldonorlivers:determiningtheboundariesChapter2 Biliarycomplicationsfollowinglivertransplantation 19 In:ClavienPA,TrotterJF,editors.MedicalandSurgicalCareofLiverTransplantationPatients.Wiley-Blackwell;2020Chapter3: Donorhepatectomytimeinfluencesischemia-reperfusion 45 injuryofthebiliarytreeindonationaftercirculatorydeath livertransplantation Surgery.2020(inpress)
Chapter4: Donorbloodcompositionisariskfactorforbiliaryinjury 65indonationaftercirculatorydeathlivertransplantationSubmittedforpublication
Chapter5: Selectedlivergraftsfromdonationaftercirculatory 85deathcanbesafelyusedforretransplantationTransplInt.2020(inpress)
PartII:Transplantationofsuboptimaldonorlivers:expandingtheboundaries
Chapter6: Hypothermicoxygenatedmachineperfusionreduces 105bileductreperfusioninjuryaftertransplantationofdonationaftercirculatorydeathliversLiverTranspl.2018;24:655-664
Chapter7: Extendedhypothermicoxygenatedmachineperfusion 125enablesexsitupreservationofporcineandhuman|liversforupto24hoursJHEPRep.2020(inpress)
Chapter8: Transplantationofhigh-riskdonorliversafterexsitu 149resuscitationandassessmentusingcombinedhypo-andnormothermicmachineperfusion:aprospectiveclinicaltrial.AnnSurg.2019;270:906-914
Chapter9: Exsitumachineperfusionofhumandonorliversviathe 171surgicallyreopenedumbilicalvein:aproofofconcept.Transplantation.2019;103:2130-2135.
Chapter10: Summary,DiscussionandFuturePerspectives 185
AppendixI: CasereportrelatedtoChapter6:
Thefirstreportofsuccessfultransplantationof 199apediatricdonorlivergraftafterhypothermicmachineperfusionPediatrTransplant.2019;23:e13362
AppendixII: CommunicationrelatedtoChapter8:
Viabilitycriteriaforfunctionalassessmentofdonor 211liversduringnormothermicmachinepreservationLiverTranspl.2018;24:1333-1335
Nederlandsesamenvatting 217
Listofpublications 225
Dankwoord 229
Curriculumvitae 236
Livertransplantation:pastandpresentLiver transplantation is currently the standard life-saving treatment for patientswith
end-stageliverdiseaseaswellasforselectedpatientswithhepatobiliarymalignancies
or certainmetabolicdiseases.The first liver transplantwasperformedbydr.Thomas
StarzlandhisteaminDenver,Colorado,in1963.1Unfortunately,asaresultofmassive
bleeding,thethree-years-oldrecipientdiedintra-operatively.Problemspersistedduring
the following five transplants, with patient survival no more than 23 days. In 1967,
Starzlperformedthefirstsuccessfullivertransplantwithpatientsurvivalexceedingone
year.2 Twelve years later, after Calne’s development of cyclosporine and Starzl’s
introduction of tacrolimus, liver transplantation steadily progressed towards a
standardizedtreatmentwithacceptableoutcomes.3,4Nowadays,1yeargraftandpatient
survivalratesofover90%areseenglobally.
Thedemandfordonor livers,however,severelyexceedsthenumberofsuitabledonor
livers available. Until the late 1990’s liver grafts were mainly donated after
determinationofbraindeathinthedonor(DBDdonation). Inanattempttowidenthe
potentialdonorpool,donationaftercirculatorydeath(DCD)wasre-introduced.5Inthe
earlyphasesofthisdevelopment,excellentresultswithDCDlivertransplantationwere
achieved.However,byextendingtheacceptancecriteriaforDCDlivers,theprevalence
of biliary complications increased. Post-transplant cholangiopathy (PTC) became the
mostfrequentcomplicationfollowingDCDlivertransplantation.6Thelargestcomponent
ofPTCsare thenon-anastomotic strictures (NAS)of thebileduct in thepresenceofa
patenthepaticartery.IncidencesofNAShavebeenreportedinupto30%ofDCDliver
recipients.6
Organpreservation
In the early 1980’s, Belzer’s group developed the University of Wisconsin (UW)
preservation solution, which became a standardized fluid used to preserve organs.
Duringorganprocurement,theabdominalcompartmentisflushedwithseverallitersof
ice-coldUWsolution,afterwhichtheliverisstoredinabagcontainingUWsolutionina
box with ice. This static preservation technique, unfortunately, does not sufficiently
prevent NAS. As a result, dynamic preservation techniques of donor livers by using
machine perfusion is increasingly studied in an attempt to improve outcomes after
(suboptimal) liver transplantation.7-10Ex situmachine perfusion can be performed at
different temperatures and time points. For example, hypothermicmachine perfusion
(4-12°C) has the potential to reduce ischemia-reperfusion injury, whereas
normothermic machine perfusion (37°C) allows viability testing and potential graft
treatment.9
Outlineofthisthesis
This thesis focuses on transplantation of suboptimal donor livers, especially livers
donated after circulatory death. Part 1 contains observational studieswhich aimed to
identifytheboundariesintransplantationofsuboptimaldonorlivers,andtorecognize
risk factorsthatdeterminetheseboundaries.Part2containsobservational,preclinical
and clinical studies with a common goal to investigate safe and successful
transplantationofsuboptimallivers.
Part I: Transplantation of suboptimal donor livers: determining the boundaries
Biliary complications, including NAS, remain the Achilles heel in DCD liver
transplantation.6 About half of the patients that develop NAS undergo re-
transplantation,withanother25%passingawaybeforeasuitabledonorliverbecomes
available.6 Several studies have focused on predicting graft survival after DCD liver
transplantation, but the prediction of NAS still remains highly difficult. Known risk
factorssuchashighdonorage,prolongeddonorwarmischemiatimesandcoldischemic
preservationperiodsarenotpresentinasignificantproportionofNAScases.Chapter2
provides a review of literature on biliary complications after liver transplantation.
Although ischemia and subsequent reperfusion injury is a main risk factor for the
development of NAS, other mechanisms, such as immune-mediated injury, bile salt
toxicity, and insufficient regeneration of the epithelium also play a role in the
pathogenesis, and are discussed in this review. Chapter 3 describes a study on the
influenceofthetimebetweenstartofcoldflushingandtheendofliverretrievalonthe
development of biliary complications after DCD liver transplantation. During liver
retrieval, donor livers maintain a temperature of around 15-20°C and therefore
continuestosufferlukewarmischemia.12Therefore,itishypothesizedthattheduration
of this period is a substantial determinant of the development of NAS. Chapter 4
contains a study on the involvement of DCD donor blood composition on the
development of biliary complications. In addition to peribiliary gland injury,
arteriolonecrosis inthebileductwall isconsideredtobeoneoftheprimeriskfactors
for thedevelopmentofNASafter transplantation.13Weconsideredthatgraft flush-out
upon procurement, and thereby the severity of the arteriolonecrosis, would be
influencedby the cellular compositionof donorblood. Inchapter5, it is investigated
whetherDCDliverscanbesafelyusedforpatientsrequiringare-transplantation.
Part II: Transplantation of suboptimal donor livers: expanding the boundaries
Overthelastyears,dynamicpreservationofdonorliversbyusingmachineperfusionis
slowlymaking itsway into clinic.The first randomized controlled trialshave recently
finished with patient accrual, however, study protocols are highly different over the
globeandtheresultsofaforementionedtrialsremainawaited.8Substantialbenefitsof
end-ischemic hypothermic machine perfusion have been reported, however, viability
testing(especiallyofthebiliarytree)remainsnotpossibleusingthistechnique.9-11End-
ischemic normothermicmachine perfusion has the benefit that it does allow viability
testing,butitexposestheorgantoanextrahitofischemia-reperfusioninjuryanddoes
notmitigate reperfusion injury.8 In the studydescribed inchapter6,we investigated
the effect of dual hypothermic oxygenated machine perfusion (DHOPE) on the
development of biliary injury during DCD liver transplantation. Biopsies were taken
upon arrival and after reperfusion in DHOPE livers and control livers, to assess the
potentialbenefitofDHOPE.Inchapter7,wedescribeastudyonthesafetyofprolonged
DHOPE, and compared liver function after 2, 6 and 24 hours of DHOPE. Prolonged
DHOPE can simplify logistics and may potentially facilitate day-time liver
transplantation. In chapter 8, we report the results from a single-arm prospective
intervention trial. In this study, end-ischemic dynamic preservation using sequential
hypo- and normothermicmachine perfusionwas applied in an attempt to resuscitate
andassessthefunctionofpreviouslydiscardedhumanlivers,andtosubsequentlyallow
safe transplantation. Chapter 9 contains a preclinical study to potentially simplify
ischemia-free liver transplantation.14 Rather than portal perfusion via an end-to-side
anastomosedautologousiliacveingraft,weinvestigatedthefeasibilityofportalvenous
machineperfusionviathesurgicallyreopenedumbilicalvein.
Locatedafterchapter10aretwoappendices.AppendixIisacasereportusingthe
techniquedescribedinChapter6.AppendixIIcontainsaneditorialinwhichviability
criteriaforfunctionalassessmentofdonorliversarediscussed.
References
1. Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR.Homotransplantationoftheliverinhumans.SurgGynecolObstet.1963;117:659–676.
2. Starzl TE, Groth CG, Brettschneider L, Penn I, Fulginiti VA, Moon JB, et al.Orthotopichomotransplantationofthehumanliver.AnnSurg.1968;168(3):392–415.
3. CalneRY,RollesK,WhiteDJ,ThiruS,EvansDB,McMasterP,etal.CyclosporinAinitiallyastheonlyimmunosuppressantin34recipientsofcadavericorgans:32kidneys,2pancreases,and2livers.Lancet.1979;2(8151):1033–1036.
4. StarzlT,FungJ,VenkatarammanR,TodoS,DemetrisA,JainA.FK506forliver,kidneyandpancreastransplantation.TheLancet.1989;334(8670):1000-1004.
5. Monbaliu D, Pirenne J, Talbot D. Liver transplantation using Donation afterCardiacDeathdonors.JHepatol.2012;56(2):474-485.
6. de Vries Y, von Meijenfeldt F, Porte R. Post-transplant cholangiopathy:Classification,pathogenesis,andpreventivestrategies.BiochimBiophysActaMolBasisDis.2018;1864(4):1507-1515.
7. JamiesonNV,SundbergR,LindellS,etal.Preservationofthecanineliverfor24-48hours using simple cold storage with UW solution. Transplantation1988;46(4):517-522
8. NasrallaD,CoussiosCC,MergentalH,etal.Arandomizedtrialofnormothermicpreservationinlivertransplantation.Nature2018;557:50-56.
9. Schegel A,Muller X, KalisvaartM, et al. Outcomes of DCD liver transplantationusing organs treated by hypothermicmachine perfusion before implantation. JHepatol2019;70:50-57.
10. DeMeijerVE,FujiyoshiM,PorteRJ.Exsitumachineperfusionstrategiesinlivertransplantation.JHepatol.2019;70:203-205.
11. VanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusion in liver transplants donated after circulatory death. Br J Surg2017;104:907-917.
12. VillaR, Fondevila C, Erill I, et al. Real-timedirectmeasurement of human liverallograft temperature from recovery to transplantation. Transplantation.2006;81(3):483-486.
13. OpdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsandvascular plexus before liver transplantation predicts formation of non-anastomoticbiliarystrictures.JHepatol2014;60:1172-1179.
14. HeX,GuoZ,ZhaoQetal.Thefirstcaseofischemia-freeorgantransplantationinhumans:Aproofofconcept.AmJTransplant2017;18(3):737-744.
Biliarycomplicationsfollowinglivertransplantation
OttoB.vanLeeuwen,IrisE.M.deJong,RobertJ.PorteIn:ClavienPA,TrotterJF,editors.MedicalandSurgicalCareofLiverTransplantationPatients.Wiley-Blackwell;2020
2
Introduction
Biliary complications are a major cause of morbidity and graft failure after liver
transplantation.Althoughadvancesinthesurgicaltechniqueoflivertransplantation
have led to a better overall outcome and fewer surgical complications, biliary
complications still occur in10–40%of recipientsandareassociatedwithmortality
rates of 8–15%.1-3 The high biliary complication rate in liver transplantation can
partlybeexplainedbytheincreasingdiversityoflivergraftsusedfortransplantation
inrecentyears.Theshortageofgraftsavailablehasledtotheincreaseduseoflivers
that have been donated after cessation of blood flow in the donor, or so called
donationaftercirculatorydeath(DCD)donors.TheorgansofDCDdonorssufferedan
extraperiodofwarmischemiacomparedtodonationafterbraindeath(DBD)livers,
andarethereforemoresusceptibletodevelopbiliarycomplications.TheuseofDCD
organs andother extended-criteriadonor livers is inevitable in an attempt to scale
down the worldwide shortage of organs. In order to expand the pool of potential
donors, split-liver transplantation and living donors have also evolved as surgical
alternatives and numbers have increased in recent years, providing particularly
youngchildrenwithanopportunitytoreceiveagraft in time.Therateofsplit-and
livingdonortransplantationshowslargevariationsamongcountries. InsomeAsian
countries, the percentage of living-donor liver transplantation rate reaches almost
100%, whereas in the US and most European countries the percentage is around
10%.Diversityinthequalityandtypeoftransplantedorgans,variationsinrecipient
risk factors, and variations in the applied surgical technique lead to a diversity in
biliary complications that may occur after liver transplantation. The three most
common types of biliary complications can are: non-anastomotic strictures (NAS),
anastomotic strictures and biliary leakage.4 These and other less frequent biliary
complicationsaresummarizedinbox32.1andwillbediscussedinthischapter.First,
aspects of organ procurement that are relevant for the prevention of biliary
complicationswillbecovered.Hereaftersurgicalaspectsofbileductreconstruction
willbediscussed,followedbyadiscussionofdiagnosticandimagingmethodsanda
descriptionofthepathogenesis,clinicalpresentation,andmanagementofthevarious
typesofbiliarycomplicationsafterlivertransplantation.
Table1.
Classificationofbiliarycomplicationsafterlivertransplantation4
1. Biliaryleakage
1A.Frombiliaryanastomosis
1B.Fromhepaticbiopsyorparenchymalinjury
1C.Fromgallbladderfossaorcysticductstump
1D.Afterremovalofbiliarydrain
2. Anastomoticstenosisof:
2A.Choledocho-choledochostomy
2B.Hepatico-jejunostomy
3. Post-transplantcholangiopathy
3A. Non-anastomotic biliary strictures (of extrahepatic and large intrahepatic
ducts)
3B.Intraductalbiliarycasts
3C.Bileductnecrosiswithintrahepaticleakageandbilomaformation
4. Biliaryabnormalitiesduetohepaticarterystenosisofthrombosis
5. Biliarystricturesduetorecurrentdisease(i.e.primarysclerosingcholangitis)
2.Surgicaltechniqueinrelationtobiliarycomplications
2.1Organprocurementandpreservation
Efforts tominimize the risk of biliary complications after liver transplantation should
start with proper surgical and preservation techniques during the donor procedure.
Aspectsof liverprocurementandpreservationthathavebeendemonstratedtoreduce
the risk of biliary complications include: 1) efforts tominimize ischemic injury of the
bileducts,2)preservationof thevasculatureof theextrahepaticbileductbyavoiding
dissectiontooclosetothebileduct,3)thoroughrinsingofthebileductlumentoremove
toxicbile,4)adequatearterialperfusionoftheliverwithpreservationfluidtopreserve
theperibiliarycapillaryplexusand5)rapidprocurementafterinitiationofcoldflushing
inthedonor.
Theseaspectsarerelevantasbiliaryepithelialcells(cholangiocytes)areverysensitive
to ischemia/reperfusion injury. In addition to primary preservation-related ischemic
injury,ischemicdamageoftheperibiliaryplexuswillresultinsecondaryischemicinjury
ofthebiliaryepithelium.Thestrongrelationshipbetweenischemiaandbileductinjury
is illustrated by studies demonstrating an association between both cold and warm
ischemia time and thedevelopment ofNAS.As long as the cold ischemia time is kept
below 10 h, the incidence of NAS is not increased, however more prolonged cold
ischemiaisclearlyassociatedwithahigherriskofthesestrictures.Warmischemiatime
has also been identified as a risk factor in several studies. The relevance of warm
ischemia isalso illustratedby thehigh incidenceofNASafter transplantationof livers
fromDCDdonors,which suffer an inevitable period ofwarm ischemia prior to organ
procurement.5,6
During organ procurement, surgeons should avoid “stripping” of the extrahepatic bile
duct, which will damage its microvascularization. The extrahepatic bile duct should
alwaysremainsurroundedbyanadequateamountof tissuetoensuresufficientblood
supply.
Preservation injury results in increased arterial resistance andmay cause circulatory
disturbancesinsmallcapillaries,suchasthebiliaryplexus.Sincethebloodsupplytothe
biliary tract is solely dependent on arterial inflow, disturbances in the blood flow
through the peribiliary plexusmay result in insufficient oxygenation and subsequent
damageofthebiliaryepithelium.
Gentle retrograde flushing of the bile ducts with preservation fluid is considered an
important method to remove bile from the bile duct lumen. Bile contains bile salts,
whicharecytotoxicduetotheirdetergentproperties.Severalstudieshaveshownthat
bile salts may contribute to toxic damage of the biliary epithelium both during liver
preservationandafterlivertransplantation.7,8Atthismoment,thereisnoconsensuson
whichflushingsolutionismostadequateforsuccessfulbileductpreservation.
University of Wisconsin (UW) solution and Histidine-tryptophan-ketoglutarate (HTK)
have been recognized as the gold standard preservation solutions. Although some
studies have suggested that highly viscous preservation solutions such as the UW
solutionmay result in an incomplete flush-out of the small donor peribiliary arterial
plexus,resultinginahigherincidenceofNAS,9,10thiscouldnotalwaysbeconfirmedin
other studies.11 Therefore, it remains debatable whether low viscosity preservation
fluids, such as HTK, are associated with a lower incidence of biliary complications.
Adequatelypoweredrandomized,controlledtrialswithlong-termfollowupareneeded
to determine whether the type of preservation fluid has an impact on biliary
complicationsafterlivertransplantation.
Onemethodtoovercomeinadequateflush-outandpreservationoftheperibiliaryplexus
is theapplicationofhighpressurearterial infusionofpreservation fluideither in vivo
duringprocurementorimmediatelyafterwardsduringtheback-tableprocedure.Some
retrospective studies have shown that additional flushing of the peribiliary plexus by
controlledarterialback-tablepressureperfusionmayresultinaconsiderablereduction
in the incidence ofNAS.12However, a prospective, randomized controlled trial on the
efficacyof additional arterial ex situback-tableperfusiondemonstrated that thisdoes
not prevent NAS after transplantation.13 Better flush-out and preservation of the
peribiliarycapillaryplexusmayalsobeachievedbymachinepreservation.Severalsmall
studies have shown that end-ischemic hypothermic oxygenated machine perfusion is
safelyapplicable in livertransplantation,andtheresults lookpromising.14-18Asof this
moment,norandomizedcontrolledtrialshavebeenfinishedyetontheoutcomesafter
theuseofhypothermicmachineperfusioninlivertransplantation.
Recently,theperiodbetweenthestartofcoldflushofthedonororgansandtheendof
liverretrievalhasbeenshowntoinfluencegraftsurvival.19Duringorganprocurement,
thetemperatureoftheabdominalorgansdoesnotdropbelow15-20°C.whichdoesnot
protecttheliverandbileductsagainstwarmischemicinjury.Therefore,afterinitiation
ofinsitucoldflushing,adonorlivershouldbeexcisedasrapidlyaspossibleandplaced
in a bowl with preservation fluid with sterile ice, where it will finally reach a
temperature<4°C.20Hereafter, the livershouldbestoredassoonaspossible insterile
bagsandaboxwithice.
2.2Biliaryreconstruction
Thetwomaintypesofbiliaryreconstructionusedinlivertransplantationtodayare:1)
choledocho-choledochostomy,alsocalledtheduct-to-ductanastomosis(usingeitheran
end-to-endanastomosisora side-to-sideanastomosis), and2)ahepatico-jejunostomy
usingaRoux-Y jejunal loop.Theuseofonetypeofreconstructioninsteadoftheother
largelydependsontheanatomicalsituationoftherecipient’sextrahepaticbileductsand
sometimesthesurgicalpreference.
In case of a duct-to-duct choledocho-choledochostomy, an anastomosis is created
between donor and recipient choledochal ducts (common bile duct). An end-to-end
anastomosisisgenerallyeasiertoperformthanaside-to-sideanastomosis,theformeris
therefore usedmore frequently. In a prospective, randomized trial comparing end-to-
end anastomosis with side-to-side anastomosis, no major differences in outcome
between the two techniqueswere found.21 An end-to-end reconstruction restores the
physiologic anatomical situation and does not carry the risk of bile sludge or cast
formationascanoccurinthedeadendsofaside-to-sideanastomosis.
In case of a Roux-Y hepatico-jejunostomy, an end-to-side anastomosis is constructed
betweenthedonorhepaticductandaRoux-Yjejunalloopcreatedintherecipient.Roux-
Yhepatico-jejunostomyismainlyusedinpatientswhosenativeextrahepaticbileductis
notsuitableforanastomosiswiththebileductofthedonorliver.Themainindications
for using a Roux-Y loop for biliary reconstruction are primary sclerosing cholangitis
with involvement of the extrahepatic bile duct, biliary atresia, significant size
discrepancy between the donor and recipient choledochal duct, and in some cases,
retransplantation.22,23Althoughahepatico-jejunostomymaybeasafealternativewhen
duct-to-duct anastomosis is not feasible, the disadvantage is that it creates an open
connectionbetween the intrahepaticbileductsof thegraftand thebowel lumen.This
may result in reflux of small bowel content into the bile ducts and subsequently
ascending bacterialmigration and (recurrent) cholangitis. An additional advantage of
using a choledocho-choledochostomy is easier access for diagnostics and therapy
comparedwithaRoux-Yhepatico-jejunostomy.Itis,therefore,generallyagreedthatthe
preferred method of biliary reconstruction in liver transplantation should be a
choledocho-choledochostomywheneverpossible.
Fewcentershaveadvocatedandreportedontheuseofadirectconnectionbetweenthe
donorbileductandtherecipientduodenum(so-calledcholedocho-duodenostomy)asa
safealternativetoahepatico-jejunostomy.24
2.3Useofabiliarydrain
Whenreconstructingthebiliarysysteminalivertransplantrecipient,thiscanbedone
eitherwithorwithouttheinsertionofabiliarydrain.AbiliarydraincanbeeitheraT-
tubeorastraight(opentip)catheter.AT-tube isa flexibletubethat is inserted inthe
choledochal duct in the proximity of the end-to-end anastomosis in case of a
choledocho-choledochostomy. This tube allows the bile to drain in two directions:
towardstheduodenumandoutwardof thebody.Alternatively,astraightcathetercan
beused,withtheadvantageofalowerriskofbileleakageuponremovalofthedrainas
itresultsinasmallerholeinthebileductafterextraction.
Choledocho-choledochostomy reconstructions over T-tubes have been the subject of
controversyformanyyears,butithasneverthelessremainedcommonpracticeinsome
transplantcenters.Yet,withincreasingsurgicalexperience,manycentershavebegunto
abandontheroutineuseofbiliarydrainsintheirlivertransplantrecipients.25,26
Thebenefitsofusingabiliarydrainincludedirectvisualevaluationofthequalityofbile
produced by the recently implanted graft and easy access to the biliary tree for
radiologicimaging.Especiallyinlivergraftsthathaveahigherriskofdevelopingbiliary
complications (e.g. livers fromDCDdonors) this could be an advantage. Some studies
have suggested that placement of a T-tube may reduce the incidence of anastomotic
strictures.27 In addition a T-tubemay result in adequate decompression of the biliary
treeandareductionoftheintraductalpressure,whichmaysubsequentlycontributetoa
lowerrateofintrahepaticbiliarystrictureandleakage.
ThemaindrawbackofusingT-tubesistheirassociationwithanincreasedrateofbiliary
complications,especiallybileleakageatthesiteofthedraininsertionafteritsremoval
occurring in5–15%ofpatients.21 Inaddition, theuseofaT-tube increases theriskof
ascendingcholangitisandperitonitis,duetoanopenconnectionofthecholedochalduct
withtheexterior.Inonesystematicreviewandmeta-analysisofstudiesfocusingonthe
useofbiliarydrainsinlivertransplantationitwasconcludedthatbiliarydrainssuchas
T-tubes should be abandoned.25 Although this meta-analysis showed lower rates of
anastomoticandNAS inpatientswithaT-tube, the incidenceof interventionswasnot
diminished in comparison topatientswithoutaT-tube.PatientswithoutaT-tubehad
fewer episodes of cholangitis and fewer episodes of peritonitis. Yet, patients with or
without a T-tube had equivalent outcomes with respect to anastomotic bile leaks or
fistulas, the need for biliary interventions, incidence of hepatic artery thrombosis,
retransplantationrate,andmortalityduetobiliarycomplications.Twoothersystematic
reviewsandmeta-analysesshowthattheuseofaT-tubemightreducetheincidenceof
biliarystrictures,but that there isnohardevidence towardsstandardizeduse in liver
transplantation.26,27
The use of alternative devices, such as internal stents, have been reported by some
centers, but these stents have been associated with increased rates of serious
complications,includingobstruction,migration,anderosionwithhemobilia.28
The use of biliary drains such as a T-tube in liver transplant recipients, therefore,
remainscontroversial.ProbablytheonlyremainingargumenttouseaT-tubeistoallow
accurate monitoring and easy access to the biliary tree in liver grafts that carry an
increasedriskofbiliarycomplications,liversfromDCDdonorsforexample.
3.Diagnosticmodalities
Inmostcases,thesuspicionofabiliarycomplicationwillariseafteranincreaseinliver
enzymes is noted. There is no specific pattern to reliably distinguish a biliary
complication from other causes of graft dysfunction, although an increase in serum
bilirubin,alkalinephosphataseand/orgamma-glutamyltransferasehasbeensuggested
to bemost specific. Alternatively, patients can presentwith upper abdominal pain or
bacterialcholangitis.Inmanyinstancesofliverenzymedisturbances,aliverbiopsywill
beperformedaftergrossbiliarycongestionandbileductdilatationhavebeenexcluded
byultrasonography.Thepresenceof specificpathologic features suchas centrilobular
cholestasis andportal changes including edema,predominantlyneutrophil polymorph
infiltration,ductularproliferationandcholangiolitismaybeindicativeofthepresenceof
a biliary complication.28 These findings, however, are not very specific and can be
absent. In addition, biopsy findings are not informative with regard to the type and
severityofbiliaryabnormalities.
Thediagnosticwork-upofan increase in liverenzymeswillalwaysdependonclinical
context such as primary disease, time after transplantation, local experience, and
informationonthebiliaryanatomy.AgeneralalgorithmisprovidedinFigure1.
Figure1:Schematicpresentationoftheclinicaldecisionsanddiagnosticstepsin
thework-upofalivertransplantrecipientwithasuspectedbiliarycomplication.
3.1Transabdominalultrasonography
Transabdominal ultrasonography is a useful primary diagnostic tool when a biliary
complicationissuspected.Allograftvascularizationcanbeassessed(especiallypatency
of the hepatic artery), fluid collections can be identified, liver parenchyma can be
studied, and dilatation of bile ducts can be identified. It should be noted that the
transplanted liver behaves differently from a normal liver, in that the biliary system
doesnot dilate as easily in thepresenceof a biliary obstruction as innormal livers.29
This leads to a limited sensitivity of approximately 60% of transabdominal
ultrasonographytodetectbiliarystrictures.29,30Thepredictivevalueoftransabdominal
ultrasonographytodetectNASisratherlow.Therefore,evenanormalultrasonography
of the livergraft inapatientwithclinicalorbiochemicalevidenceofbiliarypathology
warrantsfurtherinvestigation.
3.2Magneticresonancecholangiographyandcomputedtomography
Magnetic resonance cholangiography (MRC) is an established diagnostic tool for the
detection of biliary abnormalities. It has the strong advantage of providing excellent
anatomic information without being invasive. MRC is useful in the detection of both
leakages and strictures. The use of an additional magnetic resonance imaging or
magneticresonanceangiographyscanningprotocolcanalsoprovideinformationabout
the liverparenchymaandvasculature.The reported sensitivity and specificityofMRC
forthedetectionofbiliarycomplicationsiswellover90%.31Afterultrasonography,MRC
isthepreferreddiagnostictoolwhenabiliarycomplicationissuspected.However,one
study showed that MRC is indeed a reliable tool to detect or exclude biliary
complications, but that its reliability to grade severity of these strictures is low.32
Recently, also computed tomography (CT) scanninghasbeensuggested tobeofvalue
for the detection of post-transplant biliary complications – it has a higher spatial
resolution compared toMRC.However, the experiencewith CT cholangiography after
liver transplantation is very limited: 1) it can only be performed using a contrast
medium, 2) it is associated with significant radiation, and 3) it is less reliable in the
presence of biliary obstruction or high serum bilirubin levels. The use of CT
cholangiography to detect a biliary complication should still be considered
experimental.
3.3Directcholangiography
Direct cholangiography, either percutaneously or through endoscopic retrograde
cholangiography (ERC), has been the gold standard for the detection of biliary
abnormalitiesforalongtime.Ithastheinherentadvantageofbiliaryaccesstofacilitate
therapeuticmeasures.Sincetheuseofabiliarydrain(e.g.T-tube)isnolongerroutine
practiceinmosttransplantcenters,ERCisafrequentlyusedmethodtodetectandtreat
biliarycomplications.However,overthelastyearsthelessinvasiveMRCisincreasingly
used when compared to ERC. There is no data to suggest that ERC after liver
transplantationisassociatedwithmorecomplicationsthantheuseofERCinthegeneral
population. Considering the safety, diagnostic yield, and therapeutic potential of ERC,
this should be considered the preferred invasive method. In the presence of altered
biliary anatomy, such as a Roux-Y hepatico-jejunostomy, ERC is more difficult to
perform. In these cases, percutaneous transhepatic cholangiography (PTC) or PTC
drainage isagoodalternativemethod toobtainadequate imagingof thebileducts. In
several series successful ERC in the presence of a Roux-Y reconstruction has been
reportedusingeitheranormalduodenoscopeordouble-balloonendoscopes.33,34PTCis
most easily obtained in the presence of dilated bile ducts. In experienced hands,
however,thiscanbeasafeprocedurealsowithundilatedbileducts.35Itnotonlyallows
adequate imaging of the bile ducts, but also provides access for therapeutic
interventionssuchasballoondilatation(asdiscussedbelow).
3.4Hepatobiliaryscintigraphy
Hepatobiliary scintigraphy can be used as a diagnostic tool to detect post-transplant
biliary obstruction and leakage. It has a sensitivity of approximately 60% for these
indications.36 Themain advantage is its non-invasive nature; itsmain disadvantage is
lowresolutionandlackofdirectvisualizationofthebiliaryanatomy.Thesensitivityof
hepatobiliary scintigraphy to detect NAS is not known. With the increasing use and
availability of MRC, scintigraphy is today rarely anymore used to detect biliary
strictures.Itcouldstillbeofvalueinthosepatientsinwhomanobstructionatthelevel
oftheRoux-Yjejunal loopissuspectedorwhenMRCisnotpossible(i.e.presenceofa
pacemaker).
3.5Otherdiagnostictools
Endoscopic ultrasonography is an emerging tool for the detection of hepatobiliary
diseases. It has excellent diagnostic properties for the distal bile duct. Endoscopic
intraductal ultrasonography can be used for the characterization of intraductal
abnormalities.Useofthesetechniquesinlivertransplantrecipientsisstillanecdotal.A
potentially more valuable tool is direct cholangioscopy. With this technique, a small
endoscope (cholangioscope) can be advanced through a normal duodenoscope to
directly visualize the bile ducts. This can provide information about the biliary
epitheliumandthepresenceofstones,sludgeandstrictures.Itcanalsobeatherapeutic
tooltoadvanceguidewiresortoremovebileductstones.Thenumberofindicationsfor
thesehighlyspecializedtechniques,however,isstilllimited.
4.Pathogenesis,clinicalpresentation,andmanagement
A broad variety of biliary complications can occur after liver transplantation and the
pathophysiologyisoftenmultifactorial.Itspresentationmaybeaspecificandphysicians
canidentifybiliarycomplicationsbyoneormoreofthefollowingsymptoms:abdominal
pain, cholangitis, elevated liver enzymes and jaundice if the bile duct becomes
obstructed. In general, critical mechanisms in the development of post-transplant
cholangiopathyincludeischemia-reperfusioninjury,alteredandthereforetoxicbilesalt
composition,insufficientprotectionbytheHCO3-umbrella,aninsufficientregeneration
ofthebiliaryepitheliumbycholangiocytesandperibiliaryglands,anddifferentimmune-
mediatedinjuries.Eachofthesemechanismscanconcomitantlycontributetobileduct
damage during and after liver transplantation and result in subclinical and clinical
manifestations. Accordingly, various biliary complications overlap and share common
pathogeneses. For example, hepatic artery thrombosis (HAT) results in tremendous
ischemicaldamage, lossof cholangiocytes, andbileductwallnecrosis.NAS, casts, and
eventually,intrahepaticbileductleakagecandevelop.Inthiscase,lossoftheepithelial
barrier leads to infiltrationof toxicbile into thebileductwall and this in turn causes
morebileductdamage,necrosis,andintrahepaticbilomaformation.Castsdevelopfrom
the cumulating epithelial cells that are sloughedoff from thebile ductwall.However,
NASarenotalwaysprecededbyHATandintraductalcastsandsludgecanbedetected
withoutsignsofNAS.Thisexplainstheheterogeneityofbiliarystricturesandtherefore
we propose the term post-transplant cholangiopathy to describe the spectrum of
pathologies of the larger bile ducts in the absence of hepatic artery thrombosis or
stenosis without signs of recurrent diseases (i.e. primary sclerosing cholangitis). A
completeclassificationofbiliarycomplicationsaftertransplantationisdepictedinBox
32.1,ofthese,themostcommontypesarebiliaryleakageandbileductstrictures.
4.1Biliaryleakage
Pathogenesisandclinicalpresentation
Bileleakageafterlivertransplantationisreportedin1–25%ofrecipients.Theincidence
ofbileleakageisthehighestaftertransplantationofasplitliveroragraftfromaliving
donorduetothehepaticresectionsurface.29,37Bile leakagecaneitherbesymptomatic
or asymptomatic, and may be discovered coincidentally on a postoperative
cholangiogram. Symptomatic patients may present with abdominal pain, localized or
generalized peritonitis, fever, and sometimes elevated serum liver enzymes and/or
bilirubin.
Biliary leakage can occur at various sites and intervals after transplantation. The
majorityofpostoperativeleaksoccuratthesiteofanastomosisortheT-tubeinsertion
site,butalsotheresectionsurfaceofthegraftincaseofaliving-donororasplit-donor
transplantation is a common site for leakage. Bile leakage early after liver
transplantationmostlikelyoriginatesfromtheanastomosisortheT-tubeinsertionsite.
Anastomotic leaks aremainly related to errors in surgical technique and/or ischemic
necrosisattheendofthebileduct.Insufficientbloodsupplyortractionofthestitches
causesischemia,whichcanresultinbileleakage.Ahepaticarterythrombosiscanleadto
massivebiliarynecrosisresultingindehiscenceofthebiliaryanastomosis.Bileleakage
attheT-tubeinsertionsitecanoccurimmediatelyaftertransplantationorafterremoval
of theT-tubedue toan insufficiently formed fistulaaround the tractof thebiledrain.
Occasionally, bile leakage occurs after percutaneous liver biopsy or iatrogenic duct
damage.
Management
The management of bile leaks depends on the type of biliary anastomosis, clinical
presentation,severity,andlocalizationofthebileleak.Themajorityofbileleaksaredue
toleakageatthesiteofthebiliaryanastomosis.Ifaleakpresentsshortlyaftersurgery,
ultrasonographyshouldbemadetoconfirmarterialperfusionofthegraft.
A small anastomotic bile leak can sometimes be managed conservatively, especially
when thepatient isasymptomatic.Earlyanastomotic leakagecanbestbe treatedbya
relaparotomyandasurgicalrevisionofthebiliaryanastomosis.Symptomaticorinfected
bile collections should be treatedwith a radiologically placed percutaneous drain. An
anastomotic bile leak without disruption of the anastomosis can be successfully
managed primarily nonsurgically. Stenting of the bile duct, nasobiliary drainage,
sphincterotomyandacombinationofthesehaveallbeenusedwithasuccessrateof85–
100%. Since sphincterotomy may lead to specific complications (bleeding and
perforation),itshouldnotberoutinelyperformed.Theoptimaltimingofstentremoval
afterresolutionofsymptomsisstillunclear,but8weekshasbeenprovensuccessful.38
Inthepresenceofahepatico-jejunostomy,ERCPcanbeattempted,butisfrequentlynot
successful.Alternatively,aPTCdraincanbeplaced,eveninthepresenceofnon-dilated
bileducts.35
In the rare case of a complete disruption of the anastomosis, prompt surgery with
conversion to a hepatico-jejunostomy is most appropriate. In selected cases a repeat
choledochocholedochostomycanbeconsidered.Inthecaseofdiffusebiliousperitonitis
withhemodynamicinstabilityorsepsis,directlaparotomyshouldalwaysbeconsidered.
Leakageafterremovalofabiledraincanbemanagedsuccessfullyinone-thirdofcases
by conservative measures, including intravenous fluids, antibiotics, analgesics, and
observation.39 In the absence of improvement, ERCP with stent placement should be
performed. A laparotomy is indicatedwhen clinical signs of biliary peritonitis persist
despiteadequatedrainageofthebiliarysystem.
4.2Anastomoticstenosis
Pathogenesisandclinicalpresentation
Isolated strictures at the site of the bile duct anastomosis, so-called anastomotic
strictures, are reported in 4–9% of patients after liver transplantation. In general,
anastomoticstricturesdonotremainsubclinicalandaredetectedaftertheoccurrence
of cholestatic laboratory liver function tests, jaundice, or cholangitis.40 Anastomotic
strictures are thought to resultmainly from surgical technique and/or local ischemia,
leading to fibrotic scarring of the anastomosis. Surgical factors include inadequate
mucosa-to-mucosa adaptationat the anastomosis anddamageofmicrovascularization
duetodissectiontooclosetothebileduct.41Tominimizetheriskoflocalischemiaatthe
distal end of the donor choledochal duct, the bile duct should therefore remain
surrounded by an adequate amount of tissue. Generalized hepatic ischemia due to
hepaticartery thrombosiscanalsoresult inanastomoticstricturing.Otherrisk factors
for the development of anastomotic structures are anastomotic bile leakage after
transplantationandasexmismatchbetweendonorandrecipient.41,42
Liver transplantation using a split graft or a liver derived from a living donor is
associatedwithahigherriskofdevelopingananastomoticbileductstricture,becauseof
the frequent discrepancy between the diameter of the hepatic duct of the graft and
choledochalductintherecipient.Inaddition,vascularizationofthehepaticductcanbe
compromisedwhenapartialgraftisderivedfromalivingdonororsplitliver.Theseand
other surgical aspects of living-donor and split-liver transplantation are discussed in
moredetailinchapters23and24.
Management
The most frequently used therapeutic approach to an anastomotic stricture is
endoscopic balloon dilatation and stenting of the stenosis. This treatment has been
widelystudiedandisbothsafeandeffective.Technicalsuccessisobtainedin90–100%,
and long-termresolutionof thestricture in70–100%ofcases.43Althoughdisputedby
some,mostcentersobtainthebestresultswithaprotocolofprogressivestentingevery
8–12 weeks with increasing numbers and diameters of stents until resolution of the
stenosisisobtained.44Insomecases,thestenosisrecursdespiteeffectiveinitialtherapy.
Somecentershaveusedacoveredexpandablemetal stent to treata refractorybiliary
stenosisaftertransplantation.This,however,isnotroutinepractice.Presentationofan
anastomotic stricture more than 6 months after transplantation and previous bile
leakageatthesiteoftheanastomosisareriskfactorsfordifficult-to-managestrictures.40
When an anastomotic stenosis does not respond to repeated dilatation and stenting,
surgical revision or conversion to a Roux-en-Y hepatico-jejunostomy anastomosis is a
good alternative with excellent long-term success.40 Incidentally, narrowing at the
anastomosis can be detected while it remains unclear whether this is a clinically
relevantstricture.Insuchcases,ashorttrialofstentingcanbeofvalue.45
In the presence of a hepatico-jejunostomy, where the anastomosis is not easily
accessiblebyendoscopy,percutaneoustranshepatictreatmentbyballoondilatationand
temporarystentingisusuallysuccessful.Thisapproachcanalsobeusedaftersplit-liver
orliving-donorlivertransplantation,althoughresultsarenotasgood,possiblybecause
compromised microvascularization and local ischemia are more frequently the
underlyingcause.43,46
4.3Post-transplantcholangiopathy
The term post-transplant cholangiopathy coversmultifocal biliary abnormalities after
liver transplantation that include NAS, intraductal sludge and casts, and bile duct
necrosiswithintrahepaticleakageandbilomaformation.4Thesebileductabnormalities
represent different aspects of the post-transplant cholangiopathywith necrosis of the
bileductwallandsubsequentleakageofbileintotheliverparenchymabeingthemost
severesideofthespectrum.Othertermsusedinliteraturethatattempttodescribepost-
transplant biliary abnormalties are ischemic-type biliary lesions (ITBL) and ischemic
cholangiopathy. Yet the term post-transplant cholangiopathy is preferred since the
pathogenesisisbelievedtobemultifactorialandcannotalwaysbeidentified.
4.3.1Non-anastomoticstrictures
Pathogenesisandclinicalpresentation
NAS are strictures at any location in the donor bile duct other than the anastomosis.
Biliarystricturesmaybeconfinedtothehepaticbifurcation,butmayalsopresentasa
morediffusetypeincludingnarrowingofthemoreperipheralbileductsintheliver.This
typeofbileductstricturesisregardedasthemosttroublesomebiliarycomplicationas
thestricturesareoftenresistanttotherapyandoneofthemostfrequentindicationsfor
retransplantatie.43,47Asstatedbefore,NAScanbeaccompaniedbyintraductalsludgeor
cast formation. The clinical presentation of patients with NAS is often not specific;
symptomsmay include fever due to cholangitis, abdominal complaints, and increased
cholestaticliverfunctiontests,eitherwithorwithoutclinicaljaundice.
The reported incidence of NAS after liver transplantation varies between different
studies, ranging from1–20%,5,22,23which can partly be explained by variations in the
definitionofNASusedindifferentstudies.AbouthalfofallNASoccurwithin1yearafter
transplantation, and the remainder can be detected up to several years after
transplantation.43,47 In liversobtained fromDCDdonors, the incidenceofNAS isabout
10%higherandtheymayoccurearlierthaninliversobtainedfromDBDdonors.41,45
Knowledge about the pathogenesis of NAS is slowly emerging from clinical and
experimentalstudies.Severalriskfactorsforthistypeofbiliarycomplicationhavebeen
identified, strongly suggesting a multifactorial origin. In general, the mechanisms
underlying NAS can be grouped into three categories: 1) preservation or ischemia
related damage to the bile duct wall without sufficient regeneration of the biliary
epithelium 2) cytotoxic injury induced by hydrophobic bile salts, and 3) immune-
mediatedinjury.
These pathological mechanisms contribute, whether simultaneously or not, to
disastrous damage of the biliary epithelium. Generally, in case of epithelial loss,
cholangiocytesproliferateinanattempttorepopulatethedecayedepithelium.However,
ifthedamageisdetrimentaltoalmostallcholangiocytes,thismechanismalonecannot
restoretheintegrityofthebileduct.Asasecondrepairmechanism,stemcellssituated
in the peribiliary glands are activated to proliferate and differentiate and thereby
restoretheepitheliallining.48Thesestemcellsareresistanttoischemiaandresideinthe
bileductwallgroupedtogetherinsmallislets,theperibiliaryglands.49Inprogressionto
post-transplant cholangiopathy, also this resource of new cholangiocytes falls short,
whichmakestheuncoveredandunprotectedbileductwallsusceptibleforintrusionof
toxicbilesaltsandinfections.DamagetothePVPduetoischemiaandhistologicalinjury
totheperibiliaryglandshavebeenassociatedwiththedevelopmentofNAS.50Thelack
of adequate supply of oxygen and nutrients in this case could explain the poor
regeneration by the peribiliary glands. However, further studies are required to
understandwhy this secondmechanism tends to fail in course of biliary strictures or
otherbiliarycomplications.
Inone large clinical study inwhichpatientswere groupedbasedon the time interval
between transplantation and the occurrence of NAS, it was suggested that ischemia-
mediatedmechanisms aremainly responsible for the development of NASwithin the
first year after transplantation, whereas immune-mediated mechanisms play a more
importantroleinthepathogenesisofstricturesoccurringbeyondthefirstyear.9
The high incidence of post-transplant cholangiopathy after DCD liver transplantation
andtheradiologicsimilaritiesbetweenthebileductabnormalitiesofNASandbileduct
abnormalities seen in the presence of hepatic artery thrombosis strongly suggest an
ischemicfactorintheoriginofthesestrictures.Therelevanceofadequatebloodsupply
and the impact of ischemia on the bile ducts have been discussed in more detail in
paragraph2.1(Organprocurementandpreservation).
Anotherrelevantfactorinthepathogenesisofpost-transplantcholangiopathyistoxicity
caused by hydrophobic bile salts. Hydrophobic bile salts have potent detergent
propertiestowardscellularmembranesofhepatocytesandbiliaryepithelialcells.Under
physiological circumstances the toxic effects of bile salts are prevented by complex
formationwithphospholipidsandcholesterol(mixedmicelle).However,earlyafterliver
transplantation,thebalanceinbiliaryexcretionofthesethreecomponentsisdisturbed,
leading to the formation of more toxic bile.7 Evidence for a pivotal role of bile salt-
mediated toxicity in the pathogenesis of bile duct injury and subsequent bile duct
stricturing has gradually emerged during the last decade. Both experimental animal
studiesandclinical studieshavedemonstrated thatbiliarybile salt toxicityearlyafter
transplantationisassociatedwiththedevelopmentofmicroscopicaswellmacroscopic
bileduct injury.7Bilesalt toxicityactssynergisticallywith ischemia-mediatedinjuryof
thebiliaryepitheliumwithoutsufficientregeneration.8
Inthisview,nontoxichydrophilicbilesalts(e.g.ursodeoxycholicacid)mayhavepositive
effectsontheincidenceofpost-transplantcholangiopathy.Inarandomizedclinicaltrial,
administrationofursodeoxycholicacidearlyafterDCDtransplantationdidnotdecrease
theincidenceofNAS.Interestingly,however,biliarysludgeandcastswheresignificantly
diminished within the first year postoperative.51 More (large) studies are needed to
confirm a positive effect of administration of nontoxic bile salts to liver transplant
recipientsonpost-transplantcholangiopathy.
Several studies have provided evidence for an immunologic component in the
pathogenesisofNAS.NAShavebeenassociatedwithvariousimmunologicallymediated
processes,suchasABO-incompatiblelivertransplantation,pre-existingdiseaseswitha
presumed autoimmune component (such as primary sclerosing cholangitis and
autoimmunehepatitis), cytomegalovirus infection, chronic rejection,and finallywitha
geneticpolymorphisminoneoftheCCchemokinereceptors.21
Management
Incontrasttoanastomoticstrictures,NASaremuchmoreheterogeneousinlocalization
andseverity.General recommendationsregardingmanagementarehard tomake,and
good-quality prospective studies are rare. In the case of diffuse and severe biliary
strictureswithprogressivejaundiceandbacterialcholangitisorbiliaryfibrosis,usually
re-transplantationisthemostfavorableoption.Inmostpatients,thestricturesaremore
localizedandcirrhosishasnotyetdeveloped.Manycasesareamenable toendoscopic
therapy. In endoscopic therapy, repeated endoscopies with balloon dilatation and
multiple stents are used. With this approach, success rates are 50–75%.41 As in
anastomoticstrictures,PTCcanbeusedwhenendoscopicaccessisnotfeasible.Incase
ofNASthatareconfinedtotheextrahepaticbileducts,surgicalresectionofthediseased
part and construction of a hepatico-jejunostomy should be considered. In case of
recurrent cholangitis, maintenance antibiotics may result in long-term relief of
symptoms.Althoughwidelyused,thereisnoclinicalevidencethatsupportstheuseof
ursodeoxycholicacid.
Whilemost typesofbiliary complicationscanusuallybemanagedsuccessfully (either
surgically or by endoscopic techniques) or run a self-limiting course, NAS remain the
most challenging typeofbiliary complication, as theyare frequently therapy resistant
and frequently associated with long-term sequelae. Up to 50% of patients with NAS
eitherdieorrequireretransplantation.Mortalityratesdiffermarkedlyamongstudies.23
4.3.2Biliarycastsandsludge
BiliarycastsandsludgearefrequentlyfoundincompanyofNASandcanbeconsidered
asasequelofbileductstricturesalthoughtheycouldalsoappear independentlyor in
combination with other pathologies. Casts and sludge present as filling defects on
cholangiography. Sludge is a viscous collection of mucus, calcium bilirubinate, and
cholesterol. When left untreated, biliary casts can develop. Casts consist of retained
lithogenicmaterialmorphologicallyconfinedtobileductdimensions.Biliarysludgeand
caststendtooccurwithinthefirstyearaftertransplantation.
Multiple factors may contribute to sludge and/or cast formation, including ischemia,
infection,andpreservationinjury.5Theoretically,anythingthatincreasestheviscosityof
bile or reduces bile flow can predispose to casts or sludge. It is likely that ischemia
contributestotheformationofcastsorsludgeboththroughstasisofbile(asaresultof
strictures)andthroughitsdirectinjurytothebiliaryepithelium,resultingintherelease
ofcelldebrisintothebileductlumenaswellasincreasingtheepithelialsusceptibilityto
precipitationof lithogenicmaterials.Otherpathogenic factors thatareassociatedwith
casts or sludge arebiliary cholesterol content, bacterial infection in relation to stents,
thepresenceofahepatico-jejunostomy,fungalinfectionsandtheuseofcyclosporine.23
Regardlessofthecauseofcastsorsludgeaftertransplantation,anincidenceof5.7%was
reportedinthelargeststudysofar,including1650transplantedlivers.52
Mostpatientswithbiliarycastsand/orsludgepresentwithcholangitisandonlyasmall
percentagepresentwithabdominalpain.Despitetherelativeinfrequency,studieshave
shown an increased rate ofmorbidity andmortality as a result of biliary sludge and
casts,whichhavecausedrecurrentcholangitis,repeatedneedforsurgery,graftloss,and
death.53
Intraductal casts and sludge of the biliary tree can almost universally be managed
successfullybyendoscopic removal.However, the long-termsuccessof this treatment
willdependontheunderlyingcause. If the formationofcastsorsludge iscausedbya
localobstructionsuchasabiliarydrainorananastomoticstricturethatcanbetreated
successfully,removaloftheobstructionmaybecurative.However,whenbiliarycastsor
sludge are a symptom of ischemic bile duct injury, the severity of the latter will
determinethelong-termsuccessofcastremovalandwilldeterminethefateofthegraft.
4.4Biliaryabnormalitiesduetohepaticarterystenosisorthrombosis
HATis themostcommonandseriousvascularcomplicationwithareported incidence
that varies between 2% to 11%.54,55 More detailed information regarding vascular
complications can be found in chapter 31, however, we will cover shortly the main
impactonthepost-transplantbileductinthischapter.Toobtainasufficientamountof
oxygenandnutrients,thebiliarytreereliesonbloodsupplyfromthehepaticarteryand
the arterial branches of the gastroduodenal artery. These arteries continue in a fine
vascular network encircling the bile duct, called the peribiliary vascular plexus. After
transplantation,blood supply to thebileductsdependsentirelyon thehepatic artery.
Accordingly,incaseofHAT,thebileductexperienceswidespreadischemia,whichmay
resultinnecrosisandeventuallybileleakage.HATcanbedividedin2categories:early
HATandlateHAT,withthetimeframeusedinliteraturevaryingbetween2weeksand
100daysafter transplantation.56,57Whereas lateHATmayhavea relativemildcourse
due to the formation of vascular collaterals, earlyHAT is associatedwithwidespread
biliary ischemia and subsequent necrosis and bile leakage. Nevertheless, biliary
complicationsmayresult lateafterthediagnosisofHATandsuccessfulrestorationsof
arterialflowtotheliver.
4.5Biliarystricturesduetorecurrentdisease
Recurrent primary sclerosing cholangitis (PSC) may be another cause of biliary
strictures occurring late (>6–12 months) after transplantation. A large retrospective
multicenteranalysisevaluatingtheincidenceofbiliarystricturesafterOLTinacohortof
PSC patients reported an incidence of 36.1%.58 This is approximately 3.5-fold higher
thaninnon-PSCpatients.Moredetailedinformationregardingrecurrentdiseasesofthe
bileductcanbefoundinchapter36.
4.6Bacterialcholangitis
Bacterial cholangitis is not uncommon in immunosuppressed liver transplant patients
andcanresultinalifethreateningillness.Ingeneral,theriskofcholangitisisincreased
in patients in whom a T-tube is used, in patients who underwent a hepatico-
jejunostomy,andinpatientscomplicatedbyanastomoticorNAS.Alloftheseconditions
mayfacilitateascendingmigrationofbacteriaintothebiliarytree.Whenabiliarydrain
ispresent,positivebacterialculturesfromthebilemaysupportthediagnosis,although
it should be noted that colonization of bile is not infrequent. In other patients the
diagnosischolangitisisrarelysupportedbypositivebileculturesandusuallymadeafter
exclusion of other causes of fever. Bacterial cholangitis after liver transplantation
usuallypresentswithhighfeverwithorwithoutchills incombinationwithcholestatic
liver function test.Management of acute cholangitis after transplantation is similar to
thatrecommendedtonontransplantpatientsandshouldincludeappropriateantibiotic
therapyaftertheexclusionofananatomicalcause(e.g.anastomoticstrictures).
5.Summary
Biliary complications are a frequent cause of morbidity after liver transplantation.
Advancesinsurgicaltechniquesandpreservationmethodsduringthelastdecadeshave
ledtobetterresults,butbiliarycomplicationsstilloccurin10–40%oftherecipientsand
are associatedwithmortality rates of 8–15%. Partial liver grafts (e.g. split livers and
livers from living donors) as well as livers from extended-criteria donors (e.g. DCD
donors)areassociatedwitharelativelyhighriskofbiliarycomplications.Ofallbiliary
complications, bile duct strictures and bile leakage are most common after liver
transplantation.Whilebile leakageandanastomoticbileductstricturescanusuallybe
managedsuccessfullywithout long-termsequelae,NASarethemost troublesometype
of biliary complications. NAS are often multifocal and can be difficult to treat by
endoscopic techniques. When associated with recurrent cholangitis, jaundice or even
secondary biliary fibrosis, retransplantation may be the only treatment option left.
Future studies should focusonbetterdefining themechanismunderlyingNASandon
the development of effective preventive measures. In this respect, development and
potential implementation in liver transplant protocols of machine preservation is of
greatrelevance.
References
1. Op den Dries S, Sutton ME, Lisman T, et al. Protection of bile ducts in livertransplantation:lookingbeyondischemia.Transplantation2011;92:373–379.
2. SeehoferD,EurichD,Veltzke-SchliekerW,etal.Biliarycomplicationsafter livertransplantation:oldproblemsandnewchallenges.AmJTransplant2013;13:253–265
3. KarimianN,WesterkampAC,PorteRJ.Biliarycomplicationsafterorthotopiclivertransplantation.CurrentOpinioninOrganTransplantation.2014;19(3):209-216.
4. de Vries Y, von Meijenfeldt FA, Porte RJ. Post-transplant cholangiopathy:Classification, pathogenesis, and preventive strategies. Biochimica et BiophysicaActa(BBA)-MolecularBasisofDisease.2017;.
5. BuisCI,HoekstraH,VerdonkRC,PorteRJ.Causesandconsequencesofischemic-type biliary lesions after liver transplantation. J Hepatobiliary Pancreat Surg2006;13:517–24.
6. DubbeldJ,HoekstraH,FaridWRR,etal.Similarlivertransplantationsurvivalwithselectedcardiacdeathandbraindeathdonors.BrJSurg2010;97:744–53.
7. Buis CI, Geuken E, Visser DS, et al. Altered bile composition after livertransplantation is associated with the development of nonanastomotic biliarystrictures.JHepatol2009;50:69–79.
8. HoekstraH,PorteRJ,TianY,etal.Bilesalttoxicityaggravatescoldischemicinjuryof bile ducts after liver transplantation in Mdr2+/−mice. Hepatology 2006;43:1022–31.
9. BuisCI,VerdonkRC,vanderJagtEJ,etal.Nonanastomoticbiliarystricturesafterliver transplantation, part 1: Radiological features and risk factors for early vs.latepresentation.LiverTranspl2007;13:708–18.
10. CaneloR,HakimNS,RingeB.Experiencewithhystidinetryptophanketoglutarateversus UniversityWisconsin preservation solutions in transplantation. Int Surg2003;88:145–51.
11. ShakedA.UseofTtubeinlivertransplantation.LiverTransplSurg1997;3(Suppl1):S22–3.
12. Moench C, Moench K, Lohse AW, et al. G. Prevention of ischemic-type biliarylesionsbyarterialback-tablepressureperfusion.LiverTranspl2003;9:285–9.
13. Otto G, Heise M, Thies J et al. Liver Preservation by Aortic Perfusion AloneComparedWithPreservationbyAorticPerfusionandAdditionalArterialExSituBack-Table Perfusion With Histidine-Tryptophan-Ketoglutarate Solution.TransplantDirect.2017;3(7):e183.
14. Guarrera JV,Henry SD, SamsteinB et al. Hypothermicmachinepreservation inhuman liver transplantation: the first clinical series. Am J Transplant.2010;10(2):372-81.
15. Dutkowski P, Schlegel A, de Oliveira M, et al.. HOPE for human liver graftsobtainedfromdonorsaftercardiacdeath.JHepatol.2014;60(4):765-72.
16. Guarrera JV, Henry SD, Samstein B, et al. Hypothermic machine preservationfacilitates successful transplantation of "orphan" extended criteria donor livers.AmJTransplant.2015;15(1):161-9.
17. Dutkowski P, Polak WG, Muiesan P, et al. First Comparison of HypothermicOxygenated PErfusion Versus Static Cold Storage of Human Donation AfterCardiac Death Liver Transplants: An International-matched Case Analysis. AnnSurg.2015;262(5):764-70;discussion70-1.
18. vanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusion in liver transplants donated after circulatory death. Br J Surg.2017;104(7):907-17.
19. JochmansI,FieuwsS,TiekenI,etal.TheImpactofHepatectomyTimeoftheLiverGraftonPost-transplantOutcome.AnnalsofSurgery.2017;:1.
20. Hertl M, Howard T, Lowell J, et al.. Changes in liver core temperature duringpreservation and rewarming in human and porcine liver allografts. LiverTransplantationandSurgery.1996;2(2):111-117.
21. DavidsonBR,RaiR,KurzawinskiTR,etal.Prospectiverandomizedtrialofend-to-end versus side-to-side biliary reconstruction after orthotopic livertransplantation.BrJSurg1999;86:447–52.
22. Wojcicki M, Milkiewicz P, Silva M. Biliary tract complications after livertransplantation:areview.DigSurg2008;25:245–57.
23. Verdonk RC, Buis CI, Porte RJ, Haagsma EB. Biliary complications after livertransplantation:areview.ScandJGastroenterol2006;243(Suppl):89–101.
24. BennetW,ZimmermanMA,CampsenJ,etal.CholedochoduodenostomyisasafealternativetoRoux-en-Ycholedochojejunostomyforbiliaryreconstructioninlivertransplantation.WorldJSurg2009;33:1022–5.
25. SotiropoulosGC,SgourakisG,RadtkeA,etal.Orthotopiclivertransplantation:T-tube or not T-tube? Systematic review and meta-analysis of results.Transplantation2009;87:1672–80.
26. RiedigerC,MüllerM,MichalskiCetal.T-tubeornoT-tubeinreconstructionofthebiliarytractduringorthotopiclivertransplantation-systematicreviewandmeta-analysis.LiverTransplantation.2010;16(6):705-17.
27. SunN,Zhang J,LiX,etal.Biliary tract reconstructionwithorwithoutT-tube inorthotopic liver transplantation: a systematic review andmeta-analysis. ExpertRevGastroenterolHepatol.2015;9(4):529-538.
28. PoraykoMK,KondoM,Steers JL.Livertransplantation: latecomplicationsof thebiliarytractandtheirmanagement.SeminLiverDis1995;15:139–55.
29. St Peter S, Rodriquez-Davalos MI, Rodriguez-Luna HM, Harrison EM, Moss AA,Mulligan DC. Significance of proximal biliary dilatation in patients withanastomoticstricturesafterlivertransplantation.DigDisSci2004;49:1207–11.
30. Kok T, Van der Sluis A, Klein JP, et al. Ultrasound and cholangiography for thediagnosis of biliary complications after orthotopic liver transplantation: acomparativestudy.JClinUltrasound1996;24:103–15.
31. Boraschi P, Donati F, Gigoni R, et al. MR cholangiography in orthotopic livertransplantation:sensitivityandspecificityindetectingbiliarycomplications.ClinTransplant2009;24:E82–7.
32. den Dulk A, Wasser M, Willemssen F et al. Value of Magnetic ResonanceCholangiopancreatography in Assessment of Nonanastomotic Biliary StricturesAfterLiverTransplantation.TransplantDirect.2015;1(10):e42
33. ChahalP,BaronTH,PoteruchaJJ,etal.Endoscopicretrogradecholangiographyinpost-orthotopiclivertransplantpopulationwithRoux-en-Ybiliaryreconstruction.LiverTranspl2007;13:1168–73.
34. Kawano Y, Mizuta K, Hishikawa S, et al. Rendezvous penetrationmethod usingdouble-balloon endoscopy for complete anastomosis obstruction ofhepaticojejunostomy after pediatric living donor liver transplantation. LiverTranspl2008;14:385–7.
35. RighiD, Franchello A, Ricchiuti A, et al. Safety and efficacy of the percutaneoustreatment of bile leaks in hepaticojejunostomy or split-liver transplantationwithoutdilatationofthebiliarytree.LiverTranspl2008;14:611–5.
36. Kurzawinski TR, Selves L, Farouk M, et al. Prospective study of hepatobiliaryscintigraphy and endoscopic cholangiography for the detection of early biliarycomplicationsafterorthotopiclivertransplantation.BrJSurg1997;84:620–3.
37. Lopez-AndujarR,OronEM,CarregnatoAF,etal.T-tubeornoT-tubeincadavericorthotopiclivertransplantation:theeternaldilemma:resultsofaprospectiveandrandomizedclinicaltrial.AnnSurg2013;258(1):21-9
38. Morelli J, Mulcahy HE, Willner IR, et al. Endoscopic treatment of post-livertransplantation biliary leaks with stent placement across the leak site.GastrointestEndosc2001;54:471–5.
39. ShuhartMC,KowdleyKV,McVicar JP, et al. Predictors of bile leaks after T-tuberemovalinorthotopiclivertransplantrecipients.LiverTransplSurg1998;4:62–70.
40. Verdonk RC, Buis CI, Porte RJ, et al. Anastomotic biliary strictures after livertransplantation:causesandconsequences.LiverTranspl2006;12:726–35.
41. Jagannath S, Kalloo AN. Biliary complications after liver transplantation. CurrTreatOptionsGastroenterol2002;5:101–12.
42. Bourgeois N, Deviere J, Yeaton P, et al. Diagnostic and therapeutic endoscopicretrograde cholangiography after liver transplantation. Gastrointest Endosc1995;42:527–34.
43. SharmaS,GurakarA,JabbourN.Biliarystricturesfollowinglivertransplantation:past,presentandpreventivestrategies.LiverTranspl2008;14:759–69.
44. Zoepf T, Maldonado-Lopez EJ, Hilgard P, et al. Balloon dilatation vs. balloondilatation plus bile duct endopros-theses for treatment of anastomotic biliarystricturesafterlivertransplantation.LiverTranspl2006;12:88–94.
45. Cantu P, Tenca A, DonatoMF, et al. ERCP and short-term stent-trial in patientswith anastomotic biliary stricture following liver transplantation. Dig Liver Dis2009;41:516–22.
46. Gomez CM, Dumonceau JM, Marcolongo M, et al. Endoscopic management ofbiliary complications after adult living-donor versus deceased-donor livertransplantation.Transplantation2009;88:1280–5.
47. OpdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsandvascular plexus before liver transplantation predicts formation of non-anastomoticbiliarystrictures.JHepatol2014;60:1172-1179.
48. De Jong IEM, Matton APM, van Praagh JB, et al. Peribiliary glands are key inregeneration of the human biliary epithelium after severe bile duct injury.Hepatology2018;doi:10.1002/hep.30365
49. DeJongIEM,vanLeeuwenOB,LismanT,etal.Repopulatingthebiliarytreefromtheperibiliaryglands.BiochimBiophysActaMolBasisDis2018;1864:1524-31
50. VerdonkRC,BuisCI,vanderJagtEJ,etal.Nonanastomoticbiliarystricturesafterliver transplantation,part2:Management, outcome, and risk factors fordiseaseprogression.LiverTranspl2007;13:725–32.
51. WangS,TangH,ChenG,etal.Effectofursodeoxycholicacidadministrationafterlivertransplantationonserumlivertestsandbiliarycomplications:arandomizedclinicaltrial.Digestion2012;86:208-217.
52. ShengR,RamirezCB,ZajkoAB,CampbellWL.Biliarystonesandsludgeinlivertransplantpatients:a13-yearexperience.Radiology1996;198:243–7.
53. Shah JN, Haigh WG, Lee SP, et al. Biliary casts after orthotopic livertransplantation: clinical factors, treatment, biochemical analysis. Am JGastroenterol2003;98:1861–7.
54. Duffy JP, Hong JC, Farmer DG, et al. Vascular complications of orthotopic livertransplantation: experience in more than 4,200 patients. J Am Coll Surg2009;208:896-905
55. PropositoD,LoinazSegurolaC,GarciaGarcìaI,etal.Assessmentofriskfactorsinthe incidence of hepatic artery thrombosis in a consecutive series of 687 livertransplantations[inItalian].AnnItalChir2001;72:187-205
56. Bekker J, Ploem S, de Jong KP. Early hepatic artery thrombosis after livertransplantation: a systematic reviewof the incidence, outcome and risk factors.AmJTransplant2009;9:746-57
57. Abbasoglu O, Levy MF, Testa G, et al. Does intraoperative hepatic artery flowpredict arterial complications after liver transplantation? Transplant1998;66:598-601
58. YangY,ZhaoJC,YanLN,etal.RiskfactorsassociatedwithearlyandlateHATafteradultlivertransplantation.WorldJGastroenterol2014;20:10545-52.
Donorhepatectomytimeinfluencesischemia-reperfusioninjuryofthebiliarytreeindonationaftercirculatorydeathlivertransplantation
OttoB.vanLeeuwen,MarjoleinvanReeven,DannyvanderHelm,JanN.M.Ijzermans,VincentE.deMeijer,AadP.vandenBerg,SarwaDarwishMurad,BartvanHoek,IanP.Alwayn,RobertJ.Porte,WojciechG.PolakSurgery.2020(inpress)
3
ABSTRACT
Background: Donor hepatectomy time is associated with graft survival after liver
transplantation.Theaimofthisstudywastoidentifytheimpactofdonorhepatectomy
timeonbiliaryinjuryduringdonationaftercirculatorydeathlivertransplantation(DCD-
LT)
Methods:First,bileductbiopsiesof livers included in (pre)clinicalmachineperfusion
researchwereanalyzed.Secondly,ofthesamelivers,bilesampleswerecollectedduring
normothermic machine perfusion (NMP). Lastly, a nationwide retrospective cohort
studywasperformedincluding273adultpatientsundergoingDCD-LTbetween01-01-
2002 and01-01-2017. Primary endpointwasdevelopment of non-anastomotic biliary
strictures (NAS) within two years of DCD-LT. Cox Proportional-Hazards regression
analyseswereusedtoassesstheinfluenceofhepatectomytimeondevelopmentofNAS.
Results: Livers with severe histological bile duct injury had a higher median
hepatectomy time (p=0.03). During NMP, livers with hepatectomy time >50min had
lower biliary bicarbonate and bile pH levels. In the nationwide retrospective study,
donorhepatectomytimewasanindependentriskfactorforNASafterDCD-LT(HR1.18
pertenminutesincrease,95%CI1.06-1.30,p-value=0.002).
Conclusions:Donorhepatectomytimenegativelyinfluenceshistologicalbileductinjury
prior to NMP and bile composition during NMP. Additionally, hepatectomy time is a
significantindependentriskfactorforthedevelopmentofNASafterDCD-LT.
INTRODUCTION
The imbalance between the number of patients on the waiting list for liver
transplantation(LT)andthenumberofavailablegraftsfromdonationafterbraindeath
(DBD)donorshasresultedinanincreaseduseofliversfromdonationaftercirculatory
death (DCD) donors. In 2018, 38%of all deceased donor LT in theNetherlandswere
performedwithaDCDgraft1.
LT fromDCD donors can lead to inferior outcomes compared to LTwith DBD grafts,
especially with respect to graft survival 2-5, which is related to a higher chance of
developing early allograft dysfunction and post-transplant cholangiopathy 6-10. Among
post-transplant cholangiopathies, non-anastomotic strictures (NAS), also known as
ischemic type biliary lesions (ITBL) or ischemic cholangiopathy (IC), is the most
hazardoustype,withastrongnegativeimpactongraftsurvival11-13.
AnimportantdeterminantofoutcomeafterLTisischemiareperfusioninjury(IRI).IRI
occursinbothDBDandDCD-LT.However,DCDgraftssufferfromanadditionalperiod
ofwarmischemiainthedonorbetweenwithdrawaloflifesupportandinitiationofcold
flush out, the so called donor warm ischemia time (dWIT). Several studies have
indicatedthatthelengthofthedWITisacriticalriskfactorfornegativeoutcomeafter
DCD-LT2,14,15.
Unfortunately, thestartof in situ cold flushoutandcoolingdoesnot lead toadequate
protectionagainst ischemic injury,becausethecoretemperatureof the livergenerally
does not drop below 15-20oC during surgery16. At this temperature, organs are still
metabolically active, resulting in rapid depletion of adenosine tri-phosphate and
accumulationofmetabolitesduringanaerobicmetabolism.Livercoretemperaturefirst
reachesarelativelysafetemperature(<4oC)whenorgansarestoredinabagwithcold
preservationsolutioninaboxwithice.Therefore,itishypothesizedthat,apartfromthe
dWIT, the duration of the hepatectomy time provides an additional risk factor for
ischemicinjuryandcouldthereforeimpactoutcomeafterLT.
A recent study published by Jochmans et al. based on data from the Eurotransplant
Registry supported this hypothesis17. In this study, donor hepatectomy time was an
independent risk factor for patient mortality and graft loss. Moreover, DCD grafts
appeared to bemore susceptible to donor hepatectomy time than DBD grafts. More
recently, Farid et al. assessed the influence of the donor hepatectomy time on the
outcomes of DCD-LT in the United Kingdom, concluding that a hepatectomy time of
more than60minuteswas associatedwith ahigher riskof primarynon function and
graftfailure18.Neitherstudy,however,didassesstheeffectofdonorhepatectomytime
on the development of post-transplant cholangiopathy after DCD-LT, neither did they
evaluatewhetherhepatectomytimewasdifferentamongprocurementteams.
Several studies have shown a strong relation between bile duct injury prior to
implantation and the development of NAS after transplantation19, 20. If donor
hepatectomytimeinfluencestheratesofNAS,thiswouldbedisplayedintheseverityof
biliaryinjurypriortoimplantation.Additionally,bilecompositionduringnormothermic
machineperfusion(NMP)oflivergraftscanbestudiedtoassessbileductinjury21,22.
TheaimofthisstudywastoassesstheimpactofdonorhepatectomytimeinDCDdonors
onthedevelopmentofbiliaryinjuryduringDCD-LT.First,bileductbiopsiestakenupon
arrival in one of the three recipient centers are analyzed. Secondly, bile composition
duringNMP isstudied.Last, the influenceofhepatectomytimeon thedevelopmentof
NASafterDCD-LTisstudiedinanationwideretrospectivedatabasestudy.
METHODS
Donationprocedureandorganprocurement
Untilrecently,alldonorprocedures/procurementsintheNetherlandswereperformed
byoneoffiveregionalprocurementteams,eachcoveringacertainregionofthecountry.
Each procurement team consists of a surgeon, surgical assistant, anesthesiologist and
two operation room assistants. In the Netherlands, withdrawal of life support in a
patienteligibleforDCDorgandonationgenerallytakesplaceattheintensivecareunit.
Pre-mortemcannulationofthepatientisnotperformed,andsystemicheparinizationis
prohibited by Dutch law. When circulatory arrest has been determined, there is a
mandatory five minutes ‘no-touch’ period. After this ‘no-touch’ period, the donor is
transportedtotheoperatingtheatre.Asuper-rapidsterno-laparotomywithpressurized,
aortic-only perfusion is used as standard perfusion technique. Cold perfusion is
currentlyexecutedwithBelzerUniversityofWisconsincoldstoragesolution(Bridgeto
Life, London,UK) (UW).Whether the liver is retrieved separately or en-blocwith the
pancreas is based on the preferences of the surgeon. On the back table, the liver is
flushed via the portal veinwith at least 500ml cold preservation solution until clear
perfusate is established. The CBD and intrahepatic biliary tree are flushed with low
pressure UW 23. As there are no clear Dutch guidelines on the sequence of organ
procurement, the lungs in a DCD donor are usually procured before the abdominal
organs. The implantation is usually executedwith a caval sideclampand veno-venous
anastomosis, end-to-end arterial and portal anastomosis and duct-to-duct biliary
anastomosis.Thestandardreperfusiontechniqueusedisinitialportalveinreperfusion.
Studydesign
Thisstudyconsistsofthreeparts.First,bileductbiopsiesandbilecompositionofDCD
liverswereanalyzedforapotentialinfluenceofhepatectomytime(partA-B).Hereafter,
to validate the findings, a nationwide retrospective database analysis was performed
(partC).
PartA:Histologicalanalysisofbileducts
Of all DCD livers that underwent preclinical and clinical normothermic machine
perfusionintheUniversityMedicalCenterGroningenbetween01-01-2013and01-01-
2019,bileductbiopsiesprior tomachineperfusionwere collected.Theonly criterion
required for inclusion was that the donor hepatectomy time was available. Biopsies
were taken from the distal common bile duct beforemachine perfusion, fixed in 4%
formalin,andsubsequentlyembedded inparaffin.Slicesof4µmwerecutandstained
withHematoxylin&Eosin,andsubsequentlyexaminedusinglightmicroscopy.Thebile
ductinjury(BDI)scorewasdeterminedinablindedfashionbytworesearchers,usinga
clinicallyrelevanthistologicalgradingsystem20, 22.TheBDIconsistedofthecombined
scores for deep peribiliary gland injury, peribiliary vascular plexus injury and stroma
necrosis. The used cut-off value between low and high BDI was 4.75, as described
previously22.ComparisonsbetweengroupswereperformedwiththeChi-Squaretest,or
Fisher’sExact testwhere appropriate.ROC (ReceiverOperatingCharacteristic) curves
wereusedtoidentifymostappropriatecut-offvalues.
PartB:Normothermicmachineperfusion
AllpreclinicalandclinicalNMPprocedureswereperformedwiththeLiverAssistdevice
(Organ Assist, Groningen, the Netherlands). Protocols and outcomes are reported
elsewhere22,24,25.Tomonitorbiliarytreeviability,bilewascollectedfroma8Frbiliary
drain in the common bile duct. During NMP, bile samples were collected every 30
minutes undermineral oil to determine biliary pH, bicarbonate and glucose, as these
parameters are biomarkers of bile duct viability 22. Bile composition was compared
betweenthegroupsatdifferenttimepointsusingtheMann-Whitneytest.
PartC:Retrospectivenationwidestudy
Inthisnationwide,retrospectivecohortstudy,alladultLTperformedwithaDCDgraft
in the Netherlands between 01-01-2002 and 01-01-2017 were included. Exclusion
criteria were multi organ DCD transplants, DCD retransplantations, transplantations
involvingmachineperfusionandprocurementofDCDgraftsbya foreignprocurement
team. Additionally, cases with missing information on hepatectomy times or donor
agonalphasewereexcluded.Donorcharacteristicsandinformationontheprocurement
procedure and the regional procurement team were obtained via the Donor Data
Application of Eurotransplant. Data of recipients and transplantation outcomes were
obtained fromthedatabasesof theparticipatingcenters, completedwithmissingdata
fromtheelectronicalpatients’medicalrecords.
Donorhepatectomytimewasdefinedastheperiodbetweenthestartofcoldflushinthe
donorandthestorageoftheliverinabowlwithcoldpreservationfluidandmeltingice
on the back-table. The dWIT was calculated as the time between withdrawal of life
support and cold flush in the donor. Since in the normal situation the donor
hepatectomytime ispartof thecold ischemia time, thedefinitionof thecold ischemia
timehasbeenaltered tominimize the chanceof confounding; cold ischemia timewas
definedastheperiodbetweentheendofthedonorhepatectomyandtheremovalofthe
liverfromicepriortoimplantation.Finally,recipientwarmischemiatimewasdefined
as the time between removal of the liver from ice until either portal or arterial
reperfusion,whichevercamefirst.
TheendpointoftheretrospectivestudywasthedevelopmentofNASwithintwoyears
aftertransplantation.NASwasdefinedasdonorbileductstricturesatanylocationbut
theanastomosis,inabsenceofhepaticarterythrombosis.Tomeettheendpoint,patients
wererequiredtohaveclinicalsymptomsofcholestasis(e.g.jaundice,itch,elevatedtotal
bilirubin)withsubsequentimagingdemonstratingbileductstrictures.IfNASdeveloped
afterthisperiod, itwasconsideredtoberelatedtorecipientfactorsratherthandonor
factors. Univariable and multivariable Cox Proportional-Hazards regression models
wereusedtoevaluateindependentriskfactorsforNAS.Inbothmodels,subjectsthatdid
not develop NAS within two years were censored at two years post transplantation.
Patients who died or underwent retransplantation within the first two years after
transplantation were censored at their date of death or date of retransplantation,
respectively. Variables were included in the multivariable, backward stepwise, Cox
modelifunivariableCoxregressionyieldedap-value<0.20.Thethresholdof0.20was
chosentodecreasetheriskofoverfittingofthemodel.Thereportedhazardratios(HR)
for donor hepatectomy time refer to an increase of ten-minutes in hepatectomy time.
For the cold ischemia time and recipient warm ischemia time, the HR represent an
increaseofonehourandoneminute,respectively.
Inallthreeprojectsincorporatedinthisstudy,continuousvariableswerepresentedas
median with both total range and interquartile range (IQR), whereas categorical
variableswerepresentedasnumber[percentage]Alltestshadatwo-sideddesignwith
ap-valuebelow0.05consideredassignificant.TheanalyseswereperformedusingSPSS
version 24 (IBM, Chicago, Illinois). This study was approved by the Medical Ethical
CommitteeoftheUniversityMedicalCenterGroningen(METC.2017/504).
RESULTS
PartA:Histologicalanalysisofthebileduct
Of 40 consecutive normothermic machine perfusion procedures between 2014 and
2019,39bileductbiopsieswerecollected.Afterexclusionofbiopsieswithanunknown
donorhepatectomytime,27biopsieswere included in theanalysis.Liverswithahigh
bile duct injury score had a significant longer median donor hepatectomy time
compared to graftswith lowbile duct injury score (56 versus44 minutes, p = 0.03).
(Figure1A).ROC-curveanalysisshowedadonorhepatectomytimeof50.0minutesas
themost suitablecut-offpoint.Of liverswithhepatectomy time≤50.0minutes,17.0%
displayed high bile duct injury, versus 64% in livers with a hepatectomy time >50.0
minutes(p=0.01)(Figure1B).
Figure1:Hepatectomy time influencesbiliary injuryprior to transplantation. A:
Livers grafts with a high bile duct injury score had a longermedian hepatectomy time
comparedto liverswith lowbileduct injuryscore(p=0.027).Datapresentedasmedian
(IQR).B:Liversgraftswithadonorhepatectomytime>50minuteshavemoreseverebile
ductinjurycomparedtoliverswithahepatectomytime≤50minutes(p=0.016).*depicts
asignificant(p<0.050)difference.Abbreviations:BDI,bileductinjuryscore;min;minutes.
PartB:Normothermicmachineperfusion
Ofthe27 livers, liverswithahepatectomytime≤50.0minuteshadmorealkaloticbile
duringthefirstfourhoursofNMP.Subsequentlybiliarybicarbonatelevelswerehigher
in livers with a hepatectomy time below 50 minutes. (Figure 2A-B). Glucose
reabsorption,displayedbytheglucoseratiobetweenbileandperfusate,didnotseemto
besignificantlyinfluencedbyhepatectomytime(Figure2C).
Figure 2: Hepatectomy time influences bile composition during NMP. A:
Hepatectomy time influenced biliary bicarbonate levels during NMP. B: bile pH was
significantlylowerinthegroupwithhepatectomytime≤50minutes.C:hepatectomytime
didnotseemtosignificantlyinfluencebiliaryglucosereabsorption.*depictsasignificant
(p<0.050)difference.Abbreviations:BDI,bileductinjuryscore;min;minutes.
PartC:Retrospectivestudy
Atotalof376DCD-LTwereperformedintheNetherlandsbetween01-01-2002and01-
01-2017.Hundred-and-threecasesmetoneormoreoftheexclusioncriteria,resulting
ina totalof273 included in thisstudy(Figure3).Themedian followupperiodof the
complete cohort was 4.36 (IQR 2.81-7.08, range 0-16.8 years) years. Baseline
characteristicsarepresentedinTable1.Mediandonorhepatectomytimefortheentire
cohort was 63.0 (IQR 52.5-80.5, range 23-140) minutes. Lung procurement led to a
significantly longer donor hepatectomy time of 69 (IQR 59-80) minutes, when
compared toahepatectomy timeof61 (IQR49-81)minutes indonors inwhich lungs
werenotprocured (p=0.02).TheoutcomesafterDCD-LT in the complete cohort are
shown in Table 1. Actuarial one-, three-, and five-year graft survival rateswere 75%,
64%and60%,and87%,79%,and74%forpatientsurvivalrespectively.
Table1:Donorandrecipientdemographics
Characteristic Result(n=273)Donor Age(years) 47.0(35.5-54.0)
Range12-74 Gender Male 155[56.8%] Female 118[43.2%] Bodymassindex(kg/m2) 24.0(22.0-26.0)
Range13-34 CVAascauseofdeath No 151[55.3%] Yes 122[44.7%] ALTpeak(U/L) 43.0(23.0-87.0)
Range6-7385 LastγGT(U/L) 34.0(20.0-65.5)
Range4-747Procurement Donorwarmischemiatime(min)* 32.0(26.0-38.0)
Range15-80 Donorhepatectomytime(min)† 63.0(52.5-80.5)
Range23-140 Lungprocurement 84.0[30.8%]Recipient Age(years) 57.0(49.0-63.0)
Range22-70 Gender Male 197[72.2%] Female 76[27.8%] Bodymassindex(kg/m2) 25.7(23.4-29.1)
Range17-46 HCCasindicationfortransplantation No 175[64.1%] Yes 98[35.9%] LaboratoryMELDscore 14.6(10.0-21.0)
Range6-44Transplantation Coldischemiatime(min)‡ 359(302-431)
Range131-743 Recipientwarmischemiatime(min)§ 34.0(26.0-42.0)
Range17-144Outcomes ASTpeak(u/L) 2115(1165-4252)
Range129-20280 ALTpeak(u/L) 1620(771-2857)
Range162-10944
Intensivecareunitstay(days) 2.0(1.0-5.0)Range0-185
Totalhospitalstay(days) 18.0(13.0-27.0)Range0-235
Primarynon-function|| 8[2.90%] Non-anastomoticstrictures 70[25.6%] Withintwoyearspost-transplantation 66[24.2%] Hepaticarterythrombosis 14[5.10%] Actuarialgraftsurvival 1year 75% 3year 64% 5year 60% Actuarialpatientsurvival 1year 87% 3year 79% 5year 74%
Valuesarepresentedasmedian(interquartilerange)ornumber[%].*Thetimebetween
withdrawal of life support and cold flush in the donor. †Theperiod of timebetween the
startofcoldflushinthedonorandthestorageoftheliveroniceontheback-table.‡The
timebetweentheendofthedonorhepatectomyandtheremovaloftheliverfromiceprior
to implantation. §The time between removal of the liver from ice until either portal or
arterialreperfusion.||Patientdeathorretransplantationwithin7daysoftransplantation
without clear cause. Abbreviations: ALT, alanine aminotransferase; , AST; aspartate
aminotransferase, CVA , Cerebrovascular accident; γGT, gamma-glutamyl transferase;
HCC,hepatocellularcarcinoma;MELD,modelforend-stageliverdisease.
Sixty-sixpatients(24.2%)werediagnosedwithNASwithintwoyearsofLT.Duringthe
complete followup,25patientshaveundergonearetransplantationasaresultof this
complication. Baseline characteristics, stratified by recipient development of NAS are
provided in supplementary table 1. In a univariable Cox Proportional-Hazards
regression model, donor hepatectomy time was an independent risk factor for the
development ofNAS (HR1.14, 95%CI 1.03-1.26, p-value0.02).After adjusting for all
covariateswith a p-value below 0.2 in univariable analyses, donor hepatectomy time
remainedanindependentriskfactorfordevelopingNASwithinthefirsttwoyearspost-
LT (adjusted HR 1.18, 95% CI 1.06-1.30, p-value 0.002, Table 2 and 3). Besides
hepatectomy time, donor age and cold ischemia timewere significant risk factors for
NAS.
Table2:UnivariableCoxProportional-HazardsregressionmodelfordevelopingNAS
Hazardratio 95%CI p-valueDonor Age(years) 1.03 1.01-1.05 0.004 Gender Male REF Female 1.14 0.70-1.86 0.59 Bodymassindex(kg/m2) 0.99 0.92-1.08 0.88 CVAascauseofdeath No REF Yes 1.83 1.13-2.98 0.02 ALTpeak(U/L) 1.00 1.00-1.00 0.09 LastγGT(U/L) 1.00 1.00-1.00 0.41Procurement Donorwarmischemiatime(minutes)* 1.03 1.01-1.05 0.01 Donorhepatectomytime(10-minutes)† 1.14 1.03-1.26 0.02 Lungprocurement 0.60 0.34-1.06 0.08Recipient Age(years) 0.994 0.97-1.02 0.60 Gender Male REF Female 1.22 0.72-2.07 0.45 Bodymassindex(kg/m2) 1.02 0.97-1.07 0.55 HCCasindicationfortransplantation No REF Yes 0.77 0.46-1.30 0.33 LaboratoryMELDscore 0.98 0.95-1.02 0.35Transplantation Coldischemiatime(hours)‡ 1.17 1.04-1.33 0.01 Recipientwarmischemiatime(minutes)§ 1.02 1.00-1.04 0.17
Valuesarepresentedasmedian(interquartilerange)ornumber[%].*Thetimebetween
withdrawal of life support and cold flush in the donor. †Theperiod of timebetween the
startofcoldflushinthedonorandthestorageoftheliveroniceontheback-table.‡The
timebetweentheendofthedonorhepatectomyandtheremovaloftheliverfromiceprior
to implantation. §The time between removal of the liver from ice until either portal or
arterial reperfusion.Abbreviations:ALT,alanineaminotransferase;CVA, cerebrovascular
accident;γGT,gamma-glutamyltransferase;HCC,hepatocellularcarcinoma;MELD,model
for end-stage liver disease; PBC, primary biliary cirrhosis; PSC, primary sclerosing
cholangitis.
Table3:MultivariableCoxProportional-HazardsregressionmodelforNAS
Hazardratio 95%CI p-valueDonor Age(years) 1.03 1.01-1.05 0.01 CVAascauseofdeath - - 0.29 No Yes ALTPeak 1.00 1.00-1.00 0.05Procurement Donorwarmischemiatime* - - 0.50 Donorhepatectomytime† 1.18 1.06-1.30 0.002 Lungprocurement 0.47 0.26-0.84 0.01Transplantation Coldischemiatime‡ 1.22 1.08-1.38 0.001 Recipientwarmischemiatime§ - - 0.47
Multivariablemodelwasconductedviabackwardstepwiseapproach.Adash(-)indicates
thatvariablewasremovedfromthemodel.*Thetimebetweenwithdrawaloflifesupport
andcoldflushinthedonor.†Theperiodoftimebetweenthestartofcoldflushinthedonor
and the storage of the liver on ice on the back-table. ‡The time between the end of the
donorhepatectomyandtheremovaloftheliverfromicepriortoimplantation.§Thetime
between removal of the liver from ice until either portal or arterial reperfusion.
Abbreviations:ALT,alanineaminotransferase;γGT,gamma-glutamyltransferase.
DISCUSSION
This is thefirststudythatdemonstratesthe impactofdonorhepatectomytimeonthe
developmentofbiliary injuryduringandafterDCDlivertransplantation.Hepatectomy
time influences the severity of histological bile duct injury prior to transplantation.
Moreover,prolongedhepatectomytimesnegativelyinfluencedbilecompositionduring
NMP.Additionally,theretrospectivestudyindicatesthateveryten-minutesincreasein
donorhepatectomytimeleadstoan18percentincreasein,theriskofdevelopingNAS.
OpdenDriesetal.haveshownthatbileducthistologyishighlypredictiveofNASafter
livertransplantation20.Inthecurrentstudy,itisobservedthatprolongedhepatectomy
timesleadstoanincreasedBDIscore,depictingincreasedratesofdeepperibiliarygland
injury, peribiliary vascular plexus injury and stroma necrosis. The results from this
histologystudydemonstratethattheimpactofhepatectomytimeisalreadyvisibleprior
to graft reperfusion. In addition to histology, NMP can be used to assess biliary
function21,22. Similar results were observed during NMP, livers with prolonged
hepatectomytimeproducedbileofinferiorquality.
The results of the current study are roughly in line with those reported in the
EurotransplantregistrystudybyJochmansetal.andtheUKbasedstudyfromFaridand
colleagues: a prolonged donor hepatectomy time impairs the outcome of DCD-LT.
However,neitherofthestudieswereabletoassesstheinfluenceofdonorhepatectomy
time on the development of biliary complications. Surprisingly, the median donor
hepatectomytimeintheDutchcohortinthecurrentstudywassubstantiallylongerthan
thatoftheDCD-LTsubgroupinthestudyofJochmansetal.(63versus50minutes)17.As
within the Eurotransplant region, only theNetherlands, Belgium andAustria perform
DCD organ procurements, this implies that the donor hepatectomy time in the
Netherlandsissubstantiallylongercomparedtotheothertwocountries.Moreover,the
medianhepatectomytimeinourcohortwasalsoconsiderablylongerthanintheUnited
KingdomasreportedbyFaridetal.(63versus35minutes)18.Asaresultofthisfinding,
the Dutch Committee on Independent Procurement Teams implemented several
strategiestolowerthehepatectomytime,suchasraisingawarenessontheimpactofthe
donor hepatectomy time and endorsing knowledge and skill exchange between the
teams.Since2018,thishasresultedinasubstantialdecreaseofthedonorhepatectomy
time in theNetherlands (mean of 42minuteswith standarddeviation of 12minutes)
without an increase in liver injuries, highlighting the importance of training in organ
procurementandregularevaluation26.
ThegraftsurvivalratesreportedbyFaridetal.aresubstantiallyhigherthanthoseinour
cohort(1,3,and5yeargraftsurvivalrateof86.5%,80.9%and77.7%intheUKversus
75%,64%and60%intheDutchcohort,Table1).Sincethepatientsurvivalrateshave
notbeenreportedbyFaridetal.,itisnotpossibletoevaluatewhetherthehigherrateof
graft loss in the Netherlands is the result of more patient deaths or of more
retransplantations. However, it could possibly be explained by the difference in
hepatectomy time between the two cohorts. Nevertheless, it would be valuable to
thoroughlyinvestigatethissubstantialdifferenceingraftsurvivalrates.
Surprisingly, procurement of the lungs seemed to have a protective effect on the
development of NAS, despite the fact that lung procurement leads to a prolonged
hepatectomytime.Thisfindingisprobablytheresultofthestrictacceptancecriteriafor
DCDlungdonationhandledbythoracicsurgeonsandlungphysicians.Only lungsfrom
optimal DCD donors are accepted, otherwise the lungs are not procured. Lung
procurementisinthatcaseaproxyforamoreoptimaldonor.
Jochmansetal.statedthatportalperfusion,nexttostandardinsituaorticcoldflush,can
accelerate liver cooling and might prevent the detrimental effect of prolonged
hepatectomytime17.Inarecentpublishedstudy,Hameedetal.concludedthatinhigh-
risk donors DBD donors, dual perfusion is superior 27. Furthermore, Ghinolfi et al.
concluded recently that dual perfusion has a protective effect on the development of
ITBL after LT with grafts from octogenarian donors 28. However, a randomized
controlled trial comparing aortic flush only and combined aortic and portal flush in
DBD-LT, showed no difference in the incidence of post-transplant cholangiopathy 29.
SinceDCDgraftscouldalsobeconsideredashigh-riskgrafts, itwouldbe justifiableto
evaluate the effect of dual perfusion versus aortic only perfusion in the DCD-LT
population. Another method to potentially minimize the detrimental effect of both
donor warm ischemia time and hepatectomy time on the outcomes after liver
transplantation is the use of normothermic regional perfusion (NRP). A recently
publishedstudybyHessheimeretal.showedthatwiththeuseofNRPtheratesofbiliary
complicationsandgraftlosscouldbereducedsubstantiallywhencomparedtoasuper-
rapidrecovery30.
Recently,Kalisvaartetal.showedtheimportanceoftheagonalphaseoftheDCDdonor
andits influenceontheoutcomesaftertransplantation,consideringanarterialoxygen
saturation level below 80% as starting point for the functional donorwarm ischemia
time31.Unfortunately,inourcohort,dataonbloodpressuresandsaturationduringthe
agonal phasewere unavailable or improperly recorded. Therefore,wewere forced to
use another definition of the donor warm ischemia time. Since the agonal phase has
proven to be of importance, we chose to use the period between withdrawal of life
supportandtheinitiationofcoldflushingasthedWITinthisstudyratherthanthetime
betweencardiacarrestandcoldperfusion.Additionally,asshownbefore,thisstudyalso
underlinestheimportanceofashortcoldischemiatimeforDCDgrafts2232.Everyhour
ofcoldischemiawasassociatedwitha22%increasedriskofNAS.Finally,donorageis
onceagainshowntobeanimportantriskfactorforbiliarycomplications.
An importantstrengthof this study is the fact thathistologicalanalysesarecombined
withastudyofbilecompositionduringNMPandanationwideretrospectivedatabase
study. Another strength is that donor hepatectomy time is incorporated as an
continuousvariableintothemultivariablemodelratherthanasadichotomousvariable
setaroundacertaincut-offofdonorhepatectomytime.Thislatterwouldhaveledtoa
lossofvaluable information.Anotherstrongaspectof thisstudy is the follow-upofall
patients with detailed information on the development of biliary complications. One
limitationofthedatabasestudyistheretrospectivedesignandrelativelysmallcohorts.
In addition, aspartCwasused tovalidate the findings inpartAandB, these cohorts
consist of differentpatients.Moreover, in a substantial numberof cases, hepatectomy
timeand/ordonorwarm ischemia timewasmissing, leading to ahighexclusion rate.
Sincewe could not guarantee these variables to bemissing at random, imputation of
thesevariableswasnotdesirable.Wedonotsuspectthatourresultswereconfounded
bythus,howeverbiascannotentirelybeexcluded.
Inconclusion,donorhepatectomy timestrongly influencesbiliary injuryduring
and after DCD-LT. The donor hepatectomy time should be kept as short as possible,
especiallyinthepresenceofotherriskfactorssuchasanolderdonororprolongedcold
ischemiatime.
REFERENCES
1. Eurotransplant. Eurotransplant Statistics Library. www.eurotransplant.org:EurotransplantInternationalFoundation;2018.
2. Blok JJ, Detry O, Putter H, Rogiers X, Porte RJ, van Hoek B, et al. Longtermresults of liver transplantation from donation after circulatory death. LiverTranspl.2016;22:1107-14.
3. CallaghanCJ,CharmanSC,MuiesanP,PowellJJ,GimsonAE,vanderMeulenJH,et al. Outcomes of transplantation of livers from donation after circulatorydeathdonorsintheUK:acohortstudy.BMJOpen.2013;3:e003287.
4. deVeraME,Lopez-SolisR,DvorchikI,CamposS,MorrisW,DemetrisAJ,etal.Liver transplantation using donation after cardiac death donors: long-termfollow-upfromasinglecenter.AmJTransplant.2009;9:773-81.
5. GrewalHP,WillinghamDL,Nguyen J, HewittWR, TanerBC, Cornell D, et al.Livertransplantationusingcontrolleddonationaftercardiacdeathdonors:ananalysisofalargesingle-centerexperience.LiverTranspl.2009;15:1028-35.
6. Lee DD, Singh A, Burns JM, Perry DK, Nguyen JH, Taner CB. Early allograftdysfunction in livertransplantationwithdonationaftercardiacdeathdonorsresultsininferiorsurvival.LiverTranspl.2014;20:1447-53.
7. Croome KP, Lee DD, Perry DK, Burns JM, Nguyen JH, Keaveny AP, et al.Comparisonoflongtermoutcomesandqualityoflifeinrecipientsofdonationafter cardiac death liver grafts with a propensity-matched cohort. LiverTranspl.2017;23:342-51.
8. O'Neill S,RoebuckA,KhooE,WigmoreSJ,HarrisonEM.Ameta-analysisandmeta-regressionofoutcomesincludingbiliarycomplicationsindonationaftercardiacdeathlivertransplantation.TransplInt.2014;27:1159-74.
9. FoleyDP,FernandezLA,LeversonG,AndersonM,MezrichJ,SollingerHW,etal.Biliarycomplicationsafterlivertransplantationfromdonationaftercardiacdeathdonors:ananalysisofriskfactorsandlong-termoutcomesfromasinglecenter.AnnSurg.2011;253:817-25.
10. ChanEY,OlsonLC,KisthardJA,PerkinsJD,BakthavatsalamR,HalldorsonJB,etal.Ischemiccholangiopathyfollowinglivertransplantationfromdonationaftercardiacdeathdonors.LiverTranspl.2008;14:604-10.
11. Buis CI, Hoekstra H, Verdonk RC, Porte RJ. Causes and consequences ofischemic-type biliary lesions after liver transplantation. J HepatobiliaryPancreatSurg.2006;13:517-24.
12. Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, et al.Nonanastomotic biliary strictures after liver transplantation, part 2:Management,outcome,andriskfactorsfordiseaseprogression.LiverTranspl.2007;13:725-32.
13. de Vries Y, von Meijenfeldt FA, Porte RJ. Post-transplant cholangiopathy:Classification, pathogenesis, andpreventive strategies. BiochimBiophysActaMolBasisDis.2018;1864:1507-15.
14. KalisvaartM,SchlegelA,Umbro I,deHaan JE,Scalera I,PolakWG,etal.TheImpact of CombinedWarm Ischemia Time onDevelopment of Acute KidneyInjuryinDonationAfterCirculatoryDeathLiverTransplantation:StayWithintheGoldenHour.Transplantation.2018;102:783-93.
15. TanerCB,BulataoIG,PerryDK,SibuleskyL,WillinghamDL,KramerDJ,etal.Asystoletocross-clampperiodpredictsdevelopmentofbiliarycomplications
inlivertransplantationusingdonationaftercardiacdeathdonors.TransplInt.2012;25:838-46.
16. VillaR,FondevilaC,ErillI,GuimeraA,BombuyE,Gomez-SuarezC,etal.Real-timedirectmeasurementofhumanliverallografttemperaturefromrecoverytotransplantation.Transplantation.2006;81:483-6.
17. Jochmans I, Fieuws S, Tieken I, Samuel U, Pirenne J. The Impact ofHepatectomy Time of the Liver Graft on Post-transplant Outcome: AEurotransplantCohortStudy.AnnSurg.2017.
18. FaridSG,AttiaMS,VijayanandD,UpasaniV,BarlowAD,WillisS,etal.Impactof Donor Hepatectomy Time during Organ Procurement in Donation afterCirculatory Death Liver Transplantation: The United Kingdom Experience.Transplantation.2018.
19. HansenT,HollemannD,PittonMB,HeiseM,Hoppe-LotichiusM,SchuchmannM,etal.Histologicalexaminationandevaluationofdonorbileductsreceivedduringorthotopiclivertransplantation--amorphologicalcluetoischemic-typebiliarylesion?VirchowsArch.2012;461:41-8.
20. op den Dries S, Westerkamp AC, Karimian N, Gouw AS, Bruinsma BG,MarkmannJF,etal.Injurytoperibiliaryglandsandvascularplexusbeforelivertransplantation predicts formation of non-anastomotic biliary strictures. JHepatol.2014;60:1172-9.
21. Watson CJE, Kosmoliaptsis V, Pley C, Randle L, Fear C, Crick K, et al.Observations on the ex situ perfusion of livers for transplantation. Am JTransplant.2018;18:2005-20.
22. MattonAPM,deVriesY,BurlageLC,vanRijnR,FujiyoshiM,deMeijerVE,etal.Biliary Bicarbonate, pH and Glucose Are Suitable Biomarkers of BiliaryViability During Ex Situ Normothermic Machine Perfusion of Human DonorLivers.Transplantation.2018.
23. Nederlands Transplantatie Vereniging (Dutch Transplant Society) NTSDTF.NationalProtocolPostmortemdonororganprocurement.2017.
24. deVriesY,MattonAPM,NijstenMWN,WernerMJM,vandenBergAP,deBoerMT, et al. Pretransplant sequential hypo- and normothermic machineperfusion of suboptimal livers donated after circulatory death using ahemoglobin-based oxygen carrier perfusion solution. Am J Transplant.2019;19:1202-11.
25. opdenDriesS,KarimianN,SuttonME,WesterkampAC,NijstenMW,GouwAS,et al. Ex vivo normothermic machine perfusion and viability testing ofdiscardedhumandonorlivers.AmJTransplant.2013;13:1327-35.
26. Ooms - de Vries KM. Reducing hepatectomy times in all Dutch organprocurementteams.Bootcongres.Amsterdam2019.
27. HameedAM,PangT,YoonP,BaldersonG,DeRooR,YuenL,etal.AorticVersusDualPerfusionforRetrievaloftheLiverAfterBrainDeath:ANationalRegistryAnalysis.LiverTranspl.2018;24:1536-44.
28. GhinolfiD,TincaniG,RrekaE,RoffiN,ColettiL,BalzanoE,etal.Dualaorticandportal perfusion at procurement prevents ischaemic-type biliary lesions inlivertransplantationwhenusingoctogenariandonors:aretrospectivecohortstudy.TransplInt.2019;32:193-205.
29. Otto G, Heise M, Thies J, Pitton M, Schneider J, Kaiser G, et al. LiverPreservationbyAorticPerfusionAloneComparedWithPreservationbyAorticPerfusionandAdditionalArterialExSituBack-TablePerfusionWithHistidine-
Tryptophan-Ketoglutarate Solution: A Prospective, Randomized, Controlled,MulticenterStudy.TransplantationDirect.2017;3:e183.
30. HessheimerAJ,CollE,TorresF,RuizP,GastacaM,RivasJI,etal.Normothermicregional perfusion vs. super-rapid recovery in controlled donation aftercirculatorydeathlivertransplantation.JHepatol.2019;70:658-65.
31. KalisvaartM, deHaan JE, PolakWG,M. IJN, GommersD,MetselaarHJ, et al.OnsetofDonorWarmIschemiaTimeinDonationAfterCirculatoryDeathLiverTransplantation:HypotensionorHypoxia?LiverTranspl.2018;24:1001-10.
32. FengS,GoodrichNP,Bragg-GreshamJL,DykstraDM,PunchJD,DebRoyMA,etal. Characteristics associatedwith liver graft failure: the concept of a donorriskindex.AmJTransplant.2006;6:783-90.
Donorbloodcompositionisariskfactorforbiliaryinjuryduringdonationaftercirculatorydeathlivertransplantation
OttoB.vanLeeuwen,MarjoleinvanReeven,DannyvanderHelm,JanN.M.Ijzermans,IanP.J.Alwayn,BartvanHoek,WojciechG.Polak,TonLisman,VincentE.deMeijer,RobertJ.Porte.Submittedforpublication
4
ABSTRACT
Post-transplant cholangiopathy following ischemia-reperfusion injury (IRI) inhibits
widespreadapplicationofdonationafter circulatorydeath liver transplantation (DCD-
LT). Blood composition of the donor could influence graft flush-out and IRI. We
hypothesized that platelets, leukocytes and hematocrit of the DCD donor influence
biliaryinjuryduringDCD-LT.
Theassociationofhematocrit,plateletandleukocytecountswithbileducthistologyand
bile composition during (pre)clinical normothermic machine perfusion (NMP) was
assessed.Secondly,inanationwideretrospectivestudy,allDCD-LTbetween2010-2017
were included to assess the role of blood composition in the development of non-
anastomoticbiliarystrictures(NAS).
High donor platelet counts (OR 2.553, 95%CI 1.082-6.021, p=0.029) and low donor
leukocyte counts (OR 0.734 95%CI 0.581-0.927, p=0.009) were associated with
increased bile duct injury of 40NMP livers, and donor platelet count associatedwith
biliary bicarbonate and pH. In a multivariate Cox Proportional-Hazards regression
analysis including 235 DCD-LT, donor platelet count (HR 1.047 95%CI 1.007-1.089,
p=0.022) and hematocrit (HR 1.044 95%CI 1.005-1.083, p=0.025) were significant
independentriskfactorsforthedevelopmentofNAS.
Donor platelets and leukocytes are associatedwith biliary injury prior to and during
NMP.Additionally,plateletcountandhematocritaresignificantindependentriskfactors
forthedevelopmentofNASafterDCD-LT.
INTRODUCTION
Liver transplantation is the preferred treatment for patients with end-stage liver
disease.Theimbalancebetweenorganavailabilityanddemandhasledtotheincreased
use of donation after circulatory death (DCD) livers. The main limitation of the
widespread use of DCD livers is the frequent development of post-transplant
cholangiopathyfollowingtransplantation.Post-transplantcholangiopathyisaspectrum
of bile duct abnormalities, including non-anastomotic biliary strictures (NAS),
intraductalcastsand/orintrahepaticbilomaformation.1NASisobservedinupto30%
ofpatientsthatreceiveaDCDliver,whereasafterdonationafterbraindeath(DBD)liver
transplantation,thisvariesbetween3and13%.2-4
Injuryofperibiliaryglands(PBG)anddamageto theperibiliaryvascularplexus(PVP)
havebeen identifiedasrisk factors for thedevelopmentofNAS.Peribiliaryglandsare
essential in the regeneration of biliary epithelium after severe bile duct injury, as
encounteredduringtransplantation.5Recently,weobservedinthedatafromthestudy
byOpdenDries et al. that all biopsies gradedwith>50%deepPBGdamage alsohad
severe(>50%)damagetothePVP.Therefore,wehypothesizedthatPBGandPVPinjury
developparallelduringthedonorwarmischemicperiodandsubsequentcoldischemia
time prior to DCD liver transplantation. Accordingly, we hypothesized that if the
pathophysiology of PVP injury could be clarified, subsequent potential solutions that
decreasePVPinjurywouldalsopositivelyaffectPBGdamage.
Plateletsareoneofthemainthree(cellular)componentsofblood,andcontainseveral
prohemostatic and proinflammatory mediators.6 Several studies have shown an
influenceofplateletsonischemia-reperfusioninjuryinischemichearts,lungs,pancreata
and livers.7-14 In the early 1990’s Cywes et al. have shown that the level of platelet
adherence in donor livers grafts can predict the outcome of transplantation.15 An
increased level of platelet adherence was associated with inferior post-transplant
outcomes, and up to one-third of donor livers demonstratedmoderate to high-grade
plateletadhesion,suggestingsevereendothelialcelldamage.15Additionally,Cywesetal
haveshownthatadditionofplateletsduringperfusionofratliversaggravatedischemia-
reperfusion injury.14 At the beginning of this century, Sindram et al. have shown that
plateletsinducesinusoidalendothelialcellapoptosisofthecoldischemicratliver.16This
studyshowedthatpharmacologicalpreventionofplateletadhesionreducedsinusoidal
epithelial cell apoptosis. We hypothesize that donor platelets may influence biliary
injury by adhesion to endothelial cells in the PVP during thewarm hypoxic/ischemic
periodthatDCDgraftsencounter,subsequentlyleadingtoincreasedPVPinjury.
Inadditiontoplatelets,wehypothesizedthatalsoredbloodcellscouldinfluencebiliary
injury.Underhypoxicconditions,erythrocytesgeneratereactiveoxygenspecies(ROS).17
ROSarekeyinthedevelopmentofischemia-reperfusioninjury.18Moreover,inhypoxia,
erythrocytesinducepro-inflammatoryendothelialactivation,potentiallycausinginjury
tothePVP.19The lastof thethreecellularcomponentsofblood, leukocytes,couldalso
impact endothelial function, as in hypoxic conditions leukocytes are associated with
endothelialdamage.20
We aimed to study the potential association of platelet and leukocyte counts and
hematocritonbiliary injury inachronologicalmethod.First,bileductbiopsiesofDCD
liversprospectivelytakenpriortonormothermicmachineperfusion(NMP)wereused
to asses biliary injury at baseline. Secondly, bile produced during normothermic
machineperfusion (NMP)of thesameDCD liverswasstudied.Lastly,weperformeda
nationwideretrospectivestudy toassess the influenceofdonorplateletand leukocyte
countsandhematocritonthedevelopmentofNASafterDCD-LT.
METHODS
Studydesign
The first part of this study is a prospective cohort study including all DCD livers that
underwent preclinical and clinical NMP in the University Medical Center Groningen
(2013-2019).Extrahepaticbileductbiopsiespriortomachineperfusionwerecollected,
fixed in4% formalin,andsubsequentlyembedded inparaffin.Bileduct slicesof4µm
werecutandstainedwithhematoxylin&eosin,andsubsequentlyexaminedusinglight
microscopy.Thebileductinjury(BDI)scorewasdeterminedinablindedfashionbytwo
independentresearchers,usingaclinicallyrelevanthistologicalgradingsystem.21,22The
BDIscorewasbasedonascaleof0to7andacut-offscoreof4.75wasusedtodefine
low and high BDI, as described previously.21 Both preclinical and clinical NMP
procedureswereperformedwith theLiverAssistdevice(OrganAssist,Groningen, the
Netherlands),withprotocolsandoutcomesreportedelsewhere.21,23,24Bilewascollected
from a 8Fr biliary drain in the common bile duct. During NMP, bile samples were
collectedevery30minutesundermineraloil todeterminebiliarypH,bicarbonateand
glucoseasdescribedpreviously.21,23,24
Subsequently, in a national retrospective cohort study all DCD liver transplantations
between 01-01-2010 and 01-01-2017 were included. Exclusion criteria were
retransplantation, pediatric liver transplantation (<18 years) and the use of
hypothermicmachineperfusion.Dataondonorandorganprocurementcharacteristics
wereobtained throughtheEurotransplantDonordatadatabase.Dataof recipientsand
transplantation outcomes were obtained from the databases of participating centers,
completedwithmissingdatafromtheelectronicalpatients’medicalrecords.Thisstudy
was approved by the Medical Ethical Committee of the University Medical Center
Groningen(METC.2017/504).
Definitions
Donor hematocrit, leukocyte and platelet countwere defined as the last known value
prior towithdrawal of life-support.Non-anastomotic strictures of the bile ductswere
definedasbiliarystricturesatanyplaceinthebiliarytreeexceptfortheanastomosisin
theabsenceofhepaticarterythrombosis.ToclassifyforNAS,patientswererequiredto
haveclinicalsymptomsofcholestasiswithsubsequentimagingdemonstratingbileduct
strictures within two years after DCD liver transplantation. The total donor warm
ischemiatimewasdefinedastheperiodfromcardiacarrestuptotheinitiationofcold
flushinginthedonor.Theagonalphaseandtheasystolephasecomprisedoftheperiod
betweenwithdrawaloflife-supportandcirculatoryarrest,andcirculatoryarresttocold
perfusion,respectively.Coldischemiatimewasdefinedasthetimebetweenthestartof
coldflushandthemomentthattheliveristakenoficeforimplantationintherecipient.
Recipientwarmischemiatimewasthetimebetweenremovaloftheliverfromiceuntil
eitherportalorarterialreperfusion,whichevercamefirst.
Donationaftercirculatorydeathprocedure
In theNetherlands,withdrawalof lifesupport isgenerallyperformedon the intensive
care unit. Cannulation prior to circulatory arrest is not performed, and systemic
heparinizationisprohibitedbyDutchlaw.Afteramandatory5-minutesnotouchperiod
followingcirculatoryarrest,thedonoristransportedtotheoperatingtheatre.Asuper-
rapid sterno-laparotomy followed by aortic-only perfusion with heparinized Belzer
University of Wisconsin (UW) cold storage solution (Bridge to Life, London, UK) is
performed. The common bile duct and intrahepatic biliary tree are flushed with low
pressureUWsolution.Afterhepatectomy,theliverisflushedwithat least500mlcold
UWpreservationsolutionthroughtheportalveinuntilcleareffluentisobserved.
Statisticalanalysis
Continuous variables were presented as median and interquartile range (IQR), and
difference between groups were tested using Mann-Whitney or Kruskal-Wallis test.
Categoricalvariableswerepresentedasnumber[percentage]anddifferencesbetween
groupsweretestedusingPearson’schi-squaretestorFisher’sexacttest.
In the histological analysis, logistic regression models were used to evaluate
independentriskfactorsforahighbileductinjuryscore.Variableswereincludedinthe
multivariatelogisticregressionanalysisifunivariateanalysesyieldedap-value<0.20.
ROCcurveswereformedtoidentifythemostsuitablecut-offvalues.
Intheretrospectivecohortstudy,univariateandmultivariateCoxProportional-Hazards
regression models were used to evaluate independent risk factors for NAS. Subjects
without the event were censored at two years post transplantation. Variables were
included in a multivariate Cox Proportional-Hazards regression analysis if univariate
analyses yielded a p-value < 0.20. The reported Hazard ratios (HR) for donor
hematocrit, leukocyte and platelet count refer to an increase of 1%, 1x109/L and
50x109/L, respectively. All tests had a two-sided design with a p-value below 0.05
considered as significant. All analyses were performed using SPSS version 24 (IBM,
Chicago,Illinois).
RESULTS
HistologicalanalysisofbileductbiopsiesfromDCDlivers
Of40 consecutivepreclinical and clinicalNMPprocedures, 39bileductbiopsieswere
obtained upon arrival in our center. In a multivariate logistic regression analysis
includingdonorageanddonorcauseofdeath,donorplateletcount (OR2.553,95%CI
1.082-6.021,p-value=0.032)andcoldischemiatime(OR2.251,95%CI1.192-4.251,p=
0.012) were identified as independent risk factors for high BDI, whereas donor
leukocytecount(OR0.728,95%CI0.572-0.926,p=0.010)wasassociatedwithlowBDI
(Table 1). Cut-off values of 181 x 109/L for platelets and 12.5 x 109/L for leukocytes
wereidentifiedusingROCcurves.Liversfromdonorswithplateletsbelow181x109/L
andleukocytesabove12.5x109/LrarelyhadahighBDI,whereasthecombinationofan
increaseddonorplateletcountwithlowleukocytesoftenresultedinahighBDI.(Figure
1).
Figure1:Impactofdonorleukocyteandplateletcountonbileductinjuryscoreof
donationaftercirculatorydeathlivers.Thecombinationofaplateletcountbelow181
x109/Landleukocytecount>12.5x109/Lappearedtobeprotectiveforbileduct injury.
GreencirclesindicateliverswithalowBDI,redtrianglesindicateliverswithahighBDI.
Table1:Univariateandmultivariatelogisticregressionanalysisforahighbile
ductinjuryscore.
Univariateanalysis MultivariateanalysisVariable OR 95%CI P-value OR 95%CI P-
valueDonor GenderMale(ref)Female
ref0.437
ref0.113-1.681
0.549ref0.228
Age(years) 1.041 0.980-1.105 0.191 NS BMI 1.065 0.956-1.186 0.253 CauseofdeathCVA(ref)TraumaAnoxia
ref0.0600.056
ref0.006-0.5740.005-0.669
ref0.0150.023
NS
Hematocrit(%) 1.009 0.913-1.116 0.857 Leukocytecount(per1x109/L)
0.924 0.823-1.036 0.176 0.734 0.581-0.927
0.009
Plateletcount(per50x109/L)
1.283 0.932-1.766 0.099 2.553 1.082-6.021
0.029
WarmischemiatimeAgonalphase(min)Aystolictime(min)
1.0090.9971.086
0.979-1.0400.963-1.0310.932-1.266
0.5650.8430.292
Coldischemiatime(hours)
1.006 1.000-1.011 0.043 1.675 1.093-2.566
0.013
Abbreviations:BMI;bodymassindex,CVA;cerebralvascularattack,OR;oddsratio.NSindicatesvariablewasremovedfromtheforwardLRmodel.
Bilecomposition
Duringthe40NMPprocedures, the liversofdonorswithaplateletcountbelow181x
109/Lshowedhigherbicarbonatelevelsinbile,andahigherbilepHcomparedtobileof
liverswithaplateletcountabove181x109/L.(Figure2A-B).Leukocytecountdidnot
significantlyassociatewithbicarbonatesecretion.During the first60minutesofNMP,
liverswithaleukocytecount>12.5x109/LhadalowerbilepH.
Figure2:CompositionofbileduringNMP.Platelet count significantly influences
biliarybicarbonatelevelsandbilepH.*indicatesasignificantdifferencebetweenthe
twogroupsatthattimepoint(p<0.050).
Retrospectivecohortstudy:baselinecharacteristics
Atotalof252DCD liver transplantationswereperformed in theNetherlandsbetween
01-01-2010 and01-01-2017.After applicationof the exclusion criteria, the remaining
235caseswereincludedinthisstudy.BaselinecharacteristicsarepresentedinTable2.
Actuarialone-andtwo-yeargraftsurvivalrateswere81%and75%,and90%and89%
forpatientsurvivalrespectively.
Table2:Baselinecharacteristicsofdonor,procurementandrecipient,and
outcomesaftertransplantation.
Variable Median(IQR)N=235
Donor Age(yrs) 48(35-54)GenderMaleFemale
140(59%)95(41%)
BodyMassIndex 24(22-26)Causeofdeath:TraumaAnoxiaCVAOther
57(24%)69(29%)90(38%)19(8%)
ALTpeak(u/L) 48(24-101)GGTpeak(u/L) 34(20-68)Hematocrit(%) 34(30-38)Plateletcount(x109/L) 182(145-244)Leukocytecount(x109/L) 12.5(9.4-17.6)Procurement Donorwarmischemiatime-Agonalphase(min)-Asystolictime(min)
15(11-20)15(13-18)
Recipient Age(yrs) 55(47-63)BMI 26(24-29)GenderMaleFemale
165(70%)70(30%)
LabMELDscore 15(10-21)Transplantation Coldischemiatime(min) 423(366-494)Secondwarmischemiatime(min)# 33(26-42)OutcomesafterDCD-LT Actuarialgraftsurvival 1year 81%2year 75%Actuarialpatientsurvival 1year 90%2year 89%Primarynon-function 3(1%)Non-anastomoticstrictures<2yearsofLT 61(26%)Hepaticarterythrombosis 15(6%)Intensivecareunitstay(days) 2(1-4)Totalhospitalstay(days) 16(13-26)ASTpeak(u/L) 2019(1105-4287)ALTpeak(u/L) 1502(719-2767)
Abbreviations:ALT;alanineaminotransferase,AST,aspartaneaminotransferase,CVA;
cerebralvascularattack,GGT;gammaglutamyltransferase,LT;livertransplantation,
MELD;modelend-stageliverdisease#thetimeframefromremovaloftheliverfromice
untilgraftreperfusion.
Retrospectivecohortstudy:non-anastomoticbiliarystrictures
Sixty-one (26%) patients developed NAS within two years of transplantation. The
resultsofunivariateanalysisareshowninTable3.InthemultivariateCoxProportional-
Hazardregressionmodels,donorhematocrit(HR1.044,95%CI1.005-1.083,p=0.025)
anddonorplateletcount(HR1.047,95%CI1.007-1.089,p=0.022)wereidentifiedas
significantindependentriskfactorsforthedevelopmentofNAS(Table4).Additionally,
donor age and cold ischemia time were significant independent risk factors for NAS.
DonorleukocytecountdidnotseemtoinfluenceratesofNASintheunivariateanalysis
(Table3).Inthedonorpopulationover40years,plateletsandhematocritwerestrong
predictors ofNASafterDCD liver transplantation (HR1.122, 95%CI1.013-1.241, p=
0.027 and HR 1.050, 95% CI 1.009-1.093, p = 0.017, respectively) whereas in the
population below40 years, no influencewas observed of platelets and hematocrit on
NAS(HR1.058,95%CI0.881-1.270p=0.574andHR0.988,95%CI0.911-1.071,p=
0.764,respectively).
Table3:UnivariateCoxRegressionanalysisforthedevelopmentofnon-anastomoticbiliarystrictureswithintwoyearsoftransplantation.
Variable HR 95%CI P-valueDonor Gender
Male(ref)Female
0.957
0.574-1.593
0.864
Age(years) 1.030 1.008-1.051 0.007 BMI 0.994 0.913-1.082 0.891 Causeofdeath
CVA(ref)TraumaAnoxiaOther
0.6640.4511.398
0.344-1.2830.225-0.9070.660-2.963
0.2230.0260.382
ALTpeak(u/L) 0.998 0.996-1.001 0.186 LastGGT(u/L) 1.000 0.998-1.003 0.866 Hematocrit(%) 1.051 1.013-1.090 0.024 Leukocytecount(x109/L) 1.020 0.980-1.062 0.340
Plateletcount(per50x109/L) 1.051 1.013-1.090 0.008Transplantation Warmischemiatime
Agonalphase(min)Aystolictime(min)
1.0171.004
0.961-1.0760.987-1.022
0.5620.650
Coldischemiatime(hours) 1.274 1.122-1.447 <0.001Recipient Age(years) 0.994 0.971-1.017 0.585 BMI 0.993 0.939-1.051 0.820 Lab-MELD 0.980 0.946-1.016 0.269 Warmischemiatime(min) 1.028 1.010-1.047 0.003
Abbreviations:ALT;alanineaminotransferase,BMI;bodymassindex,CVA;cerebral
vascularattack,GGT;gammaglutamyltransferase,MELD;modelend-stageliverdisease,
Table4:MultivariateCoxRegressionanalysisforthedevelopmentofnon-anastomoticbiliarystrictureswithintwoyearsoftransplantation.
Variable HR 95%CI P-valueDonor Age(years) 1.031 1.009-1.054 0.006 Causeofdeath
CVA(ref)TraumaAnoxiaOther
NS NS NS
ALTpeak(u/L) NS NS NS Hematocrit(%) 1.044 1.005-1.083 0.025 Plateletcount(per50x109/L) 1.047 1.007-1.089 0.022 Coldischemiatime(hours) 1.252 1.098-1.427 0.001Recipient Warmischemiatime(min) 1.031 1.010-1.053 0.004
NSindicatesvariablewasremovedfromtheforwardLRmodel.Abbreviations:ALT;
alanineaminotransferase,CVA;cerebrovascularattack.
DISCUSSION
Inthispaperwepresentdatasuggestingthatdonorplateletsinfluencebiliaryinjuryin
theprocessofDCD liver transplantation. In addition toplatelets, also leukocyte count
was inversely associated with biliary injury prior to graft reperfusion. Platelet count
and, additionally, hematocrit were significant independent risk factors for the
developmentofNASwithintwoyearsofDCDlivertransplantation.
Following theevidence thatbiliarycomplicationsarepredictedby theseverityofPBG
and PVP injury, several studies have been performed on the role of PBGs in liver
transplantation.25-28 As NAS is hypothesized to be a result of reduced regenerative
capacity from the PBGs after liver transplantation, regenerative medicine offers a
potential treatment for NAS.25 However, the pathophysiology of PVP injury in the
developmentofNAShashardlybeenstudied,whereasintegrityofthePVPismostlikely
requiredtoperformanyPBGregenerativetreatment.
To our knowledge, the involvement of platelets in ischemia-reperfusion injury of the
biliarytreehasnotbeenreportedbefore.AsCywesetal.andSindrametal.haveshown
before,plateletsplayanimportantroleinischemia-reperfusioninjuryoflivergrafts.14-16
Cywes et al have shown that activation of platelets increase the extent of reperfusion
injury,whereasSindrametalobservedthatplateletsinducesinusoidalendothelialcell
apoptosis upon reperfusion. Interestingly, the current study suggests that platelets
alreadyinfluencebiliaryinjurypriortograftreperfusion.Onepotentialexplanationfor
this is that during the hypoxic/ischemic period that DCD grafts encounter, severe
endothelialdysfunctionoccurs.
Vascular endothelial dysfunction is a characteristic of human ageing, displayed by
reduced nitric oxide bioavailability, shifts from predominantly vasodilator to
vasoconstrictor prostanoid production, and lastly an increased endothelin-1mediated
vasoconstriction.29-31 Especially this last characteristic offers a potential
pathophysiologicalexplanationforthe involvementofplatelets inbiliary injury.Under
hypoxicconditions,plateletsincreasinglyadheretoendothelialcells.32Inpatientswith
endothelial dysfunction, platelet-endothelium interaction leads to enhanced release of
endothelin-1, initiating vasoconstriction.31 Vasoconstriction during the agonal and
asystolicphasewould lead to insufficient flushingof thePVP.Tostudy this,we tested
whetherthepotentialimpactofplateletsonNASwasdifferentamongtheyoungerand
the older donor population, as endothelial function decreases over age. We did not
observe a significant influence of platelet count and hematocrit in DCD liver
transplantationwithdonoragebelow40years. Indonorsabove40years, therewasa
strong influence of platelets and hematocrit on NAS. Using a rat model. Tyagi and
colleagueshavedescribed thatacutesimulatedhypoxiaresults inadeceasedbleeding
propensity and increased platelet activity.31 In the same paper, inhibition of platelet
calpain activity demonstrated reversal of hypoxia-induced platelet hyperreactivity 31.
These findings offer a potential for a therapeutic intervention, however, in many
countriesadministrationofmedicationthatisnotintendedforstabilizingthedonorbut
focussesonpost-transplantoutcomes,isforbiddenbylaw.Inafewcountries,systemic
heparinizationpriortowithdrawaloflife-supportisallowed.Gaoetal.haveshownthat
heparin potentiates platelet activity33, and Hessheimer et al showed that heparin
administrationtoporcineliverdonorsimprovesoutcomeinDCDlivertransplantation.34 Itwouldprovidevaluable information toassess the influenceofplateletsonbiliary
injury,priortoreperfusion,aswellinthecountrieswereheparinizationisallowed.
Additionally, we observed that the donor leukocyte count was associated with the
development of biliary injury prior to NMP. Large amounts of research have been
performedontherecipient’sinnateimmuneresponsefollowingtransplantation,which
constitutes a large proportion of ischemia-reperfusion injury.35,36 Interestingly, now
donorleukocytesseemtoinfluencetheischemicinjuryofthebiliarytreeintheabsence
of recipient leukocytes, and high leukocyte counts seems to be protective for biliary
injury.However,thebeneficialeffectondonorleukocytesdisappeareduponreperfusion
ontheperfusiondeviceaswellas intherecipient.Unfortunately,donorreports inthe
Eurotransplant region only state the leukocyte count, and further information of
leukocytedifferentiationisnotavailable.ArecentpaperbyRichardsetal.demonstrated
that in older adults the peripheral vasodilation during systemic hypoxia is severely
impairedcomparedtoyoungercontrols.37Impairedvasodilationfollowingthehypoxia
andischemiaoftheagonalandasystolicperiodcouldleadto lessthoroughflushingof
themicrocirculationofalivergraft.Therefore,toexplaintheprotectiveeffectofahigh
leukocyte count on biliary injury prior to reperfusion, we hypothesize that a high
leukocyte count could contribute to local vasodilation, and thereby more efficient
flushingofthePVP.Themechanismofimpairedvasodilationinolderpeoplecouldalso
beanexplanationfortheobservationthattheinfluenceofhematocritandplateletswas
only observed in the donor population > 40 years. An interesting way to test the
hypothesis that impairedhypoxicvasodilationplaysa role in thedevelopmentofPVP
injury, would be to add a strong vasodilator to the flushing solution. Potentially, this
couldalsoleadtoareductionintheinfluenceofplateletsandhematocritonNAS,asthat
wasmainlyobservedinolderdonors.
Additionally,weobservedthatdonorhematocritwasassociatedwiththedevelopment
ofNASafterDCD-LT.Morariuetal.haveshownthatUniversityofWisconsin(UW)Cold
Storagesolutionpromotesseverehyperaggregationofredbloodcells(RBC’s)compared
toRBC innormalblood.38Ashematocrit increases, there isprogressiveaggregationof
RBC’s.39Themaximumobservedsizeoftheseaggregatesis4.332µm2,comparedto137
µm2 in normal blood samples without UW.38 The presence of these aggregates could
result in inferiormicrocirculation,andthereby leadingto injuryof thePVP.There isa
large size difference between these RBC aggregates and leukocytes, which have a
diameter averaging between 10 µm and 20µm.40 Therefore we hypothesize that
leukocyteswouldnotleadtomicrovascularobstruction,whereastheseRBCaggregates
could. However, it remains unclearwhy donor hematocrit influenced the rate of NAS
after transplantation,but that itdidnot seemto influencehistologicalbileduct injury
andbileproductionduringNMP.Anotherhypothesisfortheinvolvementofhematocrit
inbiliaryinjuryisthatduringhypoxicconditionserythrocytesexcretereactiveoxygen
species (ROS). ROS cause severe injury following graft reperfusion in transplantation,
whichwould explain that the impact of hematocrit on biliary injury is only observed
after transplantation. Consequently, a higher hematocrit would thereby lead to an
increasedROSexcretion.
An interesting aspect of this study is that we suggested new factors involved in the
pathophysiologyofpost-transplantcholangiopathy.Wedobelievethatastrongpointof
this work is that histology, bile analysis and a retrospective database analysis are
combinedtothoroughlyinvestigatetheinfluenceofdonorcellularbloodcompositionon
biliaryinjuryduringDCDlivertransplantation.Anotherstrongaspectistheprospective
collection of biopsies and bile for other protocols. We are interested whether the
involvementofplatelets,leukocytesandhematocritonischemia-reperfusioninjurycan
alsobefoundintransplantationofotherorgans.Thisstudyprovidesarationaleforthe
usageofnormothermicregionalperfusion(NRP),asNRPallowsforrapidrestorationof
(microcirculatory)bloodflowfollowingthedonorwarmischemiatime.A limitationof
this study is the retrospective character of the database study, and its limited size.
Moreover,thenumbersinthehistologyandbilecompositionstudyarerelativelysmall.
In conclusion, this study shows that the cellular blood composition of the donor
influencesbiliaryinjuryduringDCDlivertransplantation.Inahistologicalanalysisprior
toreperfusion,donorleukocyteandplateletcountwereassociatedwithbileductinjury.
Plateletcount>181x109/Lalsohadanegativeimpactonbiliaryepithelialcellfunction
markersduringNMP,suchasbiliarybicarbonatesecretionandbilepH. Inaccordance
withthis,donorhematocritandplateletcountweresignificantindependentriskfactors
forthedevelopmentofNASafterDCDlivertransplantation.
REFERENCES
1. de Vries Y, von Meijenfeldt FA, Porte RJ. Post-transplant cholangiopathy:Classification,pathogenesis,andpreventivestrategies.BiochimBiophysActaMolBasisDis.2018;1864(4PtB):1507-1515.
2. den Dulk AC, Sebib Korkmaz K, de Rooij BJ, et al. High peak alanineaminotransferasedeterminesextrariskfornonanastomoticbiliarystricturesafterlivertransplantationwithdonationaftercirculatorydeath.TransplInt.2015;28(4):492-501.
3. Dubbeld J,HoekstraH, FaridW, et al. Similar liver transplantation survivalwith selected cardiac death donors and brain death donors. Br J Surg.2010;97(5):744-753.
4. O'NeillS,RoebuckA,KhooE,WigmoreSJ,HarrisonEM.Ameta-analysisandmeta-regression of outcomes including biliary complications in donationafter cardiac death liver transplantation. Transpl Int. 2014;27(11):1159-1174.
5. deJongIEM,MattonAPM,vanPraaghJB,etal.PeribiliaryGlandsAreKeyinRegenerationoftheHumanBiliaryEpitheliumAfterSevereBileDuctInjury.Hepatology.2019;69(4):1719-1734.
6. Garraud O, Cognasse F. Are Platelets Cells? And if Yes, are They ImmuneCells?FrontImmunol.2015;6:70.
7. Flores NA, Sheridan DJ. The pathophysiological role of platelets duringmyocardialischaemia.CardiovascRes.1994;28(3):295-302.
8. KurodaT, ShioharaE,HommaT, FurukawaY, Chiba S. Effects of leukocyteand platelet depletion on ischemia--reperfusion injury to dog pancreas.Gastroenterology.1994;107(4):1125-1134.
9. Mullane KM, McGiff JC. Platelet depletion and infarct size in an occlusion-reperfusionmodelofmyocardialischemiainanesthetizeddogs.JCardiovascPharmacol.1985;7(4):733-738.
10. Okada Y, Marchevsky AM, Zuo XJ, et al. Accumulation of platelets in ratsyngeneic lung transplants: a potential factor responsible for preservation-reperfusioninjury.Transplantation.1997;64(6):801-806.
11. Parratt JR.Pathophysiologyofmyocardial ischemia: importanceofplatelet-vesselwallinteractions.CardiovascDrugsTher.1988;2(1):35-40.
12. RosenR,DauschW,BeckE,KlausW.Platelet inducedaggravationof acuteischaemiainanisolatedrabbitheartmodel.CardiovascRes.1987;21(4):293-298.
13. RousseauG,HebertD,LibersanD,KhalilA,St-JeanG,LatourJG.Importanceofplateletsinmyocardialinjuryafterreperfusioninthepresenceofresidualcoronarystenosisindogs.AmHeartJ.1993;125(6):1553-1563.
14. Cywes R, PackhamMA, Tietze L, et al. Role of platelets in hepatic allograftpreservationinjuryintherat.Hepatology.1993;18(3):635-647.
15. Cywes R, Mullen JB, Stratis MA, et al. Prediction of the outcome oftransplantation in man by platelet adherence in donor liver allografts.Evidence of the importance of prepreservation injury. Transplantation.1993;56(2):316-323.
16. SindramD, Porte RJ, HoffmanMR, Bentley RC, Clavien PA. Platelets inducesinusoidal endothelial cell apoptosis upon reperfusion of the cold ischemicratliver.Gastroenterology.2000;118(1):183-191.
17. RifkindJM,MohantyJG,NagababuE,SalgadoMT,CaoZ.PotentialModulationofVascularFunctionbyNitricOxideandReactiveOxygenSpeciesReleasedFromErythrocytes.FrontPhysiol.2018;9:690.
18. Peralta C, Jimenez-Castro MB, Gracia-Sancho J. Hepatic ischemia andreperfusion injury: effects on the liver sinusoidal milieu. J Hepatol.2013;59(5):1094-1106.
19. Huertas A, Das SR, Emin M, et al. Erythrocytes induce proinflammatoryendothelialactivation inhypoxia.Am JRespirCellMolBiol.2013;48(1):78-86.
20. Zheng S, Cao Y, Zhang W, et al. Platelet-mediated adhesion facilitatesleukocytesequestrationinhypoxia-reoxygenatedmicrovessels.SciChinaLifeSci.2016;59(3):299-311.
21. MattonAPM,deVriesY,BurlageLC,etal.BiliaryBicarbonate,pHandGlucoseAre Suitable Biomarkers of Biliary Viability During Ex Situ NormothermicMachinePerfusionofHumanDonorLivers.Transplantation.2018.
22. opdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsand vascularplexusbefore liver transplantationpredicts formationof non-anastomoticbiliarystrictures.JHepatol.2014;60(6):1172-1179.
23. deVriesY,MattonAPM,NijstenMWN,etal.Pretransplantsequentialhypo-and normothermic machine perfusion of suboptimal livers donated aftercirculatory death using a hemoglobin-based oxygen carrier perfusionsolution.AmJTransplant.2019;19(4):1202-1211.
24. opdenDriesS,KarimianN,SuttonME,etal.Exvivonormothermicmachineperfusion and viability testing of discarded human donor livers. Am JTransplant.2013;13(5):1327-1335.
25. deJongIEM,vanLeeuwenOB,LismanT,GouwASH,PorteRJ.Repopulatingthebiliarytree fromtheperibiliaryglands.BiochimBiophysActaMolBasisDis.2018;1864(4PtB):1524-1531.
26. van Rijn R, van Leeuwen OB, Matton APM, et al. Hypothermic oxygenatedmachineperfusionreducesbileductreperfusioninjuryaftertransplantationofdonationaftercirculatorydeathlivers.LiverTranspl.2018;24(5):655-664.
27. DiogoD,PachecoC,OliveiraR,etal. InfluenceofIschemiaTimeinInjuryofDeep Peribiliary Glands of the Bile Ducts Graft: A Prospective Study.TransplantProc.2019;51(5):1545-1548.
28. Sutton ME, op den Dries S, Koster MH, Lisman T, Gouw AS, Porte RJ.Regenerationofhumanextrahepaticbiliaryepithelium:theperibiliaryglandsasprogenitorcellcompartment.LiverInt.2012;32(4):554-559.
29. TaddeiS,VirdisA,GhiadoniL,etal.Age-relatedreductionofNOavailabilityandoxidativestressinhumans.Hypertension.2001;38(2):274-279.
30. Taddei S, Virdis A, Mattei P, et al. Aging and endothelial function innormotensivesubjectsandpatientswithessentialhypertension.Circulation.1995;91(7):1981-1987.
31. Westby CM, Weil BR, Greiner JJ, Stauffer BL, DeSouza CA. Endothelin-1vasoconstriction and the age-related decline in endothelium-dependentvasodilatationinmen.ClinSci(Lond).2011;120(11):485-491.
32. TyagiT,AhmadS,GuptaN,etal.Alteredexpressionofplateletproteinsandcalpain activity mediate hypoxia-induced prothrombotic phenotype. Blood.2014;123(8):1250-1260.
33. Gao C, Boylan B, Fang J, Wilcox DA, Newman DK, Newman PJ. Heparinpromotes platelet responsiveness by potentiating alphaIIbbeta3-mediatedoutside-insignaling.Blood.2011;117(18):4946-4952.
34. Hessheimer AJ, Vendrell M, Munoz J, et al. Heparin but not tissueplasminogenactivatorimprovesoutcomesindonationaftercirculatorydeathlivertransplantationinaporcinemodel.LiverTranspl.2018;24(5):665-676.
35. Lu L, Zhou H, Ni M, et al. Innate Immune Regulations and Liver Ischemia-ReperfusionInjury.Transplantation.2016;100(12):2601-2610.
36. Oliveira THC, Marques PE, Proost P, Teixeira MMM. Neutrophils: acornerstone of liver ischemia and reperfusion injury. Lab Invest.2018;98(1):51-62.
37. Richards JC, Crecelius AR, Larson DG, Luckasen GJ, Dinenno FA. Impairedperipheral vasodilation during graded systemic hypoxia in healthy olderadults:roleofthesympathoadrenalsystem.AmJPhysiolHeartCircPhysiol.2017;312(4):H832-H841.
38. Morariu AM, Vd Plaats A, W VO, et al. Hyperaggregating effect ofhydroxyethyl starch components and University of Wisconsin solution onhuman red blood cells: a risk of impaired graft perfusion in organprocurement?Transplantation.2003;76(1):37-43.
39. FabryTL.Mechanismof erythrocyte aggregation and sedimentation.Blood.1987;70(5):1572-1576.
40. Schmid-SchonbeinGW,ShihYY,ChienS.Morphometryofhumanleukocytes.Blood.1980;56(5):866-875.
Selectedlivergraftsfromdonationaftercirculatorydeathcanbesafelyusedforretransplantation
MarjoleinvanReeven,OttoB.vanLeeuwen,SarwaDarwishMurad,AadP.vandenBerg,BartvanHoek,IanP.J.Alwayn,WojciechG.Polak,RobertJ.Porte.Transpl.Int.2020(inpress)
5
ABSTRACTBackground and aims: Due to the growing number of liver transplantations (LTs),
there is an increasingnumberof patients requiring retransplantation (reLT).There is
littledataontheuseofgraftsfromextendedcriteriadonors(ECD),especiallydonation
after circulatory death (DCD), for reLT. We aimed to assess the outcome of patients
undergoingreLTusingaDCDgraftintheNetherlandsbetween2001and2017.
Materialandmethods:EachDCD-reLTwasmatchedwithtwoDBD-reLTcases,based
onnumberofsuccessivereLT,BAR-score,intervalbetweenreLTandpriorLTandyear
ofreLT.Primaryoutcomeswerepatientandgraftsurvival,calculatedviaKaplanMeier
estimator.NineteenDCD-reLTwerecomparedwith38matchedDBD-reLTs.
Results:DonorsintheDCD-reLTgroupweresignificantlyyounger(38versus54years,
p<0.001)andhadalowerBMI(22versus25kg/m2,p=0.003).Comparisonofrecipient
demographics and ischemia times yielded no significant differences. Patient and graft
survivalrateswerecomparablebetweenthetwogroups.Furthermore, theoccurrence
ofnon-anastomoticstrictureswithinthefirstyearafterreLTdidnotdiffersignificantly
betweenthetwogroups(26.3%versus10.5%,p=0.143).
Conclusions: reLTwithDCD grafts does not result in inferior outcomes compared to
DBD grafts in selected patients. Therefore, DCD liver grafts should not routinely be
declinedforpatientsawaitingreLT.
INTRODUCTION
Liver transplantation(LT) is thebest treatmentoption forpatientssuffering fromend
stageliverdisease.Toexpandthedonorpoolintimesofincreasingdemand,theuseof
graftsfromextendedcriteriadonors(ECD)hasincreasedsubstantially,ofwhichgrafts
fromdonationaftercirculatorydeath(DCD)isamainparameter.1In2018,aDCDgraft
wasusedin38%and9%ofalldeceaseddonorLTintheNetherlandsandUnitedStates
of America, respectively.2,3 In the United Kingdom, 26% of deceased donor LT were
executedwithDCDgrafts(between01.04.2017and31.03.2018).4
LivertransplantationwithDCDgrafts(DCD-LT)isconsideredtobeinferiorcomparedto
DBD-LT,due to the increased riskof complications suchasearlyallograftdysfunction
(EAD) and biliary complications.5-8 Among biliary complications, non-anastomotic
strictures (NAS) are the most feared complications as they often require multiple
interventions for biliary drainage, are largely irreversible and are known to have a
negative impact on recipient andgraft survival.9The incidenceofNAS, alsoknownas
ischemic cholangiopathy (IC) or Ischemic Type Biliary Lesions (ITBL), after DCD-LT
variesbetween3and39%.6
Since the use of grafts frommarginal donors has increased, it is assumed that more
recipients will suffer from a suboptimal graft. Furthermore, due to improvements in
surgical techniques, post-operative care and immunosuppressive regimes, the short-
term survival after LT has improved significantly,10 resulting in a larger population
surviving long enough to develop late graft failure. A retransplantation of the liver
(reLT)iscurrentlytheonlydefinitivetreatmentforallograftfailure.However,itiswell
known that reLT is associated with inferior patient and graft survival compared to
primaryLT.11,12
Despite DCD liver grafts being widely accepted, transplant physicians and surgeons
tend to avoid the use of DCD grafts for reLT. However, since in some countries the
availability ofDBD grafts has decreased,13 thewaiting time for an optimal, preferably
DBDlivertobecomeavailable forareLTcandidatecouldbetoo longwithsubsequent
riskofdeteriorationofthepatient’scondition,makinghimorherineligibleforreLT.
ThereisverylittlereportedontheuseofDCDgraftsforpatientsrequiringareLT.Only
onestudyhasassessedtheoutcomesoftenpatientsundergoingreLTusingDCDgrafts.14
TheauthorsconcludedthattheuseofDCDgraftshouldbeavoidediftherecipienthasa
moderate to highModel for End-Stage Liver Disease (MELD) score. Unfortunately, no
comparison was made with reLT using DBD grafts. Since DCD-LT is common in the
Netherlands,andreLTisnotanofficialcontra-indicationfortheuseofaDCDliver,we
aimedtocomparetheoutcomesofreLTwithDCDgraftsintheNetherlandswiththatof
matchedDBDcases.
MATERIALS&METHODS
Inthismulticenterretrospectivestudy,allpatientswhounderwentare-LTusingaDCD
liver graft (DCD-reLT) in one of the three liver transplant centers in the Netherlands
from the beginning of the DCD-LT program in 2001 until January 1st 2017, were
included. Pediatric LT (<18 years), multi-organ transplantation and grafts preserved
with machine perfusion were excluded. A matched control group of DBD
retransplantations (DBD-reLT) was formed. For each DCD-reLT, two DBD-reLT were
selectedbasedonthefollowingmatchingcriteria(inorderof importance):Transplant
center, Balance of Risk score (BAR),15 number of consecutive reLT, year of reLT and
intervalbetweenpriorLTandreLT.Thislattermatchingcriterionwaschosensincean
earlyreLT(withinthreemonths), isontheonehandtechnically lesschallenging than
latereLT(easierhepatectomywithlessadhesions),butontheotherhandisperformed
inpatientswhomaybesickerpre-reLTthanpatientsundergoinga latereLT.16,17Data
on donor and organ procurement characteristics were obtained through the
Eurotransplant Donordata database. Recipient data and data on follow-up were
collected from prospective maintained databases and patients’ electronic medical
records.ThestudyhasbeenapprovedbytheInstitutionalReviewBoardoftheErasmus
MCUniversityMedicalCenterRotterdam(MEC-2019-0316).
In all DCD organ procurements in the Netherlands, withdrawal of life support takes
placeattheICUorregularward.Aftercirculatoryarrestamandatorynotouchperiodof
fiveminutesiscarriedoutafterwhichthedonoristransportedtotheoperatingtheatre.
AsdescribedintheNationalProtocolPost-mortemDonorOrganProcurement,asuper-
rapidretrievaltechniqueisusedinDCDdonorstominimizethedonorwarmischemia
time.Aftercannulationofaortaandinferiorvenacava,coldperfusionwithUniversityof
Wisconsin (UW) solution is started.18 Since pre-mortem administration of heparin is
prohibitedby law,heparin isaddedtotheperfusionsolution.Thestandardmethodof
implantation is with a piggyback caval vein anastomosis, an end-to-end arterial and
portalanastomosis,andaduct-to-ductbiliaryanastomosis.
Thetotaldonorwarmischemiatime(dWIT)wasdefinedastimebetweenwithdrawalof
life supporting treatmentandstartof coldperfusion.Thedefinitionofasystolicdonor
warm ischemia timewas the timebetween circulatory arrest and cold perfusion. The
cold ischemia time (CIT) was defined as the period between the start of the cold
perfusion in the donor and the removal of the liver from ice during the recipient
procedure.Thedefinitionofrecipientwarmischemiatime(rWIT)usedinthisstudyis
theintervalbetweenremovaloftheliverfromiceandgraftreperfusion(i.e.inthevast
majorityportalreperfusion).
The primary outcomemeasures of this studywere patient and graft survival. Patient
survivalwasdefinedastimebetweenreLTanddeath,withorwithoutfunctioninggraft.
Graft survival was calculated as time between the reLT and patient death (with or
withoutfunctioninggraft)orasuccessiveretransplantation.Secondaryoutcomeswere
incidenceofbileleakageandanastomoticstricturesaswellasthedevelopmentofNAS
withinthe firstyearaftertransplantation.NASwasdefinedasanystrictureof thebile
duct except those localized near the biliary anastomosis and in absence of an hepatic
arterythrombosis.
Continuousdatawerepresentedasmedianandinterquartilerange(IQR)andcompared
with the Mann-Whitney U test. Categorical variables were presented as number and
percentages and comparedwith the Pearson chi-square test or the Fisher’s exact test
where appropriate. Survival analyses was conducted using the Kaplan Meier method
and comparisonsweremadewith the log-rank test. All testwere two-sidedwith a p-
valuebelow0.05consideredassignificant.Thestatisticalanalyseswasperformedusing
SPSSversion24(IBM,Chicago,Illinois,UnitedStatesofAmerica).
RESULTS
Between the start of the DCD-LT program in 2001 and January 1st 2017, 19 patients
underwent a retransplantation with a DCD liver. These caseswerematchedwith 38
DBD-reLTcases.Donorand recipientdemographicsaregiven inTable1.Therewasa
male predominance in both donor groups (DCD-reLT: 52.6%, DBD-reLT: 57.9%).
Compared to DBD-reLT donors, DCD-reLT donors were significantly younger (38.0
versus53.5years,p<0.001)andhadalowerBMI(22.0versus24.5kg/m2,p=0.003).
Furthermore,DCDdonorshadmoreoftendiedfromtraumawhereasDBDdonorsdied
more from cerebrovascular accidents. In DCD-reLT themedian asystolic donorwarm
ischemiatimewas15minutes(11-18minutes)whereasthetotaldWITwas28minutes
(22–32minutes).
Themajorityof the recipientswasmale,with amedianageof51.0 years (IQR,48.0 -
58.0years)intheDCD-reLTgroupand49.5years(IQR,42.5–59.3years)intheDBD-
reLT group (p = 0.72). The most common indication for reLT was (ischemic)
cholangiopathy(42%intheDCD-reLTgroup,53%intheDBD-reLTgroup),followedby
primarynon-functionandrecurrenceof theprimarydisease.Themajorityof thereLT
were of the late type, being performed at least threemonths after the prior LT. The
medianlaboratoryMELDscoreattimeofreLTwassubstantiallylowerintheDCD-reLT
groupcomparedtotheDBD-reLTgroup(18versus26),howeverthisdifferencewasnot
statisticallysignificant(p=0.417).
Table1:Donorandrecipientdemographics
TotalgroupN=57
DCD-reLTN=19
DBD-reLTN=38
P-value
Donor Male 32(56.1) 10(52.6) 22(57.9) 0.71Age(years) 50.0
(26.5-57.0)38.0(20.0-45.0)
53.5(39.0-59.0)
<0.001
BMI(kg/m2) 24.0(22.0-26.0)
22.0(19.0-24.0)
24.5(22.0-28.0)
0.003
CauseofdeathTraumaCVAAnoxiaOther
36(63.2%)11(19.3%)9(15.8%)1(1.8%)
7(36.8%)6(31.6%)5(26.3%)1(5.3%)
29(76.3%)5(13.2%)4(10.5)0
0.03
Lastγ-GT(U/L) 29.0(16.5-42.0)
30.0(18.0-36.0)
27.5(14.8-43.3)
0.93
LastALT(U/L) 26.0(14.0-45.0)
23.0(15.0-46.0)
27.5(14.0-44.8)
0.83
AsystolicdWIT(minutes)† n/a 15.0(11.0-18.0)
n/a n/a
TotaldWIT(minutes)‡ n/a 28.0(22.3-31.8)
n/a n/a
Recipient Male 33(57.9) 11(57.9) 22(57.9) 0.999Age(years) 51.0
(44.0-59.0)51.0(48.0-58.0)
49.5(42.5-59.3)
0.72
BMI(kg/m2) 22.8(20.7-26.5)
22.5(21.3-26.5)
23.3(19.7-26.8)
0.87
LaboratoryMELDscore 22.5(10.0-28.3)
17.5(10.3-24.0)
25.5(10.0-29.0)
0.42
IndicationforreLTPNFVascular(e.g.HAT/PVT)Biliary(e.g.ITBL)RecurrentprimarydiseaseOther
12(21.1)6(10.5)28(49.1)7(12.3)4(7.0)
3(15.8)3(15.8)8(42.1)3(15.8)2(10.5)
9(23.7)3(7.9)20(52.6)4(10.5)2(5.3)
0.70
NumberofreLT123
47(82.5)8(14.0)2(3.5)
16(84.2)2(10.5)1(5.3)
31(81.6)6(15.8)1(5.3)
0.78
TypeofreLTEarlyreLT(<3months)LatereLT(>3months)
18(31.6)39(68.4)
4(21.1)15(78.9)
14(36.8)24(63.2)
0.23
TimebetweenreLTandpriorLT(days)
617(55-3549)
775(239-3903)
326(12-3158)
0.41
GrafttypeofpriorLTDBDgraftDCDgraft
42(73.7)15(26.3)
13(68.4)6(31.6)
29(76.3)9(23.7)
0.52
Dataareshownasmedian(IQR)andfrequency(proportion).†:AsystolicdWITisdefined
asthetimebetweencirculatoryarrestandstartofcoldperfusion.‡:TotaldWITisdefined
astimebetweenwithdrawaloflifesupportingtreatmentandcoldperfusion.ALT:Alanine
transaminase,BMI:BodyMassIndex,CVA:Cerebrovascularaccident,DBD:Donationafter
BrainDeath,DCD:DonationafterCirculatoryDeath,dWIT:donorWarmIschemiaTime,γ-
GT:Gamma-glutamyltransferase,LT:livertransplantation,MELD:ModelforEndstage
LiverDisease,reLT:liverretransplantation
Table2 showsoperativedataaswell asdataon thepost-operativeoutcomes.Neither
the cold ischemia time (CIT) nor the recipient warm ischemia time (rWIT) differed
significantlybetweenthetwogroups.However,atrendtowardssignificancewasfound
in perioperative blood loss (4319 milliliters in the DCD-reLT group versus 2500
millilitersintheDBD-reLTgroup,p=0.07).Patientsweredischargedfromthehospital
afteramedianof25daysintheDCD-reLTgroupand20daysintheDBD-reLTgroup(p
=0.37).
Table2:Surgicalandpost-operativedemographics
TotalgroupN=57
DCD-reLTN=19
DBD-reLTN=38
P-value
Operation
rWIT(minutes) 39.0(34.0-46.0)
43.0(35.0-48.0)
37.5(32.5-43.0)
0.18
CIT(minutes) 452(395-525)
440(374-517)
454(400-528)
0.59
Bloodloss(ml)† 2800(2150-7000)
4319(2675-8125)
2500(1500-5875)
0.07
BARscore 12.0(7.3-17.0)
11.0(8.0-18.0)
12.0(7.0-17.0)
0.86
Post-operativeoutcomes
ICUstay(days) 3.0(2.0-9.0)
2.0(2.0-5.0)
3.5(2.0-9.3)
0.37
Hospitalstay(days) 23.0(13.5-34.5)
25.0(14.0-34.0)
19.5(13.0-40.3)
0.37
PeakALTwithin1stweek 1217(613-2499)
1238(582-2522)
1159(634-2461)
0.82
Bileleak 6(10.5) 2(10.5) 4(10.5) 0.999
Anastomoticstrictures 13(22.8) 4(21.1) 9(23.7) 0.999
Non-anastomoticstrictures‡
9(15.8) 5(26.3) 4(10.5) 0.143
Death 14(24.6) 5(26.3) 9(23.7) 0.999
Retransplantation 4(7.0) 1(5.3) 3(7.9) 0.999
Dataareshownasmedian(IQR)andfrequency(proportion).†:Proportionofmissingdata
forthisvariableis19.3%.‡:incidencewithinfirstyearafterreLT.ALT:Alanine
transaminase,BAR:Balanceofrisk,CIT:ColdIschemiaTime,DBD:DonationafterBrain
Death,DCD:DonationafterCirculatoryDeath,ICU:IntensiveCareUnit,LT:liver
transplantation,MELD:ModelforEndstageLiverDisease,reLT:liverretransplantation,
rWIT:recipientWarmIschemiaTime
Survivalrates
Themedianfollow-upofthetotalcohortwas5.35years(IQR,1.82-9.26years).The30
days, 1-year, 5-year and 10-year recipient survival in the DCD-reLT group was 95%,
79%,79%and79% respectively, compared to 87%,84%,78%and78% in theDBD-
reLT group (p =0.915, Figure 1). The most common cause of death after reLT was
infection(Table3).
Figure 1: KaplanMeier curve of patient survival after DCD-reLT andDBD-reLT.
Patient survival isdefinedasdeath (withorwithout functioninggraft). DBD-reLT: liver
retransplantation with graft from donation after brain death. DCD-reLT: liver
retransplantationwithgraftfromdonationaftercirculatorydeath
Patient survival
0 2 4 6 8 100
20
40
60
80
100DCD-reLTDBD-reLT
Log Rank: p=0.915
Number entering interval 0 2 4 6 8 10
DCD-reLT 19 12 11 8 7 5
DBD-reLT 38 30 23 17 11 6
Years
Cum
ulat
ive
surv
ival
Table3:Causesofdeath
Patient Grafttype IntervalbetweenreLTanddeath(days)
Causeofdeath
1. DCD-reLT 1 Myocardialinfarctioninsepticpatient
2. DBD-reLT 9 Multipleorganfailureinsepticpatient
3. DBD-reLT 12 Progressiveliverfailure,probablyasresultofhypoperfusion
4. DBD-reLT 13 Multipleorganfailureinpatientwithimmunethrombocytopenicpurpura(transmittedfromdonor)andportalveinthrombosis
5. DBD-reLT 13 Neurologicalinfaustprognosisafterintra-operativeexsanguination
6. DBD-reLT 14 Multipleorganfailureinsepticpatient
7. DCD-reLT 129 Multipleorganfailureinsepticpatient
8. DCD-reLT 129 Recurrentgiantcellhepatitis
9. DBD-reLT 174 Criticalillnessneuropathy
10. DCD-reLT 205 PseudomonasinfectioninpatientwithrecurrenthepatitisCinfection
11. DBD-reLT 1333 Recurrentperitonitisduetomultidrugresistantbacteria.Patientwishednofurthertreatment
12. DBD-reLT 1405 Pulmonaryhypertensionandmesenterialthrombosis.Patientwishednofurthertreatment
13. DBD-reLT 3994 Bacterialperitonitisincirrhoticliver.Patientwishednofurthertreatment
14. DCD-reLT 4941 Recurrentlivercirrhosis,decompensatedaftersurgeryforhipfracture
The30days,1-year,5-yearand10-yeargraftsurvivalwas95%,79%,79%and79%for
theDCD-reLTgroupand84%,79%,70%and70%intheDBD-reLTgroup(p=0.603)
(Figure 2). Four patients needed a subsequent retransplantation: three because of
biliary complications (one in theDCD-reLT group and two in theDBD-reLT group, of
whichonecasewasaccompaniedbyrecurrenceofPSC)andonepatientintheDBD-reLT
groupduetoanearlyhepaticarterythrombosis.
Figure 2: Kaplan Meier curve of graft survival after DCD-reLT and DBD-reLT.
Graft survival is defined as death (with or without functioning graft) or consecutive
retransplantation.DBD-reLT:liverretransplantationwithgraftfromdonationafterbrain
death.DCD-reLT:liverretransplantationwithgraftfromdonationaftercirculatorydeath
Biliarycomplications
In total, 10.5%of the recipients in both groups had a bile leakage. Furthermore, four
recipients in the DCD-reLT group (21.1%) and nine in the DBD-reLT group (23.7%)
developedananastomoticstricture(p=0.999).Theproportionofrecipientsdeveloping
NAS within the first year after reLT was substantially higher in the DCD-reLT group
(26.3 % versus 10.5%), however this difference was not statistically significant (p =
0.143).ThemediantimeintervalbetweenreLTanddiagnosisofNASwas204days(IQR
118–343days).
Graft survival
0 2 4 6 8 100
20
40
60
80
100
Log Rank: p=0.603
DCD-reLTDBD-reLT
Number entering interval 0 2 4 6 8 10
DCD-reLT 19 12 11 8 7 5
DBD-reLT 38 28 21 15 10 5
Years
Cum
ulat
ive
surv
ival
DISCUSSION
TherelativeshortageofavailablelivergraftshasledtoamorewidespreaduseofDCD
grafts.However,theoutcomesafterreLTwithaDCDgrafthaverarelybeenreportedin
literature.This is the firststudytoanalyzetheoutcomesafterDCD-reLTandcompare
thesewithoutcomesaftermatchedDBD-reLT.OurresultssuggestthatreLTwithaDCD
graft in selected recipients does not result in inferior outcome when compared to
matchedDBD-reLTs.
OursurvivalratesafterDCD-reLTaresubstantiallyhigherthanpresentedinaprevious
study on DCD-reLT performed by Perry et al. in 2011.14 This could be due to the
substantiallowerMELDscoreinourpopulation(medianof17.5versusamedianof27.0
reportedbyPerryetal.).Unfortunately,itisunclearwhetherinthestudybyPerryetal.
theMELDscoreincluded(non)standardexceptionpoints.Sinceourmedianlaboratory
MELDscoreisthatmuchlower,weareunabletorefuteorendorsetheconclusionfrom
Perry et al. that the use of DCD grafts should be avoided in high MELD recipients
awaiting reLT. However, a recent published study by Taylor et al. concluded that
acceptingaDCDgrafthasasurvivaladvantageoverwaitingforaDBDliver,especiallyin
recipients with a high MELD score.19 As this study only included first-transplant
recipients,itisdoubtfulwhethertheconclusionsmadebyTaylorandcolleaguescanbe
extrapolatedtothefieldof liverretransplantation.Basedonourresults, it is indicated
that at least in recipientswith a low-moderateMELD score the use of a DCD graft is
justifiableforreLT.
Thesignificantdifference indonoragebetweentheDCD-reLTandDBD-reLTgroup in
this study is attributable to the strict upper age limit for DCD donors that was
maintained in the Netherlands until recently and to the individual choice of the
transplant surgeon or physician to accept only the best DCD livers (i.e. DCD grafts
withoutotherextendedcriteriaandrelevantcomorbidities) for the indicationofreLT.
This latter isprobablythecase inmosttransplantprogramsperformingDCD-reLT.To
assesswhethertheexcellentsurvivalratesintheDCD-reLTgroupcouldbeattributedto
the relatively lowdonor age in this group, donor agewas tested in anunivariate Cox
Proportional-Hazardsregressionmodelforbothrecipientandgraftsurvival,yieldingno
significantresult(datanotshown).Thisisinlinewithliteraturethatagealonedoesnot
impair survival outcomes after DCD-LT.20,21 Since none of the matching variables
differedsignificantlybetweenthetwogroups,itishighlyunlikelythatthedifferencein
donorageistheresultofincorrectmatching.
The difference in donor cause of death and donor BMI between the two groups are
probably theresultof the lowerage in theDCD-reLTgroup;youngerdonorsdiemore
often from trauma, whereas older donors die predominantly from cerebrovascular
accidents,andyoungerdonorstendtohavealowerBMI.22-24However,thelowerdonor
BMIintheDCD-reLTgroupcouldalsobeduetoselectionbytransplantphysiciansand
surgeons. Since there seems to be some association between BMI and degree of
steatosis,aknownriskfactorforpooroutcomeafterLT,25,26thelowerBMIintheDCD-
reLTgroupcouldtosomeextenthaveinfluencedtheoutcomeinthisgroup.
WhencomparedwithDBDgrafts,livertransplantationwithDCDgraftsaregenerallyat
higher risk of developing biliary complications post-transplantation, especiallyNAS.A
similartrend,albeitnon-significantcanbeseeninthecurrentstudy.Itisexpectedthat
withanincreasedsamplesize,thisdifferencewouldhavebecomestatisticallysignificant
between the DCD-reLT and DBD-reLT group. Surprisingly, the incidence of NAS after
especiallyDBD-reLTinthecurrentstudyishigherthanexpected.Therecouldbeseveral
explanationsforthis.First,thehighNASincidenceintheDBD-cohortcouldbetheresult
of thematching.Furthermore,untilrecentlythedonorhepatectomytime(i.e. thetime
betweenthestartofcoldperfusioninthedonorandtheliverbeingstoredonice)was
relatively long in theNetherlands.Researchhas shown that aprolongedhepatectomy
timeisariskfactorforthedevelopmentofNAS.27,28Finally,thehighincidencesofNAS
inthisreLTcohortcouldalsoimplythatareLT,independentofgrafttype,hasahigher
riskofdevelopingpost-operativeNAS.Unfortunately,literatureonthistopicislacking.
Lastly, it should be noted that of the nine patients who developed NAS, only three
requiredanewtransplant,indicatingthatNASinthisgroupofpatientswasrathermild
andcouldbetreatedconservatively.
With the renewed interest in theuseofDCDgrafts,webelieve that the resultsof our
study are very relevant for further practice in these centers. With careful selection,
recipientandgraftsurvivalafterDCD-reLTappearsimilartothesurvivalinDBD-reLT.
Therefore, grafts for reLTshouldnotbe rejectedbasedon theDCDstatusalonebuta
carefulassessmentofadditionaldonor factors isneededforacase-by-casedecisionto
use these grafts. Furthermore,making use of DCD donors for reLTmay facilitate the
currentethicaldebateregardingreLT.Thatis,iftransplantsurgeonsandphysicianswill
accept DCD grafts for retransplantation, more DBD grafts will remain available for
recipientsonthewaitinglistawaitingtheirfirsttransplant.Atthesametime,expansion
ofthedonorpoolwithDCDdonorswillresultinmoreexpeditedreLTforthoseinneed.
Finally, with the emerging technologies in the field of machine perfusion, it can be
anticipatedthat thequalityofDCDgraftscanbe improved,resulting inamongothera
decreasedincidenceofischemiccholangiopathy.29-31
OnestrengthofthisstudyisthecomparisonofoutcomeafterDCD-reLTwithamatched
controlgroupofDBD-reLTcases.Thishasmadeapropercomparisonofthetwogroups
possible, fromwhich itcanbeconcludedthatsurvivalafterDCD-reLTisundercertain
circumstances similar to that after DBD-reLT. This study also has several limitations.
Firstly,wehadtodefinedonorwarmischemiatimeastimebetweenwithdrawaloflife
supportandcoldperfusion.Wewereunabletocalculatethemoreimportantfunctional
warmischemiatimeinthedonorsincedataonhemodynamicstatusduringtheagonal
phase is lacking or improperly recorded. Furthermore, the study had a retrospective
design,whichispronetobiasandconfounding.Finally,thesamplesizeofthisstudyis
relatively small,whichmade detailed statistical analysis such asmultivariate analysis
impossible.
In conclusion, liver retransplantationwith a DCD graft can yield similar outcomes as
liver retransplantation with donation after brain death. Therefore, DCD status itself
should not preclude the use of such donors in patients awaiting retransplantation.
However, careful selection of the offered DCD livers probably remains mandatory.
Largerstudiesareneededareneededtoconfirmourresults.
REFERENCES
1. NemesB,GamanG,PolakWG,GelleyF,HaraT,OnoS,etal.Extendedcriteriadonors in liver transplantation Part I: reviewing the impact of determiningfactors.ExpertRevGastroenterolHepatol.2016;10(7):827-39.
2. Eurotransplant.StatisticsReportLibrary.http://statistics.eurotransplant.org/;2018.
3. NetworkOPaT.NationalData-DonorsRecoveredintheU.S.byDonorType.2018.
4. Transplant NBa. Organ Donation and Transplantation - Activity Report2017/18. https://www.odt.nhs.uk/statistics-and-reports/annual-activity-report/;2018.
5. denDulkAC,SebibKorkmazK,deRooijBJ,SuttonME,BraatAE,IndersonA,et al. High peak alanine aminotransferase determines extra risk fornonanastomotic biliary strictures after liver transplantation with donationaftercirculatorydeath.TransplInt.2015;28(4):492-501.
6. O'NeillS,RoebuckA,KhooE,WigmoreSJ,HarrisonEM.Ameta-analysisandmeta-regressionofoutcomesincludingbiliarycomplicationsindonationaftercardiacdeathlivertransplantation.TransplInt.2014;27(11):1159-74.
7. deVeraME,Lopez-SolisR,DvorchikI,CamposS,MorrisW,DemetrisAJ,etal.Liver transplantation using donation after cardiac death donors: long-termfollow-upfromasinglecenter.AmJTransplant.2009;9(4):773-81.
8. CallaghanCJ,CharmanSC,MuiesanP,Powell JJ,GimsonAE,vanderMeulenJH,etal.OutcomesoftransplantationofliversfromdonationaftercirculatorydeathdonorsintheUK:acohortstudy.BMJOpen.2013;3(9):e003287.
9. VerdonkRC, Buis CI, van der Jagt EJ, GouwAS, LimburgAJ, SlooffMJ, et al.Nonanastomotic biliary strictures after liver transplantation, part 2:Management,outcome,andriskfactorsfordiseaseprogression.LiverTranspl.2007;13(5):725-32.
10. SongAT,Avelino-SilvaVI,PecoraRA,PuglieseV,D'AlbuquerqueLA,AbdalaE.Liver transplantation: fifty years of experience. World J Gastroenterol.2014;20(18):5363-74.
11. BerumenJ,HemmingA.LiverRetransplantation:HowMuchIsTooMuch?ClinLiverDis.2017;21(2):435-47.
12. OnacaN, LevyMF, Ueno T,Martin AP, Sanchez EQ, Chinnakotla S, et al. Anoutcome comparison between primary liver transplantation andretransplantation based on the pretransplant MELD score. Transpl Int.2006;19(4):282-7.
13. Domínguez-Gil B, Haase-Kromwijk B, Van Leiden H, Neuberger J, Coene L,Morel P, et al. Current situation of donation after circulatory death inEuropeancountries.TransplantInternational.2011;24(7):676-86.
14. Perry DK, Willingham DL, Sibulesky L, Bulatao IG, Nguyen JH, Taner CB.Shoulddonationaftercardiacdeathlivergraftsbeusedforretransplantation?AnnHepatol.2011;10(4):482-5.
15. DutkowskiP,OberkoflerCE,SlankamenacK,PuhanMA,SchaddeE,MullhauptB, etal.Are therebetterguidelines forallocation in liver transplantation?Anovel score targeting justice and utility in the model for end-stage liverdiseaseera.AnnSurg.2011;254(5):745-53;discussion53.
16. MoonHH,KimTS,SongS,ShinM,ChungYJ,LeeS,etal.EarlyVsLateLiverRetransplantation: Different Characteristics and Prognostic Factors.TransplantProc.2018;50(9):2668-74.
17. YooPS,UmmanV,Rodriguez-DavalosMI,EmreSH.Retransplantationof theliver: review of current literature for decision making and technicalconsiderations.TransplantProc.2013;45(3):854-9.
18. Landelijk Overleg Uitname Teams (LORUT) oacotDTSNatDTFN. NationalProtocolPostMortemDonorOrganProcurement.2018.
19. TaylorR,AllenE,Richards JA,GohMA,Neuberger J,CollettD,etal.Survivaladvantage for patients accepting the offer of a circulatory death livertransplant.JHepatol.2019.
20. DetryO,DerooverA,MeurisseN,HansMF,DelwaideJ,LauwickS,etal.Donorageasariskfactorindonationaftercirculatorydeathlivertransplantationinacontrolledwithdrawalprotocolprogramme.BrJSurg.2014;101(7):784-92.
21. Schlegel A, Scalera I, Perera M, Kalisvaart M, Mergental H, Mirza DF, et al.Impactofdonorageindonationaftercirculatorydeathlivertransplantation:Isthecutoff"60"stillofrelevance?LiverTranspl.2018;24(3):352-62.
22. DariusT,MonbaliuD,JochmansI,MeurisseN,DesschansB,CoosemansW,etal.Septuagenarianandoctogenariandonorsprovideexcellentlivergraftsfortransplantation.TransplantProc.2012;44(9):2861-7.
23. SinghalAK,ShengX,DrakosSG,Stehlik J. Impactofdonorcauseofdeathontransplant outcomes: UNOS registry analysis. Transplant Proc.2009;41(9):3539-44.
24. Rabelo AV, Bastante MD, Raya AM, Méndez CSM, Ramirez ARG, Suarez YF.Liver Transplantation Results by Donor Age. Transplantation Proceedings.2016;48(9):2994-6.
25. GabaRC,KnuttinenMG,BrodskyTR,PalestrantS,OmeneBO,OwensCA,etal.Hepaticsteatosis:correlationsofbodymassindex,CTfatmeasurements,andliverdensitywithbiopsyresults.DiagnIntervRadiol.2012;18(3):282-7.
26. WuC,LuC,XuC.Short-termandlong-termoutcomesoflivertransplantationusing moderately and severely steatotic donor livers: A systematic review.Medicine(Baltimore).2018;97(35):e12026.
27. VanReevenM,VanLeeuwenOB,FujiyoshiM,DeKleineRHJ,DeBoerMT,DeJonge J, et al. Donor hepatectomy time in donation after circulatory deathdonorsisanindependentriskfactorfordevelopmentofbiliarystricturesandearlygraftlossaftertransplantation.ILTSAnnualCongres.Lisbon;2018.
28. Gilbo N, Fieuws S, Meurisse M, Pirenne J, Jochmans I, Monbaliu D. Donorhepatectomytimeandimplantationtimeincreasetheriskofnon-anastomoticbiliarystricturesandallograftdysfunctionafter livertransplantation. ESOT.Copenhagen;2019.
29. DutkowskiP,PolakWG,MuiesanP,SchlegelA,VerhoevenCJ,ScaleraI,etal.First Comparison of Hypothermic Oxygenated PErfusion Versus Static ColdStorage of Human Donation After Cardiac Death Liver Transplants: AnInternational-matched Case Analysis. Ann Surg. 2015;262(5):764-70;discussion70-1.
30. van Rijn R, KarimianN,Matton APM, Burlage LC,WesterkampAC, van denBerg AP, et al. Dual hypothermic oxygenated machine perfusion in livertransplantsdonatedaftercirculatorydeath.BrJSurg.2017;104(7):907-17.
31. Boteon YL, Boteon AP, Attard J,Wallace L, Bhogal RH, Afford SC. Impact ofmachine perfusion of the liver on post-transplant biliary complications: Asystematicreview.WorldJTransplant.2018;8(6):220-31.
Hypothermicoxygenatedmachineperfusionreducesbileductreperfusioninjuryaftertransplantationofdonationaftercirculatorydeathlivers
RiannevanRijn,OttoB.vanLeeuwen,AlixP.M.Matton,LauraC.Burlage,MariusC.vandenHeuvel,RubenH.J.deKleine,MariekeT.deBoer,AnnetteS.H.Gouw,RobertJ.Porte.LiverTranspl.2018May;24(5):655-664
6
INTRODUCTION
Theworldwideshortageofdonorliversfortransplantationhasledtoeffortstoincrease
thenumberofavailablegrafts.IncountriessuchastheNetherlands,SpainandtheUK,
thishasledtoamorefrequentuseofdonationaftercirculatorydeath(DCD)liversfor
transplantation.1,2Unfortunately,DCDlivergraftshavea3-foldhigherriskofdeveloping
non-anastomotic biliary strictures (NAS) after transplantation, compared to donation
afterbraindeath(DBD)livergrafts.ThereportedincidenceofNASrangesbetween16-
31% in DCD versus 3-13% in DBD liver grafts.3-5 This type of biliary complication is
regarded as amajor complication after DCD liver transplantation as it often requires
multiple endoscopic interventions and leads to re-transplantation in 16% of patients
anddeathin6%.6,7
Although the etiology of NAS is not fully understood, the duration of cold andwarm
ischemiaduringtransplantationhasbeenrecognizedasamajorriskfactorforNAS.8-10
Ischemic conditions lead to a complex cascade of events resulting in ischemia-
reperfusion(IR)injury.11Threeindependentclinicalstudiesrecentlydemonstratedthat
themajorityofdonor livershavehistologicalevidenceofextensivebiliary IR injuryat
the time of transplantation.12-14 Especially the degree of biliary epithelial loss, mural
necrosis,andinjuryofthedeepperibiliaryglands(PBG)andperibiliaryvascularplexus
(PVP)at thetimeof transplantationhasbeenassociatedwiththedevelopmentofNAS
after transplantation.12-14 The PBG contain biliary stem/progenitor cells that are
involvedintheregenerationandrepairofthebileductepitheliumaftersevereinjury.15-
17 Therefore, it has been hypothesized that reduced regenerative capacity of the bile
ductsduetodamageofthePBGplaysanimportantroleinthedevelopmentofNASafter
transplantation.14,18
Ashortperiodofhypothermicmachineperfusion(HMP)afterconventionalstaticcold
storage(SCS)hasbeenshowntoreduceIRinjuryofdonorlivers.19,20End-ischemicHMP
results inareductionofhepatocyteapoptosisandnecrosis,mitochondrialandnuclear
injury, endothelial injury, Kupffer cell activation, and the subsequent host immune
response.19,23Furthermore,animalstudieshavesuggestedthatHMPreducesIRinjuryof
thebileducts,asindicatedbyanimprovedbiliaryepithelialcellfunction,reducedbiliary
injury markers, and less histological bile duct wall necrosis, epithelial cell loss, and
arteriolonecrosisofthePVP,comparedtoSCSalone.24-26Thefirstclinicalseriesofend-
ischemic HMP have demonstrated that this method is safe and may lead to a lower
incidenceofbiliarycomplicationsaftertransplantation.27-31
Despite the recognizedbeneficial effect ofHMPon IR injury and a suggested reduced
riskofNASaftertransplantation,therearenostudiesthathaveexaminedtheeffectof
HMP on IR injury of human bile ducts. In the present study, we aimed to determine
whetherdualoxygenatedHMP(DHOPE)reducesreperfusioninjuryofthebileductsin
DCDlivertransplantation,byperformingasystematichistologicalcomparisonofdonor
bileductsbeforeandaftergraftreperfusion.
MATERIALS&METHODS
Studypopulation
Arecentlyperformedphase1studyinourcenterincludedtenconsecutivepatientswho
underwentDCD liver transplantationbetweenAprilandNovember2014.31Thedonor
livers were preserved with DHOPE for two hours after conventional SCS. Informed
consent for DHOPE was obtained. The study protocol conformed to the ethical
guidelinesofthe1975DeclarationofHelsinkiandwasapprovedbytheMedicalEthics
CommitteeoftheUMCG(approvalnumberMETc2014.100).
AcontrolgroupconsistedofpatientswhounderwentDCDlivertransplantation inour
centerbetweenFebruary2012andSeptember2015.Allpatientswithavailablebileduct
biopsieswereincludedinthecontrolgroup.Nopatientswereexcludedfromthecontrol
group.
Studyprotocol
AllDCDliverswereprocuredbyoneoftheregionalmulti-organrecoveryteamsusinga
rapidprocurementprotocolwithaorticcoldflush-outandsubsequentSCS.Uponarrival
in our center, the liver was inspected and prepared for perfusion by placement of
cannulas in theportal vein andaorta.The cannulaswere connected to thedisposable
tubing set of the Liver Assist device (Organ Assist, Groningen, The Netherlands). The
liverswereperfusedforatleasttwohourswith4LofUWMachinePerfusionSolution
(Bridge-to-Life Ltd, Norfolk, UK) at a temperature of 10-12 °C. Two rotary pumps
enabled pressure-controlled perfusion with pulsatile mean arterial pressure of 25
mmHg and a continuous portal pressure of 5 mmHg. The perfusion solution was
oxygenatedbytwohollowfibermembraneoxygenatorswith100%FiO2at500ml/min
peroxygenator.
Bileductbiopsies
Bileductbiopsieswereobtainedfromthecommonbileduct,asdescribedpreviously.14
The biopsies were at the end of SCS (baseline) and after graft reperfusion in the
recipient, short before constructing the bile duct anastomosis. Baseline biopsieswere
collectedafterSCSduringthebacktableprocedure,whichwasfollowedbyDHOPE.All
sampleswerefixedin4%formalin,subsequentlyembeddedinparaffinand4µmthick
slideswere stainedwithhematoxylin&eosin (H&E).The slideswere examinedusing
lightmicroscopyandscannedwithaHamamatsudevice.
Histologicalgradingofbiliaryinjury
Biliary injury was graded according to an established semi-quantitative histological
gradingsystemdescribedbyHansenetal.andmodifiedtoOpdenDriesetal.13-14(Table
1). Biopsies were scored separately by two investigators without knowledge of the
clinical data (RvR and OBvL) under supervision of two dedicated liver pathologists
(ASHGandMvdH).Incaseofdiscordantresults,slideswereexaminedbyathird
Table1:Histologicalgradingofbileductinjury
Item HistologicalCharacteristic
Grading
1. Biliary epitheliumloss
Absenceofepithelialcellsliningthebileductlumen
0:noloss1:≤50%ofthebileductwithabsentepitheliallining2:>50%
2.Muralstromanecrosis
Necrosisofthebileductwall
0:nonecrosis1:≤25%ofthewallnecrotic2:>25%and≤503:>50and≤754:>75%
3.Peribiliaryvascularplexusdamage
Damagetothevesselssuchassubendothelialedema
0:novascularlesions1:≤50%ofthevesselsdamaged2:>50%
4.Arteriolonecrosis Lossofendothelialnucleiofarteriolesandmediadegeneration
0:noarteriolonecrosis1:≤50%ofthearteriesnecrotic2:>50%
5.Thrombosis Presenceofmicro-thrombi
0:nomicrothrombi1:microthrombipresent
6.Intramuralbleeding
Presenceoferythrocytesinthebileductwall
0:nobleeding1:≤50%ofthebileductwall2:>50%
7.PeriluminalPBGloss
AbsenceofepithelialcellsinthePBGclosetothelumen
0:noloss1:≤50%loss2:>50%loss
8.DeepPBGloss AbsenceofepitheliuminthePBGlocateddeepinthebileductwall
0:noloss1:≤50%loss2:>50%loss
Abbreviations:PBG;peribiliaryglands.
Statisticalanalyses
Continuousvariableswerepresentedasmedian(interquartilerange)ormean(standard
deviation) when appropriate and were compared between groups with the 2-tailed
Mann-Whitney test.Categoricalvariableswerepresentedasnumber (percentage)and
compared between groupswith the Pearson chi-square test or the Fisher’s exact test
whereappropriate.Pvalues< .05weredefinedassignificant.Statisticalanalyseswere
performedusingSPSSversion22.0forWindows.
RESULTS
Donorandrecipientcharacteristics
BetweenAprilandNovember2014, tenpatientswere included in theDHOPEphase1
trial. Detailed clinical results have been reported previously.31 The control group
consistedof twentypatientswhopreviouslyunderwentaDCDliver transplantation in
our center and in whom bile duct biopsies were obtained during the transplant
procedurebetween2012and2014.Baselineclinicalcharacteristicsaresummarizedin
Table2.TheEurotransplantdonor risk index (ET-DRI)was similar in theDHOPEand
the control group. Thedonors in theDHOPE grouphad a higher latest serumalanine
aminotransferase(ALT)andpeakserumALTconcentration,comparedtothedonorsin
thecontrolgroup:latestALT72U/L(39-125U/L)vs.29U/L(19-46U/L),respectively
(P= .008);peakALT121U/L(42-271U/L)vs.33U/L(20-46U/L), respectively (P<
.001). The cold ischemia time was shorter in the DHOPE group, but the total
preservation time in theDHOPEgroupwas longer than in thecontrolgroup:521min
(469-592min)vs.430min(407-485min),respectively(P=.002).
Table2:Donorandrecipientcharacteristics
Characteristic DHOPEgroup
(n=10)
Controlgroup
(n=20)
Pvalue
Donorcharacteristics
Eurotransplantdonorriskindex* 2.30(1.81-2.53) 2.22(1.67-2.54) .98
Age(years) 53(47-57) 49(34-55) .18
BMI(kg/m2) 23.0(24.1-19.9) 23.6(22.0-26.0) .25
LatestALT(U/L) 72(39-125) 29(19-46) .008
PeakALT(U/L) 121(42-271) 33(20-46) .004
LatestGGT(U/L) 50(19-102) 39(17-70) .75
Preservationcharacteristics
Preservationfluid(UWvs.HTK) 10(100%) 18(90%) .54
Asystoletime(min)# 15(13-17) 15(12-19) .95
Donorwarmischemiatime(min)^ 26(23-42) 33(29-41) .35
Coldischemiatime(min)** 358(314-398) 426(402-485) .002
Totalpreservationtime(min)## 521(469-592) 430(407-485) .002
Anastomosistime(min)^^ 34(30-49) 33(31-43) .88
Recipientcharacteristics
Age(years) 57(54-62) 55(47-63) .50
Sex(male) 6(60%) 9(45%) >.99
MELDscore*** 16(15-22) 20(13-24) .56
Underlyingdisease: .08
Alcoholiccirrhosis 3(30%) 3(15%)
NASH 5(50%) 3(15%)
Primarysclerosingcholangitis 1(10%) 4(20%)
Primarybiliarycirrhosis 0 0
Autoimmunehepatitis 0 3(15%)
HepatitisBorC 1(10%) 1(5%)
Hepatocellularcarcinoma 0 0
Cryptogenic 0 3(15%)
Other 0 4(20%)
*Eurotransplantdonorriskindexisavalidatedtooltoassesstheriskoflivergraftfailure
(37).#Asystoletimewasdefinedastimebetweencirculatoryarrestandinsituaorticcold
flush.^Donorwarmischaemiatimewasdefinedasthetimeintervalbetweenwithdrawal
ofdonor life supportand initiationof in situaortic cold flush. ** Cold ischemia timewas
defined as the interval between start aortic cold flush and end of static cold storage
excluding thedurationofDHOPE. ##Totalpreservation timewasdefinedas the interval
between start aortic cold flush in the donor and portal reperfusion in the recipient. ^^
Anastomosis time was defined as the interval between donor liver out of ice and
revascularization. ***MELDscorewasdefinedas thehighestof laboratoryderivedMELD
score or the (non) standard exception MELD score. Abbreviations: ALT, alanine
aminotransferase; DCD, donation after circulatory death; GGT, gamma-glutamyl
transferase; DHOPE, dual hypothermic oxygenated machine perfusion; HTK, histidine-
tryptophan-ketoglutarate;MELD,model for end stage liver disease;NASH, non-alcoholic
steatohepatitis;UW,UniversityofWisconson.
Histologicalevidenceofbileductinjury
Theresultsbileductinjuryscoringsbasedonthesemi-quantitativehistologicalgrading
systemaresummarizedinTable3.Therewerenodiscordantresultsbetweenthetwo
investigators.Asexpected,atbaselinetherewerenosignificantdifferencesbetweenthe
twogroupsforanyitemofthehistologicalgradingsystem(Fig.1).Inthecontrolgroup,
the histological bile duct damage after reperfusionwasmore severe than at baseline.
Especially the degree of mural stroma necrosis and the degree of deep PBG injury
increasedafterreperfusion(P=.002andP=.02,respectively).Incontrasttothecontrol
group, there was no increase in the severity of histological biliary injury after
reperfusionintheDHOPEgroup(Table3).
Whencomparingtheseverityofpost-reperfusionbileductinjurybetweenthetwostudy
groups,liversintheDHOPEgroupdisplayedsignificantlylessinjuryandlossofcellsin
theperiluminal(P=.04)andthedeepPBG(P=.04),comparedtocontrols(Fig.1-3).No
differenceswereobservedintheseverityofarteriolonecrosis,stromanecrosis,orinjury
ofthePVPbetweenthetwogroupsafterreperfusion.
Fig.1.DegreeofinjuryofthebileductsofDCDliverstreatedwithDHOPEversus
controls after static cold storage and after reperfusion in the recipient. (A) The
degreeofmural stromanecrosis increasedafterreperfusioncompared tobaseline in the
controlgroup(P<.001),butnotintheDHOPEgroup.(B)Nodifferenceswereobservedfor
the degree of injury of the peribiliary vascular plexus. (C) The periluminal PBG of livers
treatedwithDHOPEdemonstratedlessinjuryafterreperfusionthaninthecontrolgroup
(P = .04). Additionally, the injury of the deep PBG in the control group increased after
reperfusion compared to baseline (P= .02). (D) ThedeepPBG in the livers treatedwith
DHOPEdemonstrated lessdamageafter reperfusion than in the controlgroup (P= .04).
Asterisks indicatedaPvalue< .05.Abbreviations:DCD,donationaftercirculatorydeath;
DHOPE, dual hypothermic oxygenated machine perfusion; PBG, peribiliary glands; PVP,
peribiliaryvascularplexus
Fig.2.RepresentativehistologicexamplesofperiluminalPBGinthecommonbile
duct. (A) Bile duct at baseline of a DCD liver in the DHOPE group. (B) Bile duct after
reperfusionofaDCDliverintheDHOPEgroup.(C)BileductatbaselineofaDCDliverin
thecontrolgroup.(D)BileductafterreperfusionofaDCDliverinthecontrolgroup.The
insertrepresentsahighermagnificationoftheperiluminalPBG(400x).Bileductsoflivers
preserved with DHOPE displayed significantly less epithelial cell loss of the periluminal
PBG, compared to control livers. Original magnification was 200x. Arrows indicate
periluminalPBG.Asterisks indicate lumenof thebile duct. Abbreviations:DCD, donation
after circulatory death; DHOPE, dual hypothermic oxygenated machine perfusion; PBG,
peribiliaryglands.
Fig.3.RepresentativehistologicexamplesofdeepPBGinthecommonbileductof
DCD livergrafts.(A)BileductatbaselineofaDCD liver in theDHOPEgroup.(B)Bile
ductafterreperfusionofaDCDliverintheDHOPEgroup.(C)BileductatbaselineofaDCD
liver in the control group. (D) Bile duct after reperfusion of a DCD liver in the control
group. The insert represents a higher magnification of the deep PBG (400x). Arrows
indicate deep PBG. Asterisks indicate the lumen of the bile duct. Bile ducts of livers
preserved with DHOPE displayed significantly less epithelial cell loss of the deep PBG,
comparedtocontrollivers.Originalmagnificationwas200x.Abbreviations:DCD,donation
after circulatory death; DHOPE, dual hypothermic oxygenated machine perfusion; PBG,
peribiliaryglands.
Table3:Comparisonofhistologicalbileductinjury
Bileductwall
component
DHOPEgroup Controlgroup
Baseline
After
reperfusion
P
value
Baseline After
reperfusion
P
value
Biliaryepitheliumloss >.99 -
Grade0 - - - -
Grade1 10% 14% - -
Grade2 90% 86% 100% 100%
Muralstromanecrosis .25 .002
Grade0 90% 57% 50% 9%
Grade1 - - 43% 9%
Grade2 10% 29% - 36%
Grade3 - 14% 7% 46%
Peribiliaryvascular
plexusdamage
.38 .72
Grade0 50% 57% 43% 36%
Grade1 50% 29% 43% 36%
Grade2 - 14% 14% 28%
Arteriolonecrosis >.99 .57
Grade0 90% 100% 93% 82%
Grade1 10% - - -
Grade2 - - 7% 18%
Thrombosis >.99 >.99
Grade0 90% 100% 93% 91%
Grade1 10% - 7% 9%
Intramuralbleeding - .11
Grade0 100% 100% 100% 73%
Grade1 - - - 18%
Grade2 - - - 9%
PeriluminalPBGloss .24 .23
Grade0 - 14% - -
Abbreviations:DHOPE,dualhypothermicoxygenatedmachineperfusion;PBG,peribiliary
glands;SCS,staticcoldstorage.
Clinicaloutcomes
Theoverall clinical outcomeafter transplantationof thepatients in theDHOPEgroup
hasbeendescribedindetailpreviously.31Completeone-yearfollowupwasavailablein
allpatients.TheincidenceofNASwas10%intheDHOPEgroupand35%inthecontrol
group (P = .15). One recipient of a DHOPE preserved liver developed local NAS in
segment2and3of the liver,whichwassuccessfully treatedwithendoscopicstenting.
None of the patients in the DHOPE groups required re-transplantation for NAS. In
contrast,4(20%)inthecontrolgrouprequiredre-transplantationinforNAS.
DISCUSSION
In the current study, we aimed to determine whether end-ischemic oxygenated
hypothermicmachineperfusion(DHOPE)ofhumanDCDlivergraftsreducesIRinjuryof
the bile ducts after transplantation. The results of this study clearly demonstrated a
reduction inbiliary IR injuryofDHOPE-preservedDCD livers, compared toDCD livers
that did not undergo DHOPE. These findings provide important new insight in the
protective mechanism of end-ischemic DHOPE and are in line with the clinically
observedreductionintheincidenceofNASafterDCDlivertransplantationwhenDHOPE
isapplied.27-31
Grade1 30% 29% 21% -
Grade2 70% 57% 79% 100%
DeepPBGloss .64 .02
Grade0 40% 43% 36% -
Grade1 40% 43% 64% 73%
Grade2 20% 14% - 27%
Inaccordancewithpreviousreports,12-14allDCDliversincludedinthisstudydisplayed
histologicalsignsofsubstantialbileductinjuryattheendofSCS.Asexpected,thedegree
ofbileductinjuryafterSCS(baseline)wasnotdifferentbetweenliversthatunderwent
DHOPEornot.IncontrolliversthatwerenottreatedwithDHOPE,thedegreeofbiliary
injury worsened after graft reperfusion in the recipient, a phenomenon that was not
observed inDHOPEpreserved livers.Especially, theseverityofmuralstromanecrosis
andinjuryofthedeepperibiliaryglandsincreasedafterreperfusionofthecontrollivers,
but not of theDHOPEpreserved livers.When comparing post-reperfusion biopsies of
bileductsofDHOPE-preserved liversandcontrols, significantly lesshistological injury
ofboththeperiluminalanddeepPDGwasfoundintheDHOPEgroup.
In a large clinical study including 128 liver transplant recipients we have previously
shownthattheseverityofbileductinjuryattheendofSCSisastrongriskfactorforthe
development of NAS after transplantation.14 Upon reperfusion of a liver graft in the
recipient, the degree of biliary injury increases further and this may result in
irreversible damage of essential components of the bile duct wall, such as themural
stroma, peribiliary vasculature, and PBG.12,14 Obviously, end-ischemic DHOPE cannot
haveaprotectiveeffectonbiliaryinjurythatisalreadypresentafterSCS.However,the
currentstudyindicatesthatDHOPEdoespreventfurtherworseningofbileductinjury
aftergraftreperfusion.
It is well known that the majority of tissue damage due to IR injury occurs in the
reperfusionperiodafterrestorationofbloodflowtothegraft.11Someofthekeyfactors
in IR injury are the depletion of cellular energy content (especially intracellular
adenosinetriphosphate(ATP))andtheformationofreactiveoxygenspecies(ROS)due
tomitochondrial dysfunction.11,32WhileROS formation results in oxidative damage of
cellularstructures,suchascellmembranesandnuclearDNA,depletionandinsufficient
restorationofATPresultsincelldeathduetoinsufficientmetabolicfunction.Although
the conditions for IR injury are generated during cold ischemic preservation, the
sequelaeofeventsthatleadtothefullblownIRinjuryisnotactivateduntilafterwarm
reperfusion.11Experimentalandclinicalstudieshavedemonstratedthatoneofthekey
protective mechanisms of hypothermic oxygenated machine perfusion is a full
restoration of cellular ATP content and “resuscitation” ofmitochondria, resulting in a
significantreductionofROSproductionaftersubsequentwarmgraftreperfusioninthe
recipient.21,22,33,34 In addition, and downstream of this, oxygenated HMP results in a
reductionofKupffercellactivationandlesssecondaryactivationoftheinnateimmune
system.21,22,33,34 Altogether, these protective effects have been shown to result in a
reductionofhepatocellularIRinjury.OurdataonthereductionofbiliaryIRinjuryarein
linewiththesepreviousstudiesanddemonstratethatnotonlyhepatocellularIRinjury,
butalsoIRinjuryofthebileductsisattenuatedbyoxygenatedHMP.
TheDHOPE-preservedliversinthepresentstudydemonstratedsignificantlylesssevere
injuryofthedeepandperiluminalPBGafterreperfusion,comparedtothecontrollivers
that did not undergo DHOPE. This histological finding is clinically relevant since the
PBGshavebeenidentifiedasa localnicheofbiliaryprogenitorcells thatcontributeto
theregenerationofbiliaryepitheliumafterinjury.15-17,35SevereinjuryofthedeepPBGat
the time of transplantation is a significant risk factor for the development of NAS.14
Therefore, the protective effect of DHOPE on PBG may lead to better preserved
regenerative biliary capacity followed by a reduction of the incidence of NAS. This is
supportedbythe(non-significant)lowincidenceofNASobservedaftertransplantation
of DCD livers preserved with HMP in the first clinical series.27-31 However, formal
evidence that oxygenated HMP reduces the incidence of NAS should come from an
adequatelypoweredrandomized,controlled trial.Suchamulticenter trialhasrecently
been initiated in transplant centers in the Netherlands, Belgium and United Kingdom
(ClinicalTrials.govNCT02584283).
Bile duct biopsies in this studywere obtained from the extrahepatic bile ducts,while
NASmainlyoccursintheintrahepaticbileducts.However,previousstudieshaveshown
thatthedegreeofinjuryoftheextrahepaticbileductcorrelateswellwiththedegreeof
injury of the intrahepatic bile ducts36 and histological assessment of the extrahepatic
bileductcanpredictthedevelopmentofNAS.14
IncontrasttoapreviousstudyonDHOPEusingaporcineDCDlivermodel,wedidnot
findareduction in thedegreeof injuryof thePVPandarteriolonecrosis in thehuman
liverbileductsafterDHOPE.24Infact,inthecurrentstudywedidnotfindasignificant
increase inthedegreeofPVPinjuryandarteriolonecrosisafterreperfusion,compared
to baseline in both groups. In the current study the post-reperfusion bile duct biopsy
was taken1-2hours after graft reperfusion and this time intervalmayhavebeen too
shortforhistologicallydetectablevascularinjurytodevelop.
Limitations of this study are the sample size and the use of historical controls. The
controlsusedinthishistologicalstudywereslightlydifferentfromtheonesusedinour
previous report on clinical outcome after transplantation of DHOPE-preserved DCD
livers,34becausethecontrolgroupconsistedofallavailableparaffinembeddedbileduct
biopsies fromDCDlivergraftswithoutapplicationofexclusioncriteria.Althoughmost
baselinecharacteristicssuchasET-DRIweresimilarbetweenthetwostudygroups,the
donors in the DHOPE group had significantly higher serum ALT levels, compared to
donors in the control group.AsALT is amarker forhepatocellular injury, theDHOPE
groupconsistedof liverswithslightlymorepre-existing injurythanthecontrolgroup.
Therefore,theobservedbeneficialeffectsofDHOPEmighthavebeenmorepronounced
if the ALT levels would have been equivalent between the groups. As expected, the
preservationmethod DHOPE affected the length of preservation periods in the study
groups resulting ina longer totalpreservation timeandshorter cold ischemia time in
theDHOPEcomparedtothecontrolgroup.Intheinterventiongroupthedonorliveris
machine perfusedwhile the recipient surgery is performed. In the control group, the
donorliverremainsintheiceboxduringthisperiod.Theshortercoldischemiatimein
theDHOPE groupmay have caused an advantage,while the longer total preservation
timemayhavecausedadisadvantage.However,themediandifferenceincoldischemia
timewasonly30minutesandbaseline levelsofbileduct injuryweresimilarbetween
thegroups.
Inconclusion,thisstudydemonstratesthatDHOPEattenuatesIRinjuryofthebileducts
after transplantation ofDCD liver grafts. In particular, DHOPE contributed to a better
preservation of the PBG and, as such, may preserve the regenerative capacity of the
donorbileductsleadingtoareducedriskofbiliarycomplicationsaftertransplantation.
REFERENCES
1. NHS Blood and Transplant. Organ Donation and Transplantation; ActivityReport 2015-2016. Accessible via http://www.odt.nhs.uk/uk-transplant-registry/annual-activity-report/
2. Dutch Transplant Foundation. Annual report 2015. Access viahttp://www.transplantatiestichting.nl/winkel/nts-jaarverslag-2015
3. denDulkAC,SebibKorkmazK,deRooijBJ,SuttonME,BraatAE,IndersonA,et al. High peak alanine aminotransferase determines extra risk fornonanastomotic biliary strictures after liver transplantation with donationaftercirculatorydeath.TransplInt2015;28:492-501.
4. DubbeldJ,HoekstraH,FaridW,RingersJ,PorteRJ,MetselaarHJ,etal.Similarliver transplantation survival with selected cardiac death donors and braindeathdonors.BrJSurg2010;97:744-753.
5. O'NeillS,RoebuckA,KhooE,WigmoreSJ,HarrisonEM.Ameta-analysisandmeta-regressionofoutcomesincludingbiliarycomplicationsindonationaftercardiacdeathlivertransplantation.TransplInt2014;27:1159-1174.
6. Blok JJ, DetryO, PutterH,Rogiers X, PorteRJ, vanHoekB, et al. Long-termresults of liver transplantation from donation after circulatory death. LiverTranspl2016;22:1107-1114.
7. VerdonkRC,BuisCI,PorteRJ,vanderJagtEJ,LimburgAJ,vandenBergAP,etal. Anastomotic biliary strictures after liver transplantation: causes andconsequences.LiverTranspl2006;12:726-735.
8. Detry O, Donckier V, Lucidi V, Ysebaert D, Chapelle T, Lerut J, et al. Livertransplantation from donation after cardiac death donors: initial Belgianexperience2003-2007.TransplInt2010;23:611-618.
9. Gilbo N, Jochmans I, Sainz M, Pirenne J, Meurisse N, Monbaliu D. ReducingNon-AnastomoticBiliaryStricturesinDonationAfterCirculatoryDeathLiverTransplantation:ColdIschemiaTimeMatters!AnnSurg2016;[Epubaheadofprint].
10. TanerCB,BulataoIG,PerryDK,SibuleskyL,WillinghamDL,KramerDJ,etal.Asystoletocross-clampperiodpredictsdevelopmentofbiliarycomplicationsinlivertransplantationusingdonationaftercardiacdeathdonors.TransplInt2012;25:838-846.
11. vanGolenRF, vanGulik TM,HegerM. The sterile immune response duringhepaticischemia/reperfusion.CytokineGrowthFactorRev2012;23:69-84.
12. BrunnerSM, JungerH,RuemmeleP, SchnitzbauerAA,DoeneckeA,KirchnerGI,etal.Bileductdamageaftercoldstorageofdeceaseddonorliverspredictsbiliary complications after liver transplantation. J Hepatol 2013;58:1133-1139.
13. HansenT,HollemannD,PittonMB,HeiseM,Hoppe-LotichiusM,SchuchmannM,etal.Histologicalexaminationandevaluationofdonorbileductsreceivedduring orthotopic liver transplantation--a morphological clue to ischemic-typebiliarylesion?VirchowsArch2012;461:41-48.
14. op den Dries S, Westerkamp AC, Karimian N, Gouw AS, Bruinsma BG,Markmann JF, et al. Injury to peribiliary glands and vascular plexus beforelivertransplantationpredictsformationofnon-anastomoticbiliarystrictures.JHepatol2014;60:1172-1179.
15. CarpinoG,CardinaleV,OnoriP,FranchittoA,BerlocoPB,RossiM,etal.Biliarytreestem/progenitorcellsinglandsofextrahepaticandintrahepticbileducts:ananatomicalinsitustudyyieldingevidenceofmaturationallineages.JAnat2012;220:186-199.
16. DipaolaF,ShivakumarP,PfisterJ,WaltersS,SablaG,BezerraJA.Identificationof intramural epithelial networks linked to peribiliary glands that expressprogenitor cell markers and proliferate after injury in mice. Hepatology2013;58:1486-1496.
17. NakanumaY,HosoM,SanzenT,SasakiM.Microstructureanddevelopmentofthe normal and pathologic biliary tract in humans, including blood supply.MicroscResTech1997;38:552-570.
18. KarimianN,OpdenDriesS,PorteRJ.Theoriginofbiliarystricturesafterlivertransplantation: is it the amount of epithelial injury or insufficientregenerationthatcounts?JHepatol2013;58:1065-1067.
19. Dutkowski P, Graf R, Clavien PA. Rescue of the cold preserved rat liver byhypothermic oxygenated machine perfusion. Am J Transplant 2006;6:903-912.
20. Guarrera JV,Estevez J,Boykin J,BoyceR,Rashid J,SunS,etal.Hypothermicmachineperfusionof liver grafts for transplantation: technicaldevelopmentinhumandiscardandminiatureswinemodels.TransplantProc2005;37:323-325.
21. SchlegelA,KronP,GrafR,DutkowskiP,ClavienPA.Warmvs.coldperfusiontechniquestorescuerodentlivergrafts.JHepatol2014;61:1267-1275.
22. Schlegel A, Rougemont O, Graf R, Clavien PA, Dutkowski P. Protectivemechanisms of end-ischemic cold machine perfusion in DCD liver grafts. JHepatol2013;58:278-286.
23. WesterkampAC,KarimianN,MattonAP,MahboubP,vanRijnR,Wiersema-Buist J, et al. Oxygenated Hypothermic Machine Perfusion After Static ColdStorage ImprovesHepatobiliaryFunctionofExtendedCriteriaDonorLivers.Transplantation2016;100:825-835.
24. OpdenDriesS,SuttonME,KarimianN,deBoerMT,Wiersema-BuistJ,GouwAS, et al. Hypothermic oxygenated machine perfusion preventsarteriolonecrosis of the peribiliary plexus in pig livers donated aftercirculatorydeath.PLoSOne2014;9:e88521.
25. Schlegel A, Graf R, Clavien PA, Dutkowski P. Hypothermic oxygenatedperfusion(HOPE)protectsfrombiliaryinjuryinarodentmodelofDCDlivertransplantation.JHepatol2013;59:984-991.
26. WesterkampAC,MahboubP,Meyer SL,HottenrottM,Ottens PJ,Wiersema-Buist J, et al. End-ischemic machine perfusion reduces bile duct injury indonationaftercirculatorydeathratdonorliversindependentofthemachineperfusiontemperature.LiverTranspl2015;21:1300-1311.
27. DutkowskiP,PolakWG,MuiesanP,SchlegelA,VerhoevenCJ,ScaleraI,etal.First Comparison of Hypothermic Oxygenated PErfusion Versus Static ColdStorage of Human Donation After Cardiac Death Liver Transplants: AnInternational-matchedCaseAnalysis.AnnSurg2015;262:764-771.
28. DutkowskiP,SchlegelA,deOliveiraM,MullhauptB,NeffF,ClavienPA.HOPEfor human liver grafts obtained from donors after cardiac death. J Hepatol2014;60:765-772.
29. Guarrera JV, Henry SD, Samstein B, Odeh-Ramadan R, Kinkhabwala M,Goldstein MJ, et al. Hypothermic machine preservation in human livertransplantation:thefirstclinicalseries.AmJTransplant2010;10:372-381.
30. Guarrera JV, Henry SD, Samstein B, Reznik E, Musat C, Lukose TI, et al.Hypothermic machine preservation facilitates successful transplantation of"orphan"extendedcriteriadonorlivers.AmJTransplant2015;15:161-169.
31. van Rijn R, KarimianN,Matton APM, Burlage LC,WesterkampAC, van denBerg AP, et al. Dual hypothermic oxygenated machine perfusion in livertransplantsdonatedaftercirculatorydeath.BrJSurg2017;104:907-917.
32. Schlegel A, Kron P, Dutkowski P. Hypothermic Oxygenated Liver Perfusion:BasicMechanisms and Clinical Application. Curr Transplant Rep 2015;2:52-62.
33. HenrySD,NachberE,Tulipan J, Stone J,BaeC,ReznikL, et al.Hypothermicmachine preservation reduces molecular markers of ischemia/reperfusioninjuryinhumanlivertransplantation.AmJTransplant2012;12:2477-2486.
34. SchlegelA,KronP,GrafR,ClavienPA,DutkowskiP.HypothermicOxygenatedPerfusion(HOPE)downregulatestheimmuneresponseinaratmodeloflivertransplantation.AnnSurg2014;260:931-938.
35. Irie T, Asahina K, Shimizu-Saito K, Teramoto K, Arii S, Teraoka H. Hepaticprogenitorcellsinthemouseextrahepaticbileductafterabileductligation.StemCellsDev2007;16:979-987.
36. KarimianN,WeederPD,BomfatiF,GouwAS,PorteRJ.Preservationinjuryofthedistalextrahepaticbileductofdonorliversisrepresentativeforinjuryoftheintrahepaticbileducts.JHepatol2015;63:284-287.
37. Braat AE, Blok JJ, Putter H, Adam R, Burroughs AK, Rahmel AO, et al. TheEurotransplant donor risk index in liver transplantation: ET-DRI. Am JTransplant2012;12:2789-2796.
Extendedhypothermicoxygenatedmachineperfusionenablesexsitupreservationofporcineliversforupto24hours
IsabelM.A.Brüggenwirth,OttoB.vanLeeuwen,YvonnedeVries,SilkeB.Bodewes,JelleAdelmeijer,JannekeWiersema-Buist,TonLisman,PauloN.Martins,VincentE.deMeijer,RobertJ.Porte.JHEPRep.2020(inpress)
7
ABSTRACT
Background:End-ischemichypothermicoxygenatedmachineperfusion(HOPE)of the
donor liver for 1-2h mitigates ischemia-reperfusion injury during subsequent liver
transplantation. Extended preservation time can be desired to facilitate difficult
recipienthepatectomyortooptimizelogistics.Wethereforeinvestigatedwhetherend-
ischemicdualHOPE(DHOPE)couldextendpreservationtimeupto24husingaporcine
liverreperfusionmodel.
Methods: Porcine liverswith 30minuteswarm ischemiawere subjected to 2h static
cold storage (SCS), followed by 2h, 6h, or 24h DHOPE (n=6 per group). Subsequent
normothermic reperfusion was performed for 4h using autologous blood. Two livers
preservedby24hSCS servedas additional controls.Aproof of principle confirmation
was carried out in two discarded human livers subjected to extended DHOPE.
Hepatocellular and cholangiocyte injury and function were assessed. Oxidative stress
levelsandhistologywerecomparedbetweengroups.
Results: Perfusion flows remained stableduringDHOPE, regardlessofduration.After
normothermic reperfusion, 24h perfused DHOPE livers had similar lactate clearance,
bloodpH,glucose,andalanineaminotransferaselevels,andbiliarypH,bicarbonate,and
LDHlevels,whencomparedto2hand6hperfusedlivers.Levelsofmalondialdehydeand
high-mobilitygroupbox1 inserumand liverparenchymaweresimilar forallgroups.
Histologicalanalysisofbileductsandliverparenchymarevealednodifferencesbetween
the groups. ExtendedDHOPE in discardedhuman livers preservedhepatocellular and
cholangiocyte functionandhistologyafterreperfusion. Incontrast, liverspreservedby
24hSCSwerenon-functioning.
Conclusion:Extendedend-ischemicDHOPEenabledsuccessfulpreservationofporcine
and discarded human donor livers for up to 24h. Extended DHOPE enables safe
extension of preservation time, which may facilitate logistics of allocation and
transplantation,andfurtherexpandthedonorpool.
INTRODUCTION
Preservation using ex situ machine perfusion has gained considerable interest to
facilitate enhanced utilization of liver grafts for transplantation, albeit with several
technical variations.1 While normothermic machine perfusion (NMP) enables
hepatobiliary viability assessment and therapeutic interventions prior to
transplantation, hypothermic oxygenatedmachine perfusion (HOPE) reconditions the
graftbyinducingahypometabolicstatewhilstrestoringmitochondrialfunctionthrough
delivery of oxygen.1 End-ischemic HOPE is a relatively simple approach. Livers are
preserved by static cold storage (SCS) after procurement and are then subjected to
machineperfusionuponarrivalattherecipientcenter.DynamicpreservationbyHOPE
for1-2hoursissufficienttomitigateorgandamageandrestoremitochondrialfunction
andcellularenergystores,resultinginpostoperativelyreducedgraftfailure.2
Previously, we have shown that a short period (2 hours) of dual HOPE (DHOPE)
improvedhepatobiliaryfunctionanddecreasedinjurytothelivergraftandbiliarytree
in discarded human livers.3,4 In a prospective cohort study, 2 hours of end-ischemic
DHOPEwas shown to be feasible and safe in resuscitating donation after circulatory
death (DCD) liver grafts with 100% one-year graft and patient survival after
transplantation.5 Another important finding was that DHOPE attenuates injury of the
biliarytreeaftertransplantationofDCDlivergraftscomparedtonon-DHOPEpreserved
livers.6 In 2015, our center initiated a large international multicenter randomized
controlledtrialcomparingDHOPEversusSCSinDCDlivertransplantationofwhichthe
firstresultsareexpectedmid2020.7
In addition to graft reconditioning, viability assessment, and potential therapeutic
interventions,machine perfusionmay also have the potential to prolong preservation
time. Traditionally, graft preservation using static cold storage (SCS) may keep good
qualityliversviablefortransplantationforseveralhours.Machineperfusion,however,
may extend preservation times, particularly in extended criteria donor (ECD) organs
which are more vulnerable to cold ischemia.8–10 Extended preservation by HOPE, for
example, could facilitate logistics for allocation and transplantation. As a proof-of-
concept,ahumandiscardedliverhasbeenpreservedfor86hoursusingexsituNMP11,
and an initially declined human liver has successfully been transplanted after
preservationfor26hours,ofwhich17.5hoursSCSand8.5hourswithNMP.12However,
little data are available regarding extended graft preservation by using (dual) HOPE,
and,currently,maximumreportedpreservationtimeusingHOPEis8hours.10,13,14
We investigated the effects of extended preservation by applying end-ischemic dual
HOPE (DHOPE) in a porcine liver ischemia reperfusion injury model. Our endpoints
included graft viability after warm reperfusion and various markers of injury during
machine perfusion, and after warm reperfusion. In addition, a proof of principle
confirmationofend-ischemicDHOPEpreservationwascarriedoutindiscardedhuman
livers.
MATERIALS&METHODS
Porcinedonationaftercirculatorydeathliverprocurement
Livers from 5-month-old white female landrace pigs were retrieved after circulatory
death. Pigs were sacrificed by a standardized procedure of electrocution followed by
exsanguination.2Lofautologousbloodwascollected ina containerwith25,000 IUof
heparin(heparinLEO5000IU/ml,LEOPharmaceuticalProducts,Denmark).Bloodwas
then stored in bags supplemented with the anticoagulant citrate-phosphate-dextrose
(Sanquin, Amsterdam, the Netherlands) and cold stored (4°C) until subsequent use.
Within30minutesaftercirculatorydeath, liverswereflushedbygravityviatheportal
vein with 1L of cold (4°C) NaCl 0.9% (Baxter BV, Utrecht, the Netherlands)
supplementedwith25,000IUofheparin,followedby2LofcoldUniversityofWisconsin
(UW)solution(BridgetoLife,Ltd,London,UnitedKingdom).Afterportalflush,theaorta
wascannulated,andsidebrancheswereclippedfollowedbycoldarterialflushoutwith
UWsolutionusingasyringe.Thecysticductwasligated,andthecommonbileductwas
cannulatedwithabilecannula(8Fr,OrganAssist,Groningen,theNetherlands).Livers
werestaticcoldstored(4°C)inUWsolutionfor2hours.Theporcineliversusedinthe
present study were retrieved from a slaughterhouse (Kroon, Groningen, the
Netherlands)wherehumanecircumstancesareappliedaccordingtonationallegislation.
According to the Dutch law, no institutional approval is needed when using a
slaughterhousemodel.
Dualhypothermicoxygenatedmachineperfusion(DHOPE)
AfterSCS,graftswererandomlyassignedtoeither2hDHOPE(DHOPE-2),6h(DHOPE-
6), or 24h DHOPE (DHOPE-24) (n=6 per group). Machine perfusion was performed
usingtheLiverAssistdevice(OrganAssist,Groningen,theNetherlands).15Liverswere
perfusedwith 2L Belzer UWmachine perfusion solution (Bridge to Life, Ltd, London,
UnitedKingdom),oxygenatedwith100%O2.Temperaturewasmaintainedbetween8–
10°C. Pressures were limited to 25 mmHg in the hepatic artery and 3 mmHg in the
portalvein.Perfusatesampleswerecollectedfromthearterialinflowcannulaattheend
of preservation. Liver tissue sampleswere obtained after procurement, at the end of
DHOPEpreservation,andattheendofwarmreperfusion.
Exsitunormothermicoxygenatedwholebloodreperfusion
After extended DHOPE preservation for 2h, 6h, or 24h, liver grafts were flushed by
gravitywith1Lofcold(4°C)salinesolutionand1Lofsalineatroomtemperature.Livers
were then transferred to a second Liver Assist device and reperfused at 37°C with
autologouswhole blood.Whole bloodwas used during this phase to simulate clinical
transplantation. Sodium bicarbonate (B. Braun Medical, Melsungen, Germany) was
addedinthefirsthourafterreperfusiontoadjusttoaphysiologicalpH.Thebloodwas
oxygenatedwithacarbogenmixtureof95%O2and5%CO2at1L/min.Theportalvein
was perfused continuously at a pressure of 11 mmHg, and the hepatic artery was
perfusedwithapulsatileflowatameanpressureof70mmHg.Perfusatesampleswere
taken before reperfusion, and at 5, 60, 120, 180, and 240minutes after reperfusion.
Arterial blood gas samples were taken before reperfusion, and every 30 minutes
thereafter. Partial oxygenpressure,Hb, pH, glucose, and lactateweremeasuredusing
thei-STATclinicalanalyzer(AbbotPointofCareInc.,Princeton,NJ).Bileproductionwas
measuredgravimetricallythroughoutreperfusion.Everyhour,bilewascollectedunder
mineral oil, as described previously,16 and biliary pH, bicarbonate and lactate
dehydrogenase (LDH) levels were measured. As controls, two porcine livers were
preserved with static cold storage (4°C) in UW-solution for 24 hours, followed by 4
hoursofnormothermicreperfusionwithwholebloodasdescribedabove.
Outcomes
Hepatocellularinjuryafterwarmreperfusionwasassessedbyalanineaminotransferase
(ALT) levels, using a standardized laboratorymethod. Nuclear subcellular injurywas
measured by release of highmobility group box-1 protein (HMGB-1) using a specific
ELISA (IBL International GmbH, Fujioka, Japan). Cell-freeDNA (cfDNA)was used as a
marker of cell damage and necrosis and measured as described previously.17 Tumor
necrosis factor alpha (TNF�) and interleukin6 (IL-6) levelsweremeasuredbyELISA
(Biotechne, Abingdon, UK). Lipid peroxidation, a marker of oxidative stress, was
quantified by measurement of malondialdehyde (MDA) in the perfusate and liver
biopsies.15MDA levels in liver parenchymawere corrected for the amount of protein
(Bradfordassay,Bio-Rad,Hercules,USA).Inaddition,8-hydroxy-2-deoxyguanosine(8-
OHdG)wasmeasured(FineTest,Wuhan,China)asaproductofoxidativedamageofDNA
by reactive oxygen and nitrogen species. Soluble thrombomodulin (sTM) was
determined using a commercially available enzyme-linked immunosorbent assay
(ELISA)(Biotechne,Abingdon,UK).18Hepaticcontentofadenosinetriphosphate(ATP)
was used as an indicator of energy status of grafts before and after DHOPE. For this
purpose, liverbiopsieswereimmediatelyfrozeninliquidnitrogenandlaterprocessed
forATPmeasurement,asdescribedpreviously.19
Histologicalanalysis
Liver biopsies were fixed in formalin and embedded in paraffin. We performed
hematoxylin-eosin(H&E)stainingtoassessnecrosisandVonWillebrandFactor(VWF)
staining to assess endothelial activation. Quantification of necrosis and VWF-positive
endothelial cells was determined in 3 random visual fields (20x). Biopsies of the
extrahepatic bile ducts were taken after procurement and at the end of reperfusion.
After H&E staining, biliary injury was assessed using a modified scoring system as
describedbyOpdenDries et al.20 Scoringwas conducted in ablinded fashionby two
independentinvestigators.
Humanprotocol
Human application of extended DHOPE was performed as a preclinical study using
discarded human liver grafts. Family of the donors gave consent for research. Donor
liverswerestaticcoldstoredoniceafterprocurementandtransferredtoourhospital.
Tomimicclinicalpracticeatourcenterascloseaspossible,graftsweresubjectedtoour
clinically used DHOPE-COR-NMP protocol.21 Extended 20-hour end-ischemic DHOPE
preservationwas applied using UWmachine perfusion solution. The timeframe of 20
insteadof24hourswaschosenbecauseoflogisticalreasons.AfterDHOPEpreservation,
UWwaschangedtoaperfusionsolutioncontainingahemoglobin-basedoxygencarrier,
as described previously.22 In accordance with our clinical protocol, discarded human
livers subsequently underwent 1 hour of controlled oxygenated rewarming (10°C to
37°C) followed by normothermic (37°C) reperfusion and liver viability testing for an
additional4hours.21
Statistics
All values are expressed asmeans ± standard error of themean for n=6 animals per
group.DifferencesbetweenthegroupsweretestedusingtheKruskal-Wallistestunless
statedotherwise.A two-sidedp-value less than0.05was considered tobe significant.
AnalyseswereperformedusingIBMSPSSsoftwareversion25forwindows.Forfurther
detailsregardingmaterialsandmethodsused,pleaserefertotheCTATtable.
RESULTS
Ischemiatimes
There were no significant differences in warm and cold ischemia times between the
groups.Meanwarmischemiatimewas24±2minutesforDHOPE-2,22±2minutesfor
DHOPE-6,and22±1minutesforDHOPE-24livers(p=0.847).Meancoldischemiatime
was129±11minutesforDHOPE-2livers,122±5minutesforDHOPE-6livers,and122
±5minutesforDHOPE-24livers(p=0.890).
FlowsduringDHOPE
The perfusate temperature was maintained at 10�C throughout all perfusions. In
addition, portal venous and hepatic arterial flows remained stable in all livers
throughoutthepreservationperiod.MeanarterialflowattheendofDHOPEwas104.8±
29.2ml/min in theDHOPE-2 group, 104.3 ± 35.2ml/min in theDHOPE-6 group, and
149.3±41.7ml/minintheDHOPE-24group(p=0.676).Meanportalflowattheendof
DHOPEwas 311.7 ± 49.6ml/min in theDHOPE-2 group, 282.0 ± 72.2ml/min in the
DHOPE-6group,and193.3±16.3ml/minintheDHOPE-24group(p=0.219).
LivergraftandbileductviabilityafterextendedDHOPE
Warmreperfusionwasusedtoassesslivergraftviabilityafterextendedpreservationby
24-hourDHOPE.Portal(Fig.1A)aswellasarterial(Fig.1B)flowssteadilyincreasedin
all liver grafts upon reperfusion. There were no significant differences between the
groups. In all groups, all livers cleared lactate (Fig. 1C). Perfusate pH was adjusted
withinthefirsthourafterreperfusionbyaddingbicarbonate.Therewerenosignificant
differencesintheamountofaddedbicarbonatebetweenthegroups.Afterthefirsthour,
nofurthercorrectionswereneeded,andpHremainedstableduringallliverperfusions
(Fig. 1D). Starting one hour after reperfusion, in all livers perfusate glucose levels
graduallydecreased(Fig.1E).
All livers produced sufficient quantities of bile,without differences in cumulative bile
production (Fig. 2A). In addition, bile duct viability was assessed during 4 hours
normothermicreperfusion.Inallgroups,biliarypHandbicarbonateincreasedduring4
hourswarmreperfusion.LevelsofbiliarypH,bicarbonateandLDHweresimilar inall
groups at the end of reperfusion (Fig. 2B-D). In this porcinemodel of DCD livers,we
observed extensive loss of biliary epithelial lining immediately after procurement (30
minofwarmischemia).Thiswasconsistentwithpreviousfindings.20Attheendofwarm
reperfusion, bile ducts of all livers displayed signs of bile duct injury. Histological
comparisonofbileductsrevealedsimilarinjuryattheendofreperfusioninallgroups
(Fig.2E,Fig.S1).
Figure 1. Perfusion flows and markers of liver function during 4 hours
normothermicreperfusionaftereither2,6,or24hoursDHOPE.(A)Portalvenous
flow,(B)hepaticarteryflow,(C)lactateconcentration,(D)perfusatepH,(E)glucoselevels.
All liversshowgoodliverfunctionduringreperfusionafterpreservationbyeither2,6,or
24hoursDHOPE.Shownherearethemeanandstandarderrorofthemeanforn=6livers
pergroup.Therewerenosignificantdifferencesbetweenthegroupsinallmarkersshown
(Kruskal-Wallistest).DHOPE=dualhypothermicoxygenatedmachineperfusion.
Figure 2. Biliary function during 4 hours normothermic reperfusion. (A)
Cumulativebile productionduring reperfusion, (B)biliarypH, (C) biliarybicarbonateat
the end of reperfusion, (D) biliary LDH at the end of reperfusion. All livers show good
biliary functionafterpreservationby either2, 6, or24hoursDHOPEand therewereno
significantdifferencesbetweenthegroups inallparametersshown(Kruskal-Wallis test).
(E)Histologyof extrahepaticbileducts, *=bileduct lumen,arrow=absenceof luminal
epithelium.Shownhereare themeanand standarderrorof themean forn=6 liversper
group. DHOPE = dual hypothermic oxygenated machine perfusion; LDH = lactate
dehydrogenase.
Next,weinvestigatedthedegreeofhepatocellularinjuryafterDHOPEpreservationfor
2,6and24hours.Weanalyzedseveralmarkersforcellularinjuryattheendof4hours
reperfusion.LevelsofALT(Fig.3A;p=0.687),HMGB-1(Fig.3B;p=0.690),orcfDNA(Fig.
3C; p=0.229) in the perfusate were not elevated by extended DHOPE preservation.
Histological analysis of liver parenchyma revealed that DHOPE preservation up to 24
hours did not result in more necrosis after reperfusion compared to shorter
preservationtimes(Fig.3DandE).
Figure 3. Markers for cellular injury at the end of normothermic reperfusion.
Perfusatelevelsof(A)ALT(p=0.687),(B)HMGB-1(p=0.690),(C)andcfDNA(p=0.229).
There were no statistically significant differences between the groups at the end of
reperfusion (Kruskal-Wallis test). (D) percentage of necrosis on histological analysis of
liverparenchymaafterH&Estaining, (E)H&Estainingof liverparenchyma.Shownhere
are the mean and standard error of the mean for n=6 livers per group. ALT = alanine
aminotransferase;cfDNA=cell-freeDNA;DHOPE=dualhypothermicoxygenatedmachine
perfusion; H&E = hematoxylin and eosin; HMGB-1 = high-mobility group 1; SCS = static
coldstorage.
Since livers were perfused for up to 24 hours with an oxygenated solution, we
investigatedmarkersforoxidativestressattheendofDHOPEpreservationandafter4
hours warm reperfusion. Extended preservation was not associated with increased
levelsofMDAintheperfusateattheendofDHOPE(Fig.4A;p=0.312),nor inbloodat
theendofwarmreperfusion(Fig.4B;p=0.308).ExtendedDHOPEpreservationwasalso
not associated with increased levels of MDA in liver biopsies at the end of DHOPE
(p=0.125), nor at the end of reperfusion (p=0.604) (Fig. 4C). Perfusate 8-OHdG
measuredattheendofwarmreperfusionwassimilarinallgroups(p=0.172)(Fig.4D).
Figure 4. Markers related to oxidative stress at the end of DHOPE and
normothermicreperfusion. (A)MDA inperfusateat the endofDHOPE (p=0.312), (B)
MDAinliverparenchymaattheendofDHOPE(p=0.125)andreperfusion(p=0.604)),(C)
MDA in perfusate at the end of normothermic reperfusion (p=0.308), (D) 8-OHdg in the
perfusate at the end of normothermic reperfusion (p=0.172). Therewere no statistically
significantdifferencesbetweenthegroupsonallparameters(Kruskal-Wallistest).24-hour
DHOPE preservation does not induce oxidative injury compared to shorter preservation
times. Shown here are the mean and standard error of the mean for n=6 animals per
group. 8-OHdG = 8-hydroxydeoxyguanosine; DHOPE = dual hypothermic oxygenated
machineperfusion;MDA=malondialdehyde.
Extended DHOPE preservation was not associated with increased release of
inflammatory cytokines TNF-a and IL-6. Mean TNF-a was 334.4 ± 55.8 pg/ml for
DHOPE2, 252.3 ± 57.8 pg/ml for DHOPE6, and 347.3 ± 123.2 pg/ml for DHOPE24
preserved livers, respectively (p=0.692) (Fig.5A).Mean IL-6was13.9±5.5pg/ml for
DHOPE2,23.9±8.7pg/ml forDHOPE6,and19.7±8.2pg/ml forDHOPE24preserved
livers,respectively(p=0.578)(Fig.5B).Finally,weinvestigatedthedegreeofendothelial
injury after prolonged DHOPE preservation. Levels of soluble thrombomodulin (sTM)
werenotaffectedbyprolongedDHOPE(p=0.985)(Fig.5C). IntensityofVWFstaining
didnotrevealmoreactivationofendothelialcellsonhistologicalanalysis(Fig.5Dand
E).
Figure5.Endothelialcellactivationandlevelsofsolublethrombomodulinduring
reperfusion.(A)TNF-ainperfusate(p=0.692),(B)IL-6inperfusate(p=0.578),(C)soluble
thrombomodulin in perfusate (p=0.985) (D) VWF staining, (E) percentage VWF positive
endothelial cells per high-power field. There were no statistically significant differences
between the groups at the end of reperfusion (Kruskal-Wallis test). Preservation by 24-
hour DHOPE did not induce more injury to endothelial cells compared to shorter
preservation times. DHOPE = dual hypothermic oxygenated machine perfusion; HPF =
high-power field; IL-6= interleukin6;TNF-a= tumornecrosis factoralpha; SCS= static
coldstorage;sTM=solublethrombomodulin;VWF=VonWillenbrandFactor.
24-hourSCSpreservedlivers
Asacontrolgroup,twoporcineliverswerepreservedbySCSfor24hours.Subsequent
warmreperfusionwasperformed for4hours to investigateviability.Macroscopically,
both livers preserved by 24 hours SCS depict large, patchy dark and greyish areas.
During 4 hours warm reperfusion of these grafts, perfusion flow rates gradually
decreased, bile production was absent, pH was decreased to <7.0, and lactate in the
perfusatereached>8mmol/Lat theendofreperfusion.Fig.6AandBdepictaporcine
liver after 24-hours DHOPE preservation, and subsequent 4 hours normothermic
reperfusion with macroscopically normal appearance. In contrast, Fig. 6C shows
normothermic reperfusion after 24-hour preservation by SCS, demonstrating severe
hemorrhagic injury. Because of the severe degree of injury after 24-hours SCS
preservation(i.e.,non-functioninggrafts),a further increase innumberof livers in the
24-hourSCSgroupwasdeemedfutile.
Figure 6. Representative pictures. (A) porcine liver at the end of 24-hour DHOPE
preservation, (B)porcine liverduringreperfusionafter24-hourDHOPEpreservation, (C)
porcineliverduringreperfusionafter24-hourSCSpreservation.Clearly,liverspreservedby
24-hour SCS depict large patchy dark and greyish areas, suggestive of a failing graft.
DHOPE=dualhypothermicoxygenatedmachineperfusion;SCS=staticcoldstorage
HumanpreclinicalexperienceinextendedDHOPE
Finally,we investigatedwhether the observations in our porcinemodel could also be
applied to clinical liver transplantation. Therefore,weperfused twodiscardedhuman
donorliversusingaprotocolcurrentlyusedatourcenter(Fig.7A).21Thefirstliverwas
from a 71-year old DCD donor, with a BMI of 29, history of smoking, macroscopic
hepaticsteatosisof40%,121minutesbetweenwithdrawaloflifesupportanddeath,a
warmischemiatimeof16minutes,and668minutesofSCS.Thesecondgraftwasfroma
59-yearolddonationafterbraindeathdonor,withaBMIof31,ahistoryofsmokingand
hypertension, and a SCS time of 466 minutes. This liver was discarded by another
transplant center because of a macroscopic appearance of poor perfusion, and
subsequently rejected for transplantation nationwide. These human liver grafts were
preserved by traditional SCS during transportation from the donor center and then
subjected to extended DHOPE for 20 hours. After 1 hour of gradual controlled
oxygenatedrewarmingfollowedbyanadditional4hoursofnormothermicreperfusion,
bothgraftsmettheviabilitycriteriathatweuseinourpractice(Fig.7B).Fig.7Bshows
data from our prospective clinical trial, inwhich the greenmargins depict livers that
weredeemedviableafter2.5hoursnormothermic reperfusion.23Thepurpleandblue
lines represent both human livers included in this study. After 2.5 hours reperfusion,
bothliversmettheviabilitycriteria,basedonlactateclearance,thedeltaofbiliaryand
arterial pH, the biliary/arterial glucose ratio, and the delta of biliary and arterial
bicarbonate. Hepatic ATP content was increased 3–5 fold during 20 hours DHOPE
preservation(Fig.7C).PerfusatelevelsofHMGB-1,TNF-a,IL-6,andcfDNAremainedlow
in both livers during the entire period ofDHOPE (Fig. 7C). At the end of reperfusion,
histologyof theextrahepaticbileducts, the intrahepaticbileductsaswell as the liver
parenchyma revealed remarkable preservationwith onlyminor cholangiocellular and
hepatocellularinjury(Fig.7D).
Figure7.24-hourDHOPEpreservationofdiscardedhumanlivergrafts.(A)pictures
of a human liver at the end of DHOPE preservation (left) and during normothermic
reperfusion (right). (B) Markers for graft viability. The green margins depict historical
data of clinically perfused livers thatwere deemed viable after 2.5 hours normothermic
perfusionandthusacceptedfortransplantation.Theredmarginsdepicthistoricaldataof
livers that were deemed non-viable after 2.5 hours reperfusion, which were secondarily
discardedfortransplantation.Thepurpleandbluelinesrepresentthetwoliversincluded
inthisstudy.Bothliversfollowthegreenmargins,indicativeofaviablegraft.Shownare
lactate clearance, the delta of biliary and arterial pH, the biliary/arterial glucose ratio,
and the delta of biliary and arterial bicarbonate. After 2.5 hours, both livers meet the
viability criteria. (C) Hepatic ATP content at the end of DHOPE, and perfusate levels of
HMGB-1, TNF-a, IL-6, and cfDNA during DHOPE preservation. (D) H&E staining of
extrahepatic bile ducts (left), intrahepatic bile ducts (middle), and liver parenchyma
(right),*=bileductlumen.
DISCUSSION
In this studywe have shown that in a porcine DCDmodelwith 30minutes ofwarm
ischemia,liverspreservedbyDHOPEremainedviableforatleast24hours,whereas24-
hourpreservationbySCS resulted innon-viable grafts.24,25DHOPE forup to24hours
appearstobefeasibletoextendexsitulivergraftpreservationtimes.
The results described in this paper provide evidence that DHOPE may substantially
extendliverpreservationtimes.Thesefindingsareimportantforseveralreasons.First,
extendedDHOPEcouldfacilitatelogisticsoforganallocation.Itmaybeusefultoextend
preservation times in cases of suboptimal livers that are more difficult to allocate.
Second,thistechniquecanbefavoredwhenliversneedtobetransportedacrossregions
oflargecountries(e.g.UnitedStates),orbetweencountries(e.g.Eurotransplant).Atthe
same time, it may reduce transportation costs when livers can be shipped with
commercial flights instead of chartered jets. Lastly, storage time can be prolonged in
cases of logistical issues at the recipient center (lack of operating rooms or medical
teams),ortoscheduletransplantationsurgerythenextdayinsteadofduringthenight,
sincethelatterhasbeenassociatedwithagreaterriskofmorbidityandmortality.26
Up to now, it has been shown that short-term (1–2 hours) (D)HOPE prior to
transplantation is an effective approach to mitigate ischemia-reperfusion injury by
slowingdownmitochondrialrespiration.2ThepresentstudyshowsthatDHOPEcanalso
be used to extend preservation times. Only a few studies investigated extended cold
perfusion of donor livers.8,27 Belzer and colleagues were the first who managed to
preserveandtransplantgoodqualitycanineliversafter72-hourhypothermicmachine
perfusion (HMP).8 More than a decade later, Xu et al. published a study on 24-hour
preservationbyHMPinaratreperfusionmodel,butwithoutverygoodresults.27Atthe
endof30minutesreperfusion,LDHwashigherintheHMPgroupcomparedtotheSCS
group, ICG clearance was similar between the groups, and hepatic hyaluronic acid
uptake showed severely impaired hepatic sinusoidal endothelial cells after 24-hour
HMP. Incontrast toourstudy,Xuandcolleaguesdidnotuseanoxygenatedperfusion
solution. It has been shown that complete absence of oxygen during HMP triggers
hepatocyte cell death via mitochondria, and fails to prevent reperfusion injury.2 The
liver is a metabolically high-demanding organ, even under hypothermic conditions.
Therefore, active oxygenation is needed, especially in grafts with more preservation
injury,suchasDCDlivers.2,28,29
A potential disadvantage of HMP is the risk of undesired endothelial injury (shear
stress)intheliversinusoidscausedbyhighervascularresistancesinthecold.30Inour
experiments,we have observed stable perfusion flows during the entire preservation
periodof24hours.Thisisincontrasttowhatotherauthorshavedescribedforextended
HMP.27,31–33 Ifmachine settings are adjustedatportalpressures≤3mmHgandarterial
pressures≤25mmHg,shearstresscanbeavoided.2,34Inthisstudy,usinglowperfusion
pressures,wedidnotobserveactivationofendothelialcells,indicatedbyVWFstaining
aswellaslowlevelsofsTM.sTMisreleasedfromthevascularendotheliumwhenliver
sinusoidsareinjuredby,forexample,graftpreservation.35LevelsofsTMhavealsobeen
correlatedwithelevated liverenzymesand increasedadherenceof leukocytes in liver
tissue.18
Research groupsworld-wide arepushing theboundaries of organpreservation times.
Morerecently,thefeasibilityofextendedpreservationbyNMPwasdemonstrated.11,36,37
The group from Cleveland even shows 86-hour liver perfusion by NMP in a non-
transplantationmodel.11Normothermicconditionsallowtestingoforganviability,butit
alsobearsa riskof severe injuryas theorgan ismuchmoremetabolically active.38 In
addition, normothermic perfusion requires more intensive labor, since the liver
produces waist products and the composition of the perfusate needs continuous
monitoringandadjusting.Hypothermicperfusioncanbeadvantageoussincetheorgan
is in a hypometabolic state with less production of waste products. In addition,
comparedtoNMP,itpreventsgraftlossiftheperfusionsystemfails(thegraftwouldstill
be preserved in SCS). This study shows that temperature can bemaintained at 10°C
without interventions, it does not require an oxygen carrier (e.g. blood), and no
adjustments of the perfusate needed to be done, making it a relatively easy and
substantiallycheaperapproach,whencomparedtoNMP.
Clearlytheseresultsmustbeassessed inthecontextofwhat isanexperimentalstudy
usingporcinelivers.Wedidnotconfirmourfindingsinatransplantationmodel,butan
ex-situ whole blood reperfusion model was used to test liver viability, as done
previously by others.15,39–41 In addition, it was recently shown that 2.5 hours of
normothermicreperfusionissufficienttoassesshepatobiliaryviability.21Itisgenerally
accepted that the pig liver is a very rigorous model of organ preservation, with
maximum successful SCS preservation times that are substantially shorter than those
regularlyachievedinclinicalpractice.36Incombinationwithourpreliminaryresultson
thetwodiscardedhumanlivergrafts,thesearegroundsforoptimismthatcomparable
resultsmaybeachievedintheclinicalsetting.Althoughtheresultsofthecurrentstudy
are encouraging, experimental work with subsequent transplantation to validate this
approach remains necessary. Until then, extended DHOPE should only be performed
withinaresearchsetting.
Inconclusion,thisisthefirststudytoshowsuccessfulextendedpreservationbyDHOPE
ofDCDporcinelivers.Ifconfirmedtotheclinicalsetting,extendedDHOPEcouldbeused
globallytofacilitatetransplantationlogisticsandexpandthedonorpool.
ACKNOWLEDGEMENTS
WearegratefultoArjanvanderPlaats,MartinKuizenga,MarkSlotemaker,andEmma
Offringa (Organ Assist, Groningen, The Netherlands) for their technical support and
assistanceduringtheperfusionexperiments.Wewouldalsoliketothanktheemployees
ofSlagerKroon,Groningen,fortheirwellwillingcooperation.
REFERENCES
1. deMeijerVE,FujiyoshiM,PorteRJ.Exsitumachineperfusionstrategiesinlivertransplantation.JHepatol.2019;70(1):203-205.doi:10.1016/j.jhep.2018.09.019
2. Schlegel A, de Rougemont O, Graf R, Clavien P-A, Dutkowski P. Protectivemechanisms of end-ischemic cold machine perfusion in DCD liver grafts. JHepatol.2013;58(2):278-286.doi:10.1016/j.jhep.2012.10.004
3. Pienaar BH, Lindell SL, Van Gulik T, Southard JH, Belzer FO. Seventy-two-hourpreservation of the canine liver by machine perfusion. Transplantation.1990;49(2):258-260.
4. TamakiT,KamadaN,WightDG,PeggDE.Successful48-hourpreservationoftherat liver by continuous hypothermic perfusion with haemaccel-isotonic citratesolution.Transplantation.1987;43(4):468-471.
5. DeCarlisR,LauterioA,FerlaF,DiSandroS,SguinziR,DeCarlisL.HypothermicMachinePerfusionofLiverGraftsCanSafelyExtendColdIschemiaforUpto20Hours in Cases of Necessity. Transplantation. 2017;101(7):e223-e224.doi:10.1097/TP.0000000000001753
6. Liu Q, Nassar A, Buccini L, et al. Ex situ 86-hour liver perfusion: Pushing theboundary of organ preservation. Liver Transplant. 2018;24(4):557-561.doi:10.1002/lt.25007
7. WatsonCJE,RandleLV.,KosmoliaptsisV,GibbsP,AllisonM,ButlerAJ.26-hourStorage of a Declined Liver Before Successful Transplantation Using Ex VivoNormothermic Perfusion. Ann Surg. 2017;265(1):e1-e2.doi:10.1097/SLA.0000000000001834
8. OpdenDriesS,SuttonME,KarimianN,etal.Hypothermicoxygenatedmachineperfusion prevents arteriolonecrosis of the peribiliary plexus in pig liversdonated after circulatory death. PLoS One. 2014;9(2):e88521.doi:10.1371/journal.pone.0088521
9. MattonAPM,deVriesY,BurlageLC,etal.BiliaryBicarbonate,pHandGlucoseAreSuitable Biomarkers of Biliary Viability During Ex Situ NormothermicMachinePerfusion of Human Donor Livers. Transplantation. November 2018:1.doi:10.1097/TP.0000000000002500
10. vonMeijenfeldtFA,BurlageLC,BosS,AdelmeijerJ,PorteRJ,LismanT.Elevatedplasma levels of cell-free DNA during orthotopic liver transplantation areassociated with activation of coagulation. Liver Transplant. August 2018.doi:10.1002/lt.25329
11. Sido BP, Datsis K, Mehrabi A, et al. Soluble Thrombomodulin—a Marker OfReperfusion Injury After Orthotopic Liver Transplantation. Transplantation.1995;60(5):462-466.
12. SuttonME,opdenDriesS,KarimianN,etal.Criteria forviabilityassessmentofdiscardedhumandonor liversduringexvivonormothermicmachineperfusion.PLoSOne.2014;9(11):e110642.doi:10.1371/journal.pone.0110642
13. opdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsandvascular plexus before liver transplantation predicts formation of non-anastomotic biliary strictures. J Hepatol. 2014;60(6):1172-1179.doi:10.1016/j.jhep.2014.02.010
14. Vries Y, Matton APM, Nijsten MWN, et al. Pretransplant sequential hypo- andnormothermicmachineperfusionof suboptimal liversdonatedaftercirculatorydeath using a hemoglobin-based oxygen carrier perfusion solution. Am JTransplant.2019;19(4):1202-1211.doi:10.1111/ajt.15228
15. vanLeeuwenOB,deVriesY,FujiyoshiM,etal.Transplantationofhigh-riskdonorlivers after ex situ resuscitation and assessment using combined hypo- andnormothermicmachineperfusion:Aprospectivetrial.AnnSurg.2019.
16. van Leeuwen OB, de Vries Y, Fujiyoshi M, et al. Transplantation of High-riskDonorLiversAfterExSituResuscitationandAssessmentUsingCombinedHypo-and Normothermic Machine Perfusion. Ann Surg. August 2019:1.doi:10.1097/SLA.0000000000003540
17. MannerM,ShultW,SenningerN,MachensG,OttoG.Evaluationofpreservationdamage after porcine liver transplantation by assessment of hepaticmicrocirculation.Transplantation.1990;50(6):940-943.
18. SteiningerR,RothE,HolzmüllerP,etal.ComparisonofHTK-andUW-solutionforliverpreservationtestedinanorthotopiclivertransplantationmodelinthepig.TransplInt.1992;5Suppl1:S403-7.
19. LonzeBE,ParsikiaA,FeyssaEL,etal.OperativeStartTimesandComplicationsAfter Liver Transplantation. Am J Transplant. 2010;10(8):1842-1849.doi:10.1111/j.1600-6143.2010.03177.x
20. XuH,LeeCY,ClemensMG,ZhangJX.Pronlongedhypothermicmachineperfusionpreserveshepatocellularfunctionbutpotentiatesendothelialcelldysfunctioninratlivers.Transplantation.2004;77(11):1676-1682.
21. LüerB,KoettingM,EfferzP,MinorT.Roleofoxygenduringhypothermicmachineperfusion preservation of the liver. Transpl Int. 2010;23(9):944-950.doi:10.1111/j.1432-2277.2010.01067.x
22. Westerkamp AC, Mahboub P, Meyer SL, et al. End-ischemicmachine perfusionreduces bile duct injury in donation after circulatory death rat donor liversindependent of the machine perfusion temperature. Liver Transpl.2015;21(10):1300-1311.doi:10.1002/lt.24200
23. Schlegel A, Dutkowski P. Role of hypothermic machine perfusion in livertransplantation.TransplInt.2015;28(6):677-689.doi:10.1111/tri.12354
24. JainS,XuH,DuncanH,etal.Ex-vivostudyofflowdynamicsandendothelialcellstructureduringextendedhypothermicmachineperfusionpreservationoflivers.Cryobiology.2004;48(3):322-332.doi:10.1016/j.cryobiol.2004.01.010
25. Minor T, Manekeller S, Sioutis M, Dombrowski F. Endoplasmic and VascularSurface Activation During Organ Preservation: Refining Upon the Benefits ofMachinePerfusion.Am JTransplant.2006;6(6):1355-1366.doi:10.1111/j.1600-6143.2006.01338.x
26. van der Plaats A,MaathuisMHJ, ’t Hart NA, et al. The Groningen HypothermicLiverPerfusionPump:FunctionalEvaluationofaNewMachinePerfusionSystem.AnnBiomedEng.2006;34(12):1924-1934.doi:10.1007/s10439-006-9207-4
27. Debbaut C, Monbaliu D, Casteleyn C, et al. From Vascular Corrosion Cast toElectrical Analog Model for the Study of Human Liver Hemodynamics andPerfusion. IEEE Trans Biomed Eng. 2011;58(1):25-35.doi:10.1109/TBME.2010.2065229
28. VerhoevenCJ,FaridWRR,deJongeJ,MetselaarHJ,KazemierG,vanderLaanLJW.Biomarkerstoassessgraftqualityduringconventionalandmachinepreservationin liver transplantation. J Hepatol. 2014;61(3):672-684.doi:10.1016/J.JHEP.2014.04.031
29. VogelT,BrockmannJG,PigottD,etal.Successfultransplantationofporcinelivergrafts following 48-hour normothermic preservation. Gruttadauria S, ed. PLoSOne.2017;12(11):e0188494.doi:10.1371/journal.pone.0188494
30. Vogel T, Brockmann JG, Quaglia A, et al. The 24-hour normothermic machineperfusionofdiscardedhumanlivergrafts.LiverTransplant.2017;23(2):207-220.doi:10.1002/lt.24672
31. Schlegel A, Muller X, Dutkowski P. Hypothermic Machine Preservation of theLiver: State of the Art. Curr Transplant reports. 2018;5(1):93-102.doi:10.1007/s40472-018-0183-z
32. Liu Q, Nassar A, Farias K, et al. Comparing Normothermic Machine PerfusionPreservation With Different Perfusates on Porcine Livers From Donors AfterCirculatoryDeath.AmJTransplant.2016;16(3):794-807.doi:10.1111/ajt.13546
33. vonHornC,HannaertP,HauetT,etal.Coldflushafterdynamicliverpreservationprotects against ischemic changes upon reperfusion - an experimental study.TransplInt.October2018.doi:10.1111/tri.13354
34. Minor T, Efferz P, Fox M, Wohlschlaeger J, Lüer B. Controlled oxygenatedrewarmingofcoldstoredlivergraftsbythermallygraduatedmachineperfusionprior to reperfusion. Am J Transplant. 2013;13(6):1450-1460.doi:10.1111/ajt.12235
SupplementaryFig.1.Degreeofinjuryoftheextrahepaticbileductsofliverstreatedwith2,6,or24hoursDHOPEpriortoSCSandafter4hoursnormothermicreperfusion.Thedegreeof(A)biliaryepithelialloss(p=1.000),(B)muralstromanecrosis(p=0.276),(C)arteriolonecrosis(p=0.159),(D)injurytothePBGs(p=1.000),and(E)intramuralbleeding(p=0.570).(F)Presenceofthrombosis(p=0.105).Therewerenostatisticallysignificantdifferencesbetweenthegroupsattheendofreperfusion(Chi-squaretest).Shownherearepercentagesforn=6animalspergroup.
Transplantationofhigh-riskdonorliversafterexsituresuscitationandassessmentusingcombinedhypo-andnormothermicmachineperfusion:aprospectiveclinicaltrial.
OttoB.vanLeeuwen,YvonnedeVries,MasatoFujiyoshi,MaartenW.N.Nijsten,RinseUbbink,GertJanPelgrim,MaureenJ.M.Werner,KoenM.E.M.Reyntjens,AadP.vandenBerg,MariekeT.deBoer,RubenH.J.deKleine,TonLisman,VincentE.deMeijer,RobertJ.Porte.AnnSurg.2019Nov;270(5):906-914
8
ABSTRACT
Objective:Toevaluatesequentialhypothermicandnormothermicmachineperfusionas
atooltoresuscitateandassessviabilityofinitiallydeclineddonorliverstoenablesafe
transplantation.
SummaryBackgroundData:Machineperfusionisincreasinglyusedtoresuscitateand
test the function of donor livers. While (dual) hypothermic oxygenated perfusion
([D]HOPE) resuscitates livers after cold storage, normothermic machine perfusion
(NMP)enablesassessmentofhepatobiliaryfunction.
Methods:Inaprospectiveclinicaltrial,nationwidedeclinedliversweresubjectedtoex
situ NMP (viability assessment phase), preceded by one-hour DHOPE (resuscitation
phase)andonehourofcontrolledoxygenatedrewarming(COR),usingaperfusionfluid
containing an hemoglobin-based oxygen carrier. During the first 2.5h of NMP,
hepatobiliary viability was assessed, using predefined criteria: perfusate lactate
<1.7mmol/L,pH7.35-7.45,bileproduction>10mLandbilepH>7.45.Liversmeetingall
criteria were accepted for transplantation. Primary endpoint was 3-months graft
survival.
Results:SixteenliversunderwentDHOPE-COR-NMP.All liverswerefromdonorsafter
circulatory death, with median age of 63 (range 42-82) years and median
Eurotransplant donor risk index of 2.82. During NMP, all livers cleared lactate and
producedsufficientbilevolume,but in5 liversbilepHremained<7.45.The11(69%)
livers thatmet all viability criteriawere successfully transplanted,with100%patient
and graft survival at 3 and6months. Introduction ofDHOPE-COR-NMP increased the
numberofdeceaseddonorlivertransplantsby20%.
Conclusions: SequentialDHOPE-COR-NMPenabled resuscitation and safe selection of
initiallydeclinedhigh-riskdonorlivers,therebyincreasingthenumberoftransplantable
liversby20%.
INTRODUCTION
Althoughlivertransplantationisalife-savingtreatmentforpatientswithend-stageliver
disease,mortalityon thewaiting list ishighdue to shortageof suitabledonororgans.
Therefore,‘extended-criteriadonor’(ECD)organsofsuboptimalqualityareincreasingly
usedfortransplantation.However,ahighnumberofECDliversisstilldeclinedbecause
theriskofprimarynon-functionorotherseverecomplicationsisconsideredtoohigh.1
Particularly livers fromdonorsaftercirculatorydeath(DCD)arepronetoseveregraft
injury and early failure due to prolonged donor circulatory arrest and hypotension
(warm ischemia).2 The biliary tract is especially vulnerable to ischemic injury,
illustrated by a 3-fold higher incidence of ischemic cholangiopathy after DCD liver
transplantation,compared to transplantationof livers fromdonationafterbraindeath
(DBD).3-5
Ex situ oxygenated machine perfusion is increasingly applied to improve graft
preservation and reduce the risk of graft failure, and various protocols are currently
tested in clinical trials.6-8 Single or dual hypothermic oxygenated machine perfusion
([D]HOPE)reducesischemia-reperfusioninjurybyresuscitatingmitochondria,resulting
inrestorationofcellularenergystoresanddecreasedreleaseofreactiveoxygenspecies
duringtransplantation.9Controlledoxygenatedrewarming(COR)aimstominimizethe
potential deleterious transition between cold preservation and warm reperfusion.10
Normothermic machine perfusion (NMP) reduces ischemic injury and allows ex situ
assessmentofhepatobiliaryfunctionbecausetheorganismetabolicallyactiveat37oC.11
However, when applied after a period of static cold storage, NMP may not provide
optimalprotectionagainstischemia-reperfusioninjury.12-14
Intwopreclinicalstudiesusingdiscardedhumanlivers,ashortperiodof(D)HOPEprior
to NMP resulted in better hepatobiliary function and less injury, compared to NMP
only.12,13AftersequentialDHOPEandNMP,hepaticadenosinetriphosphatecontentand
levels of biliary bicarbonate and bilirubin were higher compared to livers that
underwentNMPonly.12
We, therefore, hypothesized that a combination of DHOPE and NMPwouldmaximize
utilization of the machine perfusion potential when applied after a period of cold
preservation.Totestthishypothesis,weinitiatedaprospectiveclinicaltrialofcombined
DHOPE, COR, and NMP with the aim to resuscitate and test the viability of initially
nationwidedeclinedliverstoallowsafetransplantation.
METHODS
Trialdesign
In this prospective clinical trial, all livers that were nationwide declined for regular
transplantationbetweenAugust2017andOctober2018wereincluded(Figure1).The
study protocol (www.trialregister.nl; NTR5972) was approved by themedical ethical
reviewcommitteeofourcenter(METc2016.281).Allrecipientsgavewritten informed
consent.
Objective of this study was to safely increase utilization of donor livers by ex situ
resuscitation and viability assessment using a protocol combining DHOPE, COR, and
NMP. Primary endpointwas graft survival after 3months. Secondary endpointswere
graftandpatientsurvivalat6months,theincidenceofprimarynon-functionandpost-
transplantcholangiopathy(definedasaspectrumofbileductabnormalities, including
non-anastomotic biliary strictures, intraductal casts and/or intrahepatic biloma
formation),15andbiochemicalserummarkersofgraftfunctionandischemia-reperfusion
injuryatpostoperativeday1-7,andafter1and3months. Inaddition,graftutilization
ratewasdetermined.
Procurementofdonorlivers
Allliverswereprocuredinastandardizedmannerbyadedicatedprocurementteam.16
AlthoughbothDBDandDCDliverswereeligibleforinclusioninthetrial,coincidentally
all included liverswere fromDCDdonors.DCDorganprocurement in theNetherlands
includesamandatory5min‘notouch’periodafterdeclarationofcirculatorydetermined
deathandheparinizationofthedonorisnotpermitted.Afterrapidinsitucoldflushout
andprocurement,liverswerepreservedandtransportedusingstaticcoldpreservation
inUniversityofWisconsin(UW)coldstoragesolution(BridgetoLife,London,UK).Time
betweenstartofcold flushingandeitherthebeginningofmachineperfusion(DHOPE-
COR-NMP) or graft reperfusion in the comparator cohorts, was defined as static cold
ischemiatime.
Perfusionsolution
Toallowbothhypothermicandnormothermicmachineperfusionwithout theneed to
interrupt perfusion to replace the perfusion fluid, an acellular perfusion solution
containing a hemoglobin-based oxygen carrier, HBOC-201, (Hemopure, HbO2
TherapeuticsLLC,Souderton,USA)wasusedforalltemperaturephases.17-19Inaddition
to HBOC-201, the perfusion solution contained gelofusine, albumin, metronidazole,
glutathione, cefazolin, heparin, insulin and sodium bicarbonate (Supplementary Table
1). After the first five perfusions, clinical grade taurocholate came available and was
addedtotheperfusionfluid(50mgatstartofNMPfollowedbycontinuous infusionof
7.7mg/h).Taurocholatewasproducedaccordingtogoodmanufacturingpracticebyour
hospitalpharmacy.
Machineperfusionprocedure
Machine perfusion procedures were performed with the Liver Assist device (Organ
Assist, Groningen, the Netherlands) (Figure 2A). Prior to machine perfusion, a portal
veinflushwasperformedwith2Lofcoldsaline.Allliversunderwent1hourofDHOPE
(8-12ºC)withportalveinandhepaticarterypressuresof5and25mmHg,respectively.
DuringDHOPE,1L/minof100%O2wasadministered,resultinginaPaO2>80kPa.After
1hofDHOPE,temperaturewasstepwiseincreased(1°Cper2minutes),until37°C(COR
phase).Additionally,theportalveinandhepaticarterypressureswereslowlyincreased
to11and70mmHg,respectively.Afterperfusion fluid temperaturereached37ºC, the
NMP phase started to allow viability assessment. During NMP an air/oxygenmixture
wasusedforventilation,aimingatahepaticvenousoxygensaturationof55-75%.
Every 30 minutes, arterial perfusate samples were collected and analyzed with an
ABL90Flex blood gas analyzer (Radiometer, Brønhøj, Denmark). Additionally, every
hour venous outflow samples were collected to determine SvO2 and PvO2. Bile was
collected froma 8Fr biliary drain and volumewasdetermined gravimetrically. At 30-
minute intervals samplesofbilewerecollectedundermineraloil todeterminebiliary
pH,bicarbonate,andglucose.20,21
Viabilityassessment
During the first 2.5h of NMP, hepatobiliary function was tested using the following
criteria:lactate<1.7mmol/L,perfusatepH7.35-7.45,bileproduction>10ml,andbiliary
pH >7.45. When a liver met all viability criteria, the liver was accepted for
transplantation. In non-viable livers, NMPwas discontinued and the liver secondarily
discarded. Viable donor livers remained on NMP until recipient hepatectomy was
completedandimplantationcouldbeinitiated.AfterNMP,liverswereflushedoutwith
2Lof coldUWto remove themachineperfusionsolution.After implantation, the liver
was flushed with 500mL recipient blood via the caval anastomosis following portal
venousreperfusion.
Histologicalanalysis
Biopsiesweretakenfromthedistalcommonbileductbeforemachineperfusion,fixedin
4% formalin, and subsequently embedded in paraffin. Slices of 4 µm were cut and
stainedwithhematoxylin&eosinforexaminationusinglightmicroscopy.Thebileduct
injury (BDI) score was determined in-duplo in a blinded fashion, using a clinically
relevanthistologicalgradingsystem.20,22
Comparatorcohorts
ContemporarycomparatorcohortsofallconsecutiveadultDCDorDBDlivertransplants
performed in our center between January 2017 and October 2018 were formed.
Recipientsofmulti-organtransplantswereexcluded.
Statisticalanalysis
Continuous variables were presented as median (interquartile range; IQR) and
compared using the Mann-Whitney test. Categorical variables were presented as
number (percentage) and compared using Chi-square or Fisher’s exact test where
appropriate. Graft survival was determined with the Kaplan-Meier method, and
differences were determined with the log-rank test. Two-sided P-values <0.05 were
considered statistically significant. Analyses were performed using SPSS, version 23
(IBM,Armonk,NewYork,USA).
RESULTS
Inclusions
Between August 2017 and October 2018, 42 livers were offered for inclusion in the
DHOPE-COR-NMP trial afternationwidedecline for regular transplantation (Figure1).
Ofthese,16liversunderwentmachineperfusion.Donorcharacteristicsaresummarized
inTable1.AllliverswerefromDCDdonorswithamedianageof63(range42-82)years
andamedianEurotransplantdonorriskindex(ET-DRI)of2.82.23
Figure1:FlowchartoftheliversofferedforinclusionintheDHOPE-COR-NMPtrial.
A total of 42 nationwide declined high-risk livers was offered. Twenty-six livers did not
undergo machine perfusion as a result of logistic reasons, too long agonal phase or
macroscopic findingsduringorganprocurement. In theNetherlands,organprocurement
teamswithdraw ifnocirculatoryarrestoccurswithin twohoursofventilator switch-off.
Sixteen livers underwent DHOPE-COR-NMP. Abbreviations: COR; controlled oxygenated
rewarming,DHOPE;dualhypothermicoxygenatedperfusion,NMP;normothermicmachine
perfusion.
Viabilitytesting
DuringNMP,11of16(69%)perfusedlivers(depictedasgreenlinesinFigures2-3)met
all viability criteria (Figure 2B-D). The five livers secondarily declined for
transplantation(depictedasredlinesinFigures2-3)allhadabilepH<7.45at2.5hof
NMP(Figure2D).Allliversclearedlactateandproduced>10mLofbile.Nodifferencesin
portal vein and hepatic artery flows were observed between transplanted and non-
transplanted livers (Table 1). There were no major differences in baseline
characteristicsof transplantedandnon-transplanted livers, apart froma longerdonor
hepatectomytimeandstaticcoldischemiatimeinthelattergroup.
Table 1. Donor and perfusion characteristics of transplanted and non-
transplantedlivers.
Variable Transplanted(n=11)
Non-transplanted(n=5)
p-value
Donorcharacteristics Age(years) 63(52-72) 63(52-71) 0.961Bodymassindex(kg/m2) 25(21-26) 28(24-32) 0.052Gender*MaleFemale
8(73%)3(27%)
4(80%)1(20%)
0.635
Causeofdeath*TraumaCerebrovascularattackAnoxiaOther
2(18%)5(46%)3(27%)1(9%)
2(40%)1(20%)1(20%)1(20%)
0.648
Time from withdrawal of lifesupport to circulatory arrest(min)
14(11-18) 14(8-21) 0.851
Time from circulatory arrest tocoldperfusion(min)
16(14-16) 16(14-20) 0.743
Total donor warm ischemia time(min)
32(25-33) 30(18-37) 0.913
Lastsodium(mmol/L) 143(141-153) 140(133-148) 0.177LastAST(u/L) 60(32-95) 79(53-158) 0.441LastALT(u/L) 62(36-127) 81(33-178) 0.743LastGGT(u/L) 64(30-167) 55(24-543) 0.743LastALP(u/L) 63(52-78) 105(76-346) 0.013Hepatectomytime(min) 44(28-54) 70(44-93) 0.040Staticcoldischemiatime(min) 270(241-294) 326(286-480) 0.018ET-DRI# 2.81(2.60-2.90) 2.82(2.47-3.26) 0.743Perfusion characteristicsat150minutesofNMP
Portalveinflow(ml/min) 1790(1550-2070) 1750(1665-1750) 0.955Hepaticarteryflow(ml/min) 478(420-653) 515(323-871) 0.462PerfusatepH 7.42(7.40-7.44) 7.38(7.34-7.39) 0.115
Perfusatelactate 0.7(0.4-1.1) 1.7(1.3-1.9) 0.068Perfusateglucose 24.0(19.3-29.5) 27.0(24.5-29.0) 0.955BilepH 7.57(7.521-7.61) 7.39(7.32-7.40) 0.002Bilebicarbonate 27.6(24.9-29.6) 18.3(16.9-19.7) <0.001Bileglucose 13.5(6.6-17.0) 20.4(20.2-21.7) 0.055BilepH–perfusatepH^ 0.15(0.10-0.19) 0.01(-0.05-0.05) 0.005Bile bicarbonate – perfusatebicarbonate^
8.6(6.7-11.7) 2.0(1.3-3.1) 0.013
Bileglucose–perfusateglucose^ -9.8(-13.8--8.1) -4.3(-8.0--2.0) 0.052Glucoseratiobileandperfusateº 0.50(0.30-0.63) 0.82(0.76-0.90) 0.013
Continuousdataarepresentedasmedian(IQR),categoricaldataasnumber(percentage).
*Shownasnumber(percentage).#Avalidatedtooltoassesstheriskoflivergraftfailure.23
^Thedifferencebetween thebileand theperfusate. ºTheglucose level in theperfusate
divided by the glucose level in the bile. Abbreviations: AFP; alkaline phosphatase, ALT;
alanine aminotransferase, AST; aspartate aminotransferase, DBD; donation after brain
death, DCD; donation after circulatory death, ET-DRI; Eurotransplant Donor Risk Index,
GGT;gammaglutamyltransferase.
Figure 2: Viability testing during DHOPE-COR-NMP. The green lines indicate the
transplantedlivers,theredlinesrepresentthenon-transplantedliver.Thelightgreenline
indicates the transplanted liver that developed post-transplant cholangiopathy. In livers
thatdidnotmeetalviabilitycriteriaduringthefirst2.5hofNMP,NMPwasdiscontinued
and liversweresecondarilydiscarded. Inviable livers thatmetallviabilitycriteria,NMP
wascontinueduntilrecipienthepatectomywascompleted.A,Liverfroma82-yearoldDCD
donor with a functional warm ischemia time of 33 minutes. This liver met the viablity
criteria and was successfully transplanted. Portal vein and supratruncal aorta were
cannulated,anddrainswereplacedinthecommonbileductandthesuprahepaticinferior
vena cava. B, Lactate decreased during NMP. C, Perfusate pH normalized during NMP
except forone liver.D,BilepH increasedduringNMP,but remainedbelow7.45 in the5
non-transplanted livers. E, Bile glucose decreased during NMP. F, Bile bicarbonate
increasedduringNMP,butremained lowinthe5non-transplanted livers.Abbreviations:
COR;controlledoxygenatedrewarming,DHOPE;dualhypothermicoxygenatedperfusion,
min;minutes,NMP;normothermicmachineperfusion.
ClinicaloutcomesDHOPE-COR-NMPversuscomparatorcohorts
Themedian follow up of the patients that received a DHOPE-COR-NMP liver was 12
months(range8-22months).UsingtheDHOPE-COR-NMPprotocolforresuscitationand
viability testing of initially declined livers,we achieved actuarial 3-, 6-, and12-month
graftsurvivalratesof100%.Patientsurvivalwas100%atthesetimepoints.Outcomes
werecomparedtocontemporarycomparatorcohortsofregularDBDorDCDliversthat
were transplanted in our center outside the DHOPE-COR-NMP protocol (Table 2).
Notably,donorsofregularDCDliversweresignificantlyyounger(52vs.63years),and
had a significantly lower ET-DRI (2.34 vs. 2.81) (Table 2). Actuarial graft and patient
survivalratesintheDBDcomparatorcohortwere100%at3,6and12months.Actuarial
graftsurvivalratesintheDCDcomparatorcohortwere83%,83%and80%at3,6and
12months, respectively, and patient survival was 92%, 92%, and 88% at these time
points.GraftandpatientsurvivalwerenotsignificantlydifferentbetweentheDHOPE-
COR-NMP cohort and the two comparator cohorts. During execution of the trial, 56
regular deceased donor liver transplantations were performed, indicating a 20%
increaseduetothemachineperfusionprotocol.
Table2.Donor,recipientandtransplantationcharacteristicsandpost-transplant
outcomesofthetransplantedDHOPE-COR-NMPliversversusthecomparator
cohorts.
ComparatorcohortVariable DHOPE-COR-NMP
(n=11)DBD(n=36)
DCD(n=24)
p-valueDHOPE-COR-NMPversusDBD
p-valueDHOPE-COR-NMPversusDCD
Donor Typeofdonor*DBDDCD
0(0%)11(100%)
36(100%)0(0%)
0(0%)24(100%)
--
--
Age(years) 63(52-72) 61(47-66) 52(48-56) 0.227 0.005Gender(male)* 8(73%) 20(56%) 15(63%) 0.485 0.682Bodymassindex(kg/m2) 25(21-26) 26(24-28) 27(22-29) 0.057 0.092Causeofdeath*TraumaCVAAnoxiaOther
2(18%)5(46%)3(27%)1(9%)
7(19%)21(58%)7(19%)1(3%)
6(25%)8(33%)5(21%)5(21%)
0.116 0.452
Timefromwithdrawaloflifesupporttocirculatoryarrest(min)
14(11-18) - 12(8-15) - 0.046
Timefromcirculatoryarresttocoldperfusion(min)
16(14-16) - 16(14-20) - 0.445
Totalwarmischemiatime(min)
32(25-33) - 28(23-33) - 0.274
Lastsodium(mmol/L) 140(133-148) 146(144-149)
143(140-146)
0.479 0.540
LastGGT(u/L) 64(30-167) 44(21-76) 41(18-63) 0.268 0.186LastALT(u/L) 62(36-127) 40(22-69) 33(18-55) 0.123 0.025LastAST(u/L) 60(32-95) 49(28-79) 49(19-78) 0.364 0.211LastALP(u/L) 63(52-78) 66(49-85) 61(50-97) 0.904 0.923ICUstay(days) 3(1-5) 2(1-2) 3(1-5) 0.090 0.923Hepatectomytime(min) 44(28-54) 46(35-55) 48(37-84) 0.296 0.114ET-DRI# 2.81(2.60-2.90) 1.75(1.48-
1.90) 2.34(2.14-
2.49)<0.001 <0.001
Recipient Age(years) 61(55-66) 52(40-
60) 56(48-61) 0.017 0.198
Gender(male)* 7(64%) 22(61%)
13(54%) 1.000 0.721
Bodymassindex(kg/m2) 28(25-32) 25(22-28)
27(23-30) 0.150 0.494
LabMELD-score° 14(13-15) 15(10-22)
18(11-24) 0.405 0.268
ICUstaypriortotransplant
1(9%) 4(11%) 1(4%) 1.000 0.536
Retransplantation*Transplantindication*
1. NASH/NAFLD2. Post-alcoholic
cirrhosis3. Biliarydiseases≠4. Other
0(0%) 9(25%) 3(12%) 0.092 0.5364(37%)3(27%)3(27%)1(9%)
3(8%)5(14%)11(31%)17(47%)
6(25%)4(17%)6(25%)8(33%)
0.070 0.632
Transplantation Staticcoldischemiatime(min)
270(241-294) 407(352-471) 446(379-492)
<0.001 <0.001
Totalpreservationtime(min)
868(805-924) 407(352-471) 446(379-492)
<0.001 <0.001
Anastomosistime(min) 38(32-44) 42(37-51) 42(34-52) 0.124 0.352Estimatedbloodloss(ml) 4000(2400-7700) 3450(1960-
6250) 3475(1987-4886)
0.382 0.409
RBCtransfusion(units) 5(3-8) 3(1-8) 5(0-10) 0.183 0.586FFPtransfusion(units) 0(0-0) 0(0-3) 0(0-4) 0.703 0.445Implantation(piggyback)*8(73%) 32(89%) 21(88%) 0.330 0.352Post-operativeresults Actuarialgraftsurvival3-months
100%
100%
83.3%
1.000
0.159
6-months 100% 100% 83.3% 1.000 0.15912-months 100% 100% 80% 1.000 0.207PeakALT(u/L) 683(282-757) 1195(600-
2285) 1598(652-3191)
0.009 0.001
PeakAST(u/L) 751(483-1757) 1646(627-2494)
2406(1102-4573)
0.165 0.004
Bilirubinday7(umol/L) 16(8-27) 21(14-62) 16(12-37) 0.143 0.510INRday7 1.0(1.0-1.0) 1.0(1.0-1.1) 1.1(1.0-1.1) 0.123 0.076Post-transplantcholangiopathy*
1(9%) 3(8.3%) 4(18%) 1.000 0.643
Anastomoticstricture* 3(27%) 11(31%) 4(18%) 1.000 0.656Primarynon-function* 0(0%) 0(0%) 2(8.3%) 1.000 1.000Hepaticarterythrombosis*
0(0%) 0(0%) 0(0%) - -
Acuterejection* 1(9%) 3(8.3%) 1(4%) 1.000 1.000
Continuousdataarepresentedasmedian(IQR),categoricaldataasnumber(percentage).
* Shown as number (percentage). # A validated tool for assess the risk of liver graft
failure23. ° Defined as the last laboratory-derived Model for End-stage Liver Disease
(MELD) score. ≠ Including primary biliary cirrhosis, primary sclerosing cholangitis.
Abbreviations:AFP;alkalinephosphatase,ALT;alanineaminotransferase,AST;aspartate
aminotransferase,CVA,cerebrovascularaccidentCPR;cardiopulmonaryresuscitation,ET-
DRI; Eurotransplant Donor Risk Index, FFP; fresh frozen plasma, GGT; gamma
glutamyltransferase,ICU;intensivecareunit,INR;internationalnormalizedratio,NAFLD;
non-alcoholicfattyliverdisease,NASH;non-alcoholicsteatohepatitis,RBC;redbloodcell.
Developmentofpost-transplantcholangiopathy
OnerecipientofaDHOPE-COR-NMP liverdevelopedcholangiopathyat4monthsafter
transplantation, characterized by recurrent jaundice, pruritus and cholangitis. Biliary
anastomosis in this patientwas constructed using a Roux-en-Y hepatico-jejunostomy.
Magnetic resonance cholangiography revealed biliary irregularities with intraductal
casts (Figure3A). Thepatient underwent surgical removal of thebiliary casts (Figure
3B)withshorteningoftheextrahepaticbileductandre-anastomosisofthejejunalloop,
afterwhichbileflowwasrestored.Intraoperativecholangioscopydemonstratedinjury
oftheintrahepaticbileducts(Figure3C).
Duringpretransplantmachineperfusionof this liver,perfusate lactatewas<1mmol/L,
perfusatepH7.46,andbilepHwas7.45after2.5hofNMP(lightgreenlineinFigures2-
3).Althoughthislivermetallviabilitycriteria,inretrospectwehavelearnedfromthis
casethatthedifferencebetweenbileandperfusatepH,bicarbonateandglucosemaybe
morepredictiveofbileductviabilitythantheabsolutebiliaryvalues.(Figure3E-H).
Baselinebileductbiopsyof this liver showedsignsof severe injury to theextramural
peribiliaryglands,necroticvesselsanddiffusestromanecrosis(BDIscore6;Figure3D).
AnalysisofallbaselinebileductbiopsiesrevealedasignificantlyhigherBDIintheliver
whichdevelopedcholangiopathyand theothernon-transplanted livers (medianBDI5
[4-6]),whencomparedtothetransplantedliverswithoutsymptomsofpost-transplant
cholangiopathy(medianBDI3[2-4];p=0.031).
Figure3.Developmentofpost-transplant cholangiopathyafterDHOPE-COR-NMP
anddiscriminatingpowerofbilecomposition.
A, Magnetic resonance cholangiography of the patient that developed post-transplant
cholangiographyrevealedbiliaryirregularitieswithintraductalcastformation.B,Alarge
intraductal cast was subsequently removed. C, Intraoperative cholangioscopy
demonstratedinjuryoftheintrahepaticbileducts.D,Thebaselinebileductbiopsyofthe
liver that developed post-transplant cholangiopathy revealed severe injury to the
extramuralperibiliaryglands,necroticvesselsanddiffusestromanecrosis.Magnification:
10x.E-H,thedifferencebetweenbileandperfusatepH,bicarbonateandglucoseappeared
to bemore indicative of biliary damage than the absolute value of pH, bicarbonate and
glucoseinthebile.G,theglucosevalueinthebiledividedbytheglucoseintheperfusate
showed a clear difference in glucose reabsorption by the biliary epitheliumbetween the
transplanted and non-transplanted livers. Abbreviations: COR; controlled oxygenated
rewarming, DHOPE; dual hypothermic oxygenated perfusion, min; minutes, NMP;
normothermicmachineperfusion.
DISCUSSION
Thisprospective clinical trial suggests that sequentialDHOPE,CORandNMP is a safe
andefficaciousinterventiontoallowsuccessfultransplantationofinitiallydeclinedhigh-
risk donor livers. After transplantation of DHOPE-COR-NMP livers, graft and patient
survival rates were at least similar when compared to contemporary comparator
cohortsofregularDCDorDBDlivergrafts.
To the best of our knowledge, two studies have been published on transplantation of
discardedhumandonorlivers.InthefirstseriesbytheBirminghamgroup,sixdiscarded
humandonorliversunderwentviabilitytestingbyusingend-ischemicNMP,ofwhich5
liversweresubsequentlytranplanted.24Theaveragedonorageofthesefiveliverswas
45 years, and all grafts functioned well after transplantation. In this study, viability
criteria duringNMP included lactate clearance, perfusate pH >7.30, stable portal vein
andhepaticarteryflows,andahomogeneousgraftperfusion.Noviabilitytestingofthe
biliary tree was performed. In the second study conducted by the Cambridge group,
twelve discarded human donor livers underwent end-ischemic NMP, followed by
transplantation.25Inthisstudy,thecompositionofbilewasmeasured,butnotusedfor
viability testing. Of the twelve livers, one developed primary non-function and three
livers(27%)developedpost-transplantcholangiopathy.Anassociationbetweenlowbile
pHduringNMPanddevelopmentofpost-transplantcholangiopathywasfoundandthe
authors suggested bile pH as a potential viability criterion. In a follow-up paper, the
same authors described a correlation between bile pH, glucose and bicarbonate,with
biliary injury.26 Previous clinical series ofDCD liver transplantation indicated a lower
incidenceofpost-transplant cholangiopathy if liversunderwent (D)HOPE.9,27Although
these results still have to confirmed by ongoing randomized controlled trials,28 we
decidedtoperformDHOPEprior toNMPtoattenuatethebiliary ischemia-reperfusion
injury and to include biliary viability testing, to allow more safe transplantation
comparedtotheseearlierexperiences.
Inanotherrecentlycompletedstudyontransplantationofinitiallydiscardedlivers,the
VITTAL-studybytheBirminghamgroup,onlyhepatocellularfunctionwastestedduring
NMP, while viability testing of the biliary treewas not performed.29 One of themain
strengthsinthecurrentstudyisthatbothhepatocellularandcholangiocellularfunction
were assessed, based on previously determined biomarkers of bile duct viability.20 In
ourstudy,all16liversmetthehepatocellularviabilitycriteriausedintheVITTAL-study,
but only 11 met our criteria for cholangiocellular function (bile pH >7.45). In the
VITTAL-study,45%ofpatientsdevelopedbileductirregularitiesonmagneticresonance
cholangiographyand18%requiredretransplantationforbiliarystrictures.30,31Although
this may provide a strong rationale for additional biliary viability testing, definitive
proofwouldrequirearandomizedcontrolledtrial.
Withamedianfollowupof12months(range8-22months),wehaveobservedonlyone
case of post-transplant cholangiopathy after DHOPE-COR-NMP of high-risk DCD liver
graftswithamedianageof63(range42-82)years.Healthybiliaryepitheliummodifies
bile composition by secreting bicarbonate, leading to a protective alkalotic biliary
environment.20,32,33 Additionally, biliary epithelium reabsorbs glucose, decreasing
glucoselevelsinbile.20,34-37DuringtheNMP-phaseoftheoneliverthatdevelopedpost-
transplant cholangiopathy, the bile pH, bicarbonate, and glucosewere similar to their
levelsintheperfusate,suggestingimpairedbiliaryepithelialfunction.Sincethiscase,we
considerthedifferenceofpH,bicarbonate,andglucosebetweenperfusateandbileasa
markerofbiliaryviabilityinsteadofabsolutevaluesonly.
While end-ischemicDHOPE reduces reperfusion injury inDCD liver transplantation38,
post-ischemic biliary injury already present before machine perfusion cannot be
repaired.We therefore presume thatwith our currentDHOPE-COR-NMPprotocol,we
have safely pushed the boundaries of end-ischemic machine perfusion for high-risk
donorlivers,butthistechniquedoesnotenableactiverepairofpre-existingseverebile
ductinjury.Therefore,alternativestrategiessuchasnormothermicregionalperfusionof
DCDdonorsmayprovideadditionalbenefitandhelp toavoidbileduct injuryprior to
staticcoldpreservation.39,40
A limitationof thisstudy is the lackofrandomizationbetweenmachineperfusionand
traditionalstaticcoldpreservationonly.Inourcountry,post-transplantcholangiopathy
hasbeenobservedinupto30%ofDCDliverrecipientsandthereforeDCDliverswitha
donor age >60 years are usually declined for regular transplantation.3-5 Ethical
constraints refrained us from accepting these and other high-risk livers for
transplantationwithoutaddinganyinterventionandwiththesoleintentiontoserveas
a control group in this trial. We, therefore, used comparator cohorts of all adult
recipientsofregularDCDorDBDlivergraftsduringthestudyperiod.Patientandgraft
survival were not different between these groups. Another possible limitation is that
livers declined for transplantation based on a low bile pH during NMP, were not
transplantedandthereforehavenofollowup.Althoughwehavenocertaintythatthese
livers would have developed post-transplant cholangiopathy, previous (pre)clinical
studiesindicatedasubstantiallyincreasedrisk.20,22,26
In conclusion, this prospective clinical trial demonstrates the safety and feasibility of
transplantation of high-risk ECD liver grafts using sequential DHOPE, COR, and NMP.
Pretransplantresuscitationandviabilityassessmentoftheseinitiallydeclinedliversled
toa20%increaseinnumberofdeceaseddonorlivertransplantsinourcenter.
ACKNOWLEGDEMENTS
HBOC-201(Hemopure)waskindlyprovidedbyZafirisZafirelis(HBO2TherapeuticsLLC,
Souderton,USA).WearegratefultotheDutchtransplantcoordinatorsfortheirhelpin
identifying potential donors, whose livers could be eligible for the DHOPE-COR-NMP
trial.TheperfusiondeviceandsolutionusedinthisstudyarenotFDAapproved.
REFERENCES
1. National Health Service, Organ Donation and Transplantation: Activity Report2017-2018.Availableat:http://www.odt.nhs.uk.AccessedFebruari11,2019.
2. Seehofer,D,Eurich,D,Veltzke-SchliekerWetal.BiliaryComplicationsAfterLiverTransplantation: Old Problems and New Challenges. Am J Transplant2013;13:253-265.
3. den Dulk AC, Sebib Korkmaz K, de Rooij BJ, et al. High peak alanineaminotransferasedeterminesextrariskfornonanastomoticbiliarystricturesafterliver transplantation with donation after circulatory death. Transplantinternational2015;28:492-501.
4. Dubbeld J,HoekstraH,FaridW,etal.Similar liver transplantationsurvivalwithselectedcardiacdeathdonorsandbraindeathdonors.BrJSurg2010;97:744-753.
5. O'Neill S, Roebuck A, Khoo E, et al. A meta-analysis and meta-regression ofoutcomes including biliary complications in donation after cardiac death livertransplantation.TransplInt2014;27:1159-1174.
6. NasrallaD,CoussiosCC,MergentalH,etal.A randomized trialofnormothermicpreservationinlivertransplantation.Nature2018;557:50-56.
7. Schegel A, Muller X, Kalisvaart M, et al. Outcomes of DCD liver transplantationusing organs treated by hypothermic machine perfusion before implantation. JHepatol2019;70:50-57.
8. DeMeijerVE,FujiyoshiM,PorteRJ.Exsitumachineperfusionstrategies in livertransplantation.JHepatol.2019;70:203-205.
9. VanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusion in liver transplants donated after circulatory death. Br J Surg2017;104:907-917.
10. Hoyer DP, Mathé Z, Gallinat A, et al. Controlled oxygenated rewarming of coldstored liversprior to transplantation, first clinical applicationof anewconcept.Transplantation2016;100:147-152.
11. Op den Dries S, Karimian N, Sutton ME, et al. Ex vivo normothermic machineperfusionandviabilitytestingofdiscardedhumandonorlivers.AmJTransplant2013;13:1327-1335.
12. Westerkamp AC, Karimian N, Matton APM, et al. Oxygenated hypothermicmachine perfusion after static cold storage improves hepatobiliary function ofextendedcriteriadonorlivers.Transplantation2016;100:825-835.
13. BoteonYL,LaingRW,SchlegelA,etal.Combinedhypothermicandnormothermicmachineperfusionimprovesfunctionalrecoveryofextendedcriteriadonorlivers.LiverTranspl2018;12:1699-1715.
14. QuintiniC,LomaglioL,PezzatiD,etal.Combinedhypothermicandnormothermicperfusionfortheoptimizationofinjuredlivergrafts.LiverTranspl2018;12:1647-1648.
15. De Vries Y, von Meijenfeldt FA, Porte RJ. Post-transplant cholangiopathy:classification,pathogenesis,andpreventivestrategies.BiochimBiophysActaMolBasisDis2018;1864:1507-1515.
16. VanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusioninlivertransplantsdonatedaftercirculatorydeath.BrJSurg;104:907-917.
17. MattonAPM, Burlage LC, van Rijn R, et al. Normothermicmachine perfusion ofdonor livers without the need for human blood products. Liver Transpl2018;24:528-538.
18. DeVriesY,MattonAPM,NijstenMWN, et al. Pretransplant sequential hypo-andnormothermicmachine perfusion of suboptimal livers donated after circulatorydeath using a hemoglobin-based oxygen carrier perfusion solution. Am JTransplant.2019;19:1202-1211.
19. Fontes P, Lopez R, van der Plaats A, et al. Liver preservation with machineperfusion and a newly developed cell-free oxygen carrier solution undersubnormothermicconditions.AmJTransplant.2015;15:381-394.
20. MattonAPM,deVriesY,BurlageLC,etal.Biliarybicarbonate,pHandglucosearesuitable biomarkers of biliary viability during ex situ normothermic machineperfusion of human donor livers. Transplantation 2018 Nov 1; [Epub ahead ofprint].Accessedon02/11/2019DOI:10.1097/TP.0000000000002500
21. Van Leeuwen OB, de Meijer VE, Porte RJ. Viability criteria for functionalassessment of donor livers during normothermic machine perfusion. LiverTranspl2018;24:1333-1335.
22. OpdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsandvascular plexus before liver transplantation predicts formation of non-anastomoticbiliarystrictures.JHepatol2014;60:1172-1179.
23. Braat AE, Blok JJ, Putter H, et al. The Eurotransplant donor risk index in livertransplantation:ET-DRI.AmJTransplant2012;12:2789-2796.
24. Mergental H, Perera MTPR, Laing RW, et al. Transplantation of declined liverallografts following normothermic ex-situ evaluation. Am J Transplant.2016;11:3235-3245.
25. Watson CJE, Kosmoliaptsis V, Randle LV, et al. Normothermic perfusion in theassessmentandpreservationofdeclinedliversbeforetransplantation:hyperoxiaand vasoplegia – important lessons from the first 12 cases. Transplantation.2017;101:1084-1098.
26. WatsonCJE,KosmoliaptsisV,PleyC,etal.Observationsontheexsituperfusionofliverfortransplantation.AmJTransplant.2018;18;2005-2020.
27. Dutkowski P, Polak WG, Muiesan P, et al. First Comparison of HypothermicOxygenated PErfusion Versus Static Cold Storage of Human Donation AfterCardiac Death Liver Transplants: An International-matched Case Analysis. AnnSurg.2015;262:764-770.
28. VanRijnR,vandenBergAP,Erdmann JI, etal.Studyprotocol foramulticenterrandomized controlled trial to compare the efficacy of end-ischemic dualhypothermicoxygenatedmachineperfusionwithstaticcoldstorageinpreventingnon-anastomotic biliary strictures after transplantation of liver grafts donatedafter circulatory death: DHOPE-DCD trial. BMC Gastroentrol. 2019;19:40. DOI:10.1186/s12876-019-0956-6.
29. Laing RW, Mergental H, Yap C, et al. Viability testing and transplantation ofmarginallivers(VITTAL)usingnormothermicmachineperfusion:studyprotocolfor an open-label, non-randomised, prospective, single-arm trial. BMJ Open.2017;7:e017733.
30. Laing RW, Boteon YL, Kirkham A, et al. Transplantation of discarded liversfollowing viability testing with normothermic machine perfusion: the VITTAL(VIability Testing and Transplantation of mArginal Livers) trial outcomes.
[Abstract]. InternationalLiverTransplantationSociety,25thAnnualInternationalCongres2019(https://2019.ilts.org).
31. NeilD,HubscherS,LaingR,etal.Viabilitytestingandtransplantationofmarginaldonor livers VITTAL trial outcomes: bile duct injury assessment during thenormothermic machine perfusion of discarded livers. [Abstract]. InternationalLiver Transplantation Society, 25th Annual International Congres 2019(https://2019.ilts.org)..
32. SutorDJ,WilkieLI.Diurnal variations in thepHofpathological gallbladderbile.Gut.1976;17:971-974.
33. BoyerJL.Bileformationandsecretion.ComprPhysiol.2013;3:1035-1078.34. LazaridisKN,PhamL,VromanB,deGroenPC,LaRussoNF.Kineticandmolecular
identification of sodium-dependent glucose transporter in normal ratcholangiocytes.AmJPhysiol.1997;272:1168-1174.
35. MasyukAI,MasyukTV,TietzPS,SplinterPL,LaRussoNF.Intrahepaticbileductstransport water in response to absorbed glucose. Am J Physiol Cell Physiol.2002;283:785-791.
36. ScheinCJ,ZumoffB,KreamJ,CassoutoJ,HellmanL.Ablood-bileglucosebarrierinman.Gastroenterology.1968;54:1094-1097.
37. GuzelianP,Boyer JL.Glucosereabsorption frombile.Evidence forabiliohepaticcirculation.JClinInvest.1974;53:526-535.
38. vanRijnR,vanLeeuwenOB,MattonAPM,etal.Hypothermicoxygenatedmachineperfusion reduces bile duct reperfusion injury after transplantation of donationaftercirculatorydeathlivers.LiverTranspl.2018;24:655-664.
39. WatsonCJE,Hunt F,Messer S, et al. In situnormothermicperfusionof livers incontrolledcirculatorydeathdonationmayprevent ischemic cholangiopathyandimprove graft survival. Am J Transplant. 2018 Dec 27; [Epub ahead of print].Accessedon02/11/2019DOI:10.1111/ajt.15241
40. HessheimerAJ,CollE,TorresF,etal.Normothermicregionalperfusionvs.super-rapidrecoveryincontrolleddonationaftercirculatorydeathlivertransplantation.JHepatol.2019;70:658-665.
Exsitumachineperfusionofhumandonorliversviathesurgicallyreopenedumbilicalvein:aproofofconcept.
OttoB.vanLeeuwen,MasatoFujiyoshi,RinseUbbink,MaureenJ.M.Werner,IsabelM.A.Brüggenwirth,RobertJ.Porte,VincentE.deMeijer.Transplantation.2019Oct;103(10):2130-2135.
9
ABSTRACT
Background: Machine perfusion of donor livers is typically performed via the portal
veinmainstem.Instead,cannulationofareopenedumbilicalveincouldallowmachine
perfusion during organ procurement and subsequent implantation in the recipient
withoutinterruptionoftheportalvenouscirculation.Weaimedtoassessthefeasibility
ofportalvenousmachineperfusionviatheumbilicalvein.
Methods:Duringbacktableinspectionoffivehumanliversdeclinedfortransplantation,
the umbilical veinwas surgically reopened, dilated and cannulated. Hypothermic and
normothermic oxygenated machine perfusion (NMP) were performed using the
umbilicalveinforportalinflow.Threeliverswereperfusedwithhypothermicmachine
perfusion,one full livergraftunderwentNMP for fourhours, andone left lateral split
procedurewasperformedundercontinuousNMPwithportalperfusionviatheumbilical
vein.
Results: In all livers access to the portal venous system via the umbilical vein was
successfully achieved, with good portal flows and macroscopically homogeneous
perfusion.ThefulllivergraftthatunderwentNMPviatheumbilicalveinforfourhours
showedgoodlactateclearance,normalizedpHandachievedgoodbileproductionwith
pH>7.55.DuringthesplitprocedureundercontinuousNMPviatheumbilicalvein,the
left lateral segment and extended right lobe remained equally perfused, as
demonstratedbyDoppler-ultrasound.
Conclusion:Machineperfusionwithportalperfusionviatheumbilicalveinis feasible.
Portalvenousflowsweresimilartothoseobtainedaftercannulationoftheportalvein
main stem. This technique enables continuous oxygenated perfusion of liver grafts
duringprocurement,splittingandimplantation.
INTRODUCTION
Livertransplantationisthetreatmentofchoiceforpatientswithend-stageliverdisease.
However, donor organ shortage remains a limiting factor in the wider application of
liver transplantation.Thisdiscrepancybetweenorganavailabilityanddemandhas led
totheincreaseduseofso-called‘extendedcriteria’donor(ECD)grafts.TheuseofECD
livers is associated with increased rates of ischemia-reperfusion injury-related
complications, such as primary graft non-function, early allograft dysfunction, and
biliary complications.1 This has led to a large number of livers being declined for
transplantation. Ex situ oxygenatedmachine perfusion is increasingly applied to ECD
liverstoreducetheriskofgraftfailure,andhasmadethetransitiontoclinicaltrials.2
Recently,Heetal.reportedthefirstcaseofischemia-freelivertransplantation(IFLT)in
humans.3 Their innovative technique of continuous normothermic machine perfusion
(NMP) during liver procurement, preservation and transplantation is a major
breakthrough, because for the first time a liverwas successfully transplantedwithout
any ischemia or reperfusion. The authors used a donor iliac vein graft that was
anastomosedend-to-sidetothedonorportalveinmainstemtoenablecannulationand
perfusionof theportalvenoussystemwithout interruptingthebloodcirculation,even
duringporto-portalanastomosisintherecipient.3However,thisadditionalend-to-side
anastomosis may predispose to thrombosis, potentially leading to portal venous
complications.
Our group recentlypostulated theuseof the surgically reopenedumbilical vein as an
alternativeroute to theportalvenoussystemtoovercome theneed toanastomosean
iliacveingraft to theportalveinmainstem.4Access to theportalvenoussystemviaa
surgically reopenedumbilical veinhaspreviouslybeenused for successful retrograde
tumorthrombectomyoftheportalveinmainstem.5Therefore,wehypothesizedthata
surgically reopened umbilical vein would provide good access to the portal venous
system formachineperfusion (Figure1A-B).Weherepresentour first experiencesof
human livermachine perfusionwith portal perfusion via the umbilical vein in a pre-
clinicalsetting.
METHODS
BetweenJanuaryandMay2018, fivehumanECDliversdeclinedfortransplantation in
theEurotransplant regionwere offered to our center formachineperfusion research.
This studywas approved by themedical ethical committee of the UniversityMedical
CenterGroningenandtheDutchTransplantSociety,thecompetentauthorityfororgan
donationintheNetherlands.Donorrelativesprovidedconsentforresearchpriortothe
donationprocedure.Foralllivers,donationaftercirculatorydeathcombinedwithdonor
ageexceeding60yearswasthereasonforgraftdiscard.Allorganswereprocuredusing
asuper-rapidprocurementtechniquedescribedpreviously.6
Organinspectionandpreparationformachineperfusion
Allliverswerepreparedfordualmachineperfusionusingtheumbilicalveinforportal
perfusion and the supratruncal aorta for arterial perfusion. Opening of the umbilical
veinwasperformedbycarefulexplorationoftheroundligamentoftheliver(Figure1C).
Assoonastheumbilicalveinwasidentifiedanddissected,aFogartyballooncatheter(8
Fr,EdwardsLifeSciences,Nyon,Switzerland)was introduced todilate theobliterated
vessel(Figure1D)toallowadequateopeningof theentrance intothe left intrahepatic
portal veinbranch (Figure1E). Inall five livers, a connectionbetween theportalvein
and umbilical vein could be obtained easily (Figure 1F).Hereafter, the portal cannula
from the Liver Assist device (Organ Assist, Groningen, the Netherlands)was inserted
intotheumbilicalveinwithitstipclosetothelumenoftheleftportalveinbranchand
wassecured(Figure1G).Theproximalstumpoftheportalveinmainstemwasclosed
withanon-traumaticvascular clamp (Figure1H).The first three liverswereperfused
hypothermically (10-12 ºC) with University of Wisconsin (UW) Machine Perfusion
solution(BridgetoLife,London,UK).Livers#4and#5wereperfusednormothermically
(37ºC) with our clinically used NMP solution containing a hemoglobin-based oxygen
carrier.6Thehypothermicandnormothermicoxygenatedmachineperfusionprocedures
were performed using the Liver Assist, a pressure-controlled perfusion device, as
describedpreviously.6,7
Figure 1. A: Schematic drawing of human portal venous anatomy with usual machine
perfusion via the portal vein main stem. B: Schematic drawing of machine perfusion
through the umbilical veinwith alternative flowpattern. C: Theumbilical ligament of a
humandonorliverpriortodissectionoftheumbilicalvein.D:IntroductionoftheFogarty
balloon catheter to pneumatically dilate the obliterated umbilical vein. E. Adequately
dilatedinsertionoftheumbilicalveinintotheleftintrahepaticportalveinbranch(denoted
by the *). F: Connection between umbilical vein and portal vein main stem ensured
(demonstratedbyaprobe).G:Cannulationof theumbilicalveinwitha24Frcannula.H:
Normothermicmachineperfusionvia theumbilicalveinand thesupratruncalaorta.The
proximal stump of the portal veinmain stemwas closedwith a non-traumatic vascular
clamp. Abbreviations: FBC: Fogarty balloon catheter, PV: portal vein, SA: supratruncal
aorta,UL:umbilicalligament,UV:umbilicalvein.
RESULTS
Hypothermicmachineperfusionviatheumbilicalvein
In the first liver, a smaller cannula (12 Fr) than usual (24 Fr)was introduced in the
umbilical vein. However, due to the increased resistance of the smaller cannula,
umbilicalveinflowswerelower(80-100mL/minatapresetpressureof5mmHg)than
previouslydescribedduringhypothermicmachineperfusion(i.e.,200-300mL/minat5
mmHg).5Inlivers#2and#3,theumbilicalveinwascannulatedwiththeusualcannula
forportalveincannulation(24Fr).Inthesecases,umbilicalveinflowratesweresimilar
tovaluesobtainedduringnormalhypothermicperfusionviatheportalveinmainstem.
(i.e.,>200mL/minatapressureof5mmHg).6Pulsatilearterialflowswerecomparable
(75-100mL/min at a preset pressure of 25mmHg) to flows as described previously
duringdualhypothermicmachineperfusion(i.e.,50-100mL/minat25mmHG).6
Normothermicmachineperfusionviatheumbilicalvein
The fourth liver was prepared for NMP through the umbilical vein and supratruncal
aorta (Figure2A).DuringNMP, this full livergraft cleared lactate (Figure2B)and the
perfusatepHreachednormalvalueswithintwohours(Figure2C).Dopplerultrasound
analysisconfirmedaccuratepositionofthetipoftheperfusioncatheterjustpriortothe
lumenoftheleftportalveinbranch(Figure2D),demonstratedadequatebloodflowin
both the left and the right portal venous branches (Figure 2E), as well as in all the
hepatic veins (Figure 2F). To analyze the bile production from the left and right liver
lobeseparately,boththe leftandrighthepaticbileductwerecannulatedandbilewas
collectedfromeachliverlobe.Theamountofbileproducedwas>10ml.Afteronehour
ofNMP,thepHofthebilefrombothliverlobeswas>7.55,andaftertwohoursofNMP
>7.65.
Figure2.A:Normothermicmachineperfusionviatheumbilicalvein.B:Lactateclearance
of the full liver graft during normothermic machine perfusion. C: Normalization of
perfusate pH of the full liver graft during normothermicmachine perfusion. No sodium
bicarbonate was administered. D: Ultrasound image with doppler acknowledging the
position of the 24Fr perfusion cannula (denoted by the *) in the umbilical vein. E:
Ultrasound image with doppler demonstrating the patency of peripheral portal vein
branches in the right liver lobe.F: Ultrasound imagewith doppler visualizing adequate
venousoutflowfromtherighthepaticvein.Abbreviations:LPV:leftportalvein,PV:portal
vein,RHV:righthepaticvein,SA:supratruncalaorta,S7PV:segment7portalveinbranch,
UV:umbilicalvein.
Experimentalexsituleftlateralsegmentsplitprocedure
ThefifthliverwaspreparedforNMPthroughtheumbilicalveinandsupratruncalaorta
toassessthefeasibilityofaleftlateralsegment(LLS)splitprocedureundercontinuous
NMPwith subsequent continuedmachine perfusion of the LLS graft. The portal vein
cannula (24 Fr) was introduced in the umbilical vein and the arterial cannula in the
supratruncalaortaafterwhichNMPwasinitiated(Figure3A).Theorganwasperfused
at 37 ºC during transection of the liver parenchyma using the CUSA device (Excel+,
Integra LifeSciences, Tullamore, Ireland), followedby sharp division of the hilar plate
(Figure3B,C). Finally, under continuousoxygenatedNMP the right hepatic artery and
rightportalveinweredividedandthelefthepaticveinwasdissectedfromtheinferior
vena cava. The extended right lobe was removed from the reservoir while the LLS
remainedundercontinuousNMP(Figure3D).Theextendedrightlobewasimmediately
flushedandpreservedinabowlwithUWsolutionandsterileice.Inthehourfollowing
the splittingprocedure, theLLSgraft cleared lactateand thepHof theperfusion fluid
maintained within normal values (between 7.35-7.45). The umbilical venous and
pulsatile arterial flows of the LLS remained >400 mL/min and 150-200 mL/min,
respectively.
Figure3.A:Experimentalsettingforthesplittingofliver5.Theportalveinwasclamped
and the whole liver graft was perfused normothermically via the umbilical vein. B:
Experimental setting for the splittingof liver5.TheLLSwasperfusedwithNMPvia the
umbilicalveinandsupratruncalaortaafterthesplitting.TheERLwasremovedfromthe
perfusion device andpreserved on ice. C: Left lateral split procedure during continuous
normothermic machine perfusion. D: Normothermic machine perfusion of left lateral
segmentaftersplittingundernormothermicmachineperfusionviatheumbilicalveinand
supratruncal aorta. E: Conceptual clinical ex situ splitting procedure: until portal vein
dissection, continuous oxygenated machine perfusion via the portal vein main stem is
performed. The umbilical vein is cannulated but clamped to prevent blackflow. F:
Conceptual ex situ split procedure: after portal vein dissection, hypothermic machine
perfusion via both the portal vein main stem and umbilical vein allows continuous
oxygenation of both partial liver grafts during and after splitting. Abbreviations: ERL:
extended right lobe, LHV: lefthepatic vein, LLS: left lateral segment,PV:portal vein, SA:
supratruncal,aortaUV:umbilicalvein.
Proposed ex situ split procedure using continuous oxygenated hypothermic
machineperfusion.
Theabovementionedconceptcouldalsobeappliedbyusingsingle(portalvenousonly)
ordual(portalvenousandarterial)hypothermicmachineperfusiontoallowcontinuous
oxygenatedLLS andextended right lobe split, or even full-left and full-right lobe split
procedure.Todoso,portalveinmainstemandumbilicalveinshouldbothbecannulated
with a portal vein cannula (24 Fr). For dual perfusion, the arterial cannula should be
introduced in the supratruncal aorta. For the parenchymal transection phase
hypothermicoxygenatedmachineperfusioncanbeinitiatedviathecannulaintheportal
veinmainstem,while thecannula in theumbilicalveinshouldbeclamped toprevent
backflow(Figure3E).Afterdivisionofthehilarplate,theleftportalveincanbedivided
andclamped.Portalvenousperfusionviatheumbilicalveincanbeinitiatedtoperfuse
theLLSor full-left lobe,while continuousperfusionof theextendedright lobeor full-
rightlobeismaintainedviatheportalveinmainstem(Figure3F).Afterdivisionofthe
left hepatic artery, perfusion via the supratruncal aorta allows dual hypothermic
oxygenatedmachineperfusionoftheextendedrightlobeorfull-rightlobe,whereasthe
LLSorfull-leftlobecanbeperfusedviatheumbilicalveinonly.
DISCUSSION
In this proof of concept study, we show for the first time that machine perfusion of
humandonorliversviathesurgicallyreopenedumbilicalveininsteadoftheportalvein
main stem is technically feasible. This modification may simplify the previously
described technique of IFLT as it may allow procurement, preservation as well as
implantation with a standard end-to-end porto-portal anastomosis in the recipient
under continuousoxygenatedportal venousmachineperfusionvia theumbilical vein,
withouttheneedtoanastomoseaniliacveingrafttotheportalveinmainstem.Wealso
demonstrate the technical feasibility of a left lateral segment split procedure under
continuousNMPviathesurgicallyreopenedumbilicalveinaswellasthesupratruncal
aorta.
The first three liverswere perfused hypothermically, duringwhich it is currently not
possible to perform viability testing. We have assessed the flow rates through the
umbilical vein and compared this with the usual portal vein flows observed in our
clinical hypothermic machine perfusions in humans.6 We noticed that when using a
standard24Frcannula forumbilicalveinperfusion, flowswerecomparable to typical
hypothermicperfusionviatheportalveinmainstem(200-300ml/min).Meticulouscare
should be taken to avoid twisting of the umbilical vein cannula becausewe observed
thatthisimmediatelyimpairedportalvenousflow.
The fourth liver perfusion experiment demonstrated that our clinically used viability
criteria for donor livers during NMP2 (after 150 minutes of NMP: perfusate lactate
<1.7mmol/L, perfusate pH between 7.35-7.45, bile pH >7.45, Dutch Trial Register,
#NTR5972)werereachedbyusingportalvenousperfusionviatheumbilicalvein.
Inthefifthliver,wehaveperformedaLLSsplitprocedureundercontinuousNMPusing
portalvenousperfusionviathesurgicallyreopenedumbilicalvein.Aftercompletionof
thesplitprocedure,NMPoftheleftlateralsegmentwascontinued.Inthefollowinghour,
lactate was cleared and the pH remained within normal values. We propose that by
introducingacannulaintheportalveinmainstemaswellasacannulainthesurgically
reopened umbilical vein,machine perfusion of the LLS or full-left lobe aswell as the
extendedrightorfull-rightlobecanbemaintainedevenaftercompleteseparationofthe
twoliverparts.
Weenvisionthatsplittingundercontinuousoxygenatedhypothermicmachineperfusion
could be beneficial, for example, for logistical reasons to allow sequential liver
transplantation in the same centre (conceptualized in Figure 3E,F). Also, hypothermic
oxygenatedmachineperfusion is lessprone to technical failureand isassociatedwith
lowerflowrateswhenusingapressure-controlledmachineperfusiondevice.Wehave,
however,notexperiencedtroublewithflowobstructionduringtheNMPsplitprocedure.
Whenusingcontinuousoxygenatedhypothermicmachineperfusion, the transfer from
onemachinetoanotherortostaticcoldstoragepriortoimplantationcanbeperformed
without additional warm ischemic injury. At normothermic temperatures, we do not
consideritbeneficialtoperfuseboththeextendedrightorfull-rightlobeandtheLLSor
full left lobe simultaneously. For NMP, arterial perfusion is required and arterial
cannulationofeithertheleftortherighthepaticarterymayriskadditionalinjurytothe
vascularendothelium.Therefore,weproposethatcontinuoushypothermicoxygenated
machineperfusionduringsplittingwillbemostbeneficialinclinicalpractice.
In this proof of concept study,we have demonstrated for the first time thatmachine
perfusion through the surgically reopenedumbilical vein indiscardedhuman livers is
technically feasible, thereby achieving adequate portal venous flows. Future studies
should investigate theadditional clinicalutilityofmachineperfusionvia theumbilical
vein,whichshouldincludehistopathologicalanalysisoftheparenchymaandbiliarytree.
REFERENCES
1. Durand F, Renz JF, Alkofer B, et al. Report of the Paris consensus meeting onexpandedcriteriadonors in livertransplantation.LiverTranspl.2008;14:1694–1707.
2. DeMeijerVE,FujiyoshiM,PorteRJ.Exsitumachineperfusionstrategiesinlivertransplantation.JHepatol.2018;doi:10.1016/j.jhep.2018.09.019
3. HeX,GuoZ,ZhaoQ,etal.Thefirstcaseofischemia-freeorgantransplantationinhumans:Aproofofconcept.AmJTransplant.2018;18(3):737-744.
4. vanLeeuwenOB,UbbinkR,deMeijerVE,PorteRJ.Thefirstcaseofischemia-freeorgan transplantation in humans: A proof of concept. Am J Transplant.2018;18(8):2091.
5. Soyama A, Eguchi S, Takatsuki M, et al. Tumor thrombectomy via a surgicallyreopenedumbilicalveincombinedwithrighthemi-hepatectomyinapatientwithhepatocellularcarcinoma.DigSurg.2011;28(3):222-225.
6. vanRijnR,KarimianN,MattonA, et al.Dualhypothermicoxygenatedmachineperfusion in liver transplants donated after circulatory death. Br J Surgery.2017;104(7):907-917.
7. MattonAPM,BurlageLC, vanRijnR, et al.Normothermicmachineperfusionofdonorliverswithouttheneedforhumanbloodproducts.LiverTransplantation.2018;24(4):528-538.
SUMMARYPART1
The first part of this thesis contains a review and three observational studies on
identifyingtheboundariesoftransplantationofsuboptimaldonorlivers.
Afterageneralintroductioninchapter1,areviewwaspresentedinchapter2focusing
on biliary complications after liver transplantation. Bile leaks and bile duct strictures
(anastomoticornon-anastomotic)are themostcommontypesofbiliarycomplication.
Of these, non-anastomotic strictures (NAS) are themost troublesome and difficult to
treat.Patientsreceivingadonationaftercirculatorydeath(DCD)livergraft,livingdonor
graft, or a split liver graft are at increased risk of developing biliary complications.
Although ischemia and subsequent reperfusion injury of the bile ducts is amain risk
factorforthedevelopmentofNAS,othermechanisms,suchasimmune-mediatedinjury,
bilesalt toxicity,and insufficientregenerationof theepitheliumalsoplayarole in the
pathogenesis.
Inchapter3theresultsofanationwideretrospectivestudyontheassociationbetween
donor hepatectomy time and the development of biliary injury during DCD liver
transplantationarepresented.Donorhepatectomytimewasdefinedastheperiodfrom
theinitiationofcoldflushinguntiltheliverwasremovedfromtheabdominalcavityand
placedintoabowlwithice-coldpreservationsolution.Theimpactofdonorhepatectomy
timeonbiliary injurywas studied ina chronological fashion.First, itwasobserved in
humanbileductbiopsiesthatdonorhepatectomytimenegativelyinfluencedthedegree
ofbileductinjurypriortotransplantation.Secondly,liverswithprolongedhepatectomy
time produced bile of inferior quality during normothermic machine perfusion,
displayedbylowerbiliarybicarbonatesecretionandthereforealowerbilepH.Lastly,in
anationwideretrospectivedatabasestudy,donorhepatectomytimewasidentifiedasan
independent significant risk factor for the development of NAS after DCD liver
transplantation. Inconclusion:donorhepatectomytime influences thedevelopmentof
biliary injury in DCD liver transplantation. The results from this study suggest that
donor hepatectomy time should be kept as short as possible to reduce rates of post-
transplantcholangiopathy.
Chapter4containsfindingsthat implicatetheroleofdonorbloodcompositiononthe
development of NAS after DCD liver transplantation. We hypothesized that donor
hematocrit, thrombocyte and leukocyte counts could influence the rates of NAS after
transplantation.Forexample,hematocritcouldaffecttheviscosityoftheblood,platelets
can play a role in endothelial activation, and similar effects can be attributed to
leukocytes, which also can initiate local vasodilation, and all of these factors can
influencegraft flush-out,andthereby influencetheseverityofbiliary injury.First, ina
histological analysis of 40 bile duct biopsies of human donor livers, increased donor
platelet counts and reduced leukocyte counts were associated with a high bile duct
injury score (Odds Ratio 2.553, 95%CI 1.082-6.021, p=0.029 and Odds Ratio 0.734
95%CI 0.581-0.927, p=0.009, respectively). Secondly, during normothermic machine
perfusion(NMP)oftheabovementionedlivers,graftsofdonorswithincreasedplatelet
countandreducedleukocytecountproducedbilewithlowerbiliarybicarbonateandpH
levels, indicating more severe biliary injury. Lastly, in a nationwide retrospective
database analysis, donor hematocrit and platelet count were identified as significant
independent risk factors for the development of NAS after DCD liver transplantation
(HazardRatio1.04795%CI1.007-1.089,p=0.022andHazardRatio1.04495%CI1.005-
1.083,p=0.025).Altogether, thesedatasuggest thatbloodcompositionof thedonor is
associatedwiththedevelopmentofbiliaryinjuryduringDCD-LT.
In the studydescribed inChapter5,weaimed to assess the safetyof theuseofDCD
livers forpatients that requirea re-transplantationof the liver. In theWesternworld,
DBD livers are the golden standard when it comes to graft selection for re-
transplantation.However,over the last years, the three liver transplant centers in the
Netherlands have performed several re-transplantations with a DCD liver. In this
observational study, we compared the outcomes after DCD re-transplantation with a
matched cohort of DBD re-transplantations. Interestingly, graft and patient survival
weresimilaramongbothgroups.RatesofNASintheDCDcohortwerehigh(38%),but
therequirementforretransplantationfortheseNAScaseswaslow.Thisstudysuggests
thatforselectedre-transplantationcandidates,usingaDCDgraftfromayoung,healthy
donormayleadtonon-inferioroutcomes.DCDliversshouldthereforenotberoutinely
declinedforre-transplantationcandidates.
SUMMARYPARTII:
The second part of this thesis contains studies aiming to expand the boundaries of
transplantationofsuboptimaldonorlivers.
In Chapter 6, a histological analysis was performed of bile duct biopsies of 10 DCD
liversthatunderwentend-ischemicdualhypothermicmachineperfusion(DHOPE)prior
to graft implantation, compared with a historical cohort of 20 DCD livers without
machineperfusionofwhichbileductbiopsiesweretaken.Uponbaseline,prior toany
intervention, no difference was observed between the DHOPE group and the control
group.Aftergraftreperfusion,liversthathadunderwentDHOPEdisplayedlessstroma
necrosis and less periluminal and deep peribiliary gland injury after reperfusion,
comparedtothecontrolgroupofliversthatwerecontinuouslypreservedonice.From
this study, it was concluded that DHOPE attenuates the histological sequelae of
ischemia-reperfusioninjuryofthebiliarytree.
In Chapter 7, the results of a preclinical study on extended hypothermic dynamic
preservation are presented. We investigated the safety of prolonged DHOPE by
comparing liver graft function after 2, 6 and 24 hours of DHOPE. Following dynamic
preservationof2,6or24hoursusingDHOPE,reperfusionwithautologousbloodwas
performed and liver graft function was tested. Interestingly, no differences in lactate
clearance, pH stabilization, bile production and bile composition were observed
between the groups. All analyzed markers of endothelial distress and/or injury
displayednodifferencesbetweenthe2,6and24hoursofDHOPEgroups.Additionally,
as proof of concept two human livers declined for transplantation underwent
hypothermicdynamicpreservationusingDHOPEfor20hourspriortorewarmingand
reperfusion. These human liver grafts also showed excellent hepatobiliary viability
duringNMP.Fromthisstudy, itwasconcludedthatitseemssafetoextendDHOPEfor
up to24hours.Afterconfirmation ina transplantation-setting, thisstrategymayhave
substantial clinical impact because it may simplify the difficult logistics around
transplantsandcaninitiateday-timelivertransplantsurgery.
Inchapter8,wedescribetheresultsfromaprospectiveclinicaltrial,theDHOPE-COR-
NMPtrial.Inthisstudy,allnationwidedeclinedliverswereofferedforinclusioninthe
protocol.Mainly,theofferedgraftswereDCDliverswithadonorageexceeding60years,
or DCD grafts with high percentage of steatosis. Livers first underwent one hour of
DHOPE, to resuscitate themitochondriaandprevent subsequent ischemia-reperfusion
injury. After 60 minutes of controlled oxygenated rewarming (COR) to 37°C,
normothermicmachine perfusion (NMP)was continued.Within the first 2.5 hours of
NMP, livershadtomeet the followingcriteria:perfusate lactate<1.8mmol/L,pH7.35-
7.45,bileproduction>10mLandbiliarypH>7.45.Withinthetrialperiod,sixteenlivers
underwent DHOPE-COR-NMP. All livers showed adequate liver parenchymal function
andclearedlactateandproducedbile.However,onlyelevenofsixteenliversreacheda
bilepH>7.45andwere thereforesuitable for safe transplantation.One-yeargraftand
patientsurvival following theseeleven transplantswere100%.With theDHOPE-COR-
NMP protocol, 69% of livers that were previously discarded were successfully
transplantedwitha100%graftsurvivalat12months,resultinginanover20%increase
in the number of post-mortal liver transplantations in the University Medical Center
Groningen.
Theaimofthestudyinchapter9wastofindamethodtosimplifyischemia-freeliver
transplantationasperformedby the transplant team in theFirstAffiliatedHospitalof
SunYat-senUniversity, Guangzhou, China. InGuangzhou, a small interposition vein is
placed end-to-side on the portal vein, to allow cannulation and continuous perfusion
duringprocurement,preservationandimplantation.Wehypothesizedthatcannulation
ofthesurgicallyreopenedumbilicalveinwouldallowcontinuousperfusionaswell.To
test this,weperfusedfivedonor liversvia theumbilicalveinandmonitoredperfusion
closely.Thefirstthreeliverswereperfusedhypothermically,andadequateflowswere
observed with low pressures, similar to regular (D)HOPE. The next two livers were
perfusednormothermically.Thefirstclearedlactate,normalizedpHandproducedhigh
qualitybile.Thiswasalsoobservedinthesecondliver,whichwas‘splitonthepump’.In
this chapter,we have also described amethod for splitting liver grafts ‘on the pump’
withthefeasibilityofsubsequentischemia-freeimplantationoftheleftlateralsegment
graft.
Discussionandfutureperspectives
Through the studies in this thesis we have attempted to elucidate the boundaries of
transplantation of suboptimal donor livers. However, large parts of the grey area
between transplantable and non-transplantable livers remain unexplored. Future
studiescanhelprecognizethepathophysiologybehindcomplicationsthatrepresentthe
actual boundaries. Once themechanisms of these complications are fully understood,
onecanattempttopushtheboundariesbyapplyingnoveltherapies.Inthispartofthe
thesis,theresultsofthestudiesdescribedwillbediscussed,andfutureperspectivesfor
studiesonsuboptimallivertransplantationareconsidered.
In an attempt to introduce a chronological order to this thesis, chapter 2 provided
backgroundandrationaleforchapter3-5.BiliarycomplicationsformtheAchilles’heel
ofDCDlivertransplantation.Overthelastyears,thepathophysiologyofpost-transplant
cholangiopathyhasbeenextensivelystudied.1OpdenDriesetal showed in2014 that
biliarycomplicationsarelargelypredictedbytheseverityofhistologicalinjuryobserved
upon arrival of the graft in the transplant center.2 Two specific aspects of the biliary
injury have a very strong predictive value for NAS: damage to the peribiliary glands
(PBG’s)anddamagetotheperibiliaryvascularplexus(PVP)locatedinthebileductwall.
Interestingly, in the study by op den Dries, a large increase in biliary damage was
observeddirectly after graft reperfusion in the recipient, demonstrating the impactof
reperfusion injury following ischemia.2 This offers the potential for a therapeutic
intervention in the period between arrival of the organ and graft reperfusion, the so-
called‘end-ischemicperiod’,andthisformedtherationaleforinitiatingtheclinicaltrial
of which chapter 7 was a satellite study.3 Possible end-ischemic interventions can
attenuatereperfusioninjury,andtherebyreduceratesofNASaftertransplantation.
However,intheabsenceofregenerativetherapy,goingbeyondattenuatingreperfusion
injuryisnotyetpossible.Futurestudiesaimingatrepairingthedamagethatisalready
presentuponarrivalofthegraft,areeagerlyawaited.Asactiverepairisnotyetfeasible,
someofthechaptersinthisthesisarefocusedonidentifyingmechanismsthatinfluence
theseverityofbiliaryinjuryalreadybeforearrivalinthetransplantcenter.Thisincludes
chapter3,wherethedonorhepatectomytimewasidentifiedasacrucialperiodinthe
development of biliary injury. If this period is kept short, biliary injury isminimized.
However, over the last decades, training and regular feedback for organprocurement
teams has apparently been insufficient in the Netherlands. In the same period in the
United Kingdom, regulations required a donor hepatectomy time to be below 45
minutes.4 In theNetherlands, themedianhepatectomy timeover the last fifteenyears
has been 63 minutes, with cases exceeding two hours. This can partly explain the
extremelyhigh ratesofNAS in theNetherlands thathavebeenreportedpreviously.5-7
Futureperspectivesinthepreventionofhepatectomytimeinducedbiliaryinjurymainly
comprises education of donor surgeons and introduction of normothermic regional
perfusion (NRP).With NRP, impressive results have been observed in terms of post-
transplant cholangiopathy rates and graft survival.8,9 NRP is a method in which a
perfusiondevice(e.g.extracorporealmembraneoxygenationdevice)isusedtoperfuse
the abdominal (and potentially also the thoracic) cavity via large cannulas after
circulatoryarrestofthedonor.Thismethodquicklyleadstorestorationofintracellular
adenosinetriphosphatelevelsandhypotheticallyconvertsaDCDprocedureintoamore
controlledprocedure.8,9Sofar,norandomizedcontrolledtrialshavebeenperformedor
initiated to our knowledge, but NRP appears to have the potential to reduce rates of
biliarycomplicationsafterDCDlivertransplantation.
Another study on the mechanisms influencing biliary injury prior to arrival in the
recipient transplant center is described in chapter 4, which provides a significant
amountoffuelforfutureperspectives.Thereweretworationalesforthisstudy.First,it
still remains uncertain whether the two aspects of biliary injury that predict post-
transplant cholangiopathy, namely peribiliary gland and peribiliary vascular plexus
injury,bothsimplyoccursimultaneouslyasaresultofdonorwarmischemiaintheDCD
donor,or that theyoccursequential.So far,nostudieshavebeenperformed involving
bileductbiopsiestakenuponorganprocurement,butitwouldbehighlyinterestingto
see if both PBG and PVP injury are already present prior to static cold preservation
(SCS),orwhethertheydevelopsimultaneouslyduringSCS.Itcanbehypothesizedthatif
PVP injurywould develop prior to PBG injury, perhaps PBG injury can be prevented
wheninterventionsagainstPVPinjuryareinitiated.
Secondly, it is still uncertainwhether the additionalwarm ischemia that DCD donors
encounterincomparisontoDBDdonorsissolelyresponsiblefortheincreaseinbiliary
injury following DCD liver transplantation. Other mechanisms that can lead to PVP
injury are present in a DCD donor in the process of dying. Unfortunately, not much
research has been performed on how the vasculature responds to an approaching
circulatory arrest and to the first minutes after cessation of blood flow. Severe
peripheral vasoconstriction would for example lead to less effective flush-out and
therefore potentially aggravate peripheral PVP injury. The circulatory arrest and
subsequent blood stasis is also pro-thrombotic, and can cause flush-out problems by
microthrombiformation.
However,interestingly,therehasbeenquitealotofresearchperformedonthevascular
response to hypoxia,which is largely dependent on endothelial cell function.10-13DCD
donorsexperienceasignificantperiodofhypoxiapriortocirculatoryarrest.Endothelial
cellfunctionisdependentonmanyaspects,includingageandatheroscleroticdisease.It
has been described that young healthy people respond to hypoxia with peripheral
vasodilation, but that this response completely disappears as people age.10 This can
explainourobservationthatbiliary injuryuponarrival in therecipientcenter ismore
extremeinelderlydonors.Overthelastyears,afteridentifyingdonorageasariskfactor
forNAS, ithasbeenhypothesizedthatafter transplantation,oldergraftshavereduced
regenerativecapacityfromtheperibiliaryglands.However,theobservationthatbiliary
injury is already more severe upon arrival in the recipient center prior to graft
reperfusion, partially contradicts this hypothesis, and suggests involvement of other
mechanismsearlierinthetransplantprocess.
Inchapterfour,especiallythedonorplateletcountappearedtobestronglycorrelatedto
thedevelopmentofbiliaryinjury.Plateletsareknowntoinduceendothelialdysfunction
uponhypoxiaandwethereforehypothesizedinchapter5thatincreasedplateletcount
leads to more vasoconstriction and less efficient arterial flush-out, and thereby
influences biliary injury.14Minor et al observed early in this century that a pre-flush
withstreptokinasepriortoregularice-coldflushingimprovedgraftviability.15Asthisis
an easy intervention that can improve preservation ofmicrovasculature, the effect of
thisdonorpre-flushonbiliaryinjuryshouldbestudied.However,hopefully,theneedto
studysuperior flushing techniquesdisappearswhenNRPbecomesstandardof care in
DCDliverdonors.
Wehypothesized that the associationbetweenblood composition andpost-transplant
outcomes isparticularlynotablewith respect tobiliary complications.Livergraftsare
flushedthroughtheportalveinuponprocurement,andthereforeadequatecoolingcan
be achieved for the liverparenchymaevenwhen thearterial flushdidnot adequately
rinsethemicrocirculation.However,asthebileductislargelydependentonthehepatic
artery forblood supply, the importanceofhigh-quality arterial flushing is essential in
thepreventionofbiliaryinjury.
Thestudy inchapter5 removeda smallboundary thatmanycentersheldon to: that
DCD livers by definition should not be accepted for patients requiring a re-
transplantation. However, we observed no difference in graft survival between DCD
liversusedforre-transplantationandamatchedcohortofDBDlivers.Weenvisionthat
whenDHOPEwillbeusedregularly,DCDliverscanbeeasilyacceptedforstablepatients
listedforretransplantation.Asinchapter8itisdescribedthatthereisnodifferencein
livergraftfunctionafter2,6and24hoursofDHOPE,therecipienthepatectomyincase
ofaretransplantationcanbeperformedwithouttimepressurewhentheorganisplaced
ontheperfusiondevice.
TheeffectsofDHOPEhavebeenstudiedinseveralchaptersinthisthesis.Inchapter6,
itwasobservedthatDHOPEreducesreperfusioninjuryofthebiliarytree.Moreover,in
appendix I we described the first case of liver transplantation after hypothermic
machine perfusion of a pediatric liver graft, with excellent outcome. Subsequently in
chapter 7, DHOPE allowed safe preservation of liver grafts for up to 24 hours. This
studyprovides rationale for initiatingaday-time liver transplantationprogram.Every
donor liver that is expected to arrive after, for example, 20:00, can be placed on the
perfusiondeviceuntilthenextmorning.Comparisonwiththeinterventiongroupofthe
DHOPE randomized controlled trial (short periods of DHOPE) can be made to
adequatelyassessthesafetyofprolongedDHOPE.Thebenefitofday-timesurgeryisthat
anoptimalteamcanbearrangedandthatthetransplantteamiswell-rested.
With the DHOPE-COR-NMP protocol, in chapter 8 all livers showed excellent
hepatocellular viability. We are convinced that DHOPE is a safe technique and that
centers should first introduce cold perfusion into the clinic, prior to initiating a NMP
program. Starting a NMP programwithout proper experience in the field ofmachine
perfusion isrisky.16 Incontrast tootherstudieswithNMPthatattempttoassessgraft
functionofdiscardedliverstoallowtransplantation,DHOPE-COR-NMPissofartheonly
protocolleadingto100%ofliversmeetinghepatocellularviabilitycriteria.17-19Whether
thisistheresultoftheDHOPEprecedingtheNMP,shouldbestudiedinthefuture.Large
trialswillhavetodemonstratethedirecteffectofDHOPEonNASandgraftsurvival,and
as two large trials in hypothermic machine perfusion have currently closed their
inclusions,theresultsareeagerlyawaited.20,21InappendixII,viabilitycriteriathatcan
beusedtoassessgraftfunctionduringNMParediscussed.
The drawback of DCD liver transplantation remains the biliary injury. Even in the
DHOPE-COR-NMP trial, 31% of the livers were considered ‘non-viable’ based on bile
composition, which reflects bile duct viability. Including the one liver that developed
NAS, thatwouldwith the current experience be declined for transplantation, actually
38% of the livers had too severe biliary injury prior to DHOPE-COR-NMP. Therefore,
even with end-ischemic (D)HOPE for regular DCD livers, such as in the DHOPE-DCD
randomized controlled trial, the percentage of NAS will not be zero, as there will be
always be livers that already arrive with too severe biliary damage. Short donor
hepatectomyandcold ischemia timescanminimize thedegreeofbiliary injurybefore
implantation. In conclusion; DHOPE, and DHOPE-COR-NMP, have stretched the
boundariesoftransplantationofsuboptimaldonorlivers.Topushtheboundarieseven
further,severalinterventionsinthedonorhospitalshouldbestudied,suchasNRP.
LasttodiscussisaveryhopefuldevelopmentinGuangzhou,China,whereatransplant
team succeeded in performing the first series of ischemia-free liver transplantation
(IFLT)worldwide.22With this technique, biliary injurywill hopefullyno longerplay a
major role in liver transplantation. However, it will take some time before
implementation in theWestern world can begin, as a result of the complexity of the
procedureandthelogistics.InGuangzhou,alldonorsweretransferredtotherecipient
hospital,which isnotallowedinmostWesterncountries. InaDCDsetting,completely
ischemia-free transplantation is not possible, as a result of the donorwarm ischemia
time.However,withtheuseofNRPfurtherischemiawillbeavoidedandtheriskofNAS
aftertransplantationwillbelow.OnewaytosimplifyIFLTisdescribedinchapter9.
The studies described in this thesis aimed to allow safe transplantation of high-risk,
suboptimaldonor livers.However, still large amountsofdonor livers aredeclined for
transplantation.Aslongasasignificantnumberofpatientsdieonthewaitinglistforan
organ,transplantphysiciansshouldstudysafetransplantationofthesehigh-riskdonor
organs. As described in an editorial in the New England Journal of Medicine: “risk
aversion has contributed to a shift in the research portfolios of many transplant
programs,awayfromdiscoveryresearchandtowardhealthservicesscienceandclinical
outcomes studies”.23 The study aiming to allow safe transplantation of previously
declineddonorlivers(chapter8),demonstratesthatamutualrisktakenbypatientand
physiciancanleadtoalargestepforwardinthereductionofwaitinglistmortality.Many
future studies are required to decrease waiting list mortality and reduce rates of
complicationsafter transplantation.Toachieve thisgoal,physiciansshouldnotrefrain
fromrisks,but theyshouldenter theboldpath tomedicaladvances togetherwith the
patient.
REFERENCES
1. de Vries Y, von Meijenfeldt F, Porte R. Post-transplant cholangiopathy:Classification,pathogenesis,andpreventivestrategies.BiochimBiophysActaMolBasisDis.2018;1864(4):1507-1515.
2. OpdenDriesS,WesterkampAC,KarimianN,etal.Injurytoperibiliaryglandsandvascular plexus before liver transplantation predicts formation of non-anastomoticbiliarystrictures.JHepatol2014;60:1172-1179.
3. VanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusioninlivertransplantsdonatedaftercirculatorydeath.BrJSurg;104:907-917.
4. FaridSG,AttiaMS,VijayanandD,etal.ImpactofDonorHepatectomyTimeduringOrgan Procurement in Donation after Circulatory Death Liver Transplantation:TheUnitedKingdomExperience.Transplantation.2018.
5. den Dulk AC, Sebib Korkmaz K, de Rooij BJ, et al. High peak alanineaminotransferase determines extra risk for nonanastomotic biliary stricturesafter liver transplantation with donation after circulatory death. Transplantinternational2015;28:492-501.
6. DubbeldJ,HoekstraH,FaridW,etal.Similarlivertransplantationsurvivalwithselected cardiac death donors and brain death donors. Br J Surg 2010;97:744-753.
7. O'Neill S, Roebuck A, Khoo E, et al. A meta-analysis and meta-regression ofoutcomes including biliary complications in donation after cardiac death livertransplantation.TransplInt2014;27:1159-1174.
8. WatsonCJE,HuntF,MesserS,etal. Insitunormothermicperfusionof livers incontrolledcirculatorydeathdonationmaypreventischemiccholangiopathyandimprovegraftsurvival.AmJTransplant.2019Jun;19(6):1745-1758.
9. HessheimerAJ,CollE,TorresF,etal.Normothermicregionalperfusionvs.super-rapid recovery in controlled donation after circulatory death livertransplantation.JHepatol.2019Apr;70(4):658-665.
10. Richards JC, Crecelius AR, Larson DG, Luckasen GJ, Dinenno FA. Impairedperipheralvasodilationduringgradedsystemichypoxia inhealthyolderadults:role of the sympathoadrenal system. Am J Physiol Heart Circ Physiol.2017;312(4):H832-H841.
11. TaddeiS,VirdisA,GhiadoniL,etal.Age-relatedreductionofNOavailabilityandoxidativestressinhumans.Hypertension.2001;38(2):274-279.
12. TaddeiS,VirdisA,MatteiP,etal.Agingandendothelialfunctioninnormotensivesubjectsandpatientswithessentialhypertension.Circulation.1995;91(7):1981-1987.
13. Westby CM, Weil BR, Greiner JJ, Stauffer BL, DeSouza CA. Endothelin-1vasoconstriction and the age-related decline in endothelium-dependentvasodilatationinmen.ClinSci(Lond).2011;120(11):485-491.
14. Tyagi T, Ahmad S, Gupta N, et al. Altered expression of platelet proteins andcalpain activity mediate hypoxia-induced prothrombotic phenotype. Blood.2014;123(8):1250-1260.
15. Yamauchi J, Richter S, Vollmar B, Menger M, Minor T. Warm preflush withstreptokinase improvesmicrovascularprocurementand tissue integrity in livergraft retrieval from non-heart-beating donors. Transplantation.2000;69(9):1780-1784.
16. Bral M, Gala-Lopez B, Bigam D et al. Preliminary Single-Center CanadianExperienceofHumanNormothermicExVivoLiverPerfusion:ResultsofaClinicalTrial.AmJTransplant.2016;17(4):1071-1080.
17. VanLeeuwenOB,deVriesY,FujiyoshiM,etal.Transplantationofhigh-riskdonorlivers after ex situ resuscitation and assessment using combined hypo- andnormothermic machine perfusion: A prospective clinical trial. Ann Surg. 2019.DOI10.1097/SLA.0000000000003540
18. NeilD,HubscherS,LaingR,etal.Viabilitytestingandtransplantationofmarginaldonor livers VITTAL trial outcomes: bile duct injury assessment during thenormothermic machine perfusion of discarded livers. [Abstract]. InternationalLiver Transplantation Society, 25th Annual International Congres 2019(https://2019.ilts.org)
19. Watson CJE, Kosmoliaptsis V, Randle LV, et al. Normothermic perfusion in theassessmentandpreservationofdeclinedliversbeforetransplantation:hyperoxiaand vasoplegia – important lessons from the first 12 cases. Transplantation.2017;101:1084-1098.
20. van Rijn R, van den Berg A, Erdmann J et al. Study protocol for amulticenterrandomized controlled trial to compare the efficacy of end-ischemic dualhypothermic oxygenated machine perfusion with static cold storage inpreventingnon-anastomoticbiliarystricturesaftertransplantationoflivergraftsdonated after circulatory death: DHOPE-DCD trial.BMC Gastroenterol.2019;19(1).doi:10.1186/s12876-019-0956-6
21. Jochmans I, Akhtar MZ, Nasralla D, et al. Past, present, and future of dynamickidney and liver preser- vation and resuscitation. Am J Transplant2016;16:2545–2555.
22. HeX,GuoZ,ZhaoQetal.Thefirstcaseofischemia-freeorgantransplantationinhumans:Aproofofconcept.AmJTransplant2017;18(3):737-744.
23. MontgomeryR.Gettingcomfortablewithrisk.NEJM.2019Oct24;381(17):1606-1607
AppendixI: FirstReportofSuccessfulTransplantationofaPediatricDonorLiverGraftafterHypothermicMachinePerfusion
MaureenJ.M.Werner,OttoB.vanLeeuwen,IrisE.M.deJong,FrankA.J.A.Bodewes,MasatoFujiyoshi,OlafC.Luhker,RenéScheenstra,YvonnedeVries,RubenH.J.deKleine,RobertJ.Porte
PediatrTransplant.2019May;23(3):e13362
ABSTRACT
Oneof themain limiting factors inpediatric liver transplantation isdonoravailability.
Foradults,donationaftercirculatorydeath (DCD) livergraftsare increasinglyused to
expand the donor pool. To improve outcome after DCD liver transplantation, ex situ
machine perfusion is used as an alternative organ preservation strategy, with the
supplementalvalueofprovidingoxygentothegraftduringpreservation.Weherereport
the first successful transplantation of a pediatric DCD liver graft after hypothermic
oxygenatedmachineperfusion.
Thefullsizelivergraftwasderivedfroma13-year-old,femaleDCDdonorandwasend-
ischemicpre-treatedwithdualhypothermicoxygenatedmachineperfusion.Arterialand
portalpressuresweresetat18and4mmHg,slightly lowerthanprotocolizedsettings
foradultlivers.During2hoursofmachineperfusion,portalandarterialflowsincreased
from100to210ml/minand30to63ml/minrespectively.Thepre-treatedlivergraft
was implanted in a 16-year-old girl with progressive familial intrahepatic cholestasis
type 2. Postoperative aspartate aminotransferase, alanine aminotransferase and
prothrombintimenormalizedwithinaweek.Therecipientquicklyrecoveredandwas
discharged from the hospital after 18 days. One year after transplantation she is in
excellentconditionwithacompletelynormalliverfunctionandhistology.
This case is the first reportof successful transplantationofapediatricDCD livergraft
afterhypothermicoxygenatedmachineperfusionandillustratesthepotentialroleofex
situ machine perfusion in expanding the donor pool and improving outcome after
pediatriclivertransplantation.
INTRODUCTION
Orthotopiclivertransplantationistheonlyeffectivetherapyinpatientswithend-stage
liverdisease.Still,donoravailabilityisthemainlimitingfactorinlivertransplantation,
especially inpediatricpatients,whoneedaperfect size-appropriate graft.1To expand
thenumberofsuitablelivergraftsforpediatricrecipients,severaltechnicalvariantsare
practiced, including splittingofdeceasedadultdonor livergrafts and theuseof living
donors. Despite this, waiting list mortality rate is up to 20%.2 Moreover, during the
period on the waiting list children are at great risk of growth and developmental
retardation.
Foradults,donationaftercirculatorydeath (DCD) livergraftsare increasinglyused to
expand the donor pool. Good results with transplantation of DCD liver grafts are
reported, but a major concern remains the high rate of biliary complications. For
children,theuseofDCDgraftsisstillcontroversialandtheavailabledataarelimitedto
smallseries.3,4
To improve outcome of DCD liver transplantation, ex situ hypothermic machine
perfusion(HMP)is increasinglyusedasanalternativestrategyfororganpreservation,
withthesupplementalvalueofprovidingoxygentothegraftduringpreservation.5The
initial experience in adults has demonstrated that end-ischemic HMP provides better
preservationofDCD liver grafts.HMPameliorates ischemia-reperfusion injury inDCD
livergraftsbyrestoringmitochondrialfunctionbeforeimplantationanditoffersbetter
preservationofthebileductsandtheirvasculature.6,7Thisisanimportantstepforward
inreducingbiliarycomplicationsafterDCDlivertransplantation.
Sofar,machineperfusionhasonlybeenreportedinadulttoadultlivertransplantation.
Wehere report the first successful transplantationof apediatricDCD liver graft after
oxygenatedHMP.
CASEPRESENTATION
Thelivergraftwasderivedfroma13-year-old,femaleDCDdonor(65kg,167cm),who
was resuscitated after an out of hospital cardiac arrest. She was admitted to the
intensivecareunitfor7days.Lastserumalanineaminotransferasebeforeprocurement
was65U/L,lastserumsodiumwas162mmol/L.Theagonalphasebetweenwithdrawal
fromlifesupportuntilcirculatoryarrestwas19minutes.Afteramandatory5minutes
‘notouchperiod’,rapidcannulationoftheaortawasperformedandtheliverwasinsitu
perfused with ice-cold Belzer University of Wisconsin (UW) cold storage solution
(supplementedwithheparin).Thetotalperiodfromwithdrawaloflifesupporttoinsitu
coldperfusionendured34minutes.Thebileductsweregentlyflushedinaretrograde
fashionwithUWpreservation solution. Subsequently, the liverwaspacked static cold
storageandtransportedtoourcenter.
In our center the liver graftwas inspected and appeared to be of good quality. Liver
weight was 1509 gram. Because the liver was derived from a DCD donor and to
minimizefurtherischemicinjuryasmuchaspossible,itwasdecidedtopreparetheliver
graft for oxygenated HMP during recipient hepatectomy. A conventional back table
procedureofthegraftwasperformedafterwhichtheportalveinandsupratruncalaorta
were cannulated for machine perfusion. Subsequently, the liver underwent pressure-
controlled dual hypothermic oxygenated machine perfusion using the Liver Assist
(OrganAssist,Groningen,TheNetherlands).Theperfusion fluid consistedof4000mL
Belzer UW machine perfusion solution, supplemented with 3420 mg glutathione.
Perfusionfluidwasoxygenatedwith1L/min100%O2toobtainaPaO2of>70mmHg
andtemperaturewaskeptat10°C,accordingtoourHMPprotocol.6Arterialandportal
pressures were set at 18 and 4mmHg respectively, which is slightly lower than our
protocolizedsettingsforadultlivers(25and5mmHgrespectively).DuringHMPportal
flow increased adequately from 100 to 210 ml/min and arterial flow from 30 to 63
ml/min, whereas pressure and temperature remained stable (Figure 1). Perfusate
glucose level increased in the first 30minutes of HMP from 8.8 to 12.5mmol/L, and
remained stable thereafter. The perfusate lactate level decreased from 2.4 to 1.7
mmol/L.After2hoursofHMPthe liverwasdisconnectedfromtheperfusionmachine
andtransplanted.
Figure1.Portalandarterialflowratesduringtwohoursofdualhypothermic
oxygenatedmachineperfusionofan13-year-oldDCDlivergraft.
Theperfusionmachinewaspressure-controlledwithportalpressuresetat4mmHgand
arterialpressuresetat18mmHg.DCD,donationaftercirculatoryarrest.
Theselectedrecipientwasa16-year-oldgirl(42kg,156cm),whowasdiagnosedinthe
neonatal phase with progressive familial intrahepatic cholestasis type 2. To prevent
progressive damage of the hepatocytes by retention and accumulation of bile salts, a
partialexternalbiliarydiversionprocedurewasperformedwhenshewas4yearsold.8
Despite this, at the ageof14years shewas listed for liver transplantationbecauseof
deterioration of cholestasis with icterus and itching, and bile stoma bleedings. The
recipientandherparentsgaveconsenttoreceiveaHMP-preservedDCDliver.
TheHMP-pretreated full size liver graftwas implantedusing thepiggyback technique
withend-to-endportalandarterialanastomoses.Perioperativebloodlosswas1800ml
and the recipient received one red blood cell transfusion (280 ml) intraoperatively.
Totalcoldpreservationtimeofthedonorlivergraftwas512minutes,consistingof384
minutes of cold ischemic storage and 128 minutes of oxygenated HMP. Subsequent
warm ischemia timewas 33minutes. Immediately after transplantation the recipient
was extubated and admitted to the pediatric intensive care unit where vasopressive
support could be reduced to zero and intravenous heparin was administered as is
routine practice after pediatric transplantation in our center. Postoperative aspartate
aminotransferase, alanine aminotransferase and prothrombin time rapidly decreased
andnormalizedwithinaweek(Figure2a).Alkalinephosphataseandgamma-glutamyl
transferase normalized within a month and remained stable afterwards. Immediate
postoperative lactatewas3.5mmol/Land levels steadilydecreased thereafter,with a
small second peak on postoperative day 4 when an intra-abdominal bleeding was
diagnosedwhichrequiredsurgicalintervention(Figure2b).Surgicalinspectionshowed
diffuse oozing with a potential bleeding focus at the inferior vena cava which was
clippedandadditionallyahematomawasevacuated.Afterthis,therecipienthadaquick
and further uneventful recovery until she was discharged from the hospital on
postoperative day 18. One year later, the recipient is in excellent condition with a
completely normal liver function with a serum alanine aminotransferase of 16 U/L,
bilirubinof7µmol/Landanormalliverhistologyonroutineliverbiopsy.Therewereno
clinical or histological signs of biliary complications, additional imaging was not
performed.
Figure2.PanelA:SerumAST,ALT,ALPandGGTlevelsina16-year-oldrecipientafter
successfultransplantationofahypothermicoxygenatedmachineperfusedpediatricDCD
livergraft.PanelB:Serumbilirubinandlactateina16-year-oldrecipientaftersuccessful
transplantationofahypothermicoxygenatedmachineperfusedpediatricDCDlivergraft.
AST,aspartateaminotransferase;ALT,alanineaminotransferase;ALP,alkaline
phosphatase;GGT,gamma-glutamyltransferase;DCD,donationaftercirculatoryarrest.
DISCUSSION
This case reportdescribes the first successful transplantationof apediatricDCD liver
graftafterexsituoxygenatedHMP.Thereareonlyafewdescriptionsofpediatric liver
transplantationswith grafts fromDCDdonors in the current literature.3,4,9Hong et al.
reported a matched case-control study of 7 DCD liver transplantations in pediatric
patientswithexcellentlong-termoutcomes.3Abiliaryanastomoticstrictureoccurredin
onlyoneof the recipientsand the incidenceofbiliary complicationswasnotdifferent
betweenDCDanddonationafterbraindeath liver transplantations.AlsoGozinnietal.
havesuggestedthatlivergraftsfromyoungDCDdonorswithshortischemiatimescan
besafelyusedinpediatrictransplantation.9Moreover,vanRijnetal.demonstratedthat
transplantationofpediatricDCDlivergraftsresultsingoodlong-termoutcomes,when
the donorwarm ischemia time is kept under 30minutes.4 Patient- and graft survival
rates were comparable to those of pediatric donation after brain death liver grafts.
Moreover, the incidence of non-anastomotic biliary strictures after transplantation of
pediatric DCD livers was remarkably low. These studies support the use of pediatric
DCDlivergraftsfortransplantation.
AmajordrawbackofDCDlivergraftsisthedevastatingeffectofwarmwithsubsequent
coldischemia,leadingtodepletionofintracellularenergysources,suchasadenosine5'-
triphosphate, combined with other metabolic disturbances. This results into cellular
injuryanddysfunctiondue to reperfusion injuryduring transplantation.10,11 Ischemia-
reperfusioninjuryisamajorcauseofprimarynonfunction,earlyallograftdysfunction
andbiliarycomplicationsaftertransplantation.12
Inadultlivertransplantation,ithasbeendemonstratedthatashortperiod(1-2hours)
of oxygenated HMP after traditional static cold storage restores the hepatic energy
status in liver grafts, reduces ischemia-reperfusion injury, and improves early graft
survival.5,6,13Basedontheseexperiences,wedecidedtoapplyend-ischemicHMPtothe
pediatric DCD liver graft offered to our recipient. Compared to adult liver grafts,
pediatricliversaresmallerandpotentiallymoresusceptibletointravascularpressure-
induced damage. This is important because one of the potential risks of HMP is
endothelial injury due to shear stress. Shear stress occurs in case of high perfusion
pressures, especially at low temperatures when endothelial cell membranes are
susceptible to injury.14 Perfusion induced endothelial cell injury can be prevented by
using low perfusion pressures and a pressure-controlled perfusion system.13,15
Therefore, we used a pressure-controlledmachine perfusion devicewith arterial and
portalperfusionpressureslowerthanvaluesgenerallyusedforadultlivergrafts.16
In the reported casewedemonstratedHMPof a13-year-oldDCD liver graft,which is
relative large.TodetermineoptimalportalandarterialpressuresforHMPinpediatric
liver grafts, more experiences and research are required. In our opinion, perfusion
pressuresinpediatriclivergrafts,shouldbeloweredbasedondonorage,toadjustfor
the lower physiological pressure in the liver graft. For HMP in adult liver grafts,
protocolized portal and arterial perfusion pressures are set at 3-5 and 25 mmHg
respectively.6,13 Normally, an adult liver graft is used to a physiologicalmean arterial
blood pressure of 90 mmHg in the donor, whereas pediatric liver grafts are used to
lower systemic blood pressures. Perhaps we should lower perfusion pressures for
pediatriclivergraftsbasedondonormeanarterialbloodpressuresaccordingtodonor
age. For example, a 5-year old pediatric liver graft, is used to a mean arterial blood
pressureof65mmHg,whichisabout30%lowerwhencomparedto90mmHginadults.
Therefore it seems reasonable to reduce the portal and arterial pressure with 30%,
leading to a portal and arterial perfusion pressure of 3-4 and 18mmHgduringHMP,
respectively.
Inthecomingyears,furtheradvancesinorganpreservation,suchasmachineperfusion
may provide a solution to the problem of donor organ scarcity for pediatric patients.
Machine perfusion of DCD donor grafts might reduce part of the risks of DCD liver
transplantation.With this casewedemonstrated thatHMPof apediatric liver graft is
feasibleandcanbeperformedsafelywithadjustedperfusionpressures.
Apart from providing a better preservation method, machine perfusion can also
facilitate pediatric liver transplantation by enabling a split procedure of a liver graft
under continuous oxygenated perfusion. The concept of splitting a liver graft during
machine perfusion was recently shown by Stephenson et al.17 These investigators
successfullyperformeda splitprocedureof anadult liver graft resulting in a segment
2/3 and an extended right lobe graft. In addition, with the upcoming technique of
normothermicmachine perfusion, which enables ex situ functional assessment of the
liver graft prior to implantation, it might be useful to estimate the suitability of a
suboptimal liver graft for a pediatric recipient.18 Altogether, this may increase the
numberoflivergraftsthataresuitableforpediatriclivertransplantation.
In conclusion,we present the first successful transplantation of a pediatric DCD liver
graftafterexsituhypothermicoxygenatedmachineperfusion.Thiscase illustrates the
potentialroleofexsitumachineperfusiontechnologyinexpandingthedonorpooland
improvingoutcomeafterpediatriclivertransplantation.
REFERENCES
1. Wertheim JA, Petrowsky H, Saab S, Kupiec-Weglinski JW, Busuttil RW. Majorchallenges limiting liver transplantation in the United States. Am J Transplant.2011;11(9):1773-1784.
2. vanderDoefHPJ,vanRheenenPF,vanRosmalenM,RogiersX,VerkadeHJ, forpediatric liver transplantation centers of Eurotransplant.Wait-list mortality ofyoungpatientswithbiliaryatresia:Competingriskanalysisofaeurotransplantregistry-basedcohort.LiverTranspl.2018;24(6):810-819.
3. Hong JC,VenickR,YersizH, etal. Liver transplantation in childrenusingorgandonationafter circulatorydeath:A case-control outcomesanalysisof a20-yearexperienceinasinglecenter.JAMASurg.2014;149(1):77-82.
4. vanRijnR,HooglandPER,LehnerF,vanHeurnELW,PorteRJ.Long-termresultsafter transplantation of pediatric liver grafts from donation after circulatorydeathdonors.PLoSOne.2017;12(4):e0175097.
5. Dutkowski P, Polak WG, Muiesan P, et al. First comparison of hypothermicoxygenatedperfusionversusstaticcoldstorageofhumandonationaftercardiacdeath liver transplants: An international-matched case analysis. Ann Surg.2015;262(5):764-70
6. vanRijnR,KarimianN,MattonAPM,etal.Dualhypothermicoxygenatedmachineperfusion in liver transplants donated after circulatory death. Br J Surg.2017;104(7):907-917.
7. van Rijn R, van Leeuwen OB, Matton APM, et al. Hypothermic oxygenatedmachineperfusion reducesbileduct reperfusion injury after transplantationofdonationaftercirculatorydeathlivers.LiverTranspl.2018;24(5):655-664.
8. YangH,PorteRJ,VerkadeHJ,DeLangenZJ,Hulscher JB.Partialexternalbiliarydiversion in children with progressive familial intrahepatic cholestasis andalagilledisease.JPediatrGastroenterolNutr.2009;49(2):216-221.
9. GozziniS,PereraMT,MayerDA,etal.Livertransplantationinchildrenusingnon-heart-beatingdonors(NHBD).PediatrTransplant.2010;14(4):554-557.
10. de Rougemont O, Breitenstein S, Leskosek B, et al. One hour hypothermicoxygenated perfusion (HOPE) protects nonviable liver allografts donated aftercardiacdeath.AnnSurg.2009;250(5):674-683.
11. XuH,BerendsenT,KimK, et al. Excorporeal normothermicmachineperfusionresuscitates pig DCD livers with extended warm ischemia. J Surg Res.2012;173(2):e83-8.
12. DubbeldJ,HoekstraH,FaridW,etal.Similarlivertransplantationsurvivalwithselectedcardiacdeathdonorsandbraindeathdonors.BrJSurg.2010;97(5):744-753.
13. Schlegel A, de Rougemont O, Graf R, Clavien PA, Dutkowski P. Protectivemechanisms of end-ischemic cold machine perfusion in DCD liver grafts. JHepatol.2013;58(2):278-286.
14. Fondevila C, Hessheimer AJ, Maathuis MH, et al. Hypothermic oxygenatedmachineperfusion inporcinedonationafter circulatorydeterminationofdeathlivertransplant.Transplantation.2012;94(1):22-29.
15. Schlegel A, Dutkowski P. Role of hypothermic machine perfusion in livertransplantation.TransplInt.2015;28(6):677-689.
16. Shore PM, Huang R, Roy L, et al. Potential for liver and kidney donation aftercirculatorydeathininfantsandchildren.Pediatrics.2011;128(3):e631-8.
17. Stephenson BTF, Bonney GK, Laing RW, et al. Proof of concept: Liver splittingduringnormothermicmachineperfusion.JSurgCaseRep.2018;2018(3):rjx218.
18. Ravikumar R, JassemW,Mergental H, et al. Liver transplantation after ex vivonormothermicmachinepreservation:Aphase1(first-in-man)clinicaltrial.AmJTransplant.2016;16(6):1779-1787.
AppendixII: Viabilitycriteriaforfunctionalassessmentofdonorliversduringnormothermicmachinepreservation
OttoB.vanLeeuwen,VincentE.deMeijer,RobertJ.Porte
LiverTranspl.2018Oct;24(10):1333-1335
Persistingdonororganshortagehasledtoanincreaseduseofsuboptimaldonorlivers
for transplantation. Transplantation of these extended criteria donor (ECD) livers,
however, is associated with high rates of complications, including early allograft
dysfunction(EAD)andprimarynon-function(PNF).Asaresult,alargenumberofECD
liversarediscarded.ThedecisiontoacceptordeclineanECDliverfortransplantationis
largely based on empiric and rather subjective criteria available at the time of donor
organoffer,butitmaynotreflecttheactualconditionofanorganafterseveralhoursof
staticcoldstorage(SCS).Exsitumachineperfusionisincreasinglybeingstudied
as a method to resuscitate and functionally assess donor organs shortly before
transplantation. When performed at 37°C, ex situ normothermic machine perfusion
(NMP) enables a metabolic assessment of high-risk liver grafts. However, there is
currentlynoconsensusonthecriteriathatcanbeusedduringNMPtoselectlivergrafts
thatcanbetransplantedsafely,despiteinitialdeclinebasedonanestimatedtoohighof
ariskforEAD/PNF.
In this issue of Liver Transplantation, Mergental et al. report an interesting study in
which they aimed to identify criteria that can be used during NMP to predict PNF of
high-risk donor livers.1 A total of 12 discarded human donor livers underwent NMP
using a perfusion solution based on packed red blood cells for up to 6 hours after a
period of SCS. Perfusate blood gas profiles, bile production, and vascular flow
characteristicswereexaminedtoidentifyparametersthatareassociatedwithpoorliver
functionandahighdegreeofinjuryonhistologyofliverbiopsies.Initially,theauthors
identified lactate clearance as a marker for graft viability. The authors observed 2
distinctgroups:agroupof6organswithasharpdecreaseinlactatelevels,whereasthe
other6showed“fluctuationsandrises”ofthelactatelevelsintheperfusionsolution.
After this observation, further analyses were performed by comparing these lactate-
clearingandnonlactate-clearinggroups.Second,theauthorsnotedlesshepatocellular
injuryonhistology,higherhepaticadenosinetriphosphatelevels,morestableperfusate
pH, and higher bile production in the lactate-clearing group compared with the
nonlactate-clearinggroup.Thesefindingssupportedtheiruseoflactateasanindicator
ofhepatocellular functionandcorroboratespreviousresults fromothergroups.2,3Bile
production,however,wasobservedinonly4ofthe6liversinthelactate-clearinggroup
versus 1 out of 6 livers in the nonlactate-clearing group. The authors conclude that
measurable bile production can be used as a marker of good liver function, but the
absence of bile production does not necessarily imply poor function. Similar
observationshavebeenmadebytransplantgroupsfromCambridgeandCleveland.2,3
Inourexperience,wehavenoted that very loworabsentbile flowcan sometimesbe
explained by a technical issue. For example, the tip of a biliary catheter can be stuck
againstthebileductwallobstructingitslumenandprecludingbileflow.Inaddition,we
havenotedthatbileflowthroughabiliarydrainisdependentonthesizeofthedrain.If
thediameterofthedrainistoolarge,bileflowmaynotcommenceeasily,especiallyas
the drain often makes an uprising loop at the rim of the reservoir (Fig. 1B,C in the
currentarticle).Theuseofasmallfeedingtubecatheter(8-Fr)withanopentipandside
holesmayminimize the risk of these technical issues inmeasuringbile production.A
small-sized catheter provides a capillary force, which facilitates bile flow. These
potential issuesshouldbeconsideredwhenliversseemtoproduceminimalornobile
despitebiochemicalevidenceofgood functional recovery, suchasadecreasing lactate
level.
Collection of bile produced during NMP is important because it may aid in the
assessmentofbileductviabilityduringNMP.4Thisisatopicnotcoveredinthecurrent
studybyMergentaletal.,butitisclinicallyveryrelevant,especiallyintheassessmentof
high-risk livers fromdonationafter circulatorydeath (DCD).DCD livergraftsnotonly
havean increasedriskofhepatocellulardysfunctionthatmay leadtoEADorPNF,but
theyarealsopronetocholangiopathyduetocholangiocellularinjury.5Experimentaland
preclinical studies have indicated that biliary pH, bicarbonate, and lactate
dehydrogenase during NMP may reflect biliary viability.4 Cholangiocytes (biliary
epithelial cells) actively modify bile composition by secretion of bicarbonate and
resorption of glucose, resulting in an alkalotic pH and low glucose level in bile at the
level of the common bile duct. Observations made by the Cambridge group during
clinical applicationofNMP recently supported thepotential value of biliarypH in the
assessment of biliary viability (and thus the risk of posttransplant cholangiopathy)
during NMP.2 However, more research will be needed to establish the diagnostic
accuracyofbilecompositioninassessingbiliaryviability.Identificationandvalidationof
biomarkers and criteriaof bileduct viabilityduringNMPwouldbe an important step
forwardinthewideruseofDCDlivergrafts.
Interestingly,Mergentaletal.notedan increase in injuryof the intrahepaticsmallbile
ductsduringNMPinallbut1oftheliversinthenonlactate-clearinggroupandin2of
the6inthelactate-clearinggroup.Altogether,approximately50%oftheliverssuffered
an increase in biliary injury duringNMP.Unfortunately, histological data on the large
intrahepatic and or extrahepatic bile ductswere not available. Typically, these larger
bile ducts are at risk of ischemia/reperfusion injury, resulting in posttransplant
cholangiopathy.5 Although NMPmaymitigate ischemia/reperfusion injury due to the
absenceofleukocytesandplateletsintheperfusionfluid,injuryduetotheformationof
radicaloxygenspecies(ROS)maystilloccur.Infact,thefirstclinicalstudiesofliverNMP
have not shown a reduction in the incidence of biliary complications after
transplantation compared with SCS.2,6 To improve results, preceding NMP by
oxygenatedhypothermicmachineperfusion(HMP)maybemoreeffectiveasthelatter
has been shown to resuscitatemitochondria, reduce postreperfusion ROS production
andinflammation,andmitigatereperfusioninjuryofthebileducts.7Inaccordancewith
this,2preclinicalstudiesusingdiscardedhumandonorlivershaverecentlyshownthat
a short period of HMP prior to NMP improves metabolic recovery and attenuates
oxidative stress and tissue inflammation.8,9 Therefore, it may be important to
sequentially apply HMP and NMP, especially when NMP is used to assess the
transplantabilityofhigh-riskDCDlivers,which inadditionto theriskofEADandPNF
haveahighriskofdevelopingbiliarycomplicationsaftertransplantation.Liverviability
testingremainsahighlydifficultresearchfieldasthetranslationtoclinicalapplication
mustbeperformedwithexceptionalcare.On thebasisof theprincipleofprimumnon
nocere, patient safety has to be the main concern. This concern has forced clinical
researchgroupstoremainonthesafesidewhenitcomestotransplantationofinitially
declined livers after a positive viability judgment by NMP. On the other hand, a too
prudentialapplicationishamperingtheidentificationofclinicallyrelevantcutoffvalues
ofviabilitycriteria.Withincreasingexperience,however,itcanbeexpectedthatcenters
will startpushing theboundariesbystretching theacceptancecriteria.As longas this
process is carefully monitored and outcome data are published in a standardized
fashion,10 we will collectively learn from this process and be able to effectively and
safelyusethepotentialbenefitsofexsitumachineperfusioninincreasingthenumberof
suitableorgansfortransplantation.
REFERENCES
1. Mergental H, Stephenson B, Laing RW, Kirkham A, Neil D, Wallace L et al.Developmentofclinicalcriteriaforfunctionalassessmenttopredictprimarynon-function of high-risk livers using normothermic machine perfusion. LiverTranspl.2018
2. WatsonCJE,KosmoliaptsisV,PleyC,RandleL,FearC,CrickKetal.Observationson the ex situ perfusion of livers for transplantation. Am J Transplant.2018;18:2005-2020
3. LiuQ,NassarA,BucciniL,IuppaG,SolimanB,PezzatiD,etal.Lipidmetabolismand functionalassessmentofdiscardedhuman liverswithsteatosisundergoing24hoursnormothermicmachineperfusion.LiverTranspl.2018Feb;24:233-245
4. WeederPD,vanRijnR,PorteRJ.Machineperfusioninlivertransplantationasatool to prevent non-anastomotic biliary strictures: Rationale, current evidenceandfuturedirections.JHepatol.2015;63:265-275
5. de Vries Y, von Meijenfeldt FA, Porte RJ. Post-transplant cholangiopathy:Classification, pathogenesis, and preventive strategies. Biochim Biophys Acta.2018;1864:1507-1515
6. NasrallaD,CoussiosCC,MergentalH,AkhtarMZ,ButlerAJ,CeresaCDLetal.Arandomizedtrialofnormothermicpreservation in livertransplantation.Nature.2018;557:50-56.
7. SchlegelA,MullerX,DutkowskiP.Hypothermicliverperfusion.CurrOpinOrganTransplant.2017;22:563-570
8. Westerkamp AC, Karimian N,Matton APM,Mahboub P, van Rijn R,Wiersema-BuistJ,etal.Oxygenatedhypothermicmachineperfusionafterstaticcoldstorageimproves hepatobiliary function of extended criteria donor livers.Transplantation2016;100:825-835
9. Boteon YL, Laing RW, Schlegel A,Wallace L, Smith A, Attard J et al. Combinedhypothermicandnormothermicmachineperfusionimprovesfunctionalrecoveryofextendedcriteriadonorlivers.LiverTranspl.2018.DOI:10.1002/lt.25315
10. KarangwaSA,DutkowskiP,FontesP,FriendPJ,GuarreraJV,MarkmannJFetal.Machine perfusion of donor livers for transplantation: a proposal forstandardized nomenclature and reporting guidelines. Am J Transplant2016;16:2932-2942.
Eenlevertransplantatieistegenwoordigdestandaardbehandelingvoorpatiënteninhet
eindstadiumvaneenleverziekte.Deeerstelevertransplantatiewerduitgevoerddoordr.
Thomas Starzl endiens team inDenver, Colorado, in 1963.Helaas stierf de driejarige
ontvanger peroperatief als gevolg vanmassaal bloedverlies. Hetzelfde probleem deed
zich voor gedurende de volgende vijf transplantaties, met een patiëntoverleving van
maximaal 23 dagen. In 1967 slaagde Starzl erin om de eerste succesvolle
levertransplantatie uit te voeren met een patiëntoverleving van meer dan een jaar.
Twaalf jaar later, na de ontwikkeling van cyclosporine door Calne en tacrolimusdoor
Starzl,ontwikkeldedelevertransplantatiezichtoteengestandaardiseerdebehandeling
metacceptabeleuitkomsten.Opditmomentwordtwereldwijdeen1-jaartransplantaat-
enpatiëntoverlevingvanbovende90%gezien.
Helaasblijfthet tekortaandonororganen immeraanwezigenoverstijgtdevraagnaar
donorlevershetaanbod.Toteindjaren’90werdendemeestedonorleversuitgenomen
uithersendodedonoren.Omhetdonoraanboduittebreidenwerdenvanafdatmoment
ook organen uitgenomen uit patiënten die waren overleden na het stoppen van de
bloedsomloop (donation after circulatory death [DCD] donoren). In het begin werden
goede resultaten behaald bij levertransplantatie met DCD organen. Echter, toen na
enkele jaren de criteria voor DCD lever acceptatie verbreed werden, nam het aantal
postoperatieve complicaties sterk toe. Vooral galwegcomplicaties werden frequent
geziennaDCD-levertransplantatie,meteenincidentievanbijna30%.
In de vroege jaren ’80 ontwikkelde de groep van Folkert Belzer de University of
Wisconsinpreservatievloeistof(UW),dievoorvele jarendegoudenstandaardwerdin
abdominale orgaantransplantatie. Het abdominale compartiment van de donor wordt
tijdens de donoroperatie via de aorta geflushed met meerdere liters ijskoude UW.
HiernawordendeorganenzosnelmogelijkineenzakmetUWopijsineenorgaandoos
gelegd.Dezetechniekvankoudestatischepreservatieishelaasnietvoldoendegebleken
om complicaties naDCD-levertransplantatie te voorkomen. De afgelopen jaren is veel
onderzoek gedaan naar machineperfusie van donorlevers, in een poging om de
overleving na DCD-levertransplantatie te vergroten. Enerzijds wordt koude
(hypotherme, 10-12 graden Celsius) machineperfusie gebruikt om de energieniveaus
van de lever weer te verhogen voorafgaand aan transplantatie, waardoor ischemie-
reperfusieschadeverminderdkanworden.Anderzijdsbiedtwarme(normotherme,37
gradenCelsius)perfusiedemogelijkheidomdelever-engalwegfunctievoorafgaandaan
transplantatietechecken.
Ditproefschrift focustopde transplantatievansuboptimale levers;vooralDCD levers.
Het eerste deel bevat met name observationele studies die gericht zijn op het
identificerenvandegrenzenvansuboptimalelevertransplantatie,enophetherkennen
van risicofactoren die deze grenzen bepalen. Deel twee bevat observationele,
preklinische en klinische studies met het gezamenlijke doel om veilig en succesvol
transplanterenvansuboptimaleleversmogelijktemaken.
Hierondervolgteensamenvattingvanheteerstedeelvanhetproefschrift.
Hoofdstuk1dientalsalgemeneinleidingenbeschrijftderationalevoorendeopzetvan
ditproefschrift.
Hoofdstuk 2 bevat een review van de literatuur over galwegcomplicaties na
transplantatie. Het ontstaan van galwegcomplicaties wordt besproken evenals
verschillende risicofactoren hiervoor. Gallekkage en galwegstricturen zijn de meest
voorkomende galwegcomplicaties. Van de galwegcomplicaties zijn met name de niet-
anastomotische stricturen (NAS) van de intrahepatische galweg het meest
problematisch.PatiëntendieeenDCD-lever,split-lever,of levende-donor-leverkrijgen,
hebben een verhoogd risico op galwegcomplicaties. Een groot deel van het risico op
galwegcomplicatieswordt bepaald door ischemie-reperfusie schade,maar ook andere
mechanismen spelen hier een rol, zoals bijvoorbeeld immuun-gemedieerde schade,
galzout-toxiciteitenonvoldoenderegeneratievanhetepitheel.
In hoofdstuk 3 worden de resultaten van een nationale retrospectieve studie
beschreven naar de associatie tussen donor-hepatectomietijd en het ontwikkelen van
galwegschade tijdens DCD levertransplantatie. Donor-hepatectomietijd werd
gedefinieerdalsdeperiodetussendestartvanhetkoudeflushenvandedonor,tothet
verwijderenvanhetorgaanuitdebuikholte.Deinvloedvandonor-hepatectomietijdop
galwegschadewerdbestudeerdineenchronologischevolgorde.Allereerstwerdgezien
bijgalwegbioptengenomenvóórmachineperfusiedatdehoeveelheidschadebeïnvloed
werd door de donor-hepatectomietijd. Ten tweede werd tijdens normotherme
machineperfusiegeziendatleversdieeenlangehepatectomietijdhaddengehad,galvan
minder goede kwaliteit produceerden. Vervolgens is met behulp van een nationale
retrospectieve studie aangetoond dat donor-hepatectomietijd een risicofactor is voor
het ontstaan van galwegcomplicaties. Concluderend: donor-hepatectomietijd moet zo
kortmogelijkgehoudenwordenomhetrisicoopgalwegcomplicatiesteverkleinen.
Hoofdstuk4bevateenstudienaardeassociatietussendesamenstellingvanhetbloed
vandeDCD-donorenhetontstaanvangalwegschadevanhetdonororgaan.Wevormden
dehypothesedathethematocrietendehoeveelhedenwittebloedcellenenbloedplaatjes
vandedonorhetrisicoopNASkunnenbeïnvloeden.Deredenvoordezehypothesewas
dathethematocrietdeviscositeitbepaalt,bloedplaatjesendotheelactivatieveroorzaken
bijhypoxie,enleukocytenvasodilatatiebeïnvloeden,enaldezefactorenkunnenleiden
tot eenminder succesvol flushen van het donororgaan. Allereerstwerd gezien in een
histologischeanalysevan40galwegbioptenvanhumanedonorleversdatbloedplaatjes
en leukocyten de ernst van galwegschade beïnvloeden voorafgaand aan
machineperfusie (OddsRatio2.553, 95%CI1.082-6.021, p=0.029 enOddsRatio0.734
95%CI 0.581-0.927, p=0.009, respectievelijk). Vervolgens, tijdens normotherme
machineperfusie, werd deze associatie wederom geobserveerd. In een landelijke
retrospectieve database studie werd aansluitend gezien dat donor hematocriet en
bloedplaatjeshetrisicoopNASbeïnvloeden.Debloedsamenstellingvandedonor lijkt,
concluderend, sterk geassocieerd met het ontstaan van galwegschade tijdens DCD-
levertransplantatie.
Inhoofdstuk 5 worden de resultaten beschreven van een studie die als doel had te
onderzoeken of DCD-levers veilig gebruikt kunnen worden in patiënten die een
retransplantatie van de lever moeten ondergaan. Tot nu toe worden voor
retransplantatiesindeWestersewereldvrijwelaltijdDBD-leversgebruikt.Inderecente
jaren zijn door de Nederlandse centra af en toe DCD-retransplantaties uitgevoerd. In
deze observationale studie hebben we de uitkomsten na DCD-retransplantatie
vergeleken met de uitkomsten van een gematched cohort DBD-retransplantaties. De
uitkomsten na DCD-retransplantatie waren vergelijkbaar met het cohort van DBD-
retransplantaties. De resultaten van deze studie suggereren dat DCD-levers niet
standaard afgewezen worden voor patiënten in relatief goede conditie die een
retransplantatiemoetenondergaan.
Inhettweededeelvanhetproefschriftzijnhoofdstukkentevindendieeropgerichtzijn
degrenzenvantransplantatievansuboptimaledonorleversteverleggen.
Inhoofdstuk6wordteenhistologischeanalysebeschrevenvandegalwegbioptenvan
10 DCD-levers die koude machineperfusie (DHOPE) ondergingen alvorens
transplantatie in het UMCG. De ontwikkeling van galwegschade van deze gepompte
levers werd vergeleken met de schade bij 20 controlegroep DCD-levers. Bij baseline
hadden beide groepen evenveel galwegschade. Na transplantatie bleken de levers die
DHOPE hadden ondergaan minder galwegschade te hebben ten opzichte van de
controlegroeplevers. Bijdecontrolegroepleverswerdeenverergeringvandeschade
gezien na reperfusie. Deze verergering van schade was afwezig bij de DHOPE levers.
Conclusie:DHOPEvermindertreperfusieschadevandegalwegen.
Hoofdstuk 7 bevat de resultaten van een preklinische studie naar het verlengen van
DHOPE om donorlevers langer te kunnen bewaren. We hebben de leverfunctie
onderzochtna2,6 en24uurDHOPEbij zowel varkens- alshumane leversdoordeze
met autoloog bloed te reperfunderen. Opvallend genoeg bleek er geen verschil in
leverfunctiewaarneembaar.Allegeanalyseerdemarkersvanendotheelschadelietenook
geenonderscheidzientussendegroepen.Tweehumaneleverswerden20uurgepompt
metbehulpvanDHOPE,voorafgaandaanopwarmenenreperfusie.Dezeleversvoldeden
vervolgens aandeklinischenormthermemachineperfusie criteria voor transplantatie.
Of>12uurDHOPEindepraktijkevenveiligblijktals2uurDHOPE,zalmoetblijkenuit
eenprospectieveklinischestudie.
In hoofdstuk 8 hebben we de resultaten van een prospectief klinisch onderzoek
beschreven,deDHOPE-COR-NMPtrial.Indezestudiewerdenallenationaalafgekeurde
donorleversaangebodenvoorinclusie.IndepraktijkbetroffenditmetnameDCDlevers
vandonoren>60jaaroud,en/ofzeersteatotischelevers.Donorleversondergingeneerst
eenuurDHOPE,omdemitochondriaterevitaliserenendeischemie-reperfusieschade
teverminderen.Vervolgenswerderopgewarmdnaar37gradenCelsius(normotherme
machineperfusie[NMP]).Binnen2.5uurvanNMPmoestdedonorleveraandevolgende
criteria voldoen om getransplanteerd te worden: perfusaat lactaat <1.8mmol/L, pH
7.35-7.45,galproductie>10mLengalpH>7.45.Binnendestudieperiodeondergingen
zestien levers DHOPE-COR-NMP. Alle afgekeurde levers lieten een adequate
parenchymfunctiezien.Echter,elfvandezestienlevershaddenookeengalpH>7.45en
wordendustransplantabelgeacht.MethetDHOPE-COR-NMPprotocolwerd69%vande
levers die afgekeurd waren tóch getransplanteerd, met een 100%
transplantaatoverlevingna1jaar.Ditleiddetoteen>20%toenamevanhetaantalpost-
mortalelevertransplantatiesinhetUMCG.
Hoofdstuk 9 bevat een techniek die is ontwikkeld naar aanleiding van een recente
nieuwetransplantatiemethodeuitGuangzhou,China.InhetFirstAffiliatedHospitalvan
Sun Yat-sen University zijn ze erin geslaagd om als eerste ter wereld ischemie-vrije
orgaantransplantatieuittevoeren.Bijdezetechniekwerdeenkleininterpositievatend-
to-sideopdevenaportaegeanastomoseerd,waardoorcannulatieencontinueperfusie
tijdens uitname, preservatie en implantatie mogelijk was. In Groningen ontstond het
ideeom,inplaatsvanhetinterpositievatopdevenaportae,devenaumbilicalisvande
donorleverhiervoor tegebruiken.Dezebleekeenvoudig teopenenen tedilateren, en
machineperfusiedoordevenaumbilicalisbleekvervolgensnietinferieuraanreguliere
perfusie via de vena portae hoofdstam. Tevens wordt in dit hoofdstuk een nieuwe
techniekvoor‘splittenaandepomp’beschreven,metbehulpvanmachineperfusieviade
venaumbilicalis.
CONCLUSIE:
Destudiesdieinditproefschriftwordenbeschrevenhebbenhetdoelomtransplantatie
van suboptimale, hoog-risico donorlevers op veilige wijze mogelijk te maken. Helaas
wordt inNederlandnogsteeds tegende30%vanbeschikbaredonorleversafgewezen
voor transplantatie. Zo lang als ernog veel patiëntenoverlijdenopdewachtlijst voor
een donororgaan, zouden transplantatieprofessionals nieuwe technieken moeten
onderzoeken om deze afgewezen donorlevers toch te kunnen transplanteren. Zoals
recent beschreven in een editorial in de New England Journal of Medicine, “het
vermijdenvan risico’sheeft geleid tot eenverschuivingvanonderzoeksportfolio’svan
veel transplantatiecentra: ver weg van pionierswerk en juist in de richting van
leefstijlgeneeskundeenlangetermijnobservationelestudies”.Destudiewaaringetracht
is afgekeurde donorlevers toch te transplanteren met behulp van machine perfusie
(hoofdstuk8)toontaandateengezamenlijkerisicodatwordtgenomendoorpatiënten
artsleidttoteengrotestapvoorwaartsinhetminimaliserenvanwachtlijststerfte.Veel
toekomstige studies zijn nodig om wachtlijststerfte te verbannen uit
orgaantransplantatie en om de uitkomsten na transplantatie te verbeteren. Om dit te
bereiken, zullen artsen risico’s niet moeten vermijden, maar het dappere pad naar
medischeinnovatiesamenmetdepatiëntbetreden.
• deJongIEM,vanLeeuwenOB,LismanT,GouwASH,PorteRJ.Repopulatingthe
biliarytreefromtheperibiliaryglands.BiochimBiophysActaMolBasisDis.2018
Apr;1864:1524-1531.
• vanRijnR,vanLeeuwenOB,MattonAPM,BurlageLCWiersema-BuistJ,vanden
HeuvelMetal.Hypothermicoxygenatedmachineperfusionreducesbileduct
reperfusioninjuryaftertransplantationofdonationaftercirculatorydeathlivers.
LiverTranspl.2018May;24(5):655-664.
• vanLeeuwenOB,UbbinkR,deMeijerVE,PorteRJ.TheFirstCaseofIschemia-
freeOrganTransplantationinHumans:aProofofConcept.AmJTransplant.2018
Aug;18(8):2091.
• van Leeuwen OB, de Meijer VE, Porte RJ. Viability criteria for functional
assessment of donor livers during normothermic machine perfusion. Liver
Transpl.2018Oct;24(10):1333-1335.
• deVriesY,vanLeeuwenOB,MattonAPM,FujiyoshiM,deMeijerVE,PorteRJ.Ex
situnormothermicmachineperfusionofdonorliversusingahemoglobinbased
oxygen carrier: a viable alternative to red blood cells. Transpl Int. 2018
Nov;31(11):1281-1282.
• deVriesY,MattonAPM,NijstenMWN,WernerMJM,vandenBergAP, deBoer
MT,Buis CI, FujiyoshiM, deKleineRHJ,vanLeeuwenOB, et al. Pretransplant
Sequential Hypo- and Normothermic Machine Perfusion of Suboptimal Livers
Donated after Circulatory Death Using a Hemoglobin-based Oxygen Carrier
PerfusionSolution.AmJTransplant.2019Apr;19(4):1202-1211.
• deVriesY,BerendsenTA,FujiyoshiM,vandenBergAP,BlokzijlH,deBoerMT,
van der Heide F, de Kleine RHJ,van LeeuwenOB,Matton APM,WernerMJM,
LismanT,deMeijerVE,PorteRJ.Transplantationofhigh-riskdonorliversafter
resuscitationandviabilityassessmentusingacombinedprotocolofoxygenated
hypothermic, rewarming and normothermicmachine perfusion: study protocol
foraprospective,single-armstudy(DHOPE-COR-NMPtrial).BMJOpen.2019Aug
15;9(8):e028596.
• WernerMJM,vanLeeuwenOB,de Jong IEM,BodewesFAJA,FujiyoshiM,etal.
First report of successful transplantation of a pediatric donor liver graft after
hypothermicmachineperfusion.PediatrTransplant.2019May;23(3):e13362.
• van Leeuwen OB, FujiyoshiM, Ubbink R,WernerMJM, Brüggenwirth IMA, de
Meijer VE, Porte RJ. Ex situ machine perfusion of human donor livers via the
surgically reopened umbilical vein: a proof of concept. Transplantation. 2019
Oct;103(10):2130-2135.
• vanLeeuwenOB,deVriesY,FujiyoshiM,NijstenMWN,UbbinkR,PelgrimGJ,et
al. Transplantation of high-risk donor livers after ex situ resuscitation and
assessment using combined hypo- and normothermic machine perfusion: a
prospectiveclinicaltrial.AnnSurg.2019Nov;270(5):906-914.
• HeX,ChenG,ZhuZ,ZhangZ,YuanX,HanM,ZhaoQ,ZhengY,TangY,HuangS,
WangL,vanLeeuwenOB,WangX,ChenC,MoL,JiaoX,LiX,WangC,HuangJ,
CuiJ,GuoZ.TheFirstCaseofIschemia-FreeKidneyTransplantationinHumans.
FrontMed(Lausanne).2019Dec11;6:276.
• van LeeuwenOB, de Jong IEM, Porte RJ. Biliary Complications following liver
transplantation. In:ClavienPA,Trotter JF, editors.Medical andSurgicalCareof
LiverTransplantationPatients.Wiley-Blackwell;2020
• vanLeeuwenOB,vanReevenM,vanderHelmD,IJzermansJNM,deMeijerVE,
vandenBergAP,DarwishMuradS,vanHoekB,AlwaynIPJ,PorteRJ,PolakWG.
Donor hepatectomy time influences ischemia-reperfusion injury of the biliary
tree indonation after circulatorydeath liver transplantation. Surgery. 2020 (in
press).
• vanReevenM,vanLeeuwenOB,DarwishMuradS,vandenBergAP,vanHoekB,
Alwayn IPJ, Polak WG, Porte RJ. Selected livers of donation after circulatory
deathcanbesafelyusedforretransplantation.TransplInt.2020(inpress).
• Brüggenwirth IMA, van Leeuwen OB, de Vries Y, Bodewes SB, Adelmeijer J,
Wiersema-Buist J, Lisman T, Martins PN, de Meijer VE, Porte RJ. Extended
hypothermic oxygenated machine perfusion enables ex situ preservation of
porcineliversforupto24hours.JHepRep.2020(inpress).
• vanReevenM,GilboN,MonbaliuD,vanLeeuwenOB,PorteRJ,YsebaertD,van
Hoek B, Alwayn IPJ,MeurisseN, Detry O, Coubeau L, Cicarelli O, Berrevoets F,
RogiersX,IJzermansJNM,PolakWG.Liversdonatedaftereuthanasia:ajustifiable
optiontoexpandthedonorpool.Submittedforpublication.
• vanLeeuwenOB,vanReevenM,vanderHelmH,IjzermansJNM,AlwaynIPJ,van
HoekB,PolakWG,LismanT,deMeijerVE,PorteRJ.Donorbloodcompositionisa
risk factor for biliary injury during donation after circulatory death liver
transplantation.Submittedforpublication.
• deVriesY,BrüggenwirthIMA,vonMeijenfeldtFA,vanLeeuwenOB,BurlageLC,
de Jong IEM, Gouw ASH, Lisman T, Porte RJ. Dual versus single oxygenated
hypothermic machine perfusion of porcine donation after circulatory death
livers: impact on hepatobiliary and endothelial cell injury. Submitted for
publication.
Toen ik in 2014 het geluk had in het studenten leverteam te worden aangenomen,
merkte ik meteen hoe warm en stimulerend het onderzoeksklimaat binnen de
onderzoeksgroeprondomdeleverperfusiewas.Teamworkheeftaltijdvooropgestaan;
gezamenlijkwerdenprojectenvlotenmeestalsuccesvol toteeneindegebracht.Het is
een groot voorrecht om de afgelopen jaren in deze omgeving te hebben mogen
functioneren waarin ik veel heb kunnen opsteken van de chirurgen, hepatologen en
bovenaldeanderepromovendi.Ditproefschriftvoeltvoormijnietalsheteindevaneen
tijdperk,maaralseeneerstetraptrede.
Professordr.R.J.Porte,besteRobert,watbenikontzettenddankbaarvoorallekansen
envrijheiddiejemijdeafgelopenjarengebodenhebt.Ikhebheelveelrespectvoorhoe
je dag in dag uit het hoogst haalbare nastreeft en nooit akkoord zal gaan met een
binnenbocht.Indecommunicatiezijnweallebeigraag‘kortenbondig’.Jeafsprakenmet
anderepromovendi liepenvaakuit,maar ik stondmeestalbinnendehelft vande tijd
weerbuiten.HoopmaardathiergeldtzoalsMilanKunderaooit treffendschreef:“You
can't measure the mutual affection of two human beings by the number of words they
exchange”…Wehebbenveelmeegemaaktafgelopenjaren:vanmoedelozemomentenbij
afgekeurde levers na urenlange NMP’s tot het aanschouwen van ischemie-vrije
levertransplantatie inGuangzhou.Er zijnnogveel ideeënoveren ikhoopdat ik jede
komendejarenkanblijvenbijstaanbijdeuitvoeringvanhiervan.Ikhadmegeenbetere
promotorkunnenwensen.
Professordr.T.Lisman,Ton,ondanksdatiknaarjouwwetenschappelijkemaatstaven
hoogstwaarschijnlijknietdeidealepromovenduswas,hebjemijmetveelenthousiasme
gesteund. Je bent een kundig voorbeeld van denken in oplossingen in plaats van
problemen. Je scherpe analyses hebben mij regelmatig uit de klinische/praktische
tunnelvisie gehaald. Ik hoop dat we gezamenlijk de komende jaren het project met
bloedsamenstelling/stolling/endotheelactivatie en de linkmet NAS verder uit kunnen
werken.Dankvoorjesupport!
Dr.V.E.deMeijer,Vincent,watbenikonderdeindrukvanwatjeindeafgelopenjaren
in het UMCG al bereikt hebt met je enorme ambitie! Met inmiddels je geaccepteerde
Veni-aanvraagopzakweetikzekerdatjeheelveelzalbereikenkomendejaren.Ikvond
hetergfijndatwevanuitonzewerkplekkenelkaarkondenzienendatikdaardoorveel
bijjelangskonhoppenvooroverleg.Dathielddesnelheidinonzeprojectenhoog.Los
vanjewetenschappelijkeexpertisebenikeveneensdankbaarvoorhetfeitdatikmetjou
enRobert tweehele goede chirurgen als promotores heb gehad.Hierdoor heb ik niet
alleen opwetenschappelijk gebied,maar ook op klinisch vlak ontzettend veel kunnen
leren.
Beoordelingscommissie: Prof. H.G.D. Leuvenink, prof. D. Monbaliu, prof. J.K.G.
Wietasch, heel veel dank voor jullie interesse in het proefschrift en de inhoudelijke
feedback.
OLT1&OLT2’s:prof.dr.RobertPorte,dr.MariekedeBoer,drs.RubendeKleine,
dr.CarlijnBuis,dr.VincentdeMeijer,prof.dr.JoostKlaase,dr.MaartenNijkamp,
dr.FrederikHoogwater,ikbenontzettenddankbaardatjulliemijals18/19/20-jarige
leverstudentbijheelveelOLT’senelectieveHPB-operatieshebben latenassisterenen
meekijken.Datheeftbijmijvooreenhoopmotivatiegezorgdvoorditpromotietrajecten
hetheefthetmijduidelijkgemaaktwaar inhet ziekenhuismijnpassie ligt.Bovenal is
door jullie ondersteuning de machineperfusie in de afgelopen jaren volledig
geïntegreerdinhetUMCG!
Dr.M.Fujiyoshi,dearMasato, Iamthankful for thegreatyearswehad inGroningen.
Youwere always first to discuss ideas on transplantation andmachine perfusion and
youalwaysprovidedmewithsupportonmyprojects.WespentalotoftimeintheOPR
(and Burgerking) together and without your everlasting help the machine perfusion
researchintheUMCGwouldhavedevelopedmuchslower.Ihopetobeabletocometo
Japanagaininthecomingyears!
Kantoorgenoten: drs. M. Meerdink, drs. C.R. Hoepel, drs. S.J.S Ruiter, drs. A.N.
Tournicourt,BesteMark,Carlos,SimeonenAn,ikbenjulliedankbaardatjulliemijals
‘benjamin’ op de kamer accepteerden. Het heeft voor mij continu als motivatie
gefungeerdomjullieklinischeverhalentehoren.Ikhoopdatiklaternogeenkeeronder
julliebegeleidingmagwerkenindekliniek!
Chirurgisch Onderzoeks Laboratorium: Jacco Zwaagstra, Petra Ottens, Jelle
Adelmeijer, Janneke Wiersema-Buist. Ik weet niet hoe vaak ik Jacco heb horen
benadrukken: “Otto, diewerkt hier eigenlijk nooit”, Desondanks liggen van een groot
deel van mijn projecten de wortels in het COL. Ik ben jullie dankbaar voor de
behulpzaamheid en prettige werksfeer die ik altijd heb ervaren. Susanne Veldhuis,
Suus,heelveeldankvoorjehulpbijhetvarkensexperimentmetFienenmij.Wewaren
metname inhetbeginergonbeholpenennietaltijdevenwetenschappelijk,maarmet
jouwhulphebbenweereenvolwassenexperimentvankunnenmaken!
Kroon Vlees Groningen: Gert, Jan, Luitzen, en de vele anderen die ervoor gezorgd
hebbendatwe inmiddelsalredelijkwat jarensuccesvolvarkensexperimentenkunnen
uitvoeren:heelveeldankvoorjulliehulpengastvrijheid!
Drs.M.vanReeven,besteMarjolein,watwehebbentocheenprettigesamenwerking
gehad ondanks de obstakels die we zijn tegengekomen. Het meest voorkomende
probleemkwamechtervanmijnkant:dehumane-envarkensperfusiesdieweer inde
weglagen.Ikbenjedankbaarvoorjegeduldéndrivewaarmeejeonzeprojectentoteen
goedeindehebtwetentebrengen.Tevensveeldankaandr.W.G.Polak,prof.dr.J.N.M.
IJzermans,prof.dr.I.P.J.Alwayn,prof.dr.B.vanHoekendr.D.vanderHelmvoor
demooienationalesamenwerking!
(Oud) transplantatiecoordinatoren UMCG, beste TC’ers, heel veel dank voor jullie
hulpmethetidentificerenvanpotentiëledonorenvoorNMP!Dehoogtepuntenvanonze
samenwerking vonden echter plaats in de late uurtjes: in de Poelestraat of op de
congressen!
OrganAssist;WilfreddenHartog,ArjanvanderPlaats,TonMulderij,veeldankvoor
jullie support en het toestaan van onze varkensexperimenten waarmee we voor een
hoop gedoe hebben gezorgd aan de Bornholmstraat.. Ik kijk terug op een prettige
samenwerking.EmmaOffringa,Mark Slotemaker, Ernst Buiter, Martin Kuizenga:
jullie waren simpelweg geweldig!! De congressen werden met jullie altijd een groot
feest,maarookdevarkensexperimenten.Erwasaltijdeengoedesfeerenwaarweook
waren,julliegavenaltijdeengevoelvan‘thuiskomen’.
Studenten van leverteam, waaronder Silke Bodewes, dank voor jullie inzet bij het
organiserenenuitvoerenvansample-afnamesenhetverwerkenrondomde(perfusie)
levertransplantaties.
Orgaanperfusionisten, drs. Rinse Ubbink, dr. Gert Jan Pelgrim, drs. Maureen
Werner, en nu sinds kort ookdrs.MartijnHaring, Veerle Lantinga en Leonie van
Leeuwen;watbeniktrotsopderesultatendiewedeafgelopenjarenbehaaldhebben!
Het heeft de nodige flexibiliteit gekost, maar jarenlang stondenwe klaar voor iedere
perfusie.Dankvoorjullieteamworkenenthousiasme!
Leveronderzoekers:dr.AlixMatton,dr.LauraBurlage,drs.YvonnedeVries,drs.
ShaniceKarangwa,IrisdeJong,ikrealiseermewateenontzettendeluxehetisomhet
goed te kunnenvindenmet je collega’s.Alle perfusies,maarmetnamede congressen
(van Bootcongressen tot Oslo/Seattle/Toronto) werden geweldige ervaringen door
jullie!
Dr.R.vanRijn,Rianne,als18/19-jarigejongenwerdikdoorRobertaanjegekoppeld
enmocht ik jewatgaanhelpenmet jeonderzoeken.Heb(totopdedagvanvandaag)
ontzettend genoten van je indrukwekkende puurheid. Ik ben dankbaar voor je
vertrouwenendekansendiejemehebtgebodenenikgaervanuitdatikindetoekomst
nogveelvanjegaleren.
FienvonMeijenfeldt,Fien,wathebbenweeenmooivarkensexperimentneergezetmet
de retrograde flush en DNAse therapie. Lange dagen, maar altijd met goede sfeer
ondanksdesoms licht tragischeresultaten!Bedanktvoorde fijnesamenwerkingen je
verfrissendeblikopzakendievoormijvoorheenkraakhelderleken.
Drs. M.J.M. Werner, Maureen, mede onderzoeker en orgaanperfusionist, wat ben ik
onderdeindrukgeweestvanjenietaflatendeopgewektheid.Zaljecontinuesupportop
m’npersoonlijkedieptepuntopdezeiknatteHighway5vanVancouvernaarSeattleook
nooit vergeten, nog steeds dankbaar voor... De vele nachten diewe gezamenlijk in de
OPRhebbendoorgebrachtwerdendoorjoueengrootfeest!Ondanksdatwesomsmet
een lege energietank tóch weer aan een NMP moesten beginnen, sleepte je ons er
allemaal doorheen met je optimisme! Denk dat ook menig donorlever door jouw
aanstekelijkeenthousiasmetochnétaandeviabilitycriteriagingvoldoen…
IsabelBrüggenwirth,Isabel,wathebbenweveelmeegemaaktdeafgelopenjaren.Van
eindeloos veel hardlopen, inclusief marathon, tot ontzettend veel humane- en
varkensperfusies. Denk nog steeds dat we het leverperfusierecord in handen hebben
metdecombinatie‘verlengdeDHOPEvarkensexperiment+succesvollehumaneDHOPE-
COR-NMPprocedure’,waarinwevandinsdag05:00 totwoensdag18:00non-stop (37
uur) stonden tevlammen. Jebentaltijdm’neersteaanspreekpuntgeweestbijnieuwe
(en regelmatig slechte) ideeën en hersenspinsels en ik hoop dat dat nog lang zomag
blijven!
Willem Wierbos, Willem, waar menig vriendschap zou lijden onder de vele
leverperfusiesvandeafgelopen jaren,hebbenwijdaarnooit lastvangehad.Dankbaar
voor je support en trots op je ontwikkeling als zanger/acteur/poëet naast je
geneeskundestudie.Vereerddatjem’nparanimfwiltzijn!
Dr.R.B.vanLeeuwen,drs.M.A.vanLeeuwen-Buinink,mr.dr.B.J.vanLeeuwenen
drs.C.A.T.vanLeeuwen;Roeland,Marie-Anne,BarendenClaar,hetheeftdeafgelopen
jarenheelwatgekost,maarwatwashethetwaard!Hebvanjongsafaangoedvanjullie
allenkunnenafkijkenhoeveelwerkerverzetmoetwordenomietstebereikenenben
dankbaarvoordevoorbeeldfunctiesdie jullievoormijgeblekenzijn.Debezoekenaan
Apeldoornwarennietaltijdevenlangdurigdeafgelopenjarendoordefrequentelevers,
maaromBarendsingezettetraditievoorttezettenwas iksteedsopreisenaltijdthuis.
Claar;ikbentrotsopjerolalsparanimf,enbinnenkortstaanwebij jouwverdediging;
ikkijkernaaruit.Heeldankbaarvoorjulliesupport!
Curriculumvitae
OttovanLeeuwenwasbornon15thNovember1995inApeldoorn,theNetherlands.He
receivedhis secondaryeducationat the ‘GymnasiumApeldoorn’ inApeldoorn.Forhis
final research project at secondary school, Otto spent one month studying surgical
woundcare inMwananyamalaHospital,DarEsSalaam,Tanzania.Aftergraduation,he
movedtoTampa,USA.AttheUniversityofTampa,hemajoredineconomics.However,
mostofhisclassesfocussedonliteratureandacademicwriting.AfteroneyearinTampa,
he was admitted to study Medicine at the University of Groningen. During the three
years of his bachelor’s programme, Otto worked in the student liver transplantation
teamand thePrometheusnierteamat theUniversityMedical CenterGroningen.From
thefirstyearofhisbachelor’sprogramme,Ottoenjoyedworkingforprof.dr.R.J.Porte
attheDepartmentofSurgeryandstartedassistingwithresearchprojects.Hewrotehis
bachelor thesis “Increasing thequalityof suboptimaldonor livers for transplantation:a
bridgebetweenclinicandresearch”andmasterthesis“Riskfactorsassociatedwithbiliary
complications and early graft loss following donation after circulatory death liver
transplantation”underthesupervisionofprof.dr.R.J.Portebeforeapplying foraMD-
PhDposition.HewasacceptedintotheMD-PhDtrajectoryinJune2018.FromMarchto
April2018,OttoworkedinGuangzhou,China,topractisehumanandporcineischemia-
free liver transplantation. Otto is currently finishing his Master’s degree inMedicine,
hopingtopursuehisdreamofbecominga(transplant)surgeon.















































































































































































































































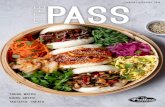









![Akademika64[03].pmd - akademika64[01]](https://static.fdokumen.com/doc/165x107/6318ef2077252cbc1a0e76df/akademika6403pmd-akademika6401.jpg)







