Phillips 1990 Exchange transfusion as an adjunct to the treatment of severe
Transcript of Phillips 1990 Exchange transfusion as an adjunct to the treatment of severe
Exchange Transfusion as an Adjunct to the Treatment of Severe Falciparum Malaria: CaseReport and ReviewAuthor(s): Peter Phillips, Stephen Nantel and W. Barrett BennySource: Reviews of Infectious Diseases, Vol. 12, No. 6 (Nov. - Dec., 1990), pp. 1100-1108Published by: Oxford University PressStable URL: http://www.jstor.org/stable/4455710 .
Accessed: 13/02/2014 15:38
Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at .http://www.jstor.org/page/info/about/policies/terms.jsp
.JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range ofcontent in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new formsof scholarship. For more information about JSTOR, please contact [email protected].
.
Oxford University Press is collaborating with JSTOR to digitize, preserve and extend access to Reviews ofInfectious Diseases.
http://www.jstor.org
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
REVIEWS OF INFECTIOUS DISEASES * VOL. 12, NUMBER 6 * NOVEMBER-DECEMBER 1990 X) 1990 by The University of Chicago. All rights reserved. 0162-0886/90/1206-0011$02.00
Exchange Transfusion as an Adjunct to the Treatment of Severe Falciparum Malaria: Case Report and Review
Peter Phillips, Stephen Nantel, and W. Barrett Benny From the Divisions of Infectious Diseases and Hematology, Vancouver General Hospital; and the University of
British Columbia, Vancouver, Canada
Malaria associated with complications or a fatal outcome is almost always caused by Plas- modiumfalciparum. The mortality due to this disease parallels the degree of parasitemia. Successful use of exchange blood transfusion as a therapeutic adjunct for this infection was first reported in 1974, although the efficacy of this procedure has not been estab- lished by randomized, controlled trials. The rationale for this form of therapy is based on: (1) rapid reduction in the parasite load by direct removal; (2) decreased risk of severe intravascular hemolysis and its consequences (disseminated intravascular coagulation and renal dysfunction); (3) improved rheology with transfused blood and reduced microcir- culatory sludging; and (4) improved oxygen-carrying capacity with transfused erythro- cytes. We describe a case of severe falciparum malaria and review the literature describing the use of exchange transfusion for treatment of this infection.
A marked increase in the incidence of malaria caused by Plasmodium fakciparum has been observed in re- cent years [1, 2]. Delays in diagnosis and in institution of appropriate chemotherapy are common features of complicated or fatal cases and are particularly likely to result in severe parasitemia in the nonim- mune host [3]. Chances of survival may be reduced if therapy is delayed by 12 hours [4].
The complications of infection due to P falcipa- rum may include cerebral malaria renal failure or respiratory insufflciency due to adult respiratory dis- tress syndrome or pulmonary edema; hematologic complications, such as severe intravascular hemoly- sis, blackwater fever, and disseminated intravascular coagulation (DIC) with profound thrombocytopenia; hepatic dysfunction; and hypoglycemia [5]. The mor- tality is directly proportional to the degree of para- sitemia [6] and to the development of complications. Mortality rates for high-grade parasitemia (parasit- ized red cells, 10Oo%-40O7o), cerebral malaria, and blackwater fever have been reported to be as high as 4007o [4], 33% [7], and 207o-300/o [8], respectively. It appears that prompt reduction in the level of parasitemia is essential to improve survival.
Received for publication 11 November 1989 and in revised form 1 March 1990.
The authors thank Dr. Jerry Vortel and Dr. Martin Olivier for assistance in translation of foreign language publications.
Please address requests for reprints to Dr. P. Phillips, Division of Infectious Diseases, St. Paul's Hospital, 1081 Burrard Street, Vancouver, British Columbia V6Z 1Y6, Canada.
Significant mortality occurs with marked parasite- mia (>5 %) despite appropriate parenteral antimalar- ial chemotherapy and general supportive care [9]. Several reports over the past 16 years [10-30] and a recent study by Miller et al. [31] based on a series of 11 patients have described the use of exchange transfusion as adjunctive therapy for this illness. Ten additional cases were briefly described in letters [32, 33]. A precipitous fall in the level of parasitemia as- sociated with marked clinical improvement was ob- served during the procedure in a number of cases [11, 13-15, 19, 23, 27, 29]. We describe a case and review the role of exchange blood transfusion in the management of malaria due to 1 falciparum.
Case Report
A previously healthy 24-year-old man was admitted to the hospital with a 1-week history of chills, spik- ing fevers, malaise, fatigue, headache, and nausea. He had recently completed a 3-week trip to Ghana, West Africa, (10 days before admission) and returned to Vancouver after a 1-week stay in Britain. He had taken 500 mg of prophylactic chloroquine (300 mg base) weekly up to the time of his admission. One day prior to admission his family doctor diagnosed malaria and prescribed quinine sulfate (600 mg po three times a day) and tetracycline (250 mg po four times a day). The quinine sulfate was not available from the pharmacy until the following day.
On admission the patient appeared ill. His tem- perature was 40?C, heart rate was 110/min, and su-
1100
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
Exchange ransfusion in Falciparum Malaria 1101
pine systolic blood pressure was 85 mm Hg. The jugular venous pulsations were not visible, and the spleen tip was palpable. He was alert and oriented, and there were no neurologic findings. The re- mainder of the physical examination was normal.
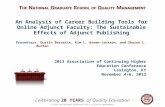
The thin blood smear for malaria showed that 25% (direct count) of the erythrocytes were parasit- ized with ring-form trophozoites of P falciparum (figure 1). He was anemic (hemoglobin level, 99 g/L) and thrombocytopenic (platelet count, 20 x 109/L) and showed evidence in laboratory studies of DIC (prothrombin time, 16.7 seconds; control, <13.5 sec- onds; partial thromboplastin time, 62.9 seconds; con- trol, <35 seconds; fibrinogen, 1.12 g/L; normal, 1.25-4.0 g/L; and fibrin degradation products, 16,000 Lg/L; normal, 0-200 gg/L). Renal abnormal- ities were noted by the levels of serum creatinine (143 gmol/L; normal, 60-110) and urea (14.0 gmol/L; normal, 1.8-8.2); and urinalysis revealed 3 + hemoglobinuria without microscopic hematuria. Other laboratory abnormalities included the follow- ing values: lactate dehydrogenase, 531 U/L (normal, 9-210), total bilirubin, 52 gmol/L (normal, 0-22), direct bilirubin, 7 jmol/L (normal, 0-5), and aspar- tate transaminase, 55 U/L (normal, 19-38). Blood gases drawn when the patient was breathing room air a few hours after admission showed the follow- ing values: pH, 7.41; Pco2, 30 mm Hg; P02, 61 mm Hg; HCO3, 18 mmol/L; and 02 saturation, 0.85. Shortly after admission his hemoglobin level de- creased to 66 g/L, presumably due to hemodilution following fluid replacement as well as ongoing hemolysis.
The first chest roentgenogram was obtained fol- lowing iv fluid replacement in the emergency depart- ment and showed evidence of interstitial changes consistent with the development of pulmonary edema. The patient was admitted to the intensive care unit and given a loading dose of quinidine, 15 mg (base)/kg iv over 4 hours followed by 7.5 mg (base)/kg iv over 4 hours three times daily. Transient hypotension (70 mm Hg systolic) occurred during administration of the loading dose of quinidine and resolved spontaneously. Serum levels of quinidine measured consecutively during iv therapy were 15, 15, 17, and 14 gtmol/L (therapeutic range, 7-15 gmol/L).
He also received therapy with tetracycline (250 mg po every 6 hours). One packed red blood cell (PRBC) exchange transfusion (10 units PRBC = 2,400 mL) was performed with the use of a cell separator
- WiIWW(
Figure 1. Peripheral blood smear before treatment, showing high-level parasitemia with ring forms of P fal- ciparum. The two dark-staining inclusions in the band form leukocyte represent malarial pigment that results from phagocytosis of parasites (Wright's stain; original magnification, x 2,000).
(COBE 2997, COBE Laboratories Inc., Lakewood, Colo.). Venous access was achieved via antecubital fossa veins with the use of standard 16-gauge aphe- resis needles. Acid citrate dextrose (ACD) solution was used as anticoagulant (total volume, 280 mL). Red blood cell (RBC) separation was performed at 1,500 rpm with RBC/plasma flow rates of 20/40 mL/min and a collection rate for RBCs of 20 mL/min. The total blood volume processed was 7,800 mL; the total volume removed was 2,880 mL; the volume replaced was 2,680 mL (10 units PRBC plus ACD solution). The total duration of the pro- cedure was 3 hours. Following exchange transfusion, the parasitemia was reduced to 3%o. Other treatment measures included platelet transfusion (six units) and supplemental oxygen.
This patient's clinical course was also complicated by self-limiting diarrhea and mild respiratory dis- tress. After 48 hours of iv quinidine, his chemother- apy was changed to oral quinine sulfate, 600 mg three times a day, and he completed a 10-day course of therapy. The fever and parasitemia completely resolved after 4 days of treatment. He made a full recovery and was discharged from the hospital 1 week after admission.
Literature Review
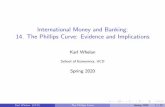
An outline of the reported cases of patients with fal- ciparum malaria who were treated with exchange transfusion is presented in table 1, excluding ten cases
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
Table 1. Falciparum malaria treated with exchange transfusion.
Parasitemia
Before After exchange exchange
Case no. trans- trans- [reference] fusion fusion Other treatment
year Age/sex (%) (%) Complications Drug therapy Exchange measures Outcome
I [10] 1974 23/m 43 0.01 CM,* DIC,t blackwater fever, Chloroquine iv, WB, two blood Steroid, heparin Survived
jaundice, hypotension, renal pyrimethamine- exchanges complications sulfadoxine im,
proguanil po
2 [111 1979 21/f 75 3 CM, DIC, jaundice, shock, renal Quinine iv, WB,i 8 L over 4 h Dialysis, steroids, calcium Survived
complications pyrimethamine- (consciousness
sulfadoxine po improved)
3 [12] 1979 21/f 55 1.7 CM, hypoxemia, renal complications Chloroquine iv, WB, 10 units Hemodialysis, steroids Survived
quinine iv
4 [13] 1979 36/m 20 1 CM, jaundice, hypoxemia, renal Quinine iv WB, 10 L over 6 h Dialysis, steroids Survived
complications (consciousness improved)
5 [14] 1982 65/f 5 <1 CM Quinine po, WB (cell separator), Steroids Survived
chloroquine po 5 L over 3 h (consciousness improved)
6 [15] 1983 48/m 72 0.7 CM, jaundice, renal complications Quinine po, WB, 10 L over 32 h Steroids Survived
chloroquine po, (consciousness
pyrimethamine- improved)
sulfadoxine po
7 [16] 1984 40/m 70 <1 ARDS,? blackwater fever, CM, Quinine po and iv, PRBCII (cell Platelets, cryoprecipitate, Survived
splenic necrosis, coagulopathy, chloroquine po separator), 2 L heparin, steroids
renal complications over 2 h x 3 in 21 h
8 [17] 1984 40/f NS# NS CM, DIC, jaundice, renal Chloroquine, po, Plasma exchange x 6 Hemodialysis, clotting Survived
complications pyrimethamine- factors sulfadoxine po, mefloquine po
9 [18] 1985 42/m NS NS Renal complications Chloroquine po, Plasma exchange x 2 Hemodialysis Survived
pyrimethamine- sulfadoxine po
10 [19] 1985 38/f 26 5 CM, renal complications Quinine iv, WB, 3.5 L over 2 h Platelets (6 units), fresh Survived
pyrimethamine- frozen plasma (2 units) (consciousness
sulfadoxine po improved)
11 [20] 1985 26/m 30 1 None Chloroquine po, PRBC, 10 units over ... Survived
quinine iv 21 h
12 [20] 1985 33/f 60 30 None Quinine iv, WB, 4 units over 8 h . . . Survived
pyrimethamine- sulfadoxine po
13 [20] 1985 52/m 33 8 DIC, jaundice, renal complications Chloroquine po and PRBC, 6 units over Fresh frozen plasma, 2 Survived
iv, quinine iv 4 h units, dialysis,
14 [21] 1986 36/m NS NS DIC, CM, renal complications Quinine iv, WB, 12 L . .. Survived
chloroquine po
(continued)
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
Table 1. (continued)
Parasitemia
Before After exchange exchange
Case no. trans- trans- [reference] fusion fusion Other treatment
year Age/sex (%) ) Complications Drug therapy Exchange measures Outcome
15 [22] 1986 58/f 16 0.3 CM, DIC, jaundice, hypoxemia, Chloroquine im, WB, 8 L Diuretic, hemofiltration Survived
renal complications quinine iv
16 [23] 1987 54/m 34 7 None Chloroquine po, WB, 5 L over 2 h . .. Survived mefloquine po
17 [25] 1987 25/m 24 4 DIC, hypoglycemia, hypotension, Mefloquine po WB, 6 L over 2 h Glucose iv Survived
renal complications (consciousness improved)
18 [23] 1987 19/m 27 9 CM, pneumonia, sepsis, pulmonary Mefloquine po WB, 6.2 L over 2 h Peritoneal dialysis, Survived
edema, renal complications mechanical ventilation
19 [23] 1987 59/m 30 11 CM, jaundice, pulmonary and renal Quinine po NA** Peritoneal dialysis, Survived
complications mechanical ventilation
20 [23] 1987 26/m 40 3 CM, jaundice, endocarditis Quinine po PRBC, 17 units (cell . . . Survived separator) (consciousness
improved)
21 [24] 1987 1/f 6.1 2 CM Quinidine civ,tt WB, 0.33 L over 2 h . . . Survived chloroquine po
22 [25] 1988 53/m 40 NS Jaundice, sepsis, respiratory and renal Quinidine civ NA Dialysis, mechanical Died
complications ventilation
23 [26] 1988 31/f 50 NS DIC, CM, jaundice, renal Chloroquine po, WB, 0.8 L/d Plasma exchange, 2 L over Survived
complications pyrimethamine- I h; dialysis, clotting sulfadoxine po, factors quinine iv, doxycycline iv, mefloquine po
24 [27] 1988 42/m 60 25 CM, jaundice, renal complications, Quinine civ, WB, 14 units, and Dialysis Survived
thrombocytopenia pyrimethamine- PRBC, 2 units (consciousness sulfadoxine po, over 10 h; plasma improved) mefloquine po, exchange 6. 1 L doxycycline po and 2 L
25 [28] 1989 33/m 1 NS Renal complications Quinine iv NA Dialysis Survived
26 [29] 1989 26/f 19 3 CM, jaundice, ARDS, pulmonary Quinine iv WB, 4 L over 3 h Mechanical ventilation Died
fibrosis (consciousness improved)
27 [31] 1989 34/m 43 NS CM, DIC, ARDS, renal complications Quinidine civ WB (cell separator), . . . Survived 8 L over 2 h
28 [31] 1989 1/f 6 NS None Quinidine civ WB, 0.33 L ... Survived
29 [31] 1989 73/m 54 NS CM, DIC, sepsis, pneumonia, Quinidine civ WB, 2 L ... Died
gangrenous leg, renal complications
30 [31] 1989 53/m 38 NS ARDS, DIC, sepsis, renal complications Quinidine civ WB, 5.5 L over 12 h ... Died
31 [31] 1989 65/m 30 NS CM, ARDS, sepsis, renal complications Quinidine civ WB, 4 L ... Died
32 [31] 1989 45/f 13 NS CM Quinidine civ WB, 5 L over 12 h . . . Survived
33 [31] 1989 2/f 28 NS Seizure Quinidine civ WB, 0.65 L ... Survived
34 [311 1989 28/m 22 NS CM Quinidine civ WB, 4.5 L over 13 h ... Survived (
(continued)
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
1104 Phillips et al.
0
a)~~~~~~
0 ~~~~~ ~~~ 0
0
0
40 -
0 a)
~~~ C#C~~, C4 O E 0 C.~~~~~~~~Cu ~ ~ ~ C
en a o '0v)
.0 S~~~~~~~. a) 0
0 0~~~~~~~~~0 a) .
73 r. .0 "O T~ co
CZu (
a) -O CY CY 0A 0
0o
CZ C
0 ~ ~~~ m C4 ~ ~ CC ~ u
0 0 0. 0. . -, %0 '
Cu 0 0 >
.0 C )Cd
uo .a OC CZ ~ ~ ~ ~ ~ u
0 ~ ~~ 0d
CuC 0 0-o
u~~~~~~~~~~~~~C O 0~
-S. O
0 m z 0 C~~ul
0 . 4.
Ct)0
0 a tQ \0 m W) WI eq *0
ON ON a, (ON., Cu
0 - m cn n cn en C
5 <~~~~~~~C a)CuZ - + O cd 0 O o . - U u DeCen Cu a)c
incompletely described in recent letters [32, 33]. TWo cases were reported twice [18, 34]. Saddler et al. [32] has reported interim results of the only randomized, prospective study of exchange transfusion of which we are aware. Only eight patients were enrolled in that trial, which was conducted in Zimbabwe. All four patients who received exchange transfusion sur- vived, but three of four patients who did not undergo this procedure died. The findings suggested a sur- vival benefit with exchange transfusion but did not reach statistical significance (P = .07, Fisher exact test).
In the cases outlined in table 1, malaria was ac- quired in East Africa (14 cases), West Africa (13 cases), Central Africa (five cases), Southeast Asia (two cases), South America (one case), and India (one case). There were two blood transfusion-related cases, and for two cases of malaria the country of origin was not specified. The duration of illness be- fore starting antimalarial therapy ranged from 3 to 21 days, with a median interval of 7 days.
Among the 36 patients with >5 %o parasitemia, the median level was 30%o and the range was 5%-757o. The most frequent complications reported for the 40 patients were cerebral malaria in 27 (68%o); renal impairment in 23 (58%o); DIC in 13 (33%); adult re- spiratory distress syndrome in eight (2007o); other pul- monary complications in five (13 %); jaundice in ten (25 0o); hypotension and/or shock in four (10%o); and sepsis in six (15%qo). Four patients (nos. 11, 12, 16, and 28) had uncomplicated cases except for the pres- ence of hyperparasitemia (>5%To of erythrocytes par- asitized).
Antimalarial drugs administered alone, in com- bination, or sequentially included iv quinine in 15 cases (38070); iv quinine by continuous infusion in one case (3qo); iv quinidine by continuous infusion in 11 cases (28 07o); iv quinidine by intermittent infu- sion in three cases (807o); oral quinine in five cases (13%o); parenteral chloroquine in four cases (10%o); oral chloroquine in 11 cases (2807o); pyrimethamine and sulfadoxine in nine cases (23 Oo); mefloquine hy- drochloride in six cases (15%o); and doxycycline or tetracycline in five cases (13 07o).
Exchange transfusion was performed with whole blood in 28 cases (7007o) and with PRBCs in seven cases (1807o), but the blood products used in three other cases (807o) were not specified. TWo patients (8 and 9) received plasma exchange but not whole blood exchange. Among the 40 cases reported, the exchange was performed manually in 32 and with
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
Exchange Transfusion in Falciparum Malaria 1105
the use of an automated cell separator in seven. The time needed to complete the exchange was specified in 21 cases and ranged from 2 to 32 hours, with a median duration of 4 hours. Exchange transfusion was associated with an abrupt decrease in the level of parasitemia. Postexchange-transfusion parasite- mia was expressed as the percentage of circulating erythrocytes that were still infected in 23 patients and ranged from <1% to 3001. The median percentages of parasitized erythrocytes before and after exchange were 30%o and 3070, respectively.
Except for five deaths included in three of the most recent series [25, 29, 30], all other patients with reported cases of malaria who were treated with ex- change transfusion survived. There were 24 survivors (8901o) among the 27 patients with cerebral malaria. Seven reports (table 1, cases 2, 4, 5, 6, 10, 17, 20, 24, and 26) indicated prompt neurologic improve- ment either during or immediately after the exchange transfusion.
The patients who had the four fatal cases shared several poor prognostic factors, including a mean age of 52 years (35 years for survivors); a pretreatment mean parasitemia level of 37170 (33%o for survivors); a pretreatment duration of illness of 8.6 days (7.6 days for survivors); and a mean of 4.4 complications per patient (2.5 for survivors).
Discussion
Erythrocytes parasitized by P falciparum exhibit membrane deformities [35], impaired rheology, ad- herence to endothelium [36], and reduced capacity for transfer of 02. These abnormalities in the micro- circulation result in tissue hypoxia and organ dysfunc- tion. P falciparum, unlike other species of Plasmodia that infect humans, uses a major transmembrane ery- throcyte protein (band 3) for attachment [37]. This protein allows P falciparum to parasitize erythro- cytes of any age, with the potential for development of high-grade parasitemia. It is believed that a prompt reduction in parasitemia is required to halt the progression of the pathophysiologic changes oc- curring in the microcirculation.
The use of exchange transfusion for treatment of severe malaria was first reported by Gyr et al. [10] in 1974. We are aware of an additional 21 reports published since then (excluding this case) that de- scribe a total of 39 patients treated with this proce- dure. An additional ten cases with incomplete clini- cal details were outlined in recent letters [32, 33]. The
close correlation between the level of parasitemia and mortality despite appropriate antimalarial chemo- therapy has provided the impetus for using exchange transfusion to rapidly reduce the number of circulat- ing parasitized erythrocytes. Data from these reports, although obtained in uncontrolled studies, provide compelling evidence of the efficacy of this treatment modality for severe malaria.
The relative importance of chemotherapy vs. ex- change transfusion in effecting a reduction in para- sitemia or a clinical response cannot be determined. However, in many cases a prompt amelioration of clinical signs and a decrease in parasitemia were tem- porally related to exchange transfusion. The survival rate of 89% of the patients in this series is higher than that for patients with similar degrees of parasitemia and similar poor prognostic factors, de- scribed earlier by other investigators [4, 7, 8]. How- ever, this may be due in part to recent improvements in supportive care in that were unavailable at the time of publication of these earlier studies. In a recent report by Vachon et al. (38], 10 (83%) of 12 patients with levels of parasitemia >10O/o survived, although they were not treated with exchange transfusion, a fact that lends support to this possibility. As far as we know, there were no reports of death following treatment with exchange transfusion before the reports of Matsuura et al. [25], Miller et al. [31], and Bernardin et al. [29]. This may be related to the ten- dency to report only successfully treated cases. It is of interest that plasma exchange has been used suc- cessfully in the management of microfilaremia in pa- tients with loiasis [39, 40].
It has been suggested that exchange of both plasma and erythrocytes (whole blood) may provide an advantage over PRBC exchange by removing cir- culating factors and parasite toxins [26]. Clark et al. [41] have presented evidence supporting the role of monokines in the pathogenesis of malaria-related bone marrow depression, DIC, glucocorticoid an- tagonism, shock syndrome, fever, and splenomeg- aly. Monokines, possibly released in response to an endotoxin-like component of the parasite, may con- tribute to the intraerythrocytic death of Plasmodia [42]. Only four case reports describe the use of plas- mapheresis for treatment of malaria [17, 18, 26, 27], and any possible therapeutic benefit in this setting remains speculative. Seven of the 40 patients de- scribed in the present study were transfused with PRBCs rather than whole blood, and all survived.
The minimum volume of blood required for an
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
1106 Phillips et al.
effective exchange transfusion in malaria is un- known. Recommendations have ranged from a two- volume exchange (equivalent to 16-20 units of blood for adults) to as little as four units [5]. Miller et al. [31] suggested that the exchange transfusion should be continued until the level of parasitemia is less than 57o. Warrell et al. [43] have pointed out the imprac- ticality of recommending the use of one- and two- volume exchanges in many of the endemic areas of the world where blood-banking facilities may be limited. The risk of blood transfusion-related hu- man immunodeficiency virus (HIV) infection may outweigh the potential benefits of exchange trans- fusion in countries with both a high prevalence of HIV infection and inadequate facilities for screen- ing donated blood. It may be anticipated that in years to come the World Health Organization's Global Program for the Control of AIDS will reduce the number of countries where this combination of prob- lems exists. Certainly, other blood-borne pathogens such as hepatitis viruses will continue to be a prob- lem for some transfusion recipients [441.
Prompt confirmation of the species of Plasmo- dium is essential so ihat potentially harmful inter- vention (e.g., parenteral cinchona alkaloids and ex- change transfusion) is avoided in benign (i.e., non-falciparum) forms of infection. Exchange trans- fusion, either manually or with a cell separator, should be performed under the supervision of a hematologist or, preferably, an apheresis specialist, if available. The advantages of mechanical exchange transfusion include safe and rapid removal of para- sitized red cells with replacement by healthy donor red cells under monitored conditions; ensurance of a balanced exchange, which is particularly impor- tant for patients presenting with renal compromise; and noninterference with concurrent chemotherapy, which makes dose adjustment unnecessary. If pe- ripheral venous access cannot be achieved, a double- lumen hemodialysis-type catheter should be inserted into the internal jugular or femoral vein. For patients with severe renal failure, concomitant hemodialysis may be performed.
If a cell separator is not readily available, a pa- tient requiring exchange transfusion should have this procedure performed manually. The more seriously ill patient may need to be transferred to a larger cen- ter for treatment. In such cases, parenteral antimalar- ial chemotherapy and vital supportive measures should be initiated prior to the patient's transfer.
The majority of the 40 cases reviewed in this study
were reported from countries in which malaria is not endemic. As noted in other reports, imported malaria caused by P falciparum usually originates in Africa [45], where chloroquine resistance is common [46].
Parenteral chloroquine remains the drug of choice for severe chloroquine-sensitive falciparum malaria [47, 48]. Severe falciparum malaria, which is sus- pected or proven to be drug resistant, requires intra- venous therapy with either quinine dihydrochloride (20 mg/kg of salt given as a loading dose over 4 hours, followed by doses of 10 mg/kg infused over 2- to 8-hour intervals, every 8 hours) or quinidine gluconate (15 mg/kg of the base as a loading dose infused over 4 hours, followed by 7.5 mg/kg infused over 4 hours, every 8 hours) [45, 47, 49]. When pos- sible oral therapy can be substituted to complete a 7-day course of treatment. Because of the greater potential for toxic cardiovascular adverse effects, in- cluding hypotension, quinidine should be reserved for those situations in which parenteral quinine is not available [47].
Miller et al. [31] reported their experience with continuous infusion of quinidine in 15 patients with severe falciparum malaria. With the use of both a lower loading dose and a lower total dose than those reported by Phillips et al. [49] for intermittent ad- ministration of intravenous quinidine, Miller et al. [31] did not observe serious drug-related adverse ef- fects. One patient had frequent premature ventricu- lar beats, and another patient had transient cin- chonism and electrocardiographic abnormalities (QT and QRS interval prolongation). There was no load- ing dose-related hypotension. A loading dose of 10 mg/kg of quinidine gluconate (salt) was infused over 1-2 hours, followed by a constant infusion of 0.02 mg/(kg-min) with the use of a constant infusion pump. The infusions were not continued beyond 3 days. Among four patients treated with continuous infusions of quinidine plus exchange transfusion, only minor reductions in the serum quinidine re- sulted, with mean pre- and postexchange levels of 3.75-3.0 mg/L, respectively. Therefore, quinidine dosage adjustment appears to be unnecessary for pa- tients treated with exchange transfusion.
Unresolved questions regarding the use of ex- change transfusion for severe malaria include spe- cific indications, minimum effective exchange vol- ume, and the choice of whole blood rather than PRBCs. Despite the lack of controlled trials demon- strating the efficacy of exchange transfusion, this procedure appears to be a useful adjunctive measure
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
Exchange Tansfusion in Falciparum Malaria 1107
in selected patients. The use of exchange transfusion for treatment of severe falciparum malaria should be considered in any of the following situations: parasitemia in >100o of circulating erythrocytes; ce- rebral malaria; DIC; and acute renal failure. The poor prognosis of elderly patients with complicated falciparum malaria raises the question of more liberal use of exchange transfusion in this popula- tion. The answers to this and other questions await further studies.
References
1. Malaria surveillance: annual summary 1980. Atlanta: Centers for Disease Control, 1982
2. Yechouron A, Nguyen C, Maclean JD, Keystone J. The chang- ing pattern of imported malaria. Can Dis Wkly Rep 1988;14(30):133-6
3. Wyler DJ. Plasmodium species. In Mandell GL, Douglas RG, Bennett JE, eds. Principles and practice of infectious dis- eases. 3rd ed. New York: Churchill Livingstone, 1990: 2056-66
4. Stone WJ, Hanchett JE, Knepshield JH. Acute renal insuffi- ciency due to falciparum malaria: review of 42 cases. Arch Intern Med 1972;129:620-8
5. World Health Organization Malaria Action Programme. Se- vere and complicated malaria. Thans R Soc Thop Med Hyg 1986;80(Suppl):1-50
6. Field JW. Blood examination and prognosis in acute falcipa- rum malaria. Trans R Soc Trop Med Hyg 1949;43:33-48
7. Marsden PD, Bruce-Chwatt LJ. Cerebral malaria. In Hor- nabrook RW, ed. Topics on tropical neurology. Contem- porary neurology series. Vol. 12. Philadelphia: F. A. Davis, 1975:29-44
8. Maegraith B. Blackwater fever anuria. TBans R Soc Trop Med Hyg 1944;38:1-23
9. Bruce-Chwatt LJ. Malaria. Epidemiology. BMJ 1971;2:91-3 10. Gyr K, Speck B, Ritz R, Cornu P, Buckner CD. Zerebrale
malaria tropica mit schwarzwasserfieber. Ein aktuelles di- agnostisches und therapeutisches problem. Schweiz Med Wochenschr 1974;104:1628-30
11. Kurathong S, Srichaikul T, Isarangkura P, Phanichphant S. Exchange transfusion in cerebral malaria complicated by disseminated intravascular coagulation. Southeast Asian J Thop Med Public Health 1979;10:389-92
12. Nielsen RL, Kohler RB, Chin W, McCarthy LJ, Luft FC. The use of exchange transfusions: a potentially useful adjunct in the treatment of fulminant falciparum malaria. Am J Med Sci 1979;277:325-9
13. Roncoroni AJ, Martino OA. Therapeutic use of exchange transfusion in malaria. Am J Thop Med Hyg 1979;28:4404
14. Yarrish RL, Janas JS, Nosanchuk JS, Steigbigel RT, Nus- bacher J. Thansfusion malaria: treatment with exchange transfusion after delayed diagnosis. Arch Intern Med 1982;142:187-8
15. Kramer SL, Campbell CC, Moncrieff RE. Fulminant Plas- modiumfakciparum infection treated with exchange blood transfusion. JAMA 1983;249:244-5
16. Files JC, Case CJ, Morrison FS. Automated erythrocyte ex- change in fulminant falciparum malaria. Ann Intern Med 1984;100:396-7
17. Bambauer R, Jutzler GA. Falciparum malaria successfully treated with plasma exchange. Plasma Ther Tiansfus Tech- nol 1984;5:343-47
18. Bambauer R, Jutzler GA. Therapeutic plasma exchange in severe falciparum malaria. Dtsch Med Wochenschr 1985; 110:1290-3
19. Hall A, Yardumian A, Marsh A. Exchange transfusion and quinine concentrations in falciparum malaria. BMJ 1985;291:1169-70
20. Chiodini PL, Somerville M, Salam I, Thbbs HR, Wood MJ, Ellis CJ. Exchange transfusion in severe falciparum malaria. Trans R Soc Tnop Med Hyg 1985;79:865-6
21. Manquat G, Bru JP, Carpentier F, Micoud M, Guignier M. Acces pernicieux, palustre. Evolution rapidement favora- ble apres exsanguino-transfusion [letter]. Presse Med 1986;15:2118
22. Schunkert H, Gladziwa U. Blutaustauschtransfusion bei zerebraler Malaria tropica. Dtsch Med Wochenschr 1986; 111:1582
23. Lataste P, Soubiran G, Nlend A, Le Bras M, Roue R, Wone C, Ragnaud JC, Buil A, Briand MC, Ripert C, Fialon B, Couprie B, Combe A, Interet de l'exsanguinotransfusion dans le traitment du paludisme grave (a propos de 5 ob- servations). Bull Soc Pathol Exot Filiales 1987;80:561-8
24. Rudnitsky G, Miller KD, Padua T, Stull TL. Continuous- infusion quinidine gluconate for treating children with se- vere Plasmodiumfakciparum malaria. J Infect Dis 1987; 155:1040-3
25. Matsuura GK, Chan LA. Ineffectiveness of continuous quini- dine gluconate infusion in the treatment of severe chloroquine-resistant Plasmodium falciparum malaria. Drug Intell Clin Pharm 1988;22:883-5
26. Stuby U Kaiser W, Biesenbach G, Zazgornik J. Successful treatment of malaria tropica with acute renal failure and cerebral involvement by plasmapheresis and hemodialy- sis. Infection 1988;16:362-4
27. Heim MU, Mezger J, Scheurlen C, TWardzik L, Wilmanns W. Exchange transfusion and (or) plasmapheresis: effec- tive measures in severe tropical malaria? Dtsch Med Wochenschr 1988;113:941-4
28. Lelarge P, Hoen B, Jeanraux N, Gerard A, Schooneman F, Kures L, Canton P, Dureux JB. A severe and atypical form of Plasmodium falciparum malaria treated with intrave- nous quinine and exsanguinotransfusion [letter]. Presse Med 1989;18:540
29. Bernardin G, Fournier JP, Quaranta JF, Marty P, Deilamonica P, Mattei M. Acute respiratory distress syndrome with fa- tal outcome after exsanguinotransfusion in pernicious malaria attack [letter]. Presse Med 1989;18:1394-5
30. Esposito R, Antinori S, Orlando G, Rizzardini G, Zocchi C, Spazzolini A, Galli M. Exchange transfusion for malaria [letter]. Lancet 1990;335:790-1
31. Miller KD, Greenberg AE, Campbell CC. Theatment of se- vere malaria in the United States with a continuous infu- sion of quinidine gluconate and exchange transfusion. N Engl J Med 1989;321:65-70
32. Saddler M, Barry M, Ternouth I, Emmanuel J. Treatment
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions
1108 Phillips et al.
of severe malaria by exchange transfusion [letter]. N Engl J Med 1990;322:58
33. Shwe T, Myint PT, Warhurst DC. Exchange transfusion in falciparum malaria [letter]. Lancet 1990;335:1034-5
34. Hall AP. Exchange transfusion and quinine levels in falcipa- rum malaria. Acta Leidensia 1987;55:121-128
35. Langreth SG, Jensen JB, Reese RT, Trager W. Fine structure of human malaria in vitro. J Protozool 1978;25:443-52
36. Udeinya IJ, Schmidt JA, Aikawa M, Miller LH, Green I. Fal- ciparum malaria-infected erythrocytes specifically bind to cultured endothelial cells. Science 1981;213:555-7
37. Okoye VCN, Bennett V. Plasmodium falciparum malaria: band 3 as a possible receptor during invasion of human erythrocytes. Science 1985;227:169-71
38. Vachon F, Wolff M, Clair B, Regnier B. lTeatment of severe malaria by exchange transfusion [letter]. N Engl J Med 1990;322:58-9
39. Muylle L, Modenhauer R, Taelman H, Van Brabant R, Peeter- mans ME. Usefulness of apheresis to extract microfilarias in management of loiasis [abstract]. BMJ 1983;287:519-20
40. Saeed AA, Green PJ, Naoroz M, Lee HA, Raman GV. Loa loa: the use of a blood cell separator to reduce microfilarae- mia before specific chemotherapy. J Infect 1984;9:161-6
41. Clark IA, Virelizier JL, Carswell EA, Wood PR. Possible im- portance of macrophage-derived mediators in acute malaria. Infect Immun 1981;32:1058-66
42. Clark IA, Richmond JE, Wills EJ, Allison AC. Immunity to intra-erythrocytic protozoa. Lancet 1975;2:1128-9
43. Warrell DA, White NJ, Looareesuwan S, Phillips RE, War- rell MJ, Bunnag D, Harinasuta KT. The treatment of se- vere falciparum malaria [letter]. BMJ 1985;291:1573
44. Aach RD, Kahn RA. Post-transfusion hepatitis: current per- spectives. Ann Intern Med 1980;92:539-46
45. Peto TEA, Gilks CF. Strategies for the prevention of malaria in travellers: comparison of drug regimens by means of risk-benefit analysis. Lancet 1986;1:1256-60
46. Cook GC. Prevention and treatment of malaria. Lancet 1988;1:32-6
47. White NJ. Drug treatment and prevention of malaria. Eur J Clin Pharmacol 1988;34:1-14
48. White NJ, Miller KD, Churchill FC, Berry C, Brown J, Wil- liams SB, Greenwood BM. Chloroquine treatment of se- vere malaria in children: Pharmacokinetics, toxicity, and new dosage recommendations. N Engl J Med 1988;319: 1493-500
49. Phillips RE, Warrell DA, White NJ, Looareesuwan S, Karb- wang J. Intravenous quinidine for the treatment of severe falciparum malaria: clinical and pharmacokinetic studies. N Engl J Med 1985;312:1273-8
This content downloaded from 128.237.134.103 on Thu, 13 Feb 2014 15:38:48 PMAll use subject to JSTOR Terms and Conditions