Perioperative complications in children with pulmonary hypertension undergoing general anesthesia...
Transcript of Perioperative complications in children with pulmonary hypertension undergoing general anesthesia...
Perioperative complications in children withpulmonary hypertension undergoing generalanesthesia with ketamine
GLYN D. WILLIAMS M B CM B C hh BB* , HARJOT MAAN B SB S†,
CHANDRA RAMAMOORTHY M DM D*, KOMAL KAMRA M DM D*,
SUSAN L. BRATTON M D M P HM D M P H‡, ELLEN BAIR N PN P* , CALVIN
C. KUAN M DM D*, GREGORY B. HAMMER M DM D* AND JEFFREY
A. FEINSTEIN M D M P HM D M P H§
*Division of Pediatric Cardiology, Department of Anesthesia, Lucile Packard Children’sHospital, Stanford University, Stanford, CA, †Medical Student, Dartmouth Medical Center,Hanover, NH, ‡Pediatric Critical Care Medicine, University of Utah, Salt Lake City, UT and§Division of Pediatric Cardiology, Department of Pediatrics, Lucile Packard Children’s Hospital,Stanford University, Stanford, CA, USA
SummaryBackground: Pulmonary arterial hypertension (PAH) is associated
with significant perioperative risk for major complications in children,
including pulmonary hypertensive crisis and cardiac arrest. Uncer-
tainty remains about the safety of ketamine anesthesia in this patient
population.
Aim: Retrospectively review the medical records of children with
PAH to ascertain the nature and frequency of peri-procedural
complications and to determine whether ketamine administration was
associated with peri-procedural complications.
Methods: Children with PAH (mean pulmonary artery pressure
‡25 mmHg and pulmonary vascular resistance index ‡3 Wood units)
who underwent general anesthesia for procedures during a 6-year
period (2002–2008) were enrolled. Details about the patient, PAH,
procedure, anesthetic and postprocedural course were noted,
including adverse events during or within 48 h of the procedure.
Complication rates were reported per procedure. Association between
ketamine and peri-procedural complications was tested.
Results: Sixty-eight children (median age 7.3 year, median weight
22 kg) underwent 192 procedures. Severity of PAH was mild (23%),
moderate (37%), and severe (40%). Procedures undertaken were
major surgery (n = 20), minor surgery (n = 27), cardiac catheterization
(n = 128) and nonsurgical procedures (n = 17). Ketamine was
administered during 149 procedures. Twenty minor and nine major
complications were noted. Incidence of cardiac arrest was 0.78% for
cardiac catheterization procedures, 10% for major surgical procedures
and 1.6% for all procedures. There was no procedure-related
mortality. Ketamine administration was not associated with increased
complications.
Correspondence to: G.D. Williams, 300 Pasteur Drive, M ⁄ C 5640, Stanford, CA 94305, USA (email: [email protected]).
Pediatric Anesthesia 2010 20: 28–37 doi:10.1111/j.1460-9592.2009.03166.x
28 � 2009 Blackwell Publishing Ltd
Conclusions: Ketamine appears to be a safe anesthetic option for
children with PAH. We report rates for cardiopulmonary resuscitation
and mortality that are more favorable than those previously reported.
Keywords: children; complications; general anesthesia; hypertension;
ketamine; perioperative; pulmonary
Introduction
Pulmonary arterial hypertension (PAH) is defined as
a mean pulmonary arterial blood pressure that
exceeds 25 mmHg at rest or 30 mmHg during
exercise in association with variable degrees of
pulmonary vascular remodeling, vasoconstriction,
and in situ thrombosis (1,2).
Children with PAH typically have an increased
requirement for medical resources (3) and may
receive multiple general anesthetics for procedures
related to PAH assessment and management. The
pathophysiology of PAH (4–6) and the associated
anesthetic considerations for adults and children
have been reviewed (4,5,7,8). PAH contributes to
perioperative morbidity and mortality (7,9–15).
Although ketamine has been used successfully in
the anesthetic management of patients with PAH
(16), its use remains controversial because it has
been associated with increased pulmonary arterial
pressure in adult patients (17). Studies evaluating
the effect of ketamine on pulmonary artery pressure
in children with PAH have reported conflicting
results (18–21).
We previously studied the hemodynamic
responses to ketamine in children with PAH and
found that ketamine in the presence of sevoflurane
did not cause increased pulmonary vascular
resistance (PVR) (22). The effects on PVR of keta-
mine, either as the sole agent or when administered
along with anesthetic agents other than sevoflurane,
were not investigated. Consequently, uncertainty
remains whether ketamine without concomitant
sevoflurane is an appropriate anesthetic option for
children with PAH. To address this ambiguity, we
conducted a 6-year retrospective review of children
with PAH who underwent diagnostic and
therapeutic procedures to ascertain the nature and
frequency of peri-procedural complications.
We hypothesized that ketamine administration dur-
ing anesthesia was not associated with peri-proce-
dural complications.
Methods
Institutional Review Board approval with waiver of
informed consent was obtained for this retrospective
cohort of children with PAH who underwent gen-
eral anesthesia for a procedure during the period
from October 1, 2002, to October 31, 2008. Potential
study participants were identified by searching the
institution’s Heart Center database for patients
with the diagnosis of pulmonary hypertension who
underwent general anesthesia for cardiac catheteri-
zation. The medical records of these patients were
then reviewed to ascertain whether criteria for study
enrollment were met.
Inclusion criteria were as follows: (i) a mean
pulmonary artery pressure ‡25 mmHg and a calcu-
lated PVR (indexed) ‡3 Wood units; (ii) all patients
receiving pulmonary vasodilator therapy for PAH
(diagnosis confirmed by cardiac catheterization);
and (iii) age <18 years.
Exclusion criteria were as follows: (i) elevation
of pulmonary artery pressure because of main or
proximal branch pulmonary artery obstructions and
(ii) the diagnosis of tetralogy of Fallot, pulmonary
atresia, and major aorto-pulmonary collaterals.
The medical records of eligible patients were
examined to identify all procedures performed
under general anesthesia during the study period.
Data were recorded describing patient demograph-
ics, preprocedure diagnoses, procedure performed,
anesthesia management, cardiac catheterization
findings, postprocedure course until discharge from
hospital, and any adverse events that occurred
during or within 48 h of the procedure. Duration
of follow-up and mortality were also recorded.
PULMONARY HYPERTENSION: IS KETAMINE SAFE? 29
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
Definitions of complications were consistent with
previous reports (23). An incident was an observed
change in monitored values that was transient, had
no effect on the patient’s condition and required
minimal or no treatment. A minor complication was a
transient event that had no long-term ill effect on the
patient and resolved with specific treatment. A major
complication was a potentially life-threatening event
requiring immediate treatment. For example, occur-
rence of an arrhythmia would be (i) excluded if there
was no hemodynamic disturbance and no interven-
tion required; (ii) an incident if the arrhythmia
caused minor hemodynamic disturbance and
resolved spontaneously; (iii) a minor complication
if there was minor hemodynamic disturbance and
a therapeutic intervention was required; and (iv) a
major complication if there was severe hemodynamic
compromise that required prompt intervention.
For each procedure, patients were classified based
on the severity of their PAH. For those undergoing
cardiac catheterization, the PAH categories were
mild [pulmonary vascular resistance index (PVRI) >
3–7 Wood units], moderate (PVRI > 7–12 Wood
units), or severe (>12 Wood units). Patients under-
going procedures other than cardiac catheterization
were classified on the basis of the preprocedure
echocardiogram as follows: mild (systolic pulmo-
nary artery blood pressure (PAP) £70% of systolic
systemic blood pressure), moderate (systolic
PAP > 70–100% of systolic systemic blood pressure)
or severe (systolic PAP > 100% of systolic systemic
blood pressure) (13). The most recent cardiac cath-
eterization data were used if PAP could not be
estimated from the preprocedure echocardiogram.
Patients were categorized as reactive to pulmonary
vasodilator therapy if the following criteria were
met at cardiac catheterization: (i) a decrease of
‡10 mmHg in mean PAP to values <40 mmHg if
baseline mean PAP was >40 mmHg; (ii) ‡20%
decrease in mean PAP and PVRI if baseline mean
PAP was <40 mmHg (24).
All medical services were provided at a tertiary
children’s hospital. Anesthesia care was provided by
pediatric anesthesiologists or by pediatric cardiac
intensivists. The anesthetic technique employed was
determined by the physician of record.
Procedures were classified as (a) nonsurgical,
which includes cardiac catheterization and other
nonsurgical procedures, and (b) surgical, which
may be minor or major. Major surgery was defined
as an extensive surgical procedure involving the
cranium, vertebral column, chest, abdomen, or
pelvic cavity.
Descriptive statistics were used, and they
included median and interquartile ranges. Categor-
ical data were compared using the chi-squared test,
while continuous data were compared using the
Mann–Whitney U test. The relative risk ratio (RR)
with 95% Confidence Intervals (CI) was calculated.
A multivariable logistic regression model to evaluate
factors associated with either major or minor peri-
procedure complications was developed. Factors
associated with complication in the bivariate analy-
sis were considered using a forward selection
procedure with entry of variables into the model
set at P £ 0.05 and removal defined as P £ 0.10 odds
ratio (OR) with 95% CI were calculated. SPSSSPSS version
15.0 software (SPSS Inc, Chicago, IL, USA) was used
for the analysis. Complication rates were reported
per procedure rather than per patient, as some
children had more than one procedure. Complica-
tions were compared for all study subjects. Then the
subgroup that had nonsurgical procedures was
evaluated separately.
Results
During the study period, 68 children (35 boys, 33
girls) underwent 192 procedures. Median (range)
patient age was 7.3 year (14 days–18.4 year) and
weight was 22 kg (2.4–105 kg). Congenital heart
defects were present in 43 (61.8%) patients; 11
children were diagnosed with genetic disorders
(trisomy 21: n = 7, trisomy 18: n = 1, Stickler
syndrome: n = 1, Williams syndrome: n = 1, multi-
ple dysmorphic features of nonspecific pattern:
n = 1). Clinical types of pulmonary hypertension
are detailed in Table 1. The classification is sub-
jective, because some patients had multiple factors
associated with PAH.
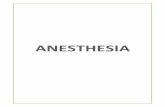
Selected details about the procedures, the patients’
preanesthesia status, and the anesthetic techniques
employed are provided in Table 2 and Figure 1.
Prior to their procedure, 17 (8.9%) patients had an
endotracheal tube or tracheostomy tube in situ, 14
(7.3%) had an arterial monitoring catheter, 21
(10.9%) had a gastrostomy tube, and 6 (3.1%) were
on intravenous inotropic support.
30 G.D. WILLIAMS ET AL.
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
Anesthesia care for the procedures was provided
by pediatric cardiac anesthesiologists [184 (96%)],
pediatric general anesthesiologists [6 (3%)], and
pediatric cardiac intensivists [2 (1%)]. An anesthe-
sia trainee (resident or fellow) was present for 161
(83.9%) procedures. Drugs utilized for induction of
anesthesia included ketamine (52.1%), sevoflurane
(47.9%), propofol (10.9%), and etomidate (3.6%),
(data given as percentage of total procedures).
Anesthetic agents for maintenance included keta-
mine (66.7%), propofol (63%), midazolam (29.1%),
isoflurane (18.2%), and sevoflurane (15.1%). The
percentage of cases per year that received ketamine
averaged about 50 during the first 2 years and
increased to about 90 during the last 2 years of the
study period. Neuromuscular blocking drugs were
administered during 57 (29.7%) and opioids in 71
(37%) procedures. The airway of many patients
[122 (63.5%)] was managed by providing nasal
cannulae oxygen or by application of a facemask.
An endotracheal tube was used in 63 (32.8%)
cases, a laryngeal mask in 4 (2.1%), and a trache-
ostomy tube was in situ in 3 (1.6%) patients.
Intravenous inotropes were administered as
a bolus or by infusion during 28 (14.6%) proce-
dures. Anesthesia records were incomplete in 2
(1%) cases.
Four incidents occurred, all during cardiac cathe-
terization procedures. Vital signs were minimally
affected and no treatment was required. Two were
pulmonary in nature (small emesis on emergence,
cough with contrast injection) and two were transient
catheter-induced cardiac events (atrial arrhythmia,
heart block). Minor (n = 20) and major (n = 9)
Table 1
Clinical classification of pulmonary hypertension in 68 patients
Category n % of total
1. Pulmonary arterial hypertension (PAH)1.1. Idiopathic 12 17.61.3. Associated with:
1.3.1. Collagen vascular disease 2 2.9Juvenile rheumatoid arthritis: n = 1Fibromuscular dysplasia: n = 1
1.3.2. Congenital systemic-to-pulmonary shunts 32 47.1Cardiac malformations: n = 29Noncardiac vascular malformations: n = 3
1.3.3. Portal hypertension (congenital hepatic fibrosis: n = 1) 1 1.51.3.6. Other 4 5.9
Polycystic kidney disease: n = 2Myeloproliferative disorders: n = 2
1.4. Associated with significant venous or capillary involvement1.4.1. Pulmonary veno-occlusive disease 8 11.8
Congenital pulmonary vein stenosis: n = 81.4.2. Pulmonary capillary hemangiomatosis 1 1.5
1.5. Persistent pulmonary hypertension of the newborn 3 4.4Distal pulmonary artery stenoses: n = 3
2. Pulmonary hypertension with left heart disease2.1. Left-sided atrial or ventricular heart disease (cardiomyopathy: n = 6) 6 8.82.2. Left-sided valvular heart disease (congenital valvular defects: n = 3) 3 4.43. Pulmonary hypertension associated with lung diseases and ⁄ or hypoxemia3.1. Chronic obstructive pulmonary disease 4 5.9
Lung disease of prematurity: n = 43.2. Interstitial lung disease 1 1.53.3. Sleep-disordered breathing (obstructive sleep apnea: n = 6) 6 8.83.4. Alveolar hypoventilation disorders (scoliosis: n = 2) 2 2.93.6. Developmental abnormalities (diaphragmatic hernia: n = 2) 3 4.44. Pulmonary hypertension because of chronic thrombotic and ⁄ or embolic disease4.2. Thromboembolic obstruction of distal pulmonary arteries 1 1.55. Miscellaneous 0 0
A total of 89 factors associated with pulmonary hypertension were identified in 68 patients. Source: Simonneau G, Galie N, Rubin LJ et al.Clinical classification of pulmonary hypertension. J Am Coll Cardiol 2004; 43: 5S–12S.
PULMONARY HYPERTENSION: IS KETAMINE SAFE? 31
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
complications of all patients are detailed in Table 3.
The nature of events that initiated complications were
ascribed as follows: cardiac (n = 14), pulmonary
(n = 10), technical (n = 4), and allergic (n = 1).
There were no procedure-related deaths. One
patient undergoing cardiac catheterization and two
patients undergoing major surgery required cardio-
pulmonary resuscitation during their procedure.
The first of these three cases involved a 15- year-
old girl undergoing heart lung transplantation for
severe idiopathic PAH who probably had a pulmo-
nary hypertensive crisis during tracheal intubation
(developed bradycardia, hypotension, and decreas-
ing oxygen saturations) after receiving midazolam,
ketamine, and rocuronium. The second case was
a 10- year-old boy with an atrial septal defect and
severe PAH who was receiving epoprostenol and
nitric oxide and underwent scoliosis surgery via
a posterior approach. Pulmonary artery pressures
were equal to systemic arterial pressures at the start
of the procedure but over the next 5 h of surgery
twice became markedly suprasystemic for periods
lasting >15 min. The second suprasystemic episode
Table 2
Types of procedures performed (n = 192) and preproceduremedical status of the patients
N (%)
Procedure typesNonsurgical procedures
Cardiac catheterization 128 (66.7%)Other proceduresa 17 (8.9%)
Surgical proceduresMinorb 27 (14.1%)Majorc 20 (10.3%)
Preprocedure medical statusBaseline PAH classificationd
Mild 45 (23.4%)Moderate 70 (36.5%)Severe 77 (40.1%)
Preprocedure medicationsPulmonary vasodilator therapye 113 (58.9%)Heart failure therapyf 58 (30.2%)Diuretic therapy 73 (38%)Anticoagulant therapyg 77 (40.1%)FiO2 > 0.21 57 (29.7%)
Preprocedure hospital statusIn-patient 58 (30.2%)
ASA physical statusII 4 (2.1%)III 113 (58.9%)IV 75 (39.0%)
ASA, American Society of Anesthesiologists. aIncluded comput-erized tomography (n = 11), radionucleotide lung perfusion scans(n = 5), magnetic resonance imaging (n = 4) and pulmonaryfunction tests (n = 1). Four patients underwent two imagingprocedures during the same anesthetic. bIncluded central venouscatheter insertion or removal (n = 18), airway examination orsurgery (n = 4), lumbar puncture and ⁄ or bone marrow aspiration(n = 2), and other procedures (n = 3). cIncluded heart and ⁄ or lungsurgery with cardiopulmonary bypass (n = 14), spine surgery(n = 3), cerebral embolization procedures (n = 2) and omphalocelerepair (n = 1). dPulmonary arterial hypertension (PAH) wasclassified as follows (see text for details): Mild: Pulmonaryvascular resistance index (PVRI) >3–7 Wood units or estimatedsystolic pulmonary artery pressure (PAP) £70% of systolicsystemic arterial pressure (SAP); Moderate: PVRI >7–12 Woodunits or estimated systolic PAP >70–100% of SAP; Severe: PVRI>12 Wood units or estimated systolic PAP >100% of systolic SAP.ePulmonary vasodilator therapy included sildenafil [69 (35.9%)procedures], treprostinil sodium or epoprostenol sodium [63(32.8%) procedures], bosentan [49 (25.5%) procedures], and nitricoxide [9 (4.7%) procedures]. fHeart failure drugs includedcaptopril, carvedilol, digoxin, dobutamine, dopamine, enalapril,epinephrine, esmolol, milrinone, nifedipine. gAnticoagulant drugsincluded coumadin and aspirin.
0
10
20
30
40
50
60
70
Ket
amin
e
Sev
ofl
ura
ne
Ket
amin
e+
sevo
flu
ran
e
Mid
azo
lam
+o
pio
id
Pro
po
fol
Ket
amin
e+
pro
po
fol
Eto
mid
ate
Sev
ofl
ura
ne
+p
rop
ofo
l
n
Drugs used for induction of anesthesia
0102030405060708090
Ket
amin
e+
pro
po
fol
Vo
lati
le
Ket
amin
e+
pro
po
fol+
vola
tile
Ket
amin
e
Pro
po
fol
Mid
azo
lam
+o
pio
id
Ket
amin
e+
vola
tile
Pro
po
fol+
vola
tile
n
Drugs used for maintenance of anesthesia
Figure 1Drugs used for induction and maintenance of anesthesia during192 procedures.
32 G.D. WILLIAMS ET AL.
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
Ta
ble
3
Su
mm
ary
of
maj
or
and
min
or
per
i-p
roce
du
reco
mp
lica
tio
ns
du
rin
g19
2p
roce
du
res
Typ
eE
ven
tM
anag
emen
tP
roce
dure
Age
(yea
r)P
VR
Min
or
(n=
20)
Car
dia
cS
up
rav
entr
icu
lar
tach
yca
rdia
Ad
eno
sin
eC
ard
iac
cath
eter
izat
ion
8.1
Sev
ere
Car
dia
cS
up
rav
entr
icu
lar
tach
yca
rdia
Res
olv
edw
ith
cath
eter
man
ipu
lati
on
Car
dia
cca
thet
eriz
atio
n9.
2S
ever
eC
ard
iac
Atr
ial
flu
tter
Ex
tern
alca
rdio
ver
sio
nC
ard
iac
cath
eter
izat
ion
10.7
Mo
der
ate
Car
dia
cM
ult
iple
epis
od
essu
pra
ven
tric
ula
rta
chy
card
iaA
den
osi
ne,
exte
rnal
card
iov
ersi
on
Car
dia
cca
thet
eriz
atio
n1.
0S
ever
e
Car
dia
cS
up
rav
entr
icu
lar
tach
yca
rdia
bef
ore
CP
BE
xte
rnal
card
iov
ersi
on
AV
SD
rep
air
(CP
B)
0.3
Mo
der
ate
Car
dia
cS
up
rav
enti
cula
rta
chy
card
iaA
den
osi
ne
Car
dia
cca
thet
eriz
atio
n0.
04S
ever
eC
ard
iac
Pu
lmo
nar
yh
yp
erte
nsi
on
Inh
aled
nit
ric
ox
ide,
epin
eph
rin
eb
olu
sP
AP
VR
rep
air
(CB
P)
3.9
Mo
der
ate
Car
dia
cH
yp
ote
nsi
on
Ep
hed
rin
eb
olu
sC
ard
iac
cath
eter
izat
ion
13.2
Sev
ere
Car
dia
cH
yp
ote
nsi
on
Ph
eny
lep
hri
ne
bo
luse
sC
entr
alli
ne
inse
rtio
n5.
4S
ever
eC
ard
iac
Hy
po
ten
sio
nE
ph
edri
ne
bo
lus
CT
ches
t,lu
ng
scan
6.4
Mo
der
ate
Pu
lmo
nar
yL
ary
ng
osp
asm
wit
hd
esat
ura
tio
nA
irw
ayse
cure
dw
ith
end
otr
ach
eal
tub
eC
ard
iac
cath
eter
izat
ion
18.4
Mo
der
ate
Pu
lmo
nar
yP
ost
op
erat
ive
som
nu
len
ce(c
hro
nic
hy
po
ven
tila
tor)
Nal
ox
on
eto
rev
erse
op
ioid
Car
dia
cca
thet
eriz
atio
n14
.8M
od
erat
e
Pu
lmo
nar
yIn
term
itte
nt
nat
ive
airw
ayo
bst
ruct
ion
Air
way
secu
red
wit
hen
do
trac
hea
ltu
be
Car
dia
cca
thet
eriz
atio
n9.
0M
ild
Pu
lmo
nar
yS
ever
eb
ron
cho
spas
mB
ron
cho
dil
ato
rd
rug
s,ad
mit
ICU
Car
dia
cca
thet
eriz
atio
n4.
1M
ild
Pu
lmo
nar
yC
ou
gh
ing
com
pro
mis
ing
nat
ive
airw
ayA
irw
ayse
cure
dw
ith
end
otr
ach
eal
tub
eC
ard
iac
cath
eter
izat
ion
1.2
Sev
ere
Pu
lmo
nar
yL
ary
ng
osp
asm
com
pro
mis
ing
nat
ive
airw
ayB
ag-m
ask
ven
tila
tio
nC
ard
iac
cath
eter
izat
ion
4.0
Mo
der
ate
Pu
lmo
nar
yIn
term
itte
nt
ob
stru
ctio
no
fn
ativ
eai
rway
Air
way
secu
red
wit
hla
ryn
gea
lm
ask
Car
dia
cca
thet
eriz
atio
n9.
2M
od
erat
eP
ulm
on
ary
Hy
po
ven
tila
tio
nA
ssis
tb
ag-m
ask
ven
tila
tio
nC
ard
iac
cath
eter
izat
ion
13.4
Sev
ere
All
erg
yR
ash
,u
nk
no
wn
etio
log
yS
tero
id,
anti
his
tam
ine
VS
Dre
pai
r(C
PB
)7.
3M
ild
Tec
hn
ical
Scr
ota
lh
emat
om
aC
on
serv
ativ
em
anag
emen
tC
ard
iac
cath
eter
izat
ion
12.4
Sev
ere
Maj
or
(n=
9)C
ard
iac
Acu
teo
nse
tp
uls
eles
sel
ectr
ical
acti
vit
yC
ard
iop
ulm
on
ary
resu
scit
atio
nC
ard
iac
cath
eter
izat
ion
1.8
Sev
ere
Car
dia
cV
entr
icu
lar
tach
yca
rdia
cfr
om
pu
lmo
nar
yh
yp
erte
nsi
ve
cris
iso
nin
du
ctio
no
fan
esth
esia
Car
dio
pu
lmo
nar
yre
susc
itat
ion
Hea
rt-l
un
gtr
ansp
lan
t(C
PB
)15
.2S
ever
e
Car
dia
cV
entr
icu
lar
tach
yca
rdia
fro
mp
ulm
on
ary
hy
per
ten
siv
ecr
isis
du
rin
gsu
rger
yC
ard
iop
ulm
on
ary
resu
scit
atio
n,
rep
osi
tio
nsu
pin
eP
ost
erio
rsc
oli
osi
sre
pai
r9.
8M
od
erat
e
Car
dia
cH
yp
ote
nsi
on
wit
hp
osi
tiv
ep
ress
ure
ven
tila
tio
nP
roce
du
reab
ort
edM
RI
ches
t15
.7S
ever
e
Pu
lmo
nar
yR
igh
tu
pp
erlo
be
atel
ecta
sis
1d
ayp
ost
pro
ced
ure
Re-
adm
itto
ICU
,re
spir
ato
ryth
erap
yC
ard
iac
cath
eter
izat
ion
16.5
Sev
ere
Pu
lmo
nar
yR
eper
fusi
on
lun
gin
jury
afte
rb
allo
on
ang
iop
last
yo
fb
ran
chp
ulm
on
ary
arte
ries
Re-
adm
itto
ICU
,re
spir
ato
ryth
erap
yC
ard
iac
cath
eter
izat
ion
17.2
Mo
der
ate
Tec
hn
ical
Ep
idu
ral
PC
Am
alfu
nct
ion
cau
sin
gh
yp
ov
enti
lati
on
Re-
adm
itto
ICU
,re
spir
ato
ryth
erap
yL
un
gtr
ansp
lan
t(C
PB
)12
.7M
od
erat
e
Tec
hn
ical
Re-
op
erat
ion
for
po
sto
per
ativ
eb
leed
ing
Flu
idre
susc
itat
ion
,su
rgic
alh
emo
stas
isH
eart
-lu
ng
tran
spla
nt
(CP
B)
10.8
Sev
ere
Tec
hn
ical
Fal
sean
eury
smo
ffe
mo
ral
arte
ryS
urg
ical
rep
air
Car
dia
cca
thet
eriz
atio
n1.
2S
ever
e
PA
PV
R,p
arti
alan
om
alo
us
pu
lmo
nar
yv
eno
us
retu
rn;C
PB
,car
dio
pu
lmo
nar
yb
yp
ass;
ICU
,in
ten
siv
eca
reu
nit
;AV
SD
,atr
iov
entr
icu
lar
sep
tal
def
ect;
VS
D,v
entr
icu
lar
sep
tal
def
ect;
CT
,co
mp
ute
rize
dto
mo
gra
ph
yim
agin
g;
PC
A,
pat
ien
tco
ntr
oll
edan
alg
esia
;M
RI,
mag
net
icre
son
ance
imag
ing
.P
ulm
on
ary
hy
per
ten
sio
nca
teg
ori
zed
asm
ild
,m
od
erat
ean
dse
ver
e.M
ild
:P
ulm
on
ary
vas
cula
rre
sist
ance
ind
ex(P
VR
I)>
3–7
Wo
od
un
its
or
esti
mat
edsy
sto
lic
pu
lmo
nar
yar
tery
pre
ssu
re(P
AP
)£7
0%o
fsy
sto
lic
syst
emic
arte
rial
pre
ssu
re(S
AP
);M
od
erat
e:P
VR
I>
7–12
Wo
od
un
its
or
esti
mat
edsy
sto
lic
PA
P>
70–1
00%
of
SA
P;
Sev
ere:
PV
RI
>12
Wo
od
un
its
or
esti
mat
edsy
sto
lic
PA
P>
100%
of
syst
oli
cS
AP
.
PULMONARY HYPERTENSION: IS KETAMINE SAFE? 33
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
appeared refractory, and epinephrine was adminis-
tered to augment left ventricular output and coro-
nary flow. Ventricular tachycardia with hypotension
ensued shortly thereafter. The third case was a
1.8- year-old girl with mild PAH and congenital
heart disease who for uncertain reasons suddenly
developed pulseless electrical activity during cardiac
catheterization. All three patients survived to dis-
charge from hospital and were alive 5, 6, and
13 months later at last follow-up. The incidence of
hemodynamic instability requiring chest compres-
sions was 0.78% for cardiac catheterization proce-
dures, 10% for major surgical procedures and 1.6%
for all procedures.
Three infants did not survive to discharge from
hospital. One was a neonate with severe PAH
unresponsive to drug therapy who underwent
cardiac catheterization and was found to have
inoperable pulmonary vein stenoses. The following
day, the parents requested that medical support be
withdrawn, and the patient died soon thereafter.
A second infant with atrioventricular septal defect
had five procedures during an 80-day hospitaliza-
tion and died 14 days after the last procedure from
complications of PAH. The third infant had trisomy
21 syndrome and lung disease of prematurity (born
at 31 weeks gestational age) and died 17 days after
cardiac catheterization from respiratory failure with
sepsis. Postdischarge information was available for
65 patients. Median duration of follow-up was
27.7 months (range 0–66.3 months). Three deaths
occurred at 50, 121, and 612 days after hospital
discharge.
Factors associated with increased risk of compli-
cations (major + minor) when all 192 procedures
were included in the bivariate analysis were type of
procedure (major surgery) (P = 0.017; RR 3.03 (95%
CI 1.32–6.94), airway instrumentation with laryngeal
mask or endotracheal tube (P = 0.004; RR 1.53, 95%
CI 1.02–2.31), and opioid administration during
anesthesia (P < 0.001; RR 1.77, 95% CI 1.22–2.58).
Preprocedure vasodilator therapy (P = 0.012; RR
0.43, 95% CI 0.22–0.81) and propofol administration
during anesthesia (P = 0.01: RR0.82, 95% CI 0.58–
1.15) were associated with decreased risk of compli-
cations. Ketamine administration was not associated
with risk of complications (P = 0.963). Because the
patient’s airway was instrumented during all major
surgeries (the procedure group associated with
significantly increased risk) and propofol was only
administered during 1 (5%) major surgery, the
bivariate analysis was repeated with nonsurgery
cases only (n = 145). Factors associated with the
risk of complications (major + minor) were airway
instrumentation (P = 0.022; RR 1.55, 95% CI 0.92–
2.62) and opioid administration (P = 0.026; RR 1.97,
95% CI 1.14–3.40). Preprocedure vasodilator ther-
apy decreased the risk of complications (P = 0.004;
RR 0.46, 95% CI 0.23–0.92). Ketamine, propofol,
and volatile agents were not associated with
complications.
The multivariable logistic regression model dem-
onstrated the following factors to be independently
associated with complications (major + minor):
preprocedure vasodilator therapy (OR 0.31, 95% CI
0.13–0.70), major surgery (OR 3.1, CI 1.1–9.0). Keta-
mine was not significantly associated with compli-
cations (P = 0.36), neither were opioids, propofol nor
airway instrumentation.
Pulmonary vascular reactivity testing was per-
formed during 40 of the cardiac catheterizations, and
in these cases, the occurrence of complications (6, all
minor) did not differ between vasodilator respond-
ers and nonresponders.
Patients received ketamine and ⁄ or volatile anes-
thesia during 180 (93.8%) of all procedures.
To examine the hypothesis that volatile anesthesia
may mitigate the possible effect of ketamine to
increase PVR and the risk of adverse events, we
grouped these cases as follows: ketamine and no
volatile agents (Group K, n = 57); volatile agents and
no ketamine (Group V, n = 31); ketamine and vol-
atile agents (Group K + V, n = 92). The occurrence
of complications were Group K: minor 6 (10.5%),
major 0 (0%); Group V: minor 4 (12.9%), major 2
(6.5%); Group K + V: minor 10 (10.9%), major 7
(7.6%). The incidence of complications did not differ
between groups (P = 0.341). Again, to reduce the
influence of procedure type on complications, non-
surgery procedures were examined to test whether
the occurrence of complications (major + minor)
was influenced by the type of anesthetic agents
administered (Table 4). Occurrence of complications
was similar irrespective of the anesthetic drug
combination employed.
The peri-procedural care of PAH patients under-
going nonsurgical procedures was relatively
uniform. Therefore, these cases (n = 145) were
34 G.D. WILLIAMS ET AL.
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
regarded as one group in order to ascertain whether
there were patient characteristics or aspects of peri-
procedure management that differed between
patients that did and did not receive ketamine
(Table 5). Patients receiving ketamine were not
different than patients that did not receive ketamine
with regard to age, weight, diagnosis, and proce-
dure. More patients in the ketamine group tended to
have severe PAH (44% vs 28%, P = 0.062). Fewer
patients receiving ketamine had their airway instru-
mented (16% vs 69%, P < 0.001), more received
antisialogogue medications (22% vs 0%, P = 0.005)
and fewer were administered opioids (25% vs 74%,
P < 0.0001). Airway instrumentation was more
likely in younger patients (median 3.0 year vs
9.0 year, P < 0.001) and less likely in patients with
severe PAH (27% vs 48%, P = 0.035).
Discussion
The new findings of this retrospective study of
children with PAH who underwent anesthesia for
diagnostic and therapeutic procedures are as
follows: (i) ketamine administration is not associated
with increased complications, either when adminis-
tered as the sole anesthetic agent or when combined
with propofol or volatile anesthesia; (ii) rates for
cardiopulmonary resuscitation and mortality were
Table 4
Peri-procedural complications that occurred during nonsurgeryprocedures (n = 145), grouped according to the anesthetic drugsadministered
Anesthetic agents n
Complications
Minor Major All (%)
Ketamine only 10 1 0 1 (10)Ketamine + propofol 37 5 0 5 (13.5)Ketamine + volatile 17 1 1 2 (11.8)Propofol onlya 3 0 0 0 (0)Propofol + volatilea 14 2 0 2 (14.3)Volatile onlya 7 1 2 3 (42.9)Ketamine + propofol+ volatile
52 6 2 8 (15.4)
Other drugsb 5 0 0 0 (0)Totals 145 16 5 21 (14.5)
The occurrence of all complications did not between groups (chi-square test, P > 0.05). aData grouped together to permit statisticalanalysis. bUnable to include in the statistical analysis.
Table 5
A comparison between patients that did and did not receive ketamine anesthesia for nonsurgical procedures (n = 145)
Characteristic Ketamine (n = 116) No ketamine (n = 29) P value
Age at procedure (median, year) 8.0 6.4 nsWeight at procedure (median, kg) 23.2 19.0 nsCardiac catheterization 104 (89.7%) 24 (82.8%) nsOther nonsurgical procedure 12 (10.3%) 5 (17.2%) nsDiagnosis of congenital heart disease 33 (28.4%) 8 (27.6%) nsInvasive monitoring of systemic arterial blood pressure 18 (15.5%) 2 (6.9%) nsAirway instrumented (endotracheal tube or laryngeal mask) 25 (21.6%) 20 (69.0%) <0.001Premedication with midazolam 77 (66.4%) 17 (58.6%) nsInduction or maintenance with propofol 89 (76.7%) 17 (58.6%) nsInduction or maintenance with volatile agents 69 (59.5%) 21 (72.4%) nsOpiate administered 22 (19.0%) 18 (62.1%) <0.001Antisialogogue administered 26 (22.4%) 0 (0%) 0.005Intravenous introp administered 9 (7.8%) 0 (0%) nsComplication (minor + major) 16 (13.8%) 5 (17.2%) nsComplication requiring external cardiac compressions 1 (0.9%) 0 (0%) nsEmesis in the postanesthesia care unita 11 (13.6%) 3 (15.0%) nsAnti-emetic administered in postanesthesia care unitb 10 (12.3%) 4 (20.0%) nsPVR group: mild 27 (23.3%) 10 (34.5%) nsPVR group: moderate 37 (31.9%) 11 (37.9%) nsPVR group: severe 52 (44.8%) 8 (27.6%) nsSame day discharged home postprocedure 33 (28.4%) 7 (24.1%) nsSame day admission to intensive care unit postprocedure 26 (22.4%) 6 (20.7%) nsHospital stay (median, h) 24.0 36.8 ns
Data reported as n (%) unless otherwise stated. ns: No significant difference between groups (chi-squared test, P > 0.05). aInformationabout postprocedure nausea and emesis during the patient’s stay in the postanesthesia care unit was available for 101 of 145 cases of which81 received ketamine and 20 did not receive ketamine.
PULMONARY HYPERTENSION: IS KETAMINE SAFE? 35
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
lower than those previously reported for children
with PAH; (iii) peri-procedure risk factors included
major surgery, airway instrumentation and opioid
administration; (iv) during nonsurgical procedures,
exposure to airway instrumentation and opioid
administration was less likely when patients
received ketamine.
PAH was a predictor of perioperative death in
adult patients undergoing cardiac (9) and noncar-
diac surgery (10). In a retrospective study of
pediatric and adult patients with congenital heart
disease undergoing noncardiac surgery, PAH was a
predictor of perioperative morbidity (12). Similarly,
preoperative PAH was a significant risk factor for
postoperative in-hospital death in infants and chil-
dren undergoing open-heart surgery (14). Taylor
and colleagues studied 70 children with PAH who
underwent anesthesia and cardiac catheterization
and found a 5.7% risk of cardiac massage and
a mortality of 1.4% (15). Carmosino et al. (13)
reviewed 246 cardiac catheterization and noncardiac
surgical procedures in children with PAH and
noted an incidence of cardiac arrest of 2.1% and
a mortality rate of 1.4% for cardiac catheterization.
Our data for children undergoing cardiac catheter-
ization (cardiac arrest 0.8%, mortality 0%) were
encouraging and better than previous reports
(13,15), but they remain inferior to the 0.5% cardiac
arrest risk reported for all children with heart
disease who underwent cardiac catheterization
(23). A perioperative 30-day mortality of 8.5% after
cardiac surgery was reported for children at risk of
PAH (14), whereas 7.1% of our study patients
required cardiopulmonary resuscitation following
open-heart surgery and none died. Complications
occurred at all time phases during and after the
procedure. Exceptional vigilance throughout the
peri-procedural period is warranted for patients of
this high-risk group.
Baseline suprasystemic PAH has been reported to
be a significant predictor of major complications
(13). Our findings suggested pulmonary vasodilator
therapy ameliorated risk and perhaps this effect
explains why we found no association between
complications and severity of PAH. Airway instru-
mentation has been associated with life-threatening
or fatal escalation of pulmonary artery pressures
(25), and we found airway management was pre-
dictive of complications. Opioids can favorably
modify the adverse hemodynamic responses to
airway instrumentation, but they may also increase
PVR secondary to respiratory depression. In our
study, patients with PAH who underwent major
surgery were particularly challenging to manage.
Perturbations of homeostasis are quite frequent
during major surgery; they resulted in pulmonary
hypertensive crises in two study patients. Long
duration of anesthesia was predictive of morbidity
in adults with PAH (12).
The increased risk of perioperative complications
in patients with PAH is attributed largely to
the adverse consequences of PAH (8). Therefore,
the finding that ketamine was not associated with
increased risk of peri-procedural complications was
consistent with our previous report that ketamine (in
the presence of sevoflurane) did not increase PVR
in children with PAH (22). Additionally, the admin-
istration of volatile anesthetic agents and ⁄ or propo-
fol concomitantly with ketamine provided no
advantage over ketamine anesthesia alone with
regard to the occurrence of complications. In terms
of safety, ketamine appears to be an acceptable
option for children with PAH.
Patients who received ketamine during nonsur-
gical procedures were less likely to have their
airways instrumented. Our earlier work showed
that ketamine maintained PaO2 and did not alter
cardiac index, mean systemic arterial pressure,
arterial pH or PaCO2 in patients breathing sponta-
neously via their native airway. Respiratory effort
seemed relatively preserved (22). While this
anesthetic technique was safe and perhaps advan-
tageous with regard to airway manipulation and
PAH, we recommend meticulous care to avoid
hypoxia and hypercapnia, because these conditions
increase PVR. The opioid-sparing effect of ketamine
was anticipated because the drug has analgesic
properties.
This investigation has the limitations of a retro-
spective study; data may be incomplete or missing.
Fortunately, complications were entered real-time
into a database by the attending physicians provid-
ing care, thus reducing concern that important
complications were not included. Another limitation
was the relatively small number of procedures.
There may be inadequate statistical power to iden-
tify a significant association between some variables
and complications (Type II error).
36 G.D. WILLIAMS ET AL.
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37
References1 Galie N, Rubin LJ. Introduction: new insights into a chal-
lenging disease. A review of the Third World Symposium onPulmonary Arterial Hypertension. J Am Coll Cardiol 2003; 43:
1S.2 Simonneau G, Galie N, Rubin LJ et al. Clinical classification of
pulmonary hypertension. J Am Coll Cardiol 2004; 43: 5S–12S.3 Tulloh R. Management and therapeutic options in pediatric
pulmonary hypertension. Expert Rev Cardiovasc Ther 2006; 4:
361–374.4 Fischer LG, Van Aken H, Burkle H. Management of pulmo-
nary hypertension: physiological and pharmacologicalconsiderations for anesthesiologists. Anesth Analg 2003; 96:
1603–1616.5 Blaise G, Langleben D, Hubert B. Pulmonary arterial hyper-
tension: pathophysiology and anesthetic approach. Anesthesi-ology 2003; 99: 1415–1432.
6 Rashid A, Ivy D. Severe paediatric pulmonary hyperten-sion: new management strategies. Arch Dis Child 2005; 90:
92–98.7 Friesen RH, Williams GD. Anesthetic management of children
with pulmonary arterial hypertension. Pediatr Anesth 2008; 18:
208–216.8 MacKnight B, Martinez EA, Simon BA. Anesthetic manage-
ment of patients with pulmonary hypertension. Semin Cardio-thorac Vasc Anesth 2008; 12: 91–96.
9 Reich DL, Bodian CA, Krol M et al. Intraoperative hemo-dynamic predictors of mortality, stroke, and myocardialinfarction after coronary artery bypass surgery. Anesth Analg1999; 89: 814–822.
10 Ramakrishna G, Sprung J, Ravi BS et al. Impact of pulmonaryhypertension on the outcomes of noncardiac surgery. J Am CollCardiol 2005; 45: 1691–1699.
11 Robitaille A, Denault AY, Couture P et al. Importance of rela-tive pulmonary hypertension in cardiac surgery: the meansystemic-to-pulmonary artery pressure ratio. J CardiothoracVasc Anesth 2006; 20: 331–339.
12 Warner MA, Lunn RJ, O’Leary PW et al. Outcomes of non-cardiac surgical procedures in children and adults withcongenital heart disease. Mayo Clin Proc 1998; 73: 728–734.
13 Carmosino MJ, Friesen RH, Doran A et al. Perioperativecomplications in children with pulmonary hypertensionundergoing noncardiac surgery or cardiac catheterization.Anesth Analg 2007; 104: 521–527.
14 Bando K, Turrentine MW, Sharp TG et al. Pulmonary hyper-tension after operations for congenital heart disease: analysisof risk factors and management. J Thorac Cardiovasc Surg 1996;112: 1600–1609.
15 Taylor CJ, Derrick G, McEwan A et al. Risk of cardiac cathe-terization under anaesthesia in children with pulmonaryhypertension. Br J Anaesth 2007; 98: 657–661.
16 Heller AR, Litz RJ, Koch T. A fine balance, one-lung ventilationin a patient with Eisenmenger syndrome. Br J Anaesth 2004; 92:587–590.
17 Spotoft H, Horshin JD, Sorensen MB et al. The cardiovasculareffects of ketamine for induction of anesthesia in patients withvalvular heart disease. Can Anaesth Soc J 1979; 26: 463–467.
18 Berman W, Fripp RR, Rubler M et al. Hemodynamic effects ofketamine in children undergoing cardiac catheterization.Pediatr Cardiol 1990; 11: 72–76.
19 Wolfe RR, Loehr JP, Schaffer MS et al. Hemodynamic effects ofketamine, hypoxia and hyperoxia in children with surgicallytreated congenital heart disease residing greater than or equalto 1,200 meters above sea level. Am J Cardiol 1991; 67: 84–87.
20 Morray JP, Lynn AM, Herndon PS et al. Hemodynamic effectsof ketamine in children with congenital heart disease. AnesthAnalg 1984; 63: 895–899.
21 Hickey PR, Hansen DD, Cramolini GM et al. Pulmonary andsystemic hemodynamic responses to ketamine in infants withnormal and elevated pulmonary vascular resistance. Anesthe-siology 1985; 62: 287–293.
22 Williams GD, Philip BM, Chu LF et al. Ketamine does notincrease pulmonary vascular resistance in children with pul-monary hypertension undergoing sevoflurane anesthesia andspontaneous ventilation. Anesth Analg 2007; 105: 1578–1584.
23 Bennett D, Marcus R, Stokes M. Incidents and complicationsduring pediatric cardiac catheterization. Pediatr Anesth 2005;15: 1083–1088.
24 Galie N, Torbicki A, Barst R et al. Guidelines on diagnosis andtreatment of pulmonary arterial hypertension. The Task Forceon Diagnosis and Treatment of Pulmonary Arterial Hyper-tension of the European Society of Cardiology. Eur Heart J2004; 25: 2243–2278.
25 Burrows FA, Klinck JR, Rabinovitch M et al. Pulmonaryhypertension in children: perioperative management. CanAnaesth Soc J 1986; 33: 606–628.
Accepted 27 August 2009
PULMONARY HYPERTENSION: IS KETAMINE SAFE? 37
� 2009 Blackwell Publishing Ltd, Pediatric Anesthesia, 20, 28–37