My publication FH
-
Upload
independent -
Category
Documents
-
view
2 -
download
0
Transcript of My publication FH
Review Article
Congenital Fibular Deficiency
Abstract
Congenital fibular deficiency (CFD) is characterized by a widespectrum of manifestations ranging from mild limb length inequality(LLI) to severe shortening, with foot and ankle deformities andassociated anomalies. The etiology of CFD remains unclear.Treatment goals are to achieve normal weight bearing, a functionalplantigrade foot, and equal limb length. The recent Birch classificationsystem has been proposed to provide a treatment guide: thefunctionality of the foot, LLI, and associated anomalies should betaken into account for decision-making. Treatment options includeorthosis or epiphysiodesis, Syme or Boyd amputation and prostheticrehabilitation, limb lengthening procedures, and foot and anklereconstruction. The outcome of amputation for severe forms of CFDhas shown favorable results and fewer complications compared withthose of limb lengthening. Nevertheless, advances in the limblengthening techniquesmay change our approach to treating patientswith CFD and might extend the indications for reconstructiveprocedures to the treatment of severe LLI and foot deformities.
Although rare, congenital fibulardeficiency (CFD), also called
fibular hypoplasia and fibular hemi-melia, is the most common congen-ital long bone deficiency, withan approximate incidence of 7.4 to20 per 1 million live births.1 Theclinical presentation of CFD repre-sents a broad spectrum of manifes-tations, ranging from mild fibulardeficiency with limb length inequality(LLI) to a significantly short limbwith foot and ankle deformities.2-5
Patients may have other anomalies inthe hip and in the lower and upperextremities.6-8 Because of the widespectrum and pattern of this disorder,Stevens and Arms8 have proposedusing the term postaxial hypoplasiarather than fibular hypoplasia orfibular hemimelia.Successful management of CFD
aims to restore functional lower limbs.Although the management of mildCFD is generally straightforward, the
treatment of severe forms is contro-versial; several authors9-11 advocateearly amputation of the foot andprosthetic rehabilitation, whereasothers12,13 recommend limb salvage.
Etiology
The etiology of CFD remains unclear.Most cases are sporadic; however,chromosomal anomalies and autoso-mal dominant, autosomal recessive,and X-linked transmission have beenreported.6 Graham14 suggested thatexogenous vascular or mechanicalinterference with limb bud functionon the embryonic apical ectodermaledge might lead to CFD. Hootnicket al15 documented angiographicabnormalities of the vasculature inthree patients with CFD. Theseabnormalities included persistence ofthe embryonic vascular pattern, fail-ure of formation of the plantar arch,absence of the anterior tibial artery or
246 Journal of the American Academy of Orthopaedic Surgeons
Reggie C. Hamdy, MD, MSc,FRCSC
AsimM.Makhdom,MD,MSc (C)
Neil Saran, MD,MHSc (Clin Epi),FRCSC
John Birch, MD, FRCSC
From the Division of OrthopaedicSurgery, McGill University, Montreal,Quebec, Canada (Dr. Hamdy,Dr. Makhdom, and Dr. Saran), theDepartment of Orthopaedic Surgery,King Abdulaziz University, Jeddah,Saudi Arabia (Dr. Makhdom), and theDepartment of Orthopaedic Surgery,University of Texas SouthwesternMedical Center at Dallas and TexasScottish Rite Hospital for Children,Dallas, TX (Dr. Birch).
Dr. Hamdy or an immediate familymember serves as a board member,owner, officer, or committee memberof the Limb Lengthening andReconstruction Society. Dr. Saran oran immediate family member hasreceived research or institutionalsupport from DePuy. Dr. Birch or animmediate family member hasreceived royalties from Orthofix.Neither Dr. Makhdom nor anyimmediate family member hasreceived anything of value from or hasstock or stock options held ina commercial company or institutionrelated directly or indirectly to thesubject of this article.
J Am Acad Orthop Surg 2014;22:246-255
http://dx.doi.org/10.5435/JAAOS-22-04-246
Copyright 2014 by the AmericanAcademy of Orthopaedic Surgeons.
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
absence of the normal trifurcation ofthe popliteal artery at the level of theknee, and the presence of one largeposterior artery in the leg. Lewin andOptiz6 introduced the theory ofdevelopmental fields defect, in whichthe fibula is hypothesized to controlthe development of the lateral footrays, anterior cruciate ligament (ACL),patella, proximal femur, acetabulum,and pubic bone, and the tibia controlsthe development of the hallux anddistal femur. A developmental defectin the fibular field will result in fibulardeficiency and may affect the otherfield components, as seen in patientswith CFD. Although CFD has his-torically been considered to be a lat-eral deficiency, Hootnick16 has arguedthat CFD is, in fact, a midline defect,based on the dissection of four footspecimens of congenitally short-limbedpatients (Figure 1).
Clinical Features
CFD is usually apparent at birth andcan vary from mild limb inequalitiesand asymmetry to severe shortening,with a wide range of associated anom-alies (Figure 2). Bilateral involvementis not uncommon, with a reportedprevalence of 9% to 52%.3,6,9,11,17-19
The incidence of CFD appears tobe predominant in males (male:female ratio, 2:1). However, in somereports, the incidence of CFD is morecommon in females.3,6,8,9,17-20 Thepatient’s history should includea detailed history of pregnancy,including such factors as smokingand the use of alcohol and anyteratogenic medications. The historyof labor and birth, developmentalmilestones, associated anomalies, andfamily history, including congenitalorthopaedic conditions, should be
obtained. A thorough physicalexamination is warranted to assessthe involved limb and to look forassociated anomalies.Most patients with a complete CFD
present with anterior or anteromedialbowing of the tibia; half of thesepatients typically have a skin dimple atthe apex of the deformity (Figure 3).Sixty percent of patients with completeCFD have a palpable posterior band(ie, fibular anlage), representing a fi-brocartilaginous fibular remnant.7,17
This anlage produces tethering effectsthat lead to tibial bowing.Upper extremity involvement
ranges from syndactyly to extensivedeficiencies.3,17 Birch et al3 notedthat patients with bilateral CFD havea higher incidence of upper extremityanomalies.Congenital shortening of the femur
and proximal focal femoral deficiency
Figure 1
AP radiograph of the right foot ofa 15-year-old boy demonstrating footdeficiency of multiple rays.
Figure 2
Skeletal diagram of a 13-year-old child demonstrating the associated anomaliesof congenital fibular deficiency.
Reggie C. Hamdy, MD, MSc, FRCSC, et al
April 2014, Vol 22, No 4 247
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
are widely recognized anomaliesassociated with CFD.3,7,8,20 Theseanomalies will add to the overall LLI.The magnitude of femoral shorteningand the severity of fibular deficiencydo not appear to correlate.17,18 Distallateral femoral hypoplasia is reportedin up to 93% of patients with CFD.20
Knee abnormalities include genuvalgum, ACL deficiency, patellaalta, and hypoplastic patella.5,8 Rouxand Carlioz21 reported in a case seriesthat 95% of 69 patients had ACL
deficiency and that 60% had posteriorcruciate ligament deficiency. Interest-ingly, only 16% of these patients re-ported instability symptoms. Severalauthors have postulated the presenceof adaptive stabilizers.1,22,23 Based onarthroscopic findings of four patientswith CFD, Gabos et al22 found thatCFDpatients with ACL deficiency hada hypertrophied ligament of Hum-phrey; the authors hypothesized thatthis ligament may contribute to thestability of the knee.
Foot and ankle abnormalities includeequinovalgus deformities (equinovarusis less frequent), missing feet rays, andankle instability.9,24 Tarsal coalition inCFD has been reported,8,17,20,25 withtalocalcaneal fusion being the mostcommon type.17,25,26 Interestingly,tarsal coalition was found to be morefrequent in children with missing lat-eral foot rays than in those with nor-mal feet.26 In older children, sphericalarticulation between the talus and tibia(ie, ball-and-socket ankle deformity)may be seen.7,8 The etiology of thisdeformity remains unclear, with someauthors27 suggesting that it is con-genital in origin, whereas others28 feelthat it is an adaptive change secondaryto the tarsal coalition.
Classification
Several classification systems havebeen proposed, including those ofAchtermanandKalamchi17 (Table 1),Letts and Vincent,29 Coventry andJohnson,2 and Stanitski and Sta-nitski.18 However, most of theseclassifications are anatomic andbased on radiographic features.Although they are useful descriptiveclassifications, they provide limitedguidance in terms of prognosis andtreatment. Recently, Birch et al3
proposed a new classification systemthat takes into consideration thefunctionality of both the foot and theupper extremities as well as the per-centage of LLI.3 It consists of twocategories based on the functionalityof the foot: type 1, in which the foot ispreservable, and type 2, in which thefoot is not preservable. The pre-servability of the foot is based on thenumber of foot rays present. At leastthree rays should be present for a footto be considered as salvageable,whereas those with fewer than threerays are considered nonsalvageable.Furthermore, type 1 fibular hemi-
melia is subdivided into four groupsbased on the percentage of overall
Figure 3
Clinical photographs of a 13-month-old boy with a 15% limb length inequality.A, Front view demonstrating typical findings associated with congenital fibulardeficiency, including a shortened femur, shortened tibia, skin dimple over thebow of the tibia, and deficient foot rays.B, Side view demonstrating anterior tibialbowing. (Photographs courtesy of Charles E. Johnston, MD, Dallas, TX.)
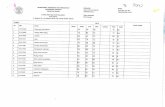
Table 1
Achterman and Kalamchi17 Classification System for Congenital FibularDeficiency
Type Description
IA Fibula is present. Proximal fibular epiphysis is distal to the level of thetibial growth plate. The distal fibular growth plate is proximal to thedome of the talus.
IB Partial absence of the fibula. The fibula is absent for 30% to 50% ofits length proximally. Distally, the fibula is present but does notsupport the ankle.
II Complete absence of the fibula
Congenital Fibular Deficiency
248 Journal of the American Academy of Orthopaedic Surgeons
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
LLI compared with the contralateralside: type 1A, none to ,6% overallshortening; type 1B, 6% to #10%overall shortening; type 1C, 11% to,30% overall shortening; and type1D, $30% overall shortening. Type2 fibular hemimelia is subdividedinto two groups based on the func-tionality of the upper extremities:type 2A, functional upper extremi-ties, and type 2B, nonfunctionalupper extremities. Birch et al3 out-lined a treatment guide with regardto each group in the classificationscheme (Figure 4). The authorsacknowledged that, in regard todecision making, surgeons andfamily must all be involved in thetreatment plan; they further empha-sized that not all five-rayed feetshould be preserved, and not all two-rayed feet should be ablated.3
Imaging
Typically, the diagnosis of CFD ismade after birth. However, prenatalultrasonographic diagnosis has beenreported.30 Themainstay of diagnosis,
in addition to clinical findings, is plainradiography. Plain radiographs of thetibia and fibula can demonstrate tibialbowing and partial or completeabsence of the fibula (Figure 5). If thefibula is present, the proximal fibularepiphysis might be distal to the tibialgrowth plate, and the distal fibulargrowth plate might be proximal to thedome of the talus.17 However, Searleet al4 identified 14 patients (16 limbs)who had had clinical findings of CFDwith radiographically normal fibula.The authors suggested that these pa-tients represent a mild subset of CFD.AP radiographs of the lower
extremities are warranted to evaluateassociated limb pathologies, includ-ing acetabular dysplasia, proximalfemoral deficiency, distal hypoplasticlateral femoral condyle, and mal-alignmentof the lower limbs.RouxandCarlioz21 reported that plain radio-graphs might demonstrate an absenttibial spine in 92% of patients withCFD who had ACL deficiency. Inaddition to looking for associatedanomalies, the AP radiographs, withblocks to accommodate the LLI,enable evaluation and quantification
of the LLI. CT scanography is anotherreliable method used to quantify LLI.MRI is a useful modality to evaluate
knee abnormalities only in patientswith symptomatic instability. MRI isalso useful to assess for both intra-articular and extra-articular kneepathology. Common findings are anabsent ACL, absent menisci, attenu-ated muscles, and absent muscles.31
MRI or ultrasonography of the feetcan also be beneficial for diagnosingtarsal coalitions. Grogan et al25 dis-sected 26 feet known to have CFD,proximal focal femoral deficiency,or both. Of these, 54% had tarsalcoalitions upon dissection, only 15%ofwhichwere detected on preoperativeradiographs. Plain radiographylikely underdiagnosed these coali-tions because they were completelycartilaginous or fibrous in nature.7,25
However, MRI is rarely indicatedunless some form of reconstructionfor these coalitions is planned.
Management Goals
Treatment of CFD is challenging. Theprimary problems in CFD are the LLI,
Figure 4
Algorithm illustrating the proposed management guidelines of Birch et al3 for congenital fibular deficiency. LLI = limb lengthinequality
Reggie C. Hamdy, MD, MSc, FRCSC, et al
April 2014, Vol 22, No 4 249
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
foot deformity, and ankle instability.The goals of management are toachievenormalweightbearing, normalgait, and equal limb length. In cases ofbilateralCFD, the overall shorteningofboth limbs should be considered.Traditionally, management of CFD
was based on the severity of the fibularinvolvement and LLI.2,17,29 Thisapproach has changed. Stanitski andStanitski18 and Birch et al3 haveemphasized the critical importance ofbasing treatment on the functionalityof the foot and the LLI; treatmentshould not be based solely on thefibular morphology and the degree ofLLI. Furthermore, treatment should
be individualized for each patient. Amultidisciplinary team, including thesurgeon, occupational and physicaltherapists, orthotist, prosthetist, socialworker, and pediatric psychologist,can be beneficial.
Management of LimbLength Inequality
Orthosis and EpiphysiodesisOptimal candidates for an orthosistypically are patients with mild formsof CFD, a functional plantigradefoot, and mild (,6%) LLI.3 Thesepatients can be managed successfullywith shoe lifts and foot orthoses. It isimportant to consider the predictedfinal LLI at skeletal maturity becausetimed contralateral epiphysiodesismay be performed to achieve limblength equality. Generally, in mostpatients with congenital limb anom-alies, the percentage of LLI remainsconstant. Birch et al3 showed that82.5% of patients with CFD followa linear growth-inhibition pattern.However, because not all patientsfollow this pattern,32 an LLI pre-diction must be done with care.Nonetheless, the percentage of LLIcan be used as a rough guide toestimating final LLI.
Limb Lengthening andEpiphysiodesis VersusAmputationThe decision to manage patients withCFD by amputation or limb length-ening is a matter of debate. In general,patients with severe foot deformity (ie,three or more absent rays) and a pre-dicted LLI of $30% at the age ofskeletal maturity, or .5 cm of dis-crepancy at birth, are candidates foramputation and prosthetic rehabili-tation;5,33,34 those with less severefoot deformities (ie, three or morepresent rays) and a predicted LLI of,30% are candidates for limblengthening procedures (Figure 6).
Foot preservation should be consid-ered in all patients with nonfunctionalupper extremities.3 Regardless of thechoice of treatment, however, surgicalintervention should be implementedwhen the patient is young (ideally atthe beginning of walking age) inorder to achieve good results andavoid complications.19,33,35,36 Wehave found that allowing the patient’sfamily to visit both reconstructive andprosthetic clinics is invaluable inenabling a more informed decision.
Amputation
Both the Syme and Boyd amputationhave been used widely to treatpatients with CFD. Syme amputationis an ankle disarticulation performedwithout disturbing the distal tibialepiphysis in order to establish a flatsurface that is covered by the heelpad.37 The disadvantage of thistechnique is that the heel pad canmigrate posteriorly from the distalresidual stump. However, manyauthors agree that this heel padmigration is not problematic forthe patient and does not affect pros-thetic fitting.33 Furthermore, long-term follow-up data have shown thatpatients who have undergone a Symeamputation were able to achieve theirpersonal goals, were very functional,and did not differ from the norm interms of occupational satisfaction,personal growth, and relationshipswith family members and peers.33
The Boyd amputation is also anankle disarticulation, but in this pro-cedure, the calcaneus is retained to befused to the distal tibia.38 This tech-nique prevents heel pad migrationand can add to the overall limblength. Both types of amputation haveadvocates, and they are used inter-changeably in many institutions.38
To avoid interference with thenormal developmental milestones ofthe child, amputation should be per-formed at the time the child starts
Figure 5
Lateral right tibial radiographdemonstrating complete absence ofthe fibula and anterior tibial bowing inan infant with congenital fibulardeficiency.
Congenital Fibular Deficiency
250 Journal of the American Academy of Orthopaedic Surgeons
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
attempts to walk (eg, by pullinghimself or herself up to stand or byholdingonto furniture).33 Timing theamputation in this way permits goodprosthetic fitting by the time thechild is walking without support.In some patients, the residual stump
following amputation might be tooshort or deformed for satisfactoryprosthetic fitting. In these instances,lengthening the residual stump orcorrecting the deformity might beconsidered. We have found that dis-
cussing such cases with the pros-thetist is beneficial in anticipatingthe patient’s personal adjustmentfollowing surgery.Fulp et al39 have advocated for the
excision of the fibular anlage at thetime of amputation in order toeliminate the tethering effect andprevent tibial bowing. They alsohave performed diaphyseal osteot-omy in patients who had an existingbow in order to improve alignmentand prosthetic fitting. However,
many authors do not advocate tibialosteotomy at the time of amputation;they feel that, when necessary, thisproblem can be dealt with by pros-thetic adjustments.One major problem with amputa-
tion is that parents may be reluctantto approve such irreversible inter-vention. Letts and Vincent29 identi-fied the reasons for apprehensionas parental denial of the naturalhistory of CFD, an acceptable footappearance and shape at the time
Figure 6
A 15-year-old boy with congenital fibular deficiency. The same patient as in Figure 1. A, Standing AP radiograph. Thepatient is standing on a 6-cm block under the right foot, documenting a total functional discrepancy of approximately 6 cm.Note the ipsilateral mild shortening of the femoral neck and shaft, valgus deformity of the right distal femur, tibialshortening, and disproportionate fibular shortening. B, Postoperative AP radiograph after medial distal femoralhemiepiphysiodesis. Note the medial bow of the midshaft tibia and the ball-and-socket ankle joint. C, Postoperative APradiograph of the patient in a circular fixator for tibial lengthening. A proximal tibial osteotomy has been performed, withacute correction of the mild tibial valgus bow deformity. A small segment of fibula has been removed to prevent itspremature consolidation. D, Standing AP radiograph after 1 year of tibial lengthening. There is small residual valgusdeformity of the leg and leg length inequality.
Reggie C. Hamdy, MD, MSc, FRCSC, et al
April 2014, Vol 22, No 4 251
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
of decision making, and—mostimportantly—a desire for the child toparticipate in the decision-makingprocess. Therefore, discussion withthe parents is required to explainclearly the consequences of theamputation and the other treatmentalternatives. Naudie et al9 suggestedthat surgeons explain to families thatthe amputation is a reconstructiveprocedure in this context and is notconsidered a failure of treatment.
Limb Lengthening
Distraction osteogenesis has beenused widely to lengthen and correctthe deformities in patients with CFD.In severe cases, multiple lengtheningstypically are required to achieve limblength equalization.9,34 Numerouslengthening strategies have beendescribed.9,13,19,36 However, no suf-ficient data are available to establishthe superiority of one strategy overanother.In our experience, patients with
CFD require at least two separatesessions of lengthening. The first ses-sion is performed when the limblength discrepancy reaches 5 to 6 cm;the second lengthening takes placeduring adolescence when the dis-crepancy reaches 7 cm. Interestingly,Griffith et al40 found no difference inthe rate of complications betweenthe first and second lengthenings.However, many authors agree thatthe rate of complications increasessignificantly when the limb segmentsare lengthened.15% to 20%.3,11,41
In some patients, a complementarycontralateral epiphysiodesis might berequired to lessen theLLI.Furthermore,a final lengthening can be performed atskeletal maturity to correct LLI pre-dictionerrors. Inpatientswithcompleteabsence of the fibula, some authorshave emphasized the importance ofearly (ie, at the end of the first year oflife) excision of the fibular anlage withthe first sessionof lengthening.19,36 The
anlage resection should minimize thetethering effect and therefore minimizethe occurrence of tibial angulation.
Treatment of Genu Valgus
It was noted that two factors corre-late to the degree of genu valgum:the degree of distal lateral femoralhypoplasia and the tibial angulation(ie, apex anterior and medial).42
These factors increase the compres-sive loads on the lateral knee com-partment. According to the Heuter-Volkmann principle, compressionforces at the physis can cause physealgrowth inhibition.43 Thus, moresevere angular deformity leads togreater compression and thereforemore inhibition of growth.The genu valgus deformity in these
patients interferes with the normal gaitpattern and causes problems withprosthetic fitting for those whoundergo amputation. Treatment isbased on the severity of the deformity.Distal medial physeal stapling of thefemur or proximal tibia can be per-formed for mild deformities; patientswith a tibiofemoral angle.15� can bemanaged with distal femoral or prox-imal tibial osteotomies.42 However,high recurrence rate of the deformitywas reported after the osteotomywhenthe procedure was performed outsidethe setting of limb lengthening.42
Therefore, it is recommended that os-teotomies be done after the age ofskeletal maturity or be done to correctthe deformities simultaneously withlengthening procedures.Angular deformities of the knee also
can occur in patients with CFD whowere treated by amputation. The eti-ology of these deformities is unknown;the cause might be secondary to theabnormal load on the proximal tibialgrowth plate as a result of the Heuter-Volkmann principle.44 In such cir-cumstances, hemiepiphysiodesis of theproximal tibial physeal growth plateprovides reliable correction.45
Treatment of KneeInstability
Knee instability in patients with CFDis mainly related to the congenitalabsence of the ACL.21,23 Becausemost of these patients have nosymptomatic reports of instability ofthe knee, many authors suggestedthat ACL reconstruction in thesepatients is unwarranted.1 Interest-ingly, Crawford et al1 objectivelyreassessed the long-term outcome forpatients who had had deficient ACLsand found no significant differencein Medical Outcomes Study 36-ItemShort Form scores compared withthe age-matched group. The authorsnoted that these patients have veryfunctional lives and that most ofthem were engaged in demandingsporting activities, such as skiing,baseball, and football. Nevertheless,ACL reconstruction has been reportedfor these patients. Gabos et al22 re-constructed four symptomatic patientsafter skeletal maturity by using tendonallograft and interference screw fixa-tion; these authors reported goodoutcomes on short-term follow-up.In our opinion, the management of
the deficient ACL should be based onpatient symptoms and functionaldemand. It is critical to be aware thatmost patients with CFD have a defi-cient ACL and that close monitoringis required when lengthening limbswith unstable joints.
Foot and AnkleReconstruction
The absence of the lateral fibularmalleolus, tight lateral fibular anlage,tight Achilles tendon, and wedge-shaped distal tibial epiphysis results ina lack of posterolateral hindfoot sup-port and contributes to equinovalgusdeformity of the foot and ankle insta-bility in patients with CFD.17,37,46
These anatomic abnormalities worsensignificantly and become problematic
Congenital Fibular Deficiency
252 Journal of the American Academy of Orthopaedic Surgeons
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
in patients who undergo limblengthening.10,13,46 Many surgicalprocedures have been described toachieve a plantigrade foot with a sta-ble ankle joint. Soft-tissue balancingwith reconstruction of the lateralmalleolus by free bone grafts has beenreported.47 However, this technique islimited because the transplantationgrafts fail to grow as the child grows;therefore, deformity recurs.Transplantation of vascularized
fibular head graft from the contra-lateral side has also been reported.48
However, the morbidity of the nor-mal (ie, donor) side was considereda major limitation of this technique.Thomas and Williams47 describeda longitudinal oblique tibial split(ie, Gruca procedure) done to pro-vide the talus a lateral buttress. Thedrawback of this procedure is thepotential growth arrest of the distaltibial physis. In a case report, Weberet al49 described the use of triangulariliac crest graft implantation withannexing apophysis and glutealfascia to cover the lateral talus. Thisimplantation was fixed by a circularfixator; at 2-year follow-up, thepatient had good results.However, none of these techniques
addressed the problem of the wedge-shaped distal tibial epiphysis untilExner50 described an osteotomy ofthe distal tibial metaphysis per-formed to bend the posterolateralthird of the distal tibial epiphysis,thus forming a concave distal tibialjoint surface. On short-term follow-up, the three patients who weretreated with this technique hadplantigrade feet with stable ankles.Recently, El-Tayeby and Ahmed51
have shown that posterolateral soft-tissue release of the ankle, excision ofthe fibular anlage, division andrealignment of the talocalcanealcoalition (when present), andadvancing the cartilaginous fibularanlage distally, followed by fixing itto the tibia with two Kirschner wires,can recreate the ankle mortise. All 13
patients in their case series haveshown favorable results on short-term follow-up. In addition, manyauthors have suggested performingankle arthrodesis as a last resort inthese patients.Although some of these studies
demonstrated good results in theshort term, the long-term outcomesare not known and are difficult topredict. In our opinion, Syme or Boydamputation should be considered thebest available treatment of such pa-tients. However, when the parentsrefuse this option, these reconstruc-tive procedures may be considered asalternatives.
Outcomes andComplications
Several studies have compared thelong-term outcomes of amputationwith those of limb preservation andlengthening.9-11,52 Walker et al52 ina retrospective review objectivelyevaluated those who had hadamputation (36 patients) versuslengthening (26 patients) and foundthat children who had undergoneamputation scored better on a jobsatisfiers content scale, had fewerdays of hospitalization, and under-went fewer procedures. Choi et al10
and Naudie et al9 also noted thatpatients who were treated byamputation had lower readmissionrates, fewer complications, andbetter function compared withthose who underwent lengthening.McCarthy et al11 repeated these re-sults in 25 patients who were treatedeither by amputation or lengthening.These studies, however, were lim-
ited by the heterogeneity between thecomparison groups. This heteroge-neitymay be related to thewide rangeof clinical presentations in CFDpatients; therefore, it might be diffi-cult to provide matched-groupscomparisons. Interestingly, however,these studies shared one common
finding: the patients who underwentamputation had had severe forms ofCFD with foot deformities comparedwith those who underwent limblengthening.9-11,52
In contrast, several authors haveargued that recent improvementsin limb lengthening techniquesshould be used as an alternative toamputation.19,35,53 El-Sayed et al19
showed favorable results by means ofIlizarov limb lengthening in a caseseries of 157 patients (180 limbs) whowere classified as having Achter-man-Kalamchi type II CFD. Theauthors’ opinion is that if the limbcan be rapidly and reliably length-ened, then amputation should notbe an option. Zarzycki et al53
suggested that, despite the high rateof complications, limb lengtheningand foot deformity correctionsmight be an alternative to ampu-tation. Gibbons and Bradish35 haveachieved the desired limb length-ening and foot deformity correc-tions by using the Ilizarov methodin 10 patients who had had severeforms of CFD. Miller and Bell12
repeated these results in 12lengthenings. However, one majorlimitation of these studies is that noamputation group was included bywhich to make an objective com-parison with the lengthening groupin terms of functional outcome.Without doubt, the rate of compli-
cation associated with limb length-ening and the need for multipleprocedures are limiting factors whencompared with amputation (Table 2).Nevertheless, future advances in limblengthening techniques might expandthe indications for these reconstructiveprocedures.
Summary
The goal of managing CFD is toachieve normal weight bearing andnormal gait and limb length. Man-agement should be based on the
Reggie C. Hamdy, MD, MSc, FRCSC, et al
April 2014, Vol 22, No 4 253
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
percentage of LLI, the functionality ofthe foot, and the associated anomalies.Discussion with the parents of thepatient is required to reviewthebenefitsand perceived drawbacks of availabletreatment options. Patients with non-functional feet are ideal candidates forSyme or Boyd amputation; those withfunctional feet are candidates for limblengthening procedures. Limb preser-vation should be considered for thosewith nonfunctional upper extremities.Furthermore, limb lengthening andfoot/ankle reconstruction proceduresshould be used as an alternative inthose patients or for those familieswhorefuse amputation.Genu valgus of the knee can be
managedwithstaplingordistal femoralor proximal tibial osteotomies, or canbe treated simultaneously with limblengthening procedures. Tibial bowingcan be corrected simultaneously iflimb lengthening is planned; however,many authors do not advocate tibialosteotomy in patients who will betreated by amputation. Treatment ofthe knee instability is generallyunwarranted and should be based onpatient symptoms and functionaldemand. Finally, further advances in
limb lengthening devices and tech-niques may change the treatmentapproach of patients with CFD andmight extend the indications of thereconstructive procedures to treatsevere LLI and foot deformities.
References
Evidence-based Medicine: Levels ofevidence are described in the table ofcontents. In this article, references9-11, 32, 40, and 52 are level IIIstudies. References 1-5, 8, 12, 13, 15-29, 31, 33-35, 37, 39, 41, 42, 44-47,49-51, and 53 are level IV studies.References 6, 7, 14, 30, 36, 38, 43,and 48 are level V expert opinion.
References printed in bold type arethose published within the past5 years.
1. Crawford DA, Tompkins BJ, Baird GO,Caskey PM: The long-term function of theknee in patients with fibular hemimelia andanterior cruciate ligament deficiency.J Bone Joint Surg Br 2012;94(3):328-333.
2. Coventry MB, Johnson EW Jr: Congenitalabsence of the fibula. J Bone Joint Surg Am1952;34(4):941-955.
3. Birch JG, Lincoln TL, Mack PW,Birch CM: Congenital fibular deficiency:
A review of thirty years’ experience atone institution and a proposedclassification system based on clinicaldeformity. J Bone Joint Surg Am 2011;93(12):1144-1151.
4. Searle CP, Hildebrand RK, Lester EL,Caskey PM: Findings of fibular hemimeliasyndrome with radiographically normalfibulae. J Pediatr Orthop B 2004;13(3):184-188.
5. Maffulli N, Fixsen JA: Management offorme fruste fibular hemimelia. J PediatrOrthop B 1996;5(1):17-19.
6. Lewin SO, Opitz JM: Fibular a/hypoplasia:Review and documentation of the fibulardevelopmental field. Am JMed Genet Suppl1986;2:215-238.
7. Fordham LA, Applegate KE, Wilkes DC,Chung CJ: Fibular hemimelia: More thanjust an absent bone. Semin MusculoskeletRadiol 1999;3(3):227-238.
8. Stevens PM, Arms D: Postaxial hypoplasiaof the lower extremity. J Pediatr Orthop2000;20(2):166-172.
9. Naudie D, Hamdy RC, Fassier F, Morin B,Duhaime M: Management of fibularhemimelia: Amputation or limblengthening. J Bone Joint Surg Br 1997;79(1):58-65.
10. Choi IH, Kumar SJ, Bowen JR: Amputationor limb-lengthening for partial or totalabsence of the fibula. J Bone Joint Surg Am1990;72(9):1391-1399.
11. McCarthy JJ, Glancy GL, Chnag FM,Eilert RE: Fibular hemimelia: Comparisonof outcome measurements after amputationand lengthening. J Bone Joint Surg Am2000;82(12):1732-1735.
12. Miller LS, Bell DF: Management ofcongenital fibular deficiency by Ilizarovtechnique. J Pediatr Orthop 1992;12(5):651-657.
13. Catagni MA, Radwan M, Lovisetti L,Guerreschi F, Elmoghazy NA: Limblengthening and deformity correction bythe Ilizarov technique in type III fibularhemimelia: An alternative to amputation.Clin Orthop Relat Res 2011;469(4):1175-1180.
14. Graham JM Jr: Limb anomalies asa consequence of spatially-restrictinguterine environments. Prog Clin Biol Res1983;110(pt A):413-422.
15. Hootnick DR, Levinsohn EM, Randall PA,Packard DS Jr: Vascular dysgenesisassociated with skeletal dysplasia of thelower limb. J Bone Joint Surg Am 1980;62(7):1123-1129.
16. Hootnick D: Midline metatarsal dysplasiais the Rosetta stone of embryonicdysvasculogenesis. Birth Defects ResearchPart A: Clinical and Molecular Teratology2010;88(5):385.
Table 2
Reported Complications After Amputation or Limb Lengthening in PatientsWith Congenital Fibular Deficiency9,11,34,40,41
Procedure Complications
Syme amputation Posterior migration of the heel padReformation of the calcaneus (ie, painful stump)Wound infectionHeel pad sloughFitting adjustment problems
Boyd amputation Delayed calcaneotibial fusion or nonunionCalcaneal migration and malalignmentWound infection
Limb lengthening Pin tract infectionsPeroneal nerve injuryTibial/femoral fracturesSevere depressionNonunion of the osteotomy siteJoint stiffnessJoint subluxationPersistent or recurrence of knee and foot deformitiesResidual limb length inequality
Congenital Fibular Deficiency
254 Journal of the American Academy of Orthopaedic Surgeons
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
17. Achterman C, Kalamchi A: Congenitaldeficiency of the fibula. J Bone Joint Surg Br1979;61(2):133-137.
18. Stanitski DF, Stanitski CL: Fibularhemimelia: A new classification system.J Pediatr Orthop 2003;23(1):30-34.
19. El-Sayed MM, Correll J, Pohlig K: Limbsparing reconstructive surgery and Ilizarovlengthening in fibular hemimelia ofAchterman-Kalamchi type II patients.J Pediatr Orthop B 2010;19(1):55-60.
20. Rodriguez-Ramirez A, Thacker MM,Becerra LC, Riddle EC, Mackenzie WG:Limb length discrepancy and congenitallimb anomalies in fibular hemimelia.J Pediatr Orthop B 2010;19(5):436-440.
21. RouxMO, Carlioz H: Clinical examinationand investigation of the cruciate ligamentsin children with fibular hemimelia. J PediatrOrthop 1999;19(2):247-251.
22. Gabos PG, El Rassi G, Pahys J: Kneereconstruction in syndromes withcongenital absence of the anterior cruciateligament. J Pediatr Orthop 2005;25(2):210-214.
23. Kaelin A, Hulin PH, Carlioz H: Congenitalaplasia of the cruciate ligaments: A reportof six cases. J Bone Joint Surg Br 1986;68(5):827-828.
24. Maffulli N, Fixsen JA: Fibular hypoplasiawith absent lateral rays of the foot. J BoneJoint Surg Br 1991;73(6):1002-1004.
25. Grogan DP, Holt GR, Ogden JA:Talocalcaneal coalition in patients who havefibular hemimelia or proximal femoral focaldeficiency: A comparison of the radiographicand pathological findings. J Bone Joint SurgAm 1994;76(9):1363-1370.
26. Caskey PM, Lester EL: Association offibular hemimelia and clubfoot. J PediatrOrthop 2002;22(4):522-525.
27. Pappas AM, Miller JT: Congenitalball-and-socket ankle joints and relatedlower-extremity malformations. J BoneJoint Surg Am 1982;64(5):672-679.
28. Takakura Y, Tamai S, Masuhara K:Genesis of the ball-and-socket ankle. J BoneJoint Surg Br 1986;68(5):834-837.
29. Letts M, Vincent N: Congenitallongitudinal deficiency of the fibula (fibularhemimelia): Parental refusal of amputation.Clin Orthop Relat Res 1993;287:160-166.
30. Pauleta J, Melo MA, Graça LM: Prenataldiagnosis of a congenital postaxiallongitudinal limb defect: A case report.Obstet Gynecol Int 2010;2010:825639.
31. Laor T, Jaramillo D, Hoffer FA, Kasser JR:MR imaging in congenital lower limbdeformities. Pediatr Radiol 1996;26(6):381-387.
32. Szoke G, Mackenzie WG, Domos G,Berki S, Kiss S, Bowen JR: Possiblemistakes in prediction of bone maturationin fibular hemimelia by Moseley chart. IntOrthop 2011;35(5):755-759.
33. Birch JG, Walsh SJ, Small JM, et al: Symeamputation for the treatment of fibulardeficiency: An evaluation of long-termphysical and psychological functionalstatus. J Bone Joint Surg Am 1999;81(11):1511-1518.
34. Changulani M, Ali F, Mulgrew E, Day JB,Zenios M: Outcome of limb lengthening infibular hemimelia and a functional foot.J Child Orthop 2010;4(6):519-524.
35. Gibbons PJ, Bradish CF: Fibular hemimelia:A preliminary report on management of thesevere abnormality. J Pediatr Orthop B1996;5(1):20-26.
36. Patel M, Paley D, Herzenberg JE: Limb-lengthening versus amputation for fibularhemimelia. J Bone Joint Surg Am 2002;84(2):317-319.
37. Westin GW, Sakai DN, Wood WL:Congenital longitudinal deficiency of thefibula: Follow-up of treatment by Symeamputation. J Bone Joint Surg Am 1976;58(4):492-496.
38. Krajbich JI: Lower-limb deficiencies andamputations in children. J Am AcadOrthop Surg 1998;6(6):358-367.
39. Fulp T, Davids JR, Meyer LC,Blackhurst DW: Longitudinal deficiency ofthe fibula: Operative treatment. J BoneJoint Surg Am 1996;78(5):674-682.
40. Griffith SI, McCarthy JJ, Davidson RS:Comparison of the complication ratesbetween first and second (repeated)lengthening in the same limb segment.J Pediatr Orthop 2006;26(4):534-536.
41. Velazquez RJ, Bell DF, Armstrong PF,Babyn P, Tibshirani R: Complications ofuse of the Ilizarov technique in thecorrection of limb deformities in children.J Bone Joint Surg Am 1993;75(8):1148-1156.
42. Boakes JL, Stevens PM, Moseley RF:Treatment of genu valgus deformity incongenital absence of the fibula. J PediatrOrthop 1991;11(6):721-724.
43. Saran N, Rathjen KE: Guided growth forthe correction of pediatric lower limbangular deformity. J Am Acad Orthop Surg2010;18(9):528-536.
44. Ranade A, McCarthy JJ, Davidson RS:Angular deformity in pediatric transtibialamputation stumps. J Pediatr Orthop2009;29(7):726-729.
45. Gyr BM, Colmer HG IV, Morel MM,Ferski GJ: Hemiepiphysiodesis forcorrection of angular deformity in pediatricamputees. J Pediatr Orthop 2013;33(7):737-742.
46. Choi IH, Lipton GE, Mackenzie W,Bowen JR, Kumar SJ: Wedge-shaped distaltibial epiphysis in the pathogenesis ofequinovalgus deformity of the foot andankle in tibial lengthening for fibularhemimelia. J Pediatr Orthop 2000;20(4):428-436.
47. Thomas IH, Williams PF: The Grucaoperation for congenital absence of the fibula.J Bone Joint Surg Br 1987;69(4):587-592.
48. Rajacic N, Dashti H: Reconstruction of thelateral malleolus using a reverse-flowvascularized fibular head: A case report.Microsurgery 1996;17(3):158-161.
49. Weber M, Siebert CH, Goost H,Johannisson R, Wirtz D: Malleolusexternus plasty for joint reconstruction infibular aplasia: Preliminary report of a newtechnique. J Pediatr Orthop B 2002;11(3):265-273.
50. Exner GU: Bending osteotomy through thedistal tibial physis in fibular hemimelia forstable reduction of the hindfoot. J PediatrOrthop B 2003;12(1):27-32.
51. El-Tayeby HM, Ahmed AA: Anklereconstruction in type II fibular hemimelia.Strategies Trauma Limb Reconstr 2012;7(1):23-26.
52. Walker JL, Knapp D, Minter C, et al: Adultoutcomes following amputation orlengthening for fibular deficiency. J BoneJoint Surg Am 2009;91(4):797-804.
53. Zarzycki D, Jasiewicz B, Kacki W, et al:Limb lengthening in fibular hemimeliatype II: Can it be an alternative toamputation? J Pediatr Orthop B 2006;15(2):147-153.
Reggie C. Hamdy, MD, MSc, FRCSC, et al
April 2014, Vol 22, No 4 255
Copyright � the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.