Parameterization of Quasigeostrophic Eddies in Primitive Equation Ocean Models
Joint Parameterization of Honorifics and Terms of Address in Kartvelian Languages
-
Upload
rtlspielefree -
Category
Documents
-
view
0 -
download
0
Transcript of Joint Parameterization of Honorifics and Terms of Address in Kartvelian Languages
Validation of genome-wide association study(GWAS)-identified disease risk alleles withpatient-specific stem cell lines
Jin Yang1,2,3, Yao Li1,2, Lawrence Chan1,2, Yi-Ting Tsai1,2, Wen-Hsuan Wu1,2,
Huy V. Nguyen1,2, Chun-Wei Hsu1,2, Xiaorong Li3, Lewis M. Brown4, Dieter Egli5,
Janet R. Sparrow2 and Stephen H. Tsang1,2,6,∗
1Barbara and Donald Jonas Laboratory of Stem Cells and Regenerative Medicine, Department of Ophthalmology,
Pathology and Cell Biology, College of Physicians and Surgeons, Columbia University, New York, NY 10032, USA,2Edward S. Harkness Eye Institute, Columbia University, New York, NY 10032, USA, 3Tianjin Medical University Eye
Hospital, Tianjin 300384, China, 4Quantitative Proteomics Center, Department of Biological Sciences, Columbia
University, New York, NY 10027, USA, 5The New York Stem Cell Foundation Laboratory, New York, NY 10032, USA and6New York-Presbyterian Hospital, Columbia University Medical Center, New York, NY 10032, USA
Received September 10, 2013; Revised December 21, 2013; Accepted January 31, 2014
While the past decade has seen great progress in mapping loci for common diseases, studying how these riskalleles lead to pathology remains a challenge. Age-related macular degeneration (AMD) affects 9 million olderAmericans, and is characterized by the loss of the retinal pigment epithelium (RPE). Although the closely linkedgenome-wide association studies ARMS2/HTRA1 genes, located at the chromosome 10q26 locus, are stronglyassociatedwith theriskofAMD, theirdownstreamtargetsareunknown.Lowpopulation frequenciesof riskallelesin tissue banks make it impractical to study their function in cells derived from autopsied tissue. Moreover, aut-opsy eyes from end-stage AMD patients, where age-related RPE atrophy and fibrosis are already present,cannot be used to determine how abnormal ARMS2/HTRA1 expression can initiate RPE pathology. Instead,induced pluripotent stem (iPS) cell-derived RPE from patients provides us with earlier stage AMD patient-specificcells and allows us to analyze the underlying mechanisms at this critical time point. An unbiased proteome screenof A2E-aged patient-specific iPS-derived RPE cell lines identified superoxide dismutase 2 (SOD2)-mediated anti-oxidative defense in the genetic allele’s susceptibility of AMD. The AMD-associated risk haplotype (T-in/del-A)impairs the ability of the RPE to defend against aging-related oxidative stress. SOD2 defense is impaired inRPE homozygous for the risk haplotype (T-in/del-A; T-in/del-A), while the effect was less pronounced in RPEhomozygous for the protective haplotype (G–Wt–G; G–Wt–G). ARMS2/HTRA1 risk alleles decrease SOD2 de-fense, making RPE more susceptible to oxidative damage and thereby contributing to AMD pathogenesis.
INTRODUCTION
Age-related macular degeneration (AMD) is one of the mostcommon irreversible causes of severe vision loss in individualsover the age of 55 (1). Despite intensive basic and clinical re-search, its pathogenesis remains unclear. Studies have shownthat both genetic factors and environmental factors, such aspersistent oxidative stress and smoking, are involved with the
onset of AMD (2). Light exposure in combination with thephotosensitizing capability of lipofuscin within the RPEmakes the retina especially vulnerable to damage by reactiveoxygen species (ROS) and by lipid-derived oxidative proteinmodifications (3). The resulting increase in oxidative stress toretinal pigment epithelium (RPE) cells elevates the risk ofAMD. We hypothesize that antioxidant capacity is influencedby genetic factors.
∗ To whom correspondence should be addressed at: Edward S. Harkness Eye Institute, New York-Presbyterian/Columbia University Medical Center, 160Fort Washington Ave. Research Annex, Room 513, New York, NY 10032, USA. Tel: +1 212 3421189; Fax: +1 212 3054987; Email: [email protected]
# The Author 2014. Published by Oxford University Press. All rights reserved.For Permissions, please email: [email protected]
Human Molecular Genetics, 2014, Vol. 23, No. 13 3445–3455doi:10.1093/hmg/ddu053Advance Access published on February 4, 2014
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
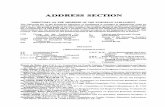
Despite progress in mapping complex aging-related diseaseloci, determining how these alleles initiate pathology duringaging remains a challenge. Genetic variants at two loci ofchromosome 10q26 and 1q31 have been strongly associatedwith the risk of developing AMD. Genome-wide associationstudies (GWAS) and linkage studies have identified theY402H variant in CFH, the rs10490924 single-nucleotide poly-morphism (SNP) in ARMS2 (OMIM# 611313) and thers11200638 SNP in HTRA1 (OMIM# 602194) as potential riskfactors for AMD (Fig. 1). The genes ARMS2 and HTRA1 arelocated on chromosome 10q26 and are in such strong linkage dis-equilibrium (LD) that their contributions to disease susceptibil-ity are indistinguishable using statistical analysis. The basicbiological function of the ARMS2 (age-related maculopathysusceptibility 2) protein still remains unclear (4, 5), and theHTRA1 (high temperature requirement-A) protein is a serineprotease; both are expressed in RPE cells. Their underlying mo-lecular mechanisms in AMD pathology remain uncertain (6).
Previous studies of macular diseases utilize post-mortemtissue, which is problematic for several reasons. First, it is diffi-cult to obtain a specific genotype; for example, only 0.5% of Cau-casians are double homozygous for the CFH (402H) andARMS2/HTRA1 (T-in/del-A) risk alleles for AMD and only25% are double homozygous for the CFH (402Y) and ARMS2/HTRA1 (G–Wt–G) protective alleles. Such low population fre-quencies make it impractical to study the pathological agingmechanisms associated with these alleles using samples fromeye banks. Second, when appropriate post-mortem AMDtissue can be obtained, it is almost always from late-stagedonors. Lastly, post-mortem tissue is usually processed undersuboptimal experimental conditions, which creates a myriad ofresearch-related problems. Autopsy eyes from end-stage AMDpatients, where age-related RPE atrophy and fibrosis arealready present, cannot be used to determine how abnormalARMS2/HTRA1 expression can initiate RPE pathology. To cir-cumvent the human tissue shortage issue, reprogramming tech-nology can be used to convert stem cells from patientshomozygous for either the risk haplotype (T-in/del-A; T-in/del-A) or the protective haplotype (G–Wt–G; G–Wt–G) intodifferentiated retinal cells. Since our research is focused onunderstanding the molecular pathways that impact early-stagedisease, we have differentiated induced pluripotent stem cells(iPSC) obtained from end-stage AMD donors into RPE (7).Using AMD patient-specific stem cells, we were able to modeland study the disease.
We used patient-specific iPSC-derived RPE cell lines contain-ing either or both the protective haplotype (G–Wt–G) and risk
haplotype (T-in/del-A). To mimic RPE cell senescence, weallowed the cells to accumulate A2E, one of the lipofuscin fluor-ophores that accumulate in RPE cells with age. A substantialportion of the lipofuscin that accumulates with age in RPEcells consists of bisretinoids that form as a consequence of reac-tions of vitamin A aldehyde in photoreceptor outer segments.Photoreceptors shed apical portions of their light-transducingouter segments daily. The RPE cells play a critical function byphagocytosing the shed outer segments, thereby taking up the bis-retinoid that has formed in photoreceptor cells. Upon blue light ir-radiation, A2E generates singlet oxygen, superoxide anion andhydrogen peroxide, agents that are widely believed to contributeto aging processes in human RPE cells (8). By introducing A2Eaccumulation as a component of the RPE aging process (9, 10),we sought to determine whether oxidative stress defense is asso-ciated with AMD gene susceptibility factors.
RESULTS
Reprogramming patient-specific fibroblasts and generationof patient-specific RPE cells
Fibroblasts were cultured from skin biopsies taken from two un-affected controls homozygous for protective haplotype and twohigh-risk AMD patient donors [one heterozygote (T-in/del-A;G–Wt–G), and one homozygous (T-in/del-A; T–in/del–A)for risk haplotype]. Colonies of iPS cells began to appearbetween 14 and 21 days after initiation of cellular reprogram-ming using lentiviral vectors expressing OCT4, SOX2, KLF4and MYC. Purified RPE cells formed after 8–12 weeks of dif-ferentiation. Through light microscopy, hexagonal-shapedcells and dark perinuclear melanin granules typically found innaı̈ve RPE were seen in iPSC-derived RPE cells, indicatingthat human iPSC-derived RPE cells were indistinguishablefrom primary cultures of human RPE (Fig. 2A). RPE-specificmarker RPE65 and tight junction cell membrane protein ZO-1immunofluorescence reactions on iPSC-derived RPE celllines were positive (Fig. 2B). All iPSC-RPE cell lines expressedsimilar levels of BEST1, CRALBP, MITF and RPE65 (Fig. 2C).Furthermore, reverse transcription–PCR (RT–PCR) analysisconfirmed positive expression of BEST1, RPE65 and MFRPin the iPSC-RPE cell lines. Skin biopsy fibroblast cells andiPS cells prior to differentiation were tested concurrently withthe negative control. Autopsy-RPE cells’ RT–PCRs areshown as the positive controls and GAPDH as the loadingcontrol (Fig. 2D). Because phagocytosis is one of the primaryroles of RPE cells, we tested for phagocytic ability in theiPSC-RPE cell lines and obtained positive results (Fig. 2E).Additionally, we observed the apical microvilli and intracellu-lar pigment by transmission electron microscopy (Fig. 2F).These tests laid a strong foundation for in vitro AMD RPEcell modeling using iPSC-RPE.
Model of aged RPE and autofluorescent imaging
After delivering A2E (10 mM in media) for 10 days, the accumu-lation of the fluorophore within the cells was evidenced by auto-fluorescent granules in light micrographs (Fig. 3A′) andlipofuscin deposits in electron micrographs (Fig. 3B′). Import-antly, these A2E-aged iPSC-derived RPE cells resembled
Figure 1. Variants at the chromosome 10q26 locus. For simplification andwithout loss of generality, the variants will be designated by the ARMS2 SNP(rs10490924) genotype for the rest of the figures.
3446 Human Molecular Genetics, 2014, Vol. 23, No. 13
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
intact, aged (24-year-old) monkey RPE (Fig. 3C′) in that theyboth exhibited a high density of intracellular deposits ofmelanin and lipofuscin mixtures, which is a typical feature ofaged RPE cells (11). On the other hand, cultured iPSC-derivedRPE cells that were not aged by A2E exhibited negative auto-fluorescence (Fig. 3A) and a very low density of the mixture oflipofuscin and melanin deposits (Fig. 3B), similar to RPE injuvenile (1-year-old) monkeys (Fig. 3C).
Label-free mass spectrometric protein profiling
Shotgun proteomic mass spectrometry-based measurementswere performed in triplicate on one homozygous for protectivehaplotype (wild-type) and one heterozygous iPSC-RPE cellline, with and without A2E. A liquid chromatography-massspectrometry (LC-MS) approach was used for the relative quan-titation and simultaneous identification of proteins within our
Figure 2. Induction of RPE cells from patient-specific iPS cells. (A) Various stages of iPSC-derived RPE cell generation from donor tissue. Comparison of primaryhuman autopsy-RPE cells with iPSC-derived RPE cells. Hexagonal shaped cells and dark perinuclear melanin granules, which are typical features of RPE, can beobserved on iPSC-derived RPE cells. Scale bars: 100 mm. (B) Immunocytochemistry. Visualization of RPE65, an RPE marker; ZO-1 showed correct morphologyand tight junction formation in homozygous high-risk T/T and protective G/G iPSC-derived RPE cells. Scale bars: 100 mm. (C and D) Western blot and RT–PCR expression profiling revealed the RPE characteristic proteins and RPE genes, respectively. Loading control, b-actin and GAPDH. (E) Immunofluorescentimages of internalized rod outer segments (ROS) in wild-type iPSC-RPE cells to verify the function of iPSC-derived RPE cells. (×20). (F) Transmission electronmicroscopic images of iPSC-RPE showed the presence of apical microvilli (arrow), intracellular pigment (×12 000). N, nucleus.
Human Molecular Genetics, 2014, Vol. 23, No. 13 3447
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
samples. This included triplicate LC/MS/MS chromatograms(technical replicates) collected for each of the three biologicalreplicates. Label-free shotgun proteomic profiling provided uswith data to identify one or more key proteins from thousandsof proteins and discern differences in protein expression pheno-types across cell lines with varying genotypes (12). Mitochon-drial superoxide dismutase (SOD2) emerged as the mostsignificant differentially expressed protein in RPE lines as ithad a unique differential expression pattern (Supplementary Ma-terial, Table S1 and Supplementary Material, Results—Proteo-mics). SOD2 protein level was 37-fold higher in RPE with thehomozygous protective haplotype after A2E treatment com-pared with untreated cells (P , 0.0004, false discovery rate cor-rection for multiple testing). No other protein in this data set hasthis striking pattern of expression (i.e. high-fold expression inwild-type + A2E and negligible expression in other treat-ments/genotypes). The mean individual SOD2 protein abun-dance values for wild-type cells before and after A2E agingwere 83 and 3129, respectively, and values for AMD high-riskcells before and after aging were 154 and 68, respectively.
Moreover, the TransOmics software generated a mean peptideion score of 9.4 (database match quality) for the eight peptidesrepresenting SOD2. This was well above the mean peptide ionquality score of 6.8 for this experiment (range of 3.5–14.6),strongly supporting the reproducibility of this identification.Peptide-integrated intensity volumes for extracted ion chroma-tograms formed the basis of protein abundance measurements.An example of this type of protein abundance measurement isgiven in a three-dimensional contour plot for one isotopiccluster (Fig. 4A) of a single SOD2 peptide highly expressed inwild-type RPE cells after A2E treatment, but not in A2E-treatedhigh-risk RPE cells. For each protein abundance measurement,multiple peptides are measured in this manner. Hence, SOD2emerged as a candidate based on the differential expressionscreening of RPE lines derived from patients’ iPSC with differ-ent genotypes. Immunoblot analyses confirmed the results fromthe proteomic profiling: similar patterns were observed in SOD2expression (Fig. 4B), with increased expression in cells homozy-gous for the protective haplotype after treatment (+A2E)and negligible changes in heterozygous cells after treatment(Fig. 4C).
SOD2 activity and antioxidant capacity test
We next examined SOD2 activity of all three genotypes (i.e.homozygous for protective haplotype, heterozygous and homo-zygous for risk haplotype) in iPS-RPE and autopsy-RPE cells,before and after A2E treatment; activity measurements weremade using a colorimetric assay (Abcam, Cambridge, MA,USA) (13–16). SOD2 activity data for each type of A2E-agedcell was normalized to its corresponding non-aged counterpart(Fig. 5A) in order for us to examine how genotype affects the re-sponse of cultured RPE to A2E aging. SOD2 activity in RPEhomozygous for the protective haplotype was dramaticallyincreased in response to the aging treatment. In contrast,SOD2 activity in RPE from high-risk (heterozygous and homo-zygous for risk haplotype) AMD patients was decreased. Thisfinding held regardless of whether the RPE came from humaniPS cells or from post-mortem tissue-derived RPE cells.
We next tested the hypothesis that low SOD2 expression andactivity, as observed in cells homozygous for risk haplotype,compromise antioxidant capacity (Fig. 5B). To do this, we cul-tured iPSC-RPE cells of the three different genotypes thatwere treated with A2E and exposed to blue light, or untreatedas controls. Cell lysates were then tested in an oxygen radical ab-sorbance capacity assay (STA-345, Cell Biolabs, San Diego,CA, USA). The assay works by the addition of peroxyl radicals(via a free-radical generator) followed by the measurement ofresulting fluorescein decay over a 60 min period. The decay isslowed by SOD2, which neutralizes peroxyl radicals. AfterA2E treatment, the decay was found to be faster in AMD high-risk (heterozygous and homozygous for risk haplotype)samples, consistent with their decrease in SOD2 antioxidant cap-acity. We qualified the decay by calculating the area between thetwo decay curves (with and without A2E treatment), whichrepresents the change in antioxidant capacity. After integratingthe area between the two curves, we found that in the lysatefrom cells homozygous for the protective haplotype, there wasa net increase in antioxidant capacity (+2.49) as a result ofA2E treatment. Conversely, antioxidant capacity decreased in
Figure 3. Model of aging in cultured RPE mimics aged monkey RPE within anintact eyeball. (A and A′) iPSC-derived RPE from AMD patients cultured ontranswell for 10 days; autofluorescence can be seen under fluorescence micro-scope in A′. (B and B′) Transmission electron microscopy; in the presence of10 mM A2E over 10 days (A2E), more structures composed of lipofuscin andmelanin appeared in B′ than before A2E treatment in B. Lipofuscin andmelanin deposits are gray and black, respectively. (C and C′) Electron micros-copy of RPE in fixed sections of eyes from 1- and 24-year-old rhesus monkeys.
3448 Human Molecular Genetics, 2014, Vol. 23, No. 13
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
the lysates from cells heterozygous and homozygous for the riskhaplotypes (20.47 and 20.85, respectively).
Increased ROS/superoxide level in AMD risk haplotype RPEcells
Red fluorescent products of varying brightness levels, indicativeof ROS, were generated across all samples using the Total ROS/Superoxide Detection Kit (ENZ-51010, Enzo, Farmingdale,NY, USA) (Fig. 6). In both autopsy-RPE and iPSC-derivedRPE, we observed a trend that was congruous with the previousobservation that superoxide levels were greatest in risk
haplotype homozygotes, followed by heterozygotes and finallylowest in protective haplotype homozygotes. Quantification offluorescence density was measured using ImageJ (1.48e). Thefluorescence values of autopsy-RPE cells were: 44.86 (G/G),161.66 (T/G) and 217 (T/T). The fluorescence values foriPSC-RPE cells were: 66.1 (G/G), 113.7 (T/G) and 197.6(T/T). There was a statistically significant difference influorescence values between the samples homozygous forthe protective haplotype and homozygous for the riskhaplotype (iPSC-RPE: P , 0.01, t ¼ 6.4341, unpaired t-test;autopsy-RPE: P , 0.05, t ¼ 3.1209, unpaired t-test). Theseresults showed that in the presence of ROS inducers, the levels
Figure 4. Shotgun proteomic mass spectrometry-based measurement of differential expression of SOD2. (A) Three-dimensional visualization of isotopic clusters of asingle SOD2 peptide example as rendered by TransOmics software. The peptide was highly expressed in RPE cells with the wild-type protective G/G genotype afterA2E treatment, but that over-expression is not seen in the risk T/G genotype after A2E treatment. Volume under peak (peak height) indicates peptide abundance(z-dimension), which is then rolled up to protein abundance as calculated by the TransOmics software. Axes represent retention time and m/z (mass-to-chargeratio). (B) SOD2 immunoblot results are the same as mass spectrometry protein level; loading control, b-actin. (C) Densitometry of SOD2 signal from Figure 3B,normalized to b-actin. Fold change measurement after treatment is shown based on protein level before treatment.
Figure 5. Impaired SOD2 stress response in cultured human RPE accompanies the presence of the high-risk allele. Cell cultures were either iPSC-derived RPE orprimary RPE from autopsy tissue. The genotype of each cell’s origin is indicated (G/G for homozygous for protective haplotype, T/G for heterozygous and T/Tfor homozygous for risk haplotype). (A) SOD2 activity was measured in triplicate cultures for each of the six cell types. The triplicate measures were averagedand then normalized (A2E-aged cells normalized to non-aged cells). SOD2 activity in RPE from protective wild-type cell lines was dramatically increased in responseto the aging treatment. In contrast, SOD2 activity in RPE from high-risk AMD patients (T/G and T/T) was decreased. (# of patients the cell lines came from: iPSC-RPEcells – nG/G ¼ 2, nT/G ¼ 1, nT/T ¼ 1; autopsy-RPE – nG/G ¼ 2, nG/T ¼ 2, nT/T ¼ 1. All samples were tested in triplicate.) Error bars show SEM for different cell linesand significance was calculated using unpaired and two-tailed t-test analyses between wild-type and T/G, T/T high-risk alleles, respectively. ∗P , 0.05; ∗∗P , 0.01.(B) Antioxidant capacity of human RPE after A2E treatment differs depending on genotype. The decay was slowed by SOD2, which neutralizes peroxyl radicals;antioxidant capacity is promoted in wild-type cell lines, while antioxidant capacity was lowered in T/G and T/T cell lines. Fluorescence intensity was measuredevery 5 min, and decay curves were generated which indicated changes in antioxidant capacity over time. The differences in net area under the curve before andafter A2E treatment were calculated (+2.49, 20.47 and 20.85, for G/G, T/G and T/T, respectively).
Human Molecular Genetics, 2014, Vol. 23, No. 13 3449
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
of ROS/superoxide exhibited are related to the risk factor geno-type, most likely due to differential SOD2 activity among thevarious cell genotypes.
Oxidative damage of RPE and disruption of b-catenin
Forkhead Box O transcription factors (FOXO) are a family ofROS level sensors (17). Increased ratios of phospho-FOXO3A(FOXO3A phosphorylated on Thr-32) to total FOXO3A afterA2E treatment with blue light exposure were found in sampleshomozygous for the risk haplotypes in both iPSC-derived RPEcell lines and autopsy human cell lines (Fig. 7B and C), but notin homozygous for protective haplotype cells lines after identicalA2E treatment (autopsy-RPE: P , 0.01, t ¼ 6.2104, unpairedt-test; iPSC-RPE: P , 0.05, t ¼ 3.6924, unpaired t-test). Add-itionally, b-catenin expression levels decreased after A2Etreatment in cells homozygous for risk haplotype (autopsy-RPE:
P , 0.01, t ¼ 6.6568, unpaired t-test; iPSC-RPE: P , 0.05, t ¼4.5795, unpaired t-test). Immunostaining for the adherence junc-tion protein b-catenin, which maintains the barrier integrity ofthe RPE, showed the disruption after A2E treatment with bluelight exposure, demonstrating movement of b-catenin from theperiphery to the inside of RPE cells (Fig. 7A). Overall, theresults show that RPE cells homozygous for risk haplotype,with decreased SOD2 activity and higher ROS levels, haveincreased FOXO3A but decreased b-catenin levels in responseto A2E treatment.
DISCUSSION
AMD is a leading cause of loss of independence in activities ofdaily living for older adults. Nine million Americans are diag-nosed with AMD, and the incidence is expected to double inthe next decade—eventually affecting 20% of Americansbetween the ages of 65 and 75, and 30% over 75 (18). There isno effective treatment and the greatest barrier to developingtreatments is the lack of knowledge about the molecular basisof disease pathogenesis. iPS cells reprogrammed from somaticcells have allowed for the generation of patient-specificdisease cells in vitro. Interest in generating human iPS cells forstem cell modeling of disease has overtaken that for patient-specific human embryonic stem cells due to the latter’s ethical,technical and political concerns. By providing a platform tostudy patient-specific targeted disease cells on a researchbench, iPS cells have great potential in regenerative medicineand modeling of human disease (19, 20). Studies of the in vitrophenotypes of disease-specific iPSC-derived cells can aid infilling the gap between clinical phenotypes and molecular orcellular mechanisms, with further applications including newstrategies for drug screening and the development of novel thera-peutic agents. Because an AMD-associated risk haplotype at theARMS2/HTRA1 locus is known to be a risk factor for AMD, wecreated specifically genotyped AMD disease models using iPSCtechnology for use as valuable tools in elucidating its molecularpathways. In conjunction with iPSC-RPE, eye bank autopsy-RPE, genotyped to have AMD high-risk and protective AMDalleles, served as experimental controls in various assays.
RPE cells generated from human iPS cells have been shown toexhibit an RPE fate (7, 21). To recapitulate the phenotype of alate-onset degenerative disease such as AMD, we acceleratedthe aging process in iPSC-derived and autopsy-RPE cell linesusing a combination of 10 mM A2E and blue light, which pro-vides us with an ideal system for modeling AMD (22–25).
A2E creates oxidative stress by light-mediated generation ofsinglet oxygen and superoxide (22, 26). An excess of reactiveforms of oxygen results from either their overproduction or in-sufficient activity of antioxidant defense systems. A2E accumu-lates in RPE cells in every individual and yet only certainpatients—those with risk haplotypes—develop AMD. There-fore, we hypothesized that RPE with the AMD-associated riskhaplotype (T-in/del-A) should have reduced antioxidant cap-acity, whereas wild-type RPE with the protective haplotypehave a greater antioxidant protective capacity. In our RPEcells modeling AMD, antioxidant defense ability was testedby the activity of mitochondrial SOD, which is localized inmitochondria and protects the cells against oxidative stress.
Figure 6. ROS/superoxide levels in cultured human RPE treated with ROSinducer (Pyocyanin) are increased in the presence of the high-risk allele. (A)Fluorescence microscopy; intensity of red signals proportional to superoxidelevels. (B) Quantified fluorescence values in relationship to risk factor genotype.Repeat fluorescence counts for at least three other distinct microscopic fieldswere obtained and averaged. There was a statistically significant difference influorescence values between wild-type (G/G) and homozygote high-risk (T/T)alleles (∗P , 0.05; ∗∗P , 0.01). This trend is observed in both autopsy and iPSC-derived RPE.
3450 Human Molecular Genetics, 2014, Vol. 23, No. 13
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
Because impaired SOD2 stress responses in RPE occur in cellscontaining the risk haplotype (Fig. 5), we conclude that oxidativestress defense is associated with GWAS risk factors.
Low SOD2 activity in high-risk RPE cells may lead toincreased susceptibility to the development of AMD. In our un-biased proteome screen of high-risk AMD cells, SOD2 was iden-tified as one of the downstream targets of ARMS2/HTRA1pathology (Supplementary Material, Fig. S1). Plasma SOD ac-tivity has been shown to be lower in neovascular AMD patientsthan in controls (13). Previous studies have also been performedto test reactions of SOD2-deficient animals to oxidative injury;RPE and retinal cells in SOD2-deficient mice showed greaterinstances of morphologic abnormalities, including features ofAMD, compared with wild-type controls (15, 16, 27). Weshowed that SOD2 activity in RPE from patients homozygousfor the protective haplotype (G-Wt-G; G-Wt-G) increased in re-sponse to the A2E aging treatment. In contrast, SOD2 activity inRPE from high-risk AMD patients (both homozygous for riskhaplotype and heterozygous) was significantly decreased. Wealso showed that decreased SOD2 activity corresponded todiminished antioxidant capacity in both high-risk RPE lysates,as verified by the oxygen radical absorbance capacity test.These results were not limited to A2E oxidant stress, as super-oxide level responses to the ROS inducer pyocyanin showed
the same trend in both autopsy-RPE and iPSC-RPE, with cellshomozygous for the risk haplotype having the highest super-oxide levels.
Diminished SOD2 protective responses in high-risk RPE cellsmay also be linked to the role of the FOXO family of transcrip-tion factors in regulating ROS stress. The FOXO family is a keycomponent in sensing and responding to ROS levels, as evi-denced by an increase in phosphorylated FOXO3A under con-ditions of oxidative stress (28, 29). One function of FOXO isto regulate pro-apoptotic genes; studies have shown that aFOXO3a mutant suppresses ROS-induced cell death (30). Inour study, RPE homozygous for protective haplotype allshowed negligible changes in ratio levels of phospho-FOXO3Ato FOXO3A expression after A2E treatment, while RPE homo-zygous for risk haplotype exhibited increased ratios aftertreatment. Our data show that decreased SOD2 activity is accom-panied by increased phospho-FOXO3A to FOXO3A ratios, con-firming that the ROS stress levels are indeed closely linked to thegenotype mediated by SOD2 antioxidant activity.
The FOXO family of transcription factors inhibits b-catenin-mediated antioxidative defense (31), which is consistent withour findings. The phospho-FOXO3A protein levels increasedin RPE cells homozygous for the risk haplotype and coincidedwith greater decreases in b-catenin levels. Since b-catenin is
Figure 7. Increased ratios of phospho-FOXO3A to total FOXO3A are accompanied by decreasedb-catenin levels in high-risk cell lines. A2E-treated RPE were trans-ferred to RPE media for 20 days before b-catenin morphological and immunofluorescence studies were performed. (A) Confocal images showed translocation ofb-catenin from the periphery to the cytoplasm of RPE cells. (B and C) A discernible decrease in b-catenin in both rs10490924 T/T cell lines from iPSC andautopsy can be seen, while phospho-FOXO3A/total FOXO3A protein levels were increased correspondingly. Error bars show SEM for different cell lines andsignificance was calculated using unpaired and two-tailed t-test analyses (∗P , 0.05; ∗∗P , 0.01).
Human Molecular Genetics, 2014, Vol. 23, No. 13 3451
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
an adherence junction protein that plays an important role in theintegrity of the RPE cell layer, decreased levels of b-cateninresulting from oxidative stress disrupts RPE junctions (32, 33),which has a stronger negative effect on cell barrier functionand may be a mechanism leading to RPE detachment and subse-quent choroidal neovascularization (33) (Fig. 8).
Dissection of the pathways affected by ARMS2/HTRA1 allelesin iPSC-derived RPE should be considered when assessingmolecular targets for AMD intervention. The AMD-associatedrisk haplotype impaired the protective SOD2 activity underconditions of oxidative stress generated by A2E. Since therewere no statistical differences between the HTRA1 expressionin AMD cells homozygous for risk haplotype and RPEhomozygous for protective haplotype (Supplementary Material,
Fig. S2), the biological relationship between genotype andSOD2 activity was not the main focus of this report.
Although the precise roles of HTRA1 and ARMS2 in AMDpathogenesis are unknown, our data suggest that the wild-type‘protective haplotype’ can decrease oxidative stress by meansof increased SOD2 activity, as evidenced by five observationsof ‘protected’ cells after A2E treatment: (i) higher SOD2 expres-sion levels; (ii) greater SOD2 activity; (iii) lower ROS levels;(iv) no increase in the ratio of phospho-FOXO3A to totalFOXO3A; and (v) a smaller decrease in protective b-cateninlevels. The differential antioxidant capacities among haplotypesof each of the three chromosome 10q26 locus variants canaccount for genetic susceptibility to AMD. In this manner, thera-peutic strategies aimed at potentiating SOD2 activity may be areasonable approach to reducing the influence of theAMD-associated variant in ARMS2/HTRA1 on the developmentof AMD.
MATERIALS AND METHODS
Research subjects
AMD-afflicted and unaffected individuals were enrolled in thestudy under protocol #IRB-AAAF1849 after we obtained fullconsent. The Institutional Review Board at Columbia Universityapproved the protocol and this study conformed to the tenets ofthe Declaration of Helsinki. Each patient received a completeclinical evaluation by the corresponding author.
Skin biopsy samples were obtained from patients and healthysubject using lidocaine anesthesia (APP Fresenius Kabi,Germany) and biopsy-punch (McKesson, VA, USA). Sampleswere processed and cultured according to protocol (7).
Cell culture
iPSC-derived RPE cell lines were obtained from wild-type (un-affected), heterozygous high-risk (affected) AMD patients andhomozygous high-risk (affected) AMD patients fibroblasts.The homozygous high-risk fibroblasts were donated by theNew York Stem Cell Foundation Laboratory. We used lentiviralvectors carrying transcription factors OCT4, SOX2, KLF4 andMYC to transduce fibroblasts into iPS cell lines in accordancewith established protocols using human embryonic stem cellmedium (HUESM) with 10 mM basic fibroblast growth factor(bFGF). iPS cells were co-cultured with mitomycin-C-treatedstromal cells from the PA6 line. Next, we further incubated thecells under 5% CO2 at 378C in differentiation medium(HUESM–bFGF with 10 nm Nicotinamide) from day 0 to day20 and 20 ng/ml Activin A from day 20 to day 40. The mediawere replaced twice a week. Upon pigmentation of the cells,we chose pigmented colonies to be replated on Matrigel-coatedplate in RPE culture medium as per protocol.
Autopsy-RPE cell cultures were generated using human eyesamples with the anterior portions removed obtained from theEye-Bank of New York. Following the RPE cell culture proced-ure developed by Maminishkis and Miller (7), we first incubatedthe eye cup at 378C with 5% CO2 for 40–60 min. Next, the retinawas removed from the optic nerve with retinal scissors, andforceps were used to separate RPE-Bruch’s membrane fromthe choroidal tissue layer. RPE sheets were then placed into
Figure 8. High-risk AMD alleles are associated with diminished SOD2 activity.ATR is generated from the photobleaching of rhodopsin in the photoreceptor diskmembrane (1). A fraction of this ATR undergoes several reactions (2) before re-leasing an A2E precursor. This A2E precursor is phagocytosed into the RPE cell(3). Cleavage of the A2E precursor in RPE lysosomes releases A2E, which accu-mulates as a component of lipofuscin (4). A2E photosensitizes the formation ofsinglet oxygen and superoxide anion (5), and the latter is detoxified in the RPEmitochondria by superoxide dismutase 2 (SOD2) (6). The present study involvesaccumulation of A2E in RPE cells (7). As the presence of high-risk AMD allelescauses a decrease in SOD2 activity, a rise in ROS will increase oxidative damage.At the same time, ROS-activated FOXO3A can down regulate b-catenin.
3452 Human Molecular Genetics, 2014, Vol. 23, No. 13
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
cold trypsin–EDTA (Gibco) solution in a 15 ml tube. Upon col-lection of RPE cells, the tissue-containing tubes were transferredinto a water bath for 10–15 min at 378C in order to separate theRPE into small clusters. Using a clinical centrifuge, we spundown the RPE cells at 1.4 rpm (Rotor radius 15 cm) for 4 min,removed the supernatant and re-suspended the cells in 15%RPE media (9 ml total). Three milliliters of cell suspensionwere placed into Primeria flasks, to which 2 ml of fresh 15%RPE media was then added. The flask was incubated at 378C,5% CO2 until the following day.
Immunoblot analyses
To confirm the RPE protein marker expression on ouriPSC-RPE, immunoblot analyses were conducted before A2Etreatment on one protective and all high-risk iPSC-RPE celllines. Extracted total cellular protein was analyzed usingsodium dodecyl sulfate–polyacrylamide gel electrophoresis.After transferring the samples to nitrocellulose membranes, weincubated them with rabbit anti-RPE65 monoclonal antibody(1:1000; a gift from T. Michael Redmond, National Institutesof Health), mouse anti-MiTF antibody, rabbit anti-Bestrophin1 antibody (1:1000; Abcam) and rabbit anti-CRALBP (1:1000;Santa Cruz Biotechnology, Santa Cruz, CA, USA). A chemilu-minescence assay (Immobilon Western; EMD Millipore,Billerica, MA, USA) was used to detect blots, whereupon mul-tiple exposures were taken using Kodak BioMax film (Kodak,New York, NY, USA) and developed with a KonicaSRX-101A medical film processor (Konica Minolta MedicalImaging USA Inc., Wayne, NJ, USA). After A2E treatmentand blue light exposure, immunoblot analysis with anti-SOD2antibody (1:1000; Abcam) was performed to confirm theresults of the label-free mass spectrometric protein profilingtest. Anti-FOXO3a (phosphorylated on T32) and anti-b-cateninwere also tested on samples with and without treatment (1:1000;Abcam).
RT–PCR assay
RNA was isolated from one protective and all high-riskiPSC-RPE cell lines using the RNeasy kit (QIAGEN, Hilden,Germany), and genomic DNA contamination was removedusing a DNA-free kit (Invitrogen). One microgram of totalRNA was used for cDNA synthesis using Superscript IIIReverse Transcriptase and Oligo (dT) primers (Invitrogen).The quality of cDNA synthesis was assessed by PCR amplifica-tion of GAPDH, as a housekeeping gene, using a combination offorward (5′-ATCACCATCTTCCAGGAGCG-3′) and reverse(5′-TGATGACCCTTTTGGCTCCC-3′) primers. The RPE65and bestrophin-1 PCR were then performed using primer setsHs01071462_m1 for RPE65 (4331182) and Hs00188249_m1for bestrophin-1 (4331182) (Applied Biosystems; Life Tech-nologies). The MFRP test used a combination of forward(5′-CAAGATCGAAGCCCTCAGCA-3′) and reverse (5′-GGTACCAGGCATGGAAACCA-3′) primers.
Immunohistochemistry
iPSC-derived RPE cells were placed in 4% paraformaldehyde(Sigma) in PBS at 218C for 2 h. We performed anti-RPE65,
anti-ZO-1 immunofluorescence staining (1:100) in order to char-acterize the iPSC-derived RPE generated from the fibroblaststaken from AMD patients. The nuclei were stained with DAPI(4′, 6-diamidino-2-phenylindole). Alexa Fluor 488 goat anti-rabbit or Alexa Fluor 555 goat anti-mouse IgG were conjugatedby secondary antibodies (1:1000; Invitrogen; Life Technolo-gies). We obtained images for all antibody labels using a fluores-cence microscope (Leica DM 5000 B) under the same settings.A2E-treated RPE were maintained in RPE medium for 20 daysbefore b-catenin immunofluorescence studies were performed.Confocal images (Zeiss LSM510) of b-catenin-stainedautopsy human RPE cells were taken before and after A2Etreatment.
A2E treatment
A2E (C42H58NO, molecular weight 592) was synthesized fromall-trans-retinal (ATR) and ethanolamine combined in a 2:1ratio (34–36). iPSC-derived RPE lines and autopsy-RPE wereseeded in 3.5 cm dishes and 4-well chamber slides. Then, theywere cultured for 10 days in the presence of 10 mM A2E.Where indicated, the cells were exposed for 10 min to 430 nm(blue) light. The light source was calibrated with a powermeter (Scientech, Boulder, CO, USA). We determined the cellu-lar autofluorescent levels using stereomicroscopy (Zeiss LSM510 META) (23, 24, 26), and A2E levels in cultured RPE cellsby HPLC (37). The same seeding density was used for all celllines and cells not treated with A2E served as negative controls.
Electron microscopy
iPSC-derived RPE cells were seeded at 24-well transwells pre-coated with poly-L-Lysine. After 10 days of A2E treatment,we performed electron microscopy according to established pro-tocols. Prior to observation by electron microscopy, areas ofinterest were trimmed for ultrathin sectioning and stained withuranyl acetate. A2E-treated and untreated cells’ EM morpholo-gies were compared with each other and with 1- and 24-year-oldmonkey RPE cells (gifts from Professor Peter Gouras).
Label-free mass spectrometric protein profiling
We extracted total proteins from one G/G genotype atrs10490924 (homozygous for protective haplotype) iPSC-derived RPE cell line and one T/G genotype at rs10490924 (het-erozygous) iPSC-derived RPE cell line, with and without A2Etreatments. For each of these cell lines, three biological repli-cates were prepared representing three separate culturesderived from each cell line, and replicates were also done separ-ately for A2E-treated samples. Proteins were extracted withTRIS-buffered saline with sodium dodecyl sulfate as previouslydescribed (38). The proteins were precipitated with chloroform–methanol and dissolved in 0.1% RapiGest detergent in 50 mMammonium bicarbonate. All protein extracts were reduced andalkylated prior to tryptic digestion, and RapiGest was cleavedwith acid. The resulting peptides were analyzed with SynaptG2 quadrupole-time-of-flight mass spectrometer (WatersCorp.) using MSE data-independent scanning (38). Initial dataprocessing was with ProteinLynx Global Server (Version 2.5RC9, Waters Corp.) for quality assurance testing of samples
Human Molecular Genetics, 2014, Vol. 23, No. 13 3453
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
and verifying instrument performance as described (38). Furtheranalysis was with TransOmics software (Waters Corp.). Thedata processing method is described in the SupplementaryMaterial, Methods—Proteomics section.
SOD2 activity and antioxidant capacity test
SOD2 activity measurements in high-risk homozygous (T/T),heterozygous (T/G) and protective (G/G) human autopsy-RPEand iPSC-RPE cells, with and without A2E treatment, weremade using a colorimetric assay (Abcam). The measurementswere based on inhibition of xanthine oxidase (XO) activity,which is linearly related to superoxide anion concentration.SOD2 activity was measured in triplicate cultures for each ofthe six cell types. The triplicate measures were averaged andthen normalized (A2E-aged cells were normalized to non-agedcells). Antioxidant capacity was determined by the oxygenradical absorbance capacity assay (STA-345, Cell Biolabs).The assay works by adding peroxyl radicals (via a free-radicalgenerator) and then measuring the resulting fluorescein decayover a 60 min period.
ROS/superoxide level test
To observe the effect of risk factor genotype on ROS/superoxidelevels in response to oxidative stressors other than A2E, we pre-pared A2E-untreated RPE samples for fluorescence microscopyusing the Total ROS/Superoxide Detection Kit (ENZ-51010,Enzo, Farmingdale, NY, USA). The samples were classifiedby AMD allele risk level (i.e. homozygote G/G protective, het-erozygote T/G high-risk and homozygote T/T high-risk), andby origin (i.e. iPSC-derived and autopsy). First, RPE cellscultured on glass slides were loaded with 30 nm SuperoxideDetection Reagent, a cell-permeable probe that reacts withsuperoxide to produce a fluorescent product. Next, we treatedthe cells with 200 mM ROS inducer (Pyocyanin) for 20 min,and then washed the cells in accordance with protocol. Usingfluorescence microscopy, we visualized the ROS/superoxidelevels in the cells using 80 ms exposure. Quantification of thedensity of fluorescence was measured by software ImageJ (1.48e).
AUTHORS’ CONTRIBUTIONS
J.Y., J.R.S. and S.H.T. designed research; J.Y., Y.L. and D.E.contributed to iPSC-RPE cell differentiation; J.Y. andW.-H.W. collected autopsy-RPE; J.Y., Y.-T.T., L.M.B.,C.-W.H and W.-H.W. performed research; J.R.S. providedA2E treatment; J.Y., X.L. and S.H.T. analyzed data; J.Y., L.C.,H.V.N., J.R.S. and S.H.T. wrote the paper.
SUPPLEMENTARY MATERIAL
Supplementary Material is available at HMG online.
ACKNOWLEDGEMENTS
We thank all the individuals and their families who donated theirskin biopsies and eyes for the study. We thank Peter Gouras andmembers of their laboratories for sharing ideas, histological
specimens from monkeys, antisera, equipment and for criticallyreading the manuscript. We thank Katherine J. Wert, RichardDavis, Deniz Erol and LiJuan Zhang for guidance and advice;and members of the Barbara and Donald Jonas Laboratory forsupport, especially our financial supporters.
Conflict of Interest statement. The authors declare no competingfinancial interests.
FUNDING
This work was supported by the National Institute of HealthCore (5P30EY019007), National Cancer Institute Core(5P30CA013696) and unrestricted funds from Research toPrevent Blindness, New York, NY, USA. S.H.T. is a member ofthe RD-CURE Consortium and is supported by the Tistou andCharlotte Kerstan Foundation, the National Institute of Health(R01EY018213), the Research to Prevent Blindness Physician-Scientist Award, Association for Research in Vision and Ophthal-mology (ARVO) Foundation, Macular Society, Retina ResearchFoundation Cox Macular Research Project, the Bernard andShirlee Brown Family Fund, the Schneeweiss Stem Cell Fund,New York State (N09G-302), the Foundation Fighting BlindnessNew York Regional Research Center Grant (C-NY05-0705-0312), the Joel Hoffman Fund, the Professor GertrudeRothschild Stem Cell Foundation and the Gebroe Family Founda-tion. H.V.N. is supported by the Research to Prevent BlindnessMedical Student Fellowship.
REFERENCES
1. Huang, L.L., Coleman, H.R., Kim, J., de Monasterio, F., Wong, W.T.,Schleicher, R.L., Ferris, F.L. III and Chew, E.Y. (2008) Oralsupplementation of lutein/zeaxanthin and omega-3 long chainpolyunsaturated fatty acids in persons aged 60 years or older, with or withoutAMD. Invest. Ophthalmol. Vis. Sci., 49, 3864–3869.
2. Wang, J.J., Buitendijk, G.H., Rochtchina, E., Lee, K.E., Klein, B.E., vanDuijn, C.M., Flood, V.M., Meuer, S.M., Attia, J., Myers, C. et al. (2013)Genetic susceptibility, dietary antioxidants, and long-term incidence ofage-related macular degeneration in two populations. Ophthalmology, pii:S0161-6420(13)00942-1. doi: 10.1016/j.ophtha.2013.10.017. [Epub aheadof print].
3. Nowak, J.Z. (2013) Oxidative stress, polyunsaturated fatty acids-derivedoxidation products and bisretinoids as potential inducers of CNS diseases:focus on age-related macular degeneration. Pharmacol. Rep., 65, 288–304.
4. Wang, G. (2013) Chromosome 10q26 locus and age-related maculardegeneration: a progress update. Exp. Eye Res., 119, 1–7.
5. Kanda, A., Chen, W., Othman, M., Branham, K.E., Brooks, M., Khanna, R.,He, S., Lyons, R., Abecasis, G.R. and Swaroop, A. (2007) A variant ofmitochondrial protein LOC387715/ARMS2, not HTRA1, is stronglyassociated with age-related macular degeneration. Proc. Natl Acad. Sci.USA, 104, 16227–16232.
6. Allikmets, R. and Dean, M. (2008) Bringing age-related maculardegeneration into focus. Nat. Genet., 40, 820–821.
7. Li, Y., Tsai, Y.T., Hsu, C.W., Erol, D., Yang, J., Wu, W.H., Davis, R.J., Egli,D. and Tsang, S.H. (2012) Long-term safety and efficacy of human-inducedpluripotent stem cell (iPS) grafts in a preclinical model of retinitispigmentosa. Mol. Med., 18, 1312–1319.
8. Liang, F.Q. and Godley, B.F. (2003) Oxidative stress-induced mitochondrialDNA damage in human retinal pigment epithelial cells: a possiblemechanism for RPE aging and age-related macular degeneration. Exp. EyeRes., 76, 397–403.
9. Ben-Shabat, S., Parish, C.A., Hashimoto, M., Liu, J., Nakanishi, K. andSparrow, J.R. (2001) Fluorescent pigments of the retinal pigment epitheliumand age-related macular degeneration. Bioorg. Med. Chem. Lett., 11,1533–1540.
3454 Human Molecular Genetics, 2014, Vol. 23, No. 13
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from
10. Sparrow, J.R., Fishkin, N., Zhou, J., Cai, B., Jang, Y.P., Krane, S., Itagaki, Y.and Nakanishi, K. (2003) A2E, a byproduct of the visual cycle. Vis. Res., 43,2983–2990.
11. Feeney, L. (1978) Lipofuscin and melanin of human retinal pigmentepithelium. Fluorescence, enzyme cytochemical, and ultrastructural studies.Invest. Ophthalmol. Vis. Sci., 17, 583–600.
12. Silva, J.C., Denny, R., Dorschel, C., Gorenstein, M.V., Li, G.Z., Richardson,K., Wall, D. and Geromanos, S.J. (2006) Simultaneous qualitative andquantitative analysis of the Escherichia coli proteome: a sweet tale. Mol.
Cell. Proteomics, 5, 589–607.
13. Zafrilla, P., Losada, M., Perez, A., Caravaca, G. and Mulero, J. (2013)Biomarkers of oxidative stress in patients with wet age related maculardegeneration. J. Nutr. Health Aging, 17, 219–222.
14. Esclapez, J., Zafrilla, B., Martinez-Espinosa, R.M. and Bonete, M.J. (2013)Cu-NirK from Haloferax mediterranei as an example of metalloproteinmaturation and exportation via Tat system. Biochim. Biophys. Acta, 1834,1003–1009.
15. Kasahara, E., Lin, L.R., Ho, Y.S. and Reddy, V.N. (2005) SOD2 protectsagainst oxidation-induced apoptosis in mouse retinal pigment epithelium:implications for age-related macular degeneration. Invest. Ophthalmol. Vis.
Sci., 46, 3426–3434.
16. Sandbach, J.M., Coscun, P.E., Grossniklaus, H.E., Kokoszka, J.E., Newman,N.J. and Wallace, D.C. (2001) Ocular pathology in mitochondrialsuperoxide dismutase (Sod2)-deficient mice. Invest. Ophthalmol. Vis. Sci.,42, 2173–2178.
17. Brunet, A., Sweeney, L.B., Sturgill, J.F., Chua, K.F., Greer, P.L., Lin, Y.,Tran, H., Ross, S.E., Mostoslavsky, R., Cohen, H.Y. et al. (2004)Stress-dependent regulation of FOXO transcription factors by the SIRT1deacetylase. Science, 303, 2011–2015.
18. Friedman, D.S., O’Colmain, B.J., Munoz, B., Tomany, S.C., McCarty, C., deJong, P.T., Nemesure, B., Mitchell, P. and Kempen, J. (2004) Prevalence ofage-related macular degeneration in the United States. Arch. Ophthalmol.,122, 564–572.
19. Tucker, B.A., Park, I.H., Qi, S.D., Klassen, H.J., Jiang, C., Yao, J., Redenti,S., Daley, G.Q. and Young, M.J. (2011) Transplantation of adult mouse iPScell-derived photoreceptor precursors restores retinal structure and functionin degenerative mice. PloS One, 6, e18992.
20. Singh, R., Shen, W., Kuai, D., Martin, J.M., Guo, X., Smith, M.A., Perez,E.T., Phillips, M.J., Simonett, J.M., Wallace, K.A. et al. (2013) iPS cellmodeling of Best disease: insights into the pathophysiology of an inheritedmacular degeneration. Hum. Mol. Genet., 22, 593–607.
21. Wang, N.K., Tosi, J., Kasanuki, J.M., Chou, C.L., Kong, J., Parmalee, N.,Wert, K.J., Allikmets, R., Lai, C.C., Chien, C.L. et al. (2010) Transplantationof reprogrammed embryonic stem cells improves visual function in a mousemodel for retinitis pigmentosa. Transplantation, 89, 911–919.
22. Jang, Y.P., Matsuda, H., Itagaki, Y., Nakanishi, K. and Sparrow, J.R. (2005)Characterization of peroxy-A2E and furan-A2E photooxidation productsand detection in human and mouse retinal pigment epithelial cell lipofuscin.J. Biol. Chem., 280, 39732–39739.
23. van der Burght, B.W., Hansen, M., Olsen, J., Zhou, J., Wu, Y., Nissen, M.H.and Sparrow, J.R. (2013) Early changes in gene expression induced by bluelight irradiation of A2E-laden retinal pigment epithelial cells. ActaOphthalmol., 91, e537–e545.
24. Westlund, B.S., Cai, B., Zhou, J. and Sparrow, J.R. (2009) Involvement ofc-Abl, p53 and the MAP kinase JNK in the cell death program initiated inA2E-laden ARPE-19 cells by exposure to blue light. Apoptosis, 14, 31–41.
25. Sparrow, J.R., Kim, S.R., Cuervo, A.M. and Bandhyopadhyayand, U. (2008)A2E, a pigment of RPE lipofuscin, is generated from the precursor, A2PE bya lysosomal enzyme activity. Adv. Exp. Med. Biol., 613, 393–398.
26. Jang, Y.P., Zhou, J., Nakanishi, K. and Sparrow, J.R. (2005) Anthocyaninsprotect against A2E photooxidation and membrane permeabilization inretinal pigment epithelial cells. Photochem. Photobiol., 81, 529–536.
27. Justilien, V., Pang, J.J., Renganathan, K., Zhan, X., Crabb, J.W., Kim, S.R.,Sparrow, J.R., Hauswirth, W.W. and Lewin, A.S. (2007) SOD2 knockdownmouse model of early AMD. Invest. Ophthalmol. Vis. Sci., 48, 4407–4420.
28. Tao, G.Z., Lehwald, N., Jang, K.Y., Baek, J., Xu, B., Omary, M.B. andSylvester, K.G. (2013) Wnt/beta-catenin signaling protects mouse liveragainst oxidative stress-induced apoptosis through the inhibition of forkheadtranscription factor FoxO3. J. Biol. Chem., 288, 17214–17224.
29. Brunet, A. (2004) The multiple roles of FOXO transcription factors. Med.Sci., 20, 856–859.
30. Zhang, S., Zhao, Y., Xu, M., Yu, L., Zhao, Y., Chen, J., Yuan, Y., Zheng, Q.and Niu, X. (2013) FoxO3a modulates hypoxia stress induced oxidativestress and apoptosis in cardiac microvascular endothelial cells. PloS One, 8,e80342.
31. Essers, M.A., de Vries-Smits, L.M., Barker, N., Polderman, P.E., Burgering,B.M. and Korswagen, H.C. (2005) Functional interaction between beta-catenin and FOXO in oxidative stress signaling. Science, 308, 1181–1184.
32. Imamura, Y., Noda, S., Hashizume, K., Shinoda, K., Yamaguchi, M.,Uchiyama, S., Shimizu, T., Mizushima, Y., Shirasawa, T. and Tsubota, K.(2006) Drusen, choroidal neovascularization, and retinal pigmentepithelium dysfunction in SOD1-deficient mice: a model of age-relatedmacular degeneration. Proc. Natl Acad. Sci. USA, 103, 11282–11287.
33. Bailey, T.A., Kanuga, N., Romero, I.A., Greenwood, J., Luthert, P.J. andCheetham, M.E. (2004) Oxidative stress affects the junctional integrity ofretinal pigment epithelial cells. Invest. Ophthalmol. Vis. Sci., 45, 675–684.
34. Sparrow, J.R. and Boulton, M. (2005) RPE lipofuscin and its role in retinalpathobiology. Exp. Eye Res., 80, 595–606.
35. Eldred, G.E. (1993) Age pigment structure. Nature, 364, 396.36. Wolf, G. (1993) The structure of the age pigment, lipofuscin, and its
accumulation site in the human eye. Nutr. Rev., 51, 348.37. Joshi, D., Field, J., Murphy, J., Abdelrahim, M., Schonherr, H., Sparrow,
J.R., Ellestad, G., Nakanishi, K. and Zask, A. (2013) Synthesis ofantioxidants for prevention of age-related macular degeneration. J. Nat.Prod., 76, 450–454.
38. Moran, D., Cross, T., Brown, L.M., Colligan, R.M. and Dunbar, D. (2014)Data-independent acquisition (MSE) with ion mobility provides asystematic method for analysis of a bacteriophage structural proteome.J. Virol. Methods, 195, 9–17.
Human Molecular Genetics, 2014, Vol. 23, No. 13 3455
by guest on June 6, 2016http://hm
g.oxfordjournals.org/D
ownloaded from