Intestinal mucosal damage caused by non-steroidal anti-inflammatory drugs: Role of bile salts
Transcript of Intestinal mucosal damage caused by non-steroidal anti-inflammatory drugs: Role of bile salts
Clinical Biochemistry 40 (2007) 503–510
Review
Intestinal mucosal damage caused by non-steroidal anti-inflammatory drugs:Role of bile salts
Michele Petruzzelli a, Michele Vacca a, Antonio Moschetta a, Rosa Cinzia Sasso a,Giuseppe Palasciano a, Karel J. van Erpecum b, Piero Portincasa a,⁎
a Clinica Medica “A. Murri”, Department of Internal Medicine and Public Medicine (DIMIMP), University Medical School of Bari, Italyb Department of Gastroenterology and Surgery, University Medical Center, Utrecht, The Netherlands
Received 17 October 2006; received in revised form 22 December 2006; accepted 15 January 2007Available online 31 January 2007
Abstract
The strong analgesic, anti-inflammatory effects of non-steroidal anti-inflammatory drugs (NSAIDs) are hampered by high occurrence ofgastrointestinal side effects. Therapeutic actions of NSAIDs result from cyclooxygenase (COX) enzymes inhibition with reduced synthesis ofprostaglandins, major modulators of inflammation. Since prostaglandins also regulate key events in gut homeostasis –mucosal secretion, bloodflow, epithelial regeneration – COX inhibition has been accepted as the reason for NSAID gastrointestinal toxicity. Several findings challenge thistheory: first, intestinal damage by NSAIDs occurs also in COX-1 knockout mice, demonstrating that topical (non-prostaglandin mediated)mechanisms are involved; second, no correlation is found in vivo between the extent of intestinal injury and the degree of inhibition ofprostaglandin synthesis; third, bile flow interruption in animal models completely prevents intestinal damage by parenterally administeredNSAIDs. What is in bile that could play a role in NSAID toxicity? This timely review will critically discuss the role of bile salts in NSAID-dependent gut damage.© 2007 The Canadian Society of Clinical Chemists. Published by Elsevier Inc. All rights reserved.
Keywords: Non-steroidal anti-inflammatory drugs (NSAIDs); Bile salts; Intestinal toxicity; Phospholipids; Farnesoid X Receptor; Cyclooxygenase (COX)
Contents
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 504Effects of NSAIDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 504
Mechanism of action . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 504Clinical toxicity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 504Pathogenesis of intestinal toxicity by NSAIDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 505
Beneficial and detrimental effects of bile salts . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 505Phospholipids protect against bile salt toxicity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 506
The intriguing connection: phospholipids, bile salts, NSAIDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 507Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 508References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 508
Abbreviations: BDL, bile-duct ligation; COX, cyclooxygenase; FXR, Farnesoid X Receptor; IMC, intermixed micellar–vesicular bile salt concentration; LDH,lactate dehydrogenase; mdr2, multidrug-resistance 2 gene; NSAID, non-steroidal anti-inflammatory drug; TDC, taurodeoxycholate.⁎ Corresponding author. Piazza Giulio Cesare 11-Policlinico-70124 Bari, Italy. Fax: +39 080 5478232.E-mail address: [email protected] (P. Portincasa).
0009-9120/$ - see front matter © 2007 The Canadian Society of Clinical Chemists. Published by Elsevier Inc. All rights reserved.doi:10.1016/j.clinbiochem.2007.01.015
Table 1Clinical manifestations of NSAID toxicity in the gastrointestinal tract
Esophagus Mucosal erosions [71]Ulcer disease [15,72]Benign stenosis [16,17]
Stomach andduodenum
Dyspeptic symptoms [18,19,73]Mucosal erosions [74]Chronic blood loss [75,76]Peptic ulcer disease [21,22,26]Upper gastrointestinal perforation [77]Upper gastrointestinal bleeding [3,23,78–80]
Small intestine Ulcer disease [26,81,82]Chronic blood loss [75,76,83]Small bowel enteropathy [27,28,83]Intestinal perforation [77,82]
Colon Worsening inflammatory bowel disease [30,84,85]Perforation of diverticula [29,86]
504 M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs) are pre-scribed worldwide for the management of pain, inflammationand fever, as well as cardio-vascular protection. AlthoughNSAIDs are highly effective, their use can be associated withhigh occurrence of intestinal side effects: mucosal erosions thatcan progress into ulcers and life-threatening complications asperforation and hemorrhage. Given the high number of patientstreated chronically with NSAIDs, gastrointestinal side effectsconstitute a chief concern for public health, estimated as thefifteenth most common cause of death in the United States [1].Furthermore, the large availability of NSAIDs as over-the-counter drugs puts millions of individuals at risk for this “silentepidemic” worldwide [2,3].
This review will first describe NSAID mechanism of actionthrough cyclooxygenase (COX) inhibition and highlight theirclinical benefits and intestinal side effects. Evidence will bethen presented to argue against COX inhibition as the sole causefor NSAID toxicity on the gastrointestinal tract. As orallyadministered NSAIDs come in close contact with bile in thegastrointestinal tract, we will focus on the potential role of bilesalts as key cytotoxic players in the pathogenesis of gut injuryinduced by NSAIDs. Last, the protective role of phospholipidsin the interaction between NSAIDs and bile salts will beexamined, also in light of future pharmacological approaches.
Effects of NSAIDs
Mechanism of action
Although different in chemical structure, all NSAIDs sharethe common pharmacological property of inhibiting COX, therate-limiting enzyme in synthesis of prostaglandins, keymediators of the inflammatory process. The most representativecompound, salicylic acid (aspirin), was isolated in the first half of19th century, but it was not until early 1970s that its clinicaleffects were linked to COX enzyme inhibition [4,5]. Aspirin wasfound to reduce the synthesis of prostaglandin E2 and I2,responsible for leukocyte infiltration at the site of inflammation,tissue swelling and increased pain perception elicited bycytokines like bradykinin [6]. Enthusiasm for the discoverydiminished because of the recognition that the same mechanismwas responsible both for NSAIDs therapeutic action and toxicity.In fact, prostaglandins are endogenous molecules that play a keyrole for gut mucosa homeostasis [7]. In the stomach prostaglan-dins are responsible for vasodilatation and PG-I2, in particular,controls mucosal blood flow. Prostaglandin E2 and prostaglan-din F2 increase mucus and bicarbonate secretion both in thestomach and intestine.Moreover, prostaglandins are essential formucosal integrity since they favor epithelial regeneration andhealing. All these events are lost or reduced during COXinhibition by NSAIDs. A strategy was therefore needed toselectively inhibit prostaglandin activity in the inflammatoryprocess, while saving their beneficial actions in the gastro-intestinal tract. The finding that acetaminophen selectivelyinhibited prostaglandin synthesis in the central nervous system
but not in peripheral tissues supported the hypothesis thatdifferent COXgene isoforms existed [8]. The possibility that twodifferent COX genes encoding two distinct groups of prosta-glandins existed was further supported by sodium salicylateselective inhibition of prostaglandin synthesis at the site ofinflammation but not in the gastric mucosa [9]. Definitive proofcame in 1991 by themolecular characterization of a gene isoformdifferent from the first cloned [10]. COX-1 isoform was found tobe constitutively expressed in several tissues, including stomach,kidney, blood vessels and platelets, while COX-2 was notexpressed in normal conditions but it was induced uponinflammation [11]. Since protective prostaglandins were theproduct of COX-1 activity andwere crucial for intestinal mucosaregeneration and defense against pathogens, hope arose aboutthe possibility of selective inhibition of COX-2 isoform. Thisinhibition could reduce the clinical effects of inflammation whilesparing the gut mucosa from deleterious side effects [12,13].
Clinical toxicity
All segments of the gastrointestinal tract are exposed topotential NSAID toxicity (Table 1) and clinical pictures rangefrom dyspepsia to serious complications such as perforation andhemorrhagic episodes [14]. NSAIDs are able to cause epithelialdamage which spans from the esophagus to the colon.Esophageal mucosal damage includes erosions, which canprogress into ulcers and – if untreated – benign esophagealstenosis [15–17]. However, stomach and duodenum are themost often involved anatomical sites and NSAID toxicityincludes asymptomatic mucosal damage as well as life-threatening complications of ulcer. The occurrence of dyspepticsymptoms in patients chronically treated with NSAIDs isrelatively low, approximately 15% [18,19]; indeed, the numberof serious gastrointestinal events anticipated by early warningsigns is the minority [20]. Hence, absence of dyspepsia does notrule out the possibility that serious gastrointestinal complica-tions can emerge. Common manifestations of NSAID toxicityon the gastro-duodenal mucosa are erosions, which can becomplicated by bleeding and secondary anemia because ofchronic blood loss [2]. The overall risk for development ofserious conditions such as ulcer disease and gastric perforation
505M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
is 4 and 6 times higher in NSAID users than in the generalpopulation [21,22]. Absolute risk for ulcer complication inNSAID users is 2% per year [23]. Several risk factors havebeen found to increase the likelihood of NSAID relatedulcer: advanced age, alcohol ingestion, previous episodes ofintestinal ulcer disease, concomitant cardio-vascular disease,anticoagulant or corticosteroid therapy. Although the role ofHelicobacter pylori infection in the development of NSAID-associated peptic ulcer has been long under debate, recentreports suggest a synergic effect between these two risk factors[24,25]. Due to technical difficulties in direct visualization, theextent and severity of complications in more distal segments ofthe intestine have been long underestimated. Autopsy studiesrevealed that 8.4% of regular NSAID consumers had ulcers injejunum or ileum, compared with 0.6% of not-treated, whilegastro-duodenal ulcers were found in 14% and 10% of the twogroups respectively. Of note, these studies showed that theabsence of upper intestinal damage does not rule out thepossibility that complications are present in more distalsegments [26]. Distal toxicity must be suspected in all patientstreated with NSAIDs, displaying clinical signs of intestinalinjury but normal upper endoscopy: iron deficiency anemia inthese subjects can be as severe as in neoplastic patients.
Small bowel enteropathy is a distinct possible complicationof NSAID consumption characterized by inflammation of thesmall intestine, increased mucosal permeability, protein loss andmalabsorption [27,28]. Colonic localization of NSAIDs inducedmucosal damage is often asymptomatic. Caution must be usedin patients with pre-existing colonic diseases like inflammatorybowel disease, in which the use of NSAIDs may burst theunderling condition, leading to increased hospitalization ratesand critical outcomes like intestinal perforation [29–31].
Pathogenesis of intestinal toxicity by NSAIDs
The deleterious effects of NSAID therapy on the gastro-intestinal mucosa have been ascribed to inhibition of endogenousprostaglandin synthesis [32]. Prostaglandins regulate key eventsin mucosal resistance against endogenous as well as exogenousfactors, including epithelial secretion of mucus and bicarbonate,epithelial proliferation and mucosal blood flow. Although thesestrong defensive properties point out the importance ofendogenous prostaglandins for the integrity of the intestinalmucosa [33] and suggest COX-1 inhibition as the explanation forincreased vulnerability toward irritants [34], the exact mechanismof NSAID-induced gastrointestinal damage remains puzzling.Indeed, several studies show that gut damage induced by NSAIDconsumption is independent of COX inhibition. Experimentsperformed in the animal model show no correlation between theextent of intestinal mucosa injury and the degree of inhibition ofprostaglandin synthesis. Although intrarectal administration ofeither indomethacin, aspirin, ibuprofen, diclofenac, ketoprofen orsulindac induces significant and comparable degree of inhibitionof prostaglandin E2 synthesis, no damage is detected in sulindac-and aspirin-treated rats and no dose dependency is observed forketoprofene-induced damage [35]. Interestingly, dose dependentrelation between inhibition of prostaglandin E2 synthesis and
intestinal toxicity is the case only for indomethacin anddiclofenac, two NSAIDs known to undergo extensive enterohe-patic circulation [35–37]. Furthermore, while both oral andparenteral aspirin administration cause major inhibition of COXactivity in the rat,mucosal damage is observed onlywhen the drugis given orally [38]. Thus, chemical and pharmacokineticproperties of individual compounds are responsible for thedissimilar ulcerogenity displayed by different NSAIDs. The roleof enterohepatic circulation in the pathogenesis of NSAID-induced gastrointestinal damage is emphasized in experiments ofbile-duct ligation (BDL), an experimental surgical procedure thatinterrupts bile flow, thus blocking enterohepatic circulation. BDLcompletely prevents gastrointestinal mucosal injury induced bysystemic administration of NSAIDs [39]. Furthermore, gastricmucosal ulceration produced in rats following intraperitonealinjection of indomethacin is gradually reduced as bile flow issurgically diverted progressively more distal to the ampulla ofVater [40]. Taken together, these findings show that absence ofbile flow (following BDL or pylorus ligation) prevents gastro-intestinal side effects of NSAIDs and suggest that othercompounds present in bile could contribute to mucosal toxicity.
More definitive evidence that NSAIDs elicit their detrimentaleffect on the gastrointestinal tract in part because of topicaldamage of the mucosa comes from recent experimentsperformed in COX-1 knockout mice [41]. Although the toxicityof intragastric administration of aspirin was more severe inCOX-1 knockout compared to wild-type and COX-2 knockoutmice, this effect was not associated with decreased prostaglandinlevels. On the contrary, aspirin induced a paradoxical 4–6-foldincrease in prostaglandin E2 levels in COX-1 knockout, butdecreased prostaglandin E2 levels in wild-type and COX-2knockout mice. Despite increased prostaglandin levels, theextent of gastric injury was more severe in COX-1 knockoutmice. A possible explanation for the increased toxicity observedin COX-1 knockout mice could be the more profound decreasein surface hydrophobicity observed in these mice as compared towild-type and COX-2 knockout. The results of this workdefinitively show that topical, non-prostaglandin mediatedmechanisms are also responsible for NSAID-induced gastro-intestinal toxicity.
Beneficial and detrimental effects of bile salts
Bile salts are powerful detergent molecules that solubilizehydrophobic lipids as cholesterol and phospholipids in micellesin the biliary tract and intestine, thus allowing bile formation,cholesterol disposal and intestinal lipid absorption [42]. Bilesalts are secreted in bile together with phospholipids andcholesterol and stored in the gallbladder in the fasting state. Afterfeeding, bile is delivered in the duodenum where bile saltmicelles allow physiological processing of nutrients like lipidsand lipophilic vitamins. Bile salts go along with intestinalcontent through the small intestine up to the terminal ileumwhere they are actively taken up by the enterocytes. After uptakeat the apical surface, selective intracellular trafficking of bilesalts delivers these molecules to the basolateral side, where theyare secreted in the blood stream. Through the portal circulation
506 M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
bile salts reach the liver where their uptake is highly efficient sothat only minimal amounts escape from the hepatic sinusoidalblood stream and enter the general circulation. The process ofhepatic secretion of bile salts, uptake in the distal ileum,secretion in the portal circulation, hepatic uptake and re-secretion in bile is known as the enterohepatic circulation ofbile salts. Cholesterol homeostasis, absorption of dietary lipidsand enterohepatic circulation of bile salts are troubled by asignificant risk of potential toxicity. In fact, given their strongdetergent activity, bile salts have the potential for solubilizingcell membranes of the epithelia of the biliary and gastrointestinaltract during their intestinal progression [42,43]. Bile salts existeither as monomers or – above their “critical” micellarconcentration – as simple micelles, i.e. aggregates of only bilesalts. Both monomers and simple micelles are responsible forbile salt detergency: these two physical forms are usuallyreferred as “intermixed micellar–vesicular bile salt concentra-tion (IMC)” (Fig. 1). The molecular mechanism of bile saltdetergency on the plasma membrane was first characterized in invitro models of cytotoxicity. The toxic activity of bile salts isstrongly dependent on their degree of hydrophobicity [44], asdemonstrated also by our group [43,45,46]: more hydrophobicbile salts like taurodeoxycholate cause cellular damage at lowerconcentration than more hydrophilic taurocholate; in contrast,tauroursodeoxycholate and taurohyodeoxycholate, both hydro-philic bile salts, cause no cytotoxicity, even at very highconcentrations. The toxicity of hydrophobic bile salts has beenshown for several cell types and tissues, including hepatocytes,erythrocytes, gastric, intestinal and gallbladder mucosa [47].
Phospholipids protect against bile salt toxicity
At physiological concentrations, both in gallbladder and bileducts, as well as within intestinal lumen, bile salts couldtheoretically damage the epithelia if separated from phospho-lipids. Phospholipids, in fact, bind bile salts to form mixed
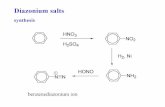
Fig. 1. Physiochemical forms of bile salts in human bile and intestinal mucosa. In thmicelles, composed exclusively by bile salts. This condition is defined “intermixed mfor bile salt cytotoxicity. Mixed micelles form when phospholipids are bound togethermicellar incorporation of indomethacin and are responsible of high toxicity.
micelles, a condition known to decrease the amount of simplemicelles and monomers (IMC), resulting in protection againstbile salts detergency (Fig. 1) [43,46–48]. The ability ofphospholipids to reduce bile salt monomeric activity andmitigate their cytotoxic action was investigated initially in vitro,and later confirmed in vivo. Mice with homozygous disruptionof the multidrug-resistance 2 (mdr2) gene disclose the crucialprotective role of phospholipids. In fact, mdr2 gene encodes anATP Binding Cassette transporter (ABC-B4) protein located atthe canalicular membrane of the hepatocyte, responsible forphospholipid efflux into the biliary canalicular lumen. Due tothe absence of mdr2 protein, mdr2 knockout mice havevirtually no phospholipids in bile and die of liver insufficiency[49]. Moreover, mdr2 knockout mice confirmed in vivo thefinding obtained in vitro of increased bile salt toxicity withincreasing hydrophobicity: dietary addition of the hydrophobicbile salt cholate, in fact, causes more severe liver pathologybecause of increased biliary secretion of – hydrophobic–taurocholate [50].
The mandatory linkage between bile salts and phospholipidsis established at gene level. Bile salts are endogenous ligandsfor the nuclear receptor Farnesoid X Receptor (FXR) [51]. FXRcontrols bile salt homeostasis in the liver, regulating thetranscription of genes involved in bile salt uptake, synthesisand biliary secretion [52]. In case of high intracellular bile saltconcentration, enhanced activity of FXR prevents their reten-tion up-regulating the expression of the canalicular transportprotein responsible for biliary secretion of bile salts [53]. Mostnotably, since higher concentration of bile salts would beharmful for biliary epithelium, FXR also enhances mdr2 geneexpression, thus coupling biliary secretion of both bile salts and“protective” phospholipids [54–56].
As a physiological process, enterohepatic circulation is notexclusive of bile salts but is also displayed by many othercompounds, both endogenous (for example bilirubin) andexogenous, most notably some NSAIDs [36,57,58].
e absence of phospholipids, bile salts are present either as monomers or simpleicellar–vesicular bile salt concentration (IMC)” and is thought to be responsiblewith bile salts and result in decreased toxicity. “Super-toxic micelles” result from
Fig. 2. Effect of indomethacin upon taurodeoxycholate (TDC) toxicity in twocomplementary in vitro models. (A) Hemolysis model: erythrocytes wereincubated for 30 min with increasing concentration of the hydrophobic bile saltTDC (from 0.5 to 10 mM), in the presence or absence of indomethacin (fixedconcentration of 5 mM). Values are expressed as percentage of 100% hemolysisobtained after incubation of erythrocytes with water. At increasing TDCconcentrations, hemolysis is progressively increased. For each TDC concentra-tion, TDC-induced hemolysis is significantly enhanced in the presence ofindomethacin. (B) LDH release from differentiated CaCo2 cells: LDH is acytoplasmic enzyme which is released in the case of cellular toxicity. Values areexpressed as percentage of 100% cytotoxicity obtained after incubation ofCaCo2 cells with 10% tritonX-100. At increasing TDC concentrations (from0.25 to 2.5 mM), cytotoxicity is progressively increased. Also in this model, foreach TDC concentration, TDC-induced LDH release is significantly increased inthe presence of indomethacin (data from Petruzzelli et al., unpublished).
507M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
The intriguing connection: phospholipids, bile salts,NSAIDs
The mucosa of the gut is covered by a thick, continuous andadherent viscous mucus secretion called mucus gel layer [59].Other than lubrificating the inside of the digestive tube thusfacilitating the passage of nutrients, mucus gel layer acts as aphysical barrier that prevents noxious agents present in thelumen to get in contact with the underlining epithelia. Theprotection offered by the mucus gel layer relies on its surfactant-like properties, specifically dependent on the presence ofphospholipids [60]. The term surfactant is a contraction of“surface active agent” and has been initially used to describe thesecretion of type II alveolar cells of the lung [61]. Surfactant isresponsible for alveolar stability and overall lung compliance:dipalmitoyl-phosphatidylcholine, the major pulmonary phos-pholipid, lines the inside of the alveoli and reduces surfacetension at the air–liquid interface since it offers the hydrophilicheadgroup to the liquid surface while the hydrophobic tail facestowards the air. Similarly to its role in the lung, the hydrophobiccovering of the gut lumen is crucial for the homeostasis of thegastrointestinal mucosa [59,62]. Intestinal mucus gel layerhydrophobicity is attributed predominantly to phosphatidylcho-line, the major phospholipid present in bile, and the mostimportant agent for prevention of bile salts detergency on bothbiliary and gastrointestinal epithelia [48,63].
Phosphatidylcholine protection is also effective againstNSAID-induced gastrointestinal toxicity: gastric injury causedby aspirin in COX-1 knockout mice, in fact, can be prevented ifaspirin is associated with phosphatidylcholine [41]. Works fromdifferent laboratories support the concept that NSAIDs exerttheir detrimental action on the gastrointestinal mucosa becausethey reduce the protection of phosphatidylcholine against bilesalt cytotoxicity [60,64]. In line with this hypothesis, phospha-tidylcholine is able to reduce bile salts toxicity on rat ilealmucosa mounted in Ussing chamber, but further addition ofindomethacin disrupts this protective effect [65]. Furthermore,in a second in vitro model of intestinal mucosa, CaCo2 –cultured colon carcinoma cell line with small intestinal cellphenotype –more phospholipids are needed to prevent bile saltstoxicity in the presence of indomethacin. In principle, twodifferent mechanisms may explain the reduced protection ofphosphatidylcholine toward bile salt detergency in the presenceof NSAIDs: either NSAIDs remove phosphatidylcholine frommixed micelles, thereby producing toxic simple micelles, orNSAIDs chemically interact with bile salts, leading to increasedmicellar toxicity. It has been suggested that NSAID sequestra-tion of phosphatidylcholine from mixed micelles increases theconcentration of bile salt in the IMC fraction, thought to beresponsible for bile salt detergency [60]. In other words,according to this hypothesis, NSAIDs do not modify pathogeniccharacteristics of bile salts, but exert their side effects in part bydecreasing the protection of phosphatidylcholine. Alternatively,micellar incorporation of NSAIDs may result in “super-toxic”micelles, which require more phospholipids for protection (Fig.1). Recent evidences support the latter hypothesis: in vitro,indomethacin added to bile salt–phospholipid mixed micelles
aggravates detergency without any direct change of bile saltconcentration or composition in the IMC fraction. Furthermore,indomethacin enhances bile salt detergency in vitro, even in theabsence of phospholipids. The effect of indomethacin upondetergency caused by increasing concentration of taurodeox-ycholate (TDC) in two complementary in vitro models oftoxicity (i.e. erythrocytes and CaCo2 cells) is shown in Figs. 2Aand B. While indomethacin alone does not cause any hemolysis(Fig. 2A) nor LDH release (Fig. 2B), indomethacin addition toTDC strongly increases bile salt toxicity. Hence, in theseconditions, the enhancement of bile salt toxicity by NSAID isindependent of phospholipid presence into micelles [66]. Thesefindings suggest that increased bile salt toxicity in the presenceof indomethacin may depend on physico-chemical interactionbetween bile salt and indomethacin molecules: incorporation of
Fig. 3. The protection induced by phospholipids against bile salt toxicity is reduced in the presence of indomethacin. In normal conditions, the canalicular lumen andintestinal mucosa are protected against bile salt cytotoxicity by phospholipids, effluxed in bile by the canalicular membrane transporter mdr2 and incorporated intomixed micelles. In the presence of indomethacin, which is also secreted into bile, micellar bile salt toxicity is enhanced and the amount of phospholipids present isinsufficient to protect intestinal mucosa from bile salt damage.
508 M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
indomethacin within bile salt micelles results in enhanceddetergency.
Normally, the biliary ratio of phospholipids and bile salts isapproximately 1 molecule of phosphatidylcholine for each 3molecules of bile salts and is sufficient to prevent micellardetergency. The required amount of phospholipids needed toavoid bile salt toxicity may increase in case of “super-toxic” bilesalt–indomethacin micelles (Fig. 3). Alternatively, indometha-cin may deposit on the cell membrane thus rendering it morevulnerable to bile salt toxicity. This seems unlikely, though,since pre-incubation of erythrocytes with indomethacin doesnot alter detergency caused by subsequent incubation with bilesalts (personal observations).
It is worth noting at this point that increased micellar toxicityin the presence of NSAIDs would also damage the canalicularepithelium. Although several reports address this possibility,hepato-biliary toxicity is not a common side effect of NSAIDtherapy [67–69]. Hepatocyte canalicular membrane as well asbiliary epithelia, regularly face micellar potential toxicity, thus,it is plausible that they are more resistant than intestinal mucosatoward NSAID–bile salt detergency. Such increased resistancemay result from the enrichment of hepatocyte plasmamembrane with sphingomyelin, which has been shown invitro to exert increased protection against bile salt detergencycompared to phosphatidylcholine [47,70].
Conclusions
NSAIDs are widely used in the clinical practice but areresponsible for significant gastrointestinal toxicity. A number ofevidences unambiguously show that COX inhibition is not the
exclusive explanation for gut damage caused by NSAIDs.Further mechanismsmust be investigated to gain knowledge anddevelop effective strategies to reduce the epidemic of NSAID-dependent gut mucosal damage. Experimental interruption ofenterohepatic circulation completely prevents NSAID toxicityon gut mucosa, thus disclosing the pathogenetic role of bile salts.Indeed, indomethacin may be incorporated in “super-toxic”micelles, which require more phospholipids for completeprotection. FXR protects liver and gut from bile salt toxicity: itsenses increased hepatic concentration of bile salts and preventscytotoxicity by increasing phospholipid output in bile. WhenNSAIDs are present in bile, no regulatory mechanism is at worksince the concentration of bile salts is unmodified, as well as thatof phospholipids. Strategies aiming to increase biliary phospho-lipid concentration (such as FXR modulators) could represent aprospective pharmacologic approach to reduce gastrointestinaltoxicity during NSAID therapy.
In conclusion, exploring pathophysiological mechanismsdifferent from those widely accepted is a promising option togather insight into mechanisms of mucosal damage caused byNSAIDs in the gastrointestinal tract and design more effectivestrategies of prevention and/or treatment.
References
[1] Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastro-intestinal complications. J Rheumatol Suppl 1999;56:18–24.
[2] Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity ofnonsteroidal antiinflammatory drugs. N Engl J Med 1999;340:1888–99.
[3] Lewis JD, Kimmel SE, Localio AR, et al. Risk of serious uppergastrointestinal toxicity with over-the-counter nonaspirin nonsteroidalanti-inflammatory drugs. Gastroenterology 2005;129:1865–74.
509M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
[4] Flower R, Gryglewski R, Herbaczynska-Cedro K, Vane JR. Effects of anti-inflammatory drugs on prostaglandin biosynthesis. Nat New Biol1972;238:104–6.
[5] Smith JB, Willis AL. Aspirin selectively inhibits prostaglandin productionin human platelets. Nat New Biol 1971;231:235–7.
[6] Ferreira SH, Moncada S, Vane JR. Prostaglandins and the mechanism ofanalgesia produced by aspirin-like drugs. Br J Pharmacol 1973;49:86–97.
[7] Campbell WB, Halushka PV. Lipid-derived autacoids: eicosanoids andplatelet-activating factor. In: Hardman JG, Limbird LE, editors. Goodmanand Gilman: The Pharmacological Basis of Therapeutics. 9th ed. TheMcGraw-Hill Companies; 1997. p. 595–604. Chap. 26.
[8] Flower RJ, Vane JR. Inhibition of prostaglandin synthetase in brainexplains the anti-pyretic activity of paracetamol (4-acetamidophenol).Nature 1972;240:410–1.
[9] Whittle BJ, Higgs GA, Eakins KE, Moncada S, Vane JR. Selectiveinhibition of prostaglandin production in inflammatory exudates andgastric mucosa. Nature 1980;284:271–3.
[10] Xie WL, Chipman JG, Robertson DL, Erikson RL, Simmons DL.Expression of a mitogen-responsive gene encoding prostaglandin synthaseis regulated by mRNA splicing. Proc Natl Acad Sci U S A 1991;88:2692–6.
[11] Vane JR, Mitchell JA, Appleton I, et al. Inducible isoforms ofcyclooxygenase and nitric-oxide synthase in inflammation. Proc NatlAcad Sci U S A 1994;91:2046–50.
[12] Meade EA, Smith WL, Dewitt DL. Differential inhibition of prostaglandinendoperoxide synthase (cyclooxygenase) isozymes by aspirin and othernon-steroidal anti-inflammatory drugs. J Biol Chem 1993;268:6610–4.
[13] Mitchell JA, Akarasereenont P, Thiemermann C, Flower RJ, Vane JR.Selectivity of nonsteroidal antiinflammatory drugs as inhibitors ofconstitutive and inducible cyclooxygenase. Proc Natl Acad Sci U S A1993;90:11693–7.
[14] Cryer B, Kimmey MB. Gastrointestinal side effects of nonsteroidal anti-inflammatory drugs. Am J Med 1998;105:20S–30S.
[15] Wolfsen HC, Wang KK. Etiology and course of acute bleeding esophagealulcers. J Clin Gastroenterol 1992;14:342–6.
[16] Heller SR, Fellows IW, Ogilvie AL, Atkinson M. Non-steroidal anti-inflammatory drugs and benign oesophageal stricture. Br Med J (Clin ResEd) 1982;285:167–8.
[17] Wilkins WE, Ridley MG, Pozniak AL. Benign stricture of the oesophagus:role of non-steroidal anti-inflammatory drugs. Gut 1984;25:478–80.
[18] Larkai EN, Smith JL, Lidsky MD, Sessoms SL, Graham DY. Dyspepsia inNSAID users: the size of the problem. J Clin Gastroenterol 1989;11:158–62.
[19] Talley NJ, Evans JM, Fleming KC, et al. Nonsteroidal antiinflammatorydrugs and dyspepsia in the elderly. Dig Dis Sci 1995;40:1345–50.
[20] Singh G, Ramey DR, Morfeld D, et al. Gastrointestinal tract complicationsof nonsteroidal anti-inflammatory drug treatment in rheumatoid arthritis. Aprospective observational cohort study. Arch Intern Med 1996;156:1530–6.
[21] Hawkey CJ. Non-steroidal anti-inflammatory drugs and peptic ulcers. BMJ1990;300:278–84.
[22] Langman MJ. Epidemiologic evidence on the association between pepticulceration and antiinflammatory drug use. Gastroenterology 1989;96:640–6.
[23] Carson JL, Strom BL, Soper KA, West SL, Morse ML. The association ofnonsteroidal anti-inflammatory drugs with upper gastrointestinal tractbleeding. Arch Intern Med 1987;147:85–8.
[24] Zapata-Colindres JC, Zepeda-Gomez S, Montano-Loza A, et al. Theassociation of Helicobacter pylori infection and nonsteroidal anti-inflammatory drugs in peptic ulcer disease. Can J Gastroenterol2006;20:277–80.
[25] Papatheodoridis GV, Sougioultzis S, Archimandritis AJ. Effects ofHelicobacter pylori and nonsteroidal anti-inflammatory drugs on pepticulcer disease: a systematic review. Clin Gastroenterol Hepatol 2006;4:130–42.
[26] Allison MC, Howatson AG, Torrance CJ, Lee FD, Russell RI.Gastrointestinal damage associated with the use of nonsteroidal antiin-flammatory drugs. N Engl J Med 1992;327:749–54.
[27] Fortun PJ, Hawkey CJ. Nonsteroidal antiinflammatory drugs and the smallintestine. Curr Opin Gastroenterol 2005;21:169–75.
[28] Bjarnason I, Zanelli G, Prouse P, et al. Blood and protein loss via small-intestinal inflammation induced by non-steroidal anti-inflammatory drugs.Lancet 1987;2:711–4.
[29] Day TK. Intestinal perforation associated with osmotic slow releaseindomethacin capsules. Br Med J (Clin Res Ed) 1983;287:1671–2.
[30] Kaufmann HJ, Taubin HL. Nonsteroidal anti-inflammatory drugs activatequiescent inflammatory bowel disease. Ann Intern Med 1987;107:513–6.
[31] Evans JM, McMahon AD, Murray FE, McDevitt DG, MacDonald TM.Non-steroidal anti-inflammatory drugs are associated with emergencyadmission to hospital for colitis due to inflammatory bowel disease. Gut1997;40:619–22.
[32] Schoen RT, Vender RJ. Mechanisms of nonsteroidal anti-inflammatorydrug-induced gastric damage. Am J Med 1989;86:449–58.
[33] Robert A, Nezamis JE, Lancaster C, Hanchar AJ. Cytoprotection byprostaglandins in rats. Prevention of gastric necrosis produced by alcohol,HCl, NaOH, hypertonic NaCl, and thermal injury. Gastroenterology1979;77:433–43.
[34] Rainsford KD, Willis C. Relationship of gastric mucosal damage inducedin pigs by antiinflammatory drugs to their effects on prostaglandinproduction. Dig Dis Sci 1982;27:624–35.
[35] Ligumsky M, Sestieri M, Karmeli F, et al. Rectal administration ofnonsteroidal antiinflammatory drugs. Effect on rat gastric ulcerogenicityand prostaglandin E2 synthesis. Gastroenterology 1990;98:1245–9.
[36] Reuter BK, Davies NM, Wallace JL. Nonsteroidal anti-inflammatory drugenteropathy in rats: role of permeability, bacteria, and enterohepaticcirculation. Gastroenterology 1997;112:109–17.
[37] Beck WS, Schneider HT, Dietzel K, Nuernberg B, Brune K. Gastro-intestinal ulcerations induced by anti-inflammatory drugs in rats.Physicochemical and biochemical factors involved. Arch Toxicol1990;64:210–7.
[38] Ligumsky M, Golanska EM, Hansen DG, Kauffman Jr GL. Aspirin caninhibit gastric mucosal cyclo-oxygenase without causing lesions in rat.Gastroenterology 1983;84:756–61.
[39] Djahanguiri B, Abtahi FS, Hemmati M. Prevention of aspirin-inducedgastric ulceration by bile duct or pylorus ligation in the rat. Gastroenter-ology 1973;65:630–3.
[40] Abtahi FS, Djahanguiri B. Decreased incidence of indomethacin-inducedgastric ulceration in rats by bile duct diversion. Br J Surg 1975;62:113–4.
[41] Darling RL, Romero JJ, Dial EJ, et al. The effects of aspirin on gastricmucosal integrity, surface hydrophobicity, and prostaglandin metabolismin cyclooxygenase knockout mice. Gastroenterology 2004;127:94–104.
[42] Hofmann AF. Bile acids: the good, the bad, and the ugly. News Physiol Sci1999;14:24–9.
[43] Moschetta A, vanBerge-Henegouwen GP, Portincasa P, et al. Hydrophilicbile salts enhance differential distribution of sphingomyelin andphosphatidylcholine between micellar and vesicular phases: potentialimplications for their effects in vivo. J Hepatol 2001;34:492–9.
[44] Coleman R, Iqbal S, Godfrey PP, Billington D. Membranes and bileformation. Composition of several mammalian biles and their membrane-damaging properties. Biochem J 1979;178:201–8.
[45] Moschetta A, Frederik PM, Portincasa P, vanBerge-Henegouwen GP, VanErpecum KJ. Incorporation of cholesterol in sphingomyelin-phosphati-dylcholine vesicles has profound effects on detergent-induced phasetransitions. J Lipid Res 2002;43:1046–53.
[46] Velardi AL, Groen AK, Elferink RP, et al. Cell type-dependent effect ofphospholipid and cholesterol on bile salt cytotoxicity. Gastroenterology1991;101:457–64.
[47] Moschetta A, vanBerge-Henegouwen GP, Portincasa P, et al. Sphingo-myelin exhibits greatly enhanced protection compared with egg yolkphosphatidylcholine against detergent bile salts. J Lipid Res 2000;41:916–24.
[48] Martin GP, Marriott C. Membrane damage by bile salts: the protectivefunction of phospholipids. J Pharm Pharmacol 1981;33:754–9.
[49] Smit JJ, Schinkel AH, Oude Elferink RP, et al. Homozygous disruption ofthe murine mdr2 P-glycoprotein gene leads to a complete absence ofphospholipid from bile and to liver disease. Cell 1993;75:451–62.
510 M. Petruzzelli et al. / Clinical Biochemistry 40 (2007) 503–510
[50] van Nieuwerk CM, Groen AK, Ottenhoff R, et al. The role of bile saltcomposition in liver pathology of mdr2 (−/−) mice: differences betweenmales and females. J Hepatol 1997;26:138–45.
[51] Makishima M, Okamoto AY, Repa JJ, et al. Identification of a nuclearreceptor for bile acids. Science 1999;284:1362–5.
[52] Moseley RH. Bile-ology 101. Gastroenterology 2001;121:218–20.[53] Gerloff T, Stieger B, Hagenbuch B, et al. The sister of P-glycoprotein
represents the canalicular bile salt export pump of mammalian liver. J BiolChem 1998;273:10046–50.
[54] Huang L, Zhao A, Lew JL, et al. Farnesoid X receptor activatestranscription of the phospholipid pump MDR3. J Biol Chem 2003;278:51085–90.
[55] Liu Y, Binz J, Numerick MJ, et al. Hepatoprotection by the farnesoid Xreceptor agonist GW4064 in rat models of intra- and extrahepaticcholestasis. J Clin Invest 2003;112:1678–87.
[56] Moschetta A, Bookout AL, Mangelsdorf DJ. Prevention of cholesterolgallstone disease by FXR agonists in a mouse model. Nat Med 2004;10:1352–8.
[57] Brink MA, Slors JF, Keulemans YC, et al. Enterohepatic cycling ofbilirubin: a putative mechanism for pigment gallstone formation in ilealCrohn's disease. Gastroenterology 1999;116:1420–7.
[58] Carey MC, Duane W. Enterohepatic circulation. In: Arias IM, BoyerJL, Fausto N, Jakoby WB, Schachter DA, Shafritz DA editors. TheLiver: Biology and Pathobiology, 3rd ed. New York: Raven Press;1994. p. 719–67 [2006].
[59] Goddard PJ, Kao YC, Lichtenberger LM. Luminal surface hydrophobicityof canine gastric mucosa is dependent on a surface mucous gel.Gastroenterology 1990;98:361–70.
[60] Barrios JM, Lichtenberger LM. Role of biliary phosphatidylcholine inbile acid protection and NSAID injury of the ileal mucosa in rats.Gastroenterology 2000;118:1179–86.
[61] Macklin C. The pulmonary alveolar mucoid film and the pneumonocytes.Lancet 1954;266:1099–104.
[62] Lichtenberger LM, Graziani LA, Dial EJ, Butler BD, Hills BA. Role ofsurface-active phospholipids in gastric cytoprotection. Science 1983;219:1327–9.
[63] Schmitz MG, Renooij W. Phospholipids from rat, human, and caninegastric mucosa. Composition and metabolism of molecular classes ofphosphatidylcholine. Gastroenterology 1990;99:1292–6.
[64] Lugea A, Antolin M, Mourelle M, Guarner F, Malagelada JR. Derangedhydrophobic barrier of the rat gastroduodenal mucosa after parenteralnonsteroidal anti-inflammatory drugs. Gastroenterology 1997;112:1931–9.
[65] Venneman NG, Petruzzelli M, van Dijk JE, et al. Indomethacin disrupts theprotective effect of phosphatidylcholine against bile salt-induced ilealmucosa injury. Eur J Clin Invest 2006;36:105–12.
[66] Petruzzelli M, Moschetta A, Renooij W, et al. Indomethacin enhances bilesalt detergent activity: relevance for NSAIDs-induced gastrointestinalmucosal injury. Dig Dis Sci 2006;51:766–74.
[67] Cappell MS, Kozicky O, Competiello LS. Indomethacin-associatedcholestasis. J Clin Gastroenterol 1988;10:445–7.
[68] Levy C, Lindor KD. Drug-induced cholestasis. Clin Liver Dis 2003;7:311–30.
[69] Lewis JH. Hepatic toxicity of nonsteroidal anti-inflammatory drugs. ClinPharm 1984;3:128–38.
[70] Oude Elferink RP, Paulusma CC, Groen AK. Hepatocanalicular transportdefects: pathophysiologic mechanisms of rare diseases. Gastroenterology2006;130:908–25.
[71] Mason JC. NSAIDs and the oesophagus. Eur J Gastroenterol Hepatol1999;11:369–73.
[72] Higuchi D, Sugawa C, Shah SH, Tokioka S, Lucas CE. Etiology,treatment, and outcome of esophageal ulcers: a 10-year experience in anurban emergency hospital. J Gastrointest Surg 2003;7:836–42.
[73] Gupta S, McQuaid K. Management of nonsteroidal, anti-inflammatory,drug-associated dyspepsia. Gastroenterology 2005;129:1711–9.
[74] Niv Y, Battler A, Abuksis G. Endoscopy in asymptomatic minidose aspirinconsumers. Dig Dis Sci 2005;50:78–80.
[75] Bowen B, Yuan Y, James C, Rashid F, Hunt RH. Time course and patternof blood loss with ibuprofen treatment in healthy subjects. ClinGastroenterol Hepatol 2005;3:1075–82.
[76] Hunt RH, Bowen B, Mortensen ER, et al. A randomized trial measuringfecal blood loss after treatment with rofecoxib, ibuprofen, or placebo inhealthy subjects. Am J Med 2000;109:201–6.
[77] Lanas A, Serrano P, Bajador E. Evidence of aspirin use in both upper andlower gastrointestinal perforation. Gastroenterology 1997;112:683–9.
[78] Lewis SC, Langman MJ, Laporte JR, et al. Dose–response relationshipsbetween individual nonaspirin nonsteroidal anti-inflammatory drugs(NANSAIDs) and serious upper gastrointestinal bleeding: a meta-analysisbased on individual patient data. Br J Clin Pharmacol 2002;54:320–6.
[79] Lanas A, Sekar MC, Hirschowitz BI. Objective evidence of aspirin use inboth ulcer and nonulcer upper and lower gastrointestinal bleeding.Gastroenterology 1992;103:862–9.
[80] Lanas A, Bajador E, Serrano P, et al. Nitrovasodilators, low-dose aspirin,other nonsteroidal antiinflammatory drugs, and the risk of uppergastrointestinal bleeding. N Engl J Med 2000;343:834–9.
[81] Brune K, Dietzel K, Nurnberg B, Schneider HT. Recent insight into themechanism of gastrointestinal tract ulceration. Scand J Rheumatol Suppl1987;65:135–40.
[82] Nagaraj HS, Sandhu AS, Cook LN, Buchino JJ, Groff DB. Gastrointestinalperforation following indomethacin therapy in very low birth weightinfants. J Pediatr Surg 1981;16:1003–7.
[83] Morris AJ, Wasson LA, MacKenzie JF. Small bowel enteroscopy inundiagnosed gastrointestinal blood loss. Gut 1992;33:887–9.
[84] Bonner GF, Fakhri A, Vennamaneni SR. A long-term cohort study ofnonsteroidal anti-inflammatory drug use and disease activity in outpatientswith inflammatory bowel disease. Inflamm Bowel Dis 2004;10:751–7.
[85] Felder JB, Korelitz BI, Rajapakse R, et al. Effects of nonsteroidalantiinflammatory drugs on inflammatory bowel disease: a case–controlstudy. Am J Gastroenterol 2000;95:1949–54.
[86] Foutch PG. Diverticular bleeding: are nonsteroidal anti-inflammatorydrugs risk factors for hemorrhage and can colonoscopy predict outcome forpatients? Am J Gastroenterol 1995;90:1779–84.