Infliximab for severe, treatment-resistant psoriasis: a prospective, open-label study
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Infliximab for severe, treatment-resistant psoriasis: a prospective, open-label study
THERAPEUTICS DOI 10.1111/j .1365-2133.2006.07316.x
Infliximab for severe, treatment-resistant psoriasis:a prospective, open-label studyC.H. Smith, K. Jackson, S.J. Bashir, A. Perez, A.L. Chew, A.M. Powell, M. Wain and J.N.W.N. Barker
Skin Therapy Research Unit, St John’s Institute of Dermatology, St Thomas’ Hospital, Lambeth Palace Road, London SE1 7EH, U.K.
CorrespondenceCatherine Smith.
E-mail: [email protected];
Accepted for publication15 December 2005
Key wordsbiologics, infliximab, psoriasis
Conflicts of interestJNWN is a consultant for Centor and Schering
Plough.
Summary
Background Infliximab, a mouse–human chimeric monoclonal antibody directedagainst tumour necrosis factor-a, has been shown to be effective for moderate tosevere psoriasis, but there are few data published on its use in recalcitrant, treat-ment-resistant disease or in combination with other antipsoriatic therapies.Objectives To report our experience with infliximab in the treatment of patientsattending a tertiary referral service with severe recalcitrant disease.Methods All patients attending a tertiary referral service for severe psoriasis whowere treated with infliximab between 2002 and July 2005 were entered into aprospective, open-label study. Details on disease phenotype, clinical course andadverse events were recorded together with measures of disease severity [Psori-asis Area and Severity Index (PASI), Dermatology Life Quality Index, clinical pho-tography] at baseline, weeks 2 and 6, and then at 2-monthly intervalsthroughout the treatment period.Results Twenty-three patients were treated with infliximab during the study; onepatient had pustular psoriasis and was therefore excluded from statistical analysis.All had severe disease (baseline PASI 26Æ5 ± 6Æ7, mean ± SD, n ¼ 22) and hadreceived at least two systemic therapies for psoriasis in the past; 16 were takingone or more concomitant therapies at the time of treatment initiation. At week10, 95% had achieved a 50% or greater improvement in baseline PASI (PASI50), and 77% had achieved a 75% or greater improvement (PASI 75). Efficacywas sustained in the longer term, with eight of 10 patients on treatment formore than 11 months maintaining at least a PASI 50. Only one patient had treat-ment withdrawn due to lack of efficacy, two suffered severe systemic infectionsincluding extrapulmonary tuberculosis (splenic abscess) and cellulitis, and sixhave discontinued due to adverse effects including infusion reactions (two),severe thrombocytopenia (one), hepatitis (one) and malignancy (two).Conclusions Data from this open-label study suggest that infliximab is a rapidlyeffective treatment for patients with severe, treatment-resistant disease, althoughapproximately 25% of patients had to discontinue therapy due to the develop-ment of serious adverse effects. Long-term follow-up, continued pharmacovigi-lance, and further controlled comparative studies will be required to evaluatefully the risks associated with infliximab in the context of this already difficult totreat population.
Patients with severe psoriasis constitute approximately 20–
30% of all patients with psoriasis, and represent a major
economic burden to the health service.1 Standard systemic
therapies are associated with a risk of toxicity with long-term
use, many are relatively expensive, and a proportion of
patients is resistant to treatment.1 Widespread dissatisfaction
among patients with commonly used therapies also
contributes to the already substantial morbidity and impaired
quality of life associated with severe disease.2–6
Infliximab (Remicade�; Schering-Plough, Welwyn Garden
City, Herts, U.K.) is a mouse–human chimeric IgG1 mono-
clonal antibody that has high specificity, affinity and avidity
for tumour necrosis factor (TNF)-a. It binds both soluble and
transmembrane TNF-a and inhibits TNF-a from binding to
160 � 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
the p55 and p75 receptors. Two randomized, placebo-
controlled trials7,8 have shown infliximab to be highly effect-
ive in the treatment of stable, moderate to severe chronic
plaque psoriasis with 90% of patients becoming clear, or min-
imally affected at 10 weeks following a standard induction
course of therapy. The larger of these two studies included
patients who had received at least one systemic therapy prior
to study entry.8 However, relatively little is known about the
efficacy or safety of infliximab in the long term, in recalcitrant
disease or in combination with other immunosuppressant
therapies. We report our experience with infliximab in the
treatment of patients attending a tertiary referral service with
severe recalcitrant disease.
Patients and methods
Patient selection
Patients attending the Special Psoriasis Clinic at St John’s Insti-
tute of Dermatology were considered for treatment with in-
fliximab in the following clinical situations: those who had
developed, or were at significant risk of developing, clinically
important drug-related toxicity and where no alternatives
existed; those intolerant of or unresponsive to available systemic
treatments; those requiring repeated inpatient management and
those with significant, coexistent, unrelated comorbidity which
precluded use of alternative systemic agents (including ciclo-
sporin, methotrexate, fumaric acid esters, hydroxycarbamide).
Funding was applied for on an individual basis to relevant pri-
mary care trusts, and where successful, treatment initiated either
in our daycare intravenous (IV) suite, or as inpatients.
Pretreatment assessment
All patients underwent a full history with particular reference to
infection (including risk factors for tuberculosis), demyelinating
disease, cardiac disease or malignancy. Clinical examination
included verification of bacille Calmette-Guerin (BCG) scar in
those vaccinated, and assessments of disease severity and quality
of life (see below). Baseline investigations were performed as
follows: full blood count (FBC), renal and liver function,
C-reactive protein, erythrocyte sedimentation rate, antinuclear
antibodies (ANA), and specific screening for hepatitis B and
human immunodeficiency virus infection in those identified to
be at risk; clinical photography; chest X-ray (CXR).
Intervention
Following informed, written consent, infliximab (Remi-
cade�) 5 mg kg)1 was given by IV infusion over 2 h ini-
tially at weeks 0, 2 and 6. Patients were monitored for 2 h
postinfusion and then allowed home. A maintenance dose
was subsequently given at 8–10, week intervals, and varied
between 3 and 5 mg kg)1 depending on individual response
to treatment. In view of the severity of disease in this
patient cohort, any concomitant systemic therapies were
continued until adequate disease control was achieved and
then reduced or stopped over subsequent months as clinic-
ally indicated.
All patients fulfilling the treatment criteria outlined above
who received at least one infusion are included in the analysis.
Monitoring
Clinical assessments
Prior to each infusion, patients were reviewed by both a der-
matology nurse specialist and a dermatologist. Disease severity
assessments comprised Psoriasis Area and Severity Index (PASI)
(or physicians’ global evaluation score where the PASI could
not be used, i.e. in pustular psoriasis) and Dermatology Life
Quality Index (DLQI) and were completed at baseline, and at
weeks 2 and 6 and subsequently 2-monthly intervals, prior to
each further infusion. Clinical photography was performed at
baseline, week 6 and then at 2-monthly intervals.
Laboratory investigations
Monitoring investigations (FBC, renal and liver profiles, ANA)
were repeated at approximately 2-monthly intervals, prior to
infliximab infusions, together with additional investigations as
clinically indicated.
Statistical analysis
Statistical comparisons were performed with the paired t-test
using SigmaStat (SPSS, Inc., Chicago, IL, U.S.A.). Pearson’s
coefficient of correlation was performed to determine the rela-
tionship between DLQI and PASI.
Results
Patients
Since 2002, 23 patients have been treated with infliximab
therapy: 18 men, five women; age 43Æ4 ± 11Æ9 (mean ± SD)
years. All had recalcitrant disease and had received therapy
with at least two systemic therapies prior to treatment with
infliximab (Table 1). Twenty-two of the 23 patients treated
had chronic plaque psoriasis. The disease course was compli-
cated by repeated episodes of erythroderma in five patients,
and generalized pustular psoriasis during pregnancy in one.
One patient had generalized pustular psoriasis only. Associated
significant psoriatic arthritis requiring specific rheumatological
input was present in eight.
Efficacy
Of 23 patients treated, 16 remain on therapy to date (July
2005) with satisfactory disease control (Fig. 1). Only one
patient has had treatment withdrawn due to lack of efficacy
and six have been discontinued due to adverse effects.
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al. 161
Short-term efficacy
Of the 23 patients initiated on therapy, one patient had gener-
alized pustular psoriasis and is therefore not included in the
analysis that follows. Of the remaining 22, at 6 weeks (i.e.
just prior to the third infusion), 90% had achieved a 50%
improvement in baseline PASI (PASI 50) and 32% a 75%
improvement in baseline PASI (PASI 75); at week 10, 95%
had achieved PASI 50 and 77% PASI 75. The PASI fell from
26Æ5 ± 6Æ7 (mean ± SD) at baseline, to 3Æ9 ± 3Æ7 at week 10
(P < 0Æ001) (Fig. 1).
Long-term efficacy
Ten patients have completed treatment for 11 months or more
(Fig. 3); eight of these continue on therapy maintaining at least
PASI 50 throughout, and four, a PASI 75. For the remaining two
patients, one (patient 4, Fig. 3) had excellent disease control
Table 1 Summary of previous treatments used in patients entered into study. Experimental therapy includes clinical trials, most recently thoseevaluating alefacept
Patient
no.
Age(years)/
sex Arthritis
Inpatient
treatment PUVA Ciclosporin Methotrexate Acitretin
Hydroxy-
carbamide
Mycophenolate
mofetil
Fumaric
acid esters
Combination
treatment Experimental
1 48/M d d d d d d d d
2 19/M d d d d d d
3 47/M d d d d d d d d
4 46/M d d d d d d d d d d d
5 52/M d d d d d d d d
6 37/M d d d d d
7 38/M d d d
8 28/M d d d d d d
9 39/M d d d d
10 51/F d d d d d d d d
11 45/M d d d d d d d d
12 33/M d d d d d d d d
13 59/M d d d d d d d
14 46/M d d d d d d d
15 48/M d d d d d d d
16 39/M d d d d d d
17 24/M d d d d d d
18 56/M d d d d d d d
19 48/M d d d d d d d d d
20 71/M d d d d
21 44/M d d d d d d
22 43/F d d d d d d
23 38/F d d d d d
PUVA, psoralen plus ultraviolet A.
0
5
10
15
20
25
30
35
40
45
Baseline Week 2 Week 6 3 m 5 m 7 m 9 m 11 m 13 m 15 m 17 m 19 m 21 m
21 19 14 12 10 9 7 34Time
Fig 1. Psoriasis Area and Severity Index (PASI)
and Dermatology Life Quality Index (DLQI)
scores during infliximab therapy. Blue bars
denote PASI scores, and purple bars, DLQI.
Mean values shown at baseline (week 0) and
up to 21 months post-first infusion. Error bars
denote SD. Numbers of patients reduce with
time due to variable length of follow-up
(shown beneath arrows).
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
162 Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al.
(PASI 75 response) for 13 months, but subsequently his psori-
asis deteriorated despite subsequent infusions and treatment was
withdrawn. He was then established on etanercept 50 mg twice
weekly and has completed 12 months of therapy with excellent
disease control. The second patient initially responded well to
therapy but at month 6, infliximab infusions became less effect-
ive and the PASI scores reverted to his preinfusion level (patient
1, Fig. 3). However, treatment has been maintained as it has
afforded disease stability, and the patient has required inpatient
admission on only one occasion. This contrasts with the clinical
situation prior to infliximab where he had required inpatient
management for severe, unstable disease four to six times per
year. Overall, the mean ± SD 11-month PASI was 8Æ2 ± 8Æ4,significantly lower than baseline (P < 0Æ001).
Quality of life
Objective measures of improvement in disease severity were
accompanied by improvements in patient-assessed quality of
life. DLQI scores fell from 14Æ9 ± 6Æ7 (mean ± SD) at base-
line, to 3Æ4 ± 3Æ4 at week 10 (mean ± SD, P < 0Æ001,Fig. 1). This improvement was sustained for most patients
throughout the treatment period with a mean DLQI of
4Æ3 ± 5Æ2 for those patients who had received 11 months
or more of treatment (P < 0Æ001). A strong correlation was
identified over time between DLQI and PASI (R2 ¼ 0Æ81)(Fig. 4). The inconvenience of attending for IV infusions
was outweighed by the benefits of better disease control
for the majority, although the postinfusion 2-h observation
period became burdensome for some with long-term
therapy.
Experience in generalized pustular psoriasis
This patient was a 38-year-old woman with a history of
pustular psoriasis since the age of 10 years. Initially, this
was confined to the palms and soles, but became more
generalized and was resistant to phototherapy and
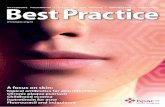
Fig 2. Patient 2 at baseline (left) and
following 5 months’ treatment with
infliximab.
Case 1
Case 2
Case 3
Case 4
Case 5
Case 6
Case 7
Case 8
Case 9
Case 10
0
5
10
15
20
25
30
35
40
45
Baseline Week 2 Week 6 3 m 5 m 7 m 9 m 11 m 13 m 15 m 17 m 19 m 21 m
Fig 3. Psoriasis Area and Severity Index
scores for patients treated with infliximab for
11 months or more (n ¼ 10).
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al. 163
combined systemic immunosuppression with ciclosporin
200 mg daily and methotrexate 30 mg weekly. An immedi-
ate improvement in her skin and quality of life was noted
following infliximab 5 mg kg)1 and her concomitant ci-
closporin was stopped (pretreatment DLQI ¼ 28, 10-week
DLQI ¼ 1, 12-month DLQI ¼ 1). Progressively, the metho-
trexate was reduced to 10 mg weekly and infliximab
reduced to 3 mg kg)1 by 12 months of treatment. At 24-
month follow-up, she had minimal disease, with a DLQI
of 6Æ0.
Nail disease
Efficacy of infliximab with respect to nail disease was not sys-
tematically assessed, but marked improvement was noted in
many patients (Fig. 5a,b).
Concomitant therapy
At initiation of infliximab, 16 patients were taking at least
one concomitant therapy, and five patients, two additional
therapies (Table 2). All patients were able either to stop or to
reduce the dose of concomitant treatment.
Treatment discontinuation and toxicity
Six patients have discontinued treatment due to adverse events
(Table 3).
Infusion reactions
In total, 171 infusions have been given to 23 patients over the
last 3 years and in general, treatment has been well tolerated.
0
2
4
6
8
10
12
14
16
18
0 5 10 15 20 25 30PASI
DL
QI
Fig 4. Mean Dermatology Life Quality Index
(DLQI) plotted against mean Psoriasis Area
and Severity Index (PASI) for all patients at all
time points, with a ‘best fit’ line. There was a
strong correlation demonstrated between
DLQI and PASI (Pearson’s correlation
coefficient R2 ¼ 0Æ81).
a
b
Fig 5. (a) Nails (patient 5) at baseline (left) and following 2 months’ treatment with infliximab. (b) Nails (patient 3) at baseline (left) and
following 7 months’ treatment with infliximab.
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
164 Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al.
Clinically significant infusion reactions occurred in two patients
(patients 20 and 22). Both occurred within 15 min of the sec-
ond and fifth infusions, respectively, and were characterized by
abdominal pain, vomiting and high temperature. Symptomatic
treatment with antihistamines (chlorpheniramine IV), and also
hydrocortisone (IV 100 mg) in the second patient, led to com-
plete resolution of all symptoms by the following morning.
Infliximab therapy was discontinued, and both patients have
been successfully established on etanercept and adalimumab,
respectively, for over a year with no evidence of local injection
site reactions or other allergic phenomena.
Autoantibody formation
Of 22 patients who were ANA-negative prior to treatment, six
have become positive, with variable titres. A further patient
noted to have weakly positive ANA titres prior to therapy has
now completed 12 months of treatment and has developed
significant titres (IgM 1 : 320; IgG 1 : 320) and additional
positive antibodies to double-stranded DNA. However, with
the exception of one patient who developed an autoimmune
hepatitis (see below), no patients have any symptoms or signs
suggestive of lupus and treatment has been continued.
Infections
Ten episodes of infection were recorded in seven patients.
Two of these were classed as severe (i.e. requiring hospital
admission) and comprised a lower leg cellulitis (patient 20)
and tuberculous abscess (patient 16). None led directly to per-
manent treatment discontinuation, although treatment had
already been discontinued in the patient with tuberculosis due
to earlier development of severe thrombocytopenia (see under
Haematological toxicity below).
Upper respiratory tract infections occurred seven times in
four patients. No abnormalities were detected on physical
examination or investigation, although infliximab infusions
were delayed on four occasions until symptoms resolved.
Lower leg cellulitis complicated the treatment course of one
elderly patient (patient 20) on monotherapy. Onset occurred
1 week following his second infusion and eventually required
2 weeks of inpatient management. Relevant comorbidity com-
prised long-standing leg varicosities and ulceration, hyper-
splenism with associated leucopenia, anaemia and
thrombocytopenia, and liver cirrhosis secondary to methotrex-
ate.
One patient developed a furuncle of the eyelid which
resolved with topical antibiotics.
Tuberculous infection
One patient (39-year-old Indian man, patient 16) developed a
tuberculous splenic abscess. Prior to (and at initiation of)
treatment with infliximab, he had been on a combination of
methotrexate (10 mg weekly) and mycophenolate mofetil
(2 g daily) for at least 3 years. His baseline CXR was normal,
and he had a visible BCG scar but did travel frequently to
India. Following three infusions of infliximab his psoriasis
cleared but he was admitted to a local hospital with epistaxis
and a swinging fever 3 weeks after his third infusion. Investi-
gations revealed a profound thrombocytopenia (platelet count
3 · 10)6 L)1) which resolved within 1 month of treatment
Table 2 Number of patients on concomitant therapy prior to andfollowing infliximab
Concomitant therapyAt
initiation StoppedDose
reducedDose
maintained
Ciclosporin 5 5 (–) (–)
Methotrexate 12 0 7 5Tacrolimus 1 1 (–) (–)
Acitretin 1 (–) 1 (–)Mycophenolate mofetil 1 1 (–) (–)
Fumaric acid esters 1 1 (–) (–)Totala 16 8 8 5
aPatients on more than one therapy counted only once.
Table 3 Summary of treatmentdiscontinuations and outcome
Reason for discontinuationDuration of treatment(number of infusions)
Current psoriasis disease statusand treatment
Inefficacy 11 Almost clear on etanercept
Adverse eventsInfusion reaction 2 Almost clear on etanercept
Infusion reaction 5 Significant but stable disease onadalimumab
Hepatitis (resolved) 4 Almost clear on etanerceptThrombocytopenia (resolved) 3 Significant but stable disease
on topical treatment andmethotrexate
CD30+ CTCL (ongoing) 3 Stable on etanercept andmethotrexate
Renal cell carcinoma 5 Deceased
CTCL, cutaneous T-cell lymphoma.
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al. 165
with pooled IV immunoglobulin. Infliximab was permanently
discontinued due to the temporal relationship with the onset
of the thrombocytopenia (see below). Despite extensive inves-
tigation, no source of infection was identified to account for
the fever which appeared to improve with time while an inpa-
tient, and his psoriasis was managed conservatively. Six
months later he was admitted to our unit, with a history of
increasing malaise, joint pains and fever. Investigations
revealed a normal CXR and echocardiogram, but supraclavicu-
lar, mediastinal and hilar lymphadenopathy on computed
tomography (CT) scan. Mycobacterium tuberculosis was subse-
quently isolated from pus aspirated from a large splenic
abscess demonstrated on abdominal ultrasound. The patient
has just completed 6 months of quadruple therapy, and has
remained on methotrexate 10 mg weekly throughout.
Liver toxicity
Significant elevations (i.e. twice greater than upper limit of
normal) in liver function tests were seen in four patients and
led to treatment discontinuation in one (patient 21). Pretreat-
ment liver morbidity was present in all and followed either
long-term methotrexate and/or alcohol excess [fatty liver only
(two), Roenigk9 stage 2 hepatitic fibrosis (one) and cirrhosis
(one)]. In the patient in whom treatment with infliximab had
to be discontinued, liver function tests prior to therapy were
normal, although he was known to have fatty liver secondary
to methotrexate and alcohol. Following his fourth infusion he
developed raised liver enzymes (maximum levels: alanine ami-
notransferase 650 uL)1; aspartate aminotransferase 370 uL)1)
which settled within 2 months of stopping treatment. His
autoantibody profile was consistent with an autoimmune
hepatitis caused by infliximab (ANA IgG 1 : 80; IgM
1 : 1280; diffuse pattern; DNA binding antibody 51%, anti-
smooth muscle antibody-positive). Subsequent treatment with
etanercept has been well tolerated, and liver function tests
have remained normal.
Haematological toxicity
A profound, isolated, thrombocytopenia developed in one
patient (patient 16) following three infusions of infliximab,
which was presumed to be drug related. No information is
available as to whether this episode was associated with platelet
autoantibodies and there has been no recurrence since. Other-
wise, infliximab therapy was not associated with significant,
persistent haematological abnormalities, despite significant
concomitant immunosuppressive therapy in many patients.
Cardiac toxicity
Persistent hypertension developed in one patient with no spe-
cific risk factors following induction therapy and has required
treatment. Atrial fibrilliation, evidence of left atrial dilatation
and moderate left ventricular dysfunction on echocardiogram
was noted in a 44-year-old man (patient 21) 3 months after
discontinuing infliximab (due to the development of hepati-
tis). The causal relationship with infliximab is unclear, given
the time lapse, and known pretreatment risk factors including
alcohol intake and moderate obesity.
Mild chronic heart failure (NYHA Class II) noted in one
patient prior to therapy showed no evidence of deterioration
during the subsequent 2 years of infliximab treatment.
Malignancies
Skin cancer
Two lentigo malignas (face and chest) and a superficial basal
cell carcinoma (trunk) have all occurred in a single patient
following 6 months of infliximab treatment on a background
of prolonged treatment with ciclosporin and psoralen plus
ultraviolet A, a prior history of a facial lentigo maligna (com-
pletely excised) and multiple nonmelanoma skin cancers. The
infliximab has been continued, as it has afforded better disease
control and enabled cessation of ciclosporin. Acitretin has
been continued for skin cancer prophylaxis. A second patient
with a similar pretreatment history has not developed any fur-
ther skin cancers.
Other malignancies
Metastatic renal cell carcinoma presented in a 48-year-old man
(patient 19) following five infusions of infliximab. He had
previously received varying combinations of immunosuppres-
sant therapy over the previous 10 years including ciclosporin
and methotrexate for the majority of that time. A focus of
increased density noted posteriorly within the seventh left rib
on his baseline CXR was presumed to be benign following a
thoracic CT scan which reported a ‘probably benign’ 2-mm
pleural tumour that was too small to biopsy. However, by the
fifth infusion (i.e. approximately 5 months after initiating
therapy), he developed persistent nausea and progressive
weight loss; clinical examination revealed a supraclavicular
node and a palpable right kidney. Bilateral pleural plaques evi-
dent on CXR were subsequently biopsied and suggested the
diagnosis of a papillary cell carcinoma. A final diagnosis of
papillary renal cell carcinoma type 2, stage pT3b pN1 pM1
was made following a right nephrectomy (right renal tumour,
lung metastases, paraortic lymphadenopathy and invasion of
the inferior vena cava). He died 12 months later following
treatment with a-interferon and palliative care.
CD30+ lymphoproliferative disease was identified in one
patient (patient 18). This 56-year-old man with a 30-year
history of chronic plaque psoriasis had previously received
multiple immunosuppressive therapies (see Table 1). At the
point of treatment initiation, he had not received ciclosporin
for 13 months, alefacept for 10 months, methotrexate for
9 months or fumaric acid esters for 4 months. After three
infusions of infliximab 5 mg kg)1, a solitary nodule devel-
oped on his back. An initial diagnosis of CD30+ cutane-
ous anaplastic large cell lymphoma was made based on the
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
166 Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al.
histological and immunocytochemical findings (i.e. a promin-
ent dermal infiltrate of medium- to large-sized lymphoid cells
with pleomorphism; diffuse positive immunocytochemical
staining for CD30, CD2 and CD4 and focal positive staining
for CD5 and CD7; anaplastic lymphoma kinase-1 and epithelial
membrane antigen were negative). There was no lymphadeno-
pathy and staging investigations were negative. Blood investi-
gations demonstrated normal lymphocyte subsets and normal
CD4 : CD8 ratio. Although IgG antibodies for Epstein–Barr
virus were positive, IgM antibodies were not detected, exclu-
ding recent infection. Human T-lymphotrophic virus antibod-
ies I and II were negative. T-cell receptor gene analysis on
tissue was equivocal for a clone using V gamma II consensus
primer and no clone was seen in blood. Approximately
6 weeks after the appearance of the original lesion, the patient
developed other similar papules on the chest, limbs, back and
neck. Histology from these lesions was more consistent with
lymphomatoid papulosis than with CD30+ anaplastic large cell
lymphoma. No further infusions of infliximab were given and
he was commenced on etanercept 25 mg subcutaneously
twice weekly to control the psoriasis and methotrexate
10 mg weekly to control the CD30+ lymphoproliferative dis-
ease. The patient remains well controlled 15 months after
diagnosis with occasional self-resolving papules and no sys-
temic manifestation of lymphoma.
Discussion
Patients with severe psoriasis can present major therapeutic
challenges and dilemmas. While standard systemic therapy is,
for the most part, effective in the short term, predictable tox-
icity and/or gradual decline in efficacy may complicate long-
term use. Rotating or combining different treatment modali-
ties mitigates against these problems, but for a significant
group of patients with severe disease adequate disease control
is impossible or achieved only with actual, or high risk of,
drug toxicity and consequent morbidity. Our experience with
infliximab suggests that this agent represents a major thera-
peutic advance for this group of patients in spite of the cost
and logistics of administration. The risk of adverse effects is
nevertheless significant as 25% of our patient cohort discon-
tinued therapy due to serious side-effects. Careful patient
selection, pretreatment assessment and monitoring during and
after completion of therapy remain essential.
In this report, we have shown infliximab to be rapidly
effective with the onset of improvement being evident after
the first or second infusion and over 75% of patients achiev-
ing a 75% improvement in PASI score at week 10. This level
of efficacy is comparable with that reported in the three rand-
omized, placebo-controlled trials examining efficacy of inflix-
imab in moderate to severe, stable chronic plaque psoriasis
published to date.7,8,10 Our patient cohort probably represents
a more severely affected, treatment-resistant group as evi-
denced by higher mean scores on measures of disease severity
(PASI and DLQI), multiplicity of previous therapies and the
fact that most patients were on concomitant therapy at the
initiation of infliximab. This response to therapy was main-
tained over time, with marked improvements in patients’
quality of life, avoidance of hospital inpatient management,
and reduction or cessation of other immunosuppressive ther-
apies.
Our patients received maintenance rather than episodic
therapy (i.e. retreatment on disease flare). This decision was
based partly on our own early observations11 and also data
from one study in psoriasis,12 suggesting that once significant
disease relapse has occurred, repeat infusions do not achieve
the same rate of disease clearance as that seen on initial induc-
tion. This possibility is further supported by findings in
Crohn’s disease, where the risk of developing treatment resist-
ance to infliximab is reduced with maintenance (rather than
as required) infusions.13,14 Nevertheless, the dramatic reduc-
tion in PASI scores we observed during the ‘induction’ phase
of therapy was not necessarily maintained with subsequent
infusions in all patients. Even allowing for the fact that mul-
tiple additional variables might have impacted on disease
activity aside from infliximab, particularly reduction in con-
comitant therapy, there is a suggestion that with time, in
some patients, there is a gradual loss of efficacy, particularly
in those continuing therapy for longer than a year. Data from
one other case series in recalcitrant disease15 suggested loss of
efficacy over time in selected patients although in that instance
treatment was given as required rather than regularly. A recent
phase III study investigating efficacy of infliximab in 378
patients with moderate to severe psoriasis over 50 weeks also
showed loss of efficacy in a small proportion of patients over
time.10 The mechanism underlying this observation is not
clear although maintenance of therapeutic response appeared
to correlate with achievement of stable serum infliximab lev-
els, and was more common in patients who were antibody-
negative for antibodies to inflixmab compared with those who
were antibody-positive.10 Notably, loss of response to inflix-
imab in our patient cohort did not preclude a response to
other anti-TNF agents, supporting a highly specific (i.e. im-
munologically mediated) mechanism.
The benefit of infliximab in combination with other agents
in psoriasis is not established, and all the trials to date have
used infliximab alone. In rheumatoid arthritis, the addition of
methotrexate appears to confer both therapeutic and safety
benefits, whereas this is not the case in Crohn’s disease, where
infliximab is routinely used as monotherapy. However, in
clinical practice, as evidenced in our case series, concomitant
therapy may need to be continued to avoid unacceptable
deterioration in quality of life and/or a potentially dangerous
flare in disease activity while waiting for the therapeutic
effects of infliximab. Wherever possible, concomitant therapy
was rationalized prior to inflximab treatment, and agents of
questionable or minimal benefit stopped. Once disease control
was achieved, doses of concomitant therapy were reduced or
stopped over relatively short periods of time and with no con-
sequent destabilizing of disease. There was no evidence of sig-
nificant, specific drug-related toxicity developing with the co-
administration of infliximab, although the additional burden
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al. 167
of ‘generic’ immunosuppression may have contributed to the
observed infections and possibly onset or dissemination of
malignancy.
The pattern and frequency of adverse events in our popula-
tion is similar to that reported in the literature. In approxi-
mately 25% of our patients, these led to treatment cessation.
This is a higher proportion than that reported in formal clin-
ical trials of infliximab in psoriasis and probably reflects the
longer-term follow-up, disease severity of our patient cohort,
comorbidity and burden of previous treatments.
ANA and, less commonly, antidouble-stranded DNA, are
known to develop in some patients during therapy but, as we also
observed, do not seem to be associated with symptoms or signs
of lupus in the majority8,10 and rates are lower in psoriasis than
in rheumatoid arthritis and Crohn’s disease.
Data from clinical trials in all diseases indicate that although
infections are common, overall the rates of infection associ-
ated with infliximab are no greater than with placebo.
However, tuberculosis is known to be particularly associated
with anti-TNF agents as TNF-a plays a key role in host defence
against mycobacterial infection, particularly in granuloma for-
mation (and hence containment of Mycobacterium) and inhibition
of bacterial dissemination.16 A postmarketing surveillance report
in 200117,18 identified 70 cases of tuberculosis after treatment
with infliximab for rheumatoid arthritis, other forms of arthritis
and Crohn’s disease of a total estimated 147 000 people treated.
Based on this report, the risk of tuberculosis with infliximab has
been estimated to be approximately six times that of untreated
patients. Our case study illustrates several of the features com-
mon to tuberculosis infection in association with anti-TNF
agents in that onset of infection tends to occur early in treat-
ment, most patients are also receiving one or more immuno-
suppressive agents, and extrapulmonary disease is common.
Atypical and extensive infection is thought to account for the
high morbidity associated with infliximab-associated tuberculo-
sis, and underlines the need to maintain a high index of suspi-
cion in all patients during and after therapy. Guidelines issued
recently by the British Thoracic Society19 aim to identify those
particularly at risk of latent tuberculosis and would have identi-
fied our patient as ‘high risk’ in view of his ethnicity and
frequent travel to India.
Other serious infections reported in association with anti-
TNF therapy include sepsis secondary to Listeria monocytogenes
and histoplasmosis.20–23 The vast majority of these cases have
occurred in association with infliximab treatment, and in most
instances, additional immunosuppressant therapy.
With the exception of the single case of hepatitis which
appeared to be clearly and specifically related to the infliximab,
hepatic toxicity was not a clinically significant problem in our
series despite pre-existing liver pathology in some patients.
Although elevations in liver function tests have been reported
only infrequently in clinical trials, one case series recorded
transaminitis (defined as 1Æ5 · upper limit of normal) in six of
16 patients treated with infliximab for recalcitrant refractory
arthritis that necessitated treatment cessation in three.
Long-term toxicity of infliximab is largely unknown and
legitimate concern exists particularly about risks of malig-
nancy. Five cases of cancer occurred in our series. The role of
infliximab in the patient with renal cell carcinoma is unclear,
although it may have contributed to the rapid dissemination
of malignancy. Risks of skin cancer and lymphoma are already
elevated in patients with psoriasis,24–27 particularly in severe
disease although the relative contribution of antipsoriatic
(often immunosuppressive) therapy to this risk is not known.
Actual and relative risks associated with infliximab, including
intermittent vs. continuous therapy, and biological therapies as
a whole, especially in the context of this already very difficult
to treat population, will become evident only with careful,
long-term follow-up and continued pharmacovigilance. Cen-
tral registration of all patients receiving infliximab (and other
therapies of the same class) should facilitate this process.
References
1 Griffiths CE, Clark CM, Chalmers RJ et al. A systematic review oftreatments for severe psoriasis. Health Technol Assess 2000; 4:1–125.
2 Sampogna F, Sera F, Abeni D. Measures of clinical severity, qualityof life, and psychological distress in patients with psoriasis: a clus-
ter analysis. J Invest Dermatol 2004; 122:602–7.3 Stern RS, Nijsten T, Feldman SR et al. Psoriasis is common, carries
a substantial burden even when not extensive, and is associatedwith widespread treatment dissatisfaction. J Invest Dermatol Symp Proc
2004; 9:136–9.4 Kirby B, Richards HL, Woo P et al. Physical and psychologic meas-
ures are necessary to assess overall psoriasis severity. J Am Acad Der-matol 2001; 45:72–6.
5 Choi J, Koo JY. Quality of life issues in psoriasis. J Am Acad Dermatol2003; 49 (Suppl. 2):s57–61.
6 Rapp SR, Feldman SR, Exum ML et al. Psoriasis causes as much dis-ability as other major medical diseases. J Am Acad Dermatol 1999;
41:401–7.7 Chaudhari U, Romano P, Mulcahy LD et al. Efficacy and safety of
infliximab monotherapy for plaque-type psoriasis: a randomisedtrial. Lancet 2001; 357:1842–7.
8 Gottlieb AB, Evans R, Li S et al. Infliximab induction therapyfor patients with severe plaque-type psoriasis: a randomized, dou-
ble-blind, placebo-controlled trial. J Am Acad Dermatol 2004;51:534–42.
9 Roenigk H, Auerbach R, Maibach H et al. Methotrexate in psoriasis:consensus conference. J Am Acad Dermatol 1998; 38:478–85.
10 Reich K, Nestle FO, Papp K et al. Infliximab induction and main-tenance therapy for moderate-to-severe psoriasis: a phase III, multi-
centre, double-blind trial. Lancet 2005; 366:1367–74.11 Chew A-L, Bennett A, Smith CH et al. Successful treatment of severe
psoriasis and psoriatic arthritis with adalimumab. Br J Dermatol2004; 151:492–6.
12 Gottlieb AB, Chaudhari U, Mulcahy LD et al. Infliximab monothera-
py provides rapid and sustained benefit for plaque-type psoriasis.J Am Acad Dermatol 2003; 48:829–35.
13 Baert F, Noman M, Vermeire S et al. Influence of immunogenicityon the long-term efficacy of infliximab in Crohn’s disease. N Engl J
Med 2003; 348:601–8.14 Hanauer SB, Wagner CL, Bala M et al. Incidence and importance of
antibody responses to infliximab after maintenance or episodic treat-ment in Crohn’s disease. Clin Gastroenterol Hepatol 2004; 2:542–53.
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
168 Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al.
15 Cassano N, Loconsole F, Amoruso A et al. Infliximab monotherapyfor refractory psoriasis: preliminary results. Int J Immunopathol Pharma-
col 2004; 17:373–80.16 Gardam MA, Keystone EC, Menzies R et al. Anti-tumour necrosis
factor agents and tuberculosis risk: mechanisms of action and clin-ical management. Lancet Infect Dis 2003; 3:148–55.
17 Keane J, Gershon S, Wise RP et al. Tuberculosis associated with in-fliximab, a tumor necrosis factor a-neutralizing agent. N Engl J Med
2001; 345:1098–104.18 Lim WS, Powell RJ, Johnston ID. Tuberculosis and treatment with
infliximab. N Engl J Med 2002; 346:623–6.
19 Ledingham J, Wilkinson C, Deighton C. British Thoracic Society(BTS) recommendations for assessing risk and managing tuberculo-
sis in patients due to start anti-TNFa treatments. Rheumatology(Oxford). 2005; 44:10205–6.
20 Lee JH, Slifman NR, Gershon SK et al. Life-threatening histoplasmo-sis complicating immunotherapy with tumor necrosis factor alpha
antagonists infliximab and etanercept. Arthritis Rheum 2002;46:2565–70.
21 Slifman NR, Gershon SK, Lee JH et al. Listeria monocytogenes infectionas a complication of treatment with tumor necrosis factor alpha-
neutralizing agents. Arthritis Rheum 2003; 48:319–24.
22 Wallis RS, Broder MS, Wong JY et al. Granulomatous infectious dis-eases associated with tumor necrosis factor antagonists. Clin Infect
Dis 2004; 38:1261–5.23 Wallis RS, Broder M, Wong J, Beenhouwer D. Granulomatous
infections due to tumor necrosis factor blockade: correction. ClinInfect Dis 2004; 39:1254–5.
24 Gelfand JM, Berlin J, Van Voorhees A, Margolis DJ. Lymphomarates are low but increased in patients with psoriasis: results from
a population-based cohort study in the United Kingdom. Arch Der-matol 2003; 139:1425–9.
25 Nijsten TEC, Stern RS. The increased risk of skin cancer is persist-
ent after discontinuation of psoralen + ultraviolet A: a cohortstudy. J Invest Dermatol 2003; 121:252–8.
26 Boffetta P, Gridley G, Lindelof B. Cancer risk in a population-basedcohort of patients hospitalized for psoriasis in Sweden. J Invest Der-
matol 2001; 117:1531–7.27 Margolis DJ, Bilker W, Hennessy S et al. The risk of malignancy
associated with psoriasis. Arch Dermatol 2001; 137:778–83.
� 2006 British Association of Dermatologists • British Journal of Dermatology 2006 155, pp160–169
Infliximab for severe, treatment-resistant psoriasis, C.H. Smith et al. 169