Haryana Medical March 2020.cdr
-
Upload
khangminh22 -
Category
Documents
-
view
5 -
download
0
Transcript of Haryana Medical March 2020.cdr
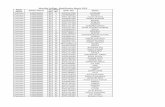
HMJ Office BearerEditor In Chief
Co-Editor
Dr Parveen Gupta, Dr Jyoti Malik
Advertisement Editor
Dr D S Goel, Dr Rakesh Gupta,
Dr Akhil Saxena
Associate Editor
Dr Mohan Lal Garg
Dr Divya
Dr Shekhar Sinha
Dr Ishwar Singh
Dr MK Tiwari
Dr Satya Samant
Dr Ashok Taneja
Dr Amita Garg
Dr Rohtas Yadav
Dr VK Kak
Dr Sangeeta
President IMA :
Dr Prabhakar Sharma
Secretary IMA :
Dr Vivek Malhotra
Ex officio
Dr K L Kokhar
Dr Vijay Kumar GuptaHisar
Members Advisory Board
Dr A Mahajan, Dr AP Setia
Dr Dhruv Chaudhary
HMJ Office BearerEditor In Chief
Co-Editor
Dr Parveen Gupta, Dr Jyoti Malik
Advertisement Editor
Dr D S Goel, Dr Rakesh Gupta,
Dr Akhil Saxena
Associate Editor
Dr Mohan Lal Garg
Dr Divya
Dr Shekhar Sinha
Dr Ishwar Singh
Dr MK Tiwari
Dr Satya Samant
Dr Ashok Taneja
Dr Amita Garg
Dr Rohtas Yadav
Dr VK Kak
Dr Sangeeta
President IMA :
Dr Prabhakar Sharma
Secretary IMA :
Dr Vivek Malhotra
Ex officio
Dr K L Kokhar
Dr Vijay Kumar GuptaHisar
Members Advisory Board
Dr A Mahajan, Dr AP Setia
Dr Dhruv Chaudhary
Dear friends
Wish you and your family members happy and prosperous new year.
New team has taken over at State and National level from 01.01.2020 onwards. I take this opportunity to thank you all for electing me as State President 2020 with your blessings and support. I will try to come upto your expectations.
We are lucky to have Dr. Rajan Sharma as National President, but it is also our added responsibilities to come upto the expectations of National IMA.
We have already started work on two very important projects of National IMA.
1) Legalfund - as directed by National IMA, we passed in SCM at Ambala, we are collecting Rs 1000 per member as legal fund (Rs 500 as National share and Rs 500 as State share)
I request all the state members to cooperate.
2) As you know, NATCON 20 is going to be hosted by Haryana, precious project for IMA National as well as for IMA Haryana.
I request everyone to cooperate and follow direction from chairman /organising secretary NATCON from time to time.
We are lucky to have ever ready ,enthusiastic and experienced chairman/ head of various wings, for any query or help you. You can consult them directly.They will be more than happy to help you.
We are passing through very difficult phase nowadays. COVID 19 is a major challenge ahead for all of us. We at private sectors are going to play major role in eradication of covid 19.We must follow all the advisories from IMA/Govt.which are issued from time to time.
IMA Haryana will not shy away from its responsibilities towards society and all the needy patients.
IMA Haryana will always have zero tolerance policy against violence against doctors and will continue its fight for Central rule for protection of medical fraternity.
IMA Haryana will always try to improve doctor- doctor and doctor- patient relationship.
Fight against NMC including bridge courses, NEXT, CROSS PATHY and other related issues to biomedical waste, municipal committee will continue.
I again thank you for giving me opportunity to serve as President, I will try to come upon your expectations.
TOGETHER WE CAN AND WE WILL
I congratulate Dr. V. K Gupta Chairman, Editor HMJ for bringing out this issue of HMJ.
With RegardsDr Prabhakar Sharma
President IMA Haryana State Branch
State President IMA Haryana
Haryana Medical Journal - March 2020, Vol. 43, Issue 01 01
Jai IMA Jai Bharat
Message
Dear friends
Wish you and your family members happy and prosperous new year.
New team has taken over at State and National level from 01.01.2020 onwards. I take this opportunity to thank you all for electing me as State President 2020 with your blessings and support. I will try to come upto your expectations.
We are lucky to have Dr. Rajan Sharma as National President, but it is also our added responsibilities to come upto the expectations of National IMA.
We have already started work on two very important projects of National IMA.
1) Legalfund - as directed by National IMA, we passed in SCM at Ambala, we are collecting Rs 1000 per member as legal fund (Rs 500 as National share and Rs 500 as State share)
I request all the state members to cooperate.
2) As you know, NATCON 20 is going to be hosted by Haryana, precious project for IMA National as well as for IMA Haryana.
I request everyone to cooperate and follow direction from chairman /organising secretary NATCON from time to time.
We are lucky to have ever ready ,enthusiastic and experienced chairman/ head of various wings, for any query or help you. You can consult them directly.They will be more than happy to help you.
We are passing through very difficult phase nowadays. COVID 19 is a major challenge ahead for all of us. We at private sectors are going to play major role in eradication of covid 19.We must follow all the advisories from IMA/Govt.which are issued from time to time.
IMA Haryana will not shy away from its responsibilities towards society and all the needy patients.
IMA Haryana will always have zero tolerance policy against violence against doctors and will continue its fight for Central rule for protection of medical fraternity.
IMA Haryana will always try to improve doctor- doctor and doctor- patient relationship.
Fight against NMC including bridge courses, NEXT, CROSS PATHY and other related issues to biomedical waste, municipal committee will continue.
I again thank you for giving me opportunity to serve as President, I will try to come upon your expectations.
TOGETHER WE CAN AND WE WILL
I congratulate Dr. V. K Gupta Chairman, Editor HMJ for bringing out this issue of HMJ.
With RegardsDr Prabhakar Sharma
President IMA Haryana State Branch
State President IMA Haryana
Haryana Medical Journal - March 2020, Vol. 43, Issue 01 01
Jai IMA Jai Bharat
Message
"let food be thy medicine and medicine be thy food"
- N Hippocrates
On the occasion of the release of HMJ 2020, I convey my best wishes to the editorial
team of HMJ,2020.
HMJ has been providing excellent and updated academic guidance from last many years
, which has contributed significantly in the academic growth of IMA Members.
The HMJ not also exhibits the growth and progress of the organization but also imprints
the hardwork, achievements and aspirations of young doctors.
I am confident that HMJ will continue with the tradition of imparting quality education
and setting a bench mark to be emulated by others.
I would also like to acknowledge the zeal and dedication of the editorial team of HMJ.
My best wishes to team IMA Haryana for a glorious year.
Dr Vivek MalhotraHony. Secretary,
IMA, Haryana State Branch
Hony. Secretary,IMA, Haryana
02Haryana Medical Journal - March 2020, Vol. 43, Issue 01
From editor desk
Side effects of unhygienic living style
The being of 2020 is marked by the declaration of pandemic due to corona virus, a virus which affects animal but has come to affect human being now. The eating habits of costal counties and especially Chinese has been questioned by all.
Spread of corona virus-Corona viruses are most commonly passed between animals and people and from person to person. The source of COVID-19 (coronavirus) is believed to be animals, but the exact source is not yet known.The virus is commonly passed on:
§ directly, through contact with an infected person's body fluids (for example, droplets from coughing or sneezing)
§ indirectly, through contact with surfaces that an infected person has coughed or sneezed on
Current information suggests that the virus may survive a few hours, or even days, on certain surfaces, but its good that a simple household disinfectants can kill it.
Safety Precautions for common human
The World Health Organisation (WHO) advises that standard recommendations to reduce exposure to and transmission of a range of illnesses are maintained. These include:
§ proper hand hygiene
§ cough/cold hygiene practices
§ safe food practices
§ avoiding close contact, when possible, with anyone showing symptoms of respiratory illness such as coughing and sneezing
Safety precautions for medical practitioners and allieds
Preventive and mitigation measures are key in both healthcare and community settings. The most effective preventive measures in the community include: performing hand hygiene frequently with an alcohol-based hand rub if your hands are not visibly dirty or with soap and water if hands are dirty; avoiding touching your eyes, nose and mouth; practicing respiratory hygiene by coughing or sneezing into a bent elbow or tissue and then immediately disposing of the tissue; wearing a medical mask if you have respiratory
From the Editor's Desk
03Haryana Medical Journal - March 2020, Vol. 43, Issue 01
"let food be thy medicine and medicine be thy food"
- N Hippocrates
On the occasion of the release of HMJ 2020, I convey my best wishes to the editorial
team of HMJ,2020.
HMJ has been providing excellent and updated academic guidance from last many years
, which has contributed significantly in the academic growth of IMA Members.
The HMJ not also exhibits the growth and progress of the organization but also imprints
the hardwork, achievements and aspirations of young doctors.
I am confident that HMJ will continue with the tradition of imparting quality education
and setting a bench mark to be emulated by others.
I would also like to acknowledge the zeal and dedication of the editorial team of HMJ.
My best wishes to team IMA Haryana for a glorious year.
Dr Vivek MalhotraHony. Secretary,
IMA, Haryana State Branch
Hony. Secretary,IMA, Haryana
02Haryana Medical Journal - March 2020, Vol. 43, Issue 01
From editor desk
Side effects of unhygienic living style
The being of 2020 is marked by the declaration of pandemic due to corona virus, a virus which affects animal but has come to affect human being now. The eating habits of costal counties and especially Chinese has been questioned by all.
Spread of corona virus-Corona viruses are most commonly passed between animals and people and from person to person. The source of COVID-19 (coronavirus) is believed to be animals, but the exact source is not yet known.The virus is commonly passed on:
§ directly, through contact with an infected person's body fluids (for example, droplets from coughing or sneezing)
§ indirectly, through contact with surfaces that an infected person has coughed or sneezed on
Current information suggests that the virus may survive a few hours, or even days, on certain surfaces, but its good that a simple household disinfectants can kill it.
Safety Precautions for common human
The World Health Organisation (WHO) advises that standard recommendations to reduce exposure to and transmission of a range of illnesses are maintained. These include:
§ proper hand hygiene
§ cough/cold hygiene practices
§ safe food practices
§ avoiding close contact, when possible, with anyone showing symptoms of respiratory illness such as coughing and sneezing
Safety precautions for medical practitioners and allieds
Preventive and mitigation measures are key in both healthcare and community settings. The most effective preventive measures in the community include: performing hand hygiene frequently with an alcohol-based hand rub if your hands are not visibly dirty or with soap and water if hands are dirty; avoiding touching your eyes, nose and mouth; practicing respiratory hygiene by coughing or sneezing into a bent elbow or tissue and then immediately disposing of the tissue; wearing a medical mask if you have respiratory
From the Editor's Desk
03Haryana Medical Journal - March 2020, Vol. 43, Issue 01
symptoms and performing hand hygiene after disposing of the mask; maintaining social distance (a minimum of 1 m) from individuals with respiratory symptoms.
Additionally for health workers-PPE appropriately; this involves selecting the proper PPE and being trained in how to put on, remove and dispose of it. The use of a simple mask alone is insufficient to provide the adequate level of protection and other equally relevant measures should be adopted.
I request all my colleagues, health workers to be aware and take necessary precautions as required and be safe so that we can serve and save suffering human beings. This is crucial time and everyone is looking and expecting from maternity fraternity.
Indian Goverment has launched Arogya Setu App for creating awareness and helping people know their COVID-19 status. The app is an appreciable move by government and we all should have app in our mobile and encourage as well as educate our patient to have app in their mobile to help in stopping the spread of Corona Virus.
04Haryana Medical Journal - March 2020, Vol. 43, Issue 01
SURGICAL DILEMMAS IN THE COVID ERA.
� This March we had to face an unknown enemy. The field of medicine was suddenly attacked by this outsider from Wuhan. We the medical fraternity were taken by surprise at the casualties that followed in rapid succession , in almost all the countries of the world. The COVID virus aka SARS CoV2 respected no boundaries and no class of people. A pandemic in the truest sense had just surfaced.
� Soon the large number of patients get t ing admit ted meant that a treatment modality had to be found. An old adage- Old is Gold was realized. Chloroquine and Hydroxychloroquine showed benefit in the hospitalized patients. Azithromycin ,Remdesivir, Lopinavir- Ritonavir , Tocilizumab, etc were soon in the pipeline.As the patients got cured, using their antibodies in convalescent plasma, was an interesting discovery. This was also used in the severely ill .
� Next came the realization that how do we do surgeries with the fear of S A R S C o V 2 l u r k i n g i n t h e background?
� A preliminary testing of each individual was not possible. So it was decided that all elective surgeries wouldn’t be done till the curve flattens. But the emergency life threatening surgeries viz oncosurgeries, trauma, obstetrics and cardiovascular surgeries would have to go on…
� But all this had to be done with
minimal risks to the patient and the operating team..
Q.� So how do we do it?
Ans-A SOP needs to be formulated based on common sense, evidence based medicine and prior experience with viral infections .
� A multi-disciplinary team is essential to take decisions . Hospitals must provide maximum protective equipment and training on how to use it to health care workers (HCW) .
� Patients can only be treated if HCW stay healthy.
� In Covid +ve cases it is better to avoid surgery as besides the considerable risk to the HCW – the patient is also likely to contract major complications.
Q.� What are the Indications for surgeries in Cardio-Vascular & Thoracic Surgery patients:
Ans- Following is applicable to cardiac surgeries in cardiac patients who are NOT known to have Covid virus infection
1.� Left main coronary artery disease with significant right coronary artery disease
2.� Critical Left main coronary artery disease
3.� Critical proximal TVD
4.� Left main equivalent DVD
5.� Patient with unstable angina not responding to OMT
6.� Critical symptomatic aortic stenosis
05Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Dr VK GUPTAEDITOR
Hisar
Dr Swarup Swaraj Pal, Dr H S Bedi, Deepak K
symptoms and performing hand hygiene after disposing of the mask; maintaining social distance (a minimum of 1 m) from individuals with respiratory symptoms.
Additionally for health workers-PPE appropriately; this involves selecting the proper PPE and being trained in how to put on, remove and dispose of it. The use of a simple mask alone is insufficient to provide the adequate level of protection and other equally relevant measures should be adopted.
I request all my colleagues, health workers to be aware and take necessary precautions as required and be safe so that we can serve and save suffering human beings. This is crucial time and everyone is looking and expecting from maternity fraternity.
Indian Goverment has launched Arogya Setu App for creating awareness and helping people know their COVID-19 status. The app is an appreciable move by government and we all should have app in our mobile and encourage as well as educate our patient to have app in their mobile to help in stopping the spread of Corona Virus.
04Haryana Medical Journal - March 2020, Vol. 43, Issue 01
SURGICAL DILEMMAS IN THE COVID ERA.
� This March we had to face an unknown enemy. The field of medicine was suddenly attacked by this outsider from Wuhan. We the medical fraternity were taken by surprise at the casualties that followed in rapid succession , in almost all the countries of the world. The COVID virus aka SARS CoV2 respected no boundaries and no class of people. A pandemic in the truest sense had just surfaced.
� Soon the large number of patients get t ing admit ted meant that a treatment modality had to be found. An old adage- Old is Gold was realized. Chloroquine and Hydroxychloroquine showed benefit in the hospitalized patients. Azithromycin ,Remdesivir, Lopinavir- Ritonavir , Tocilizumab, etc were soon in the pipeline.As the patients got cured, using their antibodies in convalescent plasma, was an interesting discovery. This was also used in the severely ill .
� Next came the realization that how do we do surgeries with the fear of S A R S C o V 2 l u r k i n g i n t h e background?
� A preliminary testing of each individual was not possible. So it was decided that all elective surgeries wouldn’t be done till the curve flattens. But the emergency life threatening surgeries viz oncosurgeries, trauma, obstetrics and cardiovascular surgeries would have to go on…
� But all this had to be done with
minimal risks to the patient and the operating team..
Q.� So how do we do it?
Ans-A SOP needs to be formulated based on common sense, evidence based medicine and prior experience with viral infections .
� A multi-disciplinary team is essential to take decisions . Hospitals must provide maximum protective equipment and training on how to use it to health care workers (HCW) .
� Patients can only be treated if HCW stay healthy.
� In Covid +ve cases it is better to avoid surgery as besides the considerable risk to the HCW – the patient is also likely to contract major complications.
Q.� What are the Indications for surgeries in Cardio-Vascular & Thoracic Surgery patients:
Ans- Following is applicable to cardiac surgeries in cardiac patients who are NOT known to have Covid virus infection
1.� Left main coronary artery disease with significant right coronary artery disease
2.� Critical Left main coronary artery disease
3.� Critical proximal TVD
4.� Left main equivalent DVD
5.� Patient with unstable angina not responding to OMT
6.� Critical symptomatic aortic stenosis
05Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Dr VK GUPTAEDITOR
Hisar
Dr Swarup Swaraj Pal, Dr H S Bedi, Deepak K
admission.
-� CXR, ECG
-� CBC,LFT,RFT, Sr LDH, Sr Ferritin, CPK MB, Viral markers
� Visitor numbers will be strictly restricted.
� M a n d a t o r y C o v i d t e s t i n g i s recommended for all patients preop (ideally RT PCR should be done).
� Staff should be asked to refrain from unnecessary travel to certain destinations – hot spots . Temperatures of all staff should be taken twice daily using hospital-issued oral digital thermometers for each employee . Anyone with fever should be investigated further as per our Medical specialists protocol.
� A separate Covid consent form must be explained and signed – video consent should be taken for each case .
� Adequate blood and blood products and all consumables required for the case should be ordered and should be in hand before the case!
Q.� Operating room management-HOW is it done?
Ans-
1.� The patient, wearing a surgical face mask, should be transported from the unit along a designated route with minimal contact with others
� A standard OR is usually designed to be at positive pressure relative to surrounding air. Nevertheless, a high frequency of air changes (25 per hr) rapidly reduces viral load within the OR.
2.� A plan is made before surgery to ensure everyone understands the plan for anesthesia and surgery. This enables seamless teamwork and ensures that all
7.� Valvular heart disease admitted in heart failure
8.� Emergency surgeries like: aortic dissection, Mechanical complication of Myocardial infarction, acute massive PE not responding to thrombolysis
9.� In-house urgent cases, who are at risk for adverse cardiac events if going home instead of staying in the hospital, might still undergo cardiac surgery at this time
10.� Cardiac trauma
11.� Acute pericardial tamponade not responding to aspiration
12.� Vascular : acute arterial embolism with Acute Critical Limb Ischemia, Acute prox massive DVT , acute problems with AV fistula , vascular trauma
13.� Thoracic : Trauma
Q.� How is the Management of patients, visitors, and staff done?
Ans-All patients referred for cardiac surgery presenting to the hospital will be screened using a standard questionnaire in Triage itself . Patients who fulfill the criteria for suspected SARS-CoV-2 infection will be isolated (scoring system can be used) , referred to an infectious d i seases spec ia l i s /phys ic ian and pulmonologist and tested for the virus.
� Elective surgery will be postponed if the patient had travelled to affected areas.
� Only of low-risk patients (no fever or respiratory symptoms, no history of recent travel or close contact with a COVID-19 patient, cleared by Medicine) will be taken for surgery after a negative COVID test (ideally) .
The following tests may be done if the patient warrants a surgery-
-� HRCT ches t may be done on
06Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� Before anesthesia induction, a HEPA filter should be connected to the patient end of the breathing circuit, and another between the expiratory limb and the anesthetic machine. Equipment should be prepared to reduce the need for circuit d isconnect ions—e.g. , any c i rcui t extensions should be attached before starting the case. A video-laryngoscope is recommended because a PAPR hood or goggles may hamper vision during direct laryngoscopy. A video-laryngoscope also keeps the incubator further from the patient’s airway during intubation. Alternatively an intubation box and face shield should be used .
� Closed, in-line tracheal suction should be used instead of open suction. Minimizing circuit disconnections is ideal, but if this is unavoidable, ensure positive pressure ventilation is ceased, turn the adjustable pressure limiting valve to zero, and consider clamping the endotracheal tube prior to disconnection. This technique may also be used before switching a patient from intensive care from the transport ventilator to the anesthetic machine
� The use of a heated humidifier is discouraged to avoid viral aerosolization. Heater cooling blanket can be used.
� Anti-emetics should be administered to reduce postoperative retching. A rigid suction catheter may be used to reduce the chance of contaminating the surroundings with the soft flexible suction catheter
� Instead of first Lining up the patient and then intubating, intubation must be done first and then lines inserted. Till this time the OT must have as minimum staff as needed. This change will allow the fomites to settle down and not be
necessary drugs and equipment have been prepared. It also minimizes the need to leave and re-enter the OR to bring in missing equipment.
� Center for Disease Control and Prevention (CDC) recommends the use of gowns, pairs of gloves, and an N95 respirator plus a face shield and/or googles when treating all patients in these times.
3.� The OT instrument trolley should be prepared after the lining of patient is over so that post intubation aerosol can settle down.
4.� The staff needed must be minimized inside the OT during the procedure.
5.� Minimal movement outside the OT should be permitted. The OT door should always be closed.
6.� All the staff in OT should be protected with N95 Mask, disposable fluid proof gown, gloves, cap, face shield or googles and shoe covers.
7.� Full Hazmat PPE should be used only by the anesthetist and assistant and surgical team.
Q.� How do we plan Anaesthesia
Ans- Ideal working conditions with AC system which is separate from other units, h a s s c a v e n g i n g s y s t e m , q u a l i t y anaesthesia machine where Low FGF upto 1 litre/ minute can be used.
� Anesthesia should be planned with two goals in mind: patient safety and infection prevention. Infection prevention entails reducing aerosol-generating procedures (i.e., airway manipulation, face mask ventilation, open airway suctioning, and patient coughing) as far as possible
07Haryana Medical Journal - March 2020, Vol. 43, Issue 01
admission.
-� CXR, ECG
-� CBC,LFT,RFT, Sr LDH, Sr Ferritin, CPK MB, Viral markers
� Visitor numbers will be strictly restricted.
� M a n d a t o r y C o v i d t e s t i n g i s recommended for all patients preop (ideally RT PCR should be done).
� Staff should be asked to refrain from unnecessary travel to certain destinations – hot spots . Temperatures of all staff should be taken twice daily using hospital-issued oral digital thermometers for each employee . Anyone with fever should be investigated further as per our Medical specialists protocol.
� A separate Covid consent form must be explained and signed – video consent should be taken for each case .
� Adequate blood and blood products and all consumables required for the case should be ordered and should be in hand before the case!
Q.� Operating room management-HOW is it done?
Ans-
1.� The patient, wearing a surgical face mask, should be transported from the unit along a designated route with minimal contact with others
� A standard OR is usually designed to be at positive pressure relative to surrounding air. Nevertheless, a high frequency of air changes (25 per hr) rapidly reduces viral load within the OR.
2.� A plan is made before surgery to ensure everyone understands the plan for anesthesia and surgery. This enables seamless teamwork and ensures that all
7.� Valvular heart disease admitted in heart failure
8.� Emergency surgeries like: aortic dissection, Mechanical complication of Myocardial infarction, acute massive PE not responding to thrombolysis
9.� In-house urgent cases, who are at risk for adverse cardiac events if going home instead of staying in the hospital, might still undergo cardiac surgery at this time
10.� Cardiac trauma
11.� Acute pericardial tamponade not responding to aspiration
12.� Vascular : acute arterial embolism with Acute Critical Limb Ischemia, Acute prox massive DVT , acute problems with AV fistula , vascular trauma
13.� Thoracic : Trauma
Q.� How is the Management of patients, visitors, and staff done?
Ans-All patients referred for cardiac surgery presenting to the hospital will be screened using a standard questionnaire in Triage itself . Patients who fulfill the criteria for suspected SARS-CoV-2 infection will be isolated (scoring system can be used) , referred to an infectious d i seases spec ia l i s /phys ic ian and pulmonologist and tested for the virus.
� Elective surgery will be postponed if the patient had travelled to affected areas.
� Only of low-risk patients (no fever or respiratory symptoms, no history of recent travel or close contact with a COVID-19 patient, cleared by Medicine) will be taken for surgery after a negative COVID test (ideally) .
The following tests may be done if the patient warrants a surgery-
-� HRCT ches t may be done on
06Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� Before anesthesia induction, a HEPA filter should be connected to the patient end of the breathing circuit, and another between the expiratory limb and the anesthetic machine. Equipment should be prepared to reduce the need for circuit d isconnect ions—e.g. , any c i rcui t extensions should be attached before starting the case. A video-laryngoscope is recommended because a PAPR hood or goggles may hamper vision during direct laryngoscopy. A video-laryngoscope also keeps the incubator further from the patient’s airway during intubation. Alternatively an intubation box and face shield should be used .
� Closed, in-line tracheal suction should be used instead of open suction. Minimizing circuit disconnections is ideal, but if this is unavoidable, ensure positive pressure ventilation is ceased, turn the adjustable pressure limiting valve to zero, and consider clamping the endotracheal tube prior to disconnection. This technique may also be used before switching a patient from intensive care from the transport ventilator to the anesthetic machine
� The use of a heated humidifier is discouraged to avoid viral aerosolization. Heater cooling blanket can be used.
� Anti-emetics should be administered to reduce postoperative retching. A rigid suction catheter may be used to reduce the chance of contaminating the surroundings with the soft flexible suction catheter
� Instead of first Lining up the patient and then intubating, intubation must be done first and then lines inserted. Till this time the OT must have as minimum staff as needed. This change will allow the fomites to settle down and not be
necessary drugs and equipment have been prepared. It also minimizes the need to leave and re-enter the OR to bring in missing equipment.
� Center for Disease Control and Prevention (CDC) recommends the use of gowns, pairs of gloves, and an N95 respirator plus a face shield and/or googles when treating all patients in these times.
3.� The OT instrument trolley should be prepared after the lining of patient is over so that post intubation aerosol can settle down.
4.� The staff needed must be minimized inside the OT during the procedure.
5.� Minimal movement outside the OT should be permitted. The OT door should always be closed.
6.� All the staff in OT should be protected with N95 Mask, disposable fluid proof gown, gloves, cap, face shield or googles and shoe covers.
7.� Full Hazmat PPE should be used only by the anesthetist and assistant and surgical team.
Q.� How do we plan Anaesthesia
Ans- Ideal working conditions with AC system which is separate from other units, h a s s c a v e n g i n g s y s t e m , q u a l i t y anaesthesia machine where Low FGF upto 1 litre/ minute can be used.
� Anesthesia should be planned with two goals in mind: patient safety and infection prevention. Infection prevention entails reducing aerosol-generating procedures (i.e., airway manipulation, face mask ventilation, open airway suctioning, and patient coughing) as far as possible
07Haryana Medical Journal - March 2020, Vol. 43, Issue 01
cases . During IMA harvest meticulously avoid damage to the lung as any air leak is hazardous . Try extrapleural IMA harvest . Avoid going on pump.
Extubation in OR / Recovery:
� Hazmat PPE during extubation. Helping staff /technician can come from head end / behind, instead of coming in line of patient’s aerosol direction. ETT cuff to be deflated at the very last, just before removal of ETT. Post extubation, protective masks to be applied at the earliest on the patient and then oxygen mask can be put over the protective face mask.
� All the soiled and disposable items should be discarded as per protocol. The ETT tube and the suction catheter should be discarded preferably in a zip- loc bag.
Q.� Any specific precautions In CTICU
-� limit coughing exercises
-� cough into a disposable thick tissue paper
-� keep a mask on face of patient
-� nurse to have a Hazmat suit with face shield
-� patient to be isolated as much as feasible
-� in case of air leak from chest tube – connect to wall suction
-� all equipment cleaned frequently
-� Ideally have a paperless system
-� Very frequent hand wash is mandatory
-� Avoid nebulisation
-� Every HCW other than primary nurse keep a safe distance
-� Shift patient to isolation as soon as possible
suspended in air minimizing the risk of infection of other staff. Equipment around the patient head should be immediately cleaned with disinfectant to reduce any chance of transmission of virus.
Induction of Anesthesia:
� As part of preventive measures, it is advisable to give chlorhexidine mouth gargles twice daily during hospital stay preoperatively and one hour before shifting to OR. This will help reduce microbial load in upper airway, if any. Bag mask positive pressure ventilation to be avoided. Oxygen is administered as part of pre-oxygenation prior to induction via anesthetic face mask connected vis a HMEF ( heat and moisture exchange with filter). HEMF without filter will be ineffective in preventing viral particle transport from patient in to the circuit,
� Rapid sequence in tubat ion i s preferred method of intubation using either Suxamethonium (scoline) or R o c u r o n i u m . A f t e r i n s e r t i o n o f endotracheal tube, the cuff is inflated immediately to get adequate seal to prevent aerosol from escaping from patient’s tracheobronchial tree.
� Post intubation ETT should be confirmed by capnography and visible chest rise. Cover the patient’s face with a non-absorbable sheet to prevent any possible aerosol dispersion under GA from patient’s oral cavity.
� Technician or helping staff should preferably maintain 2 meter distance or as much as possible at the time of induction.
Surgery ©drswaruppal#cvts
� The surgery should be well planned and each team member must know his job well. Teaching should be avoided in these
08Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Full HIV type kit protection and disposable linen for all else . - Intubating the patient before lining up will give time to aerosol to settle down - At least 15 minutes should pass before anyone else other than anesthetist is allowed into the OT to allow aerosol to settle down - All other staff in OT should have proper protective gear - It is preferable to cover all the instruments in OT with polythene sheets - Minimum required staff should be kept in OT - Minimize movement of staff and equipment in and out of OT - OT door must always be kept shut - All the used equipment should be sorted in OT itself and disposed with disposable items safely - Anesthesia goal should be directed t o w a r d s r e d u c i n g o r c o n t a i n g aerosolization - All equipment and OT should be cleaned with recommended disinfectants - PPE should be used prudently to protect the most vulnerable staff.
Q.� Any thing to check when the patient is in the Wards?
Ans.-
-� Every patient should be in a single room, both preop and postop. In a surgical case, the pt must be observed for symptoms for 5 days before embarking on surgery. It is preferable that he stays in the hospital for those 5 days.
-� The nurse taking care of him should don the requisite level of PPE as per hospital guidelines.
-� Heart rate, blood pressure, saturation a n d r e s p i r a t o r y r a t e s h o u l d b e monitoredà any deterioration in the above should be informed to the consultant. If the pt has continuous fever and coughà physician and pulmonologist should be consulted.
Q.� What are the spec ific Pos t -Operative Protocols?
Ans-After surgery, before leaving, contaminated equipment must be left in the OR and discarded into a container. It might be important not to push the equipment down into the container to avoid releasing aerosols, which could be contaminated
� Separate area should be designated where all the gowns, gloves, shoe covers etc. should be discarded.
� All personal safety protocols should be followed while removal of TEE probe and extubation.
� R o u t i n e c l e a n i n g o f a l l O T equipment’s (anesthesia Machine, TEE, diathermy, suction machine, CPB machine, pendants, trolleys etc.) and surface cleaning of all walls and floors. All equipment may be covered with a transparent plastic sheet before bringing patient in .
� After surgery, the anesthetic breathing circuit and the canister of soda lime are discarded to eliminate the negligible risk of circuit contamination. After disposing of single-use equipment in well-marked biohazard bags, all instruments are sent for decontamination and sterile reprocessing. Surfaces of all medical devices are cleaned with quaternary ammonium chloride disinfectant wipes. The OR is then cleaned with sodium hypochlorite 1000 ppm and t r e a t e d w i t h h y d r o g e n p e r o x i d e vaporization or ultraviolet-C irradiation.
� Recommendations - COVID 19 is a droplet/fomite transmission and not an airborne transmission - Full PPE is recommended only for the anesthetist and technician to protect from aerosol splash.
09Haryana Medical Journal - March 2020, Vol. 43, Issue 01
cases . During IMA harvest meticulously avoid damage to the lung as any air leak is hazardous . Try extrapleural IMA harvest . Avoid going on pump.
Extubation in OR / Recovery:
� Hazmat PPE during extubation. Helping staff /technician can come from head end / behind, instead of coming in line of patient’s aerosol direction. ETT cuff to be deflated at the very last, just before removal of ETT. Post extubation, protective masks to be applied at the earliest on the patient and then oxygen mask can be put over the protective face mask.
� All the soiled and disposable items should be discarded as per protocol. The ETT tube and the suction catheter should be discarded preferably in a zip- loc bag.
Q.� Any specific precautions In CTICU
-� limit coughing exercises
-� cough into a disposable thick tissue paper
-� keep a mask on face of patient
-� nurse to have a Hazmat suit with face shield
-� patient to be isolated as much as feasible
-� in case of air leak from chest tube – connect to wall suction
-� all equipment cleaned frequently
-� Ideally have a paperless system
-� Very frequent hand wash is mandatory
-� Avoid nebulisation
-� Every HCW other than primary nurse keep a safe distance
-� Shift patient to isolation as soon as possible
suspended in air minimizing the risk of infection of other staff. Equipment around the patient head should be immediately cleaned with disinfectant to reduce any chance of transmission of virus.
Induction of Anesthesia:
� As part of preventive measures, it is advisable to give chlorhexidine mouth gargles twice daily during hospital stay preoperatively and one hour before shifting to OR. This will help reduce microbial load in upper airway, if any. Bag mask positive pressure ventilation to be avoided. Oxygen is administered as part of pre-oxygenation prior to induction via anesthetic face mask connected vis a HMEF ( heat and moisture exchange with filter). HEMF without filter will be ineffective in preventing viral particle transport from patient in to the circuit,
� Rapid sequence in tubat ion i s preferred method of intubation using either Suxamethonium (scoline) or R o c u r o n i u m . A f t e r i n s e r t i o n o f endotracheal tube, the cuff is inflated immediately to get adequate seal to prevent aerosol from escaping from patient’s tracheobronchial tree.
� Post intubation ETT should be confirmed by capnography and visible chest rise. Cover the patient’s face with a non-absorbable sheet to prevent any possible aerosol dispersion under GA from patient’s oral cavity.
� Technician or helping staff should preferably maintain 2 meter distance or as much as possible at the time of induction.
Surgery ©drswaruppal#cvts
� The surgery should be well planned and each team member must know his job well. Teaching should be avoided in these
08Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Full HIV type kit protection and disposable linen for all else . - Intubating the patient before lining up will give time to aerosol to settle down - At least 15 minutes should pass before anyone else other than anesthetist is allowed into the OT to allow aerosol to settle down - All other staff in OT should have proper protective gear - It is preferable to cover all the instruments in OT with polythene sheets - Minimum required staff should be kept in OT - Minimize movement of staff and equipment in and out of OT - OT door must always be kept shut - All the used equipment should be sorted in OT itself and disposed with disposable items safely - Anesthesia goal should be directed t o w a r d s r e d u c i n g o r c o n t a i n g aerosolization - All equipment and OT should be cleaned with recommended disinfectants - PPE should be used prudently to protect the most vulnerable staff.
Q.� Any thing to check when the patient is in the Wards?
Ans.-
-� Every patient should be in a single room, both preop and postop. In a surgical case, the pt must be observed for symptoms for 5 days before embarking on surgery. It is preferable that he stays in the hospital for those 5 days.
-� The nurse taking care of him should don the requisite level of PPE as per hospital guidelines.
-� Heart rate, blood pressure, saturation a n d r e s p i r a t o r y r a t e s h o u l d b e monitoredà any deterioration in the above should be informed to the consultant. If the pt has continuous fever and coughà physician and pulmonologist should be consulted.
Q.� What are the spec ific Pos t -Operative Protocols?
Ans-After surgery, before leaving, contaminated equipment must be left in the OR and discarded into a container. It might be important not to push the equipment down into the container to avoid releasing aerosols, which could be contaminated
� Separate area should be designated where all the gowns, gloves, shoe covers etc. should be discarded.
� All personal safety protocols should be followed while removal of TEE probe and extubation.
� R o u t i n e c l e a n i n g o f a l l O T equipment’s (anesthesia Machine, TEE, diathermy, suction machine, CPB machine, pendants, trolleys etc.) and surface cleaning of all walls and floors. All equipment may be covered with a transparent plastic sheet before bringing patient in .
� After surgery, the anesthetic breathing circuit and the canister of soda lime are discarded to eliminate the negligible risk of circuit contamination. After disposing of single-use equipment in well-marked biohazard bags, all instruments are sent for decontamination and sterile reprocessing. Surfaces of all medical devices are cleaned with quaternary ammonium chloride disinfectant wipes. The OR is then cleaned with sodium hypochlorite 1000 ppm and t r e a t e d w i t h h y d r o g e n p e r o x i d e vaporization or ultraviolet-C irradiation.
� Recommendations - COVID 19 is a droplet/fomite transmission and not an airborne transmission - Full PPE is recommended only for the anesthetist and technician to protect from aerosol splash.
09Haryana Medical Journal - March 2020, Vol. 43, Issue 01
-� Only one healthy relative who doesn’t have covid symptoms to stay back with the pt.
-� Discharge as per current guidelines.
With these precautions and proper planning of cases , we were able to do all the emergency cases without any untoward incident. The important part was sitting a day prior to surgery and charting out the procedure with great detail in the presence of the surgeon, anaesthes i s t , scrub nurses and anaesthesia technicians. Next part was ensuring adequate PPE s were available and the donning and doffing procedure was known to all. If the PPE s were short , the HIV k i t s were used as a supplement. N95 masks covered with a 3 layer surgical mask was used in each case. AC was on throughout the case and once the patient was wheeled in, the door was shut and was opened only at the completion of the procedure. Except the surgeon who wore loupes, everyone else had a mask with a visor attached to it.
� The pandemic will take time to settle, but surgical procedures would start sooner or later. With the above guidelines[ which can be tweaked for each surgical speciality] a safe conduct of surgery is expected!
� Following are a few pics of how surgeries happen with the PPE in place…
10Haryana Medical Journal - March 2020, Vol. 43, Issue 01 11Haryana Medical Journal - March 2020, Vol. 43, Issue 01
This image shows the surgeon wearing the PPE. Note that all parts of the body must be covered in the PPE. You then
don the sterile gown as shown in the next pic
Conduct of surgery pics…Address of Correspondence HOD CVTS
Amandeep group of hospitals Amritsar, Pathankot, Jammu.
-� Only one healthy relative who doesn’t have covid symptoms to stay back with the pt.
-� Discharge as per current guidelines.
With these precautions and proper planning of cases , we were able to do all the emergency cases without any untoward incident. The important part was sitting a day prior to surgery and charting out the procedure with great detail in the presence of the surgeon, anaesthes i s t , scrub nurses and anaesthesia technicians. Next part was ensuring adequate PPE s were available and the donning and doffing procedure was known to all. If the PPE s were short , the HIV k i t s were used as a supplement. N95 masks covered with a 3 layer surgical mask was used in each case. AC was on throughout the case and once the patient was wheeled in, the door was shut and was opened only at the completion of the procedure. Except the surgeon who wore loupes, everyone else had a mask with a visor attached to it.
� The pandemic will take time to settle, but surgical procedures would start sooner or later. With the above guidelines[ which can be tweaked for each surgical speciality] a safe conduct of surgery is expected!
� Following are a few pics of how surgeries happen with the PPE in place…
10Haryana Medical Journal - March 2020, Vol. 43, Issue 01 11Haryana Medical Journal - March 2020, Vol. 43, Issue 01
This image shows the surgeon wearing the PPE. Note that all parts of the body must be covered in the PPE. You then
don the sterile gown as shown in the next pic
Conduct of surgery pics…Address of Correspondence HOD CVTS
Amandeep group of hospitals Amritsar, Pathankot, Jammu.
12Haryana Medical Journal - March 2020, Vol. 43, Issue 01 13Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� R e t g r o p e r i t o n e a l lymphangiomyomatosis ( LAM )
� Gastrointestinal polyps
� Pancreatic neuroendocrine tumours.
� Cardiac Rhabdomyomas
� o� Benign striated muscle tumour characterised by the presence of spider cells
� o� Seen in 50-65% of patients with tuberous sclerosis
Musculoskeletal
� Sclerotic bone lesions: 40-66%
� Hyperostosis of the inner table of the calvaria
� Periosteal new bone
� Scoliosis
� Bone cysts
Skin
Cutaneous lesions are present in ~95% of cases, but are rarely appreciated radiographically:
� Hypopigmented Macules ( ash leaf spots ) : seen in 90% of patients
� Facial angiofibromas (Pringle nodules or adenoma sebaceum); seen in 75% of patients
� Fibrous plaques of the forehead (15-20%)
� Confe t t i l es ions : - var ian t of leukoderma spots
� Shagreen patches : seen in 20-30% of patients
� Periungual fibroma : 20% of patients
Treatment and prognosis
Treatment of seizures is essential and depending on the degree of intellectual
number of manifestations, involving many organ systems. The most common radiographic manifestations are:
� Cortical or Subependymal tubers and white matter abnormalities
� Renal Angiomyolipoma
� Cardiac Rhabdomyoma ( s)
Neurological
� Cortical/Subcortical tubers : 50% are in the frontal lobe; high T2 and low T1 with only 10% of tubers showing enhancement; frequently calcify after two years of age
� Subependymal Harmartomas
o� Visible within the first six months of age.
o� Variable signal, frequently high T1 and iso to high T2
o� Enhancement is variable and is not a useful feature in distinguishing them from subependymal giant cell astrocytomas (SGCA); only serial growth is reliable.
Abdominal
� Renal Angiomyolipoma (s)
� o� Tuberous sclerosis accounts for 20% of all angiomyolipomas.
� o� Angiomyolipomas are seen in 55-75% of patient with tuberous sclerosis
� o� Tend to be multiple, large and bilateral
� o� Renal Cysts :
� o� 18-53% of patients with tuberous sclerosis
� R e n a l c e l l C a r c i n o m a a n d oncocytomas
BOURNEVILLE DISEASE : AN INTERESTING CASE
Dr. Sanjiv Kaushal
I came across this patient who had come from a nearby village to my Radiological Clinic in Sirsa for evaluation of seizures.
Bourneville Disease or
Tuberous sclerosis
Tuberous sclerosis, also known as Bourneville disease, is a neurocutaneous disorder characterised by the development
of multiple benign tumours of the embryonic ectoderm (e.g. skin, eyes, and nervous system).
Epidemiology
Tuberous sclerosis has an incidence of 1:6000-12,000, with most being sporadic
Clinical presentation
Tuberous sclerosis was classically described as presenting in childhood with a triad (Vogt triad) of:
1.� Seizures: absent in one-quarter of individuals
2.� Intellectual Disability: up to half have normal intelligence
3.� Adenoma Sebaceum: only present in about three-quarters of patients
The full triad is only seen in a minority of patients (~30%). Therefore, diagnostic criteria have been developed to aid the diagnosis of tuberous sclerosis.
When patients do not meet these criteria, they are sometimes referred to as manifesting a forme fruste of the condition.
Pathology
Spontaneous mutations account for 50-86% of cases, with the remainder inherited as an autosomal dominant condition.
Radiographic features
Tuberous sclerosis has a significant
12Haryana Medical Journal - March 2020, Vol. 43, Issue 01 13Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� R e t g r o p e r i t o n e a l lymphangiomyomatosis ( LAM )
� Gastrointestinal polyps
� Pancreatic neuroendocrine tumours.
� Cardiac Rhabdomyomas
� o� Benign striated muscle tumour characterised by the presence of spider cells
� o� Seen in 50-65% of patients with tuberous sclerosis
Musculoskeletal
� Sclerotic bone lesions: 40-66%
� Hyperostosis of the inner table of the calvaria
� Periosteal new bone
� Scoliosis
� Bone cysts
Skin
Cutaneous lesions are present in ~95% of cases, but are rarely appreciated radiographically:
� Hypopigmented Macules ( ash leaf spots ) : seen in 90% of patients
� Facial angiofibromas (Pringle nodules or adenoma sebaceum); seen in 75% of patients
� Fibrous plaques of the forehead (15-20%)
� Confe t t i l es ions : - var ian t of leukoderma spots
� Shagreen patches : seen in 20-30% of patients
� Periungual fibroma : 20% of patients
Treatment and prognosis
Treatment of seizures is essential and depending on the degree of intellectual
number of manifestations, involving many organ systems. The most common radiographic manifestations are:
� Cortical or Subependymal tubers and white matter abnormalities
� Renal Angiomyolipoma
� Cardiac Rhabdomyoma ( s)
Neurological
� Cortical/Subcortical tubers : 50% are in the frontal lobe; high T2 and low T1 with only 10% of tubers showing enhancement; frequently calcify after two years of age
� Subependymal Harmartomas
o� Visible within the first six months of age.
o� Variable signal, frequently high T1 and iso to high T2
o� Enhancement is variable and is not a useful feature in distinguishing them from subependymal giant cell astrocytomas (SGCA); only serial growth is reliable.
Abdominal
� Renal Angiomyolipoma (s)
� o� Tuberous sclerosis accounts for 20% of all angiomyolipomas.
� o� Angiomyolipomas are seen in 55-75% of patient with tuberous sclerosis
� o� Tend to be multiple, large and bilateral
� o� Renal Cysts :
� o� 18-53% of patients with tuberous sclerosis
� R e n a l c e l l C a r c i n o m a a n d oncocytomas
BOURNEVILLE DISEASE : AN INTERESTING CASE
Dr. Sanjiv Kaushal
I came across this patient who had come from a nearby village to my Radiological Clinic in Sirsa for evaluation of seizures.
Bourneville Disease or
Tuberous sclerosis
Tuberous sclerosis, also known as Bourneville disease, is a neurocutaneous disorder characterised by the development
of multiple benign tumours of the embryonic ectoderm (e.g. skin, eyes, and nervous system).
Epidemiology
Tuberous sclerosis has an incidence of 1:6000-12,000, with most being sporadic
Clinical presentation
Tuberous sclerosis was classically described as presenting in childhood with a triad (Vogt triad) of:
1.� Seizures: absent in one-quarter of individuals
2.� Intellectual Disability: up to half have normal intelligence
3.� Adenoma Sebaceum: only present in about three-quarters of patients
The full triad is only seen in a minority of patients (~30%). Therefore, diagnostic criteria have been developed to aid the diagnosis of tuberous sclerosis.
When patients do not meet these criteria, they are sometimes referred to as manifesting a forme fruste of the condition.
Pathology
Spontaneous mutations account for 50-86% of cases, with the remainder inherited as an autosomal dominant condition.
Radiographic features
Tuberous sclerosis has a significant
14Haryana Medical Journal - March 2020, Vol. 43, Issue 01 15Haryana Medical Journal - March 2020, Vol. 43, Issue 01
this disease leading some books to refer to it as “Bourneville-Pringle disease”.
� Heinrich Vogt (1875-1936) was a German neurologist that is notable by establishing the three pathognomonic clinical signs for tuberous sclerosis that became known as “Vogt triad”.
Address of Correspondence
� DR. SANJIV KAUSHAL [ MBBS, MD Radio-Diagnosis ]
Shubham Ultrasound Centre & City Diagnostic Centre, Sirsa
PIN :- 125055
Mob. :- 92154-25600
Email :- [email protected]
disability, supportive care may be required. Treatment will be dictated by i n d i v i d u a l m a n i f e s t a t i o n s ( e . g . Subependymal giant cell astrocytomas, or retroperitoneal haemorrhage from renal angiomyolipoma ).
� Approximately 40% of patients die by age 35 from complications of one or more of the manifestations mentioned above.
History and etymology
� Désiré-Magloire Bourneville (1840-1909) was a French neurologist that is notable by the initial description of tuberous sclerosis (“Bourneville disease”) in 1880.
� John James Pringle (1855-1922) was a Scottish dermatologist that also studied
PREGNANCY IN COVID-19
*Dr. Jyoti Malik ** Dr. Hena Kausar ,
INTRODUCTION:
Novel coronavirus (SARS-COV-2) is a new mutant strain of coronavirus causing COVID-19, first identified in Wuhan, China and remained the country with highest number of infected individuals where it appeared towards the end of 2019. It became a major epidemic in China and later on evolving pandemic worldwide. Other coraonavirus infections are common cold (HCoV 229E, NL63, OC43, Middle East Respiratory Syndrome MERS-CoV, Severe Acute Respiratory Syndrome SARS CoV) etc. This epidemic has spread to 118 countries around the world. (1).As on 20th April 2020 the world wide statistics are:
•� Covid19 World: 2.4 million cases, 600,000 recovered & 165,069 deceased,India records 1553 cases in 24 hrs; total crosses 17,000.
Transmission:
� Globally most cases of COVID-19 have evidence of human to human transmission. Virus can be readily isolated from respiratory secretions, faeces and fomites.
� With regard to vertical transmission (transmission from mother to baby antenatally or intrapartum), emerging evidence now suggests that vertical transmission is probable, although proportion of pregnancies affected and the significance to the neonate has yet to be determined. Two reports have
published evidence of IgM for SARS-CoV-2 in neonatal serum at birth (2, 3). Since IgM does not cross the placenta this indicates neonatal immune response to in utero infection.
� A case series published by Chen et al, tested amniotic fluid, cord blood, neonatal throat swabs, genital fluid and breast milk samples from COVID-19 infected mothers and all s a m p l e s t e s t e d n e g a t i v e f o r virus(4,5,6,7).
� At present there are no recorded COVID-19 positive cases from vaginal secretion infections.
Effect of COVID-19 On pregnancy:
� Pregnant women do not appear to be more susceptible to infection with COVID-19 than general population. Limited data are available at present but cases with concomitant medical disorders are to be taken care of as virus has tendency to be more virulent i n i m m u n o c o m p r o m i s e d o r chronically ill patients.
� Majority of women will experience only mild or moderate cold/flu like symptoms . Feve r, cough and shortness of breath may be present.
� M o r e s e v e r e s y m p t o m s l i k e pneumonia and hypoxia are mainly seen in immunocompromised and in those with chronic illnesses such as diabetes, cancer and chronic lung and
14Haryana Medical Journal - March 2020, Vol. 43, Issue 01 15Haryana Medical Journal - March 2020, Vol. 43, Issue 01
this disease leading some books to refer to it as “Bourneville-Pringle disease”.
� Heinrich Vogt (1875-1936) was a German neurologist that is notable by establishing the three pathognomonic clinical signs for tuberous sclerosis that became known as “Vogt triad”.
Address of Correspondence
� DR. SANJIV KAUSHAL [ MBBS, MD Radio-Diagnosis ]
Shubham Ultrasound Centre & City Diagnostic Centre, Sirsa
PIN :- 125055
Mob. :- 92154-25600
Email :- [email protected]
disability, supportive care may be required. Treatment will be dictated by i n d i v i d u a l m a n i f e s t a t i o n s ( e . g . Subependymal giant cell astrocytomas, or retroperitoneal haemorrhage from renal angiomyolipoma ).
� Approximately 40% of patients die by age 35 from complications of one or more of the manifestations mentioned above.
History and etymology
� Désiré-Magloire Bourneville (1840-1909) was a French neurologist that is notable by the initial description of tuberous sclerosis (“Bourneville disease”) in 1880.
� John James Pringle (1855-1922) was a Scottish dermatologist that also studied
PREGNANCY IN COVID-19
*Dr. Jyoti Malik ** Dr. Hena Kausar ,
INTRODUCTION:
Novel coronavirus (SARS-COV-2) is a new mutant strain of coronavirus causing COVID-19, first identified in Wuhan, China and remained the country with highest number of infected individuals where it appeared towards the end of 2019. It became a major epidemic in China and later on evolving pandemic worldwide. Other coraonavirus infections are common cold (HCoV 229E, NL63, OC43, Middle East Respiratory Syndrome MERS-CoV, Severe Acute Respiratory Syndrome SARS CoV) etc. This epidemic has spread to 118 countries around the world. (1).As on 20th April 2020 the world wide statistics are:
•� Covid19 World: 2.4 million cases, 600,000 recovered & 165,069 deceased,India records 1553 cases in 24 hrs; total crosses 17,000.
Transmission:
� Globally most cases of COVID-19 have evidence of human to human transmission. Virus can be readily isolated from respiratory secretions, faeces and fomites.
� With regard to vertical transmission (transmission from mother to baby antenatally or intrapartum), emerging evidence now suggests that vertical transmission is probable, although proportion of pregnancies affected and the significance to the neonate has yet to be determined. Two reports have
published evidence of IgM for SARS-CoV-2 in neonatal serum at birth (2, 3). Since IgM does not cross the placenta this indicates neonatal immune response to in utero infection.
� A case series published by Chen et al, tested amniotic fluid, cord blood, neonatal throat swabs, genital fluid and breast milk samples from COVID-19 infected mothers and all s a m p l e s t e s t e d n e g a t i v e f o r virus(4,5,6,7).
� At present there are no recorded COVID-19 positive cases from vaginal secretion infections.
Effect of COVID-19 On pregnancy:
� Pregnant women do not appear to be more susceptible to infection with COVID-19 than general population. Limited data are available at present but cases with concomitant medical disorders are to be taken care of as virus has tendency to be more virulent i n i m m u n o c o m p r o m i s e d o r chronically ill patients.
� Majority of women will experience only mild or moderate cold/flu like symptoms . Feve r, cough and shortness of breath may be present.
� M o r e s e v e r e s y m p t o m s l i k e pneumonia and hypoxia are mainly seen in immunocompromised and in those with chronic illnesses such as diabetes, cancer and chronic lung and
16Haryana Medical Journal - March 2020, Vol. 43, Issue 01 17Haryana Medical Journal - March 2020, Vol. 43, Issue 01
(In two Chinese case series, including a total of 18 pregnant women infected with COVID-19 and 19 babies (one set of twins), there were 8 reported cases of fetal compromise). Given this r e l a t i v e l y h i g h r a t e o f f e t a l compromise, continuous electronic fetal monitoring in labor is currently recommended for all women with COVID-19.
� If woman has signs of sepsis, investigation and treatment to be done as per guidance on sepsis in pregnancy but active COVID-19 to be considered as a cause of sepsis and investigate according to guidance.
� If maternal stabilization is required before delivery, this is the priority, as it is in other maternity emergencies e.g severe pre-eclampsia(8)
� Neonatal team should be informed in advance for delivery of moderate-severe COVID-19 patients.
� Mode of birth should not be influenced by the presence of COVID-19 infection, unless the woman’s respiratory condition demands urgent delivery.
� There is no evidence that epidural or spinal anesthesia is contraindicated in coronavirus infection. Epidural analgesia should be recommended in labor to women with suspected/confirmed COVID-19 cases to minimize the need for general anesthesia if urgent delivery is needed and there is a risk that use of Entonox may increase aerosolisation and spread of virus.
� If woman’s symptoms deteorate then individual assessment regarding the risks and benefits of continuation of
facilities.
� Antenatal ultrasonography to be recommended for fetal growth surveillance 14 days after resolution of acute illness.
� All routine investigations should be minimized.
� At the time of discharge from hospitalfollowing a period of care for confirmed COVID-19 infection. All women should be prescribed at least 1 0 d a y s o f p r o p h y l a c t i c l o w m o e c u l a l a r w e i g h t h a e p a r i n (LMWH).(9)
Intrapartum Care
� Once settled in isolation room, a comple t e an t ena t a l and f e t a l assessment should be conducted following assessment of the severity of COVID-19 symptoms including multidisciplinary team approach along with consultant obstetrician, medical specialist(infectious disease specialist if available), consultant anesthetist, nursing in charge, delivery preferably at tertiary care centre, proper maternal vitals charting (temperature, respiratory rate, and oxygen saturation)
� Confirmation of onset of labor to be done as per standard care.
� Women wi th mi ld COVID-19 symptoms can be encouraged for self isolation at home in the latent phase of labor
� Aim to keep oxygen saturation >94% and titrate oxygen accordingly.
� C o n t i n u o u s e l e c t r o n i c f e t a l monitoring is recommended in labor by using cardiotocograph (CTG).
weeks of gestation age, unless they meet self isolation criteria
� For women with mild symptoms, appointments can be deferred until 7 days after start of symptoms, unless symptoms (aside from persistent cough) become severe. Daily fetal movement count to be maintained.
� For women who are self – quarantined because someone in their household has possible symptoms of COVID-19 then there appointments should be deferred for 14 days.
� If a woman misses her routine appointment for more than 3 weeks should be contacted .( In rural areas ANMs/ASHAs can contact by telephone/routine household visits with PPE)
� If woman needed to visit her health care centre then she should take her own transport or call 108, informing about her status to the attending staff.
� Staff should take PPE (personal protective equipment) precautions as per local guidelines while handling suspected or confirmed COVID-19 cases.
� If a woman was previously negative for COVID-19, if she presents with symptoms again, COVID-19 should be suspected.
� Wo m e n s h o u l d b e e s c o r t e d immediately to isolation room, suitable for majority of care during hospital visit or stay.
� For overnight stays, isolation rooms should ideally have ante-chamber for d o n n i n g a n d r e m o v i n g P P E equipment and ensuite bathroom
heart disease etc.
� Pregnant women with heart disease are at highest risk (congenital or acquired(8)
� Mental health of pregnant women is of equal importance as uncertainty regarding diagnosis and treatment letting increased level of perinatal anxiety and also there are increased rate of domestic violence cases as an i m p a c t o f l o c k d o w n d u e t o coronavirus pandemic worldwide.
Effect of COVID-19 on the fetus:
� Currently there is no data suggesting an increased risk of miscarriage or early pregnancy loss. There is no clear evidence of preterm birth or preterm rupture of membranes related to COVID-19 infection.
� There is no evidence suggesting this virus is teratogenic.
� COVID-19 infection is not an indication for Medical Termination of Pregnancy as of now.
General advice for antenatal women:
Medical History-
� A detailed travel history within last 14 days particularly
� History of any exposure to people with symptoms of COVID-19
� Symptoms of COVID-19
� Coming from a hot spot area
� Any immunocompromised condition
Antenatal Care-
� Women should be advised to attend antenatal cl inic minimizing i t according to discretion of the maternal care provider at 12,20,28 and 36
16Haryana Medical Journal - March 2020, Vol. 43, Issue 01 17Haryana Medical Journal - March 2020, Vol. 43, Issue 01
(In two Chinese case series, including a total of 18 pregnant women infected with COVID-19 and 19 babies (one set of twins), there were 8 reported cases of fetal compromise). Given this r e l a t i v e l y h i g h r a t e o f f e t a l compromise, continuous electronic fetal monitoring in labor is currently recommended for all women with COVID-19.
� If woman has signs of sepsis, investigation and treatment to be done as per guidance on sepsis in pregnancy but active COVID-19 to be considered as a cause of sepsis and investigate according to guidance.
� If maternal stabilization is required before delivery, this is the priority, as it is in other maternity emergencies e.g severe pre-eclampsia(8)
� Neonatal team should be informed in advance for delivery of moderate-severe COVID-19 patients.
� Mode of birth should not be influenced by the presence of COVID-19 infection, unless the woman’s respiratory condition demands urgent delivery.
� There is no evidence that epidural or spinal anesthesia is contraindicated in coronavirus infection. Epidural analgesia should be recommended in labor to women with suspected/confirmed COVID-19 cases to minimize the need for general anesthesia if urgent delivery is needed and there is a risk that use of Entonox may increase aerosolisation and spread of virus.
� If woman’s symptoms deteorate then individual assessment regarding the risks and benefits of continuation of
facilities.
� Antenatal ultrasonography to be recommended for fetal growth surveillance 14 days after resolution of acute illness.
� All routine investigations should be minimized.
� At the time of discharge from hospitalfollowing a period of care for confirmed COVID-19 infection. All women should be prescribed at least 1 0 d a y s o f p r o p h y l a c t i c l o w m o e c u l a l a r w e i g h t h a e p a r i n (LMWH).(9)
Intrapartum Care
� Once settled in isolation room, a comple t e an t ena t a l and f e t a l assessment should be conducted following assessment of the severity of COVID-19 symptoms including multidisciplinary team approach along with consultant obstetrician, medical specialist(infectious disease specialist if available), consultant anesthetist, nursing in charge, delivery preferably at tertiary care centre, proper maternal vitals charting (temperature, respiratory rate, and oxygen saturation)
� Confirmation of onset of labor to be done as per standard care.
� Women wi th mi ld COVID-19 symptoms can be encouraged for self isolation at home in the latent phase of labor
� Aim to keep oxygen saturation >94% and titrate oxygen accordingly.
� C o n t i n u o u s e l e c t r o n i c f e t a l monitoring is recommended in labor by using cardiotocograph (CTG).
weeks of gestation age, unless they meet self isolation criteria
� For women with mild symptoms, appointments can be deferred until 7 days after start of symptoms, unless symptoms (aside from persistent cough) become severe. Daily fetal movement count to be maintained.
� For women who are self – quarantined because someone in their household has possible symptoms of COVID-19 then there appointments should be deferred for 14 days.
� If a woman misses her routine appointment for more than 3 weeks should be contacted .( In rural areas ANMs/ASHAs can contact by telephone/routine household visits with PPE)
� If woman needed to visit her health care centre then she should take her own transport or call 108, informing about her status to the attending staff.
� Staff should take PPE (personal protective equipment) precautions as per local guidelines while handling suspected or confirmed COVID-19 cases.
� If a woman was previously negative for COVID-19, if she presents with symptoms again, COVID-19 should be suspected.
� Wo m e n s h o u l d b e e s c o r t e d immediately to isolation room, suitable for majority of care during hospital visit or stay.
� For overnight stays, isolation rooms should ideally have ante-chamber for d o n n i n g a n d r e m o v i n g P P E equipment and ensuite bathroom
heart disease etc.
� Pregnant women with heart disease are at highest risk (congenital or acquired(8)
� Mental health of pregnant women is of equal importance as uncertainty regarding diagnosis and treatment letting increased level of perinatal anxiety and also there are increased rate of domestic violence cases as an i m p a c t o f l o c k d o w n d u e t o coronavirus pandemic worldwide.
Effect of COVID-19 on the fetus:
� Currently there is no data suggesting an increased risk of miscarriage or early pregnancy loss. There is no clear evidence of preterm birth or preterm rupture of membranes related to COVID-19 infection.
� There is no evidence suggesting this virus is teratogenic.
� COVID-19 infection is not an indication for Medical Termination of Pregnancy as of now.
General advice for antenatal women:
Medical History-
� A detailed travel history within last 14 days particularly
� History of any exposure to people with symptoms of COVID-19
� Symptoms of COVID-19
� Coming from a hot spot area
� Any immunocompromised condition
Antenatal Care-
� Women should be advised to attend antenatal cl inic minimizing i t according to discretion of the maternal care provider at 12,20,28 and 36
18Haryana Medical Journal - March 2020, Vol. 43, Issue 01 19Haryana Medical Journal - March 2020, Vol. 43, Issue 01
3. Chen H, Guo J, Wang C et al, Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of m e d i c a l r e c o r d s . Lancet2020;395:809-815
4. Chen Y, Peng H, Wang L et al. Infants b o r n t o m o t h e r s w i t h a n e w coronavirus (COVID-19). Frontiers in P e d i a t r i c s 2 0 2 0 ; 8 ( 1 0 8 ) doi:103389/fped.2020.00104
5. Li N, Han L, Peng M, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case control study. Pre –print doi: 10.1101/2020.03.10.20033605
6. Zhu H,Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Trans Pediatr. 2020;9:51-60
7. ICMR : Guidance for management of pregnant women in COVID-19 Pandemic(1.1)
8. The Royal College of Obstetrics and Gynaecology, COVID-19 Infection in Pregnancy; Version 8[online] April 17,2020. Accessed on April 19,2020.
9. Reduc ing the r i sk o f Venous Thromboembolism during Pregnancy and the puerperium. In: Royal College of Obstetricians and Gynaecologists, ed. Green - top guidelines, 2015
Address of CorrespondenceDr. Jyoti Malik
MBBS, DGO, DNB, MNAMS, MRCOG-1, FICS
(Sr. Consultant, Infertility Specialist & Lap Surgeon -
J J Institute of Medical Sciences & ROOTS IVF, Bahadurgarh,Haryana.)
baby, bottles or breast pumps.
� Follow recommendations for breast pump cleaning after each use.
� Expressed breast milk should be fed to the new-born by a healthy care-giver.
� If mother wishes to feed at the breast, she should wear a fluid resistant surgical facemask and practice hand hygiene before each feeding.
Hospital Discharge:
� Test should be negative for both mother and new-born and condition should be stable.
� At the time of discharge from hospital following a period of care for confirmed COVID-19 , which includes the birth of her baby, all women should be prescribed at least 10 days of prophylactic LMWH.(9). This should be prescribed regardless of the mode of birth. A longer course should be prescribed if indicated by existing guidance (10).
References:
1. WHO. Coronavirus disease 2019 (COVID-19) situation report 46. M a r c h 6 , 2 0 2 0 . https://www.who.int/docs/default-s o u r c e / c o r o n a v i r u s / s i t u a t i o n reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2
2. Dong L, Tian J, He S,et al. Possible vertical transmission of SARS-COV-2 From an infected mother to her n e w b o r n . J A M A 2 0 2 0 doi:10.1001/jama.2020.4621
3. Zeng H, Xu C, Fan J, et al. Antibodies in Infants Born to Mothers with COVID-19 Pneumonia. JAMA 2020 doi:10.1001/jama2020.4861
Postnatal Management
� All babies of women with suspected or confirmed cases of COVID-19 need to be tested for COVID-19.
� Babies born to COVID-19 positive mothers should undergo appropriate c l o s e m o n i t o r i n g a n d e a r l y involvement of neonatal care, if necessary.
� Babies who are born to COVID-19 positive mothers need neonatal follow-up and ongoing surveillance after discharge.
� As per current limited evidence it is advised that women and healthy infants, not otherwise requiring neonatal care, are kept together in the immediate postpartum period.
� Literature from China advised separate isolation of infected mother and her baby for 14 days.
� The decision for discontinuation of temporary separation of the mother from her baby should be made on case-by-case basis.
� If colocation (“rooming in”) of the newborn with the mother is done in accordance with mother wishes or if u n a v o i d a b l e d u e t o f a c i l i t y limitations, consider using physical barriers like curtain between mother and new-born and keep the new-born 6 feet away from the ill mother.
Breastfeeding:
� For mothers who intend to breastfeed should be encouraged to express their breast milk to establish and maintain milk supply.
� Hand washing before touching the
labor versus caesarean section to be done.
� An individualized decision to cut short second stage of labor to be made for i n s t r u m e n t a l d e l i v e r y i n a s y m p t o m a t i c w o m a n w h o i s exhausted or hypoxic.
� All p rocedures e i ther normal vaginal/ instrumental/caesarean delivery to be done wearing PPE.
� Due to lack of evidence, delayed cord clamping is still recommended after birth, provided there are no other contraindications.
Management of patients with COVID-19 Admitted to Critical Care:
� Hourly monitoring with both absolute values and trends
� Titrating oxygen saturation >94%
� A rise in respiratory rate, even if saturations are normal may indicate deterioration in respiratory function and should be managed by starting or increasing oxygen.
� Radiographic investigations should be done as per non pregnant patient e.g chest x-ray, CT scan of the chest maintaining standard protocol of abdominal shield and not delayed due to fetal concerns.
� Consider additional investigations to rule out differential diagnosis e.g ECG, CTPA, echocardiogram etc. All pyrexia not to be assumed of COVID-19 and full sepsis screening to be performed.
� A p p l y c a u t i o n w i t h I V fl u i d management with special attention to avoid fluid overload.
18Haryana Medical Journal - March 2020, Vol. 43, Issue 01 19Haryana Medical Journal - March 2020, Vol. 43, Issue 01
3. Chen H, Guo J, Wang C et al, Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of m e d i c a l r e c o r d s . Lancet2020;395:809-815
4. Chen Y, Peng H, Wang L et al. Infants b o r n t o m o t h e r s w i t h a n e w coronavirus (COVID-19). Frontiers in P e d i a t r i c s 2 0 2 0 ; 8 ( 1 0 8 ) doi:103389/fped.2020.00104
5. Li N, Han L, Peng M, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case control study. Pre –print doi: 10.1101/2020.03.10.20033605
6. Zhu H,Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Trans Pediatr. 2020;9:51-60
7. ICMR : Guidance for management of pregnant women in COVID-19 Pandemic(1.1)
8. The Royal College of Obstetrics and Gynaecology, COVID-19 Infection in Pregnancy; Version 8[online] April 17,2020. Accessed on April 19,2020.
9. Reduc ing the r i sk o f Venous Thromboembolism during Pregnancy and the puerperium. In: Royal College of Obstetricians and Gynaecologists, ed. Green - top guidelines, 2015
Address of CorrespondenceDr. Jyoti Malik
MBBS, DGO, DNB, MNAMS, MRCOG-1, FICS
(Sr. Consultant, Infertility Specialist & Lap Surgeon -
J J Institute of Medical Sciences & ROOTS IVF, Bahadurgarh,Haryana.)
baby, bottles or breast pumps.
� Follow recommendations for breast pump cleaning after each use.
� Expressed breast milk should be fed to the new-born by a healthy care-giver.
� If mother wishes to feed at the breast, she should wear a fluid resistant surgical facemask and practice hand hygiene before each feeding.
Hospital Discharge:
� Test should be negative for both mother and new-born and condition should be stable.
� At the time of discharge from hospital following a period of care for confirmed COVID-19 , which includes the birth of her baby, all women should be prescribed at least 10 days of prophylactic LMWH.(9). This should be prescribed regardless of the mode of birth. A longer course should be prescribed if indicated by existing guidance (10).
References:
1. WHO. Coronavirus disease 2019 (COVID-19) situation report 46. M a r c h 6 , 2 0 2 0 . https://www.who.int/docs/default-s o u r c e / c o r o n a v i r u s / s i t u a t i o n reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2
2. Dong L, Tian J, He S,et al. Possible vertical transmission of SARS-COV-2 From an infected mother to her n e w b o r n . J A M A 2 0 2 0 doi:10.1001/jama.2020.4621
3. Zeng H, Xu C, Fan J, et al. Antibodies in Infants Born to Mothers with COVID-19 Pneumonia. JAMA 2020 doi:10.1001/jama2020.4861
Postnatal Management
� All babies of women with suspected or confirmed cases of COVID-19 need to be tested for COVID-19.
� Babies born to COVID-19 positive mothers should undergo appropriate c l o s e m o n i t o r i n g a n d e a r l y involvement of neonatal care, if necessary.
� Babies who are born to COVID-19 positive mothers need neonatal follow-up and ongoing surveillance after discharge.
� As per current limited evidence it is advised that women and healthy infants, not otherwise requiring neonatal care, are kept together in the immediate postpartum period.
� Literature from China advised separate isolation of infected mother and her baby for 14 days.
� The decision for discontinuation of temporary separation of the mother from her baby should be made on case-by-case basis.
� If colocation (“rooming in”) of the newborn with the mother is done in accordance with mother wishes or if u n a v o i d a b l e d u e t o f a c i l i t y limitations, consider using physical barriers like curtain between mother and new-born and keep the new-born 6 feet away from the ill mother.
Breastfeeding:
� For mothers who intend to breastfeed should be encouraged to express their breast milk to establish and maintain milk supply.
� Hand washing before touching the
labor versus caesarean section to be done.
� An individualized decision to cut short second stage of labor to be made for i n s t r u m e n t a l d e l i v e r y i n a s y m p t o m a t i c w o m a n w h o i s exhausted or hypoxic.
� All p rocedures e i ther normal vaginal/ instrumental/caesarean delivery to be done wearing PPE.
� Due to lack of evidence, delayed cord clamping is still recommended after birth, provided there are no other contraindications.
Management of patients with COVID-19 Admitted to Critical Care:
� Hourly monitoring with both absolute values and trends
� Titrating oxygen saturation >94%
� A rise in respiratory rate, even if saturations are normal may indicate deterioration in respiratory function and should be managed by starting or increasing oxygen.
� Radiographic investigations should be done as per non pregnant patient e.g chest x-ray, CT scan of the chest maintaining standard protocol of abdominal shield and not delayed due to fetal concerns.
� Consider additional investigations to rule out differential diagnosis e.g ECG, CTPA, echocardiogram etc. All pyrexia not to be assumed of COVID-19 and full sepsis screening to be performed.
� A p p l y c a u t i o n w i t h I V fl u i d management with special attention to avoid fluid overload.
20Haryana Medical Journal - March 2020, Vol. 43, Issue 01 21Haryana Medical Journal - March 2020, Vol. 43, Issue 01
SKELETAL MUSCLES IN PATIENTS WITH CHRONIC LIVER DISEASE
Dr Praveen Sharma , Dr Anil Arora
Abstract: Common known complications of cirrhotic patients are ascites, variceal bleeding, kidney dysfunction, hepatic encephalopathy and hepatocellular carcinoma. Malnutrition and loss and function of muscle mass (sarcopenia) is a complication that is been widely recognized now, and it negatively impact survival, quality of life, and response to infection and surgery in patients with cirrhosis. Despite the important role that malnutrition and sarcopenia play in the prognosis of patients with cirrhosis, they are frequently missed or not assessed due to lack of bedside easy tools. Sarcopenic obesity is a condition in which patient with cirrhosis develop simultaneous loss of skeletal muscle and increase in adipose tissue. Muscle role has been implicated in ammonia reduction, maintaining insulin resistance, non alcoholic fatty liver disease, amino acid metabolism and maintain body temperature. Sarcopenia in cirrhotic patients has shown to have i n c r e a s e d m o r b i d i t y, m o r t a l i t y, hype rammonemia , ove r t hepa t i c encephalopathy, and increased length of stay and septic complications after liver transplantation. Muscularity assessment with cross-sectional imaging studies, handgrip strength and anthropometric measurement has become an important index of nutritional status evaluation in cirrhosis, as sarcopenia reflects a chronic detriment, rather than acute severity of the liver disease.
Introduction
Skeletal muscle contributes 30–40% of total body mass in a healthy human and contains up to 70-75% of total body proteins. Besides contraction which helps in movement of body, muscle has multiple metabolic roles. It is now considered as an important endocrine organ in our body. It is a major determinant of energy expenditure including resting energy expenditure; it participates in maintaining body core temperature maintenance and is a storage site for amino acids and carbohydrates. Muscle synchronically acts with the liver and adipose tissue for regulation of energy homeostasis in our body(1,2).
Sarcopenia is defined as progressive and generalized loss of skeletal muscle mass, strength and function (3,4). On an average an adult lose their skeletal muscle at the rate of 0.5% of its mass annually, if there in no other co morbid condition like obesity, insulin resistance or diabetes. However, this process accelerates after the age of 60-65, to the extent that at the age of 80 an individual has only 40% of their peak muscle mass. It has been shown that sarcopenia leads to physical disability, and functional decline and poor quality of life (QOL) in many disease like diabetes, cardiac failure, renal disease and chronic obstructive airway disease (5-7). Similarly sarcopenia in patients with cirrhosis is associated poor prognosis and increased mortality both before and after
due to aerobic metabolic rate.These muscles are normally not affected early in chronic liver disease. Type IIa, are called fast oxidative fibers, as contain large amount of mitochondria and myoglobin. They utilize both aerobic and anaerobic metabolism, consequently generating faster, and stronger contractions. Type IIb, are called fast glycolytic fibers, these muscles are white due to a lower level of myoglobin, and they produce ATP slowly by anaerobic metabolism and break it down very rapidly. Finally, type IIx fibers contain very few mitochondria, have a high glycolytic capacity and fatigue quickly. Type II fibers are more sensitive to disease states like chronic liver disease as they are unable to counteract the upregulatation of ubiquitin in these states(14-16) (Figure-1)
Type of muscle fibre:
Prevalence of Sarcopenia in patients with cirrhosis:
Sarcopenia prevalence varies with different factors like older age, reduced physical inactivity, inadequate dietary intake of energy and/or protein, presence of malabsorption, advanced organ failure (liver, kidney, brain), inflammatory
liver transplantation(8-10).
Sarcopenia is not only restricted to skeletal muscle,these changes are also seen in the cardiac muscle which is known as cardiac sarcopenia. Cardiac sarcopenia is characterised by decrease in myocyte number (decreased muscle mass), increase of fibrosis and collagen deposition and decrease in cardiac function at during stress(11). Our diaphragm which partly consists of skeletal muscle also shows age-related atrophy and reduction of fast t w i t c h fi b e r s i n t h e d i a p h r a g m . Involvement of both cardiac and respiratory muscles can lead to clinical manifestat ions of breathlessness , weakness, reduced exercise tolerance and fatigability which can increase sarcopenia and frailty(12). These cardiac and diaphragm changes in patients with chronic liver disease have not been well established.
Muscle Composition and Fiber Types
Striated skeletal muscles are primarily composed of myofibres,stellete cells and fat. Myofibres represents bulk of muscles tissue, satellite cells helps in maintenance and regeneration of muscle. Fat may accumulate within the cytoplasm of myofibers or accumulates in adipocytes located in between muscle fibers (extra-myocellular lipid).Muscle fat content (ca l led ‘myostea tos is ’ ) has been correlated with risk of increased mortality in patients with liver disease(13).
Skeletal muscle consists of four fiber types (Type I, IIa, IIb and IIx).These muscle differ with regards to their functionality. Type I, also known as slow twitch fibers are seen in neck and spine(postural muscle), have significant amount of myoglobin and are resistant to exhaustion
20Haryana Medical Journal - March 2020, Vol. 43, Issue 01 21Haryana Medical Journal - March 2020, Vol. 43, Issue 01
SKELETAL MUSCLES IN PATIENTS WITH CHRONIC LIVER DISEASE
Dr Praveen Sharma , Dr Anil Arora
Abstract: Common known complications of cirrhotic patients are ascites, variceal bleeding, kidney dysfunction, hepatic encephalopathy and hepatocellular carcinoma. Malnutrition and loss and function of muscle mass (sarcopenia) is a complication that is been widely recognized now, and it negatively impact survival, quality of life, and response to infection and surgery in patients with cirrhosis. Despite the important role that malnutrition and sarcopenia play in the prognosis of patients with cirrhosis, they are frequently missed or not assessed due to lack of bedside easy tools. Sarcopenic obesity is a condition in which patient with cirrhosis develop simultaneous loss of skeletal muscle and increase in adipose tissue. Muscle role has been implicated in ammonia reduction, maintaining insulin resistance, non alcoholic fatty liver disease, amino acid metabolism and maintain body temperature. Sarcopenia in cirrhotic patients has shown to have i n c r e a s e d m o r b i d i t y, m o r t a l i t y, hype rammonemia , ove r t hepa t i c encephalopathy, and increased length of stay and septic complications after liver transplantation. Muscularity assessment with cross-sectional imaging studies, handgrip strength and anthropometric measurement has become an important index of nutritional status evaluation in cirrhosis, as sarcopenia reflects a chronic detriment, rather than acute severity of the liver disease.
Introduction
Skeletal muscle contributes 30–40% of total body mass in a healthy human and contains up to 70-75% of total body proteins. Besides contraction which helps in movement of body, muscle has multiple metabolic roles. It is now considered as an important endocrine organ in our body. It is a major determinant of energy expenditure including resting energy expenditure; it participates in maintaining body core temperature maintenance and is a storage site for amino acids and carbohydrates. Muscle synchronically acts with the liver and adipose tissue for regulation of energy homeostasis in our body(1,2).
Sarcopenia is defined as progressive and generalized loss of skeletal muscle mass, strength and function (3,4). On an average an adult lose their skeletal muscle at the rate of 0.5% of its mass annually, if there in no other co morbid condition like obesity, insulin resistance or diabetes. However, this process accelerates after the age of 60-65, to the extent that at the age of 80 an individual has only 40% of their peak muscle mass. It has been shown that sarcopenia leads to physical disability, and functional decline and poor quality of life (QOL) in many disease like diabetes, cardiac failure, renal disease and chronic obstructive airway disease (5-7). Similarly sarcopenia in patients with cirrhosis is associated poor prognosis and increased mortality both before and after
due to aerobic metabolic rate.These muscles are normally not affected early in chronic liver disease. Type IIa, are called fast oxidative fibers, as contain large amount of mitochondria and myoglobin. They utilize both aerobic and anaerobic metabolism, consequently generating faster, and stronger contractions. Type IIb, are called fast glycolytic fibers, these muscles are white due to a lower level of myoglobin, and they produce ATP slowly by anaerobic metabolism and break it down very rapidly. Finally, type IIx fibers contain very few mitochondria, have a high glycolytic capacity and fatigue quickly. Type II fibers are more sensitive to disease states like chronic liver disease as they are unable to counteract the upregulatation of ubiquitin in these states(14-16) (Figure-1)
Type of muscle fibre:
Prevalence of Sarcopenia in patients with cirrhosis:
Sarcopenia prevalence varies with different factors like older age, reduced physical inactivity, inadequate dietary intake of energy and/or protein, presence of malabsorption, advanced organ failure (liver, kidney, brain), inflammatory
liver transplantation(8-10).
Sarcopenia is not only restricted to skeletal muscle,these changes are also seen in the cardiac muscle which is known as cardiac sarcopenia. Cardiac sarcopenia is characterised by decrease in myocyte number (decreased muscle mass), increase of fibrosis and collagen deposition and decrease in cardiac function at during stress(11). Our diaphragm which partly consists of skeletal muscle also shows age-related atrophy and reduction of fast t w i t c h fi b e r s i n t h e d i a p h r a g m . Involvement of both cardiac and respiratory muscles can lead to clinical manifestat ions of breathlessness , weakness, reduced exercise tolerance and fatigability which can increase sarcopenia and frailty(12). These cardiac and diaphragm changes in patients with chronic liver disease have not been well established.
Muscle Composition and Fiber Types
Striated skeletal muscles are primarily composed of myofibres,stellete cells and fat. Myofibres represents bulk of muscles tissue, satellite cells helps in maintenance and regeneration of muscle. Fat may accumulate within the cytoplasm of myofibers or accumulates in adipocytes located in between muscle fibers (extra-myocellular lipid).Muscle fat content (ca l led ‘myostea tos is ’ ) has been correlated with risk of increased mortality in patients with liver disease(13).
Skeletal muscle consists of four fiber types (Type I, IIa, IIb and IIx).These muscle differ with regards to their functionality. Type I, also known as slow twitch fibers are seen in neck and spine(postural muscle), have significant amount of myoglobin and are resistant to exhaustion
22Haryana Medical Journal - March 2020, Vol. 43, Issue 01 23Haryana Medical Journal - March 2020, Vol. 43, Issue 01
to sarcopenia in patients with cirrhosis. Impaired liver function and portosystemic shunting leads to increased ammonia, reduction in testosterone and growth hormone, increased endotoxemia, as well as decreased dietary nutrient intake contribute to sarcopenia. Increased amino acid disturbances like reduction in the branched chain amino acid, increase in aromatic amino acids and consequent impaired global protein synthesis also contribute to sarcopenia in cirrhosis(24-30).
Assessment of Sarcopenia
Assessment of sarcopenia is a major component of evaluation of malnutrition in patient with cirrhosis. Cross sectional imaging of skeletal muscle using computed tomographic (CT) image analysis at the L3 vertebra is almost universally accepted method to quantify muscle loss. Measurement of Psoas muscles, para spinal and abdominal wall muscles are considered as core skeletal muscles and are assessed for sarcopenia. These muscles are relatively independent of activity and water retention which are seen in cirrhosis, but are consistently altered by the metabolic and molecular perturbations of cirrhosis. Hence L3 SMI is ideal for sarcopenic measurement. Cost
disease like rheumatoid arthritis and inflammatory bowel d i sease and malignancy. Therefore, the prevalence of sarcopenia is higher in elder patients with chronic diseases and/or increasing disease severity. Prevalence of sarcopenia also varies according to the definition of sarcopenia, and the cutoff points for the measurement of muscle mass and strength(17-20).
In cirrhosis sarcopenia is seen in up to 70% of patients and depends upon the method used, stage of liver disease, obese cirrhosis versus non obese cirrhosis, etiology of cirrhosis as alcohol versus non alcohol and gender.
Sarcopenic obesity is a frequent finding in patients with cirrhosis and obesity. Obesity is frequently observed in cirrhosis (20%40%), regardless of the aetiology of liver disease, and patients with cirrhosis may develop simultaneous loss of skeletal muscle and gain of adipose tissue(21). In an analysis of 678 patients with cirrhosis, sarcopenia, sarcopenic obesity and myosteatosis was present in 43%, 20% and 52% respectively(22). Alcohol has been associated with increased prevalence of sarcopenia in few studies and active alcohol intake increased the r isk further(23,24).
Pathogenesis of Sarcopenia:
Skeletal muscle mass is an individual is maintained by a critical balance between protein synthesis, breakdown and regeneration by satellite cells. Skeletal muscle mass depends on a number of factors which include age, gender and ethnicity, cirrhosis stage and etiology of cirrhosis.
Liver dysfunction and portosystemic shunting is prime culprit that contributes
and not affected by the presence of fluid retention. These tests are simple to perform even by a paramedical person and as compared to the diagnosis of sarcopenia by CT or magnetic resonance, the predictive value of MAMC has shown to be reasonable (16,33) . Handgrip strength is a very simple, bedside inexpensive tool which is a effective method to detect malnutrition in cirrhotic patients; and has been shown to predict incidence of major complications and mortality in patients with cirrhosis (19).
and radiation exposure limits the routine use of CT imaging for nutritional assessment in clinical practice. Cut-off values derived from cirrhotic patients on the liver transplant list are 50 cm2/m2 for men and 39 cm2/m2 for women(16,31).
Similarly other body mass assessment can be obtained using simple bedside anthropometric methods including mid-arm muscle circumference (MAMC, defined as mid-arm circumference minus triceps skinfold (TSF)x 0.314), mid-arm muscular area and tricep skin fold which are simple to perform, rapid, low cost,
Screening and diagnosis tools for sarcopenia in cirrhosis
Anthropometry DEXA CT/MRI BIA Handgrip
Overall body size(BMI, MAC),predicted muscle(MAMC), predictedvisceral adipose tissue(WC, W:H, TSF)
Whole‐body andregionalfat, lean, bone mineralcontentand BMD
L3-SMI calculate lean andfat mass
Muscle strength
Abbreviations: BIA, bioelectrical impedance analysis; BMD, bone mass density; BMI, body mass index; CT, computed tomographic; DEXA, dual-energy x-ray absorptiometry; MAC, mid-arm circumference; MAMC, mid-arm muscle circumference; MRI, magnetic resonance
Simplicity� +++� ++� +� +� +++
Cost� +� ++� ++++� ++� +
Validity� +� ++� ++++� ++� +
Clinical use� ++� +� ++� +� ++
and mortality of patients undergoing surgery. Several studies had examined the impact of sarcopenia on the survival of patients on the waiting list of LT and found to be an independent predictor of mortality. Sarcopenia is also a risk factor
Sarcopenia and effect on overall mortality in cirrhosis
Malnutrition is common in patients of cirrhotic patients. It is an independent prognostic factor in predicting morbidity
22Haryana Medical Journal - March 2020, Vol. 43, Issue 01 23Haryana Medical Journal - March 2020, Vol. 43, Issue 01
to sarcopenia in patients with cirrhosis. Impaired liver function and portosystemic shunting leads to increased ammonia, reduction in testosterone and growth hormone, increased endotoxemia, as well as decreased dietary nutrient intake contribute to sarcopenia. Increased amino acid disturbances like reduction in the branched chain amino acid, increase in aromatic amino acids and consequent impaired global protein synthesis also contribute to sarcopenia in cirrhosis(24-30).
Assessment of Sarcopenia
Assessment of sarcopenia is a major component of evaluation of malnutrition in patient with cirrhosis. Cross sectional imaging of skeletal muscle using computed tomographic (CT) image analysis at the L3 vertebra is almost universally accepted method to quantify muscle loss. Measurement of Psoas muscles, para spinal and abdominal wall muscles are considered as core skeletal muscles and are assessed for sarcopenia. These muscles are relatively independent of activity and water retention which are seen in cirrhosis, but are consistently altered by the metabolic and molecular perturbations of cirrhosis. Hence L3 SMI is ideal for sarcopenic measurement. Cost
disease like rheumatoid arthritis and inflammatory bowel d i sease and malignancy. Therefore, the prevalence of sarcopenia is higher in elder patients with chronic diseases and/or increasing disease severity. Prevalence of sarcopenia also varies according to the definition of sarcopenia, and the cutoff points for the measurement of muscle mass and strength(17-20).
In cirrhosis sarcopenia is seen in up to 70% of patients and depends upon the method used, stage of liver disease, obese cirrhosis versus non obese cirrhosis, etiology of cirrhosis as alcohol versus non alcohol and gender.
Sarcopenic obesity is a frequent finding in patients with cirrhosis and obesity. Obesity is frequently observed in cirrhosis (20%40%), regardless of the aetiology of liver disease, and patients with cirrhosis may develop simultaneous loss of skeletal muscle and gain of adipose tissue(21). In an analysis of 678 patients with cirrhosis, sarcopenia, sarcopenic obesity and myosteatosis was present in 43%, 20% and 52% respectively(22). Alcohol has been associated with increased prevalence of sarcopenia in few studies and active alcohol intake increased the r isk further(23,24).
Pathogenesis of Sarcopenia:
Skeletal muscle mass is an individual is maintained by a critical balance between protein synthesis, breakdown and regeneration by satellite cells. Skeletal muscle mass depends on a number of factors which include age, gender and ethnicity, cirrhosis stage and etiology of cirrhosis.
Liver dysfunction and portosystemic shunting is prime culprit that contributes
and not affected by the presence of fluid retention. These tests are simple to perform even by a paramedical person and as compared to the diagnosis of sarcopenia by CT or magnetic resonance, the predictive value of MAMC has shown to be reasonable (16,33) . Handgrip strength is a very simple, bedside inexpensive tool which is a effective method to detect malnutrition in cirrhotic patients; and has been shown to predict incidence of major complications and mortality in patients with cirrhosis (19).
and radiation exposure limits the routine use of CT imaging for nutritional assessment in clinical practice. Cut-off values derived from cirrhotic patients on the liver transplant list are 50 cm2/m2 for men and 39 cm2/m2 for women(16,31).
Similarly other body mass assessment can be obtained using simple bedside anthropometric methods including mid-arm muscle circumference (MAMC, defined as mid-arm circumference minus triceps skinfold (TSF)x 0.314), mid-arm muscular area and tricep skin fold which are simple to perform, rapid, low cost,
Screening and diagnosis tools for sarcopenia in cirrhosis
Anthropometry DEXA CT/MRI BIA Handgrip
Overall body size(BMI, MAC),predicted muscle(MAMC), predictedvisceral adipose tissue(WC, W:H, TSF)
Whole‐body andregionalfat, lean, bone mineralcontentand BMD
L3-SMI calculate lean andfat mass
Muscle strength
Abbreviations: BIA, bioelectrical impedance analysis; BMD, bone mass density; BMI, body mass index; CT, computed tomographic; DEXA, dual-energy x-ray absorptiometry; MAC, mid-arm circumference; MAMC, mid-arm muscle circumference; MRI, magnetic resonance
Simplicity� +++� ++� +� +� +++
Cost� +� ++� ++++� ++� +
Validity� +� ++� ++++� ++� +
Clinical use� ++� +� ++� +� ++
and mortality of patients undergoing surgery. Several studies had examined the impact of sarcopenia on the survival of patients on the waiting list of LT and found to be an independent predictor of mortality. Sarcopenia is also a risk factor
Sarcopenia and effect on overall mortality in cirrhosis
Malnutrition is common in patients of cirrhotic patients. It is an independent prognostic factor in predicting morbidity
24Haryana Medical Journal - March 2020, Vol. 43, Issue 01 25Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Health Aging 2009;13:717-723.
3. Merli M, Berzigotti A, ZelberSagi S, Dasarathy S, Montagnese S, Genton L, et al. Practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70:172193
4. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014 ;15(2):95-101.
5. Collamati A, Marzetti E, Calvani R, Tosato M, D’Angelo E, Sisto AN, et al. S a r c o p e n i a i n h e a r t f a i l u r e : m e c h a n i s m s a n d t h e r a p e u t i c s t r a t e g i e s . J G e r i a t r C a r d i o l 2016;13:615-624
6. Moorthi RN, Avin KG. Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens. 2017;26(3):219-228
7. Munhoz da Rocha Lemos Costa T, Costa FM, Jonasson TH, Moreira CA, Boguszewski CL, Borba VZC. Body composition and sarcopenia in patients with chronic obstructive pulmonary disease. Endocrine. 2018 ;60(1):95-102.
8. Montano-Loza AJ, Meza-Junco J, Prado CM, Lieffers JR, Baracos VE, Bain VG, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol 2012;10:166-173,
9. Tandon P, Ney M, Irwin I, Ma MM, Gramlich L, Bain VG,et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transpl 2012;18:1209-1216.
Summary
Skeletal muscle constitutes one third of total body mass and contains up to 75% of total body proteins in a healthy person. Muscles not only helps in movement of the body but also contributes significantly in maintain body core temperature, amino acid and glucose metabolism and in disposable of ammonia in patients with cirrhosis. Common known complications of cirrhosis include ascites, hepatic e n c e p h a l o p a t h y, v a r i c e a l b l e e d , hepatorenal syndrome. Sarcopenia is now the commonest complication of cirrhosis which is defined as generalized loss of skeletal muscle mass,function and strength. Its presence may aggravate morbidity and mortality in patients with cirrhosis who are on wait list for liver transplantation. Sarcopenia also affects post liver transplant patients as it may increase hospital stay and increase the risk of infections. The evaluation of the skeletal muscle mass and function is difficult due to the lack of a uniform definition and assessment tools. A therapeutic strategy to improve sarcopenia includes dietary manipulations, increased physical activity and exercise, hormone replacement therapies , ammonia-lowering strategies and targeting the underlying liver disease.
References
1. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412-423
2. Bo i r i e Y. Phys iopa tho log i ca l mechanism of sarcopenia. J Nutr
be accomplished by adding either isoleucine or valine, which provides direct a n a p l e r o t i c i n p u t . T h e deamination/transamination of these amino acids as anaplerotic agents results i n r e l e a s e o f a m m o n i a i n a 1 : 1 stoichiometric ratio with only one net ammonia removed during the formation of glutamine (39). Treatment aimed at ammonia reduction has shown to be effective in the prevention and treatment of hepatic encephalopathy but lowering ammonia restores muscle mass in humans has not been validated.
Role of muscle in insulin resistance and n o n a l c o h o l i c f a t t y l i v e r disease(NAFLD)
NAFLD is a spectrum of disease ranging from benign steatosis (fatty liver) to non-alcoholic steatohepatitis (NASH) and is associated with insulin resistance (IR). Mechanisms relating sarcopenia to NASH include the following: insulin resistance, increased inflammation, myokines secreted by skeletal muscle, myostatin, adiponectin, vitamin D deficiency and physical inactivity. In presence of IR, the mTOR pathway remains inactive and cannot inhibit autophagy, or lysosomal degradation of proteins and organelles. These effects contribute to accelerated muscle loss in insulin resistance states(40-42).
Sarcopenia also promotes IR, as the skeletal muscle is the primary tissue responsible for insulin-mediated glucose disposal. Similarly, myosteatosis, is associated with IR. The presence of both sarcopenia and obesity acts synergistically leading to a more severe IR and dysglycemia. Thus, the cycle continues partially explaining the propagation of NASH.
for hepatic encephalopathy and increased risk of decompensation. Not surprisingly, it is associated with a 5-fold increased risk of mortality, independent of MELD-Na score.
Post liver transplantation most of the complications related to liver cirrhrosis and portal hypertension generally improved (or even reversed) however the course of sarcopenia following LT is variable with either improvement, remaining unchanged or continuing to decline. The underlying pathogenesis and mediators of post LT sarcopenia are unclear. Several immunosuppressive agents, especially corticosteroids and mTOR inhibitors, have negative impact on skeletal muscle and appear to be the key drivers of postLT sarcopenia(35-38)
Role of muscle in decreasing ammonia in cirrhosis
Ammonia plays a major role in the pathogenesis of sarcopenia and minimal/ overt HE in cirrhosis(17). Functional hepa tocy t e s l o s s , po r to sys t emic collaterals and increased ammonia production in kidneys play a key role in increasing ammonia level in cirrhosis. Skeletal muscle plays a significant compensatory role in ammonia disposal v i a g l u t a m a t e s y n t h e s i s i n t h e mitochondria followed by its conversion to glutamine in the cytosol that is transported to the circulation in exchange for leucine that is transported into the muscle. Since the primary mechanism of skeletal muscle ammonia disposal is via ca t ap le ros i s ( lo s s o f TCA cyc le intermediates by enzymatic reactions) of α ketoglutarate (αKG), one option is to increase anaplerosis (addition of 4 and 5 carbon TCA cycle intermediates). This can
24Haryana Medical Journal - March 2020, Vol. 43, Issue 01 25Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Health Aging 2009;13:717-723.
3. Merli M, Berzigotti A, ZelberSagi S, Dasarathy S, Montagnese S, Genton L, et al. Practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70:172193
4. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014 ;15(2):95-101.
5. Collamati A, Marzetti E, Calvani R, Tosato M, D’Angelo E, Sisto AN, et al. S a r c o p e n i a i n h e a r t f a i l u r e : m e c h a n i s m s a n d t h e r a p e u t i c s t r a t e g i e s . J G e r i a t r C a r d i o l 2016;13:615-624
6. Moorthi RN, Avin KG. Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens. 2017;26(3):219-228
7. Munhoz da Rocha Lemos Costa T, Costa FM, Jonasson TH, Moreira CA, Boguszewski CL, Borba VZC. Body composition and sarcopenia in patients with chronic obstructive pulmonary disease. Endocrine. 2018 ;60(1):95-102.
8. Montano-Loza AJ, Meza-Junco J, Prado CM, Lieffers JR, Baracos VE, Bain VG, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol 2012;10:166-173,
9. Tandon P, Ney M, Irwin I, Ma MM, Gramlich L, Bain VG,et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transpl 2012;18:1209-1216.
Summary
Skeletal muscle constitutes one third of total body mass and contains up to 75% of total body proteins in a healthy person. Muscles not only helps in movement of the body but also contributes significantly in maintain body core temperature, amino acid and glucose metabolism and in disposable of ammonia in patients with cirrhosis. Common known complications of cirrhosis include ascites, hepatic e n c e p h a l o p a t h y, v a r i c e a l b l e e d , hepatorenal syndrome. Sarcopenia is now the commonest complication of cirrhosis which is defined as generalized loss of skeletal muscle mass,function and strength. Its presence may aggravate morbidity and mortality in patients with cirrhosis who are on wait list for liver transplantation. Sarcopenia also affects post liver transplant patients as it may increase hospital stay and increase the risk of infections. The evaluation of the skeletal muscle mass and function is difficult due to the lack of a uniform definition and assessment tools. A therapeutic strategy to improve sarcopenia includes dietary manipulations, increased physical activity and exercise, hormone replacement therapies , ammonia-lowering strategies and targeting the underlying liver disease.
References
1. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412-423
2. Bo i r i e Y. Phys iopa tho log i ca l mechanism of sarcopenia. J Nutr
be accomplished by adding either isoleucine or valine, which provides direct a n a p l e r o t i c i n p u t . T h e deamination/transamination of these amino acids as anaplerotic agents results i n r e l e a s e o f a m m o n i a i n a 1 : 1 stoichiometric ratio with only one net ammonia removed during the formation of glutamine (39). Treatment aimed at ammonia reduction has shown to be effective in the prevention and treatment of hepatic encephalopathy but lowering ammonia restores muscle mass in humans has not been validated.
Role of muscle in insulin resistance and n o n a l c o h o l i c f a t t y l i v e r disease(NAFLD)
NAFLD is a spectrum of disease ranging from benign steatosis (fatty liver) to non-alcoholic steatohepatitis (NASH) and is associated with insulin resistance (IR). Mechanisms relating sarcopenia to NASH include the following: insulin resistance, increased inflammation, myokines secreted by skeletal muscle, myostatin, adiponectin, vitamin D deficiency and physical inactivity. In presence of IR, the mTOR pathway remains inactive and cannot inhibit autophagy, or lysosomal degradation of proteins and organelles. These effects contribute to accelerated muscle loss in insulin resistance states(40-42).
Sarcopenia also promotes IR, as the skeletal muscle is the primary tissue responsible for insulin-mediated glucose disposal. Similarly, myosteatosis, is associated with IR. The presence of both sarcopenia and obesity acts synergistically leading to a more severe IR and dysglycemia. Thus, the cycle continues partially explaining the propagation of NASH.
for hepatic encephalopathy and increased risk of decompensation. Not surprisingly, it is associated with a 5-fold increased risk of mortality, independent of MELD-Na score.
Post liver transplantation most of the complications related to liver cirrhrosis and portal hypertension generally improved (or even reversed) however the course of sarcopenia following LT is variable with either improvement, remaining unchanged or continuing to decline. The underlying pathogenesis and mediators of post LT sarcopenia are unclear. Several immunosuppressive agents, especially corticosteroids and mTOR inhibitors, have negative impact on skeletal muscle and appear to be the key drivers of postLT sarcopenia(35-38)
Role of muscle in decreasing ammonia in cirrhosis
Ammonia plays a major role in the pathogenesis of sarcopenia and minimal/ overt HE in cirrhosis(17). Functional hepa tocy t e s l o s s , po r to sys t emic collaterals and increased ammonia production in kidneys play a key role in increasing ammonia level in cirrhosis. Skeletal muscle plays a significant compensatory role in ammonia disposal v i a g l u t a m a t e s y n t h e s i s i n t h e mitochondria followed by its conversion to glutamine in the cytosol that is transported to the circulation in exchange for leucine that is transported into the muscle. Since the primary mechanism of skeletal muscle ammonia disposal is via ca t ap le ros i s ( lo s s o f TCA cyc le intermediates by enzymatic reactions) of α ketoglutarate (αKG), one option is to increase anaplerosis (addition of 4 and 5 carbon TCA cycle intermediates). This can
26Haryana Medical Journal - March 2020, Vol. 43, Issue 01 27Haryana Medical Journal - March 2020, Vol. 43, Issue 01
myostatin by an NF-kappaB-mediated mechanism. Proc Natl Acad Sci U S A 2013;110:18162–18167.
31. Van Vugt JL, Levolger S, de Bruin RW, van Rosmalen J, Metselaar HJ, IJzermans JN. Systematic review and meta-analysis of the impact of computed tomography-assessed skeletal muscle mass on outcome in patients awaiting or undergoing liver transplantation. Am J Transplant 2016;16:2277–2292.
32. Wu LW, Lin YY, Kao TW, Lin CM, Liaw FY, Wang CC, et al. Mid-arm muscle circumference as a significant predictor of all-cause mortality in male individuals. PLoS One 2017;12 e0171707.
33. Giusto M, Lattanzi B, Albanese C, Galtieri A, Farcomeni A, Giannelli V, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy Xray absorptiometry and anthropometry. E u r J G a s t r o e n t e r o l H e p a t o l 2015;27:328–334.
34. DiMartini A, Cruz RJ Jr, Dew MA, Myaskovsky L, Goodpaster B, Fox K,et al . Muscle mass predicts o u t c o m e s f o l l o w i n g l i v e r transplantation. Liver Transpl. 2013;19(11):1172-80
35. Englesbe MJ, Patel SP, He K, Lynch RJ, Schaubel DE, Harbaugh C, et al.Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211(2):271-8
36. Pravisani R, Soyama A, Isola M, Sadykov N, Takatsuki M, Hidaka M et al. Chronological changes in skeletal muscle mass following living donor
Liver Disease. Clin Liver Dis. 2016 Aug;20(3):535-50
24. Dasara thy J , McCul lough AJ , Dasarathy S. Sarcopenia in alcoholic liver disease: clinical and molecular advances. Alcohol Clin Exp Res 2017;41:1419–1431.
25. Sinclair M, GrossmannM, Hoermann R, Angus PW, Gow PJ. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: a randomised controlled trial. J Hepatol 2016;65:906–913.
26. Zenith L, Meena N, Ramadi A, Yavari M, Harvey A, Carbonneau M, et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol 2014;12:e1922.
27. Nishikawa H, Enomoto H, Ishii A, Iwata Y, Miyamoto Y, Ishii N, et al. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J C a c h e x i a S a r c o p e n i a M u s c l e 2017;8:915–925.
28. Chen HW, Dunn MA. Muscle at risk: the multiple impacts of ammonia on sarcopenia and frailty in cirrhosis. Clin Transl Gastroenterol 2016;7:
29. HolecekM. Branched-chain amino acid supplementation in treatment of liver cirrhosis: Updated views on how to attenuate their harmful effects on cataplerosis and ammonia formation. Nutrition 2017;41:80–85.
30. Qiu J, Thapaliya S, Runkana A, Yang Y, Tsien C, Mohan ML, et al. Hyperammonemia in cirrhosis induces transcriptional regulation of
hepatic encephalopathy: results of a prospective study. Metab Brain Dis 2013;28:281–284
18. Giusto M, Lattanzi B, Albanese C, Galtieri A, Farcomeni A, Giannelli V, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy Xray absorptiometry and anthropometry. E u r J G a s t r o e n t e r o l H e p a t o l 2015;27:328–334.
19. Alvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition 2005;21:113–117
20. Tandon P, Raman M, Mourtzakis M, Merli M. A practical approach to nutritional screening and assessment i n c i r r h o s i s . H e p a t o l o g y 2017;65:1044–1057
21. Montano Loza AJ, Angulo P, MezaJunco J, et al. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J Cachex ia Sarcopen ia Musc le . 2016;7:126135
22. Tai ML, Goh KL, Mohd Taib SH, R a m p a l S , M a h a d e v a S . Anthropometric, biochemical and clinical assessment of malnutrition in Malaysian patients with advanced cirrhosis. Nutr J. 2010;9:27
23. Dasarathy S Nutrition and Alcoholic Liver Disease: Effects of Alcoholism on Nutrition, Effects of Nutrition on Alcohol ic Liver Disease , and Nutritional Therapies for Alcoholic
10. Borhofen SM, Gerner C, Lehmann J, Fimmers R, Gortzen J, Hey B, et al. The royal free hospital-nutritional prioritizing tool is an independent predictor of deterioration of liver function and survival in cirrhosis. Dig Dis Sci 2016;61:1735–1743.
11. Haykowsky MJ, Brubaker PH, M o rg a n T M , K r i t c h e v s k y S , Eggebeen J, Kitzman DW. Impaired aerobic capaci ty and physical functional performance in older heart failure patients with preserved ejection fraction: role of lean body mass. J Gerontol A Biol Sci Med Sci 2013;68:968-975
12. Elliott JE, Greising SM, Mantilla CB, Sieck GC. Functional impact of sarcopenia in respiratory muscles. R e s p i r P h y s i o l N e u r o b i o l 2016;226:137-146
13. Frontera, W.R Ochala, J. Skeletal muscle: a brief review of structure and function. Calcif. Tissue Int.2015; 96, 183–195
14. Iizuka K, Machida T, Hirafuji M. Skeletal muscle is an endocrine organ. J Pharmacol Sci 2014;125:125-131
15. Schiaffino S, Reggiani C. Fiber types in mammalian skeletal muscles. Physiol Rev 2011;91:1447-1531
16. Carey EJ , Lai JC, Wang CW, Dasarathy S, Lobach I, Montano-Loza AJ,et al. A multicenter study to define sarcopenia in patients with endstage liver disease. Liver Transplant. 2017;23:625633
17. Merli M, Giusto M, Lucidi C, Giannelli V, Pentassuglio I, Di Gregorio V, et al. Muscle depletion increases the risk of overt and minimal
26Haryana Medical Journal - March 2020, Vol. 43, Issue 01 27Haryana Medical Journal - March 2020, Vol. 43, Issue 01
myostatin by an NF-kappaB-mediated mechanism. Proc Natl Acad Sci U S A 2013;110:18162–18167.
31. Van Vugt JL, Levolger S, de Bruin RW, van Rosmalen J, Metselaar HJ, IJzermans JN. Systematic review and meta-analysis of the impact of computed tomography-assessed skeletal muscle mass on outcome in patients awaiting or undergoing liver transplantation. Am J Transplant 2016;16:2277–2292.
32. Wu LW, Lin YY, Kao TW, Lin CM, Liaw FY, Wang CC, et al. Mid-arm muscle circumference as a significant predictor of all-cause mortality in male individuals. PLoS One 2017;12 e0171707.
33. Giusto M, Lattanzi B, Albanese C, Galtieri A, Farcomeni A, Giannelli V, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy Xray absorptiometry and anthropometry. E u r J G a s t r o e n t e r o l H e p a t o l 2015;27:328–334.
34. DiMartini A, Cruz RJ Jr, Dew MA, Myaskovsky L, Goodpaster B, Fox K,et al . Muscle mass predicts o u t c o m e s f o l l o w i n g l i v e r transplantation. Liver Transpl. 2013;19(11):1172-80
35. Englesbe MJ, Patel SP, He K, Lynch RJ, Schaubel DE, Harbaugh C, et al.Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211(2):271-8
36. Pravisani R, Soyama A, Isola M, Sadykov N, Takatsuki M, Hidaka M et al. Chronological changes in skeletal muscle mass following living donor
Liver Disease. Clin Liver Dis. 2016 Aug;20(3):535-50
24. Dasara thy J , McCul lough AJ , Dasarathy S. Sarcopenia in alcoholic liver disease: clinical and molecular advances. Alcohol Clin Exp Res 2017;41:1419–1431.
25. Sinclair M, GrossmannM, Hoermann R, Angus PW, Gow PJ. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: a randomised controlled trial. J Hepatol 2016;65:906–913.
26. Zenith L, Meena N, Ramadi A, Yavari M, Harvey A, Carbonneau M, et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol 2014;12:e1922.
27. Nishikawa H, Enomoto H, Ishii A, Iwata Y, Miyamoto Y, Ishii N, et al. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J C a c h e x i a S a r c o p e n i a M u s c l e 2017;8:915–925.
28. Chen HW, Dunn MA. Muscle at risk: the multiple impacts of ammonia on sarcopenia and frailty in cirrhosis. Clin Transl Gastroenterol 2016;7:
29. HolecekM. Branched-chain amino acid supplementation in treatment of liver cirrhosis: Updated views on how to attenuate their harmful effects on cataplerosis and ammonia formation. Nutrition 2017;41:80–85.
30. Qiu J, Thapaliya S, Runkana A, Yang Y, Tsien C, Mohan ML, et al. Hyperammonemia in cirrhosis induces transcriptional regulation of
hepatic encephalopathy: results of a prospective study. Metab Brain Dis 2013;28:281–284
18. Giusto M, Lattanzi B, Albanese C, Galtieri A, Farcomeni A, Giannelli V, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy Xray absorptiometry and anthropometry. E u r J G a s t r o e n t e r o l H e p a t o l 2015;27:328–334.
19. Alvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition 2005;21:113–117
20. Tandon P, Raman M, Mourtzakis M, Merli M. A practical approach to nutritional screening and assessment i n c i r r h o s i s . H e p a t o l o g y 2017;65:1044–1057
21. Montano Loza AJ, Angulo P, MezaJunco J, et al. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J Cachex ia Sarcopen ia Musc le . 2016;7:126135
22. Tai ML, Goh KL, Mohd Taib SH, R a m p a l S , M a h a d e v a S . Anthropometric, biochemical and clinical assessment of malnutrition in Malaysian patients with advanced cirrhosis. Nutr J. 2010;9:27
23. Dasarathy S Nutrition and Alcoholic Liver Disease: Effects of Alcoholism on Nutrition, Effects of Nutrition on Alcohol ic Liver Disease , and Nutritional Therapies for Alcoholic
10. Borhofen SM, Gerner C, Lehmann J, Fimmers R, Gortzen J, Hey B, et al. The royal free hospital-nutritional prioritizing tool is an independent predictor of deterioration of liver function and survival in cirrhosis. Dig Dis Sci 2016;61:1735–1743.
11. Haykowsky MJ, Brubaker PH, M o rg a n T M , K r i t c h e v s k y S , Eggebeen J, Kitzman DW. Impaired aerobic capaci ty and physical functional performance in older heart failure patients with preserved ejection fraction: role of lean body mass. J Gerontol A Biol Sci Med Sci 2013;68:968-975
12. Elliott JE, Greising SM, Mantilla CB, Sieck GC. Functional impact of sarcopenia in respiratory muscles. R e s p i r P h y s i o l N e u r o b i o l 2016;226:137-146
13. Frontera, W.R Ochala, J. Skeletal muscle: a brief review of structure and function. Calcif. Tissue Int.2015; 96, 183–195
14. Iizuka K, Machida T, Hirafuji M. Skeletal muscle is an endocrine organ. J Pharmacol Sci 2014;125:125-131
15. Schiaffino S, Reggiani C. Fiber types in mammalian skeletal muscles. Physiol Rev 2011;91:1447-1531
16. Carey EJ , Lai JC, Wang CW, Dasarathy S, Lobach I, Montano-Loza AJ,et al. A multicenter study to define sarcopenia in patients with endstage liver disease. Liver Transplant. 2017;23:625633
17. Merli M, Giusto M, Lucidi C, Giannelli V, Pentassuglio I, Di Gregorio V, et al. Muscle depletion increases the risk of overt and minimal
PRIMARY INTRACRANIAL DURAL-BASED EWING SARCOMA/PERIPHERAL PRIMITIVE NEUROECTODERMAL TUMOR MIMICKING
A MENINGIOMA: A CASE REPORT
1 2 3Dr Mohan Lal , Dr Vijay Kumar Gupta , Dr Shveta Bansal
Abstract
Ewing sarcoma/peripheral primitive neuroectodermal tumor (ES/pPNET) is a malignant small, round cell tumor arising from bone and soft tissue in children and young adults. It can occur at osseous and extraosseous sites. Its usual locations are diaphysis of long bones followed by pelvis, ribs, vertebrae, and rarely skull. We reviewed the literature and PubMed advanced search on ES/pPNET occurring at extraosseous sites, mainly involving the central nervous system (CNS). We reported a case of a 22-year-old male presenting with seizure finally diagnosed as a case of ES/pPNET. The challenges in management of this rare CNS tumor and its differential diagnosis are highlighted. We found that most cases of ES involving CNS represent secondary metastases from extracranial sites of ES/pPNET and there are rare case reports of primary intracranial ES-pPNET. Furthermore, among these intracranial tumors, most common tumors occupy an intraaxial location and only a handful of cases of dural-based or extraaxial tumors mimicking meningioma are reported. Differentiation of pPNET from central PNET (cPNET) is important as it has definitive therapeutic and prognostic implications. Awareness of this entity of ES/pPNET, its rare dural presentation, and
differentiation from the more common cPNET is needed for appropriate patient management. Meningeal ES/pPNET has to be kept in mind in the differential diagnosis of meningeal tumors eroding bone.
Keywords: Central nervous system Ewing s a r c o m a / p e r i p h e r a l p r i m i t i v e neuroectodermal tumor, dural tumor, Ewing’s sarcoma, intracranial primitive neuroectodermal tumor, meningioma, peripheral primitive neuroectodermal tumor, primary
Introduction
Ewing sarcoma/peripheral primitive neuroectodermal tumor (ES/pPNET) is a malignant small, round cell tumor arising from bone and soft tissue in children and young adults. It can occur at osseous and extraosseous sites. Its usual locations are diaphysis of long bones followed by pelvis, r ibs , ver tebrae , and rare ly skul l . Intracranial ES/pPNET is usual ly metastases from extracranial sites of ES/pPNET. When primary ES/pPNET affects central nervous system (CNS), w h i c h i s r a r e , i t i s u s u a l l y i n t r a p a r e n c h y m a l l o c a t e d supratentorially or in the spinal cord. An extra axial/dural presentation of ES/pPNET mimicking meningioma is extremely rare. These tumors pose a diagnostic challenge to neurosurgeons.
is an independent risk factor for non-a l coho l i c s t ea tohepa t i t i s and s ignificant fibrosis . J Hepatol 2017;66:123-131.
41. Zhang HJ, Zhang XF, Ma ZM, Pan LL, Chen Z, Han HW, et al. Irisin is inversely associated with intrahepatic triglyceride contents in obese adults. J Hepatol 2013;59:557-562.
42. Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is a s s o c i a t e d w i t h N A F L D independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008-2011). J Hepatol 2015;63:486-493
liver transplantation: An analysis of the predictive factors for long term post transplant low muscularity. Clin Transplant. 2019;33:e13495.
37. Bhanji RA, Takahashi N, Moynagh MR, Narayanan P, Angirekula M, Mara KC et al. The evolution and impact of sarcopenia pre and postl i v e r t r a n s p l a n t a t i o n . A l i m e n t m P h a r m a c o l T h e r . 2019;49:807813.
38. Kaido T, Tamai Y, Hamaguchi Y, Okumura S, Kobayashi A, Shirai H et al. Effects of pretransplant sarcopenia and sequential changes in sarcopenic parameters after living donor liver t r a n s p l a n t a t i o n . N u t r i t i o n . 2017;33:195198
39. Jindal A, Jagdish RK. Sarcopenia: Ammonia metabolism and hepatic encephalopathy. Clin Mol Hepatol. 2019 Sep;25(3):270-279
40. Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia
Address of CorrespondenceDr Anil Arora
ProfessorDepartment of Gastroenterology
Sir Ganga Ram Hospital, New DelhiEmail:[email protected]
28Haryana Medical Journal - March 2020, Vol. 43, Issue 01 29Haryana Medical Journal - March 2020, Vol. 43, Issue 01
PRIMARY INTRACRANIAL DURAL-BASED EWING SARCOMA/PERIPHERAL PRIMITIVE NEUROECTODERMAL TUMOR MIMICKING
A MENINGIOMA: A CASE REPORT
1 2 3Dr Mohan Lal , Dr Vijay Kumar Gupta , Dr Shveta Bansal
Abstract
Ewing sarcoma/peripheral primitive neuroectodermal tumor (ES/pPNET) is a malignant small, round cell tumor arising from bone and soft tissue in children and young adults. It can occur at osseous and extraosseous sites. Its usual locations are diaphysis of long bones followed by pelvis, ribs, vertebrae, and rarely skull. We reviewed the literature and PubMed advanced search on ES/pPNET occurring at extraosseous sites, mainly involving the central nervous system (CNS). We reported a case of a 22-year-old male presenting with seizure finally diagnosed as a case of ES/pPNET. The challenges in management of this rare CNS tumor and its differential diagnosis are highlighted. We found that most cases of ES involving CNS represent secondary metastases from extracranial sites of ES/pPNET and there are rare case reports of primary intracranial ES-pPNET. Furthermore, among these intracranial tumors, most common tumors occupy an intraaxial location and only a handful of cases of dural-based or extraaxial tumors mimicking meningioma are reported. Differentiation of pPNET from central PNET (cPNET) is important as it has definitive therapeutic and prognostic implications. Awareness of this entity of ES/pPNET, its rare dural presentation, and
differentiation from the more common cPNET is needed for appropriate patient management. Meningeal ES/pPNET has to be kept in mind in the differential diagnosis of meningeal tumors eroding bone.
Keywords: Central nervous system Ewing s a r c o m a / p e r i p h e r a l p r i m i t i v e neuroectodermal tumor, dural tumor, Ewing’s sarcoma, intracranial primitive neuroectodermal tumor, meningioma, peripheral primitive neuroectodermal tumor, primary
Introduction
Ewing sarcoma/peripheral primitive neuroectodermal tumor (ES/pPNET) is a malignant small, round cell tumor arising from bone and soft tissue in children and young adults. It can occur at osseous and extraosseous sites. Its usual locations are diaphysis of long bones followed by pelvis, r ibs , ver tebrae , and rare ly skul l . Intracranial ES/pPNET is usual ly metastases from extracranial sites of ES/pPNET. When primary ES/pPNET affects central nervous system (CNS), w h i c h i s r a r e , i t i s u s u a l l y i n t r a p a r e n c h y m a l l o c a t e d supratentorially or in the spinal cord. An extra axial/dural presentation of ES/pPNET mimicking meningioma is extremely rare. These tumors pose a diagnostic challenge to neurosurgeons.
is an independent risk factor for non-a l coho l i c s t ea tohepa t i t i s and s ignificant fibrosis . J Hepatol 2017;66:123-131.
41. Zhang HJ, Zhang XF, Ma ZM, Pan LL, Chen Z, Han HW, et al. Irisin is inversely associated with intrahepatic triglyceride contents in obese adults. J Hepatol 2013;59:557-562.
42. Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is a s s o c i a t e d w i t h N A F L D independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008-2011). J Hepatol 2015;63:486-493
liver transplantation: An analysis of the predictive factors for long term post transplant low muscularity. Clin Transplant. 2019;33:e13495.
37. Bhanji RA, Takahashi N, Moynagh MR, Narayanan P, Angirekula M, Mara KC et al. The evolution and impact of sarcopenia pre and postl i v e r t r a n s p l a n t a t i o n . A l i m e n t m P h a r m a c o l T h e r . 2019;49:807813.
38. Kaido T, Tamai Y, Hamaguchi Y, Okumura S, Kobayashi A, Shirai H et al. Effects of pretransplant sarcopenia and sequential changes in sarcopenic parameters after living donor liver t r a n s p l a n t a t i o n . N u t r i t i o n . 2017;33:195198
39. Jindal A, Jagdish RK. Sarcopenia: Ammonia metabolism and hepatic encephalopathy. Clin Mol Hepatol. 2019 Sep;25(3):270-279
40. Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia
Address of CorrespondenceDr Anil Arora
ProfessorDepartment of Gastroenterology
Sir Ganga Ram Hospital, New DelhiEmail:[email protected]
28Haryana Medical Journal - March 2020, Vol. 43, Issue 01 29Haryana Medical Journal - March 2020, Vol. 43, Issue 01
these, only one case was reported as ES. A recent study by Krishnamani . showed et althat of 332 cases of ES diagnosed over an 11 years period, seven cases were of primary ES skull. These tumors clinically present with signs of increased intracranial pressure, headache, vomiting, or with s e i z u r e s a n d d i s t u r b a n c e s o f c o n s c i o u s n e s s . M o t o r d e fi c i t o r uncommonly visual disturbances and endocrine abnormalities can occur depending on location. Ever since the first description of this tumor by Ewing as “diffuse endothelioma” controversy has persisted about the histogenesis of ES. The present case is discussed to clarify and stress upon two different aspects: First, the confusing terminology of ES, pPNEt, and cPNET and second is the unusual p r e s e n t a t i o n o f t h i s t u m o r a s a meningioma. ES and PNET are defined as round cell sarcomas showing varying d e g r e e s o f n e u r o e c t o d e r m a l differentiation. The term “ES” is used for t u m o r s w i t h a b s e n t o r l i m i t e d neuroectodermal differentiation whereas “PNET” i s employed for tumors demonstrating definite neuroectodermal features. “ES/pPNET” best describes this overlapping entity. The cPNET is defined as an embryonal tumor composed of undifferentiated or poorly differentiated neuroepithelial cells displaying divergent differentiation along neuronal, astrocytic, muscular, or melanocytic lines occurring within any region of the CNS other than cerebellum. This group includes CNS-PNET not otherwise specified (NOS), neuroblastoma, ganglioneuroblastoma, medulloepithelioma, ependymoblastoma, and embryonal tumor with abundant neutrophils and true rosette.
Discussion
Primary intracranial ES/pPNET is a recently recognized entity of CNS PNET. There are < 15 case reports of this entity in the literature. A study conducted by Paulus et al. showed that out of total 2500 cases of brain tumors, only 9 were sarcomas. Of
Figure 2 Photomicrograph showing a richly vascular small round cell tumor adjacent the dura (H and E, ×100)
Figure 3 Photomicrograph showing tumor composed of sheets of uniform small round cells with scant cytoplasm an area of necrosis and several mitotic figures (H and E, ×200)
30Haryana Medical Journal - March 2020, Vol. 43, Issue 01 31Haryana Medical Journal - March 2020, Vol. 43, Issue 01
right quadrigeminal cistern along with extension & mass effect [Figure 1]. Features suggested poss ibi l i ty of meningioma. Planned craniotomy was done. Intraoperatively, the tumor was seen as a soft reddish highly vascularized mass not eroding the overlying bone. Partial resection of the tumor with the attached dura was done. Histopathological examination of the attached soft tissue pieces showed a richly vascular tumor with small round cells arranged in lobules, sheets, and cords [Figure 2]. The tumor was composed of monotonous small, round to oval cells with regular nuclear outline, vesicular chromatin, and scant amount of clear to pale eosinophilic cytoplasm [Figure 3] Cytoplasmic vacuolation was also noted. Some tumor cells were larger with prominent nucleoli and irregular nuclear contour. Homer wright rosettes were not seen.. Necrosis was seen in few areas. There was involvement of dura. Tu m o r d i d n o t i n v a d e t h e b r a i n parenchyma. I t was diagnosed as ES/pPNET. Postoperatively, patient was observed in surgical intensive unit. Extensive workup was done including CT scans of the thorax, abdomen, and pelvis . Final diagnosis was primary ES/pPNET of dura. Patient is under routine follow-up .
Intraparenchymal cerebral tumors may be misdiagnosed as central PNET (cPNET) or other primary CNS tumors and the dural tumors very closely mimic meningioma, clinically and radiologically. An early and accurate diagnosis of ES/pPNET is required so that multimodality treatment approach can be adopted as early as possible to prevent distant metastases which occurs quite early in this tumor. As the tumor presents in young age, long-term s u r v i v a l r e m a i n s a c h a l l e n g e i n management of ES/pPNET patients. We report a case of intracranial ES/pPNET presenting as meningioma in a 25-year-old male with complains of headache & vomiting.
Case Report
A 25-year-old male presented with complains of headache & vomiting. On examination, Glasgow coma score was E4 V5 M6. Papilledema was present on left side. Patient had no previous history of unconsciousness, and focal neurological deficit. There was no significant drug history or family history. Contrast-enhanced MRI showed multiple intense enhancing extra axial mass lesion involving left sphenoid wing , left cp angle , infra cerebellar region & along
Figure 1 Axial CEMRI showing a relatively well-defined dural-based tumor showing contrast enhancement
these, only one case was reported as ES. A recent study by Krishnamani . showed et althat of 332 cases of ES diagnosed over an 11 years period, seven cases were of primary ES skull. These tumors clinically present with signs of increased intracranial pressure, headache, vomiting, or with s e i z u r e s a n d d i s t u r b a n c e s o f c o n s c i o u s n e s s . M o t o r d e fi c i t o r uncommonly visual disturbances and endocrine abnormalities can occur depending on location. Ever since the first description of this tumor by Ewing as “diffuse endothelioma” controversy has persisted about the histogenesis of ES. The present case is discussed to clarify and stress upon two different aspects: First, the confusing terminology of ES, pPNEt, and cPNET and second is the unusual p r e s e n t a t i o n o f t h i s t u m o r a s a meningioma. ES and PNET are defined as round cell sarcomas showing varying d e g r e e s o f n e u r o e c t o d e r m a l differentiation. The term “ES” is used for t u m o r s w i t h a b s e n t o r l i m i t e d neuroectodermal differentiation whereas “PNET” i s employed for tumors demonstrating definite neuroectodermal features. “ES/pPNET” best describes this overlapping entity. The cPNET is defined as an embryonal tumor composed of undifferentiated or poorly differentiated neuroepithelial cells displaying divergent differentiation along neuronal, astrocytic, muscular, or melanocytic lines occurring within any region of the CNS other than cerebellum. This group includes CNS-PNET not otherwise specified (NOS), neuroblastoma, ganglioneuroblastoma, medulloepithelioma, ependymoblastoma, and embryonal tumor with abundant neutrophils and true rosette.
Discussion
Primary intracranial ES/pPNET is a recently recognized entity of CNS PNET. There are < 15 case reports of this entity in the literature. A study conducted by Paulus et al. showed that out of total 2500 cases of brain tumors, only 9 were sarcomas. Of
Figure 2 Photomicrograph showing a richly vascular small round cell tumor adjacent the dura (H and E, ×100)
Figure 3 Photomicrograph showing tumor composed of sheets of uniform small round cells with scant cytoplasm an area of necrosis and several mitotic figures (H and E, ×200)
30Haryana Medical Journal - March 2020, Vol. 43, Issue 01 31Haryana Medical Journal - March 2020, Vol. 43, Issue 01
right quadrigeminal cistern along with extension & mass effect [Figure 1]. Features suggested poss ibi l i ty of meningioma. Planned craniotomy was done. Intraoperatively, the tumor was seen as a soft reddish highly vascularized mass not eroding the overlying bone. Partial resection of the tumor with the attached dura was done. Histopathological examination of the attached soft tissue pieces showed a richly vascular tumor with small round cells arranged in lobules, sheets, and cords [Figure 2]. The tumor was composed of monotonous small, round to oval cells with regular nuclear outline, vesicular chromatin, and scant amount of clear to pale eosinophilic cytoplasm [Figure 3] Cytoplasmic vacuolation was also noted. Some tumor cells were larger with prominent nucleoli and irregular nuclear contour. Homer wright rosettes were not seen.. Necrosis was seen in few areas. There was involvement of dura. Tu m o r d i d n o t i n v a d e t h e b r a i n parenchyma. I t was diagnosed as ES/pPNET. Postoperatively, patient was observed in surgical intensive unit. Extensive workup was done including CT scans of the thorax, abdomen, and pelvis . Final diagnosis was primary ES/pPNET of dura. Patient is under routine follow-up .
Intraparenchymal cerebral tumors may be misdiagnosed as central PNET (cPNET) or other primary CNS tumors and the dural tumors very closely mimic meningioma, clinically and radiologically. An early and accurate diagnosis of ES/pPNET is required so that multimodality treatment approach can be adopted as early as possible to prevent distant metastases which occurs quite early in this tumor. As the tumor presents in young age, long-term s u r v i v a l r e m a i n s a c h a l l e n g e i n management of ES/pPNET patients. We report a case of intracranial ES/pPNET presenting as meningioma in a 25-year-old male with complains of headache & vomiting.
Case Report
A 25-year-old male presented with complains of headache & vomiting. On examination, Glasgow coma score was E4 V5 M6. Papilledema was present on left side. Patient had no previous history of unconsciousness, and focal neurological deficit. There was no significant drug history or family history. Contrast-enhanced MRI showed multiple intense enhancing extra axial mass lesion involving left sphenoid wing , left cp angle , infra cerebellar region & along
Figure 1 Axial CEMRI showing a relatively well-defined dural-based tumor showing contrast enhancement
TRIGEMINAL NEURALGIA: A REVIEW OF CLINICAL LITERATURE
Dr Utkarsh , Dr JS Tiwana
Abstract
The trigeminal nerve, fifth cranial nerve is a mixed nerve having motor and sensory components. The sensory portion supplies to face skin and mucous membrane and it is responsible Trigeminal Neuralgia. The aim of this study is to review the literature on the characteristics of Trigeminal Neuralgia, the relevant aspects for the diagnosis and treatment options. Neuralgia is characterized by sudden electric shock like pain with a duration of a few seconds to few minutes in nerve distribution. The pain is triggered by touches in few points in the face or with/after movements of the facial muscles. This Frequently seen in elderly woman. Commonly it has unilateral presentation with pain attacks more in the maxillary and mandibular divisions area. Rarely it is seen affecting all three branches of trigeminal nerve.
Keywords: trigeminal neuralga, anatomy, pain, t ic douloureux, psychiatry, neurology, mvd, radiofrequency
Introduction
Tr igemina l neura lg ia (TN) i s characterized by paroxysmal excruciating and sudden, like a shock pain lasting for a few seconds to few minutes. Commonly seen pain in oro-facial area. (TODA, 2007).1
Neuralgia frequently is seen in the second and third divisions of the
trigeminal nerve. The attacks may be associated with salivation, lacrimation, rhinorrhea, nasal mucosa congestion, skin redness, facial swelling, or clonic contraction, ipsilateral hemifacial spasm and/or contraction of the muscles acting on the jaw. It is also characterized by regions of increased sensitivity, called trigger zones. In general, it affects more elderly women in sixth and eighth decade o f l i f e . ( G O T O , I S H I Z A K I , YOSHIKAWA et al., 1999).2
General practitioner are often the first clinician to encounter patients with excruciating pain of trigeminal neuralgia.
Classification
International headache society defined strict clinical criteria for TN diagnosis (Eller JL et al)3. According to this TN is diagnosed if 3 attacks of unilateral facial pain occurs characterized by 1) occurring in one or more divisions of the trigeminal nerve, with no radiation beyond the trigeminal distribution and 2) pain with at least three of the fol lowing four characteristics: a) recurring in paroxysmal attacks lasting from a fraction of a second to 2 minutes; b) severe intensity; c) electric shocklike, shooting, stabbing, or sharp in quality; and d) precipitated by innocuous stimuli to the affected side of the face. Important criteria for clinical diagnosis are also the lack of evident neurologic deficit and a pain that cannot be attributed to another disorder.
32Haryana Medical Journal - March 2020, Vol. 43, Issue 01 33Haryana Medical Journal - March 2020, Vol. 43, Issue 01
rare tumors in the differential diagnosis of common tumors like meningioma. Awareness of this entity of ES/pPNET, its rare dural presentation, and differentiation from the more common cPNET is needed for appropriate patient management. Meningeal ES/pPNET has to be kept in mind in the differential diagnosis of meningeal tumors eroding bone.
Conflicts of interest
There are no conflicts of interest.
Address of CorrespondenceDr Mohan Lal
Consultant Radiologist,
V.K Neurocare Hospital Hisar
Both cPNETs and pPNETs are aggressive tumors, but they differ in their cell of origin. The cPNETs arise from a precursor cell of the subependymal matrix of the CNS or external granular layer of the c e r e b e l l u m , p i n e a l o c y t e s , a n d subependymal cells of the ventricles whereas pPNETs derive from the neural crest located outside the CNS. Cases of pPNET in meninges of cranial vault and epidural space of the spinal canal have been reported. It is clinically important to differentiate the two as their clinical presentation, treatment, and prognosis differ variably.
Conclusion
This case comes as a reminder to neurosurgeons as well as radiologists and pathologists for careful consideration of
TRIGEMINAL NEURALGIA: A REVIEW OF CLINICAL LITERATURE
Dr Utkarsh , Dr JS Tiwana
Abstract
The trigeminal nerve, fifth cranial nerve is a mixed nerve having motor and sensory components. The sensory portion supplies to face skin and mucous membrane and it is responsible Trigeminal Neuralgia. The aim of this study is to review the literature on the characteristics of Trigeminal Neuralgia, the relevant aspects for the diagnosis and treatment options. Neuralgia is characterized by sudden electric shock like pain with a duration of a few seconds to few minutes in nerve distribution. The pain is triggered by touches in few points in the face or with/after movements of the facial muscles. This Frequently seen in elderly woman. Commonly it has unilateral presentation with pain attacks more in the maxillary and mandibular divisions area. Rarely it is seen affecting all three branches of trigeminal nerve.
Keywords: trigeminal neuralga, anatomy, pain, t ic douloureux, psychiatry, neurology, mvd, radiofrequency
Introduction
Tr igemina l neura lg ia (TN) i s characterized by paroxysmal excruciating and sudden, like a shock pain lasting for a few seconds to few minutes. Commonly seen pain in oro-facial area. (TODA, 2007).1
Neuralgia frequently is seen in the second and third divisions of the
trigeminal nerve. The attacks may be associated with salivation, lacrimation, rhinorrhea, nasal mucosa congestion, skin redness, facial swelling, or clonic contraction, ipsilateral hemifacial spasm and/or contraction of the muscles acting on the jaw. It is also characterized by regions of increased sensitivity, called trigger zones. In general, it affects more elderly women in sixth and eighth decade o f l i f e . ( G O T O , I S H I Z A K I , YOSHIKAWA et al., 1999).2
General practitioner are often the first clinician to encounter patients with excruciating pain of trigeminal neuralgia.
Classification
International headache society defined strict clinical criteria for TN diagnosis (Eller JL et al)3. According to this TN is diagnosed if 3 attacks of unilateral facial pain occurs characterized by 1) occurring in one or more divisions of the trigeminal nerve, with no radiation beyond the trigeminal distribution and 2) pain with at least three of the fol lowing four characteristics: a) recurring in paroxysmal attacks lasting from a fraction of a second to 2 minutes; b) severe intensity; c) electric shocklike, shooting, stabbing, or sharp in quality; and d) precipitated by innocuous stimuli to the affected side of the face. Important criteria for clinical diagnosis are also the lack of evident neurologic deficit and a pain that cannot be attributed to another disorder.
32Haryana Medical Journal - March 2020, Vol. 43, Issue 01 33Haryana Medical Journal - March 2020, Vol. 43, Issue 01
rare tumors in the differential diagnosis of common tumors like meningioma. Awareness of this entity of ES/pPNET, its rare dural presentation, and differentiation from the more common cPNET is needed for appropriate patient management. Meningeal ES/pPNET has to be kept in mind in the differential diagnosis of meningeal tumors eroding bone.
Conflicts of interest
There are no conflicts of interest.
Address of CorrespondenceDr Mohan Lal
Consultant Radiologist,
V.K Neurocare Hospital Hisar
Both cPNETs and pPNETs are aggressive tumors, but they differ in their cell of origin. The cPNETs arise from a precursor cell of the subependymal matrix of the CNS or external granular layer of the c e r e b e l l u m , p i n e a l o c y t e s , a n d subependymal cells of the ventricles whereas pPNETs derive from the neural crest located outside the CNS. Cases of pPNET in meninges of cranial vault and epidural space of the spinal canal have been reported. It is clinically important to differentiate the two as their clinical presentation, treatment, and prognosis differ variably.
Conclusion
This case comes as a reminder to neurosurgeons as well as radiologists and pathologists for careful consideration of
characteristics:
1. Lasting from a fraction of a second to two minutes
2. Severe intensity
3. Electric shock-like, shooting, stabbing or sharp in quality
B. Precipitated by innocuous stimuli within the affected trigeminal distribution
C. Not better accounted for by another ICHD-3 diagnosis
Differential Diagnosis—Clinically, the TN can be confused with disorders related to teeth, facial bones and paranasal sinuses, leading to a variety of therapeutic incorrect. Disease severity is underscored by having one of the highest suicide rates in relation to any disease, and is considered one of the most painful diseases known (NEVILLE, DAMM, ALLEN et al., 2004). 10
from the primary headaches of short duration
Krafft (2008) affirmed that the diagnosis is essentially clinical, but may need some evaluations of image or specialized tests in patients who have unusual characteristcs such as bilateral symptoms, dizziness or vertigo, age less than 40 years, hearing loss or disorder, episodes of pain with longer than two minutes, visual disturbances and pain that is not in the trigeminal distribution.
The diagnosis of TN is important to perform the analgesic block (at least at the beginning of neuralgia), rapidly stopping the pain and triggering due to the occurrence of these in the area of the affected nerve. The neurogenic pain in the orofacial region may be mistaken for masticatory pain. Therefore, we must consider the characteristics of each one.
ICHD-3 diagnost ic cr i ter ia for trigeminal neuralgia
ICHD-3: International Classification of Headache Disorders
ICHD-3 Diagnostic Criteria for Trigeminal Neuralgia
A. Pain has al l of the fol lowing
ICHD-3: International Classification of Headache Disorders
ICHD-3 Diagnostic Criteria for Trigeminal Neuralgia
A. Pain has all of the following characteristics:
1. Lasting from a fraction of a second to two minutes
2. Severe intensity
3. Electric shock-like, shooting, stabbing or sharp in quality
B. Precipitated by innocuous stimuli within the affected trigeminal distribution
C. Not better accounted for by another ICHD-3 diagnosis
Common Causes of Facial Pain
Oral cavity and salivary gland lesions (infection, trauma, inflammation, space-occupying lesion)
Facial bones and joint diseases
Paranasal sinus disease
Neuro-vascular disorders
Psychosomatic disorders
34Haryana Medical Journal - March 2020, Vol. 43, Issue 01 35Haryana Medical Journal - March 2020, Vol. 43, Issue 01
pathophysiological mechanisms not fully understood. Neville, Damm, Allen et al. (2004) affirmed that the TN may be idiopathic, but is generally associated with a condition at some point during the course of the nerve, such as an intracranial tumor, being referred to as trigeminal neuralgia symptomatic.
Clinical presentation
Due to the difficulty in diagnosing the mechanisms triggering TN, it is important to conduct detail interview, considering the symptoms reported by patients, and additional exams, such as imaging exams, studies for clinical evaluation of the anatomy of the trigeminal nerve and adjacent structures (LUNA, GRAÇA, SILVA et al., 2010). 11
The TN is a painful disease, unilateral face. The pain is often triggered by trivial stimuli, such as washing, shaving, smoking, talking, eating, applying makeup and brushing your teeth, but may occur spontaneously. The pain is of sudden onset and termination, and may decrease in in tens i ty fo r va ry ing pe r iods ( E S K A N D A R , B A R K E R a n d RABINOV, 2006). 12
It is most common between the pains orofacial, returns in irregular periods, being triggered by stimuli not Necessarily painful, by the simple act of speaking, or chewing (TODA, 2007)1.
Diagnosis
The diagnosis of TN is mainly based on clinical signs and symptoms mentioned by the patient, as typical paroxysms, refractory periods and zones trigger (TÜRP and GOBETTI, 1996).9
In the diagnosis should be excluded
A new classification has more specifically has been proposed to d i ffe ren t ia te TN 4 in to : 1 ) type 1(previously referred to as classic or typical TN), which is an idiopathic episodic pain with the previouslyreported clinical characteristics, lasting several seconds, with pain-free intervals between attacks and 2) type2, describing idiopathic trigeminal facial pain that is aching, throbbing, or burning for more than 50% of thetime and is constant in nature (constant background pain being the most significant attribute) with a minor component of sharp, episodic pain.
Pathophysiological of TN
Trauma, such as facial bone fractures, especially fractures of the zygomatic-maxillary complex, especially when it involves the floor of the orbit, injuring the infra-orbital nerve (FRIZZO, HASSE and VERONESE, 2004). 5
Vascular-TN has been related to a neurovascular compression in the prepontine cistern at the nerve rootentry-zone due to an abnormal artery or vein, arteriovenous malformation, aneurysm, vessels aggregation
T u m o u r - v e s t i b u l a r schwannoma,meningioma, epidermoid cyst, tuberculoma, various other cysts and tumors(Jamjoom et al ) 6,(Guo Z et al )7, (Kano H et al )8
I n fl a m m a t i o n – a r a c h n o i d i t i s , odontogenic inflammatory diseases, and otolaryngological pathology, such as sinusitis,19–21 ,22-31
Degenerative -MS, diabetes mellitus, Türp and Gobetti (1996)9
Idiopathic- The TN is a disease with
characteristics:
1. Lasting from a fraction of a second to two minutes
2. Severe intensity
3. Electric shock-like, shooting, stabbing or sharp in quality
B. Precipitated by innocuous stimuli within the affected trigeminal distribution
C. Not better accounted for by another ICHD-3 diagnosis
Differential Diagnosis—Clinically, the TN can be confused with disorders related to teeth, facial bones and paranasal sinuses, leading to a variety of therapeutic incorrect. Disease severity is underscored by having one of the highest suicide rates in relation to any disease, and is considered one of the most painful diseases known (NEVILLE, DAMM, ALLEN et al., 2004). 10
from the primary headaches of short duration
Krafft (2008) affirmed that the diagnosis is essentially clinical, but may need some evaluations of image or specialized tests in patients who have unusual characteristcs such as bilateral symptoms, dizziness or vertigo, age less than 40 years, hearing loss or disorder, episodes of pain with longer than two minutes, visual disturbances and pain that is not in the trigeminal distribution.
The diagnosis of TN is important to perform the analgesic block (at least at the beginning of neuralgia), rapidly stopping the pain and triggering due to the occurrence of these in the area of the affected nerve. The neurogenic pain in the orofacial region may be mistaken for masticatory pain. Therefore, we must consider the characteristics of each one.
ICHD-3 diagnost ic cr i ter ia for trigeminal neuralgia
ICHD-3: International Classification of Headache Disorders
ICHD-3 Diagnostic Criteria for Trigeminal Neuralgia
A. Pain has al l of the fol lowing
ICHD-3: International Classification of Headache Disorders
ICHD-3 Diagnostic Criteria for Trigeminal Neuralgia
A. Pain has all of the following characteristics:
1. Lasting from a fraction of a second to two minutes
2. Severe intensity
3. Electric shock-like, shooting, stabbing or sharp in quality
B. Precipitated by innocuous stimuli within the affected trigeminal distribution
C. Not better accounted for by another ICHD-3 diagnosis
Common Causes of Facial Pain
Oral cavity and salivary gland lesions (infection, trauma, inflammation, space-occupying lesion)
Facial bones and joint diseases
Paranasal sinus disease
Neuro-vascular disorders
Psychosomatic disorders
34Haryana Medical Journal - March 2020, Vol. 43, Issue 01 35Haryana Medical Journal - March 2020, Vol. 43, Issue 01
pathophysiological mechanisms not fully understood. Neville, Damm, Allen et al. (2004) affirmed that the TN may be idiopathic, but is generally associated with a condition at some point during the course of the nerve, such as an intracranial tumor, being referred to as trigeminal neuralgia symptomatic.
Clinical presentation
Due to the difficulty in diagnosing the mechanisms triggering TN, it is important to conduct detail interview, considering the symptoms reported by patients, and additional exams, such as imaging exams, studies for clinical evaluation of the anatomy of the trigeminal nerve and adjacent structures (LUNA, GRAÇA, SILVA et al., 2010). 11
The TN is a painful disease, unilateral face. The pain is often triggered by trivial stimuli, such as washing, shaving, smoking, talking, eating, applying makeup and brushing your teeth, but may occur spontaneously. The pain is of sudden onset and termination, and may decrease in in tens i ty fo r va ry ing pe r iods ( E S K A N D A R , B A R K E R a n d RABINOV, 2006). 12
It is most common between the pains orofacial, returns in irregular periods, being triggered by stimuli not Necessarily painful, by the simple act of speaking, or chewing (TODA, 2007)1.
Diagnosis
The diagnosis of TN is mainly based on clinical signs and symptoms mentioned by the patient, as typical paroxysms, refractory periods and zones trigger (TÜRP and GOBETTI, 1996).9
In the diagnosis should be excluded
A new classification has more specifically has been proposed to d i ffe ren t ia te TN 4 in to : 1 ) type 1(previously referred to as classic or typical TN), which is an idiopathic episodic pain with the previouslyreported clinical characteristics, lasting several seconds, with pain-free intervals between attacks and 2) type2, describing idiopathic trigeminal facial pain that is aching, throbbing, or burning for more than 50% of thetime and is constant in nature (constant background pain being the most significant attribute) with a minor component of sharp, episodic pain.
Pathophysiological of TN
Trauma, such as facial bone fractures, especially fractures of the zygomatic-maxillary complex, especially when it involves the floor of the orbit, injuring the infra-orbital nerve (FRIZZO, HASSE and VERONESE, 2004). 5
Vascular-TN has been related to a neurovascular compression in the prepontine cistern at the nerve rootentry-zone due to an abnormal artery or vein, arteriovenous malformation, aneurysm, vessels aggregation
T u m o u r - v e s t i b u l a r schwannoma,meningioma, epidermoid cyst, tuberculoma, various other cysts and tumors(Jamjoom et al ) 6,(Guo Z et al )7, (Kano H et al )8
I n fl a m m a t i o n – a r a c h n o i d i t i s , odontogenic inflammatory diseases, and otolaryngological pathology, such as sinusitis,19–21 ,22-31
Degenerative -MS, diabetes mellitus, Türp and Gobetti (1996)9
Idiopathic- The TN is a disease with
be difficult to treat and can recur after surgical treatments Thus, new therapeutic modalit ies have been tried. More specifically, according to a recent overview, gabapentin combined with regular ropivacaine injections into trigger sites improves pain control and quality of life.
Recently, Hu et al 16 systematically reviewed the therapeutic efficacy and safety of injection of botulinum toxin type A (BTX-A) in TN and found a response in approximately 70%–100% of patients with mean pain intensity and frequency reduced by approximately 60%–80% with no major adverse events reported. These results are in agreement with Cruccu and Truini,17 who recently reviewed the literature on the medical management of refractory TN and found that there is increasing evidence that BTX-A injections are efficacious and may be offered to patients before surgery or to patients unwilling to undergo surgery.
Although it represents a promising treatment of TN with favorable risk-to-benefit ratio, to investigate the optimal dose of BTX-A treatment, the duration of therapeutic efficacy, the side effects, and the time and indications for repeat in jec t ion , fur ther wel l -des igned , randomized, controlled, double-blinded trials are needed.
Pain techniques
Percutaneous destructive procedures, involving a trans foramen ovale approach to the retrogasserian portion of the trigeminal nerve and the radiofrequency rhizotomy, balloon compression and glycerol rhizotomy
local anesthetics
Treatment
The TN treatment may be medical or surgical. The medical therapy is the first choice, resorting to the functional neurosurgery only in cases where clinical therapy proves ineffective.
Phenytoin was the first drug used for TN with positive effects.(Mcquay H et al).13 However, according to the recent EFNS guidelines,13 two drugs are considered as first-line therapy in TN: carbamazepine (CBZ; 200–1,200mg/day) and oxcarbazepine (OXC; 600–1,800 mg/day). The effectiveness of CBZ was demonstrated in several studies. (Wiffen PJ et al) 14,(Rockcliff BW et al )15. Specifically, CBZ has been found to reduce both the frequency and intensity of painful paroxysms and was equally efficacious on spontaneous and trigger-evoked attacks. Nevertheless, frequent adverse event has been reported during CBZ therapy, especially in elderly patients. Thus, OXC is often used as initial treatment for TN due to accepted greater tolerability and decreased potential drug interactions.
Other drugs have been used in TN:baclofen was found to be superior to placebo in reducing the number of pain attacks. Lamotrigine, pimozide, and tocainide were reported to have good efficacy on pain a t tacks control . Lamotrigine in combination with CBZ or phenytoin was also found to be more effective than placebo. In patients having already undergone trigeminal surgery or taking concurrent medications, tizanidine was found to be better than placebo, but its effect decayed within 1–3 months.
Newer medical therapy
It is common experience that TN can
36Haryana Medical Journal - March 2020, Vol. 43, Issue 01 37Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Differential diagnosis of trigeminal neuralgia
HZ: Herpes Zoster, TN: trigeminal neuralgia, SUNHA: short-lasting unilateral neuralgiform headache attacks
be difficult to treat and can recur after surgical treatments Thus, new therapeutic modalit ies have been tried. More specifically, according to a recent overview, gabapentin combined with regular ropivacaine injections into trigger sites improves pain control and quality of life.
Recently, Hu et al 16 systematically reviewed the therapeutic efficacy and safety of injection of botulinum toxin type A (BTX-A) in TN and found a response in approximately 70%–100% of patients with mean pain intensity and frequency reduced by approximately 60%–80% with no major adverse events reported. These results are in agreement with Cruccu and Truini,17 who recently reviewed the literature on the medical management of refractory TN and found that there is increasing evidence that BTX-A injections are efficacious and may be offered to patients before surgery or to patients unwilling to undergo surgery.
Although it represents a promising treatment of TN with favorable risk-to-benefit ratio, to investigate the optimal dose of BTX-A treatment, the duration of therapeutic efficacy, the side effects, and the time and indications for repeat in jec t ion , fur ther wel l -des igned , randomized, controlled, double-blinded trials are needed.
Pain techniques
Percutaneous destructive procedures, involving a trans foramen ovale approach to the retrogasserian portion of the trigeminal nerve and the radiofrequency rhizotomy, balloon compression and glycerol rhizotomy
local anesthetics
Treatment
The TN treatment may be medical or surgical. The medical therapy is the first choice, resorting to the functional neurosurgery only in cases where clinical therapy proves ineffective.
Phenytoin was the first drug used for TN with positive effects.(Mcquay H et al).13 However, according to the recent EFNS guidelines,13 two drugs are considered as first-line therapy in TN: carbamazepine (CBZ; 200–1,200mg/day) and oxcarbazepine (OXC; 600–1,800 mg/day). The effectiveness of CBZ was demonstrated in several studies. (Wiffen PJ et al) 14,(Rockcliff BW et al )15. Specifically, CBZ has been found to reduce both the frequency and intensity of painful paroxysms and was equally efficacious on spontaneous and trigger-evoked attacks. Nevertheless, frequent adverse event has been reported during CBZ therapy, especially in elderly patients. Thus, OXC is often used as initial treatment for TN due to accepted greater tolerability and decreased potential drug interactions.
Other drugs have been used in TN:baclofen was found to be superior to placebo in reducing the number of pain attacks. Lamotrigine, pimozide, and tocainide were reported to have good efficacy on pain a t tacks control . Lamotrigine in combination with CBZ or phenytoin was also found to be more effective than placebo. In patients having already undergone trigeminal surgery or taking concurrent medications, tizanidine was found to be better than placebo, but its effect decayed within 1–3 months.
Newer medical therapy
It is common experience that TN can
36Haryana Medical Journal - March 2020, Vol. 43, Issue 01 37Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Differential diagnosis of trigeminal neuralgia
HZ: Herpes Zoster, TN: trigeminal neuralgia, SUNHA: short-lasting unilateral neuralgiform headache attacks
3. Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurg Focus. 2005;18(5):E3.
4. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition ( b e t a v e r s i o n ) . C e p h a l a l g i a . 2013;33(9):629–808.
5. FRIZZO, HM., HASSE, PN. and VERONESE, RM. Neuralgia do Trigêmeo: RevisãoBibliográficaAnalítica. Revista de Cirurgia e TraumatologiaBuco-Maxilo-Facial, 2004, vol. 4, n. 4, p. 212-217.
6. Jamjoom AB, Jamjoom ZA, al-Fehaily M, el-Watidy S, al-Moallem M, Nain-Ur-Rahman. Trigeminal neuralgia related to cerebellopontine angle t u m o r s . N e u r o s u r g R e v . 1996;19(4):237–241.
7. Guo Z, Ouyang H, Cheng Z. Surgical treatment of parapontine epidermoid cysts presenting with trigeminal n e u r a l g i a . J C l i n N e u ro s c i . 2011;18(3):344–346.
8. Kano H, Awan NR, Flannery TJ, et al. Stereotactic radiosurgery for patients with trigeminal neuralgia associated with petroclival meningiomas. S t e r e o t a c t F u n c t N e u r o s u r g . 2011;89(1):17–24.
9. TÜRP, JC. and GOBETTI, JP. Trigeminal neuralgia versus atypical facial pain: a review of the literature and case report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 1996, vol. 81, n. 4, p.424-432.
10. NEVILLE, BW., DAMM, DD.,
Gasser ganglion an effective method, widely used in patients over 50 years (FRIZZO, HASSE and VERONESE, 2004). 5
In decompression, the purpose is to remove the irregularities of skull base, which are close to the trigeminal nerve and/or microvascular decompression with the removal of blood vessels, which are located on the trigeminal nerve, leading them to a position closer to the normal. Thus the blood vessels are deprived of nerve fibers of the ganglion (NEVILLE, DAMM, ALLEN et al., 2004)10.
Conclusion
In conclusion, TN is more common among facial neuralgias, and since, in most cases, the patient seeks the dentist because of the location of pain, it is important that these professionals have knowledge of anatomy and function of the trigeminal nerve, keeping up with studies conducted in this area in order to correctly diagnose and perform control pain through medication or indicate surgical treatment.
References
1. TODA, K. Trigeminal neuralgia: Symptoms, diagnosis, classification, and related disorders. Oral Science International, 2007, vol. 4, n. 1, p. 1-9. http://dx.doi.org/10.1016/S1348-8643(07)80006-1
2. G O T O , F . , I S H I Z A K I , K . , YOSHIKAWA, D., OBATA, H., ARII, H. and TERADA, M. The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using a high concentration of tetracaine dissolved in bupivacaine. Pain, 1999, vol. 79, p. 101 103. http://dx.doi.org/10.1016/S0304-3959(98)00156-0
38Haryana Medical Journal - March 2020, Vol. 43, Issue 01 39Haryana Medical Journal - March 2020, Vol. 43, Issue 01
diameter equivalent to the tip of a ballpoint pen, is inserted a catheter into the patient face, inside the cheek.
Surgical treatment
The choice of method depends on the surgical condition where the patient is the etiology of facial pain, and the skill of the neurosurgeon.
Surgical treatment is based on the assumption that the cause is of peripheral origin, such as trigeminal nerve damage in a blood vessel, by a tumor or an inflammatory lesion (MAESTRI and HOLZER, 1993). 20
According to Tronnier, Rasche and Hamer (2001),21 the decompression technique that is considered to promote relief for a longer time, with control of pain by more than 70% of patients over 10 years. The decompression is indicated in young individuals who want to preserve the facial sensitivity, when there is suspected lesion towards trigeminal neuralgia or when this is combined with other facial neuralgia or hemifacial spasm.
Various surgical approaches have been proposed for the treatment of drug-resistant TN. MVD is performed with the objective to resolve the neurovascular conflict between an abnormal vessel and the trigeminal nerve. MVD is the primary ablative technique.
On the other hand, gamma knife radiosurgery (GKRS) aiming at damaging trigeminal nerve.
In recent years, the two most common procedures used were: a differential percutaneous electrocoagulation of the trigeminal nerve and trigeminal vascular d e c o m p r e s s i o n a n d a l s o w i t h radiofrequency thermocoagulation of the
The glycerol rhizotomy is performed by injecting a caustic material around nerves that leave or enter the ganglion of the trigeminal nerve. In percutaneous radiofrequency rhizotomy, there is selective destruction of sensory nerve fibers by crushing or by applying heat (GUSMÃO, MAGALDI and ARANTES, 2003).18
In rhizotomy occurs traumatization or destruction of nerve fibers selected close to or within the trigeminal ganglion. With the patient is sedated puts a needle driven by X-ray fluoroscopy, inside the ovale foramen. Being driven by the sensitivity of the patient, are located on the nerve fibers painful condition involved, and the fibers a re se lec ted and des t royed by a radiofrequency or by deposition of a toxic substance such as glycerol (by glycerol rhizotomy). This technique damages i r revers ib ly th in myel ina ted and u n m y e l i n a t e d fi b e r s h e a t e d a t temperatures ranging from 55 °C to 70 °C.
The compression balloon is simpler than radiofrequency rhizotomy can be performed under local anesthesia and the patient is awake, but without their participation. The type of anesthesia varies with the experience of professionals involved in the surgery. May be general, with or without intubation, or by blocking the region to be treated, lidocaine or other d r u g e q u i v a l e n t ( P E T E R S a n d NURMIKKO, 2002). 19
Balloon compression is a technique that offers comfort for a longer time and w i t h l o w e r r e c u r r e n c e r a t e s (approximately 30%), and have lower morbidity and no mortality. The procedure lasts a few minutes and does not require cutting. Carried out a small hole with a
3. Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurg Focus. 2005;18(5):E3.
4. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition ( b e t a v e r s i o n ) . C e p h a l a l g i a . 2013;33(9):629–808.
5. FRIZZO, HM., HASSE, PN. and VERONESE, RM. Neuralgia do Trigêmeo: RevisãoBibliográficaAnalítica. Revista de Cirurgia e TraumatologiaBuco-Maxilo-Facial, 2004, vol. 4, n. 4, p. 212-217.
6. Jamjoom AB, Jamjoom ZA, al-Fehaily M, el-Watidy S, al-Moallem M, Nain-Ur-Rahman. Trigeminal neuralgia related to cerebellopontine angle t u m o r s . N e u r o s u r g R e v . 1996;19(4):237–241.
7. Guo Z, Ouyang H, Cheng Z. Surgical treatment of parapontine epidermoid cysts presenting with trigeminal n e u r a l g i a . J C l i n N e u ro s c i . 2011;18(3):344–346.
8. Kano H, Awan NR, Flannery TJ, et al. Stereotactic radiosurgery for patients with trigeminal neuralgia associated with petroclival meningiomas. S t e r e o t a c t F u n c t N e u r o s u r g . 2011;89(1):17–24.
9. TÜRP, JC. and GOBETTI, JP. Trigeminal neuralgia versus atypical facial pain: a review of the literature and case report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 1996, vol. 81, n. 4, p.424-432.
10. NEVILLE, BW., DAMM, DD.,
Gasser ganglion an effective method, widely used in patients over 50 years (FRIZZO, HASSE and VERONESE, 2004). 5
In decompression, the purpose is to remove the irregularities of skull base, which are close to the trigeminal nerve and/or microvascular decompression with the removal of blood vessels, which are located on the trigeminal nerve, leading them to a position closer to the normal. Thus the blood vessels are deprived of nerve fibers of the ganglion (NEVILLE, DAMM, ALLEN et al., 2004)10.
Conclusion
In conclusion, TN is more common among facial neuralgias, and since, in most cases, the patient seeks the dentist because of the location of pain, it is important that these professionals have knowledge of anatomy and function of the trigeminal nerve, keeping up with studies conducted in this area in order to correctly diagnose and perform control pain through medication or indicate surgical treatment.
References
1. TODA, K. Trigeminal neuralgia: Symptoms, diagnosis, classification, and related disorders. Oral Science International, 2007, vol. 4, n. 1, p. 1-9. http://dx.doi.org/10.1016/S1348-8643(07)80006-1
2. G O T O , F . , I S H I Z A K I , K . , YOSHIKAWA, D., OBATA, H., ARII, H. and TERADA, M. The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using a high concentration of tetracaine dissolved in bupivacaine. Pain, 1999, vol. 79, p. 101 103. http://dx.doi.org/10.1016/S0304-3959(98)00156-0
38Haryana Medical Journal - March 2020, Vol. 43, Issue 01 39Haryana Medical Journal - March 2020, Vol. 43, Issue 01
diameter equivalent to the tip of a ballpoint pen, is inserted a catheter into the patient face, inside the cheek.
Surgical treatment
The choice of method depends on the surgical condition where the patient is the etiology of facial pain, and the skill of the neurosurgeon.
Surgical treatment is based on the assumption that the cause is of peripheral origin, such as trigeminal nerve damage in a blood vessel, by a tumor or an inflammatory lesion (MAESTRI and HOLZER, 1993). 20
According to Tronnier, Rasche and Hamer (2001),21 the decompression technique that is considered to promote relief for a longer time, with control of pain by more than 70% of patients over 10 years. The decompression is indicated in young individuals who want to preserve the facial sensitivity, when there is suspected lesion towards trigeminal neuralgia or when this is combined with other facial neuralgia or hemifacial spasm.
Various surgical approaches have been proposed for the treatment of drug-resistant TN. MVD is performed with the objective to resolve the neurovascular conflict between an abnormal vessel and the trigeminal nerve. MVD is the primary ablative technique.
On the other hand, gamma knife radiosurgery (GKRS) aiming at damaging trigeminal nerve.
In recent years, the two most common procedures used were: a differential percutaneous electrocoagulation of the trigeminal nerve and trigeminal vascular d e c o m p r e s s i o n a n d a l s o w i t h radiofrequency thermocoagulation of the
The glycerol rhizotomy is performed by injecting a caustic material around nerves that leave or enter the ganglion of the trigeminal nerve. In percutaneous radiofrequency rhizotomy, there is selective destruction of sensory nerve fibers by crushing or by applying heat (GUSMÃO, MAGALDI and ARANTES, 2003).18
In rhizotomy occurs traumatization or destruction of nerve fibers selected close to or within the trigeminal ganglion. With the patient is sedated puts a needle driven by X-ray fluoroscopy, inside the ovale foramen. Being driven by the sensitivity of the patient, are located on the nerve fibers painful condition involved, and the fibers a re se lec ted and des t royed by a radiofrequency or by deposition of a toxic substance such as glycerol (by glycerol rhizotomy). This technique damages i r revers ib ly th in myel ina ted and u n m y e l i n a t e d fi b e r s h e a t e d a t temperatures ranging from 55 °C to 70 °C.
The compression balloon is simpler than radiofrequency rhizotomy can be performed under local anesthesia and the patient is awake, but without their participation. The type of anesthesia varies with the experience of professionals involved in the surgery. May be general, with or without intubation, or by blocking the region to be treated, lidocaine or other d r u g e q u i v a l e n t ( P E T E R S a n d NURMIKKO, 2002). 19
Balloon compression is a technique that offers comfort for a longer time and w i t h l o w e r r e c u r r e n c e r a t e s (approximately 30%), and have lower morbidity and no mortality. The procedure lasts a few minutes and does not require cutting. Carried out a small hole with a
CASE REPORT: SUCCESSFUL TERM PREGNANCY IN A PATIENT
WITH UTERUS DIDELPHYS, PREGNANCY IN LEFT UTERUS AND IUCD IN RIGHT UTERUS
Dr. Anjali Sharma
ABSTRACTBACKGROUND:
Mullerian duct anomalies (MDAs) are congenital defects of the female genital sys tem that ar ise f rom abnormal embryological development of the Mullerian ducts. A didelphys uterus, also known as a “double uterus,” is one of the least common amongst MDAs.
Uterus Didelphys is a congenital malformation of the Mullerian duct that occurs because of complete failure of fusion of the ispilateral ducts. It results in the developments of a longitudinal vaginal septum, two vaginas, and two hemi-uteri each with its separate ovary and fallopian tube. The incidence of this anomaly is 1 in 3000 [1]. It remains a challenge to the obstetricians especially when it is undiagnosed before onset of labor. Patients are usually asymptomatic, but the anomaly may be associa ted with dysmenorrhoea, dyspareunia, infertility, spontaneous abortion, preterm labor, fetal malpresentation, intrauterine growth restriction, PROM, renal agenesis, decreased live births and caesarean delivery [1-6].
Diagnosis is usually initiated by the findings of a longitudinal vaginal septum and two vaginal openings during a vaginal examinat ion . A 3-D t ransvaginal
sonography is an excellent non-invasive method of investigation [6]. Others methods of investigations include sonohysterography, hysterosalpingography, hysterolaparoscopy and pelvic magnetic resonant imaging. The incidence of caesarean delivery in uterus Didelphys in pregnancy may be as high as 82% [2]. Several good pregnancy outcomes including vaginal deliveries, twin and triplet pregnancies have, however, been reported [7-11]. The aim of this case report is to make clinicians to have high index of suspicion of uterine anomaly when investigating cases of dysmenorrhea, dyspareunia, infertility, spontaneous a b o r t i o n , p r e t e r m l a b o r , f e t a l malpresentation, intrauterine growth restriction, PROM, and renal agenesis. Early diagnosis, meticulous follow up can avert most of these complications.
This report discusses a case of didelphys uterus that successfully conceived, carried her pregnancy to term, and delivered by caesarian without any significant complications.
Case report
Patient ABC 24yrs old female G P L2 1 1
with 40wks 4days postdated pregnancy with previous LSCS 2yrs back girl child with uterus didelphys with IUCD in one uterus, outside booked patient presented to
40Haryana Medical Journal - March 2020, Vol. 43, Issue 01 41Haryana Medical Journal - March 2020, Vol. 43, Issue 01
18. GUSMÃO, S., MAGALDI, M. and ARANTES, A. Rizotomia trigeminal por radiofrequência para tratamento da neuralgia do trigêmeo: resultados e modificação técnica. Arquivos de Neuro- Psiquiatria, 2003, vol. 61, n. 2-B, p. 434-440. PMid:12894280.
19. PETERS, G. and NURMIKKO, TJ. Peripheral and gasserian ganglion-level precedures for the treatment of trigeminal neuralgia. Clinical Journal of Pain, 2002, vol. 18, n. 1, p. 28 34. PMid:11803300.
20. MAESTRI, JM. and HOLZER, F. Fisiopatología de la neuralgia del trigémeno. Revista Chilena de Neuro-Psiquiatria, 1993, vol. 31, n. 3, p. 317-321.
21. Rasche D, Rinaldi PC, Young RF, Tronnier VM. Deep brain stimulation for the treatment of various chronic pain syndromes. Neurosurg Focus. 2006;21(6):E8.
22. Comparative evaluation of surgical procedures for trigeminal neuralgia. Parmar M, Sharma N, Modgill V, Naidu P. J Maxillofac Oral Surg. 2013;12:400- 409.
23. Trigeminal neuralgia pain relief after gamma knife stereotactic radiosurgery. Baschnagel AM, Cartier JL, Dreyer J, et al. Clin Neurol Neurosurg.2014;117:107-111.
24. CW. Trigeminal neuralgia – a dental diagnosis challenge. Northwest Dentistry, 1999, vol. 78, n. 3, p. 19-24
Address of CorrespondenceDr Utkarsh
Surat Medical Collage, Surat
ALLEN, CM. and BOUQUOT, JE. Patologia Oral e Maxilofacial. 2. ed. Rio de Janeiro: Guanabara Koogan, 2004. p. 865-67
11. LUNA, EB., GRAÇA, LFA., SILVA, DCO., BÉRZIN, F., SILVA, Z., SOUZA, GC. and MITRI, FF. AspectosAnatômicos e Patológicos da Neuralgia do Trigêmeo: umarevisão da literatura para estudantes e profissionais da saúde. Bioscience Journal, 2010, vol. 26, n. 4, p.661-674.
12. ESKANDAR, E., BARKER, FG. and RABINOV, JD. Case records of the Massachusetts General Hospital. Case 21-2006. A 61-year old man with left-sided facial pain. New England Journal of Medicine, 2006, vol. 355, p. 183-188. PMid:16837683. http:// dx.doi.org/10.1056/NEJMcpc069011
13. McQuay H, Carroll D, Jadad AR, Wiffen P, Moore A. Anticonvulsant drugs for management systematic review. BMJ. 1995;311(7012):1047–1052
14. Wiffen PJ, Derry S, Moore RA, Kalso EA. Carbamazepine for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2014;4:CD005451.
15. Rockcliff BW, Davis EH. Controlled sequential trials of carbamazepine in trigeminal neuralgia. Arch Neurol. 1996;15(2):129–136.
16. Hu Y, Guan X , Fan L , e t a l . Therapeutic efficacy and safety of botulinum toxin type A in trigeminal neuralgia: a systematic review. J Headache Pain. 2013;14:72.
17. AAN-EFNS guidelines on trigeminal neuralgia management. Cruccu G, Gronseth G, Alksne J, et al. Eur J Neurol. 2008;15:1013-1028.]
CASE REPORT: SUCCESSFUL TERM PREGNANCY IN A PATIENT
WITH UTERUS DIDELPHYS, PREGNANCY IN LEFT UTERUS AND IUCD IN RIGHT UTERUS
Dr. Anjali Sharma
ABSTRACTBACKGROUND:
Mullerian duct anomalies (MDAs) are congenital defects of the female genital sys tem that ar ise f rom abnormal embryological development of the Mullerian ducts. A didelphys uterus, also known as a “double uterus,” is one of the least common amongst MDAs.
Uterus Didelphys is a congenital malformation of the Mullerian duct that occurs because of complete failure of fusion of the ispilateral ducts. It results in the developments of a longitudinal vaginal septum, two vaginas, and two hemi-uteri each with its separate ovary and fallopian tube. The incidence of this anomaly is 1 in 3000 [1]. It remains a challenge to the obstetricians especially when it is undiagnosed before onset of labor. Patients are usually asymptomatic, but the anomaly may be associa ted with dysmenorrhoea, dyspareunia, infertility, spontaneous abortion, preterm labor, fetal malpresentation, intrauterine growth restriction, PROM, renal agenesis, decreased live births and caesarean delivery [1-6].
Diagnosis is usually initiated by the findings of a longitudinal vaginal septum and two vaginal openings during a vaginal examinat ion . A 3-D t ransvaginal
sonography is an excellent non-invasive method of investigation [6]. Others methods of investigations include sonohysterography, hysterosalpingography, hysterolaparoscopy and pelvic magnetic resonant imaging. The incidence of caesarean delivery in uterus Didelphys in pregnancy may be as high as 82% [2]. Several good pregnancy outcomes including vaginal deliveries, twin and triplet pregnancies have, however, been reported [7-11]. The aim of this case report is to make clinicians to have high index of suspicion of uterine anomaly when investigating cases of dysmenorrhea, dyspareunia, infertility, spontaneous a b o r t i o n , p r e t e r m l a b o r , f e t a l malpresentation, intrauterine growth restriction, PROM, and renal agenesis. Early diagnosis, meticulous follow up can avert most of these complications.
This report discusses a case of didelphys uterus that successfully conceived, carried her pregnancy to term, and delivered by caesarian without any significant complications.
Case report
Patient ABC 24yrs old female G P L2 1 1
with 40wks 4days postdated pregnancy with previous LSCS 2yrs back girl child with uterus didelphys with IUCD in one uterus, outside booked patient presented to
40Haryana Medical Journal - March 2020, Vol. 43, Issue 01 41Haryana Medical Journal - March 2020, Vol. 43, Issue 01
18. GUSMÃO, S., MAGALDI, M. and ARANTES, A. Rizotomia trigeminal por radiofrequência para tratamento da neuralgia do trigêmeo: resultados e modificação técnica. Arquivos de Neuro- Psiquiatria, 2003, vol. 61, n. 2-B, p. 434-440. PMid:12894280.
19. PETERS, G. and NURMIKKO, TJ. Peripheral and gasserian ganglion-level precedures for the treatment of trigeminal neuralgia. Clinical Journal of Pain, 2002, vol. 18, n. 1, p. 28 34. PMid:11803300.
20. MAESTRI, JM. and HOLZER, F. Fisiopatología de la neuralgia del trigémeno. Revista Chilena de Neuro-Psiquiatria, 1993, vol. 31, n. 3, p. 317-321.
21. Rasche D, Rinaldi PC, Young RF, Tronnier VM. Deep brain stimulation for the treatment of various chronic pain syndromes. Neurosurg Focus. 2006;21(6):E8.
22. Comparative evaluation of surgical procedures for trigeminal neuralgia. Parmar M, Sharma N, Modgill V, Naidu P. J Maxillofac Oral Surg. 2013;12:400- 409.
23. Trigeminal neuralgia pain relief after gamma knife stereotactic radiosurgery. Baschnagel AM, Cartier JL, Dreyer J, et al. Clin Neurol Neurosurg.2014;117:107-111.
24. CW. Trigeminal neuralgia – a dental diagnosis challenge. Northwest Dentistry, 1999, vol. 78, n. 3, p. 19-24
Address of CorrespondenceDr Utkarsh
Surat Medical Collage, Surat
ALLEN, CM. and BOUQUOT, JE. Patologia Oral e Maxilofacial. 2. ed. Rio de Janeiro: Guanabara Koogan, 2004. p. 865-67
11. LUNA, EB., GRAÇA, LFA., SILVA, DCO., BÉRZIN, F., SILVA, Z., SOUZA, GC. and MITRI, FF. AspectosAnatômicos e Patológicos da Neuralgia do Trigêmeo: umarevisão da literatura para estudantes e profissionais da saúde. Bioscience Journal, 2010, vol. 26, n. 4, p.661-674.
12. ESKANDAR, E., BARKER, FG. and RABINOV, JD. Case records of the Massachusetts General Hospital. Case 21-2006. A 61-year old man with left-sided facial pain. New England Journal of Medicine, 2006, vol. 355, p. 183-188. PMid:16837683. http:// dx.doi.org/10.1056/NEJMcpc069011
13. McQuay H, Carroll D, Jadad AR, Wiffen P, Moore A. Anticonvulsant drugs for management systematic review. BMJ. 1995;311(7012):1047–1052
14. Wiffen PJ, Derry S, Moore RA, Kalso EA. Carbamazepine for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2014;4:CD005451.
15. Rockcliff BW, Davis EH. Controlled sequential trials of carbamazepine in trigeminal neuralgia. Arch Neurol. 1996;15(2):129–136.
16. Hu Y, Guan X , Fan L , e t a l . Therapeutic efficacy and safety of botulinum toxin type A in trigeminal neuralgia: a systematic review. J Headache Pain. 2013;14:72.
17. AAN-EFNS guidelines on trigeminal neuralgia management. Cruccu G, Gronseth G, Alksne J, et al. Eur J Neurol. 2008;15:1013-1028.]
6.� Madureira AJ, Mariz CM, Bernardes JC, Ramos IM (2006). Case 94: Uterus D i d e l p h y s w i t h O b s t r u c t i n g Hemivaginal Septum and Ipsilateral Renal Agenesis. Radiology 239: 602-606.
7.� C. Magudapathi (2012). “Uterus didelphys with longitudinal vaginal septum: normal deliver—case report,” Journal of Clinical Case Reports, vol. 2, article 13.
8.� R. Garg, A. Kwatra, and V. Bangal, “A rare case of uterus didelphys with full term pregnancy in each horn,” Pravara Medical Review, vol. 2, no. 4, pp. 22–24, 2010.
9.� Mashiach S, Ben-Rafael Z, Dor J, Serr DM (1981) Triplet Pregnancy in Uterus Didelphys with Delivery Interval of 72 days. Obstet Gynecol 58: 519-521.
10.�Magudapathi C (2012), Uterus Didelphys with Longitudinal Vaginal Septum: Normal Delivery. Journal of C l i n i c a l C a s e R e p o r t s . 2 : 1 3 https://dx.doi.org/10.4172/2165-7920.1000194.
11.�Mohd Subhail, Hina Khan, Sofia Suhail (2010). Uterus Didelphys having Single Pregnancy in her right horn: A Case Report. Journal of Chinese Clinical Medicine Volume 5 (1): 46-49.
12.�Green LK, Harris RE (1976).Uterine anomalies; frequency of diagnosis, and obstetric complications, 47 (4):427-428.
deliveries [11]. Recent advances in diagnostic techniques, and availability of met iculous medical services and t r e a t m e n t s f o r t h e a s s o c i a t e d complications that favor good outcomes depict the international clinical relevance of early diagnosis of the subject.
Conclusion
Clinicians should have high index of suspicion of uterine anomaly to make early diagnosis of uterus Didelphys. Pregnancy in a uterus Didelphys deserves early diagnosis of the anomaly, and meticulous care in pregnancy and delivery to avert the associated adverse outcomes.
References
1.� Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Dervoey P (2001) Clinical implications of uterine malformation and hysterscopic treatment results. Hum Reprod Update 7: 161-174.
2.� Heinonen P K (1984), “Uterus didelphys: a report of 26 cases,” European Journal of Obstetrics & Gynecology and Reproduct ive Biology, vol. 17, no. 5, pp. 345–350.
3.� Heinonen PK (2000), “Clinical implications of the didelphic uterus: long-term follow-up of 49 cases,” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 91, no. 2, pp. 183–190.
4.� Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, and Pellicer A,(1997) “Reproductive impact of congenital Mullerian anomalies,” Human Reproduction, vol. 12, no. 10, pp. 2277–2281.
5.� Acien P (1993), “Reproductive performance of women with uterine malformations,” Human Reproduction, vol. 8, no. 1, pp. 122–126.
Address of CorrespondenceDr Anjali Sharma
Senior Resident Obstetrics and Gynaecology Department
Kalpana Chawla Medical College, Karnal
tertiary care centre.On history taking there was history of threatened abortion in first trimester. No history of infertility, no h/o preterm labour pains. On examination PR 96/min, BP 120/70mmHg, chest clear.
P/A uterus re laxed ,cephal ic presentation, FHS 140bpm. On PV examination,2 vaginal openings felt with vaginal septum. CuT Thread was not felt. Ultrasonography was done suggestive of live pregnancy in left uterus with IUGR and IUCD in situ in right uterus. Patient consented for Caesarian section. A live girl baby was delivered 2.4kg. Double uterus was diagnosed intraoperatively. No s i g n i fi c a n t c o m p l i c a t i o n s n o t e d intraoperatively. Patient and relatives refused for tubal ligation. IUCD thread was removed vaginally. The postoperative recovery was uneventful. Patient was discharged on day 5 post op after counseling her on family planning and how to manage her subsequent pregnancie and further postnatal follow up was explained.
Longitudinal vaginal septum and two vaginal openings
INTRAOPERATIVE FINDINGS
Discussion
Uterus Didelphys is rare and sometimes not even diagnosed. It occurs in 0.1% -0.5% of healthy fertile population [12]. Heinonen PK (2000) [3], evaluated the long-term clinical consequences, and reproductive performances of 49 women with uterus Didelphys that were followed up to 6.3 years. He found obstructed hemi vagina in 9 (18%) with 8 (16.3%) having ipsilateral renal agenesis. Five (13%) had primary infertility. Thirty four out of 36 (94%) women who wanted to conceive became pregnant, 21% had miscarriage while 2% were ectopic pregnancy. The fetal survival rate was 75%, prematurity 24%, fetal growth retardation 11%, perinatal mortality 5.3%, and caesarean delivery rate 84%. Pregnancy was located in the right uterus in 76% cases. Many of the patients with uterus Didelphys have normal sex lives, pregnancies, and
42Haryana Medical Journal - March 2020, Vol. 43, Issue 01 43Haryana Medical Journal - March 2020, Vol. 43, Issue 01
6.� Madureira AJ, Mariz CM, Bernardes JC, Ramos IM (2006). Case 94: Uterus D i d e l p h y s w i t h O b s t r u c t i n g Hemivaginal Septum and Ipsilateral Renal Agenesis. Radiology 239: 602-606.
7.� C. Magudapathi (2012). “Uterus didelphys with longitudinal vaginal septum: normal deliver—case report,” Journal of Clinical Case Reports, vol. 2, article 13.
8.� R. Garg, A. Kwatra, and V. Bangal, “A rare case of uterus didelphys with full term pregnancy in each horn,” Pravara Medical Review, vol. 2, no. 4, pp. 22–24, 2010.
9.� Mashiach S, Ben-Rafael Z, Dor J, Serr DM (1981) Triplet Pregnancy in Uterus Didelphys with Delivery Interval of 72 days. Obstet Gynecol 58: 519-521.
10.�Magudapathi C (2012), Uterus Didelphys with Longitudinal Vaginal Septum: Normal Delivery. Journal of C l i n i c a l C a s e R e p o r t s . 2 : 1 3 https://dx.doi.org/10.4172/2165-7920.1000194.
11.�Mohd Subhail, Hina Khan, Sofia Suhail (2010). Uterus Didelphys having Single Pregnancy in her right horn: A Case Report. Journal of Chinese Clinical Medicine Volume 5 (1): 46-49.
12.�Green LK, Harris RE (1976).Uterine anomalies; frequency of diagnosis, and obstetric complications, 47 (4):427-428.
deliveries [11]. Recent advances in diagnostic techniques, and availability of met iculous medical services and t r e a t m e n t s f o r t h e a s s o c i a t e d complications that favor good outcomes depict the international clinical relevance of early diagnosis of the subject.
Conclusion
Clinicians should have high index of suspicion of uterine anomaly to make early diagnosis of uterus Didelphys. Pregnancy in a uterus Didelphys deserves early diagnosis of the anomaly, and meticulous care in pregnancy and delivery to avert the associated adverse outcomes.
References
1.� Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Dervoey P (2001) Clinical implications of uterine malformation and hysterscopic treatment results. Hum Reprod Update 7: 161-174.
2.� Heinonen P K (1984), “Uterus didelphys: a report of 26 cases,” European Journal of Obstetrics & Gynecology and Reproduct ive Biology, vol. 17, no. 5, pp. 345–350.
3.� Heinonen PK (2000), “Clinical implications of the didelphic uterus: long-term follow-up of 49 cases,” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 91, no. 2, pp. 183–190.
4.� Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, and Pellicer A,(1997) “Reproductive impact of congenital Mullerian anomalies,” Human Reproduction, vol. 12, no. 10, pp. 2277–2281.
5.� Acien P (1993), “Reproductive performance of women with uterine malformations,” Human Reproduction, vol. 8, no. 1, pp. 122–126.
Address of CorrespondenceDr Anjali Sharma
Senior Resident Obstetrics and Gynaecology Department
Kalpana Chawla Medical College, Karnal
tertiary care centre.On history taking there was history of threatened abortion in first trimester. No history of infertility, no h/o preterm labour pains. On examination PR 96/min, BP 120/70mmHg, chest clear.
P/A uterus re laxed ,cephal ic presentation, FHS 140bpm. On PV examination,2 vaginal openings felt with vaginal septum. CuT Thread was not felt. Ultrasonography was done suggestive of live pregnancy in left uterus with IUGR and IUCD in situ in right uterus. Patient consented for Caesarian section. A live girl baby was delivered 2.4kg. Double uterus was diagnosed intraoperatively. No s i g n i fi c a n t c o m p l i c a t i o n s n o t e d intraoperatively. Patient and relatives refused for tubal ligation. IUCD thread was removed vaginally. The postoperative recovery was uneventful. Patient was discharged on day 5 post op after counseling her on family planning and how to manage her subsequent pregnancie and further postnatal follow up was explained.
Longitudinal vaginal septum and two vaginal openings
INTRAOPERATIVE FINDINGS
Discussion
Uterus Didelphys is rare and sometimes not even diagnosed. It occurs in 0.1% -0.5% of healthy fertile population [12]. Heinonen PK (2000) [3], evaluated the long-term clinical consequences, and reproductive performances of 49 women with uterus Didelphys that were followed up to 6.3 years. He found obstructed hemi vagina in 9 (18%) with 8 (16.3%) having ipsilateral renal agenesis. Five (13%) had primary infertility. Thirty four out of 36 (94%) women who wanted to conceive became pregnant, 21% had miscarriage while 2% were ectopic pregnancy. The fetal survival rate was 75%, prematurity 24%, fetal growth retardation 11%, perinatal mortality 5.3%, and caesarean delivery rate 84%. Pregnancy was located in the right uterus in 76% cases. Many of the patients with uterus Didelphys have normal sex lives, pregnancies, and
42Haryana Medical Journal - March 2020, Vol. 43, Issue 01 43Haryana Medical Journal - March 2020, Vol. 43, Issue 01
•�Pain management, as many impairments can be associated with considerable discomfort
•�Counselling
•�Medication to either restore function or prevent a worsening of the patient’s condition
•�Operative techniques.
Methodology
� We performed a comprehensive literature search in the PubMed, Google Scholar, Cochrane electronic database to review relevant articles in English using keywords “ yoga, physical exercise, neuro log ica l condi t ions- S t roke , P a r k i n s o n , M u l t i p l e S c l e r o s i s , Alzhimer ’s, Neuropathy, Epilepsy, Migraine and Sinusitis. A total of 900 articles were available in respective to the above mentioned keywords. Of 900 articles, 87 articles that fit into the following inclusion and exclusion criteria were reported in this review. Inclusion criteria: clinical trials, controlled trials, randomized controlled trials, systematic review and meta-analysis that are dealing with yoga and physical therapy in combination with or without other therapies. Exclusion criteria: Research protocol, comments, articles that do not have either abstract or full text in English, articles with lack of information.
Yoga and physiotherapy
� Physiotherapy can be defined as a treatment method that focuses on the science of movement and helps people to restore, maintain and maximize their physical strength, function, motion and overall well-being by addressing the underlying physical issues.(6)
� Physiotherapy is a health care profession
60–70% of cases. The prevalence of migraine is more than 10% worldwide.(2)
Most common sign and symptoms of Neurological disorders are: Partial or complete paralysis, Muscle weakness, partial or complete loss of sensation, seizures, difficulty reading and writing, poor cognitive abilities, unexplained pain, mood disorders, anxiety, depression, d e c r e a s e d a l e r t n e s s , e m o t i o n a l disturbances, abnormal movements and abnormal behaviour.(3)
Evaluating and diagnosing damage to the nervous system is complicated and complex. In addition to a complete medical history and physical exam, diagnostic procedures for nervous system disorders may include the following: Computed tomography scan (also called a CT or CAT scan), Electroencephalogram (EEG), Magnetic resonance imaging (MRI), Electrodiagnostic tests, such as electromyography (EMG) and nerve conduction velocity (NCV), Positron emission tomography (PET), Arteriogram (also called an angiogram), Spinal tap (also called a lumbar puncture), Evoked p o t e n t i a l s , M y e l o g r a m , Neurosonography, ultrasound etc.(4)
There are various possible treatment options available for neurological disorders (5) may often consist of:
•�Lifestyle changes to either prevent or minimize the impact of neurological disorders such as sedentary lifestyle, smoking, alcohol and eating habits.
•�Physiotherapy to manage the symptoms and restore some function such as electrotherapeutic modalities (e.g. diathermy, TENS, muscle stimulator, biofeedback), various exercises and yoga.
44Haryana Medical Journal - March 2020, Vol. 43, Issue 01 45Haryana Medical Journal - March 2020, Vol. 43, Issue 01
EFFECTS OF YOGA AND PHYSICAL EXERCISES IN NEUROLOGICAL CONDITIONS
Dr Shilpa Mehta
Abstract
Some studies have proven that CAM (compl imen ta ry and a l t e rna t i ve medicine) methods has positive effects on the mental and psychological health, as well as on motor emotional and cognitive deficit in patients with neurological diseases. Though yoga and physical exercises are widely used mind body medicine for health promotion, disease prevention and as a possible treatment modality for neurological disorders, there is lack of evidence based review. We performed a comprehensive search in the PubMed, Google Scholar and Cochrane electronic database to review relevant articles in English using keywords “ yoga, physical exercise and neurological disorders like Stroke, Parkinson’s, M u l t i p l e s c l e r o s i s , E p i l e p s y , Migraine/Headache, Alzheimer and Neuropathies so on. There are not many randomized and controlled studies, but yoga and physical exercises can improve mental and physical heal th with improvement of quality of life. Based on available literature, it could be concluded that yoga and physical exercises might be considered as an effective adjuvant therapy for the patients with various neurological disorders.
Introduction
Neurological disorders are defined as the diseases of the central and peripheral nervous system such as the region of brain, spinal cord, cranial nerves,
peripheral nerves, nerve roots, autonomic nervous system, neuromuscular junction, and muscles. These disorders include epilepsy, Alzheimer disease, dementias, cerebrovascular diseases including stroke, sinusitis, migraine, headache, multiple sclerosis, hydrocephalus, Parkinson’s disease, neuroinfections, brain tumours, traumatic disorders of the nervous system mainly due to head trauma, infection and malnutrition.(1)
These diseases may result from a wide range of pathophysiologies including traumatic injury to the central nervous s y s t e m , n e u r o d e g e n e r a t i o n a n d neuroinflammation. Many bacterial (i.e. Mycobacterial tuberculosis, Neisseria meningi t ides) , viral ( i .e . Human Immunodefic iency Vi rus (HIV) , Enteroviruses, fungal (i.e. Cryptococcus, Aspergillus), and parasitic (i.e. malaria, Chagas) infections can also affect the nervous system.(1)
According to recent report of WHO, Hundreds o f mi l l ions o f people worldwide are affected by neurological disorders. More than 6 million people die because of stroke each year; over 80% of these deaths take place in low- and middle-income countries. More than 50 million people have epilepsy worldwide. It is estimated that there are globally 47.5 million people with dementia with 7.7 mi l l ion new cases eve ry yea r - Alzheimer’s disease is the most common cause of dementia and may contribute to
•�Pain management, as many impairments can be associated with considerable discomfort
•�Counselling
•�Medication to either restore function or prevent a worsening of the patient’s condition
•�Operative techniques.
Methodology
� We performed a comprehensive literature search in the PubMed, Google Scholar, Cochrane electronic database to review relevant articles in English using keywords “ yoga, physical exercise, neuro log ica l condi t ions- S t roke , P a r k i n s o n , M u l t i p l e S c l e r o s i s , Alzhimer ’s, Neuropathy, Epilepsy, Migraine and Sinusitis. A total of 900 articles were available in respective to the above mentioned keywords. Of 900 articles, 87 articles that fit into the following inclusion and exclusion criteria were reported in this review. Inclusion criteria: clinical trials, controlled trials, randomized controlled trials, systematic review and meta-analysis that are dealing with yoga and physical therapy in combination with or without other therapies. Exclusion criteria: Research protocol, comments, articles that do not have either abstract or full text in English, articles with lack of information.
Yoga and physiotherapy
� Physiotherapy can be defined as a treatment method that focuses on the science of movement and helps people to restore, maintain and maximize their physical strength, function, motion and overall well-being by addressing the underlying physical issues.(6)
� Physiotherapy is a health care profession
60–70% of cases. The prevalence of migraine is more than 10% worldwide.(2)
Most common sign and symptoms of Neurological disorders are: Partial or complete paralysis, Muscle weakness, partial or complete loss of sensation, seizures, difficulty reading and writing, poor cognitive abilities, unexplained pain, mood disorders, anxiety, depression, d e c r e a s e d a l e r t n e s s , e m o t i o n a l disturbances, abnormal movements and abnormal behaviour.(3)
Evaluating and diagnosing damage to the nervous system is complicated and complex. In addition to a complete medical history and physical exam, diagnostic procedures for nervous system disorders may include the following: Computed tomography scan (also called a CT or CAT scan), Electroencephalogram (EEG), Magnetic resonance imaging (MRI), Electrodiagnostic tests, such as electromyography (EMG) and nerve conduction velocity (NCV), Positron emission tomography (PET), Arteriogram (also called an angiogram), Spinal tap (also called a lumbar puncture), Evoked p o t e n t i a l s , M y e l o g r a m , Neurosonography, ultrasound etc.(4)
There are various possible treatment options available for neurological disorders (5) may often consist of:
•�Lifestyle changes to either prevent or minimize the impact of neurological disorders such as sedentary lifestyle, smoking, alcohol and eating habits.
•�Physiotherapy to manage the symptoms and restore some function such as electrotherapeutic modalities (e.g. diathermy, TENS, muscle stimulator, biofeedback), various exercises and yoga.
44Haryana Medical Journal - March 2020, Vol. 43, Issue 01 45Haryana Medical Journal - March 2020, Vol. 43, Issue 01
EFFECTS OF YOGA AND PHYSICAL EXERCISES IN NEUROLOGICAL CONDITIONS
Dr Shilpa Mehta
Abstract
Some studies have proven that CAM (compl imen ta ry and a l t e rna t i ve medicine) methods has positive effects on the mental and psychological health, as well as on motor emotional and cognitive deficit in patients with neurological diseases. Though yoga and physical exercises are widely used mind body medicine for health promotion, disease prevention and as a possible treatment modality for neurological disorders, there is lack of evidence based review. We performed a comprehensive search in the PubMed, Google Scholar and Cochrane electronic database to review relevant articles in English using keywords “ yoga, physical exercise and neurological disorders like Stroke, Parkinson’s, M u l t i p l e s c l e r o s i s , E p i l e p s y , Migraine/Headache, Alzheimer and Neuropathies so on. There are not many randomized and controlled studies, but yoga and physical exercises can improve mental and physical heal th with improvement of quality of life. Based on available literature, it could be concluded that yoga and physical exercises might be considered as an effective adjuvant therapy for the patients with various neurological disorders.
Introduction
Neurological disorders are defined as the diseases of the central and peripheral nervous system such as the region of brain, spinal cord, cranial nerves,
peripheral nerves, nerve roots, autonomic nervous system, neuromuscular junction, and muscles. These disorders include epilepsy, Alzheimer disease, dementias, cerebrovascular diseases including stroke, sinusitis, migraine, headache, multiple sclerosis, hydrocephalus, Parkinson’s disease, neuroinfections, brain tumours, traumatic disorders of the nervous system mainly due to head trauma, infection and malnutrition.(1)
These diseases may result from a wide range of pathophysiologies including traumatic injury to the central nervous s y s t e m , n e u r o d e g e n e r a t i o n a n d neuroinflammation. Many bacterial (i.e. Mycobacterial tuberculosis, Neisseria meningi t ides) , viral ( i .e . Human Immunodefic iency Vi rus (HIV) , Enteroviruses, fungal (i.e. Cryptococcus, Aspergillus), and parasitic (i.e. malaria, Chagas) infections can also affect the nervous system.(1)
According to recent report of WHO, Hundreds o f mi l l ions o f people worldwide are affected by neurological disorders. More than 6 million people die because of stroke each year; over 80% of these deaths take place in low- and middle-income countries. More than 50 million people have epilepsy worldwide. It is estimated that there are globally 47.5 million people with dementia with 7.7 mi l l ion new cases eve ry yea r - Alzheimer’s disease is the most common cause of dementia and may contribute to
dosage of exercise intervention and application to disease severity. (23)
� Exercise’s neuroprotective benefit on the brain is a current area of research study. Exercise is believed to slow aging at the cellular level and produce regenerative effects on the brain. Cardiovascular exercise increases blood flow to the brain and stimulates the development of growth factors in the brain that encourage the growth of new neurons and synapses.(24)
� Exercise regimes from more traditional treadmill training, (25,26) balance exercise and progressive. resistive strengthening (27) to alternative types of physical activity like Nordic walking (28) , tango (29) and Tai Chi (30) have been investigated.
� Although PD is a progressive disorder, several studies have found that increasing physical activity can improve aerobic capacity (31), strength and flexibility (32), balance (33), increase movement time (34) and gait parameters including speed (35,36) which in turn may contribute to independence in activities of daily living , improved physical function and mobility and increased longevity . Regular physical activity may delay the onset of PD symptoms.(37)
� Lyengar Hatha yoga provides a gentle alternative method of exercise that can be easily adapted in people with physical disability and neurological disorders because of the progression from body awareness to relaxation to flexibility to strength activities.(38) Yoga has been shown to significantly improve measures of gait, fatigue, quality of life, and physical function in healthy elderly and people with neurologic disorders.(39-42)
Multiple sclerosis
improvements in strength and range of m o v e m e n t o r w a l k i n g a b i l i t y ; psychological improvement in sense of calmness and social improvement in terms of the possibility of reconnecting and accepting a different body.(18) Compared with usual care, yoga resulted in a significant improvement in exercise capacity and in health related quality of life QOL.(19)
� Mood disorders are prevalent in people after stroke, and a disorder’s onset can exacerbate stroke related disabilities (20). Whereas practice of yoga has shown to reduce the symptoms of anxiety (19) and practice of yoga combined with exercise has shown to be feasible, safe, acceptable and effective in improving mood in patients with stroke.
� In another study, 3 month practice of yogic breathing techniques along with body manipulations, and ingestion of coconut oil has shown to be effective in improving language, visual attention, and mood measures in a patient with post-stroke aphasia.(21)
Parkinson’s disease
� Parkinson’s disease (PD) is the second most common neurodegenerative brain disorder that is caused by nerve cell degeneration in a region of the brain that controls voluntary movement. The symtoms include tremors, a shuffling walk, muscle stiffness, stooped posture, and a mask like, expressionless face. Other non motor symtoms include depression, dementia and cognitive impairment. (22)
� Current management of PD involves both pharmacological treatment and p h y s i c a l a c t i v i t y, b u t r e s e a r c h demonstrates the benefits of physical activity in PD are widely varied in type and
46Haryana Medical Journal - March 2020, Vol. 43, Issue 01 47Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� Cerebrovascular accident (CVA) is a common nervous system disorder that occur due to abnormal blood circulation in the brain , resulting either from ischaemic stroke or intracranial haemorrhage. (11)
� Stroke is an increasing public health concern throughout the world. The world health organization (WHO) defines stroke as a clinical syndrome characterized by “ rapidly developing clinical sign of focal disturbance of brain function with symptoms lasting 24 hours or leading to death with no apparent cause other than vascular origin.”(12) Since strokes occur suddenly with effects lasting a lifetime, methods to prevent strokes and to help patients rehabilitate with yoga and physical exercises. (13) Post-stroke therapy may improve recovery and reduce long-term disability. Yoga seems to offer a relief from a long list of medical ailments in stroke by alleviating both the mind and the body from stress.(14)
� Yoga and meditation act on both the psychological and physical levels, and improvements in patients’ mindsets. Improvement in the mindsets of people with the disease can potentially lead to a change in behavior and ultimately an improvement in health. Impairment in balance is common after stroke. (15)
� Previous studies on 8 week (twice per week) yoga-based rehabilitation have shown to potentially improve multiple post stroke variables such as significant improvement in balance (Berg Balance Scale), fear of falling, pain, range of motion of neck and hip, upper extremity strength, and 6-min walk scores in patients with chronic stroke.(16,17)
� In another study, 10 week practice of yoga has reported to produce physical
which assists people to restore, maintain and maximize their strength, function, movement, and overall well-being. Physiotherapy includes rehabilitation, as well as prevention of injury, and promotion of health and fitness. It can help i n n e u r o l o g i c a l c o n d i t i o n s , m u s c u l o s k e l e t a l , o r t h o p a e d i c s , cardiopulmonary, sports, obstetrics and gynaecological, antenatal and prenatal conditions.(7,8)
� Yoga is an ancient practice that has its roots in Hindu religion. The word “yoga” comes from the Sanskrit “yuj,” meaning “yoke” or “union.” It is believed that “yoga” describes the union between the mind and body, and it is used as a therapeutic intervention in a variety of diseases. Yoga consists of three primary c o m p o n e n t s : a s a n a s ( p o s t u r e s ) , pranayama (breathing exercises), and dhyana (meditation).
� Yoga can be defined as a Hindu spiritual and ascetic discipline which including breath control, simple meditation, and the adoption of specific bodily postures that is widely practised for health and relaxation. A Hindu philosophy that teaches a person to experience inner peace by controlling the body and mind. (9)
� Yoga is thought to treat symptoms of certain neurological and psychiatric disorders through a variety of biological mechanisms related to either the aerobic components of yoga (the changing sequence of asanas) or the breathing and meditative components of yoga(10) (pranayama and dhyana).
Practice of Yoga and Physical exercise and its effects in various neurological disorders
Stroke
dosage of exercise intervention and application to disease severity. (23)
� Exercise’s neuroprotective benefit on the brain is a current area of research study. Exercise is believed to slow aging at the cellular level and produce regenerative effects on the brain. Cardiovascular exercise increases blood flow to the brain and stimulates the development of growth factors in the brain that encourage the growth of new neurons and synapses.(24)
� Exercise regimes from more traditional treadmill training, (25,26) balance exercise and progressive. resistive strengthening (27) to alternative types of physical activity like Nordic walking (28) , tango (29) and Tai Chi (30) have been investigated.
� Although PD is a progressive disorder, several studies have found that increasing physical activity can improve aerobic capacity (31), strength and flexibility (32), balance (33), increase movement time (34) and gait parameters including speed (35,36) which in turn may contribute to independence in activities of daily living , improved physical function and mobility and increased longevity . Regular physical activity may delay the onset of PD symptoms.(37)
� Lyengar Hatha yoga provides a gentle alternative method of exercise that can be easily adapted in people with physical disability and neurological disorders because of the progression from body awareness to relaxation to flexibility to strength activities.(38) Yoga has been shown to significantly improve measures of gait, fatigue, quality of life, and physical function in healthy elderly and people with neurologic disorders.(39-42)
Multiple sclerosis
improvements in strength and range of m o v e m e n t o r w a l k i n g a b i l i t y ; psychological improvement in sense of calmness and social improvement in terms of the possibility of reconnecting and accepting a different body.(18) Compared with usual care, yoga resulted in a significant improvement in exercise capacity and in health related quality of life QOL.(19)
� Mood disorders are prevalent in people after stroke, and a disorder’s onset can exacerbate stroke related disabilities (20). Whereas practice of yoga has shown to reduce the symptoms of anxiety (19) and practice of yoga combined with exercise has shown to be feasible, safe, acceptable and effective in improving mood in patients with stroke.
� In another study, 3 month practice of yogic breathing techniques along with body manipulations, and ingestion of coconut oil has shown to be effective in improving language, visual attention, and mood measures in a patient with post-stroke aphasia.(21)
Parkinson’s disease
� Parkinson’s disease (PD) is the second most common neurodegenerative brain disorder that is caused by nerve cell degeneration in a region of the brain that controls voluntary movement. The symtoms include tremors, a shuffling walk, muscle stiffness, stooped posture, and a mask like, expressionless face. Other non motor symtoms include depression, dementia and cognitive impairment. (22)
� Current management of PD involves both pharmacological treatment and p h y s i c a l a c t i v i t y, b u t r e s e a r c h demonstrates the benefits of physical activity in PD are widely varied in type and
46Haryana Medical Journal - March 2020, Vol. 43, Issue 01 47Haryana Medical Journal - March 2020, Vol. 43, Issue 01
� Cerebrovascular accident (CVA) is a common nervous system disorder that occur due to abnormal blood circulation in the brain , resulting either from ischaemic stroke or intracranial haemorrhage. (11)
� Stroke is an increasing public health concern throughout the world. The world health organization (WHO) defines stroke as a clinical syndrome characterized by “ rapidly developing clinical sign of focal disturbance of brain function with symptoms lasting 24 hours or leading to death with no apparent cause other than vascular origin.”(12) Since strokes occur suddenly with effects lasting a lifetime, methods to prevent strokes and to help patients rehabilitate with yoga and physical exercises. (13) Post-stroke therapy may improve recovery and reduce long-term disability. Yoga seems to offer a relief from a long list of medical ailments in stroke by alleviating both the mind and the body from stress.(14)
� Yoga and meditation act on both the psychological and physical levels, and improvements in patients’ mindsets. Improvement in the mindsets of people with the disease can potentially lead to a change in behavior and ultimately an improvement in health. Impairment in balance is common after stroke. (15)
� Previous studies on 8 week (twice per week) yoga-based rehabilitation have shown to potentially improve multiple post stroke variables such as significant improvement in balance (Berg Balance Scale), fear of falling, pain, range of motion of neck and hip, upper extremity strength, and 6-min walk scores in patients with chronic stroke.(16,17)
� In another study, 10 week practice of yoga has reported to produce physical
which assists people to restore, maintain and maximize their strength, function, movement, and overall well-being. Physiotherapy includes rehabilitation, as well as prevention of injury, and promotion of health and fitness. It can help i n n e u r o l o g i c a l c o n d i t i o n s , m u s c u l o s k e l e t a l , o r t h o p a e d i c s , cardiopulmonary, sports, obstetrics and gynaecological, antenatal and prenatal conditions.(7,8)
� Yoga is an ancient practice that has its roots in Hindu religion. The word “yoga” comes from the Sanskrit “yuj,” meaning “yoke” or “union.” It is believed that “yoga” describes the union between the mind and body, and it is used as a therapeutic intervention in a variety of diseases. Yoga consists of three primary c o m p o n e n t s : a s a n a s ( p o s t u r e s ) , pranayama (breathing exercises), and dhyana (meditation).
� Yoga can be defined as a Hindu spiritual and ascetic discipline which including breath control, simple meditation, and the adoption of specific bodily postures that is widely practised for health and relaxation. A Hindu philosophy that teaches a person to experience inner peace by controlling the body and mind. (9)
� Yoga is thought to treat symptoms of certain neurological and psychiatric disorders through a variety of biological mechanisms related to either the aerobic components of yoga (the changing sequence of asanas) or the breathing and meditative components of yoga(10) (pranayama and dhyana).
Practice of Yoga and Physical exercise and its effects in various neurological disorders
Stroke
functions in dementia. (66)
Epilepsy
� Seizure, occasionally referred to as a fit, is defined as a transient symptom of “abnormal excessive or synchronous neuronal activity in the brain”. The outward effect can be as dramatic as a wild thrashing movement or as mild as a brief loss of awareness. The medical syndrome of recurrent, unprovoked seizures is termed epilepsy. The World Health Organization estimates that around 50 million people in the world have epilepsy. Epilepsy is caused out of unexpected storm or hyperactivity of the brain cells.
� The purpose of practice of asana and pranayama is to develop control over the body and the mind. Asana prepares the entire physical functioning of the body, while pranayama improves the physiology of the body. Asana stretches the nerves system and pranayama oxygenates the brain which ultimately controls and stabilise the brain cells from getting too excited.
� Research found that meditat ion improved the brain wave activity of people with seizure disorders leading to a reduction in seizures. It is found that patients who learned to control their breathing had an improvement in their seizure frequency.(67)
� In one such study, 20 patients (fourteen males, six females, age range 15 to 47 years) with established diagnoses of epilepsy underwent a yoga-meditation protocol (YMP) for 20 minutes twice daily (mornings and evenings) at home and one supervised session of YMP every week for three months. Patients who remained in the program past three months continued the yoga-meditation protocol without any
improved quality of life, balance, and neuropathic symptoms.(62)
� Chemotherapy induced peripheral neuropathy is a frequent side effect of drug that are used in treatment of cancer. Affected people suffer from motor, sensory or autonomy nerve damage. In a review, alternative therapies including yoga have reported to produce good symptomatic results in patients with chemotherapy induced peripheral neuropathy.(63)
Alzheimer’s disease
� Alzheimer’s disease is a chronic progressive neurological disorder that causes memory loss and loss of cognitive movement. In this disease, the brain cells get degenerated and dies. Alzheimer’s disease disrupts a person’s ability to perform daily activities and forces them to require assistance.
� There is no permanent cure for Alzheimer’s disease in conventional treatment options. The treatment process of Alzheimer’s disease focuses on reducing the symptoms of the disease and helping the patient in recovering the ability to perform daily tasks. In the advanced stages of Alzheimer’s disease, a person loses the ability to perform brain functions and could even result in death. (64)
� In a study 8 weeks practice of Sit N Fit chair yoga has shown to be effective in improving six minute walk test, walking speed and balance in older adults with moderate and severe AD (65)
� Studies on 8 weeks practice of yoga meditation have shown to produce a significant reduction in depression, anxiety, mental, physical and cognitive
49Haryana Medical Journal - March 2020, Vol. 43, Issue 0148Haryana Medical Journal - March 2020, Vol. 43, Issue 01
practice of integrated yoga intervention as an adjunct to standard medical care has shown to be safe and effective in improving bladder symptoms such as post-void residual urine, scores on mic tu r i t ion f requency check l i s t , incontinence impact questionnaire-7, and urogenital distress inventory-6 in patients with MS associated with neurogenic bladder dysfunction.(51)
� In another study, 3 month (60–90 min per session, 8 sessions per month) practice of yoga has shown to improve physical activities and sexual satisfaction function of women with MS.(52)
Peripheral Neuropathy
� Peripheral neuropathy, one of the most common complications of diabetes mellitus,(53) typically is characterized as a symmetrical distal degeneration of peripheral nerves and impaired nerve regenerat ion. Diabet ic peripheral neuropathy (DPN) can cause impairments in tactile sensitivity, vibration sense, lower limb proprioception, and kinesthesia. The loss of sensation associated with the neuropathy is thought to contribute to impaired balance, altered gait patterns, and increased risk of falling.(54,55)
� A e r o b i c e x e r c i s e i n t e r v e n t i o n demonstrated decreased pain interference as well as decreased general and physical fatigue.(56-58)) In a randomized controlled trial, Dixit et al also found that aerobic exercise had a positive effect on nerve conduction velocity.(59) Whole-body vibration (WBV) training used to supplement balance exercise was also recently shown to benefit people with DPN,(60) and 12 weeks of tai chi has resulted in improved median and tibial nerve conduction velocities(61) and
� M u l t i p l e s c l e r o s i s ( M S ) i s a n unpredictable, often disabling disease of central nervous system that disrupts the flow of the information within the brain, and between the brain and body. MS is an autoimmune inflammatory demyelinating disease of the central nervous system.(43) According to the National Institute of Neurological Disorders and Stroke, the age of disease onset is typically between 20 and 40 years, with a higher incidence in women.(44) Individuals with MS experience a wide range of symptoms, with varying degrees of severity affecting fatigue , mobility limitation, gait impairment, falls due to balance problems (imbalance), spasticity, chronic pain, bladder and bowel dysfunction, cognitive impairment , sensory dis turbance, auditory, visual and speech impairments, depression, anxiety and reduced QOL.(45-49)
� Yoga is relatively inexpensive, generally safe and may potentially improve multiple sclerosis symtoms.(43) MS clinical trial found that yoga decreased fatigue, anxiety, depression, bladder function, pain, spasticity, weakness and walking.(39) These conditions may secondarily worsen disability and QOL but yoga practice can slow them. (50)
� MS is characterized by a significant deterioration in auditory and visual reaction times but a study on 3 week (5 days a week, 5 h per day) practice of integrated yoga and physical therapy has showed a significant improvement in audiovisual reaction times in chronic MS patients.(39)
� Neurogenic bladder dysfunction is a common distressful symptom in MS. In a study, 21 days (2 h per day for daily)
functions in dementia. (66)
Epilepsy
� Seizure, occasionally referred to as a fit, is defined as a transient symptom of “abnormal excessive or synchronous neuronal activity in the brain”. The outward effect can be as dramatic as a wild thrashing movement or as mild as a brief loss of awareness. The medical syndrome of recurrent, unprovoked seizures is termed epilepsy. The World Health Organization estimates that around 50 million people in the world have epilepsy. Epilepsy is caused out of unexpected storm or hyperactivity of the brain cells.
� The purpose of practice of asana and pranayama is to develop control over the body and the mind. Asana prepares the entire physical functioning of the body, while pranayama improves the physiology of the body. Asana stretches the nerves system and pranayama oxygenates the brain which ultimately controls and stabilise the brain cells from getting too excited.
� Research found that meditat ion improved the brain wave activity of people with seizure disorders leading to a reduction in seizures. It is found that patients who learned to control their breathing had an improvement in their seizure frequency.(67)
� In one such study, 20 patients (fourteen males, six females, age range 15 to 47 years) with established diagnoses of epilepsy underwent a yoga-meditation protocol (YMP) for 20 minutes twice daily (mornings and evenings) at home and one supervised session of YMP every week for three months. Patients who remained in the program past three months continued the yoga-meditation protocol without any
improved quality of life, balance, and neuropathic symptoms.(62)
� Chemotherapy induced peripheral neuropathy is a frequent side effect of drug that are used in treatment of cancer. Affected people suffer from motor, sensory or autonomy nerve damage. In a review, alternative therapies including yoga have reported to produce good symptomatic results in patients with chemotherapy induced peripheral neuropathy.(63)
Alzheimer’s disease
� Alzheimer’s disease is a chronic progressive neurological disorder that causes memory loss and loss of cognitive movement. In this disease, the brain cells get degenerated and dies. Alzheimer’s disease disrupts a person’s ability to perform daily activities and forces them to require assistance.
� There is no permanent cure for Alzheimer’s disease in conventional treatment options. The treatment process of Alzheimer’s disease focuses on reducing the symptoms of the disease and helping the patient in recovering the ability to perform daily tasks. In the advanced stages of Alzheimer’s disease, a person loses the ability to perform brain functions and could even result in death. (64)
� In a study 8 weeks practice of Sit N Fit chair yoga has shown to be effective in improving six minute walk test, walking speed and balance in older adults with moderate and severe AD (65)
� Studies on 8 weeks practice of yoga meditation have shown to produce a significant reduction in depression, anxiety, mental, physical and cognitive
49Haryana Medical Journal - March 2020, Vol. 43, Issue 0148Haryana Medical Journal - March 2020, Vol. 43, Issue 01
practice of integrated yoga intervention as an adjunct to standard medical care has shown to be safe and effective in improving bladder symptoms such as post-void residual urine, scores on mic tu r i t ion f requency check l i s t , incontinence impact questionnaire-7, and urogenital distress inventory-6 in patients with MS associated with neurogenic bladder dysfunction.(51)
� In another study, 3 month (60–90 min per session, 8 sessions per month) practice of yoga has shown to improve physical activities and sexual satisfaction function of women with MS.(52)
Peripheral Neuropathy
� Peripheral neuropathy, one of the most common complications of diabetes mellitus,(53) typically is characterized as a symmetrical distal degeneration of peripheral nerves and impaired nerve regenerat ion. Diabet ic peripheral neuropathy (DPN) can cause impairments in tactile sensitivity, vibration sense, lower limb proprioception, and kinesthesia. The loss of sensation associated with the neuropathy is thought to contribute to impaired balance, altered gait patterns, and increased risk of falling.(54,55)
� A e r o b i c e x e r c i s e i n t e r v e n t i o n demonstrated decreased pain interference as well as decreased general and physical fatigue.(56-58)) In a randomized controlled trial, Dixit et al also found that aerobic exercise had a positive effect on nerve conduction velocity.(59) Whole-body vibration (WBV) training used to supplement balance exercise was also recently shown to benefit people with DPN,(60) and 12 weeks of tai chi has resulted in improved median and tibial nerve conduction velocities(61) and
� M u l t i p l e s c l e r o s i s ( M S ) i s a n unpredictable, often disabling disease of central nervous system that disrupts the flow of the information within the brain, and between the brain and body. MS is an autoimmune inflammatory demyelinating disease of the central nervous system.(43) According to the National Institute of Neurological Disorders and Stroke, the age of disease onset is typically between 20 and 40 years, with a higher incidence in women.(44) Individuals with MS experience a wide range of symptoms, with varying degrees of severity affecting fatigue , mobility limitation, gait impairment, falls due to balance problems (imbalance), spasticity, chronic pain, bladder and bowel dysfunction, cognitive impairment , sensory dis turbance, auditory, visual and speech impairments, depression, anxiety and reduced QOL.(45-49)
� Yoga is relatively inexpensive, generally safe and may potentially improve multiple sclerosis symtoms.(43) MS clinical trial found that yoga decreased fatigue, anxiety, depression, bladder function, pain, spasticity, weakness and walking.(39) These conditions may secondarily worsen disability and QOL but yoga practice can slow them. (50)
� MS is characterized by a significant deterioration in auditory and visual reaction times but a study on 3 week (5 days a week, 5 h per day) practice of integrated yoga and physical therapy has showed a significant improvement in audiovisual reaction times in chronic MS patients.(39)
� Neurogenic bladder dysfunction is a common distressful symptom in MS. In a study, 21 days (2 h per day for daily)
functional outcomes in neurological conditions. Physical therapy (PT) focuses p a r t i c u l a r l y o n s e n s o r y – m o t o r i m p a i r m e n t s , p o s t u r a l c o n t r o l coordination, breathing control and prevention of abnormal behaviour, anxiety and depression. PT has a significant influence on quality of life, independent living and life expectancy. Hospital-based short-term intensive PT aimed at the recovery of musculoskele ta l and neurological function, limbs positioning, and handling due to hypertonic or spastic muscles.
� PT for neurological patients is a comprehensive process that intends to teach, guide, and promote brain plasticity, thus reducing the threats for any functional and cognitive variations. Although there is strong support that a structural PT program for neurological patients could actually affect brain functions by assisting neurogenerative, neuroadaptive and n e u r o p r o t e c t i v e p r o c e s s e s . Neurorehabilitation may be implemented in the framework recommended by the International Classification of Function, Health and Diseases. (83)
Physiotherapy and occupational therapy are frequently administered in intensive care units (ICUs) after neurological disorder to promote recovery. (84)
� Yoga is emerging as a widely practiced complementary and integrative therapy. World Health Organization officially began promoting yoga in 1978 and yoga has been widely used for therapeutic p u r p o s e a s a n a l t e r n a t i v e a n d complementary means of therapy. This paper brings to light the utility of yoga as a non-invasive means of treating many neurological disorders and improving the
activities. For some people, a warning symptom known as an aura occurs before or with the headache. An aura can include visual disturbances, such as flashes of light or blind spots, or other disturbances, such as tingling on one side of the face or in an arm or leg and difficulty speaking. (80)
� Asana and Pranayama improve the neuromuscular activities and control the entire physiological function of the body and the psychological structure of the mind. Progressive muscle relaxation, meditation and Yoga can make a big difference in our life styles to tackle and prevent the attack. Practice of Yoganidra can give the ultimate relaxation to the body and rest to the mind. Regular practice of Asanas reduces stress and prevent migraines and reduce medications. (81)
� The three-month study randomly assigned 160 adults (ages 18–50) who experience episodic migraine with or without aura (a migraine with sensory disturbances) to either a combination of medical treatment and yoga practice or med ica l t he rapy on ly. The yoga participants practiced three supervised sessions a week for four weeks at a medical research center in New Delhi, India, followed by five session/week at home for the duration of the study. The results concluded that the yoga group experienced more relief from migraine in conjunction with their medication than the medical therapy alone. ( 82)
Discussion:
� Maximum world’s population faces neurological disorders and decline of function that can affect lifestyle and well-being.
� Recent advances in rehabilitation techniques have produced be t te r
50Haryana Medical Journal - March 2020, Vol. 43, Issue 01 51Haryana Medical Journal - March 2020, Vol. 43, Issue 01
immune and cardiovascular function. (68,69)
Sinusitis
� Sinuses are the empty spaces behind the nose and face bone. Inflammation of these sinuses is called sinusitis, which may or may not be as a result of bacterial and fungal, viral infection, allergic or a u t o i m m u n e d i s e a s e . ( 7 0 ) N e w c l a s s i fi c a t i o n o f s i n u s r e f e r t o rhinosinusitis, taking into account that inflammation of sinuses cannot occur without some inflammation of the nose as well as (rhinitis). Sinusitis is one of the most frequent entities in clinical practice, being a lifestyle ailment cause lot of discomfort in day to day life. There’s difficulty in breathing because of mucus build up and swelling in nasal region, resulting in blocked nose. Also, this build up affects the whole face, the head feels heavy, swelling and redness in eyes area, blocked ears.(71)
� Yoga has the potentiality to prevent and cure the disease of both body and mind. Yogasana (posture), Mantra recitation, Jala Neti, Sutra Neti, Kunjal Kriya, Gomukhasana (cow face pose), Janu s i r sasana ( Head to knee pose ) , Setubandhasana, Bhastrika pranayama, Anulom vilom pranayama, Bhujangasana, Kapalbhati and Meditation. Yogic kriya is beneficial in improving the status of patients with sinusitis. (72-79)
Migraine/ headache
� A migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily
supervision. The outcome measure was the seizure frequency at three, six, and twelve months of the treatment period. At three months, a significant reduction in seizure frequency was noted in all except one patient. Of the sixteen patients who continued the yoga-meditation protocol beyond three months, fourteen patients showed a significant reduction in seizure frequency, with six of the patients being completely seizure-free. (68)
� In another similar study, researchers examined the effects of posture, breathing, and meditation on autonomic functions of epileptic patients. The yoga group (n=18) received supervised training in yoga while a second group (n=16) practiced simple routine exercises. After ten weeks of daily functions, a subset of autonomic functions was measured. Data were compared with those of healthy volunteers (n=142). The y o g a g r o u p s h o w e d s i g n i fi c a n t improvement in parasympathe t ic parameters and a decrease in seizure frequency scores. While there was not much improvement in blood pressure parameters in either group, few patients in the yoga group achieved normal autonomic functions at the end of ten weeks of therapy, with limited changes in the exercise group.(69)
� Both studies suggest that a yoga-meditation protocol may have a role as an adjunct therapy in the management of epilepsy. yoga’s benefits include, but are not limited to, increases in muscle strength and tone, improvement in respiration, energy, and vitality, improvement in physical performance and increases in blood flow. Similarly, meditation reduces stress, anxiety, and depression, seizure frequency, strengthens the brain areas, improves awareness, and strengthens the
functional outcomes in neurological conditions. Physical therapy (PT) focuses p a r t i c u l a r l y o n s e n s o r y – m o t o r i m p a i r m e n t s , p o s t u r a l c o n t r o l coordination, breathing control and prevention of abnormal behaviour, anxiety and depression. PT has a significant influence on quality of life, independent living and life expectancy. Hospital-based short-term intensive PT aimed at the recovery of musculoskele ta l and neurological function, limbs positioning, and handling due to hypertonic or spastic muscles.
� PT for neurological patients is a comprehensive process that intends to teach, guide, and promote brain plasticity, thus reducing the threats for any functional and cognitive variations. Although there is strong support that a structural PT program for neurological patients could actually affect brain functions by assisting neurogenerative, neuroadaptive and n e u r o p r o t e c t i v e p r o c e s s e s . Neurorehabilitation may be implemented in the framework recommended by the International Classification of Function, Health and Diseases. (83)
Physiotherapy and occupational therapy are frequently administered in intensive care units (ICUs) after neurological disorder to promote recovery. (84)
� Yoga is emerging as a widely practiced complementary and integrative therapy. World Health Organization officially began promoting yoga in 1978 and yoga has been widely used for therapeutic p u r p o s e a s a n a l t e r n a t i v e a n d complementary means of therapy. This paper brings to light the utility of yoga as a non-invasive means of treating many neurological disorders and improving the
activities. For some people, a warning symptom known as an aura occurs before or with the headache. An aura can include visual disturbances, such as flashes of light or blind spots, or other disturbances, such as tingling on one side of the face or in an arm or leg and difficulty speaking. (80)
� Asana and Pranayama improve the neuromuscular activities and control the entire physiological function of the body and the psychological structure of the mind. Progressive muscle relaxation, meditation and Yoga can make a big difference in our life styles to tackle and prevent the attack. Practice of Yoganidra can give the ultimate relaxation to the body and rest to the mind. Regular practice of Asanas reduces stress and prevent migraines and reduce medications. (81)
� The three-month study randomly assigned 160 adults (ages 18–50) who experience episodic migraine with or without aura (a migraine with sensory disturbances) to either a combination of medical treatment and yoga practice or med ica l t he rapy on ly. The yoga participants practiced three supervised sessions a week for four weeks at a medical research center in New Delhi, India, followed by five session/week at home for the duration of the study. The results concluded that the yoga group experienced more relief from migraine in conjunction with their medication than the medical therapy alone. ( 82)
Discussion:
� Maximum world’s population faces neurological disorders and decline of function that can affect lifestyle and well-being.
� Recent advances in rehabilitation techniques have produced be t te r
50Haryana Medical Journal - March 2020, Vol. 43, Issue 01 51Haryana Medical Journal - March 2020, Vol. 43, Issue 01
immune and cardiovascular function. (68,69)
Sinusitis
� Sinuses are the empty spaces behind the nose and face bone. Inflammation of these sinuses is called sinusitis, which may or may not be as a result of bacterial and fungal, viral infection, allergic or a u t o i m m u n e d i s e a s e . ( 7 0 ) N e w c l a s s i fi c a t i o n o f s i n u s r e f e r t o rhinosinusitis, taking into account that inflammation of sinuses cannot occur without some inflammation of the nose as well as (rhinitis). Sinusitis is one of the most frequent entities in clinical practice, being a lifestyle ailment cause lot of discomfort in day to day life. There’s difficulty in breathing because of mucus build up and swelling in nasal region, resulting in blocked nose. Also, this build up affects the whole face, the head feels heavy, swelling and redness in eyes area, blocked ears.(71)
� Yoga has the potentiality to prevent and cure the disease of both body and mind. Yogasana (posture), Mantra recitation, Jala Neti, Sutra Neti, Kunjal Kriya, Gomukhasana (cow face pose), Janu s i r sasana ( Head to knee pose ) , Setubandhasana, Bhastrika pranayama, Anulom vilom pranayama, Bhujangasana, Kapalbhati and Meditation. Yogic kriya is beneficial in improving the status of patients with sinusitis. (72-79)
Migraine/ headache
� A migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily
supervision. The outcome measure was the seizure frequency at three, six, and twelve months of the treatment period. At three months, a significant reduction in seizure frequency was noted in all except one patient. Of the sixteen patients who continued the yoga-meditation protocol beyond three months, fourteen patients showed a significant reduction in seizure frequency, with six of the patients being completely seizure-free. (68)
� In another similar study, researchers examined the effects of posture, breathing, and meditation on autonomic functions of epileptic patients. The yoga group (n=18) received supervised training in yoga while a second group (n=16) practiced simple routine exercises. After ten weeks of daily functions, a subset of autonomic functions was measured. Data were compared with those of healthy volunteers (n=142). The y o g a g r o u p s h o w e d s i g n i fi c a n t improvement in parasympathe t ic parameters and a decrease in seizure frequency scores. While there was not much improvement in blood pressure parameters in either group, few patients in the yoga group achieved normal autonomic functions at the end of ten weeks of therapy, with limited changes in the exercise group.(69)
� Both studies suggest that a yoga-meditation protocol may have a role as an adjunct therapy in the management of epilepsy. yoga’s benefits include, but are not limited to, increases in muscle strength and tone, improvement in respiration, energy, and vitality, improvement in physical performance and increases in blood flow. Similarly, meditation reduces stress, anxiety, and depression, seizure frequency, strengthens the brain areas, improves awareness, and strengthens the
movement disorders, Parkinson’s disease, PD fitness, yoga for Parkinsons.
25.� Skidmore FM, Patterson SL, Shulman LM, Sorkin JD, Macko RF (2008) Pilot safety and feasibility study of treadmill aerobic exercise in Parkinson disease with gait impairment. J Rehabil Res Dev 45: 117-124.
26.� Kurtais Y, Kutlay S, Tur BS, Gok H, Akbostanci C (2008) Does treadmill training improve lower-extremity tasks in Parkinson disease? A randomized controlled trial. Clin J Sport Med 18: 289-291.
27.� Toole T, Hirsch MA, Forkink A, Lehman DA, Maitland CG (2000) The effects of a balance and strength training program on equ i l ib r ium in Pa rk inson i sm: A preliminary study. NeuroRehabilitation 14: 165-174.
28.� van Eijkeren FJ, Reijmers RS, Kleinveld MJ, Minten A, Bruggen JP, et al. (2008) Nordic walking improves mobility in Parkinson’s disease. Mov Disord 23: 2239-2243.
29.� Hackney ME, Kantorovich S, Levin R, Earhart GM (2007) Effects of tango on functional mobility in Parkinson’s disease: a preliminary study. J Neurol Phys Ther 31: 173-179.
30.� Hackney ME, Earhart GM (2008) Tai Chi improves balance and mobility in people with Parkinson disease. Gait Posture 28: 456-460.
31.� Canning CG, Alison JA, Allen NE, Groeller H (1997) Parkinson’s disease: an investigation of exercise capacity, respiratory function, and gait. Arch Phys Med Rehabil 78: 199-207.
32.� Reuter I, Mehnert S, Leone P, Kaps M, Oechsner M, et al. (2011) Effects of a flexibility and relaxation programme, walking, and nordic walking on Parkinson’s disease. J Aging Res 2011: 232473.
2011;17:1-8
15.� Lazaridou A, Philbrook P, Tzika AA. Yoga and mindfulness as therapeutic interventions for stroke rehabilitation: a s y s t e m a t i c r e v i e w. E v i d B a s e d C o m p l e m e n t A l t e r n a t M e d 2013;2013:357108.
16.� Schmid AA, Van Puymbroeck M, Altenburger PA, et al. Post-stroke balance improves with yoga: a pilot study. Stroke 2012;43(9):2402–7.
17.� Schmid AA, Miller KK, Van Puymbroeck M, et al. Yoga leads to multiple physical improvements after stroke, a pilot study. C o m p l e m e n t T h e r M e d 2014;22(6):994–1000.
18.� Garrett R, Immink MA, Hillier S. B e c o m i n g c o n n e c t e d : t h e l i v e d experience of yoga participation after s t r o k e . D i s a b i l R e h a b i l 2011;33(25–26):2404–15.
19.� Desveaux L, Lee A, Goldstein R, et al. Yoga in the management of chronic disease: a systematic review and meta-analysis. Med Care 2015;53(7):653–61.
20.� Chan W, Immink MA, Hillier S. Yoga and exercise for symptoms of depression and anxiety in people with poststroke disability: a randomized, controlled pilot t r i a l . A l t e r n T h e r H e a l t h M e d 2012;18(3):34–43.
21.� Mohapatra B, Marshall RS, Laures-Gore J. Yogic breathing and Ayurveda in aphasia: a case study. Top Stroke Rehabil 2014;21(3):272–9
22.� Lewy body dementia Association (800) 539-9767. www.parkinson.org
23.� Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL (2008) The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 23: 631-640.
24.� Exercise and Nutrition, meditation,
52Haryana Medical Journal - March 2020, Vol. 43, Issue 01 53Haryana Medical Journal - March 2020, Vol. 43, Issue 01
2018;5(1):1-10.
3.� Neurological disorders: public heath challenges. World health organisation. ISBN 92 4 156336 2 (NLM classifi cation: WL 140) ISBN 978 92 4 156336 9
4.� Siuly S and Zhang Y. Medical Big Data: Neurological Diseases Diagnosis Through Medical Data Analysis. Data Science and Engineering 2016; 1(2):54-64.
5.� Gray JT and Gravin CM. Assessment and management of neurological problems. Emerg Med J 2005; 22:440–445.
6.� Definition of physical therapy: Merriam Webster, updated on June 8th, 2018.
7.� Guide to physical therapy practice, 682 (American Physical Therapy Association, 2nd ed. 2003).
8.� Amrit B & Mantu P. Recent advancement in the field of Physiotherapy. June, 2012.
9.� Mooventhan A and Nivethitha L. Evidence based effects of yoga in neurological disorders. Journal of clinical neuroscience 2017:1-7.
10.� Taylor CB, Sallis JF, Needle R: The Relation of physical activity and exercise to mental health. Public Health Rep 1985;100:195-202
11.� Eas ton JD, Hauser S , Mar t in J . Cerebrovascular disease. Harrison’s Principles of Internal Medicine, New York: McGraw-Hill Publisher,2001
12.� World health organization . stroke 1989. Recommendation on stroke prevention and diagnosis and therapy. Report of WHO. Task force on stroke and other cerebrovascular disorders. Stroke. 20:1407-31.
13.� Mishra SK, Singh P, Bunch SJ, et al. The therapeutic value of yoga in neurological disorders. Ann Indian Acad Neurol 2012;15(4):247–54
14.� Field T. Yoga clinical research review. Compliment Therapy Clinical Practice.
overall quality of life.
� Research demonstrated improvements in cardiovascular parameters with a various meditation program. There are significant reductions in resting systolic blood pressure (BP) in adolescents with high normal BP. A reduction in reactivity of BP, heart rate, and cardiac output to simulated stressors reflects the beneficial effects of yoga at rest and during stressful states. The practice of yoga is also a s s o c i a t e d w i t h s o m e p r o f o u n d biochemical changes. There is a great potential for specific yoga programs to be u s e d i n t h e r e h a b i l i t a t i o n o f musculoskeletal injuries and neurological disorders to maintain muscle tone. (85)
� Evidence showed that yoga and various therapeutic exercises are effective in neurological disorders like epilepsy, migraine, multiple sclerosis, stroke, Parkinson’s disease, peripheral nervous system diseases and many more.(86)
Conclusion
� Based on the available literature, it could be concluded that physiotherapy and yoga both are considered as an effective adjuvant therapy for the patients with various neurological disorders including stroke, Parkinson’s disease, multiple sclerosis, epilepsy, Alzheimer’s disease, d e m e n t i a , h e a d a c h e , m i g r a i n e , neuropathies and so on.
References :
1.� The Types of Neurological Conditions and Physiotherapy Used. Available at http://ThePhysioSite.com. Accessed February 24, 2009.
2.� Rizk MZ, Fouad GI and Aly HF. Neurological disorders: causes and treatment strategies. International journal of mental health and neurosciences
movement disorders, Parkinson’s disease, PD fitness, yoga for Parkinsons.
25.� Skidmore FM, Patterson SL, Shulman LM, Sorkin JD, Macko RF (2008) Pilot safety and feasibility study of treadmill aerobic exercise in Parkinson disease with gait impairment. J Rehabil Res Dev 45: 117-124.
26.� Kurtais Y, Kutlay S, Tur BS, Gok H, Akbostanci C (2008) Does treadmill training improve lower-extremity tasks in Parkinson disease? A randomized controlled trial. Clin J Sport Med 18: 289-291.
27.� Toole T, Hirsch MA, Forkink A, Lehman DA, Maitland CG (2000) The effects of a balance and strength training program on equ i l ib r ium in Pa rk inson i sm: A preliminary study. NeuroRehabilitation 14: 165-174.
28.� van Eijkeren FJ, Reijmers RS, Kleinveld MJ, Minten A, Bruggen JP, et al. (2008) Nordic walking improves mobility in Parkinson’s disease. Mov Disord 23: 2239-2243.
29.� Hackney ME, Kantorovich S, Levin R, Earhart GM (2007) Effects of tango on functional mobility in Parkinson’s disease: a preliminary study. J Neurol Phys Ther 31: 173-179.
30.� Hackney ME, Earhart GM (2008) Tai Chi improves balance and mobility in people with Parkinson disease. Gait Posture 28: 456-460.
31.� Canning CG, Alison JA, Allen NE, Groeller H (1997) Parkinson’s disease: an investigation of exercise capacity, respiratory function, and gait. Arch Phys Med Rehabil 78: 199-207.
32.� Reuter I, Mehnert S, Leone P, Kaps M, Oechsner M, et al. (2011) Effects of a flexibility and relaxation programme, walking, and nordic walking on Parkinson’s disease. J Aging Res 2011: 232473.
2011;17:1-8
15.� Lazaridou A, Philbrook P, Tzika AA. Yoga and mindfulness as therapeutic interventions for stroke rehabilitation: a s y s t e m a t i c r e v i e w. E v i d B a s e d C o m p l e m e n t A l t e r n a t M e d 2013;2013:357108.
16.� Schmid AA, Van Puymbroeck M, Altenburger PA, et al. Post-stroke balance improves with yoga: a pilot study. Stroke 2012;43(9):2402–7.
17.� Schmid AA, Miller KK, Van Puymbroeck M, et al. Yoga leads to multiple physical improvements after stroke, a pilot study. C o m p l e m e n t T h e r M e d 2014;22(6):994–1000.
18.� Garrett R, Immink MA, Hillier S. B e c o m i n g c o n n e c t e d : t h e l i v e d experience of yoga participation after s t r o k e . D i s a b i l R e h a b i l 2011;33(25–26):2404–15.
19.� Desveaux L, Lee A, Goldstein R, et al. Yoga in the management of chronic disease: a systematic review and meta-analysis. Med Care 2015;53(7):653–61.
20.� Chan W, Immink MA, Hillier S. Yoga and exercise for symptoms of depression and anxiety in people with poststroke disability: a randomized, controlled pilot t r i a l . A l t e r n T h e r H e a l t h M e d 2012;18(3):34–43.
21.� Mohapatra B, Marshall RS, Laures-Gore J. Yogic breathing and Ayurveda in aphasia: a case study. Top Stroke Rehabil 2014;21(3):272–9
22.� Lewy body dementia Association (800) 539-9767. www.parkinson.org
23.� Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL (2008) The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 23: 631-640.
24.� Exercise and Nutrition, meditation,
52Haryana Medical Journal - March 2020, Vol. 43, Issue 01 53Haryana Medical Journal - March 2020, Vol. 43, Issue 01
2018;5(1):1-10.
3.� Neurological disorders: public heath challenges. World health organisation. ISBN 92 4 156336 2 (NLM classifi cation: WL 140) ISBN 978 92 4 156336 9
4.� Siuly S and Zhang Y. Medical Big Data: Neurological Diseases Diagnosis Through Medical Data Analysis. Data Science and Engineering 2016; 1(2):54-64.
5.� Gray JT and Gravin CM. Assessment and management of neurological problems. Emerg Med J 2005; 22:440–445.
6.� Definition of physical therapy: Merriam Webster, updated on June 8th, 2018.
7.� Guide to physical therapy practice, 682 (American Physical Therapy Association, 2nd ed. 2003).
8.� Amrit B & Mantu P. Recent advancement in the field of Physiotherapy. June, 2012.
9.� Mooventhan A and Nivethitha L. Evidence based effects of yoga in neurological disorders. Journal of clinical neuroscience 2017:1-7.
10.� Taylor CB, Sallis JF, Needle R: The Relation of physical activity and exercise to mental health. Public Health Rep 1985;100:195-202
11.� Eas ton JD, Hauser S , Mar t in J . Cerebrovascular disease. Harrison’s Principles of Internal Medicine, New York: McGraw-Hill Publisher,2001
12.� World health organization . stroke 1989. Recommendation on stroke prevention and diagnosis and therapy. Report of WHO. Task force on stroke and other cerebrovascular disorders. Stroke. 20:1407-31.
13.� Mishra SK, Singh P, Bunch SJ, et al. The therapeutic value of yoga in neurological disorders. Ann Indian Acad Neurol 2012;15(4):247–54
14.� Field T. Yoga clinical research review. Compliment Therapy Clinical Practice.
overall quality of life.
� Research demonstrated improvements in cardiovascular parameters with a various meditation program. There are significant reductions in resting systolic blood pressure (BP) in adolescents with high normal BP. A reduction in reactivity of BP, heart rate, and cardiac output to simulated stressors reflects the beneficial effects of yoga at rest and during stressful states. The practice of yoga is also a s s o c i a t e d w i t h s o m e p r o f o u n d biochemical changes. There is a great potential for specific yoga programs to be u s e d i n t h e r e h a b i l i t a t i o n o f musculoskeletal injuries and neurological disorders to maintain muscle tone. (85)
� Evidence showed that yoga and various therapeutic exercises are effective in neurological disorders like epilepsy, migraine, multiple sclerosis, stroke, Parkinson’s disease, peripheral nervous system diseases and many more.(86)
Conclusion
� Based on the available literature, it could be concluded that physiotherapy and yoga both are considered as an effective adjuvant therapy for the patients with various neurological disorders including stroke, Parkinson’s disease, multiple sclerosis, epilepsy, Alzheimer’s disease, d e m e n t i a , h e a d a c h e , m i g r a i n e , neuropathies and so on.
References :
1.� The Types of Neurological Conditions and Physiotherapy Used. Available at http://ThePhysioSite.com. Accessed February 24, 2009.
2.� Rizk MZ, Fouad GI and Aly HF. Neurological disorders: causes and treatment strategies. International journal of mental health and neurosciences
58.� Fisher MA, Langbein WE, Collins EG et al. . Physiological improvement with moderate exercise in type II diabetic n e u r o p a t h y. E l e c t r o m y o g r C l i n Neurophysiol. 2007;47:23–28. [PubMed] [Google Scholar]
59.� Dixit S, Maiya AG, Shastry BA. Effect of aerobic exercise on peripheral nerve functions of population with diabetic peripheral neuropathy in type 2 diabetes: a single blind, parallel group randomized c o n t r o l l e d t r i a l . J D i a b e t e s Complications. 2014;28:332–339. [PubMed] [Google Scholar]
60.� Lee K, Lee S, Song C. Whole-body vibration training improves balance, muscle strength and glycosylated hemoglobin in elderly patients with diabetic neuropathy. Tohoku J Exp Med. 2013;231:305–314. [PubMed] [Google Scholar]
61.� Hung JW, Liou CW, Wang PW et al. . Effect of 12-week tai chi chuan exercise on peripheral nerve modulation in patients with type 2 diabetes mellitus. J Rehabi l Med. 2009;41:924–929. [PubMed] [Google Scholar]
62.� Ahn S, Song R. Effects of tai chi exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. J A l t e r n C o m p l e m e n t M e d . 2012;18:1172–1178. [PMC free article] [PubMed] [Google Scholar]
63.� Jung M, Rein M, Fuches B Physical Therapy for Chemotherapy induced Peripheral neuropathy in Pediatric Oncology. Klin Padiatr 2016;228(607): 313-8
64.� Yoga for Alzheimer’s Disease: Provide strength to brain nerves and Boost ability to perform daily tasks with Therapeutic Iyengar Yoga & Meditation
65.� McCaffery R, J Park, Newman D et.al. The Effect of Chair Yoga in Older Adults
Comparison of the effect of 8 weeks A e r o b i c a n d Yo g a Tr a i n i n g o n Ambulatory Function, Fatigue and Mood Status in MS Patients. Iran Red Crescent Med J 15: 449-454
51.� Patil NJ, Nagaratna R, Garner C, et al. Effect of integrated yoga on neurogenic bladder dysfunction in patients with multiple sclerosis – a prospective observational case series. Complement Ther Med 2012;20(6):424–30.
52.� Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among the Iranian women with multiple sclerosis: a randomized controlled trial. Afr J Tradit C o m p l e m e n t A l t e r n M e d 2014;11(5):78–82
53.� Pasnoor M, Dimachkie MM, Kluding P, Barohn RJ. Diabetic neuropathy, part 1: overview and symmetric phenotypes. Neurol Clin. 2013;31:425–445. [PMC free article] [PubMed] [Google Scholar]
54.� Mueller MJ, Minor SD, Sahrmann SA et al. . Differences in the gait characteristics of patients with diabetes and peripheral neuropathy compared with age-matched controls. Phys Ther. 1994;74:299–308. [PubMed] [Google Scholar]
55.� Simoneau GG, Ulbrecht JS, Derr JA et al. . Postural instability in patients with diabetic sensory neuropathy. Diabetes Care. 1994;17:1411–1421. [PubMed] [Google Scholar]
56.� Yoo M, D’Silva LJ, Martin K et al. . Pilot study of exercise therapy on painful diabetic peripheral neuropathy. Pain Med. 2015;16:1482–1489. [PMC free article] [PubMed] [Google Scholar]
57.� Kluding PM, Pasnoor M, Singh R et al. . Safety of aerobic exercise in people with diabetic peripheral neuropathy: single-g roup c l in ica l t r i a l . Phys Ther. 2015;95:223–234. [PMC free article] [PubMed] [Google Scholar]
54Haryana Medical Journal - March 2020, Vol. 43, Issue 01 55Haryana Medical Journal - March 2020, Vol. 43, Issue 01
on gait in the elderly: an exploratory study. Arch Phys Med Rehabil 86: 1830-1837.
42.� Bastille JV, Gill-Body KM (2004) A yoga-based exercise program for people with chronic poststroke hemiparesis. Phys Ther 84: 33-48.
43.� Winterholler M, Erbguth F, Neundorfer B (1997). The use of alternative medicine by multiple sclerosis patients- patient characteristics and patterens of use. FortschrNeurolPsychaitr 65: 555-561
44.� Rogers KA, MacDonald M. Therapeutic yoga: symptom management for multiple sclerosis. J Altern Complement Med 2015;21(11):655–9.
45.� Ahmadi A, Arastoo AA, Nikbakht M, et al. Comparison of the effect of 8 weeks aerobic and yoga training on ambulatory function, fatigue and mood status in ms patients. Iran Red Crescent Med J 2013;15(6):449–54.
46.� Hassanpour-Dehkordi A, Jivad N. Comparison of regular aerobic and yoga on the quality of life in patients with multiple sclerosis. Med J Islam Repub Iran 2014;28:141.
47.� Guner S, Inanici F. Yoga therapy and ambulatory multiple sclerosis assessment of gait analysis parameters, fatigue and balance. Bodyw Mov Ther 2015;19 (1):72–81.
48.� Chobe S, Bhargav H, Raghuram N, et al. Effect of integrated yoga and physical therapy on audiovisual reaction time, anxiety and depression in patients with chronic multiple sclerosis: a pilot study. J Complement Integr Med 2016;13 (3):301–9.
49.� Senders A, Wahbeh H, Spain R, et al. Mind-body medicine for multiple s c l e r o s i s : a s y s t e m a t i c r e v i e w. Autoimmune Dis 2012;2012:567324.
50.� Ahmadi A,Arastoo AA, Nikbakht M, Zahednejad S, RajabpourM (2013)
33.� Stankovic I (2004) The effect of physical therapy on balance of patients with Parkinson’s disease. Int J Rehabil Res 27: 53-57.
34.� Bergen JL, Toole T, Elliott RG, 3rd, Wallace B, Robinson K, et al. (2002) Aerobic exercise intervention improves aerobic capacity and movement initiation in Park inson’s d i sease pa t ien ts . NeuroRehabilitation 17: 161-168.
35.� Sunvisson H, Lokk J, Ericson K, Winblad B, Ekman SL (1997) Changes in motor performance in persons with Parkinson’s disease after exercise in a mountain area. J Neurosci Nurs 29: 255-260.
36.� Brichetto G, Pelosin E, Marchese R, Abbruzzese G (2006) Evaluation of physical therapy in parkinsonian patients with freezing of gait: a pilot study. Clin Rehabil 20: 31-35.
37.� Kuroda K, Tatara K, Takatorige T, Shinsho F (1992) Effect of physical exercise on mortality in patients with Parkinson’s disease. Acta Neurol Scand 86: 55-59.
38.� Jacobs BP, Mehling W, Avins AL, Goldberg HA, Acree M, et al. (2004) Feasibility of conducting a clinical trial on Hatha yoga for chronic low back pain: methodological lessons. Altern Ther Health Med 10: 80-83.
39.� Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, et al. (2004) Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 62: 2058-2064.
40.� Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, et al. (2006) Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med 12: 40-47.
41.� DiBenedetto M, Innes KE, Taylor AG, Rodeheaver PF, Boxer JA, et al. (2005) Effect of a gentle Iyengar yoga program
58.� Fisher MA, Langbein WE, Collins EG et al. . Physiological improvement with moderate exercise in type II diabetic n e u r o p a t h y. E l e c t r o m y o g r C l i n Neurophysiol. 2007;47:23–28. [PubMed] [Google Scholar]
59.� Dixit S, Maiya AG, Shastry BA. Effect of aerobic exercise on peripheral nerve functions of population with diabetic peripheral neuropathy in type 2 diabetes: a single blind, parallel group randomized c o n t r o l l e d t r i a l . J D i a b e t e s Complications. 2014;28:332–339. [PubMed] [Google Scholar]
60.� Lee K, Lee S, Song C. Whole-body vibration training improves balance, muscle strength and glycosylated hemoglobin in elderly patients with diabetic neuropathy. Tohoku J Exp Med. 2013;231:305–314. [PubMed] [Google Scholar]
61.� Hung JW, Liou CW, Wang PW et al. . Effect of 12-week tai chi chuan exercise on peripheral nerve modulation in patients with type 2 diabetes mellitus. J Rehabi l Med. 2009;41:924–929. [PubMed] [Google Scholar]
62.� Ahn S, Song R. Effects of tai chi exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. J A l t e r n C o m p l e m e n t M e d . 2012;18:1172–1178. [PMC free article] [PubMed] [Google Scholar]
63.� Jung M, Rein M, Fuches B Physical Therapy for Chemotherapy induced Peripheral neuropathy in Pediatric Oncology. Klin Padiatr 2016;228(607): 313-8
64.� Yoga for Alzheimer’s Disease: Provide strength to brain nerves and Boost ability to perform daily tasks with Therapeutic Iyengar Yoga & Meditation
65.� McCaffery R, J Park, Newman D et.al. The Effect of Chair Yoga in Older Adults
Comparison of the effect of 8 weeks A e r o b i c a n d Yo g a Tr a i n i n g o n Ambulatory Function, Fatigue and Mood Status in MS Patients. Iran Red Crescent Med J 15: 449-454
51.� Patil NJ, Nagaratna R, Garner C, et al. Effect of integrated yoga on neurogenic bladder dysfunction in patients with multiple sclerosis – a prospective observational case series. Complement Ther Med 2012;20(6):424–30.
52.� Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among the Iranian women with multiple sclerosis: a randomized controlled trial. Afr J Tradit C o m p l e m e n t A l t e r n M e d 2014;11(5):78–82
53.� Pasnoor M, Dimachkie MM, Kluding P, Barohn RJ. Diabetic neuropathy, part 1: overview and symmetric phenotypes. Neurol Clin. 2013;31:425–445. [PMC free article] [PubMed] [Google Scholar]
54.� Mueller MJ, Minor SD, Sahrmann SA et al. . Differences in the gait characteristics of patients with diabetes and peripheral neuropathy compared with age-matched controls. Phys Ther. 1994;74:299–308. [PubMed] [Google Scholar]
55.� Simoneau GG, Ulbrecht JS, Derr JA et al. . Postural instability in patients with diabetic sensory neuropathy. Diabetes Care. 1994;17:1411–1421. [PubMed] [Google Scholar]
56.� Yoo M, D’Silva LJ, Martin K et al. . Pilot study of exercise therapy on painful diabetic peripheral neuropathy. Pain Med. 2015;16:1482–1489. [PMC free article] [PubMed] [Google Scholar]
57.� Kluding PM, Pasnoor M, Singh R et al. . Safety of aerobic exercise in people with diabetic peripheral neuropathy: single-g roup c l in ica l t r i a l . Phys Ther. 2015;95:223–234. [PMC free article] [PubMed] [Google Scholar]
54Haryana Medical Journal - March 2020, Vol. 43, Issue 01 55Haryana Medical Journal - March 2020, Vol. 43, Issue 01
on gait in the elderly: an exploratory study. Arch Phys Med Rehabil 86: 1830-1837.
42.� Bastille JV, Gill-Body KM (2004) A yoga-based exercise program for people with chronic poststroke hemiparesis. Phys Ther 84: 33-48.
43.� Winterholler M, Erbguth F, Neundorfer B (1997). The use of alternative medicine by multiple sclerosis patients- patient characteristics and patterens of use. FortschrNeurolPsychaitr 65: 555-561
44.� Rogers KA, MacDonald M. Therapeutic yoga: symptom management for multiple sclerosis. J Altern Complement Med 2015;21(11):655–9.
45.� Ahmadi A, Arastoo AA, Nikbakht M, et al. Comparison of the effect of 8 weeks aerobic and yoga training on ambulatory function, fatigue and mood status in ms patients. Iran Red Crescent Med J 2013;15(6):449–54.
46.� Hassanpour-Dehkordi A, Jivad N. Comparison of regular aerobic and yoga on the quality of life in patients with multiple sclerosis. Med J Islam Repub Iran 2014;28:141.
47.� Guner S, Inanici F. Yoga therapy and ambulatory multiple sclerosis assessment of gait analysis parameters, fatigue and balance. Bodyw Mov Ther 2015;19 (1):72–81.
48.� Chobe S, Bhargav H, Raghuram N, et al. Effect of integrated yoga and physical therapy on audiovisual reaction time, anxiety and depression in patients with chronic multiple sclerosis: a pilot study. J Complement Integr Med 2016;13 (3):301–9.
49.� Senders A, Wahbeh H, Spain R, et al. Mind-body medicine for multiple s c l e r o s i s : a s y s t e m a t i c r e v i e w. Autoimmune Dis 2012;2012:567324.
50.� Ahmadi A,Arastoo AA, Nikbakht M, Zahednejad S, RajabpourM (2013)
33.� Stankovic I (2004) The effect of physical therapy on balance of patients with Parkinson’s disease. Int J Rehabil Res 27: 53-57.
34.� Bergen JL, Toole T, Elliott RG, 3rd, Wallace B, Robinson K, et al. (2002) Aerobic exercise intervention improves aerobic capacity and movement initiation in Park inson’s d i sease pa t ien ts . NeuroRehabilitation 17: 161-168.
35.� Sunvisson H, Lokk J, Ericson K, Winblad B, Ekman SL (1997) Changes in motor performance in persons with Parkinson’s disease after exercise in a mountain area. J Neurosci Nurs 29: 255-260.
36.� Brichetto G, Pelosin E, Marchese R, Abbruzzese G (2006) Evaluation of physical therapy in parkinsonian patients with freezing of gait: a pilot study. Clin Rehabil 20: 31-35.
37.� Kuroda K, Tatara K, Takatorige T, Shinsho F (1992) Effect of physical exercise on mortality in patients with Parkinson’s disease. Acta Neurol Scand 86: 55-59.
38.� Jacobs BP, Mehling W, Avins AL, Goldberg HA, Acree M, et al. (2004) Feasibility of conducting a clinical trial on Hatha yoga for chronic low back pain: methodological lessons. Altern Ther Health Med 10: 80-83.
39.� Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, et al. (2004) Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 62: 2058-2064.
40.� Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, et al. (2006) Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med 12: 40-47.
41.� DiBenedetto M, Innes KE, Taylor AG, Rodeheaver PF, Boxer JA, et al. (2005) Effect of a gentle Iyengar yoga program
56Haryana Medical Journal - March 2020, Vol. 43, Issue 01 57Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Research Foundation, No.9 Appajappa Agrahara, Chamarajpet, Bangalore-560018)
79.� Krishna Bhat Dr., post graduate class notes on the topic “ Basic principles of Yoga therapy”
80.� Headache classification subcommittee of the international headache society. The international classification of headache
nddisorder : 2 Edition. Cephalgia 2004;24 suppl 1:9-160
81.� Tekur P, Singphow C,Nagendra HR, Raghuram N. effects of short term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain : A Randomized Controlled study. J Altern compliment Med 2008;14:637-44
82.� Andrea –Rice: Attention Migraine Sufferers: New Study Finds Yoga an Effective Form of Treatment
83.� Carmeli E. Physical Therapy for Neurological Conditions in Geriatric Populations. Front Public Health 2017; 5:333
84.� H e l l w e g S . E f f e c t i v e n e s s o f Physiotherapy and Occupational Therapy after Traumatic Brain Injury in the Intensive Care Unit. Critical Care Research and Practice 2012: 1-5
85.� M
86.� Mishra SK, Singh P, Bunch SJ and Zhang R. The therapeutic value of yoga in neurological disorders. Annals of Indian Academy of Neurology 2012;15(4):247-254.
87.� Mooventhan, A., & Nivethitha, L. (2017). Evidence based effects of yoga in neurological disorders. Journal of Clinical Neuroscience, 43, 61–67.
with Moderate and Severe Alzheimer’s Disease. Res Gerontol Nurs 2014:7 (4): 171-7
66.� Waelde LC, Thompson I, Gallagher-Thompson D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J Clin psychol 2004:60 (6): 677-87
67.� Yoga therapy for epilepsy : Asana Andiappan collage of yoga and research centre.
68.� Rajesh B, Jayachandran D, Mohandas G et. Al. a pilot study of yoga and meditation for patients with medically refractory epilepsy. J Altern, compliment Med 2006;12(4): 367-71
69.� Satyaprabha TN, Satishchandra P et. al. A modulation of cardiac autonomic balance with adjuvant yoga therapy in patients with refractory epilepsy. Epilepsy Rehab 2008;12(2):245-52
70.� h t tp : / /www.dr tba lu . com/ f ron ta l -sinus.html accessed on 22/02/2013.
71.� Hodder Arnold (JAYPEE). Diseases of the Nose, throat and Ear, 1st ed. New Delh i : Jaypee Brothers Medica l Publishers (P) Ltd;2007,47.
72.� Bhavanani AB. Scientific Basis for some Yoga practices in sinusitis 2013,157.
73.� Wankhede SD. Effect of Shuddhikriya- Jalaneti in chronic sinusitis with special reference to JeernaPratishaya 2017.
74.� https://yourstory.com/2017/06/heal- sinusitis-yoga
75. literature.awgp.org/akhandjyoti/2010/sep_oct/v1.9
76.� https://www.stylecraze.com/articles /yoga-for-sinusitis
77.� www.indianmirror.com
78.� Shirley Telles et.al., research paper, “Breathing through a particular nostril can alter metabolism and autonomic activities”, Vivekananda Kendra Yoga
Address of CorrespondenceDr Shilpa MehtaVK Neurocare &
Trauma Research HospitalN-159, Model Town, Hisar
56Haryana Medical Journal - March 2020, Vol. 43, Issue 01 57Haryana Medical Journal - March 2020, Vol. 43, Issue 01
Research Foundation, No.9 Appajappa Agrahara, Chamarajpet, Bangalore-560018)
79.� Krishna Bhat Dr., post graduate class notes on the topic “ Basic principles of Yoga therapy”
80.� Headache classification subcommittee of the international headache society. The international classification of headache
nddisorder : 2 Edition. Cephalgia 2004;24 suppl 1:9-160
81.� Tekur P, Singphow C,Nagendra HR, Raghuram N. effects of short term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain : A Randomized Controlled study. J Altern compliment Med 2008;14:637-44
82.� Andrea –Rice: Attention Migraine Sufferers: New Study Finds Yoga an Effective Form of Treatment
83.� Carmeli E. Physical Therapy for Neurological Conditions in Geriatric Populations. Front Public Health 2017; 5:333
84.� H e l l w e g S . E f f e c t i v e n e s s o f Physiotherapy and Occupational Therapy after Traumatic Brain Injury in the Intensive Care Unit. Critical Care Research and Practice 2012: 1-5
85.� M
86.� Mishra SK, Singh P, Bunch SJ and Zhang R. The therapeutic value of yoga in neurological disorders. Annals of Indian Academy of Neurology 2012;15(4):247-254.
87.� Mooventhan, A., & Nivethitha, L. (2017). Evidence based effects of yoga in neurological disorders. Journal of Clinical Neuroscience, 43, 61–67.
with Moderate and Severe Alzheimer’s Disease. Res Gerontol Nurs 2014:7 (4): 171-7
66.� Waelde LC, Thompson I, Gallagher-Thompson D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J Clin psychol 2004:60 (6): 677-87
67.� Yoga therapy for epilepsy : Asana Andiappan collage of yoga and research centre.
68.� Rajesh B, Jayachandran D, Mohandas G et. Al. a pilot study of yoga and meditation for patients with medically refractory epilepsy. J Altern, compliment Med 2006;12(4): 367-71
69.� Satyaprabha TN, Satishchandra P et. al. A modulation of cardiac autonomic balance with adjuvant yoga therapy in patients with refractory epilepsy. Epilepsy Rehab 2008;12(2):245-52
70.� h t tp : / /www.dr tba lu . com/ f ron ta l -sinus.html accessed on 22/02/2013.
71.� Hodder Arnold (JAYPEE). Diseases of the Nose, throat and Ear, 1st ed. New Delh i : Jaypee Brothers Medica l Publishers (P) Ltd;2007,47.
72.� Bhavanani AB. Scientific Basis for some Yoga practices in sinusitis 2013,157.
73.� Wankhede SD. Effect of Shuddhikriya- Jalaneti in chronic sinusitis with special reference to JeernaPratishaya 2017.
74.� https://yourstory.com/2017/06/heal- sinusitis-yoga
75. literature.awgp.org/akhandjyoti/2010/sep_oct/v1.9
76.� https://www.stylecraze.com/articles /yoga-for-sinusitis
77.� www.indianmirror.com
78.� Shirley Telles et.al., research paper, “Breathing through a particular nostril can alter metabolism and autonomic activities”, Vivekananda Kendra Yoga
Address of CorrespondenceDr Shilpa MehtaVK Neurocare &
Trauma Research HospitalN-159, Model Town, Hisar
58Haryana Medical Journal - March 2020, Vol. 43, Issue 01 59Haryana Medical Journal - March 2020, Vol. 43, Issue 01
58Haryana Medical Journal - March 2020, Vol. 43, Issue 01 59Haryana Medical Journal - March 2020, Vol. 43, Issue 01