Differential N-Glycosylation Patterns in Lung ... - eScholarship.org
Glycosylation as a marker for inflammatory arthritis
Transcript of Glycosylation as a marker for inflammatory arthritis
Cancer Biomarkers 14 (2014) 17–28 17DOI 10.3233/CBM-130373IOS Press
Glycosylation as a marker for inflammatoryarthritis
Simone Albrechta, Louise Unwina, Mohankumar Muniyappaa,b and Pauline M. Ruddc,∗aNIBRT Complete Process and Product Characterisation Group, National Institute for Bioprocessing, Researchand Training, Dublin, IrelandbVeterinary Sciences Centre, University College Dublin, Dublin, IrelandcConway Institute of Biomolecular and Biomedical Science, University College Dublin, Dublin, Ireland
Abstract. Changes in serum protein glycosylation play an important role in inflammatory arthritis. Altered galactosylation ofimmunoglobulin G (IgG) in rheumatoid arthritis attracts special attention due to the devastating nature of the disease. Studyingglycosylation changes of serum proteins has been recognized as a potential strategy to provide added value regarding diagnostics,aetiopathology and therapy of inflammatory arthritic diseases. Key questions, which are approached in these fields of research,are whether or not glycosylation can be used as a complementary pre-clinical and clinical marker for disease differentiation,diagnosis, the prediction of disease course and severity as well as for the evaluation of disease therapies. These studies mainlyfocus on TNF antagonists, which present a new and promising way of treating inflammatory arthritis. The recent availability ofnew high-throughput glycoanalytical tools enables a more profound and efficient investigation in large patient cohorts and helpsto gain new insights in the complex mechanism of the underlying disease pathways.
Keywords: Inflammatory arthritis, serum protein glycosylation, diagnostics, aetiopathology, therapy
1. Introduction
Glycans are one of the key fundamental classes ofmolecules which are important for maintaining nor-mal cellular activity, such as immunogenicity and celladhesion [1,2]. Glycosylation is an important post-translational modification which has a significant influ-ence on the biological functioning of proteins. A largevariety of glycoproteins are present in human serum asthese are key components of the native and adaptiveimmune system [3]. Immunoglobulins (Ig) are impor-tant products of the humoral immune response and canbe divided into five classes (IgG, IgM, IgA, IgE andIgD). Immunoglobulins are heavily glycosylated withN-linked glycosylation sites located in the Fc and Fabregion of the molecules [4].
∗Corresponding author: Pauline M. Rudd, Conway Institute ofBiomolecular and Biomedical Science, University College Dublin,Belfield, Dublin 4, Ireland. Tel.: +353 12158 142; Fax: +353 12158116; E-mail: [email protected].
Protein glycosylation is not genetically determinedbut depends on the presence and activity of glycosi-dases and glycosyltransferases in the respective cell.Alteration in physiological cirumstances, such as dis-ease, can therefore have a significant influence on gly-cosylation and biological functioning of proteins andmay lead to an inflammatory response of the humoralimmune system [5–8].
Inflammatory arthritic diseases are autoimmune dis-orders in which the host immune system self-invadesthe host defence mechanism, resulting in a gradual de-generation of the normal immune response and thus in-flammation. Rheumatoid arthritis (RA), juvenile idio-pathic arthritis (JIA), juvenile chronic arthritis (JCA),psoriatic arthritis (PsA) and ankylosing spondylitis(AS) are typical inflammatory arthritic diseases. RAis a major inflammatory disorder with 0.5–1% of theworld population suffering from RA. The name RAwas first introduced in the 1850’s [9,10] and describesa disease of severe devastating nature. Synovial jointsare the primary site of attack in RA [11,12], result-
ISSN 1574-0153/14/$27.50 c© 2014 – IOS Press and the authors. All rights reserved
18 S. Albrecht et al. / Glycosylation in inflammatory arthritis
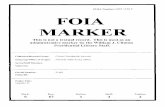
Fig. 1. Typical HILIC-HPLC profile of the serum N-glycome from an RA-patient in which > 130 glycans have been identified, includingmonosaccharide sequences and linkage information [15]. Some of the major structures are shown and abbreviated according to Harvey et al. [128].The increased level of peak 1 (FA2) indicates elevated agalactosylation (G0) which is characteristic for RA.
ing in inevitable joint pain as well as irreversiblejoint destruction. An early diagnosis is necessary inorder to minimize joint damage but requires com-plementary and disease-specific biomarkers. Changesin serum protein glycosylation during inflammatoryarthritic disorders have been extensively studied andpresent an interesting and promising basis for the diag-nosis, aetiopathology and therapy of the diseases.
2. Recent advances in glycan analysis
Studying serum protein glycosylation is a challeng-ing analytical task. A typical N-glycan profile for anRA patient, which shows the structural complexityof the N-glycan structures from serum glycoproteins,is shown in Fig. 1. HILIC-HPLC and HILIC-UPLC(hydrophilic-interaction high- and ultra-performanceliquid chromatography) with fluorescence detectionare commonly used for the analysis of N-glycans [13,14]. The use of UPLC for HILIC separation providesincreased resolution and reduced analysis time com-pared to HPLC and has recently been facilitated bythe introduction of ethylene bridged hybrid (BEH)
based stationary phases with particle sizes of merely1.7 μm [13].
2.1. High-throughput glycan release and fluorescentlabelling for HILIC-HPLC analysis
Prior to analysis, N-glycans are typically releasedfrom glycoproteins using enzymatic digestion.PNGase F (peptide N-glycosidase F) releases all mam-malian N-linked glycans and cleaves between the coreN-acetyl glucosamine (GlcNAc) of the glycan struc-ture and the asparagine residue of the protein. The re-leased glycans are subsequently labelled with a fluo-rescent label, such as 2-aminobenzamide (2-AB) [15].Glycan release and fluorescent labelling are tediousand time-consuming tasks. Thus, a high-throughput96-plate format method for glycan release and la-belling from total serum has been developed which sig-nificantly improves the efficiency of sample prepara-tion [15,16]. Additionally, the possibility to use totalserum or plasma for N-glycan profiling provides ad-vanced information on the whole profile of glycanspresent on serum proteins. Likewise, a novel 96-well
S. Albrecht et al. / Glycosylation in inflammatory arthritis 19
Table 1Glycosylation changes in acute phase proteins (APPs) in response to acute and chronic inflammation and inflammatory diseases
Glycoprotein Inflammation induced glycosylation change Inflammatory disease Referenceα-1-acid glycoprotein (AGP) increased expression of sLex Acute inflammation [117]
increases in biantennary structures and α1,3 fucosylation Acute inflammation [118]increases in tri- and tetra-antennary α1,3 fucosylation Chronic inflammation [118]increased expression of sLex Severe trauma and RA [119]increased fucosylation RA [120]increased levels of glucosamine, galactose and mannose RA [121]increased sialylation [47]increase in outer arm α1,3 fucosylation and increase inbranching (tetra-antennary structures)
Chronic pancreatitis and pan-creatic cancer
[122]
decrease in biantennary stuctures Chronic pancreatitis [122]
α1-Antichymotrypsin (ACT) increased expression of sLex Severe trauma and RA [119]
α-2-Macroglobulin (AMG) change in glycosylation reflected by an increase in reac-tivity to Concanavalin A
SLE, scleroderma, mixed con-nective tissue disorder, RA
[123]
change in glycosylation reflected by an increase in reac-tivity to Concanavalin A, observed increase in concentra-tions of galactose and mannose
SLE [36]
change in glycosylation reflected by an increase in reac-tivity to Concanavalin A
SS [123]
Haptoglobin (HAP) change in glycosylation reflected by an increase in reac-tivity to Concanavalin A
SLE, scleroderma, RA, SS [123]
increased fucosylation RA [48]increased expression of sLex Severe trauma and RA [119]reduction in mannosylation RA [121]increased expression of sLex Crohn’s disease [124]increase in outer arm α1,3 fucosylation and decrease inbi-antennary structures
Chronic pancreatitis [122]
increase in branching (tetra-antennary structures) Chronic pancreatitis and pan-creatic cancer
[122]
Fetuin (FET) increase in outer arm α1,3 fucosylation (sLex) and in-crease in branching (tri- and tetra-antennary structures)
Chronic pancreatitis [122]
Transferrin (TFN) increased branching RA [125]increased branching and sialylation Ulcerative colitis [126]increased core fucosylation and outer arm α1,3 fucosy-lation sLex, bisected structures, decrease in biantennarystructures
Chronic pancreatitis [122]
decrease in sialylation Sepsis (first 2 days) [127]
protein G monolith plate was recently developed andused to isolate immunoglobulin G (IgG) from plasmaof 2298 individuals for subsequent N-glycan analy-sis [17].
2.2. Advanced structural characterization of glycans
The use of mass spectrometry (MS) offers advancedstructural elucidation by mass fragmentation. Matrix-assisted laser desorption ionisation (MALDI) or elec-trospray ionisation (ESI) with quadrupole or time-of-flight (TOF) mass analysers are MS techniques com-monly used for glycan analysis [18,19] and can ei-ther be used as a stand-alone technique or in-line withHPLC or UPLC with fluorescent detection [20].
Exoglycosidase sequencing of fluorescently labelledglycans and structural assignment by database search-
ing are supplementary strategies which allow an effi-cient and detailed characterisation of the monosaccha-ride sequences and linkages of glycans [15]. The exten-sion of recently established databases such as EURO-CarbDB (http://www.ebi.ac.uk/eurocarb/home.action)and GlycoBase (http://glycobase.nibrt.ie) is currentlyin progress [21,22].
2.3. Other analytical tools for glycan analysis
The use of analytical techniques for the characteri-zation of glycans has been vastly reviewed [23,24]. Be-sides HILIC, stationary phases based on porous graphi-tized carbon (PGC) are commonly used for glycananalysis by HPLC and UPLC [25]. Other frequentlyused analytical techniques are capillary electrophoresis(CE) or CE-MS [26] as well as lectin affinity assays.
20 S. Albrecht et al. / Glycosylation in inflammatory arthritis
Lectin affinity assays are useful for the identificationof many glycosylation-lectin binding interactions in asingle sample [27] and do not require high-end analyt-ical equipment.
3. Serum protein glycosylation in inflammatorydiseases
Altered glycosylation of key serum glycoproteinshas been extensively studied over the years, includingimmunoglobulin G (IgG) [8,28], immunoglobulin A(IgA) [29] and acute phase proteins (APPs) such asα-1acid glycoprotein (AGP) [30], haptoglobin (HAP) [31,32], transferrin (TFN) [33–35], α-2 macroglobulin(AMG) [36] and C-reactive protein (CRP) [37,38].
IgG is one of the most abundant proteins in serum,with concentrations ranging from 4–16 mg/ml. N-glycans attached to Asn-297 in each of the CH2 do-mains of the Fc regions are a nested set of 36 com-plex bi-antennary structures. Effector functions of IgG,such as cytokine release, are mediated through Fc re-ceptors and can be modulated by the N-glycans at-tached to the Fc domain of the molecule [24,39].
Changes in IgG glycosylation, such as alterationsin bisecting GlcNAc, core fucose, terminal sialic acidand galactosylation level (G0, G1, G2; peaks 1, 3and 4/5 in Fig. 1, respectively) have been related toa number of diseases including infection and auto-immunity [4]. Significantly, a decrease in galactosy-lation has been observed for patients with inflamma-tory disorders, such as Crohn’s disease, systemic lu-pus erythemathous (SLE), anti-neutrophil cytoplasmicantibody (ANCA)-associated systemic vasculitis andmyositis [40–42]. Increased levels of agalactosylatedIgG (IgG-G0) and a significant decrease in IgG sialyla-tion has also been observed in the serum IgG N-glycanprofiles from patients of gastric, lung and ovarian can-cer [43–45].
APPs are serum proteins expressed and secreted bythe hepatocyte cells of the liver in response to inflam-matory stimuli. This process can be described as anacute phase response. Positive APPs, such as AGP,CRP and HAP show increased plasma concentrationduring inflammation whereas negative APPs, which in-clude TFN and albumin show decreased plasma con-centration. Several APPs include glycoproteins and al-terations in glycan structures during acute and chronicinflammation have been reported [46]. Examples ofAPPs and their respective inflammation-associatedglycosylation changes are described in Table 1. Hyper-
sialylation, branching and glycans enriched in SialylLewisx (SLex) epitopes (which are α1,3 fucosylatedon their outer arms) are typical characteristics for APPssuch AGP and HAP during inflammation [32,47,48].Furthermore, the glycan profiles of many APPs havebeen demonstrated to be altered in the presence of tu-mours as described by Dempsey et al. [49].
4. Serum protein glycosylation in inflammatoryarthritis
The glycosylation status of serum proteins plays anessential role in the pathology of inflammatory arthri-tis. IgG glycosylation in RA showed to be of specialimportance. Aglycosylated IgG obtained by treatmentof the glycoprotein with endo-β-N-acetylglucosamini-dase inhibited the induction of arthritis in (BALB/c xB10,Q) F1 mice and was correlated to the reduced IgGbinding to Fc receptors and the hindrance in formingstable immune complexes [39]. Similar results, whichpointed out the impact of protein glycosylation on thepro-inflammatory response were obtained by studyingthe response of aglycosylated IgG in murine autoim-mune model systems [50]. Studying serum protein gly-cosylation has therefore been recognized as a potentialstrategy to provide added value regarding aetiopathol-ogy and therapy of inflammatory arthritis and to gaininsight into the underlying biochemical disease path-way.
4.1. The role of IgG glycosylation in diseasepathogenicity
Modifications of IgG glycosylation were first re-ported by Parekh et al. in 1985 where significantlydecreased levels of galactosylation were observed insamples obtained from RA patients [51]. ReducedIgG galactosylation has also been observed in otherarthritis-related diseases, for example SLE [42,52].Truncated IgG glycans result in antigenicity and causean altered immune response of these antibodies, as hasextensively been reviewed by Alavi et al. and Gorniket al. [53–55]. These IgGs can bind to and trigger theproduction of autoantibodies [56], bind to pathogenicrheumatoid factor (Rf) [57,58] and are prone to formimmune complexes [59,60]. Hypogalactosylated IgGinteracts with lectin-like molecules, such as mannose-binding protein, which activates a complement path-way leading to inflammatory response [61,62]. Agalac-tosylation of IgG also implicates a lack of sialyla-
S. Albrecht et al. / Glycosylation in inflammatory arthritis 21
tion. The absence of sialic acid effects an enhanced in-flammatory response [63]. IgG-G0 structures showedincreased core-fucosylation [55,64]. Changes in IgGcore-fucosylation may lead to an altered antibody-dependent cellular cytotoxicity (ADCC) [65,66].
4.2. Disease diagnostics
Early diagnosis and initiation of disease modify-ing therapy can minimize irreversible joint destructionin RA [67]. A disease-specific prognosis is thus re-quired before disease onset. Clinical diagnosis of RAis based on standardised classification criteria as set upby the American College of Rheumatology and the Eu-ropean League against Rheumatism [68]. The diagno-sis is mainly based on serological tests for rheumaticfactor (Rf) and anti-citrullinated protein antibodies(ACPAs). Rf and ACPAs are autoantibodies which canbe present in serum long before onset of clinical symp-toms in RA [69]. However, merely 70% of RA patientshave positive Rf and/or ACPA titers [70,71]. PositiveRf serum titers can also result from other diseases (e.g.Sjoegren’s Syndrom (SS)) or occur in healthy individ-uals. The specificity of Rf and ACPA for RA is approx.80–90% and 95–97% respectively [70,71]. Thus, thesensitivity and selectivity of Rf- and ACPA in the di-agnosis of RA is rather low and additional biomarkersare required.
The determination of altered IgG-G0/G1 levels pre-sents an attractive diagnostic way to predict RA in anearly stage. Increased IgG-G0 levels are characteristicfor RA and were found to be present in serum longbefore disease onset [64,72,73]. The ratio of serumG0/G1 levels in RA patients can be significantly dis-tinguished from healthy individuals up to 3.5 years be-fore disease onset [72]. Combined with Rf titers, thedetermination of serum G0/G1 has a positive predic-tive value of 94% for RA [74]. The determination ofIgG-G0/G1 levels for disease diagnostics has not yetbeen put into routine practice, as this kind of anal-ysis requires high-end analytical equipment such asHPLC/UPLC and mass spectrometry [72]. Alterna-tively, methods are available which do not involve theuse of high-end analytical equipment. Anti-galactosylIgG antibodies in serum can be determined by lectinenzyme immunoassays which results in a specificity of85% for RA [56].
4.2.1. Significance of ACPA glycosylation in RAdiagnostics and pathogenicity
The role of ACPA in RA diagnostics and pathogeni-city has recently gained specific scientific interest. A
positive ACPA titer is connected to a more severe dis-ease course and predicts the development of joint dam-age [75,76]. ACPA is present in serum and to an exces-sive extent in synovial fluids. Rheumatoid synoviumis proposed to be a production site for ACPA [77,78].As RA is a synovial inflammation, ACPA may havea characteristic role in disease pathogenicity and maybe of different quality than ACPA in serum. Addition-ally, ACPA-IgG might be of different quality comparedto the repertoire-IgG from serum. ACPA-IgG can beselectively extracted from serum by preparative chro-matography based on epitope-affinity to a synthetic cit-rullinated peptide (JED) [72]. The method was usedfor studying the glycosylation of serum and ACPA-IgG from ACPA- and IgG-positive patients. A higherlevel of agalactosylation was found for the ACPA-IgGfraction compared to the serum fraction [72]. As well,a positive relation between clinical ACPA-responseand sG0/G1 aberrancy was established, after correc-tion of DAS28-scores, which summarizes clinical pa-rameters such as swollen and tender joints [79]. An ex-tensive study on ACPA glycosylation was performedby Scherer et al. after selective extraction of ACPA-IgG from serum and synovial fluid using commerciallyavailable ELISA plates with covalently attached citrul-linated peptide antigens. ACPA-IgG in synovial fluidshowed to be highly agalactosylated, low in sialyla-tion and highly fucosylated and can be distinguishedfrom ACPA-IgG in serum [78]. This may explain thepresence of synovial immune complexes enriched inIgG-G0 [59,60] and the synovium being the centre ofinflammation in RA [63,80]. For serum, an increasedACPA-IgG-G0 level compared to the repertoire IgG-G0 was found for Rf positive but not for Rf negativepatients. Reduced sialylation of the ACPA-IgG-poolin serum was stated for Rf-positive as well as for Rf-negative patients. Correspondingly, the presence of Rfcould be related to RA exclusively in the presence ofACPA [81] and thus points to an interaction of Rf andACPA. Rf from serum of RA-patients exhibits a highbinding affinity to agalactosylated IgG [57,60]. Thehypothesis stating that G0/G1 aberrancy is predomi-nantly present in the IgG fraction which is synthesizedas a response to autoimmune stimulation is thus rein-forced [72].
4.3. Disease differentiation
The differentiation between different rheumatic dis-eases might be complicated by overlapping clinicalsymptoms. N-glycan profiling of IgG in rheumatic dis-
22 S. Albrecht et al. / Glycosylation in inflammatory arthritis
eases may aid disease differentiation. Three examplesof published data demonstrate that each rheumatic dis-ease is associated with a particular pattern of glyco-sylation. The first study of this type was publishedin 1999 by Watson et al. who set out to determinethe IgG glycosylation variants specific to differentrheumatic diseases. Using HPLC technology, the pro-portions of 16 neutral (galactosylated) and 3 sialylatedN-linked oligosaccharide structures present on IgG insamples obtained from patients suffering from one ofsix different diseases related to inflammatory arthri-tis (RA, JCA, PsA, SLE, AS and SS) were analysed.Unique oligosaccharide associations, i.e. ‘sugar prints’of IgG, specific for each disease group were deter-mined. Essentially, RA and JCA patients had predomi-nantly agalactosyl structures whereas SLE and AS pa-tients had predominantly digalactosyl structures [64].In 2001 Martin et al. used fluorophore linked carbo-hydrate electrophoresis to obtain serum IgG glyco-sylation ‘sugar prints’ and were able to differentiateRA, PsA and AS samples and those from healthy con-trols [82]. A third example, published by Axford etal. in 2003, used high-density electrophoresis to de-termine IgG ‘sugar prints’ mainly focussing on di-,mono- and agalactosylated as well as sialylated gly-cans. Early RA was distinguishable from RA and theseconditions along with six other rheumatic diseases (i.e.PsA, early PsA, AS, SLE, JIA and early undifferen-tiated seronegative arthritis) were differentiated fromosteoarthritis [83].
4.4. Disease activity
Increased levels of agaloctosylated IgG are the hall-mark of RA [64,72,73] and correlate with disease ac-tivity, duration and radiological progression [72,84–87]. Highest IgG-G0 scores were observed for patientswith severe radiological progression, elevated scoresof CRP and swollen and tender joints [72,84,85], aswell as for patients with a long disease history, i.e.15 years [84]. In the case of remission, IgG-G0 scoressimilar to healthy controls were observed for RA andJCA [86,88].
As well, the presence and glycosylation of APPs re-flects disease activity as was discussed in paragraphthree and reviewed by Gornik et al. [55].
4.4.1. Influence of pregnancy on disease activityPregnancy results in a temporary improvement of
RA, followed by a relapse postpartum. For both healthyindividuals as well as RA patients, glycosylation chan-
ges of serum N-glycans were found for the timespre- and postpartum [89–92]. Pregnancy is accompa-nied by an increase in IgG galactosylation and a di-rect decrease after delivery which correlates with dis-ease activity [89,91,92]. Similar results were foundregarding IgG sialylation, but neither an effect onbisecting GalNAc levels nor fucosylation were de-scribed [91,92]. For both, healthy individuals as wellas RA patients in remission, increased branching anddecreased α3-fucosylation of AGP were found duringpregnancy [90]. Alterations on a hormonal level andcytokine-expression may be responsible for changes inglycosyltransferase (GTase) activity and hence serumprotein glycosylation [90,93,94]. Interestingly, RA pa-tients who had negative ACPA and RF titers showedless symptoms during pregnancy [95], highlighting thepossible importance of autoantibody-glycosylation indisease pathogenicity, as previously discussed.
4.5. Disease therapy
Recently, promising biological drugs which tar-get the dysregulated immune-system have emergedin the field of RA therapy. Most widely used arethe tumor necrosis factor (TNF) antagonists adali-mumab (fully humanised monoclonal antibody), inflix-imab (chimeric mouse-human antibody) and etaner-cept (dimeric TNF-receptor-IgG fusion protein). Thetherapeutic mechanism of TNF antagonists is basedon the inhibition of TNF-α-receptor binding, thus, in-terrupting the cell signaling pathway of these pro-inflammatory cytokines [96].
Anti-TNF-α therapy is often combined with chem-ically synthesised disease-modifying anti-rheumaticdrugs (DMARDs), mainly methotrexate, which in-creases the release of the anti-inflammatory mediatoradenosine [97]. The complex biochemical pathwaysunderlying the therapy of arthritis are not fully under-stood. Therapy of arthritic diseases with biological andchemical drugs is accompanied by changes in serumprotein glycosylation [79,98–104]. An overview ofchanges in serum N-glycosylation as a response to dif-ferent therapeutic agents used in inflammatory arthritisis given in Table 2. Clinical improvement in patientstreated with anti-TNF-α, methotrexate or a combina-tion of both, was accompanied by the restoration of ahealthy IgG-G0/G1 level [79,98–102,105]. A positivecorrelation between ACPA status, C-reactive proteinlevel, Rf-titers and sG0/G1 aberrancy was found [79].However, it was not possible to distinguish between theindividual anti-TNF agents or methotrexate concern-
S. Albrecht et al. / Glycosylation in inflammatory arthritis 23
Table 2Changes in serum N-glycosylation as a response to different therapeutic agents used in inflammatory arthritis
Therapeutic agent Therapy-induced glycosylation changes upon clinicalimprovement
Disease References
Infliximab/methotrexate Increased IgG galactosylation RA [99, 102]Infliximab/methotrexate methotrexate Increased IgG galactosylation RA [100]Infliximab Increased IgG galactosylation RA, Spondyloarthropaty [101]InfliximabEtanerceptAdalimumabMethotrexate
Increased IgG galactosylation, in correlation withACPA, CRP, Rf
RA [79]
EtanerceptAdalimumab
Increased IgG galactosylationIncrease in core-fucosylated and bi-antennary galac-tosylated serum protein glycansDecrease in sialylated tri-antennary serum proteinglycans with/without outer arm fucose
RA, PsA [98]
Sulphasalazine Increased IgG galactosylation and GTase activitywith clinical improvement
RA, AS [108]
Methotrexate Decrease in AGP-fucosylation and sialylation RA [103]NSAIDsOral steroids
Decrease in core-fucosylation of biantennary glycansDecrease in core-fucosylated triantennary glycanswith outer-arm fucose and high mannosylated glycans
Inflammatory diseases [105]
ing their respective influence on the sG0/G1 level andthe concomitant scores of clinical improvement [79].The prediction of patient response to anti-TNF agentsbefore or shortly after beginning therapy presents anurgent need in view of the considerable costs, toxicside effects and the high non-responder rate amongpatients. Approximately 30% of RA patients do notrespond to therapy with anti-TNF-α [106]. So far,no correlation between G0/G1 status and therapy re-sponse, neither at baseline nor after 2 weeks of therapy,has been found [79]. Genetic approaches seem to bemore promising for the prediction of response [107].As well, the question remains whether the therapeu-tic agent directly influences IgG galactosylation, by af-fecting the lymphocytic GTase activity, which is re-duced during RA [108,109]. So far, only the chem-ical DMARD sulphasazine has been shown to effectthe lymphocytic GTase activity [108]. In addition tothe commonly observed restoration of IgG-G0/G1 lev-els, increased levels of core-fucosylated biantennarygalactosylated glycans and decreased levels of sialy-lated triantennary glycans, partly fucosylated at theirouter arms, were found by analysis of whole serumsamples of patients suffering from RA and PsA af-ter one-year anti-TNF treatment [98]. Correspond-ingly, when selectively studying AGP fucosylation, in-fliximab/methotrexate therapy decreased the total fu-cosylation level after 54 weeks [104]. Glycosylationchanges of serum proteins during anti–TNF therapythus reflect the suppression of the autoimmune in-flammatory response, initiated by the cytokine TNF-α during inflammation [96]. A recession of the in-
flammatory process could also be monitored by theglycosylation changes of APPs and by changes inplasma-N-glycosylation in general, after methotrexatetherapy and medication with either nonsteroidal anti-inflammatory drugs (NSAID) or oral steroids [103,105].
4.6. Potential impact of gender, age and commonlifestyle parameters on disease evolvement
Serum N-glycosylation can be affected by gender,age and common lifestyle parameters. In return, thesechanges might be involved in the evolvement of in-flammatory arthritic diseases. Interesting links can beobserved but extensive studies of large patient cohortswould be necessary to scientifically prove these obser-vations.
4.6.1. AgeAge has a considerable influence on serum N-
glycosylation, mainly resulting in a decrease of IgG-galactosylation and increase of bi-secting GalNAc withage [17,110,111]. Interestingly, the incidence of RAincreases with age [112]. A low galactosylation rate,which is comparable to that found for adults aged 60–70 years old, was also stated for young children under3 years of age [111,113]. Correspondingly, JIA mostfrequently occurs around 2–3 years of age [114].
The use of sG0/G1 levels for disease diagnosticsis not influenced by the age-dependent glycosylationchanges, though. Despite the elevated agalactosylationrate, which occures in early childhood, agalactosyla-
24 S. Albrecht et al. / Glycosylation in inflammatory arthritis
tion nevertheless proved to be a marker for JIA; evenmore excessive sG0/G1 rates were found for JIA pa-tients compared to healthy children [113].
Age may therefore contribute to but not be an exclu-sive factor for the evolvement of inflammatory arthriticdiseases.
4.6.2. GenderWhereas gender was generally rated to have a mi-
nor influence on glycosylation [17], a recent study onplasma from 1914 individuals showed, that the level ofseveral glycans is sex-dependent [110]. Glycosylationchanges with aging were more pronounced in females,notably during the transition from pre-menopausal topost-menopausal age. A hormonal influence of theserum-N-glycosylation mechanism is thus probable aswas also suggested for pregnancy-related glycosyla-tion changes [93].
Interesting links can be seen between gender andfrequency as well as gender and activity of inflamma-tory arthritic diseases. Correlation of disease-activityscores with sG0/G1 ratios revealed a high correlationfor the female but not for the male subpopulation [72].Supplementary to that, the frequency of RA was shownto be higher in women compared to men [115].
4.6.3. Common lifestyle parametersEnvironmental factors, such as metabolites from
vitamins and common lifestyle parameters, such asbody mass, plasma lipid status and smoking influenceserum-N-glycosylation to a certain extent [110,116].So far, it is not known whether these factors have aninfluence on the incidence or pathogenicity of inflam-matory arthritic diseases.
5. Conclusion
Serum protein glycosylation is a useful complemen-tary marker for inflammatory arthritic diseases and al-lows a disease-specific diagnosis at an early stage. IgGand APPs are highly subject to glycosylation changesin inflammatory arthritis, which reflects the inflamma-tory immune response and which can thus be targetedduring disease therapy by the use of TNF antagonists.With the emergence of new high-throughput analyticaltools, it is possible to gain new insights into the bio-chemical disease mechanisms, leading to the conclu-sion that glycosylation of autoantibodies, in particularACPA, may play a crucial role in disease aetiopathol-ogy and pathogenicity.
References
[1] F. Nimmerjahn and J.V. Ravetch, Fc-receptors as regula-tors of immunity, in: Advances in immunology, vol 96, F.W.Alt, K.F. Austen, T. Honjo, F. Melchers, J.W. Uhr and E.R.Unanue (eds.), Elsevier Academic Press Inc, San Diego,2007, pp. 179-204.
[2] O. Vagin, E. Tokhtaeva, I. Yakubov, E. Shevchenko and G.Sachs, Inverse correlation between the extent of N-glycanbranching and intercellular adhesion in epithelia – contribu-tion of the Na,K-ATPase beta(1) subunit, J Biol Chem 283(2008), 2192-2202.
[3] P.M. Rudd, M. Butler, I.A. Wilson, J. Jaeken and R.A. Dwek,Roles for glycosylation in the immune system, Glycobiology11 (2001), 865-865.
[4] J.N. Arnold, M.R. Wormald, R.B. Sim, P.M. Rudd and R.A.Dwek, The impact of glycosylation on the biological func-tion and structure of human immunoglobulins, Annu Rev Im-munol 25 (2007), 21-50.
[5] R.T. Lee, G. Lauc and Y.C. Lee, Glycoproteomics: Proteinmodifications for versatile functions. Meeting on glycopro-teomics, EMBO Rep 6 (2005), 1018-1022.
[6] G. Lauc, Sweet secret of the multicellular life, Biochim Bio-phys Acta 1760 (2006), 525-526.
[7] K. Ohtsubo and J.D. Marth, Glycosylation in cellular mech-anisms of health and disease, Cell 126 (2006), 855-867.
[8] M.M. Chavan, P.D. Kawle and N.G. Mehta, Increased sialy-lation and defucosylation of plasma proteins are early eventsin the acute phase response, Glycobiology 15 (2005), 838-848.
[9] G.O. Storey, M. Comer and D.L. Scott, Chronic arthritis be-fore 1876: Early british cases suggesting rheumatoid arthri-tis, Ann Rheum Dis 53 (1994), 557-60.
[10] D.L. Scott, F. Wolfe and T.W. Huizinga, Rheumatoid arthri-tis, Lancet 376 (2010), 1094-108.
[11] A.J. Landre-Beauvais, The first description of rheumatoidarthritis. Unabridged text of the doctoral dissertation pre-sented in 1800, Joint Bone Spine 68 (2001), 130-143.
[12] V. Majithia and S.A. Geraci, Rheumatoid arthritis: Diagnosisand management, Am J Med 120 (2007), 936-939.
[13] J. Ahn, J. Bones, Y.Q. Yu, P.M. Rudd and M. Gilar, Separa-tion of 2-aminobenzamide labeled glycans using hydrophilicinteraction chromatography columns packed with 1.7 μmsorbent, J Chromatogr B 878 (2010), 403-408.
[14] M. Melmer, T. Stangler, M. Schiefermeier, W. Brunner, H.Toll, A. Rupprechter, W. Lindner and A. Premstaller, HILICanalysis of fluorescence-labeled N-glycans from recombi-nant biopharmaceuticals, Anal Bioanal Chem 398 (2010),905-914.
[15] L. Royle, M.P. Campbell, C.M. Radcliffe, D.M. White,D.J. Harvey, J.L. Abrahams, Y.-G. Kim, G.W. Henry, N.A.Shadick, M.E. Weinblatt, D.M. Lee, P.M. Rudd and R.A.Dwek, HPLC-based analysis of serum N-glycans on a 96-well plate platform with dedicated database software, AnalBiochem 376 (2008), 1-12.
[16] A. Knezevic, O. Polasek, O. Gornik, I. Rudan, H. Camp-bell, C. Hayward, A. Wright, I. Kolcic, N. O’Donoghue, J.Bones, P.M. Rudd and G. Lauc, Variability, heritability andenvironmental determinants of human plasma N-glycome, JProteome Res 8 (2009), 694-701.
[17] M. Pucic, A. Knezevic, J. Vidic, B. Adamczyk, M. No-vokmet, O. Polasek, O. Gornik, S. Supraha-Goreta, M.R.Wormald, I. Redzic, H. Campbell, A. Wright, N.D. Hastie,J.F. Wilson, I. Rudan, M. Wuhrer, P.M. Rudd, D. Josic and
S. Albrecht et al. / Glycosylation in inflammatory arthritis 25
G. Lauc, High throughput isolation and glycosylation analy-sis of IgG-variability and heritability of the IgG glycome inthree isolated human populations, Mol Cell Proteomics 10(2011), DOI: 10.1074/mcp.M111.010090.
[18] M. Wuhrer, J.C. Stam, F.E. van de Geijn, C.A.M. Koeleman,C.T. Verrips, R. Dolhain, C.H. Hokke and A.M. Deelder,Glycosylation profiling of immunoglobulin G (IgG) sub-classes from human serum, Proteomics 7 (2007), 4070-4081.
[19] H.J. Jeong, Y.G. Kim, Y.H. Yang and B.G. Kim, High-throughput quantitative analysis of total N-glycans bymatrix-assisted laser desorption/ionization time-of-flightmass spectrometry, Anal Chem 84 (2012), 3453-3460.
[20] G. Zauner, A.M. Deelder and M. Wuhrer, Recent advances inhydrophilic interaction liquid chromatography (HILIC) forstructural glycomics, Electrophoresis 32 (2011), 3456-3466.
[21] M.P. Campbell, L. Royle, C.M. Radcliffe, R.A. Dwek andP.M. Rudd, GlycoBase and autoGU: Tools for HPLC-basedglycan analysis, Bioinformatics 24 (2008), 1214-1216.
[22] C.-W. von der Lieth, A.A. Freire, D. Blank, M.P. Campbell,A. Ceroni, D.R. Damerell, A. Dell, R.A. Dwek, B. Ernst, R.Fogh, M. Frank, H. Geyer, R. Geyer, M.J. Harrison, K. Hen-rick, S. Herget, W.E. Hull, J. Ionides, H.J. Joshi, J.P. Kamer-ling, B.R. Leeflang, T. Lutteke, M. Lundborg, K. Maass,A. Merry, R. Ranzinger, J. Rosen, L. Royle, P.M. Rudd,S. Schloissnig, R. Stenutz, W.F. Vranken, G. Widmalm andS.M. Haslam, EUROCarbDB: An open-access platform forglycoinformatics, Glycobiology 21 (2011), 493-502.
[23] K. Marino, J. Bones, J.J. Kattla and P.M. Rudd, A systematicapproach to protein glycosylation analysis: A path throughthe maze, Nat Chem Biol 6 (2010), 713-723.
[24] C. Huhn, M.H.J. Selman, L.R. Ruhaak, A.M. Deelder andM. Wuhrer, IgG glycosylation analysis, Proteomics 9 (2009),882-913.
[25] L.R. Ruhaak, A.M. Deelder and M. Wuhrer, Oligosaccharideanalysis by graphitized carbon liquid chromatography-massspectrometry, Anal Bioanal Chem 394 (2009), 163-174.
[26] M. Pioch, S.C. Bunz and C. Neususs, Capillary elec-trophoresis/mass spectrometry relevant to pharmaceuti-cal and biotechnological applications, Electrophoresis 33(2012), 1517-1530.
[27] T.T. Yue and B.B. Haab, Microarrays in glycoproteomics re-search, Clin Lab Med 29 (2009), 15-29.
[28] P.M. Rudd, R.J. Leatherbarrow, T.W. Rademacher and R.A.Dwek, Diversification of the IgG molecule by oligosaccha-rides, Mol Immunol 28 (1991), 1369-1378.
[29] J. Barratt, E.M. Bailey, K.S. Buck, J. Mailley, P. Moayyedi,J. Feehally, J.H. Turney, J.E. Crabtree and A.C. Allen, Exag-gerated systemic antibody response to mucosal Helicobac-ter pylori infection in IgA nephropathy, Am J Kidney Dis 33(1999), 1049-1057.
[30] J. Alper, Searching for medicine’s sweet spot, Science 291(2001), 2338-2343.
[31] H. Stibler, Carbohydrate-deficient transferrin in serum: Anew marker of potentially harmful alcohol consumption re-viewed, Clin Chem 37 (1991), 2029-2037.
[32] S. Thompson, E. Dargan, I.D. Griffiths, C.A. Kelly andG.A. Turner, The glycosylation of haptoglobin in rheuma-toid arthritis, Clin Chim Acta 220 (1993), 107-114.
[33] G. de Jong, J.P. van Dijk and H.G. van Eijk, The biology oftransferrin, Clin Chim Acta 190 (1990), 1-46.
[34] K. Yamashita, N. Koide, T. Endo, Y. Iwaki and A. Kobata,Altered glycosylation of serum transferrin of patients withhepatocellular carcinoma, J Biol Chem 264 (1989), 2415-23.
[35] L. Sturiale, R. Barone, A. Fiumara, M. Perez, M. Zaffanello,
G. Sorge, L. Pavone, S. Tortorelli, J.F. O’Brien, J. Jaeken andD. Garozzo, Hypoglycosylation with increased fucosylationand branching of serum transferrin N-glycans in untreatedgalactosemia, Glycobiology 15 (2005), 1268-1276.
[36] C. Panzironi, B. Silvestrini, M.Y. Mo, R. Lahita, D. Mrukand C.Y. Cheng, An increase in the carbohydrate moietyof alpha(2)-macroglobulin is associated with systemic lu-pus erythematosus (SLE), Biochem Mol Biol Int 43 (1997),1305-1322.
[37] T. Das, A.K. Sen, T. Kempf, S.R. Pramanik and C. Mandal,Induction of glycosylation in human C-reactive protein un-der different pathological conditions, Biochem J 373 (2003),345-355.
[38] T. Das and C. Mandal, Variations in binding characteristicsof glycosylated human C-reactive proteins in different patho-logical conditions, Glycoconj J 20 (2004), 537-543.
[39] K.S. Nandakumar, M. Collin, A. Olsen, F. Nimmerjahn,A.M. Blom, J.V. Ravetch and R. Holmdahl, Endoglycosidasetreatment abrogates IgG arthritogenicity: Importance of IgGglycosylation in arthritis, Eur J Immunol 37 (2007), 2973-2982.
[40] M. Holland, K. Takada, T. Okumoto, N. Takahashi, K. Kato,D. Adu, A. Ben-Smith, L. Harper, C.O.S. Savage and R.Jefferis, Hypogalactosylation of serum IgG in patients withANCA-associated systemic vasculitis, Clin Exp Immunol129 (2002), 183-190.
[41] I. Perdivara, S.D. Peddada, F.W. Miller, K.B. Tomer andL.J. Deterding, Mass spectrometric determination of IgGsubclass-specific glycosylation profiles in siblings discor-dant for myositis syndromes, J Proteome Res 10 (2011),2969-2978.
[42] M. Tomana, R.E. Schrohenloher, W.J. Koopman, G.S. Alar-con and W.A. Paul, Abnormal glycosylation of serum IgGfrom patients with chronic inflammatory diseases, ArthritisRheum 31 (1988), 333-338.
[43] Y. Kanoh, T. Mashiko, M. Danbara, Y. Takayama, S. Ohtani,T. Imasaki, T. Abe and T. Akahoshi, Analysis of theoligosaccharide chain of human serum immunoglobulin Gin patients with localized or metastatic cancer, Oncology 66(2004), 365-370.
[44] K. Kodar, J. Stadlmann, K. Klaamas, B. Sergeyev and O.Kurtenkov, Immunoglobulin G Fc N-glycan profiling in pa-tients with gastric cancer by LC-ESI-MS: Relation to tumorprogression and survival, Glycoconj J 29 (2012), 57-66.
[45] R. Saldova, L. Royle, C.M. Radcliffe, U.M.A. Hamid, R.Evans, J.N. Arnold, R.E. Banks, R. Hutson, D.J. Harvey, R.Antrobus, S.M. Petrescu, R.A. Dwek and P.M. Rudd, Ovar-ian cancer is associated with changes in glycosylation inboth acute-phase proteins and IgG, Glycobiology 17 (2007),1344-1356.
[46] C. Gabay and I. Kushner, Acute-phase proteins and othersystemic responses to inflammation, N Engl J Med 340(1999), 448-454.
[47] M.A. Elliott, H.G. Jørgensen and K.D. Smith, Hypersialyla-tion of α1-acid glycoprotein in rheumatoid arthritis, PharmPharmacol Commun 4 (1998), 545-547.
[48] S. Thompson, C.A. Kelly, I.D. Griffiths and G.A. Turner,Abnormally-fucosylated serum haptoglobins in patients withinflammatory joint disease, Clin Chim Acta 184 (1989), 251-258.
[49] E. Dempsey and P.M. Rudd, Acute phase glycoproteins: By-standers or participants in carcinogenesis? Ann NY Acad Sci1253 (2012), 122-132.
[50] H. Albert, M. Collin, D. Dudziak, J.V. Ravetch and F. Nim-
26 S. Albrecht et al. / Glycosylation in inflammatory arthritis
merjahn, In vivo enzymatic modulation of IgG glycosylationinhibits autoimmune disease in an IgG subclass-dependentmanner, Nat Acad Sci Proc 105 (2008), 15005-15009.
[51] R.B. Parekh, R.A. Dwek, B.J. Sutton, D.L. Fernandes, A.Leung, D. Stanworth, T.W. Rademacher, T. Mizuochi, T.Taniguchi, K. Matsuta, F. Takeuchi, Y. Nagano, T. Miyamotoand A. Kobata, Association of rheumatoid-arthritis and pri-mary osteo-arthritis with changes in the glycosylation pat-tern of total serum IgG, Nature 316 (1985), 452-457.
[52] R.B. Parekh, D.A. Isenberg, B.M. Ansell, I.M. Roitt, R.A.Dwek and T.W. Rademacher, Galactosylation of IgG associ-ated oligosaccharides – reduction in patients with adult andjuvenile onset rheumatoid-arthritis and relation to disease-activity, Lancet 1 (1988), 966-969.
[53] A. Alavi and J.S. Axford, Glyco-biomarkers: Potential deter-minants of cellular physiology and pathology, Dis Markers25 (2008), 193-205.
[54] A. Alavi and J.S. Axford, Sweet and sour: The impact ofsugars on disease, Rheumatology 47 (2008), 760-770.
[55] O. Gornik and G. Lauc, Glycosylation of serum proteins ininflammatory diseases, Dis Markers 25 (2008), 267-278.
[56] H. Das, T. Atsumi, Y. Fukushima, H. Shibuya, K. Ito, Y.Yamada, Y. Amasaki, K. Ichikawa, O. Amengual and T.Koike, Diagnostic value of antiagalactosyl IgG antibodies inrheumatoid arthritis, Clin Rheumatol 23 (2004), 1218-222.
[57] Y. Imafuku, H. Yoshida and Y. Yamada, Reactivity of agalac-tosyl IgG with rheumatoid factor, Clin Chim Acta 334(2003), 217-223.
[58] A. Matsumoto, K. Shikata, F. Takeuchi, N. Kojima and T.Mizuochi, Autoantibody activity of IgG rheumatoid factorincreases with decreasing levels of galactosylation and sia-lylation, J Biochem 128 (2000), 621-628.
[59] K.A. Leader, G.C. Lastra, J.R. Kirwan and C.J. Elson,Agalactosyl IgG in aggregates from the rheumatoid joint,Brit J Rheumatol 35 (1996), 335-341.
[60] A.J. Soltys, A. Bond, O.M. Westwood and F.C. Hay, Theeffects of altered glycosylation of IgG on rheumatoid factor-binding and immune complex formation, Adv Exp Med Biol376 (1995), 155-160.
[61] P. Garred, H.O. Madsen, H. Marquart, T.M. Hansen, S.F.Sorensen, J. Petersen, B. Volck, A. Svejgaard, N.A. Grau-dal, P.M. Rudd, R.A. Dwek, R.B. Sim and V. Andersen, Twoedged role of mannose binding lectin in rheumatoid arthritis:A cross sectional study, J Rheumatol 27 (2000), 26-34.
[62] R. Malhotra, M.R. Wormald, P.M. Rudd, P.B. Fischer, R.A.Dwek and R.B. Sim, Glycosylation changes of IgG associ-ated with rheumatoid-arthritis can activate complement viathe mannose-binding protein, Nat Med 1 (1995), 237-243.
[63] Y. Kaneko, F. Nimmerjahn and E.V. Ravetch, Anti-inflammatory activity of immunoglobulin G resulting fromFc sialylation, Science 313 (2006), 670-673.
[64] M. Watson, P.M. Rudd, M. Bland, R.A. Dwek and J.S.Axford, Sugar printing rheumatic diseases: A potentialmethod for disease differentiation using immunoglobulin Goligosaccharides, Arthritis Rheum 42 (1999), 1682-1690.
[65] R. Niwa, A. Natsume, A. Uehara, M. Wakitani, S. Iida, K.Uchida, M. Satoh and K. Shitara, IgG subclass-independentimprovement of antibody-dependent cellular cytotoxicity byfucose removal from Asn(297)-linked oligosaccharides, JImmunol Meth 306 (2005), 151-160.
[66] T. Shinkawa, K. Nakamura, N. Yamane, E. Shoji-Hosaka,Y. Kanda, M. Sakurada, K. Uchida, H. Anazawa, M. Satoh,M. Yamasaki, N. Hanai and K. Shitara, The absence offucose but not the presence of galactose or bisecting N-
acetylglucosamine of human IgG1 complex-type oligosac-charides shows the critical role of enhancing antibody-dependent cellular cytotoxicity, J Biol Chem 278 (2003),3466-3473.
[67] J.F. Fries, C.A. Williams, D. Morfeld, G. Singh and J. Sibley,Reduction in long-term disability in patients with rheuma-toid arthritis by disease-modifying antirheumatic drug-basedtreatment strategies, Arthritis Rheum 39 (1996), 616-622.
[68] D. Aletaha, T. Neogi, A.J. Silman, J. Funovits, D.T. Felson,C.O. Bingham, N.S. Birnbaum, G.R. Burmester, V.P. Byk-erk, M.D. Cohen, B. Combe, K.H. Costenbader, M. Douga-dos, P. Emery, G. Ferraccioli, J.M.W. Hazes, K. Hobbs,T.W.J. Huizinga, A. Kavanaugh, J. Kay, T.K. Kvien, T.Laing, P. Mease, H.A. Menard, L.W. Moreland, R.L. Naden,T. Pincus, J.S. Smolen, E. Stanislawska-Biernat, D. Sym-mons, P.P. Tak, K.S. Upchurch, J. Vencovsky, F. Wolfeand G. Hawker, Rheumatoid arthritis classification crite-ria: An american college of rheumatology/european leagueagainst rheumatism collaborative initiative, Arthritis Rheum62 (2010), 2569-2581.
[69] S. Rantapaa-Dahlqvist, B.A.W. de Jong, E. Berglin, G. Hall-mans, G. Wadell, H. Stenlund, U. Sundin and W.J. van Ven-rooij, Antibodies against cyclic citrullinated peptide and IgArheumatoid factor predict the development of rheumatoidarthritis, Arthritis Rheum 48 (2003), 2741-2749.
[70] U. Sauerland, H. Becker, M. Seidel, H. Schotte, P. Willeke,A. Schorat, B. Schluter, W. Domschke and M. Gaubitz, Clin-ical utility of the anti-CCP assay - experiences with 700 pa-tients, in: Autoimmunity: Concepts and diagnosis at the cut-ting edge, M.E. Gershwin and Y. Shoeenfeld (eds.), NewYork Acad Sciences, New York, 2005, pp. 314-318.
[71] I. Vallbracht, J. Rieber, M. Oppermann, F. Forger, U. Siebertand K. Helmke, Diagnostic and clinical value of anti-cycliccitrullinated peptide antibodies compared with rheumatoidfactor isotypes in rheumatoid arthritis, Ann Rheum Dis 63(2004), 1079-1084.
[72] A. Ercan, J. Cui, D.E.W. Chatterton, K.D. Deane, M.M.Hazen, W. Brintnell, C.I. O’Donnell, L.A. Derber, M.E.Weinblatt, N.A. Shadick, D.A. Bell, E. Cairns, D.H.Solomon, V.M. Holers, P.M. Rudd and D.M. Lee, Aber-rant IgG galactosylation precedes disease onset, correlateswith disease activity, and is prevalent in autoantibodies inrheumatoid arthritis, Arthritis Rheum 62 (2010), 2239-2248.
[73] R.B. Parekh, R.A. Dwek, B.J. Sutton, D.L. Fernandes, A.Leung, D. Stanworth, T.W. Rademacher, T. Mizuochi, T.Taniguchi, K. Matsuta and et al., Association of rheumatoidarthritis and primary osteoarthritis with changes in the gly-cosylation pattern of total serum IgG, Nature 316 (1985),452-7.
[74] A. Young, N. Sumar, K. Bodman, S. Goyal, H. Sinclair,I. Roitt and D. Isenberg, Agalactosyl IgG - an aid todifferential-diagnosis in early synovitis, Arthritis Rheum 34(1991), 1425-1429.
[75] K. Forslind, M. Ahlmen, K. Eberhardt, I. Hafstrom, B.Svensson and B.S. Grp, Prediction of radiological outcomein early rheumatoid arthritis in clinical practice: Role of an-tibodies to citrullinated peptides (anti-CCP), Ann Rheum Dis63 (2004), 1090-1095.
[76] C. Turesson, L.T.H. Jacobsson, G. Sturfelt, E.L. Matteson,L. Mathsson and J. Ronnelid, Rheumatoid factor and an-tibodies to cyclic citrullinated peptides are associated withsevere extra-articular manifestations in rheumatoid arthritis,Ann Rheum Dis 66 (2007), 59-64.
[77] F. Humby, M. Bombardieri, A. Manzo, S. Kelly, M.C.
S. Albrecht et al. / Glycosylation in inflammatory arthritis 27
Blades, B. Kirkham, J. Spencer and C. Pitzalis, Ectopiclymphoid structures support ongoing production of class-switched autoantibodies in rheumatoid synovium, PlosMedicine 6 (2009), 59-75.
[78] H.U. Scherer, D. van der Woude, A. Ioan-Facsinay, H. elBannoudi, L.A. Trouw, J. Wang, T. Haupl, G.R. Burmester,A.M. Deelder, T.W.J. Huizinga, M. Wuhrer and R.E.M.Toes, Glycan profiling of anti-citrullinated protein antibod-ies isolated from human serum and synovial fluid, ArthritisRheum 62 (2010), 1620-1629.
[79] A. Ercan, J. Cui, M. Hazen, F. Batliwalla, L. Royle, P. Rudd,J. Coblyn, N. Shadick, M. Weinblatt, P. Gregersen, D. Leeand P. Nigrovic, Hypogalactosylation of serum N-glycansfails to predict clinical response to methotrexate and TNF in-hibition in rheumatoid arthritis, Arthritis Res Ther 14 (2012),R43.
[80] R.M. Anthony, F. Nimmerjahn, D.J. Ashline, V.N. Reinhold,J.C. Paulson and J.V. Ravetch, Recapitulation of IVIG anti-inflammatory activity with a recombinant IgG FC, Science320 (2008), 373-376.
[81] A. Ioan-Facsinay, A. Willemze, D.B. Robinson, C.A.Peschken, J. Markland, D. van der Woude, B. Elias, H.A.Menard, M. Newkirk, M.J. Fritzler, R.E.M. Toes, T.W.J.Huizinga and H.S. El-Gabalawy, Marked differences in finespecificity and isotype usage of the anti-citrullinated proteinantibody in health and disease, Arthritis Rheum 58 (2008),3000-3008.
[82] K. Martin, R. Talukder, F.C. Hay and J.S. Axford, Charac-terization of changes in IgG associated oligosaccharide pro-files in rheumatoid arthritis, psoriatic arthritis, and ankylos-ing spondylitis using fluorophore linked carbohydrate elec-trophoresis, J Rheumatol 28 (2001), 1531-1536.
[83] J.S. Axford, G. Cunnane, O. Fitzgerald, J.M. Bland, B. Bres-nihan and E.R. Frears, Rheumatic disease differentiation us-ing immunoglobulin G sugar printing by high density elec-trophoresis, J Rheumatol 30 (2003), 2540-2546.
[84] E. Gindzienska-Sieskiewicz, P.A. Klimiuk, D.G. Kisiel, A.Gindzienski and S. Sierakowski, The changes in monosac-charide composition of immunoglobulin G in the course ofrheumatoid arthritis, Clin Rheumatol 26 (2007), 685-690.
[85] J.K. Lacki, W. Porawska, U. Mackiewicz, S. Mackiewiczand W. Muller, Changes in agalactosyl IgG levels correlatewith radiological progression in early rheumatoid arthritis,Ann Med 28 (1996), 265-269.
[86] R. Parekh, D. Isenberg, B. Ansell, I. Roitt, R. Dwek andT. Rademacher, Galactosylation of IgG associated oligosac-charides: Reduction in patients with adult and juvenile on-set rheumatoid arthritis and relation to disease activity, TheLancet 331 (1988), 966-969.
[87] N. Tsuchiya, T. Endo, M. Shiota, N. Kochibe, K. Itoand A. Kobata, Distribution of glycosylation abnormalityamong serum IgG subclasses from patients with rheumatoid-arthritis, Clin Immunol Immunopathol 70 (1994), 47-50.
[88] M. Flogel, G. Lauc, I. Gornik and B. Macek, Fucosylationand galactosylation of IgG heavy chains differ between acuteand remission phases of juvenile chronic arthritis, Clin ChemLab Med 36 (1998), 99-102.
[89] A. Alavi, N. Arden, T.D. Spector and J.S. Axford, IgG gly-cosylation changes are associated with the clinical outcomeof rheumatoid arthritis in pregnancy, Arthritis Rheum 40(1997), 711.
[90] E.C. Havenaar, J.S. Axford, E.C.M. Brinkman-van der Lin-den, A. Alavi, E.C.R. Van Ommen, B. van het Hof, T. Spec-tor, A. Mackiewicz and W. Van Dijk, Severe rheumatoid
arthritis prohibits the pregnancy-induced decrease in alpha3-fucosylation of alpha(1)-acid glycoprotein, Glycoconj J 15(1998), 723-729.
[91] J.M. Pekelharing, E. Hepp, J.P. Kamerling, G.J. Gerwigand B. Leijnse, Alterations in carbohydrate-composition ofserum IgG from patients with rheumatoid-arthritis and frompregnant women, Ann Rheum Dis 47 (1988), 91-95.
[92] F.E. van de Geijn, M. Wuhrer, M.H.J. Selman, S.P. Willem-sen, Y.A. de Man, A.M. Deelder, J.M.W. Hazes and R. Dol-hain, Immunoglobulin G galactosylation and sialylation areassociated with pregnancy-induced improvement of rheuma-toid arthritis and the postpartum flare: Results from a largeprospective cohort study, Arthritis Res Ther 11 (2009), DOI:10.1186/ar2892
[93] E.C.M. BrinkmanVanderLinden, E.C. Havenaar, E.C.R.VanOmmen, G.J. VanKamp, L.J.G. Gooren and W. VanDijk,Oral estrogen treatment induces a decrease in expression ofsialyl Lewis x on alpha(1)-acid glycoprotein in females andmale-to-female transsexuals, Glycobiology 6 (1996), 407-412.
[94] W. Van Dijk and A. Mackiewicz, Interleukin-6-typecytokine-induced changes in acute phase protein glycosyla-tion, in: Interleukin-6 type cytokines, A. Mackiewicz, A. Kojand P.B. Sehgal (eds.), New York Acad Sciences, New York,1995, pp. 319-330.
[95] Y.A. de Man, L.E. Bakker-Jonges, C.M. Dufour-van denGoorbergh, S.P.R. Tillemans, H. Hooijkaas, J.M.W. Hazesand R. Dolhain, Women with rheumatoid arthritis negativefor anti-cyclic citrullinated peptide and rheumatoid factorare more likely to improve during pregnancy, whereas inautoantibody-positive women autoantibody levels are not in-fluenced by pregnancy, Ann Rheum Dis 69 (2010), 420-423.
[96] M. Feldmann, F.M. Brennan and R.N. Maini, Role ofcytokines in rheumatoid arthritis, Annu Rev Immunol 14(1996), 397-440.
[97] B.N. Cronstein, M.A. Eberle, H.E. Gruber and R.I. Levin,Methotrexate inhibits neutrophil function by stimulatingadenosine release from connective-tissue cells, Proc NatlAcad Sci USA 88 (1991), 2441-2445.
[98] E.S. Collins, M.C. Galligan, R. Saldova, B. Adamczyk, J.L.Abrahmans, M.P. Campbell, C.-T. Ng, D.J. Veale, T.B. Mur-phy, P.M. Rudd and O. FitzGerald, Glycosylation statusof serum in inflammatory arthritis in response to anti-TNFtreatment, Rheumatology 52 (2013), 1572-1582.
[99] A. Croce, O. Firuzi, F. Altieri, M. Eufemi, R. Agostino, R.Priori, M. Bombardieri, C. Alessandri, G. Valesini and L.Saso, Effect of infliximab on the glycosylation of IgG of pa-tients with rheumatoid arthritis, J Clin Lab Anal 21 (2007),303-314.
[100] M. Pasek, M. Duk, M. Podbielska, R. Sokolik, J. Szechin-ski, E. Lisowska and H. Krotkiewski, Galactosylation of IgGfrom rheumatoid arthritis (RA) patients – changes duringtherapy, Glycoconj J 23 (2006), 463-471.
[101] K. Van Beneden, K. Coppieters, W. Laroy, F. De Keyser,I.E. Hoffman, F. Van den Bosch, B.V. Cruyssen, M. Dren-nan, P. Jacques, P. Rottiers, G. Verbruggen, R. Contreras, N.Callewaert and D. Elewaut, Reversible changes in serum im-munoglobulin galactosylation during the immune responseand treatment of inflammatory autoimmune arthritis, AnnRheum Dis 68 (2009), 1360-1365.
[102] A. Crore, O. Firuzi, F. Altieri, M. Eufemi, R. Agostino, R.Priori, M. Bombardieri, C. Alessandri, G. Valesini and L.Saso, Effect of infliximab on the glycosylation of IgG of pa-
28 S. Albrecht et al. / Glycosylation in inflammatory arthritis
tients with rheumatoid arthritis, J Clin Lab Anal 21 (2007),303-314.
[103] T.W. de Graaf, E.C.R. van Ommen, M.E. van der Stelt, P.Kerstens, A.M.T. Boerbooms and W. van Dijk, Effects oflow-dose methotrexate therapy on the concentration and theglycosylation of alpha(1)-acid glycoprotein in the serum ofpatients with rheumatoid-arthritis – a longitudinal-study, JRheumatol 21 (1994), 2209-2216.
[104] A. Olewicz-Gawlik, I. Korczowska-Lacka, J.K. Lacki, K.Klama and P. Hrycaj, Fucosylation of serum alpha(1)-acidglycoprotein in rheumatoid arthritis patients treated with in-fliximab, Clin Rheumatol 26 (2007), 1679-1684.
[105] R. Saldova, J.E. Huffman, B. Adamczyk, A. Muzinic, J.J.Kattla, M. Pucic, M. Novokmet, J.L. Abrahams, C. Hay-ward, I. Rudan, S.H. Wild, A.F. Wright, O. Polasek, G. Lauc,H. Campbell, J.F. Wilson and P.M. Rudd, Association ofmedication with the human plasma N-glycome, J ProteomeRes 11 (2012), 1821-1831.
[106] K.L. Hyrich, K.D. Watson, A.J. Silman, D.P.M. Symmonsand T.B.B. Register, Predictors of response to anti-TNF-αtherapy among patients with rheumatoid arthritis: Resultsfrom the british society for rheumatology biologics register,Rheumatology 45 (2006), 1558-1565.
[107] C.Y. Liu, F. Batliwalla, W.T. Li, A. Lee, R. Roubenoff,E. Beckman, H. Khalili, A. Damle, M. Kern, R. Furie, J.Dupuis, R.M. Plenge, M.J.H. Coenen, T.W. Behrens, J.P.Carulli and P.K. Gregersen, Genome-wide association scanidentifies candidate polymorphisms associated with differen-tial response to anti-TNF treatment in rheumatoid arthritis,Mol Med 14 (2008), 575-581.
[108] J.S. Axford, N. Sumar, A. Alavi, D.A. Isenberg, A. Young,K.B. Bodman and I.M. Roitt, Changes in normal glycosyla-tion mechanisms in autoimmune rheumatic disease, J ClinInvest 89 (1992), 1021-1031.
[109] A. Kobata, Function and pathology of the sugar chains ofhuman immunoglobulin G, Glycobiology 1 (1990), 5-8.
[110] A. Knezevic, O. Gornik, O. Polasek, M. Pucic, I. Redzic, M.Novokmet, P.M. Rudd, A.F. Wright, H. Campbell, I. Rudanand G. Lauc, Effects of aging, body mass index, plasma lipidprofiles, and smoking on human plasma N-glycans, Glyco-biology 20 (2010), 959-969.
[111] R. Parekh, I. Roitt, D. Isenberg, R. Dwek and T.Rademacher, Age-related galactosylation of the N-linkedoligosaccharides of human-serum IgG, J Exp Med 167(1988), 1731-1736.
[112] C.G. Helmick, D.T. Felson, R.C. Lawrence, S. Gabriel,R. Hirsch, C.K. Kwoh, M.H. Liang, H.M. Kremers, M.D.Mayes, P.A. Merkel, S.R. Pillemer, J.D. Reveille, J.H. Stoneand W. Natl Arthritis Data, Estimates of the prevalence ofarthritis and other rheumatic conditions in the united states,Arthritis Rheum 58 (2008), 15-25.
[113] A. Ercan, M.G. Barnes, M. Hazen, H. Tory, L. Hender-son, F. Dedeoglu, R.C. Fuhlbrigge, A. Grom, I.A. Holm,M. Kellogg, S. Kim, B. Adamczyk, P.M. Rudd, M. BethSon, R.P. Sundel, D. Foell, D.N. Glass, S.D. Thompson andP.A. Nigrovic, Multiple juvenile idiopathic arthritis subtypesdemonstrate pro-inflammatory IgG glycosylation, ArthritisRheum (2012), DOI: 10.1002/art.34507.
[114] K.J. Murray, M.B. Moroldo, P. Donnelly, S. Prahalad, M.H.Passo, E.H. Giannini and D.N. Glass, Age-specific effects ofjuvenile rheumatoid arthritis-associated HLA alleles, Arthri-tis Rheum 42 (1999), 1843-1853.
[115] E. Myasoedova, C.S. Crowson, H.M. Kremers, T.M. Th-erneau and S.E. Gabriel, Is the incidence of rheumatoidarthritis rising? Results from olmsted county, minnesota,1955–2007, Arthritis Rheum 62 (2010), 1576-1582.
[116] J. Wang, C.I.A. Balog, K. Stavenhagen, C.A.M. Koele-man, H.U. Scherer, M.H.J. Selman, A.M. Deelder, T.W.J.Huizinga, R.E.M. Toes and M. Wuhrer, Fc-glycosylation ofIgG1 is modulated by B-cell stimuli, Mol Cell Proteomics10 (2011), DOI: 10.1074/mcp.M110.004655.
[117] T.W. de Graaf, M.E. van der Stelt, M.G. Anbergen and W.van Dijk, Inflammation-induced expression of sialyl Lewisx-containing glycan structures on alpha-1-acid glycoprotein(orosomucoid) in human sera, J Exp Med 177 (1993), 657-666.
[118] K. Higai, Y. Aoki, Y. Azuma and K. Matsumoto, Glycosy-lation of site-specific glycans of alpha(1)-acid glycoproteinand alterations in acute and chronic inflammation, BiochimBiophys Acta 1725 (2005), 128-135.
[119] E.C.M. Brinkman-van der Linden, P.F. de Haan, E.C. Have-naar and W. van Dijk, Inflammation-induced expressionof sialyl Lewis(x) is not restricted to alpha(1)-acid gly-coprotein but also occurs to a lesser extent on alpha(1)-antichymotrypsin and haptoglobin, Glycoconj J 15 (1998),177-182.
[120] I. Ryden, P. Pahlsson, A. Lundblad and T. Skogh, Fucosy-lation of alpha 1-acid glycoprotein (orosomucoid) comparedwith traditional biochemical markers of inflammation in re-cent onset rheumatoid arthritis, Clin Chim Acta 317 (2002),221-229.
[121] A. Saroha, S. Biswas, B.P. Chatterjee and H.R. Das, Al-tered glycosylation and expression of plasma alpha-1-acidglycoprotein and haptoglobin in rheumatoid arthritis, Jour-nal Chromatogr B 879 (2011), 1839-1843.
[122] A. Sarrats, R. Saldova, E. Pla, E. Fort, D.J. Harvey, W.B.Struwe, R. de Llorens, P.M. Rudd and R. Peracaula, Gly-cosylation of liver acute-phase proteins in pancreatic cancerand chronic pancreatitis, Proteom Clin Appl 4 (2010), 432-448.
[123] L. Saso, B. Silvestrini, A. Guglielmotti, R. Lahita and C.Y.Cheng, Abnormal glycosylation of alpha(2)-macroglobulin,a non-acute-phase protein, in patients with autoimmune-diseases, Inflammation 17 (1993), 465-479.
[124] M.T. Goodarzi, J.S. Axford, S.S. Varanasi, A. Alavi, G. Cun-nane, O. Fitzgerald and G.A. Turner, Sialyl Lewis(x) expres-sion on IgG in rheumatoid arthritis and other arthritic con-ditions: A preliminary study, Glycoconj J 15 (1998), 1149-1154.
[125] R.A. Feelders, G. Vreugdenhil, G. Dejong, A.J.G. Swaakand H.G. Vaneijk, Transferrin microheterogeneity inrheumatoid-arthritis – relation with disease-activity and ane-mia of chronic disease, Rheumatol Int 12 (1992), 195-199.
[126] M. Grzymislawski, K. Derc, M. Sobieska and K. Wiktorow-icz, Microheterogeneity of acute phase proteins in patientswith ulcerative colitis, World J Gastroentero 12 (2006),5191-5195.
[127] O. Gornik, I. Gornik, I.Z. Kolednjak and G. Lauc, Change oftransferrin sialylation differs between mild sepsis and severesepsis and septic shock, Internal Med 50 (2011), 861-869.
[128] D.J. Harvey, A.H. Merry, L. Royle, M. P. Campbell, R.A.Dwek and P.M. Rudd, Proposal for a standard system fordrawing structural diagrams of N- and O-linked carbohy-drates and related compounds, Proteomics 9 (2009), 3796-3801.