Final Report of IMNCI Training Courses in Five Selected ...
-
Upload
khangminh22 -
Category
Documents
-
view
5 -
download
0
Transcript of Final Report of IMNCI Training Courses in Five Selected ...
Final Report of IMNCI Training Courses in
Five Selected States and Regions
2016-2018
Taungdwingyi Township, Magway Region
Ingapu Township, Ayeyarwaddy Region
Minbya Township, Rakhine State
Tang Yang Township, Northern Shan State
Mongyai Township, Northern Shan State
Mong Kai Township, Southern Shan State
MCSP Child Health Team
July 2018
Acknowledgements
MCSP is a global USAID initiative to introduce and support high-impact health interventions
in 25 priority countries to help prevent child and maternal deaths. MCSP supports
programming in maternal, newborn and child health, immunization, family planning and
reproductive health, nutrition, health system strengthening, water/sanitation/hygiene, malaria
control, prevention of mother to child transmission of HIV, and Paediatric HIV care and
treatment. MCSP will tackle these issues through approaches that also focus on household and
community mobilization, gender integration and digital health, among others.
In Myanmar, under the leadership and direction of the Child Health Development Division
(CHD), MCSP collaborated with the MOHS in updating IMNCI guidelines for Basic Health
Staff. The CHD has provided guidance and oversight for all aspects of the training cascade,
implementation and post-training supervision. State and Regional Child Health teams closely
collaborated with MCSP in the township Multiplier training and post-training supervision to
the trained BHS and health facilities.
This report is make possible by the generous support of the American people through the
United States Agency for International Development (USAID) under the terms of the
Cooperative Agreement AID-OAA-A-14-00028. The contents of this report are the
responsibility of the Maternal and Child Survival Program and do not necessarily reflect the
views of USAID or the United States Government.
July 2018
Cover Photo: A midwife conducting patient examination during a post-training supervision
visit, Maternal and Child Health center, Mong Kai township, Southern Shan State
1
Contents
Page
Contents 1
Abbreviation 3
1. Introduction 5
2. Background 6
3. Activity 7
3.1 Developing Updated IMNCI guidelines (2017) 7
3.2 Launching ceremony of Updated IMNCI guidelines (2017) (2-59 months) 7
3.3 Township selection meetings, June and July 2017 7
3.4 Training 10
3.4.1 Central MToT updated IMNCI training, Nay Pyi Taw 10
3.4.2 Central MToT Follow-up training, Nay Pyi Taw 11
3.4.3 State and Regional ToT training 12
3.4.4 State and Regional ToT for follow-up training 12
3.4.5 Township-level multiplier training 12
3.5 CME session 12
3.6 Learning and Performance Improvement Centers (L&PICs) 13
3.7 Post-training supervision visits 13
4. Implementation activity in 5 selected States and Regions 14
4.1 Magway region 14
4.2 Ayeyarwaddy region 16
4.3 Rakhine state 18
4.4 Northern Shan state 19
4.5 Southern Shan state 23
5. Summary of Training and Post-training supervision visits 25
5.1 Training 25
5.2 Post training supervision visits 29
5.2.1 Assessment on clinical skills management 29
5.2.2 Infrastructure 29
5.2.3 Drug stock management 30
6. Key Recommendations 33
7. References 34
8. Annexes 35
Annex 1. Agenda of Central MToT on updated IMNCI guidelines (2017), Nov 2017 35
Annex 2. Agenda for Central MTOT on Follow-up training of updated IMNCI
guidelines (2017), January 2018 39
Annex 3. Agenda for State level Follow-up training of updated IMNCI guidelines (2017),
S Shan state 42
2
Annex 4. Agenda for Township level Multiplier training, Mong Kai township,
S Shan state, February 2018 46
Annex 5. List of participants in training and supervision visits 50
Annex 6. Number and percentage of trained MOHS trainers in the state,
regional and township training teams 52
Annex 7. BHS (LHV and Midwife) existing, trained and supervised 52
Annex 8. Health centers (UHC, MCH, RHC, sub-center) existing, trained
and supervised 53
Annex 9. (a, b) Pre- and Post-test scores of participants in trainings 54
Annex 10. Case Scenarios (OSCE) for Pre- and Post-tests in updated IMNCI training 55
Annex 11. Follow-up activity after training – Supervision Tools (English translation) 57
Annex 12. IMNCI Materials placed at L&PICs (5 states/regions) 64
Annex 13.Success stories 66
– Magway Region 67
– S. Shan State 69
– N. Shan State 71
– Rakhine State 73
Tables
Table 1. Geographical situation and 2017 health profile data of implementing townships 8
Figures
Fig 1. Number of participants who attended ToT from States and Regions 23
Fig 2. Percentage of BHS, trained and supervised in six selected townships 24
Fig 3. Percentage of health centers, trained and supervised (Health centers: UHC, MCH, RHC,
sub-center) 24
Fig 4. Pre- and Post-test scores achievement 25
Map
1. Locations of six selected townships in five states and regions implementing
IMNCI activity 9
3
Abbreviations
ART Antiretroviral Therapy
BHS Basic Health Staff
CHD Child Health Development Division
CME Continuing Medical Education
EPI Expanded Programme on Immunization
IMCI Integrated Management of Childhood Illness
IMNCI Integrated Management of Neonatal and Childhood Illness
IMR Infant Mortality Rate
L&PIC Learning and Performance Improvement Center
LB Live Births
LHV Lady Health Visitor
MW Midwife
NAP National AIDS Program
NHP National Health Plan
NMCP National Malaria Control Program
NMR Neonatal Mortality Rate
MCH Maternal and Child Health
MCSP Maternal and Child Survival Program
MDG Millennium Development Goal
MR Mortality Rate
MTOT Master Training of Trainers
OPD Out-patient Department
ORS Oral Rehydration Salt/Solution
OSCE Objective Structured Clinical Examination
RHC Rural Health Center
RUTF Ready-to-Use Therapeutic Food
SDG Sustainable Development Goals
THN Township Health Nurse
TOT Training of Trainers
U5 MR Under 5 Mortality Rate
5
1. Introduction
The Integrated Management of Childhood Illness (IMCI) is an integrated approach to child
health that intends to reduce death, illness and disabilities and promote proper growth and
development among under 5 children through both preventive and curative activities1. WHO
and UNICEF developed this approach in 1992 and currently more than 100 countries use the
IMCI guideline and approach globally. The IMCI approach is mainly focused on improving
case management skills of health care providers, improving family and community health
practices, and improving overall health systems2.
Since 2007 neonatal health has been added to the IMCI approach, as one of the essential
components to address overall mortality and morbidity of under 5 children. IMCI or IMNCI
(with neonatal care added to IMCI) guidelines and approaches are mainly intended for child
health care in the public health sector, especially in developing countries.
The IMNCI strategy was introduced in Myanmar in 1999 and the neonatal component was
formally incorporated as IMNCI in 2011. Since then, IMNCI training has been ongoing to
achieve nationwide coverage. The IMNCI modules used in Myanmar training were updated in
2017, based on the updated WHO IMNCI guidelines. The IMNCI strategy is intended to give
under 5 children a better quality of life by promoting both preventive and curative child care
and is implemented by the Basic Health Staff (BHS), in partnership with the families and
community. The IMNCI strategy also includes improvement of health infrastructure, such as
drugs and commodity management, patient data recording, documentation and reporting
systems.
In the Myanmar National Demographic Health Survey (2015-16) the under-5 mortality rate
was reported as 50/1000 live births (LBs), infant mortality rate was 40/1000 LBs and neonatal
mortality rate was 25/1,000 live births3. The Millennium Development Goal No. 4, set by the
Ministry of Health, aimed to reduce under-5 mortality to 37 per 1,000 live births and infant
mortality to 28 per 1,000 live births by 2015 in Myanmar 4. However, in 2016, both U5MR and
infant mortality rate (IMR) in Myanmar were higher than the global rates of 40.8 per 1,000
LBs for U5MR and 30.5 per 1000 LBs, although all three mortality rates (under-5, infant and
neonatal) declined in Myanmar from 2011 to 2016.
At the end of the MDG years, most countries in the world had not reached the MDG 4 target
of reducing under-5 mortality by two-thirds. Following the MDG period, a new global
development agenda has been established with new targets, referred to as Sustainable
Development Goals (SDG) (2015-2030). The child survival targets in the SDG are intended to
further reduce the deaths of children under 5 from preventable diseases. By 2030 in Myanmar,
the target is to reduce neonatal mortality to 12 deaths per 1,000 live births and reduce under-5
mortality to 25 deaths per 1,000 live births5.
6
2. Background
IMNCI trainings are conducted under the leadership of the Child Health Development
Division, Ministry of Health and Sports, in Myanmar, and primarily intended for the Basic
Health Staff at the township level of States and Regions. The IMNCI guidelines were updated
by the MOHS, with technical support from MCSP, in 2017, to ensure that the latest IMNCI
information from WHO was incorporated, to be in line with the global IMNCI strategy.
The updated IMNCI guidelines (2017) are designed to be user friendly and easily
understandable, promoting easy access to updated knowledge, and effective use by the BHS
and the community, as well as family members of the child patient. It is composed of five
books: Provider Guide, Facilitator Guide, Exercise Book, Handbill or Chart Booklet, Photo
Book, plus a DVD with learning video clips and a Power Point CD. The content of the books
covers childhood illness and management of sick children from 2 to 59 months old (5 years).
In the IMNCI training, the updated IMNCI guideline books (2-59 months) are used, together
with the introduction book and the follow-up after training book, for instruction on correct
utilization of forms and formats used in the post-training supervision visits.
The updated IMNCI guidelines (2017) are published in Myanmar language in order to be easily
understood by the users and the BHS. The provider Guide is the main textbook and contains
all needed information. A trainer or facilitator uses the Power Point CD, which contains all the
contents of updated IMNCI guidelines during the training. The exercise book contains
questions for each chapter on physical examination, clinical management, and making a
diagnosis. The answers to the questions are included in the Facilitator Guide to assist the
trainers/facilitators in checking the answers of the training participants.
The updated IMNCI guidelines (2017) are composed of five main chapters: (1)Assess and
Classify the Patient, (2) Identify Treatment, (3) Treat, (4)Counsel the Mother and (5) Follow-
Up the Child. The guidelines explain how to ask the mother about the child's problem, and
check for the general danger signs of the common childhood illnesses. It includes how to assess
the signs and symptoms and classify the common childhood illnesses, such as cough or difficult
breathing, diarrhea, fever, ear problems, malnutrition and anemia, mouth and gum infection,
HIV infection and immunization status. According to the classification of the disease, the BHS
makes the decision for identifying the correct treatment, such as providing suitable antibiotics
and care according to the drug dosages in the guidelines. The updated IMNCI guidelines (2017)
are intended to support the BHS to develop counseling skills for talking with the mother about
childcare, treatment and feeding of the child. At the end, the BHS will provide health education
to the mother and make an appointment for a follow-up visit if necessary.
The BHS will record the patient consultation by using the patient record form and file the
document. The patient identification, diagnosis and treatment are noted down in the patient
register book.
7
3. Activity
3.1 Developing updated IMNCI guidelines (2017)
The MCSP Child Health team, in close collaboration with the Director of Child Health
Division, provided support to the Child Health Development Division, MOHS for updating the
IMNCI guidelines (2017). The 2-59 months portion of the previous existing IMNCI guidelines
was redesigned to be user-friendly, compact and concise with updated global IMNCI
information, and completed with additional chapters on HIV infection, mouth and gum
infection and growth and development. The updated guidelines were developed in Myanmar
language, except for some medical terminology and drug selection and dosages. The content
of the updated guidelines was mainly based on the WHO guidelines and prepared to be in line
with the country context. Additional technical information was provided by the Program
Managers of the National AIDS Program (NAP), National Malaria Control Program (NMCP),
Expanded Program of Immunization (EPI) and the National Nutrition Program.
The new IMNCI guidelines were developed for a 4-day training of Trainers (ToT) at central
and state/regional level and a 5-day training for the BHS at the township level. After one month,
there was a three-day follow-up training for the supervisors of 5 States and Regions, focusing
on the utilization of supervision check lists, forms and formats and organization of follow-up
plans. At the State and Regional level, the follow-up training is conducted for 3 days
(sometimes modified to 2 days, by decision of the State Health Department), followed by one
day of orientation on use of the Continuing Medical Education (CME) modules for Pneumonia
and Diarrhea.
3.2 Launching ceremony of updated IMNCI guidelines (2017) (2-59 months)
The updated IMNCI guideline was included in the launching ceremony for "Early Essential
Newborn Care (EENC), Care for Small Babies and Updated Integrated Management of
Childhood Illness" which was organized by the Child Health Development Division, MOHS,
on 30th May, 2017 in Nay Pyi Taw. There were about 150 participants from Departments of
MOHS, local and International organizations working with CHD, WHO, UNICEF and donor
agencies. MCSP staff from Child Health and Newborn teams participated. The opening speech
was provided by Dr. Thet Khaing Win, Permanent Secretary of the MOHS, and Dr. Myint
Myint Than, Director of the Child Health Development Division. The participants were
introduced to the two guidelines developed on Early Essential Newborn Care and the updated
IMNCI guideline (2-59 months) and were informed of the future plans, training cascade and
follow-up activity of MCSP on Newborn and Child Health care.
3.3 Township selection meetings - June and July 2017
MCSP activities for improving the capacity of Public Health staff in maternal, newborn and
child health are carried out in LPIC-linked States and Regions, that is Magway region,
Ayeyarwaddy region, Rakhine state, Northern and Southern Shan state. In order to plan for
trainings to strengthen the technical knowledge and skills of the BHS at the implementing level,
township selection meetings were organized in June and July 2017, through coordination with
States and Regional Health Departments and training teams. Township selection criteria were
8
based on (i) high under-5 mortality rate (ii) inclusion in the 151-township list (those that have
completed a previous IMNCI training) and (iii) inclusion in the National Health Plan Year-1
townships list. The Child Health Development Division, MOHS has a plan to provide the
updated IMNCI guideline training to the remainder of the 181 townships in 2018 and onward.
According to the selection criteria, there were six townships selected for implementation of
IMNCI (2-59 months) training and follow-up activities. They are: Taungdwingyi township
(Magway region), Ingapu township (Ayeyarwaddy region), Minbya township (Rakhine state),
Tang Yan and Mongyai townships (N Shan state) and Mong Kai township (S Shan state).
Among the six townships selected for IMNCI implementation, Taungdwingyi township
(Magway) had the largest total population and largest under-1 population. Minbya township
(Rakhine) had the largest under-5 children population. Mongyai township (N. Shan) had the
highest IMR and Mong Kai township (S. Shan) had the second highest IMR. Mong Kai
township (S. Shan) had the highest U5 mortality rate and Mongyai township (N. Shan) had the
second highest U5 MR.
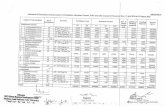
Table 1. Geographical situation and 2017 health profile data of implementing townships
Ref. Township Health
Profile 2017 2017 2017 2016 2017 2016
State/ Region Magway Ayeyarwaddy Rakhine N Shan S Shan
Township Taungdwingyi Ingapu Minbya Tang Yan Mongyai Mong Kai
Area (Sq. Kilometer) 1968 1005
1,338
4,710
1,693
2,120 sq.
miles
Total Population 277,736 221,912
221,381
170,512
63,705
74,895
Under 1 population 4,349 3,587
4,244
3,693
1,368
1,640
Under 5 population 20,699 16,072
22,035
16,836
6,951
8,328
No. of existing total BHS
(HA, LHV, midwife, PHS I,
II) 146 178
92
48
39
28
Health Infrastructure
i) Township hospital 1 1 1 1 1 1
ii) Station hospital 2 4 1 0 0 0
iii) UHC 1 1 0 0 0 1
iv) MCH unit 1 1 1 1 1 1
v) RHC 8 11 6 4 3 3
vi) sub-center 40 52 29 16 16 9
IMR per 1,000 LB 11.98 (2016) 6.1 (2017) 15 (2017) 13.4(2016) 22.1(2017) 19.1(2016)
U5 MR per 1,000 LB 13.82 (2016) 8 (2017) 18 (2017) 16.6(2016) 26.37(2017) 34(2016)
10
3.4 Training
3.4.1 Central MToT updated IMNCI training, Nay Pyi Taw
The Central MToT training on the updated IMNCI guidelines was conducted from 27th to 30th
November 2017, in Man Myanmar Hotel, Nay Pyi Taw. Twelve medical doctors/team leaders,
8 nursing officers and 1 Health Assistant, from the five State and Regional Health Department
training teams attended the training, for a total of 21 participants. There were 5 participants
each from Magway, Ayeyarwaddy and N. Shan, 4 from S. Shan and 2 from Rakhine state. The
training was held for four days and led by 8 trainers from the Child Health Development
Division, MOHS, including two Deputy Directors, Dr. Theingi Aung and Dr. Thida Win. Five
MCSP staff from the Child Health Team also participated in the training. Each trainer and
participant was provided with a package of updated IMNCI guideline (10 books with 1 learning
DVD and 1 power point CD). The training methodology used included lectures, two-way
discussions, group work, presentations, role-plays and clinical skills assessments by
performing Objective Structured Clinical Examination (OSCE). The knowledge of the
participants was assessed by pre- and post training test questionnaires. Training aids were used
by the trainers for demonstration to the participants. Based on their implementation experience
in the field, the training participants provided feedback and suggestions on the updated
guidelines. The two Deputy Directors and the CHD trainers reviewed the inputs and made some
minor adjustments technically. The revised version of the updated guideline was used for all
subsequent training sessions.
Photo 1: Updated IMNCI Central MToT Training, Naypyitaw, November 2017
11
3.4.2 Central MToT Follow-up training, Nay Pyi Taw
The follow-up training was organized about 6 weeks after the central MToT, from 10th to 12th
January, 2018 in Nay Pyi Taw. The participants were primarily the same as those who attended
the Central MToT. The follow-up training is the second part of IMNCI training and is intended
to strengthen the clinical skills management of BHS, to address the challenges found in
utilizing the IMNCI guideline, to understand the general situation on the ground and to collect
the data and information from the supervision visits. The supervision team is composed of
trainers from State and Regional training teams and township training teams. During the
follow-up training, the trainers/supervisors focused on ways of assessing the BHS to enhance
understanding of the importance of post-training supervision visits, how to use the supervision
checklists and follow-up forms, to assess the health center infrastructure and drug stock
management, how to conduct data recording and preparing the supervision report.
Eighteen participants attended the
training from the States and Regional
training teams. It was a three-day
training led by 5 trainers from the
Child Health Development Division,
MOHS, Nay Pyi Taw. On Day 1, the
participants learned how to use the
follow-up forms, supervision checklist,
and formats. On Day 2, the participants
had a field visit to a nearby RHC and
sub-center to practice the supervision
activity with BHS and caretakers of
under-5 children. Ah Lyin Lo RHC
was visited in the morning and Pauk
Taw sub-center in the afternoon.
Participants (supervisors from each
state and region) were divided into four
groups. Two groups observed the BHS
conducting clinical care management
and provided the assessment scores by
using the supervision checklists, while
the other two groups practiced the
supervision of the drug stock
management. At the end of the visit,
the supervisors combined their
findings and provided feedback to the
BHS on their performance and
practice. The supervision report, with comments and recommendations, was sent to the Child
Health Development Division, MOHS, Nay Pyi Taw. Seven MCSP staff participated in the
field visit of supervision activity and provided comments and suggestions.
On Day 3, the participants presented their findings with recommendations for group discussion.
Each state and regional team prepared their supervision visit plans with support from the Child
Health Development Division trainers. It was a good opportunity for the state and regional
Photo 2: Field visit to A Lyin Lo RHC, Central
MToT Follow Up after Training, Naypyitaw,
January 2018
12
trainers to meet with the trainers of the Child Health Development Division for sharing
experiences, constraints and challenges, which were useful inputs for planning future
supervision visits.
3.4.3 State and Regional ToT training
State and Regional level ToT trainings were conducted in each of the five selected States and
Regions after the central MToT training in Nay Pyi Taw in December 2017 and January 2018.
The selected State and Regional training team members who attended the central MToT
disseminated the training to the other training team members of the State/ Region and township
training teams of NHP Year-1 townships. These trainings were usually conducted in the
training hall of the State and Regional Health Department. Each participant was provided with
the updated IMNCI guideline package. The training aid materials were used for demonstration
and practice during the trainings. Details of the individual State and Regional-level trainings
are included later in this report under Section 4.
3.4.4 State and Regional ToT for Follow-up training
The follow-up training was usually organized in state and regional health departments of the 5
states and regions at least one month after the State and Regional ToT training, with almost the
same individual participants. Follow-up training was focused on utilization of forms and
formats, supervision checklist, organizing supervision plans, and assessment of the clinical
skills management of the trained BHS. The participants of the follow-up training were
members of the State and Regional Training teams and Township Training teams. The follow-
up guideline booklet was used, with some revised forms with additional checklists, and based
on the updated IMNCI guideline. The training curriculum contained lectures in the training hall
and field visits to nearby health centers for practice.
3.4.5 Township-level multiplier training
The trained State, Regional and Township training team trainers conducted the multiplier
training to the Lady Health Visitors (LHV) and Midwives (MW) of the 6 selected townships
from January to April 2018. It was the 5-day training with lectures, individual and group
discussion, learning through video clips. The clinical skills management of the BHS was
assessed through use of case scenarios in OSCE sessions.
3.5 Continuing Medical Education session
MCSP prepared two CME modules on Pneumonia and Diarrhea, based on the updated IMNCI
guidelines. This was developed as a package, ready to be utilized in the monthly CME sessions
at the township level to refresh the BHS knowledge on common childhood illness, management
and treatment. The BHS will share their experience on case management, problems, challenges
and finding solutions through group work and discussion. There was one CME module session
conducted in Mong Kai township, S. Shan state on 30th March 2018, covering both diarrhoea
and pneumonia for 49 BHS, utilizing the new modules.
13
3.6 Learning and Performance Improvement Centers
L&PICs were set up in each
State and Regional Health
Department of the five selected
States and Regions; Magway,
Pathein, Sittwe, Lashio and
Taunggyi. They contain
maternal, newborn and child
health training materials and
are meant to support the clinical
practice of trained participants.
Some MOHS staff, which were
members of the state training
teams, were trained as skill lab
coordinators. The training and
practical sessions were
conducted in the L&PIC for the
BHS to practice their clinical
skills for patient management.
At the end of the implementation, training materials along with updated IMNCI guidelines and
CME module handouts were handed over to the L&PICs.
3.7 Post-training supervision visits
Post-training supervision visits were usually conducted about one month after the IMNCI
training to the BHS at the township level. These visits were intended to assess the clinical skills
management of the trained BHS to ensure quality care and treatment of under-5 children
according to the IMNCI guidelines. Additionally, the drug stock management and health
infrastructure were assessed. The number of supervised BHS and health centers were selected
by the state and township training teams, based on the availability of supervision teams and
accessibility of the health centers and the BHS. All supervision visits were joint visits done by
the MOHS staff and MCSP Program Officers. The supervisory team was divided into groups
and assessed the BHS on their ability to follow the guidelines, proper use of handbills, use of
the patient record form in screening diseases, and utilization of the materials in the health
centers for diagnosis of the patients. Supervisors assessed every step of patient management
using the standard checklists.
At the end of the visit, the supervisors provided feedback to the supervised BHS, recognized
their efforts, discussed about strong and weak points, and suggested solutions for better
achievements in the future. The supervision reports prepared by the supervisory teams were
submitted to the Child Health Development Division, MOHS, Nay Pyi Taw. There were post-
training supervision checklist forms used by the supervisors to assess the ability of the BHS on
clinical skill management according to the IMNCI guidelines. If the performance of BHS in
case management was correct according to the supervisor checklist, it was recorded as "1"
scores and if not, it was recorded as "0" score.
Photo 3: Learning and Performance Improvement Center
Opening Ceremony, Magway, February 2018
14
4. Implementation activity in 5 selected States and Regions
4.1 Magway region
Training
The State and Regional ToT training was organized for four days from 27th to 30th December
2017, in Magway. There were 25 participants from the Regional and Township training teams
of the National Health Plan (NHP) year-1 townships, namely Taungdwingyi, Saytottara,
Myaing, Htilin and Minhla townships. The training was led by 5 trainers of the Regional
training team in Magway, consisting of 3 medical doctors/Team leaders, 1 Nursing Officer and
1 Health Assistant. (Annex 5 and 6)
The State and Regional ToT for follow-up training was organized from 1st to 3rd February 2018
for the same 25 participants. The training was conducted both in the training hall of Magway
Regional Health Department and the Rural Health Centers during the field visit. On Day 1, Dr.
Ohnmar Aye, Assistant
Director of the Regional Public
Health Department of Magway,
and Dr. Khine Su Mar, Team
Leader of the Child Health team
in Magway, explained about the
forms and formats used in the
supervision visit. On Day 2, the
participants were divided into
two groups for the field visit to
Daung Nay RHC and Kan Thar
Gyi sub-center to practice
supervision. In the morning
session of Day 3, the
supervision teams presented
their findings and comments in
individual groups. In the CME
session in the afternoon, under
the guidance of the trainers, the participants became familiar with the diarrhea and pneumonia
modules to be used at the township level in the monthly CME sessions.
In Taungdwingyi township there were two batches of multiplier training conducted on 15th to
19th January and 15th to 19th February 2018. A total of 60 BHS (4 LHV and 56 Midwives) were
trained out of existing 68 BHS, with 30 participants in each batch. There were 5 trainers (2
medical doctors, 2 HA and 1 LHV) in the first batch and 4 trainers (2 HA, 1 Township Health
Nurse and 1 LHV) in the second batch of multiplier training (Annex 5 and 7).
Post-training supervision visits/ Follow-up activity
Post-training supervision visits were conducted in Taungdwingyi township from 8th to 12th
March and 15th to 19th March 2018. The field visits were led by three supervisors/trainers from
the Regional Training team and 1 trainer from the township training team, jointly with Dr. Han
Set Lu, MCSP Program Officer. During the visits, 4 trained LHVs and 22 midwives out of 56
Photo 4: Field Visit, State Level Follow Up after Training,
Magway, February 2018
15
trained were supervised. The supervision team reached 7 out of 8 RHCs and 14/36 sub-centers
for the BHS supervision and drug stock and infrastructure management (Annex 5, 7 and 8).
Findings (Taungdwingyi township, Magway region)
Assessment of BHS
Among supervised BHS, 95% checked the general danger signs and 100% checked the
symptoms of four main diseases (cough, diarrhea, fever and ear problems). Only 73% of
supervised BHS checked the HIV status, and 68% assessed growth and development.
All supervised BHS (100%) correctly performed the case management on referral cases
according to the supervisory checklist. Eighty-six percent of supervised BHS performed
correctly while providing suggestions to mothers for patient care for diarrhoea at home and
mentioned two danger signs for immediate return to the health center. More than 90% of BHS
were able to assess the immunization status, assess the feeding practice of the child and provide
counseling to mother on feeding and proper nutrition according to the checklist.
Assessment of caretakers or mothers
Twenty-two mothers or caretakers with child patients were interviewed as part of the
assessment. More than 90% of interviewed mothers were able to describe the correct home
treatment and ORS solution preparation. All of them (100%) were able to describe three home
care methods for the child patients.
All mothers (100%) said that they were satisfied with the performance of the BHS on case
management of the patients, including duration of patient examination, treatment provision and
communication with the mothers. Some of them (95%) mentioned that they received additional
health knowledge from the BHS.
Health infrastructure and drug stock management
There were 21 health centers (7 RHC and 14 sub-centers) assessed by the supervision team.
All the basic health infrastructure materials such as weighing machines, wall clock, IMNCI
guidelines (2017) package, MCH booklet and patient registers were available in all health
centers (100%). The general patient register, for use on a daily basis, and a specific patient
register for the 0-59 month patients were both available in every RHC and sub-center.
ORT corners were available in 38 % of the health centers only and ORT register books were
present in 29% of health centers. However, most health centers (90%) had availability of
drinking water and essential materials for establishing an ORT corner.
All health centers (100%) had proper cold chain system, vaccine storage and availability of all
types of vaccines. None of them had functioning sterilizers for disinfection purposes. All health
centers (100%) had patient treatment records, but only 38% of them completed the patient
record forms in the OPD.
In the drug lists of all health centers, there was no stock of Injection Diazepam, inhaled
bronchodilators, spacers, Injection Artesunate, Ready-To-Use Therapeutic Food (RUTF) and
ART drugs.
16
Amoxicillin capsules, Paracetamol tablets, ORS sachets, Vitamin A capsules and Albendazole
deworming agents were available in all health centers (100%). Nystatin syrup and nasal tubes
were available only in 14% of health centers. Anti-malaria drugs such as Chloroquine and
Primaquine tablets were available in only 10% of health centers.
4.2 Ayeyarwaddy region
Training
The State and Regional ToT training was from 26th to 29th December 2017, and attended by 20
participants; 2 from the Regional training team and 18 from the NHP Year-1 township training
teams of Pantanaw, Kanguidaunt, Ingapu, Kyan Khin, Lay Myat Hnar and Yay Kyi townships.
The participants were 2 medical doctors, 13 LHV, 4 THN and 1 Midwife. The training was led
by 6 trainers (4 medical doctors and 2 senior nurses). Four trainers were from the Ayeyarwaddy
Regional Health Department and Dr. Thida Win, Deputy Director of CHD joined the training
as technical support from Nay Pyi Taw.
The Follow-up training was organized from 19th to 21st March 2018, and attended by 21
participants/trainers - 3 persons from State Training team and 18 persons from the NHP year-
1 township training team. On days 1 and 3, training was organized in the training hall of the
Regional Public Health Department, Pathein, and there was a field visit on Day 2 to an RHC
and sub-centers. The supervision team divided into four groups for practicing the activities.
The training and supervision visits were led by four trainers from the Regional training team
(2 medical doctors, 1 THN and 1 Nursing Officer). Dr. Aung Kyaw Htwe, the Regional Health
Director, provided the closing remarks on the last day of the training.
In Ingapu township, three batches of township-level multiplier training were conducted on 15th
to 19th January, 3rd to 7th February and 5th to 9th March 2018 for 75 BHS (4 LHVs and 71
midwives from 1 MCH, 11 RHC and 51 sub-centers). The training was led by 6 trainers in
Batch 1, 5 in Batch 2, and 4 in Batch 3, all from the Regional and Township training teams.
Dr. Myo Swe, MCSP Program Officer, participated in all three batches as the facilitator,
working in close collaboration with the MOHS training teams (Annex 5 and 8).
Post-training supervision visits
Out of 75 trained BHS in Ingapu township, post-training supervision visits were conducted to
25 midwives (33%) from 1 MCH, 6 RHCs and 13 sub-centers. There was some limitation of
transport due to flooding in the area and only 32% of health centers were accessed during the
supervision visits. The midwives from other RHCs and sub-centers came to these health centers
for assessment of their knowledge and clinical skills. The supervisory team was composed of
1 Medical Doctor (Child Health team leader), 1THN, 2LHVs, and Dr. Myo Swe (Program
Officer of MCSP) for the joint supervision visits. The field visits were conducted on 27th
February, 20th March, and 26th to 30th March 2018 (Annex 5, 7 and 8).
Findings (Ingapu township, Ayeyarwaddy region)
17
Assessment of BHS
All supervised BHS (100%) checked the general danger signs and symptoms of four main
diseases (cough, diarrhea, fever and ear problems). More than 90% of supervised BHS checked
the child’s nutritional status, EPI and mouth and gum problems. Eighty-eight percent of BHS
checked the HIV status and growth and development of child patient.
All BHS (100%) had good knowledge about patient referral criteria and performed the referral
service well, according to the supervisory checklist. All of them provided the oral antibiotics
and anti-malaria drugs correctly according to the checklist. More than 80% of BHS knew the
correct treatment for diarrhoea patients and stated two danger signs for emergency return,
according to the supervisors' assessment. Almost all BHS (96%) were able to provide
information and management on immunization as required for the child patient. Only 72% of
BHS assessed the feeding practice and 84% conducted counseling to mothers.
Half of the supervised BHS (48%) asked the mother about other health problems of the child.
Assessment of caretakers or mothers
Twenty-five mothers or caretakers were interviewed as part of the supervision activity. All
interviewed mothers (100%) were able to describe the home treatment of diarrhea and ORS
solution preparation for the child patient; 96% of them knew three home care methods. All
interviewed mothers (100%) said that they were satisfied with the performance of the BHS on
case management, patient examination, treatment and health education provision.
Health infrastructure and drug stock management
There were 20 health centers out of 63 trained (32%) assessed by the supervision team. Some
health centers were not accessible due to limited transportation, damaged bridges and flooding.
All the basic health infrastructure materials such as weighing machines, wall clock, IMNCI
guidelines package, MCH booklet and patient register books were available in all health
centers. Patient treatment records were completely filled up with treatment information
(100%). There was an ORT corner in all health centers (100%) along with the essential
materials and drinking water. None of health centers had an ORT register book. For the EPI
activity, there was a proper cold chain system, and all types of vaccines were stored in the
functioning storage system. But there was no specific sterilizer used in the health centers for
EPI activity because disposable syringes were used.
There was no stock of Injection Gentamycin in any of the health centers. ORS sachets were
available in nearly half of health centers (45%). There was a shortage of some drugs and
materials in health centers. It was found the availability of the drugs as Primaquine tables
(35%), Ciprofloxacin capsules (25%), cannula (30%) and nasal tubes (25%). There was no use
of Bin cards in some health centers, according to the comments of the supervision team.
As Ingapu township is not a malaria-endemic area, only Rapid Diagnostic Test kits are
provided to the BHS. If the patient is RDT positive, he or she will be referred to the Ingapu
township hospital for anti-malaria drugs and further treatment. ART drugs were basically not
available in the RHC and sub-centers, and the HIV positive patients can get drugs from the
township NAP team, after proper counseling. Some drugs and commodities were in shortage
such as Nystatin syrup, disposable syringes and Gentian violet. Oral salbutamol tablets, inhaled
18
bronchodilator and nasal tubes were requested from the Regional to the central level for
procurement next year.
4.3 Rakhine state
Training
The state and regional ToT on the
updated IMNCI guideline was
organized in Sittwe General
Hospital Meeting hall, from 15th to
18th January 2018. There were 3
participants from each NHP year-
1 township in Rakhine State
(Pauktaw, Minbya, Ponnagyun
and Gwa) and 5 participants from
the state training team, for a total
20 participants. Myebon township
was added by the MOHS for
training. It was a four-day
training, led by 4 trainers who had
attended the Central MToT of
IMNCI. Dr. Thida Win, Deputy
Director of Child Health
Development Division, also joined as a trainer (Annex and 6).
The Township Multiplier training on the updated IMNCI guideline was conducted in Minbya
township in two batches. The first batch was conducted from 23rd to 27th February and the
second batch was from 25th to 29th March 2018 in Minbya General Hospital. A total of 45 BHS
(7 LHVs and 38 midwifes) participated in two batches. Dr. Aung Than Oo, Program Officer of
MCSP, participated in all trainings as a facilitator (Annex 5 and 7).
Post-training supervision visit
The visits were conducted in Minbya township from 5th to 18th May, 2018. The supervisors
were 2 trainers from the State health training team and 3 from the township health training
team, supported by Dr. Aung Than Oo, Program Officer of MCSP. Three LHVs (42% of those
trained) and 20 midwives (53% of trained MWs) of 1 MCH, 6 RHCs and 13 sub-centers were
supervised in the follow up visits (Annex 7 and 8).
Findings (Minbya township, Rakhine state)
Assessment of BHS
There were 23 BHS (3 LHV and 20 midwives) supervised out of 45 trained (51%). All
supervised BHS (100%) checked the general danger signs, signs and symptoms of four main
diseases. All of them assessed the nutritional status of the patient and checked the signs and
Photo 5: Role-play Activity, IMNCI Updated Guideline
State Level Training, Sittwe, Rakhine state, January
2018
19
symptoms of mouth and gum disease. Only 48% of supervised BHS checked the growth and
development of the child patient.
All supervised BHS (100%) knew the criteria for classification of diseases and followed the
IMNCI guidelines for patient referral in required cases. All of them (100%) correctly
performed the case management in providing oral antibiotics and treatment with ORS solution
according the supervisory checklist. All supervised BHS (100%) assessed the immunization
status of the child, checked other health problems and counseled the mother for proper feeding
of the child until 2 years of age, according to the checklist used by the supervision team.
Assessment of caretakers or mothers
Almost all (96%) of the interviewed persons knew the home treatment of the sick child and
ORS solution preparation and three home care methods. All respondents (100%) said they were
satisfied with the performance of the BHS on case management, examination, treatment and
communication skills. All of caretakers (100%) discussed with the BHS about common child
health problems.
Health infrastructure and drug stock managements
One MCH (100%), 6 RHC (100%) and 13 sub-centers (45%) were supervised. Weighing
machines, wall clocks, MNCI guidelines and MCH booklets were available in all supervised
health centers (100%). Ninety-five percent of health centers had patient register books with
complete treatment records. Only 30% of health centers had ORT corners. However, all of
them had drinking water and essential materials for ORS preparation. None of them had an
ORT register book. For EPI activities, all supervised health centers (100%) had cold chain
facility, immunization records, and all types of vaccines under the proper storage system. All
health centers did not have a specific sterilizer. The BHS used disposable syringes during EPI
activities and for providing injectable drugs to patients. Injection Diazepam, injection
Artesunate, inhaled bronchodilator, spacers, ART for HIV patients, iron syrup, Nystatin syrup
and nasal tubes were not available in all supervised health centers. Antibiotics, such as
injectable Ampicillin and injectable Gentamycin were available in some health centers only
(26% - 30%). The majority of essential drugs and materials were available in most of the
supervised health centers (83% and above).
4.4 Northern Shan state
Training
The State and Regional ToT training was organized for four days from 27th to 30th December
2017, in Lashio. The training was attended by 14 participants from State and township training
teams from the five NHP- year 1 townships (Tang Yan, Mongyai, Muse, Mabein, Moe Meik
and Hopan townships).
The State ToT of Follow-up training was organized from 5th to 7th March 2018 for the 13
participants who had already attended the IMNCI State ToT training. On Day 1, Dr. Aung Than
Swe, Child health team leader, Dr. Nwe Nwe Win and Daw Nang Mwe Lin San led the lectures.
On the second day, participants divided into 3 groups and went to Enai RHC for supervision
practice on clinical case management and stock management. In the afternoon, participants
presented their findings and discussed the results. On Day 3, CME modules on diarrhoea and
20
pneumonia were introduced. The CME handouts, handbill and power point presentations were
distributed to each participant and module exercises were conducted.
In Northern Shan State,
Township level IMNCI
Multiplier trainings were
conducted in Mongyai and
Tang Yan townships. In
Mongyai Township, it was
organized in the training hall of
township health department
from 27th to 30th March 2018. It
was attended by 20 BHS (1
LHV and 19 midwives) out of
the existing 26. The training
was led by 4 trainers from the
Township health training team.
In Tang Yan Township, the
township level multiplier
training was organized in the
township health department
training hall from 27th to 30th
April 2018. It was attended by 30 BHS (1 LHV and 29 midwives). The training was led by 5
trainers from the Township Health training team. Trainings were facilitated by Dr. Thu Naing
and Dr. Han Set Lu, Program Officers of MCSP (Annex 5 and 7).
Post-training supervision visits
Mongyai Township
Post-training supervision visits were conducted in Mongyai Township from 14th to 16th May.
The field visits were led by three supervisors/trainers, one from the Regional training team and
2 trainers from the Township training team, jointly with Dr. Han Set Lu, MCSP Program
Officer. During the visit, 7 midwives out of 20 trained BHS (35%) were supervised. The
supervision team reached 1 out of 2 RHCs and 6 sub-centers out of 16 sub-centers for the BHS
supervision and drug stock and infrastructure management (Annex 7and 8).
Findings
Assessment of BHS
Out of 20 trained BHS, 7 BHS were supervised by the State and township training team and
MCSP Program Officer. Eighty-six percent of supervised BHS checked the general danger
signs and all of them (100%) checked the symptoms of four main diseases (cough, diarrhoea,
fever and ear problems). The HIV, EPI status, and growth and development of the child were
assessed by 71% of supervised BHS, while 57% checked on nutritional status and mouth and
gum problems of the child patients.
Photo 6: OSCE Examination, IMNCI Updated IMNCI
Guideline BHS Level Training, Tang Yan, N Shan state,
April 2018
21
All supervised BHS (100%) knew the criteria for referral cases and provided the pre-referral
services as required for the patients, according to the supervisory checklist. All BHS (100%)
correctly performed provision of oral antibiotics including anti-malaria drugs according to the
checklist. Most BHS (86%) correctly performed treatment for diarrhoea patients and explained
about two danger signs for emergency return. Immunization status of child patients was
checked by 86% of supervised BHS. All BHS (100%) assessed the feeding of children less
than 2 years and 86% conducted counseling to the mothers for proper feeding practice.
Assessment of caretakers or mothers
Seven mothers or caretakers of sick children were interviewed during the assessment. All
mothers (100%) were able to describe the home treatment and ORS solution preparation and
86% knew about the home care methods. All interviewed mothers (100%) said that they were
satisfied with the performance of the BHS on case management and 86% highlighted that they
received health information and knowledge from the BHS.
Health infrastructure and drug stock management
There were 7 Health centers (1 RHC and 6 sub-centers) assessed by the supervision team. All
the basic health infrastructure materials such as weighing machines, wall clock, IMNCI
guidelines (2017) package, MCH booklet/mother’s card and patient register books were
available in all health centers (100%).
There was no area specifically identified as an ORT corner in all health centers and none had
an ORT register book. However, essential materials for ORT treatment were available in all
health centers (100%) and drinking water was available in 86% of health centers. In all health
centers (100%), all types of vaccines were available, kept properly in a cold chain system and
storage. Immunization records were found in all health centers but there were no functioning
sterilizers. Patient treatment records were properly used in all health centers, but only in 71%
of health centers were the forms completely filled up.
In all health centers, there were no stock of Injection Diazepam, inhaled bronchodilators,
spacer, Injection Artesunate, ART, RUTF, Iron syrup, Gentian violet, cannulas and nasal tube.
Oral anti-malaria drugs were available in more than half of the health centers. Two types of
disposable syringes were available only in 14% of health centers. However ORS sachets,
Paracetamol tablets, Iron/Folate tablets and deworming agents were available in all health
centers (100%).
Post-training supervision visits
Tang Yan Township
Post-training supervision visits were conducted in Tang Yan Township from 28th to 30th May.
The field visits were led by three supervisors/trainers, one from the State Training team and 2
trainers from the township training team, jointly with Dr. Aung Than Oo, MCSP Program
Officer. There were 10 BHS (1 LHV and 9 midwives) supervised in 1 MCH center, 2 RHCs
and 3 sub-centers (Annex 5, 7 and 8).
22
Findings
Skills assessment of BHS
Almost all BHS (90%) assessed general danger signs and symptoms of four main diseases in
childhood illnesses. All supervised BHS (100%) assessed the status of Nutrition, HIV, EPI and
mouth and gum condition in children. However only 70% of BHS assessed the growth and
development of children.
All BHS (100%) knew the referral criteria for severe patients and knew how to provide pre-
referral services according to the supervisory checklist. They all (100%) knew how to provide
oral antibiotics and anti-malaria drugs to those in need. According to the checklist of the
supervisors, all BHS (100%) knew to provide suggestions for home care management for the
sick child and danger signs for immediate return to the health centers. Only 70% of BHS
assessed the immunization status of the child and discussed appointments for next visits for the
children in need. Only 60% of BHS assessed the feeding practice of children under 2 and 70%
conducted counseling to the mother on child feeding practices. Less than half of BHS (40%)
discussed about other health problems of the children.
Assessment of caretakers or mothers
There were 10 mothers interviewed and all of them (100%) were able to describe the home
treatment and ORS solution preparation. All of them knew three home care methods in the
treatment of diarrhoea. All interviewees said they were satisfied with the case management of
the BHS and 60% of them received health education from the BHS.
Health infrastructure and drug stock management
There were 6 health centers supervised and all of them (100%) had basic infrastructure and
materials such as weighing machine, wall clock, IMNCI guidelines, MCH booklet and patient
register books.
None of the supervised health centers had a specific identified place for the ORT corner, but
all of them had an ORT register book. Many health centers had drinking water (83%) and
essential materials for an ORT corner (67%). All supervised health centers (100%) had an
effective cold chain system, proper vaccine storage, accessible immunization records and all
types of vaccines available. None of them used sterilizers because all BHS used disposable
syringes and needles. All health centers had patient treatment records and they were completely
filled up.
In the drug storage, all health centers did not have Injection Diazepam, Injection Artesunate,
inhaled bronchodilators, spacer, RUTF, iron syrup, nasal tubes and ART drugs. ORS sachets
were found available in all health centers (100%). Anti-malaria drugs such as ACT tablets were
available in 50% of health centers, while Chloroquine and Primaquine tablets were available
only in 33%. Cotrimoxazole tablets, Gentian violet and cannula were available in only 17% of
health centers.
23
4.5 Southern Shan state
The State and Regional ToT training was conducted from 16th to 19th January 2018, attended
by 24 participants, with 3 participants each from the township training teams in Mong Kai,
Mong Hsu, Pindaya, Ywa Ngan, Mauk Mai, Lang Kho, Mong Pan, and Nan Sang townships.
The participants were 4 medical doctors, 5 THNs, 1 LHV, 8 Senior Nurses and 6 Trained
Nurses. The training was led by 5 trainers, namely 3 medical doctors and 2 senior nurses, from
the State training team.
The Follow-up training was done from 13th to 16th February, for the same 24 participants. The
training was led by 5 trainers from the State Training team, composed of 3 Medical doctors, 1
District Public Health Nurse and 1 Nursing Officer. It was organized for four days, with the
initial 3 days consisting of lectures and field visits to Nam Kok RHC and Long Hay sub-center
for practice. On the 4th day, the participants learned about use of the CME modules under the
guidance of the trainers. Dr. Kaung Myat Bo, MCSP Program Officer, participated in all
activities from training to supervision visits in close collaboration with the MOHS team. The
supervision visit plan was prepared by the township supervision teams, in discussion with the
state training teams and MCSP staff.
The township-level multiplier training was organized in the training hall of Mong Kai township
health department on 21st to 25th February 2018. It was attended by 22 BHS (4 LHVs and 18
midwives) from the Urban Health Center, MCH center, 3 RHC and 9 sub-centers. The training
was led by 7 trainers (2 medical doctors and 5 nurses) from the State and township training
team.
Photo 7: Field visit group photo, IMNCI State Level Follow Up after Training, Long Hay Sub-
center, Hopong Township, Southern Shan state , February 2018
24
CME session
MCSP introduced the two CME
modules on Pneumonia and
Diarrhoea at the monthly CME
sessions in the township
meeting hall on 30th March
2018. A total of 49 BHS from
all RHC and sub-centers and
two staff from the township
hospital participated. Each
participant was provided with
the handout for the modules and
handbills. Five trainers from the
State and township training
teams led the session and
explained about the two
common childhood diseases by
using power point
presentations. The participants refreshed their knowledge by using the handbills and shared
their experience of case management in health centers for cases of pneumonia and diarrhea in
children.
Post-training supervision visits (Mong Kai Township, S Shan state)
During the supervision visits conducted from 28th March to 2nd April 2018, 3 out of 4 trained
LHV (75%) and 13 out of 18 trained midwives (72 %) were assessed and supervised. The
Urban Health Center, MCH and 3 RHCs were supervised, along with 3 sub-centers out of 9
sub-centers (33%). Dr. Kaung Myat Bo participated in the supervision visits along with three
township supervisors, to support and facilitate the activity (Annex 5, 7 and 8).
Findings
Out of 22 BHS trained, 16 were jointly supervised by the township training team and MCSP
Program Officer. All supervised BHS (100%) checked the general danger signs and 88%
checked the symptoms of four main diseases. Almost all BHS (94%) checked the status of the
patient on EPI, Nutrition and mouth and gum problems. Around 70% of BHS checked HIV
status and growth and development of the child.
All supervised BHS (100%) correctly knew about the criteria for referral of severely ill patients
and conducted the pre-referral service according to the checklist. All BHS (100%) correctly
performed while providing oral antibiotics and anti-malaria drugs according to the supervisory
checklist. The majority of BHS (88%) provided suggestions on diarrhoea management at home
and explained about two danger signs for immediate return (94%). All BHS (100%) did not
miss to check the immunization status of the child and made an appointment for the next
immunization of the children in need. More than 75% of supervised BHS assessed the feeding
practice of the child and counseled the mother for proper feeding practices for children under
2 years. All the supervised BHS (100%) asked the mother about other health problems of the
Photo 8: CME Activity, Mong Kai Township, S Shan state,
March 2018
25
child. Due to renovation work, there was not enough space for patient care in two sub-centers.
Health centers were open from 9 am to 4 pm every day, however they were accessible anytime
for emergency cases.
Assessment of caretakers or mothers
There were 16 mothers interviewed for their opinion on the BHS's performance. In assessing
the mothers' knowledge on treatment provided, 100% of interviewed mothers were able to
describe the home treatment for their child’s illness and ORS solution preparation according to
the checklist. Additionally, 94% of them well knew about three home care methods.
Most interviewed mothers (94%) said that they were satisfied with the performance of the BHS
on case management, patient examination, treatment provision and health knowledge received
from the BHS.
Health infrastructure and drug stock management
There were 8 Health centers (1 UHC, 1 MCH, 3 RHC and 3 sub-centers) included in the
assessment visits. All the basic health infrastructure materials such as weighing machines, wall
clock, IMNCI guidelines (2017) package, MCH booklet and patient register book were
available in all heath centers (100%). There was an ORT corner with accessible drinking water
in every health center (100%). Only one third of health centers (38%) had the essential
materials for ORT corners and none of them had an ORT register book to record the cases
treated.
For the EPI activity, there was a proper cold chain system, vaccine storage and availability of
all types of vaccines in the health centers (100%). They said there was no sterilizer used in all
the health centers. The BHS used the disposable syringes during EPI activity and when
providing injectable drugs to the patients. All health centers (100%) had patient treatment
records in the OPD and they were completed with treatment information.
There was no stock of inhaled bronchodilators, spacer, RUTF, Nystatin syrup, cannula and
ART in supervised health centers. Drugs and consumables such as Injection Gentamycin, ORS
sachets, Zinc Sulphate tablets, ACT and paracetamol tablets were available in all health centers
(100%). Other essential drugs and consumables such as Inj. Ampicillin, Ciprofloxacin
capsules, some oral anti-malaria drugs and Iron/Folate tablets were available only in some
health centers (50-75%).
5. Summary of Training and Post-training supervision visits
5.1 Training
Both trainers and BHS were provided training on updated IMNCI guidelines. A total of 124
trainers from five States and Regions were trained during implementation. The highest number
of participants attending the ToT was in Magway region (30 pax) and the lowest number was
in Northern Shan state (19 participant trainers). Among the trained participants, 23% were
Medical doctors, 29% were LHVs and 15% were Township Health Nurses (Figure 1, Annex
6).
26
Fig 1. Number of participants who attended ToT from five States and Regions
There were 280 existing BHS (34 LHVs and 246 midwives) in six townships, which was the
target of MCSP for IMNCI training at township level. Out of them, a total of 252 BHS (21
LHVs and 231 midwives) participated in the training. Among those trained, 107 BHS (11
LHVs and 96 Midwives) were supervised. In total, 90% of existing BHS (LHVs and midwife)
participated in the training and 42% of the trained BHS were supervised. The trainer:
participant ratio was 1:5-8 in most trainings, in order to provide proper attention to the
participants by qualified trainers (Figure 2, Annex 7).
Fig 2. Percentage of BHS, trained and supervised in six selected townships (BHS: LHVs & midwife)
In six implementing townships, there were 206 existing health centers (UHC, MCH, RHC and
sub-centers). The BHS from 196 health centers participated in the township multiplier
trainings. Out of them, 82 heath centers were accessed during the post-training follow-up visits.
In total, 95% of existing health centers participated in the training and 42% of them were
included in the post-training supervision visits. The supervisors assessed clinical skills
28
19
22
25
30
S Shan state
N Shan state
Rakhine state
Ayeyarwaddy region
Magway region
NO. OF PARTICIPANTS WHO ATTENDED TOT(FIVE STATES & REGIONS)
88
% 94
%
87
% 94
%
77
%
10
0%
90
%
43
%
33
%
51
%
33
%
35
%
73
%
42
%
T A U N G D W I N G Y II N G A P U M I N B Y A T A N G Y A N M O N G Y A I M O N G K A I T O T A L
PERCENTAGE OF BHS (LHV & MIDWIFE) TRAINED AND SUPERVISED
% of BHS trained % of BHS supervised
27
management of BHS, health care facilities, health center infrastructure and drug stock
management (Figure 3, Annex 8).
Fig 3. Percentage of health centers, trained and supervised in six selected townships ( Health centers: UHC,
MCH, RHC, sub-center)
Each training participant was tested on their clinical skills assessment. There were three case
scenarios developed by the Child Health Development Division, and each participant in the
training selected one of them randomly. Three case scenarios were based on child patients with
signs and symptoms of several common childhood illnesses, such as diarrhoea, pneumonia,
asthma, growth and development problems. Within the time limitation, the participant filled up
the patient record form while presenting how to conduct the clinical examination and treatment.
To the trainer or examiner, the participant presented the steps of clinical assessment according
to the IMNCI guideline.
In all training batches, there was a remarkable increase in the assessment scores from Pre- test
to Post-test. The minimum average score increased from 2.7 to 6.8 (total possible score was
10) between Pre- and Post-tests. The maximum average scores increased from 4.9 to 8.1
between Pre- and Post-tests. In all implementation sites, the post-test scores were increased
between 1.4 times to 2.6 times over the pre-test scores (Fig.4).
Some individual scores in the Post-test reached 10 out of 10 among participants in trainings in
S Shan state. The percent increase overall was 45% in N Shan and 156% in S Shan (Annex 9
a, b).
The BHS required time to find the correct treatment selection and dosages in the handbills.
With practice they became more familiar with the handbill. Some BHS forgot to provide health
education messages to the mother and sometimes forgot to make an appointment for the follow-
up visit.
90
% 97
%
10
0%
90
% 95
% 10
0%
95
%
47
%
32
%
56
%
32
%
35
%
57
%
42
%
T A U N G D W I N G Y II N G A P U M I N B Y A T A N G Y A N M O N G Y A I M O N G K A I T O T A L
PERCENTAGE OF HEALTH CENTERS, TRAINED AND SUPERVISED
Health centers trained Health centers supervised
28
Fig 4. Pre- and Post-test scores achievement
Almost all BHS and supervisors were positive about the Updated IMNCI guidelines (2017),
as they felt it has been developed with a user-friendly design, and there were good linkages
between the provider guide, handbill, exercise book, photo book and video clips. The handbill
(chart booklet) is the most vital material, with key points of the IMNCI guidelines organized
concisely for the BHS, for easy access to essential information on patient care and treatment.
As it is a bit large and heavy, there is some limitation or challenge for the BHS to carry the
handbill to the mobile clinic service sites in the hard-to-reach areas.
Most BHS were pleased to use the patient record form, because by following the screening
method, there was very little chance of missing any common childhood illness.
One office copy of the updated IMNCI guidelines (2017) should be kept in the RHC and sub-
centers in case the trained BHS are transferred. Most BHS would prefer to take the IMNCI
guidelines materials package with them when they are transferred to another location. There
was some disagreement between the BHS and Health Assistants, as the latter would like the
guidelines to be left in the health center. To solve this problem, more copies need to be
provided.
The WHO video clips include counseling for the patient/caretaker, plus examination and
treatment, including for mother's care at home. These can be used as IEC materials to be shown
to the mothers in the health centers, during health education sessions to motivate and increase
public awareness about under-5 childcare and treatment.
One State Health Director pointed out that it is important to have a treatment and patient care
approach that is consistent in all States and Regions. The Updated IMNCI training should be
provided to the BHS of all townships throughout the entire country as soon as possible.
It has been suggested by the state and regional training teams that the updated IMNCI
guidelines (2017) be included in the pre-service training curriculum of the BHS in the
midwifery school and other related trainings.
Refresher training to the BHS and the supervisors is required to be included in the schedule
for every alternate year.
4.7 4.8
3.7
4.9
2.7
8.1
7.9
6.8 7
.1
6.9
M A G W A Y A Y E Y A R W A D D Y R A K H I N E N S H A N S S H A N
PRE- AND POST-TEST SCORES ASSESSMENT
Pre-test average scores Post-test average scores
29
The font of text in the handbill is small and some older BHS could not read the words properly.
The handbill was designed as a flow-chart with assessment, diagnosis, classification and
treatment in one page. Due to the limited space available, the small font size was used.
Training participants should be consistent (the same persons) for the whole training cascade,
as much as possible. New participants who have not participated in the State and Regional
training would find challenges to catch up with the activity in the Follow-up training.
It was suggested by trained BHS to include IMNCI review in the monthly meetings at
township level.
5.2 Post-training follow-up and supervision visits
5.2.1 Assessment on clinical skills
Almost all BHS (97%) assessed the general danger signs, four main signs and symptoms of
childhood illnesses. Ninety-three percent assessed the EPI status of the child and checked the
condition of the mouth and gums, while 92% checked the nutritional status of the patient.
Eighty-two percent of BHS checked the HIV status of mothers/caretakers and children.
However, only 70% of BHS assessed growth and development status of the children.
All BHS (100%) correctly knew the referral criteria and pre-referral service recommended
(providing intramuscular injection). According to the supervisory checklist, 100% of
supervised BHS correctly performed in providing oral antibiotics for child patients with
malaria, dysentery and ear infections while 98% performed correct pneumonia management.
More than 90% of the supervised BHS were able to decide which patients were in need of
diarrhoea treatment by ORS and conducted counseling on home-care management.
Ninety-three percent of supervised BHS checked the immunization status of the child patient
and made appointments for the next immunization as needed. Eighty-four percent of BHS
assessed the feeding practice of the mother for the child under 2 years of age and 88% provided
counseling to the mother for feeding and nutrition purposes. It was also found that 77% of BHS
assessed other health problems of children.
In assessing the mother's satisfaction, almost all of the interviewed mothers (98%) were able
to describe the home treatment for sick children and ORS solution preparation. Out of them,
96% were able to mention three home care methods for a child patient with diarrhoea.
It was found out that 99% of mothers were satisfied with the clinical case management of their
child by the BHS. All mothers (100%) were satisfied with the treatment provided and 93% of
interviewed mothers said that they gained health knowledge from the BHS.
5.2.2 Infrastructure
All supervised health centers (100%) had basic materials such as weighing machine, wall
clocks, IMNCI guideline, MCH booklet and 99% had a patient register book. Fifty-one percent
of health centers did not have a proper ORT corner. Most health centers had accessible drinking
water (95%) and essential materials for providing treatment (89%). Only 15% of health centers
had separate ORT register books. In the rest of the health centers, the diarrhoea patient data
were recorded in the general register.
30
All health centers (100%) had a functioning cold chain system with all types of vaccines
available. All health centers maintained a specific immunization register book. Disinfection
equipment, such as sterilizers, was not functioning or accessible in all health centers and BHS
used disposable syringes for the EPI program and other injections. All health centers (100 %)
had patient treatment records, but only 82% had complete records.
Some health centers were under renovation of their infrastructure, resulting in a lack of
feasibility to adequately observe the drug storage and management. There was limited space
for proper ORT corner set up, appropriate for child treatment. There was inadequate space for
the OPD and drug storage due to the damaged infrastructure in some health centers. Some sub-
centers had limited access to running water. Placing water containers in the building solved
this issue. There was inadequate furniture for proper storage of drugs and consumables in some
health centers.
5.2.3 Drug stock management
All health centers (100%) did not have inhaled bronchodilator, spacer and ART. HIV patients
went to the township NAP team for the ART.
Nearly 90% of health centers had ACT tablets for malaria, but only half of them (53%) had
Chloroquine and Primaquine tablets and18% of health centers had injection Artesunate.
There was a shortage of some essential drugs in health centers, resulting in limited availability
of injection Diazepam (8%), injection Ampicillin (44%), injection Gentamycin (49%), Gentian
violet (45%) and Nystatin syrup (23%). ORS sachets were seen in 85% of health centers. More
than 95% of health centers had Amoxicillin capsules, Paracetamol tablets, Vitamin A capsules
and deworming agents available. As consumable materials, cannula and scalp vein were
available in more than half of supervised health centers; nasal tubes were available in only 12%
of health centers.
The MOHS trainers and supervisors provided the following comments and
recommendations based on their findings during the supervision visits.
OPD: It was suggested by the supervisors that there should be separate ORT corners for
diarrhoea patients. Due to the limited availability of real patients, some non-patient children,
who had actually been ill and treated a few days earlier, were used for the practical sessions
during the supervision visits. Although the supervisors could not see the real treatment
situation, it was partially effective for them to observe how the trained BHS followed the
guidelines and used the patient record forms. The Health Assistants were motivated and eagerly
participated in the supervision visits. The BHS felt more confident in treating patients using
the updated IMNCI guidelines (2017) due to their clear instructions and guidance for treatment.
Regular supervision, at least quarterly, is needed to the trained BHS who are concerned with
providing IMNCI services for children 2-59 months. The high transport cost and workload of
both township supervisors and BHS are the main barriers to regular supervision to the trained
BHS for assessing their management of under-5 children. The patient record forms used by the
BHS and the supervision checklists used by the supervisors, need to be provided in sufficient
31
quantity. Some Health Assistants mentioned that they will provide the required forms by
photocopying them in the township health departments.
Interviews with mothers: In the interviews with mothers, no one refused to respond about the
HIV testing results during pregnancy and delivery. During the assessment of the mother's
experience and her opinion of the BHS and service of the health center, it sometimes happened
that the trained BHS were nearby, due to the limited physical space in the health centers.
Therefore, the feedback received from the mothers may not always have been accurate and
reliable.
Training guidelines and supervision tools: According to the updated IMNCI guidelines
(2017), the BHS clearly understood the disease classifications and the danger signs. The severe
patients were identified for early referral, for further health care management at a higher-level
facility. The BHS need to use the handbills and patient record forms in the management of
every case of childhood illness, in order to have more practice, and to improve their diagnosis
and treatment and confidence in using the tools.
Some indicators and definitions in the supervision check lists, such as sterilization materials,
patient register book, MCH booklet, need to be clear and consistently understood by the
supervisory teams in states and regions.
Register books, forms and formats: BHS are to be encouraged to use the patient record forms,
along with handbills, in the clinical management of every child patient. Most BHS have patient
register books in the health centers, which are used for all patient consultations. There were no
separate register books to record data for newborns and children 2-59 month. Supervisors
suggested that the BHS maintain the under-5 patient register separately.
By following the history-taking and screening process in the patient record forms, there was a
build-up of trust between the mother and the BHS. However, some mothers did not have
patience for the long duration of the assessment of the child, according to the guidelines and
patient record form. However, some mothers were pleased and satisfied with the thorough
assessment for accurate diagnosis and treatment.
As challenges, there were not enough referral forms to provide for the patients referred to the
higher health facilities. Due to difficult transportation, limited access to remote places and the
large workload of the BHS, there were no regular follow-up visits to the patients by the BHS.
There were limited transportation facilities in hard-to-reach areas, which affected the likelihood
of completed referral of patients to township hospitals from health centers.
Drugs and drug stock management: Most of the essential drugs needed for the treatment of
2-59 months children were available, with valid expiry dates, with the exception of: injectable
diazepam, bronchodilator inhalers, spacers, ready-to-use-therapeutic food (RUTF) for
malnourished children, anti-malaria drugs, antiretroviral therapy (ART) drugs and nasal tubes.
ART drugs were only available at ART centers at the township level. These required drugs and
materials will be on the procurement order of the MOHS for next year’s plan.
Rectal suppositories of Diazepam should be included in the drug procurement list and available
in health centers instead of Injectable Diazepam. Inj. Diazepam ampules were not provided to
the health centers due to their inclusion in the narcotic drugs group. The diagnosed HIV positive
patients were referred to the township NAP team for the ART drugs. Some equipment and
32
materials, such as MUAC tapes, record forms for z-scores and height measuring equipment
were not adequate in some health centers. In most health centers, there was no proper sterilizing
machine for disinfection purposes. The BHS used disposable syringes during EPI activities and
when providing injection treatment to the patients.
There needs to be an adequate and regular supply of drugs for management of sick children (2-
59 months) according to the IMNCI guideline’s recommended drug list. The BHS need to
inform their supervisors (HA or LHV) if there is any shortage of drugs or nearly expired drugs.
The BHS need to conduct a regular update of drugs and material consumption in the drug stock
management and maintain bin cards to improve their system. In order to keep some drugs and
paper documents safely and properly, the BHS should request additional cupboards, if
necessary.
The supervision reports submitted by the State/Regional, and Township training teams contain
useful information for the CHD for assessing the effectiveness of the guideline utilization, and
problems and challenges at the implementation level. These inputs can guide timing of the
refresher training to the BHS and future revisions of guidelines. The supervision visits provided
feedback, experience and lessons learned on the utilization of the updated IMNCI guidelines
(2017).
LPIC center: There was limited use of Learning and Performance Improvement centers by the
trained BHS. The LPIC centers are situated in the State and Regional Health Department and
the BHS trained on the Updated IMNCI guidelines (2017) are in the township at RHCs and
sub-centers. The distance from the township to the LPIC and the routine workload of the BHS
are barriers for the trained participants to use the LPICs, except when they get a chance during
other meetings or trainings. Most IMNCI training aid materials are already familiar to the
existing BHS and most of the medicines and equipment displayed in the L&PICs are used
currently in the RHCs and sub-centers for patient examination and treatment.
CME modules: Based on the format of the two modules and handouts, already developed for
pneumonia and diarrhea CME, the township health teams can develop other modules for CME
on seasonal diseases and the nutrition, HIV, and growth and development sessions, as well.
Experience sharing and presenting problems and challenges of using the Updated IMNCI
guidelines (2017) can be done by the BHS at the township CME sessions occasionally. It will
be good practice for the participants, as similar CME sessions are prepared on seasonal diseases
of childhood illness, based on the updated information in the IMNCI guideline.
33
6. Key Recommendations Training
- Roll out the updated IMNCI training nationwide as rapidly as possible for
consistency in management of childhood illness.
- Conduct refresher courses every 3 years to cover as many trained staff as
possible – considering time and budget limitations.
- Develop a plan for efficient training of newly assigned BHS if trained staff are
transferred.
- Allow transferred staff to take their IMNCI training materials with them to
their new post
- Print and distribute additional copies of the IMNCI training materials to all
BHS and office copies to be kept in all health centers.
Infrastructure
- Strengthen the infrastructure of health centers to provide clean water access
and basic equipment, e.g. for functioning ORT corners.
- Consider the need to provide support for some essential materials such as
availability of running water, sterilizers for smooth implementation and better
patient management.
Drug management
- Strengthen drug supply chain and provision of consumable materials to
prevent stock out of essential drugs and equipment as defined in the updated
IMNCI guidelines (2017). Currently missing items include: bronchodilators,
spacers, salbutamol, diazepam suppositories, nasal tubes, etc.
- Involve additional national programs (such as National AIDs Program, NMCP
and TB) to inform the further addition of specific drugs to the supply for
RHCs.
General support
- Provide sufficient quantities of the Patient Record form to ensure that IMNCI-
trained staff have the necessary tools for use with each new case.
- Perform regular follow-up and supervisory visits (preferably quarterly).
(Where human resources and time may be limited, supervision could be
initially targeted to facilities where the staff showed some challenges in
grasping the information provided in the training. Use pre and post test scores
from training to help identify areas where more support may be needed).
- Provide feedback on utilization of the updated IMNCI guidelines in the
program evaluation meeting on yearly basis.
- Procure needed drugs and materials in the near future
- Encourage more family and community participation, to work in close
collaboration with the BHS, to support reduction of IMR and U5MR in the
townships, states/regions and nationwide.
34
Photo 9: MCSP, Child Health Team (JSI-Myanmar) at Follow up after Training TOT, Naypyitaw
7. References
1. WHO (2018) Integrated Management of Childhood Illness (IMCI). Available at
http://www.who.int/maternal_child_adolescent/topics/child/imci/en/ (Accessed 12
June 2018)
2. WHO Introduction, IMCI Training Player, ICATT (2013). Available at
http://online.icatt-training.org/se-266098999fe14093b27ad8d5df779ffd/82019dd0-
5fe1-4b1e-958d-e544d17ea473/
3. MOHS, Nay Pyi Taw (2017) Myanmar Demographic Health Survey (2015-16).
Available at https://dhsprogram.com/pubs/pdf/FR324/FR324.pdf
4. UNICEF fact sheet. https://www.unicef.org/eapro/MNH_Myanmar.pdf
5. Sustainable Development Goal 3. https://sustainabledevelopment.un.org/sdg3
35
8. Annexes
Annex 1. Agenda of Central MToT on updated IMNCI guidelines (2017)
Man Myanmar hotel, Nay Pyi Taw
Note: Similar training curriculum was used in State and Regional level IMNCI training in five states and
regions.
စ
စစ
စစစ
စစစ
စစစစစစ စစစစစစစစစစ
စစစစစစ (စစ.စစ.စစစစ )
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ဧ၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
All Trainers
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Theingi Aung
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Thida Win
၁ ၁၁၁၁၁
- ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Zaw Myo Aung
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Kyaw Thant Sin
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Wai Min Oo
၁၁ ၁၁၁၁ -
၁၁၁၁
Role play exercise with OSCE All trainers
စစစစစစစစ (စစ.စစ.စစစစ )
၁ ၁၁၁၁ -
၁၁၁၁
Recap and Tea Break All trainers
36
၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁
Dr. Dr. Thida Win
၁ ၁၁၁၁၁
- ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁
၁၁၁၁၁၁
Dr. Zaw Myo Aung
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁\
၁၁၁၁၁၁၁၁၁၁ ၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Kyaw Thant Sin
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁
Dr. Wai Min Oo
၁
၁၁၁၁၁
- ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Kyaw Thant Sin
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Wai Min Oo
၁၁ ၁၁၁၁ -
၁၁၁၁
Role play exercise with OSCE All trainers
စစစစစစစ (စစ.စစ.စစစစ )
၁ ၁၁၁၁ -
၁၁၁၁
Recap and Tea Break
၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁\
၁၁၁၁၁၁၁၁၁၁ ၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Theingi Aung
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Thida Win
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
Dr. Zaw Myo Aung
37
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁Exer
cise and Role play Dr. Wai Min Oo
၁ ၁၁၁၁၁
- ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ Dr. Kyaw Thant Sin
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ Dr. Kyaw Thant Sin
၁၁ ၁၁၁၁ -
၁၁၁၁
Role play exercise with OSCE All trainers
စစစစစစစစ (စစ.စစ.စစစစ )
၁ ၁၁၁၁ -
၁၁၁၁
Recap and Tea Break ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁
-
၁၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁
-
၁၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁
-
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (knowledge) ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁
- ၁၁၁၁
Luncg break
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill using OSCE) ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁ -
၁၁၁၁
Coffee break
၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill using OSCE) ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill using OSCE) ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
English Translation
Agenda of Central MToT on updated IMNCI guidelines (2017)
Man Myanmar hotel, Nay Pyi Taw
No Date and time Topic Responsible person
First Day (27.11.2017)
1) 8:00 – 9:00 Registration
2) 9:00 – 10:00 Opening Ceremony and Tea Break
3) 10:00 – 10:45 Pretest All Trainers
4) 10:45 – 11:15
Introduction, Assess and classify child, Ask
the mother about the child problems, Check
for general danger signs, Exercise
Dr. Theingi Aung
38
5) 11:15 – 12:00
Assess cough and difficult breathing and
Classification, Assess diarrhoea and
classification
Dr. Thida Win
6) 12:00 – 1:15 Lunch Break
7) 1:15 – 2:15
Assess fever, Assess ear problem, Check for
acute malnutrition and anaemia, Classification
and exercise
Dr. Zaw Myo Aung
8) 2:15 – 2:30 Coffee Break
9) 2:30 – 3:30
Check for HIV infection, Check
immunization, Vitamin A and Deworming
status
Dr. Kyaw Thant Sin
10) 3:30 – 4:30
Assess other problems including mouth and
gum conditions, Feeding children, Assess
development
Dr. Wai Min Oo
11) 4:30 – 5:00 Role Play Exercises with OSCE All trainers
SECOND DAY (28.11.2017)
1) 8:00 – 9:00 Recap and Tea Break All trainers
2) 9:00 – 10:00 Identify treatment for child with cough and
difficult breathing, and diarrhoea, Exercise Dr. Dr. Thida Win
3) 10:00- 10:45 Identify treatment for child with fever, ear
problem, malnutrition and anaemia Dr. Zaw Myo Aung
4) 10:45-11:15
Identify treatment for child infected with HIV,
during Immunization, Vit A, deworming and
Exercise
Dr. Kyaw Thant Sin
5) 11:15-12:00
Identify treatment for child with teeth and
gums problems, feeding and developmental
milestones, Exercise
Dr. Wai Min Oo
6) 12:00-1:15 LUNCH BREAK
7) 1:15-2:15 Treatment of cough, difficult breathing,
diarrhoea and Exercise Dr. Kyaw Thant Sin
8) 2:15-2:30 COFFEE BREAK
9) 2:30-3:30 Treatment of Fever, Ear Problems, Nutritional
Status and Anaemia, and Exercise Dr. Wai Min Oo
10) 3:30-4:30 Role Play Exercises with OSCE All trainers
THIRD DAY (29.11.2017)
1) 8:00-9:00 AM Recap and Tea Break
2) 9:00-10:00
Treatment of HIV infected child,
Immunization, Vit A, Deworming and
Exercise
Dr. Theingi Aung
3) 10:00-10:45
Treatment of teeth and Gums problems,
Feeding and Developmental Milestones and
Exercise
Dr. Thida Win
4) 10:45-11:15 Counselling of Mother Dr. Zaw Myo Aung
5) 11:15-12:00 Counselling of Mother, Exercise and Role
Play Dr. Wai Min Oo
6) 12:00-1:15 LUNCH BREAK
7) 1:15-2:15 Follow-up the child Dr. Kyaw Thant Sin
8) 2:15-2:30 Coffee Break
9) 2:30-3:30 Follow-up visit and Exercise Dr. Kyaw Thant Sin
10) 3:30-4:30 Role Play Exercises with OSCE All trainers
39
FOURTH DAY (30.11.2017)
1) 8:00-9:00 Recap and Tea Break All trainers
2) 9:00-10:00 Role Play Exercises with OSCE All trainers
3) 10:00-10:45 Role Play Exercises with OSCE All trainers
4) 10:45-11:15 Role Play Exercises with OSCE All trainers
5) 11:15-12:00 Evaluation after Training (Knowledge) All trainers
6) 12:00-1:15 LUNCH BREAK
7) 1:15-2:15 Evaluation after Training (Skill using OSCE) All trainers
8) 2:15-2:30 COFFEE BREAK
9) 2:30-3:30 Evaluation After Training (Skill using OSCE) All trainers
10) 3:30-4:30 Evaluation After Training (Skill using OSCE) All trainers
40
Annex 2. Agenda for Central MTOT on Follow-up training of updated IMNCI guidelines
(2017)
Man Myanmar Hotel, Nay Pyi Taw
စ
စစ
စစစစစ
စစစစစစ
စစစစစစ
စစစစစစစစစ စစစစစစစစစစ
စစစစစစ (စစ.စ.စစစစ)
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁
၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
Coffee break
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁ - ၁.၁)
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁)
၁၁၁၁၁၁၁ ၁၁၁၁
၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁ - ၁.၁ - ၁.၁)
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ -
၁၁၁၁
Coffee break
၁၁
၁
၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁)
၁၁၁၁၁၁၁ ၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁
၁
4:30-5:00 ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
41
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁) ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
စစစစစစစစ (စစ.စ.စစစစ )
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁
၁၁၁၁၁(၁)၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁
၁၁၁၁၁(၁)၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
စစစစစစစ (စစ.စ.စစစစ )
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
Coffee break
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ -
၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
English Translation
Agenda for Central MTOT on Follow-up training of updated IMNCI guidelines (2017),
January 2018
Man Myanmar Hotel, Nay Pyi Taw
No Date and time Topic Responsible person
Day 1 (10.1.2018)
1 8:00-9:00 Registration
42
2 9:00- 10:00 Goals and objectives of IMNCI follow up
after training
Dr.Theingi Aung
3 10:00-10:45 Coffee break
4 10:45-11:15 Follow up after training (1.1 - 1.2) Dr.Theingi Aung
5 11:15- 12:00 Follow up after training (1.3) Dr.Theingi Aung
6 12:00-1:00 Lunch break
7 1:15-2:15 Follow up after training(1.4-1.5-1.6) Dr.Soe Ye Yint Htun
8 2:15-2:30 Procedures and guidelines for follow up after
training, meeting and central meeting
Dr.Aung Naing Soe
9 2:30-3:30 Coffee break
10 3:30-4:30 Teaching on check list for follow up after
training (1)
Dr.Zaw Myo Aung
11 4:30-5:00 Teaching on check list for follow up after
training (2) & linked with card exercises
Dr.Zaw Myo Aung
Day 2 (11.1.2018)
1 8:00-12:00 Supervision visit to RHC by dividing four
groups
All participants
2 12:00-1:15 Lunch break
3 1:15-4:30 Supervision visit to SRHC by dividing four
groups
All participants
Day 3 (12.1.2018)
1 9:00-10:00 Group discussion on follow up after training All participants
2 10:00-10:45 Coffee break
3 10:45- 12:00 Group discussion on follow up after training All participants
4 12:00-1:15 Lunch break
5 1:15-4:15 Group discussion on follow up after training All participants
6 4:15-4:30 Closing ceremony
43
Annex 3. Agenda for State level Follow-up training of updated IMNCI guidelines (2017),
Taunggyi, S Shan state
စ
စစ
စစစစစ
စစစစစစ
စစစစစစ
စစစစစစစစစ စစစစစစစစစစ
စစစစစစ (စစ.စ.စစစစ)
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
Coffee break
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁ - ၁.၁)
၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁)
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁.၁ - ၁.၁ - ၁.၁)
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁ - ၁၁၁၁ Coffee break
၁၁
၁
၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
(၁)
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁
၁
4:30-5:00 ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
(၁) ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
စစစစစစစစ (စစ.စ.စစစစ)
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁
၁၁၁၁၁(၁)၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁
၁၁၁၁၁(၁)၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
44
စစစစစစစ (စစ.စ.စစစစ)
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
Coffee break
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁ ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
စစစစစစစစ (စစ.စ.စစစစ)
၁၁ ၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
Coffee break
၁၁ ၁၁၁၁၁ -
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
CME ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁ ၁၁၁၁၁ -
၁၁၁၁
Lunch break
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
CME ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ - ၁၁၁၁ Coffee break
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
45
၁၁၁၁၁၁၁၁၁
CME ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁
English Translation
Agenda for State level Follow-up training of updated IMNCI guidelines (2017), Taunggyi, S
Shan state
No Date and time Topic Responsible person
Day 1 (13.2.2018)
1 8:00-9:00 Registration
2 9:00- 10:00 Goals and objectives of IMNCI follow up
after training
Daw Aye Aye San
3 10:00-10:45 Coffee break
4 10:45-11:15 Follow up after training (1.1 - 1.2) Daw Aye Aye San
5 11:15- 12:00 Follow up after training (1.3) Daw Sein Lae Nway
6 12:00-1:00 Lunch break
7 1:15-2:15 Follow up after training(1.4-1.5-1.6) Daw Sein Lae Nway
8 2:15-2:30 Procedures and guidelines for follow up
after training, meeting and central meeting
All facilitators
9 2:30-3:30 Coffee break
10 3:30-4:30 Teaching on check list for follow up after
training
Dr. Khaing Myae
11 4:30-5:00 Teaching on check list for follow up after
training
Dr. Khaing Myae
Day 2 (14.2.2018)
1 8:00-12:00 Supervision visit to RHC by dividing four
groups (Nam Kok RHC, Hopong Township)
All participants
46
2 12:00-1:15 Lunch break
3 1:15-4:30 Supervision visit to SRHC by dividing four
groups (Long Hay SRHC, Hopong
Township)
All participants
Day 3 (15.2.2018)
1 9:00-10:00 Group discussion on follow up after training All participants
2 10:00-10:45 Coffee break
3 10:45- 12:00 Group discussion on follow up after training All participants
4 12:00-1:15 Lunch break
5 1:15-4:30 Group discussion on follow up after training All participants
Day 4 (16.2.18)
1 9:00 – 10:15
AM
Review session about Pneumonia and
Diarrhoea
All participants
2 10:15 – 10:45
AM
Coffee Break
3 10:45 – 12:00
PM
Group presentation on
Pneumonia/Diarrhoea by each township
training team
All participants
4 12:00 – 1:00
PM
Lunch
5 1:00 – 3:00 PM Group presentation on
Pneumonia/Diarrhoea by each township
training team
All participants
6 3:00 – 3:30 PM Coffee Break
7 3:30 – 4:30 PM Group presentation on
Pneumonia/Diarrhoea by each township
training team
All participants
8 4:30 – 5:00 PM Closing Ceremony
47
Annex 4. Agenda for Township level Multiplier training, Mong Kai Township, S Shan state,
February 2018
Note: Similar training agenda was used for other townships.
စ
စစ
စစစစစ
စစစစစစ
စစစစစစ
စစစစစစစစစ စစစစစစစစစစ
စစစစစစ (စစ.စ.စစစစ)
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ဧ၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁
၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁
စစစစစစစစ (စစ.စ.စစစစ)
၁ ၁၁၁၁ - ၁၁၁၁
Recap ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ -
၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
စစစစစစစ (စစ.စ.စစစစ)
48
၁ ၁၁၁၁ - ၁၁၁၁
Recap
၁ ၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁
၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁
၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
စစစစစစစစ (စစ.စ.စစစစ)
၁ ၁၁၁၁ - ၁၁၁၁
Recap
၁ ၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁\ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁
၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
စစစစစစစ (စစ.စ.စစစစ)
၁ ၁၁၁၁ - ၁၁၁၁
Recap and Tea Break
49
၁ ၁၁၁၁ - ၁၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
Role play exercise with OSCE ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
(knowledge)
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill
using OSCE)
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁
၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill
using OSCE)
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
၁၁ ၁၁၁၁ - ၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ (skill
using OSCE)
၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁
50
English translation
Agenda for Township level Multiplier training, Mong Kai township, S Shan state, February
2018
No Date and time Topic Responsible person
First Day (21.2.2018)
1) 8:30 – 9:00 Registration and Opening Ceremony
2) 9:00 – 9:30 COFFEE BREAK
3) 9:30 – 10:00 Pretest All Trainers
4) 10:00 – 10:30 Introduction Daw Sein Lae Nway
5) 10:30 – 12:00 Assess and classify child, Ask the mother
about the child problems, Check for
general danger signs, Exercise
Daw Sein Lae Nway
6) 12:00 – 1:00 LUNCH BREAK
7) 1:00 – 2:30 Assess cough and difficult breathing and
Classification
Daw Aye Aye San
8) 2:30 – 3:00 COFFEE BREAK
9) 3:30 – 4:30 Identify treatment for child with cough
and difficult breathing and Exercises
Daw Aye Aye San
SECOND DAY (22.2.2018)
1) 9:00 – 9:15 Recap All trainers
2) 9:15 – 10:15 Assess diarrhoea and classification Daw Nang Kham
Hlaing
3) 10:15 – 10:30 COFFEE BREAK Dr. Zaw Myo Aung
4) 10:30 – 12:00 Identify treatment for child with diarrhoea
and Exercises
Daw Nang Kham
Hlaing
5) 12:00 – 1:00 LUNCH BREAK Dr. Wai Min Oo
6) 1:00 – 2:30 Assess ear problem and classification Daw Nang Mo Ngin
7) 2:30 – 3:00 COFFEE BREAK Dr. Kyaw Thant Sin
8) 3:00 – 4:30 Identify treatment for ear problem and
Exercises
Daw Nang Mo Ngin
THIRD DAY (23.2.2018)
1) 9:00 – 9:15 Recap All Trainers
2) 9:15 – 10:15 Assess fever and classification Daw Nang Kham Lu
3) 10:15 – 10:30 COFFEE BREAK Dr. Thida Win
4) 10:30 – 12:00 Identify treatment for fever and Exercises Daw Nang Kham Lu
5) 12:00 – 1:00 LUNCH BREAK Dr. Wai Min Oo
6) 1:00 – 2:30 Check for acute malnutrition and
anaemia, Classification and Exercises
Daw Sein Lae Nway
7) 2:30 – 3:00 COFFEE BREAK Dr. Kyaw Thant Sin
8) 3:00 – 4:30 Assess feeding Children and
developmental milestones and Exercise
Daw Sein Lae Nway
FOURTH DAY (24.2.2018)
1) 9:00 – 9:15 Recap All Trainers
51
2) 9:15 – 10:15 Check for HIV infection, Identify
treatment for child infected with HIV and
Exercises
Daw Aye Aye San
3) 10:15 – 10:30 COFFEE BREAK All trainers
4) 10:30 – 12:00 Check immunization, Vitamin A and
Deworming status, Identify treatment and
Exercises
Daw Nang Kham
Hlaing
5) 12:00 – 1:00 LUNCH BREAK All trainers
6) 1:00 – 2:30 Assess other problems including mouth
and gum conditions, Identify treatment for
child with teeth and gums problems and
Exercises
Daw Nang Mo Ngin
7) 2:30 – 3:00 COFFEE BREAK All trainers
8) 3:00 – 4:30 Role play exercise with OSCE All Trainers
FIFTH DAY (25.2.2017)
1) 9:00 – 9:15 Recap and Tea Break All Trainers
2) 9:15 – 10:15 Role play exercise with OSCE All Trainers
3) 10:15 – 10:30 COFFEE BREAK All trainers
4) 10:30 – 11:15 Role play exercise with OSCE All Trainers
5) 10:30 – 12:00 Knowledge Examination (post-test) All Trainers
6) 12:00 – 1:15 LUNCH BREAK Daw Nang Mo Ngin
7) 1:15 – 2:15 Skill Examination using OSCE All Trainers
8) 2:15 – 2:30 COFFEE BREAK All Trainers
9) 2:30 – 3:30 Skill Examination using OSCE All Trainers
10) 3:30 – 4:30 Skill Examination using OSCE All Trainers
52
Annex 5. List of participants in training and supervision visits
No Training Date
Training Name Place Central/Region/State/
Township
Number of Participants Types of
participants
Types of
activity From To Male Female Total
IMNCI Training and follow-up activity
Central MTOT in Nay Pyi Taw
1 27-11-17 30-11-17 Central MToT IMNCI Training Naypyitaw Central 8 13 21 Trainers Training
2 10-01-18 12-01-18 Central MToT, Follow-up training Naypyitaw Central 4 14 18 Trainers Training
Magway Region
1 27-12-17 30-12-17 State/ Regional Level ToT Training Magway Regional 11 14 25 Trainers Training
2 15-01-18 19-01-18 Township level BHS Multiplier
Training Taungdwingyi Township 0 30 30
BHS Training
3 01-02-18 03-02-18 State/Regional Level Follow-up
Traiining Magway Regional 11 14 25
Trainers Training
4 15-02-18 19-02-18 Township level BHS Multiplier
Training Taungdwingyi Township 0 30 30
BHS Training
5 08-03-18 19-03-18 Follow-up activity Taungdwingyi Township 0 26 26 BHS Supervision
Ayeyarwaddy Region
1 26-12-17 29-12-17 State/ Regional Level ToT Training Pathein Regional 0 20 20 Trainers Training
2 15-01-18 19-01-18 Township level BHS Multiplier
Training Ingapu Township 0 27 27
BHS Training
3 03-02-18 07-02-18 Township level BHS Multiplier
Training Ingapu Township 0 27 27
BHS Training
4 05-03-18 09-03-18 Township level BHS Multiplier
Training Ingapu Township 0 21 21
BHS Training
5 19-03-18 21-03-18 State/Regional Level Follow-up
Traiining Pathein Regional 0 21 21
Trainers Training
6 27-02-18 27-02-18 Follow-up activity Ingapu Township 0 1 1 BHS Supervision
7 20-03-18 20-03-18 Follow-up activity Ingapu Township 0 4 4 BHS Supervision
8 26-03-18 30-03-18 Follow-up activity Ingapu Township 0 20 20 BHS Supervision
53
No Training Date
Training Name Place Central/Region/State/
Township
Number of Participants
Types of
participants
Types of
activity
From To Male Female Total
IMNCI Training and follow-up activity
Central MTOT in Nay Pyi Taw
Rakhine state
1 15-01-18 18-01-18 State/ Regional Level ToT Training Sittwe Township 3 17 20 Trainers Training
2 23-02-18 27-02-18 Township level BHS Multiplier
Training Min Bya Township 0 23 23
BHS Training
3 25-03-18 29-03-18 Township level BHS Multiplier
Training Min Bya Township 0 22 22
BHS Training
4 05-05-18 18-05-18 Follow-up activity Min Bya Township 0 23 23 BHS Supervision
Northern Shan
1 27-12-17 30-12-17 State/ Regional Level ToT Training Lashio State 0 14 14 Trainers Training
2 05-03-18 07-03-18 State/Regional Level Follow-up
Training Lashio State 0 13 13
Trainers Training
3 27-03-18 30-03-18 Township level BHS Multiplier
Training Mongyai Township 0 20 20
BHS Training
4 27-04-18 30-04-18 Township level BHS Multiplier
Training Tang Yan Township 0 30 30
BHS Training
5 14-05-18 16-05-18 Follow-up activity Mongyai Township 0 7 7 BHS Supervision
6 28-05-18 30-05-18 Follow-up activity Tang Yan Township 0 10 10 BHS Supervision
Southern Shan
1 16-01-18 19-01-18 State/ Regional Level ToT Training Taunggyi State 3 21 24 Trainers Training
2 13-02-18 16-02-18 State/Regional Level Follow-up
Training Taunggyi State 3 21 24
Trainers Training
3 21-02-18 25-02-18 Township level BHS Multiplier
Training Mong Kai Township 0 22 22
BHS Training
4 30-03-18 30-03-18 CME activity Mong Kai Township 10 39 49 BHS CME session
5 28-03-18 02-04-18 Follow-up activity Mong Kai Township 0 16 16 BHS Supervision
54
Annex 6. Number and percentage of trained MOHS trainers in the state, regional and township training teams
Trained trainers on updated IMNCI
Med-
ical Doctor Nursing Officer THN SN TN THA HA LHV MW PHS 1 Tutor Total
Magway region 12 2 2 2 10 2 30
Ayeyarwaddy region 5 1 5 13 1 25
Rakhine state 1 2 2 4 9 1 1 2 22
N Shan state 4 4 11 19
S Shan state 6 1 6 8 6 1 28
Total number 28 6 19 8 6 2 14 36 2 1 2 124
Total percentage 23% 5% 15% 6% 5% 2% 11% 29% 2% 1% 2%
Medical Doctors: Team leaders of Child Health team or Township Medical Officer or Station Medical Officer
Nursing Officer: Senior nurse based at State and Regional Health Department
THN: Township Health Nurse at Township Health Department
SN: Staff Nurse at the Township Health Department
TN: Trained Nurse at the Township Health Department
THA: Township Health Assistant
HA: Health Assistant
LHV: Lady Health Visitor
MW: Midwife
PHS 1: Public Health Supervisor 1
Tutor: Nurse at the Nursing and Midwifery Training School
Annex 7. BHS (LHV and Midwife) existing, trained and supervised
State/ Region Township LHV Midwife Total
Existing Trained Supervised Existing Trained Supervised Existing Trained Supervised
Magway Taungdwingyi 9 4 (44%) 4 (100%) 59 56 (95%) 22 (39%) 68 60 (88%) 26(43%)
Ayeyarwaddy Ingapu 6 4 (67%) 0 74 71 (96%) 25 (35%) 80 75 (94%) 25 (33%)
Rakhine state Minbya 9 7 (78%) 3 (42%) 43 38 (88%) 20 (53%) 52 45 (87%) 23 (51%)
N Shan Tang Yan 3 1 (33%) 1 (100%) 29 29 (100%) 9 (31%) 32 30 (94%) 10 (33%)
N Shan Mongyai 3 1 (33%) 0 23 19 (83%) 7 (37%) 26 20 (77%) 7 (35%)
S Shan Mong Kai 4 4 (100%) 3 (75%) 18 18 (100%) 13 (72%) 22 22 (100%) 16 (73%)
Total 34 21 (60%) 11 (52%) 246 231 (94%) 96 (42%) 280 252 (90%) 107 (42%)
55
Annex 8. Health centers (UHC, MCH, RHC, sub-center) existing, trained and supervised
Region/
State Township
UHC MCH RHC Sub-center Total
Existi
ng
Traine
d
Superv
ised
Existi
ng Trained
Superv
ised
Exist
ing
Traine
d
Supervis
ed
Existi
ng Trained
Supervis
ed
Existi
ng
Traine
d
Supervis
ed
Magway Taungdwin
gyi 1 1
1
(100%) 0 8
8
(100%)
7
(88%) 40
36
(90%)
14
(39%) 50
45
(90%)
21
(47%)
Ayeyarwa
ddy Ingapu 1 1
1
(100%)
1
(100%) 11
11
(100%)
6
(55%) 52
51
(98%)
13
(25%) 65
63
(97%)
20
(32%)
Rakhine Minbya 0 1 1
(100%)
1
(100%) 6
6
(100%)
6
(100%) 29
29
(100%)
13
(45%) 36
36
(100%)
20
(56%)
N Shan Tang Yan 0 1 1
(100%)
1
(100%) 4
4
(100%)
2
(50%) 16
14
(88%)
3
(21%) 21
19
(90%)
6
(32%)
Mongyai 0 1 1
(100%) 0 3
2
(67%)
1
(50%) 16
16
(100%)
6
(35%) 20
19
(95%)
7
(35%)
S Shan Mong Kai 1 1
(100%)
1
(100%) 1
1
(100%)
1
(100%) 3
3
(100%)
3
(100%) 9
9
(100%)
3
(33%) 14
14
(100%)
8
(57%)
Total 3
1
(33%)
1
(100%) 6
6
(100%)
4
(67%) 35
34
(97%)
25
(74%) 162
155
(96%)
52
(33%) 206
196
(95%) 82
(42%)
56
Annex 9 (a). Pre- and Post-test scores of participants in trainings
# participants
Pre-test (/10 scores) Post-test (/10 scores)
Minimum scores Maximum scores Average scores Minimum scores Maximum scores Average scores
Nay Pyi Taw Central MToT 20 2.5 10 5 2 10 6
Magway State and Regional ToT training 25 2 4 2.7 6.5 9.5 8.3
Township training, Batch 1 30 4 5 4.4 7 9 7.8
Township training, Batch 2 30 2 5 3.2 7 10 8.2
Ayeyarwaddy State and Regional ToT training 18 3 6 4.8 5 9 7
Township training, Batch 1 27 3 8 4.4 6 9.5 8
Township training, Batch 2 27 3 8 4.9 6 9.5 8.2
Township training, Batch 3 21 3 7 5 6 9.5 8.2
Rakhine State and Regional ToT training 13 1 8 4.8 6 8.5 7.3
Township training, Batch 1 23 2 6 3.8 5 8 6.6
Township training, Batch 2 22 1 4.5 2.4 5 9 6.4
N Shan State and Regional ToT training 14 3 7.5 4 4 8.5 5.3
Township training, Tang Yan 24 3.3 7.7 5 6.7 10 8.8
Township training, Mongyai 20 3 8.5 5.7 6 9 7.3
S Shan State and Regional ToT training 24 1 5.5 3.3 5 10 7
Township training, Mong Kai 22 1 6 2.1 4.5 10 6.8
Annex 9 (b). Percent increase
Township
Pre-test
average
scores
Post-test
average
scores
Difference Percent
increase
Central MToT 5 6 1 20
Magway 4.7 8.1 3.4 72
Ayeyarwaddy 4.8 7.9 3.1 65
Rakhine 3.7 6.8 3.1 84
N Shan 4.9 7.1 2.2 45
S Shan 2.7 6.9 4.2 156
57
Annex 10. Case Scenarios (OSCE) for Pre- and Post-tests in updated IMNCI training
(၁) ၁၁၁၁၁၁၁၁ - ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁-(၁)၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁-
(၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁- (၁၁)၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁- (၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁)၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ (၁၁) ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
(RUTF) ၁၁၁၁၁၁၁ ၁၁၁၁၁(၁၁)၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁) ၁၁၁၁၁၁၁၁- ၁၁၁၁၁၁၁ ၁၁၁၁ (၁)၁၁၁၁ (၁)၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁-
(၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁း ၁၁၁၁၁၁၁၁၁၁-(၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁-
(၁၁.၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁(၁)၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁ MUAC၁၁၁
(၁၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁(၁)
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁(၁၁)၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁
(၁) ၁၁၁၁၁၁၁၁- ၁၁၁၁၁ ၁၁၁၁(၁)၁၁၁၁၁၁ (၁၁)၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ HIV-positive ၁၁၁၁၁
၁၁၁၁၁၁၁ ART prophylaxis (၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁
(၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁(၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁(၁၁)၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ Salbutamol ၁၁၁၁၁၁၁ ၁၁၁၁၁(၁၁)၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁ (၁၁)၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁ DNA-PCR ၁၁၁၁၁၁၁၁၁၁၁၁၁၁ Negative၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ HIV Counseling ၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁ ၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁၁
58
English Translation
1) Name – Maung Maung, Age – (3) Yrs, Body Weight – (10) kg, Height – (98) cm
He has a complaint of fever with cough. It is his first time to clinic. He has body temperature 38˚C. There is
no general danger signs on the child. He has been coughing for (5) days. On examination, respiratory rate of
the child is 43/min. There is no chest indrawing and stridor. But he has wheezing. The child does not have
diarrhoea. He lives in no Malaria area. He has no history of Measles. There is no mouth and gum ulcers and
eye problem. He does not have any sign about Dengue Haemorrhagic Fever. There is no ear problem in this
child. When health worker checked the nutrition status of the child, there is no pitting oedema and palmar
pallor. He can eat half of RUTF within (30) minutes. The child was not infected with HIV. He has not been
received any immunization according to the age. He also never takes Vitamin-A pill or Deworming pills.
When health worker checked Maung Maung’s development for age, he can climb up and down the ladder.
He is able to speak his name and age. But he cannot draw a circle. Treat the child according to IMNCI.
2) Name – Aye Aye, Age – (1) yr and (3) mths
She is having a diarrhoea and this is her first time to clinic. Her body weight is (12) kg and she is (86) cm
tall. Her body temperature is 37.4˚C at the time of measuring. There is no general danger signs on the baby.
She does not have cough and difficult breathing. She has been having loose motion for three days and there
was no mucus or blood. The stool is watery but not cloudy. The baby is not lethargic. She drink eagerly and
her skin pinch goes back slowly. The mother said that the baby has sunken eyes. There is no other health
problems. She does not have history of HIV Exposure. Her MUAC is (120) mm and there is no pitting
oedema. When health worker assessed the feeding history of the baby, he found that the baby has two meals
of rice per day. And her mother stopped breastfeeding her. The one who feeds the baby is her 10 years old
sister. Since the baby had fever, the regular meals are ceased and she drinks only water. She never received
immunization and Vitamin pills. She can walk. She can drink with cup. She can speak “May May”. Treat the
child.
3) Name – Mu Mu, Age – (2) yr and (10) days
The mother of the baby is PMCT-positive mother and the baby got ART Prophylaxis (6) weeks. The baby’s
complaint for now is difficult breathing with “Shuu Shuu” breathing sound. Her body weight is (4) kg and
she is (53) cm tall. This is her first time to clinic for difficult breathing. There is no general danger signs. The
baby is difficult in breathing and her respiratory rate is (60) per minutes. There is no chest indrawing and
stridor. The baby had wheezing and was treated with inhaled bronchodilator (Salbutamol). Her respiratory
rate dropped to 40 per minute and she asked for food after being treated with inhaled bronchodilator. There
is no loose motion, no fever. The baby has oral thrushes. She does not have ear problem and anaemia. There
is no sign of malnutrition. DNC-PCR test result is negative. The baby is not breastfed. She was bottle fed
according to HIV counseling. She was not stop drinking milk. The baby received all the immunization. She
is able to hold head up. She knows her mother’s face. She usually wakes up through loud sounds. She can
response with a smile to teasing. Treat the baby according to IMNCI guideline.
59
Annex 11. Follow-up after training_ Supervision tools (English translation)
Follow-up after training, Form 1
State/Region___________________
District_________________
Township_______________
Name of Supervisor______________
Position________________
Address___________ Date______
____
Please note down the name of health center, name of staff and date.
Name of Health Center
Total Date
Name of Staff
Activity 1 2 3 4 5
If supervisor's opinion is the same as staff's opinion, please mark (ì). If not, please mark (o). If the activity is not required to do, please mark cross line through two columns.
Sup
ervisor
Staff
Sup
ervisor
Staff
Sup
ervisor
Staff
Sup
ervisor
Staff
Sup
ervisor
Staff
Total scores
by Supervisor (ì)
Total scores by staff
(ì)
1. ASSESSMENT
1.1
General danger signs
1.2
Four main diseases ( Coughing, Diarrhoea, Fever, Ear Problems)
1.3
Nutrition : weighing the child's body weight and record on Weight Chart, Check Z-score, knows how to measure the mid upper arm circumstances
60
1.4
HIV : HIV testing, Asking mother for HIV infection status during pregnancy and delivery. If HV (+), ask about the HIV status of the child such as HIV testing and results.
1.5
EPI: assessment on immunization status of the child
1.6
Mouth and Gum : Assessment on mouth and gum and other health problems
1.7
Growth and Development : Assessment according to child's age
2. TREATMENT
2.1
Patient referral of severe disease
Providing intramuscular injection
2.2
Oral antibiotics (or) Oral anti-malarial drugs
Antibiotics for pneumonia
Antibiotics for ear infection
Antibiotics for dysentry
61
Oral anti-malarial drugs for malaria
2.3
Providing ORS solution for diarrhoea
Suggest to provide more fluids and to continue meals
Explain to provide more fluids and to continue meals and explain two dangers signs for emergency return
3.
Immunization given during this visit or appointment for next immunization
4. ASSESSMENT AND COUNSELLING ON FEEDING
4.1
Assessment on feeding including breast feeding in under 2
4.2
Counselling on child feeding and nutrition according to the age of under 2
5.
ASSESSMENT OF OTHER HEALTH PROBLEMS
Duration
Please note down the name of health center, name of staff and date.
62
Follow-up after training, Form 2
Use one column for one person.
1 2 3 4 5
Health Knowledge of caretaker
If he/she can answer correctly, please
mark (ì). If not, please mark (o). Please make cross mark along the column for
unnecessary line.
Note down the numbers of person
interviewed and numbers of person who know correct
answer.
DISCUSSIONS
1 The mother is able to describe the home treatment.
2 The mother correctly knows the ORS solution preparation.
3
The mother is able to describe the home treatment and ORS solution preparation.
4
The mothers know the (3) home care methods as giving fluid, food and indication for urgent return
Mother/Caretaker's Satisfaction
5 Mother's satisfaction on BHS' case management
6 Detail Description
6.1 Agree on examination time of BHS
6.2 Ways of BHS examination on the child
6.3 Treatment provided by BHS
6.4 Communication skills of BHS
63
6.5 Health knowledge received from BHS
6.6 Others
Follow-up after training, Form 3
State/Region________________
District________________
Township______________
Department________
Check the following items. If you found dufficulties, please mark (*). Please mark () on possible solutions.
1. Infractures and Materials Possible Solutions
a) Patient Examination Place Reposition the clinic space
1. Enough Space Advice the mininum standard for patient examination place. 2. Table, Chairs
3. Weighing Machine Submit requests for requirements to TMO or Supervisor. 4. Wall Clock
5. IMNCI Guideline Books
6. MCH booklet
7. Patient Registration
8. Patient Record Book
9. Water, Mug and Spoon
2. ORT Corner Possible Solutions
1. ORT Corner Advice to position ORT corner and required materials for ORT corner. Did babies receive ORT?
2. Enough Space Advice to have drinking water.
3. Table and Chair (For mother/caretaker) Select responsible person for ORT corner.
4. Water pot Submit requests for requirements to TMO or Supervisor. 5. Glass, Measuring Jar and Spoon for ORS
preparation
6. ORT Register Book
3. Immunization place and materials Possible Solutions
1. Enough Space Advice to have enough space for immunization.
2. Table and Cupboard Submit requests for requirements to TMO or Supervisor. 3. Vaccine Carrier, Cold Box
4. Freeze Test
5. Sterilizer
6. Immunization Records
7. Suitable Temperature (4˚C to 8˚C)
8. All vaccines (+/-) (BCG, OPV, DPT, Measles, HBV)
64
4. Outpatient Clinics and Referral Possible Solutions
1. Clinic opening time as planned Prepare clinic opening time is accessable by
children.
2. Does clinic opening time match with patients' free time?
Advice to provide health education during the waiting time.
3. Is there child patients? Discussion about emergency treatment and referral.
4. Can you provide medicine on every clinic day? Check for places that can support referral.
5. Can you provide immunization on everyday? Submit requests for requirements to TMO or Supervisor. 6. Does ORT Corner open on every clinic day?
7. Is it possible to refer to nearest hospital in time?
8. Can be referred on both day and night?
5. Case Management (If missed, please mark (*). Possible Solutions
1. Regular Patient Registration For routine activities,
2. Weighing - delegate tasks
3. Assessment and Classification diseases - solve problems
4. Referral - sharing knowledges to other staff
5. Identifying breastfeeding and other feeding problems
- prepare for readiness (less time consuming)
6. Counselling on feeding and nutrition - esure all the patients are checked during clinic opening time. 7. Advices to take medicine at home
8. Can provide ORS?
9. Teach mothers "How to prepare ORS solution at home"
10. Patient Record Completeness
11. Can you provide first treatment before referral?
12. Advices to take medicine at home
13. Can you provide drugs?
14. Can you provide immunization?
6. Record Keeping Possible Solutions
a) Do you keep records for every patient? Advice to keep records systematically.
b) If yes, what do you keep? Trained with a child patient to be able to keep patient records. - History taking, Physical Examination
- Classification (or) Diagnosis
- Treatment
- Supervision Records
7. Drug Management Possible Solutions
1. Drug stock books Advice to keep records systematically.
- Do you keep drugs in cupboards? Advice how to fill the stock ledgers and how to keep the records. - Does the storage place dry?
65
- Do you keep ORS sachets in dry place?
- Do you fill drug stock books correctly?
8. Drugs Possible Solutions
At the time of supervision visit, check the following drugs are enough for next three months or not. Please mark absent drugs with (*).
Try to find out the related problems with drugs and materials.
Injection Diazepem
Injection Ampicillin
Injection Gentamycin
Amoxicillin Capsules
Oral Sabultamol
Inhaled bronchodilator
Spacer
ORS sachet
Zinc Sulphate tablets
Ciprofloxacin capsules
Injection Artesunate
ACT tablets
Chloroquine tablets
Primaquine tablets
Paracetamol tablets
RUTF
Iron/Folate tablets
Iron syrup
Cotrimoxazole tablets
Nevirapine(NVP) tablets
Zidovudine (AZT) tablets
Tetracycline eye oinment
Gentian Violet
Nystatin syrup
Vit A capsule
Albendazole Deworming tablets
water for injection
Disposable syringes
1 cc
3 cc
5 cc
10 cc
Scalp vein set
cannula (Yellow)
Alcohol spirit
Nasal tube
Other drugs and drugs supplies
66
Annex 12 . IMNCI Materials placed at L&PICs (5 states/regions)
Description Unit Amount Remark
1.Paracetamol 500 mg tablet (10x10) Box 1 Essential drugs
2.Paracetamol 120mg/5ml, oral suspension Bot 1 Essential drugs
3.Paracetamol 250mg/5ml oral suspension Bot 3 Essential drugs
4.Amoxicillin 250 mg capsule (10x10) Box 1 Essential drugs
5.Amoxicillin 125mg/5ml oral suspension Bot 2 Essential drugs
6.Cotrimoxazole 80/400mg tablet (10x10) Box 1
Essential drugs
7.Ciprofloxacin 250mg tablet (10x10) Box 1 Essential drugs
8.Metronidazole 200mg tablet (10x10) Box 1 Essential drugs
9.Metronidazole 200mg/5ml oral suspension Bot 2 Essential drugs
10.Inj Ampicillin (500 mg) vial for injection Amp 2 Essential drugs
11.Inj Gentamycin (80 mg) vial for injection Amp 2 Essential drugs
12.Diazepam suppository Cap 0 Essential drugs
13.ORS sachet Sachet 2 Essential drugs
14.Clean water bottle (1 liter) Bot 2 Essential drugs
15.Zinc supplementation solution (10 mg/5ml) Bot 2 Essential drugs
16. Gentian violet solution 15ml (0.25 %) Bot 2 Essential drugs
17.Anti-malaria drugs -ACT , card Box 1 Essential drugs
18.Primaquine 7.5 mg tablet (10x10) Box 0 Essential drugs
19.Inj IM Artesunate 60mg ampule Amp 0 Essential drugs
20.Ferrous sulfate 200mg +250 µg Folate (10x10) Box 1 Essential drugs
21.Ferrous fumarate syrup, 100mg per 5ml Bot 2 Essential drugs
22.Albendazole 400 mg tablet, single tablet Tab 5 Essential drugs
23.Nystatin oral suspension, 60ml Bot 1 Essential drugs
24.Tetracycline 1% eye ointment tube Tube 2 Essential drugs
25.Nebulizer with chamber Set 2 Essential drugs
26.Salbutamol Respirator Solution (Ventolin solution) 5mg/ml
(10ml) Amp 2
Essential drugs
27.Intravenous infusion bottles (DW) 500ml Bot 2 Injections
28.Intravenous infusion bottles ( DS) 500 ml Bot 2 Injections
29.Intravenous infusion bottles ( MS) 500ml Bot 2 Injections
30.Intravenous infusion bottles (RL) ml Bot 2 Injections
31.Infusion sets, piece Set 4 Injections
32.Butterfly needle (scalp vein 23G) piece Pcs 2 Injections
33.Cannula (24 G, Yellow) piece Pcs 2 Injections
34.Oropharyngeal Airway (Guedel) Pcs 2 Materials
35.Bags and Masks (child size) Set 1 Materials
36.Respiratory timer (if not available any timer will do) Pcs 2 Materials
37.Pulse oxymeter Pcs 1 Materials
38.BP cuff (child) Pcs 1 Materials
39.Glucometer Pcs 1 Materials
67
40.Glucometer test kits 25’s box Box 1 Materials
41.Disposable syringe (1 ml) Pcs 0 Materials
42.Disposable syringe (3 ml) Pcs 2 Materials
43.Disposable syringe (5 ml) Pcs 2 Materials
44.Disposable syringe (10 ml) Pcs 2 Materials
45.Feeding tube (size 6) Pcs 7 Materials
46.Feeding tube (size 8) Pcs 0 Materials
47.Feeding tube (size 10) Pcs 0 Materials
48.Feeding tube (size 12) Pcs 4 Materials
49.Weighing machine Pcs 1 Nutrition
50.MUAC (MOHS approved version) Pcs 1 Nutrition
51.Weight chart (MOHS approved version) Pcs 0 Nutrition
52.Immunization chart (MOHS approved version) Pcs 0 Nutrition
53.HIV rapid test kit (Commonly used test kit) (MOHS approved) Pcs 2 Infectious
disease
54.Malaria rapid test (RDT) (MOHS approved) Pcs 2 Infectious
disease
55.Dengue Haemorrhagic fever (DHF) test kit (MOHS approved) Pcs 2 Infectious
disease
56.Thermometer (Digital) Pcs 1 Infectious
disease
57.Cup for the ORS preparation Pcs 2 Accessories
58.Spoon for the ORS preparation Pcs 2 Accessories
59. Hand gel 20ml bottle Bot 2 Accessories
60.Cotton wool Pcs 1 Accessories
61.Spelling bandage Pcs 2 Accessories
62.Spirit bottle, 60ml Pcs 2 Accessories
63.Micropore Pcs 3 Accessories
64.Stethoscope Pcs 2 Accessories
65.Handy plaster Pcs 5 Accessories
66.Disposable or plastic gloves box Box 1 Accessories
67.Salter Scale Pcs 1 Materials
68.Thermometer ( Mercury) Pcs 2 Materials
69. IMNCI guidelines set Set 2 Guidelines
70. CME modules set Set 1
Modules
booklets with
CD