Emerging therapeutic approaches for osteogenesis imperfecta
Transcript of Emerging therapeutic approaches for osteogenesis imperfecta
Emerging therapeutic approaches forosteogenesis imperfectaSophia Millington-Ward, Helena P. McMahon and G. Jane Farrar
Department of Genetics, Trinity College Dublin, Dublin 2, Ireland
Osteogenesis imperfecta (OI) is an incurable genetic
brittle-bone disease. Although drug therapy, surgery
and physiotherapy represent current treatments for OI,
the search is ongoing for effective and innovative new
therapies targeting the underlying causes of the disease.
In this regard, recent advances in the fields of gene and
stem-cell therapies have been considerable. In spite of
the many challenges that remain, potential new thera-
pies for OI, which have been tested in cell culture
systems, animal models and patients, offer hope for the
future development of successful therapies. Recent
progress in the field is reviewed here.
Osteogenesis imperfecta (OI)
OI is a debilitating disease affecting around one in 12 000people, usually resulting from mutations in the COL1A1and COL1A2 genes (Figure 1). These genes encode type Icollagen, themost abundant protein inmammals and vitalfor bone flexibility and strength. Patients with OI present
Gx x Y xx
G
Yx
GxY YG
G
G x GG
G
Y Y Y xYx x Y x
GGxY Y
G
G
G xY Y
Gx
x Y xxG
Yx
G xY Y
G
GG x G
GG
Y Y Y xY
Gx
x Y xxG
Yx
G xY Y
GG
G x G G GY Y Y x
Y Gx
x Y xxG
Yx
G xY Y
G
G
G x GG
G
Y Y xY
Y
(a)
(b)
COL1A1 gene
Wild-type α1(I) chain Wild-type α2
Wild-type Type I collagen triple helix
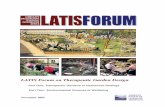
Figure 1. Schematic representation of the COL1A1 and COL1A2 genes and partial wild-ty
and introns (green box) and PolyA signals (pink) in the 3 0 untranslated regions (UTRs
respectively (AF017178 and AF004877). (b) The type I collagen triple helix consists of two
G–X–Y amino acid repeat sequence present in the chains (in which G is glycine, X is freq
hexamer, disrupts helix formation and stability and will probably give rise to OI.
Corresponding author: Millington-Ward, S. ([email protected]).Available online 10 May 2005
www.sciencedirect.com 1471-4914/$ - see front matter Q 2005 Elsevier Ltd. All rights reserved
with bone fragility resulting in fractures, frequently uponminimal impact. Themildest form of the disease, type I OI,is usually caused by COL1A1 null mutations, in which theencoded protein is not incorporated into type I collagen[1,2]. More severe forms of OI, types II–IV, typically resultfrom dominant-negative mutations in either COL1A1 orCOL1A2 [3]. In these cases, collagen fibrils are disruptedby the incorporation of mutant protein. Although over 250different OI mutations have been characterized for thesetwo genes, how different mutations result in suchclinically varied phenotypes has not been resolved. (Fora description of different mutations and the resultingtypes of OI, see http://www.1e.ac.uk/genetics/collagen; fora detailed description of classifications, see ref. [4].) Here,we focus on emerging therapies for type-I-collagen-associated forms of OI.
Type I collagen is a triple-helical heterotrimer consist-ing of two a1(I) and one a2(I) chains encoded by theCOL1A1 and COL1A2 genes, respectively. Key to theformation of this structure is a 1014 amino acid repeat
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005
TRENDS in Molecular Medicine
x x Y xG
GxY YG
G
G xY Y Yx GxG
GY xYGx Y
xG
GG
Y xY
G
xx Y x
G
Yx
G xYG
GG x
G
Y YY
xY
Gx x Y xx
GxG xY Y
GG
G x GG
GY Y
Y Gx x Y xx
G
YxGxY Y
G
G
G xY Y Y xY
xx Y x
GG x
Y YG
G
G xY YY
x GxGG
Y xY
GxY
xG
GG
xY
xG
Y
YG Y
COL1A2 gene
(I) chain Mutant α1(I) chain
Mutant Type I collagen triple helix
pe and mutant type I collagen. (a) Promoters (yellow), TATA boxes (blue), 52 exons
) (green line) are indicated. Notably, the genes are thought to be w18 and 39 Kb,
a1(I) and one a2(I) chains. Triple-helix formation and stability is dependent on the
uently proline and Y is hydroxyproline). A glycine substitution, indicated with a red
. doi:10.1016/j.molmed.2005.04.006
TRENDS in Molecular Medicine
Self-renewal
Proliferation anddifferentation
Proliferation anddifferentaion
Proliferation anddifferentaion
Mesenchhymal stem cell
Mesenchhymal progenitor cell
Stromal cell
Osteoblast Adipoblast Fibroblast-like cell Chondroblast Myoblast
Osteocyte Adipocyte Chondrocyte Myocyte
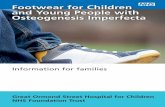
Figure 2. Diagrammatic representation of MSC proliferation and differentiation. Uncommitted MSCs can undergo self-renewal, maintain pluripotency or proliferate and
differentiate into mesenchymal progenitor cells. These pluripotent cells further differentiate into a variety of precursor cell types – osteoblasts, multipotent stromal cells,
adipoblasts, chrondroblasts and myoblasts. These cells can differentiate into osteocytes (bone cells), adipocytes (fat cells), chondrocytes (cartilage cells) and myoctes
(muscle cells). Notably, the hierarchy of cells presented here has not been fully resolved.
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005300
sequence Gly–X–Y (in which Gly is glycine, X is frequentlyproline and Y is hydroxyproline) (Figure 1). Glycine, thesmallest amino acid, is necessary at every third aminoacid position to enable triple-helix formation and stability.Although glycine substitutions represent the most com-monly observed type of OI mutation, deletions or dupli-cations have also been reported, as have mutations in theC-terminal end and mutations involving exon skipping.
Current treatments for OI include physiotherapy and asurgical procedure called rodding, which involves insert-ing intramedullary rods into femora and tibiae of youngpatients with OI. However, treated bones typically remainfragile. Bisphosphonate drugs, which slow bone resorptionby osteoclasts [5], have also been used to treat OI.Although bone pain and fracture incidence are signifi-cantly decreased in both OI mice [6] and patients [7,8],some calcification of cartilage has been observed [6]. Thequality of bone in treated patients after prolonged use ofthe drug might, therefore, be compromised [9]. Notably,none of the conventional treatments is long term oraddresses the underlying cause of OI; namely, thequantitative or qualitative deficiency of type I collagen.
Given the limitations of current treatments, severalinnovative therapeutic approaches for OI are beingexplored. For example, cellular therapies for OI havebeen investigated; there has been a particular focus on theuse of mesenchymal stem cells (MSCs), mesenchymalprogenitor cells and marrow stromal cells, all of which
www.sciencedirect.com
might give rise to, among other cell types, bone cells(Figure 2) [10]. In addition, gene therapies for OI havebeen contemplated. In some studies, gene therapy andstem cells have been combined to circumvent the primarydefect in the patient’s stem cells, thereby generating acorrected renewable cell source [11]. The assimilation ofknowledge concerning aspects of OI, from molecularpathogenesis and the generation of animal models to theexploration of therapeutic strategies, has gained signifi-cant momentum in recent years.
Animal models
Animal models of OI provide vital tools to gain insightsinto the molecular mechanisms underlying the disease.Furthermore, they represent essential systems to evalu-ate the efficacy and safety of new drug-, gene- or cell-basedtherapies. The first transgenic murine model of OI wasengineered to express a COL1A1 gene carrying a domi-nant-negative G859C mutation. Transgene expressionresulted in a reduction in type I collagen production andperinatal death [12]. Another murine OI model, Mov-13,carries a retroviral insertion in the first intron of theCOL1A1 gene, preventing the initiation of transcription[13,14]. Heterozygous Mov-13 mice display a mild pheno-type akin to human type I OI [15]. Homozygous Mov-13mice die in utero as a result of the absence of type Icollagen synthesis. The Brtl IV mouse is an elegant knock-in mouse with a classic glycine substitution (G349C) in the
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005 301
murine COL1A1 gene [16]. Brtl IV resembles human OImore accurately than previous models because the glycinemutation was introduced in the correct genomic context.Mice present with a variable phenotype, ranging frommoderately severe to lethal, mirroring the variabilityobserved in patients carrying the same glycine mutation[16]. The minigene mouse is the only model carrying ahuman mutant COL1A1 transgene [17], consisting of4.5 Kb of promoter sequence, exons and introns 1–5 and46–52 and 2 Kb of 3 0 sequence. Proteins derived from thetransgene are truncated and interact with wild-type a2(I)chains, disrupting normal collagen fibril assembly [18]and leading to a severe dominant-negative form of OI. Anaturally occurring mouse model for COL1A2-linked OI,oim, carries a deletion in the COL1A2 gene, which resultsin a2(I)-chain synthesis but not incorporation into thetype I collagen molecule. As a result, a1(I)-collagen homo-trimers are formed, leading to a severe form of OI [19].Naturally occurring forms of OI have also been charac-terized in cats, dogs, cattle and sheep [20]. Such modelsrepresent a vital resource for the future evaluation of OItherapies.
Cellular therapies
Adult stem cells have generated enormous interest inrecent years. In addition to having the capacity for self-renewal and maintaining an undifferentiated phenotypeduring the lifespan of an organism, adult stem cells candifferentiate into a select number of tissues in response tosignals. MSCs have been isolated from the stromalcompartment of marrow and have the potential todifferentiate, in vitro and in vivo, into cells of connective-tissue lineages (such as bone, fat, cartilage and muscle),epithelial cells and early neural progenitors (Figure 2)[21]. They are thought to represent w0.001–0.01% of thetotal population of nucleated cells in marrow [22]. MSCsare routinely isolated from human bone marrow from theiliac crest [22], but can also be isolated from other tissues[21]. MSCs have several interesting features. Forexample, systemically injected donor MSCs have beenshown, in sheep [23] and mice [24], to engraft into avariety of tissues, including bone. In addition, MSCsappear to migrate specifically to sites of injury [25,26].However, it appears that their homing ability decreasessubstantially after progressive culturing ex vivo [21].Furthermore, MSCs might represent vehicles for deliver-ing gene therapies to target tissues of mesenchymalorigin, potentially resulting in long-term transgeneexpression.
Allogeneic MSC transplantation might represent ameans for treating OI. Theoretically, MSCs can be injectedsystemically (making use of their potential to engraft intotissues, including bone) or directly into the bone cavity ofpatients, engraft and thereby provide a long-term sourceof wild-type type I collagen. There is some evidence thatMSCs might be either non- or hypo-immunogenic,suggesting that allogeneic MSC transplantation from anunmatched donor is a possibility without the occurrence ofgraft-versus-host disease [27–29]. In the context of OI,marrow stromal cells from wild-type mice have beenintroduced systemically to irradiated OI minigene mice.
www.sciencedirect.com
DNA from donor cells was detectable for up to 2.5 monthsin marrow, bone, cartilage, lung and other tissues. Inaddition, a small increase in collagen and mineral contentof bone was detected one month after infusion [30]. Thesame group had previously determined that levels ofengraftment of allogeneic mesenchymal progenitor cells(Figure 2) after systemic delivery to irradiated mice werebetween 1.5 and 12% [31]. Allogeneic bone-marrowtransplantation (BMT) was carried out in a human clinicaltrial involving three children with severe OI. After threemonths, 1.5–2.0% of patient osteoblasts were thought to beof donor origin. An increase in total-body bone-mineralcontent was also observed [27]. In a second study, sixchildren, who had previously undergone standard allo-geneic BMT for OI, received a further infusion ofallogeneic MSCs. One patient showed no engraftment ofdonor cells and no increase in growth velocity. Theremaining patients showed engraftment in several tis-sues, including bone, skin andmarrow stroma and showeda 60–94% increase in growth velocity during the sixmonths following transplantation. The level of donor-derived osteoblasts found in these patients was less than1% [32].
In addition to BMT and allogeneic MSC transplan-tation, autologous MSCs, modified to produce wild-typetype I collagen, represent another therapeutic option.Autologous transplantation has not yet been attempted inpatients with OI or animal models; however, the appeal isapparent. Whereas no rejection of allogeneic donor MSCshas been observed directly, only small numbers of donor-derived cells have been identified in animal and humantransplantation studies: survival rates of autologous cellscould be increased. The nature of the target tissue for OI –the skeleton – represents a significant challenge in termsof efficient dissemination for any therapy. MSCs andmesenchymal progenitor cells might represent a potentialsolution. However, this will depend, at least in part, onefficient engraftment of therapeutic cells when adminis-tered to patients. The pros and cons associated with theuse of allogeneic versus autologous cells remain to beexplored fully.
Gene therapies
In addition to cellular therapies, gene therapies for OIhave been contemplated. However, given that OI mightresult from null alleles or dominant-negative mutations inCOL1A1 or COL1A2, a variety of gene-therapyapproaches must be considered. In terms of nullmutations, gene therapy could involve supplying a func-tional COL1A1 or COL1A2 gene to target tissues. Theapproach is deceptively complicated owing to the intricateregulatory elements controlling these two genes. Addition-ally, collagen genes are large, making manipulation anddelivery problematic. Nonetheless, gene supplementationhas been explored.
Cultured cells from homozygous Mov-13 embryos, witha COL1A1 null allele, have been transfected with thehuman COL1A1 gene [33]. Efficient transgene expressionresulted in the generation of stable heterotrimers consist-ing of two human a1(I) chains and one mouse a2(I) chainand type I collagen secretion. The electrophoretic
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005302
migration of a1(I) and a2(I) chains in human–mousehybrid heterotrimers was retarded compared with a1(I)and a2(I) chains from wild-type mouse heterotrimers,probably owing to over-modification, which is alsoobserved in some patients with lethal OI. The oim mousehas also been used to explore a gene-replacementapproach. The transduction of bone-marrow stromalcells (Figure 2) from oim mice with an adenovirus (Ad)carrying murine COL1A2 resulted in the secretion ofstable collagen heterotrimers in cells. In addition, thein vivo production of type I collagen, subsequent tointradermal injection of Ad into oim mice, was demon-strated [34].
In contrast to gene-replacement therapies, gene thera-pies aimed towards treating dominant-negativemutationsmight require the suppression of mutant-alleleexpression. A variety of molecular tools are available forsequence-specific suppression of gene expression. Thesuppression of both COL1A1 and COL1A2 has beenattempted using antisense oligonucleotides [35,36], ribo-zymes [37–39] and, most recently, small-interfering RNAs(siRNAs) [40].
The principle of antisense technology – that is, the useof oligonucleotides complementary in sequence to a giventranscript to stimulate its cellular degradation – has beenused to suppress COL1A1 and COL1A2 expression. Forexample, mouse NIH 3T3 cells (which express type Icollagen endogenously) have been stably transfected withthe human COL1A1 minigene, previously used to gen-erate the minigene mouse described above. Short anti-sense oligonucleotides (ASOs) were transfected into NIH3T3 cells. ASOs that specifically downregulated tran-scripts from the human COL1A1 minigene were ident-ified: 37–80% suppression was achieved [35,36]. Inanother study, a longer antisense oligonucleotide directedto the human COL1A1 minigene was evaluated [41]. Micewith an antisense transgene, similar to the humanminigene construct except that the 3 0 end of the constructwas inverted, were generated. When antisense mice werebred with human-minigene mice, the lethality of theminigene phenotype was reduced in the offspring from93% to 27%. The study demonstrated in vivo that thesuppression of mutant collagen might be therapeutic forOI. Antisense technology has also been considered forCOL1A2-linked OI. Antisense oligonucleotides weredesigned to target a point mutation in the COL1A2transcript [42]. The mutation, at a splice donor site,causes the deletion of exon 16. Antisense oligonucleotides,targeting the exon 15–17 junction in mature RNA and thepoint mutation in immature RNA, were evaluated inhuman fibroblasts from a patient with OI. Mutant proteinwas suppressed 50–85%. In spite of moderate successes,the short half-life of unmodified antisense oligonucleotidesand the toxicity associated with chemical modification haslargely limited its application to date, stimulating a searchfor alternative gene-suppression tools.
Ribozymes are RNA enzymes that can be designed totarget and cleave in a sequence-specific manner anytranscript, using a catalytic core and antisense arms toguide the ribozyme to its target transcript [43]. Ribozymeshave been explored as an alternative means to suppress
www.sciencedirect.com
COL1A1 and COL1A2 expression. For example, fiveribozymes targeting two human COL1A1 mutationshave been shown to downregulate mutant transcriptsin vitro [39]. Ribozymes have also been shown to suppressmutant COL1A1 mRNA by up to 50% in fibroblasts in apatient with OI [39]. Furthermore, ribozymes have beenused to suppress efficiently and specifically the humanCOL1A1 minigene expressed in a murine osteoblast cellline [44]. Subsequently, ribozyme expression was opti-mized [37] using an attenuated T7-pol vaccinia virus toproduce T7 polymerase, which acts on the T7 promoterand drives efficient expression of the ribozyme, or bygenerating an octamer version of the ribozyme, which wasengineered to self-cleave into eight almost identicalribozymes, thereby increasing intracellular levels ofribozyme. Although ribozymes, similar to antisenseoligonucleotides, can be engineered to suppress a giventarget, achieving in vivo the potencies obtained in vitrohas proved difficult, promoting the search for alternatives.
A relatively new molecular tool, RNA interference(RNAi), which can be used to achieve sequence-dependentsuppression of gene expression, has emerged [45]. RNAi canbe orchestrated using small double-stranded RNA mol-ecules termed siRNAs, which are typically 19–27 nucleo-tides in length.RNAi technologywill probablybevaluable inthe development of therapeutic approaches for OI. In arecent study, this technology was combined with MSCtechnology to develop a mutation-independent therapeuticstrategy for dominant-negative forms of OI [40].
Mutation-independent gene therapies
OI is immensely heterogeneous, involving at least 250different mutations in the COL1A1 and COL1A2 genes. Interms of dominant-negative forms of OI, it is improbablethat it will be possible or cost-effective to design specificsuppressors for every mutation site. It would therefore bepreferable to design therapies that are independent ofspecific mutations and hence can be used for patients withdifferent mutations. In this regard, several elegantmutation-independent strategies have been proposed.
Recently, Chamberlain et al. [11] rationalized that if asevere dominant-negative mutant COL1A1 could beconverted to a null allele, this should lead to a mildphenotype akin to type I OI. To achieve this, an(integrating) adeno-associated virus (AAV) was used todisrupt, through gene targeting, the COL1A1 gene inMSCs obtained from two patients with OI. The targetingvector, which carried a neomycin-resistance gene, wasdesigned to disrupt exon 1 of COL1A1; 31–90% ofneomycin-resistant MSC clones were found to haveundergone gene targeting at one allele of the COL1A1gene, with the targeting event equally distributedbetween mutant and wild-type alleles. When seeded inceramic cubes, targeted MSCs differentiated towards theosteogenic lineage and when implanted subcutaneously inimmunodeficient mice the quality of bone deposited wasimproved. Type I collagen from half of the transducedMSC colonies showed wild-type electrophoretic migration(consistent with no over-modification of the protein) andhalf showed aberrant migration (consistent with over-modified mutant type I collagen). The study demonstrated
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005 303
for the first time that gene targeting by homologousrecombination can occur at high frequency in mammaliancells and that a possible therapeutic approach fordominant-negative COL1A1 mutations might involve thedisruption of one COL1A1 allele, thereby circumventingmutational heterogeneity.
Three additional strategies for mutation-independentsuppression have been outlined [46]. These approachesuse unique features of the genome to correct the primarygenetic lesion. Two strategies involve the suppression ofboth mutant and wild-type alleles of a gene in conjunctionwith supplying a replacement gene, the nucleotidesequence of which has been altered at the site ofsuppression. The replacement gene sequence can bealtered at degenerate (wobble) sites or in the untranslatedregion (UTR), thereby avoiding suppression and stillencoding wild-type protein. The third strategy involvessuppressing a mutant allele specifically at a polymorphicsite; in principle, the wild-type allele, which carries theother polymorphic variant, escapes suppression[38,40,46–48].
In the context of OI, mutation-independent suppressionbased on polymorphism has been investigated in vitro [47]and in MSCs [38] using a ribozyme targeting a poly-morphism in the COL1A1 gene. In the latter study, theribozyme was incorporated into a retrovirus and used tostably transfect MSCs; 50% suppression of the targetpolymorphic allele was demonstrated at both RNA andprotein levels [38]. Recently, the same polymorphism hasbeen used as a target sequence for potent siRNAs, with upto 85% suppression achieved in MSCs [40]. However, inthis case, although allele preference for the targetpolymorphic COL1A1 allele was demonstrated, thealternative allele was also suppressed. It is clear thatthe significant mutational diversity inherent in OI willdemand innovative therapeutic solutions.
Gene delivery
The success of any nucleotide-based therapy will depend,in part, on the vector used to deliver it to the target tissueand provide sustained transgene expression at the appro-priate level without inducing a harmful immune response.Because OI affects the whole skeleton, obtaining sufficientbiodistribution of the therapeutic presents a significanthurdle. Furthermore, the COL1A1 and COL1A2 genes arelarge (the genomic and cDNA sequences being 18.6 Kb and5.9 Kb, and 38.6 Kb and 5.4 Kb, respectively), disqualify-ing several attractive viral-vector options, which areunable to package large DNA fragments. In light ofthese constraints, various viral and nonviral vectorscontemplated for OI are discussed below, including retro-viruses, adenoviruses (Ads), AAVs, physical and chemicalmethods of transfection, mammalian artificial chromo-somes and a bacteriophage-based integrase system.
Retroviruses are double-stranded RNA viruses, whichintegrate into the host genome and facilitate sustainedgene expression [49]. In the context of OI, there have beenseveral reports detailing the transduction of MSCs withretroviral vectors in vitro. Transduction efficiencies variedbetween 18% and 85% and MSCs retained normalbiological activity, including wild-type osteogenic
www.sciencedirect.com
potential [38,50–52]. In one study, MSCs from oim mice,transduced ex vivo, were detected in the marrow cavityand trabecular bone of mice following infusion into mousefemurs [53]. Additionally, MSCs transduced with a greenfluorescent protein (GFP)-gene-carrying retroviruseswere primarily observed in the lung, subsequent tointravenous administration into nude mice. However,GFP-expressing cells were also found in bone andcartilage [54]. Although studies indicate that retroviralvectors can efficiently infect MSCs, there are seriouslimitations with these vectors. Given their maximumtransgene capacity of w9 Kb [49] and the size of thecollagen genes, in some instances the therapeutic mightnot fit into retroviruses. Furthermore, retroviruses mightpreferentially integrate into transcriptionally activeregions of the genome [55]. For example, in a SCIDhuman clinical trial, three out of 11 children treated withretrovirus developed leukaemia, probably owing to inser-tional mutagenesis [56].
An alternative to retrovirus is Ad. Attractive features ofAds include broad tropism and large transgene capacity[57]. Ads have been shown to transduce MSCs and expresstransgenes in cells and in vivo without detectable toxicity[58–60]. For example, Ads have been used to deliver amurineCOL1A2 gene toMSCs from oimmice [34]. In spiteof their transgene capacity and efficacy at transducingMSCs, Ads are non-integrating, providing only transientexpression and limiting their use.
Although the DNA virus AAV has attractive character-istics as a delivery vehicle, including genomic integration,broad host-cell range and the absence of associatedpathology in humans, the virus has a limited transgenecapacity of w4 Kb [61], probably precluding the use ofAAV for the development of OI therapeutics requiring thereplacement of collagen genes. By contrast, AAV has beenused in MSCs to implement the innovative gene-targetingtherapeutic strategy described above [11].
Viral integration and host immune response have madenonviral-vector alternatives attractive from a safetyperspective. These do not usually have the size constraintsassociated with many viral vectors. Nonviral therapiescan be delivered as naked DNA or using a multitude ofchemical or physical means, including lipids, polymersand electroporation [62,63]. For example, stable genetransfer into human MSCs has been achieved throughelectroporation [64]. Transfected MSCs retained theability to differentiate into adipocytes and osteoblasts.A significant limitation with many nonviral approaches isthe transient nature of transgene expression. In thisregard, a novel system based upon the Streptomyces phagefC31 integrase might hold great potential. Phage inte-grases facilitate site-specific unidirectional recombinationreactions between specific sites on phage and bacterialgenomes [65]. The human genome has similar sites, whichintegrase can recognize and effect a recombination eventwith a site on a plasmid [66]. Theoretically, large DNAfragments can be inserted and integrate nonrandomly.The system has been used to deliver type VII collagen tokeratinocytes from patients with recessive epidermolysisbullosa (RDEB) [67] anddystrophin tomyoblasts, the targetcell type for Duchenne muscular dystrophy (DMD) [68].
Box 1. Pertinent issues to future therapeutic development
Osteogenesis imperfecta (OI) is a genetically and clinically hetero-
geneous disorder resulting in the formation of brittle bones and is
largely due to mutations in the COL1A1 and COL1A2 genes, which
encode type I collagen. Significant barriers to the future develop-
ment of therapies include the genetic and clinical diversity of OI, the
extensive nature of the target tissue (the skeleton) and the size of the
collagen genes. For example, there are over 250 known mutations in
the COL1A1 and COL1A2 genes. Furthermore, these genes are large;
many viral vectors, including retroviruses and adeno-associated
viral-delivery vectors, are unable to hold such large DNA sequences.
In addition, the vast clinical heterogeneity inherent in OI might make
the evaluation of benefit derived from human clinical trials complex
and many COL1A1 and COL1A2 gene-control regions, such as
appropriate promoter sequences, which elicit tissue- and level-
specific expression of collagen genes in vivo, have not been fully
elucidated. Furthermore, for dominant-negative forms of OI, sup-
pression of the mutant gene will be required. Although new
technologies, such as RNA interference (RNAi), have emerged,
unresolved issues remain, such as suppressor specificity and
potency. Bone-marrow precursor cells hold great promise as either
direct therapies or as a means of providing a delivery vehicle for ex
vivo gene therapies. However, engraftment and survival levels to
date have been low and would need to be optimized to provide
significant therapeutic benefit. Nevertheless, it is timely to explore
potential therapeutic interventions for OI given the knowledge
regarding molecular pathogenesis, the availability of animal models
recapitulating human OI, the development of efficient nonviral- and
viral-vector options and the identification and characterization of
human bone precursor cells. With substantial progress made during
the past few years in this challenging field of research, we can look
forward to rewarding times ahead.
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005304
Another alternative is mammalian artificial chromosomes(ACEs), which enable the delivery of large fragments ofDNA. Notably, a red-fluorescent-protein gene has beendelivered to human MSCs using ACEs and expression wasobserved in 11% of cells following transfection [69]. Insummary, a diverse range of viral and nonviral vectors existHowever, future studies will be required to define which ofthese will prove optimal for OI therapies.
Concluding remarks
New advances in the field of OI therapeutics have beenencouraging. Now, for the first time, many of thecomponents necessary for generating viable therapies forOI might be in place. Animal models recapitulatinghuman OI enable the detailed evaluation of gene- andcellular-based therapies. Furthermore a battery of viraland nonviral vectors have been developed to assessnucleotide delivery to, for example, MSCs. MSCs andtheir osteogenic potential have been studied extensivelyand the delivery of MSCs in animals and patients appearsto provide modest therapeutic benefit. In addition, theconcept of combining cellular and gene therapy inautologous MSCs is being actively investigated, in thehope of increasing transplant efficiencies. It is as yetunknown whether the long-term survival of autologousMSCs will be better than for allogeneic MSCs followingtransplantation. With the emergence of siRNAs, a power-ful suppression agent, it might be possible to suppressmutant-collagen expression. This, combined with novelmethods to circumvent the mutational diversity inherentin type-I-collagen-linked OI, brings the development oftherapies for OI closer to becoming a reality. However,
www.sciencedirect.com
translating modest investigative triumphs into viable OItherapies still presents a multitude of challenges (Box 1)at the gene delivery and gene-therapy levels. Perhaps thenature of the target tissue for OI therapies, the entireskeleton, represents the most significant challenge to thedevelopment of successful therapies for OI. In addition,assessing beneficial effects remains complex, given theclinical variance observed among patients with OI.However, future research using MSCs in conjunctionwith new molecular tools for gene suppression and genedelivery should aid in achieving therapies for OI.
References
1 Willing, M.C. et al. (1992) Osteogenesis imperfecta type I is commonlydue to a COL1A1 null allele of type I collagen. Am. J. Hum. Genet. 51,508–515
2 Willing, M.C. et al. (1993) Molecular heterogeneity in osteogenesisimperfecta type I. Am. J. Med. Genet. 45, 223–227
3 Sillence, D.O. et al. (1979) Genetic heterogeneity in osteogenesisimperfecta. J. Med. Genet. 16, 101–116
4 Rauch, F. and Glorieux, F.H. (2004) Osteogenesis imperfecta. Lancet363, 1377–1385
5 Devogelaer, J.P. et al. (1987) Radiological manifestations of bispho-sphonate treatment with APD in a child suffering from osteogenesisimperfecta. Skeletal Radiol. 16, 360–363
6 Camacho, N. et al. (2001) A controlled study of the effects ofalendronate in a growing mouse model of osteogenesis imperfecta.Calcif. Tissue Int. 69, 94–101
7 Glorieux, F.H. et al. (1998) Cyclic administration of pamidronate inchildren with severe osteogenesis imperfecta. N. Engl. J. Med. 339,947–952
8 Plotkin, H. et al. (2000) Pamidronate treatment of severe osteogenesisimperfecta in children under 3 years of age. J. Clin. Endocrinol.Metab. 85, 1846–1850
9 Marini, J.C. (2003) Do bisphosphonates make children’s bones betteror brittle? N. Engl. J. Med. 349, 423–426
10 Baksh, D. and Tuan, R.S. (2004) Adult mesenchymal stem cells:characterization, differentiation, and application in cell and genetherapy. J. Cell. Mol. Med. 8, 301–316
11 Chamberlain, J.R. et al. (2004) Gene targeting in stem cells fromindividuals with osteogenesis imperfecta. Science 303, 1198–1201
12 Stacey, A. et al. (1988) Perinatal lethal osteogenesis imperfecta intransgenic mice bearing an engineered mutant pro-a1(I) collagengene. Nature 332, 131–136
13 Schnieke, A. et al. (1983) Embryonic lethal mutation inmice induced byretrovirus insertion into the a1(I) collagen gene.Nature 304, 315–320
14 Jaenisch, R. et al. (1983) Germline integration of moloney murineleukemia virus at the Mov13 locus leads to recessive lethal mutationand early embryonic death. Cell 32, 209–216
15 Bonadio, J. et al. (1990) Transgenic mouse model of the mild dominantform of osteogenesis imperfecta. Proc. Natl. Acad. Sci. U. S. A. 87,7145–7149
16 Forlino, A. et al. (1999) Use of the Cre/lox recombination system todevelop a non-lethal knock-in murine model for osteogenesis imper-fecta with an a1(I) G349C substitution. Variability in phenotype inBrtlIV mice. J. Biol. Chem. 274, 37923–37931
17 Khillan, J.S. et al. (1991) Transgenic mice that express a mini-geneversion of the human gene for type I procollagen (COL1A1) develop aphenotype resembling a lethal form of osteogenesis imperfecta.J. Biol. Chem. 266, 23373–23379
18 Prockop, D.J. et al. (1993) Mutations in type 1 procollagen that causeosteogenesis imperfecta: effects of the mutations on the assembly ofcollagen into fibrils, the basis of phenotypic variations, and potentialantisense therapies. J. Bone Miner. Res. 8 (Suppl. 2), S489–492
19 Saban, J. et al. (1996) Heterozygous oim mice exhibit a mild form ofosteogenesis imperfecta. Bone 19, 575–579
20 Seeliger, F. et al. (2003) Osteogenesis imperfecta in two litters ofdachshunds. Vet. Pathol. 40, 530–539
21 Barry, F.P. and Murphy, J.M. (2004) Mesenchymal stem cells: clinicalapplications and biological characterization. Int. J. Biochem. Cell Biol.36, 568–584
Review TRENDS in Molecular Medicine Vol.11 No.6 June 2005 305
22 Pittenger, M.F. et al. (1999) Multilineage potential of adult humanmesenchymal stem cells. Science 284, 143–147
23 Liechty, K.W. et al. (2000) Humanmesenchymal stem cells engraft anddemonstrate site-specific differentiation after in utero transplantationin sheep. Nat. Med. 6, 1282–1286
24 Allers, C. et al. (2004) Dynamic of distribution of human bone marrow-derived mesenchymal stem cells after transplantation into adultunconditioned mice. Transplantation 78, 503–508
25 Mosca, J.D. et al. (2000) Mesenchymal stem cells as vehicles for genedelivery. Clin. Orthop. Relat. Res. (397 Suppl.), S71–S90
26 Rombouts, W.J. and Ploemacher, R.E. (2003) Primary murine MSCshow highly efficient homing to the bone marrow but lose homingability following culture. Leukemia 17, 160–170
27 Horwitz, E.M. et al. (1999) Transplantability and therapeutic effects ofbonemarrow-derived mesenchymal cells in children with osteogenesisimperfecta. Nat. Med. 5, 309–313
28 Mahmud, N. et al. (2004) Studies of the route of administration androle of conditioning with radiation on unrelated allogeneic mis-matched mesenchymal stem cell engraftment in a nonhuman primatemodel. Exp. Hematol. 32, 494–501
29 Majumdar, M.K. et al. (2003) Characterization and functionality of cellsurface molecules on human mesenchymal stem cells. J. Biomed. Sci.10, 228–241
30 Pereira, R.F. et al. (1998) Marrow stromal cells as a source ofprogenitor cells for nonhematopoietic tissues in transgenic mice with aphenotype of osteogenesis imperfecta. Proc. Natl. Acad. Sci. U. S. A.95, 1142–1147
31 Pereira, R. et al. (1995) Cultured adherent cells from marrow canserve as long-lasting precursor cells for bone, cartilage, and lung inirradiated mice. Proc. Natl. Acad. Sci. U. S. A. 92, 4857–4861
32 Horwitz, E.M. et al. (2002) Isolated allogeneic bone marrow-derivedmesenchymal cells engraft and stimulate growth in children withosteogenesis imperfecta: implications for cell therapy of bone. Proc.Natl. Acad. Sci. U. S. A. 99, 8932–8937
33 Schnieke, A. et al. (1987) Introduction of the human pro a1(I) collagengene into pro a1(I)-deficient Mov-13 mouse cells leads to formation offunctional mouse–human hybrid type I collagen. Proc. Natl. Acad. Sci.U. S. A. 84, 764–768
34 Niyibizi, C. et al. (2001) Transfer of pro-a2(I) cDNA into cells of amurine model of human Osteogenesis Imperfecta restores synthesis oftype I collagen comprised of a1(I) and a2(I) heterotrimers in vitro andin vivo. J. Cell. Biochem. 83, 84–91
35 Laptev, A.V. et al. (1994) Specific inhibition of expression of a humancollagen gene (COL1A1) withmodified antisense oligonucleotides. Themost effective target sites are clustered in double-stranded regions ofthe predicted secondary structure for the mRNA. Biochemistry 33,11033–11039
36 Colige, A. et al. (1993) Use of an antisense oligonucleotide to inhibitexpression of a mutated human procollagen gene (COL1A1) intransfected mouse 3T3 cells. Biochemistry 32, 7–11
37 Smicun, Y. et al. (2003) Enhanced intracellular availability andsurvival of hammerhead ribozymes increases target ablation in acellular model of osteogenesis imperfecta. Gene Ther. 10, 2005–2012
38 Millington-Ward, S. et al. (2002) Validation in mesenchymal progeni-tor cells of a mutation-independent ex vivo approach to gene therapyfor osteogenesis imperfecta. Hum. Mol. Genet. 11, 2201–2206
39 Grassi, G. et al. (1997) Cleavage of collagen RNA transcripts byhammerhead ribozymes in vitro is mutation-specific and showscompetitive binding effects. Nucleic Acids Res. 25, 3451–3458
40 Millington-Ward, S. et al. (2004) RNAi of COL1A1 in mesenchymalprogenitor cells. Eur. J. Hum. Genet. 12, 864–866
41 Khillan, J. et al. (1994) Partial rescue of a lethal phenotype of fragilebones in transgenicmicewitha chimeric antisense genedirectedagainsta mutated collagen gene. Proc. Natl. Acad. Sci. U. S. A. 91, 6298–6302
42 Wang, Q. and Marini, J.C. (1996) Antisense oligodeoxynucleotidesselectively suppress expressionof themutanta2(I) collagenallele in typeIV osteogenesis imperfecta fibroblasts. A molecular approach totherapeutics ofdominantnegativedisorders.J.Clin. Invest.97, 448–454
43 Cech, T. (2002) Ribozymes, the first 20 years. Biochem. Soc. Trans. 30,1162–1166
www.sciencedirect.com
44 Toudjarska, I. et al. (2001) Delivery of a hammerhead ribozymespecifically downregulates mutant type I collagen mRNA in a murinemodel of osteogenesis imperfecta. Antisense Nucleic Acid Drug Dev.11, 341–346
45 Dykxhoorn, D.M. et al. (2003) Killing the messenger: short RNAs thatsilence gene expression. Nat. Rev. Mol. Cell Biol. 4, 457–467
46 Millington-Ward, S. et al. (1997) Strategems in vitro for gene therapiesdirected to dominant mutations. Hum. Mol. Genet. 6, 1415–1426
47 Millington-Ward, S. et al. (1999) A mutation-independent therapeuticstrategem for osteogenesis imperfecta. Antisense Nucleic Acid DrugDev. 9, 537–542
48 O’Neill, B. et al. (2000) Ribozyme-based therapeutic approaches forautosomal dominant retinitis pigmentosa. Invest. Ophthalmol. Vis.Sci. 41, 2863–2869
49 Pages, J.C. and Bru, T. (2004) Toolbox for retrovectorologists. J. GeneMed. 6 (Suppl. 1), S67–82
50 Allay, J.A. et al. (1997) LacZ and interleukin-3 expression in vivo afterretroviral transduction of marrow-derived human osteogenicmesenchymal progenitors. Hum. Gene Ther. 8, 1417–1427
51 Kalajzic, I. et al. (2001) Use of VSV-G pseudotyped retroviral vectors totarget murine osteoprogenitor Cells. Virology 284, 37–45
52 Zhang, X-Y. et al. (2004) Transduction of bone-marrow-derivedmesenchymal stem cells by using lentivirus vectors pseudotypedwith modified RD114 envelope glycoproteins. J. Virol. 78, 1219–1229
53 Oyama, M. et al. (1999) Retrovirally transduced bone marrow stromalcells isolated from a mouse model of human osteogenesis imperfecta(oim) persist in bone and retain the ability to form cartilage and boneafter extended passaging. Gene Ther. 6, 321–329
54 Niyibizi, C. et al. (2004) Gene therapy approaches for osteogenesisimperfecta. Gene Ther. 11, 408–416
55 Li, Z. et al. (2002) Murine leukemia induced by retroviral genemarking. Science 296, 497
56 Hacein-Bey-Abina, S. et al. (2003) LMO2-associated clonal T cellproliferation in two patients after gene therapy for SCID-X1. Science302, 415–419
57 Volpers, C. and Kochanek, S. (2004) Adenoviral vectors for genetransfer and therapy. J. Gene Med. (Suppl. 1), S164–S171
58 Kang, Q. et al. (2004) Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediatedgene delivery. Gene Ther. 11, 1312–1320
59 Franceschi, R.T. et al. (2000) Gene therapy for bone formation: in vitroand in vivo osteogenic activity of an adenovirus expressing BMP7.J. Cell. Biochem. 78, 476–486
60 Dayoub, H. et al. (2003) Human mesenchymal stem cells transducedwith recombinant bone morphogenetic protein-9 adenovirus promoteosteogenesis in rodents. Tissue Eng. 9, 347–356
61 Lundstrom, K. (2003) Latest development in viral vectors for genetherapy. Trends Biotechnol. 21, 117–122
62 Kichler, A. (2004) Gene transfer with modified polyethylenimines.J. Gene Med. 6 (Suppl. 1), S3–10
63 Kumar, V.V. et al. (2003) Cationic transfection lipids in gene therapy:successes, set-backs, challenges and promises. Curr. Med. Chem. 10,1297–1306
64 Peister, A. et al. (2004) Stable transfection of MSCs by electroporation.Gene Ther. 11, 224–228
65 Groth, A.C. and Calos, M.P. (2004) Phage integrases: biology andapplications. J. Mol. Biol. 335, 667–678
66 Groth, A.C. et al. (2000) A phage integrase directs efficient site-specificintegration in human cells.Proc.Natl. Acad. Sci. U. S. A. 97, 5995–6000
67 Ortiz, L.A. et al. (2003) Mesenchymal stem cell engraftment in lung isenhanced in response to bleomycin exposure and ameliorates itsfibrotic effects. Proc. Natl. Acad. Sci. U. S. A. 100, 8407–8411
68 Quenneville, S.P. et al. (2004) Nucleofection of muscle-derived stemcells and myoblasts with fC31 integrase: stable expression of a full-length-dystrophin fusion gene by human myoblasts. Mol. Ther. 10,679–687
69 Vanderbyl, S. et al. (2004) Transfer and stable transgene expression ofa mammalian artificial chromosome into bone marrow-derived humanmesenchymal stem cells. Stem Cells 22, 324–333