M. Ed. Spl. Ed. (HI / ID) ODL Programme - Netaji Subhas Open ...
ED 336 904 AUTHOR Berendes, Heinz W., Ed. - ERIC
-
Upload
khangminh22 -
Category
Documents
-
view
5 -
download
0
Transcript of ED 336 904 AUTHOR Berendes, Heinz W., Ed. - ERIC
ED 336 904 EC 300 636
AUTHOR Berendes, Heinz W., Ed.; And OthersTITLE Advances in the Prevention of Low Birthweight.
Proceedings from an International Symposium (CapeCod, Massachusetts, May 8-11, 1988).
INSTITUTION National Center for Education in Maternal and ChildHealth, Waseington, DC.
SPONS AGENCY Health Resources and Services Administration(DHHS/PHS), Rockville, MD. Bureau of Maternal andChild Health and Resources Development.; NationalInst. of Child Health and Human Levelopment (NTH),Bethesda, Md.
PUB DATE 91
CONTRACT MCU-117007NOTE 247p.
AVAILABLE FROM National Maternal and Child Health Clearinghouse(NMCHC), 38th and R Streets, N.W., Washington, DC20037 (single copies free).
PUB TYPE Collected Works - Conference Proceedings (021)
EDRS PRICE MFC1/PC10 Plus Postage.DESCRIPTORS *Birth Weight; *Congenital Impairments; Etiology;
Infants; Medical Researcn; Neonates; Nutrition;Perinatal Influences; Pregnancy; *Premature Infants;*Prenatal Influences; *Prevention; *PreventiveMedicine; Smoking; Social Support Groups; StressVariables
ABSTRACTThis proceedings document contains papers addressing
trends, determinants, and interventions in preventing lowbirthweight. Papers have the following titles and authors: "Trends inRates of Low Birthweight in the United States" (Mary McCormick);"Evolution of the Preterm Birth Rate in France" (Gerard Breart); "TheEtiology and Prevention of Low Birthweight: Current Knowledge andPriorities for Future Research" (Michael Yramer); "Support and Stressduring Pregnancy: What Do They Tell Us about Low Birthweight?"(Jeanne Brooks-Gunn); "Results of a Three-Year Prospective ControlledRandomized Trial of Preterm Birth Prevention at the University ofPittsburgh" (Eberhard Mueller-Heubach); "Decrease and Rise in Ratesof Prete= Deliveries: Haguenau Prenatal Study, 1971-1988" (EmilePapiernik et al.); "The West Los Angeles Prematurity PreventionProject: A Progress Report" (Calvin Nobel et al.); "The SouthCarolina Multicentered Randomized Controlled Trial To Reduce LowBirthweig1it,9 (Henry Heins et al.); "A Prematurity Prevention Projectin Northwest North Carolina" (Paul Meis et al.); "The Family WorkersProject: Evaluation of a Randomized Controlled Trial of a PregnancySocial Support Service" (Brenda Spencer); "The Social Support andPregnancy Outcome Study' (Ann Oakley and Lynda Rajan); "Prevention ofPreterm Deliveries by Home Visiting System: Results of a FrenchRandomized Controlled Trial" (Beatrice Blondel et al.); "SmokingInterventions during Pregnancy" (Mary Sexton); "Cervical Cerclage:New Evidence from the Medical Research Council/Royal College ofObstetricians and Gynecologists" (Adrian Grant); "Prevention ofIntrauterine Growth Retardation with Antiplatelet Therapy" (SergeUzan); "Does Calcium Supplementation Reduce Pregnancy-InducedHypertension and Prematurity?" (Jose Villar); "MagnesiumSupplementation in Pregnancy: A Double-Blind Study" (LudwigSpatling); "An Overview of Trials of Social Support during Pregnancy"(Diana Elbourne and Ann Oakley); "Inhibition of Preterm Labor: Is ItWorthwhile?" (Marc Keirse). Appendixes provide the symposium program
and list of participants. (DB)
Advana- in thePrewntion qf
Low Birthuvight
An Intenzational Sympasil tin
Proceedings
41
BEST COPY AVAILABLE
U.S. DIAARTINEP4Tor EDUCATIONOfftoit of Mahon* Ramtarch and liftgonxemottEDUCA11ONAL RESOURCES INFORMATION
CENTER {ERIC)0 his 000urnitot Disn 1110todoced
recfnvirCt from the poison of organaattononsinating ithirnof change!, have Plum MO to unpfOrreproductson ovaIlty
Pomts of veiny or opinions tatio ri Ms docu-ment do not necessinlir reortient attic*OE RI poalt;on or policy
Advances in thePraention of
Low BirthtteightSyinpasium
May 8-1 I, 1988Chatham Bais
Cape Cod, Massachusetts
Proceedings
Heinz U. Berendes. .11.11.S.. Sanuwl kessel. .11.1.1.. .11.1).11., Sumner }affe..11.1,1., editors
.spfmsiireit by the
Bureau (il. Maternal and Child Health mut 14)sources 1.1erelopnu,nt
lealtb Resources WU/ SeiTiCeS Ad1111111.tilnitiO1l
eind the
National Institute qiChild Health curd Human Developuwnt
Natimud Institutes (y.1 lealtb
(y' the
1'nitecl Slates Public Sen'ice
Mpartunent (!l. 1 learn) an(/ Human 4C1Th'es
Pmducol by
,Vaticinal Center n- Education in .11aternal and (Aid Health
tl'ilshingt( in. 1).C.
e".
4
Cite asBerendes, H., Kessel, S., and Yaffe, S. (1991). Advances in the Prevention of Low Birthweight:International Svmposium, Washington, D.C.: Natkmal Center for Education in Maternal and ChildHealth.
Advances in the Prevention of Low Birthweight An International Symposium is not copyright-ed. Readers are free to duplicate and use all or part of the informatkm contained in this publication. Inaccordance with accepted publishing standards. NCEMCII requests acknowledgment, in print, of anyinformatkm repa)duced in another publication.
Library of Congress Catalog Card No,: 91-60905
The National Center for Education in Maternal and Child I lealth (NCEMCI I) provides information ser-vices, educational materials, and technical assistance to organizations. agencies, and individuals withmaternal and child health interests. The Center was established in 1982 at Georgetown I Tniversity,within the Department of Obstetrics and Gynecology. NCEMCH is funded primarily by the LI.S.Department of Health and Human Services, through its Maternal and Child Health Bureau (formerly theOffice of Maternal and Child Health. Bureau of Maternal and Child I lealth and ResourcesDevelopment),
Piimhied and published by:National Center for Education in :Maternal and Child lit:Ali(NCEMCI38th and R Streets. NWWashington, DC 200i7(202) 625-8-400
Sil447le copies this publication are available at no cost from:National Nlaternal and Child Ilealth Clearinghouse(NMCHC)38th and R Streets, N\X''Washington. DC 200-S7(202) 62i-8410 or (703) 821-89Si x 25.4
This publication has been produced by the National Centerfor &location in Maternal and Child Healthunder its cooperatity agreement (MCI'- I 170071 with the Maternal and Child Health Bureau. HealthResources and Services Administration. Public Health Service, I S. Department 411ailth and HumanSerliaN.
5
Tableof
Contents
Acknowledgments xiii
Foreword XV
Section I: 'Rends`Frends in Rates of IJ)w Birthweight in the lnited States
.1Iary McCormick, M.D.,Se.D., Boston, Massachnssells 3
Evolution of the Preterm Binh Rate in FranceGerard Tht;art, France 13
Section II: DeterminantsThe Etiology and Prevention of Low Birthweight: Current knowledge and Priorities fcg Future
ResearchMichael Knimer M.D.. Montreal, Canada )5
Support and Stress During Pregnancy: What Do They Tell l's About Low Birthweight?Jeanne Bmoks-Gunn. PhD.. Princeton. .Ven'ioNey
Section III: hzterventionsResults of a Three-Year Pnrspective Controlled Randomized Trial of Preterm Birth Prevention atthe ITliVQrsitV of Pittsburgh
LheriPard Muellerikulmcb, Piltsbitugh. Pow.9'franiel 61
Decrease and Rise in Rates of Preterm Deliveries: I laguenau Prenatal Study, 19-1-1985Emile papiemik. (..t al., Paris. I,rance 69
The West Los Angeles Prematurity Prevention Project: A Progress ReportIlobel. M.D.. el al., Los Angeles. California 79
The South Carolina Multicentered Randomized Controlled Trial to Reduce Low BirthweightHem). LleinslLD., et al.. (..harleston. Swab Carolina
1.
A Prematurity Prevention Project in Northwest North CarolinaPaul Meis. MD., et al., Winston-Salem. North Otrolina 101
The Family Wcykers Project: Evaluation of a Randomized Controlled Trial of a Pregnancy SocialSupport Service
Brenda Spencer PhD., Manchester. !niter! Kingdom 109
The Social Support and Pregnancy Outcome StudyAnn Oakley awl lynda Rafitn, London. I 'tilled Kingdom
Prevention of Preterm Deliveries by I lome Visiting System: Results of a French RandomizedControlled Trial
Beatrice Blonde!. M.D.. et al.. Paris. France
Smoking Interventions During PregnancyAkin' Sexton, PhD.. M.P.H., Baltimore. Maryland 153
Cervical Cerclage: New Eviclence From the Medical Research CounciVRoyal College ofObstetricians and Gynecologists
Adrian Gmnt. 046rd, ()tiled Kingdom 107
Prevention of Intrauterine Growth Retardation with Antiplatelet TherapySerge t`zan. MD.. Paris. France 1--
Does Calcium Supplementation Reduce Pregnancy-Induced I lypertension and Prematurity?Jose Villar. MD.. Bethesda. Mar.vland 187
Vagnesium Supplementation in Pregnancy: A Double-lilind StudyLudwig Vatling, Herne. West Gernutily 197
An Overview of Trials of Social Support During PregnancyDiana Elhourne. PhD.. a:id Ann Oakkr. 0.0)rd. l'uited Kingdom kl3
Inhibition of Preterm Labor: Is It Worthwhile%Marc Keirse. Leiden. Netherlawls
AppoulicesSymposium Pr()gra in
List of Participants '05
10.1
Tablesand
Figures
Trends in Rates of Low Birthweight in the I Tnited Statc...s (Figure 1.1)Figure 1.1: Proponion of LBW and \IBA Births (By Race)
Statistical Findings: Evolution of Preterm Birth in France (Figure 2.1: Tables 2.1-2.9)rgure 2.1: :Maternity l'nits Invoked in the Swdv 20
Table 2,1: Design of the National Surveys 19
'table 2.2: Evolution of Gestational Age tl\ati(Whil Data) 19
Table 2.3: Ev()Iuticm ()t. Birthwcight (Natim;t1 Data} 19
Table Ev olution <f Prolatai Carc C National Data t 19
'Ethic.. 2.5: Changes in Demographic Factors tNatictnal Data) 19
'Fable 2.6: Evoltitilm of Pre(erit) Birth Rate t(lrude and Sumdardited Rate. Natittnal Data) 21
Table 27 Evollitic WI of Prefenn Birth t 1 lospital I )ata
Table 2,8 Fvolution ()I Risk Inditait r I li spiial Data)
Table 2.9 Preterm Ball) Rale t< $n Veckst in Nordic. Countries
Statistical Findings: The Elio! )gy and Prevention of Low Birthweight (Figures 3.1-3.3: Table 3.1)Figure 3.1: Relati)c Importance of Fstahlished Factors with 1)frect Caus,..d Impacts on II 'GR in
a Rural Deveh)ping Country with Endemic Malaria . .......
Figure 3.2:Relative linponamv t Fstabhshed Factors with 1)irect hnpacts on II "GR ina Developed Cc nintry Where 10 Percent of Women Smoke During Pregnancy
Figure $.3: Rehtive lmpciitthce c)t. Established Factms with Direct Causal Impacts on Pronaturity it)De%clopecf Country Where 10 Percent of Women Smoke During Pregnancy__ ................
Tahlc 3.1: FaLtors Assessed for Independent Cau),a1 Impact on Intrauterine Growth and C. iestatt(mal Duration .3i
Statistical Findings: The Role of Support and Stress During Pregnancy I Figures A.1-1.2e: Table i.1)Figure f.1: Social Support and the Buffering IfypothesisFigure 1.2: Five Possible N1(Klels tOr Studying .Associati( in, Between Psych( is( icial Factors and Pregnancy ( )utconws
Ei,ore i.)11.: Direct Niects Minty!. ...... ............... , ..... i()Figu e 1.21): Direct OC'ets .11Hdel. bIterrehahms.liiiinig PsivhisoculI Eacti)r .....
Figure i..2c: Direct and Indirect /Weds .11ridel.
bilernitiliHns Intwg, and Bettirot Psivhomie lid Fat 1(nN and .Stic iudenirtgrapInc ..S0
Figure Durtt antiP810.7u..ncial Sociottenupgraphic LimihtualS, Hcalth Ik'bdtlor it)
Ilediated Mudd. 1:fik Thrwigh Health Beharuir
Tahle #.1: Correlates of Cigamte-Smoking in Pregnanc\ Among Women of Central I larlem . .
Results of a Three-Ycar Prospective Controllr2d Randomized Trial of Preterm 13irth Prevention atThe University of Pittsburgh (Figure 5.1)
Figur-L. 5.1:Percentage of Patients with Preterm Pretenn Birth, and Tocolysis During theThree Years of the Study
Statistical Findings: Decrease and Rise in Rates of Preterm DeliveriesHaguenau Prenatal Study 1971-1978 (Tables 6.14).8)
Figure 0.1:Regression Curve for Wc,inen by Group and Number of Pretenn DeliveriesTable 0.1: Pretenn Deliveries and Live BirthsTable 0.2: Transfers to a Ne( 'natal Intensive Care 1Table 0.3: Days of ilospitalization Related to Pretenn DeliveryTable OA: Neonmal Deaths Po. Thousand Live Births -0Table 0.5: Rates of Preterm Births, by Risk Factor. by PeriodTable 0.0: Rates of Pretem Births. When a Risk Factor \Vas Observed or Not Obsen,' 70Table 0.-": Rates of Iligh-Risk Factors Anumg Pregnant Women by Study Pericid -0Table 0.8; Change in lkenatal Caw and Pretenn Binh Rate According to Parental Educational Level
The West Los Angeles Prematurity Prevention Project: A Progress Report (Tables -7. l-1.2)Table '.1: West I.os Angeles Prematurity Prevention Project Preliminary Data .......... 82Table 7 .2: Psychosocial Risk Factors Associated with Preterm Birth 83
Statistical Findings: The South Carolina MulticenteredRandomized Controlled Trial to Reduce Low Birthweight (Figure 8.1; Tables 8.1-8.5)
Figure 8.1:The South Carolina Multicentered Contn4lcd tz Ili! R Ito ..i'LLICV LOW Birthweight .
Thhle 8.1: Selected Maternal Characteristics 96Table 8.2: Selected Maternal Characteristics 9-Table 8.3: South Carolina Randomized Controlled Trial Sur\ ce Statist cs t Live Births). Analytical GnIup 98Table 8.i: Birthweight Outcoines (Live Births) 99Table 8.5 Birthweight ()utcomes (Live Births) 9')
Statistical Findings: A Prematurity Prevention Project in Northwest North Carolina(Figures 941-9.5: Table 941)
Figure 9.1: Rates of LBW and VLBW Births in Northwest North . ..Figure 9.2: Rates of LBW Births Within the Projeu s. Rates Among 1'nenrolled Private Patients ............... .Figore 9.3: Rates of VLBW Births Within the Project vs Rates Among I'nenrolled Private Patients 1(K)
Figure 9.1: Rate!-: of Premature Births t< 38 Weeks Gestation) Within the Project vsRates Aiming l'nenrolled Private Patients 100
Figure 9.5:Rates of P-LBW Births Within the Pniject vs Rates Among I 'nenrolk.d Private Patientsable 9.1; Private Births in Northwest North (;:irolina
Statistia Findings: The Family Workers Project: Evaluation of aRandomized Controlled Trial of a Pregnancy Social Support Service (Figure 10.1; Tables 10.1-107)
Figure 10.1: Overview of Trial ..........Table 10.1: Study PopulationTable 10.2: Reasons for Non-AcceptanceTable 10.3: Outccime Information Not ObtainedTable 10.4: Mean Birthweight (Singleton Live and Stillbirths) and Length of Gestation
0Table 1.5: Proponion I.(iw Birthweight. Small for Gestaticinal Age. and Preturm Babies
118
119
120
2(11211
Table 10.0: Outctnth: of Pregnancy 121
Table 10.7: Categorization ()I t.;statkmal Age. Excluding Terminations for litith Stu. al and Medical Reasons 121
Statistical Findings: The Sodal Support andPregnancy Outcome Study (Figures 11.1-11.2; Tables I 1.1-11.19)
Figure 11.1: Consent. Randomization. and Data Collection Provediires 133
Figure 11.2; Study Sample :ind Pregnancy Outcome by Assigmnent into Interventkm ..tnd Comrol 133
Table 11.1: Structure And Content of the SSPO Interventkm 134
Table 11.2: Otinparability of Groups at Reeruittnent to 'Fria! 13.1
Table 11.3: NIcan Birthweight 134
Table 11.4: Low Birthweight 13i
Tidily 11.5: Ges:iilion it Delivery 135
Table 11.0; Onset of Libor 135
Table 117: Mean Length of Labor 135
TAIle 11,8: Type of DeliveryTable 11.9: Analgesia .Anesthesia in Libor'raffle 11,10: Maternal Phsieal Ifealth in Pregnancy 130
11:ii(6)
Table 11.11: Medical C:ire in PregnancyTable 11.12: Nlaternal Physical Ilcalth Atter BirthTable 11.13: Baby's Condition After Birth
1.4Table 11.1 t: Baby's Care After Birth 132
Table 11.15: Baby's 1Icalth After Birth'Lillie 1 1 . 16: Psvcluisocial Outcomes 13"
able IAA": Partner's Stipp( wt and IlcIp During Pregnancy. Birth, and Atter Birth 1 3-
Tahle 11.18: Attitudes Toward the Intervention 138
l'ahle I 1.19: Value cif Contact with NIidwile in Pregnancy 13S
StAistical Findings: Prevention of Preterm Deliveries 1w !Ionic Visiting System (Tables 12.1-12.0)Table 1 2.1: Nlaternal DemographL tnc1 Scwial Characteristics 149
'Fable 12,2: Conn.:it:0(qm Cervical state at Study Entry 149
Table 12.3: Prenatal Care Alter Study EntryTable 12.4: Nlother's View ot Prenatal Care1...11)1e 12.5: Ink Wination CAintractions ;end liedrest
Tahle 12.o: tiedit..st and limle
150
Statistical Findings: Smoking Interventicms During Pregnancy (Tables 13.1-13.9)'Lihie 13.1: !:.stimates ut Relative Risk tor Principal It 'C,R Risk Factors
Table 13.2: Smoking Characteristics Contnil and Treatment Groups at Eighth Nli)illh t Pregnano- .
Table 13.3: Nleasurement ()t. status (4. Newhtirn
163
13.,f: Restilis of Three Randoini/ed Clinieal Trials
1(13
1
16113.5: Smoking and Gestaticinal Characteristks by it(71's Examining Birthwvight
Table I $.0: inter\ ention and Vic k.ation Characteristics ot RCI's of Examining Binhw eight .. ...... 11(6,34
Table 13,-: Quit Rates and l3irilvglns 1)V Rini Ica 11: and Nlarvland Colton,. . 105
Table 13,8: Quit Rates and Birthw eights tor Blacks and \\'hites in Nlaryland Cohort
Table 13.9: Additional Randonlifed Clinic:al Trials of Smoking Cessat )n
........... 1 (r";
1 tv;
Statistical Findings: Crvical Crckige: New Evidence From the Medical Research CtnincilRoyal College of Obstetricians and Gynecok)gists (Tables 1.1.1-1,4.5)
Table Ill: Iiti ii CcRical Cerclage c in C )bstetric Nlanagement----FA idcnie hoin the Rand,imized Trials 1-3
TAN,: j +.2., HIcts Cvrcical Ccrdage t n ( A) 1)cliverv 1h.tOre 33 Wc'eks and ( B) NliNcarriage,
;Ind Neunatai Death Ctimbined--Evidenie truni the Four Randinni/ed Trials 1- t
Table 1 t.3: 11 it Prophylactic. (:rvical Cerclage Atter Pre ions Second Trimester Nlicarriage e ir Preterm
Delivery fin ) 1)eliery Before 3 Vi.eks and ( HI Miscarriage. Stilibioh, and Neonatal Death._ ..... .1-
Tahle 1 ie t PR)phyLalik. Cervical COI:Lige kir Tv. in PR.griani. on (A I h. hytTV 1 M.( v 33 Wecks and
Ili) Miscarriage, Stillbinh, and Neonatal Dcath 1-5
Statistical Findings: Cervical Cerclage: New Evidence From the Medical Research Council/Roya' College of Obstetricians and Gynecologists (Thb les 1-+.1-1.1.5. Continued)
A)1(.. 1.1.5: Effects of Prophylactic Cervical Cerdage for Women at Moderate or Low Risk of Early Dehvery on(A) Delivery Before 33 Weeks and (13) Miscaniage. Stillbirth. and Neonatal Death 175
Statistical Findings: Prevention of Intrauterine C;rowth Retardation withAntiplatelet Therapy (Tables 15.1-15.4)
Table Design Characteristics of Five Rev.ewed Studies 183Table 11.2: Sampie Sizes and Other Criteria (4. Eive Reviewed Studies 153Table 14;.3: Summary of Results of Three Completed Studies 1S:tTable ICA: Evolution of Iii(nnechanical M(mitors
18.1
Statistical Findings: Does Calcium SupplementationReduce Pregnancy-Induced I iypertension and Prematurity? (Figure's 16.1-16.3: Table's 10.1-16.()
Figure 10.1: Differences in Adjusted Mr-cid Pressure Nlean Values at Term Between Calcium and PlaceboGroups (Adjusted for Race and Initial Blood Pressure < 2( Aeeks) .194
Figure 10.2: Differences in Systolic Blood Pressure at Term Between Calcium-Supplemented and theCoiTesponding PLicelto Groups in Two Studies of Calcium Supplementatkin 1/uring Pregnancy ..... 19:1
Figure 10.3: Study Design. Randomized D(mhle-Blind Controlled Clinical TrialTable 10.1: Incidence of Pregnancy-Induced I lypertension Data from Calcium Supplementation Studies 193Table 10.2: Reliability of Bloc id Pressure Measurements. Rosario. Argentina (Whites) 193Table 10.3: Reliability of Bloc )d Pressure Measurements. Johns llopkins Ilospital (Blacks) 193Table 10,:t: Outcome Variables f( ir the Randomized Clinical Trial ot Calcium Supplementation
/uring Pregnanc19-1
Table )03: Effect cif Calcium Supplementati(in in 1111 Preeclampsia:A Randomi/ed Double-Blind Contnilled Clinical Trial 19.t
T.thle 10.0: Etruct )1 Calcium Supplementatkin on the Ineidence of Prematurity and 1.(itt 13inhtt eight 19a
Nlagnesium SLipplementation in Pregnancy: A I)ouhle-Blind Study (Tables 1-.1-1-.2)Thhk 1-.1 Comparison Between Magnesium and Placebo ('InnipsTable 1-.2: Ccimpariscin Betwecn NLtgnesium and PLicebo Groups After Exclusion of
Patients Who Did Not Take Their Tablets Regularly 2(10
Statistical Findings: Prevention of Preterm Deliveries by I Ionic Visiting Systcm(Figures 18.1-18.8; Tables 18.1-18.2)
Figure 18.1: Effect of S ocial Support in Pregnancy (as an Explicit co-lniert entioni tinPreterm ' /divert- Rate (< 3- \\ eeks)
Figure Effect (CI Social support in Pregnancy (as a Primary Inter\ ention)Pieteriii I/cliverv Rate (< 3 Veeks) 221
Figure 18.3: Effect (if oci.il suppon in Pregnanct (as an Eylio (:(,-InterN entu CI)Extremely Preterit) Dein cry Rate (< 33 Weeks) 'I
Figure 18. Effect of St n ial Supp(irt in Pregnancy (as a Pr)mal) Inter\ ention3 (Extremely Preterm Delivery Rate « 33 weeks)
Figure 183: Ettect tit S oct:il StIppcla in Pregnancy (as an Explicit (:(-Intervention) inrow Birthweight Rate t< 2:1(H) g)
Figure 18.0: Iltect of Social Support in Pregnancy (as a Prnriary Intervention, onIt iw Bin Int eight Rate t< 2-400 gi
. . ......... 123
Effect of s cicial Stipp( in it) Pregnancy (as an ExpIk.it Co-Interventicin I onVery 1.(A% Binhv eight Rate (< 1500 g)
Figure 18.8: Effect of St )cial Suppon in Pregnancy (as a Pr Mart Interventicm) tinVerv I.( At Birthweight Rale (< I SOO gt
Statistical Findings; Does Calcium Supplementation ReducePregnancy-Induced Hypertension and Prematurity? (Figures 18.1-18.8; Tables 18.1-18.2, Continued)
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy '13TaNe 18.2: t ncompleted Trials of Explicit Social Support in Pregnancy )70
Statistical Findings; Inhibition of Preterm Labcr:Is It Worthwhile? (Figures 19.1-19.6; Tables 19.1-19..1)
Figure 19.1: Effect of B,etamimetic Drug Treatment in Preterm Lahor on the Incidence of DeliveryWithin 2+ flours in the 1.f Trials Which Plovided Data on this Outcome '53
Figure 19.2: Effects of Bet:unimetk. Drug Treatments in Preterm Labor: 'Typical Odds Raticr..With l'heir 25 Percent (:onliiknce Inter-v:0s. ..kcrossi.ri:ds for the V.iri)us Outcomes Studied
)nwFigure 19.3: Effect cif Betamimetic Drug Treatment in Preterm Lalxir On the tocidence of Severe Respirahwv
Disc wders Including Respiratory Dktress Syndr( 25 I
Figure 19.-t: Effect of liciamimoic Drug Treatment in Preterm Libor on the Incidence of Perinatal NlortalitvNot Attributable to I.ethal Congenital Malformations )51
Figure 193: Comparison Between Betainimetic Drugs and Eth:mol for Treatment iF Preterm Labor:Effects on the Incidence of Delivery Within '18 to -.2 liEmrs After Entrt: into the Trial 2-S5
Figure 19.0: Effects of lndomethacin in Preterm Labor: 'Typical' Odds Ratios. With Their 95 Percent ConfidenceIntervals. Across Trials for the Various Outcomes Studied 255
Table 19.1: Summary of Appntaches Vsed to Inhibit Preterit) Labor in the Past Years and TheirPurported Success Rates in the First English Language Publication Documenting Their I se
Table 19.2: Characteristics of Birth and In-Hospital Mortality and Morbidity in Infants Born Alive Bel( we32 A-CAS (22.1 Days) of Gestatkyn in the Netherlands in 1983 14-,1
Table 19.3: Agents Reported to he 1 sed for the Inhibition ot Preterm Labor in the Liteure Since 1980 )432
Table 19..1; Characteristics cif the Trials Comparing Betatnimetics With Ethainil tor Inhi1,41 in (if Preterm Labor ....252
xi
Acknowledgments
TIIE STEERING CONIMITIVE IS INDEIffED TO Till'.sponsorship of the meeting by the Task Forceon the Prevention of Low Birthweight of theSecretaty of Health and Human Services andthe financial support provided by the Maternaland Child Health Bureau. Ilealth Resourcesand Services Administration. and the NationalInstitute of Child Health and HumanDevelopment, National I nst itut es of Health ofthe Public Ilealth Service. United StatesDepartment of Health and Human Services.We also acknowledge gratefully the supportprovided by Ruby Hearn from the RobertWood Johnson Foundation and Richard
lorton from the Nlarch of Dimes.Much of the credit for obtaining
manuscripts from the conference participants,editorial corrections and assembling of finalmanuscript drafis belongs to Martha Gordonwho also contributed immensely to the plan-ning and arrangements for the originalCltatIlam conference.
Foreword
A MAIM DITERNIINANT OF INFANT NIORTALITYis low birthweight. particularly very low birth-weight births. Very low birthweight births(under 1500 grams) account for almo,zt 50 per-cent Of deaths during the first year of life.
Neonatal intensive care is very expensive.particularly for the very low birthweight orseverely premature baby. and the cost ofneonatal care in the tinited States has beenestimated to be about S2---S2.5 billion per year.In addition, a significant prop( )11ion of surviv-ing small premature babies have substantialneun )gical, behavioral or learning pa )blemsas they grow up in society.
Prevention of low birthweight. therefore,has become ',I mai( w national objective. andresearch and interventions designed to achievea reduction in the risk of low birthweight areof the highest priority.
In 1985 Dr. Emile Papiernik organized ameeting entitled "Pievention of Pretenn Births"with the subtitle -New Goals and New Practices
14
Advance.. in the tremnion qf Lute Birlinveight
in Prenatal Care- which was held in Evian.France. May 19-22, 1985. It brought togetherscientists from around the world involved inclinical trials or community-based interventionsaimed at reducing the risk of preterm delivery.This meeting was highly successfUl and provid-ed an excellent assessment of the then-ongoingeffort to prevent preterm births and served asan important forum for exchange among vari-ous investigators. It also emphasized the impor-tance of clinical triak in perinatal medicine.
In this spirit, a steering eonimittee wasformed in 1987 to plan for a follow-up ilmfer-ence which was entitled -Advances in thePrevention ()FLOW Birthweight- which many ofus affectionately called Evian II. Members ofthe Steering Committee included Drs. RobertCreasy, Cal Hubei. Woodie Kessel. IrwinMerkatz. Richard Morton. Sunnier Valle andHeinz Berendes. We wanted to bring togetherresearchers conducting clinical trials or commu-nity-based interventions aimed at reducing therisk of low hirthweight. It was our belief thatexpanding knowledge through this state-of-the-art review of strategies for preventing loN:birthweightthe principal determinant of riskfor poor survival and or life-Icingmorbiditywill greatly enhance our ability toprovide quality health services to vulnerablepopulations and significantly cc mtrihute to theadvancement of matemal and child health inthe I'nited States and worldwide.
The papers presented in this volume covera broad array of scientific investigaticms whichincludes biological (...xposures, clinical trials ofthe effect of social support during pregnancy onbirth oUtcoine, the Use of antiplatelet therapy toprcvent preeclampsia. and possible beneficial
effects on the risk of pretem delivery throughcalcium supplementation or magnesium supple-mentation. A concluding discussion attempted toidentify directions for future research.
There was a spirited exchange alx)ut scien-tific intervention projects in urban populationsand international collabcnatk)n. Slumld we testsingle or multiple interventions, especially ininner-city populations? Dr. Papiernik's interven-tion strategy in France consisted of multipleinterventkms. His pnigram also appeared to bemost effective in low- or medium-risk womenrather than high-risk women. Overwhelmingsocial problems in inner-city populations in theUnited States May create immense obstacles tothe evaluation of the Papiernik educatkmalinterxention model and therefore socially high-risk groups may be inappropriate for testing ofthese interventions. In designing social supporttrials what is meant by social support? Patients'percepticni may be different film) investigators'intention. There is urgent need for an improvedrisk assessment tool although the currentimprecisi(m of risk assessment may be an accu-rate reflection of our very limited understand-ing of the determinants of preterm delivery orintrauterine gn)wth retardaticm.
Considerable attention v.as devoted to adiscussicm of methodological issues and end-points (A interventions sudi as biological vari-ables and or rroNies for mortality andmorbidity.
We have the sincere hope that this seriesof conferences which Dr. Emile Papiernik initi-ated in Evian in 1985 has made a significantccmtributkm to our knowledge and ability IC )improve the health and well-being of futuregeneratic ms.
15h Arewon I
Treridc in Rates qf Low Bilibueightin the United States
NIARIE MCCORMICK, 1\1D,, Sc.1).
INTRoDuclioNPresenting this topic to this audience repre-sents a classic example of the "coals toNewcastle" phenomenon. This phenomenonwill become particularly evident as the discus-sion unfoIdssince it relies so heavily on thework of several here. What I hope to achieve,therefore, is to summarize what can be charac-terized as -what we already know" hy way ofintroduction to this conference.
IMPOWIANCE OF Low. Bum WEIGI-IT
What do we -know- al)out the importance oflow birthweight (LBW)? In the United States, in-fant mortality rates remain relatively high com-pared to other industrialized countries.' Mostinfant deaths now occur in the neonatal period,and the majority of neonatal deaths occur
Advances in the Pretention Birtinveight
among LB\X1 infants." The persistence of highlevels of infim; mortality is not because we havefailed to achieve dramatic declines in infant mor-tality over the past 20 years. These declines,however. reflect our success in reducing themortality rates anumg small babies; indeed, ourbirthweight-specific mortality rates may beamong the best in the world. A recent reportfrom the U.S. Congress' Offk.e of TechnologyAssessment (MAY illustrates this point. Over thepast 20 years, the mortality rate among very tinyinfants has declined dramatically, while the pro-portion surviving with severe to moderate handi-cap remains small. Thus, the proportion ofsurvivors in reasonable health has increased.
In spite of this increase, the persistentminority who survive with appreciable levels ofhandicap is of concern. Nh)reover, the cost Ofcare for such tiny infants is substantial, andremains high even when compared to our seem-ingly exorbitant costs for a -normal- delivery.-Thus, both on a health and on a financial basis,low birthweight presents an important pix)blern.
MEANING )l IA AV BUM tWl1GIFF
Likewise, we know that a discussion of10 )w birthweight is really a shortlund notationfor the adequacy of a complex physiologic pro-cess: intrauterine fetal gr()wth. At each week ofgestation, there is a distributkin of birthweights.Using a cut .off point or grouping based cmhirtIm eight, then. clearly captures a gr()up thatis heterogeneous for duration of gestation:Both birthweight and gestational age are relat-ed to mortality,- and fc)r many purposes gesta-tional age is the better indicator of risk.
Birthweight tends to be inure accurately mea-sured and less likely to be missing from ourvital statistics data, however, and has thereforebecome the tneasure most frequently used indata from the t Inited States.
Let us also quickly acknowledge that refer-ring to birthweight groupings or cut-offsreflects a somewhat arbitrary point along acontinuum of risk and mortality. In otherwords, 2500 g or 1500 g does not represent abiolc)gic discontimity, but a cut-c)ff point whichhas achieved utility as a marker of risk throughrepeated usage. Because certain groupings orcut-off points have achieved currency and theirmeaning is well understood, we will continueto use them in this discussion.
Let us return, however, to pursue the pointof intrauterine growth a hit further. Low weightat birth may result from one of two pro )cesses.either independently or in combination: ( )
shortened duration of gestation, or (2) lessgrowth than womid be anticipated fon a givenlength of gestaticm. Among the former, growth(height and weight) is appropriate for gestatk )11-a I age (A( A), but delivery has occurred befc)re37 weeks of completed gestation. t 'nlike growthretardatkm, the causes of preterm labor and thefactors which increase the risk of it require fur-ther elucidation.' Among the latter, which isattributed to intrauterine growth retardation(11'GR), the infants are judged to be small forgestational age (SGA) hy being horn less thanthe established percentile fc)r growth fc)r a givengestational age. A variety of conditions are asso-ciated with An SGA infant may ako bepremature. At a given gestatk)nal age. an SGAinfant is less likely to survie than an AGA infantwhere higher weight confers an advantage. At a
1 s
Trends in Rates (f tow Biabweight in the ()tiled States
6 -A
given birthweight, however, maturity confers theadvantage to the SGA infant until term.'
CI IANGES OVER TIME
What, then, has the recent U.S. experiencebeen in terms of trends in low birthweight overtime? Unfortunately, the rates of low birth-weight are not changing very much. The pro-portion of live births less than 2501 g hasdecreased slowly by a little more than 15 per-cent in die past 15 years (see figure 1.1). Theproportion of live births less than 1501 g. how-ever, has remained the same or risen slightly.Thus. while the prc)portion of LIM births hasdeclined overall, this population is now weight-ed toward the lower end of the birthweight dis-
Mends
tribution with a higher proportion of the veryhigh-risk births.9 Most births less than 1501 g,both AGA or SGA, are also preterm. Thesetrends suggest that much of thv decrease whichwe have experienced is in low birthweight dueto IUGR. This interpretation is supported byother analyses."'" What factors may be invokedto explain this trend or lack of trend?
FActI AssoctATED WM !-
TRENDS IN .Low Bun 1WEIGIrr
The most striking factor in the U.S. experi-ence remains the racial disparity in rates of lowbirthweight." The LBW rate for blackAmericans is twice that of whites and otherracial/ethnic groups, and is well above the
Figure 1.1Proportion of LBW and VLBW Births, By Race
4 -
A A
1(150 1955 196() 1%4 1'170 PM7
NtrnA hitt. < 2500 g Whitt. < 2500 g
Marie McCormick
1 5
11111 Non-whitv <. I 500 g Whitt- < I -AM g
Advances in aw Prelyntion cf Low Birthweigbt
objective set for 1990. This higher rate of LBWis paralleled by higher infant mortality rates.although unlike LBW, the mortality rates aredeclining." What accounts for this difference?
One hypothesis is that there are genetic orinherited differences in birthweight distributions.Support for this argument can be derived fromstudies which document an intergenerationaicorrelation of birthweight. In addition. analy-ses which compare the full range of birth-weights between ethnic groups reveal that theentire birthweight distribution for blacks is shth-ed downward." Such shifts suggest that standardcut-off points, such as 2500 g. do not connotethe same degree of risk for black b::-ths as fornonblack births. Indeed, for a given low birth-weight. black infants have lower birthweight-specific mortality rates than whites. Adjusting forbirthweight distributions results in higher mortal-ity rates throughout the birthweight distributionfor blacks, however, supporting the argumentthat they are at a disadvantage." While thepotential genetic contribution of race to birth-weight and the appropriate statistical techniquesfor adjusting for differences in birthweight distri-bution require further study. disparities in birth-weight among subgroups within the blackpopulation using conventional markers of birth-weight risk suggest room for improvement with-in the current genetic endowment. It is thesedisparities among subgroups which we willexplore further.
Epidemiologic tradition has identified threesociodemographic characteristics which areassociated with increased risk of low birth-weight: (1) young maternal age. (2) low mater-nal educational attainment. and (3) maritalstatus.' Blacks remain at a disadvantage by hav-
ing higher proportions of births to women char-acterized by these factors than whites. For bothgroups, however, the pr()portion of mothers lessthan 18 years of age and mothers with less than12 years of education (graduatk)n/schooMeavingnorm for the ITnited States) has decreased: theproportion of mothers who are unmarried hasincreased, but this probably does not connotethe same degree of risk now as it did in morepermissive times. It' anything, then, the relativerisk for these variables has declined, which rep-resents a trend that is not consistent with thetrend in low birthweight.
These factors are not independent. Awoman who initiates childbearing earl is lesslikely to complete school and to he married.Kleinman and Kessel have examined this ques-tion for selected states in the years 1973 and1983.'" When these factors are analyzed in com-bination. the relative differences between blacksand whites diminish among the high-riskwomen. In other words, women who are at highrisk by virtue of their age and or educationalattainment have similar pregnancy experiencesregardless of race. Thus, part, but not all. of theracial disparity can then be attributed to the factthat black births are niore likely to occur amongwomen who fall into the high-risk categories.
If this is the case, then, what is it aboutmaternal age or education which leads tO thehigher rates of IOW birthweight? Although blacksare twice as likely tO be adolescent mothers, andsubstantially more likely to he very young moth-ers. the relative risk of a low birthweight birthfor young hlack mothers c(nnpared to olderblack mothers is less than the relative risk foryoung white mothers compared to older whitemothers. These findings are consistent with the
2 0
Trends in Rules (y* 1.(m' Birtbeivigbt in the ()tiled States
increased risk of eVen -low-risk" black mothersnoted earlier. They are also consistent with an in-terpretation that age per se does not confer risk.Such an interpretation is reinforced by the find-ings of special programs for adolescent motherswhich reduce the risk of adverse outcome, hutonly to the level of older mothers in their emi-ronment. A similar picture emerges with educa-tion.1; Thus, changes in sociodemographiccharacteristics of mothers account for a relativelysmall percent of the trends in low birthweight.
If education or age per se does not accountfor what we see, then perhaps the questk msshould be rephrased. Is there some factor whichis associated with early child bearing. 10 AV educa-tional attainment, and perhaps black face whichleads to adverse outcome? In other words. arethese factors markers for other, truly causal fac-tors, factors which would pertain to luith whitesand blacks, but to blacks disproportionately? Animmediate candidate leaps to mind; poverty.
Consideration of poverty as a causal factorsuggests a number of pathways by which therisk of low birthweight might be increased.Since much of the remainder of the conferencewill be spent in discussion of many of thesefactors and potential interventions to amelioratetheir effects, 1 will restrict the following discus-sion to illustrative examples.
One aspect of poverty is a restriction Offinancial resources to obtain needed goods andservices. A necessary. if not totally sufficient, ser-vice or set of services hi attaining positive preg-nancy oflit (*Mlle S is adequate prenatal care.Inadequate prenatal care is higher anumg low-income gnitips and among the high-risk groupspreviously noted.`' This deficit for mothers in theUnited States reflects, in pan, gaps in payment
Marie McCornikk
21
l'rends
for maternity services which stem from our medi-cal care financing customs: 17 percent of allwomen of childbearing age lack insurance formaternity services. Even with private insurancecoverage for MOSE medical services, maternitycare may only be partially covered or not cov-ered at all, since pregnancy is considered anelective event not amenable to classical insur-ance actuarial techniques. Another 10 percent ofwomen of childbearing age rely on publicresources, but even those eligible for public sup-port may find obtaining prenatal care difficult.Participation may be limited by complex applica-tion processes and inadequate fee schedules tocover the usual costs of maternity services:
Consistent with a relationship between pre-natal care and pregnancy outcoine is the fact thatgnmps identified as high risk are more likely toreceive inadequate care.' Mc wet )Ver. the propor-tion of women potentially at higher risk foradverse outcome who start their care in the firsttrimester has changed little over the past few
years, which is again consistent with the lack ofchange in pregnancy outcome. As with maternalsociodemographic characteristics, however, elim-ination of those with less than adequate carew(mld have only a modest effect on the rate oflow birthweight (a 12-1.C('4, reductkm ), Even
c(mibining this with reductions of those withsociodemographic risk results in a decrease ofonly 29 percent in the LBW rate for whites and30 percent in the rate for blacks.'"Fhus. accessto prenatal care is only part of the problem.
Constrained financial resciurces may alsoindicate an inability to obtain other necessitiesfor a good pregnancy outcome. One which hasreceived attention is adequate nutrition.Controversy exists as to the proportion of the
Advances in the Prevention (y. Low Birthweight
U.S population experiencing hunger or aninability to Obtain the needed daily caloricintake to sustain weight. Mtal caloric depriva-tion, however, is less likely than inappropriatemixture of basic foods and other nutrients.Since it is not clear what an "appropriate mix-should be. the exact deficits in the diets of thepoor cannot be readily identified. That thereare deficits is suggested by the data on theeffectiveness of the WIC program (SpecialSupplemental Food Program for Women,Infants and Children).'" This is not unalloyedevidence, however, since this program providesa mixture of services, as well as ft >Oct supple-ments. The area of appropriate nutrition repre-sents :in area of further research.
Consideration of other aspects of theeffects of poverty reveals additional mecha-nisms by which it may contribute to adversepregnancy outcome. Substantial evidence existsto support a relationship between poverty andpoor health generally. With regard to pregnan-cy outcome. maternal health factors wouldinclude the (I) relationship of specific healthproblems as complications of pregnancy, and(2) health practices which might affect bonfimaternal and child health. Among the latter arethe use of cigarettes, illicit drugs, and excessivealcohol, In addition, certain types of physicalactivity inav increase the risk of pun. pregnan-cy outcome., ;IS suggested by the data forwomen with physically and emonkmally stres.s-ful lobs which require long commutes.th In theUnited States as a whole, approximately 30 per-cent of women smoke and 55 percent drinkbefore their pregnancies. hut a pro)portionbecome abstinent during pregnancy, so thatclose to half of U.S. women do neither during
their pregnancies.'" National data on smokingdo non reveal much disparity between the ratesof black and white wo)men, and black womentend to drink less. The role of illicit drugs isnotoriously difficult to assess both due to thereluctance of individuals to report drug use andthe uncertain content of "street- drugs. A well-established correlate of poverty is the lack ofemployment. Thus, such health-related habitswould appear, at first blush, not necessarily tobe related to) racial inequities in birthweight.
It would seem, however, that the questionsought to be more sophisticated than that. First,the lack of paid employment does not rule outstressful labor, given the lack of financialresources to invest in labor-saving houselmldappliances. More importantly, such factors mayconfer a different level of risk for womenwhose health may already be connpromnised bylong-term exposure to health risks associatedwith disadvantaged environments. In a recentstudy of the mothers of young infants in centralHarlem. H) percent had been hospitalized inthe year since delivery; 12 percent rated theirhealth as fair or poor; and 1.4 peecent set ved inthe distressed range on a mental health scale.Nloreover, soma.. ( f the risk factors fo)r poorpregnancy ciutcome also correlated with poormaternal health subsequent to pregnancy, sug-gesting an interactive effect.
More current infonnatitm is needed on thehealth pro)blems and behaviors of women ofchildbearing age as they might affect their capac-ity for reproduction. Perhaps our very low mater-nal mortality rates have provided a sense ofsecurity which may require further re-examina-tion. although black .white disparities in thishealth status indicator may have caused somie
228 Trends in Rates (y. blet. Birthweight In the I 'tilled States
concern.' Ve do collect 11ealth clata on womenof childbearing age through the Natkmal I lealthInterview Survey (our Harlem data parallelnational data on black women), the NationalNatality Survey, and birth certificate analyses, Itis difficult to establish, however, how the subsetOf %%Innen who bear chiklren may differ from thelarger group of women of childbearing age,since at any one time only a minority of women
are experiencing pregnancy and childbirth.Seeking prenatal care and changing health
habits to improve pregnancy outcome require acertain amount of anticipation or planning. Thegroups nuist at risk, however, are the ones leastlikely to have intended to he pregnant.' Thesefindings suggest that, in addition to prenatalcare. low-income women may have difficulty inachieving access to family planning services aswell. It is small wonder that such access may hedifficult to sustain given the fact that reproduc-tive care for low-income women may he spread
across several types of clinics: family planningclinics, gynecology clinics, clinics for sexuallytransmitted diseases, abortion clinics, and obstet-ric clinics (many with legally dictated separa-tions of facility and stall).-
Nh)re( wer. overcoming harriers to care andmodifying unheahhful behaviors requires motiva-tion. energy, and support.' As the earlier data onmaternal mental health suggest. other aspects ofdisadvantaged envir(mments also adversely affectwomen in this sphere. Again in this same cohortof young mothers, envir(mmental stress as mea-sured lw stressful life events is high, hut socialsupportas measured by the ability to identifyan individual by name and relationship to pro-vide help in six common situationsis not.These factors relate to maternal health, and sonny
Mark, McO)rnik-k
irriuts
studies have implicated such combinations in the'risk of adverse pregnancy outcome."
St 'N1MARN' AND St IGGES11ONS
In summary, the km birthweight rate inthe United States remains high, with only slowdecreases and a predominance of prematuwbirths. These high rates reflect the persistenceof socioeconomic disadvantage. especiallyanumg blacks. The factors underlying thesetrends are complex, and this complexity sug-gests that change will not come easily.
In view of this complexity and lack ofready explanation for the persistence of lowbinhweight, our own experiences and those ofothers suggest some questicms and appr()acheswhich, while not exhaustive nor even perhapsoriginal, may be useful in the next two days.The first question relates to our understandingof "risk.- The majority of low-inc(mie women, orblack women, or poorly educated women. orvery young women have normal hirthweight( NW ) infants. We tend to treat woinen withthe.se characteristics as if they were homoge-nec us. and yet each of these labels masks ccm-siderable heterogeneity. Perhaps we should beconsidering more -micro- studies on the risk fac-tors within communities and trends in outcomesat a more local level with more focused data tounderstand the nature of this heter()geneitv.
Secondly, even with established risk fac-tors, we need to be more specific about themechanisms by which such factors alter riskand the potential modifiers of both the effect ofthe risk factor and interventkms to ameliorateits effect. We are recurrently taken aback by the
C)
Advances in the Provntion (y. Lou' Iiinbueight
relatively small contribution of prenatal care tochanges in birthweight. vet the relevance of theindividual components of that package of ser-vices which we call prenatal care to the currentprciblems affecting pregnancy ou;come requirefurther examination. Furthermore, examples ofsuccessful programs are rarely described in suf-ficient detail to assess the generalizability of theinterventkm. Likewise, the modifiers whichmay contribute to the persistence of a well-rec-ognized risk like cigareue smoking are not welldescribed. For example. in our study, envin ni-
mental stress and lack of micial support did notcontrilnite directly to birthweight differences.but were clearly associated with smokingbehavkw in pregnancy, Additionally. we needbetter information on how sociodelllOgraphicand behavioral risk factors translate into biolog-ical pr()cesses affecting fetal growth.
Finally. we may need to pursue some morecomplex intervention models. A comparableproblem is the mental retardation seen in chil-dren who come from disadvantaged back-grounds. There :Ire now several well-document-ed randomized trials of successful interventicms.and their success provides support for expandingnational programs for early childhood education.These experiences, however. rely on well-devel-oped and explored ctmceptuahzations of earlychildhood development and specific curriculumsaimed at the identified deficiencies of sufficientintensity to achieve the desired results. It is
hoped that the presentations over the next fewdays will raise us all to this more sophisticatedlevel of approach tO this complex problem,
REFERENCES
I. Wcgman. E. .Nnnual stitninArystatistics: 1956. Poliatrics 80,
2. Hogue, It.. Buehler, .1. W., Strauss. 1.. T.. :indSmith. J. C. (19S-1. Overview tit the \ational InfantMortality stir% cillanee priwet: Deslgn methods Andresults. Public Health 102. 1 20- 1 .38.
SILipirci, S., NIct'airmick. tl. (... Suffield. B. 1 I.,
Krischcr. .1. P.. .,ind Noss. 1). (195( I) Relevance ofcorrelates of infant deaths jor significant nImBidity atme year )1 age. .1 moleau ./(qtrnat crfObstdricx mid
0:17recobigr 13o, 303-3-3.
f. . (.Ongrl'sr. t It'dint)it )gy AsS:sstill`nt.I I t)8-). Avoaata1 alleastne care lote hallairtghtatlaats (.4s1s atul clfivtavaess ( Health iivbilalagrcase Study :;,+' Publication No. OTI-11CS-35.Washington, I)C: 1.,s. Congress. ()Mei: ot.Tt.'d mok igy Asst.,ssmem,
Gold, H. B.. Kenney. A.. and Singh. S. t 198' I.Bie.:ed cvcuts and the lu ;mon Fina ;icingmaternity caw in the maws. VA\ York: Alan
inStialte.
Suffield. li., Shapiro. S.. Ntet:orinkk, NI. and1 irnss, 1). t 1982 I. Mortality and morhildity withIntratiterim. growth retanlation, turaal poillatricsto!, trs-9s3.
Williams, H. I... Creas. H. K.. cunningharn. G C.,S. F... I'. D., et al. (1952). Fetal
.v.rt)w II) ,ind 1.11111ity In)bstetrics mai O'racc-ology -;(), ()2., +-(02.
5. k..raincr, NI. S. (1)5-) Intrauterine gimili and ges-utional duration deiermin.ims Pciliatrics so.;02-4;11.
t) \aticin.11 Cuntcr Statistics I980). I le,alth'nned Shifts ?9,SY) 1)1111S Puhlicatii in \ is
1232. Wasl»ngton. DC: Government Printing Office.
10. Kcssel s s I. Bet-Click's. II, N5... and \ugent.I. P. (19s ii. The changing t hA% hirth-
cight in the I niick1 I. ./Hurilell (?,1the .1/nem an Medical Assoc uau ta -5 1 . 19"M-1952.
11. Sarpcntield. W. 51.,Hogue. ( J. It. Strauss. 1.. T.. and Smith. .1. C.lt)S-). Dilterenti..s in nctinata1 And pystneiinatal
111(0.1111v hy binh m..cight and gestational agc.Publn. loath Rep orts 1u2. 182-192
24
Trends in Rates (!j* tott. Birthweigbt in the I lifted States
12. Klebanciff. M. A.. and Yip. R. i198"). Influence ofmaternal birth weight on rate of fetal gRiwth andduration of gest a Hi Ui. parrna/ (4. Pediatri(s 111,28--292.
13, Klebantiff . N1 .... . . tiratibard. B. L. Kessel. S. S.. andBerendes. 11. \\.. (1984), LOW birth weight acrossgenerations. finirnal af the American MedicalAssociation 252. 27.
1.1. Wilcox. A. .1.. and Russell. I. . 41983). Perinatalmortahty: Stanclardizing for birthweight is biased.Americali.journal (!fhpulemifdtigy 118.85"--64.
15. Insbtute of N1edicine. Committ to study thePreventkin of Low Birthweight. 1f)85). Proem/lig/Awe Birihweighi, Washington, DC: NationalAcademy Press,
16. Kleinman. .1. C.. and Kessel, S. S. (198"). RACI:11 (fir
fcrinces In lcm ltili \\ eight: Trends ;ind risk fac-tors. .Veu. EngIaad j(wrnal 01. MecheiMe .
17. K(nelchuck. Schwan,. J. H.. .nelerka. M. T.. antiFinison. K. s (198.4), VIC parridpation and preg-nancy outcomes: Massachusetts statewide evaluationprotect. American fiat rued Pubhc I.
10S6-1092
18. Mamelle. N.. Luman B.. and Laiar. P. t 19s e I.
Prematurity .ind (it cupational tUi ity during preg-nancy. American journal 01. Fptdomuilf,,10. 119.309-322.
19. Prager. K.. Manlin. 11.. spieglet. D.. Van \ALL P.. andPlacek, P (198+ ). Smoking and drinking behaviorsbefore and during pregnancy of married Inutherslive-born infants and stillborn infants. Public
Mika-is 99. 11"-128.
20. McCormick. NI. C.. Brooks-(unn, .1.. Shorter, T..Holmes. J. It, Wallace. C. Y.. and fleapits, M. C.(198"). Ilealth in the Year following delivery amonglow -Meow wi 'men. Pediatnc Research 21.2.85A.
21. Sachs, B. P. 13n iwn. D. A.. Driscoll. S G.. Schulman,F., Acker, D.. Ransil. B. et al. (198-1. Maternal
int irtalit in Nlassachusetts: Trends and pies ention..\eir kn,Q1and.harrual ,?/.1hAlic-ine 310. 60--(-2.
Aries, N. (198). Fragmenution and reproductisefreedom: Federally subsith/ed famil planning set-V iCes. 190()-- 1980. American Journal vf Pub/N.-111.'0h-, 1393-1 395.
7Yends
23. Istvan, I. C 198(, ). Stress. anxiety and birth out-comes: A critical review. of tile CV denee.
BUlleliP/ 100. 331-348,
24. Brooks-Ounn. I.. NkCormk.k. M. C.. and Ileagarty,I . c. 19881. Prventing infant mortality and mor-
bidity: 1)evelopmental perspectives. Americanjuunuif cg. Urthypsvcbiatti. S. 2$8-290,
Marie McCormick 1 I
25
Erni ution ((the Preterm Birth Ratein Fiance
(FRAR1) BREAM', M.D.
INTRODt (711ON
During the 1970s in France, reduction in thepreterm birth rate was considered a majorobjective in perinatal medicine. This objec-tive was included in a perinatal programimplemented between 1970 and 1975.4 Thisprogram included incentives to increase prena-tal care, outpatient clinics for high-risk women,and educational programs. It was I( )l lowed in1975 by a series of measures, including regula-tions for the working conditions of pregnantwomen and implementation of a home visitingsystem. Since 1981. no new specific programsor actions have been devekved.
The aim of this paper is to trace the evolu-tion of the preterm birth rate in France. Thepaper will be divided into two parts. The firstpart corresponds to the evolution of the
Advances in tile Prelention (V. Lou' Birthweight
preterm birth rate between 197 2 and 1981 .
based on national data, and the second corre-sponds to the evolution between 1984 and1986, based on hospital data.
Ex01.1.110N OF '11IF PREITRM BIRT11 RATE
BEWEEN 1972 AND 1981
Material ai id ined.xxlsThe data h4.re presented are derived from
three national surveys conducted in France in1972, 1976, and 1981 on representative samplesof birth.' Each sample was obtained br a two-stage (maternity unit, and deliveries within tileunit) sampling procedure (see tabk. 2.1). Forevery delivery included in the surx.ey, a ques-tionnaire was completed. The representative-ness of the data was assessed by comparisonwith data on all births. The main objective ofthese surveys was to evaluate, at the nationallevel, the results of the perinatal program.
Reszals
Table 2.2 shows that. between 19-2 and1981, the preterm birth rate decreased from 8.2percent to 5.6 percent. It should be noted thatthis decrease Was observed for births (Kcurringbefore 34 weeks gestation. as well as for birthsoccurring between 3-1 and 36 weeks' gestation.
This reduction in the preterm birth rateWaS acc(mipanied by a reductk)n in the rate Oflow birthweight births between 1984 and 1986(see table 2.31. This reductkm was observed I( n'very low birthweights as well.
During this same period, prenatal care
Ii
changed dramatically in France (see tableboth quantitatively and qualitatively. For exam-ple. the percentage of women with 7 or moreprenatal visits increased from 22 percent to 5.5percent. The temporal relationship between themodification of prenatal care and the decreasein preterm births is not su. tH....c.ent to prove acausal relationship. Other factors may have hadan impact on the rate of preterm birth. Amongthem, the denuTraphic factors are the nu)stimportant. Table 2.5 shows that women whodelivered in 1981 were at lower risk forpreterm hirth than women who delivered in1972. There were fewer women younger than20 years of age, fewer women with 3 or moreprevious pregnancies, and fewer women with ash(wt interval since the previous birth.
To take into account the evolution of thesefactors, standardized rates of preterm birthwere computed (see table 2.(). The 1972 popu-latkm was used as the reference populatkm.The comparison between crude and standard-ized rates shows that changes in denu)graphicfactors explained only (me-third of the decreasein the number of preterm births.
OnnitlentsIn adchtion to the changes in demographic
factt )rs. there have been other changes. Not allof the changes led to a decreased risk inpreterm birth. however: some of the changes.in fact. lud the opposite result. Therefore .
changes in maternal characteristics. as evaluat-ed through the data collected. do not appearsufficient to explain the decrease in pretermbirth. It is likely that the modificatkm in prena-tal care (including nonmedical care) had an
0"iv
Erellahni (y. tbe Preterin Birth Rate in Emuice
impact on the overall rate of preterm birth.Since many interventions have been imple-
mented at the same time. ranging fromincreased use of betamimetics to regulationsconcerning working conditions, it is very diffi-cult to evaluate the efficacy of any one particu-lar intervention.
It is now accepted' that some of the pro-posed interventitms have been overused ormisused. flowever. in agreement with what isknown about risk factors of preterm birth.'which are multiple and cannot explain all ofthe cases of preterm birth. it is believed that areduction in the ',menu birth rate could notbe obtained through a single intervention.Instead, a comprehensive program is neededwhich includes several types of interventions.among which obstetricians, midwives, andsocial workers could choose one (or several)specifically adapted to each v(nnan accordingto her living and working c(mditions as well asto the symptoms she presents. Since theknown risk factors explain only part of theoverall rate of prtierm birth.- a pn)gramdecrease preterm birth sh(Aild not be limited tohigh-risk women. but shoiad be targeted to allwomen in the general population.
Evou "no \ orTHE PIUTIIRNI HIRTI i RM'E SINCE 1983
In recent \Val's. it seems that the views ofFrench obstetricians- concerning prevention ofpreterm birth have changed. This change seemslinked to two main causes: First, concernsabout the safety of very conuncmly used drugs.such as betamimetics: and. sect )nd. progress in
''rends
neonatology. Another factor which may haveinfluenced French obstetricians is the trend, forfetal growth-retarded letuse.s, toward anincrease in premature termination of pregnancyto prevent long-term handicap. Those factorshave raised some questions concerning therecent trend in the preterm birth rate in France.In order to collect the necessary inf(wmation, asurvey was conducted aincmg several maternityunits. The results ore presented here.
Material cuul methodsTo obtain information on the recent evolu-
tion of the preterm birth rate, as well as itsdeterminants, a questknmaire was sent to 30maternity units known to be users of the samet \ pe of computerized record. These unitsbelong to an association called Association desrtilisateurs d'1111 Dossier Informatise enPerinatoh)gie. Obstetrique et Gyttecologh.'. Thepurpose of the questionnaire was to collectdata for the three more recent Years (198-4,1985, and 198( ) on the pretenn birth rate:birthweight and mortality rates; social, demo-graphic. and medical characteristics of the pop-ulation: and policy adopted for the preventicmof preterm birth. Among the 30 unitsapproached. only 9 were able t() provide com-plete data. They are iocated in different parts ofFrance (see figure 2.1). and 2W)00 women peryeor deliver in these units.
ResitIts
In the inaternity units studied (see table2.7). the preterin birth has increased from (0percent to percent. According to impor-
Gourd lin31rI 15
0 V
Advances in the Prevention ql Lou Birthweight
tance of prematurity (< or > 3-1 weeks), or t oinduction of labor (artificial or spontaneous),an increase was observed for spontaneouspreterm delivery no matter what the gestation-al age, whereas an increase in induced pretermdelivery was observed only for very low gesta-tional age (< 3.4 weeks). Table 2.7 shows thatinure than one-quarter of the increase inpreterm births was directl- related to anincwase in preterm induction for terminationof pregnancy.
To screen the possible factors which mighthave led to an increase in spontaneous pretermbirth, the evolution of sonie risk indicators(e.g., frequency of women with previouspreterm birth, maternal age under 20 years,unemployment, use of betamimetics, and firstprenatal visit at the unit during the firsttrimester) was examined during this period.Among the five indicators studied, twothepercentage of w(mien receiving I>etainimeticsand the percentage of women coming to unitduring the first trimestervaried markedly (seetable 2.8). Both frequencies decreased duringthe period.
Cbmtneills
Even if the increase in preterm birthsobserved in some hospitals in France cannot beconsidered as representative of the actual trendat the national level, the dat:i collected showedthat an increase in the pretenn birth rate hasbeen observed at the same time as modifica-tions in preventive attitudes have beenobserved. Modifications in obstetricians' ;1.10-tudes have been observed (as demonstrated inthe increase in preterm induction and restric-
dons in the use of betaminietics), as well asmodificatkms in women's attitudes as reflectedby the percentage of women starting their pre-natal care, after the first trimester, at the outpa-tient clinics of the units. This change may notbe due only to changes in women's attitudes,however, but also to changes in general practi-tkmers' attitudes, who could have delayed thereferral to the maternity unit, or to socioeco-nomical problems, which could have made itmore difficult to access the maternity unitsunder study.
The modificatkm of the obstetricians' atti-tudes seems to be recent.' as does the upwardtrend in the preterm birth rate. Several of thematernity units which have experienced arecent increase in the preterm birth rate haddocumented a decrease during the 1970s.
The increase in preterm birth has not beenobserved only in French hospitals. Table 2.9shows that it has been observed in Sweden,Norway, and Iceland as well:"
CoNct.t siox
From the data presented here, it can prc)h-ably be ccmcluded that a portkm of the pretermbirths can be prevented. This statement isbased on the decrease observed in France dur-ing the 19M)s and the recent increase in somehospitals. This variation in trend in "spomta-neous- preterm birth suggests the possibleeffect of scmie environmental factors. Thesefactors could be social, demographic. or medi-cal, since the observed change in the pretermbirth rate corresponds to changes in preventivepolicies (e.g., increase in medical intervention
2 9
/6 Evolution (01.7e Preternt Birth Rate France
during the first period, and decrease duringsubsequent periods) as well as changes insocial factors. The type of data presented heredoes not allow anv conclusions to be drawnconcerning the factors which are responsiblefor the decrease or the increase in pretermbirth. Such conclusions can only be drawnfrom experimental surveys. The results of therandomized controlled trials presented at thissymposium, as well 'as presented at theEvian meeting," do not lead to clear conclu-sions concerning which interventions canreduce preterm birth and which interventionscannot. These conflicting and disappointingresults might be due to the fact that preventionof preterm births can only be obtained throughmultiple interventions, each of them aloneresulting in too few benefits to be observed inan experimental study.
Another conclusion which can be drawnfrom the hospital data is that prevention ofpreterm birth cannot be considered as anobjective per se, but as a means to reducelong-tenn handicaps. in some circumstances,obstetricians will induce preterm terminatim ofpregnancy because of fetal distress, and anincrease in preterm birth rates might lead tobetter long-term results. Therefore, the overallpreterm birth rate can no longer be considereda good indicator of perinatal results. A distinc-tion must be made between spontaneous andinduced preterm deliveries, and perinatal pro-grams should be evaluated based on long-termoutcome or on indicators which are highly cor-related with long-term outcome. Such indica-tors remain to be defined.
7*rends
REFERENCES
I. Bouyer, J Dreyfus. J.. Guegen, S.. Lazar. P.. andPapiernik. E. (19)8). La prt;maturitC'. Paris:INSERM: EnquCie Perinatale 1 laguenau.
2. Breart. Goujard, J., Blonde!, B.. Maillard. F.,Chavigny, C., Sureau. C.. and Rumeau-Rouquene, c,( 1981 ). A ct nnpa rist )1'1 of two policies of antenatalsupervision for the prevention of prematurity.linernationallournaltf EpidernicIlogv 2.+1-2.41.
3. Papiernik. E. (1969/. Coefficient Lk. risqued'aconichement preimiture. Presse Medicate 77(21),
.
Rumeau-Rouquent... C.. and Blondel. B. (198=0. TheFrench perinatal program, In: I. Vallin and A. D.
)pez Eds. ). flealtbixdicy, social Ltxdic.y and mortal-ity provects (pp. 299-3311. Liege; Ordina.
S. Rumeau-Rouquette. (.. du Niazauhrun. C.. andRaharison. (Eds.). (1984). Aaitty en France: Dixans di:volution. Paris: INSERM.
6. Papiernik. E.. Wean. G.. and Spiro, N. (1986).Prevention tie la naissance prOmaturc;e. INSERNI,
138.
Sureau. C.. Blt.)t. P. IL. Cairo). Cavaille. F.. andGermain. G. (1986). Control and management ofparturition. 1NSERM John Lihhey.
8. Kramer, M. S. 41987'1, Determinants of low birth-weight: Nlethodological assessment and meta-analv-sis. Bulletin ty. the World Health Organization663-7'37.
9. Blondel. B.. Ringa, V.. and Breart, C. (1989). Theuse of ultrasound evaminations. intrapartum fetalheart rate nu)nitoring and betamimetics drugs inFrance. British Journal of Obstetrics antiGynae(Mhigy 90.
(1957). Births in ihe Nordic countries: Registration(ye the outcome q1" pregnancy 1979- /91S'3. Reykjavik:Nomesko Publieatkms.
Gerard Bread I 7
3 0
Mends
StatisiicalEvolution of Preterm Birth
in France
Table 2.1
Design of the National Surveys
1972 1976 1981
Sampling fraction 0.01.37 0.0068 0.0068
Number of units 637 420 .390
Number of deliveries 11,254 4,685 5,508
Table 2.2Evolution of Gestational Age (National Data)
1972 1976Percentage Percentage
Number of Weeks
1981
Percentage
< 34 2.4 1.7 1.1
34-36 5.8 5.1 4.4
37-39 .37.0 p< 0.01 34.9 pc 0.01 17.9
40-42 50.8 54.0 5.3.1
43+ 4.0 4.3 3.4
<. :36 8.2 p< 0.01 6.8 p < 0.05 5.6
Table 2.3Evolution of Birthweight (National Data)
1972PeR entage
1976 1981
Percentage Percentage
1500 g 0.8 0.7 0.4
1500-1999 g 1.2 0.9 1.0
2000-2499 g 4.2 4,9 3.8
2500-2999 g 19.1 NS 17.9 p< 0.01 18.0
3000-3499 g 41.8 42.3 41.3
3500-3999 g 25.5 26.4 )7. 7
4000 g + 7,4 6.9 8.0
< 2500 g 6.2 NS 6.5 p< 0.01 r
Table 2.4Evolution of Prenatal Care (National Data)
1972 1976 1981
Percentage Percentage Percentage
Number of prenatal visits< 4 15.3 10.6 3.9
4 35.4 29.1 16.5
5-6 27.1 p< 0.01 26.4 p< 0.01 24.7+ 22. 3.3.9 54.9
iospitalization during pregnancy7.3 p< 0.01 13.0 p< 0.01 15.6
Betamimetics8.9 pc 0.01 14.7
Care by general practitioner only20.8 p< 0.01 8.8
nc't ailable
Table 2.5Changes in Demographic Factors
(National Data)
Maternal age< 20 years> 40 years
1972 1976 1981
Percentage Percentage Percentage
9.9
2.48.5 6.0 p< 0.0011.1 0.9
Number of previous pregnanc ies3 + 18.3 14.1
Previous birth< 17 months
15.4 p< 0.001
21.6 15.4 10.2 p < 0.001
Gerard [Wad /9
31
Advances in the Prevention of Low Birthweight
PoitouCharentes
20
3 'Statistical Findings: Emlution of Pretenn Blab in France
Table 2.6Evolution of preterm birth rate
(Crude and Standardized*Rate, National Data)
Crude rate
1972 1976 1981
Percentage Percentage Percentage
8.2 6.8 5.6
Standardized rate 8.2 NS 7.8 p < 0.05 6.7
StilnOaultration in) age. flUlTlik'r of pal I 11.1 PTI;nd interv.ilbeat, een
Table 2.7Evolution of Preterm Birth (Hospital Data)
1
Year*
2 3
< 34 weeks 2.6 2.9 3.3
spontaneous 1.5 1.6 1.8
induced 1.1 1.3 1.5
35.-36 weeks 4.0 4.4 4.4
spontaneous 2.3 2.5 2.7
induced 1 .7 1.9 1.7
* Years 1, 2 and 3 generally represent 1984, 1985, and1986.
Table 2.8
Evolution of Risk Indicators (Hospital Data)
Year*
1 2
Per ,ntage Percentage Percentage
Betamirnetics Use 21.8 20.5 17.5
1st visit during1st trinwster 50.3 45.3 44..
nyncis
Table 2.9Preterm Birth Rate (< 36 Weeks) in
Nordic Countries
1979 1980 1981 1982 1983
Denmark 4.9 5.0 4.9 4.8 4.8Finland 5.2
Iceland 2.6 2.7 3.0 3.1 3.4
Norway 4.9 4.9 5.1 5.0 r
Sweden 4.5 3.6 5.8 5.9 6.1
Source: l'apk.rnik, E., 8re.,art. G., slnd Spita, N. (19861. Prevention de lanaissance prentaturee. INSERM, 138.
(erani Bri.;art 3 t)21
The Etiology and Pretention ofLow Birthuvight:
iirent Kilowledge and Prioritiafor Future Rovarch
MR :11AEI. S. KRAMER, M.D.
NTRODI. ICTION
In l)oth developing and developed countries,low birthweight (LBW), that is, birthweight lessthan 2500 g, is a major risk factor for neonatalmortality and fin subsequent morbidity andimpaired functkmal NI-tin-mance. The designof interventions to prevent LBW depends on asufficient understanding of its etiokTic deter-minants. Although it is widely acknowledgedthat causality of LI3W is multifactorial, therehave been considerable a mfusion tnCI conta)--versy about which factors have independentcausal effects, as well as the quantitativeimportance of those effects. One of the mAjorreasons for this confusion and controversy hasbeen a failure to distingthsh LBW caused by a
Athwuces in the Prevention q' Lou' Birthweight
short duration of gestation (i.e., prematuredelivery) from LI3W caused by intrauterinegrowt h retardation ( It VTR ).
Prematurity is defined as a gestational ageless than 37 weeks. IUGH. which is also referredto as small for gestational age (SGA) or small fordates (SFD), is usually defined as birthweightless than the 10th percentile for gestational agefor a "standard- reference population. (It is obvi-ous from these definitions that babies can bepremature or growth retarded without necessari-ly weighing less than 2500 g. Thus, while it is
true that LBW babies are either premature orgrowth retarded or both, the converse is notnecessa r..y 1.1e case, particularly in well-nour-ished populations from devel()ped countries.)
The distinction between prematurity andIt TGR is of crucial importance because they dif-fer considerably not only in etiology, hut alsoin terms of their prognostic significance andrelative incidence in different settings.
For example, premature infants are atgreater risk for developing hyaline membranedisease, apnea, intracranial hemorrhage, sepsis,retrolental fibroplasia, and other conditionsrelating to physiologic immaturity. Several ofthese conditions are responsible for the fargreater neonatal mortality in premature babies.
On the other hand, It TGR infants are morelikely to I.rave deficits in growth, and at leastJme of these deficits appear to be permanent.
As to relative incidence, Villar and Iklizan haveanalyzed data from 25 developing and 1 I
developed regions.' In devel()ping countries.nu)st LBW births ippear to he due to 11.`( R.whereas in developed countries (especiallythose with the k)west LBW rate), in()st are dueto prematurity. Thus, the focus of preventive
efforts, both in terms of clinical and publichealth policy and future research priorities, willdiffer in different settings depending on the rel-ative incidence of prematurity and It TGR.
Reported discrepancies concerning the eti-ology of LBW may have explanations otherthan the IUGR -prematurity distinction. Primaryamong these is the matter of association versuscausation; that is, "markers- of LBW versus truecausal determinants.
The issue here is not merely the theoreticalconcern t'or "scientific puritv.- Rather. the asso-ciation/causation distinction is of considerablepractical import for improving public health,since an intervention will succeed in reducingLBW only if it affects a true causal factor. Manyof the potential determinants are highly associ-ated with one another, and adequate controlfor confounding is thus required to identify andquantify their causal effects. Two possible sta-tistical explanations for the reported discrepan-des concern the portion of the birthweight orgestational age distribution (e.g., middle v.l)wer tail) on which a determinant acts andinadequate statistical power in studies withsmall sample sizes.
In an attempt t() help clarify these issuesand synthesize the recent literature, I recentlyundertook a methodologic review and meta-analysis of the English and French literaturepublished between vro and 1984.'' Althoughseveral issues have been further clarified overthe last several years, I believe the results ofthat review still provide a reasonable synthesisof our current state of knowledge about the eti-ologic determinants of prematurity and I I 'GR.The following section summarizes the methodsand results of that review.
3626 The Etiologr (Ind Prelottion (y. Lou. Binbuvight
CURRENT KNOWLMGE
Summary qf 1970-84 Review
The 1970-84 review was restricted to sin-gleton pregnancies occurring in women living atsea level without chronic illness, Factors Ofextremely low prevalence (e.g.. maternal rubellainfection or uterine malformation) were not con-sidered. because even though such factors willbe of great importance to the individual womenin whom they occur. they are not responsiblefor a significant portion of IUGR and prematurityon a population-wide basis. Also excluded fromconsideration were medical complications ofpregnancy, such as pregnancy-induced hyper-tension, abruptio placentae. placenta praevia.and premature rupture of the membranes. In myview. such conditions should he considered asintermediate outcomes of pregnancy. Theirinclusion in a multifactorial model of causaticinwill inevitably lead to an underestimate of theeffect of factors whose impact on intrauterinegrowth or gestational duration may operatethrough one of the conditions.
After these restrictions and exclusions, '13fact( rs (or groups of factors) were left for assess-ment. These are listed in table 3.1. The literaturesearch began by examining the subject catalogueof the World !leak h Organization library forbooks and mom)graphs published since 1 (r0. A
similar search was carried out for review articleslisted in Index .1/edicus over the same time peri-od, These were supplemented by a MEDLINEcomputer search fig the years 1982-4;4. Finally. a"snowball- procedure was used, by which eacharticle or book chapter located was examined forfurther references published since 1970, followedby the references cited in those secondary
Determinants
reports. and so on. Each reference idemified bythe search was examined for data concerning 1or more of the '13 factors.
Methodokigic standards were established apriori for studies of each candidate factor. Theseincluded such general aspects of research de,,ignas definition of the target population and studysample, description of study participation andfollow-up rates, clear demonstration of theappropriate temporal sequence between the fac-tor and outcome, and the use of an experimen-tal research design (where feasible and ethical).The remaining standards pertained to the poten-tially confounding variables requiring control fornonexperimental studies and differed accordingto the factor under assessment.
Studies satisfactorily meeting (SM) or par-tially meeting (PM) the standards were selectedfor further analysis. SM studies fulfilled themajority of the predetermined criteria. PM stud-ies gave some attention to rigorous design andanalysis, but fulfilled less than half the criteria.For several of the factors, certain standardswere judged to he of overriding importance inassigning an SM or PM rating. Based on thestudies selected for further analysis, each factorwas issessed for the existence of an indepen-dent causal effect on birthweight, gestati(malage. prematurity, and 11'GR. If an independentcausal effect was judged to be denuinstrated onthe basis of the combined evidence of theselected studies, and sampling variatkm couldbe excluded as an explanation (Le_ p< MS), theeffect size was extracted from each study, Forbirthweight or gestational age. this may havetaken the form of the difference in means froma rand()mized trial (g a matched cohort study,an adjusted difference derived from an analysis
Micbael S. Kramer 27
3 7
Advances in tbe Prevention of Low Birthuvigbt
of covariance, or a regression coefficient from amultiple linear regression analysis. For prematu-rity and ItTGR, the corresponding effet sizeextracted was the relative risk or odds ratioadjusted for potential confounders by usingmatching. the Mantel-Haenszel procedure, ormultiple logistic regression analysis.
The extracted effect sizes were thenweighted by the study-speci sample sizes toyield an overall estimate for each factor. Finally,using available data on the prevalence of eachdemonstrated causal factor in different popula-tion groups, etiologic fractions were calculatedfor prematurity and It1GR. The etiologic frac-tion (EV), which is also known as the popula-tion attributable risk or attributable risk percent,is defined as the proportion of HIGH or prema-turity in a populatkni that is attributable to agiven factor. It is calculated as follows:
EF = RR-l)
P(RR-I) +
where P is the prevalence of the factor in thepopulation and RR is its corresponding relativerisk or odds ratio.
The literature search using the ccmibinedsnowball procedure identified a total of 921publications. Of these, 895 or 97.2 percent,were successfully located and reviewed.Although a majority of the reports originatedfrom developed countries in North America andwestern Europe, a large number also camefrom developing countries in Latin America,India, Africa, and southeast Asia. The totalnumber of factor assessments carried out was1,566. Even though some of the reports did notcontain original data bearing on any of the fac-
tors. this total far exceeds 895, since manyreports provided data on several factors.
Factors with well-established direct or indi-rect (i.e., acting via one or more direct-actingfactors) effects on intrauterine growth are listedin table 3.2. Those with effects on gestationalduration are contained in table 3.3. In order toillustrate the quantitative importance of thewell-established direct determinants, I haveconstructed pie diagrams in which the size ofthe pie slices is roughly proportional to the eti-ologic fraction for each of the indicated factors.Figure 3.1 is the pie diagram for It1GR in a typi-cal rural developing country in which malaria ismoderately endemic but pregnant women donot smoke. Nonwhite racial origin is probablyresponsible fin a large proportion of IUGR indeveloping countries with high prevalences ofblack or Indian racial origins. The other majorfactors are poor gestational nutrition. lowprepregnancy weight, short maternal stature,and malaria. It is important to emphasize that.of the five leading facfiws, three may be mcKlifi-able in the short term: Gestational nutrition,prepregnancy weight, and malaria.
Figure 3.2 shows the pie diagram for adeveloped country in which 40 percent of thew(mien smoke during pregnancy. In this setting.the most important single factor by far iscigarette smoking. This is followed by poor ges-tatknial nutrition and low prepregnanc) weight.The three leading factors are all potentiallymodifiable, once again, with obvious implica-tions for public health intervention. Althoughthe overall size of the pie is smaller than in thedeveloping country setting (i.e., the II1GR rate islower), a larger proporticm of existing fetalgrowth retardation may be preventable.
3°28 The Etiokr and Prevention qt. Lore Birthweight
A pie diagram for the well-establisheddirect determinants of prematurity in the devel-oped country setting is shown in figure 3.3. Ofthe five factors with well-established directcausal effects, cigarette smoking and lowprepregnancy weight are modifiable butaccount for a relatively small proportion of pre-mature births. The major message from figure3,3 is that the majority of prematurity occurringin the population remains unexplained. In part.this large gap in our knowledge reflects the farless intense previous effon in studying gesta-titmal duration as compared to intrauterinegrowth. This has been especially true in devel-oping countries.
Recent Developments.
Since this assessment was carried out, anumber of studies that bear on prevention ofprematurity have been published in developedcountry settings. Although I have undertaken noformal assessment of the literature a ppea ringsince 198-i. I would like to highlight three areasin which research has shown promise for pre-venting prematuritv: (1) Reducticm of maternalwork and physical activity during pregnancy: (2)identification and close surveillance of womenat high risk f(mr premature delivery: and (3) treat-ment of genital tract infection,/colonizatkm.
The available evidence permits no defini-tive conclusions as to whether work and physi-cal activity during pregnancy are beneficial,harmful. or irrelevant for gestat k mal duration.Recent evidence does s ggest that prolongedstrenuous or stressful v. ork activities, aerobicendurance-type exercise continued into thethird trimester, and upright posture mayincrease the risk of prematurity, and that mod-
Michael S. Kramer
Determinants
crate sport and exercise may reduce it (at leastamong well-nourished women in developedcountries),' " but further studies are required. ASubcommittee on Dietary Intake and NutrientSupplements During Pregnancy has been con-vened by the Food and Nutrition Board,National Academy of Sciences. to synthesizethe information available in this area. This com-mittee slumid be publishing its report withinthe next several months. [Editor's note: Thispublication was released in 1990. It is entitledNutrition During Noma/icy. and is availablefrom the National Academy of Sciences]
Another area of intense recent researchactivity concerns identification and closesurveillance of women at high risk for prema-ture delivery. The assessment of high risk isbased on multifetal gestation. uterine malforma-tion, inc( )mpetent cervix. or a history of previ-ous premature birth or second trimesterabortion. Surveillance has used such m(xlalitiesas frequent pelvic examinations, teaching moth-ers to recognize early signs of uterine contrac-tions. and, most recently. ambulatorytocodymunometry (i.e.. 11(mie numitoring ofuterine contractions using a portable recordingdevice). The evidence from intervention studiesinvolving these modalities is inconclusive,' 'sbut some of the results have been quite impres-sive and certainly are sufficient to justify furtherresearch. It should be emphasized. however.that even if effective methods can be devel-oped for preventing prematurity in women athigh risk, the overall impact on a populaticm-wide basis will depend on the predictive valueof the risk assessment and on the proportion ofall premature births that occur in women classi-fied as at high risk.'"
3a
Advances in tlw Prevention (y. Low Birthweight
Finally, sufficient evidence exists concern-ing the possible etiokTic role of bacterial 'agi-nosis and genital tract infection or cokmizationwith such organisms as Ureaplasma ure-alyticum. akunydia itathomatis, GardnervIlavaginalls, species of 13actervides. and otheranaerobes to justify randomized antibiotic trialsin women colonized with these organisms inthe second and early third trimesters.'"
Several such trials are already in progressin the United States. including a large multicen-ter study supported by NICHD. and the resultsare eagerly awaited. Recent evidence also indi-cates that genital tract infection:colonization inwomen with preterm labor is associated withfailure of conventional tocolytic therapy."'-Further trials should be undertaken of broad-spectrum antibiotic treatment as an adjunct toroutine tocolysis in women with preterm laboror rupture of the membranes.
GENERAL 1\1iMiol)01.(x;ic Ism 'ES
Since a major focus of this symposium isintervention studiesand. particularly. rand(mi-ized clinical trialsaimed at reducing the rateof prematurity li.sd IUGR. I will conclude thispaper with a summary of several key method-ologic issues that apply generally to such trials.These issues are: Individual versus group ran-domization, blinding and unblinding. U ie effectof participation on outc()Me. selective subjectparticipaticm. and c(mipliance.
Iiidiiicliial 11.1NUS Group Ralulowizaliou
Random allocation of treatment to eachsubject maximizes the likelihood that tieatment
assignment remains unpredictable hy either thesubject or the investigator. It also tends to resultin groups which are similar for both knownand mknown susceptibility factors that couldotherwise confound the treatment effect. Thus,randomization of individual subjects is a plimedesideratum for a methodologically sound clini-cal trial. For some types of interventions. how-ever, random assignment by individuals canactually be detrimental because interactionbetween subjects may lead to consequent "con-tamination" of the interventicm, and, hence, abiased comparison.
For example. randomizing half of thewomen within a given work setting to a changein posture or position during work (e.g., byallowing them to sit rather than stand whileperforming certain tasks) or to a shortening ofthe work day is likely to lead to a "spill-over"effect to the other half of the women workingin the same setting who are randomized to thecontrol intervention. The result would be adiminution of the difference in the treatmentsreceived by the to groups of women and thepossibility of a false negative result. In such sit-uations, where relatively closed. naturallyf(gmed groups are capable of imxlifying theintervention allocated to individuals withinthose groups. group randomization appearspreferable to the randomization of individualsubjects.
Unfortunately. group allocation carrit:ssome hazards mn. inherent in the individualapproach. Since individuals within a group can-not necessarily be regarded as independentfiom one an()ther. the effective sample size isreduced by the extent of within-gnmp depen-dence. Ideally, the solution to this problem is
4 0
30 71.7e Etiology enui 'mention 'Low Birtinveigbt
to base the statistical analysis on the number ofwork settings (e.g.. companies or factories)rather than on the number of individualwomen. Because of the large number of worksettings required in such studies. however, thisstrategy will often be infeasible.
A more practicable approach wouldinvolve the use of a pre-intervemion study todemonstrate that individuals in two or moredifferent work settings experience similar birth-weight and gestational age distributions beforeinstitution of the intervention. Equivalent pretri-al results increase the plausibility that any dif-ferences in outcome that occur when thoSework settings are exposed to different interven-tions during the actual trial are attributable tothe intervention, rather to potentially c(mf(aind-ing differences between the different settings.The randomized interventkms could even beintroduced in selected settings sequentially mertime so that efficacy could be evaluated yiabefore and after comparisons. as well as con-current comparisons between intervention andcontrol work settings.
Blinding and I 'nblinding
Blinding of study subjects and observers(i.e., double blinding) is highly desirable inplacebo-contmlled interventions involvingdrugs. Such a design is clearly feasible for suchinterventions as placelx) controlled antibiotictrials. It is obviously infeasible. however. forreduction in physical activity or ambulatorymonitoring of uterine contractions, hn the lat-ter types of interventic ns. observers involved inassessing gestational age and birthweight canusually be kept blind. hut the women them-selves cannot.
Mic..hael S. Kramer
Determinants
Mothers knowledge of the group to whichthey have been assigned can then lead to abiased treatment comparison. This is especiallytrue when the comparison is one of interven-tion versus no intervention. Mothers whoreceive the intervention will obviously heaware that they are among the "chosen.- andthis awareness may create a feeling of special-ness that can exert a profound (and uncon-trolled) placebo effect.
Although subjects in these types of inter-vention studies cannot be kept blind to theactual intervention they receive. they can andshould (when ethically defensible) be keptblind to the interventions being compared andto the study hypothesis. Placebo-type controlinterventions can be designed in ways to facili-tate this type of blinding. For example, womenenrolled in a trial to assess tIk' effect of reduc-tion in maternal energy expenditure could beasked to participate in a study of workchanges. Changes in work activities would heimplemented in both intervention and controlgr()ups. with the former changes f()cusingenergy-reducing maneuvers and the latterinvolving other changes not expected to reducematernal energy expendiwre. In this example.blinding would be relatively easy to maintain.as long as the two study groups worked in dis-tinct gow,raphical settings.
1:11ect Participatiwi (al Outoinic
SRIChy participation can change behavic >r.even in the control group. and the behavioralchange itself may affect the outcome understudy (this is known as the I lawthorne effect).It seems likely that the feeling of spedalnessattendant upon participation in an intenention
Advances in the Prevention cf Low Birtinveigbt
study might itself havc a beneficial effect oncertain outcomes. Study participation might, forexample, serve as a fOrm of social support andthus mitigate the effect of stress, thereby reduc-ing the risk of premature delivery. Because thepotential magniwde of the benefit of the inter-vention may be limited (the ceiling effect), theend result may be either a smaller treatmentdifference or no significant difference, and thusa false negative result concerning the effective-ness Of the intervention.
If possible. investigators should attempt tokeep study subjects unaware that they arebeing studied, or at least unaware of the mainoutcomes being ctnnpared. For most types ofinterventions, however, keeping study mothersin the dark will not he ethically defensible. Inthose cases, the potential for a Hawthorneeffect should he acknowledged by the study'sinvestigators, and inferences should be mitigat-ed accordingly.
Selective Sulyect Participation
In general, participation rates tend to belower in intervention studies than in observa-ti(mal studies. Although statistical power can hemaintained by approaching additional Wo men.those who agree to participate may be quitedifferent from those who do not. L'nf()rtunately,therefore, the study's findings may not he gen-eralizable to all mothers who are eligible toreceive the interventkm in the real world.
Investigators should make every effort tokeep track of, and include in all resulting publi-cations, both the numbers and relevant charac-teristics of all women who accept and declineparticipatiom. The characteristics of importanceare those that, independent of the intervention
under study, can affect the susceptibility todevelop IUGR or prematurity. Socioeconomicstatus, age, parity, height, prepregnancy weight,cigarette smoking. and alcohol consumptionare examples of the types of characteristics thatshould be considered.
Compliance
Many of the interventions currently underinvestigation for prevention of low birthweightinvolve some effort b study women to complywith the assigned intervention. To the extentthat women do not comply, differences in out-come between the intervention and controlgroups will be correspondingly reduced. Onceagain, this can lead to false negative inferencesabout the intervention's efficacy. Investigatorsshould routinely include strategies for stimulat-ing and maintaining subject compliance, aswell as measuring its extent, Monitoring ofcompliance could involve pill counts or tracerlabels detectable in urine for interventionsinvolving medication, or onsite observations forsuch interventions as reduction in maternalwork .physical activity or recording of uterinecontractions.
The Indirl statistical analysis for any ofthese intervention studies slumld be based onthe intenticm to treat. that is, a comparison ofall women (or groups or other units of rand(mi-i7.3' randinnized to the IWo) study groups.not just those who comply. A secondary analy-sis comparing those subjects with good compli-ance, however, can suggest what the potentialbiological efficacy of the intervention is andpoint to efforts required in future trials toachieve the c()mpliance necessary to (kmum-strate overall treatment effectiveness.
4'MC Etiology cord Pretottion tow Birthuvight
PRIORMS FOR Ft TURF RIMARC:1
Future intervention studies should focusOn modifiable factors of potential quantitativeimportance for which the evidence of causalimpact on prematurity or IUGR is inconclusive.
In developing countries, the emphasis shouldbe on preventing HIGH. Based on currentknowledge, one promising intervention con-cerns reduction of strenuous maternal workduring pregnancy, particularly in women with
poor prepregnancy or gestational nutrition.Improved prenatal care tin terms of timing, fre-
quency, or c(mtent) should he another high-pri-ority target. Because a few studies have shown
a beneficial effect of folk acid supplementa-tion, further randomized trials in women withfokue-deficient diets should also he undertak-
en. Although the available evidence concerningiron deficiency and ;memia indicates no signifi-
cant effect on intrauterine growth, additionaltrials of iron supplementation in anemic oriron-deficient women may he necessary to rule
out such an effect. Other intervention trialsmight involvc supplementation with other vita-
mins or trace elements (e.g., calcium or zinc)and reduction in exposure to indoor smoke.
In developed countries, future researchshould focus on preventing prematurity. The
most promising avenues to pursue at this timeinclude reduction in strenuous or stressfulmaternal work and physical activity, monitoring
of uterine contractions in winnen at high risk
for premature delivery, and treatment of
women with bacterial vaginosis Or colonizationby certain genital tract pathogens.
In both developing and developed coun-
tries, these research priorities presentformidable methodologic and practical chal-
Determinants
lenges. A randomized trial design should beused whenever feasible and ethical. As I havediscussed, however, the vagaries of humanbehavior, especially during a period as psycho-
logically sensitive as pregnancy, can affect trial
participation, compliance, blinding, and out-come. Thus, a study's use of this design doestun necessarily confer certainty on its conclu-sions. The planning, execution, and analysis ofintervention studies to prevent low birthweightprovide great scope for creative science andhigh hope fin improved public health.
ACKNOWLEIX;MENT
From the Departments of Pediatrics and ofEpidemiology and Biostatistics, McGill
University Faculty of Medicine. This work wascarried out while Dr. Kramer was a National
Health and Research Scholar of the NationalHealth Research and Development Program,
I lealth and Welfare Canada.
REFERENCF.S
I. McCormick. NI. C. (1)8i). The eontributhin ofhirthweight to infant numality and chikflu)od m( r-bidity. NewEngiancilaurna/crrtledicine 312. 82-90.
2. Villar. J., and Belizan. J. NI. (1)82). The timing fac-tor in the pathophysiolc)gy of the intrauterine grcm-thretardation syndrome, 0/),stetrica/ and Gyne-CtibigiCal Stinky 37. 499-5(K).
.4. Kramer. M. 5. (1)8'). Determinants of low birth-weight: A methodological assessment and meta-analysis. Bulletin (il Ibe world uvula) (n:iallization65,063-73-.
Kramer, NI. S. (1987). Intrauterine growth and ges-tational duration determinants. Pediatrics 80,
502-511.
Berkowitz. G. S.. Kelsey. Ifolford, T. R.. andlierkowit7. R. I. (198.4l. Physical activity and therisk of sp(mtanyous pretenn dclivcry. journal (Y.ReproduCtire Medicine 25. S81-S55.
,,Atichael S. Kramer.33
Advances in the Prevention qf Lone Birthweight
C. tarret. J. C.. and Spellacv, NV. N. (1983). jogging dur-ing pregnancy: An impuwed outcome? obstetricsand o.'www,logy 61. 705-709.
7. Clapp. J. F., and Dickstein. S. (1984). Enduranceexercise and pregnancy outc(nne. Medicine andScience in Sports and Evercise10.556-562.
8. Mainelle. N. Laumon. B.. and Lazar. P. ( 198.1).Prematurity and (x.cupational activity during pregnan-cy. American Journal fpidemiology 119. 3(19-322.
9. Saurel-Cubizolles. M..L. Kaminski. M., Llado-Arkhipolf..1.. du Mazaubrun. C.. Estryn-13ehar, M.. Berthier. C..Mouchet. M.. and Kelfa. C. (1985). Pregnancy and itsoutcome anuing hospital personnel according to o(cu-pation and working conditions. ournal cifEphloniology and COMMUnity Health 39. 129-13.i,
10. Stengel, B.. Saurcl-Cubizolles. NI, J.. and Kaminski, NI.(1986). Pregnant immigrant women: Occupationalactivity. antenatal care and (111ICCM1e. Intern(4ll(MalJournal +)./EpidemPdoj 15. 533-5$9.
11. Zuckerman. B. S.. Frank, 1). A.. I hngson. R., Morelock.S.. and Kavne. II. L. (1986). Impact of maternal workoutside the luime during pregnancy oil neonatal out-(ome. Pediatrics:7.45'9-464.
12. Saurel-Cubizolles, NI. J.. and Kaminski, NI. (1987).Pregnant women's working conditions and theirchanges during pregnancy: A national study inFrance. Bitish finirnal of Industrial Medallic ft.230-243.
13. Mamelle. N.. And Munoz. F. ( 1987 ). Occupat ion.11working conditi( ns and preterm birth : A reliable scor-ing system. American journal (f Epidemiology 12ft150-152.
14. Grunebaum. .A.. Nlink(iff. II.. and Blake. I). (1)8-).Pregnancy am( ng ()bstetricians: A (.i)mparisonbirths before. during. and after residency. Americanhurnal (Y. (thstetrics auI 6.17/(Vgihigr I'S-. "9-83
15. Herron \I Katz NI.. and Creasy. R. K. ( 1982).Evaluation Of a preterm birth fvcvention prograill: A
preliminary report. Obstetrics and Gyneculugy 59.452-456.
16. Papiernik. E.. Bouyer. J.. Dreyfus. .1., ( an, 1),,Winisdorfter. Guegen, S. Lecomte. M.. and Li /:1 r.P. (1985). Prevention (if preterin births: A perinatalstudy in ilaguenau. France. Poliatrics -0.151-158.
17. Morrison..1. C.. Martin. J. N.. Martin. R. NX... Gookin. K.S.. and Wiser. W. 1.. (1987). Prevention of preterm
birth by ambulatory assessment of uterine activity: A
randomized study, American lwirnal of Obstetricsand (iyilecologr 150,536-543.
18. lamns. I. 1)., Johnson, F. F., O'Shaughnessy, NV.. andWest, L. C. (1987). A prospective random trial ofhome uterine activity monitoring in pregnancies atincreased risk of preterm labor. American journal (fobstetrics and Gynecolow 157. 038-643.
19, Main. D. NI.. and Gablv. S. G. (1987). Risk scoringt or preterm labor: Where do we go from here?Amerawn journal qf Obstetrics and Gynecology 15-.789-793.
20. Graven, M. Nelson. H. P.. Deliciiien. Critchlow,C.. Eschenback. D. A.. and Holmes. K. K. (1986).Independent associations of bacterial vaginosis andChlamydia tnichonuitis infection with adverse preg-nancy outcome. Journal of tiv American Medicalzissociation 256. 1899-1993.
Lamont. R. F.. Taylor-1i( )hinson, D., Newman, NI.,Wigglesworth, .1.. and Elder, NI. G. (1986). sponun-e(nis early preterm lalunir associated with abnormalgenital bacterial cc )l on zatic in. British Journal ofObstetrics and C.,:ynaccology 93.804-8B).
Berman. S. M., Harrison. li. R.. Boyce. W. T., flaffner.W. J., Lewis. NI.. and Arthur. J. B. (198-). Low birth-weight, prematurity. and ilostpartum undometritis:Association with prenatal cervical Mycoplasma hoini-nis and chlanlydia tmchomatis infecticms, Journal .71.the American Medica1.-Issociation 25. 1189-119 i.
23. Manius..l.. Krohn. NI. A.. 111111er. S. L., Stamm. W. F..Holmes. K. K.. and Eschenbach. D. A. ( 1988 ).ReLnionships of vaginal factobacillus species. cervicalChlanirdia trachomatis. and bacterial vaginosis topretenn birth. oNtetrics and Gynceidogy 71. 89-95.
).4. ..perimg, R. S., Newton. E.. and Gibbs, H. S.Intraamniotic infection in low birthweight infants../(mrual of Infrctious niseaseN I 5. 113-117
25. Potkul. R. K.. Moawas. A. II., and Polito, K. I,. (19$5).The ass( nlatiun suhchnkAI infection with pretermlain*: The role of C-reactiye protein. AmericanJournal cy'(71i8letrics and Gynecolifrgy J53.6 +2-6 +5.
26. McGregor. .A.. French..1 L. Heller. L. B., 'nick!. J. K..and Mak()wski. F. L. i 1,N6), Adjunctive ervtlininIVCintreatment tor idiopathic preterm labor: Results of arandomized. double-blinded, placebo-controlled trial.American ournal of Cibstetric. and Gynecolugy 14; f,98-103.
4 4$4 The EtiolQgy and Pretentiwt Lue Birthue0.7t
Determinants
Statistical Findings:The Etiology and Prevention of
Low Birthweight
Table 3.1
Factors Assessed for independent Causal Impact on intrauterine Growth and Gestational Duration
Infant Sex'
A. Genetic and Constitutional Factors
Racial/Ethnic Origin* Maternal f leight' Maternal Prepregnanc y Weight; Maternal Hemodynamics
Paternal Height and Weight* Additional Genetic' Factors
Maternal Age
B. Deniographic and PsyChos00.31 Fac-tors
Socioeconomic Status Marital Status iAaternal Psyc holcigic Uact )rs
C Obstetric factors
Parity" Birth or Pregnanc y Interval Sexual Ac tivity Intrauterine Growth and Gestational Duration in Prior Pregnancies
In Uter() EXpOtillre to Diethylstilbestror'' Pnor induced Abortion Prior Stillbirth or Neonatal Death
Prior Intert Prior Spontarwous Aborticm"
Gestational %Veight Gain* Vitamin B,
Protein Intake/Status Iron arid Anemia
O. Nutritional Factors
Caloric Intake" Energy Expenditure, Work, arid l'hysk-al Activity
Folic A. id and Vitamin B.. Calcium, Phosphorus, and Vitamin D
Other Vitamins and Trace Elements Zinc and Copper
General Morbidity and Episodic Illneso
E. Maternal Morbidity During Pregnancy
Nialaria* Urinary I rac t !rite( non Genital Tract Infection
f gablishey/ drret delern»nants or int rair141 grrni h U7I lode imam! .4e, r.n ial'ottioi( prepre,gnanc V Wetgill, pahVihil hVight and tteight,
motyrnal height and 4t 4.4,071 panty. ,nrior I 81V. ,t4t...lationd I %%eight gain a I oric intake, .14(./leral morbiditv, malaria. igarettc smoking, alcohdl con-
surnptidn, and folio( 0 ( ing
t Estahlished indirect determlnants intrauter int, et:rots fir? rni Ithit, maternal age and mg ith% oncnrr( status.
4; rautors tiith is ell-estalrlistrcst drrec t aosal 1.1710,1( t mslat dna/ duration in( ludo pIpTi,t).)f, s vir;ht in id
nt titrro diethvIstillx-strol cpo.urc. and cigarette smoking,
prtmlturd% prror spuntanvoirs abor-
rat tors v% ith tell-e.tablis"lcd inchrec t causal rit1pa4 I or? gcst,rt road darati(ur Inc lud( matt.rnal age and sin toe( noir/nit status,
.1 ichael Kramer
4 5
Advances in the Prevention of Low Binhweight
Figure 3.1
Relative Importance of Established Factors with Direct Causal Impacts on 1UGR In a RuralDeveloping Country with Endemic Malaria
E.1 General morbidity A.6 Small paternal size, other
A.7, C.4 Maternal LBWand prior LBW history
A.2 Non-white race
A.3 Short stature
0.1, D.2 Low caloricintake or weight gain
A,4 Low prepregnant weight *KO 151212
Figure 3.2
Relative Importance of Established Factors with Direct Causal Impacts on IUGR In a DevelopedCountry Where 40 Percent of Women Smoke During Pregnancy
E.1 General morbidity
A.7, C.4 Maternal LBWand prior LBW history
A.2 Non-white race
A.3 Short stature
A.1 Female sex
Other
F.1 Cigarette smoking
C.1 Primiparity
A.4 Low prepregnant weight
0.1, D.2 Low caloricintake or weight gain
wt./01151M
36 ,S7atistical Findings: Me Etio/ogy arid Prevention (f Birthweighi
Determinants
Figure 3.3
Relative Importance of Established Factors with Direct Causal Impacts on Prematurity in a
Developed Country Where 40 Percent of Women Smoke During Pregnancy
r
F.1 Cigarette smokingV
trVV
I
VVC.4, C.5 Prior PT and
VV . spontaneous abortion.
OPP
s..
0 NN,,*.N.`.". A.4 Low prepregnant weights-
SK S
VVVV VVV
Unknown VVV
C.9 In utero DES exposure
*WO SS122.
Michael Kramer4
.3 7
Strms ai id Siipport Ditritig
Pregnancy What Do They Tell Us
Abolit Low Binthueight?
EANNE BROOKti-GuNN, Pita
INTRO1M rnoNThe remarkably high incidence of low birth-weight births in the I Tnited States over the past25 years remains vety much a puzzle. Whiletimely antenatal care is assodated with betterbirthweight outcomes, the increases in the pro-portion of women receiving early care in thelast two decades have not resulted in compa-rable declines in the low birthweight rate. Inadditkm, race difkrentials in the proportion oflow birthweight have not changed during thishistorical period (there is a 2:1 ratio betweenblacks and other racial and ethnic groups).'''
It is estimated that perhaps 40 percent ofthe valiance in low birthweight births is due toenvironmental and psychc)social factms (TheInstitute of Medicine 1985 report identifiedhealth behavior, psychosocial and physicalstress, demographic conditions, and toxic expo-
4S
Advances in tlye Pretvntion cd Low Birtbweigbt
sure as principle nonmedical risk factors). Tosolve the puzzle, then, we need to know whichenvironmental and psychosocial events arecontributing to low birthweight; how physio-logical, enviammental, and psychosocial condi-tions each contribute to pregnancy outcome ina relative sense; and what the links might bebetween environmental events or psychologicalstates and subsequent physiological changesleading to early labor.
The focus in this chapter is on which psy-chosocial events are important, rather than howthey actually might initiate early labor or whatthey contribute over and above medical factors.Direct proximate links between psychosocialfactors and actual physiok)gical consequenceshave not been studied in great detail.`' Most ofthe studies conducted to date center on healthbehaviors whose affects are believed to hecumulative in naure (e.g., smoking, postponingantenatal care, and eating poorly); psychosocialstates that are thought to influence the preg-nant woman over a relatively long period oftime (e.g., anxiety, depression, and stress expe-rienced due to negative life events); and envi-ronmental events that are chronic (e.g..poverty, low level of education, and crowdedliving conditions). Since the human fetus isbelieved to be relatively protected (at least pri-mates seem to be less influenced by negativeenvironmental conditions than are rodents),"Thcontinuous exposure to a negative condition isthought to he necessary for a poor pregnancyoutcome. Indeed, the possible effects of short-term stressors in addition to chronic stressors ormultiple negative life events on the long-termmental and physical health of the pc)stpart urnhuman are just beginning to be studied."'"
Five issues are addressed in this chapter:(a) the commonly held belief's about psychoso-cial contributions to poor pregnancy outcome,particularly as they relate to anxiety, stressfullife events, and social support; (b) the associa-tion of these psychosocial factors with healthbehavior; (c) the importance of considering thecontext in which these health behaviors andpsychological factors occur, especially withregard to ethnicity and social class; (d) the use-fulness of different models for studying theeffects of health behaviors and psychosocialfactt)rs simultaneously; and (e) the implicationsof both beliefs and conceptual models for thetypes of preventative programs that have beenand might he initiated.
Siiiss AND St xlIAI. SI l'PORT:
EFFECTS ON PHR ;NANCY 01 TCONIF.
The following assumptiims permeate thepopular and clinical literature about pregnancy:
Anxiety and emotional distress during preg-nancy result in poor pregnancy outcomes.
The occurrence of negative life events, andthe stress associated with coping with suchevents, negatively influence a pregnancy.
Social support acts as a moderatt )r. or 'aS
buffer, from the untoward effects of stressfullife experiences and emotional dysfunction.
Ernotkmal dysfunction and stress have directeffects on pregnancy outcomes ( via some asvet not-well-specified physiological path-ways) over and above health behaviors.such as smoking, nutrition, and exercise.
440 .Sb.ess and Support During Pregruincy
Persistent race differences in neonatal out-come are accounte(I for in part by the factthat blacks arc more likely to live in poverty,have lives that are more stressful, have expe-riences that are more difficult and anxiety-producing, and have fewer available socialsupports (both f)rmal and informal).
Results linking obstetric and neonatal Out-come to emotional states, negative life events,and social support will be reviewed separately.'
It is important to realize, however, that allthree factors are associated with current notionsabout stress. The physiological effects of emo-tional distress or upset have been document-ed."' Often, emotional upset is presumed tobe caused by negative life events and amelio-rated by social support.
Stress is often considered to occur whenan individual is confronted with an event (a)that is perceived as threatening; (b) thatrequires a novel response; (c) that is seen asimportant (i.e.. demands a response); and (d)for which the individual does not have anappropriate coping response available." Stress
has been associated with physical illness aswell as negative emotional states. Stress isbelieved to influence illness via changes inneuroendocrine functioning, immune systemresponses, and health behaviors. Thus, stressmight influence pregnancy outcome directly (interms of physiology) or indirectly (in terms ofhealth behavior).
It has been hypothesized that social sup-port ameliorates these effects at different pointsbetween the appraisal of an event as stressfuland a physical illness. As illustrated by Cohenand Willis," social support may alter the indi-
Jeanne Brooks-Gunn
Determinants
vidual's initial determination that an event isindeed stressful, thereby helping the individualcope successfully, so that the event is not per-ceived as stressful (see figure 4.1). In addition,social support may alter the individual's behav-ioral or physiological response to an eventactually pe-ceived as stressful. Support mayhelp individuals regulate health behaviors,lessen their responses to stress, or help solvethe problem.".'"
Anxiety and Emotional Distress
The idea that emotional upset is associatedwith pc)or pregnancy outcome has a time-hon-ored history. Folk wisdom has linked stress inpregnancy to abnormalities in neonates asdescribed in the Old Testament, by Greekphysicians, and in the writings from the MiddleAges to the present:1- Currently, associationsbetween emotional states and obstetric andpregnancy outcome have been examined, witha number of these studies being reviewedrecently by Istvan and earlier by McDonald.'8'Typically, this literature has focused on anxiety,and, to a lesser extent, on depression, anger,and hostility. In the 1950s and 1960s, nonstan-dardized measures of anxiety were often used,making it difficult to make across-study com-parisons. In addition, most studies havefocused on the more trait-like (i.e., presumablymore stable and enduring) aspects of anxityand emotional upset, rather than on the moresituation-mediated aspects of anxiety (i.e., pre-sumably less continuous or enduring). This issurprising, given that the folk wisdom usuallymentions emotional distress cau:.,ed by a specif-ic situation and that theories such as that ofSeyle consider short-term stressors as well as
41
Adivnces in the Prevention cf Low Biribueight
long-term adaptation to difficult situations.Finally, some (but not all) studies are prospec-tive in nature. In retrospective studies, it is
quite likely that women with preterm infantswill reintopret past events or emotional statesas having been more stressful.'" No studieshave followed a sample of women prior toconception tluough pregnancy and delivery.Thus, no baseline data exist with which tocompare levels of anxiety during pregnancy. orprepregnancy differences between women whoreport high and low levels of anxiety duringtheir pregnancies. Even studies of changes inanxiety throughout the pregnancy are rare.
With these caveats in mind, what do thestudies (focusing primarily on the prospectiveones), tell us about the belief that emotionalupset affects poor obstetric outcome? The twostudies conducted in the 1950s-'"-'' did not sup-powt the thesis and indeed, if anything, provid-ed evidence of the opposite (that is, anxietywas associated with better obstetric Outcome).Of the nine studies reviewed lw Istvan- fromthe 1960s, seven reported sonne evidence of linkbetween anxiety and poor obstetric outcomeand two) did not.' '' BY the 1970s. when morestandardized scales were being used withgreater frequency, of six studies (excludingthose with very small samples), two) providedconfirmatory" and lona had discomfirmakwyfindings.'1- Two) studies from the 1980s foundno significant direct links.- Of particular inter-est is the study of Beck and colleagues:- whoassessed state rather than just trait anxiety andfound no associations with obstetric outcomeduring the third trimester. A measure taken justbefore delivery, ho )wever. was associated withlength of labor. Thus, of 19 studies. 9 report
evidence for the commonly held belief, and 10do not.
Turning to neonatal, rather than obstetricoutcomes, the folk wisdom is comparable.Indeed, the assumptions about links are sub-stantiated in the nonprimate literature. In most(but not all) studies of nxients. emotional stress(as inferred by environmental conditions suchas crowding, and exposure to light, heat andnoise) is associated with poor neonatal out-e.nue (i.e.. prematurity and low birthweight).The human literature is less etmvincing. Onlylooking at prospective studies, three havereported positive associations' "and eighthave not."-- All of these studies usedbirthweight or Apgar scores as their neonataloutcomes.
In brief. the commonly held beliefs aboutmaternal emotional upset, at least whenassessed as anxiety. arc not validated by thecurrent literature. While more support exists forlinks with obstetric than neonatal outcomes.the most recent studies using standardizedmeasures of emotional distress have not alwayssupported the conclusions reached in theobstetric outcome literature of the 1960s.
Stre.s...%/tr/ Evotts
The occurrence of many life events isbelieved to constitute a stressor with implica-tions for emotic Ma 1 and physical well-being.Indeed, events such as the illness or death of aspouse, child, sibling, or parent. as well as theoccurrence of many events simultaneously or ina short period of time, have been associatedwith many illnesses, either as an etiological oran exacerbating factor.'=" Recent work has doc-umented changes in immunological and corti-
Stre.s-s and Sunxin During Pregnano.
sol functioning in the aftermath of negativeevents." "' In addition, the occurrence of multi-ple life events as well as chronic stress oftenassociated with some life events and conditionshas been shown to place individuals atincreased risk for decrements in well-being."''.'"A huge body of literature exists exploring theconditions under which multiple life events arelikely to be detrimental and to buffer the indi-vidual ftom untoward effects."''."''
Research attempting to demonstrate linksbetween negative life events and obstetric out-come is not as extensive as that on emotionaldistress, possibly because most of the theoreti-cal work on life events is fairly recent. Of thesix studies reviewed that looked at obstetricoutcome, results are tr IA)oking at "situa-tional" stresses (perhaps the precursors to neg-ative life events). Grimm and Venet found noassociations with obstetric outcomes.' In the1970s. several studies found positive associa-tions. but only when considered in relation tosocial support. ' " The findings from thesethree studies are difficult to interpret, however.and caution sh(mid be taken in consideringthem as confirmatory.- In addition. two recentstudies either reported no association or a"marginal" one:8"
In four prospective studies focusing onneonatal outcome, an association between neg-ative life events and neonatal status (i.e., lowbirthweight or premature contracti(ms and:ordeliveries) was fOlind tfl two:1'''' a mediatedeffect was found in the third, where life eventswere associated with a -sense of permanence,"which in turn was negatively associated withneonatal problems: and no effect was foundin the fourth." In three retrospective studies.
eanne Brooks-Glitill
Determittants
two reported associations between negative lifeevents and prematurity: In brief, the litera-ture is inconclusive with respect to associationsbetween negative life events and poor out-comes.-
Social Support
The availability and use of s(icial Supportbuffers the individual fr(nn the possible delete-rious effects of negative life events.-" Indeed,some research validates this claim, even thoughquestions have been raised as to whether whatis being measured is a direct effect of lifeevents upon social support or an interaction ofevents and support.'" In addition, social supportmay affect psychological state (and, by infer-ence, physioh)gical state) directly. rather thanthrtmgh interactkm with life events.
It is commonly believed that social supportprotects the pregnant woman or neonate fromthe untoward effects of stressful life events oremoti(mal distress. Perhaps the most oftenquoted study is that of Nuckolls. Cassel. andKaplan:2 in which the occurrence of negativelife events and the availability of social supportwere assessed. While neither was associatedwith obstetric outcome, of the women who hada number of life changes. those with low socialsupport were more likely to have obstetricpr()blems than those who had high social sup-port. This study has been widely cited as evi-dence f()r the importance of social support forbuffering the pregnant woman against the pos-siNe negative effects of stressful life events. AsIstvan points out, however, the result wasbased on a difference of five cases between thetwo groups. and few studies have appeared inthe literature that have replicated the original
Advances in the Prevention of Lou' Birtbweight
finding. In one, which was a retrospectivestudy, an interaction between life change andcomplications was found; specifically, high lifechanges and low social support were associat-ed with neonatal problems (low life changesand low social support were inexplicably asso-ciated with labor and delivery problems, how-even.'" In another, duration of support wasassociated with neonatal complications, hot hdirectly and indirectly.'
HEALTH BEI iAVK)R AND lit.FSS
In the discusskm to date, and in almost allof the studies just reviewed, no considerationhas been given to possible associationsbetween psychosocial factors and women'shealth-related behavior. The implicit premise isthat they affect pregnancy outcomes directly,via physiological processes related to stress. Analternative possibility is that they play an indi-rect role. operating thniugh health behavior,That is, enu)tional distress, social support. andnegative life events might influence women'scompliance with health regimes, or at least mayco-occur with p;trticular health behaviors. Forexample. in the study by Newton and I lunt.life events were associated with low birth-weight, hut this correlation was not significantafter contr()Iling for cigarette smoking. Inanother study demonstrating a link between lifestress and prematurity, the mothers of preterminfants were more likely to smoke and drinkthan the mothers of term infants (unfortunately,the effects of substance use in mediating theoriginal association were not examined). .=
In a study of 500 disadvantaged minority
-i4
women in Harlem who w...re first seen duringtheir first or second clinic visit, a somewhat dif-ferent tack was taken. No differences in theproportion of low hirthweight births were seenfor schooling, work, maternal age, or psychoso-cial factors such as stressful events, social sup-port, and emotional functioning, while smokingand adequacy of care were associated with lowbirthweight. Indirect effects were found, how-ever, as smoking status was associated with thewomen's adequacy of prenatal care, stressfulevents, sodal support, mental health, and prioradverse pregnancy outcome."4"' Current smok-ers were less likely to have adequate care inthe current pregnancy and more likely to haveexperienced :I prior adverse ne(matal outcomethan nonsmokers. They had experienced fewernegative life events than nonsmokers; however,they were less likely to he Hying with a hus-band or boyfriend (see Table +I ).
In brief, previously documented associa-tions between psychosocial factc)rs and birth-wcight may 1 x mediated by health behaviors.That is, social support and emotional function-ing ma% influence health behavi(Is such assmoking and prenatal care, which in turn influ-ence pregnancy outcome. In acklitkm, a differ-ent mix of psvchosocial factors may he relevantft ir different health hellaVit Ks: fur eX:1,111i ile. ill
the a hove-ment lolled study, the psychosocialcorrelates of timing of antenatal-care onset werestimewhat different than those f(ir smoking.
ATRIBI )Ns w En Ni( rry AN/ ) Pc wERTy
Thus far, ethnicity and poverty have mqbeen ccnisidered, even though both are known
Stre.ss and Support During Provtancy
to be associated with low birthweight birthsand both form the context in which a numberof psychosocial conditions occur, For example,the occurrence of negative life events is associ-ated with emotional and physical well-being:'"In addition, undesirable life events are moreprevalent in the economically disadvantaged,the poorly educated, the female, the young,and the unmarried."'' Not only are certaingroups likely to experience negative events,but these very same groups are more vulnera-Ne to them: that is, they will be more likely toexhibit psychological disturbance when con-fronted with negative events, as Kessler hassuggested.7'
Such vulnerability may be due, at least inpart, to the unavailability of reurces, asdemonstrated elegantly in several studies,where the joint occurrence of many stressfulevents and low social support are more predic-tive of psychological distress than either one isseparately:'-` One study has demonstrated thisinteraction in pregnant women: high supportand personal control reduced the impact ofnegative life events significantly. Anotherapproach to considefing the importance of raceand poverty as possible mediators, or as code-terminants of psychosocial functk ming, consid-ers high-risk populations. Demographiccharacteristics, such as race, age, and educa-tion, and risk factors on a population-widebasis, may lose some of their discriminatorypower within low-income groups. That is,increased risk may be confounded with disad-vantage. For example, in the Harlem study, noassoci!fons were found between birthweightand the traditional demographic risk factorssuch as maternal status, education, occupation-
Jeanne Bruoks-Gunn
Ikkytnittants
al status, and ethnicity (Hispanic and black).Thus, the risk associated with these factors maybe more generally due to poverty status. inadditkm, few or relatively weak associationsbetween birthweight and psychosocial factorswere found. This may be because poverty con-fers increased risk for lx)th environmental stressand pocw pregnancy outcomes,"
A final approach involves the possibility ofinteractions between sociodemographic factorsand health behaviors. In one study, blackmothers with preterin deliveries had more med-ical and social conditions than those withoutpreterm deliveries, but the strongest medicalpredictor, hemocrit values, was associated withsocial risk factors (e.g., being unmarried, ateenager, on welfare, or having a low level ofeducati()fl). The authors suggest that combina-tions of medical and sociodeinographic factorsare most likely to be predictive of pretermdelivery and that models including such combi-nations are more likely to reduce the black-white differences than models of socio-dem()graphic conditions alone.--.
Mo Drts To STil».Psycitc)s( VIAL FACR )RS AN!) I UAL-1i I BEI IAVIORS
It is imp(mant to consider the conceptualmodels that are implicit in the studies conduct-ed to date. Indeed, one of the slumcomings ofthe literature is that simple, direct-effects mod-els are usually tested, even though the 1,he-1101IIC11011 under study is bcuer represented bymediated or indirect-effects models. We alsoneed to consider whether relations are bestcharacterized as linear, cumulative, or threshold.
45
Advances in the Prevention of Low Birthweig1.7t
At least five models are relevant (seeFigure 4.2).
1. The first is considered a simple, direct-effects m( x.e.1 1, wAere the links between socialsupport, emotional distress, and life events onthe one hand and poor pregnancy outcome onthe other are examined. Most of the studiesconducted to date have relied implicitly on thismodel.
2. The second, a somewhat more complexdirect-effects model, assumes that interrelaticmsmay exist among the psychosocial factors., theTurner and Noll study is an exemplar.Interestinply, of the more than 20 studiesreviewec that considered both emotional dis-tress and life events, none considered how thetwo might he related.
3. The third model builds upon the secondby adding sociodeniographic factors into theequation. This is important because. as indicat-ed earlier, suhgr(mps differ with respect to theirexperience of social supp(wt, life events, anden-union:II distress (these conditions not beingequally distributed across the population), andthose subgroups at highest risk for stressfulevents may be the very ones with fewerresources available to cope with such events.
4. The fourth model extends this mediatedmodel to include health behaviors. Healthbehaviors and psychosocial factors are hypoth-esized to interact with (me another and to heassociated with poor pregnancy outcomes. Anexample is the work by Newton and associates,in which cigarette smoking and life events wereassociated. with both relating to poor neonataloutcome. When controlling for sinoking, theassociatam between life events and outc( medisappeared.
S. The fifth in()del differs from the f(mrthin that psychosocial factors are assumed toaffect pregnancy outcome via their influence onhealth behavior: no direct effects of psychoso-cial factors are hypothesized. F(n- example. thelarlem study found psyclu)social factors not to
be related to low birthweight. but to be associ-ated with smoking and timeliness of antenatalcare, which in turn influenced low birthweight.
Not only do investigators need to beexplicit about what m(Klel they are testing andbelieve to best represent the links betweenpregnancy conditions and outcome, but theshape of the hypothesized associatilms must beconsidered. Generally, the illustrations in Figure2. like most of our models, are cast in linearterms. At least three other curve shapes must
considered--the curvilinear, the interactive,aiLl the weighted. With respect to life changes.a linear associatirm would imply that a cumula-tive nu)del may be operating; that is, as addi-ti(mal life stressors occur, they increase theprobability of poor outcome accordingly. Eachlife event, therefore. has the Sallie weight. Acurvilinear association (depending on theshape) might suggest that a threslu)ld modelc(mld he operating. That is. a link between lifechanges and poor outcomes would not he seenuntil a critical number of life changes hadoccurred. An interactive association (adding inlife changes separately as well as adding in theinteractions among the changes). if tested forand found, would suggest a more c(miplex.multilevel model. That is, life changes wouldnot be influencing pregnancy outcome in acumulative fashion. but different events, incombination with others. would be in()st pre-dictive. This is in essence the type of model
r46 sirvss am/ Support Ourin,c; Prcgnano.
used in a few studies reviewed, although thesewere examining links between life events andsocial support, rather than different lifeevents.'"2-' A weighted model would assigndifferent weights to life changes, making theassumption that some events are more likely tohe stressful than others; these weights wouldthen be used. either in a cumulative, threshold.or interactive model (sociological literature sug-gests that links between stressful events andmental well-being are no altered appreciablyby using weighted instead of unweighted sumsof life events).
IMPLICAIIONS FOR PREVENTION STRAMIES
The types of preventative services offeredto pregnant women and the subgroups whoare provided services are influenced by beliefsabout the effects of social support and stress onthe pregnant women. In addition, the ways inwhich stress and social support are thought toaffect pregnancy will influence how a programis structured.
Type, !TAT/ iceS
Types of services might be different if thepn wider thought that psychosocial factors influ-enced low birthweight directly or indirectly, viahealth behavior. Se.:eral programs offer socialsupport to pregnant women in the belief that
support may buffer the woman fr(nn the unto-ward effects of stressful life events. In sUrnecases, the implicit gc)al seems to Ix. amehorat-ing emotional distress: in others, minimizingthe effects of life changes, If interactive orbuffering models are found to be applkaNe to
Jeanne Bryoks-GunitG
Determittattts
low binhweight, then these strategies are likelyto be effective. Other programs offer socialsupport with the expectation that women willbecome more adept at managing stressfulevents: in other words, pregnant women areprovided resources or skills in the hopes thatthey will learn how to obtain support for them-selves. becoming less reliant on a caseworkeror other support person in the health servicesystem. The services offered by these programsare often diverse, ranging from informationabout pregnancy, delivery, and child care;referral services for housing; nutrition; medicalcare; jobs; child care; welfare; and so on. In afew, specific curriculums have been developedto teach problem-solving skills. altlumgh theseprograms have not been used extensively forpregnant women. They have been developedmore frequently for new mothers, specificallythose who are disadvantaged, young, or whohave a low birthweight infant.
If, however. a program developer acceptsthe premise that psychosocial factors in and ofthemselves are less important than how thesefactors affect health behavior, then differentstrategies. or a mix of strategies, might beadopted. For example, programs attempting tobring women into antenatal health care earliermay find inf(wmation on the psychosocial cor-relates Of late entry helpful. In an extensiveoutreach effort to identify pregnant women notenrolled in antenatal care in Harlem. compar-isons were made between wc)inen who enteredthe Harlem system via mitreach efforts andthose who came into the system through othermeans. The former group turned out to benum.. socially isolated and slightly older thanthe latter gr(mp.- In a recent paper. discussion
Advances in the Ptvvention Lou' /*dime:phi
centers on the ways in which this informationmight be used to design future outreachefforts." This is particularly important since thepercentage of black mothers with early antena-tal care did not increase in the early 1980s.8R
The mix of services also may be affectedby the ways in which psychosocial factors arethought to influence low birthweight. .v1ost pro-grams provide a mix of services, because (a)providers believe that multiple services areneeded to alter behavior; (b) providers areunsure what services actually make a difference(given the research findings to date, this is notan unreasonable assumption); (c) providerswish to target a variety of outcomes andbelieve that different services are necessary fordifferent outcomes; or (d) services often aresubject to changes in funding levels and per-sonnel complements. While appropriate interms of offering clients a rich array of services,it is impossible to find out what actually makesa difference when a mix of services is provid-ed. Few pregnancy programs allow for separa-tion of different program components (evenwhen randomized control designs are used,typically one group receives the enriched ser-vice package and the other does not).
Because few -strong" models exist toexplain how and in what circumstances some-thing like social support would influencewomen's behavior or emotional state, few pro-grams have developed a specific detailed cur-riculum. Such work is being done for mothersof young children and may be relevant to preg-nancy programs.'M It is critical to collectinf(mation on what service prcwiders actuallydo with their clients; process data would bewelcome. Parenthetically, process data are criti-
cal in order to document changes in the deliv-ery of a service or curriculum over time; suchchanges probably always occur.
Even when a particular group or communi-ty has been targeted (as is the case in most pro-grams), it is important to document whichwomen actually received services, or whatintensity of services each woman received. Inprinciple, most programs provide s:rvicesequally to all women; however, in reality, this isprobably rare. Sr.)me women have more prob-lems, some women seem to need more support,some women more readily stay in touch withproviders, and sone women comply more read-ily with program requirements. All of these fac-tors influence on whom the service providerfocuses. How this situation affects outcome oreffk.,q data is not well documented.
Pwgrant Outcomes
Assumptions about stress and supportinfluence what data are gathered. With mediat-ed models, the out("mnes over and above earlylabor, low birthweight, i GR. and Apgar scoresare relevant. We need to expand our outcomemeasures, however, to look at subgroups, andto consider long-term effects. In the ElmiraProject, in which support and educatim wereprovided to rural disadvantaged pregnantwomen in New York, home visits were associ-ated with reductions in smoking, preterm deliv-ery for the smokers, and in low birthweight forthe young adolescents (those under 17 years).'In addition, nurse-visited women were morelikely to attend childbirth class and the W1.:program; they also reported using social sup-ports more frequently. Such positive outcomesmay increase the chances of good child health
r48 J Stro.s and Suppoil During Pregnancy
and development following the birth.sq Asanother example, long-term effects of a sup-portive curriculum may be seen well after theprogram has ended. In a randomized trial ofthe efficacy of special and comprehensive pre-natal services for teenagers, no effects wereseen for pregnancy outcomes (as indicated byApgar scores and low birthweight). Thoseyoung women who attended the special clinic,however, were more likely to delay their sec-ond birth than those who did not. This delaywas associated with not being on welfare 17years later."' Long-term effects on children (butnot mothers) were seen in Project Redirection,
a program for teenage mothers.'
CONCIA;SION
In conclusion, the literature on psychoso-cial influences on pregnancy outcome, whilenot particularly strong, provides some clues forfuture research directions. More sophisticatedmodels could be derived in order to test specif-ically the associations between and within psy-chosocial factors, sociodermgraphic conditions,and health behavior. Links between chronicstress and uterine contractions, and the possi-bility that social support could alter these asso-dations, should be studied further. Efforts to"explain" race differentials need to take intoaccount factors other than sociodemographicones, to determine why these differentials areso persistent. Finally, research designs takinginto account mediated effects may be useful inthe design of prevention programs.
jeanize Brooks-Gunn
Determinants
ENDNOTES
a. Race differentials may be accounted for in part by eth-nic group vanations in demographic risk factors andhealth behavior. Although controlling for factors suchas education, age, initiation of prenatal care, smoking,and prior low birthweight births reduces race differen-tials, it does not totally eliminate them.2."'
K A slightly different approach has been taken byKramer." who has attempted, via meta-analysis, tospecify the proportion of variance in low hirthweight
and premature births accounted for by various envi-ronmental, psychosocial and medical factors.
c. Other psychosocial factors not discussed here may Ix.relevant for an understanding of pregnancy outcome:InfOrmation Neeking, relationships with mother andspouse, and self-definitions associated with mother-hood are such factors. Iligh information seeking isass(wiated with high self-esteem; the former may act toalleviate anxiety and elevate self-esteem in the preg-nant women, although this hypothesis has not beentested directly.' In addition. relationships withspouse and mother may be particularly salient duringpregnancy. both as social support and, in the case of amother, as a source of information about and rolemodel for parenting:" they are associated with anxietyas well as perceptions of little support."' Womenestablish definitions of themselves as "mothers" dunngpregnancy. Pregnant women who have self-confidenceas mothers and have no difficulty visualizing them-selves as mothers tend to have better postpartumadjustment; they also may he less anxious. althoughlittle research ha.s addres,sed this issue.'"
A retrospective e(miparison of women who hadpreterm. term, and post-term deliveries suggested thatmt)thers with pre-terms had more psychological dis-tress with mothers with terms, who in turn had higherscores than mothers with post-terms. The autluns sug-gest that women with post-term labors are less sensi-tive to oxyt(win than women with pre-term or termlabors.'
e. Alm)st none of the studies reviewed here report themagnitude of the associations. Typically, less than 10percent of the variance in mental and physical healthoutcomes is accounted for by life events." Possiblereasons for the relatively weak associations include the
49
Advances in the Preventkm (y. [)e Birthweight
following: the importance of 4.;ontextually specific factssurrounding the occurence of a negative life event.inadequacy of assessnient instruments, and the r()Iechronic stressors rather than specific life events."'"The last is particularly important in the study of preg-nant women. For example. chronic stressors possiblycould be a contributing factor to the race diffrentialsin low birthweight and prematurity, over and abovefactors such as age of mothers. number of children.marital status, and education.'
ACKNOWLEGN1EN1'
Support was provided by the Bureau ofMaternal and Child Ifealth and the NationalInstitute of Child flealth and HumanDevelopment. The chapter was written while theauthor was a Visiting Scholar at the Russell SageFoundation. The support is appreciated. MarieMcCormick is to be thanked for her comments.
REFERENCES
1. Kessel. S. 5,. Villar. J.. Bert...fides, II. W..andNugent. R. P. (1984). The changing patterns oflow birthweight in the l'nited States: 19-0-1980.Journal ry' the American Meelk.al sso('iati(?n 24;1.1978-1982.
Kleinman..J. C., and Kessel. S. S. (198-'). Racialdifferences in low birthweight: Trends and riskfactors. Neu. England Journal yl Medicine 31-.7-49-7'53.
3. Institute of Medicine. Committee to Study thePrevention of Low Birthweighl. (198.i ).Preventing b)ii. birtbiecight. Washington. DC:National Academy Press.
-4. Fuchs. A. R , and Fuchs. F. (1984). Endocrinologyof term and preterm labor, In: F. Fuchs. and P. G.Stubbk.field (Eds.). Preterm birth: C(IuseN. prctru-lion. (old management. New Yiwk: Macmillan
Myers. R. F.. and NIvers, S. E. ( 19-9). use ofsedative. analgesic, and anesthetic drugs (luringlabor and and delivery: Bane or botm? Americanjournal if Obstetrics and C,:rnecologr 133. 83-10i.
50
Anderson. 1). K., Rhees. R. W., and Fleming. D. F.(1985). Effects of prenatal stress on differentiationof the sexually dimorphic nucleus of the preopticarea (SDN-POA) of the rat brain. Brain Rescyirch332, 113-118.,Istvan. I. (198(,). Stress, anxiety, and birth out-comes: A critical review of the evidence.Ps)'chological Bulletin 10(1, 331-3-19.
5. Riopelle. A. J. (1982). Prenatal pri)tein deprivati(mand early behavioral development. In: J. Orbach(Ed./. Neu rivsycht,logy alter lashlev: Filty _yearsSi 11 CC 1 he publication of Brain Mechanisms andIntelligence. Hillsdale, NJ: Erlbaum.
9 Kessler. R. C.. Price. R. and Wortman. C. B.(198i). Social factors in psychopathology. Annual
Psycliologv 36, 531-5'72.
10. PeaJin. 1.. I. (1983). Role strains and personalstress. In: II. B. Kaplan (Ed.). Psrchiisocial stress;Trenl ... in tbeury and research. Nvw v(Irk,Acadc..rnic Press.
11. Cann( n. W. B. (1939). The wisdom (/ the inhlv.New YiKk: Norton.
12. Seyle. IL (1982). 1 listorV and pres('nt status of thestress concept. In: 1.. Goklberger and S. Brezniti(Eds.). Hatuibi.)4 (fstress: 777eoretical and clinicalaspects. New York: Free Press.
13. (:ohen, S. and Wills, T. A. I985). Stress, social sup-port. and the buffering hypothesis. RsTchuliceilBulletin 95. 310--3-S-.
1,azanis. R. S. (196(). l'svehoh)gical stress anti thecoping process. New York: Mc(1raw
I.azarus. R. S.. and Launier. R. ( vr8). Stress-relatedtransactions between persons and environment. In:
I.. A. Pervin and M. Lewis (Eds.). Perspective innitenictional psyclu dojo.. NeW York Plenum.
16 !louse:J. S. (1981 ). 't irk streSS svcial supprotReading. NIA: Addison-Wesley.
1. Ellis. IL (1936i. The psychic state during pregnan-cy. In: II. Ellis (Ed.). Studies in the psychology ofsex (Yol. 2 ). New itwk: Modern Library. (Originalwork published 190(0
18 NIcDonakl. R. I.. (1968). The role of emotional Lu.tors in obstetric complications. A re iew,Psivt)suinatic Medicinc 30.
Stress and Supprnl Ottrint; Prtgnallo'
19. Omer. H.. Friedlander, D.. Patti. Z.. and Shekel, I.(1986). Life stresses and premature lahc)r: Real con-nection Or artificial findings? PsychosomaticMedicine 48. 362-369.
Cramond. (1951). Psvchological aspvcts of uter-ine dysfuncticm. Lancet 2.1241-1245.
21. Scott, E. Nt. and Thomson. A. NI. (195(,). A psycho-logical investigation of prinligravidae. IV:Psychological factors and the clinical phenomena oflabour. Journal (y. Obstetrics and Gynecology 03.502-508
Grimm. E. R. (1%1). Psychological tension in preg-nancy. Psycluisomatic Medkine 23. 52o-52-.
23. Dayids, A.. DeVault. S., and Talmadge, NI. (1%1).Psychological study of emotional factors in pregnan-cy: A preliminary report. Psychosomatk Medicine23, 93-103.
24. Dayids. A.. and DeVault. S. (1%2). Maternal anxietyduring pregnancy and childbirth abnormalities.Psychosomatic Medkine 404-470.
25, Kapp, F. T.. Hornstein. S.. and G-.-ahmu. V. . (1%3).Sotne psychologic factors in prolonged labor due toinefficient uterine action. Comprebensin, Psychiatry4, 9-18.
26. McDonald. R. L.. Gynther. NI. D.. and Christakos.C. (1963). Relationships between maternal anxietyand obstetric complications. PsychosomaticMedicine 25, 35--363.
Grimm. E. R.. and Venet. W. R. (1%6). The relation-ship of emotional adjustnwnt and attitudes to theCOLIN( and Outcome of pregnancy. PsychosomaticMedkine 28. 34-49.
28. McDonald. K. L.. and Christakos. A. C. (1963).Relationshio of enuiticinal adjustment during preg-nancy to obstetric complications. Amerkan Journal(y'obsterrics (no 6:myco1ogy 86. 3,41-348.
McDonald. R. L. (196:3.), PeNonality characteristicsin patients with three obstetric complications.Pswhosontatic Medicine 38$-389.
30. NIcDonald. R. L.. and Parham. K. J. (19641. Relationof emotional changes during pregnancy to obstetriccomplications in unmarried primigravidas..1111(0CtIll Journal (!f Obstetrics (nut Gynecohig,y 90.19S-.201.
Jeanne 13moks-Gunn
Detertninants
31. Gorsuch. R. 1... and Key. M. K. (1974). Abnormal-ities of pregnancy as a function of anxiety and lifestress. Psychosomatic Medicine 30, 352-362.
32. (;randon. A. J. (1979). Maternal anxiety and obstet-ric complications: Journal of PsychosomaticResearch 23. 109-111
33. Nlorcos, 1. 11.. and Funke-Ferber. J. (1980). Anxietyand depression in the mother and father and theirrelationship to physical conlplications of pregnancyand labour. In: L. Carenza and L. Zichella (Eds.).Emotion and reproiducthm: Proceedings (?/. the Serono.s.ymposia (VOL 2011i. London: Academic Press.
34. Jones. A. C. (19-s). Life change and psychologicaldistress as predictors of pregnancy outcome.Pswbosomatic Medicine -*O. ,+02.--.+12.
35. Burstein, E.. Kinch. R. A.. and Stern. L. (197.o.Anxiety pregnancy labor and the neonate.American Journal (Thstetlks and Civneco/ogy 118.195-199.
36. Edwards. K. 11., and Jones. NI. R. (19-0). Person-ality changes related to pregnancy and obstetriccomplications: Proceedings of the 78th A nnualConvention of the <-11t1CriCati Psycl)ologicalAssociation 5. 341- 3.+2.
37 Beck. N. C.. Siegel. I.. J.. Davkison. N. P.. Kormeier.S.. Breitenstein. A.. and Hall. D. C. (1980). The pre-diction of pregnancy outcome: Maternal preparationanxiety and attitudinal sets. Journal (if Psych(,-somatic Research 21. 3.43-351.
38. Norbeck. J. S.. and Tilden. V. 1'. (1983), Life stressscippcwt and emotional disequilibrium in compli-
cations of pregnancy: A prospective multivariate study.Journal (y' Health and Social Behavior 24. 30-46.
39. Ottinger. D. R.. and Simmons. J. E. (1964). Behaviorof human net mates and prenatal maternal anxiety.Psychological Reports 1 4, 391-394.
Standley. K.. Souk.. B.. and Copans. S. (19-9).Dimensimls or prenatal anxiety and their influenceon pregnancy outcome. American Journal ofobstetrics and c.,:ynecolo,i,o, 135. 22-26.
.11. Ching. J.. and Newton. N. (1982). A prospectivestudy of psychological and social factors in pregnan-cy related to pretern) and low-birthweight deliveries.In. if. Prill and NI. Stauber (Eds.). Ackances inpsychosomatic obstetrics and gynecolor.J. :New York:springer,Verlag.
51
Advances in the Prevention of Low Birthuvight
42. Bunny, W., Shapiro, A., Ader, R., Davis. J., Herd,A., Kopin, I. J., Krieger, D., Matthysse, S.,Stunkard, A., Weissman, M., and Wyatt. R. J.(1982). Panel report on stress and illness. In: G.Eliot and C. Eisdorfer (Eds.), Stress and humanhealth,. Analysis and implications (if research.New York: Springer.
43. Cox, D. J., Taylor, A. G., Nowacek, G., Holley-Wilcox,P.. Pohl. S. L., and Guthrow, E. (1984). The relation-ship between psychological stress and insulin-depen-dent diabetic blood glucose control: Preliminaryinvestigatü m s. Health Psychology 3, 63-75.
44. Kiecolt-Glaser, J. K.. Fisher, I.. D., Ogrocki. P., Stout.J. C., Speicher, C. E., and Glaser, R. (1987). Maritalquality, marital disruption and immune function.Psychosomatic Akdicine 49,13-34.
45. Schleifer. S. J.. Keller, S. E., Camerino, M.. Thornton.J. C., and Stein, M. (1983). Suppression of lympho-cyte stimulation f011owing bereavement, journal qfthe American Afedical Association 250, 374-377.
46. Glaser. R., Kiecolt-Glaser, J. K.. Stout, J. C.. Tarr% K.L., Speicher, C. E., and Ilolliday, J. E. (1985). Stress-related impairments in cellular immunity. PsychiatryResearch 16, 233-239.
47. Dohrenwend. B. S., and Dohrenwend, B. P. (Eds.).(1981). StresVid hfr events and their contests. NewYork: Prodist.
48. Thoits. P. A. (1984). Coping, social suppm-t. andpsychohigical outcomes: The central role of emo-tion. In: P. Shaver (Ed.). Review qf personality andsocial psychology (vol. 5). Beverly lills: Sage,
-49. Kaplan. 11. B. (1983). Psychosocia/stress: Tren(Is Iiitheon and research. New York: Academic Press,
50. Thoits. P. A. (1983). Dimensions of life events thatinfluence psycholcigical distress: An evaluation andsynthesis of the literature. In: II. I'. Kaplan (Ed.).Psycliosocial stress: Trends in theory and research.New York: Academic Press.
Sarason, I. 15,, and Sarason. 15. R. (1984). Social sup-port: Theoty research and applications. The Iiague:Martinus
52. Nuckolls, K. 15.. Cassel..1.. and Kaplan. B. II. (1972).Psychosocial assets. life crisis, and the prognosis ofpregnancy. American Journal (!l* Epidemiology 95.431-+4 I .
52
53. Smilkstein, G., Helsper-Lucas, A., Ashworth, C.,Montano, D., and Pagel, NI. (1984). Prediction ofpregnancy complications: An application of thebiopsychosocial model. Social SCienCe and Medicine18, 315-321.
54. Newton, R. W.. and Hunt, L. P. (1984). Psychosocialstress in pregnancy and its relation to low hirthweight.British Medical journal 288. 1191-1194.
55, Boyce. W. T.. Schaeffer, C., and Utti. C. (1985).Permanence and change: Psychosocial factors in theoutcome of adolescent pregnancy. Social Science andMedicine 21. 1279-1287.
56. Berkowitz, G. S and Kasl, S. V. (1983). The role ofpsychosocial factors in spontaneous preterm delivery.Journal of Psychosomatic Research 27, 283-290.
57. Newton, R. W., Webster, P. A. C., Binu, R S., Maskrey,N.. and Phillips, A. B. (1979). Psychosocial stress inpregnancy and its relation to the onset of prematurelabor. British Aledicalfournal 2, 411-113.
58, Williams. C. C., Williams, R. A., Griswold, M. J., andHolmes. T. H. (1975). Pregnancy and life change.Journal of Psychosomatk Research 19, 123-129.
59. Cassel, J. (1976). The contributOn of the social envi-ronment to host resistance: The Fourth WadeHampton Frost Lecture. American Journal ofhpidemictlogy 101, 107-123.
00. C(ibh. S. (1970). Social support as a moderator of lifedistress. Psychosomatic Afedicine 10, 300-31,1.
01. Thoits. 1'. A. (1982). Life stress social support andilsychological vulnerability: Epidemiological consider-ations. ./ournal gl'Community Psychology 10, 3.41-302.
62. Berkowitz, G. S.. Holford, T. R.. and Berkowitz. R. L.(1982). Effects of cigarette smoking, alcohol, coffee.and tea consumption of preterm delivery. EarlyHuman Develipment 7. 239-250.
03. Brooks-Gunn. J.. Nict.:ormick. M. C.. and Heagartv,C. (1988). Preventing infant mortality and morbidity:Developmental perspectives. ..1,71CriCall fOttr?/(11
Orthopsychiatry 58, 288-290,
(1,1. McCormick. M. C.. Brooks-Gunn. J., Shorter T..Holmes. J. H.. Wallace. C. Y., and fleagarty. NE C.(1990). Factors associated with smoking in low-income pregnant women: Relationship to birthweight,stressful life events, social support . health behaviors.and mental distress. Journal (y. anical lpidemioloKy43, +11-448.
61 Stress (yid Support During Pregnanc.).,
65. Dohrenwend, B. S., and Dohrenwend B. P. (1974).Stressful 0. events: Their nature and Cifra.c. New
York: Wiley.
66, Mueller, D., Edwards, D. W.. and Yarvis, R. M. (1977).Stressful life events and psychiatric symptomatology:Change or undesirability, journal cif Health andSocial Behavior 18, 307-316.
07. Ross, C. E., and Mirowski, J. (1979). A comparison oflife event weighting schemes: Change undesirabilityand effect proportional indices. journal qf Healthand Social Behavior 20, 166-177.
68. Brown, G. W., Bhrolchain. NI. N.. and Harris. T.(1975). Social class and psychiatric disturbance amongwomen in an urban population. Sociolw 9, 225-254.
69, Pearlin. L. I., and Johnson, J. S. (1977). Marital status,life strains, and depression. A nzerican SociohgicalReileu. 42, 70+-715.
70. Pearlin. L. L. and Lieberman. M. A. (1977), Social
sources of emotional distress. In: It Simmons (Ed.).Research in community and mental health.Greenwich. CT: JAI Press.
71. Kessler. R. C. (1979). Stress social status and psycho-logical distreSS. journal (f I et -411 h and Social Behal'Ufrr20, 259-272.
72. Kessler. It C.. and Cleary. P. D. (1980). Social classand psychological distress. Anwrican Sociobwkal
i5, 63-78.
73. Kessler. R. C., and Essex. M. (1982). Marital statusand depression: The role of coping resources. SocialForces 61. 484-507.
Liem. R., and Lion. J. (1978). Social class and mentalillness reconsidered: The role of economic stress ands()cial suppcirt. journal cf Heald) and Social Behavior19, 139-156.
75, Turner. It J.. and Noh, S. (1982), Class and psycho-logical vulnerability among wcimen: The significanceof social support and personal control. journal (fHealth and Social Behavior 2.i. 2-15.
76, Lieberman. E.. Ryan. K. .1.. Monson. R. R., andSclux..nbaum. S. C. (1987). Risk factors accounting forracial differences in the rate of premature birth. Neu,
England journal cf Medicine 317,7.43-7-48.
77. Behrman. R. E. (1987). Premature births among blackwomen. (Editorial). Neu' England Journal qf ,ttedicine317. 763-765.
*Jeanne Brooks-Gunn
Determinants
78. Olds, D. L., Henderson, C. R.. Jr., Tatelbaum, R., andChamberlin. R. (1986). Improving the delivery of pre-natal care and outcomes of pregnancy: A randomizedtrial of nurse-home visitation. Pediatrics 77 , 16-28.
79. Clewell, B. C., Brooks-Gunn, J., and Benasich. A. A.(1989). Evaluating child-related outcomes of teenageparenting programs. Family Relations 201-209.
80. Zigkr, E., and Valentine, J., (Eds.). (1979). ProjectHead Start: A legacy of the war on poverty. NewYork: Macmillan Publishing.
81. The Infant Health and Development Program Staff.(1990). F.nhancing the outcomes of low birthweight,premature infants: A multisite randomized trial.journal of the r1nterican Medical Association 263,3035-3070.
82. limoks-Gunn, J. (1990), Promoting healthy devel-opment in young children: What educational inter-ventions work? In: D. E. Rogers and E. Ginzberg(Eds.), Improving the life chances cf children at risk.Boulder, CO: Westview Press.
83. McCormick. M. C.. Brook.s-Gunn, J., Shorter, T.,Holmes, J. IL, Wallace, C. Y.. and Heagarty, M. C.(1989). Outreach as casefinding: Its effect on enroll-ment in prenatal care. Medical Care 27, 95-102.
84. Brooks-Gunn. j.. McCormick, M. C., Gunn, R. W.,Shorter, T.. Wallace. C. Y.. :md Ife2g:trty, r.(1989). Outreach as casefinding: The process oflocating low income pregnant women. MedicalCare 27, 95-102.
85. Ingram, D. D.. Makuc. D.. and Kleinman. J. C.(1986). National and state trends in use of prenatalcare. 1970-1983. .4mericalt lottrnal qf Pith& Health70, 415-t23.
86. Brooks-Gunn, .1., and I learn. R. (1982). Early inter-vention and developmental dysfunction:Implicaticms for pediatrics. In: Advances in pedi-atrics. New York: Yearbook Publishers. Inc.
87. Lazar. I.. and Darlington, R. (1984). Lasting effectsof early education. Monographs of the Society forResearch in Child Development 47.(1-2. Serial No.194).
88. Ramey. C. T.. and Campbell, E. A. (1986). TheCarolina Abecedarian Project: An educational exper-iment concerning human malleability. In: J. J.Gallagher and C. T. Ramey (Eds.). The malleability ofchildren. Baltimore: Brooks Publishing Co.
53
A(/vances in the Prevention of Lou' Birthuvigbt
89. Brooks-Gunn. J. C1990). Identifying the vulnerableyoung child. In: D. F. Rogers and E. Ginzberg( Eds.). Improving the chances (?,0' children at risk.Boulder. CO: Westview Press.
Furstenberg, F. E. Jr.. Brooks-Gunn. J.. and Morgan.1'. (1987'). Adolescent mothers and their children inlater lifi. New York: Cambridge University Press.Also Family naming.; PersM'ctil 198-7: 19:142-51
91. Polit. D. F. (1989), Effects of a comprehensive pn)-grant for teenage parents: Five years after ProjectRedirection. Family Planning Perspectives 21.16.1-169.
92. NIcCormick. M. C. (1985), The contribution of I()W
birthweight to infant mortality and clnldhood mor-bidity. A'ew England Journal (y Medkine 312, 82-90.
93. Kramer. NI. S. (198-). Intrauterine growth and ges-tational duration determinants. Pediatrics 30.502-511.
94. Deutsch. F. M.. Ruble. D. N.. Fleming. A., Brooks-Gunn. J.. and Stangor. C. (1988). Information-seekingand self-definition during the transition to niother-hood, Journal cf Personality and Social Psychology55, 420-431.
95, Ruble. D. N.. Brooks-Gunn. J.. Fleming A S
Fitzmaurice. G.. Stangor. C.. and Deutsch. F. (1990).Transition to nmtherhood and tilt! self:Measurement. salability and change. Journal ofPemoudity aml Social Psychology...18..450-163.
96. Oakley. A. t 1980). Women confined: Tineards asociology 4childbirth. New York: Sclux:hen B( >oks.
97'. Belsky. J. (1984), The determinants of parenting: A
process model. 07thi Derehonent 55. 83-96.
98. Takagashi. K.. Diamond. F.. Biencarz..I.. et al. (1980).Uterine contractility and oxymevn sensitivity inpreterm term and postterm pregnancy. AmericanJournal (y. (thstetrics and 6.yiweo1oto, 136.
99. Rabkin..1. and Struening. F. L (19-6). Life eventsstress and illness. Science 194. 1013-1020.
1.00.Brown. G. K. (19" O. Meaning measurement andstress of life events. In: B. S. Dohrenwend and B. P.Dohrenwend (Pds.). Stressful life events: Theirnature and effects. New 'York: John Wiley and sons.
54 6 3 stress too Sumort fluring Povtano'
Detennitiatzts
Statistical Fiiidings:Stress and SupportDuring Pregnancy
Table 4.1
Correlates of Cigarette-Smoking in Pregnancy Among Women of Central Harlem
Health Habits and Prenatal Care
Never
(N = 195)
Smoking Status
Quit ForPregnancy
(N = 70)
Current
(N 179)
Uses alcohol 9.7 9.0 10.5
Started care on first trimester 39.9 40.8 32.1
Numer of visits > 4 86.1 87.0 78.5
Adequate care 32.6 31.1 18.7*
Stressful Events/Social Support/Mental Health
Stressful events < 24.6 22.9 14.0*
Lives with husband/boyfriend 35.0 27.6 20.3*
Belongs to a church 58.6 41.7 41.7*
No situations with support 23.1 18.6 10.6*
GHQ > S 25.1 47.1 27.4*
p < 0 OS, ic v%ith appropnote degrees ot treillontFun?? Mt On tip< h, tit .11., present pubbt ation
Figure 4.1
Social Support and the Buffering Hypothesis
Two points at which social support may intertvre vvith the hypothesized causal link between stressful events and illness*
Potentialstresstuleventisr
Soi. ;al Support'may prevent stress
apprais.11
App aisalProt ess
' fro!, 0)17111 N 1(485, page I
JeC11111V kc-6.1111 11
f (ntts,apprAisecias stressful
64
So< tal +tipporfmay result in rtypprais,11,inhibition or maladjustiveiresponses, or tat ilitation nt
arliustRe t our er responses
I motionally linked ph% Sr( 1-
logic al respr ins(' or lwha% -
moral adaptation
andiorbeha%ior
55
Advances in the Prevention qf Low I3irthavight
Figure 4.2Five Possible Models for Studying Associations Between Psychosocial Factors and Pregnancy Outcomes
4.2aDirect Effects Model: Simple
Psychosocial Factors Pregnancy Outcome
4.2bDirect Effects Model: Interrelations Among
Psychosocial Factors
Emotional Distress .
Negative Life Events Pregnancy Outcomewr
Social Support
Figure 4.2cDirect and Indirect Effects Model: InterrelationsAmong and Between Psychosocial Factors and
Sociodemographic Conditions
Emotional Distress
Negative Life Events
Social Support #
Education
Age
Number of children
Income
Race
0.47 Pregnancy CJutcome
Figure 4.2dDirect and Indirect Effects Model: Psychosocial
Factors, Sociodemographic Conditions, andHealth Behavior
Emotional Distress
Life Events
Support
!Aealth Behavior *A
11
1
Education
Age
Number of children
Income
Race
Pregnancy Outcome
56 Statisi441 Findings: Stress and Support During PnignancyO
Emotional Distress
Life Events
Social Support
Education
Age
Number of children
lnconwA
Race
Figure 4.2e
Mediated Model: Effects Through Health Behavior
Health BehaviorDuring Pregnancy
Jeanne Brouks-Gutin 6 ;
Determinants
ID- Pregnancy Outcome
Rau lts of a Three-Year Praspectiu?
ControlW Randomized Trial ofPretenn Birth Prevention at the
Univetsily of Pittsburgh
EMU LARD Mt ELIER4 1E1.13AC11, M.1).
INTRODITCVION
Measures of health care in difkrent societiesare difficult to compare; however, it is oftenstated that infant mortality (momility during thefirst year of lif) is an important indicator ofhealth care in a nation. According to the latestavailable statistics, the United t;iates ranks 19thin infant mortality among the nations of theworld, a decline from the rank of 15th held in1968. Upon examination of the differences ininfant mortality in different societies, it is readi-ly apparent that by far the most important fac-
tor is neonatal mortality due to pretermdeliveiy. In countries with lower infant mortali-ty rates, fewer neonates die as a result ofpreterm delivery. Thus, the causes and the
Adtzinces in the Prowntion qf Lou, Birth u vigb t
prevention of preterm birth are of utmost con-cern to individuals interested in perinatal healthcare. Definition of preterm birth as birth beforecompletion of the 36th week is preferable to adefinition by birthweight (<2500 g) because thelatter includes term newborns who are grmthretarded and have lower morbidity and mortali-ty. Definition of preterm birth by gestational ageis often difficult, however, due to uncertaintyalxmt the gestational age in some patients
Preventiom of preterm birth is the ultimategoal of perinatal health care, and any promis-ing approach in this area is readily embraced,often without careful scientific scrutiny, bymeans of prospective randomized trials.Reports of a reduction in preterm births as aresult of preterm birth prevention pmgrams inthe United States, France,' and Martinique'prompted us to evaluate a preterm birth pre-vention program in an indigent clinic pcpula-tion at our institution. In contrast to thepublished reports. we planned to study thepotential efficacy of such a prograin in aprospective controlled randomized designusing birth before 36 completed weeks of ges-tation to define preterm birth.
MATERIAL AND MI:11101)5
During a three-year period, all patientswho registered for prenatal care at Magee-Women's Ilospital in Pittsburgh were screened,and the scoring system of Greasy et al: wasused to assign risk scores for preterm labor andbirth. A score of 10 or more placed the patientin a high-risk group for pretenn labor andbirth, while patients with a score below 10
were considered to be in a low-risk category.Patients who presented for the first time after28 weeks' gestation were excluded. Similarly,patients whose estimated date of delivery wasafter the end of the three-year study periodwere not enrolled. Patients assigned to thehigh-risk group were approached and invitedto particirate in a prospective randomized con-trolled trial of preterm birth prevention.Participants signed a consent fc)rm appnwed bythe Institutional Review Board. Patients whodid not participate were classified as refusers ifthey declined participation; they were classifiedas ineligible if they could not be randomizedbefore 28 weeks' gestation or if they did notreturn for prenatal care after randomizationuntil they were 28 or more weeks' gestation.
Patients were randomly allocated to either acontrol group with the usual prenatal care or anintervention group. Two nurses with extensiveobstetrical experience gave individual teachingto patients in the intervention grcnip regardingsubtle symptoms and signs of preterm labor.such as appearance of -menstrual cramps." lowerback pain, -gas pain." suprapubic pressure, thighpain, or change in vaginal discharge. Thepatients were instructed in self-palpation of theuterus and the contrast in feeling between a con-tracted and a relaxed muscle was demonstratedto them. Patients were told that they should liedown on their side when they noticed contrac-tions and drink a quart of liquid within an hour.If contracticms did not subside during this hour,patients were instructed to come to the hospitalfor evaluation. Weekly cervical examinationsfrom 20 to 37 weeks' gestation were performedon patients in the interv-...ntion group, with gentlepalpation of cervical effacemem and dilation.
6 ; )
62 A Prospective Contmlled Randomized Trial qf Preterit? Binb Nervation at tbe I .niversity (plias-burgh
Rescreening of low-risk patients was donebetween 22 and 26 weeks' gestation. as well asupdating of the initial risk score at other timeswhen new findings were made.
Repeated teaching sessions were given bythe investigator and the two study nurses to theresident physicians and the nurses involved inthe care of clinic patients. The physicians andnurses were informed about the instructionsgiven to patients in the intervention group inorder to assure a proper response lw medicalpersonnel during communications with patientsin this group.
All data cencerning risk scoring, admis-sions for preterm labor, and deliveries wereplaced on special forms from which they wereentered into a computer data base to permitdata analysis upon completion of the study.Preterm deliveries were classified :is sponta-neous, indicated, or iatmgenic. Data from theMagee-Women's Ilospital Perinatal ComputerData Base fin- an eight-month period before ini-tiation of the study were used to establish ahistoric control period. Chi-squared or Fisherexact tests were used for statistical analysis.
l(zst tus
A total of 5,i57 patients had initial riskscoring fc)r preterm labor, of which 4.595 deliv-ered at 20 or m( re weeks gestatkm. Alx)rtkmand loss to f()Ilow-up accounted tbr the differ-ence. Risk scores of > 10 (high risk) were pre-sent in 831 of the .)ri patients (18.1%). Thepreterm birth rate (less than 3(' completedweeks) was 10,1 percent for all patients. Thisrate was about 3 times higher in patients scored
Eberhard .tfuellerlIeltbach
/Wen VIItions
as being at high risk of pretcrm labor (21.9%)compared to patients scored as being at lowrisk (7.4%). The majority of patients deliveringpreterm (60.4%), however, were in the low-riskgroup. Rescreening at 22 to 26 weeks was donein 2,145 of the patients initially scored at lowrisk; only 33 patients (1.5%) became high risk.Six additional patients became high risk as aresult of updating risk scores.
Comparison of high-risk intervention, con-tn)1, refuser, and ineligible groups demonstratedsimilar preterm birth rates (22.1%, 22.8%, 19.5%,and 23,6%, respectively) throughout the study.There was, however, a significant decline inpreterm births between the first and secondyears of the study (from 13.8% to 9.3%, p <0.001). This decline was maintained during thethird year when cc unpared to the second (.!.ar
(9.3% v. 8,7%, NS). The decline in pretermbirths from the first to the second year was ofthe same magnitude in the high-risk population(-29.1%) as in the low-risk population (-32.1%).During the first year of the study, the attitude ofresident physicians and nurses involved in thecare of the clinic population toward the pretermbirth prevention program changed from skepti-cism to acceptance and then to genuine interest.Being concerned about the problem of pretermbirth. these health care professionals appliedthe instructions learned in the multiple teachingsessions tO all patients under their care.
In order to verify that the decline in pretermbirths during the second and third years of thestudy was related to the preterm birth preven-tion program. we first examined whether thepreterm birth rate during the first year of thestudy was exceptionally high by comparing it tothe rate during the eight months before the
706.3
Adt,ances in the Prevention qf Low Birthweight
study (the historic control period). There was nosignificant difference in preterm birth ratebetween the historic control period and the firstyear of the study (14.1% v. 13.8%, NS).
To exclude the possibihty of a time-relateddecrease in the preterm birth rate during thehistoric control period and the three years ofthe study unrelated to the preterm birth preven-tion program, we studied the preterm birth ratein the private patients who delivered at ourinstitution and had received their prenatal careby private physicians in their offices in the area.Neither these private physicians nor their officestaffs were aware of the content of the pretermbirth prevention program. During the historiccontrol period and the 3 years of the study, thepreterm birth rate in the private patient popula-tion (with an average of 7,764 births per year)did not change significantly and ranged from8.0 to 8.6 percent. When the historic controlperiod and the first year of the study were com-pared with regard to preterm birth rate in clinicand private patients, the preterm birth rate wasfound to be significantly lower ( p < 0.001) inthe private patients. Due to the decline inpreterm births in the study clinic patients duringthe second and third years of the study, therewas no significant difference in the pretermbirth rate between clinic study patients and pri-vate patients during these time perk xis.
We evaluated the study population (exclud-ing patients with indicated preterm deliveries)regarding episodes of preterm labor, use oftocolysis, and prolongaticm of pregnancy to termin patients having received tocolysis. No cse ofiatrogenic preterm birth was noted in our study.
There was no significant differencebetween the percentage of patients presenting
with preterm labor in the high-risk interventiongroup and those in the high-risk control group,but significantly more patients in the interven-tion group were candidates for tocolysis =
0.01). Nevertheless, there was no significant dif-ference among patients receiving tocolysis withrespect to prolongation of pregnancy to term.Figure 5.1 illustrates the frequency of pretermlabor, preterm birth, and tocolysis in the totalstudy population during the three years of thestudy. The decline in the preterm birth rate isclearly related to the fact that fewer patientspresented with preterm labor during the sec-ond and third years of the study. The frequencyof tocolysis was unchanged during the threeyears of the study. Thus, it appears that the
Table 5.1: Percentage of Patients with PretermLabor, Preterm Birth, and Tocolysis During the
Three Years of the Study12
11
10
9
8
7
6% of
Patients
5
3
2
7 0
Year l Yew 2 Year 3
64 A Prospectite Contrail& Randomized Trial VPreterm Birth Pretvntion ell the CfPittsburgib
teaching and the change in attitude was associ-ated with a decrease in the nunther of patientspresenting with preterm labor. On the otherhand, this was not accompanied by a decrease
in the incidence of tocolysis, indicating that thediagnosis of preterm labor was more oftenmade correctly by patients.
A reduction in preterm births may lead to adecrease in neonatal mortality in infants deliv-
ered before 37 weeks' gestation without congen-ital anomalies. There was a significant decrease
in neonatal deaths in this category when the his-torical control period was compared to the sec-ond year of the study (from 9.1/1000 to2.2/1000. p 0.0089) and the third year of thestudy (from 9 1/1000 to 2.8/1000, p = 0.0217).
DNA'S:410N
Preterm birth prevention programs attemptto increase the awareness and recognition ofsubtle symptoms and signs of preterm labor
among patients and their health care providers.As a result of the teaching sessions in ourstudy. such a change became apparent duringthe first year of the study when health care per-sonnel asked many questions about this pro-gram, became aware of the subtle symptomsand signs of preterm labor, and conveyed these
to the patients. Patients were frequently sent tothe study nurses for enrollment in the pretermbirth prevention program when they, in fact,
had been previously randomized into the con-trol group. Evaluation of the preterm birth rates
in our study revealed no difference betweenthe high-risk interventk)n and control groups,but an overall significant decrease during the
Eberhard Afileller-I ieu bad)
7
Intenentions
second and third years of the study irrespectiveof the risk assignment.° Thus, the health careproviders, with their concern about pretermbirth, had defeated the prospective controlledrandomized design of the study by also chang-ing their care for patients who were not in the
high-risk intervention group.The initial risk scoring system classified
'18.1 percent of the patients as high-riskpatients, but only 39.6 percent of the pretermbirths occurred in the high-risk group.Conversely, a patient in the high-risk group had
a 78.1 percent chance of delivering at term.Rescreening and updating of risk scoreschanged the initial risk score in few cases.Thus, the concept of risk scoring may either beof limited value or specific risk scoring systemsneed to be developed for specific populations.The results of our study suggest that education-al programs applied to entire patient popula-tions may he preferable.
It is clear that the observed decline inpreterm birth rate in the study population was
not a time-related trend independent of thepreterm birth prevention program becausecomparison with the preterm birth rate in theprivate population during the same time perioddid not reveal such a trend. The decline in the
preterm birth rate observed in our study maynot he possible in all patient populations. In amuch smaller, similarly designed study of poor,inner-city black women in Philadelphia, theinvestigators were not able to show any differ-
ence between high-risk control and interven-tion patients.- This is in agreement with ourfindings; however, the study was not largeenough to possibly document any of thechanges over time which we observed in our
65
Advances in the Prevention of Low 131n/weight
large, three-year study. Considering the magni-tude of the problem of preterm birth, with itsaccompanying neonatal mortality and seriouslong-term morbidity (such as permanent neuro-logical handicaps, bronchopulm(mary dyspla-
and retrolental fibroplasial, any promisingeffort to reduce the preterm birth rate shouldbe pursued. Attempts should be made to evalu-ate whether a preterm birth prevention pro-gram can lower preterm birth rates in otherpopulations with the same degree of effective-ness as it did in our indigent clinic populationin Pittsburgh.
Supported by March (if Dimes Grant 2-196/C-404
REFERENCES
1. The National Commission to Prevent Infant Atonality.(1988. August). Death btyOre e: The tiligedyinjant mortalit.y. Washington, DC: Author.
2. 1Ierron N1 Katz. M.. and Creasy. R, K. (1982).Evaluation of a preterm birth prevention program:Preliminary report. obstetrics and Gynecology 59.452-456.
3, Papiernik, E., Bouyer. I.. Dreyfus..L. Collin. D.,Winisdortier. Guegen, S., Leconte. N1., and Lazer.
(1985). Preventkm of preterm births: A perim1t:t1study in I laguenau. France. Pediatrics 70, 154-158.
1. (;()u)on. 11.. Papiernik. E.. and Main, D. (1984). Theprevention of preterm delivery thrc)tigh prenatalcare: An intervention study in Martinique.International Journal (?1Gynaecology (Ind obstetrics22339-3.+3.
5. Creasy, R. K Gummer. B. A.. and Liggins. C. C.(198(1). System for predicting spontaneous pretermbirth. Obstetrics and 6:yneodoAy 55. (92-095.
(). Mueller-I leulLich, E.. Reddick. D., Barnett. B andBente. R. (1989). Preterm birth prevention:Evaluation of a pnispective controlled rand( wnizedtrial. .4mericanjournal cy Obstetrics andGynec(dogy I U. II72-117s.
Main. D. NI.. Gabby. S. Cr.. Richardson. D.. andStrong. S. (198,4). Can preterm deliveries be pre-venlecl? Americanicornal f!1( )bstetries andGynecology 892-898.
8. Institute of Medicine. ( 1985 Prewnting low birth(p. 31-38). Washington, DC: National
Academy Press.
'7
66 A Prospectne Controlled Randomized Dial qf Prelerm Birth Pretention at the t nivercity ((Pittsburgh
Decrease and Rise in Rates ofPretenn Deliveries:
Haguenau Prenatal Study,1971-1988
EMILE PAPIERNIK, M.D.
JEAN BOUYER, PHD.
JEAN DIU:XI-Vs, M.D.
GERARD WINISIX)RFER, M.D.
DOMINIQUE COLLIN, M.D.
INTRODI X.:MN
A 17-year study on the prevention of pretermdeliveries in a delimited region of France hasbeen used as an evaluation tool for the mea-sure of effectiveness of a national policy forimproving perinatal outcome (1971-1988). Thesame tool served as a measure of the recur-rence of higher rates of preterm deliveries afterthis national policy was no longer followed.
This paper will describe the ways in whichpregnant women have changed their behavior,coming earlier in the course of their pregnancyto the maternity outpatient clinic and moreoften to seek the best available prenatal care. It
'7
Advances in the Prevention uflow 13irthweight
was observed that the reduction in the rates ofpreterm births was obtained not in the high-riskcategories, as was expected, but in the lowerrisk categories.
After cessation of the government drive, weobserved how the efforts of pregnant women tocome early and often to the maternity outpatientclinic were turned down, and how this resultedin the rise in the number of preterm deliveries.
PATIENTS AND NIEIIK)Ds
The Ilaguenau Maternity Hospital serves aspecific limited region in Alsace. France, and wasused as an evaluation tool to measure the effec-tiveness of a policy applied nationwide. Theprinciples of preventive measures to reduce therates of preterm deliveries have been exposed inprevkms papers. They consist of a community-based intervention proposing to all pregnantwomen a new type of prenatal care. The majorcomponents of the intervention are a risk analy-sis for individual factors predicting a pretermdeliverv. and several measures aimed at decreas-ing uterine contractions and preterm deliveries,which have been described in detail elsewhere.'
The basis for applying this policy was a gov-ernment program appnwed for five years in1971. and extended for five additional rears in1976. The objectives were to rethice perimitalaccidents leading to death and perinatal-inducedhandicapping conditions. The means employedincluded financial inducements for the publichospitals to help improve their equipment fordelivery and neonatal care; financial induce-ments for postgraduate training sessions for doc-tors, midwives, and nurses working in the field;and financial inducements to speed up public
70
information directed at women to encourage bet-ter perinatal follow-up.
This government initiative helped inspreading basic concepts and techniques forthe improvement of prenatal and intrapartumcare, and neonatal resuscitation measures aswell as neonatal care. In addition, the drivehelped in spreading new ideas, such as theprevention of preterm delivery using tech-niques we proposed.
After 1981, a new government took overand decided not to pursue this established poli-cy. As good results had been achieved, theopinion of the politicians was that the programhad served its purpose and that no supplemen-tary efforts were needed to maintain the ongo-ing measures. Thus, perinatalogy came to beout of fashkm, and public attention was drawnto other aspects of reproduction, specifically toquestions centered around in utero fertilizationin the early 1980s and to AIDS in the late1980s.
In the present study, we measure theknowledge and conviction of pregnant womento use the best accessible prenatal care systempnivided free of cost at the Outpatient clinic ofthe Haguenau Maternity Hospital; specifically.the proportion of women consulting in the firsttrimester (instead of being followed by theirgeneral practitioner) and the number of prena-tal visits made before 20 weeks.
Information about the women and theirpregnancies was very carefully gathered usingthe best knowledge available by the last men-stnial period (LNIP). length of cycle, ultrasoundscan, and pediatric examinatkm of the neonate.All of the data were computed in die days fol-lowing delivery. All babies transferred to a
Decrease and Rise in Rates of Preterni 1)eliveries--11aguenau Prenatal Study. 1971-1988
neonatal intensive care unit were included inthe study, as well as Ixthies of women trans-ferred to a referral center.
REst.iLis
The results were examined for two succes-sive policy application periods. The firstsequence, from 1971 to 1982, WaS divided intothree periods of four years each. The secondsequence will show the last period of fouryears, from 1983 to 1986.
Reduction in preterm deliveriesA pn)gressive reduction in preterm deliver-
ies was observed during the 12-year periodfrom 1971 to 1982. The global rate of pretermbirths defined as less than 37 weeks of gesta-tion from the first day of the last menstrualperiod was reduced from 1971 to 1974 andfrom 1979 to 1982 (see table 6.1).
Reduction in tran. encto a neonatal intensive core unit
As the number of babies in need of inten-sive care had decreased, the transferral to aneonatal intensive care unit because of pretermbirth was significantly reduced (see table 6.2).
It should be noted, however, that the propor-tion of transferred babies to the number ofpreterm births was not reduced but ratherincreased. In the same period, transfers for
other reasons and, specifically, for malforma-
tion of the newborn were augmented.
Reduction in length cy' hospitalizationrequired hypreterm newborns
The need for intensive care for pretermnewborns has been quantified according to) the
Emile Papiernik ci aL
1nterivntions
number of days of hospitalization required for
the babies transferred to a Level III center neo-natal intensive care unit (WU) in Strasbourg
as well as to the neonatal care unit in the localhospital of Haguenau (see table 6.3).
Reduction in neonatal mortalityNeonatal mortality was reduced in this
time sequence, and the decrease in the numberof preterm babies was a part of this reduction.Table 6.4 describes the total neonatal mortality
in the three successive time periods. A directstandardizaticm was done, as if the pa)portkmof preterm births would not have changed from
that of the first period (1971-1974). with week-specific mortality rates for 1971 to 1978 and for
1979 to 1982. 11 1sAows that about half of the
progress can be attributed to an improvementin the care of newborns and that half of theprogress can be explained by the reduction inthe number of pretenn babies. The total reduc-
tion of neonatal deaths was then obtained bybetter care as well as "better babies."
Reduction in proeml birthsin women with no defined 1-isk filctoIN
The reduction in preterm births was notobtained in high-risk w(mien; that is, thosewomen with a previous preterm birth, with aprevious stillbirth, of short stature, of less thanaverage weight, of less than 21 years, of morethan 35 years. or with a history of bleeding inthe second or third trimester. On the otherhand, a significant reduction in preterm births
was observed when the women did not fall inthe above-mentiomed risk group. Thus. fewer
preterm births were observed in those womencharacterized by the absence of a defined risk
71
Advances in tbe Prevention of low Birtburight
factor; that is, with no previous preterm birth,with no previous stillbirth (among pawnswomen), with a normal stature (above 152 cm),with a normal prepregnancy weight (more than48 kg), of between 24 and 34 years of age, andwith no history of bleeding in the second orthird trimester (see table 6.5).
Reduction in bigb-riskfactotNThe rate of high-risk factors was reduced in
the observed population. This reduction wasobserved for previous preterm birth, for age lessthan 21 years and more than 35 years, and forbleeding in the second or third trimester (seetable 6.6). The relationship between this reduc-tion in risk factors and the population of preg-nant women will be discumed subsequently.
Early obstetrical prenatal careand prelyntion oJpretertn delii)eries
Our hypothesis was that a new type ofprenatal care could prevent preterm deliveries.The basic premise was that 7-duction in job-related and home-related excessive physicalefforts for at-risk women would be effective.That meant that women had to be convinced tocome early and often to meet the teams ofobstetricians and midwives able to inform themand offer specific risk assessments for eachWOMarl at each prenatal visit.
The pregnant women had to be convincedto come early and often to meet these new pro-posals. Then the early enrollment in the obstetri-cal outpatient clinic and the number of prenatalvisits before the end of the 6th month couldserve as accurate measures of the acceptance ofthis care proposal and of the effectiveness of theinformation given to the general public and to
all women. We used these simple measurementsas markers of the success of the governmentefforts in the prevention of preterm births.
Table 6.7 and figure 6.1 show the relation-ship between earliness of care and pretermdeliveries for four-year periods and for threegroups of women defined hy the number ofyears of school completed (Up to 9 years,10-12 years, and 13 years and above). Theacceptance measures here described are:
A. The mean number of prenatal visits in thefirst two trimesters of pregnancy at the out-patient clinic of the obstetrical department;
H. The proportion of women in each groupenrolled in this outpatient clinic;
C. The proportion of pregnant wc.)men in eachgroup who never had a prenatal visit at thisoutpatient clinic of the obstetrical depart-ment; and
D. The proportion of preterm deliveries (bygroup and by study period).
The new type of prenatal care was accept-ed and was requested by all groups of women.with important differences between groups.The more informed the women were, the earli-er they came in. For the first 12 years of study,from 1971 to 1982, a progressive rise in accep-tance of care was noted, with persistent differ-ences between groups, and with a time lag ofabout four years between women with 13 yearsof schooling and women with 10-12 years, anda time lag of eight years between women with13 years of schooling and women with up tonine years. In the meantime, during this periodof progressive acceptance of prenatal care, therate of preterm deliveries went down, with per-
7772 Decrease and Rise in Rates cf Preterm lkiiivries--11aguenati Prenatal Study. 1971- 1988
sistent differences between groups. and alsowith a time lag difference between groups ofthe same order as that observed on the behav-ior of acceptance of new care. After 12 year:,in the fourth period (1983-1986), instead ofimprovement, a new movement of reduction ofthe three measures was observed. The pregnantwomen sought consultation much later in thecourse of their pregnancies and came less oftenin the first two trimesters. In addition, moreWOMCII came in directly for delivery withoutbeing previously followed. During the sameperiod, the rates of preterm deliveries went upfor the three observed groups of women.
Mathematical relationship beturenprenatal care and preterm delitteries
A regression analysis was done to measurethe precise relationships between the precedingcharacteristics of prenatal care and the outcomein terms of the proportion of preterm births.The regression curve for women by group andnumber of preterm deliveries is shown in figure6.1, with the equation Y(pr()ortion of pretermbirths) = X (proportion of pregnant women byschool attendance group enrolled in prenatalcare at the outpatient clinic of the maternityhospital in the first trimester).
1' = 0.078-0.07.1X
r -0.95
p = 0.001A similar relationship was found lvtween
the number of prenatal units at the outpatientclinic of the maternity hospital and the numberof preterm births, and a similar correlation wasfound between the proportion of women notfollowed by the obstetrical team and the num-ber of preterm births.
Intert,entioits
Disct ISSION
The observed mathemthical relationship be-tween the characteristics of care and outcomeare very similar to a dose-effect relationship. Thisfeature supports the hypothesis of a causal rela-tionship between this type of care and theobserved effect. This point is important. as ourpolicy has been applied in the whole of France,and without the opportunity to apply an experi-mental design, as we would like, to support ademonstration of the effectiveness of our policy.On the other hand, we know the effort to pre-vent preterm deliveries has been applied inFrance, but has not been applied in Germany,the United kingdom, or the United States. It hap-pens that France is the only country among thesefour to have observed a reduction in pretermbirths between 1970 and 1980, and, during thissame period, no reduction could be demonstrat-ed in the three other countries. Obviously, this isnot as good a demonstration as a randomizedtrial would have been; however, this differencecannot be discarded.
We did not expect that France, by itself,could serve as a control. But the cessation of thenational policy in the perinatal field in 1981 hasprovided us with this quasi-experimental design.We can take advantage of this to propose a newargument fm a causal relationship between thenew type of care and prevention of pretermdeliveries, as the numbers were exactly thesame on the regression curve backup,
REFERENCES
Papicrnik, E. (19(9 }. Coefficient de risqucd'accouchcment prCmature. Presse Medic-ale
2.
793--7(Xl.
Pvicrnik, F. (1)8,4). Pniposals fur a programmedprevention policy of preterm birth. ClinicalObstetrics attd 6:rtwcolfxr 27. 61-4-035.
Emile Papiernik et al. 7$
7:1;
Interventions
Statistical Findings:Decrease and Rise in Rates of Preterm Deliveries
Haguenau Prenatal Study 1971-1988
Table 6.1Preterm Deliveries and Live Births
1971-74 1975-78 1979 82 P Value
< 32 weeks 5.4 4.0 3.6 0.001
299/5548 192/4787 210/5811
35-36 weeks 2.9 2.1 2.4 N.S.
159/5548 102/4787 142/5811
33-34 weeks 1.1 0.8 01 0.0559/5548 .39/4787 39/5811
< 33 weeks 1.5 1.0 0.5 0.001
81/5348 51/4787 29/5811
Reduction ot preterm births ihve-brrthi time perio4 and by duration 01 gestation sun e last 1.81P. The observed redut non in imeterm births is al onebirth tOr the total preterm figure's, and is one halt tar the most dangerous preterm births des+ than 3 3 weeks,
Table 6.2Transfers to a Neonatal Intensive Care Unit
1971-74 1975-78 1979-82
33 weeks 38/81 27/51 12/29
33-36 weeks 15/218 17/141 17/181
> 37 weeks 58/5548 17/4787 22/5811
The numbers at transfered babies tsere signitie antiv rechrced for termlubies a, st as far the less than ;1 weeks birth babres. The prep it-
lion at transfers t ompared to preterit) birth was not redue-ed, the recicie -turn was only possible by the eftx rease in early preterm births.Numbers of days of StaV in the intensive c-are unit rat Strasbourg reterralcenter-I or in the neonatal pediatric ward in liagUNTall hospital tarIvbies born bethre 15 It evils, atter exc fusion or hospitalizations due to
malfarmatran .N the r/h/tor ( 16r 1,000 birthsr
Emile Papienlik et al.
Table 6.3Days of Hospitalization Related to Preterm Delivery
1971-.74 1975-78 1979-82 P Value
NICLI 425 296 182 0.001
Strasbourg
Neonatalpediatricward
4:37 320 2 23 0,001
Haguenau
Thu number at dat s needed tar hospitalizaturn related to preterni deliten bias significantly reticle ed tor transferee! babies to NK.0 and to thelex al pediatric cvard.
Adc.ances in the Prevention of Low Birth Weight
Table 6.4Neonatal Deaths Per Thousand Live Births
1971-74 1975-78 1979-82 P Value
0/00 8.3 6.5 3.1 0.00146/5548 31/4787 18/5811
Standardized 8.3 7.9 5.0rates andconfidenceinterval
48/96 30/76
The upper line shows the observed figures of neonatal deaths amonglive births by study period. The lower line depicts the figures obtainedafter standardization, as if the distribution of births by gestional agewould not haw changed in the second or third study periods, and withweek-specific mortalib rates ut these specific periods.
Table 6.5Rates of Preterm Births, by Risk Factor,
by Period
1971-74 1975-78 1979-82
Previous 12.7 12.5 12.3preterm 52/408 31/248 33/269
No previous 4.3 3.2 2.9preterm 124/2868 71/2247 88/3008
Previous 10.8 13.2 8.9still-born 7/65 7/53 7/79
No previous 5.3 .3.9 3.6still-born 169/3211 95/2442 114/3198
Height 8.2 7.8 6.3< 1.52 m 19/232 1 7/2 19 16/252
Height 5.6 4.0 3.8> 1.52 m 272/4871 179/4439 209/5478
Weight 7.5 5.4 5.3< 48 kg 50/668 35/645 41/777
Weight 5.5 4.2 '3.8
> 48 kg 245/4489 164/3944 186/4951)
76
PValue
4-5
0.01
N.S.
0.001
N.S.
0.001
0.001
Table 6.6Rates of Preterm Births, When a Risk Factor was
Observed or Not Observed
1971-74 1975-78 1979-82 P Value
Age less than 7.3 6.5 6.0 N.S.21 years 70/961 52/801 49/806
21-35 years 5.4 3.9 3.6 0.001217/4172 146/3770 177/4851
> 36 years 6.7 5.5 5.6 N.S31/461 10/181 10/180
Bleeding in second trimester
yes 18.2 20.6 14.3 N.S27/148 20/97 18/126
no 6.2 3.9 3.8 0.001120/1931 108/2804 164/4371
Bleeding in third trimester
yes 17.1 11.8 23.0 N.S24/140 8/68 10/87
no 5.3 4.0 3.6 0.001179/3392 159/3967 194/5429
Table 6.7Rate of High-Risk Factors Among Pregnant
Women by Study Period
1971-74 1975-78 1979-82 P ValuePrevious 12.5 10.0 8.3 0.001preterrn 428/3418 259/2604 280/3357
Previous 2.0 2.1 2.4 N.Sstillbirth 69[3418 54/2604 81/3357
Height 4.6 4.9 4.5 N.S152 cm 242/5292 236/4807 263/5819
Height 12.9 14.1 13.6 N.S48 cm 688/5.336 664/4721 790/5818
Age 21 years 17.4 17.1 14.1 0.0011014/:311 341/4918 839/5948
Age 35 years 8.4 4.0 3.1 0.001488/5811 196/4915 187/5948
Bleeding 7.1 3.3 2.8 0.0012nd trimester 151/2134 99/2961 126/4514
Bleeding 3.9 1,7 1.6 0.0013rd trimester 143[3630 71/4122 88/5572
Decrmse and Rise in Rates Preterm Delireries-Ilaguenau Prenatal Study. 1971-1988
A
Interventions
Table 6.8Change in Prenatal Care and Preterm Birth Rate According to Parental Educational Level
School attendance
2
3
1
2
3
1
2
3
1
2
3
1
2
N : numbers ot pregnant 1.somen In school
attendam 0 group
A : mean number of prenatal isits at the outpationt clinic (4 the obstctru departmt.nt.
1971-74
2794
1965
282
0.9
1.5
2.2
17.7
30.0
47.5
46.2
27 .7
10.6
6.8
5.6
3.7
1975-78
2975
1640
377
1979-82 1983-86 P Value
3806
1 725
433
2984
2109
475
1.8 2.3 2.3 0.001
3.0 3.5 2.8 0.001
3.8 3.8 3.1 0.001
28.4 38.6 37.5 0.001
49.5 61.6 48.4 0.001
65.5 69.5 55.2 0.001
23.9 8.6 18.8 0.001
8.8 3.6 20.7 0.001
4.0 0.9 17.3 0.001
5.0 4.5 5.2 0.001
3.5 3.3 4.3 0.01
2.7 2.5 3.6
13 : proportion of f ?regnant Komen ernolledthe (nit Athent hnu of the ohstetnt aldepartment.
proonlum 01 pregnant w ()men not to/ .lowed at tlu. ohstetric al department.
: rates or preterm births by group and byperr(xl.
Figure 6.1
Regression Curve for Women by Group And Number of Preterm Deliveries (See Page 7 3)
.07 A
.06 -
.05 -
.04
.03 -
.02 -
.01 - A
e 13n
C H.1 F of;
I mei CO
SL hoohng
.1 0 .20 .30 .40 .50 .60
t'ear7 74 75- 781t9- 82 83-86F
t {11 ( 1+ 1)
4 Lfv" 0.078-0.074Nr =p < 0 001
Emile Papiernik et al 77
S I
The West Los AngelesPrematurity Prevention Project:
A Progress Report
CALVIN J. I 1013EL, M.D.
Row. L. BEMIS, R.N.P.
G. Ros,s, MD.J. ROIWRT BRA( ;ONIER, M.D., PH.D.
Mc. >RAVE 13. 13EAR
BRNANT M. MORI
INTROIM1C11ON
During the 1970s, the I. Tnited States observeda dramatic reduction in perinatal morbidityand mortality. On the other hand, the inci-dence of low birthweight (LBW) births duringthis period decreased only 11 percent(approximately 1% per year).' Thus, the tech-nological advances in obstetrical and neonatalcare, which were thought to impact morbidityand mortality, did not significamly influencethe incidence of LBW. Since prematurity, amajor component of the low birthweightproblem, is now the leading cause of poor
Advances in the Prevention of Low Birthweigbt
pregnancy outcome, we must begin to devel-op strategies for prevention.
Beginning in 1970, we collected baselinedata from the west area of Los Angeles Countyto identify pregnancy-related problems. Usingthese data, we developed a risk scoring system,which was global in design, to idvntify preg-nancies at risk for neonatal morbidity and mor-tality. Between 1975 and 1979, our experienceshelped us recognize that our global approachto risk assessment needed to be redefined anddirected toward identifying patients at risk forspecific problems, such as preterm birth,intrauterine growth retardation, diabetes, andhypertension." Thus, over time we developed astrategy of prenatal care based on levels of risk,with special attention given to the preventionof specific problems.
Guidelines for the implementation of pro-grams for the preventkm of preterm birth camefrom two sources: (1) A risk assessment system,described by Papiernik in 1969, which formedthe basis for identifying patients at risk and fordeveloping prevention strategies:4 and (2) pre-liminary data subsequently published byIlerron et al. in 1982, which described the con-tent of a program thought to significantlyreduce the incidence of prematurity.'
These preliminary data generated tremen-dous interest in the prevention of prematurityin the linited States. Ompling these guidelinesand this interest, we developed a project forstudying prematurity prevention in our patientsat risk. The following provides a progressreport on that project.
DEVELOPMENT 01, A PREVENTION PROJECT
We believe that a prematurity preventionprogram thould include three major components.
Prenatal Care A),stemA well-organized prenatal care system is
an absolute requirement fin a prematurity pre-vention program. A new pn)gram encomraginga different philosophy and a change inprovider behavior will not be successful unlessthe system is prepared to provide a differenttype of prenatal care from that customarilyprovided in America.
Risk Assessment ,S:rstem
A task tOrce was established in 1978 by theWorld Ifealth Organization to set forth guide-lines for developing risk assessment systems formaternal and child health." This task force rec-ommended that risk assessment systems shouldbe developed from and tested on the populationto which they are to be applied prior to begin-ning intervention programs. The process is asfolknvs: First, a risk assessment system is devd-oped from rorospectively collected data and itssensitivity and specificity is determined. Next,the risk assissment system is applied prospec-tively to validate its sensitivity and specificity.The final step is to test the scoring system in aprospective type intervention study using a con-trol population to again test the scoring system'ssensitivity and specificity. Most risk assessmentsystems have not been properly designed andtested prior to instituting intervention strategies.
Data 5:ystentAn important component of Our preven-
tion project is our ability to manage the large
,r,1113 t)
80 Me West Los Angeles Prematurity Prevention Prolect: A Progress Report
amounts of data gathered from each patient.The source document for our program is thePOPRAS (Problem Oriented Perinatal RiskAssessment System) perinatal record.- Usingthe POPRAS record, we have developed anonline interactive computerized networkreferred to as PIDS (POPRAS Interactive DataSystem). This network links our west LosAngeles prenatal clinics with the scientific datacenter located at CedarsSinai Medical Center.
our project headquarters. and theHarborUCLA Medical Center. This system pro-vides us with the following:
1. Computerized risk assessment:
A randomization scheme for assignment ofintervention protocol;
3. An appointment scheduling system;
4 . Patient tracking and compliance checks;
5. Real-time reports:
6. Online hcispital data management; and
7. Rapid turnaround data management andanalysis.
FtNDING PREvEN*110N PROJECT
This project is funded by the Maternal andChild Ilealth Branch of the state of California.
Smin DEslo\
We were initially confronted with the taskof determining what types of interventionsshould he tested for preventing prc:erm birth.
Inten'entions
Our review of the literature suggested that theetiology of prematurity is most likely multifae-torial, yet stress appeared to be a central issue.In 198.1, we had proposed a hypothesis for theetiology of preterm labor where stress was feltto be a predisposing condition. We thereforedirected our attention toward interventionswhich reduced stress and interventions whichpromoted the maintenance of pregnancy. Thisapproach was in concert with the interventionsused by Papiernik.
For our prematurity prevention project, wedecided to test five treatment protocols forhigh-risk women. The precise study designalgorithm was previously published.9 The inter-vention protocols selected were bed rest, psy-chosocial support, and an oral progestin(Provera) matched with a placebo and a con-trol (education and nutrition only).
DEscumoN OF PROJECI'
The patients' risk status is determinedusing the PIDS program. Patients who haveone or more selected high-risk factors ate con-sidered high-risk patients and are randomizedinto one of Ilk. five interventions.' In additionto standard risk assessment, a detailed psy-chosocial history is taken but not used in theassessment of risk.
All high-risk patients receive educationabout preterm labor, signs and symptoms. whatactions to take if symptoms occur, and a class
detailing what to expect in the hospital. Inaddition, all patients receive extensive nutritioncounseling and support. Most patients deliver
at I larbort*CLA Medical Center and their data
liobel et al. 81S4
Advances in the Provention of Low Birthweight
are entered into the data system by labor anddelivery room nurses or data entry clerks.
THE PRELLMINARY REsi LTS
Preliminary results from 4,034 total deliver-ies occurring between January 1, 1979. andJune 30, 1986, are presented in table 7.1. Thesedata were previously published in abstractform." The importance of these preliminaryresults is to recognize that during the earlyphase of our study we had an apparent impacton the incidence of preterm deliveries, espe-daily those with very low birthweight infants (<1500 g). The very low birthweight infants arethe most costly to care for and account for themajority of preterm infants who are left withdisabilities or handicaps.
In addition, a preliminary analysis has beencarried out to assess the association of psy-chosocial stress with prematurity. This has also
been published in abstract form.0 In a retrospec-tive study of 359 women with preterm deliveriesmatched with a group of women delivering atterm, 4 factors were found to he significantlyassociated with preterm birth (see table 7.2). Inour prospective study from 1 January 1979 to 30June 1986, only three factors were determinedto be significantly associated with preterm birth(see table 7.2). These preliminary results suggestthat there may he certain psychosocial factorswhich could be used to facilitate the identifica-tion of patients at risk for preterm birth,
SUN1N1AW AM) FunRE DIREcnoN
As of May 1988, the \Vest Area Los AngelesPrematurity Prevention Demonstraticm Project iswell established and has completed its fifthyear of operation. The strategy of risk assess-ment, randomized application of specific inter-ventions. and computerized monitoring to
Table 7.1
West Los Angeles Prematurity Prevention Project Preliminar y Data
Baseline Prematurity Rate (percentage) Study Prematurity Rate (percentage)" (4,034 patients)
< 37 CompletedWeeks of Gestation
< 31 CompletedWeeks of Gestation
1979-1982(8,249 patients)
1982-1983(:3,108 patients)
ControlClink.s
ExperimentalClinics
ControlClinics
ExperimentalClinics
High Risk
Low Risk
11.74
5.04
9.92
4.58
8.54
4.77
5.70f
5.53
1,02
0.41
0.6P
0.40
Oata as vi 6/30 6(7. 4q",, dv reds.? compared %iith I 979-82 baseline.4 ?",, increaw ( orrpared rth 198244 bdr.e,line.
3 3', in( reawd compared tt ith Control Croftsto= .05.
S
40" de( reaw compared tt ith Control (slinics.
82 The West Los Angeles Prematurity Prerentiwt Pro/ect: A Progress Report
assess their impact on preterm birth appearspromising for providing new information tofacilitate our understanding of the problems ofpreterm birth.
Randomization of high-risk patients to spe-cific interventions will be completed as of 31December 1988, and the project will end byJuly 1989, at which time all patients enteredinto the study will have delivered. At that time,a final analysis of the overall effect of the pro-ject, as well as the effect of each specific inter-vention, will be determined. In addition, animportant part of the final analysis will includevalidation of our risk assessment screening toolin the control population to determine whetherit has maintained its original sensitivity andspecificity. Since psychosocial risk factors werenot originally included in our risk assessmentmodel, we will test the inclusion of certain ofthese factors into our scoring system to deter-mine whether they would improve the sensitiv-ity and specificity of our original tool.
Interventions
REFERENCES
1. Committee to Study the Prevention of LowBirthweight. (1985). Preventing low birthweight. In:
Institute of Medicine. Trends in low birtbuteight (pp.95). Washington, DC: National Academy Press.
2. Hobe!, C. J., Hyvarinen, M. A., Okada, D. M. and Oh,W. (1973). Prenatal and intrapartum high risk screen-ing. I. Prediction of the high-risk neonate. AmericanJournal of Obstetrics and Gynecology 117, 1-9.
3, Hobe!, C. J. (1979). Assessment of the high risk fetus.Clinics in Obstetrics and Gynaecology 6. 367-377.
4. Papiernik, E. (1969). Coefficient de risqued'accouchement premature. Presse Medicate 77,793-796.
5. Herron, M. A., Katz, M.. and Creasy, R. K. (1982).Evaluation of a preterm birth prevention program:Preliminary repoit Obstetrics and Gynecololgv 59, 452.
6. World Health Organization. (1977). Something for all
and more for those in greater nevd: A -risk approach"for integrated maternal and child health care. WHO
Chronicle 31,150-151.
7. Hobel, C. J. (1982). Development of POPRAS:Problem oriented perinatal risk assessment system.In: T. R. Harris and T. D. Bahr (Eds.), Me use ofcomputers in perinatal medicine (pp. 117-139).New York: Praeger Scientific.
Table 7.2Psychosocial Risk Factors Associated with Preterm Birth
Retrospective Study (Preliminary Results)
I. Mother working throughout pregnancy;
2. Patient not living with the baby's father;
3. Perceived problem or crisis near delivery; and
4. Perceived excessive stress during pregnancy.
Prospective Study (Preliminary Results)
I. Mother born in the United States;
2. Patient having had thoughts of hurting self orunborn baby; and
3. Patient having a close family member die duringpregnancy.
Calvin Hobel et al. 83
Advances in the Prevention of Low Birthweight
8, Bragonier, J. R., Cushner, 1. M., and Hobel, C. J.(1984). Social and personal factors in the etiology ofpreterm birth. In: F. Fuchs and P. G. Stubblefield(Eds.), Preterm birth: Causes, prevention, and man-agement (pp. 64-435). New York: MacMillian.
9. Hobel, C. J., and Bemis, R. L. (1986). The west areaLos Angeles prematurity prevention demonstrationproject. In: E. Papiernik and G. Breart (Fds.),Prevention of preterm birth (pp. 205-222). ColloqueINSERM, VoL 138.
10. Ross, M., Hobe!, C. J., Bragonier, R. J., and Bear, M.(1986). Prematurity: A simplified risk scoring sys-tem. American Journal of Pertnatology 3, 339.
11. Hobel, C., Bragonier, R., Ross, M., Bear, M., Bemis,R., and Mori, B. (1987, March). Significant impact:West Los Angeles premature prevention program.Abstract presented at the Society for GynecologicInvestigation 34th Annual Meeting, Atlanta, GA.
12. Ross, M. G., Hobe!, C. J., Bragonier, J. R Bemis, R.,and Bear, M. (1988, February). Psychosocial stress:Association with prematurity. Abstract presented atthe Society of Perinatal Obstetricians, Las Vegas, NV.
84 Me West Los Angeles Prenuiturity Prevention Pro/ea: A Progress Report
The South Carolina MulticenteredRandomized Controlled Trial to
Reduce Low Birthweight
HENRY C. HEINS, MD., M.P.H.
NANCY WEBSTER NANCE, C.N.M., M.S.N.
BRIAN 1 MCCARTHY, M.D.
CATHY NIELVIN PAM, PH.D.
)LIABORAMI G ROL T*
INTROD1'(:FION
South Carolina has one of the highest lowbirthweight rates (LBWR, < 2500 g) and verylow birthweight rates (VLBWR, < 1500 g) inthe United States. This dubious distinctioncontributes heavily to the state's excessiveinfant mortality rate, also one of the highest inthe nation.'
As other causes of infant mortalitydecrease, low birthweight assumes greaterimportance. In the United States, the LBWR is7 percent and accounts for 80 percent of theinfant deaths. Very low birthweight rates havenot changed significantly in the last 20 years.'
Adt.ances in the Pretvntion (ye Low Birthuvight
These small infants are not only at high risk fordying, but also for long-term morbidity, such ascerebral palsy and other neurological deficits.'
Several investigators have described inter-ventions to reduce preterm birth (< 37 complet-ed wtA:s' gestation) and low birthweight withinconsistent results.". This paper reports on amulticentered randomized controlled trial (RCT)of an intervention used in an attempt to reducethe LBWR in a group of women identified asbeing at increased risk for this poor perinatalOutcome.
Experience 1th two previous SouthCarolina programs provided the basis for thehypothesis tested in this study. One programused nurse-midwives in the adolescent clinicsof the Medical University of South Carolina(MUSC) to provide high-quality, comprehensiveprenatal care to adolescents. This program.although not an RCT. reported a reduction ofthe LBWR in these young women." The otherprogram used public health nurses to success-fully screen for high-risk patients in thestatewide high-risk perinatal program.'" Thestated hypothesis was that the low birthweightrate in the intervention group would be lessthan the LBWR in the control group.
o'reenrille Hospital Svsu,nt: Turn (,ailey, M.1).; kirriMc Own. LAM: Ray Re.milds. RA; Libby ,s,leelmall. RA;
McLeod Regional Medical Center: Steve Adams. .11 IX.Linda 14neson. kV Marilyn Polony. kV: Beth Turner,
lnirers.ity South Caroling: Ilenr) c.['COM %!.I) Nanc.V Nance, cAllf: lanna llliui.. c:VM:Patricia PcIpie, CAM: Barham Stone. CAM; R(ihnttStone. R.V; Rich/mut Momirial jankeM.D.; Barbara France. CAM: .Spartanbutg RoVonalMedical C:entcr. Hal Rubel. M.D.: Pat Rubel. R.V, Southc`..arolina Depannient vj Health and Environmental(.ontrol.. I.'ienise Ingram. .11.1).
Mim 101)5
Study PopulationWomen who attended state-funded prena-
tal clinics were eligible for randomization ifthey had a score of 10 points or greater on ascoring system using the risk factors ofPapiernik," later modified by Creasy.'2 Publichealth nurses in prenatal and the SpecialSupplemental Food Program for Women,Infants and Children (WIG) clinics administeredthe scoring index after being trained in its use.In addition, women who had a low birthweightinfant in their last pregnancy were eligible forrandomization. All women randomized had tohe free of known medical or pregnancy com-plications (i.e., hypertension, diabetes, renaldisease, or multiple pregnancy). Women withthese complications were eligible for thestatewide high-risk medical piligram and werenot rand(imized. If a randomized woman deyel-oped any of these complications during theindex pregnancy, she continued in the studyand also received treatment from an obstetri-cian for the complications.
'Random ..11/ocationA list of etnuputer-gcnerated randomized
numbers was sealed in sequentially numberedopaque envelopes. Upon identification of aneligible patient in the clinic, a central telephonenumber was called and the next envelope waschosen by a lay administrator not involved inpatient care. Patients were assigned to attendeither a separate low birthweight preventionclinic (study group) or to attend the regularhigh-risk obstetrical clinic (control group), Bothgroups had access to the WIG program, nutri-
SMe South Carolina Multicentered Randomized Onitrolled Thal to Reduce Low Birthuvight
tionists, public health nurses, and completefunding for prenatal care by the state healthdepartment. All women received intrapartumcare by obstetricians at the five regional centerscollaborating in the trial.
Sample SizeFrom the beginning of the study, it was felt
that it would be essential to pay for the prena-tal care of both the program and controlpatients. Funds were made available from mul-
tiple sources (e.g., the jobs Bill, theDepartment of Health and EnvironmentalControl, and the March of Dimes) for supportof approximately 1,600 total patients. The sam-ple size necessary to detect a change from aLBWR of 13% (the estimated low birthweightrate of the high-risk group) to 8% (the stateLBWR) at p 5...05 with a power of 90 was calcu-
lated to he 1,546 patients. The sample sizedetermination to test a similar hypothesis forthe VLBWR exceeded projected resources. Theoriginal sample size of 1,54> was, however.reduced to 1,435 women due to limitedresources extended over a prolcmged peric)d of
time.
hiterventionAs soon as possible after randomization
(within three weeks), the women in the pro-gram group vvere seen in the low birthweightpret.vntion clinic. An initial hour-long, one-on-one teaching session identified the women'sspecific risks with careful analysis of lifestylebehaviors, including substance abuse, nutritionstatus, stress, level of activity, and social sup-port. Patients were taught to recognize the sub-tle signs and symptoms of preterm labor and to
Interventions
palpate for contractions. They were given thephone number of the low hirthweight clinicnurse and the labor room and encouraged tocall with any problem. The return visits lasted20-30 minutes, with a review of all the initialteaching done each time. The same nurses ornurse-midwives saw the patient at one- to two-week intervals throughout the piegnancy. Agentle cervical exam to monitor possible cervi-cal change was done at each visit, with caretaken not to enter the endocervical canal.Recommendations to decrease physical activitywere based on the information gathered duringthe visits.
Intensive follow-up was done by the nurs-es/nurse-midwive.s on women who had mi.ssedappointments. The assistant study director madequarterly site visits to each of the centers toreview charts and monitor adherence to the pro-tocol. Case loads were assessed to ensure thatthe time allotted for each patient was adequateto maintain the protocol. In addition, staff fromall five regional centers met quarterly to discuss
problems and receive feedback on data collec-tion but without knowledge of perinatal out-comes in either the program or control group.
(msentThe Institutional Review Boar.; of the
Medical University of South Carolinadetermined that no f()rmal consent was neces-sary for women to enter the study since therewas no unusual or hazardous risk involved inprenatal care given in either group.
Interim Anal)wisAfter accumulating 800 pregnancy out-
comes, an interim analysis was conducted by a
Henry lkins et al. 89
Advances in the Prevention of Low Birthweight
team of three investigators who were notdirectly involved in the clinical management ofthe trial. All were independent of the study andthe institutions associated with it. The datareview group met in Atlanta on 26 March 1986,together with the principal investigator of thestudy and two consultants from the Centers forDisease Control.
The analysis concentrated on live birthssince they represented the denominator of thelow birthweight rate, which was the measureused in the hypothesis. The predictive powerof the screening tool for low birthweight andvery low birthweight was two to three timeshigher than for U.S. population rates. Therewas essentially no difference in the low birth-weight rate between the groups. Similarly, themean birthweight did not differ. The proportionof live births with birthweight less than 1500 g,
*however, was 2.1 percent in the program groupversus 4.2 percent in the control group. Theapparent effect of the program was to shiftbirths from the very low birthweight to themoderately low birthweight group, with noapparent shift from the moderately low birth-weight group into the normal birthweightgroup. The d'ita review group ccmcluded thatthere were no reasons for stopping the trial.encouraged its continuation, and kept theirreport confidential from the project staff.
RE.st.urs
The trial began on 1 .1uly 1983, and endedon 31 October 1987. During this period, 1,458women were randomized, 728 to the programand 730 to the control group (see figure 8.1). A
90
total of 17 women had multiple gestation, 11 inthe program and 6 in the control group. Sixwomen were not pregnant, three in eachgroup. Of the remaining 1,435 singleton preg-nancies, 34 resulted in abortions (22 programand 12 control.). There were 13 fetal deaths (3program and 10 control). Forty-two patientswere lost to follow-up (22 program and 20control). All of the above women were exclud-ed from analysis either because they did nothave a live singleton birth or because the out-come of their pregnancy was unknown. Allexclusions were validated by a blinded observ-er not connected with the study. The profile ofthe exclusions does not vary significantly withthe profile of those women included in theanalysis (see table 8.1).
A total of 1,346 women with live births andknown outcome, 667 in the program group and679 in the control group, were included in thereported analysis. The randomization processachieved comparability between groups formaternal race, education (in years), marital sta-tus, age (in years), risk scores, gravidity, andgestational age at randomization at clinic sites(see table 8.2). Nearly one-third of the patientswere less than 16 gestational weeks when ran-domized. Randomization of the patients to theprogram and control occurred evenly withineach hospital. One site (MUSC) accounted for30 percent of the patients (see table 8.3).
The group birthweight distribution for boththe program and the control groups is present-ed in table 8..4. There were no statistically sig-nificant differences, either in the very lowbirthweight rate or in the low binhweight rate,between program and control patients. Theodds ratio for program versus control patients
91 try^
The South Carolina Alulticentered Randomized Cwitmlled Trial to Reduce Lou' Birthweight
for LBW was 1.09 (95% CL, 0.8 1.4), and forVLBW was 1.15 (95% CL, 0.7-2.0).
Race was not considered in the hypothesis.hut interest as to whether intervention mayhave affected risk groups differently led to ananalysis by risk category and race. This post-hoc analysis suggested that black programwomen with a risk score of 10 or more had astatistically significant lower very low birth-weight rate than black control women (seetable 8.5). When the risk group""9 was exam-ined, no significant difference occurred in ges-tational age for either the total population orfor any one particular race (see table 8.5).
DISCUSSION
This randomized controlled trial withpatients in public health clinics demonstrated lit-
tle change in the low birthweight rate. Effective
interventions have been reported in somepatient populations, but have not been replicat-ed by other investigators. Thus, it is becomingapparent that low birthweight prevention pro-grams involving risk assessments which targetspecific populations for interventions do notbenefit all populations to the same degree. Itappears that the importance of specific risk fac-
tors for low birthweight and their correspondingintervention may depend on the populationstudied.
Papiernik first claimed benefit from assess-ment and early intervention in Francel' witheducation, cervical check. cerclage, and/ortocolysis. Creasy modified Papiernik's risk fac-tors in the pilot study in California." Papiernilehas also demonstrated general improvement
Henry Heins et al.
Interventicits
and acceptance of low birthweight preventionprograms by social class of the patient.
Main et al., in a randomized controlledtrial with inner-city patients, failed to detect anyincrease in gestational duration, but their studyhad a very small sample size (60 patients ineach group). They subsequently reported dis-appointment in the lack of sensitivity andspecificity in efforts to validate Creasy's scoringsystem.r
Moore described an educational programfor doctors and patients with much more suc-cess in private patients, but little change detect-ed in results in public health programs for lessadvantaged women.' Meis and Moore reportedthe etiology of preterm labor in the patientpopulation to be a factor in the success of th,.,irprevention program.19
The value of social support in improvingperinatal outcomes has been the subject ofstudies by Oakley' and Spencer.21. Differencesin bitthweight were found in South Carolina ina case control study of social support using aresource mother favoring this kind of socialsupport."
In a state where the ac.c.css to and avail-
ability of prenatal care for indigent women atrisk for low birthweight outcomes is an increas-ing concern, this study provides importantinsight as to the future direction that researchshoukl take. It appears from this RCT that nurs-es/nurse-midwives may have provided prenatalcare to a high-risk population with comparableresults, rather than better results (as stated inthe original hypothesis) when compared to out-comes of women provided care by obstetri-cians in high-risk clinics. This hypothesis.should be tested in a future study. The sample
9 91
Advahces in the Prevention of Lotv Birthuvight
size necessary to test this hypothesis is not pro-hibitive and the study would provide importantpublic health information.
The trend of black women in the programgroup to do better than black women in thecontrol group is even more encouragingbecause it suggests that some component oftheir persistently higher low birthweight ratemay be more amenable to this interventionthan their white counterparts. This observation,however, was not in the original hypothesis,and needs to be studied specifically by repeat-ing this RCT with that as the stated hypothesis.Possibly the difference in low birthweight/voylow birthweight by race was related to accessto quality prenatal care. Greenberg" noted agreater effect of prenatal care in those patientsat greatest socioeconomic risk. KorenbroVsreported a trend toward lowering of the lowbirthweight and very low birthweight rates witha package of quality care.
The unchanging rates of low birthweightpreterm births should be recognized as a veryserious maternal and child health problem.Despite improvements in infant mortality, theUnited States compotes unfavorably with devel-oped nations.= Our birthweight-specifk mortal-ity (i.e., survival within birthweight groups),however, ranks with the best in the world
Intensive care crisis intervention is seen asthe pinnacle of our achievement and a measureof our SUCCCSS. Lost from sight is the fact thatthe neonatal intensive care unit (NICU) shouldserve as a backup adjunct to prevention. Oneshould not let the previous strides made intechnological and expensive treatment over-shadow the small hut important steps that canbe made toward prevention. The expense asso-
dated with mounting further research is mini-mal compared to the savings in human andfinancial terms if a 50 percent reduction in theVLBWR is potentially achievable.
ACKNOWLEIXiMENTh
The authors wish to acknowledge theencouragement and scientific advice of IanChalmers, Director, National Perinatal Epidem-iology Unit, Oxford, England. We also wish toexpress our grititude to the March of Dimes,the South Carolina Department of Health andEnvironmental Control, and the Robert WoodJohnson Foundation for their support of thisreport.
ft.F.FEREN('ES
1. Kleinman, J. (1988). Natality Report 1983- /985tcumuLitive).11yattsville, N11): National Center HealthStatistics.
2. Wegman. M. E. (1987). Annual summary of vitalswtistics - 1986. Pediatrics 80,817-827.
3. Taffel, S. (1980). Factors associated with birth-u.eight ('nited States, 19 76 t Pub. No. (1)115). 80-1915). Hyattsville. MD: National Center for !leak')Statistics.
-+. NicCormick, NI. C. (1985). The contrthution of lowbinhweight to infant mortality and childhood mor-bidity. Neu England journal (y. Medicine 312. 82-90.
Shapiro. S.. McCormick. M. C.. starfield, B. H.,ltrischer, J. P. and Bross, 1). (1980), Relevance ofcorrelates of infant deaths for significant morbidity atone year of age. .-tinerican Journal (?I' ohstctrics andC.,:vnecaogy 136. 36$-373.
6. l'apiernik-Berkhauer, E. (1969). Coefficient de risqued'accouchement premature. Presse .ift;dicale 77.793-796.
Johnson. J. W. C.. Austen. R. L.. and .lones. C. S.(1975). Efficacy of 17-alpha hydroxyprogesteronecoporate in the prevention of premature labor.England journal cy'Afedicitw293. 675-680,
C).)
Neu,
92 Me South Carolina Muiticentered Randomized Controlled Trial to Reduce Low Birthweight
8. Herron. M., Rati. M.. and Creasy. R. K. (1982).Evaluation of a preterm birth preventkm program.Obstetrics and Gyrwcology 59, 452-45(,
9. Piechnik. S., and Corbett. M. A. (1985). Reducing kwbirthweight among socioeconomically high risk ado-lescent pregnancies. Journal (?1* Nurse MiduoijiTy 30.88.
10. Heins, H. C.. Miller. J. M., and Sear. A. (1983).Benefits of a statewide high risk perinatal program.Obstetrics and Gynecology 02. 29,4-290.
11. Papiernik-Berkhauer. E. (1980). Prediction of thepreterm baby, clinical Obstetrics and Gynecology 11.315-319.
12. Creasy. R. K.. Geimmer. B. A., and Liggins. G. C.(1980). System for predicting spontaneous pretermbirths. Obstetrics and Gyttecology SS, 692-698,
13. Papiernik-I3erkhauer. E. (19(9). Coefficient de risquecraccouchement prematme. Press(' Medicale 77.793-790.
14. Herron. M., Ratz. M.. and Creasy. R. R. (1982),Evaluation of preterm birth prevention program.Obstetrics and Gynecology 59,452-,50.
15. Papiernik. F... Bouyer, J.. and Yaffee. K.. et al. (1986).Women's acceptance of a perinatal birth preventionprogram, ilmerican Journal of Obstetrics andGyrwcohR1*155. 939-940.
16. Main. D. M.. Gabbe. S. C , Richardson. D.. et al.(1985). Can preterm deliveries be prevented?AnteriCcill lottrnal (?I Obstetrics and Gynecology 151.892-898.
17, Main. D. M., and Gabbe, S. C. (1987). Risk scoringfor preterm labor: Where do we go from here?Anler1Catt Journal cy Obstetrics and 6:171ecolugY I.789-.793.
18. Moore. M. L.. Meis. P. J.. Ernest. J. M., et al. (1986). Aregional program to reduce the incidence of pretermbirths. Journal Perinatology 210-22o.
19 Meis. P. J.. Ernest. J. M.. Moore. M. L.. et al. (198).Regional program for prevention of premature Nrthsin northwestern tic mb Carolina. Amencan jutirnalobstetrics and (,yttecolQqr 157,550-Sio.
20. Oakley. A., Macl'arlarw. A.. and (halmers, I. ( 0)82).Social class stress and repro)duction. In: A. R. Reesand 11, Purcell (Eds.). Disease environment. NewYork: John Wiley and sons Ltd.
Interventions
21. Spencer, H.. Morris, J., and Thomas, H. (1987). SouthManchester family worker scheme. HealthPromotion 2,1.
22. Heim, H. C., and Nance, N. 'W. (1987). Social sup-port in improving perinatal outcome: The resourcemother program. Obstetrics and Gynecology 69.263-266.
23. Greenberg, R. S. (1983). The impact of prenatal carein different social groups. Amerkan Journal ofObstetrics and Gynecology 1.43, 397-801.
2.4. Korenbrot. C. (1983). Risk reduction in pregnanciesof low income women: Comprehensive prenatal carethrough the Oh Access Project. Mobios 34.
25. lichrman, R. E. (1985). Preventing low hirthweight: Apediatric perspective. Pediatrics 107.8-H-849.
20. Lantos, J. (1987). Sounding board-Baby Doe fiveyears later: Implications for child health. NewEngland _Journal qic Medicine 31, 44-4-440.
Henry Heins et al. 93
1ntementions
Statistical Findings..The South Carolina Multicentered Randomized Controlled Trial
to Reduce Low Birthweight
Figure 8.1The South Carolina Multicentered Randomized Controlled Trial to Reduce Low Birthweight
Randomized Patients1,458
Multiple Gestations17
Exclusions
Nut Pregnant6
Program1 1
Control
Total Birth , Singletons1, 35
AlxrtionsFetal Peaths
47
Program25
(.ontrol22
Total Births, Singletons1,388
Live BirthsKnown Outcomes
1,346
Henry Heins et al.
Moved 1142
Program22
Control20
Program3
Control3
95
Advances in the Prevention of Low Birthuvight
Table 8.1
Selected Maternal CharacteristicsSouth Carolina Randomized Controlled Trial
Patient Analytical StatusMaternalCharacteristic*
Total SingletonsNumber Percentage
ExcludedNumber Percentage
Analytical GroupNumber Percentage
Total Participants 1,435 100 89 6.6 1,346 93.4
RaceWhite 759 52.9 41 46.1 718 53.3Black 648 45.2 34 38.2 714 45.6Other 6 0.4 0 0.0 6 0.4Missing 22 1.5 14 15.7 8 0.6
Education (Years)12+ 110 7.7 7 7.9 103 7.712 .392 27.3 19 21.3 .37.3 27.7<12 887 61.8 47 52.8 840 62.4Missing 46 3.2 16 18.0 30 2.2
Marital StatusMarried 633 44.1 33 :37.1 600 44.6Single 772 53.8 34 38.2 738 54.8Missing 30 2.1 22 24.7 8 0.6
Age (years)Under 18 249 17.4 4 4.5 245 18.218-34 1,069 74.5 32 35.9 1,037 77.1Over 34 43 3.0 1 1.1 42 3.1Missing 74 5.1 .)r
). 58.4 12 1.6
Risk Score0-9 126 8.8 8 9.0 118 8.810-19 1,056 73.6 58 65.2 998 74.120-29 176 12.3 9 10.1 167 12.430+ 43 3.0 3 .3.4 40 3.0Missing 34 2.4 11 12.4 1.7
Grayida1 264 18.4 7 7.9 257 19.1
2-4 915 6.3.8 56 62.9 859 63.85+ 231 16.1 1.3 14.6 218 16.2Missing 25 1.7 13 14.6 1.) 0.9
* No statistically significant difference occurred between program and control for any of th narameters above.
0 0
6 Statistical Findings: South Carolina Multicentered Randomized Controlled Mal to Reduce Lou. Birthweiglit
Interventkms
Table 8.2
Selected Maternal CharacteristicsSouth Carolina Randomized Clinical Trial
MaternalCharacteristic Number
Patient TypeProgram (P)
Percentage NumberControl (C)
Percentage
Total Participants 667 679
RaceWhite 310 46.5 304 44.8
Black 348 52.2 370 54.5
Other 5 0.7 1 0.1
Missing 4 0.6 4 .6
Education (years)12+ 55 8.2 48 7.1
12 183 27.4 190 28.0
<12 421 63.1 419 61,7
Missing , 8 1.2 22 3.2
Marital StatusMarried 300 45.0 300 44.4
Single 364 54.6 374 55.1
Missing 3 0.4 5 0.7
Age (years)Under 17 127 19.0 118 17.4
18-19 85 12.7 114 16,8
20-34 427 64.0 411 60.5
35+ 17 2.5 25 3.7
Missing 11 1.6 11 1.6
Risk Score0-9 61 9.1 5'1 7.5
10-19 490 73.5 508 74.8
20-29 85 12.7 82 12.1
30+ 18 2.7 27 3.2
Missing 13 1.9 10 1.5
Gray ida1 134 20.1 123 18.1
2-4 411 61.6 448 66.0
5+ 117 17.5 101 16.0
Missing 5 0.7 7 1.0
Henry Heins et al, 97
Advances in the Prevention of Low Birth weight
Table 8.3South Carolina Randomized Controlled Trial
Service Statistics (Live Births), Analytical Group
Year ofRecruitment
TotalNumber Percentage
ProgramNumber Percentage
ControlNumber Percentage
1,435 100.0 667 100.0 679 100.01983 125 9.3 62 8.9 63 8.819E4 405 30.1 194 28.0 211 31.01985 420 31.2 207 30.5 213 30.81986 371 27.6 191 28.0 180 26.3
Missing 25 1.8 12 4.3 11 3.3
Gestational Ageat Randomization(Onset of Care)
<12 81 6.0 29 4.3 52 7.712-16 247 18.4 114 17.1 133 19.617-20 252 18.7 132 19.8 120 17.721-24 251 18.6 128 19.2 123 18.125-29 313 23.3 188 28.2 125 18.4
>30 124 9.2 63 9.4 61 9.0Missing 78 5.8 13 1.9 65 9.6
Clinic SiteGHS* 180 13.4 95 14.2 85 12.5
MRMC 233 17.3 109 16.3 124 18.3MUSO 487 36.2 242 36.3 245 36.1RMH" 190 14.1 93 13.9 97 14.3SGHI 255 18.9 127 19.0 128 18.9
Missing 1 0.1 1 0.3 0.0
*Greenville Hospital System'McLeod Regional Medical Center'Medical University of South CarolinaRichland Memorial Hospital'Spartanburg General Hcspital
98 Statistical Findings: South Carolina Multicentewd Randomized Controlled Trial to Reduce Lou Birthuvight
Interventions
Table 8.4Birthweight Outcomes
South Carolina Randomized Clinical Trial (Live Births)
Patient Type
Birthweight Program (P) Control (C)
Group Number Percentage Number Percentage Odd Ratio (95% CL)C vs. P
TotalVLBW 24 3.6 28 4.1 1.15 (0.7-2.0)
LBW 103 15.4 111 16.3 1.09 (0.8-1.4)
NBW 540 81.0 540 79.6
Total 667 (100.0) 679 (100.0)
Table 8.5*Birthweight Outcomes
South Carolina Randomized Clinical Trial (Live Births)
Patient Type
BirthweightGroup
White
Program (P)Number Percentage
Control (C)Number Percentage Odd Ratio (95% CL)
C vs. P
VLBW 11 3.5 8 2.6 0.73 (0.3-1.9)
LBW 38 12.3 33 10.8 0.83 (0.5-1.3)
NBW 261 84.2 263 86.5
Total 310 100.0 304 100.0
BlackVLBW 12 3.4 20 5.4 1.6 (0.8-3.3)
LBW 64 18.4 76 20.5 1.25 (0.9-1.8)
NBW 272 78.2 274 74.1
Total 348 100.0 370 100.0
Risk Group 10-19
WhiteVLBW 6 2.4 5 2.0 0.83 (0.2-2.7)
LBW 27 10.8 24 9.6 0.86 (0.5-1.5)
216 86.7 221 88.4
Total 249 100.0 250 100.0
BlaikVLBW 6 2.6 17 6.7 2.85 (1.1-7.3)
LBW 40 17.0 46 18.0 1.35 (0.9-2.1)
NBW 189 80.2 192 75.3
Total 235 100.0 255 100.0
* Table 8.5 includes only white and black infants.
Hemy Heim et al. 9 9 99
A Prematurity Prevention Projectin Northwest North Carolina
PAUL J. MEIS, M.D.
PAUL A. Bt TESCI ER, PH.D.
J. M. ERNEST, M.D.
MARY Lou MOORE, R.N.C., PH.D.
ROBERT MK:I-11E11TM, P11.D.
PENNY SHARP, M.En.
INTRODUCTION
Premature or low birthweight (LBW) births area major cause of infant mortality and neonataland postneonatal morbidity." Rates of LBWand very low birthweight (VLBW) births arehigh in southern states of the United States andhave not shown great improvement over thepast decade.' An example of this lack ofimprovement is shown in the rates of LBWand VLBW births in northwest North Carolinafrom 1980 to 1985 (see figure 9.1).
Although the basic mechanism or cause ofmost premature births is not known, preven-tion strategies may be of some use. Papiemik'and Creasy' have described their experiences
Advances in the Prevention of Low Birthweight
with a system of risk assessment, patient educa-tion, intensive prenatal care, increased maternalrest, appropriate use of tocolytic drugs, andother methods which were successful inimproving birth outcomes. Papiernik'4 reportedsuccess with this program in a number of differ-ent populations in metropolitan France andMartinique; Creasy' reported success in patientsof a clinic in San Francisco. Recently, however,these encouraging reports have been temperedby results from randomized prospective trials ofthis risk assessment-educational model. Main"reported a lack of effectiveness in a small groupof patients in Philadelphia, and early reports ofthe multicenter March of Dimes trial have notindicated effectiveness in the patients studied.*
The purpose of this chapter is to report onour experience with a LBW or prematurity pre-vention project in northwest North Carolina.
MEM-10M
This project was implemented in the 20-county area in northwest North Caroiina consti-tuting Perinatal Care Region 2. This region is amixture of urban and rural counties withapproximately 21,000 births per year, approxi-mately one-fourth of North Carolina's totalnumber of births per year. The program wasbased on the principles of Creasy and includedthe following: Risk assessment and educationfor all patients, routine vaginal examination at26 weeks' gestation to evaluate cervical change,more intensive prenatal care for patientsthought to he at risk, and hospital care includ-
Morton, R. Personal communication.
ing tocolytic drugs when appropriate. The pro-gram was presented to private obstetricians andfamily physicians and to county health depart-ment clinics throughout the region. Details ofthe development and presentation of the pro-gram have been described elsewhere."
All health department clinics in the regionchose to participate in the project. A portion ofthe private physicians chose to participate, andthe remainder of the private providers chosenot to participate in the program. Since patientsof public health department clinics are low-income patients known to be a high-risk group,the results from these patients were excludedfrom the present evaluation and comparisonswere made between births of patients ofproviders who participated in the program andbirths of patients whose physicians chose not toparticipate. Using birth data obtained from theNorth Carolina State Center for Health Statistics,birth outcomes were examined for residents ofPerinatal Region 2 for 1985 and 1986, the firsttwo years of full project implementation. Birthsof less than 500 g were excluded from theresults, as were births to women who did notreceive prenatal care. Comparisons were thenmade between birth results of private patientsenrolled in the program and private patients notenrolled in the program.
RESULTS
In 1985 and 1986. 12,704 births occurred toprivate patients enrolled in the program and23,757 births occurred to women whose physi-cians chose not to enroll patients in the pro-gram. The results are shown, categorized by
102 A Prematurity Prevention Project in Northwest North Carolina
race, in table 9.1 and figures 9.2-9.5. Births list-
ed as "nonwhite" are almost entirely of blackrace, as very few other nonwhite births occurin this region. These results are shown as thepercentage of births less than 1500 g (VLBW),less than 2500 g (LBW), less than 38 weeks'(266 days) gestation, and less than 38 weeks'gestation and less than 2500 g (premature lowbirthweight EP-LBW) births).
The percentage of births less than 2500 gwas significantly lower for both white and non-white patients enrolled in the project comparedwith patients not enrolled in the project. Thepercentage of births less than 1500 g was lowerin patients enrolled in the project, but this dif-
ference did not reach statistical significance innonwhite patients, as the absolute number ofbirths was small. Premature births (less than 38wteks' gestation) were less frequent in non-white patients enrolled in the project. No signif-icant difference was observed for rates ofpremature births in white patients or for ratesof P-LBW births in white or nonwhite pdtients.
DISCI .NSION
Clear differences exist in birth results ofprivate patients enrolled in the program com-pared with those not enrolled. As all publicpatients in Region 2 were enrolled in the pro-gram. no similar comparison group exists.Evaluation of results in the public patients byother methods is under study.
The results of this study may be biased bydifferences in the characteristics of patients par-ticipating in the project compared with thosenot participating in the project. Although a
Interventions
greater proportion of the nonproject birthswere nonwhite or black, differences in birthoutcomes remained when these results wereexamined by race. An earlier evaluation ofLBW births in Perinatal Care Region 2, conduct-ed in 1985 by Buescher, used a multivariateanalysis. After correction for a number of riskfactors, including age, race, education, andmarital status, the relative odds ratio for LBWbirth to women not enrolled in the project was1.32 higher than for women enrolled in theproject.
Although better birth outcomes occurred tononwhite or black women enrolled in the pro-ject, the rates of premature or LBW birthsremained roughly twice as high for nonwhitebirths as for white births. This disparity wasseen both in project and nonproject births.
The difference in the apparent success ofthis prevention model in this project (and inthe reports of Papiernik and Creasy) comparedwith the reports of Main and the March ofDimes trial may be related to characteristics ofthe populations involved. We have previouslyreported that LBW births in patients of a publichealth department clinic are frequently relatedto premature rupture of the fetal membranes,impaired fetal growth, or medical problems.'"Prevention strategies are unlikely to affect theoutcome in pregnancies with these problems.In contrast, in our previous study, privatepatient LBW births were more likely to be relat-ed to idiopathic premature labor, which may befavorably influenced by prevention techniques.Thus, the relative success or effectiveness ofthe Papiernik-Creasy prevention model maydepend in part on the characteristics of thepopulation for whom it is employed.
Paul J. MeiS et cii. 103102
Advances in the Prevention of Low Birthweight
Although a difference was seen in the ratesof LBW births between women enrolled in theproject and those not enrolled, no differencewas seen in the rates of P-LIAV births. Kessel etal. have previously found that national trendsin P-LBW birth rates may be more resistant toimprovement than those of term LBW birthrates."
The apparent improvement in the rates ofVLBW births to patients enrolled in this projectis encouraging. These births arc the most likelyto have adverse outcomes," and even modestreductions in the rates of VLBW births can havesignificant social and financial impact."
In summaiy, the results of this project indi-cate that this prematurity prevention model canbe utilized in private patients in a southernstate. Improvement in LBW rates occurred inboth white and black patients of privateproviders who utilized the program,
AMMAN/El ximENT
The authors are indebted to MichaelPatetta of the North Carolina Center for HealthStatistics for his assistance in collecting perti-nent data from birth certificate information.
REFERENCES
I. Lee, K., Paneth. N Gartner. L M., and Pearlman, NI.(1980). The very low birthweight rate: Principal pre-dictor of neonatal mortality in industrialized popula-tions. Journal qf Pediatrks 97, 759-764.
2. Skeoch, C.. Rosenberg, K., Turner. T., Skeoch. H.,and McIlwaine. G. (1987). Very low birthweight sur-vivors: Illness and readmission to hospital in the first15 months of life. British Medical Journal 195,579-580.
3. National Center for Health Statistics. (1984). Advancereport on final natality statistics, 1982. NCHS MonthlyVital Statistics Rcpori 33(Suppl.), 6.
4. Papiernik, E., Bouyer. J., Dreyfus, J., et al. (1985).Prevention of preterm births: A perinatal study inIlaguenall, France. Pediatrics 76, 154-158.
5. Creasy, R. K., and Herron, NI. A. (1981). Preventionof preterm birth. Seminars in Perinatolgy 5, 295-302.
6. Main, D. NI., Gabbe, S. G.. Richardson. D.. andStrong, S. (1985). Can preterm deliveries be prevent-ed? American Journal of Obstetrics and Gynecology151, 892-898.
7. Nleis. P. J, Ernest, J. NI., Moore. NI. L. Michielutte, R..Sharp. P. C., and Buescher, P. A. (1987). Regionalprogram for prevention of premature birth in north-western North Carolina. American journal qfObstetrics and Gynecology 157, 550-556.
8. Moore, NI. L.. Meis, P. J.. Ernest, J. NI., Michielutte, R..Sharp, V. Grover, C., and Hill, C. (1986). A regionalprogram to reduce the incidence of preterm birth.journal (il. Perinatology 6. 216-220.
Buescher, P. A., Meis, V J.. Ernest, J. NI., Moore, M.L.. Michielutte. R.. and Sharp. P. (1988). A compari-son of women in and out of a prematurity preven-ti(m project in a North Carolina perinatal care region.A nwrican Journal qf Public Health 78, 264-267.
10. Meis. P. J.. Ernest. J. M.. and Moore, NI. L. (1987).Causes of low birthweight births in public and pri-vate patients. American Journal of Obstetrics andGyrwcology 156, I 165-1168.
11. Kessel S S Villar, J.. I3erendes, H. W.. and Nugent,R. P. (1982). The changing pattern of low birthweightin the United States. Journal 4 the AmericanMedical Associatiori 251. 1978-1982.
9.
104 A Prematuray Prevention Project in Northut,st North Carolina
Inteiventions
Statistical Findings:A Prematurity Prevention Project in
Northwest North Carolina
Table 9.1
Private Births in Northwest North Carolina1985-86
Project Non-Project
Total Births 12,704 23,715
Percentage Breakdown:
X'
< 1500 g 0.75 1.33 25.19 < 0.005< 2500 g 5.94 7.32 25.06 < 0.005< 38 wks 9.54 10.71 12.09 < 0.005
P-LBW 3.83 4.11 1.67 NS
White Births 11,035 19,051
Project Non-Project
Total Births 12,704 23,715
Percentage Breakdown:< 1500 g 0.60 1.04 15.95 < 0.005< 2500 g 5.35 6.05 6.34 < 0.02< 38 wks 8.62 8.87 0.55 NS
P-LBW 3.41 3.52 0.26 NS
Non-Whitc-Births 1,669 4,664
Project Non-Project
Total Births 12,704 23,715
Percentage Breakdown:< 1500 g 1.74 2.1.5 1.57 NS
< 2500 g 9.83 12.09 6.21 < 0.02< 38 wks 15.58 18.55 8.07 < 0.005
P-LBW 6.58 6.56 0.00 NS
Paul Meis et at.
Figure 9.1
Rates of LBW and VLBW Births in NorthwestNorth Carolina*
1980 1981 1982 1983 1984 1985
Percentage rates of LBW (500-2500 g) births in north-west North Carolina are shown in the upper scale of thechart and rates of VLBW (500-1500 g) births are shownin the lower scale.
Figure 9.2
Rates of LBW Births Within the Project vs. Rates
Among Unenrolled Private Patients*
1980 1981
p < 0.005
1982 1983
p < att.?
1984 1985
Non-Whitep < 0.02
* Percentage rates of LBW (500-2500 gt births in privatepatients enrolled in the project (gray bars) are comparedwith rates of LBW births in private patients not enrolledin the project (white bars).
104105
Advances in the Prevention of Lou, Birthweight
Figure 9.3
Rates of VLBW Births Within the Project vs. Rates
Among Unenrolled Private Patients*
2.5
2
1.5
1
0.5
0
Project
fj Non-project
Total Whitep < 0.005
Non-White
* Percentage rates of VLBW (.500-1500 g) births in privatepatients enrolled in the project (gray bars) are comparedwith rates of VLBW births in private patients not en-rolled in the project (white bars).
Figure 9.4
Rates of Premature Births ( < 38 Weeks' Gestation)
Within the Project vs. Rates Among Unenrolled
Private Patients*
20
15
10
5
II Project
1:1 Non-project
Total Whitep < 0.005
Non-White
* Percentage rates of premature births ( < 38 weeks' gesta-tion) in private patients enrolled in the project (graybars) are compared with rates of premature births in pri-vate patients not enrolled in the project (white bars).
Figure 9.5
Rates of P-LBW Births Within the Project vs. Rates
Among Unenrolled Private Patients*
7
6
5
4
3
2
1
111 Project
O Non-project
Total White Non-White
* Rates of premature low birthweight (P-LBW) births inprivate patients enrolled in the project (gray bars) arecompared with rates in private patients not enrolled inthe project (white bars).
105
106 Statistical Findings: A Prematurity Thevention Project in Northuest North Carolina
The Family Workers Project:Evaluation of a Randomized
Controlled Trial of a PregnancySocial Support Service
BRENDA SPENCER, PH.D.
INTRODIJCTION
The Short Report, published in 1980 by thehouse of Commons Social Services Commit-tee highlighted widespread variations in peri-natal health among different areas of thecountry. Birthweight is acknowledged to beone of the best available indicators of perinatalhealth,' and, using this indicator, theManchester region compared badly with thecountry at large. Here, 10.2 percent of all new-born infants weighed less than 2500 g, com-pared with a figure of 7.3 percent for Englandand Wales as a whole.'
Low birthweight arises as a consequenceof premature onset of labor or retarded fetalgrowth, and is more commonly found amongsocially disadvantaged women. Psychosocial
Advances in tbe Prewntion of Low Birtbweight
stress is one possible mechanism by whichsocial diyadvantage may give rise to poor preg-nancy outcome. Factors often cited as con-tributing to psychosocial stress are low income,inadequate access to and consumption of ser-1,ices, inadequate access to information, lack ofphysical effort, isolation, improper diet, poorliving conditions, ambivalence about the preg-nancy, and lack of social support."
While it is not possible for health servicesto reverse the social disadvantage reflected inperinatal statistics, it may be possible to com-pensate for it by the appropriate redirection ofprovision. This possibility prompted the institu-tion of the South Manchester Family WorkerScheme, which aimed to provide additionalsocial support for women at above-average riskof giving birth to a low :)iithweight baby. Itwas intended that this support would reducethe level of stress, thereby improving the well-being of the mothers-to-be and, ultimately, thehealth of their babies.
The role of the family worker is modeledafter that of the travailleuse familiale who hadbeen provided as part of the Maternal andChild Health Service in the Département ofSeine-Saint-Denis.' In Manchester, short-termfunding for family workers was obtained fromthe Manpower Services Commission Womenselected for the posts were hired on the basisof personality and general life experience; theyhad no formal qualifications in health or socialservices. The service adopted a client-centeredapproach, with the tasks of the worker varyingaccording to each client's situation. In practice,these ranged from providing help with obtain-ing state benefits, housing, shopping and otherdomestic work, and childcare, to promoting
110
appropriate use of health and social services,and community facilities; and generally actingas confidante.1'
The effect of intervention by the familyworkers was evaluated in the form of a ran-domized controlled trial. The trial was designedt*i evaluate the potential impact of such a ser-vice; therefore, randomization took placebefore knowing which women would eventual-ly accept a family worker. The "treatment" didnot consist of having the assistance of a familyworker, but in receiving the offer of a familyworker.
MEITIOD
The trial took place in two phases, fromJune 1982 to June 1983 and from June 1984 toSeptember 1985. The year-long gap betweenthe two phases was attributable to problemswith funding for the family workers. Anoverview of recruitment and participation inthe trial is shown in figure 1. Women eligiblefor the trial were identified following their reg-istering visit to either of the two maternity unitswithin the South Manchester Health District.Eligibility was determined according to criteriaindicating increased risk of giving birth to alow birthweight baby, and was mainly basedon national birthweight statistics' and on previ-ous research.'' Any woman satisfying at leasttwo of the entry criteria illustrated by an aster-isk in table 10.1 was included.
In the second phase of the trial the entrycriteria were modified slightly to increase therate of recruitment. Two new criteria wereintroduced: "Interpregnancy interval 6
1 7 The Family Workers Project
months" and "parity 3." Existing criteria werein some cases broadened; for example, whatwas formerly "previous perinatal death" wasextended to "previous fetal/infant death > 12weeks' gestation and up to 1 year of life", and"marital status single" was extended to includeknown cohabitees. Also, owing to the problemsin using the negistrar General's Classijkationof Occupations'" to classify women's occupa-tions by social class, the decision was made tocategorize certain occupations for women asbelonging to social classes IV or V. althoughthey are not officially classified as such (seetable 10.1).
As the family worker was intended to pkiya preventive rok, any women registering laterthan the 20th week of pregnancy wereexcluded. Intervention began as soon after reg-istering as could practically be arranged, Asianwomen were excluded from the trial in view ofthe lower birthweighi distribution of these eth-nic groups.:' Entry to the trial was also confinedto those living within the district and prede-fined adjoining areas. During the two periodsof recruitment the notes of all women attendingthe registering clinics were screened. In anaverage month of recruitment those eligible forthe trial represented approximately one-quarterof all women registering at the 2 clinics, givinga final total of 1,288 women. Allowing forwomen lost to follow-up and pregnancy loss, itwas estimated that each group would haveapproximately 600 cases; this would give a 76percent chance of detecting a difference inmean birthweight of 77 g between the twogroups. significant at the 5 percent level (two-tailed test) assuming a standard deviation of500 g. (It was estimated that, if the intervention
Interventions
was to be clinically of interest, a difference inmean birthweight of 77 grams between thegroups would need to be detected. This figureis derived from the difference in mean birth-weight between social classes I and II com-bined and III. IV, and V comllined); however,the chance of detecting a decrease in the pro-portion of low birthweight babies from 10.2percent to 7.3 percent, significant at the 5 per-cent level, would be less than 50 percent.
Following recruitment. participants wererandomly allocated to either the control orexperimental group using random numbertables. The women in the experimental groupwere then sent information describing thescheme, as illustrated in figure 10.2. and a let-ter indicating a date and approximat,f imewhen the family worker supervisor would call.On her visit, the supervisor explained thescheme in more detail, ascertained whether thewoman was ,nterested in having a familyworker and, if so. which of the workers wouldbe most appropriate. In the first phase, thescheme consisted of 10 full-time workers, plusa supervisor and project assistant; in the sec-ond, the equivalent of 20 full-time workerswere employed on a full- and pan-time basis,plus a supervisor, assistant supervisor, and pro-ject assistant (although during the last 3months the staffing was reduced to one-third).On average, a full-time worker would have sixclients, each of whom would receive one totwo visits per week (although. as the service
as flexible to the needs of each individual.some received more extensive help than thisand others received less). Information on birth-weight, together with other outcome data onperinatal health, as collected from the
Brenda Spencer 1 0S711
Advances in the Preamtion of Low Birthweight
women's hospital records. Results have beenanalysed (1 and X' tests) using the SPSS com-puter package."
RESUCIN
The population covered by the study isshown in table 10.1. As illustrated, the processof randomization was effective in ensuring com-parability between the two groups. A minimumof two criteria were sufficient to qualify for entryto the study, but approximately two-thirds ofthose recruited satisfied three or more criteria.
Of the women in the intervention groupwho were eligible to have a family worker, -11.4percent received help. As shown in table 10.2,there were a number of reasons why theremainder of the experimental group could not,or did not, accept the offer of a family worker,the most common being because enough sup-port was already available.
Of the 1,288 women recruited to the trial(see figure 10.1), outcome data were unavail-able for 52 women (25 in the control and 27 inthe experimental group). the most commonreason being relocating out of the area beforechildbirth (see table 10.3). The characteristics ofwomen for whom no outcome was obtaineddid not differ from those on wh(ml the finalanalysis was conducted. In addition, twins Vc 'ereexcluded from the outcome analysis, whichwas therefore conducted on 1,227 women.
Data on mean birthweight and gestation forlivebirths and stillbirths are presented in table10.4. No statistically significant differences werefound between the two groups. The experimen-tal group contained a slightly higher proportion
712
(53.1%) of male babies than did the controlgroup (47.7%). Therefore, in view of the fact thatmale babies are on average heavier than femalebabies, male and female birthweights are pre-sented separately in the tables and figures. Table10.5 presents outcome in terms of the proportionof babies in each group who were of low birth-weight, the proportion who were assessed assmall for gestational age, and the proportionwlm were born before term. Figures are alsoincluded on very preterm and very low birth-weight births. Being small for gestational agewas defined as those babies whose birthweightfell below the 10th centile on the birthweightgestation charts for males and females publishedby Milner and Richards." The odds ratios calcu-lated on the proportions and the associated con-fidence intervals demonstrate the similarity ofresults obtained from the two groups.
The outcome of all pregnancies in terms ofsurvival is shown in table 10.6. The proportionsof pregnancies resulting in a livebirth in thecontrol and experimental groups were 96.5 per-cent and 95.-i percent, respectively (stillbirthwas defined as any baby horn dead at or after28 weeks gestation). Of the livebirths, threebabies in the control group and one baby inthe experimental group died within the firstweek, the latter death being due to a lethalcongenital malformation. The largest discrepan-cy in the table is in the number of terminationscarried out for social reasons; however, exami-nation of the relationship between the stage inthe pregnancy at which these terminations tookplace and the timing of the visit of the familyworker supervisor did not suggest any connec-tion between the two.
Details on gestational age for all pregnan-
The Family W`orkm Prgject
cies, excluding those terminated by inducedabortion, are presented in table 10.7. There wasno evidence to suggest any differences in distri-bution of gestational length observed in the twogroups. (In order to obtain the best estimate ofgestational age, the woman's dates were used ifshe was certain of the date of her last menstrualperiod. For those who were uncertain, gestation-al age was based on assessment by ultrasoundscan if this was performed before the 20th weekof pregnancy or, where no such reading wasavailable, was taken from the woman.s uncertain
dates. A comparable proporti9n of women inthe control and experimental group were able toreport their dates with certainty.)
As two maternity units were involved inthe study, their entry and outcome data werestudied separately to check for any possiblediscrepancies between the two hospitals. It wasfound that approximately equal numbers oftrial participants had been recruited from eachcenter, and the profile of the two populationswas equivalent both in terms of characteristicsat entry to the trial and mean birthweight andlength of gestation of the baby.
DISCISSION
From the results it is clear that makingavailable the provision of a family worker ser-vice to the at-risk group as defined did not sig-nificantly influence either the overall meanbirthweight or the proportion of low birth-weight; nor was there any indication that eitherof the component elements of low birthweight,that is, preterm birth and fetal growth retarda-tion, were affected.
Inten,entions
As with many clinical trials, the size of thestudy population is perhaps not sufficient for anydefinite conclusions to be drawn, the final num-bers and standard deviation (550 g) providing a69 percent power of detecting the difference inbinhweight felt to be clinically important. Therewas, however, no indication in the results of anoutcome favoring the experimental group, and,indeed, the actual mean birthweight of the con-trol group was greater than that of the experi-mental group. Moreover, the 95 percentconfidence interval for the difference betweenthe mean binhweights does not include a differ-
ence of 77 g in favor of the experimental group.In addition to birthweight and gestation, a num-ber of other outcome measures were examinedwith no suggestion of any clinically importantdifferences between the two groups.
There are a number of possible ways inwhich these results might be interpreted, eachinterpretation having different implications interms of policy and future research. The firstconclusion which may be drawn is that thesocial support of a family worker given to awoman in pregnancy does not influence thelikelihood of her giving birth to a low birth-weight baby. The hypothesis that social supportcouki improve perinatal oukome, as measuredby birthweight, was developed on the basis of
a substantial amount of previous research. Ithas variously been suggested that stress andlack of social support give rise to adverse out-come and that intervention programs may miti-
gate their effect.' Our experience in
conducting the scheme strongly indicated thatfamily workers increased the subjective well-
being of their clients. Nonetheless, it could bethat the increase in well-being had no impact
13reilda Spencer 113
1 1
Advances in the Prevention of Low Birthuvight
on the development of the fetus, or that it wasinsufficient to effect any change. Perhaps forthose women at greatest risk the support of afamily worker was not able to counterbalancethe adverse factors leading to low birthweight;or their help was not intensive enough; or,beginning after the first trimester, it came at toolate a stage in the process.
Another line of interpretation concerns thetarget group on whom the study was conducted.It might be argued that the criterh applied result-ed in the selection of a group which was inap-propriate for the intervention. The group may besaid to he inappropriate either because just overone-half of those offered a family worker did notor were not able to accept, or because the entrycriteria did not adequately target those most like-ly to benefit from additional support.
\Xbmen eligible for the trial were not pre-screened to select those who would be morelikely to accept a family worker. Although a cer-tain level of nonacceptance was expected, sincenot all women would need additional support,the nonacceptance rate obtained in practice(SS.7%) was nonetheless higher than was feltdesirable and would obviously partially accountfoi the 'nonsignificant findings. Analyses weretherefore conducted between those womenwho did accept and those who did not acceptcombined with the control group. These (lid notshow any statistically significant differenct.sbetween the two groups, although. owing tothe uneven groupings, the chance of detecting adifference was unacceptably low at 52 percent,and, in addition, the groups were not compara-ble because some criteria were associated witha higher rate of acceptance than were others.There tended to he a greater acceptance of the
114
service among women who were eligiblebecause they had experience of previousadverse pregnancy outcome, or who qualifiedunder the "social class IV or V/unemployment"criterion. An analysis of variance to examine theeffect of these criteria on eventual birthweightoutcome showed that the weight of babies bornto women who entered the trial on the groundsof previous adverse pregnancy outcome wassignificantly lower than that of others born inthe trial (p < .001).
The criteria used resulted in the selection ofa population with a rate of low birthweight (live-births) of 8.6 percent The overall rate for SouthManchester during the years the trial took placewas only marginally lower than this figure.:".'"(Earlier published figures based on theManchester area as a whole arc higher becausethe Central and North Districts have higher rates.)Given that trial participants were identified asbeing at above-average risk, one might haveanticipated a higher rate of low birthweight rela-tive to the local population than was obtained. ltmay be that the exclusion of Asian women fromthe trial accounted in part for this discreNncy,but, even taking this factor into account, it doesappear that the criteria did not prove sufficientlystringent to identify those most at risk. Indeed,since during the second phase they applied toapproximately one-quarter of all those register-ing, they might he considered extensive.
Although psychosocial stress may give riseto the birth of a low birthweight infant, not alllow birthweight is attributable to this cause.Similarly, the risk factors adopted as criteriareflect both collectively and individually a com-bination of social and medical risk, not all ofwhich could potentially be reduced by social
111 The Fa may Wbrkers Project
support. The choice of low birthweight risk fac-tors as criteria directs the intervention to a groupwith a potentially higher rate of low birthweight;however, this may nonetheless result in an inad-equate targetting of those most likely to benefitfrom the intervention, since only a certain pro-portion of that risk could be mitigated throughsocial support. It may therefore be argued thatonly certain groups within the overall at-riskpopulation stand to benefit from additionalsocial support. Particular concern is oftenexpressed about the needs of adolescent moth-ers, for example. A subgroup analysis of womenless than 20 years old expecting their first childshowed a smaller proportion of low birthweightand premature babies in the experimentalgroup, but because of small numbers the resultswere statistically inconclusive.
The adoption of lc.)w birthweight andpreterm delivery as general indicators of peri-natal health is standard, but these are nonethe-less proxy measures and may not be entirelyappropriate for a trial of this kind. Very lowbirthweight is more strongly associated withadverse outcome, but, since it is a much rarerevent, its use as a measure would require largertrials than it is usually feasible to mount. Theoverview of research on social support duringpregnancy by Elbourne and Oakley (see pages203-224) reports that, in common with theManchester study, the two other trials in whichsocial support has been the primary interven-tion found a non-statistically significant fall inthe rate of very low birthweight infants. Evenafter combining results with such small num-bers, however, no conclusions can be drawn.
The trial was designed to be populationbased and, broadly speaking, to be conducted
Brenda Spencer
1 I_
Interventions
under conditions similar to those which prevailunder nonexperimental conditions. For this rea-son, entry criteria were based on routinelyavailable data from medical records, and noadditional prescreening took place. Thisapproach is similar in concept to that of thepragmatic trial as described by Schwartz et al.'"Given the findings of the trial, however, it is
apparent that simply providing a service andtargetting it on one-quarter of the populationdefined as at above-average risk according to amixture of broadly based criteria, will not affectthe incidence of low birthweight in that popu-lation. On the basis of our experience with theSouth Manchester Family Worker Scheme, wewould thervfore advocate that future researchbe conducted to ascertain whether social sup-port through family workers may be effectivefor certain groups within the overall at-riskpopulation. This would entail closer targettingof those most likely to benefit using only crite-ria indicative of stress, social isolation, or depri-vation, and including in the trial only thosewomen both prepared and able to accept thehelp of a worker. We would also recommendthat future research include outcome variableswhich assess maternal well-being in addition toclinical indicators of the baby's health.
REFF.RENCEs
1. liouse of Commons Social Services Committee. (1980.19 June). Perinatal and neonatal mortality. London:His Majesty's Stationety Office,
Chalmers. 1. (1979). The search for indices. Lancet 2,1063-1065.
3. Office of Population Censuses and Surveys. (1981a).()PCS Monitor. infant and perinatal monality 1980.Department of Health 3. 81/3.
115
Advances in the Prevention qf Low Birthweight
4. Office of Population Censuses and Surveys. (1981b).Birthuvight statistics 1980. Department of Ilealth 3,81/4.
5. Oakley, A., MacFarlane. A., and Chalmers, I. (1982).SOCial class, stress and reproduction. In: A. R. Rees,and H. Purcell (Eds.), Disease and the environment(pp. 11-50). Sussex. England: John Wiley and Sons.
6. Newton, R. W., Webster, P. A. C., Binu, P. S.. Maskrey,N., and Phillips. A, B. (1979). Psychosocial stress inpregnancy and its relation to the onset of premature
British Medical Journal 2, 411-413.
7. Newton. R. W.. and Hunt, L. P. (1984). Psycluisocialstress in pregnancy and its relation to low binhweight.British Medicallournal 288,1191-1194.
8. Hart. J, T. (1971). Inverse care law. Lancet 1,405-412,
9. Papiernik, E. (1984). Prediction of the preterm baby.anics in obstetrics and Gynaecology 11, 315-336.
10. Spira. N., Audras. E, Chapel, A.. Debuisson.Jacquelin. J., Kirchhoffer. C.. Lebrun, C., and Prudent,C. (1981). Surveillance A domicile des grossessespathologiques par les sages-femmes: Essai comparatifcontrOle sur 996 femmes. Journal de Gynecologic,Obstetrique et Biologie de la Reproduction I(). 543-548.
11. Wolkind. S.. and Zajicek. E. (Eds). (1981).Pregnancy: A psychological and social study. NewYork: Academic Press.
12. Brown, G. \V.. and Harris. T. (1978). Social origins (ildepression: A study o .1' psychiatric disorder in women(pp. ro--293 Lond()n: Tavistock.
13. Berkowitz. G. S., and Kasl. S. V. (1983). The role ofpsychomicial factors in spontaneous preterm deliver-v.Journal qf Psychosomatic Research 2'. 283-290.
14. Stein, A.. Camplx.11, E. A., Day. A.. McPherson. K.. andCoop:2r, P, J. (1987). Social adversity, low birth-weight. and prderm delivery. British Medical Journal295, 291-293.
15. Spencer. B. (1982). Family workers in Prance. SocialWork Service (30), .4-8.
16. Spencer. B.. Morris, J.. and Thomas. II. (1987). TheSouth Manchester family worker scheme. HealthPromotion 2. 29-38.
17. Bakketeig, L. S. Hoffman. IL J.. and Harley. E. E.(1979). The tendency to repeat gestational age andbirthweight in successive births. .1 ,nericanl01(rn1l rffObstenles and Gynecology13i. 1086-1103.
116
18. Eedrick, J., and Adelstein. P. (1973). Influence ofpregnancy spacing on outcome of pregnancy. BritishMedical Journal 4, 753-756.
19. Naeye, R. L. (1979). Weight gain and the outcome ofpregnancy. .4 ?rierican Journal of Obstetrics andGynecology 135, 3-9.
20. Office of Population Censuses and Surveys. (1980).
aamijication qf occupations 1980. IA mdon: HMSO.
21. Kurii, K. IL, and Edouard, L. (1984). Ethnic differ-ence in pregnancy outcome. Public Health 98.205-208.
22. Nie. N. C. H.. Jenkins, J, C., Steinbrenner, K..and Bent. D 11. ( I 975). Statistical package fin- thesocial sciences. New York: McGraw-Hill.
23. Milner, R. D. G., and Richards, B. (1974). An analysisof birthweight by gestational age of infants born inEngland and Wales, 1967-1977. journal if Obstetricsand 6:v1:act:Wow of Ow British Commonwealth 81,956-967.
2.3. Sokol, R. .1 Woolf. R. B.. Rosen. M. G., andWeingarden. K. (1980). Risk, antepanum care, andoutcome impact of a maternity and infant care project.obstetrics and Gynecology 56. 150-156,
Larson. C. P. (1980), Efficacy of prenatal and postpar-tum home visits (in child health and development.Pediatrks 66, 191-197.
2. Okis. D.. Tatdbaum, R.. Chamberlin, R.. and Roberts,J. (1980, 22 Oct()ber). 'The effrcts ty. a nurse home-vic-nation on impnwing the outcome of pregnancy: .4
preliminary rem.41. Paper presented at the AmericanPublic licalth Association Annual Meeting, Detroit.
27, Ri)s,, S. E. and Rutter. A. C. (1978. November).Healthiest babi.s possible: An nitreach program.Vancouver: \ancouver Perinatal I lealth Project.
28. Oakley, A. (1985). Sodal support in pregnancy: The"soft- way to increase birthweight. Social Science andMedicine 21.1259-1268.
)9, Office of Population Censuses and Surwvs. (1984. 31July). Infant and perinatal monality. Department ofHealth 3, 8-tr
30. Office of Population Censuses and Surveys. (1985. 13August). Infinu and pernuital mortality. Deparunentof' Health 3, 85. 3.
31. Schwartz. D Elamant, R.. and LdlGuch, J. (1980).Clinical trials. London: Academic Press.
11J The Fafrnily WOrken,..- Project
Interventions
Statistical Findings:The Family Workers Project: Evaluation of a Randomized
Controlled Trial of a Pregnancy Social Support Seivice
271 acceptors
No outcome 8
Figure 10.1
Overview of Trial
Randomization
Experimental Control
655 633
384 non-acceptors
N.No Outcome 19 No outcome 25
Twins 1 Twins I
262 334
626 women 601 women
1227 women
Twins 7
Brenda Spencer 117
114
Advances in the Pmvention of Low Birth Weight
Table 10.1
Study Population
Experimental Control
Age (mean, standard deviation)*Percentage less than 20 years
N = 655
StandardMean deviation
23.0 5.245.5
N = 6 3 3
StandardMean deviation
23.2 5.443.6
Weight (kg) 57.2 10.1 (12)* 57.4 11.2 (7)*
Height (m) 1.6 0.7 (20)* 1.6 0.7 (13)*
Weight II Height- 22.3 3.6 (30)a 22.6 4.0 (20)*
Number of cases for which information was unavailable
Number Percentage Number Percentage
Underweight* 247 37 222 35Parity % '0 415 63 398 63
1-2 165 25 163 26'3+ 75 12 72 11
Previous low birthweight (< 2500 g) 0 587 90 574 91
'1 61 9 52 851 8 1 8 1
Previous preterm birth (< 37 weeks) 0 605 92 578 91
1 42 6 47 7
>1 8 1 8 1
Previous spontaneous abortion 0 634 97 610 9612-28 weeks +1 15 2 22 4
51 6 1 1 1
Previous perinatal death 0 641 98 614 9728 weeks-lst week of life '1 14 2 19 3
51
Previous neonatal and post-natal 0 640 98 620 98deaths 2nd week-51st week life 1 15 2 12 2
'>1 1 1
Previous terminations for 0 646 99 619 98medical reasons 1 9 1 14 2
>1
118 115 The Family Workers Project
Interventions
Table 10.1 (Continued)Study Population
ExperimentalNumber Percentage
ControlNumber Percentage
Previous terminations for 0 590 90 568 90
social reasons 1 60 10 59 9
>1 5 1 6 1
Inter-pregnancy interval < 6 months' 27 5 24 4
Single/widowed/divorced/separated' 398 61 376 59
Woman's social class IV or V or unemployed 511 78 477 75
Partner's social class IV or V or unemployed 216 63 219 62
(Percentage of those with partner only)
Diabetic 2 1 1 1
Smoking (number of cigarettes per day) 0 326 50 313 49
1-5 69 11 59 9
5-20 247 38 243 39
>20 11 2 14 2
t entrY criteria
Women's social dass IV or V includes singleiwidoweddivorced women, nursinie aukil rit, shop'Sales ass tants and harrdressersind all unem-
ployed and unclassified women. Women unemplowd includes housewives and students.
Partner unemployed includes men in prigrn, self-employed, students and disabled/skk
Table 10.2Reasons for Non-Acceptance
Number Percentage
Not in when visited 91 13.9
No longer/never was pregnant 15 2.3
Moving out of study area 39 6.0
Employed ful -t i me 41 6.3
Not interested 55 8.4
Well supported 143 21.8
Total non-acceptors 384 58.7
Acceptors 271 41.3
Total 655 100.0
Brenda Spencer 1 10I 19
Advances in the Provntion uf Low Birth Weight
Table 10.3Outcome Information Not Obtained
Experimental Control
Reason Outcome Information Not Obtained Number Percentage Number Percentage
Moved 11 1.7 13 2.0
Transferred to hospital outside study area 5 0.8 3 0.5
No trace 3 0.5 3 0.5
Medical record unavailable 1 0.1 0 0.0
Not pregnant 7 1.1 3 0.5
Home delivery 0 0.0 3 0.5
Total 27 4.2 25 4.0
Table 10.4Mean Birthweight (Singleton Live and Stillbirths) And Length of Gestation
Experimental Control 95% ConfidenceInterval on
Standard Standard Mean differenceNumber Mean deviation Number Mean deviation difference p between means
Birthweight: All 602 * 3179.6 549.9 581 3214.5 553.5 -34.9 0.3 -97.8 to 28.0Female 282 3113.3 511,9 304 3146.3 522.4 -33.0 0.4 -90.5 to 24.5
Male 320 .3238.0 575.8 277 3289.3 577.5 -51.3 0.3 -143.8 to 41.2
Gestational age (days) 603 279.0 18.7 581 278.4 19.1 0.6 0.6 -1.6 to 2.8
Birthweight missing Itif fflJ' stillbirth
1 1
120 'Me Family Vtr`orkenc Project
InkTrentions
Table 10.5Proportion of Low Birthweight, Small for Gestational Age, and Preterm Babies
Number of low birthweight babies (<2500 g)
ExperimentalNumber Percentage
ControlNumber Percentage
Oddsratio
live births and stillbirths 54* 8.8 50 8.6 1.0
liyebirths only 52 8.7 49 8.4 1.0
Number of very low birthweight babies (<1500 g) 5 0.8 6 1.0 0.8
Number of small for gestational age** 61 10.0 59 10.2 1.0
Number of preterm babies (<37 weeks)** 60 10.0 54 9.3 1.1
Number of very preterm babies (<33 weeks)** 9 1.5 11 1.9 0.8
Birthweight missing tor one stillhirth lite and stillbirths
95% ConfidenceInterval onodds ratio
0.7 to 1.60.7 to1.60.3 to 2.50.7 to 1.50.7 to 1.60.3 to 1.9
Table 10.6Outcome of Pregnancy
Outcome of pregnancy
Termination for
ExperimentalN = 626
N
medical reasons 0.5
Termination forsocial reasons 11 1.8
Miscarriage: <12 weeks 3 0.5
>12 weeks 6 1.0
gestation not known 0 0.0
Stillbirth: antepartum 5 0.8
intrapadum 0 0.0
gestation not known 1 0.2
Live birth 597 95.4
Early neonatal death(1-7 days) 1* 0.2
Late neonatal death(8-28 days) 0 0.0
Survivors at I month 596 99.8
to lethal c ononital malformation
None due to lethal ccmgenital maltorm
Control= 601
1 0.2
1
6
11
1
0
0
1
0.2
1.0
1.8
0.2
0.0
0.0
0.2
580 96.5
3** 0.5
0 0.0
577 99.5
Table 10.7Categorization of Gestational Age,
Excluding Terminations torBoth Social and Medical Reasons
Number of Weeks'Gestation
0-24 (<174 days)
25-27 (175-195 days)
28-31 (196-223 days)
32-36 (224-258 days)
37-41 (259-293 days)
42+ (>294 days)
Tota
Experimental= 626
9 1.5
2 0.3
5 0.8
53 8.7
456 74.5
87 14.2
612 100.0
C;eslational age ts as cilia% ailable, tor one mi.(gestation was assumed to be <1.-4 (1.14s.
Control= 601
0/0
20* 3.3
1 0.2
7
44
443
84
599
1.2
7.4
73.9
14.0
100.0
Idge. for this case
Broicia Spencer 1211.1S
The Social Support andPregnancy Outcome Study
ANN OAKLEY
LINDA RAJAN, M.D.
INTRODUCTION
The Social Support and Pregnancy OutcomeStudy (SSPO) is a randomized controlled trialof a social intervention involving home visitsto women at high risk of giving birth to a lowbirthweight (LBW) baby. It was organized andcoordinated from the Thomas Coram ResearchUnit (TCRU), part of the University of LondonInstitute of Education, and funded by theBritish Department of Health and SocialSecurity (DHSS) for a period of three years,from September 1985 to August 1988. The trialitself ran from January 1986 to November1987. This chapter describes the backgroundand methodology of the study and presentssome of the initial findings. At the time of writ-ing, data analysis is still in progress.
1 n)
Advances in the Prevention of Lou, Birthweight
BAC:1(3RM IND AND AIMS oF Tin: STUDY
The SSPO study is an attempt to assess theeffect of social support in pregnancy on arange of pregnancy outcomes. An importantreason for undertaking the study was to investi-gate the potential effectiveness of social sup-port in preventing adverse clinical outcomes,particularly low birthweight. The study wasalso designed, however, to evaluate the possi-ble effects of social support on outcomeswhich are conventionally described as "softer"because they arc concerned with the psychoso-cial health of the mother.'
The general background to the study isthe concept that health is a social, as well as amedical, product.2.` Health is promoted notonly by medical services but by a healthy envi-ronment which enables individuals to makefull use of their own personal and socialresources in maintaining health. Theseresources include the social relationships andnetworks in which individuals are involved.The health-promoting effect of social supporthas received increasing emphasis in epidemio-logical and medical sociological research overthe last 20 years. There is now a good deal ofevidence that social support promotes healthin general.' There are also both observationaland experimental studies demonstrating therelevanci of social support to healthy child-bearing and childrearing. Having reviewedthese studies, it seemed important to try toadvance the debate concerning the effective-ness of social support in pregnancy by under-taking an intervention study using randomallocation to control both those factors knownto influence pregnancy outcome and those fac-tors whose effect is yet unknown. Since most
previous interventions in this field have provid-ed social support in addition to other servicessuch as health education, psychosocial coun-seling, or intensified clinical care, an importantaim of the SSPO study was to attempt to sepa-rate the provision of social support from othertypes of intervention.
The broad aims of the SSPO study were:
1. To conduct a randomized controlled trial(RCT) of a program of antenatal supportand interviewing by midwives in a sampleof women at high risk of delivering a LBWinfant;
l'o collect information on the social cir-cumstances, health, and self-perceivedpregnancy needs of such women; and
3. lb evaluate the relevance of data obtainedfrom (I) and (2) to the type of antenatalcare currently provided for high-riskwomen and to the future prevention ofLBW and other adverse pregnancy Out-comes.
The size of the SSPO sample was initiallycalculated in relation to the birthweight out-come on the basis of a comparison of meanbirthweight between intervention and controlgroups rather than of the proportion of womenin the two group.i giving birth to a LBW baby.The latter calculation would have demanded aconsiderably larger sample size. tIsing meanbirthweight as an outcome required a samplesize of 420 to show a significant increase of 150g in mean birthweight in the intervention group(power of 80%, p = 0.05). The actual achievedsample size was 509,
In addition to testing the hypothesis that
1 ,)
124 The Social Support and Pregnancy Outcome Study
a social support intervention in high-risk preg-nancy might be capable of increasing meanhirthweight, the SSPO study was designed totest the idea that social support might affectthe birthweight distribution, some birthweightgroups more than others, and particularlythose women who were socially unsupportedor whose obstetric histories indicated socialrather than biological reasons for previousLI3W delivery. Other initial hypotheses werethat the provision of additional social supportin pregnancy might affect maternal hospitaladmissions in pregnancy, the incidence ofhypertension and other physical morbidities,the length of labor, the use of analgesia, theincidence of instrumental delivery and othersuch procedures, and, in the postpartum peri-od, the incidence of maternal depression.infant and maternal morbidity and health ser-vice use, and the women's confidence asmothers.
SIt 'I )1* DING \
The study was catjed out in four centers,two in the Midlands and two in the south ofEngland. Women registering at these four cen-ters were eligible to enter the trial providedthey met the following eligibility criteria: A his-tory of at least one previous low birthweightdelivery unassociated with major congenitalmalformations; booking before weeks` ges-tation with a singleton pregnancy; and reason-able fluency in English. The first criterion waschosen in order to select an at-risk group sothat the chance of showing some effect of theintervention woukl be maximized. This strategy
Ann Oakley and Lynda Rajan
Interventions
appears to have been successful, judging fromthe obstetric and social characteristics of thefinal study sample, and was considerably easierto carry out than more complex risk scoringsystems. Women entering care very late in theirpregnancy were excluded from the study inorder to allow time for the intervention to begiven. Restrictkm of the study to English speak-ers was unfortunately necessary', as fundingwas insufficient to cover the cost of interpretingand translating for non-English-speaking ethnicminority mthers; however, four perceat of thefinal sample identified their ethnicity as Afro-Caribbean, Asian or -mixed," and five percentof the partners were described as belonging tothis category.
The social support intervention in theSSPO study was provided by midwives whoworked as research midwives on a part-timebasis for the duration of the trial, one in eachof the four centers. The chief reason for usingmidwives to provide the intervention was thatthe Department of Health, which funded thestudy, was concerned that the intervenersemployed should, for policy reasons. he repre-sentative of a group that already had an estab-lished role in maternity services. In the eventthe study demonstrated benefits of support inpregnancy, the policy implications would thenbe relatively easier to translate into practicethan if staff not linked with the maternity ser-vices had acted as sources of support. There isalso a sound historical and professional ratio-nale for seeing midwives as potential socialsupporters, as individual social care fOr w(nnenhas always constituted a key element in theprofessional ideology and practice of mid-wifery.'
121/25
Advances in the Prevention of Lou, Birtbuvight
Figure 11.1 shows the consent, riindom-ization, and data collection procedures used inthe SSPO study. From January 1986 to May1987, the four research midwives selectedfrom the case notes of all the women register-ing at the four centers those who fit the studyeligibility criteria. The aims and design of thestudy were then described to each woman.The midwife explained that, if a womanagreed to take part, she would not necessarilyreceive the social support intervention, butwould have a 50/50 chance of being in thecontrol group. The importance of random allo-cation was emphasized, as was the fact thatevery woman would receive standard antena-tal care, irrespective of study participation orallocation. The midwives also explained thatevery woman wno entered the study would beasked to complete a postal questionnaire sixweeks after delivery.
When a woman agreed to take part, themidwife telephoned TCRU for an allocationand then informed the woman to which groupshe belonged. Women allocated to the inter-vention group received the social supportpackage in addition to their normal antenatalcare; those allocated to the control group hadstandard antenatal care only. Obstetric datawere collected after delivery on all of thewomen participating in the study.* A postalinstrume:-.t was used to collect informationfrom the mothers postpartum, both to reducecost and to avoid the potential problem of themidwives who had provided the social sup-port intervention collecting information theymight wish to see establishing the benefits oftheir work. The two main disadvantages of a
postal survey are loss of qualitative material
1
and low response rates. The format of thequestionnaire used in the SSPO study enwur-aged women to write open-ended, unstruc-tured answers if they wished to, and manydid; assiduous follow-up of initial nonrespon-ders produced an overall response rate of 95percent.'
NATURE OF THE SOCIAL SUPPORT INTERVENTION
The WO study was set up to evaluatethe potential of nonspecific social support toimprove pregnancy outcome. As emphasizedabove, it was not a study of a health educa-tion, intensified clinical care or other directlyservice-related intervention, hut rather anattempt to provide and assess the value ofsupport to women in their own homes duringpregnancy in whatever way seemed appropri-ate to them. The SSPO intervention consistedof a minimum package of three home visits,ideally at 14, 20, and 28 weeks' gestation, plustwo telephone calls (or brief home visits forwomen without telephones) from the researchmidwives. The midwives were asked to try toprovide this minimum package for everyintervention group woman and to providemore than this if asked to do so by thewoman (providing the midwife's caseloadallowed this). In addition, the research mid-wives were provided with radiopagers, andintervention group women were informedthat they could call the midwife assigned tothem whenever they wanted to, on a 24-hours-a-day basis.
During the home contacts, the midwivesWere asked to do a number of things: First of
.1
126 The Social Support and Pregnancy Outconw Study
all, to listen to what women had to say; sec-ondly, to discuss with the women their preg-nancy needs and circumstances; thirdly, togive information when required; and lastly, tocarry out appropriate referrals to other agen-cies, such as social workers or hospital spe-cialists. To provide a structure for theinteraction between the research midwivesand the women they were supporting, threesemistructured interview schedules were avail-able, and normally used. A portion of eachhome contact was tape-recorded to generate abasis for comparing the midwives with oneanother, and also to provide some qualitativedata for the analysis of the study results. Aftereach contact with a woman in her interventiongroup, the midwife completed a short datasheet on which she assessed the woman'sneeds, her state of mind, and the type of helpgiven, if any.
Table 11.1 gives some guidance as to howthese specifications for the interventionworkcd in practice. The home visits were car-ried Out at approximately 18, 2,4, and 30weeks, somewhat later than planned, duelargely t-.) the women registering to hospitaland thus being recruited into the trial laterthan amicipated. Twenty-five percent of the
Interventions
women received less than the minimum socialsupport package (normally because they deliv-ered early) and 70 percent received more thanthe minimum package. 11,1ore than one-half ofthe intervention women were referred by theresearch midwives to health professionals atsome stage in their pregnancies, and one-quarter were referred to welfare agencies; onein five women did not receive referrals of anykind. Information about the specific healthtopics of smoking, alcohol, and diet wasrequested and given to 12 percent, 8 percent,and 24 percent, respectively, of the interven-tion group;- one-third of the women were notgiven any lifestyle information at all. Theresearch midwives were provided with guide-lines as to how to respond to specific topics inorder to standardize the type of informationgiven. Throughout the trial regular monthlymeetings were held in London and attendedby all of the midwives. These meetings serveda number of purposes, including facilitatingthe standardization of the social support beinggiven and allowing the research midwives todiscuss the inevitably stressful nature of thework involved in giving support to womenwith large numbers of social and obstetricproblems.
* .e.:scept ji.rr tuy) teho Mot,ed away during the study and could not be traced.
t Particular thanks are due to Sarulra Stonepr this,
5 The interview ,7chedule5 were used partly as a roult of experience (il. the Perth Social Support and Preventhm ofPreterm Labour Thal. in which it was iinind that sometimes contvrvations between research midwives and interven-tkni ,e;roup u,omen did not easily get ol:f the ground. due to lack of an ot,ert rationale, Me PrridWities in the SSPO study
were asked not to use the interview schechtles when they.felt it ilyis awkward or inadvisable to do so. It is important tonote. botilTer; that interviewing. as used in social Science research. IS (Ow everienced as a Suppollive eXereise by
interlieu'ees.""
Flirtber analysis of data penammg to these important issues will be carried wit and published elsewhere,
Ann Oakley and Lynda Raftm I '7
I 2 ;*,'
Advances in the Prevention of Lou' I3irthweight
Mil: SAMPLE
Figure 11.2 shows the SSPO sample.together with the pregnancy outcomes. Of the510 women who agreed to take part in thetrial. 256 women were randomized to the inter-vention group and 254 to the control group.One intervention group woman proved to havebeen incorrectly entered; two women, one ineach arm of the trial, moved and became inac-cessible to the study, Five women were carry-ing twins which were not diagnosed until afterrecruitment to the trial; these women wereexcluded from the main analyses, as the SSPOstudy was mounted as a trial of social supportin singleton pregnancy. Equal numbers ofwomen in the intervention and control groupshad terminations and spontaneous abortions.There were three stillbirths in the interventiongroup, three intrapartum stillbirths associatedwith abruptio placentas and one antepartumstillbirth due to placental insufficiency at 36weeks (weight of 1,760 g). There were 240 livebirths in the intervention group and 243 in thecontrol group. After allowing for five neonataldeaths, 238 intervention group and 240 controlgroup babies remained at the end of the studyperiod.
Table 11.2 shows the comparability of thetwo groups at entry to the trial. There Was nodifference in mean gestation at booking, themother's age, smoking status at booking. orparity. A slightly higher percentage of the inter-vention group women were married or cohabit-ing. Approximately three-quarters of bothgroups were categorized as working classaccording to the present or previous occupa-tion of the baby's father. One in five women
had partners who were unemployed. Aboutone-third of the women were themselvesemployed during pregnancy and similar pro-portions left school at or before 16 years ofage. These are indications that the sample wasdisadvantaged socially as well as being at highrisk obstetrically. There are no indications thatthe differences in pregnancy outcomesdescribed below which favor the interventiongroup might reflect the fact that this group isless disadvantaged socially than the controlgroup; if anything, the figures suggest that theOpposite may he the case.
RE.seas
13irthweight, (kstation, Law anti DelitoyTable 11.3 gives mean birthweight. The ini-
tial aim of increasing birthweight by 150 gproved to be overambitious, Taking singletonbabies who survived (the most important crite-rion from the mother's point of view), the dif-ference between the intefvention and controlgroups is 50 g. For live singleton births it is
about the same, but the difference is less whenthe stillbirths are included. It is interesting tonote that a recent overview by David Rush" ofdietary interventions in pregnancy ccmcludedthat the overall birthweight effect of these inter-ventions is in the range of 40-50 g.
From table 11.4 it can be seen that therewere fewer LBW babies in the interventiongroup. Table 11.5 shows that our interventionhad no effect on mean gestational age.
Tables 11.6-11.9 give the findings for thelabor and delivery variables we identified atthe outset as possible areas of effectonset
128 Tim Social Support and Pregnancy Outcome Study
of labor, mean length of labor, type of deliv-
ery, and analgesia/anaesthesia in labor. Thereare few differences here that are statisticallysignificant in the accepted sense (the tablescarry a p value where this is less than 0.1). Itis clear, however, that the direction of almostall of these results is in favor of the interven-tion group.
Maternal Physical Health and Medical CareFigures for some dimensions of the
women's physical health in pregnancy and useof medical care are given in Tables 11.10-11.12.
There is a suggestion in Table 11.11 dill' symp-toms of hypertension were less con,mon in theintervention group; these women also experi-enced fewer hospital admissions for threatened
preterm labor. The lower incidence of tirednessand insomnia in the intervention group may he
linked with the lower incidence of depression
in pregnancy (see table 11,16). There was nodifference in the incidence of medical diagnosesof intrauterine growth retardation or uses of cer-
vical suture and betamimetics (see table 11,11).Fewer women in the intervention groupreceived more than one ultrasound scan, and
fewer had antenatal cardicnocography. The moststriking finding in these tables is the incidence
of antenatal hospital admissions, which was sig-
nificantly lower in the intervention group.Table 11.12 provides data on the period
after birth. There were significant differ.ncesbetween the two groups. with 70 percent of
the intervention women, compared with 60percent of the control women, reporting theirown health as good or very good. In responseto the question of whether or not there arecontinuing physical problems as a result of the
Intementions
birth, there is also a difference between the
two groups.Finally, fewet intervention group women
made use of the health services (apart fromtheir routine postnatal check-up), and therewas a significant difference in the use of prima-ry health care.
Baby's ConditionTables 11.13-11.15 relate to the condition
of the baby. There was some differenceobserved in terms of Apgar scores. About the
same number of babies in each group wereresuscitated, but there was a statistically signifi-
cant distinction in the methods used.Intervention group babies were more likely to
have their airways cleared and/or simple suc-tion, and control group babies were more like-
ly to need oxygen or more invasive methods ofresuscitation (see table 11.13). Approximatelythe same number of babies in the two groupswent to the neonatal unit; however, there weresome differences in the care received withinthe neonatal unit, with control babies usingmore. Method of feeding at discharge from thehospital also tended to differ (see table 11.14).According to their mothers, intervention groupbabies were somewhat healthier than controlgroup babies. This appears to be reflected inthe figures for babies' health service use after
birth, which parallel the findings of the moth-
ers. A significantly greater proportim of theintervention grcnip babies were not health ser-vi,v users. About the same proportions werestill n or had been readmitted to the hospital,but intervention babies were taken back to thehospital somewhat less than the others (seetable 11.15),
Ann Oakley and Lynda Raja?! 129123
Advances in the Prevention of Low Birthweight
Psychosocial OutcomesInformation on psychosocial outcomes is
taken mainly from the postnatal questionnaire.According to table 11.16, the most statisticallysignificant difference from this point of viewbetween intervention and control group womenlies in the area of "worries" about the baby afterbirth Measures of perceived control over one'slife and depression (taken in the hospital afterdelivery) also favor the intervention group, asindeed do all of the outcome measures shownin this table. Table 11.17 demonstrates whatmight be regarded as a serendipitous effect ofthe intervention, which was to increase thedomestic participation of men in pregnancy andin the early weeks of parenthood.
CONCLUSION
This paper presents some of the initialfindings from an RCT of a social support inter-vention in high-risk pregnancy. On the basis ofthese data, it can be said that there is no evi-dence that this intervention did any harm to themothers and babies who received it, and agood deal of evidence that the effects werebeneficial. Tables 11.18 and 11.19 give somesummary measures of the way in which theSSPO intervention was seen by the supportersand by those supported. Listening was the sin-gle most valued characteristic attributed to theresearch midwives. As one woman remarked:
. . . This time I've been lucky. becauseI've been able to talk, and I mean I'vegot a lot of fears and anxieties in rnymind that I've been able to tell youabout, that I wouldn't have been able to
talk about to a doctor. . . . I have beenlooking forward to you coming. I'vebeen saying that woman is coming onWednesday. .
Research midwife, protesting:
"I'm not THAT WOMAN, Fm Susan."
"I mean I can talk about it to my friendsand that, but it's just that little bit of extraprofessional help. . ."
The help that the research midwives in theSSPO study were able to give has to be seen inthe context of women's ordinary experienceswith maternity services. In both Europe andNorth America, there is convincing evidencethat these services are frequently felt by moth-ers to be unsupportive and demoralizing.'"Poor doctor-patient communication was oftencommented on in the SSPO study, as it was bythis woman discussing a previous stillbirth:
. . There's a lot of questions you wantto ask . . . but you just can't. Everythingis rushed and you can't think (properly). . . and when you do ask them, youthink you're being silly because they tryto put you off. . . . When we lost the lastbaby, I had to go there for the postnataland we thought it was for the results ofthe postmortem . . . and (the doctor)said, 'Why have you come? What haveYou come for?' So I said, 'I don't know, Ithink I've come for the results of thepostmortem,' . . . and he said, 'Don'tyou know why your baby died then?'And I said, 'No,' . . . and he said, 'Ohwell, at 25 weeks, what do you expect?'and passed it off. . . .
2 t;130 The Social Support and Pregnancy Outcome Study
Many of these women had unresolvedproblems to do with their past experience ofgiving birth to a LBW baby; for some, it wasthe first time they had been given the oppor-tunity to discuss their feelings fully with any-one. It would thus seem that the therapeuticeffect of a social support intervention in thepregnancies of such women may have asmuch to do with the reconstruction of themeaning of past experiences as with the medi-ation of present experiences. It is salutary tonote (see table 11.19) that the importance ofthe supporters' help in these circumstancesmay often be undervalued by the supportersthemselves, who may feel skeptical about thepotential of the modest help they are able togive in counteracting the effects of the multi-ple social deprivation which affects the lives ofmany urban families in the 1980s.
ACKNOWLEDGMENTS
We are grateful to the DHSS for supportingthe SSPO study. Particular thanks are due toSandra Stone for preparing the manuscript, and toPenrose Robertson for his computing expertise,
REFERENCES
Oakley, A. (1983). Social consequences of obstetrictechnology: How to measure 'soft' outcomes. Birth
10, 99.
2, Dubos. R. (1960). The mimge 1-y. health, London:
Allen and Unwin,
3. McKeown. T. (1979). 7he mle rye medicine, Oxford:Basil Blackwell.
Cohen, S., and Syme, S. L. (1985) . Social supponand health. London: Academic Press.
Interventions
5. Berkman, L. F. (1984). Assessing the physical healtheffects of social networks and support. Review ofPublic Health 5, 413.
6. Oakley, A. (1985). Socill support in pregnancy:The 'soft' way to increase birthweight? SocialScience and Medicitw 21(11), 1259-1268.
7. Oakley, A. (1988). Is social support good for thehealth of mothers and babies? Journal qf Infertilityawl Reproductity Psychology 6, 3-21.
8, Elbourne, D., and Oakley, A. An overview of trialsof Social Support during pregnancy: Effects on ges-tational age at delivery and hirthweight. In: H.13erendes (Ed.), Advances in the pretwntion qf lOWbirthweight. (See Chapter X, p. X)
9. Oakley, A. (1984). Alternative perinatal services:Report of a pilot survey. In: I. M. L. Phaff (Ed.),Perinatal health services. London: Croom Helm.
10. Oakley, A. (1981). Interviewing women: A contra-diction in terms? In: H. Roberts (Ed.), Doing femi-nist research. London: Routledge and Kegan Paul.
11. Rush, D. (1989). Effects of changes in protein andcalorie intake during pregnancy on the growth of thehuman fetus. In: I. Chalmers, M. Encon. and MNC.Kierse (Eds.), afectity care in pregnancy and child-birth (Vol. I). Oxford: Oxford University Press.
12. Garcia, J. (1982). \Vomen's views of antenatal care,In: M. Enkin and I. Chalmers (Eds.), Effectivenessand satisfaction in antenatal care. London: SpasticsInternational Medical Publications.
13. Rothman, 13. K. ( 1982). In labor. Women andpower in the birthplace. New York: W. \V. Notion.
Ann Oakley and Lynda Rafan 131
127
Inten'entions
Statistical Findings:The Social Support and
Pregnancy Outcome Study
Figure 1 1.1
Consent, Randomizaiion, and Data Collection Procedures
Eligible women identifiedby research midwives from
case notes
Explanation of study andrequest for consent to
participate
Randomization(by phone to TCRU)
Intervention Group
Social Support Intervention
Obstetric case note data
Postnatal questionnaire(sent out 6 weeks after delivery)
Control Group
Obstetric case note data
Postnatal questionnaire(sent out 6 weeks after delivery)
Figure 11.2
Study Sample and Pregnancy Outcome by Assignment into Intervention and Control
Eligible and asked535
Agreed and Randomized515
r-
Intervention258
Excludtd1
Moved1
Twins3
Singletons251
i
Tops1-
Mistst,
Still Births3
Live Births240
iSWOON
2 38NNE)
2
Control254
Singletons251
Twins1-
Mo(ed1
Excluded0
Live Births243
Still Births0
Mkcs6
Tops7
Surviving240
NM)3
Ann Oakley and Lynda Rafan 133
1.23
Advances in the Prevention of Lou, Birthuright
Table 11.1Structure and Content of the SSPO intervention
Mean gestational age (weeks) at:
1st home contact 17.82nd home contact 24.03rd home contact 29.7
1st telephone contact 22.32nd telephone contact 27.3
Women who received:
minimum socialsupport package
less than minimumsodal support package
more than minimumsocial support package
percentage number
5 12
25 61
70 170
No referral of any kind 22 54
Referred to:
health professional(s) 52 125
welfare agencies 27 64
No lifestyle information given 34 81
Given information about:
smoking 12 28
alcohol 8 18
diet 24 58
Table 11.2Comparability of Groups at Recruitment to Trial
Intervention Control
Mean gestation (weeks) 15.7 15.6
Mother's age (years) 27.9 28.1
Percentage of group:
Under 20 years of age 4 4
Married/cohabiting 84 81
Working class* 77 72
Partner unemployed* 21 20
Employed during pregnancy* 33 35
Education completed at orbefore 16 years of age. *
31 31
Smoking at timeof enrollment
41 40
Parity 1.8 1.8
Mean number of previous LBW deliveries:1 85% 86%
11o/o 12O/0
3 + 40/0 2%
Total Numbers 255 254
' Information taken owl postnatal questionna fres.
Table 1 1.3Mean Birthweight
Intervention Control
Surviving singletons 2973.9 g 2923.1 g(N=238) (N=240)
Live singleton births 2956.3 g 2906.5 g(N=240) (N=243)
Singleton live and 2944.4 g 2906.5 gstillbirths (N=243) (N=243)
134 Statistical Findirigs: The Social Support and Pregnancy Outcome Study
Table 11.4Low Birthweight
Intervention Controlpercentage number percentage number
Live Singleton Births
17 42 21 52
83 198 79 191
100 240 100 243
< 2500 g
>2500 g
Total
Singleton live and stillbirths
< 2500 g> 2500 g
Total
19 45 21 52
81 198 79 191
100 243 100 243
Table 11.5Gestation at Delivery
Intervention
Mean gestational ageat delivery (weeks)
Percentage of deliveries:
< 28 weeks
< 37 weeks
Total numbers (all pregnanciesexcept for terminations)
38.2
3.6
19.3
249
Control
38.2
3.2
20.5
249
Spontaneous
Elective
Emergencycesarean
Total*
Table 11.6Onset of Labor
Intervention Controlpercentage number percentage number
74 180 68 163
22 53 26 64
4 10 6 14
100 243 100 241
*All singhlon live births and stillbirths for whic
Ann Oakley and Aynda Rafan
intormation ts'a5 available
Interventions
Table 11.7Mean Length of Labor
Intervention ControlFirst stage (hours) 5.3 5.4
Second stage (minutes) 20.4 21.1
Third stage (minutes) 10.0 7.2
Total* (hours) 5.7 5.9
"Based on Nz--202 (Intervention) and N.193 (Control), live and still-births, non-cesarean-delivered mothers, for whom information was
available.
Table 11.8Type of Delivery
Intervention Controlpercentage number percentage number
Spontaneous 81 197 75 182
Forceps/vacuumextraction
2 5 5 11
Cesareansection
17 41 21 50
Total* 100 243 100 243
'All singleton hve births and stillbirths for wh. 'hinfomtation was available.
Table 11.9Analgesia/Anesthesia in Labor
Intervention Controlpercentage number percentage number
None/Entonox 45 108 40 95
Pethidine 26 162 26 61
Epidural 11 27 16 39
GA 17 41 )8 43
Other 1 3
Total* 100 241 100 238
"All singleton
13J
e births and stillbirths for which information was available.
135
Advances in the Prevention of Low Bird:weight
Table 11.10Maternal Physical Health in Pregnancy
Intervention Controlpercentage number percentage number
Proteinuriaon own 24 51 27 64
with bp 8 8 11 11
Suspected 1UGR 21 51 22 54
Threatenedmiscarriage*
14 9 20
Admitted foithreatened pre-term labour
14 34 18 43
Tiredness* 78 180 83 187
insomnia* 22 50 27 62
Swollen ankles* 26 59 32 73
Mother's information
Table 1 1 .1 1
Medical Care in Pregnancy
Intervention Controlpercentage number percentage number
Cervical suture 4 9 4 13
Betamimetics .3 8 4 10
More than oneultrasound scan
73 178 77 187
Antenatal CTG 40 97 49 118p < .06
Mean numberof hospital visits
5.1 5.1
Admitted to 41 97 52 126hospitalantenatally
p < .01
Mean number of daysin hospital antenatally*
7.2 8.3
Base for calculation is number ot women admitted.
Table 1 1 .1 2
Maternal Physical Health After Birth
Intervention Controlpercentage number percentage number
Health very 70 161 60 133good/good p < ,03
Has no physical 59 69 46 52problems now (N = 118)* (N =113)*
No health service 40 93 31 70use (except forroutine postnatal)
p < .05
Still in/readmitt-ed within 6 weeksof delivery
4 8 4 8
Hospital visit(excludingroutine postnatal)
4 9 8 18
Visit to/from GP 29 67 39 88p < .03
Other 6 13 7 16
Based on S4 = 2 i0 (Intervention! and = 22O (Control) surviving single-ton babies whose mothers returned postnatal questionnaire andanswered relevant questions.
Number mho recorded any phyiica/ problem after the hirth.
Table 11.13Baby's Condition After Biah
Intervention Controlpercentage number percentage number
Apgar: <7 at 1 min 12 29 15 35<7 at 5 min 4 4 8
Not resuscitated 34 81 13:3 81
Cleared airways/suction only 64 100 54 83
0: by bag and mask/
other resuscitat;on 32 50 38 59
Endotracheal intubation 5 7 9 13
(N = 157) (N = 155)p .04 for resusc itahon method.
Based on singleton live births for whit h rntOrmation on Apgarscores/resuscitation was available.
Lii136 Statistical Findings: The Social Support and Pregnang Outcome Study
Table 11.14Baby's Care After Birth
Intervention Controlpercentage number percentage number
To neonatal unit 15 35 15 37
Mean number of days 9.6 17.1
Ventilated 3 8 5 13
Mean number of days 5.0 6.18
Supplemental 0: 3 8 5 13
Mean number of days 3.85 10.08
Totally intravenously/ 5 13 5 13
tubefUMean number of days 6.62 18.62
Breastfed at discharges 45 105 39 89
Rased on N = 240 (Intervention) and N = 24 (Control), all singleton livebirths. Means in each case based on number reiviving the prot (qua,:figures tAclude I baby who died in neonatal Lnit and 8 who are still in.
Survivors tor whom into, lation 2.30 Or Inter-tent ion
and N 226 tor Control).
Table 11.15Baby's Health After Birth
Intervention Controlpercentage number percentage number
No problems after 74 157 66 142
discharge p < .07
No healthservice use 35 81 24 54
p < .007
Still in/readmit edto hospital
7 16 7 15
Hospital visit 11 24 16 .35
Visit to/from GP 45 104 43 98
Other 13 29 13 30
Based on N = 2 4) dnrenentiow and N = 226 (('(filtrol1 %urvn ington babies whose miithers returned postnatal questumnarre an(1answered relevant questions.
Ann Oakkr and Iynda Ralan
Interventions
Table 11.16Psychosocial Outcomes
Intervention ControlpuLentage number percentage number
Enjoyed birth 66 151 58 130p < .08
'Excellent' relation-ship with baby now
64 148 60 134
Depressed in pregnancy 14 31 18 40
Depressed after 40 92 48 107
birth p < .08
Control over life 72 166 63 143
p < .08
Worried about 16 36 28 63
baby now p< .001
itiSed on N 230 (Intervention) and N = 226 (Control), mothers of sur-viving singleton babies who returned postnatal questionnaire andanswered relevant questions.
Table 11.17Partner's Support and Help
During Pregnancy, Birth, and After Birth
Intervention Controlpercentage nunther percentage number
Present during labor 78 177 76 171
'Took days off' very 30 56often/often 'to be withyou' during pregnancy
27 47
In pregnancy helped very often/often with:
shopping 85 187 77 161p < .01
other children 94 191 89 173p < .05
After birth helped very often/often with:
shopping 88 189 81 169p < .02
other children 97 197 92 178p < .05
Rjsefi on N = 2 JO );ntervention.) and N 226 ((ontrol) n7others whoreturned the postal questionnaire and answered relevant questions.
1 of) 42137
Advances in the Prevention of Low Birthiveight
Table 11.18Attitudes Toward the Intervention
Percentage of women who said it was important that:
She listened 80"/o
She gave advice
I saw her throughout pregnancy 56%
She gave information 56%
She was a midwife 33%
Total N 236
Table 11.19Value of Contact with Midwife in Pregnancy
Midwifeconsidered
Very/particularlyhelpful
Quitehelpful
Other/noinformation
herself* 13% 42% 450/
Womanconsideredmidwife' 50% 44% 6%
* Mean of 3 home contact assessments.
From postnatal questionnaire.
1 3
138 Statistical Findings: The Social Support and Pregnanq Outcome Study
Pretention of Preterm DeliveritBY Home Visiting System:
Results of a French RandomizedControlled Trial
BFAMICE BLONDEL, M.D.
josil IA LIAIX)
GRAM) 1312f:ART, M.D.
Ti IE HOME VISMNG SysITMIn France, the home visiting system is a part ofMaternal and Child Health Services, a programcreated after the Second World War to reduceinfant mortality and to promote the health ofmothers and children under six years of age.Through clinics and home visits, Maternal andChild Health Services provide health care,screening, and immunition free of cost. Theprogram is staffed by multidisciplinary teamsconsisting of doctors, midwives, nurses, nurs-ery nurses, and social workers.
During the 1960s. home visits were madeby nursery nurses to children only. A home
3 -1
Advances in the &mention of Low Birdmen*
visiting system for pregnant women was laterintroduced as part of a national program whichbegan in 1970 and which intended to reduceperinatal mortality and the incidence of handi-capped infants.' It included allocation of finan-cial resources to develop health services;educational programs; and regulations toimprove maternity unit equipment, prenatalcare, and the working conditions of employedwomen. The first domiciliary midwife beganvisiting pregnant women who were registeredat Antoine Beclere Hospital (Department of Dr.Emile Papiernik) in 1975. At present, between500 and 600 midwives make home visits inFrance.
The activities of the domiciliary midwivesare not defined precisely. In accordance withthe regulation, home visits should be offered totwo specific high-risk populations; Women whohave difficult life circumstances, and womenwho have pregnancy complications. For thefirst group, the home visiting system is consid-ered as a means of reaching women who arereluctant to use health services, improvingwomen's health habits, encouraging their rela-tives and friends to help them with housework,and establishing a link between the familiesand agencies employing home helpers. For thesecond group of women, the task of the mid-wives is to monitor pregnancy complications.Routine medical examination includes measure-ment of blood pressure, analysis of urine glu-cose and protein, measurement of fundalheight, monitoring of fetal heart rate and fetalmovements, and assessment of cervical state.Domiciliary midwives are not allowed to pre-scribe drugs.
High-risk women who receive home visits
also have routine visits at prenatal clinics.Home visits are free for every pregnantwoman.
The importance of the two basic activitiesof domiciliary midwivessupport and carevaries according to geographical area. In Paris,supervision of pregnancy complications is themain activity. In 1982, 80 percent of the preg-nant women received home visits because theyhad a threatened preterm labor; the other indi-cations were hypertension, intrauterine growthretardation, and multiple gestation. In Paris,each midwife works closely with one maternityunit and visits pregnant women who attend theoutpatient clinic of this unit.
BACKGROUND AND AIM OF THE Slum'
Two randomized controlled trials (RCTs)were conducted to study the effectiveness ofroutine home visits during pregnancy. Olds etal. evaluated a program of prenatal and postna-tal home visits among socially disadvantagedwomen in New York State. Nurses made anaverage of nine visits from the beginning ofpregnancy until delivery. Their activities includ-ed parent education, enhancement of thewomen's informal support systems, and linkageof the parents with community services. AFrench RCT was conducted during the sameperiod (1978-1980), but in this study womenwere visited at home when they had pregnancycomplications. Seventy percent of the womenwere at high risk for preterm labor.' Midwivesmade an average of six visits from the onset ofthe complication to delivery. Both of thesestudies failed to demonstrate any decrease in
13 5142 Prevention of Preterm Deliveries by Home Viisitini.; System
low birthweight and preterm delivery ratesamong the overall population, and 1 signifi-cantly higher perinatal mortality rate wasobserved in the intervention group in theFrench trial.
The publication of the French trial raisedseveral questions concerning the effectivenessof home visits and the benefits which could heexpected from this care system. The higher riskof perinatal mortahty associated with the homevisits could be explained by the inclusion crite-ria used in the trial: It was conducted only afew years after creation of the home visitingsystem, health benefits may have been overesti-mated, and some high-risk women should nothave been enrolled in the trial.
Moreover, against the French background.it may be difficult to show any health benefitsof home visits on pregnancy outcome in casesof threatened preterm labor because there is avery active management of this complication inFrance and we can expect a high level of careamong women visited at home and womenattending prenatal clinics.
If the chance to show a health benefit issmall, other effects of home visits should beconsidered (mainly, the cost of medical careand the women's view). Policymakers might heinterested in this medical care arrangement if itreduces the overall cost of care during preg-nancy, especially the costs related to hospital-ization. The choice of a pattern of medical careshould not be based on financial reasons only,however; the women's views of prenatal carearrangenlents also should be taken intoaccount. The aims of our study were to ascer-tain if a home visiting s}stem reduces the costof medical care during pregnancy and if the
Interventions
women's satisfaction with medical care isgreater when they have experienced home vis-its as compared with the usual care provided inthe outpatient clinics.
METHOD
The study design consisted of a random-ized controlled trial. The protocol and ques-tionnaires were prepared with the domiciliarymidwives who were working in Paris.
The study was restricted to women whohad threatened preterm labor because it wasthe main indication for prescribing home visits.The eligibility criteria were defined accordingto the usual practice in Paris: Women wererecruited if they had a moderate threatenedpreterm labor, and wonwn who received intra-venous betamimetics were excluded becausethese drugs are administered for acute threat-ened preterm labor in hospital exclusively.Women were enrolled between 2( and 36weeks of gestation.
Two groups of women were compared.Women in the intervention group were provid-ed one .)r two home visits per week; in addi-tion. women had access to the domiciliarymidwives by phone calls. Considering that theaim of this study was to assess the existinghome visiting system, the intervention was con-ducted by the present midwives without anyextra intervention. No home visit was providedto women of the control group. Women in bothgroups received routine prenatal care fromobstetricians or midwives at the outpatient clin-ics, Lmd they were hospitalized if necessary.
The women were allocated into the inter-
I3eatrice Blondel et al. 143
136
Advances in the Prevention of Low Birtbweight
vention group and the control group by ran-domization with sealed envelopes; this random-ization occurred in two different settings: (1) Inthe outpatient clinic, when a threatenedpreterm labor was diagnosed during a prenatalvisit; and (2) in tl .npatient ward, when therisk of preterm delivery of a hospitalizedwoman was decreasing and the discharge wasconsidered.
The sample size estimation was based onthe number of hospital days during pregnancy,which is the main part of medical cost beforedelivery. The number of women required forthe study was estimated to be 90 in eachgroup. This size should enable us to detect astatistically significant reduction of number ofdays in hospital equivalent to 50 percent of thestandard deviatkm; this standard deviation wasdetermined from observational studies conduct-ed in France. The probability of observing atrue difference between the two groups was 95percent.
The study was carried out in four maternityunits of the public and private sector located inParis: Hospital of the Deacons, Notre Dame ofBonsecours Hospital, Saint Anthony's Ilospital.and Tenon Hospital. The first women wereenrolled in November 1985 and the last womendelivered in August 1987. Data collection wasneeded at different points in the study. A sheetwas completed at study entry to ascertain theeligibility of each woman and to assess the riskof preterm delivery according to the state of thecervix and the frequency of contractions. Afterdelivery, a questionnaire was given three tofour days after birth, when the woman was stillin the maternity unit. It was a self-administeredquestionnaire. which focused on the women's
views of prenatal care arrangement andinquired about the medical knowledge of thewomen, bed rest, and support during the lasttrimester of the pregnancy. Data on prenatalcare, delivery. and pregnancy outcome werecollected from medical records by one or twomidwives in each hoypital.
Statistical analysis was carried out by theuse of X= and t tests, as appropriate.
REstrrs
A total of 158 women were randomizedinto either the intervention or the controlgroup. Six women were lost to follow-up afterenrollment; it was impossible to identify thesewomen and to know whether they differedfrom the other women. The following resultsare based on 79 women in the interventiongroup and 73 women in the control group.
Compliance with the allocation wasassessed. Four women in the interventiongroup had no home visit. Two of them werehospitalized several days after allocation, andthey stayed in the hospital a long time. In thecontrol group, eight women had home visits;they might have a higher risk of preterm deliv-ery than the other women. Six women werehospitalized after randomization, For the analy-sis, we retained the groups as they were origi-nally allocated.
In the intervention group. the midwivesmade an average of ,6 home visits. The aver-age length of the home visiting service was 30days. In general, the last visit occurred duringthe .35th or 30th week of gestation.
At study entry, the intervention group and
137
144 Preventiwi (y. Preterin Deliveries by Home lIsititig System
the control group were similar on the majorsociodemographic characteristics (see table12.1). The distribution of age and parity wasthe same; the proportion fo. women who weremarrit:d or who were cohabiting with thechild's father and the proportion of womenwith French citizenship did not differ signifi-cantly. Furthermore, both groups had the samesocial class distribution.
The distribution of risk factors fm pretermdelivery was similar in the two groups. Theproportion of women who had had a previouspreterm delivery was 5 percent in the inter-vernion group and 8 percent in the controlgroup: this difference was not significant. Atstudy entry, 77 percent of the women wereperceiving contractions in the interventiongroup versus 79 percent in the control group(see table 12.2). A vaginal examination wascarried out for every woman before enroll-ment. Dilatation of the internal os and shortcervix were less frequent among the interven-tion group, and soft cervix and middle posi-tion of the cervix was more frequent in this
group: nevertheless, none of these characteris-tics of the cervical state differed significantly inboth groups.
The proportion of women who deliveredbefore 37 weeks of gestation was 18 percent inthe intervention group and 15 percent in thecontrol group. Two perinatal c Ieat .1S wereobserved in the intervention group and one inthe control group; these three deaths occurredamong premature babies whose gestational ageat birth was 32 or $3 weeks and whose birth-weight was between 1700 and 1800 g. Theseresults show that the study population had ahigh risk of preterm delivery: in the control
Intenvntims
group. the preterm delivery rate was threetimes higher than it was in Paris in 1981.'
The trial was designed to assess the cost ofmedical care during pregnancy mainly throughthe cost of hospitalizations. The proportion ofadmissiens to hospital was slightly higher inthe intervention group than in the controlgroup. and the mean stay in hospital was a lit-tle longer in the intervention group; however,none of these differences was significant (seetable 12.3). The difference (intervention groupminus control group) of the mean stay in hos-pital was 1.4 days (C1 = 0.8. + 3.5); the c-onfi-dence interval included a range of situations.from a reduction of about 1 day in hospitalthrough the home visiting system up to anincrease of 3.5 days, Thus, the chance of reduc-ing the cost of medical care related to hospital-ization was very small.
The home visiting system neverthelessreduced the number of prenatal visits at theoutpatient clinic, and the difference was signif-icant: 33 percent of the women in the inter-vention group had prenatal visits or mo7-e,compared to 5.4 percent of the women in thecontrol group. All of the women except twowere treated with tocolytic agents after studyentry: the treatment was similar in bothgnmps.
After delivery, we asked mothers whetherthey had been satisfied with their medical carewhen they had had a threatened pretermlabor. Four answers were proposed: Very satis-fied, satisfied, unsatisfied, and very unsatisfied.No woman was unsatisfied or very unsatisfiedin the intervention group. and 3 women wereunsatisfied or very unsatisfied in the c(mtrolgroup. The proportion of very satisfied
Beatrice Blondel et al. 1 3 SI 5'
Advances in the Prevention of Low Birthweight
women was m. feh higher in the interventiongroup (78%) than in the control group (44%),and the difference was significant (see table12.4). Another question was related to the pre-natal care arrangement: "According to you,what is the best prenatal care arrangementwhen a threatened preterm labor is diag-nosed?" The home visiting system was pre-ferred more frequently than the otherarrangements in both groups, but the propor-tion of women who preferred the home visit-ing system was 89 percent in the interventiongroup and 60 percent in the control group.The proportion of women who would havepreferred hospitalization was similar in bothgroups; none of the women in the interven-tion group preferred numerous prenatal visitsat the outpatient clinic. but 26 percent of thewomen in the control group did.
One of the tasks of domiciliary midwives isto provide information and support, with theobjective of reducing tiring living conditions.improving home help, and encouraging womento have rest.
Hedrest was more frequently recommend-ed among the intervention group than amongthe control group. Seventy percent of thewomen in the intervention group were askedto stay in bed the whole day, compared with58 percent of the women in the control group.but this diffeence was not significant (see table115). The women in the intervention groupwere taught to identify contractions more fre-quently than the women in the control group.This difference was statistically significant. Infact. the proportion of women who staved inbed the whole day was higher (58%) in theintervention group than in Ow control group
(42%) (see table 12.6); the difference was notsignificant, but the p value was 0.07.
In general, the women in the interventiongroup had more help than the women in thecontrol group: 86 percent of the women in theintervention group, versus 70 percent in thecontrol group, said that the amount of help hadbeen higher during the episode of threatenedpreterm labor than during the first trimester ofpregnancy. In the intervention group, 56 per-cent of the women who had previous childrendid not participate at all in child care; this pro-portion was 30 percent in the control group.and the difference was significant. The numberof people who took responsibility of hometasks was nevertheless not different in bothgroups.
CONCE SIONS
Women's satisfaction with medical carewas much more important in the interventiongroup than in the control group. Satisfactionmay have 1(mg-tertn effects on such outcomesas postpartum depression or mother-child rela-tionship. Follow-up of the study populationwas not planned in our protocol, and we donot know the cc msequences of the women.ssatisfaction.
Several studies have reported that pregnantwomen are satisfied with whatever care theyhave experienced and prefer it to alternativepossibilities. This statement was noted in rela-tion to a new schedule of prenatal visits.epidural," continuous fetal heart monitoringduring labor. and early discharge afterdelivery.' It is not verified f(n. home visits, how-
1 3 ,
146 Prevention of Preterm Deliveries 4y Home Visiting S:ysteni
ever; in our study, at least 60 percent of thewomen in both groups preferred the home vis-iting system. In some cases, a new organizationof medical care cannot be an improvement forthe majority of the women; but, in general,women have difficulties considering the advan-tages and disadvantages of a new procedure ortreatment which they have not experienced.Furthermore, differences between alternativepossibilities sometimes mean veiT little. On thecontrary, home visits may represent a real dif-ference in care, tiredness, and relationship withmidwives, and women who did not experiencehome visits could easily imagine how this sys-tem was managed.
This study does not show that the homevisiting system reduced the number of days inhospital. In the best situation, there is adecrease of one day in the intervention group,but actually the cost of home visits per womanis almost equal to the cost of one day in hospi-tal. Thus, in this hypothesis, medical cost isequivalent in both care systems. In the worstsituation, the number of hospital days is muchhigher in the group of woinen visited at homethan in the other group.
Against the background of medical practicein Paris, it seems difficult to reduce the numberof days in hospital through the home visitingsystem. French obstetricians have a very activeapproach to threatened preterm labor, whichincludes high rates of hospitalization, and theymay be reluctant to decrease this standard ofcare even if another prenatal care systemproposed. Furthermore, the domiciliary mid-wives who were involved in the trial could notinterfere with admissions to hospital. Themajority of the women were admitted on their
Beatrice Blondel et al.
Interz'entions
own initiative, and only 14 percent of the hos-pitalizations were decided by the midwivesduring a home visit. In addition, when awoman was admitted because of a threatenedpreterm labor, the medical staff may have beeninclined to keep her at the hospital for at leastthree to five days, with the obiective of pre-scribing a treatment and mmitoring the compli-cation over several days. In the trial, a shorthospital stay was not more frequent in thegroup of women who received home visitsthan in the other group. In general, a greaternumber of visits may induce a greater numberof medical interventions. Women who hadhome visits had about twice as many internalexaminations as the other women; therefore,the chance to detect a complication was higherin the intervention group, Furthermore, womenin this group were more aware of the signs ofpregnancy complication man the other womenand they might pay more attenticm to thosesigns.
The results on the number of days spent inthe hospital depend on the local medical prac-tice. In a prevkms trial, Spira et al. did not find
any significant difference in the mean stay inthe hospital, but this study was carried out ashort time after the creation of this care system.whereas several years are required to have anadjustment of current medical practice to aninnovation. Therefore, it would be important tohave results on more recent studies in otherareas or in other maternity units.
This study was restricted to threatenedpreterm labor. It does not give any conclusionfor other pregnancy complications which aresupervised by domiciliary midwives, such ashypertension. It also does not give any conclu-
1 4147
Advances in the Prevention (f Low Birthweight
sions for another type of care which is provid-ed by domiciliary midwives; Out of largetowns, the midwives provide home visits tosocially disadvantaged women; their basicactivity is to encourage women to attend prena-tal clinic and to have regular rest and appropri-ate diet. The benefits of such care have not yetbeen assessed in France. Research on theeffects of home visits among underprivilegedwomen should be considered in the future.
AcKNomnx;mENTs
This study was supported by grants fromthe Ministre des Affaires Sociales et de l'Emploi(Direction Generale de la Sante). We thank thechiefs of the four Departments of Obstetricsand Gynecology for permission to carry outthe trial. Our thanks also go to MariecielAllard, Dominique Decoudun, Marie-PauleLeloup, Dominique Lignac, and FrederiqueTeurnier, who are domiciliary midwives inParis, for their help in preparing the protocoland the questionnaires. We wish to thankMarie-Christine Nourry for preparation of themanuscript.
REFER1ACES
1. Rumeau-Rouquette. (.. and Blonde]. B. (198'i'). TheFrench perinatal prognimme. In: J. Vallin and A. 1).Lopez (hIs.). Health policy, socia policy an(I mortal-ity prolkficts (pp. 299-311), Liege: Ordina.
2. Okls, D. L.. Henderson. C. R. . Thtelhaum. R.. andChamberlin. R. (1)8(). Improving the delivery ofprenatal care and Outcomes ot pregnancy: A ran-domized trial of nurse home visitation. Pediatrics77, 10-28.
3. Spira, N. Audras, F., Chapel. B.. Debuisscm, E..lacquelin. J., Kirchhoffer. C.. Lebrun. C.. and
(4.
Prudent, C. (1981). Surveillance a domicile desgrossesses pathologiques par les sages-femmes:Essai comparatif contrOle sur 9{X) funnies. Journalde GynC,cologie, Ohstc3trhlue et Biologie de laReproduction 10, 5.43-518.
Rumeau-Rmiquette, C., du Mazaubrun. C.. andRabarison. V. (Eds.). (1984). Naltm en !Wince: Dixans daolution. Paris: INSERM/Doin.
S. Porter. M.. and Maclntyre, S. (198.1). What is, mustbe bust: A research note on conservative or deferen-tial responses to antenatal care provision. SocialScience and Medicine 19, 1197-12(X).
Cartwright. A. (19'79). The dignity cf labor? studyqf childbearing and induction. London: Tavistock.
7. Garcia. J.. Corrv, M., MacDonald, D., Elhourne, D.,and GrantA. (1985). Mother's views of continuouselectronic fetal heart monitoring and intermittent aus-cultation in a randomized controlled trial. Birth 2,79-85.
8. Blonde}, B., Garel. M., Breart, G.. and Sureau. C.(1983). La sortie precoce des femmes apresl'accouchement: Enquete d'opinion aupres despatientes et du personnel d'un service. journal deGynecologie. Obstetrique et Biologie de laRep?.oduction 12, 457-460.
Olds, D. L. Ilenderson, C. R.. Chamberlin, R.. andTatelhaum, R. (198( ). Preventing child abuse andneglect: A randomized trial ot nurse home visitation.Pediatrks 78, 65-78.
141148 Prevention qf Preterm Deliveries by Home Visiting System
Intenvntions
Statistical Findings:Prevention of Preterm Deliveries
bY Home Visiting System
Table 1 2.1
Maternal Demographic and SocialCharacteristics
Intervention Controlgroup group
percentage percentage(N = 79) (N = 73)
Table 12.2Contractions and Cervical State at
Study Entry
Intervention Controlgroup group
percentage percentage
Perceived
Age (years) contractions 77 79 NS
< 24 25 18
25-29 34 37 NS Cervical
> 30 41 45 Dilationno 5 6
Parity external os 46 40 NS
0 49 49 internal os 49 54
1 36 40 NS
2 or more 15 11 Length of thecervix (cm)
Fr. citizenship 20 30 NS < 1 .35 30
2 52 54 NSMarried orcohabiting withthe child's father 91 93 NS
> 3
Consistency
13 16
firm 23 26Social class* medium 41 46 NS
31 30 soft 36 28II 23 15
III 17 27 NS PositionIV 29 28 posterior 7 -P 59
mid 42 38 NS
anterior 1
* According to occupation of the child's father; womenwho were living alone were excluded. Low station 4 NS
I: managers, engineers, professional workers.
IV: manual workers, unemployed.Expansion ofthe lower uter-ine segment 79 79 NS
Beatrice Blundel et al. 1.4,2 /49
Advances in the Prevention Qf Lou' Birthueight
Table 1 2.3
Prenatal Care After Study Entry
Percentageadmittedto hospital
Intervention Controlgroup group
45 36 NS
Total number of hospital days*
Hospitalizedwomen 9.4 + 8.2 8.3 + 8.8 NS
all women 4.3 + 7.2 2.9 + 6.6 NS
Prenatal visits atoutpatient clinic(percentage)
0-1 17 102-3 40 36 NS4 or more 33 54
* mean + s.d.
Table 12.4Mother's Views of Prenatal Care
Intervention Controlgroup group
percentage percentaw
Were you satisfied with your prenatal care since you hada threatened preterm labour ?
very satisfied 78 44
quite satisfied 22 51 < 0.001
unsatisfied orvery unsatisfied 0 5
According to you, what is the best prenatal care arrange-ment when a threatened preterm labor is diagnosed ?hospitalization 11 15
more visits at theoutpatient chnic 0 26 < 0.001
home visits by amidwife 89 60
Table 12.5
Information about contractions and bedrest
Intervention Controlgroup group
percentage percentageI)
Identificationof contractions 77 59 < 0.05
Stay in bed
no recom- 9 18mendation
some hours 21 24 NS
the whole day 70 58
Table 12.6Bedrest and Home Help
Intervention Controlgroup group
percentage percentage
Bedrest duringthe whole day 58 42 0.07
More helpthan during thefirst trimester 86 70 < 0.05
Number of people who participate in house work0
.3 or more
Child care bythe father oranother personexclusively *
* Multiparae only
I 4
5.3 6032 32 NS
15
56 30 < 0.05
150 Statistical Findings: Prevention qt. Preterrn Deliveries by Home Usiting System
Smoking InterventionsDuring Pregneliicy
MARY J. SEVION, M.R H.
INTRopt rnoNIn this paper, three issues are addressed: (1)The importance of cigarette smoking duringpregnancy as a risk factor; (2) the causality ofcigarette smoking in reduced birthweight; and(3) the effectiveness of smoking cessation assis-tance in achieving abstinence. The discussionsbelow often overkill ;at least two of these issues.
TilE IMPOMANCE OF SMOKING As A RN: FACFOR
The 1985 Institute of Medicine report synthe-sized a large number of studies in the area oflow birthweight. To organize the findings anddiscussions, risk factors were divided into thef011owing categories: Demographic risk factors,medical risk factors that predate the currentpregnancy, medical risk factors during the cur-rent pregnancy, behavkral and environmentalrisk factors, and health care filo:tors. The data in
14.;
Advances in the Prevention of Low Birthweight
table 13.1 were abstracted from informationpresented in that report. For each broad catego-ry of risk, the table shows the specific factor forwhich the literature showed the largest relativerisk for babies with intrauterine growth retarda-tion (IUGR). Some estimates of relative riskwere less reliable than others, and this was indi-cated by a range of estimates. In general, how-ever, the largest single risk factor within each ofthese categories showed a relative risk of abouttwofold or threefold. Smoking had about thesame level of relative risk as most other factors.The data showed that smokers are at threetimes the risk of having an ILIGR baby; theincreased risk associated with smoking is, over-all, as high as for other risk factors for IUGR.
Only a few studies have used either IUGRor preterm delivery as the dependent variable,compared with a much larger number of stud-ies that have examined average birthweight orlow birthweight. The reason for concentratingon the IUGR relative risk, however, is that thework of Sexton and 'Jebel, as well as others,supports the hypothesis that maternal smokingduring pregnancy results primarily in a problemof intrauterine growth retardation.
In addition to the high level of increasedrisk, the importance of smoking in relation tohirthweight from a public health point of view isfurther underscored by its prevalence. Over one-fourth of all pregnancies begin with the womansmoking; of these, only a fairly modest percent-age of women quit on their own and continuetheir abstinence throughout the pregnancy.'
THE ImPORTANC1 OF SMOMM; As A CAI:SAI, FACFOR
In assessing the risk associated with stnok-ing from a clinical point of view, a major con-
sideration is the extent to which the observedreduction in growth of the fetus is causal andthe extent to which it can be reversed. If smok-ing is causally related to birthweight, its impor-tance is much more significant. Over the lastthree decades, hundreds, if not thousands, ofstudies have replicated Simpson's earlier obser-vation that maternal smoking is related to thebirthweight of the infant.' Despite the over-whelming consistency of the data, a hotlydebated issue arose almost immediately andhas continued regarding whether smoking istruly causal since smokers were known tohave, or more often just suspected of having.characteristics other than smoking that couldaccount for the lower birthweight of theirinfants.' Arguments against smoking as a causalfactor could best be refuted or supported byexperimental evidence.
Results from Three RCTs on BirthweightThere have been only three randomized
clinical trials (RCTs) reported on smoking cessa-tion and birthweight. One has reported no dif-ference; one, a statistically significant difference;and the latest, a difference in the expecteddirection, but not a statistically significant one.Despite the need for such experimental evi-dence to clarify the issue of causality, it was notuntil 197S that Donovan reported results fromhis randomized clinical trial of smoking inter-vention and birthweight conducted in England,''His trial showed no difference in the birth-weight of the babies born to the two randomlyallocated groups of pregnant smokers. Theintervention group had, on average, babies whoweighed 12 g less than babies born to mothersin the control group. Some of the details of the
4 5
154 Smoking Interventions During Pregnancy
Donovan trial will be discussed later.The second of the three randomized clini-
cal trials that have examined birthweight is thatof Sexton and Hebei.' It is the only reportedrandomized trial that has been conducted witha U.S. population, although it should be notedthat two additional U.S. trials with plans toexamine birth outcomes have been initiated.The first is a trial conducted at KaiserPermanente in Oregon, in which the investiga-tors intended to examine birthweight, but didnot do so (probably because of the poor resultsobtained in quit rates).- The second is an ongo-ing trial in Vermont under the direction ofSecker-Walker.s Birth outcomes have been col-lecwd; but although there are plans to examinethem, there has not yet been a report.
The Sexton and Hebel study was designedto test the causal hypothesis that a reduction insmoking during pregnancy would increase theaverage hirthweight of the infant. It is the onlyone of the three trials that has found a signifi-cant difference in quit rates and hirthweights.Thus, the details of this trial are of special inter-est. With the cooperation of more than 50 pri-vate obstetricians in the Baltimore metropolitanarea, 935 pregnant smokers were enrolled. Thepregnant women filled out a brief questionnairewith information related to smoking and lastmenstmal period, and stated their willingness tobe contacted by project staff. From theseresponses, was determined: Smokersof 10 or more cigarettes at the beginning ofpregnancy were eligible (regardless ot whetherthey were currently smoking or not) if they hadnot passed the 18th week of gestation. Ikcauseof expected high rates of recidivism, smokerswho had quit prior to registration for care
Interventions
(baseline quitters) were included in the trial.The eligibles were contacted and a baseline visitscheduled. At that visit, written consent to par-tidpate and a questionnaire were obtained; asample of saliva was also obtained, from whichsalivary thiocyanate was measured (thiocyanateis correlated with smoking status)." The smokerswere randomly allocated to either a treatmentor a control group.
On average, the women were approxi-mately 25 years of age, they had completed alittle more than 12 years of schooling, andabout 40 percent were black. About one-thirdhad had no previous pregnancies, and theywere, on average, at about 15 weeks gestation.
The women smoked about a pack ofcigarettes at the beginning of pregnancy. buthad reduced this to about half at tlw time ofrandomization. The baseline level of salivarythiocyanate was comparable in the two groups.Both experimental groups were ccnnparable atthe time of randomization.
The antismoking intervention was given byproject staff, outside the health care setting,with a variety of contacts, including one per-sonal visit at the time of enrollment, a monthlyphone call, and biweekly contact by mail (usu-ally in the form of a newsletter).'"
The smoker was provided health informa-tion on the risks to her own health and to thatof her baby. The main assistance, however, wasin the form of information on how to quitthrough suggestions and guidance in behav-ioral strategies. The smoking cessation coun-SCION gave no information On caffeine, alcohol,nutrition, or weight gain. When a woman askedabout these factors, she was told to talk withher physician. Discussion of these factors was
Mary" Sexton 14 155
Advances in tbe Prevention qf Low Birthuvigbt
refrained from in an effort to keep the interven-tion purely an antismoking one.
Table 13.2 shows the results for the smok-ing inform,ion obtained at the 8th month ofpregnancy. Twenty percent 9f the women inthe control group quit smoking and 43 percentof the women in the treatment group (p< 0.01)reported that they had quit smoking. Consistentwith the quit rates are the differences in thedistribution of smoking between the twogroups. The biochemical measurement. salivarythiocyanate, was also statistically different at asignificant level. Thus, the several assessmentsshowed a significant decrease in smoking forthe intervention women.
The pregnancy outcomes for the twoexperimental groups were comparable; 96.7percent of the control pregnancies resulted in asingle live birth, as did 96.6 percent of thepregnancies in the intervention program. Therewas no indication of differential pregnancy lossfor the two groups. The birthweight hypothesiswas tested on 867 single live births. As shownin table 13.3, the babies in the control groupweighed 3,186 g; those in the treatment groupweighed. on average. 3,278 g (I) < 0.05). Basedon the evidence of the quit rates and the birth-weights, the null hypothesis of no difference inaverage birthweight was rejected. The percent-age of babies weighing less than 2500 g at birthis also shown; 8.9 percent of the controlbabies, compared with 6.8 percent of the treat-ment babies, were low birthweight babies. Thepercentages of babies weighing less than 1500g was 1.1 for control babies and 1.9 for treat-ment babies. Neither of these last two compar-isons was significantly different.
The most recently reported liCT is that of
MacArthur, Newton, and Knox," conducted inthe United Kingdom. Mothers allocated toreceive assistance with their smoking hadbabies weighing 34 g more, hut this differencefailed to reach statistical significance.
Comparisons of the Three RCTsAt first glance, the results of the three trials
appear to be in conflict with each other; how-ever, insight into the reason for the apparentdifferences is gained by examining some of thedesign and implementation features of the stud-ies. Table 13.4 shows the birthweight results bythe two experimental groups for the three ran-domized clinical trials. As stated earlier, the firsttrial, conducted by Donovan, showed no signif-icant difference in birthweights between infantswhose mothers were in the treatment groupand those whose mothers were in the controlgroup. The trial conducted by Sexton andHebel showed a statistically significant differ-ence of 92 g. MacArthur et al. found a differ-
of 34 g. The table also shows the quitachieved in the two more recent trials.
enceratesDonovan has never reported the quit rates forhis trial, but concluded that the differencebetween the two groups was modest at bestand may not have differed at all:' In the latesttrial, MacArthur et al. reported an increase of 3percent in the quit rate in the treatment groupcompared to that of the control group (9% v.6%). In the Maryland study, the difference inquit rates is reported to be 23 percent. If thewomen who had already quit before enroll-ment (baseline quitters) are excluded (for clos-er comparability with the MacArthur et al.study), the quit rates between the two experi-mental groups in the Maryland cohort still differ
4 7
156 Snwking Interventions During Pregnancy
substantially: 32 percent for the treatmentgroup versus 7 percent for the control group.Thus, the failure to find birthweight differencesin the two United Kingdom randomized clinicaltrials results directly from their not achievinglarge enough differences in the relative quitrates. The reason the quit rates were so radical-
ly different from the Maryland rates probablystems from the features of the studies.
Design Features of the StudiesSome of the design features of the three
studies are shown on table 13.5.
LocationAS indicated, two of the studies were con-
ducted in the United Kingdom, one in ,c,.idon
and one in Birmingham; the Sexton and Hebeistudy was conducted in Maryland. Cultural dif-ferences alone might explain the quit rates, butthere seem to he other possibilities as well.
Snwkitzg StanisAmount Smoked and Gestation at EnrollmentThe smokers included in the studies varied.
Donovan included smokers of any amount at the
beginning of pregnancy if they were smokingfive or more cigarettes at the time they were ran-domized into the study. The average gestationalage of the women included in the trial WASalmost 16 weeks (he had included women up to30 weeks of gestation.) Sexton and Hebeienrolled women who smoked more at the begin-ning of pregnancy (10 or more cigarettes), but
because they had no cut-off regarding smokingat the time of enrollment. they included womenwho had already quit at the time of enrollment.MacArthur et al. enrolled all pregnant smokers at
Mat31. Sextort
Intenoztions
the time of booking regardless of the amount.The women enrolled in their study and in that ofSexton and Hebei were earlier in their gestationthan the enrollees in the Donovan study, givinga little more time for intervention. The differ-ences in the smoking criteria used for these threestudies are reflected in the averages of theamount of smoking for those enrolled in thestudy. The women in the two United Kingdomstudies smoked about 18 cigarettes per day atthe time they became pregnant. The women inthe Maryland study smoked over 20 cigarettesper day at the time they became pregnant, butwere smoking only 11 cigarettes per day at thetime of enrollment. Women in the two UnitedKingdom studies had to he smoking at the timeof entry into the study, so there was not as greata reduction in the amount smoked betweenonset of pregnancy and entry into the study. Ifthe baseline quitters are excluded from theMaryland cohort, the women smoked an averageof 21.7 cigarettes at the beginning of pregnancyand decreased to 13.5 cigarettes by the time ofregistration for prenatal care (on average at 15weeks gestation). Thus, the Maryland study sub-jects at baseline had already reduced smoking to
a lower level than seen in the two UnitedKingdom studies.
Assessment of SmokingIn the last column of table 13.5, it can be
seen that the studies differed in the way inwhich snictking status at the end of pregnancywas determined. The two 1.7nited Kingdomstudies assessed the smoking status only after
delivery by self-reported recall information.Neither reported any biochemical assessment ofsmoking. In the Maryland study, both self-
1 4 :3157
Advances in the Prevention of Lou, Birthweight
reported data and salivary thiocyanate wereobtained prospectively. The different assess-ment of smoking rates introduces some uncer-tainty about the comparability of the data.Nevertheless, the differences in the amountsmoked by the subjects in the three trials andthe time the woman could be exposed to theintervention (gestational age at enrollment) donot seem great enough to account for the dif-fering quit rates achieved in the studies.
IntertvntionIn addition to the differences in the amount
of cigarettes smoked, other features of the threestudies varied and are the ones most likely toexplain the quit rates. These features relate tothe intensity of the intervention sites and theintervention staff. The two United Kingdomstudies were conducted within a small numberof clinical settings, and the intervention was car-ried out by the clinic staff themselves. In theMaryland study, the smokers were recruitedfrom a much larger number of practice settings,and the intervention was conducted outside ofthe practice setting by staff recruited and trainedby the project. In the Birmingham study, theamount of time and attention given to the inter-vention varied from one staff member to anotherand at times was not conducted as planned.From discussions with both of the UnitedKingdom study groups, the antismoking inter-vention was, on average, relatively weak com-pared to the number of contacts, intensity, andtime given in the Maryland study.
Allocation SchemeThere was also some possible compromise
in the integrity of the two experimental groups
from the studies being given in the clinical set-ting and implemented by the regular prenatalstaff. In the Donovan study, the smokers wererandomized on an individual allocation basis.In contrast, for practical reasons, the accrual ofsubjects for the MacArthur study was by four-week periods in which all smokers booking atthe hospital received the intervention during adesignated four-week interval followed by afour-week interval during which smokersreceived no intervention. The same clink. staffwere responsible for patient care during theintervention and nonintervention phases.
The brief highlighting of some of thedesign differences among the three randomizedclinical trials is helpful in identifying severalpossible explanations of why there was such amarked difference between thc reported quitrates in the two United Kingdom studies andthe quit rate in the Maryland study and theaccompanying lack of difference in hirthweight.The United Kingdom studies had a less inten-sive intervention than the Maryland study andhad less control over the implementation of theintervention. Furthermore, the same clinic staffwere in contact with both treatment and con-trol smokers, providing the opportunity forcontamination (although the modest quit ratesfor the control groups indicate that this wag nota substantial problem). Since the UnitedKingdom studies did not include an objectiveassessment of smoking, such as cotinine, it is
difficult to know what the precise magnitude ofresponse to the intervention really was, but itwas surely vei-y low.
Although the two United Kingdom studiesdid not produce evidence to refute the nullhypothesis, the most reasonable explanation for
14;.)
158 Smoking Intertentions During Pregnancy
this is because the intervention was not strongenough to achieve a substantial difference inquit rates. The birthweight hypothesis can betested only if there is a difference in quit ratesthat is large enough to produce a birthweightdifference. It is much more reasonable, there-fore, to conclude that the two United Kingdomstudies produced no evidence on whethersmoking causes reduction in birthweight thanto conclude that antismoking assistance has noeffect on birthweight. The weight of evidenceproduced by the large number of observationalstudies and by the Mai}, land randomized clini-cal trial supports a causal effect on the birth-weight of the baby from maternal smokingduring pregnancy. If the mother quits smokingduring pregnancy, her baby will, on average.have an increase in birthweight. It must be rec-ognized, however, that, to date, there is still nota solid base of experimental results on whichto rest this statement.
SUBGROL ANALYSES
Regardless of whether an overall effect forthe randomized clinical trial is found or not,some analysis is usually directed toward sug-gestions of differential effects among subgroupsof subjects. These subgroup analyses have tobe viewed as unplanned anal'ses and, there-fore. caution must be appropriately exercisedin their interpretation.
ParityThe Birmingham data were analyzed and
reported by parity. A larger difference in quitrates was found between the treatment and con-
Intenv itions
trol groups for nulliparous women. These smok-ers (see table 13.7) had quit rates of 14 percentand 7 percent, respectively, in the treatmentgroup and control group. In contrast, the respec-tive quit rates among multiparous women were 7percent and 6 percent for the treatment and con-trol groups. The pattern of birthweiglns was con-sistent with the pattern of quit rates. Thenulliparous women in the treatment group hadbabies who weighed an average of 96 g morethan the control group babies. These findingsgive further support to the causal role ofcigarette smoking: An increase in quitting causesan increase in birthweight. They also suggest,however, that smoking cessation intervention hasvery little impact either on quit rates or birth-weights when the smoker has already had apregnancy. Similar Maryland data are shown atthe bottom of table 7 for the same stratifiedgroups. Among the nulliparous subjects. about10 percent of the control group of women quitsmoking and alxmt 36 percent of the treatmentgroup quit smoking. This represents a 26 percentdifference in the quit rates between the twoexperimental groups. Unlike the MacAnhur et al.finding, the quit rates also differed between thetwo groups of women who had had one or moreprevious pregnancies. The higher quit rates inthe treatment group were consistent with thefinding of heavier weight babies in the treatmentgroup. The multiparous women in the treatmentgroup had babies who averaged 3,275 g, anincrease of 112 g compared with the controlgroup babies. When the quit rates in theVermont study were examined, they did not dif-fer according to the number of previous preg-nancies the smoker had. The self-reported quitrates were 14.7 percent and 1.4.1 percent, respec-
itkoyl Sexton 1595
AdtwItCeS in the Prevention (1. Lou' Birthweight
tively, for women with no previous pregnancyversus those with 1 or more.* While somegroups of nulliparous women, such as those inthe Birmingham study, may he more responsiveto a smoking cessation intervention, it is not aconsistent finding. Thus, the most reasonableconclusion at this time is that all women, regard-less of their parity, will benefit from antismokingintervention both by achieving higher quit ratesand increased birthweights of the babies.
RaceBecause of the concern for the increased
low birthweight rates among blacks, theMaryland data were examined to determinefor blacks the extent of response to smokingcessation intervention and the extent ofimpact on birthweights of the babies. Very lit-tle information on quit rates, if any, has beenreported separately for black and white preg-nant females. On the one hand, black andwhite females, overall, smoke in about thesame proportionaround 25-30 percent. Onthe other hand, black females smoke fewercigarettes per day than their white counter-parts.'' Table 13.8 shows that for the 296blacks in the Maryland cohort who were stillsmoking at time of enrollment, 39 percent ofthose in the treatment group quit smoking,compared with 6 percent in the control group.Not as many whites in the treatment groupquit (only 28%). The quit rates for blacks andwhites i the control group were similar.Thus. ti:e intervention produced a largerincrease in quitting among blacks comparedwith whites. It did not, however, produce a
Seclicr-Walker. R. II. personnal communication
larger differential in birthweights. For blacks,the treatment women had ba hies w howeighed, on average, 94 g more at birth, Forwhites, the treatment group babies averaged136 g higher in weight. Nevertheless, bothblacks and whites derived significant benefitfrom the antismoking intervention.
In summary, the birthweights in all threerandomized clinical trials and in the subgroupanalyses seem consistently to follow clearly thepattern of quit rates, providing additional con-fidence in the conclusion that maternal smok-ing does cause a significant decrease inbirthweight.
Em.rnvENTss OF
SNIOKINO CE,SSAIION ASSISTANCE
int' or mation from the three trials that havereported birthweights has already been pre-sented on the differential quit rates betweentwo randomly allocated groups (see table13.1). Three additional randomized clinical tri-als have reported on quit rates, hut have notreported on birthweights. These have all beenconducted within the prenatal care setting butwith different approaches to the interven-tion.'"'. An indication the type of prc)gramis shown. The Baric and Windsor studies had afairly modest level of interventicm. consistingof self-help materials on smoking and a healthmessage given in the Baric study by the physi-cian or nurse and in the Windsor study by ahealth educator. The approach in the ongoingSecker-Walker study is much more intensivethan in the other two in terms of the frequencyof contacts, length. and focus of the interven-
1 r160 Smoking Interventions During Pregnancy
tion. The quit rate for the treatment groups for
each of the three studies is 1,4 percent (in theWindsor study, a second treatment group hada 6% quit rate). The quit rates in the controlgroup varied from study to study, resulting in adifferential between the two experimentalgroups of around 5-1D percent. It is not likelythat, with the modest differentials in quit ratesand the sample sizes, a significant difference inbirthweights would be found. These studies doshow, however, that a modest level of inter-vention can increase the rate of quitting.Overall, the highest quit rates were producedin the Maryland study, with a 25 percent differ-
ential in the quit rates found. Even in thatstudy, a very large proportion of smokers didnot quit.
From the small number of randomized tri-als that have reported smoking and birth-weight, there is room for optimism. Assistanceto the pregnant smoker after she has registeredfor prenatal care can be effective in raising the
proportion who quit and in increasing thebaby's birthweight. There is still much more tolearn, however. about how to provide effective
intervention fiw sm()king cessation during andfollowing pregnancy.
REi7ERENcEs
1. Institute of Medicine. (1985). Preventinj; low birth.teet;i4bt. Washingnm. DC.: National AcadtAny Press,
Sext(in. M., nd !Abel, J. R. (198.4). A clinical trialof change in maternal smoking and its effect on birth
weight, journal (!f the American Medical Assocknion251. 911-91c.
3. Sexton. NI. (1986). Smoking. In: Ct. (hamberlainand J. Lumley (Eds.). Prepregnano. caw: rnanual
pmct(ee. Sussex. England: John Wiley and Sons.
Interventiwts
4. Simpson, W. J. 0957). A preliminary report Oncigarette smoking and the incidence of prematurity.American journal qf Ohctetrks aiul 6:rnecologi, 3,80S-815.
S. Yenishalmy, J. (1971). The relationship of parents'cigarette smoking to outcome of pregnancy:Implication as to the pr(Olem of inferring causationfrom Observed associations. American journal cfPpidemiolojo' 93, .4.43-150,
6. Donovan, J. W. (197). Rand(imised controlled trial
of anti-smoking advice in pregnancy. Britisbty. Pretyntire and Scicial .ttedicine 31. 6-12,
Loch. 13. K.. Waage. Cr_ and Bailey. J. (1983).Smoking intervention in pregnancy. In: W. F. Forbes,R. C. Freeker. and Nosthakken (Eds.). Proceedings(!l' the Fifth Worid Conference on Smoking and He(ilth.Winnipeg. Oittada (pp. 35(.)--39i),
8. Seeker-Walker. It II.. Flynn, 11, S.. Solomon. L. J. et.al. (198(- ), Attitudes, beliefs, and other smokers:Factors affecting smoking cessation during pregnan-cy. Paper presented at the American Public HealthAssociation Meetings, Las Vegas. Nevada.
Sexton. M.. Nowicki. P.. and Ik-bel. J. R. (1980).Verification of smoking status by thiocyanate in unre-frigerated. mailed sampk-s of saliva. PreventiveAtedkine 15, 28--3-4.
9.
10. Nowicki. P.. et al. (19851. Effective smoking inter-ventitm during pregnancy. Thrill 11(41, 217-224.
11. MacArthur, C., Newton. J. H.. and Kn)x. F. C.1t)S7). Effect of anti-smoking health education on
fetal size: A randomized clinical trial. liritisbjournal qi Obstetrics awl Gynaecology 9-1.
I.!. Sexton. M. (1985). Smoking among women:Proceedings. the Pennsylvania ConsensusCAniference cm Tobacco and Ifealth Priorities. (pp.-ti-791. Pennsylvania I)epartment of licalth.
13 Ririe. 1,.. MacArthur. C.. and Sherwciod. M. (19-6).,A study ot health educati(In aspects of smoking inpregnancy. International Journal of HealthEdtkation 19 (2. Suppl
iL \\'indsor. H. A.. Cutter. C.. et al (1985). The effec-tiveness of smoking cessation methods for simikersin public health maternity clinics: A randomizedtrial. American Journal of Public Health -S.1389--1392.
Maly J. Scytoit rA..
Interivntions
Statistical Findings.Slizoking Interventions
During Pregnancy
Table 13.1Estimates of Rt ;atiye Risk forPrincipal IUGR Risk Factors
Risk Category IUGR RR
Demographic:
Risk Category
MedicalCurrent Pregnancy:
IUGR RR
Black 2.4 Preeclampsia./Toxemi 2.3-15.8
MedicalPredating Pregnancy: Behavioral and Environmental:Previous IUGR Baby 2.9-7.98 Smoking 3.04
Source: Institute of Medicine. g85). Preventing low htrth weight Health Care:Washington. D.C.: National Academy' Press. Absent/Inadequate Prenatal Care 2.0
Table 13.2Smoking Characteristics of Control and Treatment Groups at Eighth Month of Pregnancy*
Control GroupPercentage ReportiogSmoking, Cigarettes/day'
Treatment Group Thiocyanate, Control Group Treatment Groupmole/L
389 380
N .395' .395 Mean + 2,452 + 1,228 2,094 + 1,209
0 20.0 43.0 ' hides insIs s iinitin s ho had nc)t been deh ervd hi the eIghth-nnynth ttintact.
1-5 12.7 19,1 t 1),riterern.e Iii dtstributft)ns ot number.: igairttes ;.ser ii.ii. vs,vs statistic alls
na+cant hv Nolmogorm Srria-noi test p < Ut
6-10 22.0 16.2 rnw.ing on As(i sublects.
11-20 31.4 17.8 ! I ),,qa 1711.0071g on five sublet ts
> 20 13.9 .3.9potereni e in mean t,gatettes smoked via, qattstical4 NismNant fi Student sttest (f) < .017
Mean + SD1 12.8 + 11.5 6.4 + 8.7 j Vittercnce in MEW? tht0c ,Inate, isaS statrsttcalls It student t
test ip c .01".
Table 13.3Measurement of Status of Newborn*
Primary factors
Birthvveight (grams)
Percentage < 2.500
Percentage < 1,500
438
438
438
Control Group
Mean + SD
3,186 + 566
8.9
1.1
429
429
429
Treatment Group
Mean + SD
3,278 + 627
6.8
1.9
2.28.
includes only single, live births. t p < .05 h! Ntudent'N I teNt.
Maty Sexto?1 163
5 ,3
Advances in tbe Prevention ((Low Birtbuvight
Table 13.4Results of Three Randomized Clinical Trials
Birthweight (g)ControlRandomized Clinical Trial TX
Donovan (1972) 552 3172
Sexton/Flebel (1979) 867 3278
Macarthur/Newton/Knox (1981) 982 3164
Not Reported
3184
3186
3130
Quit RatesTX Control
43%
9%
20%
6%
RC T
Donovan(London)1972
Sodon, Hebef(Maryland)1979
Table 13.5
Smoking and Gestational Characteristics by RCT's of Examining Birthweight
Number at
Ra ndom -
z at ion
549'
9 15
Macarthur, 1156Newton, Knox(Birmingham, UK)1981
Eligibility on
Smoking Status:
at Pregnancy at Randomization
> 10
> 1
Amount Smoketi at
Time of:
Pregnancy Randomization
17.7 15.2
20.8 11.2
18.2 14.1
Assessment ot
Late Pregnancy
Smokmg Status
ft't ft )5 pet- ti Ve
self- seport
prospec fiveself-rep< )rt
thkx yanate
retrospectiveself-reoort
Gestational
Age at Entry
15.9
15.0
15.2
Table 13.6Intervention and AHocation Characteristics of RCT's of Examining Birthweight
RCT
Donovan (London)
Sexton, Nobel (Maryland)
Macarthur, Newton, Knox(Birmingham, UK)
Study Sites
maternity hospitals
52 private obsand university clinic
1 maternity hospital
Implementation of Intervention
Within clinic by clinic staff
Outside clinic by project staft
Within clinic by clinic staff
1 5
Allocation Scheme
Individual randomization
Individual randomization
Alternating 4-week accrual
164 Statistical Findings: Smoking Intert'entions During Pregnancy
Parity0
> 1
Parity
0> 1
I able 1 3.7Quit Rates and Birthweights by Parity for UK and Maryland Cohorts
Percentage Quit Late Pregnancy, UK* Birthweight, UK*
TX
13`)/0
7(%)
7%()DA)
(TX-C)6%IT0
Percentage Quit Late Pregnancy, MD'
TX (TX-C)
TX
31643163
TX
Interventions
(TX-C)
3068 963171 -8
Birthweight, MD'
36'N, 10% 26% 3226 3102
.31% 6% 2,5% 3275 3163
MacArthur, Newton and knotSexton and Hebel: This excludes baseline quitters.
(TX-C)
124112
Table 13.8Quit Rates and Birthweights for
Blacks and Whites in Maryland Cohort
Percentage Quit Late Pregnancy* Birthweight
Race TX (TX-C) TX
Blacks (N 2961** 39% 6% 3.3t% 3080 2986
Whites (N 439)" 28% /3% 20% 3384 3248
" Eighth month** Excludes baseline quitters
(TX-C)94
136
Table 13.9Additional Randomized Clinical Trials of Smoking Cessation
Investigations (1st Author, Location,and Total Number)
Baric (United Kingdom); ,N = 1 0
Secker-Walker (Vermont); N = 249
Windsor (Alabama); = 309
N = 309
A second snuAing group using the Am('n( an 1 ung 4.
Mary Sexton
Program
Health provider message; materials
Health education; 4 individualcounseling sessions; materials
Health education (brief)
Windsor's self-help guide*
Quit (Percentage)TX Control
14% 4%
1,4% 9%
14% 2%
.,?t1017S -Freedom iron, Sm(71..ing gunle had .1b.?;? qua rdre.
155165
Cervical Cerclage: New Evidencefrom The Medical Research
Council/Royal College ofObstetricians and Gynecologists
ADRIAN GRANT, M.D.
INTRODI TCTION
This paper is an update of a review of cervicalcerclage prepared for the symposium onpreterm birth held at Evian in 1985.1 Sincethen, the interim results of the first 905 womenparticipating in the Medical ResearchCouncil/Royal College of Obstetricians andGynecologists (MRC/RCOG) randomized con-trolled trial have been published.' The purposeof this update is to review the interim resultsof the MRC/RCOG trial in the context of thetnree smaller trials of cervical cerclage whichwere discussed in some detail at Evian." Fulldetails of the MRC/RCOG trial are availableelsewhere,' so only the most important fea-tures will be described here.
.1 5 G
Advances in the Prevention qf Low Birthuvight
MEDICAL RESFARCI1 COUNCIL/ROYAL COLLEGE OF
OBSTETRICIANS .AND GYNECOLOGISTS TRIAL
The impetus behind the MRC/RCOGCervical Cerclage Trial was recognition of thehigh mortality and morbidity associated withpreterm delivery."4' Cervical cerclage was identi-fied as a strategy for prevention which hadbeen poorly assessed. It was recognized that, inrare cases, the operation may have seriousadverse effects, and that there was no soundevidence of its efficacy. Uncertainty about theplace of the operation was confirmed in a sur-vey conducted by the MRCIRCOG WorkingParty on Preterm Labor in 1979 (unpublishedobservations), which revealed extraordinarilywide variation in the use of the procedure byBritish consultant obstetricians. This variationwas one of the reasons for choosing relativelyflexible entry criteriaobstetricians' uncertain-ty as to. the advisability of cerdage. There wasno possibility of reaching consensus aboutwhere the uncertainty lay. Furthermore. it wasargued that cases which would meet more rigidentry criteria would be entered into a trial withmore open criteria by those obstetricianswhose uncertainty happened to coincide withthe rigid criteria. The advantage of this strategywas that other types of cases for which otherobstetricians were uncertain about the advis-ability of cerclage would be entered into thetrial. Any beneficial effect would be expectedto be mediated by prokmgation of pregnancyirrespective of indication. Nevertheless, the use-fulness of cerdage is likely to depend on theindication. It was therefore hoped that a widevariety of patients would be randomized andthat secondary analysis of patients in six pre-
specified subgroups would then help to deter-mine who (if anyone) could be expected tobenefit from cerclage.
In practice, 70 percent of the women whoentered the trial had had one or more secondtrimester miscarriages or preterm deliveries, 10percent had a history of possible past cervicaldamage (for example. cone biopsy or cervicalamputation); and, in the remaining 20 percentof the cases, cerclage was considered on thebasis of other indications, such as previous ter-mination of pregnancy and/or previous firsttrimester miscarriage. The trial groups werewell balanced with respect to these variousindications. The design of the trial was prag-matic. It was recognized that the clinical situa-tion might change as pregnancy progressed,and the aim was to compare two policies in theform of recommended management at trialentry. In fact, 92 percent of those allocated tocerclage received a suture (of those who didnot, .5(zi) did not wish to have a suture and 3%miscarried before the stitch could be inserted),and, of those allocated to the control group, 7percent had cerclage (5(!io because the cervixwas judged to be opening and 2 Q'i) because thepatient decided after entry that she would likea suture).
Two hundred Obstetricians (from 12 coun-tries) have contributed cases to the trial.Although randemization witbin specialty wasnot performed, cerclage and control cases wereevenly distributed for each participating obste-trician. Most cases (95) were entered before20 completed weeks gestation: the latest gesta-tion at entry was 29 weeks. Cases were enteredand randomized lw telephone. Most Obstetri-cians used the telephone randomization service
168 1 5 -;Cerclage
provided by the Clinical Trial Service Unit inOxford, but other rand(mlization centers wereestablished in Italy, Zimbabwe, and Hungary.
REVIEW OF THE OVERALL RESULTS
OF THE FMR RANIX)MIZED 1RIALS
Since the MRC:RCOG trial was established,the three smaller randomized controlled trialscomparing cervical cerclage with conservativemanagement have been reported.' These werediscussed at Evian' and have been reviewedelsewhere. Only Rush's study' of singletonpregnancies with an overall preterm deliveryrate of 33 percent shows much similarity to theMRC/RCOG trial. Dor' investigated twin preg-nancies only; Lazar' recruited women with sin-gleton pregnancies with an overall pretermdelivery rate of only six percent.
Obstetric maturgemeritThe results of the MRC:RCOG trial' are
consistent with those of the previously reportedtrials (where data are available) in suggestingincreased obstetric intervention associated withcerclage as judged hy admission to hospital, theuse of oral betamimetics, induction of labor.and cesarean sectim (see table 14. ).
Pregnancy outcomeWhere the MRC. RCOG trial does differ
from the other trials is in its suggestion of abeneficial effect of cerclage on length of gesta-tion and vital outcome (see table 14.2). Thethree smaller trials show a tendency towardshorter gestation and higher mortality in thecerclage group. In contrast, there were 5 per-
hlterl'entions
cent fewe Ir Le..ver.es .)etween 20 and 32weeks' gestation in the MRC/RCOG trial, which,if real, would be equivalent to the preventionof 1 preterm delivery for every 20 suturesinserted. The result is of only marginal statisti-cal significance, however, and is compatiblewith a wide range of possible effects of theoperation on the occurrence of delivery before33 weeks. The difference in the timing of deliv-ery in the MRC/RCOG trial was also reflected inimproved survival, again contrasting with thesmaller trials '.sce table 14.2).
CEIWICAL C.ERCLAGE FOR SPECIFIC INDICATIONS
As planned, possible differential effects ofcervical cerclage were investigated in sec-ondary analyses of the MRC/RCOG data strati-fied by possible indications for cerclage, suchas past obstetric history of second trimestermiscarriage or preterm delivery. or previoussurgery to the cervix, or multiple pregnancy.'Three of the strata generated in this way arebroadly similar to WOMen recruited to the otherthree trials.
Cemical cerclage after previous second trimestermiscarriage and/Or preterm delivery
Six hundred and thirty women (70%) in theMRC RCOG interim analysis had singleton preg-nancies and a past history of one or more sec-ond trimester miscarriages or preterm deliveries(but no history of surgery to the cervix). Thesecharacteristics are similar to the entry criteria ofthe South African trial.' Table 14.3 provides anoverview of the outcome in these two sub-gn nips with respect to delivery before 33 weeks
Adrian Grarrt 169
1 5 '3
Advances in the Prevention of Low Birthweight
and fetal or neonatal death. As discussed earlier,the South African trial, if anything, suggested asmall adverse effect of cerclage, but with wideconfidence intervals. In contrast, the stratifiedanalysis of the MRC/RCOG data suggests a largebeneficial effect of the operation, with estimatesof the odds ratios of 0.67 and 0.66. In fact, thisanalysis revealed that most of the differencesobserved in the primary analyses of theMRC/RCOG trial were in women with a pasthistory of second trimester miscarriage orpreterm delivery. Furthermore, the more earlydeliveries in the past, the greater the apparentbenefit.' The MRC/RCOG trial provides 80 per-cent of the data in table 14.3: this explains thetypical odds ratios of 0.79 and 0.76 with confi-dence intervals between 0.52 and 1.10. To statethese results another way, the estimate is thatthe insertion of about 18 cervical sutures willprevent 1 delivery before 33 weeks, but thisstatement cannot be made with any confidence.
Previous surgery to the cenixas an indication fir cervical cerclage
Only 96 women in the MRC/RCOG interimanalysis had a past history of cone biopsy or cer-vical amputation, and there are no women withsimilar histories in the other trials. The oddsratios for the main measures of outcome were allnear unity. but because confidence intervals arevery wide, these analyses are of little practicaluse. Far larger numbers are required.
Twin pregnancy asan indication lbr cervical cordage
The 50 cases in the Israeli trial' Were alltwin pregnancies, and there were 24 twin preg-nancies in the interim analyses of the MRC:
RCOG trial. The outcome with respect to deliv-ery before 33 weeks and miscarriage, stillbirth,an-I neonatal death for these 74 cases is sum-marized iti table 14.4; the data are too sparse toallow any conclusions. In the Dor study, 14 ofthe 50 fetuses in the cerclage group did notsurvive the early neonatal period, as opposedto 11 of the 50 in the control group. The timingof these hsses was generally similar in the twogroups. In the sutured group, three womenmiscarried in the 14th, 16th, and 17th weeks,while in the nonsutured group, two womenmiscarried in the 15th and 16th weeks. Thisdemonstrates how difficult it is to make a judg-ment in individual cases as to whether or notthe insertion of a cervical suture actuallycaused a miscarriage. Three women in eachgroup subsequently delivered prior to 33 com-pleted weeks, The extra miscarriage in thesutured group is largely responsible for the dif-ference in mortality: Thirty-nine (78%) survivedthe neonatal period in the control group, com-pared with 36 (72%) in the cerclage group.
Cervical cerclage jhr other reasons in women atmoderate or low risk (?,f early delivery
One hundred and fifty-five women (17%)included in the interim analysis of theMRC:RCOG trial had neither a previous secondtrimester miscarriage, nor preterm delivery, norprevious surgery to the cervix, nor twin preg-nancy. Many had histories of previous firsttrimester miscarriages. This stratum seems mostsimilar to the French trial, and the outcome ofthese two groups is summarized in table 11.5.Again, the confidence intervals of the typicalodds ratios are wide because the numbers ofevents are so small.
1 70 cercleNe1.5:;
EVIDENCE FROM THE RANDOMIZED TRIALS OF
POSSIBLE ADVERSE EFFECN OF CEWICAL CERCJAGE
A wide variety of possible adverse effectsof cervical cerclage (in addition to increascdobstetric intervention) were reported in theinterim analysis of the MRCIRCOG trial. It wasimpossible to ascribe many of them to theoperation with any confidence. Cervical traumaand difficulties in removing the stitches wereeach reported in 6 of the 450 women treatedwith cerclage. Pre labor rupture of the mem-branes was associated with cervical cerclage inthe South African trial, but this difference wasnot observed in the Israeli trial.' Puerperalpyrexia was reported more frequently in thecerclage group of both the MRC.,7 RCOG trialand the South African trial. This is consistentwith observational studies and appears to he 3real effect of the operation.
CONCLISIONS
The 1,655 cases entered into the four ran-domized controlled trials included in thisreview provide a less than adequate basis forclinical decisions about the use of cervical cer-clage. Three hundred more cases have beenentered into the MRC/RCOG trial; ideally, how-ever, far larger numbers are required, particu-larly for the important analyses of subgroups.
Unlike most medical treatments, cervicalcerclage has the paradoxical potential to bothprevent and cause early delivery. The balancebetween these two effects is likely to dependon the inherent risk of early delivery in thecases treated. Taking this consideration and the
Interventions
other recognized adverse effects of the opera-tion into account, it seems sensible to limit theuse of the operation to cases with a high likeli-hood of benefit. Current evidence suggests thatincreasing numbers of previous secondtrimester miscarriages or preterm deliveriesconstitute the firmest basis for making this deci-sion. There is curremly no sound evidence tosupport the use of cervical cerclage on thebasis of previous surgery to the cervix or multi-ple pregnancy.
Cervical cerclage remains unsatisfactorilyevaluated. It is unfortunate that larger numbersof randomized studies have not been conducted.Nevertheless, the trials which have been mount-ed are beginning to provide good evidenceabout the balance between the benefits and haz-ards. They should provide a template for futureresearch into the effectiveness of the procedure.
ACKNOWLEIX;MINES
I am very grateful to the Department ofHealth and Social Security for salary and othersupport. The MRC/RCOG trial was supportedby a Special Project Grant from the MedicalResearch Council.
REFERENCES
1. Grant. A. (1980). Cervical cerelage: Evaluation stud-ies. In: E. Papiernik. lirt:art and N. Spira (Eds.),Prevention of preterit; birth: New goals and newpractices in prenatta care (pp. 53-)9). Paris:INSERM.
MIZCIi.COG Working Party on Cervical Cerclage.(1985). Interim report of' the Medical ResearchCouncirlioyal College of Obstetricians andGynaecologists multicentre randomised trial of cervi-cal cerclage. British Journal qf Obstetrics andG.rnaecolug3 ,9S.
Adrian Grant 171
.16j
Advances in the Prevention qf Low Birtburight
3. Dor, J.. Shalev, J., Mashiach, C.. Blankstein, .1., andSerr. D. M. (1982). Elective cervical suture of twinpregnancies diagnosed ultrasonically in the firsttrimester following induced ovulation. Gynecologicand Obstetric Intlestigation 13, 55-60.
4. Lazar, R. Gueguen, S.. Dreyfus. J.. Renaud. R..Pontonnier, G., and Papiernik. E. (1984).Multicentred controlled trial of cervical cerclage inwomen at moderate risk of preterm delivery. BritisbJournal qf Obstetrics and Gynaecology 91, 731-735.
5. Rush, R. W Isaacs, S., McPherson. K.. Jones. L.,Chalmers, I.. and Grant, A. (1984). A randomisedcontrolled trial of cervical cerclage in women at highrisk of pretenn delivery. British journal of Obstetricsand Gynaecology 91. 724-730.
6. Rush, R. W., Keirse, M. J. N. C., liowat, R, Baum, J.D., Anderson, A. B. M., and Turnbull. A. C. (1976).Contribution of preterm delivery to perinatal mortali-ty. British Medical journal 2, 965-968.
7. Sinclair, . C. (1986). Increasing costs and effective-ness of neonatal care of very low birth-weightinfants. In: E. Papiernik, C. Breart, and N. Spira(Eds.), Pretvntion qfpreterm birth: New goaLs andnew practices in prenatal care (pp. 31-46), Paris:I NS ERM .
8. Verkxwe-Vanhorick. S. P.. Verwey, R. A.. Brand. R..Bennebrock-Gravenhorst, J.. and Keirse. M. J. N. C.(1986). Neonatal mortality risk in relation to gesta-tional age and binhweight. Lancet 1, 55-57,
Grant. A. (Forthcoming). Cervical cerclage. In: M.Enkin, M. J, N. C. Keirse. and I. Chalmers (Eds.),Efli,ctire care in pregnancy and childbirth. Oxford:Oxford University Press.
9.
172 161 Cen,ical Cerclage
Intementiolts
Statistical Findings:Cervical Cerclage: New Evidence From the Medical Research
CounciVRoyal College of Obstetricians and Gynecologists
Table 14.1
Effects of Cervical Cerclage on Obstetric ManagementEvidence from the Randomized Trials
A. Admission to hospital
Cerclage No Cerdage Odds Ratio 95% Confidence Interval
MRC/RCOG interim report (1988) 135/454 114/451 1.25 0.93-1.67
Rush et al. (1984) 30/96 19/98 1.87 0.98-3.57
Lazar et al. (1984) 85/268 41/238 2.17 1.45-3.24
typical odds ratio (95% CI) 1.55 1.24-1.93
B. Use of oral tocolytics
MRC/RCOG interim report (1988) 113/454 107/451 1.07 0.79-.1.44
Rush et al. (1984) 12/96 8/98 1.59 0.63-4.01
Lazar et al. (1984) 127/268 73/238 2.01 1.41-2.87
typical odds ratio (95% CI) 1.40 1.12-1.75
C. Induction of labor
MRC/RCOG interim report (1988) 85/454 69/451 1.27 0.90-1.80
Rush et al. (1984) 9/96 8/98 1.16 0.43-3.14
Lazar et al. (1984) 49/268 39/238 1.14 0.73-1.81
typical odds ratio (95% CI) 1.22 0.93-1.59
D Cesarean section
MRC/RCOG interim report (1988) 68/454 56/451 1.24 0,85-1.81
Rush et al. (1984) 19196 18/98 1.10 0.54-2.24
Lazar et at. (1984) 33/268 22/238 1.37 0.78-2.40
Dor et al. (1982) 9/25 7/25 1.43 0.44-4,65
typical odds ratio (95% Cl) 1.26 0.95-1.66
Adrian Grant 173
.16:2
Advances in the Pnwntion of Low Hirthweight
Table 14.2Effects of Cervical Cerclage on (A) Delivery Before 33 Weeks and (B) Miscarriage, Stillbirth, and
Neonatal Death CombinedEvidence from the Four Randomized Trials
A. Delivery betbre 33 weeks
Cerdage No Cerclage Odds Ratio 95% Confidence Interval
MRC/RCOG interim report (1988) 59/454 82/451 0.67 0.47-0.97
Rush et al. (1984) 12/96 10/98 1.26 0.52-3.04
Dor et al. (1982) 6/25 S/25 1.26 0.33-4.73
Lazar et al. (1984) 4/268 1/238 2.99 0.51-17.41
typical odds ratio (95% CI) 0.79 0.58-1.09
B. Miscarriage, stillbirth, and neonatal death
MRC/RCOG interim report (1988) 37/454 54/451 0.66 0.43-1.01
Rush et al. (1984) 9/96 9/98 1.02 0.39-2.69
Dor et al. (1982) 7/25 6/25 1.23 0.35-4.28
Lazar et al. (1984) 2/268 1/238 1.74 0.18-16.84
typical odds ratio (95% CI) 0.76 0.52-1.10
Table 14.3Effects of Prophylactic Cervical Cerclage After Previous Second Trimester Miscarriage or Preterm
Delivery on (A) Delivery Before 33 Weeks and (B) Miscarriage, Stillbirth, and Neonatal Death
A. Delivery betbre 33 weeks
Cerclage No Cerclage Odds Ratio 95% Confidence Interval
MRC/RCOG interim report (1988) 43/325 61/305 0.61 0.40-0.93
Rush et al. (1984) 12/96 10/98 1.26 0.52-3.04
typical odds ratio (95% CI) 0.70 0.48-1.02
B. Miscarriage, stillbirth, and neonatal death
MRC/RCOG interim report (1988) 25/325 41/305 0.54 0.33-0.90
Rush et al. (1984) 9/87 9/89 1.03 0.39 -2.71
typical odds ratio (95% CI) 0.62 0.40-0.98
174 16J Statistical Findings: Cervical Cerclage
Interventions
Table 14.4Effects of Prophylactic Cervical Cerclage for Twin Pregnancy on (A) Delivery Before 33 Weeks and
(B) Miscarriage, Stillbirth, and Neonatal Death
A. Delivery betbre 33 weeks
Cerclage No Cerclage Odds Ratio 95% Confidence Interval
MRC/RCOG interim report (1988) 1/10 4/14 0.34 0.05-2.40
Dor et al. (1982) 6/25 5/25 1.26 0.33-4.73
typical odds ratio (95% CO 0.83 0.28-2.49
B. Miscarriage, stillbirth, and neonatal death
MRC/RCOG interim report (1988) 1/10 1/14 1.43 0.08-25.35
Dor et al. (1982) 7/25 6/25 1.23 0.35-4.28
typical odds ratio (95% CO 1.26 0.40-3.96
Table 14.5Effects of Prophylactic Cervical Cerclage for Women at Moderate or Low Risk of Early Delivery on
(A) Delivery Before 33 Weeks and (B) Miscarriage, Stillbirth, and Neonatal Death
A. Delivery before 33 weeks
Cerclage No Cerclage Odds Ratio 95% Confidence Interval
MRC/RCOG interim report (1968) W73 7/82 0.96 0.31-2.98
Lazar et al. (1984) 4/268 1/238 2.99 0.51-17.41
typical odds ratio (95% CI) 1..34 0.52-.3.47
B. Miscarriage, stillbirth, and neonatal death
MRC/RCOG interim report (1988) 3/73 5/82 0.67 0.16- -2.77
Lazar et al. (1984) 2/268 1/238 1.74 0.18-16.84
typical odds ratio (95% Cl) 0.87 0.26-2.92
Adrian rant 175
1 E;
Prevelltiota of IntrauterineGrou7th Retardation with
Aiitiplatelet TheraAp
SERGE UZAN, M.D.
M. BFAtEts, W.).M. tizAN
CTION
The treatment of intrauterine growth retarda-tion (with or without associated hypertension)and complications of pregnancy-inducedhypertension (e.g., preeclampsia, eclampsia,and abruptio placenta) is most often purelypalliative. Delivery of the fetus is usually theonly cure, which often results in serious pre-maturity and neonatal problems.
Numerous studies" have attempted toanalyze the phenomena responsible for thesecomplications. As a result, the following ele-ments have been clarified to date:
1.Preeclampsia is often associated with a dis-
seminated intravascular coagulopathy with areduction in the platelet count. a consump-
Adtwnces in the Prevention of Low Birthweight
tion of factor VIII. and an augmentation offibrin degradation products. The microscopicand grossly visible placental thromboticlesions which are commonly seen are a eon-sequence of these coagulation disturbances.
2. These placental infarcts appear to be associ-ated with the presence of fibrin deposits inthe intet-villous spaces. In certain cases, suffi-cient fibrin is accumulated to produce a trueretroplacental hematoma. In addition, similarfibrin deposits are commonly found in otherorgans (e.g., the liver or the brain). Thesefindings encourage us to believe that thecoagulation abnormalities observed inpreeclampsia are critical to the developmentof both maternal and fetal complications.
In pregnancy-induced hypertension, anincrease in the production of thromboxane A-)(TXA)) is often found. This product (the princi-pal metabolite of arachadonic acid in platelets)is a powerful vasoconstrictor and a stimulatorof platelet aggregation. The origin of theenhanced production of TXA2 appears to be atthe level of the placenta and the platelets them-selves. The increase in TXA2 without a corre-sponding increase in the production of"prostacyclin leads to a relative predominance ofthromboxane A-) in the uteroplacental circula-tion. Prostacyclin works in opposition to throm-boxane A). both in terms of vascular tone andplatelet function. This imbalance 1)etweenthromboxane A ) and prostacyclin ) is believedto be due to pathological interactions at theplatelet-platelet and platelet-vascular level.
Previously, research teams have attemptedto treat preeclampsia with heparin. Results havebeen either disappointing or. at best, transitory.
In our opinion, this ineffectiveness may havebeen due to relative late initiation of therapy.
In one epidemiological study, Crandon4reported that women who frequently usedaspirin had a decreased incidence of gestationalhypertension or, if present, fewer additionalcomplications such as preeclampsia.
By 1978, we had decided to establish astudy which examined the effectiveness of thecombination of aspirin and dipyrimadole in theprevention of pregnancy-induced hypertensivecomplications. There were several reasons forthis choice. First, aspirin effectively impedesplatelet aggregation, probably through inhibi-tion of platelet cyclooxygenase. which thenresults in blockage of the synthesis of throm-boxane A2. Second, aspirin has been extensive-ly prescribed by cardiologists to reducethrombotic complications in patients with valvu-lar protheses and following coronary arterysurgery. Lastly, aspirin has been used to preventrecurrences of arterial thrombotic problems.
The majority of authors' '' have utilizedsmall dosages of aspirin (less than 150 mg perday) in order to preset-ve the beneficial effectsof prostacydin. the hypothesis being that thesynthesis of prostacyclin in the vascularendothelium is less sensitive to aspirin inhibi-tion than that of thromboxane A) in platelets.
The second medication, dipyrimadole.'"has been associated with aspirin in a numberof studies; however, it has been difficult to dis-tinguish its specific action from that of aspirin.Through its inhibition of phosphodiesterase. itmay potentiate the action of aspirin by retard-ing the destruction of adenosine monophos-phate. thus making platelets more sensitive toprostacyclin. Dipyrimadole may also have an
178 Prevention qf IntrauterktiVmwth Retardation with Antiplatelet 'Therapy
autonomous action; it may stimulate prostacy-din synthesis in platelets.
These considerations logically support theproposal of aspirin and dipyrimadole as a pre-ventive therapy modality for pregnancy-induced hypertension.
We will first examine a review of the thera-peutic trials using aspirin and/or dipyrimadole.Tables include only statistics from published tri-als; inf(wmation from brief or oral communica-tions and studies in progress will he includedin the discussion.
These studies can be analyzed accordingto four criteria:
1.What were the criteria for inclusionintrauterine growth retardation exclusively, orcomplications of gestational hypertension ingeneral?
2. Was the study prospective?
3. Were the patients randomized?
4. Was there a placebo-cmtrol group?
At this time, to our knowledge, five con-trolled studies exist: The study by our groupbegun in 1978;s the study by Wallenburg pub-lished in 1986;m the study by Wallenburg pub-lished in 1987;- and the two multicentric studiescurrently in progress in France and in Belgium(group Peigar and group Epreda ). Table 15.1summarizes different aspects of' these studies.We will next examine the meth( yds and resultsof the three studies actually completed.
MATERIAL AND METIIODS
For each study, we have indicated the cri-teria for inclusion, treatment regimens, gesta-
Ititenvntions
tional age at onset, number of patients includ-ed, and number of pregnancies observed (seetable 15.2).
The expression treatment utilized meansuniquely antiplatelet aggregation therapy. Othermore traditional antihypertensive medicationsare not specified.
Concerning criteria for inclusion, the fol-lowing should be noted:
1. Study A (see table 15.1) has a heterogeneousrecruitment (this is probably one of its princi-pal faults). A certain number of patients areeven selected under the heading, -vascularrisk."
2. Study B has an original and interesting selec-tion process in that it proposes a method fortesting nulliparas. Their criteria for inclusionis an increased sensitivity to an intravenousangiotensin 11 challenge. A response is con-sidered positive if diastolic blood pressurerises by 20 mm Hg at a dose equal to or lessthan 10 mg/kg/min.
3. The three final studies used fetal weightrelated to gestational age at delivery of eitherone or two preceeding pregnancies as thesole criterkm for admission.
REst 'ut's
The principal criteria evaluated duringthese studies are shown in table 15.3. Thenumbers and the mode of expression (i.e.,abso:ute numbers or percentages) are as pub-lished. When two numbers are listed, the firstcorresponds to the control group, and the sec-ond to the treatment group.
Serge Uzan et al. 167 1 79
Advances in the Pret,ention of Lou Birthuvight
Disu SSION
Before beginning the discussion of results,it appears more logical to comment on the cri-teria of inclusion, certain ethical problems, theoptimal dosage, and the possible adverseeffects of this therapy.
criteria Jiff incluskmThe most k)gical selection process (and the
method being used for the two studies inprogress) is to use prior 11.1GR confirmed atdelivery as the criteri( n for inclusion. It is theonly One that can be considered objective. Thetwo studies (I) and E on table 15.1) includetwo types of patients classified according towhether there have been one or two priorepisodes of It GR. This stratification attempts toidentify future indi,.ations for therapy. Perhapsthe benefits of therapy will be shown to out-weigh the risks when the probability of recur-rence is high (i.e., when there have been twopreceding pathological pregnancies).
Trial B, using the angiotensin II sensitivitytest as its inclusion criterion, resolves only par-tially the problem of identification in primiparas.
Ethical OmsiderationsParticipation in a study such as this posed
numerous ethical questions which were dis-cussed at length by our ethics committee. Theprincipal point of debate was whether or not itwas apprc)priate to propose to women with ahistory of two prior pathological pregnanciesthat they attempt a third pregnancy with a pos-sible placebo. Wallenburg chose not to enterhis patients into an internal control groupbecause of his implicit belief in the following
two arguments: (1) That the efficacy of treat-ment was beyond any doubt (in our Opinion,this position was not sufficiently admissible);and (2) that the treatment was innocuous (inOur opinion, this argument was also uncertain).Because we believed that formal proof did notexist for either of these two arguments, we feltthat our study was justified.
Optimal DosageIn our first study, the treatment regimen of
150 mg aspirin per day with 300 mg dipyri-madole per day was used; however, it
appeared that even smaller doses might be aseffective. Dosages currently being used arebetween 1 and 2 mg/kg/day for aspirin and225 mg/day for dipyrimadole. In Wallenburg'sstudy (1987), it was shown that dosages ofaspirin as low as 50 mg/dav and of dipyri-madole as low as 22i mg/day significantlydiminished production of platelet thromboxaneA2, which was inferred indirectly through mea-surements of malondialdehyde. Concentrationsof makmdialdehyde, a stable byproduct ofplatelet thromboxane synthesis, were reducedto 5- 10 percent of baseline levels. On the otherhand, levels of 6-oxoprostaglandin El, a prosta-cyclin Metabolite, were not significantlydecreased. Both of these observaticms lend fur-ther support to the effectiveness of low doseaspirin and dipyrimadole.r.
Each c)f the three completed studiesunequivocally- demonstrated in its treatmentgroup (whether randomized or in comparimmwith the controls) the following findings: ( I) Areduction in the rate of intrauterine growthretardation, and (2) a reduction in the rate ofsecondary complications.
ilL
180 Prevention of Intrauterine Groulb Retardation u'ith Antiplatelet Therapy
The above findings were also indirectlyconfirmed by other parameters. Placental exam-ination revealed a reduction in placentallesions: and our study (as noted in table 15.4)demonstrated an improvement in plasma vol-ume, plasma uric acid, and platelet count.
In our study, the duration of pregnancy atthe time of delivery in the treatment group wasincreased significantly, whereas in Wallenburg'sstudy (1987). it was one to two weeks shorterin the treatment group than in the controlgroup. This latter difference was not significant.
The disparity between the two studies may per-haps be explained by population differences,with an usually high incidence of prior uterinescar and repeat cesarean section in
Wallenburg's treatment group when comparedwith his control group.
In our study (and we believe it will heconfirmed by the larger study in progress). thereduction in prematurity is one of the majorbenefits of treatment.
In all three studies, no hemorrhagic compli-cations were n()ted in either mother or ne(mate.In addition, no fetal malformations wereobserved in any of the treatment groups thatcould be attributed to the medications. In ourstudy, several patients receiving dipyrimadolecomp4led of headaches. These regressedrapidly with reduction in the dipyrimadole dose.Cessation of treatment was never required.
It seems premature, however, to concludethat the treatment regimen is innocuous.
When considering the potential adverseeffects of aspirin, it is important to note thatthis medication does not generally modify the
classical coagulation parameters except for
those of platelet aggregation. In practice. bleed-
Inten'entions
ing time (as measured by the IVY method,which is the most reproducible) is necessary toevaluate hemostatic changes. In patients receiv-ing low-dose aspirin, significant prolongation oftheir bleeding time may occasionally beobserved. Moreover. after stopping aspirin ther-apy, a delay of six to eight days is usuallyrequired for normalization of platelet function.
Several publications have reported inci-dences of maternal hemorrhagic complicationsat the time of delivery and neonatal cutaneousand mueosal lesions in WOInen consumingaspirin." It must he noted. however, that thesestudies involved considerably higher dosages ofaspirin. The same explanation can be madeconcerning the study by Daffos, in which hereported an umbilical cord puncture associatedwith a moderately severe fetal coagulation dis-turbance in a woman taking aspirin.
Cases of premature closure of the ductusarteriosus have been described in women onaspirin therapy (again, dosages were largerthan those in our study).
CONCU 'SION
It is our belief that aspirin and dipyri-madole will be shown to be an effective thera-py in the prevention of intrauterine growthretardatk)n in women who have had a prk)rsimilarly complicated pregnancy. and perhapseven more significantly effective in womenwith a history of two abnormal pregnancies.This treatment modality appears to be botheffective and equally devoid of major risks. Acontrolled randomized double-blinded studywith a placebo group. however, is felt to be
Sew Uzan et al. 181
Advances in the Pret,ention qf Lou Birthuvight
necessary before encouraging utilization ofthese medications. In addition, the respectiveroles of aspirin and dipyrimadole need to beclarified. This study is currently in progress.
REFERENCES
1. fr.eI d..man, S. A. (1988). Preeclampsia: A review ofthe role of prostaglandins. Obstetetrics andGynecology 71, 122-137.
2. Stuart. M. J.. Sunderji. S. G.. Yambo. T. et al. (1981).Decreased prostacyclin production: A characteristicof chronic placental insufficiency syndromes, lancet1. 1120-1128.
3. Walsh, S. W. (1985). Preeclampsia: An imbalance inplacental prostacydin and thromboxane production.Anwrican Journal qf Obstetetrics and 6.'ynecology152. 335-3-+0.
4, Crandon, A. J.. and Isherwood. D. M. (1979). Effectof aspihn on incidence of preechunpsia. lancet 1.1356.
5. Beaufils. M.. Uzan. S.. Donsimoni. R.. and Colau. J.C. (1985). Prevention of preedampsia by earlyantiplatelet therapy. Lancet I. 840-842.
.6. Elder, M. G.. De Swiet. M.. Robertson. A., Elder. M.and Hawkins, D. F ( 1988). Low-dose
aspirin in pregnancy. lancet 1. 4 10,
7. Lubbe. W. E. (1987). lAnv-dose aspirin in preventionof toxemia of pregnancy: Does it have a place?Dnigs 5I5-518.
8. Wallenburg, 1.1. C. S.. Makovitz..I. W.. Dekker. C. A..and Rotmans. N. (198(3). Low dose aspirin preventspregnancy-induced hypertenskm and preeclampsiain angiotensin-sensitive primigravidae. Lancet 1. 1.
9. Wallenburg, 11. C. S.. and Rotmans. N. (1987).Prevention of recurrent idi()pathic fetal growth retar-dation by low dose aspirin and dipyridamole.American Journal of Obstetetrics and Gynecology157, 1230-1235.
10. Moncada. S.. and Korbut. R. (1978). Dipyridamoleand other phosphodiesterase inhibitors act as anti-thrombotic agents by potentiating endogenousprostacv din. Lancet 1. 1286-1289.
II. Masotti, G., Poggesi, L., cialanti, G., Abbate. R., andNeri Semen. G. G. (1979). Differential inhibition ofprostacyclin pn)duction and platelet aggregati(ni byaspirin. lancet 2. 1213-1216.
12. Pedersen. A. K., and Fitzgerald. G. A. t198.1), Dose-related kinetics of aspirin: Presystemic acetylation of'platelet cyclooxygenase. Neu' Englwa Journal ofMedici,w 311. 12(X1-1211.
13. Stuart. M. J.. Gross. S. J.. Elrad. 11., and Graeber. J. E.(1982). Effects of acetylsalicylic acid ingestion onmaternal and neonatal hemostasis. New EnglandJournal (tf Medicine 307, 909-912,
1 7 )
182 Prevention qf Intrauterine Growth Retardation ulth Antiplatelet Thempy
Interventions
Statistical Findings:Prevention of Intrauterine Growth
Retardation with AntVatelet Therapy
Table 15.1Design Characteristics of Five Reviewed Studies
A
Prospective + +
Randomization + +
Double-blind +
Placebo control +
Date 1978-1984 *-1986
+ + +
+
4- +
+ +
1983-1986 1985-* 1985-'
* Start date ti)r Ntudy not available Study not completed at the time ot this wnting.
Table 15.2Sample Sizes and Other Criteria of Five Reviewed Studies
A
Criteria for IUGR Acc. HTN I Pare Test IUGR > 2 RJGR: 1 IUGR: 1
Inclusion HTN ess. Terrain Angio II IUGR > 2 IUGR > 2
Treatment
group 1 Asp. 150 Asp. 60 Asp. 60 Asp. 150
Dip. 300 Dip. 225 Dip. 225 Dip. 225
group 2 0 0 0 Placebo Asp. 150
group 3 Placebo
Gestational Age 16 28 16 16 16
at onset
Number of Patients 93 44 48 300* :300*
Number of Pregnancies 93 44 57 300 300
Serge trzan et al. 171 783
Advances in the Prevention qf Low Birthuright
Table 1 5.3*
Summary of Results of Three Completed Studies
Treatmentgroup
AControlgroup
Treatmentgroup
Controlgroup
Treatmentgroup
Controlgroup
Number of pregnancies 48 45 21 23 30 27
Premature births 12 r3 4 0
Mean gestational age at delivery 36.5 38.6 39 40 38 37
IUGR p 3 7 0 3 0 7 0
IUGR p 10 13 4 6 4 16 4
Hypertension 22 19 4 2 15% 6%
Intrauterine fetal development :3 0 0 1 0 1
IUFN + Neonatal death 5 0
Abruptio placenta 3 0
Preeclampsia 6 0 7 0
Edampsia 0 0 1 0
Cesarean sections 13 8 7 111% 44%
Birthweight 2625 3172 3040 3190
Normal pregnancies 12 29
Placental weight 509 599
'Whet tvro numbyri arc Iistod. the first corrcvonds to the control group.
Baseline:
Table 15.4Evolution of Biomechanical Monitors
Treatment Group (N--.48) Control Group cv,45)
Plasma uric acid (um01/1) 221 + 62 220 4- 52 NS
Platelet Count (x1.000/m1) 245 + 57 233 + 59 NS
Week Prior to Delivery
Plasma Uric Acid 270 + 69 293 + 83 NS
Platelet Count 249 + 66 209 + 57 < 0.02
Plasma Volume 56 + 7.5 49 + 8.1 < 0.02
184 Statistical Findings: Prevention (y hitrauterine Growth Retardation u'ith A ntiplatelet Therapy
Does Calcium SupplementationReduce Pregnancy-Induced
Hypertension and Prematurity?
JOSE VELAR, M.D.
J.M. BELIZAN. M.D.
J.T. REME, M.D.
INTRODLTCTION
Pregnancy represents a period of veryhigh calcium demand. There is an increasedfetal requirement resulting in a total calciumaccumulation at term of approximately 30 g,30 percent of which is deposited during thethird trimester. Some of the maternal adaptivemechanisms that could compensate for suchhigh fetal demands are partially inhibited dur-ing pregnancy.) Furthermore, pregnancy hasbeen suggested to be a period of "obligatory"high urinary calcium output,- while maternalbone calcium is protected. Finally, althoughintestinal absorption of calcium can increase,4this is associated with an increased parathyroidhormone secretion during pregnancy.
17J
Advances in the Prevention qf Lou' Birthweight
It is possible, therefore, that when preg-nant women are put in a nutritional situationthat can alter this metabolic balance, they canbe at higher risk for pathological events thathave calcium-dependent mechanisms. Thiscould affect smooth muscle contractility of thevascular system and uterus. Several epidemio-logical studies in pregnant and in normotensiveand hypertensive subjects consistently showedan inverse relationship between calcium intakeand blood pressure.' ''
Randomized controlled clinical trials of cal-cium supplementation in normotensive women,men, and mildly hypertensive patients havedemonstrated a significant reduction in bloodpressure. Data from two randomized clinical tri-als show a significant reduction in blood pres-sure in the calcium-supplemented group at term(see figure 16,1). Furthermore, a dose-effect rela-tionship is observed when our two studies arecombined (see figure 16.2). The effect is maxi-mized with a daily dose of 2.0 g of calcium andis less with 1.0 g of calcium supplementation.
Based on this information, we developedthe hypothesis that calcium supplementationduring pregnancy can decrease the incidenceof pregnancy-induced hypertension (PHD/preeclampsia and preterm delivery when com-pared with the placebo group. The effect couldbe mediated by reducing smooth muscle ten-sion (e.g., vascular and uterine),
BACKGROI 'NI) INFORNMON:
THE RELATIONSHIP BEFWEEN CALCIV:k1
SIPPLEMENTAPION AND PH 1/PREE0A\1pstA
Table 16.1 presents summary data fromfour studies that provided information on the
effect of calcium supplementation orPIII/preeclampsia rates, Three randomizedplacebo controlled clinical trials and oneuncontrolled matched study were conducted.In one of our clinical trials, which was notdesigned to evaluate the incidence of PILL theplacebo group had a relative risk of 2.8 ofdeveloping P111 as compared with the calciumgroup (11.1% V. -4.0%): A preliminary reportfrom a randomized clinical trial conducted inEcuador demonstrated that the group receiving2.0 g of calcium a day (V = 46) had an inci-dence of PHI of 6.5 percent, as compared witha placebo group (X = 16) which had an inci-dence of 28.2 percent < 0,011.° Finally, a ran-domized controlled clinical trial was conductedin India in a population with a dietary calciumintake of 500 mg/day. The study populationwas randomly assigned to a dietary intake of375 mg/day of elemental calcium and 1200 IVof vitamin D/day or to a placebo group. A non-statistically significant reduction in the inci-dence of preedampsia (> 140/90 mm Hg andurinary proteins > 300 mg/21 hrs) (6%) wasobserved in the calcium-supplemented groupCV = 188) as compared with the placebo group(9%) LV = 182). It should be remembered that,to detect a difference of this magnitude with aa = 0.05 and a power between 76 and 8,4 per-cent, it would have been necessary to study atleast 8(X) patients in each group. When resultsfrom the three randomized controlled trialswere pooled using the Mantel and Haenszelmethod," women receiving calcium supple-mentation had a statistically significant reducedrisk for pregnancy-induced hypertension,pooled or typical OR = 0.41 (95, CI 0.39-0.78).as compared with the placebo group.
171
188 Does Calcium Supplementation Reduce Pregnancy-Induced IIypertension ciul Premattolty?
PRELIMINARY EVIDENCE OF 11IF EFFIVI OF
CALCILM St l'PLEMEN1ATION ON PREGNANCY-
INDUCED HYPERTENSION/PREECIAMPSIA
We will present here preliminary results ofa double-blind, randomized, controlled clinicaltrial of the effect of 2.0 g of elemental calcium(calcium carb)nate) a day or a placebo that isbeing conducted in two different populations.A white lower middle class population wasstudied at the Centro Rosarino de EstudiosPerinatales, Rosario, Argentina. All patientswere nulliparous and clinically healthy. At thetime of this presentation, 26 patients had beenenrolled and delivered their infants. The sec-ond population was obtained from theAdolescent Pregnancy Clinic of the JohnsHopkins Hospital, Baltimore, Maryland. ByMarch 1988, 177 patients had been enrolledand delivered. All patients were less than 17years of age at the time of recruitment. Most ofthe subjects were nulliparous with a known lastmenstrual period ( L.MP) and had singletonpregnancies. All were free of any underlyingmedical disorders, as determined by history,physical examination, and laboratory tests.
Participants in bc)th centers were ranclinnlyassigned in a double-blind fashion before 26weeks' gestation to one of the two treatmentgroups using a randomization schedule pre-pared in advance for each population. Amongwhite women. 230 were assigned to the calci-um-supplemented group and 196 to the place-bo group. Among black women, 85 wereassigned to the calcium-supplemented groupand 89 to the placebo group. Prenatal care wascarried out according to the protocols of eachparticipant's hospital. The study prcnocol was
Jose tillar et al.
Intentqltions
approved by the ohns fiopkins Hospital's JointCommittee on Clinical Investigation.
Figure 16.3 summarizes the study design,criteria for patient eligibility, and follow-uprequirements. The calcium-supplementedgroups received four tablets of calcium carbon-ate per day. Each of these tablets provides 500mg of elemental calcium, for a total of 2.0g/day. The placebo group received four tabletsof the same w,Aght, size, color, and organolep-tic characteristics as the calcium tablets.
Both centers implemented a very elaboratemechanism of monitoring tablet intake andcompliance as well as data quality control.Treatment compliance evaluation includedquestioning patients on pill intake, pill count-ing at every visit (percentage of pillstaken,'expected number of pills in that period).changing bottles at fixed times, and countingremaining tablets and urinary excretion of calci-um in a random sample of patients.
Blood pressure, one of the main outcomes,was obtained by trained personnel workingexclusively for the study; continuous monitor-ing and quality control mechanisms wereimplemented. All blood pressures wereobtained using random zero sphygmomanome-ters. Table 16.2 presents reliability evaluation ofblood pressure measurements in the three par-ticipant hospitals of the Argentina center. Itshows high agreement values between the fielddirector and the study nurses. Table 16.3 pre-sents, as an example, evidence of high repro-ducibility of the blood pressure measure duringpregnancy at the Ilopkins center, as well as akm. zero terminal digit preference for the pm-ject coordinator.
Table 16.4 summari;.es the primary out-
175 IH9
Advances in the Prevention of Low Birthweight
come variables and the definitions used in thisstudy. Blood pressure values, used indepen-dently or with proteinuria obtained by thestudy nurses or project coordinator, and thediagnosis of PHI and/or preeclampsia made byobstetricians in charge of the clinical care of thepatients, but unrelated with the study, wereused as one of the primary outcomes.
Gestational age, obtained by using the bestobstetric estimation, which includes any ultra-sound measure, LikIP, uterine height, and thetime of the first fetal movements detected, wasused to calculate the incidence of prematurity(< 37 weeks).
In the Argentinean (white) population,women enrolled in the calcium-supplementelgroup took 87 percent of the total expectednumber of tablets, similar to 86 percent in theplacebo group. In the Hopkins population,although compliance fk ures were lower. theywere very similar between the calcium-supple-mented and placebo groups (66% V.respectively). The calcium-supplemented andplacebo groups were very similar in most ofthe sociodemographic and baseline characteris-tics for the black and white populations. Therevvre, however, differences in maternal weightat randomization, with white patients in the cal-cium-supplemented group and black women inthe placebo group statistically significantlyheavier.
Table 16.5 presents the effect of calciumsupplementation on the incidence ofPIII/preeclampsia. The calcium-supplementedgroups had a lower incidence of Pill, as wellas a lower incidence of preeclampsia in thewhite population and lower incidence of pro-teinuria in the black population (NS). The rates
190
observed in the calcium groups were almosthalf the values obtained in the placebo groups.The rates of preeclampsia were not presentedfor the black population because the indepen-dent clinical diagnoses were not available atthe time of this presentation. At term, however,the placebo group had higher mean systolicblood pressure 115 (+ 9.9) mm 11g, as com-pared with the calcium group 109.4 (+ 11.2)mm Hg < 0.01), and higher diastolic bloodpressure 74.2 H- 6.5) mm Hg versus 68,7 (+ 9.1)mm Hg < 0.01) than the calcium group.
Table 16.6 presents the incidence of pre-maturity V 37 weeks) and LBW V 2500 g) bytreatment for the two studied populations. Thecalcium-supplemented groups had a lower inci-dence of preterm deliveries, 5.4 percent forwhites and -7,1, percent for blacks, than theplacebo groups, 9.9 percent for whites and 19.1percent for blacks. The incidence of LBW wasalso lower in the calcium group; however.among whites, the magnitude is smaller.Among blacks, those supplemented had anincidence of low birthweight of 10,3 percent,compared with 20.0 percent in the placebogroup (p= 0.07).
DISCI'SSION
We have presented preliminary informa-tion on the effect of calcium supplementationon gestational age, blood pressure. andPIH/preeclampsia. In agreement with previousreports (see table 16.1). there is a systematicreduction in blood pressure values and newevidence of reduction in prematurity in the cal-cium-suppk.mented grtnips. There is also pre-
17,
Does Calcium Supplementation Reduce Pregnancy-Induced 113pertension tind Prenuaurity?
liminary evidence from the white populationthat calcium supplementation can prevent thedevelopment of preeclampsia. Nevertheless,caution should he exercised in interpretingthese results. They are obtained from two trialsin progress, and some of the results could bemodified when all of the patients are recruitedand analyzed. It is unlikely, however, that theobserved direction of the effect will changedramatically. There remains a need to furtherelucidate the mechanism whereby calcium sup-plementation exerts its effect. Previous reportshave suggested possible effects on parathyroidhormone,' plasma renin activity,'' and serummagnesium.''
Increases in parathyroid hormone (PM)have been shown to increase intracelluhir calci-um in several cell types. The presumed mecha-nism is an increase in membrane permeabilitywith subsequent facilitated movement of calci-
um via slow channels from the extracellular tothe intracellular compartments. The questionremaining is what effect lcmg-term calcium sup-plementation will have on PTH, and whetherchronic suppression of PTH will in fact result inlower levels of intracellular calcium.
We have previously repurted that, in preg-nant individuals with initial low levels of plas-
m a renin activity (PRA), calcium supplementa-tion resulted in a greater reduction in bloodpressure than in women with higher initialPRA." The uterine vascular bed, being sensitiveto angiotensin II, may be affected by calcium-induced changes in plasma renin activity.
Patients with renin-dependent hyperten-sion frequently have depletion of magnesium.Our previous report" has also demonstratedincreased serum magnesium levels among
Interventions
those pregnant women receiving calcium sup-plementation. The role of magnesium in hyper-tension has been well established. Its role asan efficacious tocolytic has also been wellestablished.'" There is a consistency in theseobservations. The interaction of calcium,parathyroid hormone, plasma renin activity,and magnesium results in alterations of intracel-lular calcium. The reduction of intracellular cal-cium will result in myocyte relaxation. There is
no reason to believe that this effect is limited tothe vasculature. A similar effect should beexpected in the myometrium, with resultantrelaxation of the uterine smoth muscle. Thisalteration of intracellular calcium (i.e., reduc-tion) is presumably the final common pathwayin the action of betamimetics, magnesium sul-
fate, prostaglandin synthesis inhibitors, and cal-cium channel blockers. Thus, it is notinconsistent to expect that calcium supplemen-tation could have an effect not only on blood
pressure but on uterine activity, and thereforeon gestational age, and, ultimately, birthweight.While the results presented here are clearlypreliminary, we suggest that they are provoca-tive and encouraging. Further research at theclinical and basic science levels will be neededto better characterize the role of calcium inhuman reproduction.
ACKM MI.FGMENT
Partially supported by grants from theNational Dairy Board, the National DairyCouncil, and the International DevelopmentResearch Center (IDRC), Ottawa, Ontario,CANADA.
Jose tillar et al. 191
17?
Advances in tbe Prer'ention of Low Birthweight
REFERENCB
1. Belizan, J. I. Villar, J., and Repke. J, (19881. Therelationship between calcium intake and pregnancy-induced hypertension: Up-to-date evidence.American Journal cy Obstetrics and Gynecology 158,898-902,
2. Duggin, G. G.. Lyneham. R. C., Dale, N. E.. Evans,.A.. and Tiller, D. J. (1974), Calcium balance in preg-nancy. Lancet 2, 926.
3. Reynokls, \X'. A., Williams, G. A.. and Pitkin. R. M.(1981). Calcitropic hornume resp(msiveness duringpregnancy. American Journal (1 Obstetrics andG:ynecology 139, 855,
Ileaney. R. P.. and Skillman. T. G. (1971). Calciummetabolism in normal human pregancy. journai ofClinical Endocrinology and Metabolism 36.661.
5. Villar, J., Repke. J.. and Belizan, 3. M. ( 1986),Calciutn and blood pressure. clinical Nutritm S.153-160.
6, Parrot-(,arcia, M., and NIcCarron, 1). A. t 1984).Calcium and hypertension. Nutrition Reviews -12.205.
7, Villar, J.. and Belizan. J. M. (198( ). Calcium duringpregnancy. Clinical Nutrition 5, 55-62.
8. Villar, I., Repke. J.. and 13elizan, J. NI. ( 198').Calcium supplementation reduces blood pressureduring pregnancy: Results from a randomized con-trolled clinical trial. Obsteiric$ and (iynecology '0,317-322.
9. Marya. R. K.. Rathee. S. and Manrow, M. (198).Effect of calcium and vitamin 1) st/nplementation ontoxemia of pregnancy. (O'nech/gic and obstetricItutestigation 24, 38-42.
10. Lopez-Jaramillo P.. Narvaez NI.. Weigel R. I. andYepez R. (1989). Calcium supplementation reducesthe risk of pregnancy-induced hypertension in anAndes populatkm, British Journal qf Obstetrics andGynecology 19, 6.18-1i5S.
11, Kawasaki. N.. Matsui. K., Ito. M. et al. (1985). Effectof calcium supplementation on the vas( ular sensitivi-ty to angiotension 11 in pregnant women. Americanjournal c!f Obstetrics and Gynecology 153, 570-582.
12. Mantel, N., and Haenszel, NV, (1959). Statisticalaspects of the analysis of data from retrosp....ctivestudies of disease. journal of the National (.-incerInstitute 22. 719-748.
13. Altman, 1).. and Elbourne. I), Combining resultsfrom .several clinical trials. British journal ofObstetrics and Gynaecoh)gy 95, 1-2,
Repke, J. T., Villar. J.. Anderson. C,, Pareja,Dubin. N.. and Belizan. J. (Forthcoming).Biochemical changes assodated with calcium supple-mentati( n induc.:d bl(x)d pressure reduction duringpregnancy. American journal of Obstetrics a ul d6:311000logr,
IS. Resnick. 1.. M.. Laragh, J. 11., Sealey, J. E., andAlderman. M. It (1983). Divalent cations in essen-tial hypertension: Relati( Ms between serum ionizedcalcium, magnesium and plasma renin activity. Neu.England Journal (d.tfediciiie 309, 888.
16. Petrie. R. NI. (1981/. Tocolvsis using magnesiumsulfate. Seminars in l'erinatoh,gy 5, 266-27-3.
17s192 Does Calcium Supplementation Reduce Pregnancy-Induced IIJpertension and Prematurity?
Interventions
Statistical Findings:Does Calcium Supplementation Reduce
Pregnancy-Induced Hypertension and Prematurity?
Table 16.1Incidence of Pregnancy-Induced Hypertension (PIK Data From Calcium Supplementation Studies
Study
Elemental CalciumSupplement (mg/day)
Total CalciumIntake (mg/day)
Blood Pressure(mm Hg)
PIM incidence (Percentage)Calcium Placebo
Kawasaki, N. et As 156 942 No effect 4.5 21.2 p < 0.10(22) (66)
Villar et al. 1500 900 4-5 4.0 11.1 NS
(24) (25)
Marya R. et al. H 375 500 4-7 6.0 9.0 NS
1,200 L11 Vit D (188) (182)
Lopez jaramillo 2,000 300 6.5 28.2 p < 0.01
NOn-R4n(jiV771./i0---Nio Place4)0
t Source:Kawasaki N., Matsui K., Ito M. et al. i198S). Lttect of calcium supplementatitm on the vascular sensitivity to angiotension II in pregnant
women. American journal 01 Oh5fetric s and Gymvology, 153, 576-, 582.
Source: Villar 1., Rvpke I., and Belizan I. M. 1 987). Cak ium supplementation reduc es blood pressure during pregnant v: Result from a random-
ized controlkd clinical trial. Obstetric and (ynecolergy, 70, 117-322.
It Sourcv: Marva R. K., Rathee S. and Manrosv M. (1987). Eftec t ot cal( iurn and t namin D supplementation on tosemia of pregnant v Gyne(ologic
and CThstetric investigation, 24, 38-42.
f Source.: Lopez-laramillo P., Narvaez M., Weigel R.14., and fvfx'l R. ( 989). Calc ium supplementation redu«.s the risk ot pregnancy-induced hyper-
tension in an Andes population. British lournal of Obstetrics and Gvnec okigy. 19, 648-655.
Preeu lampsia (> 140/90 rnm I fg and urinar proteins > 100 ry1,1/..!4 hours
Table 16.2Reliability of Blood Pressure Measu(ements
Rosario, Argentina (Whites)
tV Systolic Diastolic
Hospital A 58 0.82* 0 81
B 28 0.77 0.50
C 54 0.74 0.81
" Correlation cc.)ettit rents between field dire( tor and stuch. nirrws
Jose t'illar et al.
Table 16.3Reliability of Blood Pressure Measurements
Johns Hopkins Hospital (Blacks)
A. correlation coefficients between blood pressure valuesby estationaI age for project coofdinator
Weeks of Gestation Systolic Diastolic
28 v. 30 0.76 0.63
32 v, 34 0.61 0.51
36 v, 38 0.81 0,71
38 v. 41 0.66 0.65
13. Zero terminal digit preference (N 1,011 measures)
Systolic 14.1 no
Diastolic- 13.1 MO
17 (;) 193
Advances in the Prevention of Low Birtinveight
Table 16.4Outcome Variables for the Randomized Clinical
Trial of Calcium Supplementation DuringPregnancy
Blood Pressure (mm Hg)(study nurses and project coordinator)
Random zero sphygmomanometer(diastolic B.P. 4th and 5th found)
Seated position (Hopkins)
Supine and lateral (Argentina)
Proteinuria: 300 mg/I proteinuria two timesmore than 6 hours apart
(Argentina)
> 300 mg/1 or (+) (Johns Hopkins)
Clinical diagnosis of PIH or Preeclampsiamade by obstetricians not related to the study
Gestational age (weeks)
Best OB estimation (ultrasound. LMP,uterine height, fetal movements)
Physical examination newborn
Birthweight (grams)
Table 1 6.5Effect of Calcium Supplementation on
PII-1/Preeclampsia: A Randomized Double-Blind Controlled Clinical Trial
Whites BlacksPreeclampsia
BP' > 140 BP* and > 300 > 300 mg/mm Hg and/or mgi Proteinuria
Proteinuria Proteinuria
Calcium 11.7 (230) 1.7 (230) 5.9 (68)
(2.0 g/day) (NS)
Placebo 19.4 (196) 3.6 (1%) 11.4 (70)
Treatment started tx.tm 20 and 26tseeks" gestat2 times > 6 hours> 300 mg/1= (+)
Table 16.6Effect of Calcium Supplementation on the
Incidence of Prematurity and Low Birthweight
Whites
Preterm(< 37 weeks)(Percentage)
LBW(< 2,500 g)
(Percentage)
Calcium 5.4 (223) 8.9 (223)
Placebo 9.9 (192) 10.4 (192)
Blacks
Calcium 7.1 (85) 10.3 (86)
Placebo 19.1 (89) 20.0 (89)
p= 0.01 p= 0.07
Gestational age: Best obstetric estimation: LW'. Ultrasound, rundalheight. and early tetat movement.
Figure 16.1Differences in Adjusted Blood Pressure Mean
Values at Term Between Calcium and PlaceboGroups (Adjusted for Race and Initial Blood
Pressure < 26 Weeks)
-6
-s
Blood
pressu t -4
differenc e
t mint -
-2
Sample size(Placebo-Cai
-4.09*-3.65"
-4.94"
Supine Lateral Supine Lateral
27-23 27-23 26-24 26-24Systolic Diastolic
'Between grouos: p 0.(16"Between slopes1.3 last nleasures); p 0.05
,)
194 Statistical Findings: Calcium Supplementatio and Pregnancy-Induced IIlpertensUm and Prematurity
Interventions
Figure 16.2Differences in Systolic Blood Pressure at Term Between Calcium-Supplemented and the
Corresponding Placebo Groups in Two Studies of Calcium Supplementation During Pregnancy
-9 -8.5 mm Hg'
Placebo 1 g
(Reference Group;
1.5 gCalcium Croups
Lateral Position.
2 g
'Source: Author. (See chapter lb).
'Source: Marva R. K., Rathee S. and Manrow M. 11987). Effect of calci-
um and vitamin 0 supplernentation on toxemia of pregnancy.Gynecologic and Obstetric Investtgation, 24, 38-42.
locap 86-387
Rasehne
Subjects eligible n:Clinically healthy Placebo Blacks
Single PregnancyParity 0-1Knoell t_MPRegistered hetore 20 weeksNO drugs or treatments
Figure 16.3Study Design
Randomized Double-Blind Controlled Clinical Trial
Randomization
VWhites = 196
Chnical ex iminationBlood samples24 hour dietary, recallUr nary sample
g Flemental Calt ion a DavCalcium
2t1 14
Whites N. 230
Blacks = 87
rm
fuse 1.711ar et al. 195
1 53
Magnesium Suppkmentation inPregnancy: A Double-Blind Study
LUDWIG SPATLING, M.D.
INTRODUCTION
The recent interest in the element magnesiumis probably in part accident and in part due tothe development of new techniques, such asatomic absorption spectrophotometry permit-ting accurate assays. These technologicaladvances facilitate correlation of laboratoryresults with clinical disorders.
First some important qualities of magne-sium are identified. After potassium, magne-sium is the second most abundant intracellularcation. On the one hand, its biological effectcan be attributed to the formation of chelationcompounds. On the other hand, it is a cofactorof ATP (adenosine triphosphate), thus explain-ing its influence on al)out 300 enzymatic reac-tions, such as carbohydrate metabolism, lipidmetabolism, and nucleic acid metabolism. It is
Advances in the Prevention of Low Birthweight
involved in stages of protein synthesis and isan important prerequisite for the proper func-tioning of energy-releasing reactions, such asglycolysis and oxidative phosphorylation.2
A person needs 0.16-0.21 mmol of magne-sium per kilo of bodyweight per clay, whichcorresponds to 11.5-14.4 mmol per day for abodyweight of 70 kg. During growth and preg-nancy, an additional 4 mmol per day are need-ed. Based on metabolic studies of pregnantwomen, the World Health Organization (WHO)Food and Nutrition Boards recommend a sup-ply of 18.5 mmol of magnesium per day duringpregnancy (1 mol Mg = 24.3 g Mg).'
Investigations during recent years haverepeatedly shown that the magnesium contentof plasma falls significantly during pregnancy,particularly at the beginning.4 It is discussed asa physiologic dilution. It should be mentionedthat renal magnesium loss in pregnancyincreases by 26 percent, shown by 24 urinc'samples in healthy women during the wholepregnancy.'
Chronic hypomagnesemia in the pregnantwoman carries over to the tissues. Usingnwometriwn samples of over 100 cesarean sec-tions, it could be documented that the magne.sium content of the smooth uterine musclesdecreases significantly with increasing pregnan-cy age. There is also a highly significant corre-lation between the muscle magnesium contentand plasma level.°
This leads to the conclusion that, althoughmagnesium intake is not increased during theperiod of greater need, there is yet more lossthrough the kidneys due to the increasedglomerular filtration, which is not or is inade-quately compensated for, and that this long-term
hypomagnesemia shows up in growing tissue.The possibility that magnesium deficiency
might cause early delivery was first contemplat-ed following the accidental observation that thereduction of premature labor was improved bytreating calf muscle cramps with magnesium. Ina subsequent study, 10-15 mmol of magnesiumper day were given orally where the dosage ofbeta-adrenergic drugs could not be reduced.Subjective and objective methods of assessmentshowed decreased incidence of uterine contrac-tions, and, at the same time, indicated that therequired beta-adrenergic dose could bereduced.-
The publication of this pilot study caused anumber of other studies. In a retrospectivestudy, lower incidences of intrauterine growthretardation, preterm rupture of the membranes,and preeclampsia by magnesium supplementa-tion during pregnancy were described.8
Because of the studies cited above, a dou-ble-blind study was conducted to clarifywhether or not magnesium supplementationhas any influence on the pregnant woman andthe fetus or the newborn, respectively.
Dot 'BLE-BUND 511.DY
A total of 568 women (normal and high-risk) who attended the outpatient clinic at theDepartment of Obstetrics, University of Zurich,agreed to participate in the study. They wereenrolled in the study as early as possible. butnot later than 16 weeks of gestation. The sam-ple size was determined by the limitation of therecruitment period, which, for practical reasons,could not exceed two years.
1SJ
198 Magnesium Supplementation in Piegnancy: A Double-Blind Study
The method of allocation was based onthe subjects' even or odd date of birth.According to their group assignment, the sub-jects were given either 15 mmol of magnesium-aspartate-hydrochloride (Magnesiocard, VerlaPharmacy, Tutzing, FRG) or 13.5 mmol ofaspartic acid per day. At each visit, patientswere questioned on regular intake, number oftablets, and side-effects of the medication. Asubsidiary analysis was based on 437 womenwho claimed that they had regularly ingestedthe magnesium or placebo.
The Mann-Whitney U test was used tocompatv the central trends. Categorical vari-ables were analyzed using the chi-squared test.The results were considered significant at the 5percent level. Assessment always used two-tailed tests. Values were given as medians andthe 5th and 95th centile. For various reasons,such as refusal to take further tablets, deliveryin other hospitals, or abortion, some data werenot available for analysis.
Two hundred seventy-eight women weretreated with magnesium, and 290 received theplacebo. Age, parity, and gravidity were thesame in boll groups. There was no differencewith regard to the birthweight of children bornbefore the start of this study or the duration ofprevious pregnancies. Based on the clinical his-
tory of the patients, the risk of abnormal preg-nancy was comparable in the two groups.
The frequency of complaints attributed tothe tablets svas low and comparable in the twogroups. In the magnesium group. 1 womancomplained of diarrhea, .4 of nausea, 6 of vom-iting, and 6 of heartburn; in the placebo group,2 complained of diarrhea, 1 of nausea, 10 ofvomiting, 6 of heartburn, and 1 of fullness.
Interventions
Median maternal weight increase was 11 kg inboth groups, and there was no differenceregarding the systolic and diastolic blood pres-sure and different degrees of oedema.Magnesium serum levels showed no differencesbetween the groups.
Patients were hospitalized if they experi-enced antepartum hemorrhage, irregularpreterm contractions, or progressive cervix mat-uration. In the magnesium group, 44 womenwere hospitalized for 533 days. In the placebogroup, 65 women had to stay in hospital for887 days. The average duration of each admis-sion to hospital was the same in both groups.Among indications fbr admission to hospital,hemorrhage during pregnancy, incompetentcervix, and preterm labor were significantlymore frequent in placebo-treated women.There was also no difference in the number ofmiscarriages.
The median gestation was significantlylonger in women treated with magnesium,although the difference between the medianswas not more than one day. Delivery before 37weeks occurred less in the magnesium group,but the difference was not significant. Theserum analysis showed that low magnesiumlevels in the first half of pregnancy are of nopredictable value for preterm birth. There wereno differences regarding the duratkm of thefirst and second stages of labor. The same istrue for the incidence of surgery or other com-plications during delivery.
There are no statistically significant differ-ences between the unselected groups withrespect to placental and infant weight; lengthand head circumference; and birthweight below2500 g, below 1500 g, and below the 10th per-
1S .4Ludwig spading 199
Advances in the Preivntion of Lou Birthweight
centile; however, fewer infants with a head cir-cumference less than 33 cm were found in themagnesium group. There are also no statistical-ly significant differences in arterial and venousumbilical pH or frequencies of infants with anAPGAR score of 7 or less. Significantly fewerinfants in the group receiving magnesium wereadmitted to the neonatal intensive care unit.The biggest differences were found in theadmission rates for preterm birth and asphyxia.The numbers of the subgroups arc too small toshow any statistical difference.
In the subsidiary analysis, we excludedise women who did not fulfill the protocol of
medication as prescribed, leaving 217 women inthe magnesium group and 220 in the placebogroup. As expected, the effect of magnesiumsupplementation demonstrated itself more clear-ly (see table 17.1). Some of the results that only
Table 17.1Comparison Between
Magnesium and Placebo Groups
Magnesiumgroup
Placebogroup Significance
Variable
Indication forHospitlization
(N =278)50th centile
(N =290)50th centile
Hemorrhage (N) 4 17 < 0.05
Incompetentcervix (N.) 8 17 < 0.05
Preterm labor (N) 12 26 < 0.05
Gestational ageat delivery(weeks/days) 40/0 39/6 < 0.05
Admission toneonatal intens-ive care unit (N) 20 36 < 0.01
reflected a trend in the main study became sta-tistically significant, while other results that werealready significant in the main study were con-firmed at a higher level of significance.
The difference between hospitalization fre-quencies was significant at a higher level. Thenumber of infants below 2500 g and below 500g was also significantly smaller in the group ofmothers who regularly took magnesium. Thedifference between numbers of children with ahead circumference below 33 cm became high-ly significant.
A general trend toward iiv7roved fetal out-come and adaptation, already seen in the mainstudy, was confirmed by statistically significantresults; birthweight, length, and head circumfer-ence were higher, and the number of childrenwith a 10-minute APGAR score of 7 or belowwas less in the group with regular magnesium
Table 17.2Comparison Between Magnesium and Placebo Groups
After Exclusion of Patients Who Did Not Take TheirTablets Regularly
Variable
Magnesiumgroup
(N 217)50th centile
Placebogroup
(N -= 230)50th centile
Significance
Birthweight (g) 3340 :3300 < 0.05
No. < 2500 g 6 18 < 0,05
No. < 1500 g 0 6 < 0.05
Infant length (cm) 50 49 < 0.05
Head circum-ference (cm) 35 34 < 0,05
No. with10-min Apgarscore 5 7 0 5 < 0.05
No, of womenhospitalized 26 48 < 0.01
1SLJ
200 Magnesium Supplementation in Pregnancy: 4 Double-Blind Study
supplementation. Fewer mothers with mildedema were counted in the magnesium group.
The advantageous effect of magnesiumsupplementation during pregnancy is clearlydocumented in decreased incidences of hemor-rhages, incompetent cervix, and preterm labor,and in prolonged gestation. If preterm deliveryis defined as birthweight below 2500 g, in thisstudy, we could reduce the incidence from 7.7to 18 percent. A statistical difference betweenthe frequencies of abortion could not be seen:however, a positive effect of magnesium sup-plementation during pregnancy in respect to itsclinical syndrome was evidenced by the lowincidence of hemorrhage. It is interesting tonote that the two infants who were very lightfor gestational length were seen in the placebogroup. One infant born at 31 weeks' gestationweighed 1000 g and another one horn at 32weeks weighed 1190 g. Of course, this numberis still too small to establish a significant influ-ence of magnesium supplementation onintrauterine growth retardation.'
CONO.1.'SION
Magnesium supplementation during preg-nancy was associated with significantly fewermaternal hospitalizations, a reduction in pretermdeliveries, and less frequent referral of new-borns to the neonatIA intensive care unit. Theresults suggest that magnesium supplementationduring pregnancy has a significant influence onfetal and maternal nunbidity both bef,ire andafter delivery. The results of this study stronglyrecommend magnesium supplementation duringthe whole period of pregnancy.
Luduig Spat !hitt;
Interventions
REFERENCES
1. Spading, L., and Spading, G. (1988). Magnesiumsupplementation in pregnancy: A double-blindstudy. British finirnal qf Obstetrics arid Gynaecology95,120-25. (The results are published in parts,)
Gunther, T. (1981). Biochemistry and pathobio-chemistry of magnesium. Magnesium Bulletin 3,91-101
3, Seelig, M. S. (1980). Magnesium deficiency in thepathop,enesis of disease. New York: PlenumPublishing Corporation.
4, De orge, F. 13.. Domingos, D., de 1.7lhoa Cintra, A.B.. and Antunes. M. L. (1)05), Magnesium concen-tration in the blood serum of normal pregnantwomen. Obswtrk's and Gynecology 26, 253-255.
i. Sp;itling. L.. Kunz. P. A_ Fluch, R.. and flue)), A.(19851. Magnesium and calcium excretion duringpregnancy. Magnesium Bulletin 91-93.
Spading. L.. Kunz. P. A., \Onderschmitt, D. J.. Iluch,R.. and !Inch. A. (1983). Zum Magnesiumgehalt dernerusmuskulatur im 111, Trimenon. Archives ofGynecology 235. .rn
SpAling. 1.. 1981/. Orate Magnesium-Zusatz-therapie lxi vorz.eitiger Wehent tigkeit. Geburtshiyemuenbeik -4 1 () 1- 102
8. Conradt, A.. Weidinger. H., and Algayer. H. (1984).on the role of magnesium in fetal hypotrophy, preg-nancy induced hypertension and preeclampsia.Magnesium Bulletin 6, 68-76.
201
An Ovetview of Trials ofSocial Support During Pregnancy
DRNA ELBOURNE, PH.D.
ANN OAKLEY
NTRODI ICTION
The main purpose of this chapter is to updateour earlier review in Evian of controlled trialsof social support in pregnancy.' We begin,therefore, by summarizing the focus, methods,and conclusions of that review. We then pointOut the ways in which we have altered thesemethods for our present work, show theupdated results, and discuss their implicationsfor current practice and future research.
1986 REVIEW
We started from the presumption that apregnant woman is more than just the carrier ofher unborn child. She is a person in her own
1S7
Advances in the Prevention qf Low Birthuvight
right, with a lik apart from that seen by mostantenatal caregivers. This life includes a numberof stresses and strains. Pregnancy, althoughoften a joyful experience, may also add to theseexisting pressures, and may create new stresses.Studies of the relationship between social class,stress, and reproduction suggest that social sup-port in pregnancy may be able to mitigatematernal stress and improve maternal and infanthealth.' We therefore examined the controlledtrials of social support in pregnancy.
Mimms
Selectiotz ((trialsIn order to find these trials, we searched
the Oxford Database of Perinatal Trials for pub-lished and unpublished' reports. The criteriafor entry in the computerized data base are thatthe trial participants should be human; that thetime of intervention should be during pregnan-cy or the neonatal period; and that allocation tothe intervention should be random or quasi-random (i.e., using alternate alk)cation or usingdate of birth or casenote numbers).
For the Evian review, we selected all trialson the data base coded as -counseling, support,and educatim in pregnancy.- Trials included inthe analysis were either those designed explicit-ly to provide social support or those utilizingwhat we judged to he supportive approaches toantenatal care. These included such disparateinterventions as antismoking advice; health edu-cation; organization of maternity care; incomesupport; and preparation for pregnancy, child-birth, and parenthood. In the 29 trials of socialsupport in pregnancy so identified we
considered seven pregnancy outcomes: Lowbirthweight, preterm delivery, anaesthesia, anal-gesia, prolonged labor, instrumental delivery,and adverse psychosocial outcomes.
Statistical nwtlxxlsWe followed the methods of yusuf and his
colleagues' to formally combine informationfrom these trials in a procedure which hasbecome kmmn as meta-analysis or oveniew.
For each trial, we calculated an odds ratio,which is the odds of getting a particular (usual-ly adverse) outcome (e.g., low birthweight) inthe experimental group, compared to or divid-ed by the odds of getting the same outcome inthe control group. If the odds ratio is I, it
implies that the odds are the same in theexperimental and the control group (i.e., forthat outcome, it makes no difference whetherthe intervention is experimental cw c(mtrol). Ifthe odds ratio is less than 1, it suggests that th,..experimental intervention offers some protec-tion against this adverse outcome. If the oddsratio is greater than I, it suggests that theexperimental intervention may do harm. Theodds ratio is .in estimate, and so the confidencewith which it can he stated varies directly withthe size of the study; that is, the smaller thestudy, the less confident one c..m be that theestimate is a true reflection of reality, and thewider the confidence interval is that can heplaced around the estimate. Conversely. a largesample size means greater precision and asmaller confidence interval the estimate isa more precise reflection of the truth).Therefore, for each study, we show an estimateof the odds ratio with its 95 percent confidenceinterval. In an overview of several trials, we use
1ES
204 An Vi 'en 'ieu f l'rials (yr Social Szeppor t During Pregnancy
all of these within-trial estimates to calculate atypical odds ratio, but because several trials areincluded, we thereby increase the precision ofthe estimatethat is, we can narrow the confi-dence intervals.
CONGA tiIONS
Our conclusions in 1986 were that "Interms of the seven outcomes considered, theavailable experimental evidence shows theseeffects (of the social interventions) to be eitherinconclusive or beneficial:1 and this is support-ed by the conclusions of the observati(malstudies." We ended our review by calling forbetter designed, larger trials, specifically in thefield of social support.
PRSENT OVERVIEW
The aims of our present overviewtoreview the experimental evklence of the effectsof social supp( rt in pregnancyare largely thesame as they were three years ago. In thisupdate. IRAvever, we ad()pt thur slightly differ-ent approaches.
First, this chapter focuses on the two preg-nancy outcomes most relevant to the title of theconference: Gestational age at delivery. andbirthweight. A number of other outonnes (suchas intrapartum events, the health of the motherand baby, health-related behavior. the attitudesand feelings of the mother, and the baby'sdevelopment) will be considered and discussedelsewhere..
Secondly. our earlier review was based on
biterventions
all trials on the data base with interventionscoded as "counseling, support, and education inpregnancy." What this disparate group had incommon was that we thought they were thetype of' intervention that might be supportive.As a response to comments received followingthis 1986 review, we have limited our inclusionsin the present chapter to those in which socialsupport was an explicit aim of' the trial (i.e., theauthors' intent, rather than our surmise).
Thirdly, the overviews are presented inorder of' their methodological quality. Thisquality is assessed in terms of the likely exis-tence of three types of bias: Selection bias atentry, selection bias after entry. and measure-ment bias. The "best" trials are put first, and the-worst" are put last.
The final inethodological differencebetween the Evian review and the presentreview arises because, in the interim, a numberof trials primarily concerned with social supporthave been mounted. Thus, we have been ableto subdivide (wr analyses into those based ontrials in which social support is the primaryintervention, and those trials in which it is anexplicit co-intervention. We have looked for adose effect, expecting that the benefits of sup-port would be greater in the former group.
CI IARA(ITERItirICS OF TRIALS OF
EXPLICIT So XIII. SI. *PPORT IN PREGNANCY
We identified 35 trials of social support inpregnancy. The characteristics of these trials aredescribed in table 18.1. The final column of thisTa ble provides examples of the f()rm of wordswhich helped us to decide on their inclusion.
Diana Ilbourne and Ann Oakley 205S;)
Advances in the Prevention of Low Birthuvight
The results of some of the trials have nc)tyet been published!' u and still must be consid-ered provisional.
We have categorized the studies under sixmain headings. The provision of social supportis the primary aim in six studies.'"'' The remain-ing 29 trials all aim to provide explicit socialsupport, but as a co-intervention. In these trials,the other primary interventions are antismokingadvice (3);1')-" income support (1);" informationfeedback and information sharing (6);" " theorganization of care (7); '- and preparation forpregnancy, childbirth, and parenthood (12)." "This last group includes such diverse interven-tions as, for example, preparation for breast-feeding. nutritional advice, and enhancement ofmaternal attachment processes. The headingsare not necessarily mutually exclusive, andsome studies could be categorized under morethan one heading.
The entry criteria for the trials included inour overview vary greatly. To a large extent.this reflects the differing aims of the studies. Forinstance, those studies aimed at reducing thenumber of cigarettes smoked were targeted atwomen who WM' smokers (e.g., [191), Somestudies wishing to alter the organization of caretoward more midwifery control concentrated onwomen at low risk of poor obstetric outcomes(e.g., [391). In others, midwifery care is com-pared to medical care for women at high risk(e.g., [10)). In fact, because the principal entrycriterion for the study by Rehrer and Wolin'was residence in a low-income neighborhood,the studies do not even share in common theentry criterion of being a pregnant woman!
Allocation to the intervention is clearlyquasi-random (e.g., using casenote numbers) in
five studies.''''''' Allocation is said to be ran-dom in the remaining 30, hut often the detailsare sketchy, or suggest that the author may beusing the word random in a nontechnical sense.
The sample sizes are equally variable,ranging from 10 women° R) 1,763 pregnantwomen.'" In two papers'''" the sample size isnot given. Overall, the studies are based on atleast 5.500 women allocated to a supportiveintervention in pregnancy, and at least -1.600women with less support serving as controls.
As with the entry criteria, the outcomesunder investigation largely reflect the type ofintervention being offered. Some include suchtraditionally clinical outcomes as birthweightand gestation at delivery (e.g 1,40,1), whereasothers empk)y a number of sociopsychok)gicaloutcomes such as 'love scores' or postpartumattachment behavior."
It is worth noting at this point that the trialhy Runnerstronf9 is not only the largest (andtherefore the most influential in the overviews),but is also the trial most likely to suffer fromselection biases. These biases could occur bothat allocation (using casenote numbers) andafter entry (by excluding complicated deliver-ies). Therefore, where relevant, the typical oddsratio is calculated twice, with and without thec(mtribution of Runnerstrom.s study.
PREGNANCY O.( TCOMES
Gestational age at deliroy(completed aeeks)
Seven of the twenty-nine trials of explicitsocial support in pregnancy as a co-interventiongive information about the preterm (< 37 com-
206 An Overview of Thais qf Social suppert During Pregnancy
pleted weeks) delivery rate. They find no evi-dence to suggest that such support has any effecton this outcome (see figure 18.1). The same con-clusion follows from the typical odds ratio basedon four of the six trials in which support is theprimary intervention (see figure 18.2).
Very few trials provide information aboutthe rate of extremely preterm V 33 completedweeks) delivery, Neither the one trial in whichsocial support is an explicit co-interventkm (seefigure 18.3) or the three in which it is the pri-mary interventkm (see figure 18.4) provideconclusive evidence of an effect of social sup-port on this rate.
Bllarmuo rr
Fifteen of the thirty-five trials in whichsocial support in pregnancy is an explicit inter-vention provide some information about thelow birthweight V 2500 g) rate. The typicalodds ratio based on 10 trials in which socialsupport is an explicit co-intervention suggestthat such support may result in a statisticallysignificant reduction in this rate (see figure18.5). The 95 percent confidence intervals of allbut the last trial, however, include unity.Excluding this trial from the overview shows nostatistically significant effect of social support onthe low birthweight rate. The same conclusioncan be drawn from the five trials in which sup-port is the primary intervention (see figure 6).
Six trials give information about the verylow birthweight V 1500 g) rate. All three inwhich support is a co-intervention, separatelyand together, suggest that such support is asso-ciated with a nonstatistically significant increase
Interventions
in the rate of very low birthweight (see figure18.7). In contrast, all three trials in which sup-port is the primary intervention suggest a non-statistically significant decrease in the rate (seefigure 18.8). Although this may be indicative ofa dose effect, the nunthers are small, and theconfidence intervals overlap.
Drsu IssION
It is perhaps disappointing that thisoverview has provided no conclusive evidenceabout the effects of social support in pregnancyon the two selected clinical outcomes consid-ered above. Certainly, there are no clear impli-cations for current practice.
There are a number of possible explana-tions for this continued uncertainty about theeffect of such support.
It is possible. of course, that social supportin pregnancy has such negligible effects that noamount of further research will provide a clearanswer to whether it is either beneficial orharmful. From these overviews, particularlythose in which support is the primary interven-tion, it is possible that there are some benefits,but that these are likely to be modest. Thisimplies that larger numbers are needed to avoidmaking a "type 2- errorthat is. of not beingable to detect an effect, even if one exists.
Larger numbers could be obtained fromtwo main sources. Firstly, none of the outcomesoverviewed contain data from all of the 35 trialslisted in table 18.1. It is possible that renewedattempN to elicit such information from theirauthors may yield some dividends. Not onlywere many of these trials carried out quite some
Diana Mourne and Ann Oakhy 207
191
Advances in the Prevention of Low Birthweight
time ago, however, but, given their heterogene-ity (particularly in the larger group of trials (29)in which support was a co-intervention), it is
unlikely that such data were ever collected.A second route to obtaining larger numbers
is by increasing (from 3;) the number of studiesin the overview. There may be completed andpublished trials which we have not been able toidentify from our search of the Oxford Databaseof Perinatal Trials. This is perhaps more likely inthe field of social support than for other inter-ventions considered in this book, as suchresearch may not have been conducted by theclinicians nor published in the clinical journalswhich have been the prime sources of entryonto the data base. It is also possible that trialsin which support was not the primary interven-tion were not coded sufficiently to ensure theiridentification as having support as a co-inter-vention. While we continue to be alert to boththese possibilities, it is unlikely that concentrat-ing on them will yield great dividends.
We are aware, however, of a number of tri-als from which results will be available in thenear future (see table 18.2). At least four ofthese trials have already conipleted recruitmenthut cannot yet provide data suitable for inclu-sion in the Overviews (see table 18.2A?). At leastfive more trials are still in progress (see tablel',.2B?). We are also aware of other trials whichare at the planning stage. As the results fromthese trials accumulate, we are likely to obtainmore definitive answers to our questions aboutthe effects of social support in pregnancy on thespecific outcomes considered in this chapter.
A further explanation for the inconclusive-ness of the results here presented is that we areconsidering either the -wrong" outcomes. or
that these outcomes are of relevance but thereare additional outcomes to which we shoulddevote our attention.
If only because of the vvay in which 'W2.have chosen to present our overviews, we haveimplicitly assumed that low birthweight andpreterm delivery are unwelcome outcomes.This assumption is certainly arguable. Both ofthese outcomes are to some extent proxy mea-sures associated with adverse outcomes for thechild. But there are certainly also argumentsagainst considering low birthweight andpreterm delivery as adverse in themselves,unless they are associated with a worse out-come in the longer term. Nonetheless, in gener-al, the selected outcomes are associated withadverse events, and so may provide usefulinformation about the effects of support.
Othei outcomes are also 4 relevance. Asindicated earlier in this chapter, we intend toreview the effects of supportive interventionson other clinical outcomes, such as fetal andinfant mortality and morbidity. Inevitably, someindicators of morbidity will also be proxy mea-sures (such as Apgar scores, neonatal resuscita-tion, and admission to special care nurseries).We also wish to draw on the example of thework of Olds et al." on child abuse, and byGutelius et al."' on childhood behavior to con-sider possible longer term effects on the moth-er, the child, and the interaction between them.These examples also indicate that we plan toexamine outcomes other than those whichmight be defined as strictly clinical. These canbe categorized broadly as health-related behav-ior (such as cigarette smoking. bfeastfeeding.and clinic attendance) and sociopsychologicaloutcomes (e.g., postnatal depression, satisfac-
)4 41.
208 An Ckviview of Mak Social Support During Pregnancy
c..
tion with the intervention, involvement byother family members or friends in caring forthe baby, and doing housework).
These are of interest both in their ownright (as outcomes of the supportive interven-tion) and also as indications of the possiblemechanisms for the effect of the support. Forinstance, does support, by reducing stress anddepression, have some biochemical effect onfetal growth? Alternatively (or additionally).does support help to encourage pregnantwomen to attend regularly at antenatal clinics,thereby facilitating more effective clinicalsurveillance?
In addition to trying to increase the quanti-ty and range of information in subsequentoverviews of social support, we also plan toconsider the quantity and type of interventionsbeing provided. To some extent, we havebegun this process of examining a dose effectby separating those interventions in which sup-port is an explicit co-intervention (low dose)from those in which the support is the primaryintervention (high dose). But we also wish totake into account the length of time over whichthis support is provided. The total or parthalabsence of social support is often a long-termproblem. Hence, it may be unrealistic to seekto substantially remedy its adverse effects with
a short-term dose of support in pregnancy.Indeed, it may be argued that offering and thenquickly withdrawing such help may even wors-en the situation. There may, therefore, he acase for increasing the dose by continuing sup-port into early parenthood. The work conduct-ed by Olds et al."' suggests that such a doseeffect may, indeed, exist.
It is clear from the above discussion that
Diana Mourne and Ann Oakley
Interventions
the process of overview in this field (as inmany others) is ongoing and (auto)dynamic.The effects of social support in pregnancy are.as yet unclear, but the wealth of informationwhich will become available over the next fewyears should provide some of the answers (aswell as raise more questions).
At this stage, we can only concur with theconclusion by Bryce and his colleagues, that'even if the trials fail to demonstrate a benefit,the cooperation between social scientists andobstetricians to undeitake this research shouldbenefit pregnant women in that it promulgatesa more holistic view of pregnancy:'''
REFERENCES
1. Blondel. 13., et al. (n.d.). Prevention of pretermdeliveries by home visiting midwives: Results of aFrench randomised controlled trial. Unpublishedmanuscript.
2. Bryce, R. L.. Stanley, R. J.. and Enkin. M. W. (1988).The role of social support in the prevention ofpreterm birth. Birth 15. 19-23.
3. Campbell. S., Reading, A. E., Cox. D. N., Sledmee,C. M.. Mooney. R., Chudleigh. P.. Beedle. 3.. andRuddick, H. (1982). Ultrasound scanning in preg-nancy: The short-term psychological effects of earlyreal-time scans. journal it/ Psycf.nymmunic Obstetricsrind 6:ynaecology 1. 57-61.
4. Carpenter. J., Aldrich. K.. and Boverman. 11, (19M).The effectiveness of patient interviews: A controlledstudy of emotional support during pregnancy.Architvs (il- General Psychiatry 19. 110-112.
S. Carter-Jessop. L. (1981). Promoting maternal attach-ment thr(mgh prenatal intervention, Maternal-ChildNaming journal 6. 107-112.
6. ( halnwrs. L. Hetherington. J.. Newdick, M., Mutch.L.. Grant. A.. Enkin, M., Enkin, E.. and Dickersin.(1986). The Oxford Database of Perinatal Trials:Developing a register of published reports of con-trolled trials, Cuntrulled Clinical Mats'. 306-324.
1 93209
Advances in the Prevention of Low Birthweight
7. Cogan. R., and Winer, J. L. (1982). Effect of child-birth educator communication skills training on post-pattum reports of parents. Birth 9, 241-244.
8, Dance, J. (1987). A social inteivention by linkwork-ers to Pakistani women and pregnancy outcome.Unpublished manuscript.
9. Dolcetta, G.. Azzini, V., Zacche, G., Zimmermann-Tansella, C., Bertagni, P., Siani, R., and Tansella, M.(1979). Traditional and respiratory autogenic trainingin psychoprophylaxis for childbirth. A controlledstudy on psychological and clinical effects in primi-parous. In: L. Zichella (Ed.), Psychosomaticmedicine in obswtrics and gynecology (pp. 929-936).Proceedings of the 5th International Congress, Rome.
10. Donovan. J. W. (1977). Randomised controlled trialof antismoking advice in pregnancy. British journalof Provntitte and Social Medicine 31, 6-12.
11. Donovan, J. W., Burgers. P. L.. Hossack. C. M.. andYudkin. G. D. (1975). Routine advice against smok-ing in pregnancy. journal qf the RQyal College (fGeneral Practice 25. 264-268.
12. Durham, L.. and Collins. M. (198(j). The effect ofmusic as a conditioning aid in prepared childbirtheducation. journal of Obstetric. Gynecologic, andNeonatal 4Vursing15, 268-270.
13. Elbourne. D. (1987). Subjects' views about partici-pation in a randomised controlled trial. Journal cfRepmductije and Inliint Psycholou 5, 3-8.
14. Elbourne. D., and Oakley, A. (Forthcoming). Therole of social interventions in pregnancy. In: M.
Enkin, M. J. N. C. Keirse, and I. Chalmers (Eds.).iffectire care in pregnancy and childbirth. Oxford:Oxford University Press.
15. Elbourne. I).. Richardson. M.. Chalmers, I.,Waterhouse, I.. and Holt, E. (1987). The NewburyMaternity Care Study: A randomized controlled trialto assess a policy of women holding their ownobstetric records. British journal qf Obstetrics andGynaecology 9.4, 612-619.
16, Ellis, D, J., and Ilewat. R. J. (1984). Factors relatedto breastfeeding Juration. Canadian FamilyPhysician 30, 1479-1484,
17. Field, T.. Sandberg. D.. Quetel. T. A., Garda. R.. andRosario, M. (1985). Effects of ultrasound feedbackon pregnancy anxiety, fetal activity, and neonataloutcome. Obstetrics and Gynecology 66. 525-528.
18. Fischer, W. M., Huttel, F. A., Mitchell, I., and Meyer,A. F.. (1972). The efficacy of the psychoprophylac-tic method of prepared childbirth. In: N. Morris(Ed.), Psychosomatic medicine in obstetrics andgynecology: Proceedings of the 3rd InternationalCmgress, London (pp, 4-44). Basel: Karger.
19. Flint. C., and Poulengeris, P. (1987). Know yourmidwife. London: Heinemann.
20. Gutelius, M. F., Kilsch, A. D., MacDonald. S.. Brcioks.M. R.. and McErlean. T. M. (1977). Controlled studyof child health supervision: Behavioural results.Pediatrics 60, 294-30.4.
21. Hebei. J. R.. Nowicki. P.. a'nd Sexton. M. (1985).The effect of antismoking ntervention during preg-nancy: An assessment of interactions with maternalcharacteristics. .4merican journal (..y Epideinkfty122.135-148.
22. Heins. H. C., and Nance, N. W (1986). A statewiderandomized clinical trial to reduce the incidence oflow birthweight'very low birthweight infants inSouth Carolina. In: E. Papiernik. 0. Bream and N.Spira (Eds.). Prevention of preterit! birth (pp.387-410). Paris; INSERM.
23. Heins. II. C., Nance, N.. and Efird, C. (n.d.).Multicenter randomized controlled clinical trial forthe prevention of low birthweight in South Carolina.Unpublished manuscript.
2.4. Hetherington, J. (1987). An international survey toindentify unpublished and ongoing perinatal trials,6mtrolled "trials 8, 287.
25. Hobel, C. J.. and Bemis. R. L. (1986). West area LosAngeles prematurity prevention demonstration pro-ject, In: E. Papiernik, 0. Bréart, and N. Spira (Eds.),Prevention (9`. preterm birth (pp. 205-222). Paris:INSERM.
20. Hol)el. C. J.. Bragonier. R.. Ross. M., Bear, M.. Bemis.R.. and Mori. B. (1987). West Los Angeles prema-ture prevention program: Significant impact.journal qf Perinatal Medicine 15. 112.
27. Kehrer, B. 11.. and Wolin. C. M. (1979). Impact ofincome maintenance on low birth weight: Evidencefrom the Gary experiment. journal of HumanResources1,i, .f34-462.
28, King. II.. and Eiser. J. R. (1981). A strateAy forcounselling pregnant smokers. Ikalth Educationjournal 40, 66-68.
210 An Overview of Ma& of Social Support During Pregnancy
29, Utley, J., and Forster, D. P. (1986). A randomisedcontrolled trial of individual counselling of smokersin pregnancy. Public Health 100, 309-315.
30. Little, B. C., Hayworth, J., Benson, P., Hall, F., Beard,R. W., Dewhurst, H., and Priest, R. G. (1984).Treatment of hypertension in pregnancy by relax-ation and biofrzedhack. Lancet I, 865.4367.
31. Lovell, A., and Elbourne, D. (1987, 19 March).Holding the baby and your notes. Health SewkeJournal, 335.
32, Lovell, A., Zander, L. I., James, C. E., Foot, S Swan,A. V., and Reynolds, A. (1986). St. Thomas'Maternity Case Notes study: Why not give motherstheir own case notes? London: Cicely NorthcoteTrust.
33. Lovell, A., Zander, L. I.. James, C. E., Foot, S., Swan,A. V., and Reynolds, A. (1987). The St. Thomas'Hospital Maternity Case Notes Study: A randomisedcontrolled trial to assess the effects of giving expec-tant mothers their own maternity case-notes.Paediatrks and Perinatal Epidemiology 1, 57-66.
34. Oakley, A. (1985). Social support: The -soft" wayto improve birthweight? Social Science andMedicine 21, 1259-1268.
35. Oakley, A., Chalmers, 1., and Elbourne, (1986).The effects of social interventions in pregnancy. In:
E. Papiernik, G. Brart, and N. Spira (Eds.),Prevention of preterm birth: Neu, goals and newpractices in prenatal care (pp. 329-361). Paris:INSERM.
36. Oakley, A., Macfarlane!, A. J.. and Chalmers, I.(1982). Social class, stress and reproduction. In: A.
R. Rees and H. Purcell (Eds.), Disease and the envi-ronment (pp. 11-50). Chichester: John Wiley.
37. Oakley, A., et al. (n.d.). Social support during preg-nancy. Unpublished manuscript.
38. Olds, D. L., Hende-:;on, C. R., Tatelbaum, R.. andChamberlin, R. (1986). Improving the delivery ofprenatal care and outcomes of pregnancy: A ran-domized trial of nurse home visitation. Pediatrics77, 16-28.
39. Olds, D. L., Henderson, C. R., Chamberlin, R., andTatelbaum, R. (1986). Preventing child abuse andneglect: A randomized trial of home nurse visita-tion. Pediatrics 78, 65-78.
Intertvntions
40, Olds, D. L., Henderson, C. R., Tatelbaum, R., andChamberlin, R. (1988). Improving the life coursedevelopment of socially disadvantaged mothers: Arandomized trial of home nurse visitation.American Journal of Public Health 78, 1436-1445.
41. Reading, A. E., Campbell, S., Cox, D. N., andSledmere, C. M. (1982). Health beliefs and healthcare behavior in pregnancy. Psychologi,w1 Medicine12, 379-383,
42. Reading, A. E., and Cox, D. N. (1982). The effectsof ultrasound examination on maternal anxiety lev-els. journal of Behavioral Medicine 5, 237-247.
43. Reading, A. E., Cox, D. N., Sledmere, C. M., andCampbell, S. (1984). Psychological changes overthe course of pregnancy: A study of attitudestowards the fetus/neonate. Health Psychology 3,211-221.
44. Reading, A. E., and Plan, L. D. (1985). Impact offetal testing on maternal anxiety. Journal ofReproductitv Medicine 30, 907-910.
45. Reid, M. E., Gutteridge, S., and Mcilwaine, G. M.(1983). A comparison of the delivery of antenatalcare between a hospital and a peripheral clinic:Report to Health Services Research Committee,Scottish Home and Health Department.
46. Runnerstrom, L. (1969). The effectiveness of nurse-midwifery in a supervised hospital environment.Bulletin of the American College qf Nurve-Midwifery14, 40-52.
47, Sanunons, L. N. (1984). The use of music bywomen during childbirth. Journal of Nurse-Midwife?), 29, 266-270.
48. Scott, K. '.1984). Reduction of low birthweight withenhanced antenatal care. Pediatric Research 18(i),345A.
49. Sexton, M., and Hebei, J. R. (1984). A clinical trialof change in maternal smoking and its effect onbirth weight. Journal of the American MedicalAssociation 215, 911-915,
50. Shereshefsky, P. M., and Lockman, R. F. (1974),Comparison of counselled and non-counselledgroups and within-group differences. In: P. M.Shereshefsky and L. J. Yarrow (Eds.), Psychologicalaspects qf a first pregnancy and early postnataladaptation (pp. 151-163). New York: Raven Press.
Diana Elbourne and Ann Oakley 211
195
Advances in the Prevention of Low Birtinveight
51. Spence Cagle, C. (1984). Changed interpersonalneeds of the pregnant couple: Nursing roles. JOGNNursing 13, 56.
52. Spencer, B., and Monis, J. (1986). The family workerproject: Social support in pregnancy. In: E.Papiernik, G. Bream and N. Spira (Eds.), Preventionof prekrm birth: New goals and new practices in pre-natal care (pp. 363-382). Paris: INSERM.
53, Spencer, B., Thomas, H., and Morris J. (1989), Thefamily worker project: A randomised controlled trialof the provision of a social support service duringpregnancy. British Journal of Obstetrics andGynaecology 96, 281-288.
54. Spira, N., Audras, F Chapel, A.. Debuisson, J.,Jacquelin, C.. Kirchhoffer, C., Lebrun, C., and Prudent.C. (1981). Domiciliary care of pathological pregnan-des by midwives: Comparative controlled study on996 women. journal de Gynecologie Obstetrique etBiologie de la Reproduction 10, 543-548.
55. Stanley, F. J.. and Bryce, R. L. (1986). The pregnancyhome visiting program. In: F. Papiernik, G. Breart,and N. Spira (Eds.), Provntion of preterm birth: Aewgoals and new practices in prenatal care (pp.309-328). Paris: INSERM.
56: Sweeney. C., Smith, H., Foster, J. C.. Place, J. C.,Specht, J., Kochenour. N. K., and Prater, li. NI.
(1985). Effects of a nutrition intervention programduring pregnancy: Maternal data phases 1 and 2.Journal of Nurw-Afidulfety 30, 149-158.
57. Wiles, L. S. (1984). The effect of prenatal breastfeed-ing education on breastfeeding success and maternalperception of the infant. jOGNNursing 13, 253-2i7,
Yanover, NI. J., Jones. D., and Miller. M. 1). (1978).Perinatal care of low-risk mothers and infants, Neu.England Journal ofMedicine 94,702-705.
59. Yauger, R. A. (1972). Does family-centred care makea difference? Nutsing Outlook 20, 320-323.
60. Yusuf, S., P:to, R., Lewis, T., Collins. R., and Sleight.P. (1985), bol !Acvkade during and after myocardialinfarction: An overview of randomised trials.Progress in Cardiozuscular Diseases 27. 336-371.
01. Zimmermann-Tansella, C.. Doketta, G., Azzini. V.,Zacche. G., Bertagni. P., Skull, R., and Tansella,(1979). Preparation courses for childbirth in primi-para: A comparison. journal qf PsychosomatkResearch 23, 227-233,
58.
212
inAn Oven,iew ql1rials qf Social Support During Pregnancy
Interventions
Statistical Findings:Prevention of Preterm Deliveries
by Home Visiting System
Study(papers & dates)
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy
Types ofinterventions
Entry Criteria Allocation toInterventions
Nunthers Outcomes Inclusion Criteria(for overview)
Blondel et al.(unpublished) Ill
Carpenter et al.1968 141
Carter-lessop1981 151
Cagan and Winer1982 171
Dance 1987(unpublished) 181
Organization of care
Usual care + 1-2home visits a weekby midwives,
Usual care forwomen withthreatened preternilabor.
Women attending hospitaloutpatient clinics orhospitalised with threatenedpreterm labor; 26-36 weeks'gestation,
4
Lmottunal s,uppw-t Women registered in ahospital prenatal
interviews at intervals clinic.throughout pregnancy,labor, and the puer-perium with 1st yearmedical students,
Usual care
Preparation forparenthomi
Enhancement ofmaternalattat hment proc ess.
Usual antenatal care,
Preparation torchildbirth
Communicationworkshop to giveinstruction andpractit e in listeningand responding topeople's behavioralneeds.Usual training.
-
Socia/ support
Usual care + "link-workers" (minimum 3home visits and 2telephone
Usual care.
,t-
Women between 32 and 37weeks pregnant, fromprivate Obstetricians'practices. Primiparae,svhite, married, expectingnom omplicatedpregnancies, attention( eat childbirth classes,
Childbirth educators.
Immigrant Pakistaniwin-nen from ruralvillages in Azad Kashmirand Rawlpindi, withhistory at 1 or morelow birthweight babies,riot ass(t wed withelettise cesarean,gross malformation, ormultiple birth.
Random (sealedenvelopes)
lime of prenatalvisits
Random
Random
-
, Alternate
79
71
Costs; women's views,including satisfactionwith care; birthweight;gestational age.
Nervousness and use ofmedication before,
52 during, and after labor;length of labor.
SO
22
21
Postpartum attac hrnentbehavior.
Parents feelings andperceptions of events inpregnant v, labor andpuerperium.
Birthwerght, maternalphysic al ps hostx tat
25 health, intrapartum care,; neonatal health. know
ledge of health.
25
Smial support
"Provision ot emotionalsupport" ip.109),
"Maternal attachmentpaxess , enhanced by
specific prenatalintervention" (p,1093.
'Mothers encouraged toincrease awareness offetal activity and noticehow they cart affect theiractivity" ip,111i. _'Nonjudgmental wpportfor expectant parents"43,241).
Antenatal supptinlinkstorkers
Diana Elbourne and Ann Oakley 213197
Advances in the Prevention of Low Birthweight
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & dates)
Types ofInterventions
Entry Criteria Allocation toInterventions
Numbers Outcomes Inclusion Criteria(for overview)
Donovan 1977 1101Donovan et al.1975 L111
Antismoidng advice
Doctor at each ante-natal visit givingintensive individualantismoking advice.
Usual antenatal care.
Women attending ante-natal clinics at 3hospitals; smoking >cigarettes daily; < 35years; < 30 weeks'gestation; no previousperinatal deaths,
Durham andCollins 1986 1121
Preparahon (orchildbirth
Childbirth educationfollowing textbook byHasid and tape-recorded music duringconditioning exetcisesand relaxation/breathing techniques.
Childbirth educationfollowing textbook byHasid.
PrimagravIda couplesreceiving private child-birth educationinstruction.
Table of randomnumbers
280
308
Birthweight; gestationalage; other neonatalmeasures; smoking inpregnancy; smokingadvice; instrumental/operative delivery rate.
Table of randomnumbers
15
15
Elbourne et at.1987 1151Mourne 1987 1131
Ellis and Hewat1984 1161
Informal on feedbacWsharing
Women held soleobstetric record fromregistration until 10days postpartum.
Women held usualcooperation cards.
Preparation forparenthood
Nurses educated aboutfireastfeeding. Mothersgiven in-hospitalassistance by nurseclinician and prenatalbreastfeeding classes,and encouragement totelephone for support,and postnatal help.
Nurses educated aboutbreastfeeding. Mothersgiven in-hospitalassistance by nurseclinician.
Field et al, 19851171
Information feedback/sharing
Women viewed ultra-sound monito r. and given
running descriptions.
Women told about fetus'well-being and gestation.
Women < 34 weeks'gestation registered forantenatal care with 1obstetrician in aperipheral antenatalclinic.
Pregnant women planningto breastfeed; able tocommunicate in English;cohabiting: resident inurban toll-free zone.
Women referred torultrasound assessmentsot gestation,
Random(consecutivelynumbered, sealedopaque envelopes)
Random
Random
147
143
*Support needed andcontact . .. maintained"(Donovan et al. 1975,p.266).
frequency of intrapartummedication.
-Relaxation decreasesanxiety ... musictherapy as an aid topsychological andphysical control of pain"(p.268).
'Music .. providedcommon ground for-couples to relate witheach other" (p.270).
62
60
Women's feelings ofsatisfaction, beinginformed, anxious,confident, in control;father's involvement;depression; health-related behavior;analgesia/anesthesia;mode of delivery; lengthof labor; birthweight;gestational age;administrative effects.
--t--
Hypothesized that lwomenholding their ownobstetric notesl wouldfeel less anxious, moreconfident, more incontrol . . and wouldfind it easier tocommunicate with staff"(Mourne et al., p.613).
Breastfeeding at 1 4nd "Erxoaraged to telephonethree months; use ot nurse clinician forsemi-solids at 3 and support" (p.1481)six months,
tAnxiety; fetal activity; "Attempt . , . tomaternal sleep; obstetric alleviate pregnancyand postnatal complica- anxiety" tp.525).
20 tions; neonatal behavior.
20
214 Statistical Findings; An Overview of Trials of Social Support Dr;ring Pregnancy
Interventions
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & dates)
TYPes ofInterventions
Entry Criteria 11/ Allocation toInterventions
Numbers Outcomes Inclusiun Criteria(for overview)
Fischer et al.1972 1181
Preparatkut forchikfbirth
Course on psycho-prophylactk methodot prepared childbirthTwo sessions with 6couples at a time
Usual care.
Flint andPoulengeris 19871191
Gutelius et al.1977 1201
Heins et al. 19861221
Heins et al.(unpublished)1231
Organisation ot care
'know VOW midwife'c are. Team of 4 mid-wives thrmighoutpregnancy, latxu, andpuerperium.
Printiparae. By EDD
1-Women of low obstetric risk Random (sealedenrolling for full envelopestconsultant antenatal anddetiverv care.
Normal hospital care.;
Preiuration tor Unmarried printigravidae tiv stern at random
parenthood ages 15-18 before 7 ! numbers
months gestationProied nurse from 7thmonth of preAnancv.Routine health careand crxinseling onpreparation for infantiand «mtinuity of care 1for 3 years)
Usual prenatal careOne visit neonatally,
Svc support
intensive antenatal tarefrom nurseimidssite in 5reponal low hirthweightc inics; sot ial supportand stress reduction;increased number ofvisas; assessment ofcervis: education resigns of pretermlabor and on health-relatt-si behavior:emphasis on weightgain; continuity of care.
Usual antenatal care in! high-risk clinic.
-tKehrer and Wolin ! Income supix)rt1979 1271
Negative income tas
tami I les received fv% e
monthly payments when
previous month's
earnings below'break even" level)
No negative income tas
< weeks' gestation;previous low birthweightbaby; > 10 t m Crvasv risk-s( oring system; free ofmedic al or obstetriccomplications (e.g.,hypertension, renaldisease, diabetes, ormultiple pregnant
Residents ot low-incomene;ghllorhoods.131at khead of household; atleast 1 tkpendent< 18 years.
Random R omputer.gerwrated randomnumbers in sealedopaque envelopes atcoordinating center,opened in responseto tetephone call from1 of S tertiarycenters)
31
41
4--
503
498
47
48
Length of labor:analgesia in labor.
-Emphasized that martyrdomwas not the point" ip.381.
"Stress husbandparticipation" ip.40).
Clinical detailsinc luding birthweight:gestational age: lengthof labor; use ofanalgesia andanesthesia; mode otdelberY; mothers' VieWS.
Intant and maternalbeh.w(or.
Birthweight; gestationat delivery: maternal
684 weight gain
h87
Rarxiom twang Watts- ;
Conlisk ally( ation! model) ! 102f3'
241,
771
Birthyseight
'Mothers will esperrencegreater emotionalsatisfaction."
"Counseling ndantic ipatory guidame"(p.294i.
"frequent contact tp,29h).
"Social support and stressreduction" .
income matntenanceprogram to encourageincreased utilization ofprenatal care" tp.440).
"May have broad influenceon social behavior"ip 457i
Families148: " Single live births
/111
Diana Mourne and Ann Oakky 21519)
Advances in the Prevention of Low Birthuvight
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & datesi
Types ofInterventions
Entry Criteria Alkscation toInterventions
Numbers Outcomes Inclusion Criteriador overview)
Liffey and Fonter1986 1291
Little et al. 19841301
Lovell et al. 1986132)
Lovell et al. 19E371331
Mourne 1987 011
Oakley et al(unpublished) I 71
Olds et al. 1986a1481
Olds et al. 19861)139)
Okls et 31 Onpress) 1401
Anti-smoking advke
Including advice andbooklets at first ante-natal visit plusreinforcing letter after2 weeks and home visit
further 2 weeks later.
Usual antenatal care.
Informatton feedback/sharing
A. Relayation tra n ng.
O. Relayation trainingand biofeedback.
C. Usual practice.
Information feedback'sharing
Women held sok.obstetric record fromregistraticm to delivery.
Women held usual co-operation cards
Sochi] support
Sot ial support Inc furl.mg home visits bymidwives. andtelephone calls towomen and 24-hour'hotline to midwives.
Usual antenatal are.
Soc ial support
A C ontrol no servicespre wided throughrt-se,eri h projec
Free transportationand regular prenatal
and well,child care
( As (81lus ourse-home visitor duringpregnant s
D. As ar plus nursehome-v isitor untilc hrld rear bee. 2
years of age
Smokers (> 1 cigaretteper day1 at first ante-natal visit; < 28 weeks'gestation
Women with HP 135/85 mm Hg at 2successme antenatalvisits
Simple random inhltxksuf 8
; Sequentially
Women attending hospital Random iwnsecutivelvantenatal c knit. ot 1 numbered sealedobstetrician. env-elopes)
-7. - -.
Previous lens birthweightbaby iwithout maiorformation, multiplepregnancy, or electivedelivery). FluentEnglish.speakers,
Prim yams vvrimen either< 19 years or singleparent or loss k4X W-
e( 0410(111( status: <sseeks gestation.
Random by centraltelephone alkx.ation
Stratified by maritalstatus, rat e, geograph-
ical regions.Assigned at randomWomen dress assignmem dec k ot
ards. Decks recon-stituted periodicallytel in-errepresenttreatment withsmaller number ofsulsiec ts ias E.fron'sbiased win design).
Smoking in pregnanty.
77
74
Antenatal hospitaladmission; length ofantenatal stay; blood
18 pressure in fatepregnancy: pregnant
18 outcomes,
24
115
1 20
251
254
9(1
94
100
16
2,..
v
Women's feelings ofsatistaction; sense ofcontrol; communicationswith staff; lather'sinvolvement: health-related behavior:clinic al outcomes suchas birthweight, gestation,intrapartum anesthesia,length of labor, mode ofdelivery; administrativeeffects.
Hirthweight; gestationalage at delivery; maternalmaternal and infantmorbidity. maternalpsychological conditionpostpartum, andsatisfaction with care
Obstetrical labor andneonatal details: use othealth services: bealthhabits inc luding dretand smoking: gestationalage at delivery; birth.weight.
1-
*Individual counseling"ip.3011.
*Reinforcing advice . .
additional encouragement. . home visit" ip.310i.
"Extend relaxationachieved in biofeedbackand relaxation sessions tostresses experienced ineveryday life" (p.865).
'Communication .. women'schoices" ip.t
"Encourage informationsharing and increasedparticipation in decisionmaking.-
Soc ial support to'influent e mother'sphysical and mental healthiantenatally and post-natally), affec t processof labor and delivery . . .
and inc Tease women's self-ontidenc e about mothering.'
'Apple( iation fur the fullset of stressful familyand community influenceson wornen's health habitsand behaviors" ip.16).
'Home visitation by nursesshould be an ettedisemeans cM . respondingflexibly to the oressfulIrte c ire umstances withShk.h sex tally disadvantagedwomen must «Intend' ip.17).
'Parent education. enharument ot the women's informalsupport sYstems toemphasize the strengths ofthe ssonwn and their families'tp.171
216 Statistical Findings: An Overview of Thals cf Social Support During Pregnancy
Interventions
Table 18.1 : Characti_ristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & dates)
Types ofInterventions
Entry Criteria Allocation toInterventions
Reading et a).1984 1431Reading et al.19821411Reading and Cox1982(42)Campbell et al.1982131
Infonnation feedback'sharing
High feedbackshownscreen and given feed-back about size, shape,and movement.
Low feedbacknotshown screen, globalevaluation of progress.
Reading and Platt Information feedtxu is`1985 1441 t.haring
Reid et al. 19811451
High feedbackultrasoundsaw screenand nurse indicatedfeatures visualized.
Low feedbackultrasoundnot shownscreen, globalevaluation.
Fetal monitoringoon-stress or contractionsstress test using externalferal heart monitor.
Video controlshosynultrasound record thatthey were aware wasnot their own.
ONanizaPon ot care
Community antenatalclinic.
Routine hospital sersice.:;
Primievae having real-time ultrasound jr10-14 weeks. Caucasian,in stable relationship;ages 18-32; withouthistory of miscarriage,infedility, Of risk ofcongenital malformations.
High.risk population.
Women referred by CPfrom Easterhouse areafor ddivery at GlasgowRoyal Maternity Hospital.
Runnerstrom 19691461
. _
Sammons 1984(471
()rganization oft are
lbstetric care given by(1) nurse midwives(21 obstetric residents.
Preparation torchildbirth
Exposure to tapedmusic during activerehearsal of breathingpatterns.
Usual antenatal classes.
Women coded' "uncomplicated" attend ng
large training hospital.
Women attending Lamazechildbirth classes
RAMum
Random
Random withstratification
tasenote nunlbers
Numbers Outcomes Induskm Criteria(for overview)
67
62
Attitudes to scan, aboutpregnancy, about fetus,(especially anxiety):health related.
^Scanning informativeand emotionally rewardingwhen specific anddetailed (eedback madeavailable to mother" (p.59).
"Enhances awareness oifetus" (p.60).
-Shtirt-term effects onansiety levels" tp.239t.
-tAttitudes to scan, "Psychologic impact ofabout pregnanc y. about technology. . . concernfetus (especially stressful e(fects-
11 anxiety). (p.907).
8
100
100
7581().05
Random designationof «msecutive
I class series24
30
Obstetric morbidity andmortality; birthweight;intrapartum anesthesiaand analgesia;instrumenteoperatisedelivery rate; patternof usage of ditties;financial effects;communication;women's perceptionsof pregnancy and child-birth and reportedmanagement of firstmonths ot infant lite.
prenatal visits;analgesia andanesthesia; length oflabor; birthweight;mode of delivery:comphcations; conditionof baby.
Use ot music duringlabor; perceived effectof musk.
*Anxiety levels' (p 910).
To deal w ith "failure ofcommunic ation nd (ack ofcontinuity of care'(P.3).
"f eel full-time nurse-midwifery service withcommitment to patient andfamily c an provide moreintegrateci and ccmsecutivecare, comhaningfragmentation" (p.41).
"Uplifting effects otmusic arise (rom music'sability to OforitOre inter-cwrsonal relationships, tofacilitate ac hievement ofcell-esteem and to energizeand bring order throughrhythm" (p.2bbi.
Diana Mourne and Ann Oakkv 20 1 217
Advances in the Prevention of Low Birth:might
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & dates!
Types ofInterventions
Entry Criteria AlIncatIon tointerventions
Numbers Outcomes Inclusion Criteria(for overviessi
SexMn and Hebe)1984 1211
Hebei et al. 19851491
Anti-smoking advke
Staff assistance withsmoking cessation. Atleast 1 personal visitsupplemented byfrequent telephrmeand mail contacts.Encouragement throughinformation, support,practical guidance,behavioral strategies.
Smokers of at least 10cigarettes per day atbeginning of pregnancy:< 18 weeks' gestation.
Usual antenatal care.
Shereshefsky and Preparation for "Normal" women andLOckman 1973 1501 pregnancy/childbirth/ their husbands during
wrenthood tipit pregnancV
Spence Cagle 1984(511
Spencer and Morris1986 1521
Spencer ('t al.lin press) 1531
Splra et al.1541
Soc 1.31 work;
counseling service.
Control.
Preparation lin.pregnark
In-( lass homeworkaimed at couple.Interpersonal needstor control, affection,and inclusion duringpregnancy.
Usual Lamaz classc
So(' stipport
Otter of family worker,Client-centeredapproach.
Usual care.. .
1981 Organization of care
Usual care. .
Sweeney et al,1985 15W
Dom it iliary r are hymidwives.
Nutritional advice
Individual nutritionalads it e based on tfiggins'formota from MontrealDiet Dispensarywest optic in andcounseling.
Usual care.
Coupk., parte loafingin Lamaze classes.
Women at increased riski te having loss birth-
weight baby regkteringat 2 maternity units inSouth Man( hester.
; Pregnant women at highrisk of poor auk cures.(-pathologic atpregnant les").
Able to commune ate inEnglish: tree ot pre-existing medic aldisorders: not privatepatients or teenagers;singletons.
_
Random
Random
Random
Random
Random
Operative/Instrument,i1deloery rate
Random if fron'.biased coin design)within pre-gravidweight, and weightgain in test 20weeks. strata
441.i
472
ti55
4'18
425
22
21
Smoking habits; preg-nancy aukardes: birth-weight; gestational age;intrapartunt anesthesiaand analgesia; mode otdelivery; length ot labor.
E motional disturbancein pregnancy; physicalcomplications in preg-nancy and diddhirth;relationship betweenhusband and wite in thepregnanc y.
Caring relaticm-inventory: fundamentalinterpersonal relation..orientation behavior.
"Assistance with smokingcessation . . support"tp.9191.
ounsel ng wry ice"41.1511
"Dem ted to emotionalneeds ot pregnant womenarid their tamdies-ip.1529.
',stinted at couple inter-personal needs torcontrol, affection, andinclusion' cp.Rn.
l3inihsse'ight; outcome ot "Social support service."pregnancy; gestationalage; intrapartum anal:gesia and anesthesia;length of tailor: modetI dellyery.
-
Preterm delis VrIV.:hi rttuvelght, death .
antenatal admission,
Maternal protein andalorie intake and
maternal weight gain inlate pregnant y. Ante-natal, intranartum, andpostpartum maternalornplic meets: infant
birthweight andgestation at delivers .
"( ant inuit t c' aro at
home, net by strangers inhospital.'
"Providing indisidual c areaccording to the spec Mcneeds ot eat h uniquemother-intant unit"
2 r.'
218 Statistical Findings; An Overvitiw of Trials qt. Social Support During Pregnancy
Interventions
Table 18.1: Characteristics of Trials of Explicit Social Support in Pregnancy (Continued)
Study(papers & dates)
Types ofInterventions
Entry Cnteria Allocation toInterventions
Numbers Outcomes Inclusion Criteriador overview)
Wiles 1984 1571 Preparation for breast-feedirw and parenthood
Breastieeding educationclass.
Normal childbirthpreparation class,
Primigravtdae; > 32weeks' gestation;planning to breastfeed;attending chlkibirtheducation classes;vaginal delivery; nomedical complications;gestation at delivery36-43 weeks; 5 minuteApgar:. 7; normallyformed.
Randomly assignedtaccording to theclass in which theywere enrolled) 20
20
Breastfeeding; maternalperception of infant.
'Anticipatory guidance . .
for assisting parents*(p,253).
Yanover et at1976 1581
Organization of care
Family-centered caremainly postpartum butincluding continuity ofcare from prenatalclasseS.
Traditional care,
Vauger et at 1972 Organization ot care1591
Zimmermann-Tansella et al.1979 161,Doketta et al1979 191
amily-centered care:nursing service,identifying pwbtemsand needs of familyand providingappropriate care.Minimum of 4 home
Usual care.
Preparation tin-childbirth
Prenatal classesincluding autogenoustrainingdeeprelaxation.
Prenatal c lasses in( kid-ing specific gymnasticexert. ises.
Parity 0, 1; 19-15 yearsold; low risk medically;12th grade education:parents 1Mng together;father prepared to attendantertatal classes ,
Residents of specifiedareas; 3-8 monthspregnant; at leastchild < S years.
Random
Random
Married primiparae ages Random20-15; rto physicalabnormalities.
Diana Mourne and Ann Oakley 203
44
44
30
Length of labor;analgesia; anesthesia:mode of delivery; lengthof hospital stay;complications in motherOr baby,
Health knowledge;health behavior:health status,
Anxiety; p.Un; ciuliditionot baby. includinghirthweight; analgesia:
14 length ot labor; modeot delivery.
'Endeavor to respond towishes of numerousfamilies to enhance familyparticipation .collaborative perinatal
continuity ut care.-
-'Family-centered care . .
identification of problemand needs of family andprovision of appropriate
I service for even, member"ip.3207.
4-----autogenous training . . .
effects of deep relaxationdiametrically opposed toansiety . . related tofeelings ut calmness'
219
Advances in the Premntion of Low Birthweight
Principal investigatorand place
S. ElliottT. level-tonLondon, England
Table 18.2: Uncompleted Trials of Explicit Social Support in Pregnancy
A. Recruitment Complete Awaiting Data Analysis and Report(s)
Nature of the intervention
Social support-educationgroups led by psychologktor health visitor
I. king Supportive antismokingI.R. Eiser advice reinforced byBristol, England 1281 counseling and bkxhemical
testing at home_t
C. Larson Prenatal home visits byMontreal, Canada community health nurses
K. ScottNova SCotia, Canada 1481
Enhanced maternal carefrom physical and lifestsk.assessment by communityhealth nurses
Sample
First- and secondarmemothers ts =2001
Smokers attending first ante-natal visit (s w 300)
w 1,548)
Women with history Of loibirthweight delivery
=, 10,574t
Allocation
Week of clinic enrollment
Random
Random
Stratified random
Outconws of intervention
Incidence of psychiatric disorder, espet ratiypostnatal d vression ; psychological well-being; use of support networks; hirthweight
Number of t igarettes smoked; mother'scooperation
Health and social status of mother and t hadto 3 years postpartum, childrearing attitudesand behavior of mothin
-
Patient compliance and behavior change;antenatal referrals; obstetric interventions;birthweight; stillbirths; NICU admissions;infant mortality, morbidity
Principal insestigatorand place
Nature tit the intervention
S. NgNew York, U.S.A.
F. StanleyR. BrycePerth, Australia ISSI
J. lar
E. Kest lerLatin Ament a(Argentina, CubaGuatemala, Mesir
CitobelR. BemisLos Angeles, O.S.A, 125.21i1
Intense crenatal tare includingweekly visit, ptblyicexamination; edut aticm onself-palpation; ho ITW Uter ineontraction monitor; %O.( ial
servke referral
Social support via homes tsning bY midwives
!tome visits by trainedwomen (including nurses,sot sal KV rkers, and layw(nker%) to provide personaland ramify support healtheducation, and use I), st aland health services
. .
Psvc hosot (al supptotsotialwork to reduce stress
8. In Progress
Sample
iistory of preterm dells eft,stillbirth. of spontaneousabortion > 2052: age .4 1O,> 33; registered for prenatalcare More 1b/52 is 41t1)
Anv tI the tollinsing:ores mus preterm birth;perinatal death; spontaneous
mid-trimester abortion; >brst trimester abortions; APH,low birthwerght (s ..:72000)
Women attendingspecified antenatal clinicbefore 20152, withoutimportant t fink al problems,but haying I or more riskfat tors: previous towbirthweight birth; age 17
malnutrition: low income,maternal educ anon, lack otsupport is = 2000)
High-risk women in Sespenmental c linKS
Allot ation
-+
Stratified randomization sothat equal numbersassigned to each treatmentat any point in time
Outt ames ot intervention
Preterm delivery; stillbirths, spontaneousabortions in 211d or Ird trimester: hirthweight
Computer-generated random Preterm delivery; birihweight: C ost: ansietv;numbers in blot ks of 4 sot ial support; focus of ontrol; ondut t of
. labor
Random stratified by center IUGR, LBW1, preterm debverv; maternalweight gam: obstetric interventions, labort ()wilt awns, breasneeding. neonatalmorbidity; use of health and soc al services:satisfaction; support; portpartum depression
Random assignment orc fink s to ever i talent.)or ontrof status, thenrandom assignment of high.risk women withinesperimental clinics to 1 of
interventions--1 cif whic his support
4't
Gestational age at deliver% hirthweight
220 Statistical Findings: An Overview of Thals of Social Support During Pregnancy
Interventions
Figure 18.1: Effect of Social Support in Pregnancy (as An Explicit Co-Intervention) onPreterm Delivery Rate (< 37 Weeks)
Graph of Log Odds Ratios
& Confidence Interval
.1 .5 1 2
Study Experiment
(%)
Control
(%)
Log Odds Rat(o
(95% Confidence Interval)
,01
Blonde), 8. (unpublished) 14779 07.72) 11/73 (15.07) 1,21
(0.51-2.85)
Sexton, M. el al. (1984) 34/429 (7.931 4(/438 (9.13) 0.8fr83.5.1-1.38)
Mourne, D. R. et al. 0987) 10/140 t7,1 4) 9/127 (7 09) 1 01
(0.40-2.56)
Flint, C. et al. t1987) 31/488 (6,35) 11/479 (6.47) 0.98t0.59-1.64)
Lovell, A. et al. (198b) 5N5 (5.26i 4/102 0.92) 1 .3b
(0.3o-5.16)
Spira, N. et al. (1981) 45/458 (9.83) 30/425 (7.06i 1.43(0.89-2.29)
Donovan, I. 11977) 1 252 t5,511) 181279 it) 45) 0.8;(0.42-1.75)
Typical Odds Ratio 1 DO
OS"), Confidence Interval) (0 al-1 34)
10
Figure 18.2: Effect of Social Support in Pregnancy (as a Primary Intervention) onPreterm Delivery Rate (< 37 Weeks)
Study Eperimvnt
("el
Control Log Ocids Ratio
(93% Confident e Interval)
Oakley. A. tunpubtichedt 34/243 0 3,991 33/243 0 3.581 1,04(0.b2-1.75)
Spencer, B. et al. (198b1 60/602 (9.971 54/581 i9.29i 1.08
----- 10.71-1.59)
Olds, D. L. et a). (1986) 11/1nn (h.63) 12/142 18,45) 0,77al. 33- 1 80i
Oame, I. iunpublishetil 3/25 )20,00) 4!2 I tr.001 1 3010.31-5,441
Typical Odds Ratio1.03
i95°.;, Confidence Interval!10.78-1. 17,
Study
,01
0,10 to Log Odds Ratios
& Confident e interval
.1 .5 1 2 10
Figure 18.3: Effect of Social Support in Pregnancy (as an Explicit Co-Intervention) onExtremely Preterm Delivery Rate (< 33 Weeks)
Lsperiment Control
("o)
Log Odds Rano
(93"., Contitienc e Interval;
Graph or Log Odds Ratios
is. Confident e Intenal
.01 1 5 1 2 10
Mourne, (), R. et al. (1987 t 3/140 2.14)
Typical Odch Ratio(95% Confidence interval,
I/ 27 (2.36r 0.91t0.18-4.56)
0.91(0,18-4.56t
Diana Mourne and Ann Oakky 205 221
Advances in the Prevention of Low Birthweight
Figure 18.4: Effect of Social Support in Pregnancy (as a Primary Intervention) onExtremely Preterm Delivery Rate (< 33 Weeks)
Study Experiment
(%)
Control
(%)
Log Odds Ratio
195% Confidence interval)
.01
Oakley, A. (unpublished) 13/243 (5.35) 13/243 (5.35) 1 00(0.45-2.20)
Spencer, EL et al. (1986) 9/603 (1.49) 11/581 (1.89) 0.79(0.32-1.90)
Dance, J, (unpublished) 2/25 (8.00) 1/25 (4.00) 2.00(0.20-20.20)
Typical Odds Ratio 0.91(95% Confidence interva)) (0.1(4-4.56)
Graph of Log Odds Ratios
& Confidence interval
,5 1 2 10
Figure 18.5: Effect of Social Support in Pregnancy (as an Explicit Co-Intervention) onLow Birthweight Rate (< 2500 g)
Study Experiment
(%)
Control
(%)
Log Odds Ratio
(95% Confidence lruerval)
.01
Blonde), B. (unpubhshed) 9/79 (11.39) 6/73 4822) 1,41
__.(0.49-4.13)
Sexton, M.1. et al. (19134) 29/429 (6.76) 39/435 (8.97) 0,74(0.45-1.21)
Elbourne, D. R, et a) (1987) 11/143 17.691 12/130 (9.23) 0 82_ (0,35-1.92)
Flint, C. et al, (1987) 31/478 (6.49) 18/471 (8.07) 0.79(0.48-1.29)
Lovell, A. et al. (1986) 5/95 (5.26) 11/102 (10.78) 0.4810.17-1 131
Reid, M. E. et al. (19831 6/76 (7.89) 10/79 (12.661 0.60(0 .21- 1.68)
Spira, N. et A. (1 981) 51/458 (11.14) 40/425 19.4n 1,20(0.78-1.86)
_
Donovan, .1, W. 0 9771 27/263 (10.27) 261289 0.00)___ .
1.16(0.66 2,04)
Zimmerman-Tansella, C. et al. 1/14 (7.14) 1/20 (5.(0) 1.46DATE? (0.08- 25.42)
Runnerstrom, L. (1969) 61/768 (7,94) 121/1005 (12.04) 0.640.47-0.87)
Typical Odds Ratio 0.81(95% Confidence interval) 10.68-0.97)
Typical Odds Ratio minus Runnerstrom 0.91(95% Confidence interval) t 0.74 1.141
Graph of Log Odds Ratios
& Confidence interval
.1 .5 1 2 10
"""
A
1,1444.
APA,P11.0.1
222 Statistical Findings: An Overview of Trials qf Social Support During Pregnancy
Study
Interventions.
Figure 18.6: Effect of Social Support in Pregnancy (as a Primary Intervention) onLow Birthweight Rate (< 2500 g)
EAperiment Control Log Odds Ratio Graph of tog Odds Ratios
tig Confidence Interval
.1 .5 1 2
Oakley, A. (unpubl(shed) 45/243
Heins, a C. et al. (unpublished) 118/633
sPencer. a. et al. 0986) 54/602
ads, a L. et al. (1986) 101166
Dance, ). tunpubfiYhed) 3/25
Typical Odck Ratio
i'!.) 195% Confidence Interval)
01
118.52) 52f243 (21.40) 0.84(0.54-1.30)
(18.64) 137/642 (21.34) 0.84(0.64-1.11)
18.971 50/581 (8.61) 1 05(0.70-1.561
16.02) 4/142 12.821 2.0910.71-6.11)
0 2.00) 4125 (16.00) 0.72(0.15-3.51)
0.91
10
.."641
: /....4.4,...4, ,i.,,...
10.75-1.111 1
Study
Figure 18.7: Effect of Social Support in Pregnancy (as an Explicit Co-Intervention) onVery Low Birthweight Rate (< 1500 g)
EAperiment
A
Control Log Odds Ratio Craph of Log (kids Ratios
(93% Confidence interval) ey Confidence interval
01 .5 1 2 10
Reid, M. E et .31.1198 it 2/76 (2.63) 1/79 (1.27) 2.04(0.21-19.95)--.
Sexton, M. I. et al. (1987) 8/429 11.8bi 5/436 i1 15) 1 62(0.54-4.85)
Elbourne, D. R. et al. i19871
Typical Odds RatioContidence interval(
.3/143 t2.1W 2/110 1.16(0.23-7 991
.61
(0.68 1 811
Figure 18.8: Effect of Social Support in Pregnancy (as a Primary Intervention) onVery Low Birthweight Rate (< 1500 g)
Study k %penmen! Control
i"o
Log Odds Ratio
(9c", Confidence Interval(
01
Hein, Ff. C. et .0. (unpublohedi 26,3J 1.3.4b1 i0/1142 (4.b7; 0.74(0.42- 1.28(
Oakley, A. tunpublished) 4/243 11 .63, 9/243 , 1.70( 0.45(0.15-1.
Spencer, 8. et al. 11986) 5/603 i0.81) 6'581 (1.01, 0.80
TyPi1:11 Odds Ratio
(0.24- 2.631_ . .
0 690.43 1 O8)
Graph ot I og Mds Ratios
& C orthdenc v Inter
1 .5 1 2 10
4
41
14
Diana Elbourne and Ann Oakky 223207
Inhibition of preterrn Labor:Is It Worthwhile?
MARc J.N.C. KEIRSE, M.D.
INTRODUCTION
For a normally formed infant, there is nogreater risk than to be born too early in preg-nancy. The transition from fetus to newborn isa hurdle to survival that is more than 100 timeshigher for the preterm infant than it is for theinfant born at term." Yet, there is a lack ofunderstanding of the mechanisms that initiatelabor too early in pregnancy. and there arelarge deficiencies in our ability to foretell andtimely recognize them. Failure to understandand prevent preterm labor has made cliniciansturn their attention to means and methods thatcould stop it in time to prevent its main conse-quence, preterm delivery. At first glance, theyappear to have been extremely successful indoing so. Most of the approaches introducedin the past few decades have shown such highsuccess rates in the initial reports documenting
20S
Advances in the Prevention of Low Birthweight
their use that one would expect the problem ofpreterm labor to have been resolved manyyears ago (see table 19.1).
This, however, has not happened. Norhave all of these treatments disappeared fromthe obstetric armentarium On the contrary,some of them have been supplemented withother treatments in the hope that two unvali-dated treatments will be better than one. Thus,the term tocolysis, introduced by Mosler inGermany in 1964 and now generally acceptedas synonymous for inhibition of labor, gave riseto the term Zusatztokolysis to refer to the vari-ety of treatments that are added to either aug-ment the effects or counteract the side effectsof tocolysis. In addition, new drug treatmentscontinue to capture the imagination of clini-cians desiring to solve the issue of pretermlabor once and for all. The introduction ofthese new treatments also continues to followthe traditional pattern in which enthusiasm forthe treatment seems to be at least as com-pelling as evidence that it works.
WHAT MAY OR MAY NOT BE WORTH INHIBITING?
Preterm delivery and preterrn laborThere is a widely held misconception that
resolving the problem of preterm labor willresolve all of the problems associated withpreterm birth. This is not so. Studies whichhave examined causes of perinatal mortalityLshave shown that more than 50 percent of thatmortality is due to fetal death before the onsetof labor, or to lethal congenital malformations,or both. These infants account for 12-15 per-cent of all preterm births, but for 60-65 percent
of the mortality associated with pretermNone of that mortality would he affected byabolishing preterm delivery, and none of thesepreterm labors are worth inhibiting.
What applies to mortality also applies tomorbidity. This is emphasized by the fact that,currently, about one-third of preterm deliveriesin singleton pregnancies do not result fromspontaneous preterm labor. They result fromdeliberate obstetric intervention to end pregnan-cy because the obstetrician believes that therisl.s of a continuing pregnancy to mother orfetus have become unacceptably high." The factthat approximately half of all preterm births areassociated either with twin pregnancies (10%),with fetuses who died before labor or havelethal malformations (10-15%), or with electiveobstetric intervention (25-30%) is rarely empha-sized in the literature.° This may, in part, explainthe failure of many preterm prevention pro-grams to lower the (crude) incidence of pre-term birth. It certainly emphasizes that, for about40 percent of preterm deliveries, inhibition oflabor is not only superfluous, but harmful.
Also readily forgotten is the fact that spon-taneous preterm labor and delivery are oftenassociated with clinically significant maternaland fetal pathology. In comparison to birth atterm, preterm birth is associated with a muchhigher incidence of inadequate fetal growth,'prelabor rupture of the membranes,8 placentapraevia,9 placental abruption,4 fetal congenitalmalformations,' and severe maternal disease.""Studies which have specifically addressed theincidence of maternal and fetal pathology inspontaneous preterm birth' have indicated thatabout half of all singleton preterm births thatresult from spontaneous preterm labor are asso-
226 Inhibition of Preterm Labor
dated with such pathology. Often that patholo-gy is the very same pathology which, in theabsence of preterm labor, leads the obstetricianto artificially end pregnancy, either by inductionof labor or by elective cesarean section.'
All of this suggests that, in many instances,nothing can be gained, but a great deal can belost by inhibition of preterm labor and delivery.
Preterm labor and preterm contractionsJudging whether labor has started or not is
by no means easy. Predicting whether it will orwill not lead to delivery can be extremely diffi-cult, as witnessed by the high "success" rates ofplacebo "treatments" in stopping pretermlabor." Lack of precision in the diagnosis oflabor would create no problems if one couldawait the signs and symptoms that invariablyclarify the diagnosis. Signs of steady progress indescent and dilatation may be useful to preparefor delivery. They are not very helpful, howev-er, if delivery needs to be averted and if laboritself is undesirable and needs to be stopped.The more advanced labor is, the more difficultit is to stop. On the other hand, the lessadvanced it is, the more likely it is to stop of itsown accord without any tocolytic treatment.
Successful inhibition of preterm labor,therefore, depends on early and accurate diag-nosis. Early diagnosis, however, particularlydiagnosis based on uterine contractions, isnotoriously inaccurate for predicting whetherpreterm delivery will occur or not. Some2 haveeven suggested that this diagnosis may be erro-neous about 80 percent of the time. We recent-ly found that 31 percent of women who caineto the delivery unit with preterm uterine con-tractions could safely return home undelivered
Interventions
and without specific treatment. Several authorshave attempted to improve upon the classicaldiagnostic criteria by measurement of hormonelevels," assessment of fetal breathing move-ments,".36 measurement of prostaglandinmetabolites,'' or assessment of thromboxaneexcretion.'m Some have attempted to forestallthe problem by serial cervical examinations inpregnancy,° by antenatal monitoring of uter-ine contractions,2'-24 or by screening for the riskof preterm delivery." Some of these approacheshave resulted in the administration of labor-inhibiting drugs to more than 40 percent oflow-risk pregnant women,26 demonstrating thatthe best results of treatment are obtained whenthere is nothing to be treated.
It is fair to conclude that, despite all ofthese attempts, the diagnosis of preterm laborhas remained as problematic as ever. This hasimmediate consequences for the inhibition ofpreterm labor and for assessing the effects oftocolytic treatments. In many instances, appar-ently progressive preterm labor will stop irre-spective of whether or not any treatment isinstituted. The finding that uterine contractilityis suppressed does not necessarily mean thattreatment has been effective, nor does it neces-sarily mean that delivery will be postponed toan extent that is clinically useful.
Numerous criteria have been applied todescribe "successes" of one treatment or anoth-er (see table 19.1). Some of the most common-ly used treatments relate to temporary arrest ofuterine contractions, number of hours or daysgained before delivery, number of deliveriesdelayed until 36 or 37 weeks' gestation, num-ber of infants weighing more than 2500 g atbirth, and increases in mean gestational age or
Marc Keirse 227
210
Advances in the Prevention of Low Birthuvight
mean birthweight at delivery. None of theseoutcomes are of great relevance to mother andbaby unless they are accompanied by anincrease in the number of survivors or by anincrease in the quality of life for the infants andtheir mothers.
Early and late preterm gestationsPreterm is internationally defined as less
than 37 completed weeks (259 days) of gesta-tioni-29 but inhibition of labor is not equallyuseful at all gestational ages that are character-ized as being preterm. Cut-off points drawn fordemographic and public health reasons, particu-larly when they require international consensus,have a tendency to follow the reality of clinicalpractice at a safe distance rather than to lightthe way. This has been emphasized in the pastby the expression prematurity, originallydefined as a birthweight of 2500 g or less30 andlater defined as a gestational age of less than 37weeks,m which was abolished and replaced bypreterm-"A2 long after it had become obviousthat "born too early" does not mean the same as"born too small" and that two different defini-tions of the same word are not very helpful indistinguishing these two situations.
The incidence of preterm delivery increas-es with increasing gestational age up to thecut-off point at 37 weeks. From the limiteddata that are available on geographicallydefined populations, less than one-quarter ofall preterm deliveries occur below 32 weeks'gestation.'""
It is particularly these deliveries, generallyreferred to as being very preterm, that presentthe greatest challenge. It should be realized,however, that these births also form a very het-
erogeneous mixture. This is exemplified in table19.2, which summarizes some of the data on allinfants with a gestational age of less than 32weeks who were born alive in the Netherlandsin 1983.4' Even in this category (0.6% of allbirths in the country in 1983), which wouldseem to be the one most likely to benefit frominhibition of preterm labor, 15 percent of births(excluding stillbirths) resulted from deliberateobstetric intervention to end pregnancy andanother 44 percent followed prelabor rupture ofthe membranes (see table 19.2).
Thus, the following statements appear tobe true. First, the majority of preterm deliveriesoccur at gestational ages that are advancedenough to offer little potential for improvinginfant outcome by prolonging the pregnancy.Second, even at gestational ages at which theinfant might theoretically benefit from prolon-gation of pregnancy, many other factors needto be taken into account if that theoretical ben-efit is to be matched by a real benefit. If deliv-ery can be postponed or pregnancy prolongedfor a duration which is thought to be clinicallysignificant, it does not necessarily follow thatthe outcome for the infant will be improved. Inaddition, drug treatments that are powerfulenough to suppress preterm labor effectivelyare bound to have other effects on the motheror the baby, some of them undesirable, thatmust be taken into account.
The conclusion of all of this should beclear. Emphasizing the uterine relaxant effectsof tocolytic treatments, without consideringwhat is gained in terms of quantity and qualityof survival and without considering the possi-ble hazards to mother and baby, is needlesslynaive.
228 Inhibition qf Preterm Labor211
Assessment of the effects of tocolytic drugsA large number of tocolytic agents have
been employed for the inhibition of pretermlabor. Not all of these are still relevant. Table19.3 lists those that were reported to be in usein the literature of the past 10 years. Some of
these, such as antibiotic treatmene9 and oxy-tocin analogues,4° have been recent introduc-
tions that will require validation before beingintroduced into clinical practice."' Others, such
as ethanol, have been used for many years,"but are now mainly of historical interest as wit-
nessed by the results of questionnaire surveysconducted among obstetricians in Europe"'''and Australia."' Still others, such as magnesiumsulfate24.4'.4" and diazoxide,49 have been reported
to be widely used in some centers in theUnited States, although there are no controlled
trials which have shown them to be moreeffective than placebo for inhibiting pretermlabor. Admittedly, magnesium sulfate has beencompared with other drug treatments in fourcontrolled trials."--" Neither of these has, onbalance,'' invalidated the opinion expressedeven by proponents of this tocolytic treatmentthat, "once labor has brought about cervicaldilatation, the drug is reasonably ineffective."4-
In the light of present day evidence, only
two categories of drugs merit consideration interms of their potential benefits for inhibitingpreterm labor. These are betamimetic agents and
inhibitors of prostaglandin synthesis. Calcium
antagonists, although comprising a wide catego-
ry of different chemical compounds with inter-esting properties, have been so poorly evaluated
for the inhibition of preterm labor493."' that they
cannot, as yet, be considered to have any clini-cal value for this indication.
Interventions
Betamimetic drugsBetamimetic agents are used more exten-
sively than any of the other approaches that areemployed to achieve tocolysis in pretermlabor.""7 Since the first reports in 1961;4°9 agreat variety of betamimetic drugs have beenapplied to the inhibition of preterm labor. Theyhave included, among others, isoxsuprine,44."orciprenaline,"° mesuprine," ritodrine ,62
fenoterol," salbutamol,"4 buphenine, hexopre-naline,"" and terbutaline."'
There is a wealth of literature on the phar-
macological effects of betamimetic drugs. They
are all chemically and pharmacologically relat-ed to the catecholamines, epinephrine(adrenaline) and norepinephrine (nora-drenaline), and all stimulate the 13- receptorsthat are present in the uterus and in otherorgans throughout the body."8 Many effortshave been directed at developing agents thatwould selectively stimulate the S-2 receptors in
the uterus. These efforts have only partiallybeen successful, and all betamimetic agentsavailable also stimulate to some extent S-1
receptors. Beta-2 selectivity currently onlymeans that interaction with 1-2 receptorsoccurs at lower agonist concentrations thaninteraction with 1-1 receptors. Stimulation of 13-
1 receptors is responsible for actions such as anincrease in heart rate and stroke volume, relax-
ation of intestinal smooth muscle, and lipolysis.
Beta-2 stimulation mediates glycogenolysis andrelaxation of smooth muscle in the arterioles,
the bronchi, and the uterus.
Placebo controlled trialsOnly three of the many betamimetic agents
available (isoxsuprine, ritodrine, and terbu-
Marc Keirse229
212
Advances in the Prevention of Low Bird:weight
Wine) have ever been compared with a controlgroup, who received either no active treatmentor placebo, for inhibition of preterm labor.Some of the drugs (such as salbutamol orfenoterol) that were reported to be used byone-third of the obstetricians in Belgium," theNetherlands," and the United Kingdom" havenever been tested against placebo or no treat-ment in preterm labor. Yet, they entered obstet-rical practice at about the same time" as otherdrugs, such as ritodrinetu or terbutaliner'"which have been subjected to several placebocontrolled trials.
Seventeen studies have been published inwhich one or another betamimetic agent wasreported to have been compared against nolabor-inhibiting drugs in preterm labor.1"2°""'""Five of these 17 studies'2"4.".' were either con-ducted or reported in a manner that precludesunbiased evaluation of the treatment given.Penney and Daniell"' reported on the use of aprolongation index for their trial, but providedno data on outcome by treatment allocation.The reasons why the four other trial reportswere considered to introduce too much bias inevaluating the effects of betamimetic treatmenthave been elaborated by King and his col-leagues." Data on four unpublished ritodrinetrials, conducted by Barden,'" Hobel,"Mariona,* and Scommegna and Bieniarzr andincluded in the report of Merkatz et al.- couldbe obtained by courtesy of the investigatorsand the company (Duphar) that manufacturesthe drug." The characteristics of the resultingtotal of 16 (published and unpublished) trialswith adequate data have been described byKing et al." These 16 trials involved a total of484 betamimetic-treated women and 406
230
women treated with placebo or some standardtreatment. All but one" of these trials involvedthe use of oral betamimetic maintenance thera-py after acute tocolysis had been achieved. Thelarge majority of the trials (12 of the 16) dealtwith ritodrine, 3 tested terbutaline, and 1, theoldest trial, dealt with isoxsuprine. Allocation tothe treatment or control group was stated tohave been blind in 11 of the 16 trials. In theothers, the method of allocation was either notdescribedu or was such that the investigatorsmay have known in advance to which groupthe woman would be allocated.""" For 12 of the16 trials, data were available on all womenentered. That information had often not beenpublished in the original reports, but King etal." succeeded in obtaining additional datafrom the authors in order to minimize the intro-duction of bias after trial entry.'"
King and his colleagues" conducted a for-mal meta-analysis of these 16 trials, using meth-od.s described by Peto et al;"' and Yusuf et al."This approach, which is extensively discussed byChalmers et al.,'" is based on calculating a ratio(odds ratio) for each trial between the odds of a
particular outcome, among women allocated tobetamimetic drug treatment, and the odds of thesame outcome, among women allocated to thecontrol group. The sum of the differencesbetween active treatment and control derivedfrom the independent trials, used in combinationwith the sum of the variances of these differ-ences, is then used to calculate a typical oddsratio. The latter provides a more sensitive esti-mate of the effect of treatment than can be ob-tained from the individual, and often small trials.
This is illustrated in figure 19.1, whichshows the effect of betamimetic drug treatment
2 I. a Inhibition of Preterm Labor
on the incidence of delivery within 24 hours oftrial entry in the 14 studies that provided infor-mation on this outcome. For each of the trials,
the figure shows the ratio between the odds inthe betamimetic treated group and in the con-trol group, with its 95 confidence interval. Anodds ratio of 1 indicates that the tiutcomeoccurs with the same frequency in the treat-ment as in the control group. An odds ratio ofless than 1 indicates that fewer women in thetreatment group delivered within 24 hours thanin the control group, while an odds ratio above1 indicates the reverse. A 95 percent confi-dence interval that crosses the vertical line,drawn at an odds ratio of 1, indicates that thedifference between the treatment and controlgroups is not statistically significant. A confi-dence interval that does not cross the verticalline, drawn at an odds ratio of 1, indicates astatistical significance at the 5 percent level orless. The figure illustrates that there were fewerdeliveries within the first 24 hours in the groupallocated to betamimetic treatment than in thecontrol group in 12 of the 14 studies, but that
this reached statistical significance in only 6 ofthem. The typical odds ratio across trials,however, was statistically highly significant, asillustrated in figure 19.2.
Figure 19.2 shows the typical odds ratios(across trials) with their 95 percent confidenceintervals for the incidences of delivery within
24 hours of trial entry, delivery within 48 hoursof trial entry, delivery before 37 weeks of gesta-tion, delivery of a low birthweight infant, respi-ratory distress and/or respiratory disease, andperinatal death not due to lethal congenitalmalformations. Further details on all of theseoutcomes have been described by King et al."
Interventions
Overall, the data from the controlled com-parisons of betamimetic drug treatment inpreterm labor thus convincingly demonstratethat the treatment results in a significant delayof delivery and in a lower incidence of pretermbirth than observed without such treatment(see figure 19.2). As mentioned earlier, in allhut one of the trials,-' acute tocolysis was fol-lowed by oral maintenance treatment, and it ispossible that this component of the betamimet-ic drug administration may have contributed tothe overall gain in gestational age. The threeplacebo controlled trials that have been report-ed on oral maintenance treatment, after anacute episode of preterm labor had been over-come,'''-"4 showed that oral maintenance treat-ment will to some extent prevent a recurrenceof preterm labor.4'
The data on the incidence of low birth-weight also suggest a beneficial effect ofbetamimetic drug treatment on this outcome,although this did not reach conventional levelsof statistical significance, with a 95 percent confi-dence interval from 0.55 to 1.02 (see figure 19.2).
The effects on delay of delivery, gestation-al duration, and birthweight did not, however,result in a detectable decrease in the incidenceof more serious infant outcomes. The incidenceof perinatal death not attributable to lethal con-genital malformations and that of severe respi-ratory disorders, including respiratory distresssyndrome, was similar in the treatment andcontrol groups. The typical odds ratio for respi-ratory distress syndrome and severe respiratorydisorders in the newborn across the 12 trials,which provided information on that outcome,was 1.07, with a confidence interval from 0.71
to 1.61 (see figure 19.2). Data for the individual
Marc Keirse 231
214
Advances in the Prevention of Low Birthweight
trials are illustrated in figure 19.3. The typicalodds ratio across the 15 trials, which provideddata on perinatal death, was 0.95, with a confi-dence interval from 0.55 to 1.67 (see figure19.2). These results are compatible with animpressive reduction in perinatal mortality ofabout 40 percent, but they are equally compati-ble with an increase in perinatal mortality ofabout the same magnitude. The lack of statisti-cal power in the individual trials is amply illus-trated in figure 19.4.
The apparent lack of effect of betamimeticdrug treatment on the serious adverse out-comes of mortality and respiratory morbiditymay be due to a number of factors. The trialsmay have included too large a proportion ofwomen in whom postponement of delivery andprolongation of pregnancy were unlikely toconfer any further benefit to the baby. A treat-ment that is effective in stopping preterm laborat 36 weeks may well reduce the likelihood ofdelivery within 24 hours, of delivery before 37weeks, and of delivering a low hirthweightinfant; but at that gestational age it will have lit-tle potential for reducing perinatal mortality orserious morbidity. The lack of effect on infantmortality and respiratory morbidity may also bedue to adverse effects of the drug treatment.These need not be direct adverse effects, butmay also result from prolongation of pregnancywhen this is contrary to the best interest of thebaby, as may be the case with clinically unrec-ognized placental abruption, severe pregnancy-induced hypertension or intrauterine growthretardat;on. It is also possible that too little usewas made of the time gained by postponingdelivery. Only four of the trial reports, forinstance, indicated whether or not corticos-
232
teroids had been given before delivery,although this treatment is known to reduceperinatal mortality and morbidity."'
Controlled comparisons with other drugsEight reports on controlled comparisons
between betamimetic agents and ethanol forthe inhibition of preterm labor have appearedin the literature.")197-h"2 Castren et al.' reporteda study in which every other patient was allo-cated to buphenine and the others to ethanol,but this alternate allocation resulted in 43buphenine- and 50 ethanol-treated women.This study was excluded from meta-analysis, asit was too likely to introduce bias into the com-parison. The report of Merkatz et al." containedno usable data on the 153 women who hadbeen randomized to ethanol or ritodrine, but150 of these women had been included in aprevious report by Lauersen et al.,"" and someof these had also been reported on by Fuchs:*
The characteristics of the trials that wereless unlikely to have introduced bias into thecomparison and the betamimetic agent used inthese trials are summarized in table 4. Althoughthe three largest trials all excluded somewomen after randomization, no attempts weremade to obtain unpublished data from theauthors. Widely different cut-off points havebeen used in these trials for describing delay ofdelivery, but four reports"-'"2 provided infor-mation on the number of deliveries within twoor three days after treatment allocation, In 2reports this related to delivery within 48hours;'"'" in 1 it related to delivery within 3days;'" and in the other, to an insufficient delayof delivery for a full 36 hours course of cord-costeroids to be given,9- These data have been
215 Inhibition of Preterm Labor
combined in figure 19.5. The typical odds ratioof 0.38, with a confidence interval from 0.23 to0.64, convincingly shows that betamimeticagents are superior to ethanol for delayingdelivery.
Two controlled comparisons have beenreported between magnesium sulphate and abetamimetic agent, either ritodrine" or terhu-taline." One of these only reported on the inci-dence of hypothermia with both treatments." Inthe other report, the method of randomizationwas not mentioned and oral ritodrine was usedfor maintenance treatment in both groups."
Several controlled comparisons have beenconducted between different betamimeticdrugs.'"3-"" The interpretation of such studies isdifficult, however, as the authors of the studiesthemselves often recognize. None of the stud-ies has been large enough to have had achance of detecting or excluding importantdifferences in the outcomes that really matter,such as infant mortality and morbidity. Nor didthe trials show that any one of the drugs test-ed was remarkably free of maternal sideeffects. When differences in the incidence ofmaternal side effects or in average gain in ges-tational age were detected, it is never entirelyclear whether the drugs were used in equipo-tent doses. The wide differences amongbetamimetic drugs in their ratio between drugweight and drug effect make this nearlyimpossible to assess. Without a dealer delin-eation of both benefit and harm, such smalldifferences are difficult to interpret, irrespec-tive of whether or not they reach statistical sig-nificance. None of the studies thus far hasinvestigated the differential in the costs oftreatment between one drug and another.
Marc keirse
Interventions
Unwanted effectsA number of subjective maternal symp-
toms may occur as a result of betamimetic-induced changes in many bodily functions. Themost frequently observed are palpitations,tremors, nausea, and vomiting. Headache,vague uneasiness, thirst, nervousness, and rest-lessness may also occur. Chest discomfort andshortness of breath should alert to the possibili-ty of pulmonary congestion.
From the placebo controlled trials dis-cussed above, there is little evidence thatbetamimetic drug treatment frequently posesgreat hazards to either mother or baby. This isnot necessarily convincing in view of the factthat all 16 trials together contained less than500 betamimetic-treated women. This is proba-bly less than one percent of the number ofwomen who annually receive treatment withone of these agents because they are at risk ofdelivering preterm. The likelihood that rare butserious adverse effects of betamimetic drugs, ifthey exist, would have been uncovered by anyone of these trials must be infinitely small.Other data in the literature, however, indicatethat these drugs are not entirely harmless.
In the late 1970s in West Germany, inci-dents of pulmonary edema, congestive cardiacfailure, and even death started to be noticedin young women who had received thebetamimetic drug, fenoterol, in combinationwith corticosteroids for preterm labor.""-"2Within a year, a case of severe pulmonaryedema following administration of terbutalineand dexarnethasone was reported from theUnited States,-4' and by 1980, a large numberof such reports had appeared in the medicalliterature." 4. 1"
216 233
Advances in the Prevention of Low Birthweight
Initially, much of the blame for this dread-ful complication was directed at conicosteroidadministration, which had been the morerecently introduced of the two drug treat-ments, or at a cumulative and potentiatingeffect of corticosteroids and betamimetic drugs.As more of these reports became available, pul-monary edema was recognized to be a compli-cation not only of the combination ofbetamimetics with corticosteroids, but also ofbetamimetics used alone.
Many of the cases described have beensecondary to fluid overload, and no instance ofpulmonary edema has been reported in womenreceiving betamimetics orally. Fluid overloadduring betamimetic treatment can occur by twomechanisms: (I) By too vigorous administrationof intravenous fluids; and (2) by decreasedrenal excretion of sodium, potassium, andwater as a direct result of high doses ofbetamimetics. The antidiuretic effect ofbetamimetics is most pronounced in the first 48hours of tocolytic treatment, and that is whenmost cases of pulmonary edema are observed.In experimental animals, the development ofintravascular hypervolaemia during betamimeticadministration has been directly correlated withincreasing doses of the betamimetics and withincreasing rates of crystalloid infusion.'2' Bothof these concur when betamimetic drugs areadministered in dilute solutions; the higher thedose, the larger the amount of fluid.
Excessive hydration has long been prac-ticed, apparently to combat the risk of hypoten-sion,us which is rarely a problem since thebetamimetic influence on blood pressure mainlyconsists of a widening pulse pressure, due to anincrease in systolic and a decrease in diastolic
234
pressures. Nevertheless, liberal administration ofcrystalloid fluids became standard practice, withas much as 400 mrm' to 1,000 of intravenousfluids often being administered routinely for 30minutes even before starting infusion withbetamimetics. Apparently, this practice hascaused more harm than it prevented.
The frequency with which pulmonaryedema develops during betamimetic drugadministration is difficult to estimate. Katz et
observed clinical signs and symptoms ofpulmonary edema in 5 percent of 160 womentreated with terbutaline for preterm labor, buthalf of the women with this complication hadtwin pregnancies. Multiple pregnancy, as wellas underlying heart disease and the use of cor-ticosteroids or multiple drugs in addition to thebetamimetic agents, is known to increase therisk of pulmonary edema. If 5 percent were areasonable approximation of the frequency ofthis complication, it would have been observedand described much earlier than in the late1970s, and it would have been noted in severalof the women who participated in the placebocontrolled trials. It is possible that this compli-cation occurs more frequently with terbutalinethan with other betamimetic drugs, as suggest-ed by Robertson et al."' Whether or not this istrue and whether or not it relates specifically tothis agent or to the way in which it is adminis-tered is not clear:" 12-
Myocardial ischaemia has been describedas the other main, but rare complication ofbetamimetic drug treatment.''' )44 This compli-cation is a separate entity from that of pul-monary edema. Diffuse micronecrosis in themyocardium has been known since 1959, whenit was induced in the rat by administration of
21; Inhibition of Preterm Labor
isiproterenol.L" Similar lesions have beenobserved in the myocardium after betamimetic-related death. Unlike genuine myocardialinfarcts, micronecrosis is not a direct result ofhypoxia. It relates to the increasing energy andoxygen requirements of the beta-stimulatedmyocardial cell; if demand exceeds supply,ischaemia develops.
Betamimetic drug administration results ina marked increase in cardiac output in preg-nancy, which is roughly of the same order asthat observed during moderate exercise.9sThis increase is attributed to the combination ofan increase in heart rate and a decrease inperipheral vascular resistance due to relaxationof vascular smooth muscle. In late pregnancy,cardiac output is already 40 percent aboveprepregnancy values, and the increase is evenlarger in twin pregnancies." The additionalwork imposed on the myocardium bybetamimetic drug treatment may thus becometoo much for women with preexisting, overt, orhidden cardiac disease.s4) These women shouldnot be given betamimetics, as the hazards forthem are likely to be greater than any benefitthat could be derived for their infants. For thesame reason, it is wise to insist on a normalelectrocardiogram before betamimetics areadministered. The likelihood of finding anabnormal electrocardiogram in a normal preg-nant woman without symptoms or suggestivehistory must he small, however. Nor can it beimplied that a normal electrocardiogram beforetreatment will protect against subsequent devel-
opment of pulmonary edeina.'2''A few trials have addressed the question as
to whether the combination of betamimeticswith other treatments could reduce some of the
Marc Keirse
Intetventions
unwanted effects of the betamimetic drugs.Some have involved the use of different infu-sion fluids,"" but it is clear that the amount offluid is far more important than the type offluid. Others have centered on the use of calci-um antagonists or 1-1 receptor blockers toreduce the systemic, and especially the cardio-vascular, effects of betamimetic agents. To beof value, such combination treatments shouldbe demonstrated to achieve at least one of thefollowing three aims. First, infant outcome interms of mortality and serious morbidity shouldbe better with/ qe combined treatment thanwith the singl treatment. Second, the additionof these drugs should decrease the incidence ofserious maternal complications duringbetamimetic drug treatment. Third, the com-bined treatment should significantly decreasethe incidence of less serious, but troublesome,maternal side effects. Thus far, there are noindications that any one of these goals hasbeen adequately met.
inhibitors ofprostaglandin synthesisThere is substantial evidence that
prostaglandins are of critical importance in theinitiation and maintenance of human labor."'Suppression of endogenous prostaglandin syn-thesis is therefore a logical approach to theinhibition of preterm labor. Several agents withwidely different chemical structures and phar-macokinetic properties'42 inhibit prostaglandinsynthesis. They are sometimes referred to asprostaglandin synthetase inhibitors. Since thereis no enzyme of this name, they are betterreferred to as inhibitors of prostaglandin syn-thesis. The inhibitors that have been used totreat preterm labor include naproxen,'" flufe-
21S235
Advances in the Prevention of Low Birthweight
namic acid,'" and acetyl salicylate,14"46 but themost widely used has been indomethacin.'"
All of these drugs act by inhibiting theactivity of prostaglandin endoperoxide syn-thase, an enzyme also known as cyclooxyge-zase. This enzyme converts fatty acids,arachidonic acid in particular, into prosta-glandin endoperoxides. It is present in highconcentrations in the myometrium of pregnantwomen,"8 but is found throughout the bodyboth in and outside pregnancy. Inhibition ofthat enzyme does not only suppressprostaglandin synthesis. It also suppresses theformation of prostacyclin and thromboxane A2,both of which may have a number of impor-tant, though largely unknown functions inpregnancy.'"" Inhibition of the enzyme is notalways achieved in the same way. Aspirin, forexample, causes an irreversible inhibition ofthe enzyme, whereas indomethacin results in acompetitive and reversible inhibition. This isbecause aspirin acetylates the enzyme, andthereby incapacitates it permanently.Indomethacin, on the other hand, competeswith arachidonic acid for utilization by theenzyme; it leaves the enzyme itself intact, and,when indomethacin levels decrease, theenzyme can resume activity.
All prostaglandin synthesis inhibitors areeffective inhibitors of myometrial contractility.both in and outside pregnancy. There is alsono doubt that they are more effective in thisrespect than any of the betamimetic drugs. Nocase has been reported in which a betamitneticdrug resulted in suppression of uterine contrac-tility after inhibition of prostaglandin synthesishad failed, while the reverse has repeatedlybeen observed."
236
Controlled comparisonsOnly two studies have been reported that
purported to compare a prostaglandin synthesisinhibitor with placebo in preterm lahor.'"1"Both used indomethacin as the active treat-ment, and both were stated to have been con-ducted in a double-blind manner. Neither ofthem was entirely placebo controlled, however,since a number of women in whom treatmentwas considered to have failed received othertocolytic drugs. In addition, three controlledstudies have been conducted in which aprostaglandin synthesis inhibitor was eitheradded or not added to treatment with otherlabor-inhibiting drugs. All of these trials alsoused indomethacin, while the other drug treat-ment used ethanol in one trial" and thebetamimetic agent, ritodrine, in the othertwo.'41" Eight reports were available on thistotal of five trials.t22 "
There are reservations al)out the heteroge-neous nature of these trials and about potentialbias in many of them. On the whole, these tri-als are of inferior quality compared with thoseof the placebo controlled trials of betamimeticagents. Nevertheless, the data that could reli-ably be extracted from all of the3e reports havebeen combined in a formal meta-analysis, theresults of which are shown in figure 6. Somereservations should be expressed, however,with regard to the interpretation of these data.The results show that indomethacin, eitheralone or in combination, was statistically signif-icantly more effective in delaying delivery for atleast 48 hours, for at least 7 to 10 days, andbeyond the preterm period than the controltreatments, which consisted of placebo,ethanol, and betamimetic agents. The typical
Inhibition of Preterm Labor
odds ratios for these outcomes, however, areeach based on only 2 of the 5 trials. There alsowas a statistically significant reduction in theincidence of low birthweight in theindomethacin-treated group across the 4 trialsthat reported on this outcome (see figure 19.6).
All reports provided data on fetal andneonatal death. Overall, the data show noreduction in the incidence of fetal and neonataldeath with the use of indomethacin in pretermlabor. The typical odds ratio of 0.61 had a con-fidence interval from 0.33 to 1.11. The inci-dence of respiratory distress syndrome alsoshowed no real difference between theindomethacin and the control groups across tri-als, with a typical odds ratio of 0.62 and a wideconfidence interval from 0.25 to 1.58.
None of the trials indicated that the use ofinhibitors of prostaglandin synthesis was associ-ated with an increased incidence of majorproblems for either mother or baby. On theother hand, none of these trials were trulyplacebo controlled, and the number of womenincluded in these trials has not been largeenough to stand a chance of uncovering rareadverse effects.
Unwanted effixtsInhibitors of prostaglandin synthesis are
not innocuous. Three points need to be consid-ered. First, there are numerous potential sideeffects because of the ubiquitous nature of theprostaglandins. Second. the drugs and dosesthat are used for inhibition of preterm laboralso suppress prostacyclin and thromboxanesynthesis. Third, the drugs are both chemicallyand pharmacologically so different from eachother that they should not be considered as
Interventions
interchangeable."' They may roughly fulfill thesame function, but this does not mean that theywill all have the same effects and ill-effects.
The most serious potential side effects arepeptic ulceration, gastrointestinal and otherbleeding, thrombocytopenia, and allergic reac-tions. Gastrointestinal irritation is common with
the use of prostaglandin synthesis inhibitors,and it can occur irrespective of the route ofadministration. With indomethacin it is less fre-quent with rectal than with oral administration,and, as the bioavailability of the drug is identi-cal with both routes of administration,'''' therectal route offers some advantage. Nausea,vomiting, dyspepsia, diarrhea, and allergic rash-es have all been observed in women treated,even briefly, with prostaglandin synthesisinhibitors in preterm labor. Headache anddizziness may occur at the very start of treat-ment. Gamissans and his associates's' reportedsystematically on the incidence of headache,maternal tachycardia above 120 heats perminute, vomiting, epigastric pain, and rectal
intolerance in their trial comparingindomethacin with placebo in association withritodrine treatment. Only two of these sideeffects were observed more frequently in theindomethacin-treated group. Epigastric painwas observed in 6 (4%) and rectal intolerancein 7 (5%) of 148 indomethacin treated women;these symptoms occurred in only 2 of 149women in the control group.
Prostaglandin synthesis inhibitors crossfrom the mother to the fetus1 ' and may influ-ence several fetal functions. A great deal ofinformation has been gathered on the fetaleffects of these drugs in experimental animals.The results are not always easy to interpret,
Marc Keine 237
220
Advances in the Prevention of Low Birthweight
however, because of the variety of speciesstudied, and differences in the type of drugused and in the dose, route, and duration ofadministration. Apart from a prolonged bleed-ing time, which is a constant feature in infantsborn with detectable levels of such drugs,effects in human fetuses and neonates aremostly based on anecdotal reports. The mostconsistent observations relate to the cardiopul-monary circulation and to renal and hemostaticfunctions.'"
The major worries about the use of suchdrugs for the inhibition of preterm labor haveresulted from their influence on the ductusarteriosus. Closure of the ductus after birth con-sists of an initial functional closure by muscularcontraction followed by definitive anatomicalclosure, which is a much slower process that israrely accomplished within the first week oflife. Prostaglandin synthesis inhibitors causeconstriction of the ductus in the neonate, aneffect that has been conclusively demonstratedin placebo controlled trials of neonatalindomethacin administration.'"3."4 Autopsy andcardiac catheterization data from infants whopresented with congestive heart failure at orafter birth, have suggested that severe constric-tion of the ductus may also occur before birthin association with inhibition of prostaglandinsynthesis.119.'m
Constriction of the ductus during fetal lifeprobably has little effect on fetal oxygenationin the short term, as effective shunting can bemaintained through the foramen ovate.,Prolonged prenatal constriction of the ductusarteriosus can lead to pulmonary hypertensionand possibly to tricuspid insufficiency in thenewborn.119 Only two cases of persistent pul-
238
monary hypertension have been reported inthe controlled trials that we reviewed. Both ofthese, one in the placebo group and one in theindomethacin-treated group, occurred inGamissans' trial in women with ruptured mem-branes.'"
Wiqvisr6 compiled reports from controlledand uncontrolled clinical studies in which care-ful pediatric examination of the newborn hadbeen carried out. For a total of 730 mothersincluded in these studies, he found 17 infantswith persistent pulmonary hypertension (2.3%);14 of these infants recovered within a few daysand 3 died. A similar approach was followedby Gamissans and Balasch,t44 who found 19cases (1,5%) among a total of 1,235 womenwho received prostaglandin synthesis inhibitorsin preterm labor; 16 of the infants survived and3 died. Whether or not this incidence is higherthan it would have been without inhibition ofprosuglandin synthesis is impossible to deter-mine from such data.
Data both from experimental animals andhuman neonates suggest that the responsive-ness of the ductus to indomethacin is lower atlower gestational ages. If such a difference inresponsiveness exists in utero, it would implythat the risk of ductus constriction and itspotential sequelae would be smallest whenmost gain is to be made from arresting pretermlabor, and largest at gestational ages whichhardly provide an indication for inhibition oflabor. It is also probable, although this is notborne out by the available controlled anduncontrolled data in preterm labor, that theduration of treatment is of influence. Thelonger prostaglandin synthesis inhibition is con-tinued, the greater the risk is likely to be.
221 Inhibition of Preterm Labor
Indomethacin treatment may alter bothfetal and neonatal renal function. Renal dys-function and reduced urinary output hasrepeatedly been noted in infants treated withindomethacin to close a patent ductus arterio-sus.'""-"'9 The effect is apparently dose relatedand transient. Renal function usually returnstoward pretreatment values within 24 hoursafter stopping the treatment."'s Several reportshave indicated impaired renal function in fetus-es and in the neonates at birth followingadministration of prostaglandin synthesisinhibitors to the mother.''2 Long-term mater-nal treatment may influence fetal urine outputenough to alter amniotic fluid volume, althoughother mechanisms may also be involved in thereduction of amniotic fluid volume occasionallyseen during indomethacin treatment.'' There isno evidence from either maternal or neonatalindomethacin treatment that the use of thisdrug in preterm labor would lead to permanentimpairment of renal function in the infant."
Inhibitors of the cyclooxygenase enzymeall inhibit platelet aggregation and prolongbleeding time. They do so in the mother, in thefetus, and in the neonate at birth.'N Sinceneonates, and particularly preterm neonates,eliminate these drugs far less efficiently thantheir mothers,"2.r4 these effects will be of longerduration in the baby than in the mother. Thereare major differences in this respect betweendifferent inhibitors of prostaglandin synthesis.Salicylates are particularly troublesome. Asmentioned earlier, they acetylate the cyclooxy-genase enzyme and permanently incapacitateit. Unlike most cells in the body, bloodplatelets cannot manufacture new enzyme. Thisimplies that not only the cyclooxygenase
Marc Keirse
Intenfentions
enzyme, but that also the platelets themselvesare rendered permanently nonfunctional. Theycannot restore normal hemostasis; for this tooccur, they must be replaced by new platelets.
CONCLUSIONS
Hopes that inhibition of uterine contrac-tions can resolve the entire issue of pretermbirth and its associated mortality and morbidityare unrealistic and naive, at best. On thewhole, the proportion of preterm births thatcan be and are worth being averted by tocolyt-ic treatment is not larger than the proportion ofpreterm births that is actually provoked withthe same hopes of avoiding Mortality and mor-bidity. This is not to say that there are no situa-tions in which inhibition of preterm labor isworthwhile. Rather, it emphasizes that stoppinguterine contractions does not necessarily meanimproving outcome either for the mother or forthe baby. Clinicians cannot escape their corn-mitmments and they must provide care forpreterm labor within the constraints of theimperfect knowledge that is available. That willinclude tocolytic treatment, and the main issueis how to maximize potential benefit and mini-mize potential harm.
In that context, only two categories ofdrugs presently merit consideration for the inhi-bition of preterm labor: Betamimetic agents andinhibitors of prostaglandin synthesis. All othersare either obsolete or in an experimenul stage.There is no longer a place for ethanol, relaxin,or progesterone in the treatment of pretermlabor. Oxytocin analogues and calcium antago-nists have been insufficiently studied to asses6
239
Advances in the Prevention of Low Birthweight
whether they have any beneficial effect. Theuse of other drugs, such as magnesium sul-phate or diazoxide, should only be permittedwithin the context of adequately controlled tri-als to determine whether or not their acclaimedbenefits exist and outweigh their knownadverse effects.
This does not imply that the evidence infavor of either the betamimetic agents or theinhibitors of prostaglandin synthesis is beyondreproach. On the contrary, there are manyflaws in the evidence available, particularlywith regard to prostaglandin synthesisinhibitors. Moreover, these two categories ofdrugs contain many compounds, not all ofwhich can be assumed to have the sameeffects. It is also worth remembering that thereare, in these wide classes of agents, drugs thathave never been evaluated against "placebotreatment" in preterm labor; have never beenshown to be superior to other, more validated,drug treatments; and, yet. have caused seriouscomplications, including maternal death.Specific agents that have never been testedagainst placebo or no treatment, or have notbeen shown conclusively to be superior to oth-ers, should probably be dropped from clinicalpractice. There is something to be said for firm-ly convincilg those pharmaceutical industrieswhich propagate such agents that pretermlabor is too serious a problem to be subjectedto drug treatments that have not been evaluat-ed by randomized controlled trials.
Betamimetics and prostaglandin synthesisinhibitors are effective in postponing deliveryand in prolonging pregnancy. There is no evi-dence that the use of these drugs reducesinfant mortality or morbidity. This would imply
that they are only useful when the time that isgained before delivety is used to implementeffective measures. Such measures couldinclude transfer of the mother to a center withadequate facilities for intensive perinatal andneonatal care, the administration of corticos-teroids to reduce perinatal mortality and mor-bidity, or the judicious use of "expectantmanagement" in the period of gestation inwhich the infants' chances of intact survival arevery poor.
Powerful drugs are dangerous when usedinappropriately. Administration of these drugsin preterm labor requires a valid indication andcareful control of maternal and fetal condition.
Betamimetic agents are currently the drugsof choice. For women with cardiac disease,hyperthyroidism, and diabetes mellitus, howev-er, the risks of betamimetic drug treatment willnearly always outweigh its potential benefits.Maternal side effects are inevitable withbetamimetic drug treatment, hut serious com-plications are largely avoidable. There is noevidence that concurrent administration of cal-cium antagonists or S-1 receptor blockers pro-tects the mother against complications ofbetarnimetic drug treatment. Nor is there anyevidence that such combinations are of benefitto the baby. There is enough evidence, albeitobservational, that vigorous hydration causesmore harm to the mother than it prevents.
On the whole, prostaglandin synthesisinhibitors are more powerful inhibitors of uter-ine contractions than the betamimetic agents.There are too few data from controlled compar-isons, and their quality is too poor, to recom-mend prostaglandin synthesis inhibitors as afirst link: approach in the inhibition of preterm
240 ')Inhibition of Preterm Labor
labor. They would appear to be the logicalchoice, however, if labor needs to be inhibitedin women with cardiac disease, hyperthy-roidism, or diabetes or if betainimetic treatmentfails at very young gestational ages. Theirpotential hazards, weighed against potentialbenefits, do not justify the use of such drugs, inthe doses that are necessary to inhibit uterinecontractions, for any longer than is necessary(two or three days). Nor does the available evi-dence justify the use of aspirin and other salicy-lates (in the large doses that are required) forinhibition of preterm labor.
REFERENCES
1. Keirse. M. J. N. C., and Kanhai. 11. II. IL (1981). Anobstetrical viewpoint on preterm birth with particularreference to perinatal morbidity and mortality. In:
11. J. Iluisjes (Ed.). Aspects qf perina(al morbidity(pp 1-35). Groningen. The Netherlands:Universitaire Boekhandel Nederland.
2' Rush, R. Keirse. N. C.. Howat. P.. Baum, .1.D.. Anderson. A. li. M., and Turnbull, A. C. (1976).Contribution of preterm delivery to perinatal mortali-ty. British Medicallouriud 2.965-9M.
3. Christensn. K. K Ingemarsson. 1., Leideman. T.,Solon), 11 and Svenningsen, N. (1980), Effect ofritodrine on labor after premature rupture of themembranes. Obstetrics tind Gynecology 55, 187-190.
Rush, R. W., Davey, 1). A.. and Segall. M. L. (1978).The effect of preterm delivery on perinatal mortality.British ournal (y. Obstetrics aiul Gynaec(?/ogy 85,800-811.
S. Van Kamp. 1.. Kanhai. II., and Keirse, M. N. C.(Forthetnning). The changing pattern of pretermbirth.
6. Keirse, N1.). N. C. (19'9), Epidemiology of pre-termlabor. In: M. J. N. C. Keirse. A. 15. M. Anderson, andJ. Bennebroek Gravenhorst (Eds,), HumanParturition: New Concepts and Developments (pp.219-23.4). The Ilague: Leiden University Press.
Intoventions
7. Tamura, R. K., Sabbagha. R. E, Depp, R., Vaisrub, N,,Dooley, S. L., and Socol, M. L. (1984). Diminishedgrowth in fetuses born preterm after spontaneouslabor or prelabor rupture of the membranes.A merka rt journ(4l of obstetrics and Gynecology 148,1105-1110.
8. Keirse, M. J. N. C. (1989). Preterm delivery. In 1.Chalmers, M. J. N. C. Keirse, and M. W. Encon(Eds.), Effective care in pregnancy and childbirth(Vol. 2, pp. 1ro-i 292). Oxford: Oxford UniversityPress.
9. Kaltreider, 1). E. and Kohl, S. (1980), Epidemiologyof preterm delivery. Clinical Obstetrics andGynecology 23. 17-31.
10, Kanhai. 11. 11. 11. (1981). Achtergnmden en konsek-wenties van vroeggelx)orte. Unpublished MD thesis.Leiden Ilniversity, Leiden, The Netherlands.
11. King. J. E. Grant, A., Keirse. M. J. N. C., andChalmers, I. (1988). lietamitnetics in preterm labor:An overview of the randomized controlled trials.British Journal of Obstetrics and Gynaecology 95,211-222.
12. O'Driscoll. NI. (19 77). Discussion. In: A.
Anderson. R. Beard. J. M. Brudenell, and P. NI.
Dunn (Eds.). Pre-term labor Proceedings of theFifth study (iroup of. the Royal Colhwe ofObstetricians and Gynaecologists (pp. 309-370).London: Royal College of Obstetricians andGynaecol()gists,
13. Cousins, I.. M., llobel, C. J.. Chang. R. J.. Okada. D.NI., and Marshall, J. R. (1977). Serum pnigestenmeand estradio1-17-beta levels in premature and termlabor. American journal of Obstetrics andGynecology 127. 012-615.
14. Suzanne. E. Fresne. J. J.. Portal, 15.. and Baudon, J.(1980). Essai therapeutique de l'indometacine dansles menaces craccouchement premature. 71.Yrapie
35, 75I-760.
15. Agustsson. P., and Patel, N. B. (1987). The predic-tive value of fetal breathing movements in the diag-nosis of preterm labor. British Journal cf Obstetricsaml Gynaecolc)gy 94, 860-8b3,
V). Castle. 15. NI., and Turnbull. A. C. (1983). The pres-ence or absence of fetal breathing movements pre-dicts the outcome of preterm labor. Lancet 2.471-473.
Marc Kelm, 241
224
Advances in the Prevention of Lout Binhuteight
17. Fuchs, A. R., Husskin, P, Sumulong, L.. Mieha, J. P.,Yusoff Dawood, M., and Fuchs, F. (1982), Plastnalevels of oxytoein and 13,14-dihydro-15-keto-prostaglandM F2a in preterm labor and the effect ofethanol and ritodrine. American Journal ofObstetrics and Gynecology 144, 753-759.
18. Noort, W A., De Zwart, F. A., Kragt, H., and Keirse,M. J. N. C. (Forthcoming). Can urinary thrombox-ane excretion presage preterm delivety? EunpeanJournal of Obstetrics. Gynecology. and ReproductiiBiokk)
19. Papiernik, E.. Bouyer, J., Collin, 11, Winisdoerffer.G., and Dreyfus, .1. (1986). Precocious cervicalripening and preterm labor. Obstetrks andGynecology 67, 238-242.
20. Stubblefield, P. G. (1978). Pulmonary edema occur-ring after therapy with dexamethasone and terbu-taline for premature labor: A case report.American Journal (f Obstetrics and Gynecokgy 132,341-342.
21. Anderson, A. B. M., and Turnbull, A. C. (1969).Relationship between length of gestation and cervi-cal dilatation, uterine contractility and other factorsduring pregnancy. American Journal of Obstetricsand 4ynecoh)g3' 105, 1207-121-4.
22. Bell, R. (1983). The prediction of preterm labor byrecording spontaneous antenatal uterine activity.British Journal of Obstetrics and Gynaecology 90,884-887.
23. Katz, M.. Newman, R. B.. and Gill. P. J. (198().Assessment of uterine activity in ambulatory patientsat high risk of preterm labor and delivery.American journal (-,f Obstetrics arid Gyneccilogy 154.44-47.
24. Morales, W. J., Diebel, N. D., Lazar. A. .1.. andZadrozny. D. (1986), The effect of antenatal dexanwthasone on the prevention of respiratory distresssyndrome in preterm gestations with premature rup-ture of membranes. Amerkan Journal of Obstetricsand G:ynecology 154, 591-595.
25. Alexander, S.. and Keirse. M. J. N. C. (Forthcoming).Formalized risk assessment. In: M. W. Enkin.N. C. Keirse. and I. Chalmers (Eds.). Iffective care inpregnancy and childbirth. Oxford: OxfordUniversity Press.
26. BrC!art. G., Gouiard. J.. Blondel, B., Maillard, F.,Chavigny, C., Sureau. C., and Runwau-Rouquette, C.(1981). A comparison of two policies of antenatalsupervision for the prevention of prematurity.International Jouriud of Epidemiology 10, 241-244.
27. FIGO News. (1976). Lists of gynecologic and obstetri-cal terms and definitions. International Journal ofGYnaecology and Obstetrics 14, 570-576.
28. World Health Organization. (1977). Recommendeddefinitions, terminology and format for statistical tablesrelated to the perinatal pericx1 and use of a new certifi-cate for cause of perinatal deaths. Acta ObstetriciaGynecol(frgica kandinavica 56, 247-253.
29. World Health Organization. (1969). Prevention ofperinatal morbidity and mortality. Public healthpapers 42 Geneva: World Health Organization,
30. World Health Organization. 0950). Expert group onprematurity final report. kchnical report series 27Geneva: World Health Organization.
31. World Health Organization (1961). Public healthaspects of low birthweight. Technical report series21 7 Geneva: World Health Organization.
32. \Thrld Health Organization. 0979-1. Definitions andrecommendations. International statistical classifka-lion of diseases (9th rev.). Vol. 1. 763-768. Geneva:World ficalth Organization.
33. Chamberlain. R. (1975). Birthweight and length ofgestation. In: British births /97(/ tiI. I . The firstuwek (00, (pp, 50-88). lAindon: lieinemann.
Ileinonen. K.. I lakulinen, A., and Jokela, V. (1988).Survival of the smallest: Time trends and determinantsof mortality in a very preterm popubtion during the1980s. Lancet 2. 201-20-7.
3i. flollman. H. J.. and Bakketeig. L. S. (198.4). Risk fac-tors associated with the c)ccurrence of preterm birth.clinkal obstetrics and Gynecology 27. 539-552.
36. National Center for Health Statistics. (1985). Monthlyvital statistics report, 34 (Suppl.). 6.
37, Verloove-Vanhorick. S. P.. Verwev. R. A.. Brand. R..Bennebroek Gmvenhorst. J.. Keirse. M. .1. N. C.. andRuvs, J. If. (1986), Neonatal numality risk in relatk into gestati(mal age and birthweight: Results of anational survey of preterm and %.ery-I( iw-birthweightinfants in the Netherlands. lancet 1. 55-57,
242 Inhibition (y- Preterm Labor225
`Z:541.
38. Verkmve-Vanhorick, S. P.. and Verwey. R. A. (1987).Project on preterm and small for gestational ageinfants in the Netherlands 1983: A collaborative sur-vey. Unpublished MD thesis. Leiden University,Leiden. The Netherlands.
39. McGregor. J. A., French, .1. I., Re Her, L. 13 Todd. J.K.. and Makowski. E. L. (198(). Adjunctive ery-thromycin treatment for klic)pathic prewrm labor:Results of a randomized, double-blinded, placebocc)ntRilkd trial. American journal q,1 Obstetrics andGynecology 15.1. 98-103.
40, Akerlund. M.. Straml)erg. P. Hauksson. A., Andersen,L. F.. Lyndrup, J.. Trojnar, J.. and Melin. P. (1987).Inhibition of uterine contractions of premature laborwith an oxytoein analogue: Results from a pilotstudy. British journal of Obstetrics awl Gyiuwcology94, 1040-1044.
8. Keirse, M. J. N. C. (1989). Preterm delivery. In 1,Chalmers. NI. J. N. C. Keirse. and NI. W. Encon(Eds.), Effective care in pregnancy and childbirth(Vol. 2, pp. 1270-1292). Oxford: Oxford UniversityPress.
42. Turnbull, A. C. (1987). Commentary: An oxvtocininhibitor for suppressing preterm labor. Britishjournal of Obswtrics and Gynaecology 9i,1009-1013.
43. Fuchs. F., and Fuchs. A-R. (1984). Ethanol for theprevention of preterm birth. In: F. Fuchs and P. C.Stubblefk.ld (Eds.), Preterm birth: Otuses. prawn-tion and management (pp. 207-222). New York:Macmillan.
44. Keirse, NI. J. N. C. (1984). A survey of tocolvticdrug treatment in pretenn labor. British Journal ofObstetrics and Gynaeccdov 91. 421-130,
45. Lewis. P. J.. de Swiet, M Boylan, P., and Bulpitt, C.(1980). How obstetricians in the Vnited Kingdom
manage preterm labor. British journal of OhqviricsWid Gynaecology 87,574-577.
Trudinger, B. J.. and Hoshell, L. (1987). A survey ofthe management of premature labor by Australianobstetricians. Australian and Neu. Zealand Journalof obstetrics wul Gynaecology 27, 188-195.
.17. Petrie, R. 11. (1981). I( wolysis using magnesium sul-fate. Seminws in Pehnatology 5, 2(6-23,
Spisso, K. R., I larbert. G. M.. Jr. and Thiagarajah. S.(1982). The use of magnesium sulfate as a primary
intementions
tocolytic agent to prevent premature delivery.American journal of Obstetrics and Gyiwcology 142,840-8.45.
49, Adamsons, K.. and Wallach. It C. (1984). Dia/oxideand calcium antagonists in pretenn labor. In: F.
Fuchs and P. C. Stubblefield (Eds.), Preterm birth:Causes. prevention and management. (pp. 249-263).New York: Macmillan.
50. Eskes, T. K. A. 13., Kornman, J. J. C. NI.. Buts, It S. G.M., Hein. P. R., Gimbnl.re. J. S. F., and Nimk. J. T. C.(1980). Maternal morbidity due to beta-adrenergictherapy: Ike-existing cardiomyopathy aggravated byfe not e ro I . ropea Pi jou rual of Obstetrics.6:ynecologv. and Reproductity Biology 10. 41-44.
51. Parsons. NI. T.. Owens. C. A., and Spellacy. W. N.(1987 ). Thermic effects of tocolytic agents:Decreased temperature with magnesium sulfate.Obstetrics and qynecology 69, 88-90.
52, Steer. C. NI.. and Petrie. R. 11. (1977). A comparisonof magnesium sulfate and alcohol for the preventionof -preMittlre labor. American journal of Obstetricsand Gynecohmgy 129
53. Tchilinguirian, N. C., Natem. R.. Sullivan. C. 13.. andCraparo, F. 3. (1984). The use of ritodrine and mag-nesium sulfate in the arrest of premature labor.International louriud of 6:ynaecology and Obstetrics22,117-123.
51. ,Andersscin, K. F. (1977). Inhibition of uterine activi-ty by the calcium antagonist nifedipine. In: A.
nderson, R. Heard. J. M. lirudenell. and P. NI. Dunn(Eds.), Pre-term labor Proceedings (y. the Fifth StiulyGroup of the Royal (ollege of Obstetricians andGynaecologists (pp. 101-11.0. London: RoyalCollege of Obstetricians and (...lynaecologists.
55. Read, NI. I) and \XCliby, D. E. (1986). The use of acalcium antaw mist (nifedipine) to suppress pretermlabor. British journal mf Obstetrics mind Gynaecokmgy93,9,23-937.
Ilmsten, Andersson. K. E., and Wingerup. L.(1980). Treatment of premature labcir with the calci-mn antagonist nifedipine. Archires qf Gynecology2"). 1-c.
Keirse, M. 1. N, C. (1984). lietamimetic drugs in theprophylaxis cif preterm labor: Extent and rationaleof their use. l3ritish Journal of Obstetrics amid(J:vnaecofiNy 91. t3 1-437.
Marc Keirse 2,43
226
Advances in the Prevention of Low Birthweight
58. Bishop, E. 11,. and Woutersz, T. B. (1961).Ismcsuprine, a myometrial relaxant: A preliminaryreport. Obstetrics and Gynecology 17, 442-446.
59. Hendricks, C. H., Cibils, L. A., Pose, S. V.. andEskes. T. K. A. B. (1961). The pharmacologic con-trol of excessive uterine activity with isoxsuprine.American journal Obstetrics and Gynecology 82.
1064-1078.
60. Baillie, P., Meehan, F. P., and Tyack, A. J. (1970).Treatment of premature labor with oreiprenaline.British Medical Journal 4, 154-155.
61. Barden. T. P. (1971). Inhibition of human prema-Lute labor by inesuprine hydrochloride. Obstetricsand Gynecology 37. 98-105.
62. Wesselius-De Casparis, A., Thiery, M., Yu Le Sian,A., Baumgarten, K.. Brosens. I,, Gamissans, 0.,Stolk, J. G., and Vivier, W. (1971). Results of dou-
multicentre study with ritodrine in prema-ture labor. British Medkal Journal 3. 144-147.
63. Edelstein, H., and Bane. P. (1972). The use offenoterol (Berotec) as compared with orciprenaline(Alupent) in the treatment of premature labor: A
companaive study. Med Prot* 18, 92-96.
64. Liggins, G, C., and Vaughan, G. S. (1973).Intravenous infusion of salbutamol in the manage-ment of premature labor. Journal qt. Obstetrics andGynaecology of the Britith Commonwealth 80,29-33.
65. Gummerus. M. (1975). fiemnning der drohendenFrOhgeburt mit Nylidrin und Verapamil. Zeitschrill
Geburtshilfe und Perinatologie 179, 261-266.
66. Lipshitz. Bane. P., and Davey. D. A. (1976), Acomparison of the uterine 14-2-adrenoreceptor selec-tivity of fenoterol, hexoprenaline. ritodrine andsalbutamol, South African Medical journal SO,1969-1972,
67. Ingemarsscm, I. (1976), Effect of terbutaline onpremature labor: A double-blind placebo con-trolled study, American Journal qf Obstetrics andGynecology 125, 520-524.
68. Eskes, T. K. A. 13.. and Essed. G. G. NI. (1979).Inhibition of uterine contractility with Is-mimeticdrugs. In: M. J. N. C. Keirse. A. 13. M. Anderson.and J. Bennebroek Gravenhorst (Eds.), Human par-turition (pp. 165-187). The Hague: LeidenUniversity Press.
69. lngemarsson. 1,, Azulkumaran, S.. and Kottegoda, S.R. (1985). Complications of betamimetic therapy inpretenn lalxir. Australian and Arm' Zealand Journal(fObstetrics and Gynaecology 25,182-189.
70. Adam, G. S. (1966). Isoxuprine and prematurelabor. Australian and New Zealand Journal ofObstetrics and Gynaecology 6, 294-298.
71. CaiderA. A., and Patel, N. B. (1985), Arebvtamimetics worthwhile in preterm In: R.
W, Beard and F. Sharp (Ed.s.), Pre-term labor and itsconsequences: Proceedings qf the Thirteenth StudyGroup of the Royal C.'cillege of Obstetricians andGynaecologists (pp. 209-218). London; RoyalCollege of Obstetricians and Gynaecologists.
Castren, 0,, Gummerus, NI., and S ..rikoski, S.(1975). Treatment of imminent premature labor: A
ccnnparison between the effects of nylidrin chlorideand isoxuprine chloride as well as of ethanol. ActaObstetrica et Gynecologica Scandinarica 5.i, 95-100.
73. Cotton, D. 13,, Strassner, H. T., Hill. L. M., Schifrin, B.S., and Paul, R. H. (1984). Comparison of magne-sium sulfate. terbutaline and a placebo for inhibitkmof preterm labor: A randomized study. ournal ofRepmductity Medicine 29, 92-97.
74. Csapo, A. I.. and Herczeg, J. (1977). Arrest of pre-mature labor by isoxsuprine. American Journal qfObstetrics and Gynecology 129, 482-491.
75. Das. R. (1969). Isoxsuprine in premature labor.journal of Obstetrics and Gynaecology of India.
566-570.
70. Howard, T. E., Killam. A. P., Penney, L. L., andDaniell. W. C. (1982). A double-blind randomizedstudy of terbutaline in premature labor. MilitaryMedicine 147. 305-307.
77. Larsen. .1. F.. Eldon. K.. Lange, A. P. Leegaard.Osler. M.. Sederberg Olsen. J.. and Permin, M.(1986). Ritodrine in the treatment of preterm labor:Second Danish multicenter study. Obstetrics andGynecology 67, 607-613.
78, Larsen, J. F.. Hansen, M. K.. Hesseldahl, H.,Kristoffersen. K., Larsen. P. K.. Osier. M., Weber, J.,Eldon. K., and Lange. A. (1980). Ritodrine in thetreatment of preterm labor: A clinical trial to com-pare a standard treatment with three regimensinvolving the use of ritodrine. British journal ofObstetrics and Gynaecology 87, 949-957.
244 Inhibition qt. Preterm Labor2 :? -7
79. Levin, D. L. (1980). Effects of inhibition ofprostaglandin synthesis on fetal development, oxy-genation, and the fetal circulation. Seminars inPerinatology 4, 35-44.
80. Merkatz, I. R., Peter. J. B., and Barden. T. P. (1980).Ritodrine lwdrochloride: A beutnimetic agent fm usein preterm labor. 11. Evidence of efficacy. Obstetricsand Gynecoky 56, 7-12.
81. Penney, L. L and Daniell, W. C. (1980). Estimationof success in treatment of premature labor:Applicability of prolongation index in a double-blind,controlled, randomiz.ed trial. American Journal ofObstetrics and Gynecokw. 138, 345-346,
82. Sivasamboo. R. (1972). Premature labor. In: K.
Baumgarten and A. Wesselius-De Casparis (Eds.),Procivdings of the International Symposium on theTreatment o.f Fetal Risks, Baden. Austria (pg. 1(-20).Vienna: University of Vienna Medical School.
83. Spellacy, W. N., Cruz, A. C., Birk. S. A., and Buhi, W.C. (1979). Treatment of premature labor with filo-drine: A randomized controlled study. obstetricsand Gynecology 54, 2Z0-223.
84. Barden. T. P. Unpublished data included in thereports of Merkatz et al. (1980) and King et al. (1988).
85. Hobel, C. J. Unpublished data included in the reportsof Merkatz et al. (1980) and King et al. (1988).
86. Mariona, F. G. Unpublished data included in thereports of Merkatz et al. (1980) and King et al. (1988).
87. Scommegna, A., and Bieniarz, . Unpublished dataincluded in the reports of Merkatz et al. (1980) andKing et al. (1988).
88, Leveno, K. Klein, V. R., Guzick, D. S., Young, D. C..Hankins. G. D. V., and Williams, M. L. (1986).Single-centre randomised trial of ritmirine hydrochlo-ride for preterm labor. Lancet 1. 1293-1296.
89. lialmers, I., Hetherington, J., Enkin, M., and Keirse.M. J. N. C. (Forthcoming). Meth(xis used for synthe-sizing evidence. In: NI. W. Enkin, NI. J, N. C. Keirse,and I. Chalmers (Eds.), afective care in prcNnancyand childbirth. Oxford: Oxford University Press.
90. Peto, R Pike, M. C., and Armitage. P. (1976 ).Design and analysis of randomised clinical trialsrequiring prolonged observation for each patient:Introduction and design. British journal (?/. Cancer34, 585-612.
Interivntions
91 Yusuf, S., Peto, R., Lewis, J., Collins, R., and Sleight.P. (1985). 8-bk)ckade during and after myocardialinfection: An overview of the randomized trials.Progress ift Cardiovascular Di.seases 5, 335-371.
92. Brown. S. Nt, and Teiani. N. A. (1981). Terbutalinesulfate in the prevention of* recurrence of prematurelabor. Obstetrics and Gynecology 57, 22-25.
93. Creasy, K. K Go!bus, M. S., Laros, R. K., Parer, J. T.,and Roberts, J. M. (1980). Oral ritodrine mainte-nance in the treatment of preterm labor. AmericanJournal of Obstetrics and Gynecology 137, 212-219.
9.1. Smit. D. A. (1983). Efficacy of orally administeredritodrine after initial intravenous therapy.Unpublished MD thesis, University of Limburg, TheNetherlands.
95. Crimley, P. (Forthcoming). PlInnoting pulmonarymaturity. In: NI. W. Enkin, M. J. N. C. Keirse, and I.Chalmers (Eds.). Effective care in pregnancy andchildbirth. Oxford: Oxford University Press.
96. Liggins, G. C.. and Howie, R. N. (1972). A con-trolled trial of antepartum &corticoid treatment forprevention of the respiratory distress syndrome inpremature infants. Pedknrics 50. 515-525.
97. Caritis, S. N., Carson, D., Greebon, D., McCormick,M., Edelstone. D. L. and Mueller-Heubach, E.(1982). A comparison of terbutaline and ethanol inthe treatment of preterm labor. American Journal ofObstetrics and Gynecology 142, 183-190.
98. Finley, J Katz, NI., Roias-Perez. NI.. Roberts. J. NI.,Creasy, R. K.. and Schiller, N. B. (1984).Cardiovascular consequences of placebo controlledagonist tocolysis: An echocardiographic study.Obstetrics cind Gynecology 64, 787-791.
99. Lauersen, N. IL, Merkatz. R.. Tejani, N., Wilson, K.II_ Roberson, A., Mann, L. I., and Fuchs. F. (1977).Inhibition of premature labor: A multicenter com-parison of rit()drine and ethanol. .4mericanjournalof Obstetrics and Gynecolopi, 127, 837-845.
100.Reynolds, J. W. (1978). A comparison of salbutamoland ethanol in the treatment of premature labor.Australian and New Zealand Journal of Obstetricsand Gynaecology 18, 107-109.
101.Sims, C. D.. Chamberlain, G. V. P., Boyd. I. E., andLewis. P. J. (1978). A comparison of salbutamol andethanol in the treatment of preterm labor. BritishJournal of Olytetrics ami G:ynaecc 'logy 85, 761-766.
Marc Kora, 245
22S
Advances in the Prevention of Low Birthweight
102.Spearing, G. (1979), Akohol, indomethacin andsalbutamol: A comparative trial of their use inpretetm ObsMrics and Gyrwcology
103,Beall. M. IL. E-ar. B. W.. Paul. R. IL. and Smith-Wallace, T. (1985). A comparison of ritodrine. terbu-taline. and magnesium sulfate for the suppression Ofpreterm labor. Anwikan journal cf Obstetrics andGynecology 153, 85,t-859,
104.Caritis, S. N.. Toig. G., lieddinger. L. A., andAshmead, G. (1984). A double-blind study compar-ing ritodrine and terbutaline in the treatment ofpreterm labor, American journal (,/' Obsretrks andG3.neco1ogy 150, 7-1.1.
105.Essed, G. G. M.. Eskes. T. K. A. B.. and ,fongsma. 11.W. (1978). A randomized trial of two beta-mimeticdrugs for the treatment of threatening early labor:Clinical results in a prospective comparative studywith ritodrine and fenoterol. Fungrean journal ofObstetrics, Gynecofirgy. and Reproductivt, Biology 8,341-348.
106.Gummerus, M. (1983). Tocolysis with hexoprenalinand salbutamol in clinical comparison. Geburtsbilfi,und Frauenheilkunde 43. 151-155.
107,Karlsson. K.. Krantz_ M.. and Ilamberger. L (1980).Comparison of various betamimetics on preterni Liborsurvival and development of the child. journal (y.Perbtatal Medicine 8. 19-26.
108.Kosasa. T. S.. Nakayama. R. T.. liale. R. W.. Rinzler. G.5,. and Ereitas. C. A. (1985). Ritodrine and terbu-!aline eimipared for the treatment of preterm labor.Ada Ohstetricia el Gynecohwica Scandinarica 04.421-426.
109.Ryden. G. (1977). The effect of salbutamol andterbutaline in the management of premature lalx)r.Acta ohNtetrieia et Gynecologic(' Seandirtatiea293-296.
110.Bender. If. G.. Goeckenian. Meger. C.. andNIUntefering. IL (197). Zuni mutterlichen Risiko dermedikamentOsen Thkolvse mit Fenoterol (Partusisten).GeburtshilW und Fraeuribeilku rule 37. 065-674.
111.jonatha, Goessens. 1... Traub. E.. and Dick. W.(197'). Eulmonale Komplikaticmen wahrend derTokolyse. In: IL Jung and E. Friedrich (Eds.).Fenoterol (Partusisten ) bei (ler Bebandlung in derGeburtsbilie unit Peril/Wu/ogle (pp. 6S- I (8 ).Stuttgart: Georg Thieme,
112.Kubli, F. (1977), Discussion. In: A. Anderson, R.Beard. J. M. Brudenell, and P. M. Dunn (Eds.). Pre-term labor Proceedings qf the Ili% Study Group efthe RQvat oitlege of Obstetricians and Gmaeccdogists(pp. 218-220). London: Royal College ofObstetricians and Gynaecologists.
113.Abr.untwici, It. Lewin. A., Lissak. A.. and Palant,(1980). Nlaternal pulmonary edema occuring aftertherapy with ritodrine for premature uterine contrac-tions. A eta Obstet ricia et Gyilecologicascandinaviea 59, 555
114,Babenerd. J.. and Flehr. I. (1979). MOtterlicheZwischentalle umer (ier Tokolyse mit Fonoterol.Medizinische Uclt 30. 537-5-II.
115.Barden. T. P. Peter, J. B., and Nkrkatz. I. R. (1980).Ritodrine hydrochloride: A betamimetic agent foruse in preterm labor. I. Pharmact logy. clinical his-tory, admiffistration, side effects, and safety.Obstetrics and Gynecology 56, 1-6.
I1O.Daubert. J. C., Gosse. P.. Rio, NI.. Gran. J. Y..Bourdonnec. C., Pony. J. C.. and (iouffault.(1978). Myocardiopathies en cours de grossesse:Role possible des bOtamimetiques. Archives desMaladies du Coeur et des litiwaux 71. 1283-1290.
117.Elliott. It R., bdulla. L. jj,f iLlyeti, J. (1978).Pulmonary oedema asstrciated with riux.frine infusionand betamethasone administration in prematureIalmr. British Medkal journal 2.-99-800,
118.1 acobs. NI. N1.. Knight. A. 13., and Arias. F. (1980).Materna! pulmcmary edema ITS LI III ii g fromlvtamimetic and glucocorticoid therapy, Obstetricsand Gynecology 5(,. 56-59.
I19.Milliez. J.. Blot. P.. and Sureau. C. (1980). A casereport of maternal death associated with betamimet-ics mid betamethasone administration in prematurelaben. Film/wan Journal of Obstetrics. Gyilecol(gy.and Reproductive 1üolo,e0'11, 95-104).
120.Neihuhr-Jorgensen, 1'. (1980). Pulmonary oedemafolkiwing treatment with rit(kIrinc and betametha-sone in premature labor. Danish Medical Bulletin2'. 99-100,
121.Rogge, :' Yming. S.. and Goodlin. R. (1979).Post-partum pulmonary oedema ass(sciated with pre-ventive therapy for premature labor. lancet 1.102-1027.
246 2 ') InhiNtion of Preterit, Ittbor
122.Tinga. 1). J.. and Aarnoudse. J. G. (1979). Post-par-
tutn pulmonary (iedema ass(wiated with preventivetherapy for premature labor, lancet 1. 1026.
123.Wolff. F.,Mc ier, U., and Hoke. A. (1979).Untersuchungen zum Pathoinechanismus schwererkardicipulmonaler Komplikationen tinter tokolytisch-er Behandlung mit 1A-adrenergen Substanzen undBetanwthason. Zeitschrill ftir Geburtisbilfe rindPerinatologie 183. 343-347.
124.Grospietsch. G.. Fenske. M., Dionch, B., and Ensink.E. B. M (1982). Effect of the tocolytic agentfenoterol on body weight. urine exeretkin. bloodhematocrit. hemoglobin. serum pr()tein. and ek.c-trolyte levels in non-pregnant rabbits. Americanjournal cy'Obstetrics and Gynecolt v. 143. (th7-672.
I25.Caritis. S. N.. Edelstone, D. 1., and Mueller-lIeubach.E, (1979). Pharmacologic inhibition of pretermlabor, American journal of Obstetrics andGynecology 133, 557-578,
126.Katz. M., Robertson, P. A.. and Creasy. R. K. (1981).Cardiovascular complications associated with terbu-taline treatment for preterm labor. Americanlout-rad of011stetrics and 6)necology 139, 605-608,
127.Robenson, P. A., Herron. M.. Katz, M.. and Creasy. R.K. (1981). Maternal morbidity associated with isox-suprine and terinitaline tocolysis. Eumpean journalqi obstetric:, Gynecology, and Reproductin, Biologr11, 371-378.
128.Benedetti. T. .1. 0983). Maternal complications ofparenteral 14-sympathomimetic therapy for premature.labor. American Journal of Obstetrics andGynecology
129.1)hainaut. I.. Boutonnet. G., Weber. S.. andDegeorges. M. (1978). ResponsabiW des lu-Aa-2-minu'liques Cliins la genese chine cardiomyopathiedu postpartum Nouvelle Nesse .1tedicale-, 058.
130.Hendrklis. S. K.. Keroes. .1., and Katz, M. (1986).Electrocardiographic changes associated with rito-drine-induced maternal tachycardia andhypfikalemia. American Journal (,1* obstetrics andGynecoltigy 1 921-923,
131.Kubli. F. (1980). Commentary on maternal morbidi-ty due to beta-adrenergic therapy. Eu ropea njournal of obstetnCs. Gmecology. and ReproductitvIiiologv lii. 1.4-4-i.
interventions
132.Michalak. D., Klein. V., and Marquette, G. P.(1983), Myocardial ischemia: A comphcation ofritodrine tocolysis. American journal (f Obstetrksand Ciptecolgy 146, 861-862.
133.Ries. G. H. ( 1979). Kasuistische Mitteilungither dasAuftrcten einer Myokardischilmie unter medikamen-loser Tokolyse mit Ritodrin (Pre-Par). Geburtthilfeand Entuenbeilkande 39, 33--37.
134.Ving, V. K., and Tejani. N. A. (1982). Angina pec-toris as a complication of ritodrine hydrochloridetherapy in premature. labor. Obstetrics and(l)wecologv 60,385-388.
135.Rona, G., Chappel, C. I., Balazs, T and (haudry. R.(1959), An infarct-like myocardial lesion and othertoxic manifestations produced by is(iproterenol inthc r;at. rchii les ofPat/Nikki. 67. 443-455.
136.Bieniarz. J.. Ivankovich. A., and Scommegna. A.t 19-74). Cardiac output during rimdrine treatment inpremature labor. Amerkan journal of Obstetricsaiitl Gyttecology 118. 910-919.
137.1)e Swiet, M. (1980). The cardiovascular system.In: F. E. Hytten and ( . Chamberlain (Eds.),Clinical physi(//ogy in pregnancy (PP. 3-42).Oxliird: Blackwell Scientific Publications.
138.Eerguson, 3. E.. Hensleigh. P. A.. and Kredenster,I). (1984), Adjunctive use of magnesium sulfatewith ritodrine for preterm labor tocolysis.American Journal of Obstetrics and Gynecology148, 166-171.
139.1.enz. S Detk.fsen. G.. Rygaard. C.. and Veicrslev. L.(1985). Isotonic dextrose and isotonic saline. as sol-vents for intravenous treatment of premature laborwith ritodrine, journal of Obstetrics andG:ynaecology 5,151-154.
140.Philipsen. T., Eriksen, P. S.. and Lynggard. F.(19811. Pulmonary edema following ritc)drinc..-salineinfusion in premature labor. Obstetrics and0:31teculo,L1. 58. 30-4-308.
14I,Keirse, M, I. N. C., Noon. W.. and Erwich..1. J. H. NI.(1987). The role. of prost agl a nd i n s andprcistaglandin synthesis in the pregnant uterus. In:
M. J. N. C. Keirse and II. J. de Koning Gans (Eds.),Printing and induction (!f* labor hy pr()staglandins:A state. of the art (pp. 1-25). Leiden. TheXe'! he'rla nds jc ,c'rl, aa e Comm it t ee forPostacademic Nk.dical Education.
,Ilarc Kelm,23
247f.)
Advances in the Prevention of Low Birthweight
142.Keirse. M. J. N. C. (1981). Potential hazards ofprostaglandin synthetase inhibitors for management ofpre-term labor. Journal (y. Drug Research 6. 915-919,
WAVicivist. N. (19797. The use of inhibitors ofprostaglandin synthesis in ohstetrics. in: M. J. N. C.Keirse. A. B. M. Anderson. and .1. BennebroekGravenhorst (Eds.). Human parturithm (pp. 189-200).The Ilague: Leiden Iniversity Press,
1+LSchwartz. A.. Brook, L. Inskr. V., Kohen. E., /or. U.,and Lindner. IL R. (1978). Effect of tlufenamic acidon uterine contractions and plasma kvels of 15-keto-13.14-dihydro-prostaglandin F2a in preterm labor.Gyneco/ogic and obgetric buestimuicin 9, 139-1 +9,
145.Dornhöfer. W.. and Nlosler. K. If. 19-57.Prosuglandine und 1;-Stimulatoren. In: 11. ung and E.K. Kliick (Eds.), Th Partusistett 1 bet derBehandlung in der Gehurtshilfe und Perinatologie (pp.194-202/. Stuttgart: Georg Thienw.
1.+0.GyOry, G., Kiss. C.. Benyo. T. BAgdany. S., Szalay, J.,Kurcz. Nt. and Virag. S. (1974). Inhibition of Ialuir byprostaglandin antagonist in impending alxirtion andpreterm and term lalxir. Lancet 2, 293,
1.17.Witter. E. R.. and Niebyl. J. R. (198(0. Inhibition ofarachidonic acid metabolism in the perinatal perit)d;Pharmacology. clinical application. and potentialadverse effects. SeMillilIN rClilltlioi(.k). 10. 310-333.
1-18.M(xmen. P.. Klok. G.. and Keirse, NI. ,1. N. C. (1984).Increase in c()ncentrations of prosuglandin endoper-Oxide synthase and prcistacyclin synthase in humannlymnetrium in late pregnancy. P).ostag/(Indins 28.309-322.
149.Nlitchell. M. 1), (1(...*407, )'athways of arachidonic acidmetab()Iism with spedfic application to the fetus andmother. Seminars in Perinatologr 10. 2.12-2-1.i.
150.11alle. II.. Ilengst. P. (198I. ZusatztoWysc Lim-6Prostaglandinsvthetasehemmung Indoinctacin.Zeitschrif Gelnirlshile rind Perinatologu, 182.307-370.
151.Van Kets. I I.. Thiery. NI.. Deront. R.. Van Egmond.and Back.. G. (1979). Perinatal hazards of chronicantchAd tocolYsis with ind(mlethain. Ph,staglandins18. 893-90'.
15.2.Niebyl. J. R.. Blake. 1). ,A.. White. R. D,. Kumor. K.NI., Dubin. N. IL. Robinson, .1. C.. and Egner, P. G.119801. The inhibition of premature labor withindomethacin. Arnerican Journal of ohstetrks andGyneoclow 136, 1014-1019,
153.Zuckennan. IL. Shaky. E.. Clilad, G., and Katzuni. E.(1984). Further study of the inhibition of premature1:111(ir lw indomethacin. Part II. Double-blind study.journal ql Perinatal Medicine 12, 25-29.
15.I.Gamissans. 0.. ani Balasch, J. (198,1).Prostaglandin synthetase inhibitors in the treatmentof preterm lab(ir. In: F. Fuchs and P. G. Stubblefield(Eds.). Preterit) birth: Causes, preivition and man-agonent (pp. 223-248). New York: Macmillan.
155.Katz. Z,. 1.ancet. NI.. Yemini. NI., Mogilner. B. NI..
Feigl. A.. and Ikn-Hur. H. (1983). Treatment of pre-mature labor contractions with combined ritodrineand indomethacine. /n/ernational jou nut/ uf(iputecology and ()Work's 21. 337-3.42,
156,1ilake, D. A., Nielwl. 3. R., White, R. D., Rumor. K.NI,. Dubin. N. If,. Robinson, J. C.. and Egner, E. G.(19801. Treatment of premature labor withindomethacin. Advances in Prostaglandin andThroniboxane Research 8, 1.466-1,467.
157.Gainissans, Canas. E., Cararach. V. Ribas,Puerto. B.. and Edo. A. (1978). A study ofind(miethacin combined with ritoklrine in threatenedpreterm labor. Eurolwan Journal of Obstetrics,o:inecolow. and Reproiluctne Biology S. 123-128.
1.58,Gamiss.ns 0.. Cararach. V.. and Serra. J. (1982).The role of prostaglandin-inhibitors. beta-adrenergicdrugs and glucoeorticciids in the management ofthreatened preterm labor. In: It Jung and G,Limberti (Eds.). Betamimetic drugs in obstetrics andperina1 Hhigri3p."1-8.47. Stuttgart: (;org
159.Alvan. C.. Orme. NI., Bertillson. I_ strand, R. E. K.,
and Pa Ini&r, L. (19-5). Pharmacokinetics ofindomethacin. Clinical Pharmacology andTherapeutics IS, 0i-373,
ImAVallusch. NV. NV.. Novak, II.. Leopold, G.. and Netter.K.41. ( 19-8t. Comparative bitiavaiLtbility: Influence()i various diets ( )11 the hioavailability ofindomethacin. hiternatumn/ journal of Clinical
rmact dog v arid lihpilarrnacy 10. ,(
101.Traeger. NOschel, IL. and ZatimseiLl. (19-3),/Air Pharmakokinctik vc)n Indomethazin icrhte.1.1i
h Kreissenden undScwangeren.Neugeborenen. Zentralblatt far Gyna4.,ologie 95.035-0-11.
IO2AVilkinson. A. K. 1980). Naproxen levels in preterminfants atter materna! treltment. Lancet 2, 591-59
248 Inhibition ofPretertn Labor231
163.6ersony. W. M,, Peckham, G. J., Ellison. R. C..Miettinen. 0. S., and Nadas, A. S. (1983). Effects ofindomethacin in premature infants with patent ductusarteriosus: Results of a national wilaborative study.Journal of Pedia(ric.. 102, 895-905.
Mahony. L.. Carnero, V.. Brett, C., Heymann, M. A.,and Clyman. It I. 0982), Prophylactic indomethacintherapy for patent ductus arteriosus in very-low-birth-weight infants. Neu. England Journal (1*.tredicine 300,506-510.
16i.Arcilla. It A.. Thilenius, 0. G., and Ranniger. K.(1969), Congestive hean failure from suspected ductalclosure in uter(). _Journal (y* Pi,diatrics
166.Wiqvist. N. (1981). Preterm labor: Other drug possi-bilities including drugs not to use. In: M. G. Eklerand C. II. Hendricks (Eds.). Preterrn labor (pp.148-175). London: Butterworths.
167.11etkerur. M. V., Yeh, T. E., Miller. K., (ilasser. It J., andPikles, It S. (1981). Indomethacin and its effect onrenal function and urinary kallikrein excretion in pre-mature infants with patent ductus arteriosus.Mhatrics 68, 99-102.
168.Gleason. C. A. (1987). Prostaglandins and the devel-oping kidney. Seininarc in Perinatologv 11. 12-21.
169.11eymann. M. A., Rudolph, A. M.. and Silverman. N. II.(19761. Closure of the ductus arterk)sus in prematureinfants by inhibition of prosuglandin synthesis. NewEngland ,l(nrrnal (..?1:11tylicipte 29c. 53(}-533.
170.Cantor. B.. Tyler. T., Nelson, R. NI.. and Stein. (3. H.( 1980), Oligohydramnios and transient neimatalanuria: A pcis,sible association with the maternal useof prostaglandin synthetase inhibitors. ournalReproductive Medicine 2i. 2211-223,
171.Itskovnz, f. Abram(>vice. II and Brandes. I. I.
11980), Oligohydramnion. meconiom and perinatalcleath concurrent with indomethacin treatment inhuman pregnancy. Journal Qt. Reproductite Medicine2 I. 1$7-1.10.
172Neerseina. D.. de .Iong, P. A.. and Van \\lick. ,1 .(1983). inchimethacin and the fetal renal nonfunetionsyndrome. European Jou nut/ ff Obstetrics.Grneothigr, and RepnidUCti1,0 Bio/ogy 1(. 113-121.
173.1)e Wit. W,. Van Mourik. 1.. and Wiesenhaan. l (1988).
Prokinged maternal indomethacin therapy associatedvith oligohydramnios: Case reports. British journal .1.1
Obstetrics and Gynaec o/ogy 95.303-305.
Interventions
174.Eriedman, Z., Whitman. V,. Maisels, M. J.. Berman,W., Jr., Marks, K. H., and Vesell, E. S. (1978).Indomethaein disposition and indomethacin-inducedplatelet dysfunction in premature infants. Journal (y.
Pinomacology 18, 272-279.
175.Abnunson, D., and Reid. D. E. (1955). Ilse of relax-in in treatment of threatened premature labor.journal qf Endocrinolcw, and Meutbolism15. 206-209.
176.Chng, P. K. (1981). An analysis of preterm singletondeliveries and assoeiated perinatal deaths in a totalpopukttion. British Journal q' Obstetrics andGynaecohlgy 88. 814-818.
r7.1)avies, A. E.. and Robertson. NI. J. S. ( 1980).Pultmmary oedema after the administratkm of intra-venous saihutamol and erpnnetrine: Case report.Britisb puma! (y. Obstetrics and Gynaecokkgy 87.539-541.
178.Erny, R., Pigne. A.. Prouvost. C., Ciamerre. NI., Malet,C,. Serment. H., and Murat, J. 11986). The elkcts oforal administration of progesterone for prematurelabor. .4 merican Journal of Obstetrics andGynecology 154,525-529,
179.Fuchs. F. (1976). Prevention of prematurity.American Journal qf Obstetrics an(1 6:rnecolcv 126,
809-4420.
180.Fuchs. F., l'uchsA-R.. Poblete. V. C., and Risk. A.11967). Effect of alc.thol on threatened prematurelabor. American Journal of Obstetrics and
viwco/ogr
181.Keirse. NI. J. N. C. (197) ). Endogermus...aglandins in human parturition. In: NI. J. N. C.
Keirse (Ed.). Human parturition: New concepts anddevelopments (pp. 10 I -1421. Leiden. TheNetherlands: Leiden t *niversity Press.
182,Morrison, I. C.. Martin. J. N.. MarVin. H. W..Gookin. K. S.. and Wiser, W. L. ( 1987).Prevention of preterm birth by ambulatory assess-ment of uterine activity: A randomized study.American journal qf Obstetrics and Gynecology156. 536-5-0.
183.Stubbs. T. NI.. Van Dorsten. J. P.. and Miller. NI. C.t 19861. The preterin cervix and preterm labor:Relative risks, predictive values, and change overtime. American jt,turnal (4. obstetrics andGvnecolozrlii, 829-834.
Marc Keirse 2494,
Advances in the Prevention of Low Birthweight
184.Tamby Raja, It L., Anderson. A. B. M., and Turnbull,A. C. (1974). Endocrine changes in prematurelabor. Brita Medical Journal 4, 67-71.
185.Tsuie, 3. J., Lai, Y. E, and Sharma, S. D. (1977). Theinfluence of acupun.lure stimulation during preg-nancy. Obswtrics and G:rnecologr 50.479-488.
186.Tumer. G.. and Collins, E. (197-if. Fetal effects ofregular salicylate ingestion in pregnancy. lancet 2,338-339.
187.Zuckerman, II., Reiss. II.. and Rubinstein. I. (1974).Inhibition of human premature labor byindomethacin. Obstetrics and Gynecoloky 44.787-792.
250 23 ' (y. Preterm Labor
Interventions
Statistical Findings:Inhibition of Preterm Labor:
Is It Worthwhile?
Table 19.1
Summary of Approaches Used to Inhibit Preterm Labor in the Past 35 Years and Their Purported
Success Rates in the First English Language Publication Documenting Their Use
Number ofAgent Year Authors women
Relaxin 1955 Abramson and Reid 121 5
lsoxsuprine 1961 Bishop and Woutersz 1231 120
Ethanol 1967 Fuchs et al, 1621 52
Orciprenaline 1970 Baillie et al. 113) 30
Mesuprine 1971 Barden 1141 17
Ritodrine 1971 Wesselius-DeCasparis vial. 117 43
Fenoterol 1972 Edelstein and Baillic 150) 28
Salbutamol 1973 Liggins and Vaughan 11131 88
lndomethacin 1974 Zuckerman et al. 1186) 50
Sodium Folicylate 1974 Gyory et al. 1721 50
Buphenine 1975 Castrtin et al.1.331 41
Terbutaline 1976 Ingemarsson 1801 15
Nifedipine 1977 Andersson 1101 10
Magnesium sulphate 1977 Steer and Petrie 115.31 31
Acupuncture 1977 1suie et al. 11631 12
Elufenamic acid 1978 Schwartz et al. 11451 18
Diazoxide 1984 Adamsons and Wallach 141 118
Oral progesterone 1986 Erny et al. 1521 57
Oxytocin analogue 1987 Akerlund et al. 161 13
Criterion ofsuccess
delivery after 36 weeks
contractions delayed 24 hours
delivery delayed 72 hours
delivery after 36 weeks
delivery delayed 24 hours
not delivered during treatment
ddivery delayed 1 week
delivery delayed 24 hours
arrest of contractions
diminished uterine activity
birthweight 2,500 g
not delivered during treatment
delivery delayed 3 days or more
contractions stopped 24 hours
delivery after 36 weeks
delivery delayed 24 hours
complete Cessation of contractions
decrease in contraction freciuency
inhibition of contractions
PercentStICCeSS
100
82
67
70
53
80
71
81
80
100
86
80
100
77
92
83
94
76
100
Table 19.2
Characteristics of Birth and In-Hospital Mortality and Morbidity in Infants Born Alive Before 32Weeks (224 Days) of Gestation in the Netherlands in 1983*
Characteristics Number Pertentage
(iwracferistics of birth
Characteristks Number Percentage
Charat teristits and morbidity (confirmed diagnoses only) ot newborn
After pwlabor rupture of membranes 453 44.8 Congenital malformations 96 9.5
More than 24 h atter rupture of membranes 226 22,4 Weight below 10th tentile for gestation 171 16.9
After use of tocolytic drugs (any timet 533 52.8 Respiratory distress syndrome 417 41.2
After corticosteroid administration 173 17.1 Intracranial hemorrhage 251 24.8
Part of a multiple pregnancy 261 26.0 Convulsions 66 6.5
Wee( h presentation 293 29.0 Septicaemia 113 13.2
Elective del iveryt 155 15..3
Cesarean section 321 .31.8tn-hospaal mortality of lweborn infants
Neonatal deaths (28 days) 285 28.2
Data from Verloove-Vanhorick and Venvey 148711701.
t Defined as anv delivery following arty obstetrical intervention aimedat !ringing pregnantly to an end before the onset ot spontaneouslabor andor spontaneous rupture of the membranes.
In-hospital deaths
Total
110
1,010
30.7
100.0
Marc Keince 23 4
Advances in the Prevention of Low Birthweight
Agents Reported
Prostaglandin synthesisinhibitors
Betamimetic agents
Table 19.3to be Used for the inhibition of Preterm Labor in the Literature Since 1980
Oxytocin analogues(receptor
blocking agents)
DiazoxideAntimicrobial agents
Ethanol
Calcium antagonistsMagnesium sulfateOral progesterone
Table 19.4Characteristizs of the Trials Compar:ng Betamimetics With Ethanol for Inhibition of Preterm Labor
Authors (date)
Caritis et al. (1982)
Spearing (1979)
Reynolds (1978)
Sims et al. (1978)
Lauersen et al. (1977)
Fuchs (1976)
Betamimetictreatment
Terbutalineiv oralmaintenancefor 5 days ifmembranes intact
Salbutamol iv-4. oral for 48 hoursafter contractions
Salbutamol iv+ 200 mg sodiumphenobarbitone
Salbutamol ivno maintenance
Ritodrine iv -0. oralmaintenance for4 weeks oruntil term
Method ofallocation
random bysealed
No. randomized:reported on
Allocated to Allocatedbetamimetic to ethanol
92:85\
envelopes ?:45 ?:40
alternate 22:20 22:22
alternate 42:42 42:42
random by 100:88open list / \
randomby sealedenvelopes
?:42 ?:46
150:135/ \
?:68 ?:o7
Other ddails
corticosteroids weregenerally given;magnesium sulphategiven if assignedtreatment failed;ruptured and intactmembranes reportedseparately.
salbutamol was givenif ethanol failedand vice versa
all ethanol treatedwomen received500 mg methylprednisolone iv
all women random-ized to betametha-sone vs. placebo;5 women ethanolbetamimetic; 2 beta-mimetic -4. ethanol
all women are alsoincluded in thereport oft auersenet al. (1977)
252 Statistical Findings: inhibition of Preterm Labor
235
Inteiventions
Figure 19.1Effect of Betamimetic Drug Treatment in Preterm Labor on the Incidence of
Delivery Within 24 Hours in the 14 Trials Which Provided Data on This Outcome*
Christensen 1980
Spellacy 1979
Barden
Hobe(
Cotton 1984
Howard 1982
Ingemarsson 1976
Larsen 1986
Calder 1985
Scommegna
Mar lona
Wessel lus 1971
Leveno 1986
Larsen 1980 4
1 4 4 1 4 1 1
Odds Ratio
0.01 0.03 0.1 0.3
1 4 1
1
4
1
4 10
1
1
41
See text for explanation on how to interpret thi.; and subsegtwnt figures.
Figure 19.2Effects of Betamimetic Drug Treatment in Preterm Labor: 'Typical' Odds Ratios, With Their 95
Percent Confidence Intervals, Across Trials for the Various Outcomes Studied
Odds Ratio
0.2 0.4 0.6 0.8 1 1.5 2
--1--- 1 1 I 4-
Delivery < 24 hours
Delivery < 48 hours 4Preterm birth
Low birthweight
Respiratory disease
Perinatal death
4 4 1 1 1 4
Marc Keirce 253
Advances in the Prevention of Low Birthavight
Figure 19.3Effect of Betamimetic Drug Treatment in Preterm Labor on the Incidence of Severe Respiratory
Disorders Including Respiratory Distress Syndrome
Odds Ratio
0.01 0.03 0.1 0.3 1 4 10
1
Christensen 1980
Spellacy 1979
Barden
Hobel
Cotton 1984 4
Howard 1982
Ingemarsson 1976
Larsen 1986
Calder 1985
Scommegna
Leveno 1986
Larsen 1980
1 1 1 1 1 1
Figure 19.4Effect of Betamimetic Drug Treatment in Preterm Labor on the Incidence of Perinatal Mortality Not
Attributable to Lethal Congenital Malformations
Odds Ratio
0.01 0.03 0.1 0.3 1 4 10
4 4- 4 4Christensen 1980 I
Spellacy 1979
Barden
Hobe! 1
Cotton 1984
Howard 1982
Ingernarsson 1976
Larsen 1986
Calder 1985
Scommegna
Marlona .-
Wessellus 1971 1 .-
Leveno 1986
Larsen 1980 4-Adam 1986 4
4.
-4
4--
254 Statistical Findings: Inhibition qf Preterm Labor Is it Worthwhile?1
.3
liztoventions
Figure 19.5Comparison Between Betamimetic Drugs and Ethanol for Treatment of Preterm Labor:
Effects on the Incidence of Delivery Within 48 to 72 Hours After Entry into the Trial
Odds Ratio
0.1 0.2 0.4 0.6 0.8 1 1.5 2
I I 4 1 1 I
Caritas et al. 1982
Spearing 1979
Sims et al. 1978
Lauersen et al. 1977
Typical Odds Ratio 1
1 4 1 I 4-4--
Figure 19.6Effects of Indornethacin in Preterm Labor: 'Typical' Odds Ratios, With Their 95 Percent Confidence
Intervals, Across Trials for the Various Outcomes Studied
Odds Ratio
0.1 0.2 0.4 0.6 0.8 1 1.5 2
4 I 4- -4- 1
Delivery < 48 hours -4-Delivery < 7-10 days 4-
Preterm birth 4-
Low birthweight
Respiratory distress 4-Perinatal death -4-
1 -4-
Mary Keim, 25523 S
Sunday, May 8,1988
6:00 p.m. REGISTItkTION
Monday, Mgy 9,1988
7:30 a.m. BREAKFAST
8:30-8:45 a.m.
8:45-10:00 a.m.
8:45 a.m.
9:05 a.m.
9:25 a.m.
10:00 a.m.
10:30 a.m.--1230p m.
10:30 a.m.
Appendices
Appendix 1".. Symposium Program
,SE;SION I: INTRODIVIIONS
Presiders: Heinz Berendes: Woodie Kessel; Sumner Yaffe
Rapporteur Phyllis Zucker
WELCat Ir
Duane Alexander, National Institute of Child Heahh and Human Development
Vince Hutchins, Bureau of Maternal and Child Health and Resources Development
SEsSION II: TRENDS
13rian McCarthy: David Rush
Rapporteli?.: Howard I-loffman
TREV/T)s LV ktThs op LowBuMi WEIGIRN IN MP 17N177:71 SEIZES
Speaker: Marie McCormick, Boston, Massachusetts
7kEvps PREIERE DEMERY .'iND Low Brnin WEIG FRAAIX
.Speaker Gerard Brea rt. Paris, France
Disci ;s:C/0,V
Ni7RT770N AAP FITNEsIs BREIK
SESsIoN DETERNI1NANIN
Presiderc: Ann Koontz: Charlotte CatzRapporteur Karla Damus
EPIDEVIOIDGICAL DE771411LVINIS or AMit "HMV GROW A.V) GES11170.\A/
Dt i4ThX, 0 RRENTSEARS .4.7) GUN LV al? KNOW .LEI K :rE
Spmker: Michael Kramer, Montreal. Canada
24 0
Advances in the Prevention of Low Birthweight
10:50 a.m.
11:10 a,m.
BIOLOGICAL DE7P:RMINANIS OF R774.11.17ildNE GROWTH 21417) GmAnawDminoN, Ct1RRENT STA7IN AAD GUN iv OIIR KNOWIRXiESpeaker: Miles Novy, Portland, Oregon
BEIL4170RAL DE7ERMIAAN7S OF A7k417ER/AE GROW 771 itm) GEszvioNALDtRAnas CURRINT STAIT5' AND aiRS' LV OIR Kvotvwxd:'Speaker:Jeanne Brooks-Gunn, Princeton, New Jersey
11:30 a.m. Disamtav
12:30-3:30 p.m. LUNCH
2:00-3:30 p.m. SEsSION IV: INTERVENTIONS
Presidem Henry Foster; Jose Belizan; Gian Di RenzoRapporteurs: Patricia Shiono; Donald MeNellis
2;00 p.m. ME M4RC7 1 OF DBMS PR1:7ERII BIRM CLINICAL na,11,Spaiker: Robert Creasy, Houston, Texas
2:30 p.m. Rh:VI:IS OF A MREE-YhAR P1?OSIV:17VE CUV1ROLLED KINDOMIZ.ED DUAL ON
PRE17:181 BIIM1 IIREVEMON AT 771E B71ERCITY OF PTI7SIII:R671
Speaker: Eberhard Mueller-Heubach, Pittsburgh, Pennsylvania3:00 p.m. DiSt.EssioN
3:30 p.m. NUIRrnON AND RINESS BREAK
4:00-5:30 p.m. SESSION V: INTERVENTIONS
Presiders: Marshall Klaus; Steven NgRapponeur Margaret Freda
4:00 p.m.
4:30 p.m.
5:00 p.m.
5:30 p.m.
DEaLV AND RISE OF PREIERM &KW MIES FRO31 /1 1 5 DAR .517 111
,Speaker Emile Papiernik, Paris, France
D'alIE ON 771E WEST LOS ANCIELES PRE11117 RE PREIEVIRAV PRQIECTSpeaker Cal Ilobel, Los Angeles. California
DISCI WON
AI )JOI 'RN
2602 4 I Alpendix
7:00 p.m.
Appendices
DINNER
SEIIPOVIIM P4R77CIIMNIN AM) US. PUBLICHEAL77I SERIICE EVERT PANEL ON 77IE
COVENT OF PRENA7A1. C4RE
hroSt: Ruby Heam, Robert Wood Johnson Foundaticm
Tuesday, Mqy 10,1988
7:30 a.m. BREAKFAST
8:30-10;00 a.m. SESSION VI: INTERVENTIONS
Presiders: Sara Depersio; Michael Ross; Dyanne Affanso
Rappodeur:Jean Konte
8;30 a.m. PIE Sat M C4ROLIN4 RANIXWIZED OINICAL TRIAL USING NURSE MIDIVIM 7t)
REIN 7CE Low' &MI Wiic;irisVeaker Henry Heins, Charleston, South Carolina
9:00 a.m. REst EIS FROM A R&M AAL PR(X,RAM BASED ON RISK ASSESMIENT RF.111tE ruE
kim oF PRE7ERM DWIERYVeaker Paul Meis, Winstcm-Salem, North Carolina
9:30 a.m. Asa xsioN
10:00 a.m. NimmoN AND FrrNEss BREAK
10:30 a.m.12:30 p.m.
10:30 a.m.
SINSION VII: I N1ERVENTIONS
Presiders: John Kennel; David Olds; Diedre 13I:mk
Rapporteur: Ruth Merkatz
DIE FAMILY WORKERS PROIELT FINAL EIALI ;AMA OF A kiNDOMED CoNIROLLED
DeLAL OF 77 IE PRol1sION OF A SOC;IAL Si PA NTSERI ICE DI VAG PREaVAA0
Veaker Brenda Spencer. Manchester, United Kingdom
11:00 a.m. SK.nl. SI l'PORT Di "RING PREGNANo`
Veaker Lynda Rajan, London, United Kingdom
Symp. Wrim Prognun 2 4 ')26/
Advances in the Prevention of Low Hirtbuteight
11:30 a.m. PRET EV770N OFIIRE7Eat Danl.:MKS' BF HOME V1S177AG Alownks: Rains OF AFKENtli R1NDOMIZFD Coymormnspeaker: Beatrice Blondel, Paris, France
12:00 noon DtsciMION
12:30-2:00 p.m. Lxcii
2:00-3:30 p.m. SESSION VIII: INTERVENTIONS
Presiders: Steven Caritis: Leslie Cooper; Lynda RajanRapportenr: Richard David
2:00 p.m. LV7717dEvnavs. RAG PREUVAM1'
Speaker Mary Sexton, Baltintore, Maryland
2:30 p.m. REct ns OF.-1 MIlnamER RIVM/MIR) CLINIC-1L ML-11. OF 01117C.11. CER0AGE
,Speaker Adrian Grant, Oxford, United kingdom
3:00 p.m. DISCI wax
3:30 p.m. NITRMON AND FUNESS BREAK
4:00-5:30 Rm. SESSION IX: INTERVENTIONS
Presiders: I)enise Main; Robert Romero; Milton LeeRapporteltrc: Ann 1-1(),ckett: Nancy Nance
8:30 a.m. (NE OF ANIIPLVELET DI/RUT MR 7711: PRI:ITN/70N CE,IVM`CEI) PRIM:RM
DEL117111ES iw PRE1EVI7ON OF PREFC.7.'IMINIA
Veaker Serge t zan, Paris, France
4:20 p.m. CALCIllt S( P1'LEMLN7A170N 7t) REIN a PIH AND PN77:11.11 DELI1TRY
Speaker: j()se Villar, Bethesda, Nlaryland
4:40 p.m. 1,1,161vEsit 31 S IPLEMIEAT177M A PREGNAVO A Doi .BLE-BLAD Sfil/1
Speaker Ludwig Spat:ding. Herne. West Germany
5:00 p.m. Dm :vim
5:30 p.m. AQIOURN
262 2 J Appei 1
8:00 p.m.
Appendices
DINNER
SKI/PM/11! P4h71C/MAIN AM) U.S. Pt WIC MUM SIUMCE EVERT PIXEL ON nx
CONMV1* OF PRENVAL CU&
Host: Richard Morton, M.D., March of Dimes Birth Defects Foundation
Wednesday May 11 1988
7:30 a.m. BREAKFAST
8:30-10:00 a.m. SESSION X: INnIAENTIONSPresiders: George Rhoades; John Hauth: Tarig SiddigiRappwiews: Rose Bemis; Donald MeNellis
8:30 aan.
8:50 a.m.
9:05 a.m.
9:25 a.m.
9:15 a.m,
10:00 a.m.
10:30 a.m.12:30 p
A kLYDGMIZED CLI.VICAL ALAI, OF 711E MIAMI/NT OF URIAPLASIL4 C0IDNIZTI1ON
AM) PRP:7E1M DELIVERY
Speaker Davkl Eschenhach, Seattle, Washington
DISO
S(X1,11. St PIVRT ARM; PRE6MAC); AV 014:R1 IEW O Cumout TRL-tis
Speaker: Diana Elbourne, Oxfcgd, United Kingd(nri
IIBMOV OF PROW 114Bol? IS IT 1170R1 1 MIME?
Veaker Marc Keirse, Leiden, Netherlands
D s (.1 Way
NI-MUM AND FITNESS BMA':
SESSION Xl: FUTURE DiRamoNsPresiders: Woodie Kessel: Sumner Yaffe: Heinz 13erendes
Rapporteu rs: Godfrey Oakley: Robert Kliegman
10:30 a.m. D/REcnms toR Ft IER RESE-IROl
Panel Moderator: Richard Behrman, Cleveland, OhioPane/ Members: Adrian Grant
Jeanne Brooks-GunnEmile PapiernikMort Rosen
Michael KramerMiles NovyIrwin MerkatzPeter Nathanielsz
Symposia nz Progra m 263
244
Dyannv Alfonso. R.N., Ph.D.Pniessor. of NursingDepartment of Muni ly NursingUniversity of California San FranciscoMail Stop N-111VS;in Frandsco, CA 9-4143
Duane Alexander. MDDIM: ICH% Nations! Institute of ChildHealth and Human DevehipmentNational Institutes of HealthBuilding 31. It )(nit 2A03Bethesda, MD 20892
Richard liehrtnan.Dean, Schinil of Medicinecast. kx!estern Re,eree I'niversity2119 Ahington RoadClevelimd. 011 .14100
105e M. Relii.an, M.D.Centro Ro.arino de Estudios PerinatalesBr. Orono 50002t.KRI Rosario. Argentina
Rose Bemis. R.N.. M.S.Division i)f Maternal Fetal Nledicinet'CLA \Wylie:it Center. Building I.1124 Wem Carson StwetTorrance. CA 90504
Heinz W. Berem.k.s. M.D.. M.11.S.Direct(ir. Pre% ention Research MigrantNatknLd Institute (if Child liealth and
!Ionian Devel(wwntNational Institutes of I lealthExecutive Plaza Ninth, 11(sn'n 610BCtittlida. MD 20892
Diedre [flank. U.N. , Ph.D.Ikmith Pumnition Disease PreventionNational t'xnter fin. Nursing ResearchNational Institutes of I lealthBldg 38A. Room B2E17Bethesda MD. 20892
Beatrice Blondel. NED.o Dr. G. Breart
INSERM123, Ixf de P(irt royal7501-4 l'aris, France
(erard Brean, M.1).de Recherches epidemi-
olergiques stir la Ntere ci 12EntantINSERM123. Kt de Port Royal7501-i Paris, France
Jeanne Bro4iks-Gunn. Ph.D.Educational Testing ServiceIiiisedale DrivePrinceton. NI °Mil
Appendix 11: List of Panictxints
titt.'VC N. (:aritis. MA),Assiwiate ProfessorDeparunent of Obstetrics and
GynecologyNiagee-Women's IlospitalForbes and Ilalket StreetPinstnirgh, PA 15213
Charkine Cat/. M.D.Chif. Pregnancy and Perinatology
BranchCenter for Research for Mothers and
ChildrenNatkinal Institutes of IlealthExecutive Plaza North. Room 0,13Bethesda, MD 20892
Leslie Cooper. RN.. M.P.H.Epidemioloa Branch Prevention
Research ProgramNati(mal Institute cif (hild Ilealth and
1)evehipmentExecutive Plaza North, Room OattBethesda, MD 20892
Robert K. Creasy. M.P.Chairman, Department of Obstetrics and
clynecologyReproductive lk.althl'niversity of Texas Medk.al Schoolot31 Fannin Street. Risint 32-0louston, 'IN 77030
Karla Dainus. Ph.D.Assistant Profe.ssor. Department of
DB .GYINAlbert Einstein College (it Ntedicine1)iteckir (if Reseatch EpidemiokigyBureau of ',Maternity Services and Family
PlanningNew l'ink City Department (if fie:dillPROPP
South Nurses Residence130) Morris Park AvenueBronx. NY 10461
Richard C. DavidFounder. Iiikos Nledical Corpiiratain182.1 East Dyer Road. Suite 21K)Santa Ana. CA 9270i
Nara I hpvlsifMedical Director for MCI1 Syr% ices)1dah(nna Dept of Ilealth
1000 N.E. loth Street on 703Oklahoma City. OK, 7.4152
Gian Carlos Di Rento, M.D.Cattedra di Purricultura PrenataicInstitut() di Ginecologia ed )steincia
Monteluce1-06100 Perugia. Italy
Diana Elboume, Ph,D.National Perinatal Epidemitik)gy ['nitRadclitk InfirmaryOxford 0X2 01E. United Kingdom
David A. Eschenbach, M.D.Professor of Obstetrics and GynecolcigyDepartnwrit of Obstetrics and
GynecologyIniversity of WashingtonSeattle, WA 98195
limy Foster, M.1),Professor and ChairmanDepartment of Obstetrk-s and
Gyneci)logyMeharry Medical College1005 Todd BoukvardNashville, TN .r208-3iv9
Ntargaret Freda. Ph.D.Assistant PnitesstirDepartment of 01)stetrics and
tlyttecculogyAnvil Einstein College of MedicineDirccuir of Ediicituin and Oimmunity
Affairs tor PROPPSouth Nurses Residence 1300 Nforris
Psrk Avenue Bronx, NY 10401
Adrian (rant. N1.1).National Perinatal EpidemiologyRadcliffe InfirmaryOxford ON2 l IF. rnited Kingdom
)(mini !Will, M.D.Chairman, .kmerican College
)bstetrics and GynecologyMaternal 'Fetal Medicine t'ainuititteeDepartment of Obstetrk.s and
Gynt'Culogy'niversitv of Alabama'niyersity SLIM m
Birmingham. Al. 3529i
Ruby Hearn, Phi).Vice presidentRobert \\A).1)(1.1nlinson FinindationColkge RoadPrinceton. NI 08i.i0
Henry Ileins.Profess( ir1)epartment of Obstetrics and (-(ynecoli)gyMedical I'Mversity of South Carolina
Charleston, SC 29425
Calvin J. I lohel, NED.Professor. Division of Maternal and Fetal
MedicineIlarbor General licispital1000 West Carson StreetTorrance. CA 9)509
Advances in the Prevention of Low Birthweight
Anne Hocken, M.S.Infant Mortality CommimionSwitzer Building. Room 2000330 C Street. S.W.1X7ashington, DC 20201
Howard Hoffinan. M.A.Chief. Biometry BranchPrevention Research ProgramNational Institute of Chikl Ikalth and
Iluman DevelopmentExecutive Plaza North, Room 030Bethesda, MD 20892
Vince L. Hutchins. M.D., MAUI.Associate DirectorMaternal and Child Health BureauParklawn Buikling. Roont 5(100Fishers Lane Rockville. MD 20857
Mare J.N.C. Keirse, M.D,Depannwnt of ObstetricsLeiden t 7niversityRijnsburgerweg 102333 AA LeidenThe Netherlands
John H. Kennel, M.D.Professor of PediatricsChief. Child Development DivisiimCase Western Reserw 1.raversitySdlool of MedicineRainbow Babies and Childrens Iluspital2074 Abington RoadCleveland, 011+1106
Wcxxlie Kessel, M.D., M.P.H.Director. Division of MCH Pnigram
Coordination and SystemsDcreli,pinent
Maternal and Chikl !health BureauParklawn Building. Room (1-17 5600Fishers Lane Rockville. MD 20857
Marshall Klaus, M.D.Children's Ilospital, Oakland747 52nd StreetOakland, CA 94609
Robert Khcgman,Vice Chairman of EducationRainbow Babies Si Children's flospital2101 Adelbert Road Rcx.nn 60Cleveland. OH 44100
Jean Konte, R.N., M.S.Coordinator ot North Cciast Perinatal
Pn)tectDepartment of Obstetrics and
Gynecology and Reproductive Sc.-lent es'niversity of California. SF
P.O. Box 0982San Franciseo, CA 941-13
Ann Koontz. CNA_ 1)r.P,11,Chief. Maternal and Infant Health BranchDivision of Maternal. Child. and Infant
IlealthMaternal and Child Health BureauParklawn Building, Room 6-1950X) Fishers LineRockvilk., MD 208i7
Michael Kramer. M.D.Associate Professor of PediatricsMcGill University Faculty of Medicine1020 Pine Avenue WestMontreal. Quebvc. Canada 113A1A2
Nlilton Lee. M.D.chief of ObstetricsDepartment of ()tweaks and
GynecokigyDrew Medical Sdlool12021 S. Wilminoin Ave,Los Angeles. CA 90059
Brian McCarthy, M.D.Pregnancy Epidemiology BranchDivision of Reproductive IlealthCenteri tOr Disease ControlBuilding 1. Room +119 WO1(1(X) Clifton Road, N.E.Atlanta. GA 30333
Marie McCormick, M.D.Joint Pnigram and NeonatologyBrigham & \\Omen's !hospital-7S Francis StreetBoston. MA 0211i
Donald McNellis. M.D.Center for Research k r Mt )thers and
ChildrenIthaca. NYNational Institutes of IlealthExecutive Plaza North. Room o.+3llethesda. MD 20892
Denise Main, M.D.Department of Ohstetrics and
Gynec()logyl'niversity of California. San FranciscoP.O. Box (1132San Francisco, CA 9i1,13
Paul Meis, M.D.Departnwnt of Obstetrics and
Gynee(slogyBowman Gray Sclusil of Medicine3(X) South Ilawthorne RoadU'inston-Sakm, NC 2-103
Ruth Merkatz, R.s . M.s.Allwrt Einstein College Ot Medicine13c)0 Morris Park AvenueBnmx. NY 10101
Irwin Merkatz, M.D.Professor and ChairmanDepartment of Obstetrics and
Gynecok)gyAlbert Einstein College Of Medicine1300 Morris Park AvenueBronx, NI' 10461
Richard F. Morton. M.D.Vice President for Medical ServicesMarch of Dimes Birth Defects
Foundation1275 Mamanmeck AvenueWhite Plains, NY 10(115
Eberhard Muelkr-lieubach, MD,Ass(s.late Pnifessor of Obstetrics and
C,yneeology'niversity of Pittsburgh
MaCiee WimiensliospitalForbes and llalket StreetsPittsburgh. PA 15213
Nancy Nance,Department of Obstetrics & GynecoliigvMedical I 'niversity of soutliCandinaCharleston, SC 29425
Peter Nathanielsz.Chief of Repoiductive SciencesCornell I 'niversitr
Steven Ng. M.D.Assistant Po)lessorC,ennide Sergievsky Center03o 1O8th StreetNew. York, NY 10032
Miles Novy, M.D.31(r Southwest Nottingham DriveNew York. NY I(X.)32
Ann Oakley. X.Yz."Uinta. Cc wam Research I 'nit41 Brunswick SquareLondon WC1N 1AZ'nited Kingdont
(;odl-rey Oakley, 51.1).Direckir. Division of Birth D...fects and
DeyelipmentalCenter for Envinninent.d I health and
Injury ControlCenters for Disease Contn)IKiiger Center. Rismi 20311000 Clifton RoadAtl.tnta, (.1.N 30333
David Olds, Ph.D.1)epartment of Pvdiatricst 'niversity of MichesterRiklicster, NY 110.12
266 Apperldix2.1i;
II
Emile Papiernik.Professor of Obstetrics and Gynecok )gyIfunun and Repnx.luctive ResearchIlospiul Antoine Bedew157, Rue de la Porte de Trivaux921,40 Clamart, France
Lynda Rajan. M.D.Thomas Comm Research I 'nitUniversity of London Institute of
Educatkin41 Brunswick SquareLondon WC1N1AZ, I'Mted Kingdom
George Rhoads. M.D.Chief, Epidoniohigy BranchPrevention Research Prt)gramNationa1 Institute of Child Ilealth at;d
Ifuman DevelopmentExecutive Plaza Ncirth, Rot-nu (40Bethesda, MI) 20892
Roberto Ronwro M.D.ale Prenatal Testing Center
03 York StreetNew Ilaven, CI. 00510
Monimer Rtrien, NM,Professor and ChairmanDepartment of Obstetrics and
GynecoltigyColumbia Presbyterian Medical Center022 West 108th StreetNew York, NY 10032
Nfichael Ross. M.D.Department of 011stetrics and
GynecokigyHarbin' General HospitalUCIA Medical School1000 \Xest Cas( in StreetTorrance, CA 90509
David Rush, \El),Department of Pediatrics and GynecologyAlbert Einstein College of MedicineRose . Kennedy Center1410 Pelham ParkwayBronx, NY 10401
Mary Sexton, M.P.H.Department of Epidemiol()gy'niversity N1ary land School ot
Preventive Medicine655 \X'. Baltimore StreetBaltimore, MD 21201
Patricia shit nio. Ph.D.Epidemiok igy BranchPrevention Research PnigrainNati( mai Insiitutv of Child Ilealth and
!Ionian DevelripmentExecutive Plaia North. Room OwBethesda. MD 20592
Tariq Siddiqi M.D.Depannent of ObstetricsCollege of Medicine.I.'niyersity of Cincinnati231 Bethesda AvenueCincinnati 011 45207-05.+1
Ludwig Spaetling,'fflyersitats-Frauenklinik Bochum
Ma rienhe )spitalI it Akeskampring -40D .4090 Iferne IFederal Republic of Germany
Brenda Spencer. Ph.D.Department of Epklemiolt)gy and Social
Researdi'niversity Ilospital of South Manchester
Kinnaird RoadN1anchester N1209y1.. I nited Kingdom
Serge l'zan. M.1).f lead of the Obstetnc staffMaternity Guy Le Lonerhipital Tentin
.4 rue de la Chine75020 Paris. France
Jose Villar.Visiting ScientistPrevention Research Pn)gr,:-,,Nalitnul Institute of Child I lealth and
Itiman DevelopmentNational Institutes of I lealthExecutive Plaza North, lit min 040liethesda. MD 20s92
Sumner Yaffe. M.D.Director, Center for Research
Ntc idlers and ChiklrenNational Institute of Child I lealth and
I finnan DevelopmentNational Instill ne f I fealthExecutive Pla/a North. RoomIkthesda, 20892
Phyllis Zucker, MS LINEDirector, Divisitm t)t Policy Analvs sOftic e of I fealth Plannnig and
EvaluationOffice of the Assistallt Secretary lOr
fealth!filbert If. 1 lumphrey Huikling. Rm AK;
2a 11 ndependent (' Avenue. SWWashington. IX: 20201
Appendices
List qf Pa rtk267
247




























































































































































































































































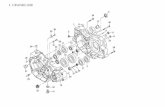
!['JNCLASSIF]ED - DTIC](https://static.fdokumen.com/doc/165x107/6323a138be5419ea700eb098/jnclassifed-dtic.jpg)












