Cavernous Nerve Repair With Allogenic Adipose Matrix and Autologous Adipose-derived Stem Cells
Dose-dependent effect of adipose-derived adult stem cells on vertical bone regeneration in rabbit...
-
Upload
independent -
Category
Documents
-
view
2 -
download
0
Transcript of Dose-dependent effect of adipose-derived adult stem cells on vertical bone regeneration in rabbit...
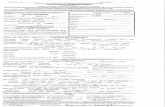
MEDLINE 09-10 01MAR10
Biomaterials. 2010 Feb 17. [Epub ahead of print]
Dose-dependent effect of adipose-derived adult stem cells on vertical bone regeneration in rabbit calvarium.
Pieri F, Lucarelli E, Corinaldesi G, Aldini NN, Fini M, Parrilli A, Dozza B, Donati D, Marchetti C.
Department of Dental Sciences, University of Bologna, Via San Vitale 59, 40139 Bologna, Italy.
Previous in vivo studies have shown a limited potential for vertical bone regeneration using osteoconductive scaffolds alone. In the present study, we investigated whether the association of adipose-derived adult stem cells (ASCs) with anorganic bovine bone (ABB) scaffold improved bone formation and implant osseointegration in a vertical guided bone regeneration model. Two pre-formed titanium domes were placed on the calvaria of 12 rabbits. Four treatment modalities were evenly distributed among the 24 domes: ABB alone, and ABB containing 3x10(5), 3x10(6), or 3x10(7) cells/graft. After 1 month, the domes were removed and one titanium implant was placed into each augmented site. One month after the second operation, the animals were killed and biopsy specimens were examined by histomorphometric and micro-CT analyses. Results indicated that at all concentrations, the ASC-loaded groups showed significantly more new bone formation and higher mean values of bone-implant contact and bone density inside threads than the ABB group. Furthermore, ASCs demonstrated a dose-response relationship, with the highest dose chosen inducing more robust bone regeneration. This study suggests that the delivery of ASCs on ABB might effectively increase vertical bone regeneration and implant osseointegration, versus ABB alone
NMR Biomed. 2010 Feb 19. [Epub ahead of print]
The effects of clinically used MRI contrast agents on the biological properties of human mesenchymal stem cells.
Kim HS, Oh SY, Joo HJ, Son KR, Song IC, Moon WK.
Department of Radiology, Seoul National University Hospital, Seoul, Korea.
This study was undertaken to compare the labeling efficiencies of three iron-oxide based MRI contrast agents [Feridex, Resovist and monocrystalline iron oxide (MION)] and to evaluate their effects on the biological properties of human mesenchymal stem cells (hMSCs). The hMSCs were cultivated for 1 and 7 days after 24-h labeling with iron oxide nanoparticles (12.5 microg Fe/mL) in the presence of poly-L-lysine (0.75 microg/mL). The hMSCs were labeled more efficiently with use of Feridex, Resovist as compared to MION. No significant differences were observed in terms of viability and proliferation of labeled hMSCs. The level of Oct-4 mRNA increased in labeled hMSCs at day 1 and the cellular phenotype changed from CD45-/CD44+/CD29+ to CD45low/CD44+/CD29+ at day 7, which closely resembles the phenotype of fresh bone marrow-derived hMSCs. Our study has demonstrated that the Feridex or Resovist is the preferred labeling agent for hMSCs. There was a change in Oct-4 and CD45 expression after labeling.
J Tissue Eng Regen Med. 2009 Oct 19. [Epub ahead of print]
Expansion of human mesenchymal stromal cells on microcarriers: growth and metabolism.
Schop D, van Dijkhuizen-Radersma R, Borgart E, Janssen FW, Rozemuller H, Prins HJ, de Bruijn JD.
Xpand Biotechnology BV, Bilthoven, The Netherlands.
Adult stem cells, or mesenchymal stromal cells (MSCs), are of great potential for cell therapy and tissue-engineering applications. However, for therapeutic use, these cells need to be isolated from tissue or a biopsy and efficiently expanded, as they cannot be harvested in sufficient quantities from the body. In our opinion, efficient expansion of MSCs can be achieved in a microcarrier-based cultivation system. This study selected a suitable microcarrier for human bone marrow-derived stromal cells (HBMSCs), optimized cell-seeding strategies by varying serum concentrations, and optimized dynamic expansion of the HBMSCs in a microcarrier-based spinner flask cultivation system by applying various feeding regimes. Cytodex 1 microcarriers in combination with a low-serum concentration (0-5%) in the medium resulted in the highest seeding efficiency for the HBMSCs. Subsequently, significant expansion of the HBMSCs on these
carriers has been observed. The highest number of HBMSCs population doublings (4.8 doublings) was obtained by a combination of 50% medium refreshment combined with addition of 30% medium containing microcarriers every 3 days. Exponential cell growth was observed for at least 9 days after seeding, provided that sufficient nutrients (such as glucose) were present, metabolite concentrations (such as ammonia) were kept below growth-inhibitory concentrations and adequate surface area was present for the cells. After dynamic expansion of the HBMSCs, the cells retained their differentiation potential and their cell surface markers, indicating that HBMSCs expansion on Cytodex 1 microcarriers did not alter the phenotypic properties of the cells.
Biomaterials. 2010 Feb 11. [Epub ahead of print]
Potent in vitro chondrogenesis of CD105 enriched human adipose-derived stem cells.
Jiang T, Liu W, Lv X, Sun H, Zhang L, Liu Y, Zhang WJ, Cao Y, Zhou G.
Department of Plastic and Reconstructive Surgery, Shanghai 9th People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai Key Laboratory of Tissue Engineering, 639 Zhi Zao Ju Road, Shanghai 200011, PR China; National Tissue Engineering Center of China, Shanghai, PR China.
Adipose-derived stem cells (ASCs) are considered as a promising cell source for cartilage regeneration. However, the heterogeneity of this cell source may affect their ability in cartilage formation. It is therefore necessary to establish an efficient method for isolating the cells that have chondrogenic potential. To date, no specific markers have been reported to be able to isolate such a cell population from human adipose tissue. In recent studies, endoglin (CD105) has been known as a relatively specific marker for identifying mesenchymal stem cells, but no studies show it is related to chondrogenic potential of human ASCs. In this study, human cells from adipose tissue were isolated, cultured, and sorted according to CD105 expression. The sorted cells were then subjected to adipogenic, osteogenic, and chondrogenic induction to confirm their multi-potentiality. In adipogenic conditions, CD105- cells showed stronger Oil Red staining and higher expression of adipose-specific genes compared to CD105+ cells. By contrast, CD105+ cells exhibited better osteogenic potential with stronger Alizarin Red staining and higher expression of osteogenic specific genes than CD105- cells. Noticeably, CD105+ cells also exhibited a much stronger chondrogenic potential than CD105- cells, with stronger collagen II staining and higher gene expression of collagen II and aggrecan. Most importantly, CD105+ cells could form a homogeneous cartilage-like tissue when seeded into a biodegradable scaffold and cultured in chondrogenic media for 8 weeks. These results indicate that sorting of ASC subpopulation with CD105 as a marker may allow better in vitro chondrogenesis and thus provide an important implications for cartilage regeneration and reconstruction using autologous cells from adipose tissue.
Tissue Eng Part A. 2010 Feb 25. [Epub ahead of print]
The Sequential Production Profiles of Growth Factors and Their Relations to Bone Volume in Ossifying Bone Marrow Explants.
Gurkan UA, Gargac J, Akkus O.
Purdue University, Weldon School of Biomedical Engineering, 206 S. Martin Jischke Drive, West Lafayette, Indiana, United States, 47907-2032, 765-496-1435; [email protected].
Osteogenesis is a complex process that involves the synergistic contribution of multiple cell types and numerous growth factors (GFs). In order to develop effective bone tissue engineering strategies employing GFs, it is essential to delineate the complex and interconnected role of GFs in osteogenesis. The studies investigating the temporal involvement of GFs in osteogenesis are limited to in vitro studies with single cell types or complex in vivo studies. There is a need for platforms that embody the physiological characteristics and the multicellular environment of natural osteogenesis. Marrow tissue houses various cell types that are known to be involved in osteogenesis and in vitro cultures of marrow inherently undergo osteogenesis process. Self-inductive ossification of marrow explants in vitro can be employed as a representative multicellular and 3-dimensional model of osteogenesis. Therefore, the aims of this study were to employ the rat bone marrow explant ossification model to determine: 1) the temporal production profiles of key GFs involved in osteogenesis, 2) the relation between GF production and ossification, and, 3) the relations between the GF levels throughout ossification. Temporal production profiles of transforming growth factor beta-1 (TGF-beta1), bone morphogenetic protein-2 (BMP-2), vascular endothelial growth factor (VEGF) and insulin-like growth factor-1 (IGF-1); and the bone-related proteins alkaline phosphatase (AP), osteocalcin (OC) were obtained by enzyme-linked immunosorbent assay (ELISA) conducted at days 2, 7, 12, 14, 19 and 21. The final amount of ossification (ossified volume, OV) was measured by micro computed tomography (muCT) at day 21. TGF-beta1, BMP-2, VEGF, IGF-1, AP and OC were produced by the ossifying marrow explants differentially over time. The early production of IGF-1 (day 2) correlated positively (r=0.868) with OV; however, latent production of IGF-1 correlated negatively (day14: r=-0.813; and day-19: r=-
0.865) with OV. OV also correlated with VEGF levels at day-12 (r=0.988) and at day-14 (r=0.970). Production of GFs also correlated to each other across time points which indicate the complex and interconnected contribution of various GFs in osteogenesis. Therefore tissue engineering strategies towards bone regeneration should consider the richness of GFs involved in osteogenesis as well as their dynamically varying participation over time.
Tissue Eng Part A. 2010 Feb 24. [Epub ahead of print]
Bolus Delivery of Mesenchymal Stem Cells to Injured Vasculature in the Rabbit Carotid Artery Produces a Dysfunctional Endothelium.
O'Shea CA, Hynes SO, Shaw G, Coen BA, Hynes AC, McMahon J, Murphy M, Barry F, O'Brien T.
1 Regenerative Medicine Institute, National University of Ireland , Galway, Ireland .
Endothelial dysfunction is an important factor in cardiovascular pathology. It has been suggested that pluripotent mesenchymal stem cells (MSCs) may contribute to repair of the endothelium through paracrine pathways. Enhanced re-endothelialization may be associated with a better outcome following angioplasty procedures. We examined the effect of the delivery of MSCs to a denuded vessel in vivo. The right carotid arteries of New Zealand white rabbits were denuded using an uninflated 3-French Fogarty balloon catheter. 1 x 10(5) MSCs in a bolus of 150 muL were then delivered intraluminally and allowed to dwell for 20 min. MSC engraftment was assessed using PKH-26 labeling and transduction with adenoviral reporter genes. Vessels were examined at 2 weeks for levels of endothelialization, as well as for neointimal hyperplasia and vasomotor function. Engraftment of MSCs was noted in the vessel wall following local arterial delivery. Endothelialization was improved following bolus MSC delivery at 2 weeks post-intervention. However, this endothelium is manifestly dysfunctional as indicated by a significant impairment in vasomotor activity and a significant increase in neointimal formation post-bolus delivery. Consistent with the formation of a dysfunctional endothelium, there was a higher rate of vessel occlusions in bolus-treated vessels due to not only predominately thrombosis but also neointimal hyperplasia. Our results suggest that naive MSCs delivered as a bolus to the occluded injured vascular segment generate dysfunctional endothelium presenting a risk of vessel occlusion. Such risks are important and need to be further assessed.
Tissue Eng Part A. 2010 Feb 25. [Epub ahead of print]
Differential gene expression in adipose stem cells cultured in allogeneic human serum versus fetal bovine serum.
Lindroos B, Aho KL, Kuokkanen H, Räty S, Huhtala H, Lemponen R, Yli-Harja O, Miettinen S, Suuronen R.
University of Tampere and Tampere University Hospital, Regea - Institute for Regenerative Medicine, Tampere, Finland; [email protected].
In pre-clinical studies, human adipose stem cells (ASCs) have been shown to have therapeutic applicability, but standard expansion methods for clinical applications remain yet to be established. ASCs are typically expanded in medium containing fetal bovine serum (FBS). However, sera and other animal-derived culture reagents stage safety issues in clinical therapy, including possible infections and severe immune reactions. By expanding ASCs in medium containing human serum, the problem can be eliminated. To define how allogeneic human serum (alloHS) performs in ASC expansion compared to FBS, a comparative in vitro study in both serum supplements was performed. The choice of serum had a significant effect on ASCs. Firstly, to reach cell proliferation levels comparable with 10% FBS, at least 15% alloHS was required. Secondly, while genes of the cell cycle pathway were overexpressed in alloHS, genes of the BMP receptor mediated signaling on the TGF-beta signaling pathway, regulating e.g. osteoblast differentiation, were overexpressed in FBS. The result was further supported by differentiation analysis, where early osteogenic differentiation was significantly enhanced in FBS. The data presented here underscore the importance of thorough investigation of ASCs for utilization in cell therapies. This study is a step forward in the understanding of these potential cells.
Tissue Eng Part A. 2010 Feb 25. [Epub ahead of print]
A survey on cell and engineered tissue therapies in Europe in 2008.
Martin I, Baldomero H, Tyndall A, Niederwieser D, Gratwohl A.
University Hospital Basel, Surgical Research, Hebelstrasse 20, Basel, Switzerland, 4031, +41 61 265 2384, +41 61 265 3990; [email protected].
Cellular therapy is an evolving investigational treatment modality in regenerative medicine but little published information is available on its current use. Starting from the established European group for Blood and Marrow Transplantation (EBMT) activity survey on hematopoietic stem cell (HSC) transplantation, a joint committee of four major scientific organizations made a coordinated attempt to collect detailed information in Europe for the year 2008. Thirty-three teams from 16 countries reported data on 656 patients to a "novel cellular therapy" survey, which were combined to additional 384 records reported to the standard EBMT survey. Indications were cardiovascular (29%; 100% autologous), musculoskeletal (18%; 97% autologous), neurological (9%; 39% autologous), epithelial/parenchymal (9%; 18% autologous), autoimmune diseases (12%; 77% autologous) or graft-vs-host-disease (23%; 13% autologous). Reported cell types were HSC (39%), mesenchymal stromal cells (47%), chondrocytes (5%), keratinocytes (7%), myoblasts (2%) and others (1%). In 51% of the grafts, cells were delivered following expansion, in 4% of the cases cells were transduced. Cells were delivered intravenously (31%), intraorgan (45%), on a membrane or gel (14%) or using 3D scaffolds (10%). This data collection platform is expected to capture and foresee trends for novel cellular therapies in Europe, and warrants further consolidation and extension.
Tissue Eng Part C Methods. 2009 Jul 14. [Epub ahead of print]
A three-dimensional gel bioreactor for assessment of cardiomyocyte induction in skeletal muscle derived stem cells.
Clause KC, Tinney JP, Liu LJ, Gharaibeh B, Huard J, Kirk JA, Shroff SG, Fujimoto KL, Wagner W, Ralphe JC, Keller BB, Tobita K.
Children's Hospital of Pittsburgh of UPMC , Cardiovascular Development Research Program, Pittsburgh, Pennsylvania, United States; [email protected].
Skeletal muscle derived stem cells (MDSCs) are able to differentiate into cardiomyocytes (CMs). However, it remains to be investigated whether differentiated CMs contract similar to native CMs. Here we developed a 3-dimensional cardiac gel bioreactor (3DGB), which induces a working CM phenotype from MDSCs and the contractile properties are directly measured as an engineered cardiac tissue. Neonate rat MDSCs were isolated from hind-leg muscles via the preplate technique. Isolated MDSCs were approximately 60% positive to Sca-1 and negative to CD34, CD45, or c-kit antigens. We sorted Sca-1(-) MDSCs and constructed MDSC-3DGBs by mixing MDSCs with acid soluble rat-tail collagen type-I and matrix factors. MDSC-3DGB exhibited spontaneous cyclic contraction by culture day 7. MDSC-3DGB expressed cardiac specific genes and proteins. Histological assessment revealed that cardiac specific troponin-T and -I expressed in a typical striation pattern and connexin-43 was expressed similar to the native fetal ventricular papillary muscle. ss-adrenergic stimulation increased MDSC-3DGB spontaneous beat frequency. MDSC-3DGB generated contractile force and intracellular calcium ion transients similar to engineered cardiac tissue from native cardiac cells. Results suggest that MDSC-3DGB induces a working CM phenotype in MDSCs and is a useful 3D culture system to directly assess the contractile properties of differentiated CMs <i>in vitro.</i>
Pathobiology. 2010;77(1):28-37. Epub 2010 Feb 25.
Role of Retinoic Acid-Related Orphan Receptor-alpha in Differentiation of Human Mesenchymal Stem Cells along with Osteoblastic Lineage.
Miyamoto S, Cooper L, Watanabe K, Yamamoto S, Inoue H, Mishima K, Saito I.
Department of Fixed Prosthodontics, Tsurumi University School of Dental Medicine, Yokohama, Japan.
Objective: In a human mesenchymal stem cell (hMSC) model of osteoblast differentiation, we identified expression of the retinoic acid-related orphan receptor-alpha (RORalpha) gene as a candidate osteogenesis-related gene using gene expression profiling. RORalpha is a member of the nuclear receptor family of intracellular transcription factors and plays multifunctional roles in tissue development and differentiation, inflammation metabolism and circadian rhythms. However, the important role of RORalpha in the differentiation of hMSC along the osteoblastic lineage is not yet fully understood. Methods: To investigate the role of RORalpha during osteoblast differentiation, we eliminated RORalpha from hMSCs with a small interfering RNA molecule (siRNA), and investigated the effects of suppressing RORalpha by RT-PCR analysis. Results: We showed that suppressing the expression of RORalpha by the siRNA inhibited the expression of both bone sialoprotein and dentin matrix protein 1. It was discovered coincidentally that the inhibitory effect of RORalpha resulted in failure of mineralization and bone nodule formation during the course of osteogenesis. Conclusion: The results of this study indicate that RORalpha must be an imperative modulator of bone sialoprotein and dentin matrix protein 1 involved in osteoblast differentiation and bone formation downstream of Wnt/beta-catenin signaling and just prior to the start of mineralization
Cells Tissues Organs. 2010 Feb 24. [Epub ahead of print]
A Simple Modification of the Separation Method Reduces Heterogeneity of Adipose-Derived Stem Cells.
Griesche N, Luttmann W, Luttmann A, Stammermann T, Geiger H, Baer PC.
Division of Nephrology, Department of Internal Medicine III, Goethe University, Frankfurt/M., Germany.
High hopes are put into the use of mesenchymal stem cells (MSCs) in various approaches for tissue engineering and regenerative medicine. MSCs are derived from different tissues with only small differences in their phenotype or their differentiation potential, but higher differences in the cell yield. Since fat is easily accessible and contains a high amount of MSCs to be isolated, adipose-derived stem cells (ASCs) are very promising for clinical approaches. ASCs are not a completely homogeneous cell population. Our study was initiated to explore an easy and convenient method to reduce heterogeneity. We tested different isolation methods: (1) the standard isolation method for ASCs based on plastic attachment, (2) the standard method with an initial washing step after 60 min of adherence and (3) immunomagnetic isolation by 4 typical markers (CD49a, CD90, CD105 and CD271). Cells isolated by these methods were evaluated using quantitative PCR and flow cytometry as well as by their differentiation potential. Washing led to a significantly lower expression of desmin, smA and six2, and a higher expression of the stem cell markers nestin, oct-4 and sall-1, compared to standard isolated cells, while the immunomagnetically isolated cells showed no significant changes. All cells independent of the isolation method could be induced to differentiate into adipocytes and osteoblasts. Our study demonstrates that a simple washing step reduces heterogeneity of cultured ASCs according to PCR analysis, whereas the immunomagnetic isolation only showed minor advantages compared to the standard method, but the disadvantage of significantly lower cell yields in the primary isolates
Cytokine. 2010 Feb 23. [Epub ahead of print]
Secretion profile of human bone marrow stromal cells: Donor variability and response to inflammatory stimuli.
Zhukareva V, Obrocka M, Houle JD, Fischer I, Neuhuber B.
Department of Neurobiology & Anatomy, Drexel University College of Medicine, 2900 Queen Lane, Philadelphia, PA 19129, USA.
Mesenchymal stem cells (MSC) derived from bone marrow are ideal transplants for a variety of CNS disorders and appear to support recovery after injury by secreting therapeutic factors. There is considerable variability in the secretion profile of MSC derived from different donors and it is known that MSC secretion changes in response to inflammatory stimuli, but no comprehensive analysis has been performed to address these issues. Here we show that MSC from seven donors secrete chemokines and cytokines in variable ranges, with some factors showing high variability. Treatment of cultured MSC with pro-inflammatory cytokines or tissue extracts from injured spinal cord resulted in up-regulation of selected cytokines, whereas treatment with an anti-inflammatory cytokine had little effect, indicating that the secretion profile is tightly regulated by environmental challenges. Patterns of up-regulated cytokines were similar in MSC from different donors suggesting a comparable response to inflammatory stimuli.
Biomaterials. 2010 Feb 23. [Epub ahead of print]
Continuous separation of cells of high osteoblastic differentiation potential from mesenchymal stem cells on an antibody-immobilized column.
Mahara A, Yamaoka T.
Department of Biomedical Engineering, Advanced Medical Engineering Center, National Cardiovascular Center Research Institute, Suita, Japan.
Here, we report that two distinctive cell populations with osteoblastic differentiation ability were found in adherent cell populations from bone marrow. Mesenchymal stem cells (MSCs) were conventionally isolated by using adherent property of bone marrow cells onto a plastic culture dish. MSCs enriched on the basis of their adherent property were considered phenotypically and functionally heterogeneous. We developed a ligand-immobilized surface for separating subpopulation of adherent cells derived from bone marrow by the cell rolling process. We successfully isolate two cell populations with high differentiation ability for osteoblasts in adherent bone marrow cells by using the anti-CD34 antibody-immobilized column. The antibody was covalently conjugated with polyacrylic acid and introduced onto the inner surface of a silicone tube. When cell suspension of MSCs was injected into the antibody-immobilized column,
different cell populations were isolated. After the cultivation of isolated cells in the osteoblastic differentiation medium for 1 week, few sub-populations were strongly induced to form osteoblastic cells. This study revealed that the ligand-immobilized surface can be used to continually separate cell populations under a labeling-free condition
J Cell Mol Med. 2010 Feb 24. [Epub ahead of print]
Tumor-associated fibroblasts and mesenchymal stem cells: more similarities than differences.
Paunescu V, Bojin FM, Tatu CA, Gavriliuc OI, Rosca A, Gruia AT, Tanasie G, Bunu C, Crisnic D, Gherghiceanu M, Tatu FR, Tatu CS, Vermesan S.
Department of Physiology, University of Medicine and Pharmacy "Victor Babes" Timisoara, Pta. E. Murgu No. 2, RO-300041 Timisoara, Romania.
Tumor-associated fibroblasts (TAFs) are part of the tumor stroma, providing functional and structural support for tumor progression and development. The origin and biology of TAFs are poorly understood, but within the tumor environment, TAFs become activated and secrete different paracrine and autocrine factors involved in tumorigenesis. It has been shown that bone marrow mesenchymal stem cells (MSCs) can be recruited into the tumors, where they proliferate and acquire a TAF-like phenotype. We attempted to determine to what extent TAFs characteristics in vitro juxtapose to MSCs' definition, and we showed that TAFs and MSCs share immunophenotypic similarities, including the presence of certain cell surface molecules (HLA-DR, CD29, CD44, CD73, CD90, CD106, and CD117); the expression of cytoskeleton and extracellular matrix proteins, such as vimentin, alpha-smooth muscle actin, nestin; and trilineage differentiation potential (to adipocytes, chondrocytes and osteoblasts). When compared to MSCs, production of cytokines, chemokines, and growth factors showed a significant increase in TAFs for vascular endothelial growth factor, transforming growth factor beta 1, interleukins (IL-4, IL-10), and tumor necrosis factor alpha. Proliferation rate was highly increased in TAFs and fibroblast cell lines used in our study, compared to MSCs, whereas ultrastructural details differentiated the two cell types by the presence of cytoplasmic elongations, lamellar content lysosomes, and intermediate filaments. Our results provide supportive evidence to the fact that TAFs derive from MSCs and could be a subset of "specialized" MSCs.
J Proteome Res. 2010 Feb 25. [Epub ahead of print]
Proteomic Analysis of Tumor Necrosis Factor-alpha-Induced Secretome of Human Adipose Tissue-Derived Mesenchymal Stem Cells.
Lee MJ, Kim J, Kim MY, Bae YS, Ryu SH, Lee TG, Kim JH.
Human adipose tissue-derived mesenchymal stem cells (hASCs) are useful for regeneration of inflamed or injured tissues. To identify secreted hASC proteins during inflammation, hASCs were exposed to tumor necrosis factor-alpha (TNF-alpha) and conditioned media derived from hASCs were analyzed by liquid chromatography coupled with tandem mass spectrometry. We identified 187 individual proteins as secreted proteins (secretome) in hASC-conditioned media; 118 proteins were secreted at higher levels upon TNF-alpha treatment. The TNF-alpha-induced secretome included a variety of cytokines and chemokines such as interleukin-6 (IL-6), IL-8, chemokine (C-X-C motif) ligand 6, and monocyte chemotactic protein-1 (MCP-1). TNF-alpha also increased expression of various proteases including cathepsin L, matrix metalloproteases and protease inhibitors, and induced secretion of long pentraxin 3, a key inflammatory mediator implicated in innate immunity. TNF-alpha-conditioned media stimulated migration of human monocytes, which play a key role in inflammatory responses. This migration was abrogated by pretreatment with neutralizing anti-IL-6, anti-IL-8, and anti-MCP-1 antibodies, suggesting that IL-6, IL-8, and MCP-1 are involved in migration of monocytes. Taken together, these results suggest that TNF-alpha-induced secretome may play a pivotal role of in inflammatory responses and that shotgun proteomic analysis will be useful for elucidation of the paracrine functions of mesenchymal stem cells.
Childs Nerv Syst. 2010 Mar;26(3):323-31.
Neuroprotective effect of combined hypoxia-induced VEGF and bone marrow-derived mesenchymal stem cell treatment.
An SS, Jin HL, Kim KN, Kim DS, Cho J, Liu ML, Oh JS, Yoon do H, Lee MH, Ha Y.
Department of Neurosurgery, Spine & Spinal Cord Institute, College of Medicine, Yonsei University, Seoul, 120-752, South Korea.
PURPOSES: To avoid unwanted adverse effects of higher doses of single treatment of stem cells and gene therapy and increase the therapeutic efficacies, we hypothesized the combined therapy with stem cells and gene therapy. This study assessed the neuroprotective effects of combined gene therapy and stem cell treatment under ischemic hypoxia conditions using hypoxia-inducible vascular endothelial growth factor (VEGF) and bone marrow-derived mesenchymal stem cells (BMSC). METHODS: Experimental groups included the control which was N2A cells transfected with empty vectors, the transfection only group which was N2A cells treated with pEpo-SV-VEGF alone, the BMSC only group which was N2A cells transfected with empty vectors and cocultured with BMSCs, and the combined treatment group which was N2A cells treated with pEpo-SV-VEGF and cocultured with BMSCs. Each group was transfected for 4 h and cultured at 37 degrees C and 5% CO2 for 24 h. Each group was then cultivated under hypoxic conditions (1% O2) for 12 h. Neuroprotective effects were assessed by reverse transcription polymerase chain reaction, annexin V, and cytotoxicity assay. RESULTS: Neurons exposed to hypoxic conditions exhibited neuronal apoptosis. Compared to single treatments, the combined hypoxia-inducible VEGF and BMSC treatment demonstrated a significant increase in VEGF expression and decreased neuronal apoptosis. CONCLUSIONS: These results suggest that combined pEpo-SV-VEGF and BMSC treatment is effective in protecting neurons against hypoxic ischemic injury
J Biomed Biotechnol. 2010;2010:101864. Epub 2010 Feb 16.
Optical spectroscopy for noninvasive monitoring of stem cell differentiation.
Downes A, Mouras R, Elfick A.
School of Engineering, The University of Edinburgh, Edinburgh EH9 3JL, UK.
There is a requirement for a noninvasive technique to monitor stem cell differentiation. Several candidates based on optical spectroscopy are discussed in this review: Fourier transform infrared (FTIR) spectroscopy, Raman spectroscopy, and coherent anti-Stokes Raman scattering (CARS) microscopy. These techniques are briefly described, and the ability of each to distinguish undifferentiated from differentiated cells is discussed. FTIR spectroscopy has demonstrated its ability to distinguish between stem cells and their derivatives. Raman spectroscopy shows a clear reduction in DNA and RNA concentrations during embryonic stem cell differentiation (agreeing with the well-known reduction in the nucleus to cytoplasm ratio) and also shows clear increases in mineral content during differentiation of mesenchymal stem cells. CARS microscopy can map these DNA, RNA, and mineral concentrations at high speed, and Mutliplex CARS spectroscopy/microscopy is highlighted as the technique with most promise for future applications.
Haematologica. 2010 Feb 23. [Epub ahead of print]
CD271 antigen defines a subset of multipotent stromal cells with immunosuppressive and lymphohematopoietic engraftment-promoting properties.
Kuçi S, Kuçi Z, Kreyenberg H, Deak E, Pütsch K, Huenecke S, Amara C, Koller S, Rettinger E, Grez M, Koehl U, Latifi-Pupovci H, Henschler R, Tonn T, von Laer D, Klingebiel T, Bader P.
Department of Hematology/Oncology, Frankfurt am Main, Germany.
Background In vitro proliferative and differentiation potential of mesenchymal stromal cells generated from CD271(+) bone marrow mononuclear cells (CD271-MSCs) has been demonstrated in several earlier and recent reports. In the present study we focused, in addition to proliferative and differentiation potential, in vitro and in vivo immunosuppressive and lymphohematopoietic engraftment-promoting potential of these MSCs compared to bone marrow-derived MSCs generated by plastic adherence (PA-MSCs). DESIGN AND METHODS: We set up a series of experimental protocols in order to determine the phenotype of CD271-MSCs, their clonogenic, proliferative, differentiation and immunosuppressive potential. Potential of CD271-MSCs to improve the engraftment of CD133(+) hematopoietic stem cells (HSCs) at cotransplantation was evaluated in immunodeficient NOD/SCID-IL2Rgamma(null) mice. RESULTS: In vitro studies demonstrated that CD271-MSCs differentiate along adipogenic, osteogenic and chondrogenic lineage (trilineage potential), produce significantly higher levels of cytokines than PA-MSCs, and significantly inhibit the proliferation of allogeneic T-lymphocytes in mixed lymphocyte reaction assay. Elevated levels of prostaglandin E2, but not nitric monoxide, mediated the majority of this immunosuppressive effect. In vivo studies showed that CD271-MSCs promote a significantly greater lymphoid engraftment than PA-MSCs when cotransplanted with CD133(+) HSCs at a ratio of 8:1 in immunodeficient NOD/SCID-IL2Rgamma(null) mice. They induced a 10.4-fold increase in the number of T-cells, a 2.5-fold increase in the number of NK-cells, and a 3.6-fold increase in the number of B-cells, indicating major qualitative difference between these two MSC populations. Conclusions Our results indicate that CD271 antigen provides a versatile marker for prospective isolation and expansion of multipotent MSCs with immunosuppressive and lymphohematopoietic engraftment-promoting properties. Their cotransplantation with HSCs in patients with
hematological malignancies may prove valuable in the prevention of impaired/delayed T-cell recovery and graft-versus-host disease.
Arch Oral Biol. 2010 Feb 20. [Epub ahead of print]
Choukroun's platelet-rich fibrin (PRF) stimulates in vitro proliferation and differentiation of human oral bone mesenchymal stem cell in a dose-dependent way.
Dohan Ehrenfest DM, Doglioli P, de Peppo GM, Del Corso M, Charrier JB.
Department of Biomaterials, Institute for Clinical Sciences, The Sahlgrenska Academy at University of Gothenburg, Sweden; The LoB5 Foundation for Research, Paris, France.
BACKGROUND: Choukroun's platelet-rich fibrin (PRF) is an autologous leukocyte- and platelet-rich fibrin biomaterial. The purpose of this study was to analyse the in vitro effects of PRF on human bone mesenchymal stem cells (BMSC), harvested in the oral cavity after preimplant endosteal stimulation. MATERIALS AND METHODS: BMSCs from primary cultures were cultivated with or without a PRF membrane originating from the same donor as for the cells, in proliferation or osteoblastic differentiation conditions. After 7 days, the PRF membranes were removed. A series of cultures were performed using 2 PRF membranes, in order to measure the dose-dependent effect. Cell counts, cytotoxicity tests, alkaline phosphatase (ALP) activity quantification, Von Kossa staining and mineralisation nodules counts were performed at 3, 7, 14, 21 and 28 days. A last independent series was carried on up to 14 days, for a morphological scanning electron microscope (SEM) observation. RESULTS: PRF generated a significant stimulation of the BMSC proliferation and differentiation throughout the experimental period. This effect was dose-dependent during the first weeks in normal conditions, and during the whole experimentation in differentiation conditions. The cultures without PRF in differentiation conditions did not rise above the degree of differentiation of the cultures in normal conditions with 1 or 2 PRF up to the 14th and 28th day, respectively. The SEM culture analysis at day 14 allowed to show the mineralisation nodules which were more numerous and more structured in the groups with PRF compared to the control groups. DISCUSSION AND CONCLUSIONS: This double contradictory proliferation/differentiation result may be due to the numerous components of PRF, particularly the presence of leukocytes: any culture with PRF is in fact a coculture with leukocytes. It could be the source of differential geographic regulation processes within the culture. The combination of oral BMSC and PRF might offer many potential clinical and biotechnological applications, and deserves new studies
Osteoarthritis Cartilage. 2010 Feb 6. [Epub ahead of print]
Spatial regulation of human mesenchymal stem cell differentiation in engineered osteochondral constructs: effects of pre-differentiation, soluble factors and medium perfusion.
Grayson WL, Bhumiratana S, Grace Chao PH, Hung CT, Vunjak-Novakovic G.
Department of Biomedical Engineering, Columbia University, New York, NY, USA.
OBJECTIVE: The objective of the study was to investigate the combined effects of three sets of regulatory factors: cell pre-differentiation, soluble factors and medium perfusion on spatial control of human mesenchymal stem cell (hMSC) differentiation into cells forming the cartilaginous and bone regions in engineered osteochondral constructs. DESIGN: Bone-marrow derived hMSCs were expanded in their undifferentiated state (UD) or pre-differentiated (PD) in monolayer culture, seeded into biphasic constructs by interfacing agarose gels and bone scaffolds and cultured for 5 weeks either statically (S) or in a bioreactor (BR) with perfusion of medium through the bone region. Each culture system was operated with medium containing either chondrogenic supplements (C) or a cocktail (Ck) of chondrogenic and osteogenic supplements. RESULTS: The formation of engineered cartilage in the gel region was most enhanced by using undifferentiated cells and chondrogenic medium, whereas the cartilaginous properties were negatively affected by using pre-differentiated cells or the combination of perfusion and cocktail medium. The formation of engineered bone in the porous scaffold region was most enhanced by using pre-differentiated cells, perfusion and cocktail medium. Perfusion also enhanced the integration of bone and cartilage regions. CONCLUSIONS: (1) Pre-differentiation of hMSCs before seeding on scaffold was beneficial for bone but not for cartilage formation. (2) The combination of medium perfusion and cocktail medium inhibited chondrogenesis of hMSCs. (3) Perfusion improved the cell and matrix distribution in the bone region and augmented the integration at the bone-cartilage interface. (4) Osteochondral grafts can be engineered by differentially regulating the culture conditions in the two regions of the scaffold seeded with hMSCs (hydrogel for cartilage, perfused porous scaffold for bone).
Arthritis Res Ther. 2010 Feb 22;12(1):R31. [Epub ahead of print]
Discrepancy between the in vitro and in vivo effects of murine mesenchymal stem cells on T cell proliferation and collagen-induced arthritis.
Schurgers E, Kelchtermans H, Mitera T, Geboes L, Matthys P.
ABSTRACT: INTRODUCTION: The goal of this study is to analyze the potential immunosuppressive properties of mesenchymal stem cells (MSC) on T cell proliferation and in collagen-induced arthritis (CIA). An additional aim is to investigate the role of interferon-gamma (IFN-gamma) in these processes. METHODS: MSC were isolated from bone marrow of DBA/1 wild type and IFN-gamma receptor knock-out (IFN-gammaR KO) mice and expanded in vitro. Proliferation of anti-CD3 stimulated CD4+ T cells in the presence or absence of MSC was evaluated by thymidine incorporation. CIA was induced in DBA/1 mice and animals were treated with MSC by intravenous or intraperitoneal injections of wild type or IFN-gammaR KO MSC. RESULTS: Purity of enriched MSC cultures was evaluated by flow cytometry and their ability to differentiate into osteoblasts and adipocytes. In vitro, wild type MSCs dose-dependently suppressed anti-CD3-induced T cell proliferation whereas IFN-R KO MSCs had a significantly lower inhibitory potential. A role for inducible nitric oxide (iNOS), programmed death ligand-1 (PD-L1) and prostaglandin E2 (PGE2), but not indoleamine 2,3-dioxigenase (IDO), in the T cell inhibition was demonstrated. In vivo, neither wild type nor IFN-gammaR KO MSC were able to reduce the severity of CIA or the humoral or cellular immune response towards collagen type II. CONCLUSIONS: Whereas MSC inhibit anti-CD3-induced proliferation of T cells in vitro, an effect partially mediated by IFN-gamma, MSC do not influence in vivo T cell proliferation nor the disease course of CIA. Thus there is a clear discrepancy between the in vitro and in vivo effects of MSC on T cell proliferation and CIA.
Connect Tissue Res. 2010 Feb 23. [Epub ahead of print]
Ectopic osteogenesis of hBMP-2 gene-transduced human bone mesenchymal stem cells/BCB.
Han D, Li J, Guan X.
Department of Plastic & Reconstructive Surgery, Ninth People's Hospital, Medical School of Shanghai Jiao Tong University, Shanghai, China.
We determined the feasibility of using scaffolds of adenoviral human BMP2 gene (AdBMP2)-modified human bone marrow mesenchymal stem cells (hBMSCs) and antigen-free bovine cancellous bone (BCB) to construct bone tissue. hMSCs were infected with AdBMP-2. Expression of BMP-2 and alkaline phosphatase confirmed successful secretion of active BMP-2. The osteogenic capability of a composite of AdBMP2-modified hMSCs with BCB was evaluated in athymic mice (group A). BCB (group B), hMSCs/BCB (group C), adenoviral beta-galactosidase genes (Adbetagal)-transfected hMSCs/BCB (group D) were controls. Formation of bone tissue was assessed by histological methods 4 weeks and 8 weeks after implantation. Implanted cells were identified by human Y-chromosome-specific fluorescence in-situ hybridization (FISH). hMSCs differentiated into osteogenic cells, and bone formation was observed. Obvious bone formation was not noted at any time point in control groups. We hypothesize that the described method is a promising method for bone regeneration.
Urol Int. 2010;84(1):94-99. Epub 2010 Feb 17.
Bone Marrow Mesenchymal Stem Cells Induce Angiogenesis and Promote Bladder Cancer Growth in a Rabbit Model.
Zhang K, Shi B, Chen J, Zhang D, Zhu Y, Zhou C, Zhao H, Jiang X, Xu Z.
Department of Urology, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, PR China.
Objectives: To investigate the effect of mesenchymal stem cells (MSCs) in the process of tumor development and the possibility of MSCs differentiating into vascular endothelial cells in the tumor microenvironment. Material and Methods: Twenty male New Zealand rabbits were randomly divided into 2 groups: a test group and a control group. MSCs were isolated and cultured by bone marrow cell adherence. The bladder tumor models were built by embedding a VX2 mass in swelled bladder mucosa in all of the rabbits (n = 20). One week later, 4',6-diamidino-2-phenylindole-labeling MSCs were transplanted into tumor tissue in the test group (n = 10). Culture medium was injected into the tumor tissue of the control group (n = 10). The maximum diameter of the tumor mass was measured by ultrasound at 2 and 4 weeks after the VX2 tumor mass was embedded. All animals were sacrificed at 4 weeks. The double labeling immunofluorescence for CD146 was performed to reveal whether engrafted cells can differentiate into vascular endothelial cells. Vascular density was compared between the 2 groups. Results: There was no significant difference in the maximum diameters of the tumor
masses between the 2 groups at 2 weeks (test group 0.77 +/- 0.15 cm vs. control group 0.71 +/- 0.15 cm, p > 0.05). The maximum diameters appeared larger in the test group at 4 weeks (test group 3.82 +/- 0.94 cm vs. control group 2.28 +/- 0.54 cm, p < 0.05). Immunofluorescence studies revealed some engrafted MSCs expressing a vascular endothelial cell phenotype (CD146). Furthermore, vascular density was augmented in the test group in comparison to the control group (10.1 +/- 0.70/0.2 mm(2) vs. 8.24 +/- 0.81/0.2 mm(2), p < 0.05). Conclusions: Engrafted MSCs can differentiate into vascular endothelial cells and contribute to angiogenesis in the tumor microenvironment, which may be the major pathway of promoting tumor growth.
Transplant Proc. 2010 January - February;42(1):345-349.
The Next Generation of Burns Treatment: Intelligent Films and Matrix, Controlled Enzymatic Debridement, and Adult Stem Cells.
Drago H, Marín GH, Sturla F, Roque G, Mártire K, Díaz Aquino V, Lamonega R, Gardiner C, Ichim T, Riordan N, Raimondi JC, Bossi S, Samadikuchaksaraei A, van Leeuwen M, Tau JM, Núñez L, Larsen G, Spretz R, Mansilla E.
Banco de Tejidos, Hospital de Quemados, CABA, Argentina.
We describe a novel technology based on nanoengineered multifunctional acellular biologic scaffolds combined with wound dressings and films of the same kind. This method allows selective delivery and release of shielded biomaterials and bioactive substances to a desired wound or damaged tissue while stimulating the selective anchoring and adhesion of endogenous circulating repairing cells, such as mesenchymal stem cells, to obtain a faster and more physiologic healing process. We also present a new controlled enzymatic debridement process for more effective burned tissue scarolysis. In light of our preliminary in vitro and in vivo data, we are convinced that these approaches can include the use of other kinds of adult stem cells, such as endometrial regenerative cells, to improve the vascularization of the constructs, with great potential in the entire tissue and organ regeneration field but especially for the treatment of severely burned patients, changing the way these lesions may be treated in the future
Exp Cell Res. 2010 Feb 18. [Epub ahead of print]
Pitfalls in spontaneous in vitro transformation of human mesenchymal stem cells.
Garcia S, Martín MC, de la Fuente R, Cigudosa JC, Garcia-Castro J, Bernad A.
Regenerative Cardiology Department. Centro Nacional de Investigaciones Cardiovasculares Carlos III. Melchor Fernández Almagro, 3. 28029 Madrid, Spain.
J Clin Neurosci. 2010 Feb 18. [Epub ahead of print]
Cultured autologous bone marrow stem cells inhibit bony fusion in a rabbit model of posterolateral lumbar fusion with autologous bone graft.
Urrutia J, Mery P, Martínez R, Pizarro F, Apablaza D, Mardones R.
Department of Orthopaedic Surgery, Pontificia Universidad Catolica de Chile, Marcoleta 352, Santiago, Chile.
Mesenchymal stem cells (MSCs) have been isolated from various tissues and expanded in culture. MSCs add osteogenic potential to ceramic scaffolds when used together. A spinal fusion rabbit model was used to evaluate whether a pellet of cultured, autologous bone marrow MSCs (BMSCs) with osteogenic differentiation could increase the fusion rate when co-grafted with an autologus bone graft compared to autograft alone. Thirty rabbits were randomly assigned to two groups. Group 1 received bone autograft alone and Group 2 received bone autograft plus a pellet of cultured and differentiated BMSCs. Group 2 rabbits had a bone marrow puncture, after which the BMSC were cultured and osteoblastic differentiation was induced. BMSC cultures were obtained from 12 of 15 rabbits. The 27 rabbits underwent a bilateral, L4-L5 intertransverse fusion with an autograft and in Group 2 rabbits a pellet of differentiated BMSCs was added to the autograft. In Group 1, the fusion rate was 53% (8 of 15 rabbits) and in Group 2 the fusion rate was 0% (p<0.05). Adding differentiated BMSCs in a pellet without a scaffold not only failed to increase fusion rate, but completely inhibited bony growth.
Stem Cells Dev. 2010 Feb 19. [Epub ahead of print]
Umbilical Cord Derived Mesenchymal Stem Cells Isolated by a Novel Explantation Technique Can Differentiate Into Functional Endothelial Cells and Promote Revascularization.
Xu Y, Meng H, Li C, Hao M, Wang Y, Yu Z, Li Q, Han J, Zhai Q, Qiu L.
Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Sciences, China; [email protected].
Stem cells transplantation holds great promise for the treatment of ischemic diseases through functional revascularization. Umbilical cord derived mesenchymal stem cells (UC-MSCs) are also an ideal candidate for cell-based bioengineering. Herein, we report on the development of a simple and effective protocol to isolate UC-MSCs, and confirm their endothelial potential both in vitro and in vivo. UC-MSCs were isolated by a novel explantation technique and induced to differentiate into endothelial-like cells. Then UC-MSCs were transplanted into ischemic mouse model and cultured on 3D Gel/MMT-CS composite scaffolds. Morphological and proliferation assessments show that sufficient UC-MSCs can be generated during a relatively short culture period with explantation technique. Increased expression of endothelial-specific markers (KDR, and vWF), and functional markers (ac-LDL uptake and UEA-1 binding), indicate that functional endothelial progenitor cells are induced after 9 days of in vitro culture. In an ischemic hindlimb mouse model, the ratio of ischemic/non-ischemic limb perfusion 4 weeks after MSCs transplantation reached 0.84+/-0.09. The capillary density of this group was 2.57 fold greater than that of sham injected mice (p<0.05). Immunofluorescence and immunohistological analyses indicate that MSCs may act to salvage the ischemic tissue by incorporating into the local vasculature. In vitro, UC-MSCs were observed to incorporate into 3D Gel/MMT-CS composite scaffolds, to secrete extracellular matrix, to remain viable, and to retain their proliferation capacity. In conclusion, UC-MSCs isolated by novel yet simple explantation technique are well suited for application in the development of novel stem cell-based revascularization therapies.
J Biomed Mater Res A. 2010 Feb 22. [Epub ahead of print]
An improved collagen scaffold for skeletal regeneration.
Oliveira SM, Ringshia RA, Legeros RZ, Clark E, Yost MJ, Terracio L, Teixeira CC.
Department of Mechanical Engineering, ESTG-Escola Superior de Tecnologia e Gestão, 3504-510 Viseu, Portugal.
Bone repair and regeneration is one of the most extensively studied areas in the field of tissue engineering. All of the current tissue engineering approaches to create bone focus on intramembranous ossification, ignoring the other mechanism of bone formation, endochondral ossification. We propose to create a transient cartilage template in vitro, which could serve as an intermediate for bone formation by the endochondral mechanism once implanted in vivo. The goals of the study are (1) to prepare and characterize type I collagen sponges as a scaffold for the cartilage template, and (2) to establish a method of culturing chondrocytes in type I collagen sponges and induce cell maturation. Collagen sponges were generated from a 1% solution of type I collagen using a freeze/dry technique followed by UV light crosslinking. Chondrocytes isolated from two locations in chick embryo sterna were cultured in these sponges and treated with retinoic acid to induce chondrocyte maturation and extracellular matrix deposition. Material strength testing as well as microscopic and biochemical analyzes were conducted to evaluate the properties of sponges and cell behavior during the culture period. We found that our collagen sponges presented improved stiffness and supported chondrocyte attachment and proliferation. Cells underwent maturation, depositing an abundant extracellular matrix throughout the scaffold, expressing high levels of type X collagen, type I collagen and alkaline phosphatase. These results demonstrate that we have created a transient cartilage template with potential to direct endochondral bone formation after implantation
Histol Histopathol. 2010 Apr;25(4):463-71.
TGF-beta1 and VEGF after fresh frozen bone allograft insertion in oral-maxillo-facial surgery.
Rodella LF, Favero G, Boninsegna R, Borgonovo A, Rezzani R, Santoro F.
Department of Biomedical Science Biotechnology Section of Human Anatomy, University of Brescia, Brescia, Italy. [email protected].
Bone regeneration technique using allografts is widely used in oral surgery to repair alveolar defects and to increase alveolar volume for endosseous implant insertions. Bone allografts promote the reabsorption and neo-synthesis of bone
tissue, which are regulated by numerous cytokines, proteins and growth factors. In this study, six patients with insufficient alveolar volume for endosseous implant insertions, were treated with bone regeneration technique using Fresh Frozen Bone (FFB) allografts collected from the femoral head or the hip. Samples of bone graft collected during graft insertion surgery and biopsies collected six months later during implantology were fixed, decalcified and analyzed histomorphologically and morphometrically by haematoxylin-eosin staining. In addition, TGF-beta1 and VEGF were analyzed by immunohistochemistry. The histological analysis of FFBs showed wide areas of calcified bone organized in osteons intermingled with areas of non-calcified matrix containing osteoblasts. However, the regenerated alveolar bone, collected six months after the graft insertion surgery, showed wide areas of non-calcified matrix. TGF-beta1 and VEGF were less expressed in FFB than in regenerated alveolar bone
Rheumatology (Oxford). 2010 Feb 24. [Epub ahead of print]
Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees.
Wang Y, Wluka AE, Pelletier JP, Martel-Pelletier J, Abram F, Ding C, Cicuttini FM.
Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Alfred Hospital, Melbourne, Australia, Osteoarthritis Research Unit, University of Montreal Hospital Research Centre (CRCHUM), Notre-Dame Hospital, ArthroVision Inc., Montreal, Quebec, Canada and Menzies Research Institute, University of Tasmania, Hobart, Tasmania, Australia.
Objectives. Meniscal extrusion is often present in knees with OA, and has been associated with cartilage changes. It is unknown whether meniscal extrusion is related to subchondral bone. The aim of the study was to examine the relationship between meniscal extrusion and knee cartilage and subchondral bone, and also changes in these structures over 2 years in a cohort with mild to moderate knee OA. Methods. One hundred and seventeen subjects with knee OA entered the study and underwent MRI on their symptomatic knee at baseline and approximately 2 years later. Meniscal extrusion was assessed at baseline; tibial cartilage volume and plateau bone area, subchondral bone marrow lesions (BMLs) and bone cysts were measured at baseline and follow-up. Results. At baseline, meniscal extrusion was associated with reduced tibial cartilage volume, increased tibial plateau area, increased prevalence of BMLs and bone cysts in both medial and lateral tibiofemoral compartments (all P </= 0.001). Baseline medial meniscal extrusion was associated with increased expansion of tibial plateau bone (P = 0.04), increases in BMLs (P = 0.02) and bone cysts (P = 0.003) in the medial tibiofemoral compartment over 2 years. Conclusions. Meniscal extrusion predicts increases in subchondral bone lesions and tibial plateau bone expansion in patients with knee OA. These data suggest that subchondral bone changes are an early consequence of meniscal extrusion. This may reflect the impaired ability of an extruded meniscus to optimally distribute mechanical loading across the tibial plateau.
J Pediatr Orthop. 2010 Mar;30(2):199-205.
Exaggerated inflammatory response after use of recombinant bone morphogenetic protein in recurrent unicameral bone cysts.
Macdonald KM, Swanstrom MM, McCarthy JJ, Nemeth BA, Guliani TA, Noonan KJ.
Department of Orthopedics and Rehabilitation, University of Wisconsin, Madison, WI.
BACKGROUND: Recurrent unicameral bone cysts (UBCs) can result in significant morbidity during a child's physical and emotional development. Multiple treatment options are available and a review of the literature fails to clearly define the optimal treatment for UBCs. Recombinant bone morphogenetic protein (BMP) has been used with success in other disorders of poor bone formation. This manuscript is the first to report on the use of recombinant BMP in the treatment of UBCs. METHODS: Three patients with recurrent UBCs underwent revision surgery with recombinant BMP. Radiographic and medical review was performed and is reported here. RESULTS: In these patients, the use of BMP failed to fully resolve their UBC; 2 patients had complete recurrence that required further surgery. In addition to poor radiographic results, all patients developed exaggerated inflammatory responses in the acute postoperative period. Each child developed clinically significant limb swelling and pain that mimicked infection. CONCLUSIONS: On the basis of our poor radiographic results and a paradoxical clinical result, we no longer recommend the use of recombinant BMP in the manner reported here for the treatment of recurrent UBCs. LEVEL OF EVIDENCE: Level IV, case series.
J Bone Joint Surg Br. 2010 Feb;92(2):224-9.
Free vascularised iliac bone graft for recalcitrant avascular nonunion of the scaphoid.
Arora R, Lutz M, Zimmermann R, Krappinger D, Niederwanger C, Gabl M.
Department of Trauma Surgery Medical University Innsbruck, Anichstrasse 35, A-6020 Innsbruck, Tyrol, Austria. [email protected]
We report the use of a free vascularised iliac bone graft in the treatment of 21 patients (19 men and 2 women) with an avascular nonunion of the scaphoid in which conventional bone grafting had previously failed. The mean age of the patients was 32 years (23 to 46) and the dominant wrist was affected in 14. The mean interval from fracture to the vascularised bone grafting was 39 months (9 to 62). Pre-operative MRI showed no contrast enhancement in the proximal fragment in any patient. Fracture union was assessed radiologically or with CT scans if the radiological appearances were inconclusive. At a mean follow-up of 5.6 years (2 to 11) union was obtained in 16 patients. The remaining five patients with a persistent nonunion continued to experience pain, reduced grip strength and limited range of wrist movement. In the successfully treated patients the grip strength and range of movement did not recover to match the uninjured side. Prevention of progressive carpal collapse, the absence of donor site morbidity, good subjective results and pain relief, justifies this procedure in the treatment of recalcitrant nonunion of the scaphoid.
J Biomed Mater Res A. 2010 Feb 22. [Epub ahead of print]
Repair of large cranial defects by hBMP-2 expressing bone marrow stromal cells: Comparison between alginate and collagen type I systems.
Chang SC, Chung HY, Tai CL, Chen PK, Lin TM, Jeng LB.
Department of Plastic Surgery, China Medical University Hospital, Taichung 404, Taiwan.
Despite a wide range of available sources for bone repair, significant limitations persist. To bioengineer bone, we have previously transferred adenovirus-mediated human BMP-2 gene into autologous bone marrow stromal cells (MSC). We have successfully repaired large, full thickness, cranial defects using this approach. We report now the effectiveness of various hydrogels as the scaffold for this type of bone regeneration, comparing specifically alginate with Type I collagen. Cultured MSC of miniature swine were infected with BMP-2 or beta-gal adenovirus 7 days before implantation. These cells were mixed with alginate, ultrapure alginate, alginate-RGD, or type I collagen to fabricate the MSC/biomaterial constructs. The results of cranial bone regeneration were assessed by gross examination, histology, 3D CT, and biomechanical tests at 6 weeks and 3 months after implantation. We found that the BMP-2 MSC/collagen type I construct, but not the beta-gal control, effectively achieved nearly complete repair of the cranial defects. No bone regeneration was observed with the other hydrogels. Biomechanical testing showed that the new bone strength was very close and only slightly inferior to that of normal cranial bone. Controlling for the integration of stem cells and ex vivo gene transfer, the alginate scaffolds has a significant negative impact on the success of the construct. Our study demonstrates better bone regeneration by collagen type I over alginate. This may have therapeutic implications for tissue engineered bone repair
J Biomed Mater Res A. 2010 Feb 22. [Epub ahead of print]
Collagen type I hydrogel allows migration, proliferation, and osteogenic differentiation of rat bone marrow stromal cells.
Hesse E, Hefferan TE, Tarara JE, Haasper C, Meller R, Krettek C, Lu L, Yaszemski MJ.
Department of Trauma Surgery, Hannover Medical School, Hannover D-30625, Germany.
Hydrogels are potentially useful for many purposes in regenerative medicine including drug and growth factor delivery, as single scaffold for bone repair or as a filler of pores of another biomaterial in which host mesenchymal progenitor cells can migrate in and differentiate into matrix-producing osteoblasts. Collagen type I is of special interest as it is a very important and abundant natural matrix component. The purpose of this study was to investigate whether rat bone marrow stromal cells (rBMSCs) are able to adhere to, to survive, to proliferate and to migrate in collagen type I hydrogels and whether they can adopt an osteoblastic fate. rBMSCs were obtained from rat femora and plated on collagen type I hydrogels. Before harvest by day 7, 14, and 21, hydrogels were fluorescently labeled, cryo-cut and analyzed by fluorescent-based and laser scanning confocal microscopy to determine cell proliferation, migration, and viability. Osteogenic differentiation was determined by alkaline phosphatase activity. Collagen type I hydrogels allowed the
attachment of rBMSCs to the hydrogel, their proliferation, and migration towards the inner part of the gel. rBMSCs started to differentiate into osteoblasts as determined by an increase in alkaline phosphatase activity after two weeks in culture. This study therefore suggests that collagen type I hydrogels could be useful for musculoskeletal regenerative therapies
Eur Cell Mater. 2010 Feb 26;19:58-71.
Quantitative ultrasound biomicroscopy for the analysis of healthy and repair cartilage tissue.
Gelse K, Olk A, Eichhorn S, Swoboda B, Schoene M, Raum K.
Department of Orthopaedic Trauma Surgery, University Hospital Erlangen, Krankenhausstr. 12, D-91054 Erlangen, [email protected].
The increasing spectrum of different cartilage repair strategies requires the introduction of adequate non-destructive methods to analyse their outcome in-vivo, i.e. arthroscopically. The validity of non-destructive quantitative ultrasound biomicroscopy (UBM) was investigated in knee joints of five miniature pigs. After 12 weeks, six 5-mm defects, treated with different cartilage repair approaches, provided tissues with different structural qualities. Healthy articular cartilage from each contralateral unoperated knee joint served as a control. The reflected and backscattered ultrasound signals were processed to estimate the integrated reflection coefficient (IRC) and apparent integrated backscatter (AIB) parameters. The cartilage repair tissues were additionally assessed biomechanically by cyclic indentation, histomorphologically and immunohistochemically. UBM allowed high-resolution visualisation of the structure of the joint surface and subchondral bone plate, as well as determination of the cartilage thickness and demonstrated distinct differences between healthy cartilage and the different repair cartilage tissues with significant higher IRC values and a steeper negative slope of the depth-dependent backscatter amplitude AIBslope for healthy cartilage. Multimodal analyses revealed associations between IRC and the indentation stiffness. Furthermore, AIBslope and AIB at the cartilage-bone boundary (AIBdC) were associated with the quality of the repair matrices and the subchondral bone plate, respectively. This ex-vivo pilot study confirms that UBM can provide detailed imaging of articular cartilage and the subchondral bone interface also in repaired cartilage defects, and furthermore, contributes in certain aspects to a basal functional characterization of various forms of cartilage repair tissues. UBM could be further established to be applied arthroscopically in-vivo.
J Reconstr Microsurg. 2010 Feb 25. [Epub ahead of print]
The Vastus Intermedius Periosteal (VIP) Flap: A Novel Flap for Osteoinduction.
Maercks RA, Runyan CM, Jones DC, Taylor JA.
Plastic and Reconstructive Surgery, Hospital General Dr Gea Manuel Gonzalez, Miami, Florida.
Periosteum's role in fracture healing is widely recognized, and its function in bone tissue engineering shows great potential. Here we introduce a novel periosteal free flap to be used as an abundant source of periosteum in the engineering and repair of bone. The descending branch of the lateral femoral circumflex vessels were isolated on 11 fresh human cadavers, preserving perforators to the vastus intermedius muscle. A cuff of vastus intermedius and ~75% of the circumference of the femoral periosteum were harvested from 6 cm proximal to the knee to 8 cm distal to the greater trochanter. Flap pedicle length and periosteal dimensions were measured. The pedicle arteries were injected with radiopaque dye, and radiographs were taken. A musculoperiosteal flap was elevated with visible descending perforators in each case. Mean flap surface area was 128 cm (2) (+/-99-143 cm (2)). Average pedicle length was 8 cm (+/-6-11 cm). Dye injection confirmed that the flaps blood supply was the descending branch of the lateral femoral circumflex artery. This anatomical study confirms the vascular supply of this large musculoperiosteal flap. Future work will test its efficacy as an osteoinductive agent in bone repair and tissue engineering in humans
Am J Sports Med. 2010 Feb 25. [Epub ahead of print]
Autologous Chondrocyte Implantation in Cartilage Lesions of the Knee: Long-term Evaluation With Magnetic Resonance Imaging and Delayed Gadolinium-Enhanced Magnetic Resonance Imaging Technique.
Vasiliadis HS, Danielson B, Ljungberg M, McKeon B, Lindahl A, Peterson L.
Sahlgrenska Academy, University of Gothenburg.
BACKGROUND: Various treatment options are available for articular cartilage lesions, but controversy exists regarding the quality of the repair tissue and the durability of the results posttreatment. Noninvasive techniques are needed for the assessment of the repair tissue. HYPOTHESIS: Magnetic resonance imaging (MRI) with delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) can give valuable information regarding the quality and quantity of the repaired cartilage lesion. STUDY DESIGN: Cohort study; Level of evidence, 3. METHODS: Thirty-six knees in 31 patients were assessed 9 to 18 years after treatment with autologous chondrocyte implantation (ACI). All patients had isolated lesions. The knees were clinically evaluated with the Knee injury and Osteoarthritis Outcome Score and the dGEMRIC technique. The T1 value was measured for 2 regions of interest (ROIs), 1 in the repair tissue area (ROI 1) and 1 in the surrounding cartilage (ROI 2), giving information of the content of proteoglycans. RESULTS: The average T1 value in ROI 1 was 467.5 milliseconds and in ROI 2, 495.3 milliseconds, which yielded no significant difference, thus suggesting comparable levels of proteoglycans in the repair tissue and surrounding cartilage. Intralesional osteophytes were in 64% of the lesions, mainly in younger patients with osteochondritis dissecans lesions or a history of subchondral bone surgeries. Medium or large bone marrow edema was found in 14% of the knees and subchondral cysts, in 39%. There was no correlation between the KOOS and any MRI findings. CONCLUSION: Magnetic resonance imaging with dGEMRIC gives valuable information for the macroscopic appearance and micromolecular quality of the repair tissue after ACI. Nine to 18 years posttreatment, the quality of the repair tissue is similar to the surrounding normal cartilage, although intralesional osteophytes, subchondral cysts, and bone marrow edema were common. The defect area is restored in most patients. However, there was no correlation between the dGEMRIC values and the KOOS outcomes.
Osteoarthritis Cartilage. 2010 Feb 6. [Epub ahead of print]
Donor sex and age influence the chondrogenic potential of human femoral bone marrow stem cells.
Payne KA, Didiano DM, Chu CR.
Cartilage Restoration Center, Department of Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA, USA.
OBJECTIVE: Damaged articular cartilage does not heal well and can progress to osteoarthritis (OA). Human bone marrow stem cells (BMC) are promising cells for articular cartilage repair, yet age- and sex-related differences in their chondrogenesis have not been clearly identified. The purpose of this study is to test whether the chondrogenic potential of human femoral BMC varies based on the sex and/or age of the donor. DESIGN: BMC were isolated from 21 males (16-82y.o.) and 20 females (20-77y.o.) during orthopaedic procedures. Cumulative population doubling (CPD) was measured and chondrogenesis was evaluated by standard pellet culture assay in the presence or absence of TGFbeta1. Pellet area was measured, and chondrogenic differentiation was determined by Toluidine blue and Safranin O-Fast green histological grading using the Bern score and by glycosaminoglycan (GAG) content. RESULTS: No difference in CPD was observed due to donor sex or age. The increase in pellet area with addition of TGFbeta1 and the Bern score significantly decreased with increasing donor age in male BMC, but not in female BMC. A significant reduction in GAG content per pellet was also observed with increasing donor age in male BMC. This was not observed in female BMC. CONCLUSIONS: This study showed an age-related decline in chondroid differentiation with TGFbeta1 stimulation in male BMC, but not in female BMC. Understanding the mechanisms for these differences will contribute to improved clinical use of autologous BMC for articular cartilage repair, and may lead to the development of customized age- or sex-based treatments to delay or prevent the onset of OA
J Bone Joint Surg Br. 2010 Feb;92(2):267-72.
Management of combined nonunion and limb-length discrepancy after vascularised fibular grafting.
Abdel-Ghani H, Ebeid W, El-Barbary H.
Department of Orthopaedics University of Cairo, Giza 12511, Egypt. [email protected]
We describe the management of nonunion combined with limb-length discrepancy following vascularised fibular grafting for the reconstruction of long-bone defects in the lower limb after resection of a tumour in skeletally immature patients. We operated on nine patients with a mean age of 13.1 years (10.5 to 14.5) who presented with a mean limb-length discrepancy of 7 cm (4 to 9) and nonunion at one end of a vascularised fibular graft, which had been performed previously, to reconstruct a bone defect after resection of an osteosarcoma. Reconstruction was carried out using a ring fixator secured with correction by half pins of any malalignment, compression of the site of nonunion and lengthening through a metaphyseal parafocal osteotomy without bone grafting. The expected limb-length discrepancy at maturity was calculated using the arithmetic method. Solid union and the intended leg length were achieved in all the patients. Excessive scarring and the distorted anatomy from previous surgery in these patients required other procedures to be performed with minimal exposures and dissection in order to avoid further compromise to the vascularity of the graft or
damage to neurovascular structures. The methods which we chose were simple and effective in addressing these complex problems.
J Bone Joint Surg Br. 2010 Feb;92(2):224-9.
Free vascularised iliac bone graft for recalcitrant avascular nonunion of the scaphoid.
Arora R, Lutz M, Zimmermann R, Krappinger D, Niederwanger C, Gabl M.
Department of Trauma Surgery Medical University Innsbruck, Anichstrasse 35, A-6020 Innsbruck, Tyrol, Austria. [email protected]
We report the use of a free vascularised iliac bone graft in the treatment of 21 patients (19 men and 2 women) with an avascular nonunion of the scaphoid in which conventional bone grafting had previously failed. The mean age of the patients was 32 years (23 to 46) and the dominant wrist was affected in 14. The mean interval from fracture to the vascularised bone grafting was 39 months (9 to 62). Pre-operative MRI showed no contrast enhancement in the proximal fragment in any patient. Fracture union was assessed radiologically or with CT scans if the radiological appearances were inconclusive. At a mean follow-up of 5.6 years (2 to 11) union was obtained in 16 patients. The remaining five patients with a persistent nonunion continued to experience pain, reduced grip strength and limited range of wrist movement. In the successfully treated patients the grip strength and range of movement did not recover to match the uninjured side. Prevention of progressive carpal collapse, the absence of donor site morbidity, good subjective results and pain relief, justifies this procedure in the treatment of recalcitrant nonunion of the scaphoid.
Crit Rev Oncol Hematol. 2010 Feb 23. [Epub ahead of print]
Neoplastic stem cells: Current concepts and clinical perspectives.
Schulenburg A, Brämswig K, Herrmann H, Karlic H, Mirkina I, Hubmann R, Laffer S, Marian B, Shehata M, Krepler C, Pehamberger H, Grunt T, Jäger U, Zielinski CC, Valent P.
Bone Marrow Transplantation Unit, Department of Internal Medicine I, Medical University of Vienna, Vienna, Austria; Ludwig Boltzmann Cluster Oncology, Vienna, Austria.
Neoplastic stem cells have initially been characterized in myeloid leukemias where NOD/SCID mouse-repopulating progenitors supposedly reside within a CD34+/Lin- subset of the malignant clone. These progenitors are considered to be self-renewing cells responsible for the in vivo long-term growth of neoplastic cells in leukemic patients. Therefore, these cells represent an attractive target of therapy. In some lymphoid leukemias, NOD/SCID mouse-repopulating cells were also reported to reside within the CD34+/Lin- subfraction of the clone. More recently, several attempts have been made to transfer the cancer stem cell concept to solid tumors and other non-hematopoietic neoplasms. In several of these tumors, the cell surface antigens AC133 (CD133) and CD44 are considered to indicate the potential of a cell to initiate permanent tumor formation in vivo. However, several questions concerning the phenotype, self-renewal capacity, stroma-dependence, and other properties of cancer- or leukemia-initiating cells remain to be solved. The current article provides a summary of our current knowledge on neoplastic (cancer) stem cells, with special emphasis on clinical implications and therapeutic options as well as a discussion about conceptual and technical limitations
J Biomech. 2010 Feb 19. [Epub ahead of print]
Alterations in damage processes in dense cancellous bone following gamma-radiation sterilization.
Dux SJ, Ramsey D, Chu EH, Rimnac CM, Hernandez CJ.
Musculoskeletal Mechanics and Materials Laboratory, Department of Mechanical and Aerospace Engineering, Case Western Reserve University, Cleveland, 10900 Euclid Ave, Cleveland, OH 44106, OH, Glennan 615A, USA.
Structurally intact cancellous bone allograft is an attractive tissue form because its high porosity can provide space for delivery of osteogenic factors and also allows for more rapid and complete in-growth of host tissues. Gamma radiation sterilization is commonly used in cancellous bone allograft to prevent disease transmission. Commonly used doses of gamma radiation sterilization (25-35kGy) have been shown to modify cortical bone post-yield properties and crack propagation but have not been associated with changes in cancellous bone material properties. The purpose of this
study was to determine the effects of irradiation on the elastic and yield properties and microscopic tissue damage processes in dense cancellous bone. Cancellous bone specimens (13 control, 14 irradiated to 30kGy) from bovine proximal tibiae were tested in compression to 1.3% apparent strain and examined for microscopic tissue damage. The yield strain in irradiated specimens (0.93+/-0.11%, mean+/-SD) did not differ from that in control specimens (0.90+/-0.11%, p=0.44). No differences in elastic modulus were observed between groups after accounting for differences in bone volume fraction. However, irradiated specimens showed greater residual strain (p=0.01), increased number of microfractures (p=0.02), and reduced amounts of cross-hatching type damage (p<0.01). Although gamma radiation sterilization at commonly used dosing (30kGy) does not modify elastic or yield properties of dense cancellous bone, it does cause modifications in damage processes, resulting in increased permanent deformation following isolated overloading.
J Bone Joint Surg Br. 2010 Feb;92(2):298-303.
Lack of a central role for osteoprogenitor cells from the femoral canal in heterotopic ossification of the hip: an experimental study in a rat model.
Toom A, Suutre S, Märtson A, Haviko T, Selstam G, Arend A.
Department of Traumatology and Orthopaedics University of Tartu, Puusepa 8, Tartu 51014, Estonia. [email protected]
We have developed an animal model to examine the formation of heterotopic ossification using standardised muscular damage and implantation of a beta-tricalcium phosphate block into a hip capsulotomy wound in Wistar rats. The aim was to investigate how cells originating from drilled femoral canals and damaged muscles influence the formation of heterotopic bone. The femoral canal was either drilled or left untouched and a tricalcium phosphate block, immersed either in saline or a rhBMP-2 solution, was implanted. These implants were removed at three and 21 days after the operation and examined histologically, histomorphometrically and immunohistochemically. Bone formation was seen in all implants in rhBMP-2-immersed, whereas in those immersed in saline the process was minimal, irrespective of drilling of the femoral canals. Bone mineralisation was somewhat greater in the absence of drilling with a mean mineralised volume to mean total volume of 18.2% (sd 4.5) versus 12.7% (sd 2.9, p < 0.019), respectively. Our findings suggest that osteoinductive signalling is an early event in the formation of ectopic bone. If applicable to man the results indicate that careful tissue handling is more important than the prevention of the dissemination of bone cells in order to avoid heterotopic ossification.
Adv Biochem Eng Biotechnol. 2010 Feb 18. [Epub ahead of print]
Outgrowth Endothelial Cells: Sources, Characteristics and Potential Applications in Tissue Engineering and Regenerative Medicine.
Fuchs S, Dohle E, Kolbe M, Kirkpatrick CJ.
Institute of Pathology, Universitätsmedizin der Johannes Gutenberg-Universität, Langenbeckstrasse 1, Mainz, Germany, [email protected].
Endothelial progenitor cells from peripheral blood or cord blood are attracting increasing interest as a potential cell source for cellular therapies aiming to enhance the neovascularization of tissue engineered constructs or ischemic tissues. The present review focus on a specific population contained in endothelial progenitor cell cultures designated as outgrowth endothelial cells (OEC) or endothelial colony forming cells from peripheral blood or cord blood. Special attention will be paid to what is currently known in terms of the origin and the cell biological or functional characteristics of OEC. Furthermore, we will discuss current concepts, how OEC might be integrated in complex tissue engineered constructs based on biomaterial or co-cultures, with special emphasis on their potential application in bone tissue engineering and related vascularization strategies.
Proc Natl Acad Sci U S A. 2010 Feb 23;107(8):3305-10. Epub 2010 Jan 19.
Regenerative Medicine Special Feature: Human stem cell delivery for treatment of large segmental bone defects.
Dupont KM, Sharma K, Stevens HY, Boerckel JD, García AJ, Guldberg RE.
George W. Woodruff School of Mechanical Engineering, Georgia Institute of Technology, Atlanta, GA 30332-0405.
Local or systemic stem cell delivery has the potential to promote repair of a variety of damaged or degenerated tissues. Although various stem cell sources have been investigated for bone repair, few comparative reports exist, and cellular distribution and viability postimplantation remain key issues. In this study, we quantified the ability of tissue-engineered constructs containing either human fetal or adult stem cells to enhance functional repair of nude rat critically sized femoral defects. After 12 weeks, defects treated with cell-seeded polymer scaffolds had significantly higher bone ingrowth and torsional strength compared to those receiving acellular scaffolds, although there were no significant differences between the cell sources. Next, stem cells were labeled with fluorescent quantum dots (QDs) in an attempt to noninvasively track their distribution after delivery on scaffolds. Clear fluorescence was observed at implantation sites throughout the study; however, beginning 7-10 days after surgery, signals were also observed at contralateral sites treated with acellular QD-free scaffolds. Although immunostaining for human nuclei revealed retention of some cells at the implantation site, no human cells were detected in the control limb defects. Additional histological analysis of implantation and control defect tissues revealed macrophages containing endocytosed QDs. Furthermore, QD-labeling appeared to diminish transplanted cell function resulting in reduced healing responses. In summary, augmentation of polymeric scaffolds with stem cells derived from fetal and adult tissues significantly enhanced healing of large segmental bone defects; however, QD labeling of stem cells eliminated the observed therapeutic effect and failed to conclusively track stem cell location long-term in vivo
Stem Cell Rev. 2010 Feb 26. [Epub ahead of print]
Laser-Assisted Photoablation of Human Pluripotent Stem Cells from Differentiating Cultures.
Terstegge S, Winter F, Rath BH, Laufenberg I, Schwarz C, Leinhaas A, Levold F, Dolf A, Haupt S, Koch P, Endl E, Brüstle O.
Institute of Reconstructive Neurobiology, Life & Brain Center, University of Bonn and Hertie Foundation, Sigmund-Freud-Str. 25, 53105, Bonn, Germany.
Due to their pluripotency and their self-renewal capacity, human pluripotent stem cells (hPSC) provide fascinating perspectives for biomedical applications. In the long term, hPSC-derived tissue-specific cells will constitute an important source for cell replacement therapies in non-regenerative organs. These therapeutic approaches, however, will critically depend on the purity of the in vitro differentiated cell populations. In particular, remaining undifferentiated hPSC in a transplant can induce teratoma formation. In order to address this challenge, we have developed a laser-based method for the ablation of hPSC from differentiating cell cultures. Specific antibodies were directed against the hPSC surface markers tumor related antigen (Tra)-1-60 and Tra-1-81. These antibodies, in turn, were targeted with nanogold particles. Subsequent laser exposure resulted in a 98,9 +/- 0,9% elimination of hPSCs within undifferentiated cell cultures. In order to study potential side effects of laser ablation on cells negative for Tra-1-60 and Tra-1-81, hPSC were mixed with GFP-positive hPSC-derived neural precursors (hESCNP) prior to ablation. These studies showed efficient elimination of hPSC while co-treated hESCNP maintained their normal proliferation and differentiation potential. In vivo transplantation of treated and untreated mixed hPSC/hESCNP cultures revealed that laser ablation can dramatically reduce the risk of teratoma formation. Laser-assisted photothermolysis thus represents a novel contact-free method for the efficient elimination of hPSC from in vitro differentiated hPSC-derived somatic cell populations.