Areas of Coverage: - ReliefWeb
-
Upload
khangminh22 -
Category
Documents
-
view
0 -
download
0
Transcript of Areas of Coverage: - ReliefWeb
NUTRITION AND MORTALITY SURVEY1
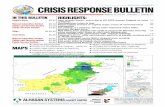
Areas of Coverage: Tieraliet, Ayai, Wathmouk, Gakrol, Panthou Payams
Aweil South County Northern Bahr el Ghazal State
South Sudan
March 2006
1 Cyprian ouma Mercy khamala Nutrition Sector ( Tearfund DMT South Sudan)
Page 2 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
2
Acknowledgements To the community of Aweil South who sacrificed their time to attend to the survey teams and who at no cost allowed as to ask them many questions while at the same time sample their young children . And to the following persons whose support, endurance and dedication made this undertaking to reach this stage: Patrick Barasa, Loice mukabane, fidelis emodo,mercy khamala, Amon Njogu, Peter Akol Angok, William Wol Kuol, Daniel Atem, James Akol Garang, Phillip Garang, Andrew Ajing, Adeng Mel Adeng, Luka Ngor Wiew, James Chour Loch, Bona Majok Ayany, Luka Akot Lual, Angelo Garang, Bhona Malual, Paul Dut Mel, James Lual Baak, Luka Deng, Peter Kuek Atak, Samuel Bol Deng, Santino Kuac Mawien, Marko Manut, Arkanjelo Ajal, Moses Yel Mangok, Joseph Wol Ajang, Santino Bol Garang, Thomas Wek Mawien, Santino Madhieu, Daniel Mayom Mel, John Akot Lual, Gabriel Garang.
Page 3 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
3
LIST OF ABBREVIATIONS
BCG Bacilli Conte Guallo BEG Bahr el Ghazel. CI Confidence Interval CMR Crude mortality rate EPI Expanded Program on Immunisation GAM Global Acute Malnutrition (<-2 Z-scores W/H +/- oedema) GoS Government of Sudan HH Household LRTI Lower Respiratory Tract Infections MSF Medicines sans Frontiers NCHS National Centre for Health Statistics NGO Non Governmental Organisation PHCU Primary Health Care Unit PPS Probability Proportional to Size SAM Severe Acute Malnutrition (<-3 Z-scores W/H +/- oedema) SPLA Sudan peoples liberation army SRRC Sudan relief and rehabilitation committee SFP / C Supplementary Feeding Programme / Centre SINGOs Sudanese Indigenous Non Governmental Organisations TFP / C Therapeutic Feeding Programme / Centre UNICEF United Nations Children’s Fund U5MR Under five mortality rate WFP World Food Programme WfH Weight for Height or Length WHO World Health Organization
Page 4 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
4
EXECUTIVE SUMMARY Due to a prediction in 2005 of the high prospects of a precarious food situation in 2006 in the county facilitated by massive flooding that destroyed large crop fields coupled with the expected exacerbation of the situation through a strain of most household food baskets and other household livelihoods because of high number of returnees, Tearfund as a lead nutrition agency in Aweil South county undertook a nutrition survey in March 2006 with the objective of assessing the current nutritional status of the population and get information that will be used to assist and guide the planning and implementation of the nutrition program and as well provide reference baseline data . The survey covered Tieralliet, Panthou, Gakrol, ajak and Wathmouk payams.The target population of 37,596 children was based on a total population of 187,980 (WHO NIDS 2004) for the 5 Payams surveyed and calculated using a 20% multiplier. The methodology employed was a two-stage cluster-sampling frame of 30 clusters each with 30 children which is appropriate for this context. Data collection was carried out using a standardized questionnaire. The Target group was Children 06-59 months (height 65cm ---- 110 cm.).In total 946 children were sampled. Data quality assurance included the use of an anthropometric standardization and cluster control sheet, thorough enumerator training, close expert supervision during the actual survey for consistency, completeness and clarity of the questionnaires ensured that data collected was of good quality. Common historical events listed in the seasonal calendar like floods, important and memorable persons, fighting were used to clarify the dates of childbirth in cases where the mother or other caretakers were not certain about the information. Data processing, validation and analysis were conducted using Epi Info version 5 and 6.04c software packages2. Anthropometric results indicate that the Global Acute Malnutrition and/ or oedema (GAM), <-2.00 SD Z-score, is 20.0% (95% CI 16.5-24.1). Severe Acute Malnutrition and/ or oedema (SAM), <-3.00 SD Z-score, is 3.7% (95% CI 2.2-6.0). No cases of nutritional oedema have been reported. Further, currently 6128 children are in need of supplementary feeding and 1392 require therapeutic feeding to curb on associated mortality3. Conclusion The prevalence of 20.0% global acute malnutrition is critical and this is further complicated by returnees, lack of good and safe water, poor hygiene, inadequate health care, poor shelter and in some instances inappropriate feeding practises . Prompt response is therefore mandatory to control the current high levels of malnutrition .These should strive to cover the traditional hunger periods that stretch between April proceeding until it links up with the first harvest in October.
2 EPI Info version 6.04c October 1997 (Y2K compliant), centres for disease control, epidemiology program office, Atlanta, Georgia, USA WHO global
program on AIDS, Geneva, Switzerland. 3 Approximation has been done to provide working figures only and inform programme planning. The Z score rather than the percent median (though
used as admission criteria) has been used to increase on the sensitivity of absolute estimation.
Page 5 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
5
TABLE OF RESULTS
Acute malnutrition prevalence as estimated by mid upper arm circumference CLMUAC | Freq Percent
A. M<11.0 Severe malnutrition 2 0.3% B. 11.0<=M<12.5 Moderate malnutrition | 48 6.0% C. 12.5<=M<13.5 At risk | 178 22.3% D. M>=13.5 Normal | 569 71.4%
Total | 797 100.0% Meal frequency in the past 7 days for under fives
Meal frequency Frequency Percent 95% ci
proportion consuming 1 meal/day N;213 22.7% 20.1---25.5 proportion consuming 2 meal/day N;675 71.9% 68.9---74.7
proportion consuming 3 meals/day N;51 5.4% 4.1---7.1 Total 939 100.0%
♠ All results expressed at 95% confidence interval
AGE GROUP EXPRESSION INDICATOR RESULT♠♠♠♠
Global Acute Malnutrition <-2z score and/or oedema
20.0 % (16.3 - 23.7 ) Z-score
Severe Acute Malnutrition<-3zscore and/or oedema
3.7 % (1.6 - 5.8)
Global Acute Malnutrition <80% and/or oedema
12.1 %(9.3 - 15.6)
6-59 N = 939
% Median
Severe Acute Malnutrition <70% and/or oedema
2.2 %(1.1 – 4.2 )
Global Acute Malnutrition<-2z score and/or oedema
22.4 %( 17.0---29.0) Z-score
Severe Acute Malnutrition<-3 z score and/or oedema
3.7 %( 1.6---7.6)
Global Acute Malnutrition <80% and/or oedema
14.1 %( 9.7---20)
Acute Malnutrition (Weight/ Height)
6-29 N=410
% Median
Severe Acute Malnutrition <70% and/or oedema
2.7 %( 1.0---6.3)
Chronic malnutrition Weight/age
underweight <-2 Z score 18.5 % (15.0---22.0)
0-5 years mortality rate 0.69 deaths/10,000/day (0.03---1.35)
Retrospective mortality
Crude mortality rate 0.26 deaths/10,000/day (0.08---0.43)
Bilateral oedema 0.0%
Page 6 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
6
Measles vaccination coverage
MEASLES Frequency Percent 95% ci
measles vaccination status as revealed by card
N;66 7.0% 5.5---8.9
measles vaccination status as revealed by mother/caretaker
N;266 28.4% 25.5---31.3
not vaccinated N;607 64.6% 61.5---67.7
Total N;939 100.0%
Vitamin A supplementation coverage
Vitamin A supplementation Frequency Percent 95% ci
proportion of sample who have received micronutrient vitamin A
N;563 60.0% 56.7---63.1
proportion of sample who have NOT received micronutrient vitamin A
N;376 40.0% 36.8---43.2
Total 939 100.0%
BCG vaccination coverage
BCG SCAR Frequency Percent 95% ci
under five BCG vaccination status as revealed by scar
N;204 21.7% 19.2---24.5
not vaccinated N;735 78.3% 75.1---80.5
Total 939 100.0%
Morbidity
ILLNESS Frequency Percent 95% ci
ill in last 2 weeks 115 N;12.2% 9.4---13.5 NOT ill 824 N;87.8% 85.4---89.7 Total 939 100.0%
Aweil South county malnutrition trends
0.00%
5.00%
10.00%
15.00%
20.00%
25.00%
Percent prevalence
GAM SAM
GAM 21.90% 17.80% 21.10% 22.60% 16.20% 13.20% 15.20% 20.50% 14.00% 20.00%
SAM 3.10% 1.40% 3.70% 3.10% 1.40% 1.80% 1.00% 3.40% 1.80% 3.70%
2003 2003 2004 2004 2005 Aug' 2001 Feb'2002 Nov'2002 Feb Nov Feb Nov March nov'2005 mar'2006
Page 7 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
7
MAIN FINDINGS
Anthropometric results indicate that the Global Acute Malnutrition and/ or oedema (GAM), <-2.00 SD Z-score, is 20.0% (95% CI 16.5-24.1). Severe Acute Malnutrition and/ or oedema (SAM), <-3.00 SD Z-score, is 3.7% (95% CI 2.2-6.0). No cases of nutritional oedema have been reported.
Currently 6128 children are in need of supplementary feeding and 1392 require therapeutic feeding to curb on associated mortality4.
Severe acute malnutrition is affecting more girls than boys.63% of the girls are severely malnourished compared to 37% of the boys.
Measures of exposure effect at [95% CI] for the age group 6-29 months and 30-59 indicate that the rates of malnutrition are not significantly different between the two groups with P value of >0.055. The relative Risk ratio6 is 1.24 [0.96<RR< 1.60]. the uncorrected chi squares is 2.66 These means that children aged less than 30 months are 1.24 times more likely to be malnourished compared to those above 30 months.
Vitamin A (retinol) which is an essential nutrient needed in small amounts by humans for the normal functioning of the visual system; growth and development; and maintenance of epithelial cellular integrity, immune function, and reproduction is still having a low coverage in the county. 60% of the sample has accessed the micronutrient .Vitamin A deficiency is a disabling and potentially fatal public health problem for children under 6 years of age. VAD-related blindness is most prevalent in children under 3 years of age hence the need for enhanced supplementation.
The frequency of under five meal consumption is poor .More than 94.6% consume less than 2 meals which is inadequate and reduces the intake of nutrients.
Malnutrition among those aged 6-29 months remains critical with 22.4% being malnourished. However it’s not significantly different from rates of children 06-59 months. The higher prevalence at the younger age group indicates the increased vulnerability during the weaning period as appropriate complementary foods might not be available. 3.7% are severely malnourished and at risk to mortality.
Analytical tests reveal that boys are at higher risk of being malnourished than girls (risk ratio, adjusted for clustered sampling is 1.15 (C.I. 0.89 <RR< 1.49). They are 1.15 times more likely to be malnourished than girls. The difference is not significant with P=0. 27 The WHZ distribution compared to the international reference population showed a significant displacement of the distribution to the left of the reference indicating poor nourishment.
The 0—5 year’s mortality rate was found to be 0.69deaths/10,000/7day and 0.26deaths/10,000/day for crude mortality rate .These is below the emergency and alert levels and is acceptable.
The population of Aweil south has a near normal structure. The boy to girl ratio is 0.908 i.e. 456/483.
The Waterlow classification indicated no presence of Marasmic-kwashiorkor. This classification is particularly useful to identify the number of Marasmic-kwashiorkor cases who are at an increased risk of death for immediate case management.
4 Estimation has bee done to provide working figures only and inform programme planning. The Z score rather than the percent median (though used as admission criteria) has been used to increase on the sensitivity of absolute approximation. 5 P corresponds to the statistical significance of the test. It’s the probability that an event occurs. 6 The risk ratio corresponds to the added risk of malnutrition. When RR is 1.0, no association is likely. 8 The sex ratio should be one in a normal structure ( a value between 0.84 and 1.20 is acceptable)
Page 8 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
8
Measles immunization coverage is low among children aged 6-59 months with an estimated 35.4%. BCG coverage was 21.7 %. Health facilities should use every opportunity to cover the vaccination needs of each child and active community mobilisation and sensitisation could be envisaged.
OBSERVATIONS AND DISCUSSIONS
Some houses are still submerged in the after effects of last years floods. Most households have diverted resources that could have been used for food needs to secure materials for new shelter constructions.
Many pools of stagnant water are all over and have continued to be a source of bad water and also rich breeding grounds for malarial mosquitoes.PHCUs are reportedly seeing more positive malaria cases which will worsen with the onset of the rains from June.
Fishing, an activity that traditionally follows every flooding season and which is usually expected to provide broth to households and more so meets the protein needs of children has been hampered by lack of fishing tools and the alteration in feeding pattern caused by lack of sorghum (dura) which is a popular and preferred accompaniment for fish broth. These have been so due to massive flood destructions of sorghum tracts in the lowland fishing and cropping food economy zone.
The grain barns that were seemingly full of grains in November 2005 are currently empty of grain with some households pulling them down for repairs for the next harvest 5-6 months away.
Page 9 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
9
RECOMMENDATIONS
Continue the supplementary and therapeutic feeding programme to link with the next harvest monitoring the situation closely to inform project phase out.
Decentralise the feeding centres by opening others in poorly accessible areas namely ajak, wuncum and malek Alel which were worst hit by the floods and where most of the malnourished children are suspected to have originated. Strategy should ensure that nutritional inputs are prepositioned before the rains.
Optimise active case finding through accelerated mobilization ,community leaders and utilise the village screening technique to identify malnourished children for admission
Assess and improve knowledge, attitudes and skills of feeding and caring practices of mothers and further strengthen the collaboration in hygiene promotion and health education.
Integrate nutrition intervention ,micronutrient supplementation and immunization .Activities as major component of health facilities, including growth monitoring and promotion;
TEARFUND to take the lead and advocate on behalf of the community for more projects and funds to address the underlying factors to malnutrition including but not limited to good water,health,hygiene,food and education.
Continued food distribution until the harvest in October.
Strengthen the food security strategies by widening the crop varieties e.g. promoting other cereals like maize, beans, millet etc in the County.
Promote improved access to safe water in the county and treat all un-protected water sources including protecting all open wells.
Conduct an in-depth assessment to estimate the impact of the current returnee needs and the extent of the strain on the livelihoods of the hosting community.
Page 10 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
10
TABLE OF CONTENTS Executive Summary.............................................................................................................................................. 4 Table Of Results ................................................................................................................................................... 5 Observations And Focus Group Disccussions................................................................................................. 8 Recommendations................................................................................................................................................ 9 1.0 Background................................................................................................................................................... 11
Description Of The Survey Area ................................................................................................................ 11 1.1 SURVEY OBJECTIVES...................................................................................................................................... 11
1.2 SURVEY LIMITATIONS..................................................................................................................................... 12
2.0 Survey Methodology .................................................................................................................................... 12 2.1.1 Sampling ............................................................................................................................................. 12 2.1.2 Selection Of Households And Children ........................................................................................... 12 2.1.3 Indicators, Guidelines And Formulas Used: ................................................................................... 12
MID-UPPER ARM CIRCUMFERENCE (MUAC)....................................................................................................... 13
2.1.6 Implementation Of Survey Activities .......................................................................................... 13 2.1.7 Data Collection ................................................................................................................................... 14 2.1.8 Mortality............................................................................................................................................... 14 2.1.9 Data Quality Control And Assurance ............................................................................................... 15 2.1.10 Data Processing, Validation And Analysis .................................................................................... 15
3.0 Survey Findings............................................................................................................................................ 16 3.1 DISTRIBUTION OF MALNUTRITION IN Z-SCORE ............................................................................................ 18
3.2 WEIGHT/HEIGHT INDEX VS. OEDEMA ........................................................................................................... 18
3.3 GLOBAL, MODERATE, AND SEVERE ACUTE MALNUTRITION BY GENDER IN Z-SCORE ................................. 18
3.4 ACUTE MALNUTRITION BY AGE CATEGORY................................................................................................... 19
3.5 DISTRIBUTION OF MALNUTRITION IN PERCENTAGE OF THE MEDIAN ......................................................... 19
3.6 PREVALENCE OF MALNUTRITION BY AGE, BASED ON WEIGHT-FOR-HEIGHT MEDIAN AND OEDEMA ....... 19
3.7 WEIGHT FOR HEIGHT VS. OEDEMA............................................................................................................... 19
3.8 PREVALENCE OF ACUTE MALNUTRITION BASED ON THE PERCENTAGE OF THE MEDIAN AND/OR OEDEMA19
3.9 MORTALITY RISK: MID UPPER ARM CIRCUMFERENCE ................................................................................. 20 3.9.1 Muac Distribution According To Nutritional Status ......................................................................................... 20
4.0 Measles Vaccination Coverage..................................................................................................................................... 20 5.0 Morbidity ......................................................................................................................................................................... 20 6.0 Meal Frequency In The Past 7 Days For Under Fives ................................................................................................. 21 7.0 BCG Vaccination Coverage........................................................................................................................................... 21 8.0 Vitamin A Supplementation Coverage ......................................................................................................................... 21 9.0 Residential Status ......................................................................................................................................................... 22 10.0 Discussion .................................................................................................................................................................... 22 11.0 Recommendations ....................................................................................................................................................... 24
Page 11 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
11
1.0 BACKGROUND
Description of the survey area
Aweil South County is made up of six Payams (namely Wathmouk, Gakrol, Tieraliet, Ayai, Panthou and Makuei Alel)9. The new proposal would increase the number of payams from 3 to 6 payams. The baseline assessment was conducted within all the newly proposed Payams.
The topography of the area is characterized by higher lying areas (known locally as gok) and lower lying areas (known locally as toic). The toic areas are rich in fish and provide grazing pastures in the dry season and have clay type of soil. The higher lying grounds may have sandy soil texture (as in Tieraliet) or rocky soil texture as in (Malek Alel). These inter-payam variations in agro-ecological characteristics create some conspicuous micro-level variations in livelihood economy at the county level. Wathmouk payam has a significant part of its territory lying in the lowland flood plains and is considered a fishing & cropping food economy zone. The major crops being produced are sorghum, sesame, and small quantity of groundnuts. The grain yield per household is determined by socio-economic status of the family, soil fertility, and topography and rainfall conditions. The peak of the rainy season is between August and September. The annual flood, expected around September of previous years was quite last year. Reports and observations show that there has been a negative impact due to the intensity of the flooding. The inhabitants of the area are agro-pastoralist. The system of farming is subsistence based rain fed agriculture with farming operations being done near the homesteads. Soil fertility is improved and maintained by addition of animal droppings. The farmers practice a mixed cropping system with the main staple crops being sorghum, sesame and groundnuts. Rice has been re-introduced recently after disruption during the period of conflict. Out of all the traditional crops being grown, sorghum is the most preferred variety because it has a high level of drought tolerance, low seeding rate and high seed-to-grain multiplication ratio. This makes it a favourite traditional crop of the area and popular for home consumptions, besides its added value in terms of palatability, ease of processing and storage. However appropriate agricultural technologies that can lead to increased household food production are still lacking. The recent cessation of hostilities between the warring parties in the conflict for the past two year has made it possible for people to move across frontlines, resulting in an influx of returnees into Aweil County. The major registration points of the returnees upon entry into the county are Ayai (Ajak), Malek Alel, Tieraliet and Panthou. A nutrition survey conducted in March/April 2005 to assess the trends in malnutrition due to reportedly poor harvest occasioned by late and erratic rains in 2004 indicated that 20.5% of children 6-59 months were suffering from global acute malnutrition according to the weight-for-height index in z-scores (WHZ) and 3.4% were suffering from severe acute malnutrition. A nutrition programme was hence opened to contain the situation and in November 2005, the level of global acute malnutrition had dropped to 14.0%.
1.1 Survey objectives
To check on the current nutritional status of children between 6 to 59 months. To estimate crude and under five mortality rate. To evaluate the measles, BCG and vitamin A coverage. To provide information and data that can be used to guide programme implementation.
9 The old Payams were Mangargier, Gakrol and Wathmouk. In the new proposal Mangargier has been divided to Tieraliet Payam and Panthou Payam. Wathmouk is divided into Wathmouk Payam and Ayai Payam; and Gakrol into Gakrol Payam and Makuei Alel Payam. However descriptions throughout this document are still based on the old Payams of Panthou, Gakrol and Wathmouk for convenience.
Page 12 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
12
1.2 Survey limitations
Mechanical constraints on the vehicles due to the rough terrain in the area. Some of the survey areas-like Ajak, were inaccessible by road, this increased travel times and resources to ensure they were assessed.
Absence of respondents in some clusters during the survey implementation. This is due to the fact that they were attending a food distribution exercise in the county headquarters.
2.0 SURVEY METHODOLOGY (Type of survey and sample size) At the time of the survey, the total population in county was 187,98010with an under five population of 37,596(Estimated with a multiplier of 20% of the total population). The smallest administrative unit was considered to be a village. A 30 x 3011WHO- EPI cluster sampling methodology was used.
2.1.1 Sampling
The target populations in the survey were children aged 6 to 59 months with a height of 65-110cm. The availability of population figures at village level enabled systematic random selection of clusters to be done according to villages by using the probability proportional to size (PPS). All randomly selected villages, constituted the first sampling unit
2.1.2 Selection of Households and Children
In the second degree of sampling, selection of the families was done in the selected clusters at the respective households. The team went to the centre of the chosen cluster and randomly determined a direction by spinning a pen. Random numbers generated using Epi Info 6.04c were used in the selection of the first household to be sampled. The remaining households were chosen by proximity, always taking the second houses on the right hand side. Where more than one family (caretaker), resided in a homestead (a family was defined as people represented by one caretaker and share a ‘cooking pot’), the residential status of the households was first established. If the families were residents’ only one family (caretaker) was randomly selected by casting lots. For each selected family (caretaker), all children aged from 6 to 59 months, with a height between 65 and 110cm were measured. Internally displaced and returnee families residing with the residents were assessed as separate households.
2.1.3 Indicators, guidelines and formulas used:
Acute Malnutrition (Weight-for-Height Index) For the children, acute malnutrition rates were estimated from the weight for height (W/H) index values combined with the presence of oedema. The W/H indices are compared with the national centre for health statistics (NCHS)12 references. W/H indices were expressed both in Z-scores and in percentage of the median. The expression in Z score has true statistical meaning; it expresses malnutrition rates more precisely and allows inter survey comparison. The percentage of the median estimates weight deficits more accurately and is used for admission in feeding programmes. Guidelines for the results expressed in Z-score:
� Severe malnutrition is defined by WFH < -3 SD and/or existing bilateral oedema on the lower limbs of the child
� Moderate malnutrition is defined by WFH < -2 SD and >= -3 SD and no oedema. � Global acute malnutrition is defined by WFH < -2 SD and/or existing bilateral oedema
Guidelines for the results expressed in percentage according to the median of reference:
10 Source: Starbase and OCHA database.
11 The minimum sample size, which allows a reasonable precision of the prevalence of malnutrition (whatever the prevalence) is at least
900 children aged 6 to 59 months (30 clusters of 30 children each), when the target population is greater or equal to 5,000 in size. In this case 930 children constituted the final sample size. 12 NCHS: National Centre for Health Statistics (1977) NCHS
Page 13 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
13
� Severe malnutrition is defined by WFH < 70 % and/or oedema on the lower limbs � Moderate malnutrition is defined by WFH < 80 % and >= 70 % and no oedema. � Global acute malnutrition is therefore defined as the proportion of children presenting with a
weight for height index < –2 z scores (or < 80% in the percent median) with/without oedema.
Classification of the severity of acute malnutrition (WHO 200013)
Indicator of acute malnutrition Classification
Global acute malnutrition (GAM) prevalence of ≥15% Critical
GAM prevalence of 10-14% Serious
GAM prevalence of 5-9% Poor
GAM prevalence of <5% Normal
Chronic Malnutrition Underweight: Underweight, based on weight-for-age, is a composite measure of stunting and wasting and is recommended as the indicator to assess changes in the magnitude of malnutrition over time. Stunting: Low length-for-age, stemming from a slowing in the growth of the fetus and the child and resulting in a failure to achieve expected length as compared to a healthy, well nourished child of the same age, is a sign of stunting. Stunting is an indicator of past growth failure. It is associated with a number of long-term factors including chronic insufficient protein and energy intake, frequent infection, sustained inappropriate feeding practices and poverty. In children over 2 years of age, the effects of these long-term factors may not be reversible. For evaluation purposes, it is preferable to use children under 2 years of age because the prevalence of stunting in children of this age is likely to be more responsive to the impact of interventions than in older children. Data on prevalence of stunting in a community may be used in problem analysis in designing Interventions. Information on stunting for individual children is useful clinically as an aid to diagnosis. Stunting, based on height for-age, can be used for evaluation purposes but is not recommended for monitoring as it does not change in the short term such as 6- 12 months.
Mid-Upper Arm Circumference (MUAC)
Children’s MUAC The weight for height index is the most appropriate index to estimate wasting in a population in emergency situations where acute malnutrition is a predominant deficiency syndrome. Nevertheless, MUAC is a useful tool for rapid screening of children at a higher risk of mortality. MUAC is only taken for children with an age of 1 year or a height of 75 cm and more.
2.1.6 Implementation of survey activities
Training of Enumerators and pre field exercise 6 teams were involved in the survey. A team was designated to carry out the survey in a cluster. Each team was composed of a team leader and two enumerator’s majority of whom had previously done an average of two surveys in the county. Three days training was done and covered aims of the assessment, Survey equipment use and handling, Interview techniques and protocols, anthropometrical measurement techniques, Questionnaire translation, familiarization and recording of answers.
13 WHO (2000) “The Management of Nutrition in Major Emergencies” WHO
Page 14 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
14
On the third day, actual practical session on anthropometrical measurements, interviews and filling out of questionnaires was conducted. The pre-testing was done to define any areas that needed rectification before the field work.
2.1.7 Data Collection
The study units were households with children aged between 06-59 months. Trained enumerators took anthropometrics measurements and administered the questionnaires. The mother and/or other caretaker of the child were the target/index respondent for the survey. Information collected included: Age: recorded with help of a local calendar of events. Sex: recorded as M = male and F = female. Weight: (Salter scale balance of 25 kg, precision of 100g). Children were weighed without cloths. Height: (Shorr measuring board, precision of 0.1 cm). Children less than 85 cm were measured lying down, while those greater than or equal to 85 cm were measured standing up and without shoes. Mid-Upper Arm Circumference: MUAC was measured at mid-point of left upper arm. Bilateral oedema: assessed by the application of normal thumb pressure on both feet. Status: The residential status (whether resident, returnee or displaced) of visited households was assessed in terms of movement into the area within a period less than 6 months prior to the survey. Retrospective mortality: mothers/caretakers were asked how many children under the age of five years alive they had presently and how many, if any, had died in the last 3 months. This question was asked at all households selected, regardless of whether they had children aged between 6 and 59 months (see mortality questionnaire in Appendix). This method may be less accurate in determining the cause of death since this will depend on the recall and diagnosis of the families, thereby introducing recall bias. Nonetheless, since most deaths occurred outside health facilities, this method is probably most reliable for the situation. Meal frequency: The number of times a child was fed in a day was enquired and recorded.
Vitamin A: caretakers were asked if the children being sampled had previously received a dose of vitamin A by being shown a capsule.
Measles and BCG coverage: caretakers were requested to confirm by card or recall if the children had been vaccinated against measles and BCG
2.1.8 Mortality
For all the households sampled (with or without under fives), the survey teams inquired for the number of household members alive and dead per specified age groups. The mortality rate (MR) was determined for both the whole population (CMR) and children (U-5MR) Defined benchmarks:14 U-5MR Alert level: 2/10,000 people/day Emergency level: >4/10,000 people/day CMR Alert level: 1/10,000 people/day Emergency level: >2/10,000 people/day The death rate (DR), FOR U-5s or the whole population, was calculated as follows: If: n= the number of deaths in the last 90days And: N= the number alive the day of the survey Then: DR=n/ (((n+N) + N)/2) The RMR = (DR X 10,000)/number of days in the period. The period corresponds to 90 days preceding the survey. Therefore, RMR = (DR X 10,000)/90. It is expressed per10000 people/day.
14 Refugee And Nutrition Information Systems Benchmarks
Page 15 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
15
Definitions of the presumed causes of the deaths reported used were: Simple diarrhea (S): case definition--- every episode of more than 3 liquid stools per day. Bloody diarrhea (B): case definition---every episode of 3 + liquid stools per day with blood. Measles (M): case definition---every episode of fever associated with coetaneous eruptions with or without conjunctivitis.
Fever (F): case definition----elevated body temperature Lower respiratory infection (R): case definition--- every episode where fever-cough are associated and at least one of the following signs: expectoration chest pain, dyspnoea (shortness of breath), wheezing.
Malnutrition (N): case definition---child with bilateral Oedema/ weight loss Accidental (A); e.g. snake bites, crocodile attacks Others (O): give details: old age, Kala-Azar.
2.1.9 Data quality control and assurance
The use of an anthropometric standardization and a cluster control sheet, thorough enumerator training, close expert supervision during the actual survey for consistency, completeness and clarity of the questionnaires ensured that data collected was of good quality. Common historical events listed in the seasonal calendar like floods, important and memorable persons, fighting were used to clarify the dates of childbirth in cases where the mother or other caretakers were not certain about the information.
2.1.10 Data processing, validation and analysis
Data processing and analysis was conducted using Epi Info version 5 and 6.04c software packages15. Anthropometric indicators were calculated using EpiNut 2.2. Outlying indices were 0.7% and were replaced before further processing of the data. Prevalence rates and 95% confidence intervals were calculated using C-sample16.Comparative statistical analysis was done using EpiCalc 2000 version 1.02 and Asmarc06.PGM.
15 EPI Info version 6.04c October 1997 (Y2K compliant), centres for disease control, epidemiology program office, Atlanta, Georgia, USA
WHO global program on AIDS, Geneva, Switzerland. 16 C-sample is a programme within Epi Info that accounts for the design effect of cluster sampling when calculating confidence intervals for
prevalence rates.
Page 16 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
16
3.0 SURVEY FINDINGS Distribution by age and sex Table 3
Age groups Boys Girls Total Ratio
no. % no. % no. % Boy: girl
6-17 months 90 49.7 91 50.3 181 19.3 1.0
18-29 months 105 45.9 124 54.1 229 24.4 0.8
30-41 months 101 49.3 104 50.7 205 21.8 1.0
42-53 months 69 43.9 88 56.1 157 16.7 0.8
54-59 months 91 54.5 76 45.5 167 17.8 1.2
Total 456 48.6 483 51.4 939 100.0 0.9
The distribution by sex shows imbalance: girls outnumber boys in all age groups except 54—59 months category. However, the total sex ratio of 0.9017 shows that the sample selection was well randomised. In this county, it is extremely rare for mothers/caretakers to know the exact birth-dates of their children in the surveyed community. An events calendar and a traditional annual seasonal county chart were used to assist in the estimation of ages since it was expected that some respondents would suffer from age recall bias. When no age was given by mothers the estimation using height18 was applied. To a large extent the inclusion of children in the sample was based on satisfaction of the height criteria of 65-110cm.
17 Ideal sex ratio is 1.0.however values between 0.84---1.20 is acceptable.
18 UNICEF-OLS guidelines South Sudan- 2001
Distribution by age and sex (March 2006)
-150 -100 -50 0 50 100 150
6-17 months
18-29 months
30-41 months
42-53 months
54-59 months
Boys Girls
Page 17 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
17
Distribution of the age in their various categories does not show a significant imbalance. However, age group 18-29 and 30-41 are presented more than the age groups 42-53, and 6-17 and 54-59. While this could be a real demographic profile in this population, this could have resulted from the same issues noted above. Other reasons include elevated mortality in particular age groups.
Anthropometrical analysis of acute malnutrition
Sample Distribution19
19 Cluster sampling methodologies means that any comparisons of malnutrition levels between individual clusters are not statistically
significant.
Distribution by age --Aweil South (March 2006)
0 50 100 150 200 250
6-17 months
18-29 months
30-41 months
42-53 months
54-59 months
Page 18 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
18
3.1 Distribution of malnutrition in Z-score
Weight/Height: Distribution by Age in Z-score Table 4
Severe wasting
(<-3 z-score)
Moderate wasting (>= -3 and <-2 z-score )
Normal (> = -2 z score)
Oedema
Age (mths)
Total no.
No. % No. % No. % No. %
6-17 181 9 5.0 40 22.1 132 72.9 0 0.0
18-29 229 6 2.6 37 16.2 186 81.2 0 0.0
30-41 205 11 5.4 23 11.2 171 83.4 0 0.0
42-53 157 2 1.3 19 12.1 136 86.6 0 0.0
54-59 167 7 4.2 34 20.4 126 75.4 0 0.0
Total 939 35 3.7 153 16.3 751 80.0 0 0.0
3.2 Weight/Height Index vs. Oedema
Table 5
<-2 z-score >=-2 z-score
Oedema present Marasmic --kwashiorkor No. 0 (0.0 %)
Kwashiorkor No. 0 (0.0 %)
Oedema absent Marasmic No. 188 (20.0 %)
Normal No. 752 (80.0 %)
The Waterlow classification indicates that 20% (188children) have Marasmus. None are suffering from Marasmus/kwashiorkor, 80 %( 752 children) of the children are normal.
3.3 Global, moderate, and Severe Acute Malnutrition by gender in Z-score
Table 6
All n = 939
Boys n = 456
Girls n = 483
Prevalence of global malnutrition (<-2 z-score and/or oedema)
(188) 20.0 % (16.3 - 23.7 95% C.I.)
(98) 21.4 % (17.6 - 25.3 95% C.I.)
(90) 18.6 % (14.1 - 23.1 95% C.I.)
Prevalence of moderate malnutrition (<-2 z-score and >=-3 z-score)
(153) 16.3 % (13.5 - 19.0 95% C.I.)
(85) 18.6 % (15.3 - 21.9 95% C.I.)
(68) 14.1 % (10.7 - 17.4 95% C.I.)
Prevalence of severe malnutrition (<-3 z-score and/or oedema)
(35) 3.7 % (1.6 - 5.8 95% C.I.)
(13) 2.8 % (0.8 - 4.9 95% C.I.)
(22) 4.6 % (2.0 - 7.1 95% C.I.)
Page 19 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
19
3.4 Acute malnutrition by age category
Table 7
6---59 N=939
6---29 N=410
Global acute malnutrition 20.0 % (16.3 - 23.7 ) 22.4 %( 17.0---29.0)
Severe acute malnutrition 3.7 % (1.6 - 5.8) 3.7 %( 1.6---7.6)
Measures of exposure effect at [95% CI] for the age group 6-29 months and 30-59 indicate that the rates of malnutrition are not significantly different between the two groups with P value of >0.0520. The relative Risk ratio21 is 1.24 [0.96<RR< 1.60]. the uncorrected chi squares is 2.66 These means that children aged less than 30 months are 1.24 times more likely to be malnourished compared to those above 30 months.
3.5 Distribution of malnutrition in percentage of the median
It’s the most common indicator for computing admissions into targeted feeding programmes since it’s easier to comprehend and calculate. It approximates weight deficits more accurately. Due to its specificity, It’s superior in predicting mortality in the under five children.
3.6 Prevalence of malnutrition by age, based on weight-for-height median and oedema
Table 8
Severe wasting (<70% median)
Moderate wasting (>=70% and <80% median)
Normal (> =80% median)
Oedema
Age (mths)
Total no.
No. % No. % No. % No. %
6-17 181 7 3.9 27 14.9 147 81.2 0 0.0
18-29 229 4 1.7 20 8.7 205 89.5 0 0.0
30-41 205 6 2.9 18 8.8 181 88.3 0 0.0
42-53 157 1 0.6 9 5.7 147 93.6 0 0.0
54-59 167 3 1.8 19 11.4 145 86.6 0 0.0
Total 939 21 2.2 93 9.9 825 87.9 0 0.0
3.7 Weight for height vs. oedema
Table 9
<80% >=80%
Oedema present Marasmic kwashiorkor No. 0 (0.0 %)
Kwashiorkor No. 0 (0.0 %)
Oedema absent Marasmic No. 114 (12.1 %)
Normal No. 825 (87.9 %)
3.8 Prevalence of acute malnutrition based on the percentage of the median and/or oedema
Table 10
n = 939
Prevalence of global acute malnutrition (<80% and/or oedema)
(114) 12.1 % (9.3 - 15.6 95% C.I.)
Prevalence of moderate acute malnutrition (<80% and >= 70%)
(93) 9.9 % (6.6 - 11.7 95% C.I.)
Prevalence of severe acute malnutrition (<70% and/or oedema)
(21) 2.2 % (1.1 – 4.2 95% C.I.)
20 P corresponds to the statistical significance of the test. It’s the probability that an event occurs.
21 The risk ratio corresponds to the added risk of malnutrition. When RR is 1.0, no association is likely.
Page 20 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
20
measles vaccination status
card
mother recall
not vaccinated
3.9 Mortality risk: mid upper arm circumference
Those who are above 12 months and are 75cm and more were included in this analysis giving a total sample of 797.
3.9.1 MUAC Distribution According To Nutritional Status
Height: > 75cm. Age : > 12 months Table 11
Criteria
Nutritional status Number percent
<11.0 cm Severe malnutrition N; 2 0.3%
11.0cm>=MUAC<12.4cm Moderate malnutrition N;48 6.0%
12.5 cm >=MUAC<= 13.5 cm At risk to malnutrition N;178 22.3%
MUAC>13.5 Normal N;569 71.4%
Total N;797 100%
4.0 Measles vaccination Coverage
Measles vaccination among the under five children was found to be 33.3%. However, there is still need for EPI campaign incorporating agencies in Aweil south to raise coverage.
5.0 Morbidity Table 12
Illness episodes in last 2 weeks among under fives
Percent 95% ci
reported being ill 12.4% 9.4---13.5
no reported illnesses 87.8% 85.4---89.7
Total 100.0%
Page 21 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
21
6.0 Meal frequency in the past 7 days for under fives Approximately 94.6% of the under fives are consuming 2 or less meals per day. This is an indicator of inappropriate feeding practises and most probably inadequate dietary intake among the children. Table 13
Meal frequency Percent 95% ci
proportion consuming 1 meal/day 22.7% 20.1---25.5
proportion consuming 2 meal/day 71.9% 68.9---74.7
proportion consuming 3 meals/day 5.4% 4.1---7.1
Total 100.0%
7.0 BCG vaccination coverage Childhood vaccination against communicable disease i.e tuberculosis’s is still low pointing to the poor coverage of immunization in the county. It’s further worsened by long distances to the only TB treatment facility in Aweil East County. This discourages most persons from seeking medical assistance.
8.0 Vitamin A supplementation coverage Vitamin A deficiency is a disabling and potentially fatal public health problem for children under 6 years of age. VAD-related blindness is most prevalent in children under 3 years of age hence the need for enhanced supplementation. 60% have received vitamin A mostly through polio NID campaigns. Though this coverage is better than most parts of south Sudan, it’s still very low and every opportunity should be utilised to increase coverage.
Retrospective mortality 8 persons of whom 6 were under fives had died in the past 90 days in the sample. The 0-5 mortality rate is 0.69 deaths/10,000/day and the crude rate is 0.26 deaths/10,000/day.the presumed causes of death include.
BCG vaccination status--aweil south county 2006
BCG scar
NO BCG scar
Page 22 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
22
9.0 Residential Status A total of 507households were visited during the survey of which 93.5% were residents, 4.3% were displaced mostly due floods in the area. 2.2% were returnees mostly from North Sudan due to the cease fire and the signing of the peace protocols. Key informants report that the county has experienced an increase in the number of returnees who are slowly being absorbed back into the community and which are expected to exert more pressure to the households hosting them.
10.0 DISCUSSION Anthropometric results indicate that the Global Acute Malnutrition and/ or oedema (GAM), <-2.00 SD Z-score, is 20.0% (95% CI 16.5-23.7). Severe Acute Malnutrition and/ or oedema (SAM), <-3.00 SD Z-score, is 3.7% (95% CI 1.6-5.8).When expressed in percentage of the median, global acute malnutrition (<80%) is 12.1 %( 9.3 - 15.6) and severe acute malnutrition (<70%) is 2.2 %( 1.1 – 4.2) No cases of nutritional oedema have been reported. The rates translate into 6128 children who are in need of supplementary feeding and 1392 children who require therapeutic treatment to curb on associated mortality22. Measures of exposure effect at [95% CI] for the age group 6-29 months and 30-59 indicate that the rates of malnutrition are not significantly different between the two groups with P value of >0.0523. The relative Risk ratio24 is 1.24 [0.96<RR< 1.60] and the uncorrected chi squares is 2.66 These means that children aged less than 30 months are 1.24 times more likely to be malnourished compared to those above 30 months. Vitamin A (retinol) which is an essential nutrient needed in small amounts by humans for the normal functioning of the visual system; growth and development; and maintenance of epithelial cellular integrity, immune function, and reproduction is still having a low coverage in the county. 60% of the 22 Estimation done to provide working figures only and inform programme planning. The Z score rather than the percent
median (though used as admission criteria) has been used to increase on the sensitivity of absolute approximation. 23 P corresponds to the statistical significance of the test. It’s the probability that an event occurs.
24 The risk ratio corresponds to the added risk of malnutrition. When RR is 1.0, no association is likely.
Presumed Causes of Death (Aweil South 2006)
Simple diarrhoea, 12.50%
Accident, 25.00%
Fever, 12.50% LRTI 12.50%
Others, 37.50% Simple diarrhoea Accident Fever Respiratory tract infection Others
Page 23 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
23
sample has accessed the micronutrient .Vitamin A deficiency is a disabling and potentially fatal public health problem for children under 6 years of age. VAD-related blindness is most prevalent in children under 3 years of age hence the need for enhanced supplementation. More than 94.6% of the under fives consume less than 2 meals predisposing them to reduced nutrient intake and uptake of malnutrition Malnutrition among those aged 6-29 months remains critical with 22.4% being malnourished. However it’s not significantly different from rates of children 06-59 months. The higher prevalence at the younger age group indicates the increased vulnerability during the weaning period as appropriate complementary foods might not be available. 3.7% are severely malnourished and at risk to mortality Further analytical tests reveal that boys are at higher risk of being malnourished than girls (risk ratio, adjusted for clustered sampling is 1.15 (C.I. 0.89 <RR< 1.49). They are 1.15 times more likely to be malnourished than girls. The difference is not significant with P=0. 27 .However, Severe acute malnutrition is affecting more girls than boys.63% of the girls are severely malnourished compared to 37% of the boys. The WHZ distribution compared to the international reference population showed a significant displacement of the distribution to the left of the reference indicating poor nourishment.
The 0—5 year mortality rate was found to be 0.69deaths/10,000/25day and 0.26deaths/10,000/day for crude mortality rate .These are below the emergency and alert levels and are acceptable. The mortality rates are much reduced compared to the same time last year when the under five rate was 1.44 deaths/10,000/day. The population of Aweil south has a near normal structure. The boy to girl ratio is 0.9026 i.e. 456/483. The Waterlow classification indicated no presence of Marasmic-kwashiorkor. This classification is particularly useful to identify the number of Marasmic-kwashiorkor cases who are at an increased risk of death for immediate case management. Measles immunization coverage is low among children aged 6-59 months with an estimated 35.4%. BCG coverage was 21.7 %. Health facilities should use every opportunity to cover the vaccination needs of each child and active community mobilisation and sensitisation could be envisaged. Observations and discussions conducted by the survey teams indicated that some houses are still surrounded by water in the after effects of last years floods. Most households have diverted resources that could have been used for food needs to secure materials for new shelter constructions. These Many pools of stagnant water have continued to be a source of bad water and also rich breeding grounds for malarial mosquitoes.PHCUs are reportedly seeing more positive malaria cases which will worsen with the onset of the rains from June. Fishing, an activity that traditionally follows every flooding season and which is usually expected to provide broth to households and more so meets the protein needs of children has been hampered by lack of fishing tools and the alteration in feeding pattern caused by lack of sorghum (dura) which is a popular and preferred accompaniment for fish broth. These have been so due to massive flood destructions of sorghum tracts in the lowland fishing and cropping food economy zone.
26 The sex ratio should be one in a normal structure ( a value between 0.84 and 1.20 is acceptable)
Page 24 of 36 010406 Tearfund Aweil South nutrition and Mortality survey March 2006
24
11.0 RECOMMENDATIONS
Continue the supplementary and therapeutic feeding programme to link with the next harvest monitoring the situation closely to inform project phase out.
Decentralise the feeding centres by opening others in poorly accessible areas namely ajak, wuncum and malek Alel which were worst hit by the floods and where most of the malnourished children are suspected to have originated. Strategy should ensure that nutritional inputs are prepositioned before the rains.
optimise active case finding through accelerated mobilization ,community leaders and utilise the village screening technique to identify malnourished children for admission
Assess and improve knowledge, attitudes and skills of feeding and caring practices of mothers and further strengthen the collaboration in hygiene promotion and health education.
Integrate nutrition intervention ,micronutrient supplementation and immunization .Activities as major component of health facilities, including growth monitoring and promotion;
TEARFUND to take the lead and advocate on behalf of the community for more projects and funds to address the underlying factors to malnutrition including but not limited to good water,health,hygiene,food and education.
Continued food distribution until the harvest in October.
Strengthen the food security strategies by widening the crop varieties e.g. promoting other cereals like maize, beans, millet etc in the County.
Promote improved access to safe water in the county and treat all un-protected water sources including protecting all open wells.
Conduct an in-depth assessment to estimate the impact of the current returnee needs and the extent of the strain on the livelihoods of the hosting community and targeting approach.
25
25
12.0 APPENDICES
MONTH Month events 2001 2002 2003 2004 2005
2006
JANUARY nyeth RUT 50 38 26 CPA 14
2
1
FEBRUARY kol MAI 49 37
Tearfund Survey 25 13
MARCH akoldit MAI 48 Election of chiefs 36 24
Tearfund survey 12
SURVEY
APRIL akachthii YATHOK 59
TEARFUND opened the program 47
a lot of cattle died of drought 35 23 11
MAY aduang YATHOK
RAJA CAPTURED BY SPLA 58 46
Dr. John Garang Visits 34
SPLMA month 22 10
JUNE alathbol KER 57
Gogrial captured by GOS 45 33 21 9
JULY akoldit KER 56 44 32 20
John Garang’s death 8
AUGUST bildit RUEL
Commander Geroge Kuac died 55 43 31 19 7
SEPTEMBER bielthii RUEL 54 42 30 18 6
OCTOBER lal RUEL
RAGA CAPTURED BY GOS 53
New commissioner installed 41 29 17 5
NOVEMBER holbekaal RUT 52 40
Nutritional survey by TEARFUND 28
Nutrition survey 16
4NUTRITION SURVEY NOV 05
15
DECEMBER konpiu RUT 51
Ajak attacked by Murahaleen 39 27 Christmas 3
26
26
Traditional calendar
F M A M J J A S O N D J
MAIN SEASON MEI KER RUEL RUTH
Land preparation
Planting
Harvest minor harvest
Flooding
Fishing mud fish swamp & river fishing mud fish
Livestock
Peak Milk yield
migration to toic
high expansion on livestock
festivals & rituals
Home Construction
Tobacco cultivation
Labour migration
Special Events
Influx of mosquitoes
School schedule
Wild Foods (peak) vegetables fruits
Hunger ‘Gap’ season
27
27
ANTHROPOMETRIC NUTRITION SURVEY QUESTIONNAIRE Children 06-59 months or less than 110cm height DATE: ------------------ TEAM ………………………..CLUSTER--------------------.
NO HH NO
Age (mths)
Sex 1=B 2=G
Weight Kg
Height Cm`
Edema Y/N
MUAC Cm
Meal frequency 1=1 times 2=2 times 3=3 +times
VIT A 1=Yes 2=No
BCG Scar 1=Yes 2=No
Measles 1. Card. 2. Carer 3. No.
Illness in <2 weeks 1=yes 2=No
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
28
28
MORTALITY SURVEY QUESTIONNAIRE DATE: TEAM: CLUSTER:
Cause: 1= Simple Diarrhoea, 2=Bloody diarrhoea (Dysentery), 3=Measles, 4=Fever, 5=Malnutrition,6=Lower Respiratory Tract Infection 7=Accident, 8= Not known, 9=Other (Specify)
HH NO.
Origin 1=Host 2=IDPs 3=Returnee
Number of People in Household
Number Under 5s in household
Number of BIRTHS IN THE LAST 90 DAYS
TOTAL DEATHS IN LAST 90 DAYS
TOTAL UNDER 5 DEATHS IN LAST 90 DAYS
CAUSES OF DEATH1
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
29
29
Nutrition Survey Training Time Plan TIME ACTIVITY DAY 1 9:00- 9:30 Climate setting Introduction of participants and facilitators Participants’ expectations Rules and regulations for the survey and training 9:30- 10:30 Statement of objectives Area of coverage and methodology 10:30- 11:00 Body measurements (theory) 11:00- 11:15 BREAK 11:15- 11:45 Body measurements (theory) cont. 11:45-12:15 Body measurements (practical – group work) Weight measurements Height measurements MUAC (adult and children) Oedema 12:15- 1:00 Regrouping and discussions 1:00- 3:00 LUNCH BREAK 3:00- 4:00 other information to collect Measles vaccination Residential status Nutritional status of the caretakers 4:15- 5:00 other information cont. Questions and discussion DAY 2 9:00- 9:30 Review of the previous day lessons 9:30- 11:00 Mortality (theory and practical) 11:00- 11:15 BREAK 11:15- 1:00 Local events calendar 1:00- 3:00 LUNCH 3:00- 4:00 Selection of households and children in the village 4:15- 5:00 Questions and discussions DAY 3 8:00- 9:00 Review of day 1and 2 9:00- 1:00 Pilot survey 1:00- 3:00 LUNCH BREAK 3:00- 4:00 Review of the pilot survey 4:00- 5:30 Allocation of the clusters Survey kit and time plan
30
30
Random Number table
1317 8783 2981 6960 7759 8355 7342 9869 718 9795
5109 8532 2142 7328 4763 970 7245 7728 2686 7743
610 3304 3367 5430 773 6693 5089 7436 5399 838
1858 214 9320 2490 3968 9227 5966 9827 2405 6150
9693 9949 8367 7518 7755 9872 164 7848 8456 115
162 4413 934 9681 5728 7926 3332 8009 9933 6225
6790 3751 2765 5284 9719 6576 4041 8809 69 6819
1907 8552 4041 3907 3606 7547 5140 8153 9147 9700
4643 5488 5705 727 8016 287 7822 4285 2341 2906
5780 7183 6950 4539 3615 3973 9794 7293 310 3382
2105 9596 248 3542 3097 3133 1475 691 261 7868
5415 2698 2831 3381 4559 137 6603 5119 7591 6747
5654 6688 6452 8358 6483 8318 7207 1107 4721 168
8166 2798 5134 4457 441 5454 9889 734 43 3223
6953 1913 4045 2839 7258 3045 132 7272 8748 3757
2991 8993 876 8963 1809 5810 5807 3936 8664 2146
7894 4895 6294 572 7286 4634 8459 6548 1941 6842
9914 1962 9994 8539 2588 9130 4258 8951 5247 957
5832 9145 4447 6253 2335 3347 632 6792 1804 8065
6427 4955 7758 4545 4671 378 7482 4202 7928 528
5662 9010 9553 1719 4494 4179 4377 412 9225 6099
6244 5472 6278 685 2299 9368 7644 5832 4100 1111
6718 4147 4832 7759 1255 2268 3760 9620 4743 1003
7759 7536 5937 135 7705 9005 7940 3281 8235 1498
7791 4614 1153 1565 2721 8926 9354 7315 2943 6186
631 4613 9934 8298 4883 4118 6838 469 7847 8808
270 6602 5654 9785 6936 8308 1550 3583 4974 1018
486 3141 1971 1188 1481 940 5440 2615 7571 8898
9414 8777 3482 7229 3346 4686 6971 7824 9198 4035
1755 6693 7040 9421 8821 7200 7971 8681 1374 7392
3752 9253 2651 1175 4377 369 8036 6514 9954 6804
8625 763 5361 7859 51 2856 5395 9435 2880 1348
2590 3192 2033 1313 5144 4231 5625 6574 4458 8383
4128 8171 9424 853 6398 1431 2148 1145 3835 1538
1669 1023 2469 5312 1283 876 4884 4384 7816 425
7338 5108 4171 3127 1581 1990 6004 4891 684 5364
6923 7293 1012 15 4906 421 4151 401 6175 2899
8714 7784 292 6278 4317 1741 1067 1513 9277 387
6384 140 8286 8247 8686 8905 7007 9422 7988 437
3551 9722 654 914 8973 9254 3874 2172 7708 8489
194 1387 8975 1268 8064 9330 7449 6460 3412 9307
3562 9666 9850 4392 4333 8310 2648 4542 7264 665
31
31
TEARFUND Cluster control form County: _________________ Village: _______ Cluster #: _______ Team code: ______ Date: _____ / _____ / 2006
HH no
Head of HH name Number of Children
Visit Result 1=completed 2 = part completed 3 = refused 4 = family not found
No. of Visits
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
32
32
Training form for Anthropometry standardization exercise Team number ____________
Number Child's name Age (months) Weight Height
1
2
3
4
5
6
7
8
9
10
11
12
13
33
33
Nutrition survey Equipment and supplies checklist
Training Field work Total
Anthropometry
Height boards
Salter scales
MUAC tapes – Child
Ball of string
Logistics & sampling
Cluster list for each team
Random number table
Cluster control forms
Survey – Child
Local calendar
Verbal autopsy questions
Clipboards
Plastic document folders
Copies of training manual
Pencils & erasers and Pencil sharpeners
Pens
Writing pads
Training equipment
Flipchart
Markers for flipchart
34
34
CLUSTER LIST
Village population U-5 cumulative Attributed Num Clusters
Nyoc Deng 1150 230 230 0-230
Nyoc Deng 900 180 410 231-410
Hong Wakdit 850 170 580 411-580
War Ayok 1430 286 866 581-866
Riang Mawel * 1110 222 1088 867-1088 1
Nyioc thok 1370 274 1362 1089-1362
War lai 1500 300 1662 1363-1662
Aguek 1400 280 1942 1663-1942
Adakbai 1100 220 2162 1943-2162
Marol * 1000 200 2362 2163-2362 2
Amac rol 1500 300 2662 2363-2662
Adak lai 790 158 2820 2663-2820
War thou 975 195 3015 2821-3015
Kem 760 152 3167 3016-3167
Akon Bet 925 185 3352 3168-3352
War Ajak 950 190 3542 3353-3542 3
Dong 1750 350 3892 3543-3892
Makuac Kiir 900 180 4072 3893-4072
Rilagok 1600 320 4392 4073-4392
Makuac Kiir 1955 391 4783 4393-4783 4
Makuac Kiir 1755 351 5134 4784-5134
Amiir 1890 378 5512 5135-5512
Abiyei 1895 379 5891 5513-5891
Wunbut 1885 377 6268 5892-6268 5
Kalbut 1890 378 6646 6269-6646
Anguoth 1845 369 7015 6647-7015
Wunpeth 1160 232 7247 7016-7247
Anyuon 1555 311 7558 7248-7558 6
Akuak 1825 365 7923 7559-7923
Rolthok 1830 366 8289 7924-8289
Rolngap * 1695 339 8628 8290-8628 7
Ayai 2070 414 9042 8629-9042
Lac Dit 2070 414 9456 9043-9456
Panraac Rin 1080 216 9672 9457-9672
Kuen Weeir 2205 441 10113 9673-10113 8
Lool Akeer 1400 280 10393 10114-10393
Nyioric 2500 500 10893 10394-10893
Mading Ring * 2250 450 11343 10894-11343 9
Aluet 2160 432 11775 11344-11775
Warlang 2200 440 12215 11776-12215
Rup Manwuot 2700 540 12755 12216-12755 10
Mayom Lac 2410 482 13237 12756-13237
Mayom Lac * 1945 389 13626 13238-13626 11
Mayom Lac 2410 482 14108 13627-14108
Mayom Lac 1800 360 14468 14109-14468
35
35
Achuan 2395 479 14947 14469-14947 12
Ajieth Boc 1440 288 15235 14948-15235
Amet wer 1960 392 15627 15236-15627
Lol Akwe 1500 300 15927 15628-15927
Mangar 1400 280 16207 15928-16207 13
Angeth 1250 250 16457 16208-16457
Malual Rou 1190 238 16695 16458-16695
Mawier 1360 272 16967 16696-16967
Wuncuei 1120 224 17191 16968-17191
Rum Amouth * 510 102 17293 17192-17293 14
Bur cuei 1020 204 17497 17294-17497
Maguer 850 170 17667 17498-17667
Linger 850 170 17837 17668-17837
Pankout 850 170 18007 17838-18007
Kuel Mayom 640 128 18135 18008-18135
Jur Ajiep 800 160 18295 18136-18295
Macot 510 102 18397 18296-18397
Panriak * 1280 256 18653 18398-18653 15
Maper 1105 221 18874 18654-18874
Bilma 880 176 19050 18875-19050
Warthiang 930 186 19236 19051-19236
Malek Lac 1040 208 19444 19237-19444
Duel 960 192 19636 19443-19636
Adhotic 1190 238 19874 19637-19874 16
Thieng Ameth 935 187 20061 19875-20061
Gekkou 1020 204 20265 20062-20265
Makuei Alel 945 189 20454 20266-20454
Majok Malek 995 199 20653 20455-20653
Adany 1105 221 20874 20654-20874
Wut Liet 1275 255 21129 20875-21129 17
Liilthok 680 136 21265 21130-21265
Malou 595 119 21384 21266-21384
Gakrol 765 153 21537 21385-21537
Mathiang Lual 340 68 21605 21538-21605
Majak 680 136 21741 21606-21741
Lool Aker 1145 229 21970 21742-21970
Wun thur 1190 238 22208 21971-22208
Wun pac * 1440 288 22496 22209-22496 18
Wun Aleu 935 187 22683 22497-22683
Anuet 1120 224 22907 22684-22907
Akol Achier 935 187 23094 22908-23094
Wunagep 2370 474 23568 23095-23568 19
Mabior 1980 396 23964 23569-23964
Panthou 1800 360 24324 23965-24324
Rum awec 1805 361 24685 24325-24685
Maluil Akaja * 1650 330 25015 24686-25015 20
Peth 1125 225 25240 25015-25240
36
36
Mayom Majuak 2160 432 25672 25241-25672
Gok 900 180 25852 25673-25852
Paker * 1610 322 26174 25853-26174 21
Riang Akeer 725 145 26319 26175-26319
Riang aker 1440 288 26607 26320-26607
Rum riit 1085 217 26824 26608-26824
Athomac 1890 378 27202 27823-27202
Thatmoc 720 144 27346 27203-27346 22
Titwol 990 198 27544 27346-27544
Athokmac 1170 234 27778 27545-27778
Athomoc 1170 234 28012 27779-28012
Pamoth 810 162 28174 28013-28174
Mayen 1080 216 28390 28175-28390
Mabior 1170 234 28624 28391-28624 23
Tiraliet 1350 270 28894 28625-28894
Malek Akol 1060 212 29106 28895-29106
Alueel 900 180 29286 29107-29286
Lolkou 2070 414 29700 29287-29700
Adip 715 143 29843 29701-29843 24
Riangkou 1080 216 30059 29844-30059
Nyorkon 900 180 30239 30240-30239
Malook 1620 324 30563 30240-30563
Panrual 1900 380 30943 30564-30943
Pankoor 1350 270 31213 30944-31213 25
Warlaap 1710 342 31555 31214-31555
Panthoi 900 180 31735 31556-31735
Anyomroom 1080 216 31951 31736-31951
War Alek 1350 270 32221 31952-32221
Marik 630 126 32347 32222-32347 26
Mur Yath 810 162 32509 32348-32509
Adhotic 1080 216 32725 32508-32725
Maper 1800 360 33085 32726-33085
Rumagany 1980 396 33481 33086-33481
Mier Ngol * 1620 324 33805 33482-33805 27
Hong dong 1980 396 34201 33806-34201
Rum Atwek 1620 324 34525 34202-34525
Alueth 250 50 34575 34526-34575
Pandong * 1350 270 34845 34576-34845 28
Pakac 2055 411 35256 34846-35256
Long Agot 1980 396 35652 35257-35652
Makuac Agep 2520 504 36156 35653-36156 29
War Ngap 1800 360 36516 36158-36516
Amuol 990 198 36714 36517-36714
Rum Awec 1710 342 37056 36715-37056
Rum thoi 1440 288 37344 37057-37344 30
Bullamum 1260 252 37596 37348-37596