A mechanism-based binding model for the population pharmacokinetics and pharmacodynamics of...
Transcript of A mechanism-based binding model for the population pharmacokinetics and pharmacodynamics of...
A mechanism-based binding model for thepopulation pharmacokinetics and pharmacodynamicsof omalizumab
Naoto Hayashi, Yuko Tsukamoto,1 William M. Sallas2 & Philip J. Lowe3
Drug Metabolism and Pharmacokinetics, Novartis Pharma AG, Basel, Switzerland, 1Drug Metabolism and Pharmacokinetics, NovartisPharma KK, Tokyo, Japan, 2Modeling and Simulation, Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA and 3Modelling andSimulation, Novartis Pharma AG, Basel, Switzerland
CorrespondencePhilip J. Lowe, Modelling andSimulation, Novartis Pharma AG,Lichtstrasse 35, CH-4056 Basel,Switzerland.Tel.: + 41 6 1324 4676Fax: + 41 6 1324 3039E-mail: [email protected]
.............................................................................................................................
Keywordsatopic asthma, binding modelmonoclonal antibody, IgE, NONMEM
.............................................................................................................................
Received4 November 2005Accepted28 July 2006Published OnlineEarly10 November 2006
AimOmalizumab, a humanized IgG monoclonal antibody that binds to human immuno-globulin E (IgE), interrupts the allergic cascade in asthmatic patients. The aim was tocompare simultaneously drug exposure and IgE biomarker responses in Japanese andWhite patient populations.
MethodsAn instantaneous equilibrium drug–ligand binding and turnover population model wasbuilt from 202 Japanese patients. A posterior predictive evaluation for the steady-statedistributions of omalizumab and IgE was then carried out against 531 White patients.
ResultsThe mean parameters estimated from the Japanese patients were as follows: omali-zumab clearance 7.32 � 0.153 ml h-1, IgE clearance 71.0 � 4.68 ml h-1 and the dif-ference between that for omalizumab and the complex 5.86 � 0.920 ml h-1, thevolume of distribution for omalizumab and IgE 5900 � 107 ml, and that for thecomplex 3630 � 223 ml, the rate of IgE production 30.3 � 2.04 mg h-1. Half-lives ofIgG (23 days) and IgE (2.4 days) were close to previous reports. The dissociationconstant for binding, 1.07 nM, was similar to in vitro values. Clearance and volume ofdistribution for omalizumab varied with bodyweight, whereas the clearance and rate ofproduction of IgE were predicted accurately by baseline IgE. Overall, these covariatesexplained much of the interindividual variability.
ConclusionsThe predictiveness of the Japanese model was confirmed by Monte-Carlo simulationsfor a White population, also providing evidence that the pharmacokinetics of omali-zumab and IgE were similar in these two populations. Furthermore, the model enabledthe estimation of not only omalizumab disposition parameters, but also the bindingwith and the rate of production, distribution and elimination of its target, IgE.
IntroductionOmalizumab is a recombinant DNA-derived humanizedmonoclonal antibody that selectively binds humanimmunoglobulin E (IgE). The antibody is an immuno-
globulin (Ig) G1 k with a human framework and comple-mentarity determining regions (CDRs) from ahumanized anti-IgE murine antibody [1]. The causal roleof IgE in allergic disease is well established [1–3]. The
British Journal of Clinical Pharmacology DOI:10.1111/j.1365-2125.2006.02803.x
© 2006 The AuthorsJournal compilation © 2006 Blackwell Publishing Ltd
Br J Clin Pharmacol 63:5 548–561 548
allergic cascade is initiated when IgE bound to high-affinity FceRI receptors on the surface of basophils andmast cells is cross-linked by allergen, resulting in thedegranulation of these effector cells and the release ofinflammatory mediators such as histamine and leukot-rienes. Omalizumab interrupts the allergic cascade by (i)forming complexes with IgE and preventing the armingof effector cells, (ii) aiding off-loading of mast cells andbasophils by trapping IgE as it dissociates from thereceptor, and (iii) downmodulating FceRI as a directconsequence of the reduction in free IgE concentrations[4–12].
Administration of omalizumab significantly decreasesserum free IgE concentrations, resulting in improvedcontrol of atopic asthma and, most probably, otheratopic conditions. As a result of omalizumab binding toIgE, lowering its free concentration, total serum IgEconcentrations rise. Such an increase could occur by twomechanisms: (i) omalizumab–IgE complexes could beeliminated more slowly than free IgE due to the abilityof the IgG portion of complexes to access the Brambellreceptor, sparing them from lysosomal degradation [13],and (ii) the complexes, being of higher molecular mass(at least 340 kDa for the dimer but up to 1000 kDa forthe hexamer [14]), filter less effectively through the vas-cular endothelium and are therefore retained within thesmaller plasma volume of distribution [15–18].
However, these mechanisms have yet to be confirmed,although a mechanism-based PK/PD model of the phar-macokinetics of omalizumab and its binding to IgE hasbeen published for a limited number of subjects [19].The concentration–time profiles of omalizumab, freeand total IgE exhibited many of the same properties asother therapeutic antibodies. In addition, the modelallowed the estimation of both drug-specific kineticparameters and those that are related to endogenous IgEproduction and elimination.
We now present an alternative model, based on theconcentration–time profiles of omalizumab, free andtotal IgE in Japanese subjects. As in the previous model,it incorporates three entities, namely free omalizumab,free IgE and the omalizumab–IgE complex, but eachwith their own clearance and volume of distribution. Therelationship between these entities is defined by the lawof mass reaction, assuming, unlike in previous work[19], that they are always at equilibrium. This simplifi-cation enabled the successful analysis of large quantitiesof sparse data using NONMEM with a binding model,which was impossible with the previous model. Giventhe timescale (weeks) of clinical studies with mono-clonal antibodies, and the short equilibration time(hours) for the antibody–IgE complexation reaction,
such an assumption is considered valid. Theconcentration–time profiles of the three compounds canthen be explored simultaneously by a population model,which enables the prediction of statistical distributionsof individual profiles using covariate values (bodyweight and baseline IgE) to decrease unexplained inter-individual variability.
Therapeutically, a table based on the pretreatment IgEconcentration and body weight has been constructed toestimate the omalizumab dose required to decreasetrough free IgE concentrations (based on samples drawnimmediately prior to drug treatment in a multiple doseregimen) to between 12 and 21 ng ml-1, the range asso-ciated with clinical efficacy [20]. The frequency distri-bution of the IgE response is such that >90% of patientsachieve suppression at concentrations <50 ng ml-1. Thepresent model mimics this frequency distribution of freeIgE. Furthermore, although the model parameters wereestimated using data from Japanese patients only, simu-lated distributions of free IgE overlay well the steady-state data from independent studies in White patientstreated according to the dosing table. This finding indi-cates that the model is predictive and that there areeffectively no differences in the pharmacokinetics ofomalizumab between Japanese and Whites.
MethodsAnalysis of omalizumab and total and free IgEAn enzyme-linked immunosorbent assay (ELISA) wasused for the analysis of total omalizumab using humanmyeloma-derived IgE from the U266B1 cell line, ATCCnumber TIB-196266 (American Type Culture Collec-tion, Manassas, VA, USA) as the capture antibody. Amonoclonal antibody was developed against the CDR ofomalizumab, conjugated with horseradish peroxidase,and used to detect plate-bound drug. Colourimetricdetection used the o-phenylenediamine reaction withhydrogen peroxide. The assay range was 0.16–10 ng ml-1, but samples were normally diluted, so thatthe lower limits of quantification (LLOQ) were160 ng ml-1 in studies 1101 and 1305, 1600 ng ml-1 instudies 007, 008 and 009. The coefficient of variationwas 4.0% at 0.90 ng ml-1.
Free IgE in serum was determined using a previouslyreported ELISA [14]. The assay had an upper limit ofquantification of 150 ng ml-1, a LLOQ of 0.78 ng ml-1
and coefficients of variation of 10.1% at 1.51 ng ml-1
and 5.4% at 21.8 ng ml-1.Pretreatment total IgE concentrations in serum were
determined by a microparticle enzyme immunoassaytest kit commercially available from Abbott Inc. (AbbottPark, IL, USA). The LLOQ of total IgE was 2.4 ng ml-1,
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 549
with a coefficient of variation of 13.6% at 3.6 ng ml-1.Measurements for total IgE in IU ml-1 were converted tong ml-1; 1 IU ml-1 total IgE = 2.42 ng ml-1 total IgE.
Study designFor the population PK/PD analysis, the data from fivestudies shown in Table 1 were integrated. Study 1101used a single dose (75–375 mg) and the remainingstudies involved multiple dosing with treatment periodsof 8–52 weeks. The sampling times were 0, 0.5, 1, 2, 4,7, 10, 14, 28, 42, 56, 70 and 84 days after administrationin the single-dose study. In the multiple-dose studies,samples were drawn immediately prior to dosing(trough) and during the post-treatment period.
Study 1101 was carried out at the Sekino ClinicalPharmacology Clinic, 28-3, Ikebukuro 3 Chome,Toshima-ku, Tokyo. Study 1305 was carried out in twocentres, in Tokyo and in Osaka, both organized by theOsaka Clinical Research Organization for MedicineClinic, 4-12-11 Kasuga, Suita-Shi, Osaka. Both studieswere approved by the Institutional Review Boards of theaforementioned organizations and all patients gaveinformed written consent. The studies were conducted inaccordance with the Declaration of Helsinki and Guide-lines for Good Clinical Practice. The data from studies007, 008 and 009 have been published [13, 14, 21].
For model building, Japanese studies 1101 and 1305were combined. Despite study 1101 not representing atherapeutic treatment period, its incorporation in themodelling permitted a better evaluation of the influenceof baseline IgE on the pharmacokinetics and pharmaco-dynamics of omalizumab because the range of baselineIgE concentrations included was broader than in theother studies.
Only subjects treated with omalizumab were used inthe modelling and validation. Values of free IgE concen-tration above the upper limit of quantification wereexcluded. All data from all subjects treated with omali-zumab in studies 1101 and 1305 were used in the modelbuilding.
In order to confirm model predictions, external vali-dation was conducted using data from clinical studies007, 008 and 009. Study 007 involved an 8-week treat-ment of patients with seasonal allergic rhinitis. In thisstudy, subjects with baseline IgE �363 ng ml-1 received300 mg of omalizumab every 4 weeks, and the othersubjects received the same dose every 3 weeks. Themedian concentration–time profiles for total omali-zumab, free and total IgE were predicted by simulationand compared with observed median data.
Studies 008 and 009 involved 52-week treatments ofpatients with allergic asthma. In these studies a dosing
table was used based on body weight and pretreatmentIgE concentration (Table 2). Predose omalizumab, totaland free IgE concentrations at steady state, at least 240days after the first dose, were predicted by simulationand compared with observed values.
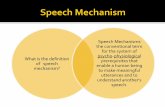
The PK/PD structural modelThe concept of the PK/PD model is shown in Figure 1.The model incorporates free omalizumab, free IgE andthe immune complex of omalizumab and IgE. The dis-position for each component was assumed to bedescribed by a one-compartment first-order eliminationmodel.
The amount of omalizumab in subcutaneous tissue(XSC), the sum of the amounts of free omalizumab andcomplex in serum (total omalizumab, XTX) and theamount of total IgE in serum (XTE) are represented inunits of nmol and described by the following differentialequations:
dX
dtk X t t f D here t dta
SCSC D= − ∗ + −( )∗ ∗ ( ) =( )∫δ δ 1
dX
dtk X CL C CL Ca
TXSC X fX C C= ∗ − −
dX
dtP CL C CL CTE
E E fE C C= − −
where the parameters are: ka, absorption rate constant(l h-1); f, absolute bioavailability; D, dose (nmol); PE,endogenous production rate of IgE (nmol h-1); CLX,clearance of free omalizumab (ml h-1); CLE, clearance offree IgE (ml h-1); CLC, clearance of complex (ml h-1); tD,dosing time (h).
Concentrations [nmol l-1 (nM)] are derived from theabove amounts and distribution volumes [VX, distribu-tion volume of free omalizumab (ml); VE, distributionvolume of free IgE (ml); VC, distribution volume ofcomplex (ml); XC, the amount of the complex in serum(nmol)] as follows:
C X VC C C=
C C CTX fX C= +
C C CTE fE C= +
CX X
VfX
TX C
X
= −
CX X
VfE
TE C
E
= −
Here, CC, CTX, CTE, CfX and CfE are, respectively, thenanomolar concentrations of complex, total omali-
N. Hayashi et al.
550 63:5 Br J Clin Pharmacol
Tabl
e1
Stud
yde
sign
san
dbl
ood
sam
plin
gtim
esfo
rst
udie
sco
ntrib
utin
gto
the
popu
latio
nph
arm
acok
inet
ican
alys
is
Stud
yPu
rpos
ePa
tient
indi
catio
n
Subj
ect
no.
Bac
kgro
und
data
(sub
ject
sus
edfo
ran
alys
is,m
ean
�SD
and
rang
e)
Trea
ted
Use
din
the
anal
ysis
*St
udy
desi
gn
Trea
tmen
tpe
riod
(wee
ks)
Bod
yw
eigh
t(k
g)B
asel
ine
IgE
(ng
ml-1
)
1101
Mod
elbu
ildin
gan
din
tern
alva
lidat
ion
usin
gal
lsam
ples
Hea
lthy
volu
ntee
rbu
tat
opic
with
high
base
line
IgE
48 (Jap
anes
e:48
)48
Sing
ledo
se–
62.5
�6.
4(5
1–79
)81
1�
473
(204
–214
3)
1305
“Se
ason
alal
lerg
icrh
initi
s15
4(J
apan
ese:
154)
154
Mul
tiple
dose
with
dosi
ngta
ble
1260
.5�
10.2
(42–
101)
373
�31
7(5
3–13
16)
007
Exte
rnal
valid
atio
nus
ing
all
sam
ples
“16
5(W
hite
:16
4)15
5Ҡ
873
.7�
13.6
(48–
110)
356
�30
5(7
2.6–
1728
)
008
Exte
rnal
valid
atio
nus
ing
stea
dy-s
tate
troug
hsa
mpl
esAl
lerg
icas
thm
a26
8(W
hite
:23
8)20
6“
5279
.6�
18.6
(39–
150)
424
�36
1(4
8.4–
2081
)
009
““
274
(Whi
te:
256)
170
“52
78.2
�16
.9(4
0.0–
148)
523
�38
7(5
1–19
70)
*Stu
dies
1101
and
1305
had
shor
ttre
atm
entp
erio
dsan
dus
edal
lthe
sam
ples
from
the
patie
nts
tobu
ildth
em
odel
.Thu
s,ne
arly
allt
hepa
tient
stre
ated
with
omal
izum
abw
ere
avai
labl
eto
cont
ribut
esa
mpl
es.S
tudi
es00
8an
d00
9ha
dre
lativ
ely
long
treat
men
tper
iods
.In
thes
est
udie
spa
tient
sw
ere
mor
elik
ely
nott
obe
avai
labl
eto
cont
ribut
eth
ene
eded
stea
dy-s
tate
troug
hsa
mpl
e(a
tlea
st24
0da
ysaf
terf
irstd
ose
and
post
dose
with
in2
days
ofth
epl
anne
ddo
sein
terv
al)
fori
nclu
sion
into
the
anal
ysis
.†In
stud
y00
7,30
0m
gw
asad
min
iste
red
ever
y3
wee
ks(I
gE>3
63ng
ml-1
)or
4w
eeks
(IgE
�36
3ng
ml-1
).
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 551
zumab, total IgE, free omalizumab and free IgE. In theclinical studies CTX, CTE and CfE were expressed in unitsof ng ml-1. In the NONMEM code they were convertedto molar units using the molecular weights of omali-zumab (150 kDa) and IgE (190 kDa).
Based on preliminary model building with the condi-tion that VX � VE, NONMEM optimization was not suc-cessful. Consequently, VE was assumed to equal VX.Because IgE and IgG have similar molecular weightsand physical structures, their transfer between blood andtissue should be similar.
The amount of complex is determined by the law ofmass action and can be described by the followingequation:
KC C
Cd = [ ][ ]
[ ]fX fE
C
∴ = −( )[ ] −( )[ ][ ]
KX X V X X V
X Vd
TX C X TE C E
C C
∴ = + +⎛⎝
⎞⎠{
− + +⎛⎝
⎞⎠ −
⎫
XK V V
VX X
K V V
VX X X X
Cd
d
1
2
42
X E
CTX TE
X E
CTX TE TX TE ⎬⎬
⎪
⎭⎪where Kd is the dissociation constant expressed in molarunits (nM). The formation of complex is far more rapidthan changes in omalizumab concentrations. Therefore,relative to the timescales of the clinical studies and theirsampling, the concentration of complex can be assumedto be always at equilibrium.
The dissociation constantFor chemical equilibria between two species forming acomplex, the dissociation constant, Kd is assumed to beconstant in the absence of any competing agent.However, the reaction between omalizumab and IgE hasbeen shown to form two trimers (X2E and E2X) and ahexamer with a 1 : 1 stoichiometry (X3E3), dependingupon whether omalizumab or IgE is in excess. There-fore, Kd varies depending upon the relative concentra-tions of omalizumab and IgE [22]. In the PK/PD model,the change in Kd was assumed to obey the followingempirical model:
K KX
Xd d= ⎛
⎝⎞⎠0
TX
TE
α
Table 2Dosing table used in studies 1305, 008 and 009. Doses specified are in mg
Baseline IgE Body weight (kg)IU ml-1 ng ml-1 30–60 >60–70 >70–80 >80–90 >90–150
�30–100 �72.6–242 150 150 150 150 300>100–200 >242–484 300 300 300 300 225>200–300 >484–726 300 225 225 225 300>300–400 >726–968 225 225 300 300 –>400–500 >968–1210 300 300 375 375 –>500–600 >1210–1452 300 375 – – –>600–700 >1452–1694 375 – – – –
*Omalizumab dose administered by subcutaneous injection every 2 weeks (in bold) or 4 weeks (not bold).
SCDose
ka & f
freeomalizumab
CLE
VC
CLC
CLX
complex
freeIgEPE
VE
VX
=Kd
[Cf X] [Cf E]
[CC]
Figure 1The PK/PD model structure
N. Hayashi et al.
552 63:5 Br J Clin Pharmacol
where a � 0. The value of Kd at XTX = XTE is Kd 0. Whenthere is an excess of omalizumab, XTX >> XTE, the valueof Kd increases, indicating a decrease in apparent affin-ity. Over the range of omalizumab and IgE concentra-tions observed in the clinical studies, the apparent Kd
shifts by a factor of about 2.
The stochastic modelThe observational equation for each of the three mea-sured compounds was represented similarly as
Y = × ( )F exp ε
where Y is the observed value in a particular individualfor a given compound at a particular timepoint, F is thecorresponding fitted value from the PK/PD model, and eis the corresponding error normally distributed withmean 0. All errors were assumed to be unrelated, withthe error from each compound being allocated a separateparameter (s1
2, s22 or s3
2) to describe its associatedintra-individual variability.
The PK/PD parameters Kd0 and a were assumed to beconstant with no interindividual variability. The popula-tion model added random effects for the remainingPK/PD parameters in order to recognize differencesbetween individuals, and similarities across observa-tions corresponding to the same individual. The PK/PDparameters were allowed to depend on multiplicativeeffects of covariates and random error. The error com-ponent for each parameter represents the unexplainedintersubject variability for the corresponding parameter.Thus, if TVPARM is the ‘typical value’, or populationmedian value for a parameter PARM, and if h1 is arandom variable, with mean 0 and variance w1
2, repre-senting the deviation of the PARM of an individualpatient from the typical value (TVPARM) on the naturallogarithm scale, then the PARM of that patient is
PARM TVPARM= × ( )exp η1
In the same way, the random effect h1 represents thenatural logarithm of the ratio of the PARM of an indi-vidual patient to the typical value (TVPARM). Otherparameters were treated similarly with a correspondingrandom effect hj. The joint distribution of the hj’s wasassumed to be normal with a mean of 0 and with blockdiagonal variance–covariance matrix W. The hj’s for PE
and CLE were assumed to be correlated and the remain-ing hj’s assumed to be unrelated to each other and withhj’s for PE and CLE. A continuous covariate xi (bodyweight or baseline IgE) was modelled as affecting the jth
PK/PD parameter, say TVPARM, as follows:
TVPARM zj ij= × × ×θ0 . . . . . .
where
z x xij i iij= ( )0
θ
and xi0 is the reference of the covariate or standardvalue.
The clearance of the omalizumab–IgE complex, CLC,was reparameterized to be additive upon the clearance offree omalizumab: CLC = CLX + DCLC. The clearance ofthe complex is greater than that of free omalizumab [19],for which there are two hypotheses. Endogenous IgG isknown to be protected from catabolism by the neonatalFc or Brambell receptor (FcRn) [23], which redirectsIgG back to the systemic compartment, thereby givingrise to a longer half-life compared with other classes ofimmunoglobulin. However, in binding a ligand, in thiscase IgE, steric hinderance may decrease the affinity toFcRn, leading to greater catabolism and clearance of thecomplex. In this regard, every antibody drug approvedby the Food and Drug Administration has a shorter half-life [18] than that reported for endogenous IgG [24, 25].The second hypothesis is that, since the complex con-tains IgE, it could be subject to the same eliminationmechanism as this protein. Therefore, the clearance ofthe complex could be equal to that of native IgG plus aproportion of the clearance of IgE. This fraction isunlikely to be equal to one, due to the steric hinderanceinvolved in the binding of omalizumab to at least oneside of the Fc portion of IgE. In either case, the DCLC
term represents the extra clearance of the complex overand above that of native IgG (free omalizumab).
Body weight, baseline IgE, age and sex were individu-ally plotted against the PK/PD parameters, and mean-ingful covariate–parameter relationships nominated.Significance was tested by backward elimination using asignificance level of P < 0.01, corresponding to a changeof at least 6.63 in the NONMEM objective function.Separate parameters for modelling the predictive effectsof baseline IgE on PE and CLE were present in the basicmodel. The range of baseline IgE values was broad andoptimization by NONMEM did not converge withoutthe inclusion of these covariates.
Model validationBoth internal validation and external validation wereperformed. Dermographic data for virtual subjects wasgenerated by randomly sampling from the actualdatasets. These virtual subjects were then given theappropriate dose and regimen as specified for eachstudy. Using these data, the PK/PD parameters weresimulated for each subject using the final populationPK/PD model parameters. For each dose and regimen
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 553
combination, 1000 virtual subjects were generated. Thesimulation reflected interindividual variability by settingthe interindividual parameter distributions to those esti-mated from the model. In addition, the simulationassumed perfect compliance with the dosing table andzero values for all intra-individual variability from theobservation equations.
For study 1101, in order to validate the model inter-nally, the simulation results and the observed data werecompared at each dose. As a guide, 80% predictionintervals and the median of the simulated values weresuperimposed on the scatter plots of the observed valuesfor total omalizumab, free IgE and total IgE.
For study 1305, in order to internally validate themodel, the observed median was compared with the95% prediction intervals for the median, which werecalculated as follows:
1 One thousand replications were generated includingthe same number of subjects as the observed numberin each combination of dose and regimen. Each rep-lication was made by resampling from the previouslysimulated dataset.
2 The median for each replication was calculated.3 The 2.5th and 97.5th percentiles of the 1000 medians,
as the end-points of the 95% prediction interval forthe median, were calculated.
For external validation, the observed serum concen-trations of omalizumab, free IgE and total IgE fromstudies 007, 008 and 009 that were not used in the modelbuilding were compared with model predictions. Forstudies 008 and 009, to ensure steady state, troughsamples had to be collected at least 240 days after thefirst dose, with a period after the last dose prior to thetrough sample within 2 days of the planned dose interval(14 or 28 days). The simulation was carried out usingregular dosing with the planned dose and dosing inter-val, and with the trough sample drawn one dosing inter-val after the dose administered 224 days after the firstdose.
Parameter uncertainty was not considered in the simu-lations. Values were calculated based on the NONMEMestimates for q, w and e. However, when making a pos-terior predictive assessment, as opposed to a predictiveevaluation of the data used to generate the model,parameters uncertainty should not be ignored. The stan-dard error (SE) of each parameter, obtained by theNONMEM $COVARIANCE procedure, was used as anestimate of uncertainty. An additional simulation usingthe SE of the q estimates was performed for the valida-tion of studies 008 and 009 according to the followingequation:
TVPARM zj j ij= +( ) × × ×θ δ0 0 . . . . . .
where Zij = (xi/xi0)(qij+dij) and dij ~ N(0,SE2 for qij).
Software used for modelling and simulationFor the model building and determination of individualPK/PD parameters, NONMEM (Version V Level 1.1)was used with the first-order conditional estimationmethod (METHOD = FOCE). S-Plus (version 6.1) wasused for the simulation, statistical computation andgraphics. For external validation, the simulation data setof trough concentration was generated by NONMEM.Noncompartmental analysis to compute terminal half-lives was carried out using WinNonlin (version 4.0.1).
ResultsIn the studies used in the model building (1101 and1305), 202 healthy subjects and patients were adminis-tered omalizumab. A total of 3192 samples (1037 oma-lizumab, 1191 total IgE and 964 free IgE) were used formodel building. Two hundred and seventy-five free IgEconcentrations that were above the upper limit of quan-tification (150 ng ml-1) were excluded. Seven hundredand seven patients were administered omalizumab instudies 007, 008 and 009; 531 patients who had evalu-able trough concentrations in these studies were used forthe external validation of the model. Demographic dataare summarized in Table 1.
The estimated PK/PD parameter values are shown inTable 3. The covariate–parameter effects (body weightfor omalizumab clearance and distribution volume andbaseline IgE for free IgE clearance and rate of IgE pro-duction) were included and confirmed as statisticallysignificant (P < 0.01). Interindividual variability for therandom effects associated with the PK/PD parametersranged from 13% (VX) to 40% (ka). Intra-individual vari-ability from the observation equations ranged from 17%to 22%. The standard error (SE) for the estimated fixed-effects parameters (q) ranged from 2% to 20% of q. Withthe exception of free IgE, the individual weightedresiduals, IWRES, showed a symmetric distributionaround zero through the whole range of predicted values(Figure 2). Free IgE showed asymmetry for higher pre-dicted values, as samples containing concentrations>150 ng ml-1 were not quantifiable.
To confirm the necessity for the expression allowingaffinity to vary with the ratio of omalizumab to IgE, thelog-likelihood NONMEM objective functions werecompared for models with and without variation in Kd.With concentration dependence allowed (a � 0), theNONMEM objective function decreased significantly by107.
N. Hayashi et al.
554 63:5 Br J Clin Pharmacol
In building the basic model, the influence of the broadrange of baseline IgE (IgE0) was not negligible and theoptimization process did not converge without the inclu-sion of covariates. Therefore, the basic model includedthe covariate of IgE0 on PE/f.
In the preliminary analysis, the influences of bodyweight, baseline IgE, age and sex on the PK/PD param-eters were evaluated visually using the scatter plotbetween POSTHOC estimations of each PK/PD param-eter and each demographic factor. As a result, thefollowing combinations of covariates and PK/PD param-eters were examined:
(1) IgE0 on CLE/f; (2) BW on CLX/f; (3) BW on VX/f; (4)BW on VC/f; (5) AGE on ka; (6) AGE on VX/f; (7) SEXon VX/f.
In the first examination step, the combinations of (1) to(4) were included in the model, and the significance was
confirmed by backward elimination. During this process(1) to (3) showed a significant change in the objectivefunction value (-2LL > 12.12, P < 0.001), and (4) didnot show a significant change. Baseline IgE was chosenas the covariate on PE/f and CLE/f, and the correlationbetween h(PE/f ) and h(CLE/f ) included the use of ablock statement in order to stabilize the model. Theinclusion of correlations, between these h’s gave signifi-cant drops in the objective function value.
In a second examination step, combinations of (5) to(7) were in corporated one by one into the model built inthe above step. No significant change in the objectivefunction value was observed for (5) to (7).
As the result, the final model was developed toinclude the covariates shown in Table 3. The apparentclearance of omalizumab (CLX /f ) and free IgE (CLE /f ),the apparent rate of IgE production (PE/f ) and apparentdistribution volume of omalizumab (VX/f ) depend on
Table 3Population estimated model parametersand related information
PK/PD parameterPopulation mean[q (SE for q)]
Interindividualvariance(w,% CV)
CLx/f (ml h-1)* 7.32 (0.153) 20.3CLX /f exponent for body weight 0.911 (0.135)
DCLC /f (ml h-1) 5.86 (0.920) 34.9CLE/f (ml h-1)† 71.0 (4.68) 25.3
CLE /f exponent for baseline IgE -0.281 (0.0312)PE /f (mg h-1)† 30.3 (2.04) 23.1
PE /f exponent for baseline IgE 0.657 (0.0301)Correlation between h(CLE/f) and h(PE/f) 0.968
VX/f (ml)*‡ 5900 (107) 13.0VX/f exponent for body weight 0.658 (0.100)
VC /f (ml) 3630 (223) 25.0ka (h-1) 0.0200 (0.00114) 39.9Kd0 (nm) 1.07 (0.118)a 0.157 (0.0306)
Intra-individualvariance(s,% CV)
Omalizumab 16.7Total IgE 21.1Free IgE 21.8
NONMEM objective function value: 37375.330. Total no. of observation records:3192. Total no. of individuals: 202. *The value at 61.1 kg of body weight. †Thevalue at 482.4 ng ml-1of baseline IgE (30.3 mg h-1 = 0.159 nmol h-1). ‡VE/f wasassumed to be the same as VX/f.
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 555
baseline IgE and body weight according to the followingequations:
CL fX body weight 61.1= × ( )7 32 0 911. .
CL fE baseline IgE 482.4= × ( )−71 0 0 281. .
P fE baseline IgE 482.4= × ( )30 3 0 657. .
V fX = × ( )5900 61 1 0 658body weight . .
Thus, doubling body weight increases the apparentclearance and volume of distribution of omalizumab by(20.911 - 1) · 100% = 88% and (20.658 - 1) · 100% = 58%,respectively. Doubling baseline IgE decreases the appar-ent clearance of free IgE by 18% and increases theapparent rate of IgE production by 58%.
The results of internal validation of the model areshown in Figure 3 for the single-dose study 1101 and in
Figure 4 (upper panel) for the multiple-dose study 1305.Free IgE is predicted to decrease as the dose of omali-zumab increases from 75 to 375 mg. Individual observedvalues were mostly within the 80% prediction intervalsand the extent of interindividual variability specified inthe model was similar to that observed. Some randomdeviations occur in the free IgE concentrations for the150 mg dose group. However, the number of pointswithin the 80% prediction intervals of free IgE for alldose groups was 390 of 491, or 79.4%. Even though theobserved values of five of 12 subjects in the 150-mggroup were not within the 80% prediction intervals, abinominal test P-value of 0.073 showed that this devia-tion was not significant. The observed median values offree IgE concentration in this group were mostly cap-tured within the 95% prediction intervals for themedians (data not shown). Figure 4 (upper panel, study
5 10 50 100
500 100 150
500
5
10
50
100
500
IPRED for free IgE (ng/mL)
Obs
erve
d fr
ee I
gE (
ng/m
L)
50 100 500 500050
100
500
1000
5000
IPRED for total IgE (ng/mL)O
bser
ved
tota
l IgE
(ng
/mL
)0.5 5.0 50.0
0.5
5.0
50.0
IPRED for Omalizumab (ug/mL)
Obs
erve
d O
mal
izum
ab (
ug/m
L)
–1.0
–0.5
0.0
0.5
1.0
–1.0
–0.5
0.0
0.5
1.0
–1.0
–0.5
0.0
0.5
1.0
IPRED for free IgE (ng/mL)
IWR
ES
0 1000 2000 3000 4000 5000
IPRED for total IgE (ng/mL)
IWR
ES
0 20 40 60 80 100
IPRED for Omalizumab (ug/mL)IW
RE
S
Figure 2Diagnostic plots for the model. The upper panels show the goodness-of-fit through the relationship between the estimated values (IPRED) and the
corresponding observed values with respect to the line of identity. The lower panels show the distributions of individual weight residuals (IWRES) for
free and total IgE and omalizumab. The broken lines indicate the S-Plus LOESS local regression lines. The upper limit of quantification for free IgE was
150 ng ml-1. Observations above this value were not quantifiable and could not be plotted
N. Hayashi et al.
556 63:5 Br J Clin Pharmacol
1305) shows that the observed median values after mul-tiple dosing were mostly captured within the 95% pre-diction intervals.
The results of the external validation are shown inFigure 4 (lower panel) for the multiple-dose study 007,and in Figure 5 for the distributions of predicted andobserved predose trough samples at steady state (studies008 and 009). The observed median values followingmultiple doses of omalizumab are close to the 95%prediction intervals of the median (Figure 4).
The shapes of the predicted and observed distribu-tions were similar (Figure 5), and the 95% predictionintervals included the observed median in most cases.Although one may initially conclude that the model isnot predictive, as >5% of the observed medians wereoutside the 95% prediction intervals, this is most likelydue to the posterior predictive simulation not accounting
for uncertainty in the NONMEM estimated values. Toovercome this, an additional simulation was performedwith uncertainty added to each parameter. The resultantuncertain 95% prediction intervals for the medians areshown in Figure 5 as horizontal bars. The intervals didnot broaden to any great extent, but now there were nosignificant deviations of observed medians outside theprediction intervals for total IgE and, most relevent toclinical efficacy, free IgE (binomial test P = 0.2262).
DiscussionConsistent with other therapeutic monoclonal antibod-ies [26] and with previously reported results [19], anincrease in total IgE was observed during treatmentwith omalizumab. This increase is caused by both aredistribution of ligand from extravascular sites, and adecrease in its rate of elimination due to slower clear-
Om
aliz
umab
co
nc (
ug/m
L)
0
5
10
15
Om
aliz
umab
co
nc (
ug/m
L)
0
20
40
60
80
DOSE: 75 mg
Tota
l IgE
(ng
/mL
)
0
2000
4000
6000
Tota
l IgE
(ng
/mL
)
0
2000
4000
6000
Tota
l IgE
(ng
/mL
)
0
2000
4000
6000
Tota
l IgE
(ng
/mL
)
0
2000
4000
6000
DOSE: 375 mg
Free
IgE
(ng
/mL
)
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Days0 20 40 60 80
Om
aliz
umab
co
nc (
ug/m
L)
0
10
20
30
DOSE: 150 mg
Days0 20 40 60 80
Om
aliz
umab
co
nc (
ug/m
L)
0
20
14
60
DOSE: 300 mg
Days0 20 40 60 80
Days0 20 40 60 80
5
10
50
100Fr
ee I
gE (
ng/m
L)
5
10
50
100
Free
IgE
(ng
/mL
)
5
10
50
100
Free
IgE
(ng
/mL
)
5
10
50
100
Figure 3Individual observed serum concentrations of omalizumab, total and free IgE in study 1101 and the 80% prediction intervals of the model
predictions.The circles are individual observed values and lines are 10%, 50% and 90% percentiles at each time point calculated from 1000
simulated subjects for each cohort. The dashed line indicates the time of omalizumab administration. The upper limit of quantification for free IgE was
150 ng ml-1. Observations above this value were not quantified and could not be plotted
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 557
ance of the omalizumab–IgE complex compared withthat of the free ligand [15–17]. The presentmechanism-based direct-ligand binding model includesboth of these mechanisms, giving rise to model param-eters that are physiologically and physicochemicallyrelevant.
Values of the apparent clearances obtained for freeomalizumab and free IgE were 7.32 and 71.0 ml h-1 fora typical 61.1-kg patient with 482.4 ng ml-1 baselineIgE. The typical apparent distribution volumes of both
compounds were 5900 ml. Therefore, the half-lives ofomalizumab and IgE were 23 and 2.4 days, very close topreviously reported values of 23 and 2.5–2.7 days forhuman IgG [24, 25] and IgE [24, 25, 27]. The meanhalf-life of total omalizumab calculated noncompart-mentally in study 1101 was 18.2 days. This difference of5 days compared with the value for free omalizumab isprobably due to the fact that noncompartmental analysiscalculates the clearance of the sum of free and com-plexed omalizumab and, therefore, the value is a mixture
(Days)
Study 1305
Study 007
Om
aliz
umab
conc
(ug
/mL
) DOSE: 300 mg/ 3 w N = 55
Tota
l IgE
(ng/
mL
)
Tota
l IgE
(ng/
mL
)
Free
IgE
(ng/
mL
)
DOSE: 300 mg/ 4 w N = 100
Om
aliz
umab
conc
(ug
/mL
)
0 50 100 150 0 50 100 150 0 50 100 1500
40
80
120
0
20
40
DOSE: 225 mg/ 2 w N = 18
0 50 100 150
Tota
l IgE
(ng/
mL
)
0
2000
4000
0
2000
4000
0
2000
4000
0
20004000
0
20004000
Free
IgE
(ng/
mL
)
Om
aliz
umab
conc
(ug
/mL
)
0
40
80
Om
aliz
umab
conc
(ug
/mL
)DOSE: 150 mg/ 4 w N = 71
0 50 100 150
0
50
500
0
50
500
0
50
500
0 50 100 150
0
50
500
0
50
500
0 50 100 150
Free
IgE
(ng/
mL
)
0 50 100 150
0 50 100 150
0 50 100 150
Free
IgE
(ng/
mL
)
0 50 100 150
0
40
80
0
40
80
Om
aliz
umab
conc
(ug
/mL
)
0 50 100 150
0 50 100 150
Free
IgE
(ng/
mL
)
0 50 100 150
Tota
l IgE
(ng/
mL
)
DOSE: 300 mg/ 4 w N = 42
0 50 100 150
Tota
l IgE
(ng/
mL
)
Figure 4Median observed serum concentrations of omalizumab, total and free IgE in studies 1305 and 007, and the 95% prediction intervals of the median
predicted time course of the respective compound for the given dosing regimen. The circles are observed medians at each time point for each dose
and regimen combination, and the lines are the 95% prediction intervals for medians calculated from 1000 simulated subjects at each time point.
The data for two dose groups in study 1305 were omitted because the number of subjects was <10
N. Hayashi et al.
558 63:5 Br J Clin Pharmacol
0 10 20 30 40
0 10 20 30 40
0.0
0.04
0.10
Free IgE (ng/mL), N = 78
Pro
babi
lity
dens
ity
0 2000 4000 6000 80000.0
0.0002
0.0005
Total IgE (ng/mL), N = 78
Pro
babi
lity
dens
ity
225 mg/2 weeks
0 50 100 150 200 250
0.0
0.010
0.020
0.0
0.04
0.10
0.0
0.0002
0.0005
0.0
0.010
0.020
0.0
0.04
0.0
0.04
0.10
0.0
0.0002
0.0
0.0006
0.0005
0.0
0.010
0.020
Omalizumab conc (ug/mL), N = 78
Pro
babi
lity
dens
ity
Free IgE (ng/mL), N = 53
Pro
babi
lity
dens
ity
0 2000 4000 6000 8000Total IgE (ng/mL), N = 53
Pro
babi
lity
dens
ity
300 mg/2 weeks
0 50 100 150 200 250
0 10 20 30 40 0 2000 4000 6000 8000 0 50 100 150 200 250
Omalizumab conc (ug/mL), N = 53
Pro
babi
lity
dens
ity
Free IgE (ng/mL), N = 34
Pro
babi
lity
dens
ity
Total IgE (ng/mL), N = 34
Pro
babi
lity
dens
ity
375 mg/2 weeks
Omalizumab conc (ug/mL), N = 34P
roba
bilit
y de
nsit
y
Free IgE (ng/mL), N = 104
Pro
babi
lity
dens
ity
0 1000 2000 3000
0 1000 2000 3000
Total IgE (ng/mL), N = 104
Pro
babi
lity
dens
ity
150 mg/4 weeks
0 20 40 60 80 100
0 20 40 60 80 100
0.0
0.02
0.05
0.0
0.04
0.0
0.0006
0.0
0.02
0.05
Omalizumab conc (ug/mL), N = 104
Pro
babi
lity
dens
ity
Free IgE (ng/mL), N = 107
Pro
babi
lity
dens
ity
Total IgE (ng/mL), N = 107
Pro
babi
lity
dens
ity
300 mg/4 weeks
Omalizumab conc (ug/mL), N = 107
Pro
babi
lity
dens
ity
0 10 20 30 40
0 10 20 30 40
Figure 5Frequency distribution of trough concentrations at steady state. Comparison of observed values and model predictions after the administration of
omalizumab every 2 or 4 weeks in studies 008 and 009. The histograms are the observed distributions of trough concentrations, and the curve
shows the distribution of trough concentrations for a simulation of 1000 subjects based on the parameters estimated from studies 1101 and 1305.
The vertical line indicates the median of observed values and the hatched area indicates the 95% prediction intervals of the median calculated from
the simulation
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 559
of the more slowly cleared free together with themore rapidly cleared complex. The clearance of theomalizumab–IgE complex was estimated to be5.86 ml h-1 higher than that of free omalizumab. It islikely that the presence of IgE bound to omalizumab IgGinterferes with the ability of the Brambell FcRn receptor[13] to rescue the IgG from lysosomal degradation.However, the fact that clearance of the complex is not asrapid as that of free IgE suggests that some level ofrescue does occur, leading to an accumulation of totalIgE compared with that observed at baseline.
When corrected for the 62% subcutaneous bioavail-ability of omalizumab [28], the absolute distributionvolumes for a typical 61.1-kg subject are 3660 ml for freeomalizumab, 2250 ml for the complex (Table 3). Thelatter is very close to the volume of plasma (2130 ml) fora subject of that body weight [29]. The volumes foromalizumab and IgE are somewhat larger, probablyreflecting distribution to the tissue interstitium [30–32]. Itis known that the concentration of immunoglobulin ininterstitial fluid is lower than in blood [30–32], due torestricted vascular endothelial permeation and continuallymphatic drainage. Therefore, as expected, the IgG–IgEcomplex, with its higher molecular weight (340–1000 kDa) and hence lower tight-junctional permeabilitythan free IgG (150 kDa) or free IgE (190 kDa), willappear to have a smaller distribution volume. Further,even if the complex were to permeate, due to the lowconcentration, any molecules of the complex should dis-sociate. Therefore, it is concluded that the observedincrease in total serum IgE is caused not only by differ-ences in clearance between IgE and complex, but also bya more restricted distribution volume.
Following internal and external validation, the modeldescribed the pharmacokinetic and pharmacodynamicresponses over a broad range of conditions with respectto different subpopulations, doses and dose intervals. Inparticular, the response at steady state was determinedby only three clearance parameters and the rate of IgEproduction. Kd was assumed to be identical in allpatients, but was dependent upon the molar ratio of totalomalizumab to total IgE.
Clearance of free IgE and the rate of production ofIgE were shown to be accurately predicted by baselineIgE concentration; clearance and volume of distributionof free omalizumab by body weight. Therefore, the phar-macodynamic response is mainly a function of bodyweight, baseline IgE and dosage. The results of thesimulations were obtained using only population PK/PDparameters from the model building, body weight andbaseline IgE concentration in the validation dataset. Thesimulations, based on the two Japanese studies, were
predictive of the distribution of the free IgE biomarkerresponse in an independent non-Japanese population.
In conclusion, a mechanism-based population PK/PDmodel was established for omalizumab binding to IgEand its predictability was confirmed for the clinicallyimportant variable, free IgE. There was no significantdeviation of predicted from observed median total andfree IgE trough concentrations at steady state. Themodel, even though its parameters were estimated fromsmall clinical pharmacological studies, mimicked theextent of free IgE variability in larger long-term PhaseIII studies, the predicted medians consistently beingwithin 25% of observed values and the tails of the pre-dicted distributions being close to those of the observeddata across a fivefold range of dose. Furthermore, sincethe model was developed using Japanese patient data,and the posterior predictive evaluation was against datafrom Whites, there are unlikely to be notable differencesin omalizumab pharmacokinetics and IgE pharmacody-namics between the populations.
Finally, the general model, specifying a monoclonalantibody, or other agent, binding to a target ligand in anequilibrium reaction with a fixed stoichiometry, is ofgeneral applicability given the increasing number of bio-technologically derived molecules being discovered anddeveloped as therapeutic agents. The model describedallows for the determination not only of drug character-istics, but also of those of an endogenous ligand, includ-ing half-life and rate of production, without directadministration of the natural ligand. This approachshould be a powerful tool in the understanding of therole of many potential target ligands in the pathophysi-ology of diseases.
Conflict of interestAll authors work for Novartis Pharmaceuticals, manu-facturers of omalizumab (trade mark Xolair™). P.J.L.owns shares in Novartis Pharmaceuticals AG and Novar-tis Corporation has granted options to W.M.S. to pur-chase American Depositary Shares of Novartis AGsubject to terms of the stock incentive plan of thecompany.
We thank Dr Günther Kaiser, Dr Gilles-Jacques Riviere,Dr Laurence Brookman, Dr Jean-Louis Steimer, DrRyosei Leo Kawai, Dr Yoko Wakui and Mr Vincent Buch-heit for their advice and support.
References1 Ishizaka K, Ishizaka T. Identification of gamma IgE antibodies as
a carrier of reaginic activity. J Immunol 1967; 99: 1187–98.
N. Hayashi et al.
560 63:5 Br J Clin Pharmacol
2 Johansson SGO, Bennich H. Immunological studies of anatypical (myeloma) immunoglobulin. Immunology 1967; 13:381–94.
3 Ishizaka K, Ishizaka T. Biological function of IgE antibodies andmechanisms of reaginic hypersensitivity. Clin Exp Immunol1970; 6: 25–42.
4 Presta LG, Lahr SJ, Shields RL, Porter JP, Gorman CM, FendlyBM, Jardieu PM. Humanization of an antibody directed againstIgE. J Immunol 1993; 151: 2623–32.
5 Jardieu P. Anti IgE therapy. Curr Opin Immunol 1995; 7:779–82.
6 Jardieu P, Schoenhoff M, Thomas D, Fox J, Presta L. IgEmodulation: potential for anti IgE therapy in asthmatic disease.In: Genetics to Quality of Life of the Optimal Treatment andManagement of Asthma, eds Chanez P, Bousquet J, Michel FB,Godard P. Seattle: Hogrefe and Huber 1996: 193–7.
7 Heusser C, Jardieu P. Therapeutic potential of anti-IgEantibodies. Curr Opin Immunol 1997; 9: 805–13.
8 Boushey HA, Fahy JV. Monoclonal anti IgE antibody E25 therapyfor asthma. Res Immunol 1998; 149: 189–92.
9 Fick RB. Therapy of allergic pulmonary diseases with anti IgEantibodies. Pediatr Pulmonol Suppl 1999; 18: 115–7.
10 Holgate ST, Corne J, Jardieu P, Fick RB, Heusser CH. Treatmentof allergic airways disease with anti IgE. Allergy 1998; 53:83–8.
11 Jardieu PM, Fick RB Jr. IgE inhibition as a therapy for allergicdisease. Int Arch Allergy Immunol 1999; 118: 112–5.
12 Patalano F. Injection of anti IgE antibodies will suppress IgE andallergic symptoms. Allergy 1999; 54: 103–10.
13 Busse W, Corren J, Lanier BQ, McAlary M, Fowler-Taylor A,Cioppa GD, van As A, Gupta N. Omalizumab, anti-IgErecombinant humanized monoclonal antibody, for the treatmentof severe allergic asthma. J Allergy Clin Immunol 2001; 108:184–90.
14 Adelroth E, Rak S, Haahtela T, Aasand G, Rosenhall L,Zetterstrom O, Byrne A, Champain K, Thirlwell J, Cioppa GD,Sandstrom T. Recombinant humanized mAb-E25, an anti-IgEmAb, in birch pollen-induced seasonal allergic rhinitis. J AllergyClin Immunol 2000; 106: 253–9.
15 Scherrmann JM, Terrien N, Urtizberea M, Pierson P, Denis H,Bourre JM. Immunotoxicotherapy: present status and futuretrends. J Toxicol Clin Toxicol 1989; 27: 1–35.
16 Sabouraud AE, Urtizberea M, Cano NJ, Grandgeorge M,Rouzioux JM, Scherrmann JM. Colchicine-specific Fab fragmentsalter colchicines disposition in rabbits. J Pharmacol Exp Ther1992; 260: 1214–9.
17 Valentine JL, Owens SM. Antiphencyclidine monoclonal antibodytherapy significantly changes phencyclidine concentrations inbrain and other tissues in rats. J Pharmacol Exp Ther 1996;278: 717–24.
18 Lobo ED, Hansen RJ, Balthasar JP. Antibody pharmacokineticsand pharmacodynamics. J Pharmaceut Sci 2004; 93: 2645–68.
19 Meno-Tetang GML, Lowe PJ. On the prediction of the humanresponse: a recycled mechanistic PK/PD approach. Basic ClinPharmacol Tox 2005; 96: 182–92.
20 US BLA ACM. XOLAIR™, BB IND 5369 Final. Available athttp://www.fda.gov/ohrms/dockets/ac/03/briefing/3952B1_01_Genentech-Xolair.pdf (last accessed: 17 October2006).
21 Soler M, Matz J, Townley R, Buhl R, O’Brien J, Fox H, Thirlwell J,Gupta N, Della Cioppa G. The anti-IgE antibody omalizumabreduces exacerbations and steroid requirement in allergicasthmatics. Eur Respir J 2001; 18: 254–61.
22 Liu J, Lester P, Builder S, Shire SJ. Characterization of complexformation by humanized anti-IgE monoclonal antibody andmonoclonal human IgE. Biochemistry 1995; 34: 10474–82.
23 Junghans RP. Finally! The Brambell receptor (FcRB). Mediator oftransmission of immunity and protection from catabolism forIgG. Immunol Res 1997; 16: 29–57.
24 Waldmann TA, Strober W. Metabolism of immunoglobulins. ProgAllergy 1969; 13: 1–110.
25 Frazer JK, Capra JD. Immunoglobulins: Structure and function.In: Fundamental Immunology, 4th edn, ed Paul WE,Philadelphia: Lippincott-Raven 1999: 37–74.
26 Charles P, Elliott MJ, Davis D, Potter A, Kalden JR, Antoni C,Breedveld FC, Smolen JS, Eberl G, de Woody K, Feldmann M,Maini RN. Regulation of cytokines, cytokine inhibitors, andacute-phase proteins following anti-TNF-alpha therapy inrheumatoid arthritis. J Immunol 1999; 163: 1521–8.
27 Waldmann TA, Iio A, Ogawa M, McIntyre OR, Strober W. Themetabolism of IgE. Studies in normal individuals and in apatient with IgE myeloma. J Immunol 1976; 117: 1139–44.
28 Xolair Omalizumab for Subcutaneous Use. Package insert. SanFrancisco, CA: Genentech, Inc. 2003.
29 Streeten DHP, Bell DS. Circulating blood volume in chronicfatigue syndrome. J Chronic Fatigue Syndrome 1998; 4:3–11.
30 Bill A. Plasma protein dynamics. Albumin and IgG capillarypermeability, extravascular movement, and regional blood flowin unanesthetized rabbits. Acta Physiol Scand 1977; 101:28–42.
31 Juweid M, Strauss HW, Yaoita H, Rubin RH, Fischman AJ.Accumulation of immunoglobulin G at focal sites ofinflammation. Eur J Nucl Med 1992; 19: 159–65.
32 Hedger MP, Hettiarachchi S. Measurement of immunoglobulinG levels in adult rat testicular interstitial fluid and serum. JAndrol 1994; 15: 583–90.
The population PK and PD of omalizumab
Br J Clin Pharmacol 63:5 561