45. Cresci 2004
Transcript of 45. Cresci 2004
2153_book.fm Page 151 Monday, October 18, 2004 8:00 AM
10
Fiber and Probiotics: Prevention of ICU Infections with Bioecological Control and Synbiotic TreatmentStig BengmarkLund University
CONTENTS
10.1 Introduction .........................................................................................................................15210.2 Interrelated Conditions........................................................................................................152
10.2.1 Exaggerated Immune Response — The Cause? ...................................................15310.2.2 Neuro–Endocrine Control of Stress of APR/CPR.................................................154
10.3 The Gut — An Important Immunological Organ...............................................................15410.4 Iatrogenic Suppression of Resistance to Disease ...............................................................154
10.4.1 Excessive and Prolonged Use of Antibiotics ........................................................15510.4.2 Inhibition of Salivation ..........................................................................................15510.4.3 Inhibition of GI Secretions ....................................................................................15510.4.4 Prophylactic Nasogastric Decompression .............................................................15610.4.5 Postoperative Drainage of Body Cavities..............................................................15610.4.6 Preoperative Bowel Preparation.............................................................................15610.4.7 Transfusion with Old Stored Blood.......................................................................15710.4.8 Overloading with Nutrients (Hyperalimentation)..................................................157
10.5 Often Neglected Measures ..................................................................................................15710.5.1 Aggressive Perioperative Enteral Nutrition ...........................................................15810.5.2 Tight Control of Blood Glucose ............................................................................15810.5.3 Supply of Antioxidants ..........................................................................................15810.5.4 Supply of Plant Fibers ...........................................................................................15910.5.5 Supplementing Flora ..............................................................................................160
10.6 A Dual Digestive System....................................................................................................16010.6.1 Mucosal Homeostasis ............................................................................................161
10.7 Combination of Pro- and Prebiotics Equals Synbiotics .....................................................16110.7.1 Acute Pancreatitis...................................................................................................16210.7.2 Abdominal Surgery ................................................................................................16210.7.3 Liver Transplantation .............................................................................................16310.7.4 Other Conditions ....................................................................................................164
10.8 Future Aspects .....................................................................................................................16410.9 Practice Points .....................................................................................................................165References ......................................................................................................................................166
1510-8493-2153-0/05/$0.00+$1.50© 2005 by CRC Press
152
Nutrition Support for the Critically Ill Patient: A Guide to Practice
AU: What patients?
U: “ICU”?
AU: Pro-noun ref unclear.
2153_book.fm Page 152 Monday, October 18, 2004 8:00 AM
10.1 INTRODUCTION
To a large extent, modern medicine has failed in its ambition to control both acute and chronicdiseases. Acute diseases, defined as medical and surgical emergencies such as myocardial infarction,stroke, and severe pancreatitis and those related to advanced medical and surgical treatments, suchas stem cell transplantation or advanced surgical operations, have an unacceptably high morbidityand comorbidity. Furthermore, the world suffers an epidemy of chronic diseases of a dimensionnever seen before, and these diseases are now like a prairie fire spreading to so-called developingcountries. Chronic diseases, including such diseases as cardiovascular and neurodegenerative con-ditions, diabetes, stroke, cancers, and respiratory diseases, constitute 46% of the global diseaseburden and 59% of global diseases. Each year, approximately 35 million individuals die in condi-tions related to chronic diseases.1 Similarly, the morbidity related to advanced medical and surgicaltreatments and emergencies, especially infectious complications, is also fast increasing. Sepsispresently increases in the U.S. by 1.5% per ten years and constitutes the tenth most common causeof death in that country.2
Each year, severe, often life-threatening infections occur in the U.S. in approximately 751,000individuals, and approximately 215,000 (29%) of these individuals will die.2,3 ICU mortalityrealistically is higher than officially reported: Vincent et al. recently reported that estimates ofintensive care unit (ICU) mortality are most likely conservative, because deaths of ICU patientsare often attributed to the original condition.4 More than half of the patients (51%), or 383,000,are treated in ICUs and about 130,000 are managed at intermediary-type care units with facilitiesfor ventilation. The extra treatment cost is calculated to be $22,100 per case, and the annual costin the U.S. alone for this treatment is at the level of about $17 billion.3
10.2 INTERRELATED CONDITIONS
The two seemingly disparate groups — those suffering chronic conditions and those developingposttreatment and ITU morbidity — are in many aspects related. Both types of condition seem tobe expressions of a failing innate immune system. To a large extent, it is also patients with imminentor obvious chronic diseases who are affected by significantly increased surgical and ICU morbidity.In fact, about half of the patients affected by sepsis are in the age group over 65 years, and 48%of the patients are neutropenic.5 Both groups of diseases are characterized by exaggerated immuneresponse with profound, although somewhat different, changes in both acute-phase proteins andcytokine response.6
The reaction of the body to acute physical and psychological stress is similar, irrespective ofthe cause: microbial invasion, allergic reaction, surgical operation, trauma, burn, tissue ischemia,tissue infarction, strenuous exercise, childbirth, or mental trauma. It is often referred to as acute-phase response (APR). The common clinical symptoms of APR are fever, chills, somnolence, andanorexia, which are accompanied by profound changes in plasma proteins, especially in so-calledacute-phase proteins (APPs) but also in lipids, minerals, hormones, cytokines, coagulation factors,and cellular components of the blood. Similar reactions are observed in patients with subclinicalor obvious chronic diseases: arteriosclerosis, Alzheimer’s, cancer, coronary heart disease, diabetes,chronic liver disease, chronic renal disease, rheumatoid arthritis, and many other chronic diseases.Elevations in acute-phase proteins, cytokines, and other signal molecules, although less pronounced,are regularly observed during weeks and months even before the patients clinically manifest disease.
The dominant clinical manifestations of what can be called chronic-phase response (CPR) are,however, somewhat different from those of APR and consist mainly of anorexia, asthenia, anemia,decline in food intake, fatigue, muscle wasting, depressed mood, and often clinically manifestmental depression. Although the extent of changes observed differs between APR and CPR,Table 10.1 lists common conditions for both. The changes in plasma proteins, lipids, minerals,
A
Fiber and Probiotics Prevention of ICU Infections
153
U: Pro-oun ref nclear.
2153_book.fm Page 153 Monday, October 18, 2004 8:00 AM
hormones, cytokines, and cellular components of blood are somewhat different. In APR, the increasein cytokines and acute-phase proteins is instant and reaches very high levels within a few hours,but is often more or less over within 10 to 14 days; in CPR, they remain at levels that are not sohigh, but are clearly increased, over months and years. While in APR, APP production constitutesapproximately 30% of the body’s total protein synthesis; it is only about 5% in CPR.8 Increase inC-reactive protein is prominent in APR, whereas increase in fibrinogen dominates in CPR.8
10.2.1 EXAGGERATED IMMUNE RESPONSE — THE CAUSE?
Individuals affected by metabolic syndrome (MS), a condition often affecting and preceding chronicdiseases, seem to respond to stress with an exuberant acute or chronic superinflammation, mani-fested by exaggerated and prolonged release of proinflammatory cytokines, such as IL-6, and acutephase proteins, such as C-reactive protein, but also plasminogen activator inhibitor 1 (PAI-1) —see reference for more information.6 IL-6 and PAI-1 are often regarded as prognosticators ofoutcome both in acute conditions, such as after operation or trauma, myocardial infarction, orpancreatitis, and in semichronic or chronic inflammatory conditions, such as arthritis, mentaldepression, or Alzheimer’s. The overwhelming IL-6 response (e.g., prolonged or extreme elevationsof circulating IL-6) seen in patients suffering from conditions such as infection, burns, or traumais strongly associated with severe exacerbation of the disease, such as acute respiratory distresssyndrome (ARDS) and multiple organ failure (MOF).9 The effect of overwhelming acute-phaseresponse on outcome is well demonstrated in a study in human liver transplantation; all patientswho had a sixfold or larger increase in the cytokines TNFα and IL-6 during the later phase of theoperation developed sepsis in subsequent postoperative days.10
Among the changes observed in overexuberant acute-phase response are augmented endothelialadhesion of polymorphonuclear (PMN) cells, increased production of intracellular adhesion mol-ecule-1 (ICAM-1) and priming of the PMNs for an oxidative burst, release of proinflammatoryplatelet activating factor (PAF), and, associated with this, a delay in PMN apoptosis.9 Visceraladipocytes are, compared to subcutaneous fat cells, known to secrete many more free fatty acidsbut also three times as much IL-6 and PAI-1 per gram of tissue, observations that well explain thehigh risk of disease in visceral obesity.11,12 The load of these and other molecules on the liver can
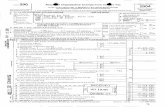
TABLE 10.1Conditions of Acute and Chronic Phase Response
APR and CPRGeneral hypermetabolism with higher resting energy expenditureIncreased hepatic gluconeogenesisIncreased glucose turnover and decreased muscle glucose uptakeHyperlipidemiaAdipose tissue lipolysisIncreased production of nonesterified fatty acidsIncreased whole-body protein turnoverIncreased hepatic protein synthesisDecreased muscle amino-acid uptakeInsulin resistanceIncreased production of cytokinesIncreased endotoxin in bloodElevated levels of catecholamines, cortisol, and glucagon
Sources: Simons, J.P., Schools A.M., Buurman, W.A., Wouters, E.F., Clin. Sci. 97, 215, 1999; and Preston, T., Slater, C.,McMillan, D.C., et al., J. Nutr. 128, 1355, 1998.
Anu
154
Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 154 Monday, October 18, 2004 8:00 AM
vary a thousand times or more because the amount of fat in the abdomen varies among individualsfrom a few milliliters to about six liters in persons with gross obesity.13
10.2.2 NEURO–ENDOCRINE CONTROL OF STRESS OF APR/CPR
The neuro–endocrine control on resistance to disease is important. Glial cells are embryologicallyand functionally related to macrophages and have the capacity to synthesize and secrete a wholerange of cytokines, such as IL1, IL2, IL4, IL6, and TNFα. In stress and other critical conditions,do these cytokines have pronounced effects on the hypothalamic–pituitary–adrenal (HPA) axis andthe function of the involved organs? Cytokines such as IL-1, IL-6, and TNFα are known to stimulatehypothalamic synthesis and secretion of corticotropin-releasing hormone, vasopressin, and otherhormones known to have profound regulatory effects. In acute conditions, activation in the CNSof cytokines will lead to symptoms such as anorexia, drowsiness, depressed mood, sleepiness,coma, and increased body temperature and, in chronic conditions such as neuro-degenerativediseases, will contribute to the destruction of neurons, cell death, and dementia.
The glial cells respond to the same stimuli as macrophages, and fatty infiltration of or otherchallenges to these cells, especially in the hypothalamic region, contribute to an exaggerated andprolonged immune response. One of the main functions of the HPA response seems to be to controland prevent overexuberant acute- (and chronic-) phase and immune responses. This also explainswhy principal immunoregulatory organs, such as Peyer’s patches, lymph nodes, thymus, and spleen,are abundantly supplied with sympathetic and parasympathetic autonomic nerves.15 Vasoactiveintestinal peptides, secreted by nerves in the Peyer’s patches, regulate the traffic of immunocom-petent cells through the small bowel wall and control the immune function of the gut.16
10.3 THE GUT — AN IMPORTANT IMMUNOLOGICAL ORGAN
The disease per se — but also nutrition and drugs supplied, changes in physical activity, sleep,mood, age, gender, circadian rhythm, and body temperature — will heavily influence lymphocytefunction, production of immunoglobulins, and resistance to disease. It is not always realized thatabout 80% of the total immunoglobulin-producing cells of the body are localized in lamina propriaof the gut and that large amounts of immunoglobulins, especially IgA, are released daily into thegut lumen.16 The synthesis of IgA is highly dependent on T-cells, and several cytokines producedby activated lymphocytes influence different steps in the IgA differentiation pathway.17 Transform-ing growth factor-β (TGF-β) in mice has been found to be the crucial “switch” factor, but othercytokines, such as IL2, IL5, and IL10, are also involved — see reference for more information.18
10.4 IATROGENIC SUPPRESSION OF RESISTANCE TO DISEASE
Multiple external and internal factors contribute to reduced resistance to disease and to immuno-paresis, especially in predisposed individuals. Also, some clinical measures can add to this condi-tion. It is especially important in this type of care that every single treatment is based on solidscientific evidence. We must admit that several measures, common in perioperative and ICUmanagement, seem not to be supported by scientific evidence, as required in modern medicine.Some such measures might also negatively affect the innate immune system, reduce resistance, andcontribute to secondary morbidity. These treatments, often instituted at a time when the demandfor scientific evidence was not as strict as it is today, should be reevaluated. Some treatments, whenstudied, might have well documented beneficial effects — but might also be accompanied bysignificant negative consequences that exceed the observed beneficial effects. Among these mea-sures to study further are:
Fiber and Probiotics Prevention of ICU Infections
155
2153_book.fm Page 155 Monday, October 18, 2004 8:00 AM
• Excessive and prolonged antibiotic treatment• Inhibition of salivation• Inhibition of gastrointestinal secretions• Prophylactic nasogastric decompression• Routine postoperative drainage of body cavities• Preoperative bowel preparation and postoperative enemas• Extensive transfusion with old stored blood• Overloading with nutrients, or hyperalimentation
10.4.1 EXCESSIVE AND PROLONGED USE OF ANTIBIOTICS
Many, if not most, modern pharmaceuticals seem to have a negative influence on immune functionand resistance to disease. As an example, it has been known for more than 50 years that supply ofantibiotics increases susceptibility to new infections.19 It has also been shown that administrationof antibiotics results in suppression of various macrophage functions, demonstrated by chemilu-minescence response, chemotactic motility, and bactericidal and cytostatic ability.20,21 Also, manyother commonly used drugs might have similar effects, although these have not been properlystudied. Numerous clinical studies show clearly that appropriately timed, short-term, most often“single shot” prophylaxis is as effective as multiple-dose prophylaxis and should not have the samenegative consequences on the immune system as are obtained with prolonged treatments.22–24
Restriction of prolonged treatment has long been recommended, but clinical policy is difficult tochange. Antibiotics are still heavily overprescribed in connection with surgery as well as for ICUpatients.25
10.4.2 INHIBITION OF SALIVATION
The amount of GI secretion in an adult is as much as 10 l/d; saliva is about 2.5 l, and another 2.5 lare gastric secretions. These secretions are extremely rich in immunosupportive factors, such asimmunoglobulins, lactoferrin, lysozyme, fibronectin, and mucin, but they are also an importantsource of healing factors, such as epidermal growth factor. Removal of the salivary gland functionleads to gastric and intestinal ulcer formation, poor healing of wounds and ulcers, and poorregeneration of organs, especially of the liver. From an immunological point of view, a praxis thatstimulates these secretions, instead of inhibiting them, should be preferred whenever possible,especially in the very sick and critically ill — see references for more information.26–28 Unfortu-nately, most drugs, especially those commonly used in ICUs, have strong antisecretory effects. Formore information, including a list of drugs, see Bengmark.26
10.4.3 INHIBITION OF GI SECRETIONS
Low gastric pH is a prerequisite for gastric nitric oxide (NO) production, a function that is totallyeliminated by the supply of H2 blockers and proton inhibitors. Maintenance of gastric NO productionis of the utmost importance for maintaining GI motility and mucosal and splanchnic blood flow,and for elimination of pathogens in the stomach.29–31 Furthermore, normal gastric acid productionis essential for absorption of several vitamins and antioxidants, including vitamin C and glutathione.In the absence of a low pH, the stomach will become a reservoir for pathogens, which areregurgitated into the lungs and frequently cause chest infections.32 Use of H2 blockers and protoninhibitors might have been useful to prevent peptic ulcers in patients on total parenteral nutrition,but with today’s aggressive and early enteral feeding, this practice is totally unnecessary and oftencounterproductive.26–28,33 Routine use of H2 blockers or proton inhibitors in enterally fed postoper-ative and ICU patients cannot be regarded as based on scientific evidence.33–35
156
Nutrition Support for the Critically Ill Patient: A Guide to Practice
AU: ChangeOK?
2153_book.fm Page 156 Monday, October 18, 2004 8:00 AM
10.4.4 PROPHYLACTIC NASOGASTRIC DECOMPRESSION
The use of nasogastric decompression — introduced by Mayo in order to prevent nausea, vomiting,and abdominal distension; to decrease postoperative ileus and wound complications; and to protectenteric anastomoses — has been forcefully questioned for more than 50 years but is still commonlyused.36–39 Use of nasogastric decompression will seemingly delay return of adequate bowel functionbut, what is more severe, will contribute significantly to septic complications. Several controlledstudies have clearly confirmed that routine nasogastric decompression can be omitted without anynegative consequences.39–42 Even if a slight gastric distention might occur, it will resolve sponta-neously, without any active measures, with no serious consequences observed. Even if a no-drainagepolicy might lead to an increased incidence of gastric distention, no other negative consequenceswill be seen, and insertion of drainage should usually not be needed.43–46 A meta-analysis basedon 26 trials (a total of 3964 patients) concluded that routine nasogastric decompression is notsupported by scientific evidence.47 Fever, atelectasis, and pneumonia are significantly less if patientsare managed without nasogastric tubes.47 Gastric distention should normally be no contraindicationto continuation of tube feeding, and high residual volumes should not automatically lead to cessationof tube feeding. Instead, the symptoms will soon disappear and the residual volume soon decreaseif tube feeding is continued.48–51
10.4.5 POSTOPERATIVE DRAINAGE OF BODY CAVITIES
Little evidence supports routine use of postoperative drainage of body cavities. Drainage tubesserve as much as an entrance for microbes as an outlet of fluid accumulations. Most body cavities,especially the abdomen, have excellent capacity for absorption of fluids, especially blood, unlessthe fluids are infected or mixed with body fluids like urine and bile. Most studies suggest that thereis no need for abdominal drainage in biliary and gastric surgery. Some controlled studies alsosuggest advantages of a no-drainage policy in liver and pancreatic surgery. Several randomizedstudies have documented clear benefits of a no-drainage policy in colonic surgery. This is especiallytrue for appendicitis, where use of drains has been associated with an increased rate of complica-tions, especially adhesion formation. There is presently little evidence to support the use of drainsthat connect body cavities with the patient’s exterior. As suggested by a recent review, the onlyvalid conclusion at present is that high-quality clinical studies are necessary in order to providesolid, evidence-based recommendations for the use of drainage devices.52 This is especially true invisceral surgery.
10.4.6 PREOPERATIVE BOWEL PREPARATION
Intact intestinal flora are needed for the production, release, and absorption of important nutrientsin the lower GI tract, but also for prevention of infection, stimulation of anastomotic healing, andprevention of excessive peritoneal adhesion formation. All of these important processes seem tobe negatively influenced by both antibiotic treatment and lavage/bowel preparation. Aggressivebowel preparation and postoperative supply of a fiber-free diet have detrimental effects on theexpression of important biological factors, such as transforming growth factor-beta 1 and pro-collagen type I, which are both important to intestinal healing.53
Long-term results of bowel surgery and the postoperative morbidity have remained unchangedin recent decades.54 The practice of bowel preparation has seemingly not improved the situation.Even if it is suggested that careful bowel preparation might not enhance microbial translocation,there are still several other important reasons for omission of extensive bowel preparation.55
Experience from some recent studies demonstrates that bowel preparation can safely be omitted.56–58
A recently published meta-analysis found no evidence that bowel preparation reduces anastomoticleaks or prevents other complications.59 Instead, accumulating experimental and clinical evidenceindicates that bowel preparation, as usually practiced today, might be harmful and that reduced
Fiber and Probiotics Prevention of ICU Infections
157
AU: First fewweeks of what?
2153_book.fm Page 157 Monday, October 18, 2004 8:00 AM
morbidity and considerable cost savings can be expected from modification of the practice.60–62
One modification, which is biologically correct and might prove successful, is to use synbiotictreatment a few days before surgery (see Section 10.7). In addition, such a practice might contributeto less anastomotic dehiscences, infections, and reduced adhesion formation.
10.4.7 TRANSFUSION WITH OLD STORED BLOOD
Cellular debris (or, as documented in experimental studies, homogenized cells) are strong inducersof coagulation and thrombosis. We observed some 35 years ago that extensive disseminatedintravascular coagulation and fibrinolysis occurs after intraportal or intravenous infusion of hemo-lyzed blood.63–65 Similar changes are also seen in organs affected by hypoxia, as in intestinal orliver ischemia, or by increased levels of alcohol in the blood.66,67 Blood transfusion has constantlybeen shown to be a major risk factor for postinjury MOF.68–70 Trauma does often occur in alcohol-intoxicated persons, who also suffer severe shock and poor organ perfusion, and often are the objectof extensive blood transfusions. Removal of old blood cells and restoration of tissues in organsdamaged by ischemia and alcohol intoxication constitute an enormous burden on the reticulo–endo-thelial system, which results in immunoparalysis and increased sensitivity to infections. A strongassociation between the number of units transfused during the first six hours, the age of the storedblood transfused, and subsequent development of MOF was recently demonstrated.70 Plenty ofevidence shows that, whenever possible, fresh blood should be used for initial resuscitation oftrauma patients but also when larger amounts of blood transfusion are needed.
10.4.8 OVERLOADING WITH NUTRIENTS (HYPERALIMENTATION)
Not long ago, overloading nutrients, called hyperalimentation, was regarded as key to success inthe care of the critically ill; this is no longer so. Today, overfeeding macronutrients is consideredmuch more dangerous than underfeeding, at least during the first few weeks. A whole series ofnegative metabolic consequences is described following overfeeding, and the degree of impairmentof both glucose and lipid metabolism seen in the ICU is reported to be significantly related to boththe severity of illness and its outcome.71,72 Increased amounts in the blood of free fatty acids (FFAs)are significantly and strongly associated with impaired immune functions. The endothelial cellsseem to play a key role because they are responsible for the transport of nutrients, such as FFAsand glucose, to the underlying cells. This function is impaired by the inflammatory response perse and by various toxins and microbes, but also by high levels of FFAs.73,74 Elevated serum FFAshave also been shown to inhibit T lymphocyte signaling, and FFA clearance through insulin infusionhas been demonstrated to improve neutrophil function significantly, as observed in diabetic cardiacsurgery patients.75,76
We observed some 35 years ago that high serum levels of fat and liver steatosis constitute poorrisks in liver resection; a similar observation was recently made for liver transplant patients.77–79
Most likely, this observation should also be valid for other types of extensive surgery, independentof whether the impaired fat metabolism and steatosis are induced by lifestyle, constitute a mani-festation of metabolic syndrome, or are induced by overloading of calories, as is often the case intotal parenteral nutrition (TPN).
10.5 OFTEN NEGLECTED MEASURES
Using supply of nutrients to modulate the inflammatory response and maximize the function of theimmune system and the resistance to diseases is becoming increasingly accepted as an effectivetool. Enteral nutrition (EN) is documented to improve outcome in critically ill and surgical patients.Proper nutrition is also an important tool to prevent chronic illnesses. Various nutrients have beenshown to preserve and augment different aspects of cellular immunity and to modify the production
158 Nutrition Support for the Critically Ill Patient: A Guide to Practice
AU: Pro-noun ref unclear.
2153_book.fm Page 158 Monday, October 18, 2004 8:00 AM
of inflammatory mediators.80 Much remains to be done before all the possibilities of immuno-modulatory nutrition are fully understood and practiced. However, some measures have provedeffective:
• Aggressive perioperative enteral nutrition• Tight blood glucose control• Rich supply of antioxidants• Rich supply of prebiotic fibers• Maintenance of flora and supplementation of probiotic bacteria
10.5.1 AGGRESSIVE PERIOPERATIVE ENTERAL NUTRITION
The inflammatory response is immediate; all attempts to control the response must therefore alsobe immediate. Recent studies have demonstrated that immediate postoperative feeding is safe andprevents an increase in gut mucosal permeability. It is reported to contribute to a positive nitrogenbalance, reduce the incidence of septic complications and postoperative ileus, and acceleraterestitution of pulmonary performance, body composition, and physical performance.81–84 An impor-tant observation is that delaying institution of EN for more than 24 hours results in a significantlyincreased intestinal permeability and significantly higher incidence of MOF, compared to immediateenteral supply of nutrition.85 Uninterrupted oral/enteral supply of nutrients the night before surgery,during surgery, and immediately thereafter might support the immune system even further andincrease resistance to complication.
10.5.2 TIGHT CONTROL OF BLOOD GLUCOSE
Hyperglycemia is known as a significant marker of in-hospital mortality that predisposes to infec-tious complications.86,87 As an example, hyperglycemia predicts myocardial infarction in patientsunder hypertensive treatment.88 Strict glucose control has been known for some time to reduce theincidence of wound infection in open heart surgery;89 however, it was not until recently that strictglucose control has been widely adopted by modern ICU and postoperative care. Until recently,the state of the art was to feed critically ill patients and not provide exogenous insulin until bloodglucose levels were up to 12 mmol/l (220 mg/dl). However, studies using strict glucose control (tobelow 6.1 mmol/l) have convincingly shown a decrease in blood stream infections by 46%, acuterenal failure and need of hemofiltration by 41%, critical illness polyneuropathy by 44%, red celltransfusions by 50%, and mortality by 34%.90,91 Equally important is the information that evensmall elevations of blood glucose (to 8 to 10 mmol/l) impairs gut motility and function andcontributes to induction and prolongation of ileus.92 This is another important reason for strict bloodglucose control in the critically ill patient.
10.5.3 SUPPLY OF ANTIOXIDANTS
Antioxidant have numerous beneficial effects in the postoperative and ICU patient.93 Among theeffects are:
• Direct antioxidant effects• Anti-inflammatory effects• Antibacterial effects • Antithrombotic effects• Anticarcinogenic effects• Vasodilatory effects
Fiber and Probiotics Prevention of ICU Infections 159
U: Larger an what?
AU: ChangeOK?
AU: Length of hospital orICU stay?
2153_book.fm Page 159 Monday, October 18, 2004 8:00 AM
The benefits of routine supply of larger amounts of various antioxidants, especially flavonoids,to surgical and ICU patients are as yet almost unexplored. It is well known that the tissue andblood concentrations of pro-oxidants are almost invariably high and the levels of various anti-oxidants and micronutrients low — often extremely low — in critically ill patients. For example,total vitamin C and ascorbic acid are reported to be < than 25% of normal values in ICU patients.94
A recently published study, performed mainly with trauma patients, reports a 19% reduction inpulmonary morbidity and a 57% lower incidence of MOF in the group receiving supplementationwith α-tocopherol and ascorbate.95 The benefit of antioxidant supplementation to surgical and ICUpatients is also supported by other studies (for a review, see Chapter 8).96
Glutathione is an important antioxidant, synthesized by the body and supplied by food, mainlyfruits and vegetables. Glutathione in serum is significantly decreased after surgery and in criticallyill patients in general, and low blood levels of glutathione are associated with impaired lymphocyteand neutrophil functions. In the critically ill patient, glutamine constitutes an important source offuel, especially for the small bowel enterocytes, but it is also a necessary substrate for the productionof glutathione.97 In experimental studies, supply of glutamine has been shown to reduce cytokinerelease, organ damage, and mortality and to counteract glutathione and lymphocyte depletion inPeyer’s patches.98,99 Significant clinical results, such as reductions in morbidity, mortality, and lengthof stay, are obtained by glutamine supply in critically ill patients.100 These benefits can also beexpected from supply of glutamine-rich fruits and vegetables, which are fermented by flora orsupplied probiotics in the lower GI tract.
10.5.4 SUPPLY OF PLANT FIBERS
Plant fibers are favored substrates for microbial fermentation in the lower digestive tract but alsohave their own strong bioactivities. Few studies on supply of plant fibers in connection with surgeryand the critically ill are to be found in the medical literature. A most interesting controlled study,published some ten years ago, reports significant reduction in postoperative morbidity after supplyof glucan (beta 1-3 polyglucose): nosocomial infections were reduced from 65 to 14% and mortalityfrom 30 to 5%.101 Most other recent studies in acute medicine have dealt mainly with the combinedsupply of probiotics and fibers (prebiotics). Experimental and clinical observations support thatprebiotics have the following functions:102,103
• Provide nutrients and energy for the consumer• Provide nutrients and energy for the flora• Provide resistance against invading pathogens• Maintain water and electrolyte balance• Maintain mucosal growth• Maintain mucosal function
The best fibers are undoubtedly those provided by eating fresh, uncooked, and otherwiseunprepared fruits and vegetables. However, this is rarely possible for the critically ill patient. Themore the fibers are processed, the more they have lost some of their potency. It is important toremember that the fibers supplied with commercial nutrition solutions are commonly hydrolyzed.This means that they are been made devoid of important antioxidants, various phytochemicals,glutathione, and other, rather unstable molecules such as glutamine. For that reason, it is recom-mended that extra fibers should be supplemented. By using a mix of several different fibers, itshould be possible to supply 20 to -30 g/d, even to the critically ill. Often-used prebiotics arevarious oligosaccharides, such fructooligosaccharides (FOS), trans-galactosaccharides, and lactu-lose. Oligosaccharides are especially rich in foods such as bananas, artichokes, leeks, onions, garlic,asparagus, and chicory. Larger molecules, such as oat fibers (beta-glucans), pectins, and resistantstarch, are extremely effective fibers and should also be supplemented in the critically ill. These
Ath
160 Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 160 Monday, October 18, 2004 8:00 AM
fibers are usually supplied as powders that can be diluted with water or acid fruit juices, such aspineapple juice, and fed through feeding tubes or mixed with mashed fruits, such as kiwis, apples,pears, or bananas, and eaten.
10.5.5 SUPPLEMENTING FLORA
A significant reduction of the commensal flora occurs very early in the disease process and isinduced by the disease and the stress per se but also by pharmaceutical treatment. A significantreduction in anaerobic bacteria, and particularly lactobacilli, is observed in both the small intestineand the colon as early as six to eight hours after induction of experimental pancreatitis.104 Thisreduction in beneficial flora pattern is almost instantly followed by significant increases in thenumber of various potentially pathogenic microorganisms (PPMs), such as Escherichia coli. Dra-matic increases in mucosal barrier permeability (lumen to blood) and in endothelial permeability(blood to tissue) are observed and accompanied by increased microbial translocation and growthof PPMs, in both the mesenteric lymph nodes and the pancreatic tissue. 104–106 For obvious ethicalreasons, few systematic studies have been done in patients, but there is much support for theassumption that patients who have undergone major operations and patients who suffer majortrauma or are treated with modern antibiotics suffer a considerable reduction in the beneficial floraand a significant overgrowth of PPMs. Early supplemented beneficial bacteria, so-called probiotics,are reported to counteract such negative effects. From experimental and clinical observations, itcan be concluded that supplied probiotics exhibit several important bioactivities, which should beof special benefit to the critically ill:102,103
• Reduce or eliminate potentially pathogenic microorganisms (PPMs)• Reduce or eliminate various toxins and mutagens from the intestinal content• Modulate innate and adaptive immune defense mechanisms• Promote apoptosis• Release numerous nutrients, antioxidants, growth factors, and coagulation and other
factors from consumed fibers
10.6 A DUAL DIGESTIVE SYSTEM
Humans and animals have two separate and hugely different digestive systems:
• One based on digestion by secretions from eukaryotic cells, especially those located inthe upper gut: saliva, pancreatic, and gastrointestinal secretions
• Another, equally important but much more complex and less understood, based onenzymatic fermentation by prokaryotic cells and microbes, occurring mainly in the lowergastrointestinal tract
Normally, the main substrates for GI fermentation will come from consumed fruit and vegetables,fibers indigestible by eukaryotic enzymes in the upper GI tract; this is why they reach the lowerGI tract almost totally undigested. In the lower GI tract, extra energy and, more importantly,numerous nutrients, vitamins, antioxidants, coagulation factors, growth factors, signal substances,etc., are released and made available to the body. The human body contains approximately. 65,000genes, which should be compared to the 300,000 to 2 million genes in the GI flora.107 Thisinformation provides an indication of the size and enormous complexity of the flora-driven digestivesystem. One can assume many more substances are released and absorbed in the lower ileum andthe large bowel than in higher levels of the GI tract.
Fiber and Probiotics Prevention of ICU Infections 161
AU: Pro-noun ref unclear.
2153_book.fm Page 161 Monday, October 18, 2004 8:00 AM
10.6.1 MUCOSAL HOMEOSTASIS
Many factors contribute to a satisfactory mucosal function, such as the following:102,103
• Satisfactory enteral supply of nutrients• Satisfactory enteral supply of antioxidants• Intact intestinal barrier• Tolerant immunity• “Normal” (not exaggerated) cytokine response• “Normal” (not increased) PPM virulence• Rich preventive flora• Maintained mucosal repair
It has been suggested that, to a large extent, optimal health and well-being depend on theavailability and “exact” balance, homeostasis, of the approximately two million different moleculesthat are said to constitute the human body. Some of these molecules are essential (e.g., must beobtained by eating); others become essential in critical conditions with increased demands andtherefore are usually called semiessential. The largest number of consumed molecules is most likelyreleased through action of prokaryotic enzymes and absorbed in the lower GI tract. Our paleolithicancestors received a much richer and more variable supply of nutrients because they ate from morethan 500 plants and, as a consequence, had significantly more abundant and richer flora. Modernhumans have, in sharp contrast to our ancestors, chosen to obtain about 90% of their nutrition fromas few as 17 plants and more than 50% of their caloric and protein need from only eight cerealgrains. The reduced variability of typical modern Western foods, in combination with modernmethods for conservation and preparation of foods, shows an obviously reduced access to nutrientsand antioxidants. The flora of modern humans are, most likely as a consequence of this reducedaccess, restricted both in volume and in richness compared to that of our ancestors. And it is evenworse in the critically ill, due to the disease and the drugs provided — but more than anything tothe artificial nutrition provided to the sickest patients.
10.7 COMBINATION OF PRO- AND PREBIOTICS EQUALS SYNBIOTICS
Supplementing enteral nutrition with both fiber and lactic acid bacteria has the potential to enhancethe immune system further and provide protection from infectious complications. It is my personalconviction that it should be provided to surgical patients though feeding tubes continuously before,during, and immediately after surgery or, in the case of trauma or medical emergency, immediatelyupon arrival at the hospital. It is important to use a mixture several bioactive fibers, and it especiallyimportant to choose lactic acid bacteria with well documented bioactivities. Genetically, there is agreat difference among the various bacteria called lactic acid bacteria (LAB); the difference fromone LAB to another can be greater than the difference between a fish and a human. Most of theLAB used by the milk industry have limited or no ability to ferment strong bioactive fibers suchas inulin or phlein, no ability to adhere to human mucus, no or low antioxidant capacity and, mostimportantly, no ability to survive the acidity of stomach and the bile acid content of the smallintestine. Stronger clinical effects thus cannot be expected from the use of LAB such as yogurtbacteria, usually chosen mainly for their palatability.
Most of the LAB suggested for use in ICU patients were originally identified on plants. Mostexperience obtained from studies of ICU patients comes from studies using two synbiotic combi-nations or mixtures of pre- and probiotics:
162 Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 162 Monday, October 18, 2004 8:00 AM
• A one LAB–one fiber composition, produced though fermentation of oatmeal with aspecific L. plantarum strain 299.108
• A four LAB–four fiber composition, called Synbiotic 2000®, consisting in a mixture of1010 (and more recently a composition with 1011 called Synbiotic 2000 forte®) of fourdifferent LAB — Pediococcus pentosaceus 5-33:3, Leuconostoc mesenteroides 32-77:1,Lactobacillus paracasei subsp paracasei 19, and Lactobacillus plantarum 2362 — com-bined with 10 g of fibers: 2.5 g of each of four fermentable fibers — betaglucan, inulin,pectin, and resistant starch.109,110 It is a common practice to supply two sachets per day(i.e., 20 g fiber and 88 resp 880 billion [forte version] of LAB).
The most recent experience is summarized in the following sections.
10.7.1 ACUTE PANCREATITIS
Patients with severe acute pancreatitis were randomized to receive daily, during the first 7 daysand administered through a nasojejunal tube, either a freeze-dried preparation containing liveLb plantarum 299 in a dose of 109 together with a substrate of oat fiber, or a similar but heat-inactivated preparation.111 The study was interrupted when, on repeat statistical analysis, significantdifferences in favor of one of the two groups were obtained, which occurred after a total of 45patients had entered the study. At that time, 22 patients had received treatment with live and another23 with the heat-killed Lb plantarum 299. Infected pancreatic necrosis and abscesses were seen in1/22 (4.5%) in the live LAB group vs. 7/23 (30%) in the heat-inactivated group (p = 0.023). Theonly patient in the lactobacillus group who developed infection, a urinary infection, did so on the15th day (i.e.., at a time when he had not received treatment for eight days). The length of staywas also considerably shorter in the live LAB group (13.7 days vs. 21.4 days), but the limited sizeof the material did not allow statistical significance to be reached.
10.7.2 ABDOMINAL SURGERY
Lb plantarum 299, in a dose of 109 and 15 gram of oat and inulin fiber, was used in a study inextensive abdominal surgical operations. The patient material consisted mainly in liver, pancreatic,and gastric resections, equally distributed among the three groups. Three groups were compared:112
• Live LAB and fiber• Heat-inactivated LAB and fiber • Standard enteral nutrition
Each group consisted of 30 patients. The 30-day sepsis rate was 10% (3/30 patients) in the twogroups receiving either live or heat-inactivated LAB, compared to 30% (9/30 patients) in the groupon standard enteral nutrition (p = 0.01). The largest difference was observed in the incidence ofpneumonia:
• Live LAB and fiber: 2 patients• Heat-killed LAB and fiber: 1 patient • Enteral nutrition only: 6 patients
The beneficial effects of synbiotic treatment were seemingly most pronounced in gastric andpancreatic resections, the sepsis rate was:
• Live LAB: 7%• Heat-inactivated LAB: 17% • Standard enteral nutrition: 50%
Fiber and Probiotics Prevention of ICU Infections 163
2153_book.fm Page 163 Monday, October 18, 2004 8:00 AM
The same pattern was observed for noninfectious complications:
• Live LAB: 13% (4/30) • Heat-inactivated LAB: 17% (5/30) • Standard enteral nutrition only: 30% (9/30)
The supply of antibiotics to the live LAB–treated patients was significantly less (p = 0.04).Also, the mean length of antibiotic treatment was considerably shorter:
• Live LAB: 4 ± 3.7 days• Heat-killed LAB 7 ± 5.2 days • Standard enteral nutrition: 8 ± 6.5 days
No differences were observed in length of hospital stay. No significant differences could beobserved in hemoglobin, leukocytes, CRP, BUN, bilirubin, albumin, total lymphocyte count, CD45RA, CD45 RO, CD4, CD8, r in NK cells, or CD4:CD8 ratio.
10.7.3 LIVER TRANSPLANTATION
A prospective randomized study with the same one LAB–one fiber preparation was performed in95 liver transplant patients by the same group of investigators.113 Three groups of patients werestudied:
• SDD — Selective digestive tract decontamination four times daily for six weeks (n = 32) • LLP— Lb plantarum 299 in a dose of 109 plus 15 g of oat and inulin fibers (n = 31)
supplied postoperatively for 12 days • HLP — Identical to LLP, but with heat-killed Lb plantarum 299 (HLP) (n = 32)
Identical enteral nutrition was supplied to all patients from the second postoperative day. Thenumbers of postoperative infections were SDD 23, HLP 17, and LLP 4. Signs of infections occurredin SDD 48% (15/32), in HLP 34% (11/32), and in LLP 13% (4/31), p = 0.017, respectively. Themost dominating infections were cholangitis, occurring in SDD in 10, HLP in 8, and LLP in 2patients, respectively, and pneumonia, observed in SDD in 6, in HLP in 4, and in LLP in 1 patient,respectively. The most often isolated microbes were Enterococci: in 8 SDD, 8 HLP, and 1 LLP 1patient, respectively, closely followed by Staphylococci: in 6 SDD, 3 HLP, and 1 LLP patient,respectively. No E. coli or Klebsiella infections were seen in the LLP group. The numbers ofpatients requiring hemodialysis were 8 SDD, 4 HLP, and 2 LLP patients. The numbers of reoper-ations were 6 SDD, 2 HLP, and 4 LLP. There were no deaths. The stay in ICU, the hospital stay,and length of time on antibiotic therapy were shorter in the LLP group but did not reach statisticalsignificance. The CD4/CD8 ratio was higher in the LLP group than in the other two groups(p = 0.06).
The same investigators have continued their efforts to reduce the septic morbidity in livertransplantation.114 In a subsequent study, the four LAB–four fiber combination (Synbiotic 2000)was tried.109,110 In a double-blind randomized study, 33 patients were supplied Synbiotic 2000 andanother 33 patients only the four fibers in Synbiotic 2000. The treatment began on the day beforesurgery and continued for 14 days after surgery. During the first postoperative month, only onepatient in the Synbiotic 2000–treated group (3%) showed signs of infection (urinary infection),compared to 17/33 (51%) in the patients supplied only the four fibers. The use of antibiotics wasalso significantly reduced in the synbiotic-treated group.
164 Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 164 Monday, October 18, 2004 8:00 AM
10.7.4 OTHER CONDITIONS
Probiotic or synbiotic treatment is also effective in other acute and chronic conditions. This isespecially well studied in acute and chronic diarrhea.115,116 Significant effects have also beenobserved when applied to prevent allergy, reduce Helicobacter infections, counteract negativemanifestations of HIV, reduce symptoms in irritable bowel syndrome (IBS) and inflammatory boweldisease (IBD), and improve the condition of and prevent sepsis in patients with chronic kidneyfailure and on dialysis treatments.117–124 Synbiotic treatment is reported to reduce serum fibrinogenand LDL cholesterol significantly when supplied to patients with moderately elevated cholesterol.125
Recent observations of effects in patients with chronic liver disease are interesting and could beof importance for the management of patients on a waiting list for liver transplantation. The invitro TNFα production in response to stimulation by endotoxin or Staph aureus enterotoxin B(SEB) was reduced by a median 46% (range: 8 to 67%), in comparison to presupplementationlevels in 8/11 (72.7%) cirrhotic patients supplied Synbiotic 2000.126
The anti-infectious and anti-inflammatory effects of synbiotic treatment in chronic liver diseaseare further supported by a double-blind controlled study of 55 patients with chronic liver disease,not yet published.127 Three groups of patients were studied:
• Synbiotic 2000 (n = 20)• Only the fibers of Synbiotic 2000 (n = 20) • Placebo (nonfermentable, nonabsorbable fiber) (n = 15)
A significant increase from 7.37 ± 047 to 9.64 ± 0.34 (p < 0.05) in the LAB flora was observedin the LAB-supplied group but not in the other two groups. The pH was significantly reduced froma level between 6.5 and 7 in the placebo group to the level of 5 to 5.5 in the two treatment groups.Statistically significant decreases in E. coli, Staphylococcus, and Fusobacterium (p < 0.001, p < 0.01and p < 0.05) were observed in the two treatment groups but not in the placebo group. No differencesdue to treatment could be observed in the Pseudomonas and Enterococcus flora. Ammonia wassignificantly reduced in the Synbiotic 2000–supplied group (60.5 ± 2.9 to 38.6 ± 3.9) and in thefiber-supplied group (63.6 ± 3.9 to 41.5 ± 5.2) but not in the placebo group (60.5 ± 2.9 to 58.6 ± 3.9).The levels of endotoxin fell significantly in the two treatment groups but not in the placebo-treatedgroup. The reduction in the levels of ALT is remarkable: it decreased from 252 ± 182 to 84 ± 65(p < 0.01) in the Synbiotic 2000–treated group and to 110 ± 86 (p < 0.05) in the fiber-supplementedgroup, but not in the placebo group. Significant improvements in psychometric tests and in thedegree of encephalopathy were also observed in the two treatment groups.
10.8 FUTURE ASPECTS
During my long career as a surgeon, I have always been frustrated by the high rate of septiccomplications, especially occurring in connection with extensive surgery. Since the early 1960s, Iperformed extensive surgery to the liver and the pancreas. Like most other surgeons of that time,I tried a perioperative and postoperative antibiotic umbrella in the hope of reducing septic mani-festations. However, on a follow-up in the mid-1980s we detected that, for unknown reasons, one-third of patients had never received any prophylactic antibiotics at all. The infection rate of thetotal material was, as in most similar published materials, about 33%. However, to our great surprise,no infections had occurred among the patients who had not received antibiotics. This observationinterested me in exploring the role of the commensal flora but also in developing techniques torefunctionalize the lower gastrointestinal tract in order to reestablish the function of the microflorain sick patients. At that time, I did not imagine that, some 20 years later, synbiotics would beregarded as a realistic, sometimes superior, alternative to antibiotics. Nor did I foresee that, some
Fiber and Probiotics Prevention of ICU Infections 165
AU: ChangeOK?
2153_book.fm Page 165 Monday, October 18, 2004 8:00 AM
years later, pre-, pro-, and synbiotics would be considered an important tool to combat endemicdiseases such as diabetes, atherosclerosis, and cancer.
Resistance to disease is a key factor in the preservation of health. The innate immune system,with its various components — traditional immune cells; epithelial, endothelial, and mesothelialcells; the glial cells; and flora — is extremely sensitive to external influence and especially tovariations in the supply of nutrients and antioxidants. As mentioned earlier, about 80% of thevarious components are located in the digestive system and the abdominal cavity. The perioperativemanagement of the abdominal cavity in general, and particularly the nutrition given, is of greatimportance to the outcome. Humans living in rural areas and consuming large amounts of freshfruits, vegetables, and various types of fermented foods have an extremely low incidence of chronicdiseases and are also resistant to morbidity in connection with trauma and surgical operations. Asa consequence of lifestyle, the flora of their digestive tract are both large (approximately 2 kgbacteria) and rich (> 500 species). In fact, the bodies of such individuals will harbor about 20 timesmore microbial/karyotic cells than human/eukaryotic cells. These flora are significantly reduced inpersons living a Western lifestyle. Important fiber-fermenting bacteria — such as Lactobacillusplantarum, Lactobacillus rhamnosus, and Lact. paracasei ssp. paracasei, but also other LAB, suchas Lactobacillus acidophilus and Leuconostoc — have often disappeared in the commensal floraof North Americans and Europeans. For example, Lactobacillus plantarum is reported to exist inonly about 25% of omnivorous North Americans, in contrast to two-thirds of the mainly vegetarianNorth American Seventh Day Adventists.128 A study of healthy European (Swedish) volunteersfound Lactobacillus plantarum, Lact. rhamnosus, and Lact. paracasei ssp. paracasei to be the mostcommon Lactobacillus flora both at the rectal and oral mucosa, occurring in 52%, 26%, and 17%of the individuals, respectively.129 Other LAB, such as Lact. reuteri, Lact. fermentum, Lact. acido-philus, Lact. oris, and Lact. vaginalis, were only found occasionally.
Persons living a rural lifestyle similar to that of our paleolithic ancestors also have a richprotective flora in other parts of the body: the skin (200 g), vagina (20 g), lungs (20 g), mouth (20g), nose (10 g), and eyes (1 g).130 It is likely that these flora also have significant health-promotingfunctions. It is well known that persons with infective and inflammatory manifestations in thevagina do well on treatment with lactobacillus preparations. It has been observed that the incidenceof diaper dermatitis is significantly reduced in children supplemented with LAB.131 It is alsointeresting that two recent reports suggest that consumption of LAB-containing drinks preventsformation of biofilm and removes both yeast and bacteria from prostheses (in this case, siliconrubber voice prostheses) suggesting that an LAB-containing gel or cream could be effective inpreventing catheter-related infections.132,133 I would not be surprised if, one day, eye or nose dropswith lactobacilli or even inhalation of lactobacillus will be shown to be effective in combatingallergic, inflammatory, and infectious conditions in the respiratory tract and the eyes. Supply oflactobacillus has proved effective in reducing allergy.134,135 Hopefully, it will be increasingly triedin prevention and treatment of various endemic chronic diseases.
10.9 PRACTICE POINTS
• Efforts should be made to preserve salivation and gastrointestinal secretions in thecritically ill, because these secretions are important for optimal innate immune systemfunction.
• H2 blockers, proton inhibitors, and other antisecretory drugs should be avoided to theextent possible, especially of the patient is on enteral nutrition.
• If not possible before, attempts should be made to start supply immediately after anoperation, acute medical illness, or trauma.
166 Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 166 Monday, October 18, 2004 8:00 AM
• If possible, insert a feeding tube into the jejunum the day before surgery and feedaggressively during the night before and after surgery. Continue with reduced speedduring and immediately after surgery.
• Avoid extensive mechanical bowel preparations.• Avoid, to the extent possible, use of all sorts of drains.• If large transfusion volumes are necessary, make efforts to provide fresh blood.• Maintain a strict control of blood sugar (below 6.1 mmol/l).• Immunosuppressed patients benefit from pretreatment with probiotics and fiber several
days before surgery, when possible.• Attempts should always be made to provide a maximum of plant fibers: whenever
possible as fresh fruits and vegetables, otherwise as supplements.• Efforts should be made to provide several plant fibers to optimize the tolerability of the
fibers supplied and the availability of substrate for fermentation and subsequent releaseof important nutrients, antioxidants, coagulation, and other factors.
• Fibers provided in enteral nutrition solutions are most often hydrolyzed and void of manyimportant antioxidants and nutrients. Whenever possible, supplementation with fruitsand vegetables or fibers such as pectins, betaglucans, oligosaccharides, and resistantstarch should be provided as separate supplements.
• Use several fibers to increase tolerance. Strive to supply up to 20 to 30 g a day.• Probiotic bacteria have, apart from eventual flatulence, no side effects and can safely be
used in immunocompromised patients.• Critically ill patients, especially those receiving antibiotics, do all suffer from a reduced
commensal flora and reduced mucosal and barrier function. Such patients can be expectedto benefit from a rich daily supply of probiotic bacteria
• For clinical purposes, only pre- and probiotics with documented strong bioactivitiesshould be chosen. The majority of lactic acid bacteria do not survive the acidity of thestomach or bile acid content of the small intestine.
REFERENCES
1. World Health Organization. Process for a global strategy on diet, physical activity and health. WHO,Geneva, February, 2003.
2. Angus, D.C., Wax, R.S. Epidemiology of sepsis: an update. Crit. Care Med. 29, 109, 2001.3. Angus, D.C., Linde-Zwirble, W.T., Lidicker, J., et al. Epidemiology of severe sepsis in the United
States: analysis of incidence, outcome and associated costs of care. Crit. Care Med. 29, 1303, 2001.4. Vincent, J.-L., Abraham, E., Annane, D., et al. Reducing mortality in sepsis: new directions. Crit.
Care 6 (Suppl. 3), S1, 2002.5. Schwartz, M.N. Hospital-acquired infections: diseases with increasingly limited therapies. Proc. Natl.
Acad. Sci. USA 91, 2420, 1994.6. Bengmark, S. Nutritional modulation of acute and “chronic” phase response. Nutrition 17, 489, 2001.7. Simons, J.P., Schools A.M., Buurman, W.A., Wouters, E.F. Weight loss and low body cell mass in
males with lung cancer: relationship with systemic inflammation, acute-phase response, resting energyexpenditure, and catabolic and anabolic hormones. Clin. Sci. 97, 215, 1999.
8. Preston, T., Slater, C., McMillan, D.C., et al. Fibrinogen synthesis is elevated in fasting cancer patientswith an acute phase response. J. Nutr. 128, 1355, 1998.
9. Biffl, W.L., Moore, E.E., Moore, F.A., Barnett, C.C. Interleukin-6 delays neutrophil apoptosis via amechanism involving platelet-activating factor. J. Trauma, Injury, Infection Crit. Care 40, 575, 1996.
10. Sautner, T., Függer, R., Götzinger, P., et al. Tumour necrosis factor-α and interleukin-6: early indicatorsof bacterial infection after human orthotopic liver transplantation. Eur. J. Surg. 161, 97, 1995.
11. Alessi, M.C., Peiretti, F., Morange, P., et al. Production of plasminogen activator inhibitor 1 by humanadipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 46,860, 1997.
Fiber and Probiotics Prevention of ICU Infections 167
2153_book.fm Page 167 Monday, October 18, 2004 8:00 AM
12. Fried, S.K., Bunkin, D.A., Greenberg, A.S. Omental and subcutaneous adipose tissues of obesesubjects release interleukin-6: depot difference and regulation by glucocorticoid. J. Clin. Endocrinol.Metabol. 83, 847, 1998.
13. Thomas, E.L., Saeed, N., Hajnal, J.V., et al. Magnetic resonance imaging of total body fat. J. Appl.Physiol. 85, 1778, 1998.
14. Felten, D.L., Felten, S.Y., Carlson, S.L., et al. Noradrenergic and peptinergic innervation of lymphoidtissue. J. Immun. 135 Suppl., 755, 1985.
15. Ottaway, C.A. Vasoactive intestinal peptide and immune function. In Psychoneuroimmunology. 2nded. Ader R, Felten DL, Cohen N, eds. Academic Press, San Diego, 1991, 225.
16. Brandtzaeg, P., Halstensen, T.S., Kett, K., et al. Immunobiology and immunopathology of human gutmucosa: humoral immunity and intraepithelial lymphocytes. Gastroenterol. 97, 1562, 1989.
17. Kiyono, H., McGhee, J.R. T helper cells for mucosal immune responses. In Handbook of MucosalImmunology. Ogra P.L., Mestecky J., Lamm M.E., et al., eds. Academic Press, Orlando, FL, 1994, 263.
18. Brandzaeg, P. Molecular and cellular aspects of the secretory immunoglobulin system. APMIS 103,1, 1995.
19. Freter, R. The fatal enteric cholera infection in guinea pig achieved by inhibition of normal entericflora. J. Infect. Dis. 97, 57, 1955.
20. Roszkowski, K., Ko, K.L., Beuth, J., et al. Intestinal microflora of BALB/c-mice and function of localimmune cells. Zeitschr. F. Bakteriol. Hyg. 270, 270, 1988.
21. Pulverer, G., Ko, H.L., Roszkowski, W., et al. Digestive tract microflora liberates low molecular weightpeptides with immunotriggering activity. Zentralbl. F. Bakteriol. 272, 318, 1990.
22. Peiper, C., Seelig, M., Treutner, K.H., Schumpelick, V. Low-dose, single-shot perioperative antibioticprophylaxis in colorectal surgery. Chemother. 43, 54, 1997.
23. Kriaras, I., Michalopoulos, A., Turina, M., Geroulanos, S. Evolution of antimicrobial prophylaxis incardiovascular surgery. Eur. J. Cardiothorac. Surg. 18, 440, 2000.
24. Kirton, O.C., O’Neill, P.A., Kestner, M., Tortella, B.J. Perioperative antibiotic use in high-risk pene-trating hollow viscus injury: a prospective randomized, double-blind, placebo-control trial of 24 hoursversus 5 days. J. Trauma 49, 822, 2000.
25. Goossens, H., Peetermans, W., Sion, J.P., Bossens, M. “Evidence-based” perioperative antibioticprophylaxis policy in Belgian hospitals after a change in the reimbursement system. Ned. Tijdschr.Geneesk. 14, 1773, 2001.
26. Bengmark, S. Gut and the immune system: enteral nutrition and immunonutrients. In SIRS, MODSand MOF — Systemic Inflammatory Response Syndrome, Multiple Organ Dysfunction Syndrome,Multiple Organ Failure — Pathophysiology, Prevention and Therapy, Baue, A.E., Faist, E., Fry, D.,eds. Springer, New York, 2000, 420–436.
27. Bengmark, S. Pre-, pro-, and synbiotics. Curr. Opin. Nutr. Metab. Care 4, 571, 2001.28. Bengmark S. Use of pro-, pre- and synbiotics in the ICU: future options. In Nutritional Considerations
in the Intensive Care Unit: Science, Rationale and Practice. Shikora S.A., Martindale R.G., Schwait-zberg S.D., eds. Kendall/Hunt, Dubuque, IA, 2002, 381–399.
29. Lundberg, J.O.N., Weitzberg, E., Lundberg, J.M., Alving, K. Intragastric nitric oxide production inhumans: measurement in expelled air. Gut 35, 1543, 1994.
30. Duncan, C., Dougall, H., Johnston, et al. Chemical generation of nitric oxide in the mouth from theenterosalivary circulation of dietary nitrates. Nature Med. 1, 546, 1995.
31. Heyland, D., Mandell, L.A. Gastric colonization by Gram-negative bacilli and nosocomial pneumoniain the intensive care unit patients. Chest 101, 187, 1992.
32. Gomes, G.F., Pisani, J.C., Macedo, E.D., Campos, A.C. The nasogastric feeding tube as a risk factorfor aspiration and aspiration pneumonia. Curr. Opin. Clin. Nutr. Metab. Care 6, 32, 2003.
33. McDonald, W.S., Sharp, C.W., Deitch, E.A. Immediate enteral feeding in burn patients is safe andeffective. Ann. Surg. 214, 177, 1991.
34. Donowitz, G.L., Page, M.L., Mileur, B.L. Alteration of normal gastric flora in critical care patientsreceiving antacid and cimethidine therapy. Infect. Control 7, 23, 1986.
35. Ben-Menachen, T., Fogel, R., Patel, R.V., et al. Prophylaxis for stress-related gastric hemorrhage inthe medical intensive care unit: a randomized controlled, single-blind study. Ann. Int. Med. 121, 568,1994.
168 Nutrition Support for the Critically Ill Patient: A Guide to Practice
2153_book.fm Page 168 Monday, October 18, 2004 8:00 AM
36. Savassi-Rocha, P.R., Conceicao, S.A., Ferreira, J.T., et al. Evaluation of the routine use of the naso-gastric tube in digestive operation by a prospective controlled study. Surg. Gynecol. Obstet. 174, 317,1992.
37. Gerber, A., Robert, F.A., Smith, L.L. The treatment of paralytic ileus without the use of gastrointestinalsuction. Surg. Gynecol. Obstet. 107, 247, 1958.
38. Gerber, A. An appraisal of paralytic ileus and the necessity for postoperative gastrointestinal suction.Surg. Gynecol. Obstet. 117, 294, 1958.
39. Farris, J.M., Smith, K. An evaluation of temporary gastrostomy: a substitute for nasogastric suction.Ann. Surg. 144, 475, 1956.
40. Mehnert, I.H., Brown, M.J., Woodward, B., et al. A clinical evaluation of postoperative nasal gastricsuction. Surg. Gynecol. Obstet. 109, 607, 1959.
41. Thomas, G.I., Metheny, D., Lundmark, V.O. Vagotomy without post-operative nasogastric suction.Northwest. Med. 60, 387, 1961.
42. Barnes, A.D., Williams, J.A. Stomach drainage after vagotomy and pyloroplasty. Am. J. Surg. 113,494, 1967.
43. Burg, R., Geigle, C.F., Faso, J.M., et al. Omission of routine gastric decompression. Dis. Colon Rectum21, 98, 1978.
44. Sitges-Serra, A., Cabrol, J., MaGubern, J., et al. A randomized trial of gastric decompression aftertruncal vagotomy and anterior pylorectomy. Surg. Gynecol. Obstet. 158, 557, 1980.
45. Schwartz, C.I., Heyman, A.S., Rao, A.C. Prophylactic nasogastric tube decompression: is its usejustified? Southern Med. J. 88, 825, 1995.
46. Petrelli, N.J., Stulc, J.P., Rodrigues-Bigas, M., et al. Nasogastric decompression following electivecolorectal surgery. Am. Surg. 59, 632, 1993.
47. Cheatham, M.L., Chapman, W.C., Key, S.P., et al. A meta-analysis of selective versus routine naso-gastric decompression after elective laparotomy. Ann. Surg. 221, 469, 1995.
48. Rombeau, J.L., Jacobs, D.O. Nasoenteric tube feeding. In Enteral Nutrition and Tube Feeding.Rombeau J.L., Caldwell M.D., eds. Saunders, Philadelphia, 1998, 261–274.
49. Norton, J.A., Otta, L.G., McClain, C., et al. Intolerance to enteral feeding in brain-injured patients.J. Neurosurg. 68, 62, 1988.
50. McClave, S.A., Snider, H.L., Lowen, C.C., et al. Use of the residual volume as a marker for enteralfeeding intolerance: prospective blinded comparison with physical examination and radiographicfindings. J. Parenter. Enteral Nutr. 16, 99, 1992.
51. Cook, D.J., Fuller, H.D., Guyatt, G.H., et al. Gastrointestinal bleeding in the critically ill: stress ulcerprophylaxis is not for everyone. N. Engl. J. Med. 330, 377, 1994.
52. Dominguez-Fernandez, E., Post, S. Abdominal drainages (in German). Der Chirurg 74, 91, 2003.53. Buckmire, M., Parquet, G., Seeburger, J.L., et al. Effect of bowel preparation and a fiber-free liquid
diet on expression of transforming growth factor and procollagen in colonic tissue preoperatively andpostoperatively. Dis. Colon Rectum 41, 1273, 1998.
54. Rabeneck, L., El-Serag, H.B., Davila, J.A., Sandler, R.S. Outcomes of colorectal cancer in the UnitedStates: no change in survival (1986–1997). Am. J. Gastroenterol. 98, 471, 2003.
55. Kale, T.I., Kuzu, M.A., Tekeli, A., et al. Aggressive bowel preparation does not enhance bacterialtranslocation, provided the mucosal barrier is not disrupted: a prospective, randomized study. Dis.Colon Rectum 41, 636, 1998.
56. Santos Jr, J.C., Batista, J., Sirimarco, M.T., et al. Prospective randomized trial of mechanical bowelpreparation in patients undergoing elective colorectal surgery. Br. J. Surg. 81, 1673, 1994.
57. Burke, P., Mealy, K., Gillen, P., et al. Requirement for bowel preparation in colorectal surgery. Br. J.Surg. 81, 907, 1994.
58. Zmora, O., Mahajna, A., Bar-Zakai, B., et al. Colon and rectal surgery without mechanical bowelpreparation: a randomized prospective trial. Ann. Surg. 237, 363, 2003.
59. Guenaga, K.F., Matos, D., Castro, A.A., et al. Mechanical bowel preparation for elective colorectalsurgery. Cochrane Database Syst. Rev. 2, CD001544, 2003.
60. Feres, O., Monteiro dos Santos Jr, J.C., Andrade, J.I. The role of mechanical bowel preparation forcolonic resection and anastomosis: an experimental study. Int. J. Colorectal. Dis. 16, 353, 2001.
61. Platell, C., Hall, J. What is the role of mechanical bowel preparation in patients undergoing colorectalsurgery? Dis. Colon Rectum 41, 872, 1998.
Fiber and Probiotics Prevention of ICU Infections 169
2153_book.fm Page 169 Monday, October 18, 2004 8:00 AM
62. Nessim, A., Wexner, S.D., Agachan, F., et al. Is bowel confinement necessary after anorectal recon-structive surgery? A prospective, randomized, surgeon-blinded trial. Dis. Colon Rectum 42, 16, 1999.
63. Bengmark, S., Hafström, L.O., Korsan-Bengtsen, K. A trial to produce intravascular coagulation byinfusion of connective-tissue homogenate and erythrocyte haemolysate: a comparative study. Br. J.Surg. 56, 619, 1969.
64. Bengmark. S., Hafström. L.O., Korsan-Bengtsen, K. A trial to produce disseminated intravascularcoagulation with intravenous infusion of homologous haemolysate and serum in cats. Acta Chir. Scand.138, 453, 1972.
65. Bengmark, S., Hafström, L.O, Korsan-Bengtsen, K. Effects of intraportal infusion of autologoushemolysate on blood coagulation factors and fibrinolysis in the cat. Am. J. Surg. 124, 647, 1972.
66. Hafström, L.O., Korsan-Bengtsen, K., Bengmark, S. Changes in blood clotting and fibrinolysis afterliver ischemia in pigs. Am. J. Surg. 127, 300, 1974.
67. Zoucas, E., Bergqvist, D., Göransson, G., Bengmark, S. Effect of acute ethanol intoxication on primaryhaemostasis, coagulation factors and fibrinolytic activity. Eur. Surg. Res. 14, 33, 1982.
68. Sauaia, A., Moore, F.A., Moore, E.E., et al. Early predictors of postinjury multiple organ failure. Arch.Surg. 129, 39, 1994.
69. Moore, F.A., Moore, E.E., Sauaia, A. Blood transfusion: an independent risk factor for postinjurymultiple organ failure. Arch. Surg. 132, 620, 1997.
70. Sauaia, A., Moore, F.A., Moore, E.E., et al. Multiple organ failure can be predicted as early as 12hours after injury. J. Trauma 45, 291, 1998.
71. Klein, C.J., Stanek, G.S., Wiles, C.E. Overfeeding macronutrients to critically ill adults: metaboliccomplications. J. Am. Diet. Assoc. 98, 795, 1998.
72. Lind, L., Lithell, H. Impaired glucose and lipid metabolism seen in intensive care patients is relatedto severity of illness and survival. Clin. Intens. Care 5, 100, 1994.
73. Steinberg, H.O., Tarshoby, M., Monestel, R., et al. Elevated circulating free fatty acid levels impairendothelium-dependent vasodilation. J. Clin. Invest. 100, 1230, 1997.
74. Pleiner, J., Schaller, G. Mittermayer, F., et al. FFA-induced endothelial dysfunction can be correctedby vitamin C. J. Clin. Endocrinol. Metab. 87, 2913, 2002.
75. Stulnig, T.M., Berger, M., Roden, M., et al. Elevated free fatty acid concentrations inhibit T lymphocytesignaling. FASEB J. 14, 939, 2000.
76. Rassias, A.J., Marrin, C.A.S., Arruda, J., et al. Insulin infusion improves neutrophil function in diabeticcardiac surgery patients. Anesth. Analg. 88, 1011, 1999.
77. Almersjö, O., Bengmark, S., Engevik, L., et al. Serum lipids after extensive liver resection in man.Acta Hepatosplenol. 15, 1, 1968.
78. Bengmark, S. Liver steatosis and liver resection. Digestion 2, 304, 1968.79. Marchesini, G., Forlani, G. NASH: from liver disease to metabolic disorders and back to clinical
hepatology. Hepatology 35, 497, 2002.80. Calder, P.C. Immunonutrition. BMJ 327, 117, 2003.81. Carr, C.S., Ling. K.D.E., Boulos, P., Singer, M. Randomised trial of safety and efficacy of immediate
postoperative enteral feeding in patients undergoing gastrointestinal resection. BMJ 112, 869, 1996.82. Bisgaard, T., Kehlet, H. Early oral feeding after elective abdominal surgery: what are the issues?
Nutrition 18, 944, 2002.83. Basse, L., Raskov, H.H., Hjort-Jakobsen, D., et al. Accelerated postoperative recovery programme
after colonic resection improves physical performance, pulmonary function and body composition.Br. J. Surg. 89, 446, 2002.
84. Kehlet, H., Holte, K. Review of postoperative ileus. Am. J. Surg. 182, Suppl, S3, 2001.85. Kompan, L., Kremzar, B., Gadzijev, E., Prosek, M. Effects of early enteral nutrition on intestinal
permeability and the development of multiple organ failure after multiple injury. Intens. Care Med.25, 129, 1999.
86. Umpierrez, G.E., Isaacs, S.D., Bazargan, N., et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J. Clin. Endocrinol. Metabol. 87, 978, 2002.
87. McCowen, K.C., Malhotra, A., Bistrian, B.R. Stress-induced hyperglycemia. Crit. Care Clin. 17, 107,2001.
170 Nutrition Support for the Critically Ill Patient: A Guide to Practice
AU: Pls complete.
2153_book.fm Page 170 Monday, October 18, 2004 8:00 AM
88. Dunder, K., Lind, L., Zethelius, B., Lithell, H. Increase in blood glucose concentration duringhypertensive treatment as a predictor of myocardial infarction: population based cohort study. BMJ326, 681, 2003.
89. Zerr, K.J., Furnary, A.P., Grunkemeier, G.L., et al. Glucose control lowers the risk of wound infectionin diabetes after open heart operations. Ann. Thorac. Surg. 63, 356, 1997.
90. Van den Berghe, G., Wouters, P., Weekers, F., et al. Intensive insulin therapy in critically ill patients.N. Engl. J. Med. 345, 1359, 2001.
91. Mesotten, D., Van den Berghe, G. Clinical potential of insulin therapy in critically ill patients. Drugs63, 625, 2003.
92. Rayner, C.K., Jones, K.L., Samson, N., Horowitz, M. Relationship of upper gastrointestinal motorand sensory function with glycemic control. Diabetes Care 24, 371, 2001.
93. Middleton Jr., E., Kandaswami, C., Theoharides, T.C. The effects of plant flavonoids on mammaliancells: implications for inflammation, heart disease, and cancer. Pharmacol. Rev. 52, 673, 2000.
94. Schorah, C.J., Downing, C., Piripitsi, A., et al. Total vitamin C, ascorbic acid, and dehydroascorbicacid concentrations in plasma of critically ill. Am. J. Clin. Nutr. 63, 760, 1996.
95. Nathens, A.B., Neff, M.J., Jurkovich, G.J., et al. Randomized, prospective trial of antioxidant supple-mentation in critically ill surgical patients. Ann. Surg. 236, 814, 2002.
96. Baines, M, Shenkin, A. Use of antioxidants in surgery: a measure to reduce postoperative complica-tions. Curr. Opin. Nutr. Metab. 5, 665, 2002.
97. Cao, Y., Feng, F., Hoos, A., Klimberg, V.S. Glutamine enhances gut glutathione production. J. Parenter.Enteral Nutr. 22, 224, 1998.
98. Wischmeyer, P.E., Kahana, M., Wolfson, R., et al. Glutamine reduces cytokine release, organ damage,and mortality in a rat model of endotoxemia. Shock 16, 398, 2001.
99. Manhart, N., Vierlinger, K., Spittler, A., et al. Oral feeding with glutamine prevents lymphocyte andglutathione depletion of Peyer’s patches in endotoxemic mice. Ann. Surg. 234, 92, 2001.
100. Kelly, D., Wischmeyer, P.E. Role of L-glutamine in critical illness: new insights. Curr. Opin. Nutr.Metab. 6, 217, 2003.
101. de Fellippe, J., da Rocha e Silva, M., Maciel, F.M.B., et al. Infection prevention in patients with severemultiple trauma with the immunomodulator beta 1-3 polyglucose (glucan). Surg. Gynecol. Obstet.177, 383, 1993.
102. Bengmark S. Aggressive perioperative and intraoperative enteral nutrition: strategy for the future. InSIRS, MODS and MOF — Systemic Inflammatory Response Syndrome, Multiple Organ DysfunctionSyndrome, Multiple Organ Failure — Pathophysiology, Prevention and Therapy, Baue A.E., Faist E.,Fry D., eds. Springer, New York, 2000, 365–380.
103. Bengmark, S. Pre-, pro-, and synbiotics in clinical enteral nutrition, In ????? etc 104. Andersson, R., Wang, X., Ihse, I. The influence of abdominal sepsis on acute pancreatitis in rats: a
study on mortality, permeability, arterial blood pressure and intestinal blood flow. Pancreas 11, 365,1995.
105. Leveau, P., Wang, X., Soltesz, V., et al. Alterations in intestinal permeability and microflora inexperimental acute pancreatitis. Int. J. Pancreatol. 20, 119, 1996.
106. De Souza, L.J., Sampietre, S.N., Figueiredo, S., et al. Bacterial translocation during acute pancreatitisin rats (in Portuguese, with English summary). Rev. Hosp. Clin. Fac. Med. S. Paolo 51, 116, 1996.
107. Hooper, L.V., Midtvedt, T., Gordon, J.I. How host–microbial interactions shape the nutrient environ-ment of the mammalian intestine. Annu. Rev. Nutr. 22, 283, 2002.
108. Johansson, M.L., Molin, G., Jeppsson, B., et al. Administration of different lactobacillus strains infermented oatmeal soup: in vivo colonization of human intestinal mucosa and effect on the indigenousflora. Appl. Environ. Microbiol. 59, 15, 1993.
109. Kruszewska, K., Lan, J., Lorca, G., et al. Selection of lactic acid bacteria as probiotic strains by invitro tests. Microecol. Ther. 29, 37, 2002.
110. Ljungh, Å., Lan, J.-G., Yamagisawa, N. Isolation, selection and characteristics of Lactobacillusparacasei ssp paracasei isolate F19. Microb. Ecol. Health Dis. 3, Suppl, 4, 2002.
111. Oláh, A., Belágyi, T., Issekutz, Á., et al. Early enteral nutrition with specific lactobacillus and fibrereduces sepsis in severe acute pancreatitis. Br. J. Surg. 89, 1103, 2002.
112. Rayes, N., Hansen, S., Boucsein, K., et al. Early enteral supply of fibre and lactobacilli vs. parenteralnutrition: a controlled trial in major abdominal surgery patients. Nutrition 18, 609, 2002.
-
Fiber and Probiotics Prevention of ICU Infections 171
AU: Update?
U: Year?
AU: Year?
U: Ini-l(s)?
AU: Page range?
2153_book.fm Page 171 Monday, October 18, 2004 8:00 AM
113. Rayes, N., Hansen, S., Seehofer, D., et al. Early enteral supply of Lactobacillus and fibre vs. selectivebowel decontamination (SBD): a controlled trial in liver transplant recipients. Transplantation 74,123, 2002.
114. Rayes, N., Seehofer, D., Theruvath, T., et al. Combined perioperative enteral supply of bioactive pre-and probiotics abolishes postoperative bacterial infections in human liver transplantation: a ran-domised, double-blind clinical trial. In press.
115. Huang, J.S., Bousvaros, A., Lee, J.E., et al. Efficacy of probiotic use in acute diarrhea in children: ameta-analysis. Dig. Dis. Sci. 47, 2625, 2002.
116. D’Souza, A.L., Rajkumar, C., Cooke, J., Bulpitt, C. Probiotics in prevention of antibiotic associateddiarrhoea: meta-analysis. Br. Med. J. 324, 1361, 2002.
117. Kalliomaki, M., Salminen, S., Arvilommi, H., et al. Probiotics in primary prevention of atopic disease:a randomized placebo-controlled trial. Lancet 357, 1076, 2002.
118. Felley, C., Corthesy-Theulaz, I., Blanco, R.J., et al. Favourable effects of an acidified milk (La-1) onHelicobacter pylori gastritis in man. Eur. J. Gastroenterol. Hepatol. 13, 25, 2001.
119. Cunningham-Rundles, S., Ahrne, S., Bengmark, S., et al. Probiotics and immune response. Am. J.Gastroenterol. 95, Suppl. 1, S22, 2000.
120. Niedzielin, K., Kordecki, H., Birkenfeld, B. A controlled, double-blind, randomised study on theefficacy of Lactobacillus plantarum 299 in patients with irritable bowel syndrome. Eur. J. Gastroentrol.Hepatol. 13, 1143, 2001.
121. Shanahan, F. Probiotics and inflammatory bowel disease: from fads and fantasy to facts and future.Br. J. Nutr. 88 Suppl. 1, S5, 2002.
122. Marteau, P., Seksik, P., Jian, R. Probiotics and intestinal effects: a clinical perspective. Br. J. Nutr. 88Suppl. 1, S51, 2002.
123. Simenhoff, M.L., Dunn, S.R., Zollner, G., et al. Biomodulation of the toxic and nutritional effects ofsmall bowel bacterial overgrowth in end-stage kidney disease using freeze-dried Lactobacillus aci-dophilus. Miner. Electrolyt. Metab. 22, 92, 1006 .
124. Hida, M., Aiba, Y., Sawamura, S., et al. Inhibition of the accumulation of uremic toxins in the bloodand their precursors in feces after oral administration of Lebenin, a lactic acid bacteria preparation,to uremic patients undergoing hemodialysis. Nephron 74, 349, 1994.
125. Bukowska, H., Pieczul-Mroz, J., Jastrzebska, M., et al. Decrease in fibrinogen and LDL-cholesterollevels upon supplementation of diet with lactobacillus plantarum in subjects with moderately elevatedcholesterol. Atherosclerosis 137, 437, 1009.
126. Riordan, S.M., Skinner. N., Nagree, A., et al. Peripheral blood mononuclear cell expression of Toll-like receptors and relation to cytokine levels in cirrhosis. Hepatology 37, 5, 1154–1164, 2003.
127. Qing-Liu, personal communication.128. Finegold, S.M., Sutter, V.L., Mathisen, G.E. Normal indigenous intestinal flora. In Human Intestinal
Microflora in Health and Disease, Hentges D.J., ed. Academic Press, New York, 1983.129. Ahrné, S., Nobaek, S., Jeppsson, B., et al. The normal Lactobacillus flora of healthy human rectal
and oral mucosa. J. Appl. Microbiol. 85, 88, 1998.130. Gustafsson, B. The Future of Germ-Free Research. Alan R. Liss, New York, 1985.131. Hoyos, A.B. Reduced incidence of necrotizing enterocolitis associated with enteral administration of
Lactobacillus acidophilus and Bifidobacterium Infantis to neonates in an intensive care unit. Int. J.Infect. Dis. 3, 197, 1999.
132. Buscher, H.J., Free, R.H., Van Weissenbruch, R., et al. Preliminary observations on influence of diaryproducts on biofilm removal from silicon rubber voice prostheses in vitro. J. Dairy Sci. 83, 641, 1999.
133. van der Mei, H.C., Free, R.H., Elving, G.J., et al. Effect of probiotic bacteria on prevalence of yeastsin oropharyngeal biofilms on silicone rubber voice prostheses in vitro. J. Med. Microbiol. 49, 713,2000.
134. Rosenfeldt, V., Benfeldt, E., Nielsen, S.D., et al. Effect of probiotic Lactobacillus strains in childrenwith atopic dermatitis. J. Allergy Clin. Immunol. 111, 389, 2003.
135. Kalliomaki, M., Salminen, S., Poussa, T., et al. Probiotics and prevention of atopic disease: 4-yearfollow-up of a randomised placebo-controlled trial. Lancet 361, 1869, 2003.
A
Atia