G I N A FIX
-
Upload
novita-dwiswara-putri -
Category
Documents
-
view
222 -
download
1
description
Transcript of G I N A FIX

GLOBAL INITIATIVE FOR ASTHMA
Pembimbing:dr. Retno, Sp. P
Anggota Kelompok:Muflikha Sofiana Putri, S. KedNovita Dwiswara Putri, S. Ked
Rizky Bayu Ajie, S. Ked
KEPANITERAAN KLINIK BAGIAN ILMU PENYAKIT DALAMRUMAH SAKIT UMUM DAERAH DR. H. ABDUL MOELOEK
FAKULTAS KEDOKTERAN UNIVERSITAS LAMPUNGBANDAR LAMPUNG
2015

G INA
G INA
lobal
itiative for
sthma
lobal
itiative for
sthma

Pendahuluan





Diagnosis Asma - Gejala

Diagnosis Asma – pemeriksaan fisik

Diagnosis Asma – variasi keterbatasan jalan napas

Alur Diagnosis Asma Patient with
respiratory symptoms
Are the symptoms typical of asthma?
Detailed history/examination for asthma
History/examinationsupports asthma diagnosis?
Perform spirometry/PEF with reversibility test
Results support asthma diagnosis?
Empiric treatment with ICS and prn SABA
Review response
Diagnostic testing within 1-3 months
Repeat on another occasion or arrange
other tests
Confirms asthma diagnosis?
Consider trial of treatment for most likely diagnosis, or refer
for further investigations
Further history and tests for alternative diagnoses
Alternative diagnosis confirmed?
Treat for alternative diagnosisTreat for ASTHMA
Clinical urgency, and other diagnoses unlikely
YES
YES
YES
NO
NO
NO
YES
YES
NO

Diagnosis Banding

Penilaian Asma

Penilaian keparahan asma

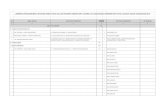
GINA assessment of symptom controlA. Symptom control
In the past 4 weeks, has the patient had:Well-
controlledPartly
controlledUncontrolled
• Daytime asthma symptoms more than twice a week?
Yes No
None of these
1-2 of these
3-4 of these
• Any night waking due to asthma?
Yes No• Reliever needed for symptoms*
more than twice a week?
Yes No• Any activity limitation due to asthma?
Yes No
B. Risk factors for poor asthma outcomes• Assess risk factors at diagnosis and periodically• Measure FEV1 at start of treatment, after 3 to 6 months of treatment to record the patient’s
personal best, then periodically for ongoing risk assessmentASSESS PATIENT’S RISKS FOR:• Exacerbations• Fixed airflow limitation• Medication side-effects
Level of asthma symptom control

Penilaian faktor resiko pada asma dengan respon yang buruk

Penatalaksanaan Asma

Siklus dasar management asma
GINA 2015, Box 3-2
Diagnosis
Symptom control & risk factors(including lung function)
Inhaler technique & adherence
Patient preference
Asthma medications
Non-pharmacological strategies
Treat modifiable risk factors
Symptoms
Exacerbations
Side-effects
Patient satisfaction
Lung function

Farmakoterapi
GINA 2015, Box 3-5, Step 1 (4/8)
PREFERRED CONTROLLER
CHOICE
Other controller
options
RELIEVER
STEP 1 STEP 2 STEP 3
STEP 4
STEP 5
Low dose ICS
Consider low dose ICS
Leukotriene receptor antagonists (LTRA)Low dose theophylline*
Med/high dose ICSLow dose ICS+LTRA
(or + theoph*)
As-needed short-acting beta2-agonist (SABA) As-needed SABA or low dose ICS/formoterol**
Low dose ICS/LABA*
Med/high ICS/LABA
Refer for add-on
treatment e.g.
anti-IgE
*For children 6-11 years, theophylline is not recommended, and preferred Step 3 is medium dose ICS**For patients prescribed BDP/formoterol or BUD/formoterol maintenance and reliever therapy# Tiotropium by soft-mist inhaler is indicated as add-on treatment for patients with a history of exacerbations; it is not indicated in children <18 years.
Add tiotropium#High dose ICS + LTRA (or + theoph*)
Add tiotropium#Add low dose OCS

Kortikosteroid inhalasi
Inhaled corticosteroid Total daily dose (mcg)Low Medium High
Beclometasone dipropionate (CFC) 200–500 >500–1000 >1000
Beclometasone dipropionate (HFA) 100–200 >200–400 >400
Budesonide (DPI) 200–400 >400–800 >800
Ciclesonide (HFA) 80–160 >160–320 >320
Fluticasone propionate (DPI or HFA) 100–250 >250–500 >500
Mometasone furoate 110–220 >220–440 >440
Triamcinolone acetonide 400–1000 >1000–2000 >2000
GINA 2015, Box 3-6 (1/2)

Lanjutan....
Inhaled corticosteroid Total daily dose (mcg)Low Medium High
Beclometasone dipropionate (CFC) 100–200 >200–400 >400
Beclometasone dipropionate (HFA) 50–100 >100–200 >200
Budesonide (DPI) 100–200 >200–400 >400
Budesonide (nebules) 250–500 >500–1000 >1000
Ciclesonide (HFA) 80 >80–160 >160
Fluticasone propionate (DPI) 100–200 >200–400 >400
Fluticasone propionate (HFA) 100–200 >200–500 >500
Mometasone furoate 110 ≥220–<440 ≥440
Triamcinolone acetonide 400–800 >800–1200 >1200
GINA 2015, Box 3-6 (2/2)

Intervensi Non-farmakologi

Kapan Dimulainya Terapi Kontrol Pada Asma??

Catatan

Penilaian Respon Terapi


Asma eksaserbasi

Asma Eksaserbasi

© Global Initiative for AsthmaGINA 2015, Box 6-8 (2/3)
PRIMARY CARE Child presents with acute or sub-acute asthma exacerbation or acute wheezing episode
ASSESS the CHILDConsider other diagnoses
Risk factors for hospitalization
Severity of exacerbation?
MILD or MODERATEBreathless, agitated
Pulse rate ≤200 bpm (0-3 yrs) or ≤180 bpm (4-5 yrs)
Oxygen saturation ≥92%
MONITOR CLOSELY for 1-2 hoursTransfer to high level care if any of:
• Lack of response to salbutamol over 1-2 hrs
• Any signs of severe exacerbation
• Increasing respiratory rate
• Decreasing oxygen saturation
START TREATMENTSalbutamol 100 mcg two puffs by pMDI + spacer or 2.5mg by nebulizer
Repeat every 20 min for the first hour if needed
Controlled oxygen (if needed and available): target saturation 94-98%
URGENT
SEVERE OR LIFE THREATENINGany of:
Unable to speak or drink
Central cyanosis
Confusion or drowsiness
Marked subcostal and/or sub-glottic retractions
Oxygen saturation <92%
Silent chest on auscultation
Pulse rate > 200 bpm (0-3 yrs)or >180 bpm (4-5 yrs)
TRANSFER TO HIGH LEVEL CARE (e.g. ICU)
While waiting give:
Salbutamol 100 mcg 6 puffs by pMDI+spacer (or 2.5mg nebulizer). Repeat every 20 min as needed.
Oxygen (if available) to keep saturation 94-98%
Prednisolone 2mg/kg (max. 20 mg for <2 yrs; max. 30 mg for 2–5 yrs) as a starting dose
Consider 160 mcg ipratropium bromide (or 250 mcg by nebulizer). Repeat every 20 min for 1 hour if needed.

© Global Initiative for AsthmaGINA 2015, Box 6-8 (3/3)
MONITOR CLOSELY for 1-2 hours
Transfer to high level care if any of:
• Lack of response to salbutamol over 1-2 hrs
• Any signs of severe exacerbation
• Increasing respiratory rate
• Decreasing oxygen saturation
TRANSFER TO HIGH LEVEL CARE (e.g. ICU)
While waiting give:
Salbutamol 100 mcg 6 puffs by pMDI+spacer (or 2.5mg nebulizer). Repeat every 20 min as needed.
Oxygen (if available) to keep saturation 94-98%
Prednisolone 2mg/kg (max. 20 mg for <2 yrs; max. 30 mg for 2–5 yrs) as a starting dose
Consider 160 mcg ipratropium bromide (or 250 mcg by nebulizer). Repeat every 20 min for 1 hour if needed.
Worsening, or failure to respond to
10 puffs salbutamol over 3-4 hrs
FOLLOW UP VISIT Reliever: Reduce to as-needed
Controller: Continue or adjust depending on cause of exacerbation, and duration of need for extra salbutamol
Risk factors: Check and correct modifiable risk factors that may have contributed to exacerbation, including inhaler technique and adherence
Action plan: Is it understood? Was it used appropriately? Does it need modification?
Schedule next follow up visit
DISCHARGE/FOLLOW-UP PLANNING
Ensure that resources at home are adequate.
Reliever: continue as needed
Controller: consider need for, or adjustment of, regular controller
Check inhaler technique and adherence
Follow up:within 1-7 days
Provide and explain action plan
CONTINUE TREATMENT IF NEEDED
Monitor closely as above
If symptoms recur within 3-4 hrs
• Give extra salbutamol 2-3 puffs per hour
• Give prednisolone 2mg/kg (max. 20mg for <2 yrs; max. 30mg for 2-5 yrs) orally
IMPROVING
IMPROVING