5. Perinatol VIII
-
Upload
diena-harisah -
Category
Documents
-
view
29 -
download
4
description
Transcript of 5. Perinatol VIII

PerinatologiPerinatologi
Bambang Mulyawan
FK - UMM

Asfiksia Asfiksia NeonatorumNeonatorum
Asfiksia Asfiksia NeonatorumNeonatorum
Dr.Bambang Mulyawan SpADr.Bambang Mulyawan SpA
Fakultas KedokteranFakultas Kedokteran
Universitas MuhammadiyahUniversitas Muhammadiyah
M a l a n gM a l a n g

Pendahuluan (1)
Asfiksia Bayi Baru Lahir (BBL) : 15% kematian BBL (5 juta) /tahun
Angka kejadian asfiksia di RS Propinsi : 25,2% (Jawa Barat)
Angka kematian asfiksia di RS Pusat Rujukan Propinsi di Indonesia : 41%
10% BBL membutuhkan bantuan untuk mulai bernafas ( bantuan ringan res.lanjut yg ekstensif)
5% BBL membutuhkan tindakan resusitasi ringan 1% - 10% BBL di RS perlu bantuan ventilasi, hanya
sedikit yg perlu intubasi dan kompresi dada15/06/1999 Dr.Bambang M 3

Pendahuluan (2)
“Sebagian besar bayi yaitu sekitar 90% tidak membutuhkan atau hanya sedikit memerlukan bantuan untuk memantap-kan pernafasannya setelah lahir dan akan melalui masa transisi dari kehidup-an intrauterin ke ekstrauturin tanpa ma-salah.”
15/06/1999 Dr.Bambang M 4

Pendahuluan (3)
Infant resuscitation required in 6% of all births. Asphyxia usually not anticipated. All labor and delivery units required to be
skilled in neonatal resuscitation (Standard of Practice)
NALS (Neonatal Advanced Life Support)

Definisi (1)
Asfiksia neonatorum : BBL yang tidak dapat bernafas secara spontan dan teratur pada saat lahir atau beberapa saat setelah lahir.
BBL : Bayi Baru Lahir pada menit-menit pertama sp beberapa jam selanjutnya
Periode neonatal : lahir 28 hari
15/06/1999 Dr.Bambang M 6

Definisi (2)
Asfiksia BBL ditandai dg keadaan : *hipoksemia *hiperkarbia *asidosis
15/06/1999 Dr.Bambang M 7

Definisi (3)
Karakteristik asfiksia BBL /Perinatal (menurut AAP dan ACOG -2004 ) : 1. asidemia metabolik atau campuran (metabolik dan respiratorik) yang jelas, yaitu ph<7, pada sampel darah yang diambil dari a.umbilikal 2. nilai Apgar 0-3 pada menit ke 5 3. manifestasi neurologi pd periode BBL segera, termasuk kejang,hipotonia,koma atau ensefalopati hipoksisk isemik 4. terjadi disfungsi sistem multiorgan segera pada periode BBL
15/06/1999 Dr.Bambang M 8

Definisi (3-a)
Inconsistent Definitions Criteria for Neonatal Asphyxia (APA and ACOG,
1992)– Profound metabolic (or mixed) acidosis (ph < 7.0)– Persistence of Apgar score 0 - 3 for > 5 minutes– Clinical neurological sequelae– Evidence of multi-organ system dysfunction

Definisi (4)
This is pathologic condition referred to neonate who have no spontaneous breathing or represented irregular breathing movement after birth. Usually caused by perinatal hypoxia. It is emergency condition and need quickly treatment (resuscitation).

birth asphyxia is defined simply as the failure to initiate and sustain breathing at birth
The common worry of health professionals and parents is the permanent brain damage that birth
asphyxia can cause.
Definisi (4-a)

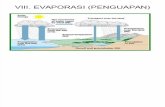
Patofisiologi asfiksia (1) BBL mempunyai karakteristik yg unik. Alveoli paru janin dalam rahim berisi cairan paru lahir
nafas pertama udara masuk alveolicairan paru diabsorpsi oleh jaringan paru dstseluruh alveoli berisi udara oksigen. Paru membutuhkan tek.puncak inspirasi dan tek.akhir ekspirasi yg tinggialiran darah paru meningkat.
Kegagalan penurunan resistensi vaskuler paru hipertensi pulmonal persisten pada BBL (Persisten pulmonary Hypertension of the neonate ) aliran drh paru inadekuat dan hipoksemia relatifekspansi par < gagal nafas ! ! !
15/06/1999 Dr.Bambang M 12

Patofisiologi (1-a)
Production of lung fluid diminishes 2-4 days before delivery
80-100 ml remain in the passageway of a full term infant
during the birth, fetal chest is compressed and squeezes fluid

Patofisiologi (1-b)
First breath is inspiratory gasp Changes trigger aortic and caratoid chemo
receptors that trigger brain’s respiratory center
Natural result of a normal vaginal delivery

Patofisiologi (1-c)
Significant decrease in environmental temperature after birth– Stimulates skin nerve endings– Newborn responds with rhythmic respirations– Excessive cooling may lead to profound
depression of cold stress

Patofisiologi (1-d)
Onset of respiration stimulates cardiovascular changes– As air enter the lungs, oxygen content rises in
alveoli and stimulates relaxation of pulmonary arteries

Patent ductus arteriosus closes– With increased oxygenated pulmonary blood flow
and loss of placenta, systemic blood flow increases, foreaman ovale closes, and PDA begins to close
– Leads to decrease in pulmonary vascular resistance-allows complete vascular flow to the lungs
Patofisiologi (1-e)

Patofisiologi (2)
When fetal asphyxia happens, the body will show a self-defended mechanism which redistribute blood flow to different organs called “inter-organs shunt” in order to prevent some important organs including brain, heart and adrenal from hypoxic damage.

Patofisiologi (3)
Hypoxic cellular damage : _reversible ( early stage ) _unreversible damage
Primary apnea Secondary apnea Other damage :
persisten pulmonary hypertension, hypo/hyperglicemia, hyperbilirubinemia
15/06/1999 Dr.Bambang M. 19

Etiologi / Faktor resiko (1)
Maternal factor: hypoxia, anemia, diabetes, hypertension, smoking, nephritis,
heart disease, too old or too young,etc Delivery condition:Abruption of placenta, placenta previa, prolapsed cord,
premature rupture of membranes,etc Fetal factor:Multiple birth, congenital or malformed fetus,etc

Etiologi / faktor resiko (2) Anticipate Asphyxia
– Preterm delivery– Thick meconium– Acute fetal or placental hemorrhage– Use of narcotics in labor– Maternal infection– Polyhydramnios: GI obstruction– Oligohydramnios: Hypoplastic lungs

Manifestasi klinis (1)
Fetal asphyxia
fetal heart rate: tachycardia bradycardia
fetal movement: increase decrease
amniotic fluid: meconium-stained

Manifestasi klinis (2)
Apgar score:
A: appearance(skin color)
P: pulse(heart rate)
G: grimace(reactive ability)
A: activity(muscular tension)
R: respiration

manifestasi klinis (2-a)
Assign Apgar Score at 1, 5, and 10 Minutes. Apgar Score more useful in Term than Preterm
Infant, but not specific for diagnosis of neonatal asphyxia.
Cord Arterial Blood Gases: Ph (< 7) and Base Deficit ( > - 4 ).

Manifestasi klinis (2-b)
Degree of asphyxia:
Apgar score 8~10: no asphyxia
Apgar score 4~8: mild/cyanosis asphyxia
Apgar score 0~3: severe/pale asphyxia

26
LOW BIRTH WEIGHT BABIES
Low birth weight
Definition : < 2500 g
Incidence : 30% neonates

Importance
LBW babies account for 25% neonatal deaths and 50% infant deaths.
LBW babies are more prone to :
- malnutrition.
- recurrent infections.
- neurodevelopmental delay.

28
Two types of LBW neonates
Preterm ( 1/3 )
Small – for – dates ( 2/3 )

29
LBW (Preterm) : Problems
Birth asphyxia
Hypothermia
Feeding difficulties
Infections
Hyperbilirubinemia
Respiratory distress
Apneic spells Intraventricular
hemorrhage Hypoglycemia Metabolic
acidosis

30
LBW (SFD) : Problems
Birth asphyxiaMeconium aspiration syndromeHypothermiaHypoglycemia InfectionsPolycythermia

Causation : IUGR / SFD
Poor nutritional status of mother.Hypertension, toxemia, anemia.Multiple pregnancy, postmaturity.Chronic malaria, chronic illness.Tobacco use.

Causation : Prematurity
Low maternal weight, teenage pregnancy, multiple pregnancy.
Previous preterm baby, cervical incompetence.
Antepartum hemorrhage, acute systemic disease.
Induced premature delivery.Majority unknown.

Identification of preterm LBW
Date of LMPPhysical features
- breast nodule, genitalia, sole creases,
ear cartilage / recoil.







Ideal place for delivery of LBW
Transfer mother before delivery to a well-equipped centre.
Prevention of hypothermia topmost priority.
Skilled person needed for effective resuscitation.

Indications for hospitalisation
Birth weight < 1800 gGestation < 34 wksUnable to feed*Sick neonate*
* Irrespective of birth weight and gestation

Sindroma Aspirasi MekoniumSindroma Aspirasi Mekonium
Meconium Aspiration SyndromeMeconium Aspiration Syndrome( MAS )( MAS )
Bambang Mulyawan
FK-UMM

Pendahuluan
MAS merupakan masalah kegawatan yg sering dijumpai di ruang bersalin ( hipoksiahipoksia intrauterine aspirasi pneumoni BBL )
Biasanya pd bayi cukup bulan dan lebih bulan ( : Kecil untuk Masa Kehamilan / KMK )
Waspada : jika BBL lahir dg cairan ketuban campur mekonium dg gejala RDS

Patogenesis dan patofisiologi
Stress intrauterin mekonium in-utero ke dlm cairan ketuban, terhisap janin ketika inspirasi o.k hipoksi dan stimulasi vagal fetal distres / sebelum persa-linan
Mekanisme keluarnya mekonium in-utero masih belum jelas

Patogenesis dan patofisiologi ( lanj.)
BBL dg cairan ketuban mekonial asfiksia antepartum atau intrapartum obstruksi jalan nafas, turunnya kapasitas paru, pe> expiratory large airway resistancxe
Obstruksi total : atelektasis. Partial : trapping udara dan hiperekspansi alveolar
Mekonium pd alveolar me< fungsi surfaktan kolaps RDS

Patogen . . . . . ( lanj. )
Hipoksia intrauterin aspirasi mekonium obstruksi mekanik / keradangan kimiawi air trapping / atelektasis ventilasi tidak seimbang / intrapulmonal shunting kebocoran udara hipoksemia asidosis sirkulasi fetal persistent

47
SINDROM ASPIRASI MEKONIUM (SAM)
Hipoksia janinHipoksia janin
Mekonium keluar & janin gaspingMekonium keluar & janin gasping
Cairan amnion yang terkontaminasi mekonium Cairan amnion yang terkontaminasi mekonium terhirup ke larings dan trakheaterhirup ke larings dan trakhea
Mekonium masuk saluran napas lebih kecil dan Mekonium masuk saluran napas lebih kecil dan alveolus alveolus
Kerusakan paru Kerusakan paru
Pembersihan sal. napas Pembersihan sal. napas tidak adekuat tidak adekuat

48
Kerusakan paru
Mekonium mengandung enzim merusak epitel bronkus, bronkiolus dan alveolus
Mekonium menyumbat sal. napas secara total/parsial beberapa bagian paru kolaps, bagian paru lain hiperinflasi

What Is Meconium?
Odorless, thick, blackish green material First seen during the third month of
gestation Accumulation of desquamated cells from
GI tract, skin, lanugo, fatty material from the vernix, amniotic fluid

Manifestasi klinis
Bervariasi : tergantung keparahan serangan hipoksik dan jumlah viskositas mekonium teraspirasi
Sering pada gestasi post matur : warna meko. pd kuku, rambut, tali pusat
Gejala RDS ( takipnea, NCH, retraksi interkostal, diameter AP dada >, sianosis
Pada gejala MAS lambat : distres nafas awal ringan. Semakin parah bbrp jam : atelektasis dan pneumonitis kimia
Auskultasi : vesikular lemag, ronki/rales, wheezing/mengi

Pemeriksaan radiologis
Foto polos dada : infiltrat kasar menyebar pd kedua lap.paru, dapat disertai pneumotoraks, atelektasis, emfisema

Chest X-Ray
Hyperinflation Coarse, patchy densities
representing scattered areas of atelectasis and consolidation mixed with air trapping


Faktor predisposisi
Insufisiensi plasenta, hipertensi, oligohidramnion, ibu kecanduan ( rokok, kokain), infeksi (chorio-amnionitis) hipoksia, manajemen jalan nafas tidak adekuat, defisiensi surfaktan, hipertensi pulmonal

Risk Factors for Meconium Passage
Postterm pregnancy Preeclampsia-eclampsia Maternal hypertension Maternal diabetes mellitus Abnormal fetal heart rate IUGR Abnormal biophysical profile Oligohydramnios Maternal heavy smoking

Infant ActiveInfant Depressed
Intrapartum suctioning of mouth, nose, pharynx
Intubate and suction trachea
Other resuscitation as indicated
Observe
Meconium in Amniotic FluidMeconium in Amniotic Fluid

Langkah diagnostik
Riwayat : PJT ( pertumbuhan janin terhambat ), kesulitan persalinan / gawat janin, persalinan dg air ketuban mekonial, asfiksia berat
Pemerksaan fisik : cair ketuban mekonial/ bayi diliputi mekonium, tl pusat/kulit bayi warna hijau, asfiksia berat bbrp jam gangguan nafas/RDS, td bayi lebih bulan
Foto toraks : AP dan Lateral Laboratorium: Hb, Ht, darah tepi, kultur Analisa Gas Darah : hipoksemia, asidemia : asidosis
metabolik, respiratorik,/kombinasi

58
Diagnosis
Cukup/lebih bulan, jarang sekali kurang bulan Cairan amnion terkontaminasi mekonium Mekonium tampak/dapat dihisap dari saluran napas
atas (bantuan laringoskop) Kulit bayi diwarnai mekonium Sesak napas Foto toraks : hiperinflasi paru disertai banyak daerah
paru yang kolaps

59
Pencegahan
Pembersihan saluran napas atas sebelum bayi bernapas saat lahir
– Penghisapan saluran napas sebelum bahu dilahirkan
– Penghisapan saluran napas (larings dan trakea) secara langsung dengan bantuan laringoskop

penatalaksanaan
Prevensi slm periode prenatal, antenatal, tindaka tepat slm intrapartum
Diagram Alur Resusitasi Neonatus

Pengobatan / terapi
Suportif : oksigen, suhu lingkungan, perawatan pernafasan, kadar gas darah arteri, terapi surfaktan, ventilasi mekanik, cairan infus glukosa 10%
Antibiotik spektrum luas Tindakan bedah :pd pneumotoraks, pneumomediastinum,
empisema subkutan : pungsi toraks, drainase

62
Perjalanan Penyakit
SAM : sesak napas sejak lahir
SAM ringan : SAM ringan : membaik membaik secara bertahap secara bertahap dalam beberapa dalam beberapa hari – beberapa hari – beberapa minggu minggu
Memburuk Memburuk secara secara progresif progresif tidak tidak tertolong tertolong
Tertolong Tertolong kerusakan paru kerusakan paru perlu waktu perlu waktu lama untuk lama untuk sembuh sembuh sempurna sempurna
SAM SAM berat berat

63
Komplikasi
1. Pneumotoraks / pneumomediastinum
2. Kerusakan akibat hipoksia pada organ lain

Pemantauan/Monitoring
Tumbuh kembang pd bayi yg selamat, hidup tanpa komplikasi (survival intact) baik
Pada bayi dg komplikasi hipoksi serebri, gagal ginjal, efek tosik O2, epilepsi, palsi serebral gangguan tumbuh kembang

Ikterus neonatorumIkterus neonatorum
-Pewarnaan kuning pada sklera dan kulit yang disebabkan oleh penumpukan bilirubin
-Terlihat pada kulit bila kadar >5 mg/dl-Terlihat pada >50% neonatus- Pada bayi prematur > bayi cukup bulan

Neonatal Hyperbilirubinemia

Jaundice is common in the first week of life and may be missed in dark skinned babies
Blanch the tip of the nose or hold baby up and gently tip forward and backward to get the eyes to open.
Teach mother to do the same at home in the first week and report to hospital if significant jaundice is observed.
Clinical assessmentJaundice
Blanching the tip of the nose
Two infants with jaundice; note yellow sclerae

Metabolisme bilirubin
HemoglobinGlobinHemeBilirubin indirek1 gram HB 34 mg bilirubin
Bil.ind terikat Albumin diangkut ke hati Diambil oleh ligandin masuk kehati Dikonyugasi oleh enzim glucoronil transferase
bilirubin direk

Metabolisme bilirubin
Bilirubin direk (empedu) disalurkan melalui duktus biliaris ke usus
Di dalam usus oleh bakteriasterkobilin dikeluarkan dengan sisa makanan sebagai feses
Sebagian diuraikan oleh enzim B-glucoronidase Bilirubin indirek diserap kembali ke darah terikat albumin hati (sirkulasi enterohepatik)

Sifat dan bahaya hiperbilirubinemia
Bilirubin indirek mudah larut dalam lemak bila kadar tinggi, tidak terikat albumin, sawar darah otak rusak melalui sawar darah – otak terikat sel otak kernikterus
Bilirubin direk larut dalam air. Bila ada atresia atau obstruksi duktus biliaris ber tumpuk dfi dalam hati merusak sel hati sirosis hepatis

Penilaian klinis ikterus
Daerah tubuh Kadar bilirubin mg/dl
Muka 4 - 8
Dada/punggung 5 -12
Perut dan paha 8 -16
Tangan dan kaki 11-18
Telapal tangan/kaki >15

Indirect Serum Bilirubin ConcentrationIndirect Serum Bilirubin Concentrationand Its Relation To The Progressionand Its Relation To The Progressionof Dermal Icterus in Full-Term Infants*of Dermal Icterus in Full-Term Infants*
11
22
44
33
55
55 55
DermalDermalZoneZone
Bilirubin (mg/100 mL)Bilirubin (mg/100 mL)
Mean ± SD Range Observations Mean ± SD Range Observations
5.9 ± 0.35.9 ± 0.38.9 ± 1.78.9 ± 1.7
11.8 ± 1.811.8 ± 1.815 ± 1.715 ± 1.7
4.3 ± 7.9 4.3 ± 7.9 5.4 ± 12.25.4 ± 12.28.1 ± 16.58.1 ± 16.5
11.1 ± 18.3711.1 ± 18.37>15 >15
13134949525245452929
1122334455
*Includes all infants whose rate of serum bilirubin rise was 0.7*Includes all infants whose rate of serum bilirubin rise was 0.7 mg/dL/h or less. mg/dL/h or less.
Dermal Zones of J aundiceDermal Zones of J aundice

Mengapa terjadi ikterus pada neonatus
Peningkatan bilirubun karena hemolisis Tidak cukup albumin sebagai pengangkut Kurang ligandin untuk mengambil ke hati Kurang konyugasi di dalam hati Ekskresi yang tidak cukup Meningkat sirkulasi entero-hepatik

Ikterus fisiologik
Timbul setelah 24 jam Kadar tertinggi pada hari ke 5 pada BCB;
pada hari ke 7 pada BKB Kadar bilirubin < 15 mg/dl Hilang dalam 14 hari Hilang tanpa perlu pengobatan

Mechanism of Physiologic Jaundice
Increased rbc’s
Shortened rbc lifespan
Immature hepatic uptake & conjugation
Increased enterohepaticCirculation

Ikterus patologik
Timbul dalam 24 jam pertama Kenaikan kadar bilirubin > 5 mg / dl / hari Bilirubin serum >15 mg / dl Ikterus berlangsung lebih dari 14 hari Warna feses dempul dan urin kuning tua Bilirubin direk > 2 mg / dl

Penyebab ikterus
Timbul dalam 24 jam pertama
* Penyakit hemolitik pada BBL: Inkompatibilitas Rh,ABO* Infeksi ; TORCH, malaria, bakteri* Defisiensi enzim G6PD

Penyebab ikterus
Timbul antara 24-72 jam* Fisiologik* Sepsis* Polisitemia* Perdarahan tertutup* Perdarahan intraventrikular* Peningkatan sirkulasi entero-hepatik

Penyebab ikterus
Timbul setelah 72 jam* Sepsis* Hematoma sefal* Hepatitis neonatal* Atresia biliaris* Breastmilk jaundice* Kelainan metabolik

Pendekatan bayi dengan ikterus
Perlu diketahui* Berat lahir* Masa gestasi* Usia dalam jam* Apakah ikterus fisiologik atau patologik* Bila ikterus adalah fisiologik dan keadaan bayi baik hanya perlu diobservasi* Bila ikterus berat periksa kemungkinan telah
terjadi kernikterus

Pemeriksaan untuk ikterus patologik
Riwayat kehamilan dan persalinan * Riwayat keluarga adanya penyakit hati * Adanya riwayat inkompatilitas darah * Penyakit ibu selama hamil * Trauma lahir, asfiksia, * Penundaan pengikatan tali pusat * Penundaan makanan per os, pengeluaran mekoneum * Pemberian ASI

Pemeriksaan untuk ikterus patologik
Pemeriksaan fisik* Prematuritas* KMK : polisitemia* Trauma lahir* Pucat : hemolisis
* Petekhie* Hepatosplenomegali Iso-imunisasi, sepsis

Pemeriksaan untuk ikterus patologik
Pemeriksaan laboratorium* Bilirubin serum total dan direk* Golongan darah dan Rhesus ibu dan bayi* Uji Coombs* Hematokrit* Hapusan darah tepi* Skrining sepsis* Fungsi hati dan tiroid untuk ikterus lanjut

Tatalaksana ikterus neonatorum
Tujuan : Mencegah keracunan oleh bilirubin
Cara1. Pencegahan hiperbilirubinemia
- Pemberian makan dini- Hidrasi adekwat
2. Penurunan kadar bilirubin- Terapi sinar- Transfusi tukar

Terapi Sinar
Prinsip : Bilirubin oleh cahaya dengan gelombang 450-460 nanometer photoisomer
yang larut dalam air Perlengkapan
lampu neon 6-8 buahtempat tidur atau inkubatoralat penutup mata

Indikasi terapi sinar
Kadar bil mg/dl Berat lahir Usia
5-9 bila hemolisis semua < 24 jam
10-14 < 2500 g >24 jam
> 2500 g (observasi)
15-19 > 2500 g >48 jam

Terapi sinar
Letakkan bayi dalam keadaan telanjang dibawah lampu dengan jarak 45 cm
Tutup mata Setiap 2 jam bayi disusui Ubah posisi bayi setiap selesai menyusui Ukur suhu setiap 4 jam Timbang bayi setiap hari Periksa kadar bilirubin setiap 12 jam Hentikan terapi sinar bila kadar < 10 mg/dl

Efek samping terapi sinar
Meningkatkan kehilangan cairan insensibel Defekasi encer Warna kemerahan pada kulit Bronze baby syndrome Hipertermia

Transfusi tukar
Indikasi :
kadar bil Berat lahir Usia
10-14 mg/dl <2500 g <24 jam
15- 19 semua <48 jam
>20 semua 0 - >72 jam

Transfusi tukar
Pilihan darah untuk transfusi tukarInkompatilitas ABO
darah golongan O +ve dalam plasma ABIsoimujjnisasi Rhesus
darah gol O –ve atau
darah golongan bayi yang Rhesus negatif
Untuk lain darah golongan bayi

Hiperbilirubinemia indirek yang memanjang
Sindrom Crigler Najjar Breastmilk jaundice Hipothiroidism Stenosis pilorus Hemolisis yang berlangsung terus Malaria

Hiperbilirubinemia direk yang memanjang
Hepatitis neonatal idiopatik Inspissated bile syndrome Infeksi Malformasi- atresia biliaris, kista kholedokus Penyakit metabolisme- galaktosemia Nutrisi parenteral total yang lama


Thanks….
But it’s not the end !!!

Brief History
A 45-year-old man was seen in the emergency department for persistent night sweats, headache, intermittent fever, and severe chills, which occurred approximately every 48 h. The patient was born in Asia and had moved to the United States 5 years earlier. At that time, he had suffered a similar illness, was treated, and appeared to make a good recovery. Blood was drawn for laboratory studies including a hemoglobin determination and thick and thin blood smears for parasites.

Brief History
The patient was slightly anemic, with a hemoglobin level of 9.5 g/dl. Examination of Giemsa-stained blood films revealed the presence of enlarged red blood cells contain ing trophozoite forms (Fig. 23.1). Several irregular ameboid trophozoites containing brown granules were seen. Eosinophilic stippling was visible in the cytoplasm of the erythrocytes. A few round to oval gametocytes were seen. Based on these findings, a diagnosis of infection with a blood parasite was made.

enlarged red blood cells contain ing trophozoite forms (Fig. 23.1).

Plasmodium falciparum and P. malariae are encountered in all shaded areas of the map (with P. falciparum by far the most prevalent). Plasmodium vivax and P. ovale are traditionally thought to occupy complementary niches, with P. ovale predominating in Sub-Saharan Africa and P. vivax in the other areas; however these two species are not always distinguishable on the basis of morphologic characteristics alone; the use of molecular tools will help clarify their exact distribution.

Features in Blood P. falciparum P. vivax P. malariae P. ovale
affected RBC normal size enlarged, a few ovalocytes
normal size normal to increased; ovalocytosis
forms in peripheral blood
ring trophozoites and gametocytes only
all forms all forms all forms
immature trophozoites (ring forms)
2 chromatin dots; 2+ rings per RBC; applique forms; rings delicate
rarely may have 2 chromatin dots or multiple rings per RBC
mature trophozoites not seen ameboid band or bayonet forms
schizonts not seen 12-24 merozoites in mature schizonts
6-12 merozoites in mature schizont, may form a circle ("daisy")
8-12 merozoites in mature schizont
gametocytes banana shaped
stippling Mauer's dots or clefts (occasional)
Schuffner's dots (usual)
Ziemann's dots (rare; if overstain)
James's stippling

Diagnostic points:- 1.Red cells containing parasites are usually enlarged. 2.Schuffner's dots are frequently present in the red cells as shown above. 3.The mature ring forms tend to be large and coarse. 4.Developing forms are frequently present.


Complications Most complications are caused by P falciparum, and they may include the following:
– Coma (cerebral malaria) • Defined as coma, altered mental status, or multiple seizures with P falciparum in the blood,
cerebral malaria is the most common cause of death in malaria patients. If untreated, this complication is lethal.
• Even with treatment, 15% of children and 20% of adults who develop cerebral malaria die. • The symptoms of cerebral malaria are similar to those of toxic encephalopathy.
– Seizures– Renal failure: As many as 30% of nonimmune adults infected with P falciparum suffer acute renal
failure.– Hemoglobinuria (blackwater fever)
• Blackwater fever is the passage of dark, Madeira-colored urine. • Hemolysis, hemoglobinemia, and the subsequent hemoglobinuria and hemozoinuria cause
this condition.– Noncardiogenic pulmonary edema: This affliction is most common in pregnant women and results
in death in 80% of patients.– Profound hypoglycemia: Hypoglycemia often occurs in young children and pregnant women. It
often is difficult to diagnose since adrenergic signs are not always present and since stupor already may have occurred in the patient.
– Lactic acidosis: This occurs when the microvasculature becomes clogged with P falciparum. If the venous lactate level reaches 45 mg/dL, a poor prognosis is very likely.
– Hemolysis resulting in severe anemia and jaundice– Bleeding (coagulopathy)

BABESIOSIS
SymptomsBabesiosis is associated with hemolytic anemia, jaundice, fever and hepatomegaly, usually 1-2 weeks after infection
DiagnosisDiagnosis is based on symptoms, patient history and detection of intraerythrocytic parasite in the patient or transfer of blood in normal hamsters which can be heavily parasitized.

Chloroquine (Aralen HCl, Aralen Phosphate) -- Inhibits parasite growth by concentrating within acid vesicles of the parasite and increasing its internal pH. In addition, inhibits hemoglobin utilization and metabolism by the parasite. Adult Dose10 mg base/kg PO, not to exceed 600 mg; then 5 mg base/kg PO; not to exceed 300 mg at 6-h, 24-h, and 48-h intervals (total 25 mg/kg)

QUESTIONS1. Which infection does this patient have? Which parasite is
infecting him?2. Describe the typical appearance of this parasite in thick and thin
Giemsa-stained smears.3. Which blood protozoan parasite morphologically resembles this
parasite?4. Comment on the size of the erythrocytes. What do we call the
eosinophilic stippling seen in these cells? Which other species causes this characteristic?
5. Describe the clinical illness caused by this parasite. Which serious complicationmay occur with this infection?
6. How does the life cycle of different species of this parasite vary? How does this fact relate to this patient's infection?
7. How would this patient be treated?