Risk factors for intensive care delirium: A systematic review
Transcript of Risk factors for intensive care delirium: A systematic review
Y
I
R
RA
BL
a
b
Uc
d
e
f
I
Disflo
M1f
(
0d
ARTICLE IN PRESSICCN-1977; No. of Pages 10
ntensive and Critical Care Nursing (2007) xxx, xxx—xxx
EVIEW
isk factors for intensive care delirium:systematic review
art Van Rompaeya,b,∗, Marieke J. Schuurmansc,illie M. Shortridge-Baggettd, Steven Truijenb, Leo Bossaerte,f
University of Antwerp, Faculty of Medicine, Division of Nursing Science and Midwifery, BelgiumUniversity College of Antwerp, Department of Health Sciences,niversiteitsplein 1, 2610 Wilrijk, BelgiumUniversity of Professional Education Utrecht, Department of Healthcare, The NetherlandsPace University, Lienhard School of Nursing, NY, USAUniversity Hospital of Antwerp, Intensive Care Department, BelgiumUniversity of Antwerp, Faculty of Medicine, Belgium
KEYWORDSIntensive care;Delirium;
Summary Delirium has been a recognised syndrome in the intensive care unit forsome years. This systematic review reports risk factors for delirium studied in theintensive care unit. Four predisposing and 21 precipitating factors, including nine
Risk factor laboratory blood values and seven items relating to the use or the administrationof medication, were found to influence the onset of delirium in the intensive careunit in six publications. The APACHE II score and hypertension were the only factorsreported twice. Risk factors for the development of intensive care delirium wereunderstudied and underreported in the literature.
l righ
tpmq
© 2007 Elsevier Ltd. Al
ntroduction
elirium is a disturbance of the cognitive processesn the brain induced by a physical cause and pre-
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
ented as an acute syndrome characterized by auctuating course. The patient encounters peri-ds of inattention in combination with disorganized
∗ Corresponding author at: University of Antwerp, Faculty ofedicine, Division of Nursing and Midwifery, Universiteitsplein, 2610 Antwerp, Belgium. Tel.: +32 3 820 25 04;ax: +32 3 820 25 01.
E-mail address: [email protected]. Van Rompaey).
a
fhlI2T1l
964-3397/$ — see front matter © 2007 Elsevier Ltd. All rights reservoi:10.1016/j.iccn.2007.08.005
ts reserved.
hinking or a changed level in consciousness. Therocess is observed as a hypoactive, hyperactive orixed type. The hyperactive type is the least fre-uent one although it is the easiest to detect (Millernd Ely, 2006; Palmieri, 2003).
The syndrome has not been well recognizedor years. In addition, it has been accepted as aarmless process. Recent evidence, however, high-ights the poor clinical outcomes (Inouye, 2006;nouye et al., 1998; Jackson, 2006; Jackson et al.,
Risk factors for intensive care delirium: A systematic2007.08.005
003; Leslie et al., 2005; Rockwood et al., 1999;homason et al., 2005; Treloar and Macdonald,997a,b). A higher morbidity, a higher mortality, aonger stay in the hospital or in the intensive care
ed.
IN
bd(ps22sapu
ttefcihlpuittepifrrhct
iiuwd
M
TaprTFii
ARTICLEYICCN-1977; No. of Pages 10
2
unit, a deterioration in the cognitive processes anda higher cost of treatment have been linked to thedelirious process. Delirium has been described as ageneral syndrome, but has been described in spe-cific settings as ‘‘postoperative delirium’’ in thesurgical patient and as ‘‘intensive care delirium’’in the intensive care unit (Roberts, 2004).
The standard assessment of delirium is per-formed by a psychiatrist using the DSM-IV criteria(Tucker, 1999). Diagnostic tools for physicians andnurses were developed during the last decade(Schuurmans et al., 2003). The confusion assess-ment method (CAM) (Inouye et al., 1990) and theNEECHAM confusion scale (NEECHAM) (Neelon etal., 1996) proved to be well validated and reg-ularly used tools to assess the delirious patient.Since the intensive care patient is not alwaysable to communicate verbally, these scales havebeen adapted for screening intubated or venti-lated patients. The confusion assessment methodfor the intensive care unit (CAM-ICU) (Ely et al.,2001b) was used most commonly in the publishedresearch concerning delirium in the intensive careunit. This scale diagnoses the delirious state by ayes or no answer to a four-point algorithm basedon the DSM-IV criteria. The NEECHAM rates thepatient on a 30—0 scale assessing the level of pro-cessing information, the level of behaviour and thephysiological condition. The patient can be clas-sified into four categories: 30—27 normal, 26—25at risk, 24—20 early to mild confused and 19—0moderate to severe confused. The intensive caredelirium checklist (Bergeron et al., 2001) and theorganic brain syndrome scale (Bjorkman Bjorkelundet al., 2006) were also commonly used diagnosti-cal tools for delirium in the intensive care unit.The development of worldwide accepted diagnos-tic tools created the opportunity to compare and toverify the onset and the process of intensive caredelirium without the need for consulting a psychi-atrist.
The intensive care patient seems to be at highrisk for the development of delirium with reportedincidences ranging from 11% to 87% (Aldemir et al.,2001; Bergeron et al., 2002; Ely et al., 2001a,b;Immers et al., 2005; Lin et al., 2004; McNicoll etal., 2005; Thomason et al., 2005). The wide range inreported incidences could be explained by the dif-ferent study designs, a difference in the method ofassessing delirium and the differences in the stud-ied population. Evidence is growing, however, thatdelirium is a common problem in all intensive care
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
units.Screening for delirium as a standard proce-
dure was often criticized. The clinical relevanceof detecting delirious patients was questioned
tahd
PRESSB. Van Rompaey et al.
ecause defined guidelines for the treatment of theiagnosed patient are still not generally acceptedLacasse et al., 2006). Multifactorial interventionrograms were developed and tested in differentettings (Inouye et al., 1999; Lundstrom et al.,005; Marcantonio et al., 2001; Milisen et al., 2001,005) albeit not in the intensive care unit. Con-equently, there seems to be an urgent need forn evidence-based development on a treatment orreventive action for delirium in the intensive carenit.
Inouye et al. created a predictive model forhe development of delirium in elderly patients inhe hospital (Inouye and Charpentier, 1996; Inouyet al., 1993). This simple model was very use-ul outside the intensive care unit. Risk factorsould be classified as predisposing or precipitat-ng. The predisposing factors e.g., age, gender,earing or visual impairment, are acquired base-ine characteristics and are patient dependent. Therecipitating e.g., disturbed laboratory blood val-es, surgical interventions, drugs or intercurrentllness, are dependent of the kind of disease andhe type of admittance to the hospital. These fac-ors are modifiable to decrease the risk a patientncounters. The onset of delirium in each individualatient is caused by an interaction of predispos-ng and precipitating factors. A higher number ofactors encountered by a patient will increase theisk on intensive care delirium. Ely et al. (2001c)eported a heavy burden on intensive care patientsaving at least 10 risk factors. Outside the intensiveare unit Inouye et al. stated that three or more ofhese factors increased the risk for delirium by 60%.
Hence, not all factors may be applicable tontensive care patients or have the same effect asn the onset of delirium outside the intensive carenit. Therefore, the aim of this systematic reviewas to explore the reported risk factors for theevelopment of delirium in the intensive care unit.
ethods
he first author searched the Pub Med databasesnd the ISI Web of Knowledge for original researchublications. Furthermore, the references of theetrieved papers were searched for additional links.he papers had to be published in English, Dutch,rench or German. Due to the tremendous ongo-ng technical, medical and nursing evolution inntensive care, publications have been limited to
Risk factors for intensive care delirium: A systematic2007.08.005
hose published during the last 10 years (Febru-ry 1997—March 2007). Moreover, most researchersave only used validated delirium assessment toolsuring the last decade to screen for the syndrome in
INY
R
iispltfTs
kswsrtttnifc2
oso
tNgwrsm(
R
TptiFacfste
ARTICLEICCN-1977; No. of Pages 10
isk factors for intensive care delirium
ntensive care patients. The papers were includedf they reported on original research in an inten-ive care unit, limited to randomized clinical trials,rospective or retrospective studies, containing ateast one risk factor for delirium. The outcome ofhe delirium assessment in the study had to beocused on the incidence or the onset of delirium.he risk factors were selected if they reached theignificance level of 95% in a multivariate analysis.
‘Intensive care delirium’ was entered as the firsteyword in the databases to focus on the inten-ive care population. Subsequently, ‘risk factor’as added. The results from both searches were
imilar, adding MESH terms or manual input by theesearcher did not reveal any further results. Afterhe systematic search, 13 publications met all ofhe inclusion criteria to be appraised by readinghe full text. After further reading only six origi-al research papers met all the criteria and werencluded in the systematic review (Fig. 1). The riskactors were presented as odds ratio (OR) with a 95%onfidence interval if possible (Bland and Altman,000).
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
A short review of the literature showed a lackf an appropriate tool for evaluation of cohorttudies. A standardized form was developed basedn the appraisal of cohort studies as published in
Figure 1 Presentation of the bibliographic research.
wSta(
ioscgCCdrwc
ptpFfap
pAtatiw
PRESS3
he British Medical Journal (Mamdani et al., 2005;ormand et al., 2005; Rochon et al., 2005). Theeneral guidelines for the review of these studiesere combined into six items in this systematic
eview. The quality of the studies was evaluatedcoring one point for each item, resulting in aaximum score of six points for the best paper
Table 2).
esults
able 1 presents a description of the includedublications. All papers were published from 2001o 2007. No randomized clinical trials concern-ng risk factors on intensive care were retrieved.ive papers reported on a prospective cohort studynd one on a retrospective record analysis. Theritical appraisal resulted in the maximum scoreor four publications, whereas two publicationscored intermediate (Table 2). In one of the latter,he description of the selected patients could notxclude a possible bias and no validated instrumentas used to assess delirium (Sommer et al., 2002).imilarly, a validated instrument was not used inhe other publication and neither the statisticalnalysis, nor the results were clearly formulatedAldemir et al., 2001).
The reported incidence for intensive care delir-um ranged from 11 to 83%. The lowest numberf included patients was 118, whereas the largestample considered 3308 patients in the intensiveare unit. The data were collected in medical, sur-ical, coronary or mixed intensive care units. TheAM-ICU and the Intensive Care Delirium Screeninghecklist were both used in two publications as theelirium assessment tool. In one research, trainedesearchers carried out a daily psychiatric interviewith a psychiatric consultation for patients with ahange in the state of consciousness.
The review identified 25 risk factors in the sixublications that proved to be significant in mul-ivariate analysis. The OR of the risk factors wasresented with a 95% confidence interval in Table 3.our factors could be classified as predisposing riskactors, 21 were precipitating factors related to thectual disease of the patient. An overview of theublished factors is synthesized in Fig. 2.
The predisposing risk factors reported were res-iratory disease, age, alcohol abuse and dementia.respiratory disease in the medical history scored
Risk factors for intensive care delirium: A systematic2007.08.005
he highest OR. Pre-existing dementia and alcoholbuse are risk factors to be considered, whereashe effect of age on the onset of delirium in thentensive care unit has been mentioned, althoughith a limited influence.
Pleasecite
thisarticle
inpress
as:Van
Rompaey
B,et
al.,Risk
factorsfor
intensivecare
delirium:
Asystem
aticreview
,Intensive
CritCare
Nurs
(2007),doi:10.1016/j.iccn.2007.08.005
AR
TIC
LE
IN P
RE
SS
YICCN-1977;
No.of
Pages10
4B.
VanRom
paeyet
al.
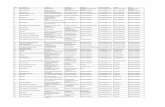
Table 1 Description of the included papers
Author, year, country, periodof data collection
Type of research Included population Delirium assessment tool Deliriumincidence
Aldemir et al. (2001), Turkey,January 1996—1997
Prospectivecohort study
N = 818 Daily psychiatric interview by trainedresearchers
11.0%
General surgery patientsadmitted to the ICU
Consult by psychiatrist for patients withchanges in state of consciousness
Age: NANo history of dementiaNo history of drug or alcohol
abuseDubois et al. (2001), Canada,
November 1998—April 1999Prospectivecohort study
N = 198 Diagnosis by an intensivist 19.2%
Medical and surgical ICU patients Confirmation by psychiatristAge: ≥18 years Intensive Care Delirium Screening
Checklist≥24 h in the ICULikely to survive ≥24 h
Sommer et al. (2002), USA,September1997—September 1998
Retrospectiverecord analysis
N = 3308 ICU admissions Haloperidol administration as anindicator of delirium occurrence (IDO)
NA
Research on 20,689 hospitalpatients
5.3% IDO (in 20,689 hospital patients)
Selection of medical and surgicalICU patients (severe illness)
Age: NAHaloperidol was administrated
McNicoll et al. (2003), USA,December 2000—July 2001
Prospectivecohort study
N = 118 CAM-ICU 31.1%
Medical ICU patientsAge: ≥65 years
Pandharipande et al. (2006),USA, February 2000—May2001
Prospectivecohort study
N = 198 CAM-ICU 83.30% Ely et al. (2001a)
Medical or coronary ICU patientsAge: ≥18 yearsMechanically ventilated
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
ARTICLE INYICCN-1977; No. of Pages 10
Risk factors for intensive care delirium
Oui
met
etal
.(2
007)
,Ca
nada
,D
ecem
ber
2003
—Au
gust
2004
Pros
pect
ive
coho
rtst
udy
N=
764
Inte
nsiv
eCa
reD
elir
ium
Scre
enin
gCh
eckl
ist
31.8
%
Med
ical
and
surg
ical
ICU
pati
ents
Age:
≥18
year
s≥2
4h
inth
eIC
ULi
kely
tosu
rviv
e≥2
4h
NA:
not
avai
labl
e;IC
U:
inte
nsiv
eca
reun
it
Iicos
aHns
iwidiDcgsTi
D
StarTscadf
rfiaca
qetotweer(
PRESS5
Among the 21 precipitating factors, the APACHEI score and hypertension were identified as signif-cant in two publications. The calculated ORs wereomparable. Hyperbilirubinaemia and the percentf days with abnormal bilirubinaemia proved to beignificant in one publication each.
Nine laboratory blood values were reported aspossible risk factor for intensive care delirium.
yperamylasaemia, hypocalcaemia, hyperbilirubi-aemia and hyponatraemia were reported as thetrongest risk factors.
Seven factors concerning the type or the admin-stration of medication in the intensive care unitere identified. Three different levels of admin-
stration of morphine influenced the onset ofelirium. The highest OR was reached for thentermediate daily dose between 7.2 and 18.6 mg.ifferent types of coma were studied for theirorrelation with intensive care delirium. The iatro-enic coma induced by medication was the onlyignificant contributor after multivariate analysis.he administration of lorazepam and dopamine also
nvoked a higher risk.
iscussion
ix original research papers, including five prospec-ive cohort studies and one retrospective recordnalysis, were selected in the systematic reviewesulting in the identification of 25 risk factors.wo factors were mentioned twice. The differentettings and the different study designs may haveaused possible factors not always to be evaluateds a risk factor. A meta-analysis was not performedue to the different context of the possible riskactors identified.
The incidence of delirium in the selected papersanged from 11% to 87% for populations rangingrom 118 to 3308 intensive care patients. Thencluded patients differed in age, medical conditionnd the type of the intensive care unit. Intensiveare delirium, however, was a severe problem inll studied units.
The diagnosis of intensive care delirium can beuestioned in two of the selected papers. Sommert al. (2002) assumed the record of haloperidol inhe patient’s database as an ‘indicator of deliriumccurrence’. A pilot pharmacy study in their hospi-al stated that 69% of the administered haloperidolas prescribed for the treatment of delirium after
Risk factors for intensive care delirium: A systematic2007.08.005
xcluding patients with a psychiatric history. Under-stimation can be expected since delirium has beeneported to be largely undetected, thus untreatedAngus and Carlet, 2002; Inouye et al., 2001;
ARTICLE IN PRESSYICCN-1977; No. of Pages 10
6 B. Van Rompaey et al.
Table 2 Critical appraisal of the included papers
Author Studydesign
Selection ofpatients
Deliriumassessment
Multivariateanalysis
Plausible Clinicallyrelevant
Total
Aldemir et al. (2001) 1 1 0 1 0 0 3Dubois et al. (2001) 1 1 1 1 1 1 6Sommer et al. (2002) 1 0 0 1 1 0 3McNicoll et al. (2003) 1 1 1 1 1 1 6Pandharipande et al. (2006) 1 1 1 1 1 1 6Ouimet et al. (2007) 1 1 1 1 1 1 6
Criteria of appraisal: (1) the study design. The description of the aim, the design and the methods were evaluated. The size ofthe sample was large enough to answer the formulated research question; (2) the selection of patients was clearly formulatedand sustained. A severe selection bias could not be detected; (3) the delirium assessment was able to retrieve all deliriouspatients. A psychiatric interview or a validated assessment tool was used to diagnose the delirious state; (4) multivariate analysiswas used to minimize possible confounding factors; (5) the statistical analysis made the results plausible. (6) The results were
aieoc
tutufs
tirorOttseTropcvnrsc
clinically relevant to medical or surgical ICU patients.
Maldonado and Dhami, 2003; Young and Inouye,2007). In the research of Aldemir et al. (2001)the psychiatric consultation was only carried outwhen the state of consciousness of the patient hadchanged. The hyperactive delirium was the mostprevalent type in this study (47%). This contradictedreports of the clinical subtypes of intensive caredelirium (Peterson et al., 2006). The assessment bytrained researchers might have missed hypoactivepatients.
The authors used different covariates in themultivariate analysis. Some factors proved to besignificant in research outside the intensive careunit (Benoit et al., 2005; Gaudreau et al., 2005;McCusker et al., 2001; Minden et al., 2005). Despitethe evidence in other settings, factors cannot beautomatically projected to the intensive care set-ting; the environment, the severity of disease andtreatment are different from the total hospital pop-ulation.
Outside the intensive care unit age is consid-ered as an established risk factor. In this reviewage was an important item in all papers as a selec-tion criterion or a possible risk factor. Patients wereincluded from 65 years in McNicoll et al. and mostof the patients in Aldemir et al. were aged under60. Whereas this factor proved to be a covariate forPandharipande et al. and Ouimet et al., it was nota significant contributor for two other researchers.After this systematic review it still can be ques-tioned if age is a strong predictor for the onset ofdelirium in the intensive care unit.
The severity of disease, measured by the APACHEII score (Knaus et al., 1985), is an important man-
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
agement tool in the intensive care unit. In thisreview, the APACHE II score was mentioned twiceas a risk factor. The score, however, was not foundsignificant in one research (Dubois et al., 2001)
tmfo
nd two researchers used the factor as an adjust-ng covariate in the multivariate analysis (Ouimett al., 2007; Pandharipande et al., 2006). Severityf disease could be an important risk factor to beonsidered in future research.
The drug related factors in this review stressedhe risk of morphine, lorazepam or the medicationsed for inducing a coma. Psychoactive drugs seemo have an active role in the onset of delirium. These of an epidural catheter could be an additionalactor either due to the extra manipulations of thetaff or the medication.
The largest group of factors was the labora-ory blood values. All except one were reportedn one publication (Aldemir et al., 2001). In thisesearch hyperamylasaemia was found in only 2.2%f the population. The other factors occurred in aange of 5.5—26.7%. This could explain the highRs with a very wide confidence. The presenta-ion of the results or the analysis did not createhe opportunity to verify the findings making themtatistically doubtful. Dubois et al. included sev-ral laboratory blood values in the data collection.hey were found not to relate to delirium. Veryecently an additional retrospective chart reviewn different risk factors (Watts et al., 2007) wasublished. Neither laboratory values nor medi-ation were significant risk factors. Continuousenovenous haemodiafiltration was the only sig-ificant risk factor in this research. The questionemains if abnormal laboratory values must be con-idered as independent risk factors or as part of thelinical picture of a more severely ill patient.
Until to now, the attention of researchers seems
Risk factors for intensive care delirium: A systematic2007.08.005
o be most focused on disease or treatment-relatedarkers. Research outside the intensive care unit
ocused on other predictive factors for the devel-pment of delirium (Blondell et al., 2004; Elie et
Pleasecite
thisarticle
inpress
as:Van
Rompaey
B,et
al.,Risk
factorsfor
intensivecare
delirium:
Asystem
aticreview
,Intensive
CritCare
Nurs
(2007),doi:10.1016/j.iccn.2007.08.005
AR
TIC
LE
IN P
RE
SS
YICCN-1977;
No.of
Pages10
Riskfactors
forintensive
caredelirium
7
Table 3 Multivariate risk factors (95% CI)
Risk factor OR (95%confidence interval)
Aldemir et al.(2001), n = 818
Dubois et al.(2001), n = 198
Sommer et al.(2002), n = 3308
McNicoll et al.(2003), n = 118
Pandharipande etal. (2006), n = 198
Ouimet et al.(2007), n = 764
Age 1.02 (1.00—1.03)Alcohol abuse 2.03 (1.26—3.25)Anemia 5.40 (1.60—17.80)APACHE II 1.06 (1.02—1.11) 1.05 (1.05—1.07)Azotemia 4.60 (1.40—5.60)Coma (with the use of
medication)3.71 (2.32—5.90)
Dementia 2.2 (1.0—5.0) RR!Dopamine 3.31 (NA)Elevated hepatic enzymes 6.30 (1.20—32.20)Epidural catheter use 3.50 (1.20—10.39)Fever 14.30 (4.10—49.30)Hyperamylasemia 43.40 (4.20—442.70)Hyperbilirubinemia 8.70 (2.0—37.70)% days with abnormal
bilirubinemia1.20 (1.03—1.40)
Hypertension 2.60 (1.14—5.72) 1.88 (1.30—2.60)Hypocalcaemia 30.90 (5.80—163.20)Hyponatremia 8.20 (2.50—26.40)Hypotension 19.80 (5.30—74.30)Infections 18.00 (3.50—90.80)Lorazepam 1.20 (1.10—1.40)Metabolic acidosis 4.50 (1.10—17.70)Morphine daily dose
0.01—7.1 mg7.80 (1.76—34.40)
Morphine daily dose7.2—18.6 mg
9.20 (2.17—39.00)
Morphine daily dose18.7—331.6 mg
6.00 (1.41—25.40)
Respiratory disease 30.60 (9.50—98.40)
All multivariate risk factors were presented as odds ratios (OR) with 95% confidence interval. Sommer et al. did not report a confidence interval for dopamine administration aftermultivariate analysis. McNicoll calculated a relative risk ratio (RR) for dementia, NA: not available.
ARTICLE IN PRESSYICCN-1977; No. of Pages 10
8 B. Van Rompaey et al.
Figure 2 Odds ratio for the multivariate risk factors with 95% CI. The odds ratio is presented on a logarithmic scale.ntia(20
R
A
A
B
B
B
B
B
B
D
D
The 95% confidence interval is presented by bars. Deme(2001); (2) Dubois et al. (2001); (3) Pandharipande et al.(6) Sommer et al. (2002).
al., 1998; Inouye et al., 1993; Korevaar et al., 2005;Voyer et al., 2006; Yamagata et al., 2005). In thissystematic review particularly, environmental riskfactors were not retrieved (Dyson, 1999; Granberget al., 1999; McCusker et al., 2001). Noise, sleepdeprivation, nursing and architectural characteris-tics of the intensive care unit were discussed, butthe effects have not been studied recently in aprospective cohort study or a randomized clinicaltrial (McGuire et al., 2000; Pandharipande and Ely,2006; Tanios et al., 2004).
Conclusion
Twenty five risk factors, 21 precipitating and 4 pre-disposing, were found to influence the onset ofdelirium in the intensive care unit. The impactof the different predisposing and precipitating riskfactors need further investigation. Additional riskfactors should be explored in the intensive care unitwith special attention to the environment and nurs-ing related factors. Hence, a tool for physicians andnurses could be developed to stratify patients indifferent risk categories and to develop preventiveactions.
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
Conflict of interest
None.
E
E
is presented as a relative risk score. (1) Aldemir et al.06); (4) Ouimet et al. (2007); (5) McNicoll et al. (2003);
eferences
ldemir M, Ozen S, Kara I, Sir A, Bac B. Predisposing factorsfor delirium in the surgical intensive care unit. Crit Care2001;5:265—70.
ngus DC, Carlet J. Surviving intensive care: a reportfrom the 2002 Brussels Roundtable. Intensive Care Med2002;29:368—77.
enoit AG, Campbell BI, Tanner JR, Staley JD, Wallbridge HR,Biehl DR, et al. Risk factors and prevalence of perioperativecognitive dysfunction in abdominal aneurysm patients. J VascSurg 2005;42:884—90.
ergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Inten-sive care delirium screening checklist: evaluation of a newscreening tool. Intensive Care Med 2001;27:859—64.
ergeron N, Skrobik Y, Dubois MJ. Delirium in critically illpatients. Crit Care 2002;6:181—2.
jorkman Bjorkelund K, Larsson S, Gustafson L, Andersson E. Theorganic brain syndrome (OBS) scale: A systematic review. IntJ Geriatr Psychiatry 2006;21:210—22.
land JM, Altman DG. Statistics notes: The odds ratio. BMJ2000;320:1468.
londell RD, Powell GE, Dodds HN, Looney SW, Lukan JK. Admis-sion characteristics of trauma patients in whom deliriumdevelops. Am J Surg 2004;187:332—7.
ubois MJ, Bergeron N, Dumont M, Dial S, Skrobik Y. Delirium inan intensive care unit: A study of risk factors. Intensive CareMed 2001;27:1297—304.
yson M. Intensive care unit psychosis, the therapeutic nurse-patient relationship and the influence of the intensivecare setting: Analyses of interrelating factors. J Clin Nurs1999;8:284—90.
Risk factors for intensive care delirium: A systematic2007.08.005
lie M, Cole MG, Primeau FJ, Bellavance F. Delirium risk fac-tors in elderly hospitalized patients. J Gen Intern Med1998;13:204—12.
ly EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L,et al. Delirium in mechanically ventilated patients: Validity
INY
R
E
E
G
G
I
I
I
I
I
I
I
I
J
J
K
K
L
L
L
L
M
M
M
M
M
M
M
M
M
M
M
N
N
O
P
P
P
P
ARTICLEICCN-1977; No. of Pages 10
isk factors for intensive care delirium
and reliability of the confusion assessment method for theintensive care unit (CAM-ICU). JAMA 2001a;286:2703—10.
ly EW, Margolin R, Francis J, May L, Truman B, Dittus RS, et al.Evaluation of delirium in critically ill patients: Validation ofthe confusion assessment method for the intensive care unit(CAM-ICU). Crit Care Med 2001b;29:1370—9.
ly EW, Siegel MD, Inouye SK. Delirium in the intensive care unit:An under-recognized syndrome of organ dysfunction. SeminRespir Crit Care Med 2001c;22:115—26.
audreau JD, Gagnon P, Harel F, Roy MA, Tremblay A. Psychoac-tive medications and risk of delirium in hospitalized cancerpatients. J Clin Oncol 2005;23:27.
ranberg A, Bergborn Engberg I, Lundberg D. Acute confusionand unreal experiences in intensive care patients in rela-tion to the ICU syndrome. Part II. Intensive Crit Care Nurs1999;15:19—33.
mmers H, Schuurmans MJ, van der Bijl JJ. Recognition of delir-ium in ICU patients: A diagnostic study of the NEECHAMconfusion scale in ICU patients. BMC Nurs 2005;4:7.
nouye SK. Delirium in older persons. N Engl J Med2006;354:1157—65.
nouye SK, Charpentier PA. Precipitating factors for delirium inhospitalized elderly persons predictive model and interrela-tionship with baseline vulnerability. JAMA 1996;275:852—7.
nouye SK, Van Dyck CH, Alessi CA, Balkin S, Siegal AP, HorwitzRI. Clarifying confusion: the confusion assessment method.A new method for detection of delirium. Ann Intern Med1990;113:941—8.
nouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A pre-dictive model for delirium in hospitalized elderly medicalpatients based on admission characteristics. Ann Intern Med1993;119:474—81.
nouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Doesdelirium contribute to poor hospital outcomes? A three-siteepidemiologic study. J Gen Intern Med 1998;13:234—42.
nouye SK, Bogardus ST, Charpentier PA, Leo-Summers L, Acam-pora D, Holford TR, et al. A multicomponent intervention toprevent delirium in hospitalized older patients. N Engl J Med1999;340:669—76.
nouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM.Nurses’ recognition of delirium and its symptoms: Com-parison of nurse and researcher ratings. Arch Intern Med2001;161:2467—73.
ackson JC. Delirium and long-term cognitive impairment: Anoverview. Clin Window Web J 2006;6:21.
ackson JC, Hart RP, Gordon SM, Shintani A, Truman B, May L, etal. Six-month neuropsychological outcome of medical inten-sive care unit patients. Crit Care Med 2003;31:1226—34.
naus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence D.APACHE II: A severity of disease classification system. CritCare Med 1985;13:818—29.
orevaar J, van Munster B, de Rooij S. Risk factors for deliriumin acutely admitted elderly patients: A prospective cohortstudy. BMC Geriatr 2005;5:6.
acasse H, Perreault MM, Williamson DR. Systematic review ofantipsychotics for the treatment of hospital-associated delir-ium in medically or surgically ill patients. Ann Pharmacother2006;40:1966—73.
eslie DL, Zhang Y, Holford TR, Bogardus ST, Leo-Summers LS,Inouye SK. Premature Death Associated With Delirium at 1-Year Follow-up. Arch Intern Med 2005;165:1657—62.
in SM, Liu CY, Wang CH, Lin HC, Huang CD, Huang PY, et al. The
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
impact of delirium on the survival of mechanically ventilatedpatients. Crit Care Med 2004;32:2254—9.
undstrom M, Edlund A, Karlsson S, Brannstrom B, Bucht G,Gustafson Y. A Multifactorial Intervention Program Reducesthe Duration of Delirium, Length of Hospitalization, and Mor-
R
R
PRESS9
tality in Delirious Patients. J Am Geriatr Soc 2005;53:622—8.aldonado J, Dhami N. Recognition and management of delirium
in the medical and surgical intensive care wards. J PsychosomRes 2003;55:150.
amdani M, Sykora K, Li P, Normand SL, Streiner DL, Austin PC,et al. Reader’s guide to critical appraisal of cohort studies:2. Assessing potential for confounding. BMJ 2005;330:960—2.
arcantonio ER, Flacker JM, Wright RJ, Resnick NM. ReducingDelirium After Hip Fracture: A Randomized Trial. J Am GeriatrSoc 2001;49:516—22.
cCusker J, Cole MG, Abrahamowicz M, Han L, Podoba JE,Ramman-Haddad L. Environmental Risk Factors for Delir-ium in Hospitalized Older People. J Am Geriatr Soc2001;49(10):1327—34.
cGuire BE, Basten CJ, Ryan CJ, Gallagher J. Intensive CareUnit Syndrome: A Dangerous Misnomer. Arch Intern Med2000;160:906—9.
cNicoll L, Pisani MA, Ely EW, Gifford D, Inouye SK. Detec-tion of Delirium in the Intensive Care Unit: Comparison ofConfusion Assessment Method for the Intensive Care Unitwith Confusion Assessment Method Ratings. J Am Geriatr Soc2005;53:495—500.
cNicoll L, Pisani MA, ZhangY, Ely EW, Siegel MD, Inouye SK.Delirium in the Intensive Care Unit: Occurrence and Clin-ical Course in Older Patients. J Am Geriatr Soc 2003;51:591—8.
ilisen K, Foreman MD, Abraham IL, De Geest S, GodderisJ, Vandermeulen E, et al. A Nurse-Led InterdisciplinaryIntervention Program for Delirium in Elderly Hip-FracturePatients. J Am Geriatr Soc 2001;49:523—32.
ilisen K, Lemiengre J, Braes T, Foreman MD. Multicomponentintervention strategies for managing delirium in hospital-ized older people: systematic review. J Adv Nurs 2005;52:79—90.
iller RR, Ely EW. Delirium and Cognitive Dysfunction inthe Intensive Care Unit. Semin Respir Crit Care Med2006;27:210—20.
inden SL, Carbone LA, Barsky A, Borus JF, Fife A, FricchioneGL, et al. Predictors and outcomes of delirium. Gen HospPsychiatry 2005;27:209—14.
eelon VJ, Champagne MT, Carlson JR, Funk SG. The NEECHAMconfusion scale: Construction, validation, and clinical test-ing. Nurs Res 1996;45:324—30.
ormand SL, Sykora K, Li P, Mamdani M, Rochon PA, AndersonGM. Readers guide to critical appraisal of cohort stud-ies: 3. Analytical strategies to reduce confounding. BMJ2005;330:1021—3.
uimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, riskfactors and consequences of ICU delirium. Intensive Care Med2007;33:66—73.
almieri TL. Intensive care unit delirium in the older patient.Curr Surg 2003;60:356—60.
andharipande P, Ely EW. Sedative and Analgesic Medications:Risk Factors for Delirium and Sleep Disturbances in the Crit-ically Ill. Crit Care Clin 2006;22:313—27.
andharipande P, Shintani A, Peterson JF, Pun BT, Wilkinson GR,Dittus RS, et al. Lorazepam Is an Independent Risk Factorfor Transitioning to Delirium in Intensive Care Unit Patients.Anesthesiology 2006;104:21—6.
eterson JF, Pun BT, Dittus RS, Thomason JWW, Jackson JC, Shin-tani AK, et al. Delirium and its motoric subtypes: A study of614 critically ill patients. J Am Geriatr Soc 2006;54:479—84.
Risk factors for intensive care delirium: A systematic2007.08.005
oberts B. Screening for delirium in an adult intensive care unit.Intensive Crit Care Nurs 2004;20:206—13.
ochon PA, Gurwitz JH, Sykora K, Mamdani M, Streiner DL,Garfinkel S, et al. Reader’s guide to critical appraisal ofcohort studies: 1. Role and design. BMJ 2005;330:895—7.
IN
T
T
V
W
Y
ARTICLEYICCN-1977; No. of Pages 10
10
Rockwood K, Cosway S, Carver D, Jarrett P, Stadnyk K, Fisk J.The risk of dementia and death after delirium. Age Ageing1999;28:551—6.
Schuurmans MJ, Deschamps PI, Markham SW, Shortridge-BaggettLM, Duursma SA. The measurement of delirium: review ofscales. Res Theory Nurs Pract 2003;17:207—24.
Sommer BR, Wise LC, Kraemer HC. Is dopamine administra-tion possibly a risk factor for delirium? Crit Care Med2002;30:1508—11.
Tanios MA, Epstein SK, Teres D. Are we ready to monitor for delir-ium in the intensive care unit? Crit Care Med 2004;32:295—6.
Thomason J, Shintani A, Peterson JF, Truman B, Jackson J, ElyEW. Intensive care unit delirium is an independent predictorof longer hospital stay: A prospective analysis of 261 non-
Please cite this article in press as: Van Rompaey B, et al.,review, Intensive Crit Care Nurs (2007), doi:10.1016/j.iccn.
ventilated patients. Crit Care 2005;9:R375—81.Treloar AJ, Macdonald AJD. Outcome of delirium: Part 2. Clin-
ical features of reversible cognitive dysfunction—are theythe same as accepted definitions of delirium? Int J GeriatrPsychiatry 1997a;12:614—8.
Y
Available online at www.s
PRESSB. Van Rompaey et al.
reloar AJ, Macdonald AJD. Outcome of delirium: Part 1. Out-come of delirium diagnosed by DSM-III-R, ICD-10 and CAMDEXand derivation of the reversible cognitive dysfunction scaleamong acute geriatric inpatients. Int J Geriatr Psychiatry1997b;12:609—13.
ucker GJ. The Diagnosis of Delirium and DSM-IV. Dement GeriatrCogn Disord 1999;10:359—63.
oyer P, McCusker J, Cole MG, Khomenko L. Influence of priorcognitive impairment on the severity of delirium symptomsamong older patients. J Neurosci Nurs 2006;38:90—101.
atts G, Roberts BL, Parsons R. Delirium in the intensive careunit: searching for causes and sources. Crit Care Resusc2007;9:26—9.
amagata K, Onizawa K, Yusa H, Wakatsuki T, Yanagawa T,
Risk factors for intensive care delirium: A systematic2007.08.005
Yoshida H. Risk factors for postoperative delirium in patientsundergoing head and neck cancer surgery. Int J Oral Maxillo-fac Surg 2005;34:33—6.
oung J, Inouye SK. Delirium in older people. BMJ 2007;334:842—6.
ciencedirect.com