Lesson Presentation Amount of Nutrition - Esher Church School
Influence of pattern of menopausal transition on the amount of trabecular bone loss
Transcript of Influence of pattern of menopausal transition on the amount of trabecular bone loss
Maturitas 55 (2006) 317–324
Influence of pattern of menopausal transition on theamount of trabecular bone loss
Results from a 6-year prospective longitudinal study
V. Seifert-Klauss a,∗, T. Link c, C. Heumann d, P. Luppa b, M. Haseitl a,J. Laakmann a, J. Rattenhuber a, M. Kiechle a
a Frauenklinik und Poliklinik, Technische Universitat Munchen, Klinikum rechts der Isar,Ismaninger Str. 22, 81675 Munchen, Germany
b Institut fur Klinische Chemie und Pathobiochemie, Technische Universitat Munchen, Germanyc
Department of Radiology, University of San Francisco, United Statesd
Institut fur Statistik, Ludwig-Maximilian-Universitat, Munchen, GermanyReceived 11 November 2005; received in revised form 22 April 2006; accepted 26 April 2006
Abstract
Introduction: Bone density is lower in postmenopausal than in premenopausal women. Recent findings have suggested thataccelerated bone loss already begins before menopause. Despite numerous cross-sectional studies on menopause-related bonedensity, longitudinal data on perimenopausal bone density changes are scarce. This study sought to characterize the dynam-ics of changes leading to postmenopausal osteopenia and to possibly find the time point at which accelarated bone lossbegins.Methods: We prospectively followed 34 pre-, peri- and early postmenopausal women without prior external hormone use,measuring their lumbar spine trabecular bone density with quantitative computer tomography at 0, 2 and 6 years. The analysisof the changes over time was done in a tri-parted fashion, since menopausal status changed variably for individual subjects: wegrouped the participants according to their currently valid menopausal classification for prospective (baseline classification),interim (2 years) and retrospective (6-year classification) analysis.Results: Six different patterns of menopausal transition were identified in our sample. Bone loss in the groups notreaching postmenopause during 6 years of observation was >50% of the maximum bone loss observed during the studyperiod.
Invariably for all analyses, the perimenopausal phase with estrogen levels still adequate was associated with the greatestreduction of trabecular bone mineral density, reaching 6.3% loss annually in the lumbar spine. By comparison, the average rateof loss was slower in the early postmenopause; total bone loss differed by pattern of menopausal transition (one-way ANOVAp < 0.05).
∗ Corresponding author. Tel.: +49 89 4140 5434; fax: +49 89 4140 4912.E-mail address: [email protected] (V. Seifert-Klauss).
0378-5122/$ – see front matter © 2006 Elsevier Ireland Ltd. All rights reserved.doi:10.1016/j.maturitas.2006.04.024
3
CQm©
K
1
oartr
mA2AsXffw
ibtsHuim“gttw5l
ewb
(
18 V. Seifert-Klauss et al. / Maturitas 55 (2006) 317–324
onclusion: The presented data for the first time show the perimenopausal course of trabecular bone loss (as measured byCT of the lumbar spine). Acceleration of bone loss during perimenopause reached half-maximal values of the total bone loss
easured around menopause, despite adequate serum estradiol levels.2006 Elsevier Ireland Ltd. All rights reserved.one loss
rdbTtfo
2
2
cIbbDpMymwidbst(ttiau(
eywords: Menopause; Bone density; Perimenopause; Estrogen; B
. Introduction
Although premenopausal bone loss occurs [1,2],steoporosis is rare during premenopause and usuallydditional risk factors – such as prolonged amenor-hoea – are relevant to this [3–5]. Little is known abouthe initiation and early time course of menopause-elated bone loss.
Longitudinal data on bone changes during theenopausal transition have been scarce until recently.study by Guthrie et al. [6] reported 2-year results on
24 Australian women aged 46–59 years at baseline.verage annual percentage rates of bone mineral den-
ity changes for the lumbar spine (measured with dual-ray absorptiometry (DXA)) ranged from +0.31%/yr
or 31 women remaining premenopausal to −2.48%/yror 42 women who became postmenopausal. 22 womenho became late perimenopausal lost −0.92%/yr.Recker et al. in 2000, published data after follow-
ng 75 women during perimenopause using semiannualone mass measurements with dual-photon absorp-iometry (DPA). During the study period, 25 womentarted HRT after menopause and 10 women startedRT before menopause [7]. The 40 women remainingntreated were divided in groups, and those remain-ng pre- or perimenopausal throughout the study were
ixed with women on hormone replacement to form anestrogen replete” group. In the total estrogen repleteroup, a linear bone loss attributed to aging was foundo be ±0%/year for the spine and −0.45% yearly forhe femoral neck. Total bone loss related to estrogenithdrawal was stated to be 10.5% for the spine and.3% for the femoral neck, but no time interval for thisoss was given.
In the presented study, we sought to elucidate thearly time course of menopause-related bone loss,
hich – according to our findings – actually beginsefore menopause.We employed quantitative computer tomographyQCT), which – other than measurement with dual X-
(
ot
ay absorptiometry (DXA) – allows measurements thatistinguish between the more hormone-sensitive tra-ecular bone and less hormone-sensitive cortical bone.his way and by taking into account the varying pat-
erns of the menopausal transition our presented studyurther expands the existing knowledge on the physi-logy of perimenopausal bone loss.
. Subjects and methods
.1. Subjects and study groups
The presented study was approved by the ethicsommittee of the Technische Universitat Munchen.nformed consent was obtained from all participantsefore entering the study. The subjects were healthy,ased on clinical and clinical-chemistry examinations.etailed description of all methods involved has beenublished with the first- and second-year results [8,9].enopausal status was classified at baseline, 2 and 6
ears as follows: premenopausal women had normalenstrual cycles with intervals of 26–32 days. Womenere classified as perimenopausal, if they reported
ncrease in menstrual cycle length of more than 5ays, irregularities of the cycle of more than 5 daysetween consecutive cycles on more than one occa-ion, and/or hot flushes of more than 5 days duringhe past year, all of which was not due to other causessee below). Postmenopausal women had experiencedheir last menstrual period 6 months to 2 years prioro the start of the study, were without another bleed-ng episode throughout the study period and addition-lly had elevated gonadotrophin levels (follicle stim-lating hormone (FSH) > 30 and luteinizing hormoneLH) > 30 IU/l) in combination with low 17�-estradiol
E2) (<50 pg/ml) concentrations.Exclusion criteria were renal insufficiency, dis-rders of lipoprotein metabolism, diabetes mellitus,hyroid disorders and any estrogenic medications 6
Maturi
matotPotmat6cwpwws
2
arbrs(mteccimoecoiamLfhata
te
2
Mu
ydtpr0
3
tra
mr12ay
rvmdahta2acmF
V. Seifert-Klauss et al. /
onths before entering the study. Other causes ofmenorrhoea were excluded by clinical investiga-ion and by demonstration of normal serum valuesf dehydroepiandrosterone sulfate (DHEAS), testos-erone (T) and thyroid stimulating hormone (TSH).rolactin (PRL) was measured only in subjects withligo-amenorrhea. All participants underwent a struc-ured medical interview including questions about
enopausal complaints, as well as past use of hormonalgents, dietary behaviour and physical activity. Afterhe initial visit, follow-up visits were scheduled at 3,, 12, and 24 months including interviews on currentomplaints and menstrual pattern. Only participantsho completed the 2-year study [9] were invited toarticipate in the 6-year follow-up study which againas approved by the ethics committee. Written consentas obtained again from all participants in the 6-year
tudy.
.2. Measurement of bone mineral density (BMD)
The BMD was examined at baseline, after 2 yearsnd after 6 years using quantitative computed tomog-aphy (QCT) of the lumbar spine (lumbar vertebralody 1–3) with two Somatom plus computed tomog-aphy systems (Siemens, Erlangen, Germany) and theame dedicated two-element solid calibration phantomOsteo calibration phantom, Siemens, Erlangen, Ger-any). Although two separate QCT machines from
he same manufacturer were used, the identical two-lement, solid calibration phantom was employed toross-calibrate the two scanners and to improve pre-ision. The longitudinal stability of QCT scannerss high, in a previous study that performed phantom
easurements over a period of 5 years, a coefficientf variation of 1–2% was calculated [10]. The QCTxaminations were performed using a standard proto-ol with 80 kVp, 146 mAs and a slice thickness (st)f 10 mm. Lateral scout images of the lumbar spinen the patients were obtained. Using the implementedutomated “Osteo”-software (Siemens, Erlangen, Ger-any) mid-vertebral sections were selected of the L1,2 and L3 regions of interest (ROIs). The values
or trabecular bone were expressed in mg calcium-
ydroxyapatite/cm3. Using this software and hardwareprecision error of 2% was previously described usinghe same calibration phantom and similar automatednalysis software [11,12]. Vertebrae that showed frac-
s
te
tas 55 (2006) 317–324 319
ures on the digital radiographs (scout views) werexcluded from the analysis.
.3. Data analysis
Patient data and measurements were collected inicrosoft Windows Excel and statistically analyzed
sing SPSS 12.0.Annual bone density changes between the first 2
ears and the 4 years thereafter were calculated byividing the measured change in bone density at eachime point by 2 or 4, respectively. Values were com-ared using Wilcoxon’s test as a nonparametric test notequiring normal distribution of variables. A p-value of.05 was used as the significance level.
. Results
Sixty-four women were originally recruited. Ofhe 42 completers of the 2-year study, 81% (n = 34)eturned for the presented 6-year-evaluation. Averagege for all subjects was 47.9 ± 5.1 years (range 33–55).
Of these participants, 10 had used external hor-one therapy for an average of 30.6 months (±19.1;
ange 15–67 months). Baseline trabecular BMD was25.1 ± 25.5 mg/cm3 and total absolute loss was1.3 ± 14.0 mg/cm3 in these users, resulting in an aver-ge bone density of 103.8 ± 25.0 mg/cm3 after the 6-ear study period.
Of the remaining 24 participants, 6 women hadeported intermittent use of local estriol or estradiol forery short time periods (mean 3.2 months, range 1–7onths). This use was considered negligible, since its
uration was less than 5% of the total study period, andll 24 women were classified as essentially untreated byormone therapy. Baseline trabecular bone density ofhese participants was 138.4 ± 35 mg/cm3, their aver-ge absolute bone loss over the total study period was3.7 ± 14.7 mg/cm3. Final BMD measurements aver-ged 114.7 ± 34.2 mg/cm3 in untreated women. Patientharacteristics are summarized in Table 1, bone densityeasurements at baseline, 2 and 6 years are shown inig. 1 in relation to menopausal status at baseline ver-
us at 6 years.No significant difference was found between short-erm hormone-ever users and untreated women forither the annual rates or the amount of total bone loss.
320 V. Seifert-Klauss et al. / Maturitas 55 (2006) 317–324
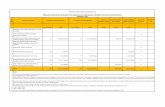
Table 1Baseline characteristics of the 24 women followed and remaininghormonally untreated throughout the study
Number of patients 24Age at baseline (years) 46.9 ± 5.4Time between baseline and study end (months) 74.2 ± 4.8Premenopausal at baseline 11Perimenopausal at baseline 7Postmenopausal at baseline 6Bodyweight at baseline (kg) 64.2 ± 15.5BMI (kg/m2) baseline 23.5 ± 3.8
Trabecular bone density (mg/cm3) baseline 138.4 ± 35.0Trabecular bone density (mg/cm3) end of study 114.7 ± 34.2Total loss in bone density (mg/cm3) during study −23.7 ± 14.8
Estradiol (pg/ml) baseline 61.1 ± 74.0Estradiol (pg/ml) study end 65.6 ± 90.7LH (IU/l) baseline 13.1 ± 10.4LH (IU/l) study end 28.5 ± 14.3FF
3
cda
ncmawr(igl
oaort(
bp(
lval
ues
and
annu
albo
nelo
ssby
men
opau
salp
atte
rnfo
rth
ree
time
poin
tsin
horm
onal
lyun
trea
ted
wom
en
nopa
usal
tran
sitio
nB
asel
ine
estr
adio
l(pg
/ml)
(±S.
D.)
Abs
olut
ean
nual
loss
year
s1–
2(m
g/cm
3)
(±S.
D.)
%A
nnua
llos
sye
ars
1–2
(±S.
D.)
from
base
line
Est
radi
olat
2ye
ars
(pg/
ml)
(±S.
D.)
Abs
olut
ean
nual
loss
(mg/
cm3)
year
3–6
mea
n(±
S.D
.)
%A
nnua
llos
sye
ars
3–6
from
2-ye
arB
MD
Est
radi
olat
6ye
ars
(pg/
ml)
(±S.
D.)
–pre
–pre
(n=
5)31
.6±
11.9
*−2
.8±
3.9
−1.7
±2.
097
.4±
37.6
*−0
.76
±2.
8−0
.7±
2.2
175.
8±
148.
9–p
re–p
eri(
n=
3)52
.0±
36.5
−0.8
±1.
4−0
.8±
1.3
88.0
±69
.8−5
.4±
3.6*
−4.3
±2.
645
.0±
45.0
ri–p
eri–
peri
(n=
2)41
.5±
37.5
−2.1
±0.
04*
−1.5
±0.
418
0.0
±24
7.5
−5.6
±1.
2*−3
.9±
0.2
90.0
±73
.5–p
eri–
post
(n=
3)41
.0±
45.0
−4.7
±7.
6−3
.6±
5.7
111.
7±
75.6
−8.0
±2.
7*−5
.5±
1.1*
54.5
±44
.5i–
peri
–pos
t(n
=5)
132.
6±
129.
3−4
.5±
5.1
−3.2
±3.
621
.0±
24.1
−6.6
±3.
0*−4
.7±
1.4*
28.2
±28
.0t–
post
–pos
t(n
=6)
47.3
±58
.3−4
.1±
2.9*
−3.4
±2.
58.
0±
5.3*
−3.0
±1.
6−2
.8±
1.4*
18.3
±3.
5*
patte
rnof
men
opau
salt
rans
ition
acco
rdin
gto
men
opau
sals
tatu
sat
base
line,
afte
r2an
d6
year
s(p
atte
rns
A–F
)and
resp
ectiv
ese
rum
estr
adio
lval
ues
atba
selin
e,an
nual
ars
1an
d2
abso
lute
(mg/
cm3/y
r)an
dre
lativ
eto
base
line
BM
D(%
/yr)
,ser
umes
trad
iola
t2ye
ars,
annu
allo
ssdu
ring
year
s3–
6ab
solu
te(m
g/cm
3/y
r)an
dre
lativ
eto
(%/y
r),a
ndse
rum
estr
adio
lat6
year
s.O
ne-w
ayA
NO
VA
:Bas
elin
ees
trad
ioln
.s.,
2-ye
ar-e
stra
diol
p=
0.05
2,6-
year
-est
radi
olp
=0.
053
for
diff
eren
ces
betw
een
grou
ps.
OV
A:a
nnua
lbon
elo
ssye
ars
1an
d2:
n.s.
;ann
ualb
one
loss
year
s3–
6p
=0.
010
and
tota
lbon
elo
ssp
=0.
012
for
diff
eren
ces
betw
een
grou
ps.
ordi
ffer
ence
from
0in
the
one-
side
dt-
test
.
SH (IU/l) baseline 27.6 ± 27.5SH (IU/l) study end 62.3 ± 36.9
.1. Annual rates of bone loss
Annual rates of bone loss for the first 2 years werealculated relative to baseline BMD, rates of bone lossuring years 3–6 relative to the bone density reachedt 2 years (Table 2).
Annual bone loss during the first 2 years differed sig-ificantly between pre- and perimenopausal women solassified at 2 years (p = 0.03). Women grouped as peri-enopausal at the 6-year-examination had experiencedtotal bone loss of −24.4 ± 9.7 mg/cm3 (18.3 ± 7.1%)hich was not significantly less than the loss expe-
ienced by women then classified as postmenopausal−29.2 ± 13.0 mg/cm3 or −21.3 ± 7.7%). The signif-cance found by ANOVA for differences betweenroups (p = 0.031) was dominated by the much loweross (−7.5 ± 13.1) in premenopausal women.
In hormonally untreated women (n = 24), webserved an acceleration of bone loss for womenpproaching peri- and postmenopause over the coursef the study, while those women who already hadeached early postmenopause at the beginning ofhe study remained relatively stable by comparisonFig. 1).
Comparing average annual rates of bone lossetween years 1 and 2 and years 3–6, women who wereremenopausal at baseline showed accelerating loss−2.8 ± 4.5 to −4.0 ± 4.21 mg/cm3/yr). This was even Ta
ble
2M
ean
estr
adio
Patte
rnof
me
Patte
rnA
:pre
Patte
rnB
:pre
Patte
rnC
:pe
Patte
rnD
:pre
Patte
rnE
:per
Patte
rnF:
pos
Subg
roup
sby
loss
duri
ngye
2-ye
arB
MD
One
-way
AN
*p
≤0.
05f
V. Seifert-Klauss et al. / Maturitas 55 (2006) 317–324 321
F - and pos s accord
mawfs
mhmi
3
swwnofi
bpftwl
mppa(awtm
ig. 1. Trabecular bone density in 24 hormonally untreated pre-, peritatus according to baseline classification. Below: menopausal statu
ore pronounced in women who were perimenopausalt baseline (3.8 ± 4.3 rising to 6.3 ± 2.6 mg/cm3/yr),hile initially early postmenopausal women slowed
rom 4.1 ± 2.9 to 3.0 ± 1.6 mg/cm3/yr (data nothown).
Classification of women according to theirenopausal status at baseline, at 2 years or at 6 years
ad no influence on the observation that the peri-enopausal years were associated with the greatest loss
n trabecular bone density (Fig. 1).
.2. Patterns of menopausal transition
During the long study period, menopausal clas-ification changed variably over time for individualomen. The perimenopausal group at 6 years included
omen who had been ‘late’ premenopausal (but hadot yet entered the perimenopausal phase) at the startf the study. Likewise, three women initially classi-ed as early postmenopausal had to be reclassified asss16
stmenopausal women at baseline, 2 and 6 years. Above: menopausaling to end-of-study classification after 6 years.
eing perimenopausal at a later time point. Thus, theerimenopausal group was the most heterogeneous. Tourther study the influence of changing menopausal sta-us over time, the time course of menopausal transitionas coded with a three-part code and longitudinal bone
oss re-analyzed according to the six resulting patterns.The chronological order of classification of
enopausal status at 0, 2, and 6 years resulted inattern A for premenopausal women who remainedremenopausal throughout the study (pre–pre–pre)nd five further patterns: B (pre–pre–peri), Cperi–peri–peri), D (pre–peri–post), E (peri–peri–post)nd F (post–post–post) as shown in Fig. 2. Womenho experienced prolonged perimenopause during
he complete 6-year study without becoming post-enopausal (group C: peri–peri–peri) experienced
ubstantial loss of trabecular bone, although theirerum estrogen remained high (serum estradiol 41.5,80, and 90 pg/ml, respectively, at baseline, 2 andyears). Their total trabecular bone loss averaged
322 V. Seifert-Klauss et al. / Maturi
Fig. 2. Bars depict annual rates of bone loss during years 1 and 2,during years 3–6, and total absolute trabecular loss in mg/cm3 forsix patterns of menopausal transition observed. Patterns according toclassification at 0, 2, 6 years—pattern A: pre, pre, pre (n = 5); patternB: pre, pre, peri (n = 3); pattern C: peri, peri, peri (n = 2); pattern D:pre, peri, post (n = 3); pattern E: peri, peri, post (n = 5); pattern F: post,post, post (n = 6). According to this grouping, women in groups A–CdEt
−otap
uospfamBw
falysl−
2−pApic
lyaeda8wng(d(
4
ivpmasmocobmicmewl
id not reach postmenopause during the study, while groups D anddid. Group A stayed premenopausal, group F was postmenopausal
hroughout the study.
26.4 ± 4.9 mg/cm3, 70% of the maximum bone lossbserved (group E: peri–peri–post:−37.5 mg/cm3 totalrabecular loss), and both groups lost more than womenlready in early postmenopause at baseline (group F:ost–post–post: −20.1 ± 6.8 mg/cm3).
The weight of the women studied was near thepper border of normal weight, with an average BMIf 24.8. Neither baseline BMI nor BMI at 2 years wereignificantly different between menopausal transitionattern groups in the Kruskal–Wallis test. ANCOVAor influence of baseline BMI on the bone loss observedfter 6 years showed no interaction between BMI andenopausal patterns. Also, no significant influence ofMI on the total bone loss (or bone loss after 2 years)as seen.One-way ANOVA analysis showed significant dif-
erences between patterns for bone loss (p = 0.010 fornnual rates in years 3–6 and p = 0.012 for total boneoss). While no differences became significant during
ears 1 and 2, the effect for loss during years three toix was dominated by significant differences in annualoss (post hoc tests) between patterns A (pre–pre–pre:0.76 ± 2.8 mg/cm3/yr) and B (pre–pre–peri: −4.3 ±
dta
tas 55 (2006) 317–324
.6 mg/cm3/yr; p = 0.026), A and C (peri–peri–peri:3.9 ± 0.24 mg/cm3/yr; p = 0.042), A and D (pre–
eri–post: −5.5 ± 1.1 mg/cm3/yr; p = 0.001), andand E (peri–peri–post: −4.7 ± 1.4 mg/cm3/yr;
= 0.002), while the difference between bone lossn patterns A and F (post–post–post: −2.8 ± 1.4 mg/m3/yr) was not significant (p = 0.176).
One-way ANOVA for differences in serum estrogenevels for the various patterns at baseline, 2 years and 6ears was barely significant only at 2 years (p = 0.052)nd at 6 years (0.053). In post hoc testing, the differ-nce at 2 years was attributable to the elevated estra-iol in pattern C (peri–peri–peri) (180.0 ± 247.5 pg/ml)nd the low estradiol in E and F (21.0 ± 24.1 and.0 ± 5.3 pg/ml), respectively. At 6 years, the womenho were still premenopausal (pattern A) had sig-ificantly higher estradiol (175.8 ± 148.9 pg/ml) thanroup B (pre–pre–peri: 45 ± 45 pg/ml) and group Fpost–post–post: 18.3 ± 3.5 pg/ml), but other patternsid not differ significantly from each other for estradiolall values shown in Table 3).
. Discussion
Our study shows significant loss of trabecular bonen perimenopausal women and the presented intraindi-idual longitudinal results offer new insight into bonehysiology around menopause. Still, it must be born inind that here trabecular bone loss only was considered
nd bone density changes would be less if total lumbarpinal body mass including all cortical bone had beeneasured by DXA. Therefore, this report is only on
ne component influencing fracture, apart from corti-al bone. Since 1996, the WHO proposes a definitionf perimenopause that includes the endocrinological,iological and clinical characteristics of approachingenopause [13]. We followed this definition by includ-
ng relevant changes in menstrual cycle in our classifi-ation. Other authors too, have found the inclusion ofenopausal symptoms useful in evaluating bone min-
ral density: thus, Salamone et al. reported that womenith irregular cycles had greater annual rates of bone
oss than asymptomatic women [14].
Despite the small sample size, we found significantifferences between the various patterns of menopausalransition. Appreciation of the existence of such vari-tions may be of value, e.g. in judging non-response
V. Seifert-Klauss et al. / MaturiTa
ble
3M
ean
estr
adio
l,L
Han
dFS
Hva
lues
atba
selin
e,af
ter
2ye
ars
and
afte
r6
year
sfo
rsi
xpa
ttern
sof
men
opau
salt
rans
ition
Patte
rnof
men
opau
salt
rans
ition
Bas
elin
ees
trad
iol(
pg/m
l)(±
S.D
.)
Bas
elin
eL
H(I
U/l)
(±S.
D.)
Bas
elin
eFS
H(I
U/l)
(±S.
D.)
Est
radi
olat
2ye
ars
(pg/
ml)
(±S.
D.)
LH
at2
year
s(I
U/l)
(±S.
D.)
FSH
at2
year
s(I
U/l)
(±S.
D.)
Est
radi
olat
6ye
ars
(pg/
ml)
(±S.
D.)
LH
at6
year
s(I
U/l)
(±S.
D.)
FSH
at6
year
s(I
U/l)
(±S.
D.)
Patte
rnA
:pre
–pre
–pre
(n=
5)31
.6±
11.9
*2.
3±
1.3
5.5
±2.
097
.4±
37.6
*3.
7(±
2.0)
3.6
(±1.
5)17
5.8
±14
8.9
5.0
±3.
74.
8±
2.6
Patte
rnB
:pre
–pre
–per
i(n
=3)
52.0
±36
.53.
2±
2.0
3.5
±0.
988
.0±
69.8
4.1
±3.
56.
3±
3.7
45.0
±45
.041
.0±
2.0
74.0
±37
.4Pa
ttern
C:p
eri–
peri
–per
i(n
=2)
41.5
±37
.518
.2±
6.9
32.3
±14
.318
0.0
±24
7.5
23.8
±5.
432
.7±
31.0
90.0
±73
.532
.0±
0.0
56.5
±7.
8Pa
ttern
D:p
re–p
eri–
post
(n=
3)41
.0±
45.0
11.1
±5.
318
.2±
4.7
111.
7±
75.6
24.7
±16
.129
.6±
10.4
54.5
±44
.534
.5±
13.4
60.5
±14
.8Pa
ttern
E:p
eri–
peri
–pos
t(n
=5)
132.
6±
129.
319
.6±
14.0
36.6
±32
.121
.0±
24.1
24.7
±10
.055
.7±
26.1
828
.2±
28.0
37.8
±8.
985
.8±
26.6
Patte
rnF:
post
–pos
t–po
st(n
=6)
47.3
±58
.320
.8±
4.5
53.9
±28
.18.
0±
5.3*
21.0
±11
.855
.7±
24.6
18.3
±3.
5*30
.2±
8.1
83.7
±21
.6
One
-way
AN
OV
A:b
asel
ine
estr
adio
ln.s
.,2-
year
-est
radi
olp
=0.
052,
6-ye
ar-e
stra
diol
p=
0.05
3fo
rdif
fere
nces
betw
een
grou
ps.O
ne-w
ayA
NO
VA
:bas
elin
eL
Hp
=0.
003,
2-ye
ar-L
Hp
=0.
009,
6-ye
ar-L
Hp
=0.
001
for
diff
eren
ces
betw
een
grou
ps.O
ne-w
ayA
NO
VA
:ba
selin
eFS
Hp
=0.
014,
2-ye
ar-F
SHp
=0.
002,
6-ye
ar-F
SHp
=0.
001
for
diff
eren
ces
betw
een
grou
ps.
*p
≤0.
05fo
rdi
ffer
ence
from
0in
the
one-
side
dt-
test
.
oFm
hps“opacoAouwt
baf2−
ptphSn
wammwt
5
ttImm
tas 55 (2006) 317–324 323
f bone density to HRT in low FSH [15], since lowSH may indicate that women are not yet peri- or post-enopausal, despite low estradiol.Accelerated bone loss around the time of menopause
as been shown to happen in most women [7], butarticularly high losses have been stated to occur in aubset of women not yet fully defined. These so-calledfast losers” were said to possibly make up for 25%f females and to be at increased risk for osteoporosisarticularly of the spine in later life according to oneuthor [16]. Increased loss was stated to correlate withalcitonin levels in cross-sectional work [17], whilethers found no evidence at all of a fast loser group [18].s the complex endocrinology of perimenopause hasnly been acknowledged in more recent years [13], thenknowing inclusion or exclusion of perimenopausalomen may have accounted for divergent findings on
he fast loser phenomenon in earlier studies.In the 2-year Australian study [6], time between
one scans (DXA) ranged from 14 to 41 months. Anverage lumbar spinal loss of −2.48%/yr was foundor 42 women who became postmenopausal, while the2 women who became late perimenopausal lost only0.92%/yr.While the Australian sample was larger than the one
resented here, we were able to study the dynamics ofrabecular as opposed to total vertebral bone densityrospectively over several predefined time points in aomogenous sample of hormonally untreated women.uch longitudinal data have not been available up toow for the perimenopausal period.
While DXA measurements enable comparisonsith larger studies in older postmenopausal subjects,
nd most data originate from therapeutic trials [19],easurements with QCT as used in this study assessore accurately early changes in trabecular bone,hich is more sensitive to hormonal stimuli than cor-
ical bone.
. Conclusion
Trabecular bone, reacting quickly and sensitivelyo hormonal changes associated with the menopausal
ransition, shows earlier loss than previously assumed.n our study, bone loss was greatest during peri-enopause, compared to both pre- and early post-enopause. Since perimenopause is often associated3 Maturi
wteTlm
ohfobedaLsmpt
pio
A
isngbHbmP
R
[
[
[
[
[
[
[
[
[
[19] Ravn P, Bidstrup M, Wasnich RD, et al. Alendronate and
24 V. Seifert-Klauss et al. /
ith elevated estrogen levels, causative factors addi-ional to or other than estrogen deprivation may be rel-vant in the early onset of menopause-related bone loss.o our knowledge, the presented paper is the first pub-
ication to explore the association between pattern ofenopausal transition and perimenopausal bone loss.In summary, we feel our findings offer a broadening
f the view on perimenopausal bone physiology per-aps also leading to studies including non-estrogenicactors associated with perimenopause. Since the timef initiation of this bone loss is not one characterizedy estrogen depletion, other mechanisms precedingstrogen depletion are candidates for influencing boneensity changes during the menopausal transition. suchs changes in levels of progesterone, inhibins, activin,H and FSH, which deserve to be studied in a largerample. Characterization of the physiology of peri-enopausal bone loss will also be valuable for com-
aring any bone density- relevant interventions duringhis life phase.
Then, possibly a more differentiated approach toerimenopausal bone loss will help to individualize thenitiation of preventive strategies for postmenopausalsteoporosis.
cknowledgements
The excellent technical support with clinical chem-stry measurements and radiology bone scans by thetaff of the departments of clinical chemistry and diag-ostic radiology at the Klinikum rechts der Isar isratefully acknowledged. This work was supportedy a PhD-fellowship to V. Seifert-Klauss under theSP/HWP-program from the German government andy unrestricted grants for clinical chemistry measure-ents from Roche Diagnostics, Germany and Solvayharmaceuticals, Germany.
eferences
[1] Sowers MR, Galuska DA. Epidemiology of bone mass in pre-menopausal women. Epidemiol Rev 1993;15:374–98.
[2] Smith R, Phillips AJ. Osteoporosis during pregnancy and itsmanagement. Scand J Rheumatol Suppl 1998;107:66–7.
[3] Soyka LA, Grinspoon S, Levitsky LL, Herzog DB, Klibanski A.The effects of anorexia nervosa on bone metabolism in femaleadolescents. J Clin Endocrinol Metab 1999;84:4489–96.
tas 55 (2006) 317–324
[4] Hampson G, Evans C, Petitt RJ, et al. Bone mineral den-sity, collagen type 1 alpha 1 genotypes and bone turnover inpremenopausal women with diabetes mellitus. Diabetologia1998;41:1314–20.
[5] Klibanski A, Biller BM, Schoenfeld DA, Herzog DB, Saxe VC.The effects of estrogen administration on trabecular bone loss inyoung women with anorexia nervosa. J Clin Endocrinol Metab1995;80:898–904.
[6] Guthrie JR, Ebeling PR, Hopper JL, et al. A prospective study ofbone loss in menopausal Australian-born women. OsteoporosInt 1998;8:282–90.
[7] Recker R, Lappe J, Davies K, Heaney R. Characterization ofperimenopausal bone loss: a prospective study. J Bone MinerRes 2000;15:1965–73.
[8] Seifert-Klauss V, Mueller JE, Luppa PB. Bone metabolismduring the perimenopausal transition: a prospective study. EurMenopause J 2001.
[9] Rosenbrock H, Seifert-Klauss V, Kaspar S, Busch R, Luppa PB.Changes of biochemical bone markers during the menopausaltransition. Clin Chem Lab Med 2002;40:143–51.
10] Braillon P. Quantitative computed tomography precision andaccuracy for long-term follow-up of bone mineral density mea-surements: a five year in vitro assessment. J Clin Densitom2002;5:259–66.
11] Kalender W. Neue Entwicklungen in der Knochendichtemes-sung mit quantitativer Computertomographie (QCT). Radi-ologe 1988;28:173–8.
12] Prevrhal SGH. Quantitative computer tomography. Radiologe1999;39:194–202.
13] Prior JC. Perimenopause: the complex endocrinology of themenopausal transition. Endocr Rev 1998;19:397–428.
14] Salamone LM, Gregg E, Wolf RL, et al. Are menopausalsymptoms associated with bone mineral density and changesin bone mineral density in premenopausal women? Maturitas1998;29:179–87.
15] Komulainen M, Kroger H, Tuppurainen MT, et al. Preventionof femoral and lumbar bone loss with hormone replacementtherapy and vitamin D3 in early postmenopausal women: apopulation-based 5-year randomized trial. J Clin EndocrinolMetab 1999;84:546–52.
16] Christiansen C, Riis BJ, Rodbro P. Prediction of rapid bone lossin postmenopausal women. Lancet 1999;1:1105–8.
17] Chen JT, Shiraki M, Katase K, Kato T, Hirai Y, HasumiK. Calcitonin physiologically regulates the postmenopausalbone loss and possibly inhibits the bone loss in fastlosers. Nippon Sanka Fujinka Gakkai Zasshi 1994;46:1056–62.
18] Keen RW, Nguyen T, Sobnack R, Perry LA, Thompson PW,Spector TD. Can biochemical markers predict bone loss at thehip and spine? a 4-year prospective study of 141 early post-menopausal women. Osteoporos Int 1996;6:399–406.
estrogen-progestin in the long-term prevention of bone loss:four-year results from the early postmenopausal interventioncohort study. A randomized, controlled trial. Ann Intern Med1999;131:935–42.