Free copper and resting temporal EEG rhythms correlate across healthy, mild cognitive impairment,...
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Free copper and resting temporal EEG rhythms correlate across healthy, mild cognitive impairment,...
www.elsevier.com/locate/clinph
Clinical Neurophysiology 118 (2007) 1244–1260
Free copper and resting temporal EEG rhythms correlate acrosshealthy, mild cognitive impairment, and Alzheimer’s disease subjects
Claudio Babiloni a,b,*, Rosanna Squitti c, Claudio Del Percio a,b, Emanuele Cassetta c,Maria Carla Ventriglia c, Florinda Ferreri c,d, Mario Tombini d, Giovanni Frisoni b,c,
Giuliano Binetti b, Mariella Gurzı b, Serenella Salinari e, Filippo Zappasodi c,f,Paolo M. Rossini b,c,d
a Dip. Fisiologia Umana e Farmacologia, Univ. ‘‘La Sapienza’’, Rome, Italyb IRCCS ‘‘Centro S. Giovanni di Dio-F.B.F.’’, Brescia, Italy
c A.Fa.R., Dip. Neuroscienze Osp. FBF, Isola Tiberina, Rome, Italyd Clin. Neurol. University ‘‘Campus Biomedico’’, Rome, Italy
e Dip. Informatica e Sistemistica, Univ. ‘‘La Sapienza’’, Rome, Italyf ISTC-CNR, Rome, Italy
Accepted 8 March 2007Available online 25 April 2007
Abstract
Objective: The present study tested the hypothesis that the serum copper abnormalities were correlated with alterations of resting elec-troencephalographic (EEG) rhythms across the continuum of healthy elderly (Hold), mild cognitive impairment (MCI), and ADsubjects.Methods: Resting eyes-closed EEG rhythms delta (2–4 Hz), theta (4–8 Hz), alpha 1 (8–10.5 Hz), alpha 2 (10.5–13 Hz), beta 1 (13–20 Hz),beta 2 (20–30 Hz), and gamma (30–40 Hz), estimated by LORETA, were recorded in 17 Hold, 19 MCI, 27 AD� (MMSE P 20), and 27AD+ (MMSE 6 20) individuals and correlated with copper biological variables.Results: Across the continuum of Hold, MCI and AD subjects, alpha sources in parietal, occipital, and temporal areas were decreased,while the magnitude of the delta and theta EEG sources in parietal, occipital, and temporal areas was increased. The fraction of serumcopper unbound to ceruloplasmin positively correlated with temporal and frontal delta sources, regardless of the effects of age, gender,and education.Conclusions: These results sustain the hypothesis of a toxic component of serum copper that is correlated with functional loss of AD, asrevealed by EEG indexes.Significance: The present study represents the first demonstration that the fraction of serum copper unbound to ceruloplasmin is corre-lated with cortical delta rhythms across Hold, MCI, and AD subjects, thus unveiling possible relationships among the biological param-eter, advanced neurodegenerative processes, and synchronization mechanisms regulating the relative amplitude of selective EEG rhythms.� 2007 International Federation of Clinical Neurophysiology. Published by Elsevier Ireland Ltd. All rights reserved.
Keywords: Copper; Ceruloplasmin; Mild cognitive impairment (MCI); Alzheimer’s disease (AD); Electroencephalography (EEG); Low resolution brainelectromagnetic tomography (LORETA)
1388-2457/$32.00 � 2007 International Federation of Clinical Neurophysiolo
doi:10.1016/j.clinph.2007.03.016
* Corresponding author. Address: Dipartimento di Fisiologia Umana eFarmacologia, Universita degli Studi di Roma ‘‘La Sapienza’’, P.le AldoMoro 5, 00185 Rome, Italy. Tel.: +39 06 49910989; fax: +39 06 49910917.
E-mail address: [email protected] (C. Babiloni).URL: http://hreeg.ifu.uniroma1.it/ (C. Babiloni).
1. Introduction
Quantitative analysis of electroencephalographic (EEG)rhythms in awakening subjects at rest is a low-cost andwidely available neurophysiological approach to the study
gy. Published by Elsevier Ireland Ltd. All rights reserved.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1245
of Alzheimer’s disease (AD) (Maurer and Dierks, 1992;Szelies et al., 1992; Leuchter et al., 1993; Schreiter-Gasseret al., 1993). When compared to healthy elderly subjects(Hold), AD patients have been characterized by an exces-sive delta (0–4 Hz) and a significant decrement of posterioralpha rhythms (8–12 Hz; Dierks et al., 1993, 2000; Huanget al., 2000; Ponomareva et al., 2003; Jeong, 2004; Babiloniet al., 2004a). EEG rhythm abnormalities in dementia havebeen associated with altered regional cerebral blood flow(rCBF)/metabolism and cognitive function as evaluatedby Mini Mental State Examination (MMSE; Ihl et al.,1989; Sloan et al., 1995; Rodriguez et al., 1998, 1999a,b;Nobili et al., 2002; Jeong, 2004). Similar EEG abnormali-ties have been reported in subjects with mild cognitiveimpairment (MCI), a clinical state between elderly normalcognition and dementia in which subjects present memorycomplaints and objective evidence of cognitive impairment(Flicker et al., 1991; Petersen et al., 1995, 2001; Gao et al.,1998). It has been shown that MCI subjects had an increaseof theta (4–7 Hz) and a decrease of alpha power (Zappoliet al., 1995; Jelic et al., 1996; Huang et al., 2000) when com-pared to Hold subjects. Furthermore, these EEG changeshad an intermediate magnitude with respect to thoseobserved in Hold and dementia patients (Elmstahl andRosen, 1997; Huang et al., 2000; Jelic et al., 2000; Jiang,2005; Babiloni et al., 2006a; Prichep et al., 2006).
Keeping in mind the above data, what is the neural sub-strate of abnormal EEG rhythms in AD? It has been sug-gested that early AD processes include loss of cholinergicbasal forebrain neurons projecting to hippocampus andfronto-parietal areas and that alpha and slower EEGrhythms can be modulated by these neurons (Helkalaet al., 1996; Holschneider et al., 1999; Mesulam et al.,2004). In contrast, brainstem cholinergic innervation ofthe thalamus would be relatively spared in AD (Mashet al., 1985; Geula and Mesulam, 1989, 1996, 1999; Mesu-lam et al., 2004). Furthermore, delta rhythms increase inAD patients as a function of atrophy in mesial–temporal,posterior, and/or frontal cortical areas (Fernandez et al.,2003; Babiloni et al., 2006a).
A corollary issue is: what is the relationship betweenEEG abnormalities in AD and neurodegenerative pro-cesses? Several lines of evidence have suggested that theseprocesses – besides other putative etiological agents – arealso related to copper homeostasis in AD. First, the metal-lochemistry hypothesis of AD proposes that a stochasticneurochemical event, such as copper elevation in AD brain,can cause a b amyloid (b-amyloid) conversion to rougeform, generating H2O2, resulting in brain damage (Bush,2003). Second, copper is specifically higher in serum ofAD patients in comparison with healthy elderly subjectsand patients with vascular dementia, and abnormalities inserum copper are representative of functional or anatomi-cal deficits in AD (Squitti et al., 2002, 2005; Smorgonet al., 2004; Giubilei et al., 2004). Third, the concentrationof copper is elevated in amyloid plaques, but appears to bedecreased at intracellular/parenchyma level (Bayer et al.,
2006; Religa et al., 2006). Fourth, an increase of the frac-tion of copper not bound to ceruloplasmin (non-cerulo-plasmin bound copper – NCC) seems to be characteristicof AD and possibly implicated in its pathogenesis; NCCis slightly bound to albumin, peptides, aminoacids and,due to its low molecular weight, is able to cross thebrain–blood barrier (Stremmel et al., 1991; Hoogenraad,2001; Twomey et al., 2005; Squitti et al., 2005, 2006). Fifth,amyloid precursor protein (APP) possesses selective zincand copper binding sequences, which might mediate redoxactivity (Citron et al., 1997; Cherny et al., 1999). Sixth,copper can catalyze a flux of reactive oxygen species thatcan damage functional and structural macromolecules inthe brain (Atwood et al., 1998, 1999, 2000). Seventh,abnormalities in copper distribution correlate with func-tional or anatomical deficits in AD (Snaedal et al., 1998;Squitti et al., 2002; Giubilei et al., 2004).
The clinical significance of NCC is well exemplified inWilson’s disease, characterized by pathological accumula-tion of copper in organs/tissues due to its impaired traffick-ing in hepatocytes. The mean value of NCC is 10 timeshigher in Wilson’s disease than in AD patients. About40% of Wilson’s disease subjects present neurologicalsymptoms (dysarthria, dyspraxia, ataxia, and Parkinsoniansigns) reversing with zinc or copper chelating agents. It hasbeen recently hypothesized a relationship between serumNCC and specific symptoms in Wilson’s disease and AD(Kitzberger et al., 2005). In Wilson’s disease, NCC over-load may affect copper-containing enzymes such as dopa-mine beta hydroxylase or Cu/Zn superoxide dismutase,thus producing neurodegenerative processes and dopami-nergic motor deficits. In AD, neurodegenerative processeswould be associated with abnormal amyloid precursor pro-tein, which has a copper-binding domain that might con-tribute as a metallotransporter to neuronal copperhomeostasis (Bush, 2003; Squitti et al., 2006). In Wilson’sdisease, the toxic effects of the NCC serum fraction aremutation dose-depending: a gradient mutation that causesa gradient copper dysfunction was found in liver, as exten-sively studied in heterozygous carriers of the ATP7B muta-tions (Sternlieb and Scheinberg, 1968; Mareck andNevsimalova, 1984). These data suggest a relationshipbetween different features of copper abnormalities and dif-ferent effects on central nervous system and sensorimotor/cognitive functions.
Abnormalities in copper metabolism can affect EEGrhythms (Mareck and Nevsimalova, 1984; White et al.,1993; Chu et al., 1991). Wilson’s disease subjects showeda reduction of alpha and an increase of theta and delta(Mareck and Nevsimalova, 1984; Chu et al., 1991). Thosewith neurological symptoms were characterized by increaseof delta magnitude, decrease of alpha magnitude, andaltered EEG topography (Dierks et al., 1999).
In the present study, a first (control) hypothesis was thatEEG sources have amplitude sensitive to the cognitive sta-tus of Hold, MCI, and AD subjects. A second (experimen-tal) hypothesis stated a correlation among EEG sources
1246 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
and NCC in the continuum across Hold, MCI, and ADsubjects. These sources were estimated by low-resolutionbrain electromagnetic tomography (LORETA; Pascual-Marqui and Michel, 1994; Pascual-Marqui et al., 1999;Pascual-Marqui et al., 2002), which belongs to a large fam-ily of tomographic procedures based on EEG linear inverseestimation (Valdes et al., 1998; Pascual-Marqui et al., 2002;Sekihara et al., 2005; Fuchs et al., 2001; Gross et al., 2003).In precedence, LORETA has been successfully used for thestudy of physiological and pathological brain aging(Anderer et al., 1998a,b, 2003; Dierks et al., 2000; Huanget al., 2002; Saletu et al., 2002; Goforth et al., 2004; Babi-loni et al., 2004a, 2006a,b,c,d,e,f).
2. Methods
2.1. Subjects and diagnostic criteria
For the present multi-centric study, we used data from54 AD patients, 19 MCI, subjects and 17 Hold subjects.They were not consecutive cases, since we had to balanceas much as possible age, education, and gender. Further-more, we could include only MCI and AD subjects witha certain degree of general cognitive status (see in the fol-lowing). Part of the individual data sets was used for previ-ous or parallel aging studies on either copper (Squitti et al.,2005, 2006) or EEG rhythms (Babiloni et al., 2004a,2006a,b). Local Institutional Ethics Committees approvedthe present study. All experiments were performed withthe informed and overt consent of each participant or care-giver in line with the Declaration of Helsinki.
Probable AD was diagnosed according to NINCDS-ADRDA (McKhann et al., 1984) and DSM IV criteria.The recruited AD patients underwent general medical, neu-rological and psychiatric assessments. Patients were alsorated with a number of standardized diagnostic and sever-ity instruments that included MMSE (Folstein et al., 1975),Clinical Dementia Rating Scale (CDR, Hughes et al.,1982), Geriatric Depression Scale (GDS, Yesavage et al.,1983), Hachinski Ischemic Scale (HIS, Rosen et al.,1980), and Instrumental Activities of Daily Living scale(IADL, Lawton and Brodie, 1969). Neuroimaging diagnos-tic procedures (CT or MRI) and complete laboratory anal-yses were carried out to exclude other causes of progressiveor reversible dementias, in order to have a homogeneousmild AD patient sample. Exclusion criteria were: (i) fronto-temporal dementia diagnosed according to criteria of Lundand Manchester Groups (1994), (ii) vascular dementia asdiagnosed according to NINDS-AIREN criteria (Romanet al., 1993), (iii) extra-pyramidal syndromes, (iv) reversibledementias (including pseudodementia of depression); and(v) Lewy body dementia according to the criteria by McKe-ith et al. (1999). The detection of vascular component indementia and MCI was based upon previous theoreticalguidelines from our network (Frisoni et al., 1995; Galluzziet al., 2005). Of note, benzodiazepines, antidepressant and/or antihypertensive were suspended for about 24 h before
EEG recordings. This did not insure a complete washoutof the drug, but made it comparable the drug conditionacross the patients. Washout of the drugs without discon-tinuation effects would have required a too long suspensionof the drugs.
The present inclusion and exclusion criteria for MCIaimed at selecting elderly persons with objective cognitivedeficits, especially in the memory domain, who did notmeet criteria for a diagnosis of dementia or AD (Rubinet al., 1989; Albert et al., 1991; Flicker et al., 1991; Zaudig,1992; Devanand et al., 1997; Petersen et al., 1995, 1997,2001). The inclusion criteria were as follows: (i) objectivememory impairment on neuropsychological evaluation, asdefined by performances P1.5 standard deviation belowthe mean value of age and education-matched controlsfor a test battery including Busckhe–Fuld and MemoryRey tests; (ii) normal activities of daily living as docu-mented by the history and evidence of independent living;and (iii) clinical dementia rating score of 0.5. Exclusion cri-teria for MCI were: (i) mild AD, as diagnosed by the pro-cedures described above; (ii) evidence of concomitantdementia such as frontotemporal, vascular dementia,reversible dementias (including pseudo-depressive demen-tia), fluctuations in cognitive performance, and/or featuresof mixed dementias; (iii) evidence of concomitant extra-pyramidal symptoms; (iv) clinical and indirect evidence ofdepression as revealed by GDS scores lower than 14; (v)other psychiatric diseases, epilepsy, drug addiction, alcoholdependence, and use of psychoactive drugs including ace-tylcholinesterase inhibitors or other drugs enhancing braincognitive functions; and (vi) current or previous systemicdiseases (including diabetes mellitus) or traumatic braininjuries.
Hold subjects were recruited mainly among patients’spouses. All Hold subjects underwent physical and neuro-logical examinations as well as cognitive screening (includ-ing MMSE). Subjects affected by chronic systemic illnesses(i.e. diabetes mellitus or organ failure) were excluded. Sub-jects with a history of present or previous neurological orpsychiatric disease were also excluded. All Hold subjectshad a GDS score lower than 14. Conditions known toaffect copper metabolism and biological variables of oxida-tive stress (e.g. diabetes mellitus, inflammatory diseases,Hodgkin’s disease, recent history of heart or respiratoryfailure, chronic liver or renal failure, malignant tumors,alcohol abuse), on the basis of past medical history andscreening laboratory tests, prompted further subject’sexclusion.
For a preliminary validation of the EEG source analy-sis, the AD patients were subdivided in two sub-groupsbased on a cut-off of 20 at MMSE score: AD� (27 subjects,MMSE P 20) and AD+ (27 subjects, MMSE < 20). Thatcriterion allowed the formation of two sub-groups of ADpatients with similar levels of age and education. The con-trol hypothesis was that EEG sources differed in line withthe cognitive status across Hold, MCI, AD� and AD+.Table 1 summarizes the relevant demographic and clinical
Table 1Demographic and neuropsychological data of interest of healthy elderly (Hold = Nold in the table according to the nomenclature of previous field papersof this Consortium), mild cognitive impairment (MCI), and mild Alzheimer’s disease (AD) subjects
Nold MCI AD� AD+
N 17 19 27 27Age (years) 70.4 (±2.2SE) 72.8 (±1.3SE) 73.6 (±1.7SE) 74.7 (±1.8SE)Gender (F/M) 10/7 9/10 24/3 19/8MMSE 27.7 (±0.4SE) 25.1 (±0.4SE) 22.6 (±0.3SE) 16.3 (±0.5SE)Education (years) 8.8 (±1SE) 9.2 (±1.2SE) 8.6 (±0.9SE) 8.2 (±0.9SE)
Of note, AD subjects were subdivided in two sub-groups: AD� (mini mental state evaluation, MMSE P 20) and AD+ (MMSE < 20).
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1247
data of the recruited Hold, MCI, AD� and AD+ subjects.As expected, women were overrepresented in the ADgroups. Three ANOVAs using the factor Group (Hold,MCI, AD�, AD+) were computed to evaluate the presenceor absence of statistically significant differences among theHold, MCI, AD�, AD+ groups for age, education, andgender. Statistically significant differences for gender(p < 0.05) were found, but not for education (p > 0.9) andage (p > 0.5). Age, education and gender were used ascovariates in the statistical evaluation of cortical sourcesof EEG rhythms, to remove possible confounding effects.
2.2. Copper and ceruloplasmin investigations
Serum from fasting blood samples was collected in themorning and rapidly stored at �80 �C. Serum copper con-centration was measured following the method of Abeet al. (Randox Laboratories, Crumlin, UK, 1989) (Squittiet al., 2002, 2005). Ceruloplasmin was measured by immu-noturbidimetric assays (Roche, Diagnostic, Germany) uti-lizing a rabbit anti-human ceruloplasmin antibody inphosphate buffer (Mancini et al., 1965).
We calculated the portion of copper bound to cerulo-plasmin (CB) as follows (Walshe, 2003): CB = n * cerulo-plasmin mg/L; n = 0.0472 (lmol/mg). By subtractingcopper bound to ceruloplasmin (CB) from the total serumcopper, NCC value was estimated (Stremmel et al., 1991;Walshe, 2003). For each serum copper and ceruloplasminpair, the copper bound to ceruloplasmin and NCC werecalculated. Statistical analysis of CB or NCC was per-formed by ANOVA (p < 0.05) including the factor Group(Hold, MCI, AD�, AD+). Age, education, and genderwere used as covariates.
2.3. EEG recordings
EEG data were recorded in resting, awake subjects(eyes-closed) by specialized clinical units. EEG recordingswere performed (0.3–70 Hz bandpass; 256 Hz frequencysampling; EB-Neuro and Micromed EEG machines) from19 electrodes positioned according to the International10–20 System (i.e. Fp1, Fp2, F7, F3, Fz, F4, F8, T3, C3,Cz, C4, T4, T5, P3, Pz, P4, T6, O1, O2). A specific kindof reference electrode was not imposed on all recordingunits of this multi-centric study, given that preliminarydata analysis and LORETA source analysis were carried
out after that EEG data were re-referenced to commonaverage reference (i.e. all electrodes were included in theaverage reference).
To monitor eye movements, electrooculogram (0.3–70 Hz bandpass) was also collected. All data were digi-tized in continuous recording mode (5 min of EEG;256 Hz sampling rate). In all subjects, EEG recordingswere performed at late morning. During all EEG record-ings, to keep state of vigilance at constant level, an oper-ator controlled on-line the EEG traces and verballyalerted the subject any time there were signs of behav-ioral drowsiness.
Of note, EEG recordings lasting 5 min allowed the com-parison of the present results with those of several previousAD studies using either recording EEG periods no longerthan 5 min (Buchan et al., 1997; Muller et al., 1997; Pucciet al., 1999; Szelies et al., 1999; Rodriguez et al., 2002;Babiloni et al., 2004a, 2006a,b,c,d,e,f) or EEG periodsshorter than 1 min (Dierks et al., 1993, 2000). Longer rest-ing EEG recordings in AD patients would have reduced thevariability of the data but would have increased the possi-bility of slowing of EEG oscillations due to reduced vigi-lance and arousal.
EEG data were analyzed and fragmented off-line inconsecutive epochs of 2 s. On average, 150 epochs(5 min) for each subject were examined. EEG epochswith ocular, muscular and other types of artefacts werepreliminarily identified by a computerized automatic pro-cedure. The EEG epochs including ocular artefact (lessthan 15% of the total ones) were then corrected by astandard autoregressive method whose performanceswere validated in a previous study (Moretti et al.,2003). In brief, this method subtracted the projectionof EOG artefact on EEG data based on estimatedweights by autoregressive method (Moretti et al., 2003).Two independent experimenters manually confirmed theEEG segments accepted for further analysis. Of note,special attention was devoted to avoid the inclusion ofEEG segments and individual data sets with EEG signsof drowsiness or pre-sleep stages. Furthermore, theexperimenters were blind to the diagnosis of the subjectsat the moment of the preliminary EEG data analysis. Atthe end of the preliminary analysis of EEG data, themean of the individual artefact-free EEG epochs was115 (±10 SE). This is a sufficient number of 2s-EEGepochs for further LORETA analysis.
Table 2Brodmann areas included in the cortical regions of interest (ROIs) of thepresent study
LORETA BROADMANN areas into the regions of interest (ROIs)
Frontal 8, 9, 10, 11, 44, 45, 46, 47Central 1, 2, 3, 4, 6Parietal 5, 7, 30, 39, 40, 43Temporal 20, 21, 22, 37, 38, 41, 42Occipital 17, 18, 19
LORETA solutions were collapsed in frontal, central, parietal, occipital,and temporal ROIs.
1248 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
2.4. Spectral analysis of the EEG data
A digital FFT-based power spectrum analysis (Welchtechnique, Hanning windowing function, no phase shift)computed power density of EEG rhythms with 0.5 Hz fre-quency resolution. The following standard band frequen-cies were studied: delta (2–4 Hz), theta (4–8 Hz), alpha 1(8–10.5 Hz), alpha 2 (10.5–13 Hz), beta 1 (13–20 Hz), beta2 (20–30 Hz) and gamma (30–40 Hz). These band frequen-cies were chosen averaging those used in previous relevantEEG studies on dementia (Leuchter et al., 1993; Jelic et al.,1996; Besthorn et al., 1997; Chiaramonti et al., 1997;Rodriguez et al., 1999a,b) and have been successfully usedin recent studies on AD of this Consortium (Babiloni et al.,2004a, 2006a,b,c,d,e,f). Sharing of a frequency bin by twocontiguous bands was allowed to be consistent with a bulkof EEG literature on dementia (Cook and Leuchter, 1996;Jelic et al., 1996; Besthorn et al., 1997; Nobili et al., 1998;Pucci et al., 1997; Kolev et al., 2002; Holschneider et al.,1999). Furthermore, it followed Klimesch and others’ the-oretical consideration that near EEG rhythms may overlapat their frequency borders (Klimesch, 1996, 1999; Klimeschet al., 1997, 1998; Babiloni et al., 2004b,c,d,e,f, 2005).
We could not use narrow frequency bands for beta 1(13–20 Hz), beta 2 (20–30 Hz) and gamma (30–40 Hz)because of the variability of beta and gamma peaks inthe power spectra. Therefore, LORETA results for the betabands could suffer from sensitivity limitations of EEGspectral analyses for large bands (Szava et al., 1994).
2.5. Cortical source analysis of the EEG rhythms byLORETA
LORETA computed 3-D linear solutions (LORETAsolutions) for EEG inverse problem within a three-shellspherical head model including scalp, skull, and brain com-partments (http://www.unizh.ch/keyinst/NewLORETA/LORETA01.htm) (Pascual-Marqui and Michel, 1994;Pascual-Marqui et al., 1999; Pascual-Marqui et al., 2002).Brain compartment was restricted to the cortical gray mat-ter/hippocampus of a head model co-registered to Talai-rach probability brain atlas and digitized at the BrainImaging Center of the Montreal Neurologic Institute(Talairach and Tournoux, 1988). This compartmentincluded 2394 voxels (7 mm resolution), each voxel con-taining an equivalent current dipole.
LORETA solutions consisted of voxel current densityvalues able to predict EEG spectral power density at scalpelectrodes. These solutions are reference free, in that oneobtains the same LORETA source distribution for EEGdata referenced to any reference electrode including com-mon average. To enhance the topographical results, datanormalization was obtained by normalizing the LORETAcurrent density at each voxel with the LORETA powerdensity averaged across all frequencies (0.5–45 Hz) andacross all 2394 voxels of the brain volume. After the nor-malization, the LORETA solutions lost the original physi-
cal dimension and were represented by an arbitrary unitscale. This procedure reduced inter-subject variability andwas used in previous EEG studies of our Consortium(Babiloni et al., 2004a, 2006a,b,c,d,e,f). The general proce-dure fitted the LORETA solutions in a Gaussian distribu-tion and reduced inter-subject variability (Nuwer, 1988;Leuchter et al., 1993).
Solutions of the EEG inverse problem are underdeter-mined and ill conditioned when the number of spatial sam-ples (electrodes) is lower than that of the unknown samples(current density at each voxel). To account for that, thecortical LORETA solutions predicting scalp EEG spectralpower density were regularized to estimate distributedrather than punctual EEG source patterns (Pascual-Mar-qui and Michel, 1994; Pascual-Marqui et al., 1999; Pasc-ual-Marqui et al., 2002). Based on this regularizationprocedure, LORETA provides a unique deterministicsource solution to the EEG inverse problem. Of course,this does not mean that such solutions are perfect modelsof EEG sources, since the intrinsic limitations in the spatialresolution of deep EEG sources common to all proceduresof the field cannot be entirely overcome (Pascual-Marquiand Michel, 1994; Pascual-Marqui et al., 1999; Pascual-Marqui et al., 2002). Furthermore, we used the standardLORETA package, which estimates EEG cortical sourceswithin a sphere that just approximates head volume con-ductor (Ding et al., 2005). This package associates eachLORETA solution with a Brodmann area. In line withthe low spatial resolution of the LORETA technique, weused our MATLAB software to collapse the voxels ofLORETA solutions at frontal, central, parietal, occipital,and temporal regions of the brain model coded into Talai-rach space. The Brodmann areas listed in Table 2 formedeach of these regions of interest (ROIs). The ‘‘low-resolu-tion’’ features of regional LORETA solutions could reli-ably take into account the slight change in the corticalvolume (resolution in millimetres) present in the mildstages of AD. Of note, the LORETA procedure has beensuccessfully used in our previous studies on aging (Babiloniet al., 2004a, 2006a,b,c,d,e,f). Finally, the main advantageof the regional analysis of LORETA solutions was thatour modeling could disentangle rhythms of contiguous cor-tical areas. For example, the rhythms of the occipitalsource were disentangled with respect to those of the con-tiguous parietal and temporal sources thanks to the abilityof LORETA to solve the linear inverse problem by taking
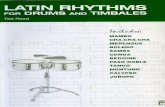
Fig. 1. Means (±standard error, SE) of portions of copper bound (CB)and non-bound (NCC) to ceruloplasmin in Hold, MCI, AD�, and AD+subjects. Hold = Nold in the figure according to the nomenclature ofprevious field papers of this Consortium.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1249
into account the well-known effects of the head as a volumeconductor.
2.6. Statistical analysis of the LORETA solutions
For the evaluation of the control hypothesis, regionalnormalized LORETA solutions from Hold, MCI, AD�and AD+ subjects were used as an input for ANOVA. Sub-jects’ age, education, gender and individual alpha fre-quency (IAF) peak served as covariates (IAF is definedas the frequency associated with the strongest EEG powerat the extended alpha range; Klimesch, 1999). Mauchly’stest evaluated the sphericity assumption. Correction ofthe degrees of freedom was made with the Greenhouse–Geisser procedure. The ANOVA used the factors Group(Hold, MCI, AD�, AD+; independent variable), Band(delta, theta, alpha 1, alpha 2, beta 1, beta 2, gamma),and ROI (central, frontal, parietal, occipital, temporal).Duncan test was used for post hoc analysis (p < 0.05).The first hypothesis would be confirmed by the statisticalANOVA effect including the factor Group (p < 0.05).
For the evaluation of the experimental hypothesis, weperformed correlations among regional LORETA solu-tions of EEG sources and normalized NCC values in allsubjects as a single group (the NCC values were normalizedby means of rescaling to 0–1 range). We tested both linearand non-linear correlations, given the complexity of thevariables implied in the neurodegenerative processes inAD. The linear correlation was computed with Pearson’stest (Bonferroni corrected, p < 0.05) using age, gender,and education as covariates (partial correlation). Thenon-linear correlations were computed evaluating the coef-ficient of determination r2 for exponential, logarithmic, andpower functions.
Finally, r2 of the non-linear simple functions was com-pared with r2 of the linear function, to evaluate the preva-lence of linear or non-linear correlations between regionalnormalized LORETA solutions and NCC.
3. Results
3.1. Serum NCC in the present Hold, MCI, and AD groups
Fig. 1 shows the mean (±SE) of portions of CB and NCCin Hold, MCI, AD�, and AD+ subjects. ANOVA showedno statistically significant difference of CB among Hold,MCI, AD�, and AD+ groups (p > 0.05). In contrast,ANOVA revealed statistically significant differences (F =4.857; p = 0037) in NCC among the groups. Post hoc testingshowed that NCC was higher in AD+ than in Hold(p = 0.005), MCI (p = 0.006), and AD� (p = 0.005) subjects.
3.2. Topography of the EEG cortical sources estimated by
LORETA
For illustrative purposes, Fig. 2 maps the grand averageof the LORETA solutions (i.e. relative current density at
cortical voxels) modeling the distributed EEG sources fordelta, theta, alpha 1, alpha 2, beta 1, beta 2 and gammabands in Hold, MCI, AD� and AD+ groups. The Holdgroup presented alpha 1 sources with the maximal valuesof amplitude distributed in parieto-occipital regions. Delta,theta and alpha 2 sources had moderate amplitude valueswhen compared to alpha 1 sources. Finally, beta 1, beta2 and gamma sources were characterized by lowest ampli-tude values. Compared to Hold group, MCI groupsshowed a decrease in amplitude of the parietal, occipitaland temporal alpha 1 sources. With respect to Hold andMCI groups, both AD� and AD+ group showed anamplitude increase of widespread delta and theta sources,along with a strong amplitude reduction of parietal, occip-ital and temporal alpha 1 sources. Finally, the amplitudeincrease of delta and theta sources was stronger in AD+than AD� group. Of note, the topography of theta sourcesin AD+ was similar to the topography of alpha 1 sources inHold group, but the amplitude of theta sources in AD+
Fig. 2. Grand average of LORETA solutions (i.e. normalized relative current density at the cortical voxels) modeling the distributed EEG sources fordelta, theta, alpha 1, alpha 2, beta 1, beta 2, and gamma bands in Hold, MCI, AD� (MMSE P 20), and AD+ (MMSE < 20) groups. The left side of themaps (top view) corresponds to the left hemisphere. Legend: LORETA, low resolution brain electromagnetic tomography. Color scale: all power estimateswere scaled based on the averaged maximum value (i.e. alpha 1 power value of occipital region in Hold). The maximal value of power is reported undereach column. Hold = Nold in the figure according to the nomenclature of previous field papers of this Consortium.
1250 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
was lower than the amplitude of alpha 1 sources in Holdgroup.
3.3. Statistical analysis of the EEG cortical sources
estimated by LORETA
Kolmogorov–Smirnov test was used to evaluate theGaussian distribution of the regional normalized LORETAsolutions in Hold, MCI, AD� and AD+ subjects. Theresults showed that almost all normalized regional LORE-TA solutions presented a Gaussian distribution of theresiduals in the four groups (p > 0.1). The violations ofthe Gaussianity were observed for the LORETA solutionsrelative to parietal alpha 2 (in AD+ subjects), central beta1 (MCI subjects) and frontal gamma (in AD+ subjects)(p < 0.05), i.e. only 3 variables out of 30. Although
ANOVA is quite robust to the violation of Gaussianity,these LORETA solutions were not considered for posthoc testing. We did not apply a second transformation ofthe data to correct that violation of Gaussianity (as men-tioned above, the LORETA solutions had been alreadynormalized).
According to the control hypothesis, Fig. 3 shows meanregional normalized LORETA solutions (distributed EEGsources) relative to a statistical ANOVA interaction(F = 1.479; p < 0.0061) among the factors Group (Hold,MCI, AD�, AD+), Band (delta, theta, alpha 1, alpha 2,beta 1, beta 2, gamma), and ROI (central, frontal, parietal,occipital, temporal). In the figure, LORETA solutions hadthe shape of EEG relative power spectra. Notably, profileand magnitude of these spectra in Hold, MCI, and mildAD groups differed in the diverse cortical regions, thus
Fig. 3. Regional normalized LORETA solutions (mean across subjects) relative to a statistical ANOVA interaction among the factors Group (Hold, MCI,AD�, AD+), Band (delta, theta, alpha 1, alpha 2, beta 1, beta 2, gamma), and ROI (frontal, central, parietal, occipital, temporal). This ANOVA designused the normalized relative current density values at regional level as a dependent variable. Subjects’ age, education and individual alpha frequency peak(IAF) were used as covariates. Regional LORETA solutions modeled the EEG relative power spectra as revealed by a sort of ‘‘virtual’’ intracranial macro-electrodes ‘‘localized’’ on the macrocortical regions of interest. Hold = Nold in the figure according to the nomenclature of previous field papers of thisConsortium.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1251
supporting the idea that scalp EEG rhythms are generatedby a distributed pattern of cortical sources. Fig. 2 showsthat main regional EEG sources having amplitude sensitiveto the cognitive status of Hold, MCI, AD�, and AD+ sub-jects were delta, theta, alpha 1, and alpha 2 sources. Table3 reports post hoc results for all bands and groups.
Table 3 reports the 9 statistically significant (p < 0.05)differences across groups. They were observed in frontal,occipital, and temporal delta sources; occipital and tempo-ral theta sources; parietal, occipital, and temporal alpha 1sources; and occipital alpha 2 sources.
Normalized LORETA amplitude values of these 9 EEGsources were correlated with NCC in all subjects as a singlegroup (Pearson test; Bonferroni correction for 9 repetitionsof the test gave the threshold p < 0.0055 to obtain the Bon-ferroni corrected p < 0.05). Age, education, and genderserved as covariates (i.e. partial correlation). Fig. 4 showsscatterplots between individual LORETA solutions andNCC of the statistically significant correlations(p < 0.0055). According to the experimental hypothesis,the NCC positively correlated with temporal (r = 0.31,p = 0.003) and frontal (r = �0.33, p = 0.002) delta sources.Table 4 reports coefficient of determination r2 betweenindividual regional LORETA solutions and NCC in allsubjects considered as a single group. In general, r2 values
for linear, exponential, logarithmic, and power functionswere quite similar.
The above correlations individual regional LORETAsolutions and NCC were computed also at the level of sin-gle groups considered separately (Pearson test; Bonferronicorrection for 9 repetitions of the test gave the thresholdp < 0.0055 to obtain the Bonferroni corrected p < 0.05).The results showed no statistically significant correlations(p > 0.05). The lack of correlation results was possiblydue to the drastic reduction of degrees of freedom and ofthe variation range of NCC within each group.
3.4. Control analyses
A control analysis was performed to verify that theamplitude of LORETA sources was not correlated withthe copper bound to ceruloplasmin (CB). NormalizedLORETA amplitude values of delta, theta and alpha 1sources in parietal, temporal and occipital areas werecorrelated with CB in all subjects as a single group(Pearson test; Bonferroni correction for 9 repetitions ofthe test gave the threshold p < 0.0055 to obtain the Bon-ferroni corrected p < 0.05). The CB correlated with noneof these 9 LORETA sources (higher correlation valuewas p = 0.13).
Table 3Post hoc results for the delta, theta, alpha 1, alpha 2, beta 1, beta 2, gamma sources
Duncan post hoc testing (p value)
Central Frontal Parietal Occipital Temporal
Delta
Nold vs MCI p = 0.8, + p = 0.5, � p = 0.8, + p = 0.9, + p = 0.7, �Nold vs AD� p = 0.7, � p = 0.2, � p = 0.4, � p = 0.02, � p = 0.1, �Nold vs AD+ p = 0.5, � p = 0.03, � p = 0.4, � p = 0.003, � p = 0.03, �MCI vs AD� p = 0.5, � p = 0.5, � p = 0.1, � p = 0.02, � p = 0.2, �MCI vs AD+ p = 0.4, � p = 0.1, � p = 0.1, � p = 0.001, � p = 0.05, �AD� vs AD+ p = 0.7, � p = 0.4, � p = 0.9, + p = 0.4, � p = 0.9, �
Theta
Nold vs MCI p = 0.6, + p = 0.8, + p = 0.2, + p = 0.3, + p = 0.6, +Nold vs AD� p = 0.6, + p = 0.9, � p = 0.4, + p = 0.7, � p = 0.6, �Nold vs AD+ p = 0.6, � p = 0.3, � p = 0.5, � p = 0.03, � p = 0.07, �MCI vs AD� p = 0.9, + p = 0.7, � p = 0.5, � p = 0.1, � p = 0.3, �MCI vs AD+ p = 0.4, � p = 0.2, � p = 0.07, � p = 0.001, � p = 0.02, �AD� vs AD+ p = 0.3, � p = 0.3, � p = 0.2, � p = 0.9, � p = 0.2, �
Alpha 1
Nold vs MCI p = 0.5, + p = 0.4, + p = 0.0002, + p = 0.08, + p = 0.5, +Nold WS AD� p = 0.2, + p = 0.6, + p = 0.00001, + p = 0.00004, + p = 0.01, +Nold vs AD+ p = 0.5, + p = 0.6, + p = 0.00001, + p = 0.00003, + p = 0.01, +MCI vs AD� p = 0.5, + p = 0.8, � p = 0.003, + p = 0.00003, + p = 0.5, +MCI vs AD+ p = 0.5, + p = 0.8, + p = 0.003, + p = 0.00002, + p = 0.5, +AD� vs AD+ p = 0.8, � p = 0.9, + p = 0.9, � p = 0.9, � p = 0.8, �
Alpha 2
Nold vs MCI p = 0.9, � p = 0.8, + p = 0.5, + p = 0.1, + p = 0.9, +Nold vs AD� p = 0.6, + p = 0.9, � p = 0.07, + p = 0.02, + p = 0.6, +Nold vs AD+ p = 0.7, + p = 0.9, + p = 0.06, + p = 0.008, + p = 0.4, +MCI vs AD� p = 0.6, + p = 0.8, � p = 0.2, + p = 0.2, + p = 0.7, +MCI vs AD+ p = 0.7, + p = 0.9, � p = 0.2, + p = 0.1, + p = 0.5, +AD� vs AD+ p = 0.8, � p = 0.9, + p = 0.9, + p = 0.8, + p = 0.8, +
Beta 1
Nold vs MCI p = 0.9, � p = 0.9, � p = 0.9, + p = 0.6, + p = 0.7, �Nold vs AD p = 0.7, + p = 0.8, � p = 0.5, + p = 0.5, + p = 0.9, �Nold vs AD+ p = 0.6, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, +MCI vs AD� p = 0.6, + p = 0.9, � p = 0.6, + p = 0.8, + p = 0.8, +MCI vs AD+ p = 0.6, + p = 0.7, + p = 0.9, + p = 0.9, + p = 0.9, +AD� vs AD+ p = 0.8, + p = 0.9, + p = 0.9, + p = 0.8, + p = 0.7, +
Beta 2
Nold vs MCI p = 0.9, + p = 0.9, � p = 0.9, � p = 0.9, � p = 0.5, �Nold vs AD� p = 0.8, + p = 0.9, � p = 0.8, + p = 0.9, � p = 0.5, �Nold vs AD+ p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, �MCI vs AD� p = 0.7, + p = 0.9, � p = 0.9, + p = 0.9, � p = 0.9, +MCI vs AD+ p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, +AD� vs AD+ p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, +
Gamma
Nold vs MCI p = 0.9, � p = 0.8, � p = 0.8, � p = 0.8, � p = 0.4, �Nold vs AD� p = 0.9, � p = 0.8, � p = 0.9, � p = 0.5, � p = 0.7, �Nold vs AD+ p = 0.9, + p = 0.9, � p = 0.9, � p = 0.9, � p = 0.9, �MCI vs AD� p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.7, +MCI vs AD+ p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, +AD� vs AD+ p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, + p = 0.9, +
These results refer to mean regional normalized LORETA solutions (distributed EEG sources) relative to a statistical ANOVA interaction (F = 1.479;p < 0.0061) among the factors Group (Hold, MCI, AD�, AD+), Band (delta, theta, alpha 1, alpha 2, beta 1, beta 2, gamma), and ROI (central, frontal,parietal, occipital, temporal). Hold = Nold in the table according to the nomenclature of previous field papers of this Consortium.
1252 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
A second control analysis was performed to verifywhether the amplitude of LORETA sources was correlatedwith the ratio CB/NCC. Normalized LORETA amplitudevalues of delta, theta and alpha 1 sources in parietal, tem-poral and occipital areas were correlated with CB/NCC
ratio in all subjects as a single group (Pearson test; Bonfer-roni correction for 9 repetitions of the test gave the thresh-old p < 0.0055 to obtain the Bonferroni corrected p < 0.05).The CB/NCC ratio correlated with none of these 9LORETA sources (higher correlation value was p = 0.25).
Fig. 4. Scatterplots among the temporal delta and alpha 1 LORETAdensity current and copper unbound to ceruloplasmin (NCC) in Hold,MCI, AD� and AD+ subjects as a single group. The r and p values arereported within the diagrams. The NCC values were normalized by meansof rescaling to 0–1 range. Hold = Nold in the figure according to thenomenclature of previous field papers of this Consortium.
Table 4Correlation (coefficient of determination r2) between individual regional LORMCI and mild AD subjects considered as a single group
Linear
Correlation between LORETA current density and copper unbound to cerulopla
Frontal delta LORETA current density 0.11Occipital delta LORETA current density 0.006Temporal delta LORETA current density 0.1Occipital theta LORETA current density 0.007Temporal theta LORETA current density <0.005Parietal alpha 1 LORETA current density 0.06Occipital alpha 1 LORETA current density 0.01Temporal alpha 1 LORETA current density 0.03Occipital alpha 2 LORETA current density <0.005
The r2 value is reported for linear (Pearson test), exponential, logarithmic, and pwere quite similar, the latter including only simple functions such as logarithmicdiscouraged complex non-linear functions such as polynomial ones. Hold = Nthis Consortium.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1253
One might argue that LORETA source differencesamong the present Hold, MCI-, AD�, and AD+ groupswere due to age, education, and gender. To address thishypothesis, we considered sub-groups of Hold (N = 10),MCI (N = 10), AD� (N = 10) and AD+ (N = 10) subjects,matched for age (from 73.6 to 73.7 years), education (from8.3 to 8.4 years), and ratios of gender (7 female and 3male). The regional normalized LORETA solutions wereused as a dependent variable. When the ANOVA includingthe factors Group (Hold, MCI AD�, AD+; independentanalysis), Band (delta, theta, alpha 1, alpha 2, beta 1, beta2, gamma), and ROI (central, frontal, parietal, occipital,temporal) was considered, a statistically significant interac-tion (F(72, 792) = 2.8; MSe = 0.52; p = 0.0001) was found.The results confirmed those obtained with the largergroups. Therefore, it is unlikely that the LORETA sourcedifferences obtained in the entire subject sample were dueto age, education, and gender.
Choice of fixed EEG bands did not account for IAFpeak. To evaluate the IAF effect, we performed two addi-tional control analyses. The first control analysis showedthat most of the subjects had IAF peaks within alpha 1band (8–10.5 Hz). In particular, mean IAF peak was9.3 Hz (±0.3 standard error, SE) in Hold subjects; 8.8 Hz(±0.3 SE) in MCI subjects; 8.8 Hz (±0.2 SE) in AD� sub-jects; and 8.4 Hz (±0.2 SE) in AD+ subjects. An ANOVAusing the factor Group (Hold, MCI, AD�, AD+) showedno statistically significant differences for IAF (p > 0.15).The second control analysis evaluated mean regional nor-malized LORETA solutions for alpha 1, alpha 2, and alpha3 sub-bands as computed according to IAF. Resultsshowed a statistical ANOVA interaction (F = 3.534;p = 0.00001) among the factors Group (Hold, MCI,AD�, AD+), Band (alpha 1, alpha 2, alpha 3), and ROI(central, frontal, parietal, occipital, temporal). Age, educa-tion, and gender were used as covariates. Table 5 reportspost hoc results for all bands and groups considered. Themain statistical differences across groups were observed inparietal, occipital, temporal regions for alpha 2 (about
ETA solutions and copper unbound to ceruloplasmin (NCC) in all Hold,
Logarithmic Exponential Power
smin (coefficient of determination r2)
0.1 0.09 0.110.009 0.007 <0.0050.07 0.07 0.070.007 0.009 0.007
<0.005 <0.005 0.0070.07 0.06 0.070.04 0.04 0.020.06 0.05 0.050.01 0.008 <0.005
ower function. In general, r2 values for the linear and non-linear functions, exponential and power ones, since the scatterplot distribution of the dataold in the table according to the nomenclature of previous field papers of
Table 5Post hoc results for the alpha 1, alpha 2, and alpha 3 sources
Duncan post hoc testing (p value)
Central Frontal Parietal Occipital Temporal
Alpha 1
Nold vs MCI p = 0.8, + p = 0.8, + p = 0.6, + p = 0.6, + p = 0.9, +Nold vsAD� p = 0.9, � p = 0.7, � p = 0.3, � p = 0.02, � p = 0.1. -Nold vs AD+ p = 0.6, � p = 0.4, � p = 0.2, � p = 0.002, � p = 0.06, �MCI vs AD� p = 0.7, � p = 0.6, � p = 0.2, � p = 0.003, � p = 0.2, �MCI vs AD+ p = 0.2, � p = 0.3, � p = 0.06, � p = 0.001, � p = 0.06, �AD� vs AD+ p = 0.6, � p = 0.6, � p = 0.6, � p = 0.4, � p = 0.6, �
Alpha 2
Nold vs MCI p = 0.3, + p = 0.4, + p = 0.00001, + p = 0.00001, + p = 0.02, +Nold vs AD� p = 0.2, + p = 0.6, + p = 0.00001, + p = 0.00001, + p = 0.01, +Nold vs AD+ p = 0.2, + p = 0.6, + p = 0.00001, + p = 0.00001, + p = 0.05, +MCI vs AD� p = 0.8, + p = 0.7, � p = 0.4, + p = 0.2, + p = 0.8, +MCI vs AD+ p = 0.9, + p = 0.7, � p = 0.6, + p = 0.6, + p = 0.7, +AD� vs AD+ p = 0.9, � p = 0.9, + p = 0.7, � p = 0.3, � p = 0.6, +
Alpha 3
Nold vs MCI p = 0.5. + p = 0.6, + p = 0.00001, + p = 0.002, + p = 0.1, +Nold vsAD� p = 0.2, + p = 0.6, + p = 0.00001 p = 0.00001 p = 0.001, +Nold vsAD+ p = 0.3, + p = 0.8, + p = 0.00001, + p = 0.00001, + p = 0.02, +MCI vsAD� p = 0.3, + p = 0.9, � p = 0.004, + p = 0.00001, + p = 0.1, +MCI vs AD+ p = 0.6, + p = 0.5, � p = 0.01, + p = 0.00001, + p = 0.3, +AD� vs AD+ p = 0.7, � p = 0.9, + p = 0.7, � p = 0.3, � p = 0.5, �
These results refer to mean regional normalized LORETA solutions (distributed EEG sources) relative to a statistical ANOVA interaction (F = 3.53;p < 0.0001) among the factors Group (Hold, MCI, AD�, AD+), Band (alpha 1, alpha 2, alpha 3), and ROI (central, frontal, parietal, occipital, temporal).Hold = Nold in the table according to the nomenclature of previous field papers of this Consortium.
1254 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
7–9 Hz, on average) and alpha 3 (about 9–11 Hz, on aver-age) sources (p < 0.02–0.00001).
4. Discussion
4.1. Validating the procedures for subjects’ selection and
NCC-EEG data analysis
According to previous studies (Squitti et al., 2006;Squitti et al., in preparation), we showed that NCC washigher in AD patients with high plasma level of NCC(AD+) than in MCI and Hold subjects, but there was nostatistically significant (p > 0.05) NCC difference betweenAD patients with low plasma level of NCC (AD�) andMCI or Hold subjects. This result indicates that the plasmaconcentration of NCC does not linearly increase acrossHold, MCI, AD�, and AD+, suggesting that the possiblerelationships among NCC and cerebral degeneration arenot simple or linear due to the complexity of the interac-tions among the underlying biological parameters.
Furthermore, EEG rhythms in MCI and AD subjectswere characterized by a marked magnitude decrease ofthe alpha sources in parietal, occipital, and temporal areaswith reference to Hold subjects. Maximum differences wereobserved at both individual low- (about 7–9 Hz) and high-(about 9–11 Hz) alpha frequencies (note that here the useof fixed EEG bands prevented a fine distinction betweenindividual low vs. high frequencies of alpha and relatedconsiderations on attentional vs. memory functions; Klim-esch, 1999). Furthermore, the magnitude of the delta and
theta EEG sources increased in AD subjects compared toHold and MCI subjects. Of note, the present results werenot due to different IAF among these groups, IAF beingthe landmark of the EEG spectrum that is crucial to disen-tangle individual alpha from theta band (Klimesch, 1999).Indeed, most of the Hold (84%), MCI (89%), and AD(83%) subjects had IAF peaks within alpha 1 band(8–10.5 Hz). Furthermore, the IAF was used as a covariatein the statistical analyses to remove the effects of slightlydifferent IAF of the groups from the statistical values ofthe EEG differences.
The results of the present control analysis are globally inline with previous evidence showing: (i) an enhancement ofthe delta rhythms in AD compared to Hold subjects (Pric-hep et al., 1994; Wolf et al., 2003; Babiloni et al., 2004a,2006a, 2005, 2006c,d), (ii) a magnitude decrease of thealpha rhythms in AD and/or MCI compared to Hold sub-jects (Dierks et al., 1993, 2000; Rodriguez et al., 1999a,b;Moretti et al., 2004; Babiloni et al., 2004a, 2006a, 2005,2006c,d), (iii) an increase of theta power in mild AD com-pared to Hold subjects (Coben et al., 1983; Huang et al.,2000; Mattia et al., 2003; Ponomareva et al., 2003). In addi-tion, a recent study in Hold subjects has shown enhance-ment of theta rhythms and decline of cognitiveperformance after the administration of a cholinergicantagonist (Osipova et al., 2003). In this vein, thetarhythms decrease in AD subjects after cholinergic therapy(Adler et al., 2001, 2004; Brassen and Adler, 2003). How-ever, it should be remarked that the physiological mecha-nisms at the basis of cortical theta rhythms are still
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1255
controversial (Klimesch, 1999), and abnormal EEGrhythms can be observed not only in people with patholog-ical aging but also in other kinds of neurologic disordersnot clearly related to an impairment of the cholinergic sys-tems (Priori et al., 2004). Therefore, the specific relation-ships between cortical EEG rhythms (including thetarhythms) and AD should be further explored in futurestudies evaluating several kinds of neurological disordersincluding vascular and frontotemporal dementias.
As an exception, our procedure could not disclose EEGchanges at beta frequencies in AD vs. Hold subjects (Clauset al., 1998, 2000). This may be due to the use of quite largefrequency bands for beta 1 (13–20 Hz) and beta 2 (20–30 Hz), together with the average of LORETA solutionsacross large cortical regions. Of note, the procedure servedto reduce the mismatch between the limited number ofEEG channels (i.e. 19) and the high number of LORETAvoxels (i.e. 2394).
4.2. Serum NCC and temporal–frontal delta EEG sources
correlated in Hold, MCI, and AD subjects
A positive linear correlation was observed betweenserum NCC and temporal–frontal delta sources in Hold,MCI and AD subjects considered as a single group. Thiswas not merely determined by age, education, and gender.The two delta sources also showed a non-linear positivecorrelation with NCC, supporting the observation thatneurodegenerative processes in AD and MCI cannot besimply described in terms of linear relationships withEEG rhythms. Differently, CB correlated with no EEGsource. These results are consistent with the finding thatNCC but not CB crosses the blood–brain barrier and hasa toxic action on AD brain (Hoogenraad, 2001, in press;Twomey et al., 2005; Squitti et al., 2006). Furthermore,they extend previous evidence showing that NCC discrim-inated AD patients from healthy controls and vasculardementia patients (Squitti et al., 2005) and can affect con-centration of cerebrospinal fluid b-amyloid in AD patients(Squitti et al., 2006). Although the present study is sup-ported by the mentioned literature on the role of copperin AD, the present results motivate further investigationsto address: (i) the relationship between NCC and EEGrhythms in Wilson’s disease patients and (ii) the effects ofthe manipulation of NCC on cholinergic basal forebrainand EEG in animals. These investigations may provide cru-cial data to support the specificity and causal role of NCCon the generation of abnormal EEG rhythms in AD.
The present results give rise to some questions. Are theresults affected by cholinergic drugs? To this regard, itshould be remarked that inhibitors of acetylcholinesterasewere administered only to AD patients (drug dose practi-cally equal in all). Therefore, it is unlikely that the cholin-ergic therapy per se could induce a marked linearcorrelation between NCC and EEG rhythms across Hold,MCI, and AD subjects. Rather, it can be speculated thatthe NCC reflects cerebral atrophy due to neurodegenera-
tive processes, in line with the hypothesis linking neurode-generative processes, cerebral atrophy, and changes ofEEG rhythms in MCI and AD subjects. Specifically, a pre-vious reference study has shown a statistical correlationamong increase of serum copper, medial temporal lobeatrophy, and poor neuropsychological performance(Squitti et al., 2002). However, the available data sets madeit possible just the evaluation of the correlative nature ofthe relationship. Causality of the relationship would haverequired serial measurements of NCC and EEG acrosstime together with a regression analysis. The present resultsstrongly motivate future investigations to address thehypothesis of a causal effect of NCC on EEG rhythms.
Remarkably, benzodiazepines, antidepressant and/orantihypertensive were suspended for about 24 h beforeEEG recordings. This did not insure a complete washoutof the drug, but made it comparable the drug conditionacross the patients. In this regard, several relevant papershave shown the effects of benzodiazepines, antidepressantand antihypertensive on EEG rhythms (Herrmann andKubicki, 1981; Yamadera et al., 1987; Breimer et al.,1990; Pechadre et al., 1993; Feshchenko et al., 1997; Pick-worth et al., 1997; Patat et al., 1999; Hotz et al., 2000;Knott et al., 2002). In particular, it has been reported that:(i) the treatment with benzodiazepines was associated withan increase of beta rhythms and a decrease of alpharhythms (Breimer et al., 1990; Pechadre et al., 1993; Fes-hchenko et al., 1997; Hotz et al., 2000); (ii) the administra-tion of antidepressant was related to an increase of delta,theta, and beta rhythms together with a decrease of alpharhythms (Herrmann and Kubicki, 1981; Yamadera et al.,1987; Knott et al., 2002); (iii) the administration of antihy-pertensive was associated with a decrease of alpha rhythmsand an increase of delta rhythms (Pickworth et al., 1997;Patat et al., 1999). Unlikely, the relatively low size of theAD sub-groups did not allow a reliable analysis of the rela-tionships between EEG rhythms and NCC in subjectstotally free from pharmacological treatment. This is clearlyan important issue for future investigations.
Why does NCC correlate with the mechanism generat-ing abnormal delta rhythms? A brief overview of the mech-anisms of delta generation can frame the issue. Duringslow-wave sleep, corticofugal slow oscillations (<1 Hz)are effective in grouping thalamic-generated delta rhythms(1–4 Hz) and spindling activity (7–14 Hz) rhythms (Steri-ade, 2003). Brain arousal provoked an immediate blockof sleep EEG figures including spindles, high and lowcomponents of the delta rhythms, due to inhibition of ret-iculo-thalamic (7–14 Hz), thalamo-cortical (1–4 Hz), andintracortical (<1 Hz) oscillators. This is induced by fore-brain (nucleus basalis) cholinergic inputs to hippocampusand cortex as well as by thalamocortical projections(Schaul et al., 1978; Steriade et al., 1996; Steriade, 2003,2004). Abnormal delta rhythms are also present in wakeconditions only following brain lesions (i.e. focal deltaabnormalities due to circumscribed lesions of connectionwhite-matter-‘‘disconnection’’ delta-, whereas diffuse delta
1256 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
increases by thalamic and brainstem lesions, Gloor et al.,1977).
Keeping in mind the above theoretical framework, thepresent correlations between NCC and delta sources mightdepend on the cholinergic basal forebrain deeply affectinggeneration of cerebral delta rhythms. This speculation isalso in accordance with previous studies in animal modelsshowing that the release of acetylcholine in the cortexreduced the amplitude of the delta EEG rhythms butincreased the amplitude of faster rhythms (Kanai andSzerb, 1965; Celesia and Jasper, 1966). The same was truefor the electrical stimulation of the forebrain cholinergicneurons (Mesulam et al., 1983; Semba and Fibiger, 1989;Metherate et al., 1992) and for the administration of cho-linergic agonists (Cuculic et al., 1968; Metherate et al.,1992). Conversely, the intra-cortical application of cholin-ergic (muscarinic) antagonists increased the amplitude ofthe delta and decreased that of faster EEG rhythms, respec-tively (Metherate et al., 1992). The same was true for theexperimental lesions of the basal forebrain (Stewart et al.,1984; Buzsaki et al., 1988; Ray and Jackson, 1991) as wellas for AD where cholinergic basal forebrain is deeplyaffected (Rodriguez et al., 1999a,b; Dierks et al., 1993,2000; Huang et al., 2000; Babiloni et al., 2004a; Morettiet al., 2004 Mesulam, 2004; Mesulam et al., 2004).
Why is NCC specifically correlated with temporal andfrontal delta sources? It can be speculated that NCC canhave an effect on early mesial–temporal degeneration onhippocampus–temporoparietal connectivity in MCI andAD subjects (Killiany et al., 1993). Furthermore, it hasbeen shown that a bilateral reduction of gray matter vol-ume in the hippocampal formation and enthorhinal cortexof the AD subjects was correlated with an increment of theslow EEG rhythms in temporo-parietal cortex (Fernandezet al., 2003). The same was true for a negative correlationbetween frontal white matter volume and frontal deltaEEG rhythms in MCI and AD subjects (Babiloni et al.,2006a). Finally, increase of delta or theta rhythms in ADwas related to progressive cortical hypoperfusion typicallyassociated with neuronal loss (Kwa et al., 1993; Steriade,1994; Passero et al., 1995; Niedermeyer, 1997; Nobiliet al., 1998; Rodriguez et al., 1999a,b). However, the possi-ble relationships among NCC, cerebral degeneration andEEG abnormalities AD subjects should not be conceivedas simple or linear, given the complexity of the biologicalparameters in play.
What is the relationship among NCC, EEG rhythms,and different neurological symptoms in AD and Wilson’sdisease? It can be speculated that neurodegenerative pro-cesses, as reflected by NCC, would mainly involve dopami-nergic system in Wilson’s disease and cholinergic system inAD. Indeed, EEG abnormalities in delta and alpharhythms seem to be more marked in AD than in Wilson’sdisease, in line with the role of these neurotransmitter sys-tems in cerebral arousal. Cerebral arousal is directly andstrongly modulated by cholinergic and serotoninergic sys-tems, whereas it is indirectly affected by dopaminergic sys-
tem (Dringenberg, 2000). Indeed, dopaminergic system cando it just by means of cholinergic system. As a conse-quence, a lesion of dopaminergic system does not preventa certain modulation of cerebral arousal by cholinergic sys-tem. In contrast, a lesion of cholinergic system blocks thearousal effects of dopaminergic system.
4.3. Conclusions
In the present study, we observed positive linear andnon-linear correlations between NCC and temporal-frontaldelta sources in Hold, MCI, and AD subjects. These resultsrepresent the first demonstration that high plasma NCC iscorrelated with cortical delta rhythms across Hold, MCI,and AD subjects, thus unveiling possible relationshipsamong the biological parameter, advanced neurodegenera-tive processes, and synchronization mechanisms regulatingthe relative amplitude of selective EEG rhythms. However,it should be remarked that because of the purely descriptivenature of the present study and the just hypothetical mech-anism(s) through which plasma NCC concentration con-fers a risk to AD, the significance of the present findingswill have to be enlightened by future multi-modal studiesin AD and Wilson’s disease subjects combining the quanti-fication of plasma NCC concentration, brain vascularlesion, neural loss, and EEG rhythms. This will be invalu-able for basic research and clinical applications (e.g.prognosis).
References
Adler G, Brassen S. Short-term rivastigmine treatment reduces EEG slow-wave power in Alzheimer patients. Neuropsychobiology2001;43(4):273–6.
Adler G, Brassen S, Chwalek K, Dieter B, Teufel M. Prediction oftreatment response to rivastigmine in Alzheimer’s dementia. J NeurolNeurosurg Psychiatry 2004;75(2):292–4.
Albert M, Smith LA, Scherr PA, Taylor JO, Evans DA, Funkenstein HH.Use of brief cognitive tests to identify individuals in the communitywith clinically diagnosed Alzheimer’s disease. Int J Neurosci1991;57(3–4):167–78.
Anderer P, Pascual-Marqui RD, Semlitsch HV, Saletu B. Differentialeffects of normal aging on sources of standard N1, target N1 and targetP300 auditory event-related brain potentials revealed by low resolutionelectromagnetic tomography (LORETA). Electroencephalogr ClinNeurophysiol 1998a;108(2):160–74.
Anderer P, Saletu B, Semlitsch HV, Pascual-Marqui RD. Electricalsources of P300 event-related brain potentials revealed by lowresolution electromagnetic tomography. 2. Effects of nootropic therapyin age-associated memory impairment. Neuropsychobiology1998b;37(1):28–35.
Anderer P, Saletu B, Semlitsch HV, Pascual-Marqui RD. Non-invasive localization of P300 sources in normal aging and age-associated memory impairment. Neurobiol Aging2003;24(3):463–79.
Atwood CS, Huang X, Moir RD, Tanzi RE, Bush AI. Role of freeradicals and metal ions in the pathogenesis of Alzheimer’s disease.Metal Ions Biol Syst 1999;36:309–64.
Atwood CS, Moir RD, Huang X, Bacarra NME, Scarpa RC, RomanoDM, et al. Dramatic aggregation of Alzheimer Ab by Cu(II) isinduced by conditions representing physiological acidosis. J Biol Chem1998;273:12817–26.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1257
Atwood CS, Scarpa RC, Huang X, Moir RD, Jones WD, Fairlie DP,et al. Characterization of copper interactions with Alzheimer Abpeptides – identification of an attomolar affinity copper binding site onAb1–42. J Neurochem 2000;75:1219–33.
Babiloni C, Binetti G, Cassetta E, Cerboneschi D, Dal Forno G, DelPercio C, et al. Mapping distributed sources of cortical rhythms inmild Alzheimers disease a multi-centric EEG study. NeuroImage2004a;22(1):57–67.
Babiloni C, Babiloni F, Carducci F, Cincotti F, Del Percio C, Della PennaS, et al. Human alpha rhythms during visual delayed choice reactiontime tasks. A MEG study. Hum Brain Mapp 2004b;24(3):184–92.
Babiloni C, Babiloni F, Carducci F, Cappa S, Cincotti F, Del Percio C,et al. Human cortical rhythms during visual delayed choice reactiontime tasks. A high-resolution EEG study on normal aging. BehavBrain Res 2004c;153(1):261–71.
Babiloni C, Miniussi C, Babiloni F, Carducci F, Cincotti F, Del Percio C,et al. Sub-second ‘‘temporal attention’’ modulates alpha rhythms. Ahigh-resolution EEG study. Cogn Brain Res 2004d;19(3):259–68.
Babiloni C, Babiloni F, Carducci F, Cappa S, Cincotti F, Del Percio C,et al. Human cortical responses during one-bit short-term memory. Ahigh-resolution EEG study on delayed choice reaction time tasks. ClinNeurophysiol 2004e;115(1):161–70.
Babiloni C, Babiloni F, Carducci F, Cappa S, Cincotti F, Del Percio C,et al. Human cortical EEG rhythms during long-term episodicmemory task. A high resolution EEG study of the HERA model.NeuroImage 2004f;21(4):1576–84.
Babiloni C, Cassetta E, Chiovenda P, Del Percio C, Ercolani M, MorettiDV, et al. Frontomedial alpha hyper-reactivity in mild dementedpatients during visual delayed response tasks. A MEG study. BrainRes Bull 2005;65(6):457–70.
Babiloni C, Frisoni G, Steriade M, Bresciani L, Binetti G, Del Percio C,et al. Frontal white matter volume and delta EEG sources negativelycorrelate in awake subjects with mild cognitive impairment andAlzheimer’s disease. Clin Neurophysiol 2006a;117(5):1113–29, Epub2006 Mar 27.
Babiloni C, Binetti G, Cassetta E, Dal Forno G, Del Percio C, Ferreri F,et al. Sources of cortical rhythms change as a function of cognitiveimpairment in pathological aging: a multi-centric study. Clin Neuro-physiol 2006b;117(2):252–68, Epub 2005 Dec 27.
Babiloni C, Benussi L, Binetti G, Cassetta E, Dal Forno G, Del Percio C,et al. Apolipoprotein E and alpha brain rhythms in mild cognitiveimpairment: a multicentric EEG study. Ann Neurol2006c;59(2):323–34.
Babiloni C, Benussi L, Binetti G, Bosco P, Busonero G, Cesaretti S, et al.Genotype (cystatin C) and EEG phenotype in Alzheimer disease andmild cognitive impairment: a multicentric study. Neuroimage2006d;29(3):948–64, Epub 2005 Oct 6.
Babiloni C, Binetti G, Cassarino A, Dal Forno G, Del Percio C, Ferreri F,et al. Sources of cortical rhythms in adults during physiological aging:a multi-centric EEG study. Hum Brain Mapp 2006e;27(2):162–72.
Babiloni C, Cassetta E, Dal Forno G, Del Percio C, Ferreri F, Ferri R,et al. Donepezil effects on sources of cortical rhythms in mildAlzheimer’s disease: responders vs. non-responders. Neuroimage2006, Epub ahead of print.
Bayer TA, Schafer S, Breyhan H, Wirths O, Treiber C, Multhaup G. Avicious circle: role of oxidative stress, intraneuronal Abeta and Cu inAlzheimer’s disease. Clin Neuropathol 2006;25(4):163–71.
Besthorn C, Zerfass R, Geiger-Kabisch C, Sattel H, Daniel S, Schreiter-Gasser U, et al. Discrimination of Alzheimer’s disease and normalaging by EEG data. Electroencephalogr Clin Neurophysiol1997;103(2):241–8.
Brassen S, Adler G. Short-term effects of acetylcholinesterase inhibitortreatment on EEG and memory performance in Alzheimer patients: anopen, controlled trial. Pharmacopsychiatry 2003;36(6):304–8.
Breimer LTM, Hennis PJ, Burm AGL, et al. Quantification of the EEGeffect of midazolam by aperiodic analysis in which are not expected tocause clinically apparent effects volunteers. Clin Pharmacokinet1990;18:245–53.
Buchan RJ, Nagata K, Yokoyama E, Langman P, Yuya H, Hirata Y,et al. Regional correlations between the EEG and oxygen metabolismin dementia of Alzheimer’s type. Electroencephalogr Clin Neurophys-iol 1997;103(3):409–17.
Bush AI. The metallobiology of Alzheimer’s disease. Trends Neurosci2003;26:207–14.
Buzsaki G, Bickford RG, Ponomareff G, Thal LJ, Mandel R, Gage FH.Nucleus basalis and thalamic control of neocortical activity in thefreely moving rat. J Neurosci 1988;8(11):4007–26.
Celesia GG, Jasper HH. Acetylcholine released from cerebral cortex inrelation to state of activation. Neurology 1966;16(11):1053–63.
Chiaramonti R, Muscas GC, Paganini M, Muller TJ, Fallgatter AJ,Versari A, et al. Correlations of topographical EEG features withclinical severity in mild and moderate dementia of Alzheimer type.Neuropsychobiology 1997;36(3):153–8.
Cherny RA, Legg JT, McLean CA, Fairlie D, Huang X, Atwood CS,et al. Aqueous dissolution of Alzheimer’s disease Ab amyloid depositsby biometal depletion. J Biol Chem 1999;274:23223–8.
Chu NS, Chu CC, Tu SC, Huang CC. EEG spectral analysis andtopographic mapping in Wilson’s disease. J Neurol Sci 1991;106(1):1–9.
Citron M, Westaway D, Xia W, Carlson G, Diehl T, Levesque G, et al.Mutant presenilins of Alzheimer’s disease increase production of 42-residue amyloid b-protein in both transfected cells and transgenic mice.Nat Med 1997;3:67–72.
Claus JJ, Kwa VI, Teunisse S, Walstra GJ, van Gool WA, Koelman JH,et al. Slowing on quantitative spectral EEG is a marker for rate ofsubsequent cognitive and functional decline in early Alzheimer disease.Alzheimer Dis Assoc Disord 1998;12(3):167–74.
Claus JJ, Ongerboer De Visser BW, Bour LJ, Walstra GJ, Hijdra A,Verbeeten Jr B, et al. Determinants of quantitative spectral electro-encephalography in early Alzheimer’s disease: cognitive function,regional cerebral blood flow, and computed tomography. DementGeriatr Cogn Disord 2000;11(2):81–9.
Coben LA, Danziger WL, Berg L. Frequency analysis of the resting awakeEEG in mild senile dementia of Alzheimer type. ElectroencephalogrClin Neurophysiol 1983;55(4):372–80.
Cook IA, Leuchter AF. Synaptic dysfunction in Alzheimer’s disease: clinicalassessment using quantitative EEG. Behav Brain Res 1996;78(1):15–23.
Cuculic Z, Bost K, Himwich HE. An examination of a possible corticalcholinergic link in the EEG arousal reaction. Prog Brain Res 1968;28:27–39.
Devanand DP, Folz M, Gorlyn M, Moeller JR, Stern J. Questionabledementia: clinical course and predictors of outcome. J Am Geriatr Soc1997;45:321–8.
Dierks T, Ihl R, Frolich L, Maurer K. Dementia of the Alzheimer type:effects on the spontaneous EEG described by dipole sources. Psychi-atry Res 1993;50(3):51–162.
Dierks T, Kuhn W, Oberle S, Muller T, Maurer K. Generators of brainelectrical activity in patients with Wilson’s disease. Eur Arch Psychi-atry Clin Neurosci 1999;249(1):15–20.
Dierks T, Jelic V, Pascual-Marqui RD, Wahlund LO, Julin P, LindenDEJ, et al. Spatial pattern of cerebral glucose metabolism (PET)correlates with localization of intracerebral EEG-generators in Alz-heimer’s disease. Clin Neurophysiol 2000;111:1817–24.
Ding L, Lai Y, He B. Low resolution brain electromagnetic tomographyin a realistic geometry head model: a simulation study. Phys Med Biol2005;50(1):45–56.
Dringenberg HC. Alzheimer’s disease: more than a ‘cholinergic disorder’ -evidence that cholinergic-monoaminergic interactions contribute toEEG slowing and dementia. Behav Brain Res 2000;115(2):235–49,Review.
Elmstahl S, Rosen I. Postural hypotension and EEG variables predictcognitive decline: results from a 5-year follow-up of healthy elderlywomen. Dement Geriatr Cogn Disord 1997;8(3):180–7.
Fernandez A, Arrazola J, Maestu F, Amo C, Gil-Gregorio P, WienbruchC, et al. Correlations of hippocampal atrophy and focal low-frequency magnetic activity in Alzheimer disease: volumetric MRimaging-magnetoencephalographic study. AJNR Am J Neuroradiol2003;24(3):481–7.
1258 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
Feshchenko VA, Veselis RA, Reinsel RA. Comparison of the EEG effectsof midazolam, thiopental, and propofol: the role of underlyingoscillatory systems. Neuropsychobiology 1997;35(4):211–20.
Flicker CS, Ferris H, Reisberg B. Mild cognitive impairment in theelderly: predictors of dementia. Neurology 1991;41:1006–9.
Folstein MF, Folstein SE, McHugh PR. ‘Mini Mental State’: a practicalmethod for grading the cognitive state of patients for clinician. JPsychiatr Res 1975;12:189–98.
Frisoni GB, Beltramello A, Binetti G, Bianchetti A, Weiss C, Scuratti A,et al. Computed tomography in the detection of the vascularcomponent in dementia. Gerontology 1995;41(2):121–8.
Fuchs M, Wagner M, Kastner J. Boundary element method volumeconductor models for EEG source reconstruction. Clin Neurophysiol2001;112(8):1400–7.
Galluzzi S, Sheu CF, Zanetti O, Frisoni GB. Distinctive clinical features ofmild cognitive impairment with subcortical cerebrovascular disease.Dement Geriatr Cogn Disord 2005;19(4):196–203.
Gao S, Hendrie HC, Hall KS, et al. The relationships between age, sex,and the incidence of dementia and Alzheimer’s disease. A meta-analysis. Arch Gen Psychiatry 1998;55:809–15.
Geula C, Mesulam M. Special properties of cholinesterases in the cerebralcortex of Alzheimer’s disease. Brain Res 1989;498(1):185–9.
Geula C, Mesulam MM. Systematic regional variations in the loss ofcortical cholinergic fibers in Alzheimer’s disease. Cereb Cortex1996;6(2):165–77.
Geula C, Mesulam MM. Cholinergic system in Alzheimer’s disease. In:Terry RD, editor. Alzheimer disease. 2nd ed. Philadelphia, PA: Lip-pincot, Williams and Wilkins; 1999. p. 69–292.
Giubilei F, Marchione F, Forte G, Bocca B, Sepe-Monti M, Bomboi G,et al. Trace and major elements in whole blood and serum of patientswith Alzheimer’s disease. Neurobiol Aging 2004;25(2):353.
Gloor P, Ball G, Schaul N. Brain lesions that produce delta waves in theEEG. Neurology 1977;27(4):326–33.
Goforth HW, Konopka L, Primeau M, Ruth A, O’Donnell K, Patel R,et al. Quantitative electroencephalography in frontotemporal demen-tia with methylphenidate response: a case study. Clin EEG Neurosci2004;35(2):108–11.
Gross J, Timmermann L, Kujala J, Salmelin R, Schnitzler A. Properties ofMEG tomographic maps obtained with spatial filtering. Neuroimage2003;19(4):1329–36.
Helkala EL, Hanninen T, Hallikainen M, Kononen M, Laakso MP,Hartikainen P, et al. Slow-wave activity in the spectral analysis of theelectroencephalogram and volumes of hippocampus in subgroups ofAlzheimer’s disease patients. Behav Neurosci 1996;110(6):1235–43.
Herrmann WM, Kubicki S. The use of electrophysiological techniques toproject typical psychotropic drug effects: some examples. EEG EMG ZElektroenzephalogr Elektromyogr Verwandte Geb 1981;12(1):21–32.
Holschneider DP, Waite JJ, Leuchter AF, Walton NY, Scremin OU.Changes in electrocortical power and coherence in response to theselective cholinergic immunotoxin 192 IgG-saporin. Exp Brain Res1999;126(2):270–80.
Hotz MA, Ritz R, Linder L, Scollo-Lavizzari G, Haefeli WE. Auditory aelectroencephalographic effects of midazolam and a-hydroxy-midazo-lam in healthy subjects. Br J Clin Pharmacol 2000;49(1):72–9.
Hoogenraad T. ‘‘Wilson’s disease’’, Intermed Medical Publishers eds,Amsterdam/Rotterdam, 2001.
Hoogenraad T. Paradigm shift in treatment of Wilson’s disease: zinctherapy now treatment of choice. Brain Dev 2006;28(3):141–6.
Huang C, Wahlund LO, Dierks T, Julin P, Winblad B, Jelic V.Discrimination of Alzheimer’s disease and mild cognitive impairmentby equivalent EEG sources: a cross-sectional and longitudinal study.Clin Neurophysiol 2000;11:1961–7.
Huang C, Wahlund LO, Svensson L, Winblad B, Julin P. Cingulate cortexhypoperfusion predicts Alzheimer’s disease in mild cognitive impair-ment. BMC Neurol 2002;2(1):9.
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinicalrating scale for the staging of dementia. Br J Psychiatry1982;140:1225–30.
Ihl R, Eilles C, Frlich L, Maurer K, Dierks T, Perisic I. Electrical brainactivity and cerebral blood flow in dementia of the Alzheimer type.Psychiatry Res 1989;29(3):449–52.
Jelic V, Shigeta M, Julin P. Quantitative electroencephalography powerand coherence in Alzheimer’s disease and mild cognitive impairment.Dementia 1996;7:314–23.
Jelic V, Johansson SE, Almkvist O, Shigeta M, Julin P, Nordberg A, et al.Quantitative electroencephalography in mild cognitive impairment:longitudinal changes and possible prediction of Alzheimer’s disease.Neurobiol Aging 2000;21(4):533–40.
Jeong J. EEG dynamics in patients with Alzheimer’s disease. ClinNeurophysiol 2004;115(7):1490–505.
Jiang ZY. Study on EEG power and coherence in patients with mildcognitive impairment during working memory task. J Zhejiang UnivSci B 2005;6(12):1213–9.
Kanai T, Szerb JC. Mesencephalic reticular activating system and corticalacetylcholine output. Nature 1965;205:80–2.
Killiany RJ, Moss MB, Albert MS, Sandor T, Tieman J, Jolesz F.Temporal lobe regions on magnetic resonance imaging identifypatients with early Alzheimer’s disease. Arch Neurol1993;50(9):949–54.
Kitzberger R, Madl C, Ferenci P. Wilson disease. Metab Brain Dis2005;20(4):295–302.
Klimesch W. Memory processes, brain oscillations and EEG synchroni-zation. Int J Psychophysiol 1996;24(1–2):61–100.
Klimesch W. EEG alpha and theta oscillations reflect cognitive andmemory performance: a review and analysis. Brain Res Rev1999;29:169–95.
Klimesch W, Doppelmayr M, Pachinger T, Russegger H. Event-relateddesynchronization in the alpha band and the processing of semanticinformation. Brain Res Cogn Brain Res 1997;6(2):83–94.
Klimesch W, Doppelmayr M, Russegger H, Pachinger T, Schwaiger J.Induced alpha band power changes in the human EEG and attention.Neurosci Lett 1998;244(2):73–6.
Knott V, Mahoney C, Kennedy S, Evans K. EEG correlates of acuteand chronic paroxetine treatment in depression. J Affect Disord2002;69(1-3):241–9.
Kolev V, Yordanova J, Basar-Eroglu C, Basar E. Age effects on visualEEG responses reveal distinct frontal alpha networks. Clin Neuro-physiol 2002;113(6):901–10.
Kwa VI, Weinstein HC, Posthumus-Meyjes EF, Van Royen EA, Bour LJ,Verhoeff PN, et al. Spectral analysis of the EEG and 99m-Tc-HMPAO-SPECT-scan in Alzheimer’s disease. Biol Psychiatry1993;33(2):100–7.
Lawton MP, Brodie EM. Assessment of older people: self maintaining andinstrumental activity of daily living. J Gerontol 1969;9:179–86.
Leuchter AF, Cook IA, Newton TF, Dunkin J, Walter DO, RosenbergTompson S, et al. Regional differences in brain electrical activity indementia: use of spectral power and spectral ratio measures. Electro-encephalogr Clin Neurophysiol 1993;87:385–93.
Mancini G, Carbonara AO, Heremans JF. Immunochemical quantitationof antigens by single radial immunodiffusion. Immunochemistry1965;2:235–43.
Mattia D, Babiloni F, Romigi A, Cincotti F, Bianchi L, Sperli F, et al.Quantitative EEG and dynamic susceptibility contrast MRI inAlzheimer’s disease: a correlative study. Clin Neurophysiol2003;114(7):1210–6.
Mareck Z, Nevsimalova S. J Inherit Metab Dis 1984;7:41–5.Mash DC, Flynn DD, Potter LT. Loss of M2 muscarine receptors in the
cerebral cortex in Alzheimer’s disease and experimental cholinergicdenervation. Science 1985;228(4703):1115–7.
Maurer K, Dierks T. Functional imaging procedures in dementias:mapping of EEG and evoked potentials. Acta Neurol Scand Suppl1992;139:40–6.
McKeith IG, Perry EK, Perry RH. Report of the second dementiawith Lewy body international workshop: diagnosis and treatment.Consortiumon Dementia with Lewy Bodies. Neurology1999;53:902–5.
C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260 1259
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM.Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDAWork Group under the auspices of Department of Health and HumanServices Task Force on Alzheimer’s disease. Neurology 1984;34:939–44.
Metherate R, Cox CL, Ashe JH. Cellular bases of neocortical activation:modulation of neural oscillations by the nucleus basalis and endog-enous acetylcholine. J Neurosci 1992;12(12):4701–11.
Mesulam MM, Mufson EJ, Levey AI, Wainer BH. Cholinergic innerva-tion of cortex by the basal forebrain: cytochemistry and corticalconnections of the septal area, diagonal band nuclei, nucleus basalis(substantia innominata), and hypothalamus in the rhesus monkey. JComp Neurol 1983;214(2):170–97.
Mesulam M, Shaw P, Mash D, Weintraub S. Cholinergic nucleus basalistauopathy emerges early in the aging-MCI-AD continuum. AnnNeurol 2004;55(6):815–28.
Mesulam M. The cholinergic lesion of Alzheimer’s disease: pivotal factoror side show? Learn Mem 2004;11:43–9.
Moretti DV, Babiloni F, Carducci F, Cincotti F, Remondini E, RossiniPM, et al. Computerized processing of EEG-EOG-EMG artefact formulticentirc studies in EEG oscillations and event-related potentials.Int J Pshycophysiol 2003;47(3):199–216.
Moretti VD, Babiloni C, Binetti G, Cassetta E, Dal Forno G, Ferreri F,et al. Individual analysis of EEG frequency and band power in mildAlzheimer’s Disease. Clin Neurophysiol 2004;115:299–308.
Muller TJ, Thome J, Chiaramonti R, Dierks T, Maurer K, Fallgatter AJ,et al. A comparison of qEEG and HMPAO-SPECT in relation to theclinical severity of Alzheimer’s disease. Eur Arch Psychiatry ClinNeurosci 1997;247(5):259–63.
Niedermeyer E. Alpha rhythms as physiological and abnormal phenom-ena. Int J Psychophysiol 1997;26:31–49.
Nobili F, Taddei G, Vitali P, Bazzano L, Catsafados E, Mariani G, et al.Relationships between 99m Tc-HMPAO ceraspect and quantitative EEGobservations in Alzheimer’s disease. Arch Gerontol Geriatr 1998;6:363–8.
Nobili F, Vitali P, Canfora M, Girtler N, De Leo C, Mariani G, et al.Effects of long-term Donepezil therapy on rCBF of Alzheimer’spatients. Clin Neurophysiol 2002;113(8):1241–8.
Nuwer MR. Quantitative EEG. I: techniques and problems of frequencyanalysis and topographic mapping. J Clin Neurophysiol 1988;5:1–43.
Osipova D, Ahveninen J, Kaakkola S, Jaaskelainen IP, Huttunen J,Pekkonen E. Effects of scopolamine on MEG spectral power andcoherence in elderly subjects. Clin Neurophysiol 2003;114(10):1902–7.
Prichep LS, John ER, Ferris SH, Reisberg B, Almas M, Alper K, et al.Quantitative EEG correlates of cognitive deterioration in the elderly.Neurobiol Aging 1994;15(1):85–90, Erratum in: Neurobiol Aging1994;15(3):391.
Pascual-Marqui RD, Michel CM. LORETA (low resolution brainelectromagnetic tomography): new authentic 3D functional images ofthe brain. ISBET Newslett ISSN 1994;5:4–8.
Pascual-Marqui RD, Lehmann D, Koenig T, Kochi K, Merlo MC, HellD, et al. Low resolution brain electromagnetic tomography (LORE-TA) functional imaging in acute, neuroleptic-naive, first-episode,productive schizophrenia. Psychiatry Res 1999;90(3):169–79.
Pascual-Marqui RD, Esslen M, Kochi K, Lehmann D. Functionalimaging with low resolution brain electromagnetic tomography(LORETA): a review. Meth Find Exp Clin Pharmacol 2002;24:91–5.
Passero S, Rocchi R, Vatti G, Burgalassi L, Battistini N. QuantitativeEEG mapping, regional cerebral blood flow, and neuropsychologicalfunction in Alzheimer’s disease. Dementia 1995;6:148–56.
Patat A, Alberini H, Bonhomme D, Soubrane C, Allain H, Gandon JM.Effects of tiapride on electroencephalograms and cognitive functions inthe elderly. Int Clin Psychopharmacol 1999;14(4):199–208.
Pechadre JC, Beudin P, Trolese JF, Gabet JY, Eschalier A. A comparisonof the electroencephalographic spectral modifications induced bydiazepam and by hydroxyzine. J Int Med Res 1993;21(5):234–42.
Petersen RC, Smith GE, Ivnik RJ, Tangalos EG, Schaid SN, ThibodeauSN, et al. Apolipoprotein E status as a predictor of the developmentof Alzheimer’s disease in memory-impaired individuals. JAMA1995;273:1274–8.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Kokmen E, Tangelos EG.Aging, memory, and mild cognitive impairment. Int Psychogeriatr1997;9(Suppl 1):65–9.
Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, et al.Current concepts in mild cognitive impairment. Arch Neurol2001;58(12):1985–92.
Pickworth WB, Fant RV, Butschky MF, Henningfield JE. Effects ofmecamylamine on spontaneous EEG and performance in smokers andnon-smokers. Pharmacol Biochem Behav 1997;56(2):181–7.
Ponomareva NV, Selesneva ND, Jarikov GA. EEG alterations in subjectsat high familial risk for Alzheimer’s disease. Neuropsychobiology2003;48(3):152–9.
Prichep LS, John ER, Ferris SH, Rausch L, Fang Z, Cancro R, et al.Prediction of longitudinal cognitive decline in normal elderly withsubjective complaints using electrophysiological imaging. NeurobiolAging 2006;27(3):471–81, Epub 2005 Oct 6..
Priori A, Foffani G, Pesenti A, Tamma F, Bianchi AM, PellegriniM, et al. Rhythm-specific pharmacological modulation of sub-thalamic activity in Parkinson’s disease. Exp Neurol2004;189(2):369–79.
Pucci E, Cacchio G, Angeloni R, Belardinelli N, Nolfe G, Signorino M,et al. EEG spectral analysis in Alzheimer’s disease and differentdegenerative dementias. Arch Gerontol Geriatr 1997;26:283–97.
Pucci E, Belardinelli N, Cacchio G, Signorino M, Angeleri F. EEG powerspectrum differences in early and late onset forms of Alzheimer’sdisease. Clin Neurophysiol 1999;110(4):621–31.
Ray PG, Jackson WJ. Lesions of nucleus basalis alter ChAT activity andEEG in rat frontal neocortex. Electroencephalogr Clin Neurophysiol1991;79(1):62–8.
Religa D, Strozyk D, Cherny RA, Volitakis I, Haroutunian V, Winblad B,et al. Elevated cortical zinc in Alzheimer disease. Neurology2006;67(1):69–75.
Rodriguez G, Nobili F, Rocca G, DeCarli F, Gianelli MV, Rosadini G.Quantitative electroencephalography and regional Cerebral BloodFlow: discriminant analysis between Alzheimer’s patients and healthycontrols. Dement Geriatr Cogn Disord 1998;9:238–74.
Rodriguez G, Copello F, Nobili F, Vitali P, Perego G, Nobili F. EEGspectral profile to stage Alzheimer’s disease. Clin Neurophysiol1999a;110:1831–7.
Rodriguez G, Nobili F, Copello F, Vitali P, Gianelli MV, Taddei G, et al.99mTc-HMPAO regional cerebral blood flow and quantitative elec-troencephalography in Alzheimer’s disease: a correlative study. J NuclMed 1999b;40:522–9.
Rodriguez G, Vitali P, De Leo C, De Carli F, Girtler N, Nobili F.Quantitative EEG changes in Alzheimer patients during long-termdonepezil therapy. Neuropsychobiology 2002;46:49–56.
Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC,Garcia JH, et al. Vascular dementia: diagnostic criteria for researchstudies. Report of the NINDS-AIREN International Workshop.Neurology. 1993;43(2):250–60.
Rosen WG, Terry RD, Fuld PA, Katzman R, Peck A. Pathologicalverification of ischemic score in differentiation of dementias. AnnNeurol 1980;7(5):486–8.
Rubin EH, Morris JC, Grant EA, Vendegna T. Very mild senile dementiaof the Alzheimer type I Clinical assessment. Arch Neurol1989;46(4):379–82.
Saletu B, Anderer P, Saletu-Zyhlarz GM, Pascual-Marqui RD. EEGtopography and tomography in diagnosis and treatment of mentaldisorders: evidence for a key-lock principle. Meth Find Exp ClinPharmacol 2002;24(Suppl D):97–106.
Schaul N, Gloor P, Ball G, Gotman J. The electromicrophysiology ofdelta waves induced by systemic atropine. Brain Res1978;143(3):475–86.
Semba K, Fibiger HC. Organization of central cholinergic systems. ProgBrain Res 1989;79:37–63.
Sekihara K, Sahani M, Nagarajan SS. Localization bias and spatialresolution of adaptive and non-adaptive spatial filters for MEG sourcereconstruction. Neuroimage 2005;25(4):1056–67.
1260 C. Babiloni et al. / Clinical Neurophysiology 118 (2007) 1244–1260
Schreiter-Gasser U, Gasser T, Ziegler P. Quantitative EEG analysis inearly onset Alzheimer’s disease: a controlled study. ElectroencephalogrClin Neurophysiol 1993;86(1):15–22.
Sloan EP, Fenton GW, Kennedy NSJ, MacLennan JM. Electroenceph-alography and single photon emission computed tomography indementia: a comparative study. Psychol Med 1995;25:631–8.
Snaedal J, Kristinsson J, Gunnarsdottier S, et al. Copper Ceruloplasminand superoxide dismutase in patients with Alzheimer’s disease, a case–control study. Dement Geriatr Cogn Disord 1998;9:239–2342.
Smorgon C, Mari E, Atti AR, Dalla Nora E, Zamboni PF, Calzoni F,et al. Trace elements and cognitive impairment: an elderly cohortstudy. Arch Gerontol Geriatr Suppl 2004(9):393–402.
Squitti R, Lupoi D, Pasqualetti P, Dal Forno G, Vernieri F, Chiovenda P,et al. Elevation of serum copper levels in Alzheimer’s disease.Neurology 2002;59(8):1153–61.
Squitti RP, Pasqualetti P, Dal Forno G, et al. Excess of serum copper notrelated to ceruloplasmin in Alzheimer disease. Neurology2005;64:1040–6.
Squitti R, Barbati G, Rossi L, Ventriglia M, Dal Forno G, Cesaretti S,et al. Excess of non ceruloplasmin serum copper in AD correlates withMMSE, csf b-amyloid and H tau. Neurology 2006.
Sternlieb I, Scheinberg IH. Prophylaxis of Wilson’s disease. N Engl J Med1968;278(20):1125.
Steriade M. Sleep oscillations and their blockage by activating systems. JPsychiatr Neurosci 1994;19(5):354–8.
Steriade M. Neuronal substrates of sleep and epilepsy. Cambridge(UK): Cambridge University Press; 2003, p. 522.
Steriade M. Acetylcholine systems and rhythmic activities during thewaking–sleep cycle. Prog Brain Res 2004;145:179–96.
Steriade M, Amzica F, Contreras D. Synchronization of fast (30–40 Hz)spontaneous cortical rhythms during brain activation. J Neurosci1996;16:392–417.
Stewart GR, Frederickson CJ, Howell GA, Gage FH. Cholinergicdenervation-induced increase of chelatable zinc in mossy-fiber regionof the hippocampal formation. Brain Res 1984;290(1):43–51.
Stremmel W, Meyerrose KW, Niederau C, Hefter H, Kreuzpaintner G,Strohmeyer G. Wilson disease: clinical presentation, treatment, andsurvival. Ann Intern Med 1991;115:720–6.
Szava S, Valdes P, Biscay R, Galan L, Bosch J, Clark I, et al. Highresolution quantitative EEG analysis. Brain Topogr 1994;6(3):211–9.
Szelies B, Grond M, Herholz K, Kessler J, Wullen T, Heiss WD.Quantitative EEG mapping and PET in Alzheimer’s disease. J NeurolSci 1992;110:46–56.
Szelies B, Mielke R, Kessler J, Heiss WD. EEG power changes are relatedto regional cerebral glucose metabolism in vascular dementia. ClinNeurophysiol 1999;110(4):615–20.
Talairach J, Tournoux P. Co-planar stereotaxic atlas of the humanbrain. Thieme: Stuttgart; 1988.
The Lund and Manchester Groups. Clinical and neuropathologicalcriteria for frontotemporal dementia. J Neurol Neurosurg Psychiatry1994;57(4):416–8.
Twomey PJ, Viljoen A, House IM, ReyHolds TM, Wierzbicki AS. Verylow plasma copper levels do not automatically imply severe copperdeficiency. Ann Clin Biochem 2005;42:405.
Valdes P, Picton TW, Trujillo N, Bosch J, Aubert E, Riera J. ConstrainingEEG-MEG source imaging with statistical neuroanatomy. Neuroim-age 1998;4:635.
Yamadera H, Ferber G, Matejcek M, Pokorny R. Quantitative pharmaco-electroencephalographic differentiation between the CNS effects ofbromocriptine and imipramine, drugs with qualitatively differentantidepressant properties. Pharmacopsychiatry 1987;20(2):54–9.
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al.Development and validation of a geriatric depression screening scale: apreliminary report. J Psychiatr Res 1982–1983;17(1):37–49.
White SR, Reese K, Sato S, Kaler SG. Spectrum of EEG findings inMenkes disease. Electroencephalogr Clin Neurophysiol1993;87(1):57–61.
Walshe JM. Research evidence and the individual patient. QJM2003;96(4):315.
Wolf H, Jelic V, Gertz H-J, et al. A critical discussion of the role ofneuroimaging in mild cognitive impairment. Acta Neurol Scand2003;107(Suppl 179):52–76.
Zappoli R, Versari A, Paganini M, Arnetoli G, Muscas GC, Gangemi PF,et al. Brain electrical activity (quantitative EEG and bit-mappingneurocognitive CNV components), psychometrics and clinical findingsin presenile subjects with initial mild cognitive decline or probableAlzheimer-type dementia. Ital J Neurol Sci 1995;16(6):341–76.
Zaudig M. A new systematic method of measurement and diagnosis of‘‘mild cognitive impairment’’ and dementia according to ICD-10 andDSM-III-R criteria. Int Psychogeriatr 1992;4(Suppl. 2):203–19.