Bone metabolism alteration on antiepileptic drug therapy
Transcript of Bone metabolism alteration on antiepileptic drug therapy
Correspondence and Reprint requests : Dr. Sunil Karande,Associate Professor of Pediatrics, Department of Pediatrics,Lokmanya Tilak Municipal Medical College & General Hospital,Sion, Mumbai 400 022, India Tel. No. : 91-22-2407 6381[DOI–10.1007/s12098–009–0005–5][Received November 22, 2007; Accepted April 28, 2008]
Original Article
Bone Metabolism Alteration on Antiepileptic Drug Therapy
Geetha Krishnamoorthy1, Sunil Karande2, Nilesh Ahire2, Lily Mathew1 and Madhuri Kulkarni2
Departments of 1Biochemistry and Pediatrics, Lokmanya Tilak Municipal Medical College & General Hospital, Sion,Mumbai, India
ABSTRACT
Objective. To investigate whether serum total alkaline phosphatase (ALP), bone-specific ALP (bone ALP), calcium,phosphorus, 25-hydroxyvitamin D (25-OHvit D) concentrations are altered early in the course of treatment withcarbamazepine or valproic acid monotherapy in ambulatory children with adequate sun exposure; and to determine theeffectiveness of simultaneous supplementation with calcium and 25-OH vitamin D at recommended dietary allowancedoses on these biochemical parameters.
Methods. For each drug, children were divided into two groups (Group A: without supplementation; and Group B: withsupplementation) and serum biochemical parameters estimated at 0, 30, 60, and 90 days of starting treatment. Statisticalanalysis: Serial changes in serum biochemical parameters (mean ± SD) were compared within each of the four groupsusing student’s paired t test. Also for each drug, serum biochemical parameters were compared between Groups A and Bat 0, 30, 60, and 90 days of starting treatment using student’s unpaired t test.
Results. For both drugs, in Group A, serum total ALP levels were significantly increased above the normal range (P<0.0001)by 90 days of starting treatment; however, serum bone ALP level was significantly increased (P=0.002) only in children onvalproic acid. For both drugs when serum biochemical parameters were compared between Groups A and B,supplementation resulted in a significant decrease in serum total ALP (P<0.0001) and bone ALP levels (P<0.001), and asignificant increase in serum calcium (P<0.0001) and 25-OHvit D levels (P<0.0001) by 90 days of starting treatment.
Conclusion. Serum biochemical changes which indicate predisposition to development of rickets or osteomalacia appearwithin 90 days of starting carbamazepine or valproic acid monotherapy. However simultaneous supplementation with oralcalcium and 25-OHvit D is effective in preventing the development of these adverse biochemical changes. [Indian J Pediatr2009; 76 (4) : 377-383] E-mail: [email protected]
Key words: Adverse effects; Anticonvulsants; Carbamazepine; Dietary supplements; Epilepsy; Valproic acid
In recent times it has been documented that epilepticchildren on long term therapy with carbamazepine orvalproic acid of more than 6 months to 2 years maydevelop increased total serum alkaline phosphatase(ALP) levels and reduced serum calcium, inorganicphosphorous, and vitamin D levels.1-7 These adversebiochemical alterations can lead to rickets (in rapidlygrowing children) and osteomalacia (in older children),and over the years to reduced bone mineral density.1-7
Since the signs and symptoms of osteomalacia are non-specific its diagnosis is frequently delayed, till itmanifests as weakness, musculoskeletal pains andincreased rate of fractures in later adult life.8 However,till date there is little data available on how early these
changes in serum ALP, calcium and vitamin D levelsoccur in epileptic children after being initiated oncarbamazepine or valproic acid therapy.8 These adversebiochemical changes have been reported to be reversibleover a period of 12 to15 months with dailysupplementation of vitamin D in epileptic patients onlong-term anti-epileptic drug (AED) therapy.9 Also, it isknown that daily calcium supplementation has apositive effect on skeletal growth in pre-pubertalchildren.10, 11
Although serum total ALP originates from differenttissues, its liver-specific (liver ALP) and bone-specific(bone ALP) isoenzymes are the most abundant parts ofits activity in the sera.12 Determination of total serumALP concentration itself cannot be used to monitoralteration of bone metabolism because the elevation oftotal ALP levels might simply reflect elevated liver ALPlevels, the “well known” adverse influence of AEDs onliver function.13 In recent times it has been recognizedthat serum bone ALP shows changes in bone
Indian Journal of Pediatrics, Volume 76—April, 2009 377
Geeta Krishnamoorthy et al
378 Indian Journal of Pediatrics, Volume 76—April, 2009
metabolism earlier than even the dual energy X-rayabsorptiometry (DXA) method.14 Serum bone ALPconcentration reflects osteoblast activity, is an indicatorof bone formation, and its elevated concentrations canhelp predict future metabolic bone disease and risk offractures independently of bone mineral density.15,16
The present study was undertaken todetermine: (i) whether serum total ALP and itsisoenzymes, calcium, phosphorus, 25 hydroxyvitaminD (25-OHvit D), magnesium, total proteins and albuminlevels are altered early in the course of treatment withcarbamazepine or valproic acid monotherapy inambulatory children with adequate sun exposure; and(ii) to determine the effectiveness of simultaneous dailysupplementation with oral calcium and 25-OHvit D onthese biochemical changes.
MATERIALS AND METHODS
Patient enrolment
Children with “newly diagnosed” uncomplicatedidiopathic epilepsy attending the pediatric out-patientdepartment, or admitted to the pediatric ward and whowere started on standard recommended doses of eithercarbamazepine (10 mg/Kg/day in b.i.d. doses; up to amaximum maintenance dose of 30 mg/Kg/day) orvalproic acid (15 mg/Kg/day in b.i.d. doses; up to amaximum maintenance dose of 40 mg/Kg/day) wereincluded in the study. Children already on calcium andvitamin D supplements, or already having clinical/biochemical evidence of rickets, or growth andneurological impairment, signs of malnutrition, or anychronic disease were excluded from the study. Thesample size was by necessity a convenience sample. Allchildren were residing in our city, ambulatory, pre-pubertal, had normal age appropriate activity andnutritionally adequate diets.
On inclusion in the study, 5 ml venous bloodsamples were collected for assessing serum ALPactivity (total & isoenzymes), calcium, inorganicphosphorous, 25-hydroxyvitamin D (25-OHvit D),magnesium, total proteins and albumin. Standardbiochemical methods were used for analyzing thesamples.17-24 Serum total ALP was estimated by the Kindand King method, ALP isoenzymes (bone ALP, and,non-bone ALP viz. liver ALP and intestinal ALP) by theheat-inactivation method, calcium by the o-cresolphthalein method, inorganic phosphorous by theFiske-Subbarow method, 25-OHvit D by high-performance liquid chromatographic method,magnesium by the titan yellow method, total proteinsby the Biuret method and serum albumin by thebromocresol green method.17-24
Included subjects (on carbamazepine or valproic
acid monotherapy) were randomly divided into twogroups A or B. The children in group A did not receiveany supplementation. The children in group B receiveddaily oral supplementation with calcium and 25hydroxyvitamin D as per recommended dietaryallowance specifications in the form of 5 ml of syrupcontaining 250mg elemental calcium and 125 IU 25-OHvit D. Children in the age group one month to lessthan one year received 3 ml thrice daily, one to less thansix years received 5 ml thrice daily and those in the agegroup of six to12 years received 7.5 ml thrice daily.Supplementation of calcium and 25-OHvit D atrecommended daily allowance doses was decidedkeeping in mind the year round abundance of sunshinein our city, the ambulatory status of the study cases andtheir regular dietary habits. A gap of minimum twohours was kept between the AED and the supplementarysyrup intake. All children in each of the four groups werefollowed up every 15 days for compliance by apediatrician (NA) and the biochemical parameters wereserially estimated at 30, 60, and 90 days.
Consent and ethical approval
The present study was approved by the scientific andethics committees of our institution. All parents hadsigned an informed consent form to participate in thestudy.
Data analysis
The Statistical Package for the Social Sciences program,version 11 for Windows (SPSS Ltd., Chicago, Illinois,USA) was used for data analysis. Data are expressed asmean ± SD values. The student’s paired t test was usedto compare the serial changes in serum biochemicalparameters after starting treatment within each of thefour groups. The student’s unpaired t test was used, foreach drug group, to compare the serum biochemicalparameters between Groups A and B at 0, 30, 60, and90 days of starting treatment. A two-tailed P value of<0.05 was used to define statistical significance.
RESULTS
(I) Children on carbamazepine monotherapy:
There were 15 children in each group and there was nosignificant difference in their age (mean yrs. ± SD) viz.Group A: 6.47 ± 3.26 (range 0.09-11) vs. Group B: 7.14 ±3.15 (range 0.08-11); P = 0.5716.
(a) Comparing serial biochemical changes within eachcarbamazepine group (Table 1).
Group A (non-supplemented group): Serum total ALPlevels were significantly increased and above thenormal range at 30 (P=0.001), 60 (P<0.0001), and 90(P<0.0001) days of starting treatment. Serum bone ALP
Bone Metabolism Alteration on Antiepileptic Drug Therapy
Indian Journal of Pediatrics, Volume 76—April, 2009 379
levels were significantly increased at 60 (P=0.032) days,but by 90 days the increase was not statisticallysignificant. Serum non-bone ALP levels weresignificantly increased at 30 (P<0.0001), 60 (P<0.0001),and 90 (P<0.0001) days. Serum calcium levels weresignificantly decreased at 60 (P<0.0001), and 90(P<0.0001) days; and serum 25-OHvit D levelssignificantly decreased at 90 (P<0.0001) days; butremained within their normal ranges. There were nosignificant changes in serum phosphorous,magnesium, total proteins, and albumin levels whichremained within their normal ranges.
Group B (supplemented group): Serum total ALP levelswere significantly decreased but within the normalrange at 30 (P<0.0001), 60 (P<0.0001), and 90(P<0.0001) days of starting treatment. Serum bone ALPlevels were statistically significantly decreased at 90(P<0.0001) days. Serum non-bone ALP levels werestatistically significantly decreased at 30 (P=0.003), 60(P<0.0001), and 90 (P<0.0001) days. Serum calciumlevels were statistically significantly increased at 30(P=0.006), 60 (P<0.0001), and 90 (P<0.0001) days;serum inorganic phosphorous levels (P=0.014) at 90days; and serum 25-OHvit D levels at 90 (P<0.0001)days; but all levels were within their normal ranges.There were no significant changes in serummagnesium, total proteins, and albumin levels whichremained within their normal ranges.
(b) Comparing serial biochemical changes betweenGroups A and B (Table 3).
Supplementation with calcium and 25-OHvit Dsignificantly prevented an increase in serum total ALPlevels above the normal range at 30 (P=0.0002), 60(P<0.0001), and 90 (P<0.0001) days of startingtreatment. Supplementation resulted in a significantdecrease in serum bone ALP levels at 90 (P=0.0003)days; and serum non-bone ALP levels at 30 (P=0.0004),60 (P<0.0001), and 90 (P<0.0001) days. Lastly,supplementation resulted in a significant increase inserum calcium levels at 30 (P=0.014), 60 (P<0.0001), and90 (P<0.0001) days; and in serum 25-OHvit D levels at90 (P<0.0001) days.
(II) Children on valproic acid monotherapy:
There were 10 children in each group and there was nosignificant difference in their ages (mean yrs. ± SD) viz.Group A: 6.50 ± 2.84 (range 2-11) vs. Group B: 5.52 ±3.32 (range 0.10-10 yrs); P = 0.4872.
(a) Comparing serial biochemical changes within eachvalproic acid group (Table 2):
Group A (non-supplemented group): Serum total ALPlevels were significantly increased at 30 (P<0.0001), andincreased even above the normal range at 60 (P<0.0001),and 90 (P<0.0001) days of starting treatment. Serumbone ALP levels were significantly increased at 60
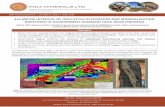
TABLE 1. Serial Changes in Serum Biochemical Parameters in Epileptic Children Receiving Carbamazepine Monotherapy (Group A: withoutSupplementation & Group B: With Calcium and Vitamin D Supplementation) at 30, 60, and 90 Days of Treatment
Parameters Group Pretreatment During Treatment
(normal range) 30 Days P 60 Days P 90 Days P
Total ALP (130-200 U/L) A 188.47 (14.12) 200.33 (15.04) 0.001 210.20 (15.95) <0.0001 243.33 (13.35) <0.0001B 185.40 (15.39) 178.20 (13.21) <0.0001 166.73 (14.17) <0.0001 121.47 (10.02) <0.0001
Bone ALP (U/L) A 72.20 (6.84) 74.33 (8.30) NS 75.60 (9.54) 0.032 73.20 (8.86) NS% bone ALP # 38.31 37.10 - 35.97 - 30.08 -
B 70.60 (9.06) 68.73 (7.08) NS 70.53 (6.94) NS 61.53 (6.14) <0.000138.80 38.57 - 42.30 - 50.65 -
Non-bone ALP (U/L) A 116.67 (13.60) 125.87 (13.90) <0.0001 134.33 (14.00) <0.0001 169.33 (13.55) <0.0001 % non-bone ALP # 61.90 62.83 - 63.91 - 69.59 -
B 114.80 (10.09) 109.47 (7.42) 0.003 96.20 (8.90) <0.0001 59.93 (4.77) <0.000161.92 61.43 - 57.70 - 49.34 -
Calcium (8.8-10.8 mg/dL) A 9.45 (0.15) 9.43 (0.13) NS 9.25 (0.17) <0.0001 9.08 (0.18) <0.0001B 9.43 (0.12) 9.55 (0.12) 0.006 9.66 (0.13) <0.0001 9.85 (0.13) <0.0001
Phosphorous (3-6.5 mg/dL) A 4.00 (0.20) 3.99 (0.26) NS 4.07 (0.30) NS 4.00 (0.25) NSB 3.99 (0.21) 4.00 (0.36) NS 4.01 (0.23) NS 4.05 (0.24) 0.014
25-OHvit D (6-55 ng/mL) A 10.55 (1.56) - - - - 7.34 (1.08) <0.0001B 11.11 (2.19) - - - - 17.84 (3.49) <0.0001
Magnesium (1.5-2.6 mg/dL) A 2.01 (0.24) - - - - 2.05 (0.24) NSB 1.94 (0.30) - - - - 1.95 (0.19) NS
Total proteins (6-8 g/dL) A 7.01 (0.31) - - - - 7.01 (0.44) NSB 7.31 (0.46) - - - - 7.35 (0.38) NS
Albumin (3.5-5 g/dL) A 4.11 (0.40) - - - - 4.13 (0.35) NSB 3.75 (0.43) - - - - 3.78 (0.43) NS
Values are mean (SD); ALP = alkaline phosphatasePaired t test; P<0.05 significant; NS = not statistically significant# Reference interval: bone ALP 11-68%; non-bone ALP 26-86%
Geeta Krishnamoorthy et al
380 Indian Journal of Pediatrics, Volume 76—April, 2009
(P<0.0001) days, and at 90 days (P=0.002). Serum non-bone ALP levels were significantly increased at 30(P<0.0001), 60 (P<0.0001), and 90 (P<0.0001) days.Serum calcium levels were significantly decreased at 60(P<0.0001), and 90 (P<0.0001) days; and serum 25-OHvit D levels significantly decreased at 90 (P<0.0001)days; but remained within their normal ranges. Therewere no significant changes in serum phosphorous,magnesium, total proteins, and albumin levels whichremained within their normal ranges.
Group B (supplemented group): Serum total ALP levelswere significantly decreased but within the normalrange at 60 (P=0.002), and 90 (P<0.0001) days ofstarting treatment. Serum bone ALP levels weresignificantly decreased at 90 (P=0.044) days. Serumnon-bone ALP levels were significantly decreased at 30(P=0.015), 60 (P<0.0001), and 90 (P<0.0001) days.Serum calcium levels were significantly increased at 30(P=0.005), 60 (P=0.006), and 90 (P<0.0001) days; seruminorganic phosphorous levels at 30 (P=0.010), and at90 (P=0.009) days; and serum 25-OHvit D levelsincreased at 90 (P<0.0001) days; but remained withintheir normal ranges. There were no significant changesin serum magnesium, total proteins, and albumin levelswhich remained within their normal ranges.
(b) Comparing serial biochemical changes betweenGroups A and B (Table 3):
Supplementation with calcium and 25-OHvit D
significantly prevented an increase in serum total ALPlevels at 30 (P=0.015) days, and an increase above thenormal range at 60 (P=0.0002), and 90 (P<0.0001) daysof starting treatment. Supplementation resulted in asignificant decrease in serum bone ALP levels at 30(P=0.026), and at 90 (P<0.0001) days; and serum non-bone ALP levels at 30 (P=0.014), 60 (P<0.0001), and 90(P<0.0001) days. Lastly, supplementation resulted in asignificant increase in serum calcium levels at 60(P<0.0001), and 90 (P<0.0001) days; and in seruminorganic phosphorous levels (P=0.022) at 30 days, butnot at 60 and 90 days; and in serum 25-OHvit D levelsat 90 (P<0.0001) days.
DISCUSSION
The present study documents that serum biochemicalchanges which indicate predisposition to developmentof rickets or osteomalacia appear within three monthsof starting carbamazepine or valproic acidmonotherapy. However, simultaneous dailysupplementation with oral calcium and 25-OHvit D inrecommended daily allowance doses is effective inpreventing the development of these adversebiochemical changes.
A Medline literature search revealed that only oneprevious study has serially evaluated serum ALPisoenzyme activities in children on carbamazepine
TABLE 2. Serial Changes in Serum Biochemical Parameters in Epileptic Children Receiving Valproic Acid Monotherapy (Group A: withoutSupplementation & Group B: With Calcium and Vitamin D Supplementation) at 30, 60, and 90 Days of Treatment
Parameters Group Pretreatment During Treatment
(normal range) 30 Days P 60 Days P 90 Days P
Total ALP (130-200 U/L) A 189.00 (16.83) 198.80 (19.79) <0.0001 205.60 (17.89) <0.0001 236.60 (16.40) <0.0001B 181.70 (12.93) 179.10 (12.12) NS 169.40 (16.87) 0.002 126.40 (9.63) <0.0001
Bone ALP (U/L) A 74.50 (8.90) 80.50 (13.43) NS 78.6 (9.23) <0.0001 85.20 (7.25) 0.002 % bone ALP # 39.42 40.49 - 38.23 - 36.01 -
B 70.30 (4.76) 69.60 (4.60) NS 71.10 (6.76) NS 64.50 (6.55) 0.04438.69 38.86 - 41.97 - 51.03 -
Non-bone ALP (U/L) A 114.70 (11.40) 122.00 (13.39) <0.0001 127.00 (12.56) <0.0001 151.40 (15.96) <0.0001 % non-bone ALP # 60.69 61.37 - 61.77 - 63.99 -
B 111.40 (10.19) 107.30 (10.52) 0.015 98.30 (11.23) <0.0001 61.90 (4.07) <0.000161.31 59.91 - 58.03 - 48.97 -
Calcium (8.8-10.8 mg/dL) A 9.42 (0.12) 9.41 (0.13) NS 9.17 (0.11) <0.0001 9.03 (0.13) <0.0001B 9.43 (0.16) 9.59 (0.25) 0.005 9.60 (0.23) 0.006 9.89 (0.18) <0.0001
Phosphorous (3-6.5 mg/dL) A 3.97 (0.21) 3.90 (0.31) NS 4.06 (0.22) NS 4.04 (0.27) NSB 4.00 (0.24) 4.18 (0.32) 0.010 4.05 (0.24) NS 4.17 (0.28) 0.009
25-OHvit D (6-55 ng/mL) A 10.90 (1.29) - - - - 7.13 (0.78) <0.0001B 11.13 (1.45) - - - - 18.89 (2.29) <0.0001
Magnesium (1.5-2.6 mg/dL) A 2.02 (0.24) - - - - 1.99 (0.20) NSB 1.99 (0.27) - - - - 2.02 (0.29) NS
Total proteins (6-8 g/dL) A 7.01 (0.31) - - - - 6.99 (0.38) NSB 6.97 (0.29) - - - - 7.01 (0.28) NS
Albumin (3.5-5 g/dL) A 4.43 (0.36) - - - - 4.33 (0.38) NSB 3.90 (0.38) - - - - 4.00 (0.41) NS
Values are mean (SD); ALP = alkaline phosphatasePaired t test; P<0.05 significant; NS = not statistically significant# Reference interval: bone ALP 11-68%; non-bone ALP 26-86%
Bone Metabolism Alteration on Antiepileptic Drug Therapy
Indian Journal of Pediatrics, Volume 76—April, 2009 381
monotherapy.25 In this study by Voudris et al (Greece),elevated concentrations of total ALP, bone ALP, andliver ALP isoenzymes were found in 22 epilepticambulatory children (aged from 5 to 12 years) at 3, 6,and 12 months of carbamazepine monotherapy.25 Toour knowledge, the present study is the first study to: (i)evaluate serum ALP isoenzyme activities in children onvalproic acid monotherapy; (ii) evaluate serum ALPisoenzyme activities in children much earlier (at 30, 60,and 90 days) in the course of starting carbamazepine orvalproic acid monotherapy; and (iii) determine theeffectiveness of simultaneous supplementation withcalcium and 25-OHvit D on serum ALP isoenzymeactivities, and calcium, phosphorus, 25-OHvit D levels.
What is the potential utility of this study? In ourcountry, epilepsy is a common disorder and manychildren are on carbamazepine or valproic acidmonotherapy. The present study highlights that thesechildren are at risk to develop rickets or osteomalaciaand that it may be prudent to start earlysupplementation with calcium and vitamin D as ithelps prevent these adverse biochemical changes. It isbeing increasingly recognized that long-termcarbamazepine or valproic acid monotherapy results inchildren having decreased bone formation and bonemineral density, and low calcium intake could be an
aggravating factor for AED-associated osteopenia.1-7, 26
Childhood is a critical period of skeletal development,and a lower peak bone mass and increased boneturnover in such epileptic children may have long-lasting consequences for bone health, associated withgreater osteoporotic fractures later in adult life.27 Arecent study by Valmadrid et al (USA) has reported thatonly 9% of pediatric neurologists prescribe prophylacticcalcium or vitamin D for children taking AEDs.28 Thepresent study will help raise pediatricians’ awarenessof this problem and help improve the skeletal health ofAED-treated children.
Several theories on the mechanism of AED-associated bone disease have been proposed, but nosingle one explains all the reported findings.8 Thecommonest explanation is that AEDs such ascarbamazepine that induce hepatic cytochrome P450enzymes cause increased conversion of vitamin D toinactive metabolites in the liver microsomes.8 Thedecreased biologically active vitamin D leads todecreased absorption of calcium in the gut, resulting inhypocalcaemia and an increase in circulatingparathyroid hormone. The secondaryhyperparathyroidism is usually subtle and can beassessed by detecting reduced serum calcium andphosphorus levels, and increased serum total ALP
TABLE 3. Comparison of Serum Biochemical Parameters (Group A: Without Supplementation & Group B: With Calcium andVitamin D Supplementation) in Epileptic Children Receiving Carbamazepine or Valproic Acid Monotherapy at 30,60, 90 Days of Treatment
Parameter AED Pretreatment 30 Days 60 Days 90Days(normal range) given Group Group P Group Group P Group Group P Group Group P
A B A B A B A B
Total ALP CBZ 188.47 185.40 NS 200.33 178.20 0.0002 210.20 166.73 <0.0001 243.33 121.47 <0.0001(130-200 U/L) (14.12) (15.39) (15.04) (13.21) (15.95) (14.17) (13.35) (10.02)
VP 189.00 181.70 NS 198.80 179.10 0.015 205.60 169.40 0.0002 236.60 126.40 <0.0001(16.83) (12.93) (19.79) (12.12) (17.89) (16.87) (16.40) (9.63)
Bone ALP CBZ 72.20 70.60 NS 74.33 68.73 NS 75.60 70.53 NS 73.20 61.53 0.0003(U/L) (6.84) (9.06) (8.30) (7.08) (9.54) (6.94) (8.86) (6.14)
VP 74.50 70.30 NS 80.50 69.60 0.026 78.6 71.10 NS 85.20 64.50 <0.0001(8.90) (4.76) (13.43) (4.60) (9.23) (6.76) (7.25) (6.55)
Non-bone ALP CBZ 116.67 114.80 NS 125.87 109.47 0.0004 134.33 96.20 <0.0001 169.33 59.93 <0.0001(U/L) (13.60) (10.09) (13.90) (7.42) (14.00) (8.90) (13.55) (4.77)
VP 114.70 111.40 NS 122.00 107.30 0.014 127.00 98.30 <0.0001 151.40 61.90 <0.0001(11.40) (10.19) (13.39) (10.52) (12.56) (11.23) (15.96) (4.07)
Calcium CBZ 9.45 9.43 NS 9.43 9.55 0.014 9.25 9.66 <0.0001 9.08 9.85 <0.0001(8.8-10.8 mg/dL) (0.15) (0.12) (0.13) (0.12) (0.17) (0.13) (0.18) (0.13)
VP 9.42 9.43 NS 9.41 9.59 NS 9.17 9.60 <0.0001 9.03 9.89 <0.0001(0.12) (0.16) (0.13) (0.25) (0.11) (0.23) (0.13) (0.18)
Phosphorous CBZ 4.00 3.99 NS 3.99 4.00 NS 4.07 4.01 NS 4.00 4.05 NS(3-6.5 mg/dL) (0.20) (0.21) (0.26) (0.36) (0.30) (0.23) (0.25) (0.24)
VP 3.97 4.00 NS 3.90 4.18 0.022 4.06 4.05 NS 4.04 4.17 NS(0.21) (0.24) (0.31) (0.32) (0.22) (0.24) (0.27) (0.28)
25-OHvit D CBZ 10.55 11.11 NS - - - - - - 7.34 17.84 <0.0001(6-55 ng/mL) (1.56) (2.19) (1.08) (3.49)
VP 10.90 11.13 NS - - - - - - 7.13 18.89 <0.0001(1.29) (1.45) (0.78) (2.29)
Values are mean (SD)Unpaired t test; P<0.05 significant; NS = not statistically significantALP = alkaline phosphatase; AED = antiepileptic drug; CBZ = carbamazepine; VP = valproic acid
Geeta Krishnamoorthy et al
382 Indian Journal of Pediatrics, Volume 76—April, 2009
levels. The hyperparathyroidism increases themobilization of bone calcium stores, resulting inincreased bone turnover and loss of cortical bone,which, in severe cases, causes rickets and painfulosteomalacia.8 However, this theory does not explainthe mechanism of valproic acid-associated bonedisease, as valproic acid is an inhibitor of thecytochrome P450 enzyme system.8
The present study has four limitations. First, thesample size is small considering the incidence ofchildren on carbamazepine or valproic acidmonotherapy in our city. Second, a detailed study oftheir dietary mineral intake could not be performed asthe patients were ambulatory. Third, due to financialconstraints we could not simultaneously measure bonedensity by the dual-energy x-ray absorptiometrymethod. But it is very unlikely that any bone densityalterations would have occurred within 90 days ofstarting treatment with carbamazepine or valproic acid.It is known that the dual-energy x-ray absorptiometrymethod might not reveal early or minor changes inmineral content or minor decrement of the bone mass.8
Fourth, it is beyond the ability of this study to evaluateto what extent elevated serum bone ALP levels in thesechildren, especially those on valproic acid, correlates toa clinically important impact on bone metabolism.Therefore, we suggest that large, prospective, controlledstudies should be undertaken to determine this clinicalimpact on bone metabolism and particularly toevaluate the risk of fractures in these epileptic children.However, we have no reason to believe that theselimitations adversely affect the utility of our results.Both due to the limitations as outlined above and thegeneral paucity of data, there is a need for further studyof this topic in pediatric neurology clinics situated allover the world.
CONCLUSION
The present study documents that treatment withcarbamazepine or valproic acid monotherapy increasesserum bone ALP activities within a few weeks,indicating altered bone function. The study alsosuggests that simultaneously starting daily oralsupplementation with calcium and 25-OHvit D inchildren initiated on carbamazepine or valproic acidmonotherapy is beneficial as it prevents development ofbiochemical changes predisposing to development ofrickets or osteomalacia.
Acknowledgements
We thank our Dean, Dr. M.V. Kulkarni, for granting uspermission to publish this study; Mr. Kailas Gandewar,our Biostatistician for his help in the statistical analysis
of the data; and the patients who participated in thestudy.
REFERENCES
1. Sheth RD, Wesolowski CA, Jacob JC et al . Effect ofcarbamazepine and valproate on bone mineral density. JPediatr 1995;127:256-262.
2. Kafali G, Erselcan T, Tanzer F. Effect of antiepileptic drugson bone mineral density in children between ages 6 and 12years. Clin Pediatr (Phila) 1999;38:93-98.
3. Erbayat Altay E, Serdaroglu A, Tumer L, Gucuyener K,Hasanoglu A. Evaluation of bone mineral metabolism inchildren receiving carbamazepine and valproic acid. JPediatr Endocrinol Metab 2000;13:933-939.
4. Rieger-Wettengl G, Tutlewski B, Stabrey A et al. Analysis ofthe musculoskeletal system in children and adolescentsreceiving anticonvulsant monotherapy with valproic acid orcarbamazepine. Pediatrics 2001;108:E107.
5. Ecevit C, Aydogan A, Kavakli T, Altinoz S. Effect ofcarbamazepine and valproate on bone mineral density.Pediatr Neurol 2004;31:279-282.
6. Babayigit A, Dirik E, Bober E, Cakmakci H. Adverse effectsof antiepileptic drugs on bone mineral density. PediatrNeurol 2006;35:177-181.
7. Kumandas S, Koklu E, Gumus H et al. Effect ofcarbamezapine and valproic acid on bone mineral density,IGF-I and IGFBP-3. J Pediatr Endocrinol Metab 2006;19:529-534.
8. Pack AM. The association between antiepileptic drugs andbone disease. Epilepsy Curr 2003;3:91-95.
9. Collins N, Maher J, Cole M, Baker M, Callaghan N. Aprospective study to evaluate the dose of vitamin Drequired to correct low 25-hydroxyvitamin D levels,calcium, and alkaline phosphatase in patients at risk ofdeveloping antiepileptic drug-induced osteomalacia. Q JMed 1991;78:113-122.
10. Johnston CC Jr, Miller JZ, Slemenda CW et al. Calciumsupplementation and increases in bone mineral density inchildren. N Engl J Med 1992;327:82-87.
11. Bonjour JP, Carrie AL, Ferrari S et al. Calcium-enrichedfoods and bone mass growth in prepubertal girls: arandomized, double-blind, placebo-controlled trial. J ClinInvest 1997;99:1287-1294.
12. Meyer-Sabellek W, Sinha P, Kottgen E. Alkalinephosphatase: Laboratory and clinical implications. J Chrom1988;429:419–444.
13. Kruse K, Bartels H, Gunther H. Serum alkaline phosphataseisoenzymes in epileptic children receving anticonvulsantdrugs. Eur J Pediatr 1977;126:237-242.
14. Watts NB: Clinical utility of biochemical markers of boneremodeling. Clin Chem 1999;45:1359–1368.
15. Looker AC, Bauer DC, Chesnut CH 3rd et al Clinical use ofbiochemical markers of bone remodeling: current status andfuture directions. Osteoporos Int 2000;11:467-480.
16. Ross PD, Kress BC, Parson RE, Wasnich RD, Armour KA,Mizrahi IA. Serum bone alkaline phosphatase andcalcaneus bone density predict fractures: a prospectivestudy.Osteoporos Int 2000;11:76-82.
17. Kind PR, King EJ. Estimation of plasma phosphatase bydetermination of hydrolysed phenol with amino-antipyrine.J Clin Pathol 1954;7:322-326.
18. Moss DW, Whitby LG. A simplified heat-inactivationmethod for investigating alkaline phosphatase isoenzymes
Bone Metabolism Alteration on Antiepileptic Drug Therapy
Indian Journal of Pediatrics, Volume 76—April, 2009 383
in serum. Clin Chim Acta 1975;61:63-71.19. Kessler G, Wolfman M. An automated procedure for the
simultaneous determination of calcium and phosphorus.Clin Chem 1964;10:686-703.
20. Fraser D, Jones G, Kooh SW, Radde IC. Calcium andphosphate metabolism. In Tietz NW, ed. Fundamentals ofClinical Chemistry, 3rd ed. Philadelphia; W B Saunders,1987;705-728.
21. Aksnes L. A simplified high-performance liquidchromatographic method for determination of vitamin D3,25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 inhuman serum. Scand J Clin Lab Invest 1992;52:177-182.
22. Neill DW, Neely RA. The estimation of magnesium inserum using titan yellow. J Clin Pathol 1956; 9: 162-163.
23. Lubran MM. The measurement of total serum proteins bythe Biuret method. Ann Clin Lab Sci 1978;8:106-110.
24. Doumas BT, Watson WA, Biggs HG. Albumin standards
and the measurement of serum albumin with bromcresolgreen. Clin Chim Acta 1971;31:87-96.
25. Voudris KA, Attilakos A, Katsarou E et al. Early alterationin bone metabolism in epileptic children receivingcarbamazepine monotherapy owing to the induction ofhepatic drug-metabolizing enzymes. J Child Neurol2005;20:513-516.
26. Tsukahara H, Kimura K, Todoroki Y et al. Bone mineralstatus in ambulatory pediatric patients on long-term anti-epileptic drug therapy [published erratum appears inPediatr Int 2002;44:466]. Pediatr Int 2002;44:247-253.
27. Sheth RD. Bone health in epilepsy. Epilepsia 2002;43:1453-1454.
28. Valmadrid C, Voorhees C, Litt B, Schneyer CR. Practicepatterns of neurologists regarding bone and mineral effectsof antiepileptic drug therapy. Arch Neurol 2001;58:1369-1374.