Barcelona, 6-8 junio 2016 Preceptorship in Multiple sclerosis
-
Upload
khangminh22 -
Category
Documents
-
view
2 -
download
0
Transcript of Barcelona, 6-8 junio 2016 Preceptorship in Multiple sclerosis
Àlex Rovira Unidad de Neurorradiología. Servicio de Radiología
Hospital Vall d’Hebron Barcelona
RM en la Esclerosis Múltiple
Barcelona, 6-8 junio 2016 Preceptorship in Multiple sclerosis
T2 and CE T1-WI
• Highly sensitive for detecting MS plaques (white matter)
• Provide quantitative assessment of disease activity and severity
• Characterize disease course over time
• Monitor and predict treatment response
• Most important paraclinical tool for diagnosing and monitoring MS
T2-weighted (FLAIR)
Post-contrast T1-weighted
MR imaging in MS
Bakshi et al. Lancet Neurol 2008;7:615–25
Incidental finding Virchow-Robin spaces normal population (5-10%) migraine (x4) Hipoxic-ischemic vasculopathies
small-vessel disease hyperhomocysthenimia CADASIL Susac’s syndrome
Primary demyelinating diseases multiple sclerosis and variants ADEM neuromyelitis optica
Vasculitis primary systemic: lupus, Behçet, APLAS Miscellaneous
neurosarcoidosis Lyme disease PML metabolic: Fabry, Leber, xantomatosis, adult forms of leukodystrophy effects of radiation therapy or drugs lymphoma metastasic disease
Multifocal WM signal abnormalities: “white spots”
Sánchez Aliaga E, Barkhof F. Handb Clin Neurol 2014;122:291-316; Charil et al. Lancet Neurol 2006;5:841-52
Solomon et al. Neurology 2012;78:1986-91
•Survey: 122 Neurologist (90% from Academic Hospitals) •95% reported having evaluated 1 or more patients who had been diagnosed with MS, but who they strongly felt did not have MS (within the last year) •Mainly due to overuse and improper interpretation of MRI (non specific findings) •>25% under treatment (difficult to take away)
Increase specificity of MRI findings is highly required
Misdiagnosis of Multiple Sclerosis
2013
2015
55 year old female with a diagnosis of multiple sclerosis. Treated with DMDs since 2009
Solomon et al. Curr Neurol Neurosci Rep 2013; Charil et al. Lancet Neurol 2006; 5: 841–52;Solomon et al. Neurology 2012;78:1986-91; Rudick et al. Neurology. 2013;80:777; Kim et al. Mult Scler. 2013;19:1060-7
•Most frequent contemporary reason for misdiagnosis •MR features not considered in the context of careful clinical evaluation •Overdiagnosis of RIS
Misdiagnosis of MS: overreliance on MRI interpretation
•Incidental multifocal WM brain lesions on MRI
normal population aged 18-50 (5-10%) migraine (x4)
Misdiagnosis has significant consequences: • Clinical, psychosocial and scientific • Health care system cost (overtreatment with DMTs; approx 40.000 subjects in US)
Comprehensive checklist for evaluation of WM spots
Brief and precise diagnostic impression that must consider:
Demographics Family history Vascular risk factors Clinical information and question Lab findings
Diagnostic strategy in subjects with incidental multifocal brain T2 lesions of unknown origin
Systematic reading
•Lesion distribution / involvement subcortical/periventricular U-fibers cortical grey matter deep grey matter corpus callosum brainstem spinal cord
•Lesion shape •Enhancement pattern •Features on special sequences: SWI •Ancillary findings
microbleeds vascular abnormalities
Kanecar et al. Radiol Clin N Am 2014; 52:241-61; Sánchez Aliaga E, Barkhof F. Handb Clin Neurol 2014;122:291-316
• Cortical lesions • Spinal cord MRI: diagnostic and prognostic value • Perivenular distribution • Iron imaging
Update on Diagnosis
Kutzelnigg et al. Brain 2005
RRMS SPMS PPMS
focal demyelinated plaques in the white matter
cortical demyelination
demyelinated lesions in the deep grey matter
Cortical gray matter involvement in MS
• Characterised by: – demyelination1
– microglial activation1
– often meningeal inflammation2,3
• Less often associated with4
– immune cell influx
– complement activation
– BBB leakage
• Difficult to detect by MRI5
• Three types of cortical lesion*6
*Based on post-mortem tissue samples taken from 22 patients with MS. Leukocortical Type I lesions involve neocortex and subcortical white matter; intracortical Type II lesions are confined to the neocortex and often located around a vessel; subpial Type III lesions extend from the pial surface into the neocortex. 1. Peterson JW et al. Ann Neurol 2001; 2. Lucchinetti CF et
al. N Engl J Med 2011; 3. Magliozzi R et al. Ann Neurol 2010; 4. Klaver R et al. Prion 2013; 5. Filippi M et al. Neurology 2010; 6. Wegner C et al. Neurology 2006
38% are Type I (leukocortical)
18% are Type II (intracortical)
44% are Type III (subpial)
Focal lesions in grey matter 90% of MS autopsy cases show cortical demyelination
Type I Type II Type III
Courtesy of Dr. García-Merino
T2-FLAIR
leukocortical lesion Lucchinetti et al. NEJM 2011;365:2188-97
Juxtacortical lesions (type I)
MRI sensitivity depends on lesion type and sequence
Geurts et al. J Neurol 2008; Wattjes et al. Am J Neuroradiol 2006; Geurts et al. Radiology 2005; Roosendaal et al. Mult Scler 2009
• cMRI detects <10% of pure intracortical lesions • Higher detection of mixed lesions • Improved sensitivity by using DIR or heavily 3D T1-weighted sequences
mixed lesion intracortical lesion
Cortical lesions (type II-III)
T2-FLAIR DIR
Type I-III lesions
Present in 44% of CIS and in 70% of MS patients
Absent in NMO, migraine…
Calabrese et al. Neurology 2012; 79:1671-6; Absinta et al. J Neurol 2012; 259:2695-8; Pareto et al. Am J Neuroradiol 2015 Oct 8. [Epub ahead of print]
Cortical lesions in CIS and diagnostic criteria
At least 2 of the following:
•1 enhancing or 1 spinal cord lesion •1 infratentorial lesion •1 cortical lesion
DIS Filippi 2010
DIS Polman 2005
DIS Polman 2010
YES
NO
DIS Polman 2005 DIS Polman 2010 DIS Filippi 2010
Sensitivity
74 % 86% 77%
Specificity
73% 42% 93%
Accuracy
74% 61% 86%
OR
7.9 4.3
47.3
Filippi et al. Neurology 2010; Filippi et al. Lancet Neurol 2016
Filippi M, et al. Lancet Neurol 2016; Fox RJ. Lancet Neurol 2016
Cortical lesions in CIS and diagnostic criteria
• Intracortical lesions typically need advanced imaging (DIR) • Assessment of intracortical lesions has a high variability • Inclusion of intracortical lesions into the diagnostic criteria has little clinical
benefit
• Corpus callosum lesions: • Subependymal lesions: • Type I-III lesions (FLAIR): • Type II-III lesions (DIR): • Type I lesions (DIR):
62 CIS patients (3.0 T) (Vall d’Hebron) Concordance analysis (two observers) Mean of kappa for all coder-pairs
Agreement (Landis and Koch)
0.0-0.2 = slight
0.21-0.40 = fair
0.41-0.60 = moderate
0.61-0.80 = substantial
0.81-1.0 = almost perfect/perfect
0.857 0.821 0.838 0.477 0.430
DIR / T2-FLAIR: intracortical vs leukocortical lesions
DIR T2-FLAIR
Nelson et al. Mult Scler 2008
3D MPRAGE
A significant proportion of lesions classified as cortical GM lesions on DIR appear to contain more WM than expected or do not involve GM
Spinal cord lesions in 30% of subjects with RIS
84% progressed to CIS or PPMS (median time 1.6 years) OR of clinical progression: 75.3
Subclinical lesions in 27-53% of patients with CIS
Spinal cord lesions 83% of patients with early relapsing MS
Spinal cord lesions in 74-92% of patients with MS and in 6% of patients with non-MS white matter diseases
O`Riordan et al. JNNP 1998; Dalton et al. JNNP 2003 Lycklama à Nijeholt GJ et al. Brain 1998; Bot et al. Neurology 2004
Okuda et al. Neurology 2011
Prevalence of spinal cord lesions
O'Riordan et al. J Neurol Neurosurg Psychiatry. 1998;64:353-7; Dalton et al. J Neurol Neurosurg Psychiatry. 2003;74:1577-80; Nijeholt et al. Brain 1998;121:687-97; Bot et al. Neurology 2004;62:226-33; Okuda et al. Neurology 2011;76:686-92
Selection of T2w MR sequences
Nayak et al. Acta Neurol Scand 2014; Riederer et al. Am J Neuroradiol 2015; Chong et al. Am J Neuroradiol 2016
PD > T2 STIR > T2
T2 STIR T2 PD
DIR > T2
T2 DIR
Cord almost isointense with surrounding CSF
Easy identification of any increase in signal
Higher sensitivity compared to T2 SE
More susceptible to artifacts (false positive)
Use it in combination with T2
Selection of MR sequences
Heavily T1-weighted sequences, such as PSIR (phase-sensitive inversion recovery) or MPRAGE /MP2RAGE (two inversion-contrast magnetization-prepared rapid gradient echo), improve MS lesion detection
Nair et al. Am J Neuroradiol 2013; Alcaide-Leon P, et al. Am J Neuroradiol. 2016
DIR MP2RAGE
T2 sequences: spinal cord
Single echo heavily T2 weighted1-2 : – limited sensitivity in depicting signal abnormalities1-2 – should not be obtained as a stand-alone sequence3
Combination of at least two T2w sequences3: T2, PD, STIR
T2 STIR
1. Philpott et al. Eur J Radiol 2011; 80:780-5; 2. Bot et al. Eur Radiol 2000; 10:753-8; 3.Rovira et al. Nat Rev Neurol 2015;11:471-82.
No cord swelling (unless active)
Unequivocal hyperintense T2 or Gd-enhancing; focal lesions
≥3mm in size; <2 vertebral segments long
Peripheral location, cigar shaped
Occupying only part of cord cross-section (less than 50%)
Typical MR imaging findings: spinal cord
Bot et al. Neurology. 2004; 62:226-33; Weier et al. Mult Scler 2012;18:1560-9; Gass et al. Lancet Neurol 2015;14:443-54
Spinal cord MRI in the diagnosis process and in monitoring
Magnims: Magnetic Resonance Imaging in Multiple Sclerosis network (Europe) CMSC: consortium of Multiple Sclerosis Centers (North America)
1.) Rovira et al. Nat Rev Neurol 2015;;11:471-82; 2.) Wattjes et al. Nat Rev Neurol Advance Pub Online 15 Sept 2015 ; 3.) Traboulsee A, et a. Am J Neuroradiol 2015 (in press)
• Spinal cord MR imaging if:1-3
• Transverse myelitis (PTM vs. LETM)
• Insufficient features on brain MRI to support diagnosis of MS
• Age >40 with non-specific brain MRI findings
• Atypical/unexpected new spinal cord symptoms
• Clinical disease progression and relapses not explained by brain MRI (Serial spinal cord imaging may add little to brain imaging alone in monitoring disease activity and progression)
Non spinal CIS not fullfilling McDonald brain MRI criteria
Spinal cord MRI in CIS: •All patients with SC presentation •Non SC patients who do not meet McDonald criteria on brain MRI
Sombekke et al. Neurology 2013
SC lesions
No SC lesions
• 7 MRI scans needed to diagnose 1 more patient • Prognostic value: identifies a subgroup that has a very
low risk of developing MS
Prognostic value of spinal cord MRI in CIS Amsterdam cohort
Prognostic value of spinal cord MRI in CIS The Barcelona inception cohort
Arrambide G et al. Poster presentation (P996) ECTRIMS 2015
Presence of SC lesions is an independent risk factor for evolving to MS
Covariables considered:
•Brain T2 lesion number •OCB in CSF •Age •Gender •CIS topography •Treatment with DMT
• Study design: single-center, observational • Sample size: 207 CIS patients (31% with a spinal cord syndrome) • Follow-up: mean 35.7 (15.8) months. • Outcomes: conversion to MS (CDMS, McDonald)
Arrambide G et al. Poster presentation (P996) ECTRIMS 2015
Prognostic value of spinal cord MRI in CIS The Barcelona inception cohort
• Study design: single-center, observational • Sample size: 207 CIS patients (31% with a spinal cord syndrome) • Follow-up: mean 35.7 (15.8) months. • Outcomes: reach significant disability EDSS ≥ 3.0
Proportion of patients with SC lesions and EDSS ≥3.0.
Presence of at least one SC lesion was associated with an EDSS ≥ 3.0: 11.8% (vs 1.8%) p=0.003
The presence of at least one SC lesion at the time of the CIS is associated with short-term disability and further contributes to estimate the risk of disability accumulation, particularly in non-SC CIS.
aHR for reaching an EDSS >=3.0. Prognostic value of SC lesions on reaching an EDSS ≥3.0. A: All patients (n=207). B: SC CIS (n=64). C: Non-SC CIS (n=143).
Indications of spinal cord MRI in Multiple Sclerosis
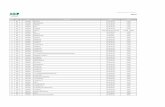
Situation Objective
Clinically isolated syndrome (all) Detect symptomatic and clinically silent lesions Rule out other diseases Increase specificity and sensitivity at diagnosis Predict disability at diagnosis
Negative brain scan, but strong clinical suspicion of MS
Increase sensitivity of diagnosis Investigate possible absence of spinal cord lesions, which could rule out MS
Nonspecific brain MRI findings (e.g. vascular-related lesions, ageing, incidental findings in migraine and/or chronic headache)
Increase sensitivity of diagnosis Investigate possible presence of spinal cord lesions, which could support the diagnosis of MS
Primary progressive MS Increase sensitivity and specificity of diagnosis Detect additional lesions Rule out other diseases
Radiologically isolated syndrome Increase specificity of diagnosis Predict risk of conversion to MS
Monitoring (disease progression and relapses not explained by brain MRI)
Detect disease activity
Rovira A, De Stefano N. Curr Op Neurol 2016 (in press)
Zecca et al. Mult Scler J 2015
Spinal cord MRI in monitoring MS
103 RRMS patients: clinically stable Median interval between scans: 17 months New asymptomatic lesions
A significant proportion of disease activity only in the SC, a fact that could have important implications in assessing and predicting treatment response
46.6%
15.5% 28.1% 9.8%
brain
spinal cord
•43.7% brain •25.2% spinal cord •9.8% only asymptomatic SC lesions
Perivenular topography of MS plaques “Dawson‘s fingers“
Post-mortem pathology studies show central vein
in > 90% white matter lesions
Jens Wuerfel (Berlin)
Dawson J. Trans Roy Soc Edinb 1916; 50:517-740
Horowitz et al. Am J Neuroradiol 1989;10:303-5
venule plaque
• Novel MR technique described by Haacke et al. (MRM 2004)
• Contrast based on the tissue ‘‘magnetic architecture’’ at the subcellular and cellular levels
• Increases sensitivity and conspicuity of MRI for detecting iron containing tissues and small veins (high concentration of deoxihemoglobin) due to their paramagnetic properties
Susceptibility-weighted iamges
Veins visibility Iron within basal ganglia and thalami
(low signal)
Susceptibility-weighted Imaging
FLAIR* sequence (3D GRE + 2D FLAIR at 3T) Central vein visibility
Tallantyre et al. Neurology 2011;76:534-9
7T
Presence of a central vein could be a marker to discriminate between MS and non-MS WM lesions
SWI in T2 lesions (7T)
FLAIR=fluid-attenuated inversion recovery. Kilsdonk ID et al. Eur Radiol. 2014;24:841–849
Axial 7-T FLAIR images of an MS patient and a patient with vascular brain lesions
Solomon et al. ECTRIMS 2015
Migraine-related WMLs vs MS
Central vein sign in MS
Absence of central vein sign in migraine
Intralesional susceptibility signal (ISS) in MS (3T)
SWI FLAIR
Intralesional susceptibility signal (ISS) 48% of non-enhancing MS lesions 58% of enhancing MS lesions
Susceptibility-weighted MR imaging
Likely represents iron-rich macrophages / microglia Myelin loss also contributes
Rovira et al. Multiple Sclerosis Journal 2015; 21 (S11):209
Hagemeier et al. J Magn Reson Imaging 2012;36:73-83; Bian et al. Mult Scler 2013;19:69-75
Serial analysis with QS mapping at 3T
•Magnetic susceptibility increases rapidly as it changes from enhanced to non-enhanced •High susceptibility values during the first 2-4 years •Then gradually decreases (susceptibility similar to NAWM)
Chen et al. Radiology 2014; 271:183-92
Susceptibility-weighted MR imaging in focal MS lesions
1. Early active
2. Center, chronic-active
Large, myelin-laden macrophages without iron
Small myelin-laden macrophages and occasional iron-containing macrophages
Macrophages with large amounts of iron, but without myelin
Perls’ staining
3. Rim, chronic-active
Myelin debris within macrophages detected with oil red-O
Mehta et al. PLOS one 2013;e57573
MS: Lession categories
1
2
3
No or only small amounts of iron
4. Chronic silent white matter lesions
Susceptibility-weighted MR imaging Determinants in image contrast
Myelin, iron, deoxyhemoglobin, and free radicals—all relevant in MS pathogenesis—influence susceptibility signal
• T2*/phase contrast in acute MS lesions appear to be influenced by the presence of free radicals
• T2*/phase contrast in chronic MS lesions appear to be influenced by the topography of iron-laden macrophages and ferritin within lesions
Absinta et al. Ann Neurol 2013
T2-FLAIR
Migraine-related WMLs vs Multiple Sclerosis (3T)
Rovira et al. Multiple Sclerosis Journal 2015; 21 (S11):209
T2-FLAIR SWI
Areas of intralesional signal loss on SWI increases
diagnostic specificity and accuracy MS
Migraine
Migraine-related WMLs vs Multiple Sclerosis (3T)
Rovira et al. Multiple Sclerosis Journal 2015; 21 (S11):209
Sinneckeret al. Neurology 2012;79:708-14
SWI in T2 lesions (7T) 2D T2*- W FLASH
Neuromyelitis optica vs. multiple sclerosis
Venocentric lesions Hypointense rim
SWI
FLAIR
Ovoid lesions
Juxtacortical lesions
Corpus callosum lesion Juxtacortical lesion
ISS within lesions
Preclinical multiple sclerosis or Radiologically isolated
síndrome (RIS)
Clinical case: young female with migraine
Subclinical spinal cord lesions
Frontal subcortical lesions
No subclinical spinal cord lesions
No juxtacortical, corpus callosum lesions
No ISS
SWI
Incidental findings
FLAIR
Clinical case: young female with migraine
Summary
Wide variety of causes may present with multifocal WM lesions
MRI is the preferred imaging technique for diagnostic workup Radiological interpretation with demographic, clinical history,
and lab findings Standardized brain (spinal cord) MRI protocol Comprehensive checklist for evaluation of WM spots is crucial
Sánchez Aliaga E, Barkhof F. Handb Clin Neurol 2014;122:291-316; Charil et al. Lancet Neurol 2006;5:841-52; Rovira et al. Nat Rev Neurol 2015;11:471-82