Application of the model of allostasis to older women's relocation to senior housing
Transcript of Application of the model of allostasis to older women's relocation to senior housing
http://brn.sagepub.com/Biological Research For Nursing
http://brn.sagepub.com/content/early/2013/01/28/1099800412474682The online version of this article can be found at:
DOI: 10.1177/1099800412474682
published online 30 January 2013Biol Res NursHeidi H. Ewen and Jennifer Kinney
Application of the Model of Allostasis to Older Women's Relocation to Senior Housing
Published by:
http://www.sagepublications.com
can be found at:Biological Research For NursingAdditional services and information for
http://brn.sagepub.com/cgi/alertsEmail Alerts:
http://brn.sagepub.com/subscriptionsSubscriptions:
http://www.sagepub.com/journalsReprints.navReprints:
http://www.sagepub.com/journalsPermissions.navPermissions:
What is This?
- Jan 30, 2013OnlineFirst Version of Record >>
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
Application of the Model of Allostasis to OlderWomen’s Relocation to Senior Housing
Heidi H. Ewen, PhD1 and Jennifer Kinney, PhD1
AbstractObjectives: Adjustment to senior housing entails significant lifestyle changes and is a stressful process. The adaptation process isdynamic and has yet to be studied using the conceptual model of allostasis. This article presents exemplars of women whoseprofiles represent three allostatic states: successful adaptation (homeostasis), ongoing adaptation (allostasis), andmaladaptation (allostatic load). Method: Older women who had relocated to senior housing participated in three interviewsand monthly saliva sample collection over a 6-month period. Saliva was assayed for diurnal cortisol secretion. Triangulation ofmixed methods was used to analyze data, and psychosocial data were mapped onto the cortisol graphs to illustrate changes instress reactivity and well-being. Results: Coping abilities, perceptions of stressors, and cortisol measures provide a detailedpicture of the interplay among events and perceptions and the effects of both on well-being. Discussion: The case exemplarsprovide detailed information on the complexity of psychosocial and physiological components of the model of allostasis. Thisstudy also fills a gap in knowledge on negative relocation outcomes using the allostatic model.
Keywordsaging, coping, adaptation, health outcomes, allostatic model
Adults face stressful life events and transitions during the
course of the aging process. Residential relocation may be par-
ticularly stressful due to the need to adapt to a new physical and
social environment while adjusting to the loss of previous
social ties, community, and a well-established home (Krout
& Wethington, 2003; Mallick & Whipple, 2000; Walker,
Curry, & Hogstel, 2007). Relocation may also be associated
with other life transitions including declines in health and phys-
ical ability, death of a spouse, dispersion of adult children, and
loss of social networks (Krause, 1999; Krout, Moen, Holmes,
Oggins, & Bowen, 2002). Despite the potential stress of
residential relocation, research on the process, especially with
respect to physiological indicators, has been limited. Increasing
our understanding of the elements of successful adaptation to
the stress of significant life events such as residential relocation
in later life is essential to the development of appropriate inter-
ventions, support systems, and policies.
The model of allostasis conceptualizes a dynamic system
that ensures physiological stability (McEwen, 2000, 2003;
Sterling & Eyer, 1988). The model emphasizes the process of
establishing stability through change and facilitates the inte-
grated study of an individual’s physiological and psychological
attempts to manage stress. Typically, researchers define a stres-
sor as any event that an individual appraises as threatening her
or his mental, emotional, and/or physical well-being (Aldwin &
Werner, 2007). Physiological responses to stress can be both
triggered and tempered by internal individual characteristics
such as personality, temperament, and lifelong learning as well
as external factors such as social support and life events (Mroc-
zek & Almeida, 2004). The perception of danger, whether
physical or psychological, activates the sympathetic nervous
system, initiating a cascade of physiological reactions. The
hypothalamic–pituitary–adrenal (HPA) axis, a complex endo-
crinological feedback loop, regulates the secretion of stress
hormones that mobilize the fight-or-flight response (Juster,
McEwen, & Lupien, 2010).
Homeostasis occurs when there is a balance among systems,
the ultimate physiological goal. If homeostasis is achieved, an
individual’s fight-or-flight reaction is ameliorated and her cog-
nitive perception of the situation becomes congruent with her
beliefs. Allostasis is the process of negative feedback that
attempts to bring systems into adjustment. Allostasis differs
from homeostasis in its emphasis on dynamic rather than static
biological set points, consideration of the brain’s role in feed-
back regulation, and view of health as a whole-body adaptation
to contexts (Juster et al., 2010; Schulkin, 2003). In the process
of trying to stabilize the system during stressful periods, the
adrenal gland produces excess cortisol in order to mobilize
1 Department of Sociology and Gerontology, Scripps Gerontology Center,
Miami University, Oxford, OH, USA
Corresponding Author:
Heidi H. Ewen, PhD, Miami University, 396 Upham Hall, 100 Bishop Circle,
Oxford, OH 45056, USA.
Email: [email protected]
Biological Research for Nursing00(0) 1-12ª The Author(s) 2013Reprints and permission:sagepub.com/journalsPermissions.navDOI: 10.1177/1099800412474682brn.sagepub.com
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
efforts to deal with the stressor. Physiological dysregulation
ensues when normal homeostatic functioning shifts toward
abnormal ranges via the prolonged secretion of stress hormones
and the subsequent maladaptations this strain exerts on interde-
pendent systems. Allostatic load is the cumulative biological
burden of adapting to life’s demands and is often expressed
as disease onset or exacerbation and even death (Juster et al.,
2010; McEwen, 2000, 2003; Schulkin, 2001; Seeman, Singer,
Rowe, & McEwen, 2001).
Despite the application of the model of allostasis to a range
of stressful life events such as competition, challenges within
social hierarchies, financial strain, and employment instability
(Lantz, House, Mero, & Williams, 2005; McEwen, 1998,
2003), researchers have not used it widely within the geronto-
logical literature. The majority of aging-related research that
uses the model of allostasis focuses on allostatic load (Juster
et al., 2010; Karlamangla, Singer, McEwen, Rowe, & Seeman,
2002; McEwen, 2002; Seeman, McEwen, Rowe, & Singer,
2001). We began to address this gap using the model of
allostasis in a mixed-methods longitudinal study of older
women’s adaptation to relocation to congregate senior housing.
Small-sample, longitudinal, mixed-methods case studies of
physiological reactivity to daily life events and stressors have
effectively captured elevations in cortisol during acute periods
of stress (Stalder, Evans, Hucklebridge, & Clow, 2010; Vincen-
nati, Pasqui, Cavazza, Pagotto, & Pasquali, 2009). For example,
Rahe, Rubin, and Arthur (1974) found repeated elevations in
peak cortisol in one participant during times of anguish and
anger over work changes and personal disappointments. They
also found that this participant’s elevated peak cortisol values
were equivalent to levels found among men engaged in militia
demolition training and diving into oceans from hovering heli-
copters, the epitome of a flight-or-fight reaction. Researchers
in the field of behavioral medicine are increasingly using small
case studies and diary research methods to understand the com-
plex interactions among biological, psychological, and beha-
vioral data (Smyth & Stone, 2003; Stalder et al., 2010).
Consistent with the model of allostasis, we utilized social sci-
ence and biological methodologies in the present study. Mea-
sures include self-reports of stressful life events and appraisals
of stress and coping and an indicator of physiological reactivity,
specifically salivary cortisol. We delve more deeply into three
case studies, each of which exemplifies one of the key processes
in the conceptual model: homeostasis, allostasis, and allostatic
load. Each case study integrates self-report and cortisol data over
the first 6 months of each participant’s relocation to a senior
housing community. Our ultimate goals are to demonstrate the
complexity of stress perceptions and reactivity while testing the
utility of the model of allostasis in studying adaptation to salient
stressors experienced by older adults during a time of potential
physical, emotional, and psychological upheaval.
Method
Participation entailed three semistructured interviews over a 6-
month period, the first within 1 month of the move and
subsequent interviews in the 3rd and 6th months post move;
monthly journals of life events in the months between inter-
views; and monthly salivary cortisol sampling. We based the
timing of interview data collection upon Castle’s (2001) results
from a meta-analysis of morbidities and death at 4, 6, and 12
months post relocation across 35 studies. Castle found the inci-
dence of morbidity and mortality increased between 3 and 12
months post relocation. The Medical Institutional Review
Board at the University of Kentucky approved the present study
(protocol #05-0044).
Sample
The managers of congregate senior housing facilities assisted
with identification and recruitment of new and prospective
female residents. Managers provided information on the study,
including contact information for the primary researcher, to
potential participants and asked the women if they would con-
sent to having their contact information shared with the
primary researcher. If the resident/prospective resident agreed,
the manager relayed this information to the project manager.
Once participants were enrolled in the study, we scheduled
an interview within the first 30 days of occupancy in the facil-
ity. The full study sample comprised 26 women between the
ages of 60 and 93 years (mean 76 + 11 years) who had moved
to congregate senior housing facilities (consisting of indepen-
dent- and assisted-living accommodations) in a small city
(population 250,000) on the western fringe of Appalachia in the
United States no more than 1 month before the first interview.
We provided women remuneration for their participation.
Measures and Procedures
Cognitive Screening. The short (6-item) blessed memory test was
administered prior to enrollment in the study. We included only
women who scored less than 10 (i.e., no cognitive impairment)
in the sample (Davis, Morris, & Grant, 1990). This scale has
established reliability and validity (McDowell & Newell,
1996) in detecting memory impairments.
Interview Protocol. We conducted semistructured interviews with
open-ended items on stressors and coping strategies in each
woman’s residence. At each of the three interviews, women
responded to prompts about what had been the most rewarding
and most stressful aspects of relocation (first interview) and the
most rewarding and most stressful aspects of their lives since
the last interview (second and third interviews). After they
identified stressors, we asked participants to indicate how they
coped with each stressor. The Perceived Stress scale (PSS;
Cohen & Williamson, 1988) was embedded in the semistruc-
tured interview, with the interviewer reading individual items
from the scale aloud to the participants and recording their
answers on a Likert-type scale. Participants had a response card
to guide them in the Likert-scale response choices. Eskin and
Parr (1996) reported reliability estimates of .84 for the
14-item and 4-item versions of the PSS.
2 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
We also asked questions regarding sleep quantity and
quality at each interview, including, ‘‘What time did you
awaken this morning? How many hours of sleep did you have
last night? What time of the day do you usually awaken? How
many hours of sleep do you get on a typical night? How many
times do you awaken during the night, on an average night? Do
you regularly take naps? If so, how long are your naps?’’
Journals. During the months when we did not conduct inter-
views, participants kept journals. In accordance with extant lit-
erature on diary research methods (Cain, Depp, & Jeste, 2009;
Clayton & Thorne, 2000; Jacelon & Imperio, 2005), partici-
pants used the journals to record significant events (related to
facility life or external factors such as family), dates of the
events, and their perceptions of the relevance and stressfulness
of each event. The journals also provided information on
procedures for monthly saliva sampling (e.g., dates for, timing
of, and procedures for collection). Participants also used the
journals to rate Likert-scaled items that inquired about sleep
quality, quantity, and degree of rest experienced the night prior
to saliva collection.
Interview and Journal Analytic Strategy. We deidentified open-
ended items for self-report of current stressors and coping
responses and entered them into a spreadsheet. We selected
keywords based upon the frequencies with which the women
mentioned them; the open-ended nature of the items allowed
for multiple responses. We grouped common keywords into
themes, created dichotomous variables representing each
theme, and added them to the database with ‘‘1’’ indicating
presence of the theme as a stressor/coping response and ‘‘0’’
representing the absence of the theme. We then matched
identification numbers with responses and entered the new
variables into the database.
Cortisol Sampling and Analysis. At the conclusion of the first inter-
view, we gave participants six cotton salivettes and instruction
sheets on how to collect the monthly cortisol specimens. Cor-
tisol has a well-documented circadian rhythm of secretion, with
peaks occurring in the morning and levels gradually declining
throughout the day (Edwards, Clow, Evans, & Hucklebridge,
2001). The peak secretion typically occurs 30 min to 1 hr after
waking and the lowest level, the nadir, during the night. The
key times to collect cortisol samples as an indicator of the
degree of stress an individual is experiencing are within 1 hr
of awakening and bedtime (Kumari et al., 2010). An acute
stress response is characterized by an elevated peak and normal
evening values, whereas more chronic stress is indicated by
elevations in both peak and late-evening values.
To assess the diurnal rhythm of cortisol release, we asked
participants to collect saliva samples by saturating a cotton
salivette at the following six time points over a 24-hr period the
day after each interview: (a) just after waking, (b) an hour after
waking, (c) between 1 and 3 p.m., (d) between 4 and 6 p.m.,
(e) between 7 and 9 p.m., and (f) at bedtime. Each salivette was
labeled with the predetermined time for collection and a
checklist to serve as a reminder for when the sample was taken.
Additionally, in the months between the first and third inter-
view, on dates indicated in their journals, participants collected
two samples once a month, within 1 hr of waking and at bed-
time, in order to assess the peak and evening cortisol levels.
There were 30-day intervals between collection dates. The par-
ticipants were asked to place the salivette in the refrigerator as
soon as the saliva collection was completed. We made monthly
reminder calls the day prior to the scheduled collection and
scheduled a specific time and date for pick up. We picked up
the salivettes within a day of the saliva collection and
transported them to the laboratory on ice.
We centrifuged samples at 1,500 g (at 3,000 rpm) for 15 min
and analyzed them in duplicate via enzyme linked immunosor-
bent assay techniques. Intraassay coefficient of variation (CV)
results ranged from 3.5 to 4.7 and interassay CVs ranged from
3.3 to 5.4, indicating acceptable precision in results.
Results
The majority of participating women were widowed (58%) or
divorced (27%) from marriages of significant duration (mean
33 + 19 years) and had been without spouses for an average
of 15 years. Educational attainment of the sample approximates
a normal curve, with 8% completing grade school, 31% obtain-
ing a high school diploma, 35% receiving some college educa-
tion, 19% completing a college degree, and 8% completing a
graduate degree. Participants’ mean self-rated health at
baseline (0¼ poorest health and 10¼ best possible health) was
6.3 (+ 2.2). The average body mass index for the sample was
28.3 kg/m2 (+ 8.42), which is classified as ‘‘overweight.’’
Only two participants were taking hormone-replacement
therapy. On average, participants slept 6.8 hr (+ 1.7) per night,
regularly awakened 3.3 times (+ 3) per night and considered
their sleep quality to be ‘‘somewhat restful’’ (60%). Half of the
sample reported taking daily naps of an average of 45 min
(+ 20) in duration.
We have organized our results below into three sections.
First, we present the distinct diurnal cortisol profiles the 26
women demonstrated. Second, we present the triangulation of
methods we used to identify case exemplars for further analy-
sis. Third, we integrate the interview, journal, and cortisol data
to present case studies of three participants that each illustrate
one of the three primary components of the model of allostasis:
adaptation/homeostasis, allostasis, and allostatic load.
Cortisol Profiles for the Sample
We began our analysis by looking at data from women who had
indicated that relocation was a stressor. It was expected that
these cases would show elevations in peak cortisol values and
that physiological trends over time would follow psychosocial
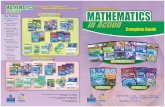
self-reports of stress. Figure 1 illustrates the four distinct diur-
nal cortisol profiles for the full sample at the time of the first
interview: a ‘‘normal’’ pattern for women over 60 years of age,
an allostatic response, aberrant diurnal cortisol rhythms, and
Ewen and Kinney 3
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
allostatic load. Prior research involving careful measurement of
basal cortisol over a period of time found that elevations related
to stress were linked to negative health outcomes and that these
effects were more pronounced in women and exacerbated by
sleep dysregulation (Otte et al., 2005). Given the diurnal
rhythms of and inextricable relations between sleep/wakeful-
ness and cortisol secretion, we evaluated data on sleep beha-
viors to adequately draw conclusions on aberrant cortisol
values (Wrosch, Miller, Lupien, & Pruessner, 2008). Allostatic
load, or exhaustion of the homeostatic mechanism, typically
results in a flattened pattern with roughly equivalent peaks and
nadirs.
Because sleep, use of certain medications, and hormone
replacement therapy affect cortisol levels (Deuschle et al.,
1997), we computed correlations among cortisol levels, self-
reports of quality and quantity of sleep in the night preceding
the collection, and use of hormone replacement therapy and
medications for depression, anxiety, and pain. We found that
peak cortisol values were correlated with perceived stress
(r ¼ .80, p � .01) and evening cortisol values (r ¼ .68,
p � .01). Neither peak nor evening cortisol values were related
to self-reported sleep quality, sleep quantity, or the number of
awakenings during the night. Use of hormone replacement
therapy or medications for depression, anxiety, or pain was not
correlated with perceived stress or the cortisol measures.
However, use of anxiolytics was related to sleep quality
(r ¼ .87, p � .001).
Identifying the Case Examplars
We compared baseline cortisol data for women who mentioned
relocation as a significant stressor in the first interview (n¼ 17)
to the data for those who had not (n¼ 9). All of the women who
had flattened diurnal cortisol rhythms (see Figure 1D) reported
Figure 1. The four distinct diurnal cortisol profiles for the full sample at baseline. A. Depicts the ‘‘normal’’ cortisol pattern for women above theage of 60 (n ¼ 11), with peak cortisol levels around waking time and levels decreasing toward evening. B. Illustrates an allostatic response withcortisol levels elevated throughout the day (n ¼ 6). C. Depicts aberrant diurnal cortisol rhythms (n ¼ 5). Such patterns are often reported toprecede allostatic load and early mortality (Sephton, Sapolsky, Kraemer, & Spiegel, 2000). D. Depicts cases of allostatic load evidenced byexhaustion of the homeostatic mechanism, a flattened diurnal cortisol rhythm, and exacerbation of chronic health conditions (n ¼ 4). Sun andmoon symbols represent the mean peak and evening values, respectively, for adult females over the age of 60 (Aardal & Holm, 1995; Edwardset al., 2001). Dashed lines above and below the mean peak and evening symbols show the 95% CIs for the peak and evening values.
4 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
at the first interview that they considered the move to be a sig-
nificant stressor. We classified women who reported relocation
to be a significant stressor and whose baseline peak cortisol
values were elevated above the 95% confidence interval (CI)
as representative of ‘‘relocation stress.’’ It was from this
category of participants that we selected the case exemplars
for the dynamic processes of homeostasis, allostasis, and
allostatic load.
We triangulated the longitudinal data from diary measures,
interviews, and cortisol data for the women in the ‘‘relocation
stress’’ category, coding self-reports of significant stressors,
effective coping strategies, and satisfaction with the facility
at the 3rd and 6th months in residence using the same method
described above for the baseline data. By examining the
biological, psychological, and behavioral data in this way, we
identified potential case exemplars for each of the three
allostatic processes.
For the process of adaptation/homeostasis, we were looking
for cases in which the cortisol pattern followed peak elevation
in the first month and return to normal range in subsequent
months, while the psychological and behavioral data indicated
that the women encountered perceived stressors but found them
to be manageable. We identified two potential exemplars. We
selected the case of ‘‘Liz’’ due to the relative stability of her
self-reported experiences and cortisol profiles. Her cortisol
levels remained within the 95% CI from Months 2 through 5.
However, a self-reported stressor in Month 6 (mother relocat-
ing) resulted in an elevation in the peak cortisol, illustrating the
dynamic system responsible for establishing stability.
For cases representing allostasis, the process by which the
body attempts to regain homeostasis, we were seeking women
who had peak elevation in the first month and reported ongoing
struggles with stressors and ways to manage those stressors.
Only one exemplar of the dynamic nature of allostasis
emerged: ‘‘Alison’’ was struggling with multiple significant
life stressors and reported emotional fatigue. As her stresses
escalated, she withdrew socially and often ruminated on the
troubles she was facing. Her cortisol profiles indicate a system
escalating cortisol production to mobilize her to face the
stressors and the resultant health impairments, both physical
and mental.
As exemplars of allostatic load, a state in which the body is
no longer able to adjust to the demands placed upon it and that
is typically characterized by onset or exacerbation of chronic
illnesses, we sought cases in which the cortisol peaks and
troughs were proximal to one another, stressors and coping
were ongoing, and health complaints were prominent. We iden-
tified two cases of allostatic load. We selected ‘‘Edna’’ as our
case exemplar based upon her intent to leave the facility within
the month following the last interview because she believed she
had not adapted to her new home, was seeking more contact
with her family, and had experienced the exacerbation of her
health conditions through the 6-month period. Her diurnal
cortisol profiles showed less distinction between peaks and
troughs than would be considered normal, and neither peaks
nor the majority of troughs were within the 95% CIs for a
woman of her age, indicating failure of the homeostatic
mechanism.
We recontacted the three respondents whose profiles we had
identified as exemplars and presented them with a schematic
timeline documenting the information presented in the case
studies below for purposes of member checking.
Case Studies
Homeostasis: The Story of Liz
Liz was a 75-year-old woman who relocated from a nearby
rural community to senior apartments in which her mother
lived. As such, Liz was familiar with the staff and many of the
residents. At the time of the move, Liz was sleeping soundly,
averaging 9 hr per night. She valued sleep and acknowledged
that this longer sleep duration was rare in women of her age.
She had few limitations in activities of daily living but reported
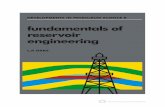
some difficulties with vigorous activities. See Figure 2 for a
graphical depiction of Liz’s cortisol peaks and troughs mapped
to major life events over the 6-month study period.
Pre-Move Major Life Events. In the year preceding the move,
Liz’s spouse died. Liz found her large house in the country too
burdensome and she sought more social contact. Moving to the
facility in which her mother lived appeared to be the ideal
solution as she believed it would also facilitate her ability to
provide assistance as her mother’s dementia progressed. Liz
reported experiencing 14 significant life events in the year
preceding the move, including the death of several family
members as well as close friends; changes in financial status;
and changes in her mother’s health and behavior. Figure 2
shows that her cortisol levels were elevated at the time of the
first interview (baseline).
Pre-Move Perceptions and Cognitive and Behavioral Responses. Liz
reported experiencing a great deal of satisfaction in selling her
home. The most stressful aspect of the year was her spouse’s
death, which precipitated her relocation. Liz used a variety of
coping mechanisms and reported that the most effective strate-
gies were prayer, reading, talking with friends, and volunteer
work.
Post-Move Life Events. At the time of the second interview, Liz
was settling into her new apartment, ‘‘instigating’’ a lot of
activities in the facility and making new friends. She was
becoming more satisfied with her situation as she became
acquainted with other residents. Her sleep patterns had changed
for the worse, with more frequent awakenings leading to her
not feeling as rested in the mornings. In the 3rd month after the
move, Liz fell and broke three ribs. In the 4th month living in
her new residence, Liz took a long weekend to visit family and
was able to leave her mother alone with no problems. Her
daughter remarried a convicted felon who was in a penitentiary,
which angered her to the point of disowning her daughter. At
the time of the third interview (in Month 6), Liz’s mother had
Ewen and Kinney 5
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
relocated to the adjacent nursing home, and Liz found herself
completely occupied with emptying her mother’s apartment.
Contact with her children was much less frequent than before.
Post-Move Perceptions and Cognitive and Behavioral Responses. In
the second interview, Liz reported that social activities and
helping others in need provided her with satisfaction. Her
mother’s health was stable and she spent time with her daily.
She mentioned only a few coping strategies, mainly solitary
activities such as reading and quilting, that helped her to wind
down at the end of each day. These activities remained
consistent through the third interview, 6 months after her move,
at which point Liz was content with her life and new home. She
reported that the most positive aspect of living in the facility
was the social connectedness. Her mother experienced more
behavior problems, particularly wandering, between the 4th
and 6th months, but Liz reported finding comfort in knowing
that her mother was receiving good care in the nursing facility.
Post-Move Cortisol. Even though she faced many stressors, a
serious fall, and changes in her daily activities over the course
of the first few months in her new residence, Liz was able to
achieve and maintain homeostasis, as determined by both her
physiologic measures and self-report data. Her self-reported
perceptions of her stress and coping efficacy were supported
by her cortisol levels, which fell within or very close to the
95% CIs for a normal diurnal profile across Months 2–5. In her
6th month, just a week after her mother relocated, her peak cor-
tisol level increased to above the 95% CI. This increase was not
surprising considering the increased level of caregiving respon-
sibilities associated with her mother’s declining mental func-
tion. The rise in the peak is consistent with her appraisal of
stress at that time. However, Liz had handled multiple stressors
successfully to this point and was well-equipped physically,
emotionally, and socially to handle these additional changes.
We would expect that Liz maintained biological homeostasis
in her new home with her social support.
Allostasis: The Story of Alison
Alison was a 79-year-old woman whose husband of 59 years
suffered vascular dementia. When her husband was unable to
0
5
10
15
20
25
30
35
Morning/Peak Evening/Nadir
Month 1 Month 2 Month 3 Month 4 Month 5 Month 6
Mother moved to nursing care. Conflict with adult child. Christmas holiday.
Feeling socially connected with co-residents. Frustration with lack of environmental control.
Vacation with family; Mother stable.Disowned adult daughter.
Fell; broke 3 ribs. Decline in energy.
Relocation following spouse death. Caregiver for mother with dementia.
Making friends and volunteering within facility. Sleep disruptions
Saliv
ary
Cor
tisol
(nm
ol/L
)
Figure 2. Profile of homeostasis: The case study of Liz. Figure illustrates peak and trough cortisol values over the 6-month study period mappedto major life events. Sun and moon symbols represent the mean peak and evening values, respectively, for adult females over the age of 60(Aardal & Holm, 1995; Edwards et al., 2001). Dashed lines above and below the mean peak and evening symbols show the 95% CIs for the peakand evening values.
6 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
live in their rural home any longer, he was placed in a nursing
home in the city. Feeling overwhelmed, Alison made the deci-
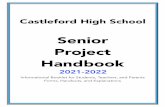
sion to sell the house and relocate to the city. See Figure 3 for a
graphical depiction of Alison’s cortisol peaks and troughs
mapped to major life events over the study period.
Pre-Move Major Life Events. Alison reported experiencing nine
significant life events (e.g., fall that resulted in a broken bone,
death of close friends, changes in her husband’s health and per-
sonality, declines in social activities) in the year preceding the
move. Alison’s sleep patterns were ‘‘awful’’ and had not been
good for several years. She reported waking an average of 12
times a night, with a typical night consisting of 4 hr of sleep.
She tried to take daily 1.5-hr naps. When she was alone, she did
not eat properly. Alison reported limitations with many daily
activities and had been unable to do certain tasks due to her
health and functional decline.
Pre-Move Perceptions and Cognitive and Behavioral Responses.Alison could not identify anything that provided her with
satisfaction in the year preceding the move. Alison’s own and
her husband’s health, coupled with financial concerns, were the
most stressful aspects of life in the year before the move. She
found distracting and solitary activities, such as reading and
watching television, somewhat effective in alleviating stress.
She reported that in the past, laughing or finding humor in a
situation had been one of her typical coping strategies, but it
was no longer effective.
Pre-Move Cortisol. Alison’s salivary cortisol peak level was
within normal range in the 1st month. The evening value was
significantly elevated, however, which indicates that the natu-
ral diurnal rhythm had shifted. Elevations in cortisol secretion
in the evening are often related to sleep disturbances in older
populations (Van Cauter, Leproult, & Kupfer, 1996) but are
also known to precede negative changes in health (Plat
et al., 1999).
Post-Move Life Events. At the time of the second interview, in her
3rd month in the assisted living facility, Alison reported better
dietary habits due to communal dining and an increase in phy-
sician visits due to an earache and surgery to remove a severely
0
5
10
15
20
25
30
35
Month 1 Month 4Month 3Month 2 Month 5 Month 6 Month 7
Moved to be nearer spouse in nursing home. Difficulties in sleeping.
Diet improved due to communal dining. New anti-anxiety meds. Teeth grinding is a problem.
Toe amputated.
Severe case of shingles. Sinus infection. Deaths of co-residents and friends. Husband’s condition worsened.
Diet and sleep poor. Depressed.
Saliv
ary
Cor
tisol
(nm
ol/L
)
Morning/Peak Evening/Nadir
Figure 3. Profile of allostatic processes: The case study of Alison. Figure illustrates peak and trough cortisol values over the study periodmapped to major life events. Though the study period was intended to be 6 months, severe health issues in Month 6 for Alison delayed thefinal interview, though she was able to complete cortisol collection for both Months 6 and 7. Sun and moon symbols represent the mean peakand evening values, respectively, for adult females over the age of 60 (Aardal & Holm, 1995; Edwards et al., 2001). Dashed lines above and belowthe mean peak and evening symbols show the 95% CIs for the peak and evening values.
Ewen and Kinney 7
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
arthritic toe. Her physician had doubled the dose of her antide-
pressant (Effexor) and prescribed Xanax to help her sleep. Both
medications affect cortisol secretion, typically decreasing
circulating levels (Hinkelmann et al., 2012; Hood et al., 2011).
Alison’s third interview, scheduled for Month 6, had to be
postponed several weeks due to her health. She had a sinus
infection and had developed a severe case of shingles that
affected both eyes and over half of her face. She was, however,
able to complete the saliva collection protocol for both Months
6 and 7, when the interview finally took place. Figure 3 thus
depicts 7 months of cortisol measures. At the time of her third
interview, in Month 7, Alison had finally managed to sleep
through a night. The shingles ‘‘laid her low’’ and her dietary
habits had returned to ‘‘awful.’’ Her husband’s physical and
mental health had declined significantly. He was discharged
to the nursing home with hospice care. She had experienced
numerous losses through death: a friend living in the nursing
home, her cat, three residents of the assisted living facility, and
a few of her childhood friends.
Post-Move Perceptions and Cognitive and Behavioral Responses. At
the second interview, Alison reported that the management and
facility staff were helpful in the week following her surgery,
stopping to check on her and delivering meals to her room. She
said that she mostly kept to herself. By the 7th month, she had
further withdrawn from the social community. Distinctly in the
throes of grief, she stated, ‘‘I lost him [husband] a long time
ago, I realize this now.’’
Post-Move Cortisol. Alison’s salivary cortisol peak levels were
within normal range in the 1st and 3rd months (see Figure 3).
In the 4th through 7th months, the peak cortisol levels vacil-
lated, with some values more than doubling and all of the val-
ues outside of the 95% CIs. Through this same time period the
evening values were within normal limits with the exception of
Month 6 when she was experiencing a shingles infection. It was
during these months that her husband’s health drastically
declined, her friends died, and she developed health complica-
tions. Cortisol dampens the immune system in order to prevent
excessive inflammation of bodily tissues (Yehuda & McEwen,
2004). As Alison’s salivary cortisol profile clearly indicates,
her cortisol levels were exceptionally high during a period that
coincided with the onset of a sinus infection and shingles.
Alison’s case study illustrates her body’s attempt to manage
stress to achieve homeostasis.
Allostatic Load: The Story of Edna
Edna was 80 years old when she relocated from her long-time
country home to senior housing. Edna’s husband had passed
away and her children had moved far from home. Afflicted
with degenerative polyneuropathy in her spine, Edna was
unable to sit, stand, or walk for long. Her granddaughter, who
provided instrumental support, had to relocate for a job, which
forced Edna to move. See Figure 4 for a graphical depiction of
Edna’s cortisol peaks and troughs mapped to major life events
over the 6-month study period.
Pre-Move Major Life Events. Edna reported experiencing 12 sig-
nificant life events in the year prior to the move, most
prominently serious health issues (e.g., blood clots and a pul-
monary embolism that resulted in lung damage). Due to the
serious nature of her health problems, she spent a few weeks
in the hospital and a rehabilitation nursing facility, followed
by 4 weeks residing with her daughters. By the time she moved
to the senior housing facility, she had experienced drastic
changes in living conditions and health behaviors. Edna
expressed a need for more sleep, reporting that she often
awakened at 4 a.m. and averaged 5 hr of sleep per night. She
found that daylight made it difficult for her to sleep, so she did
not take regular naps.
Pre-Move Perceptions and Cognitive and Behavioral Responses. In
the year preceding the move, Edna’s greatest stress was prepar-
ing for the move because she was unable to do so on her own.
‘‘I had hoped to live and die in my own bed in my own home. I
didn’t want to leave. This move nearly killed me.’’ Edna’s peak
and evening cortisol levels were below average and very close
to each other in value, indicating a flattened cortisol rhythm.
Given the nature and duration of the preceding life events and
her perceptions of them as stressful, a state of allostatic load
would be the likely result. In coping with stress, Edna reported
that her most effective strategies were prayer and reading, both
solitary activities.
Post-Move Life Events. At the time of the second interview, Edna
had developed pulmonary hypertension and had resumed
taking painkillers. The pain medications adversely affected her
breathing, which caused her speech to be broken into short sen-
tences. She had only been able to eat with other residents in the
dining room on two occasions. Residents, she reported, did not
socialize in each others’ apartments but only in the common
areas and dining room. Between the 3rd and 6th months, Edna
was hospitalized for pneumonia and was discharged with
oxygen. Within a few weeks, she was also been diagnosed with
congestive heart failure and a urinary tract infection.
Post-Move Perceptions and Cognitive and Behavioral Responses.Edna reported that she felt as though no one at the new facility
knew her. She said the lack of social contact was the greatest
stress for her. In her efforts to ‘‘mix and mingle,’’ she tended
to overdo it. She could not go to the dining room on a regular
basis and was not able to meet or make friends with the other
residents. Edna spent most of her days lying on her side on the
sofa. These perceptions remained consistent from the second to
the third interview. She was pleased with the services available
to her, including delivery of her medications from a nearby
pharmacy. Her sleep had worsened to the point that 5 hr of
sleep per night was a luxury due to constant pain and the
worsening of her respiratory illness. Her feelings of loneliness
8 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
and isolation were distressing and family members were not
visiting as often as they had when she had initially relocated.
Post-Move Cortisol. Edna’s peak salivary cortisol levels were
consistent across time; yet, they were below the mean and
95% CIs for a woman in her age range. The peak and evening
values were very close to each other across the study period,
reflecting a flattened rhythm that was particularly evident in
her cortisol samples for Month 4, during which time she was
hospitalized. This pattern is indicative of a nonresponsive
homeostatic mechanism and reflects the state of allostatic load.
Discussion
The ultimate goals of this study were to demonstrate the
complexity of stress perceptions and reactivity while testing the
utility of the model of allostasis for studying older women’s
adaptation to relocation, a transition that can be accompanied
by physical, emotional, and psychological upheaval. Reloca-
tion stress syndrome is a state in which physiological and/or
psychological disturbances occur as a result of a move from
one environment to another. Castle’s (2001) meta-analysis
identified potential negative outcomes of relocation including
mortality, morbidity, and psychological and social changes.
Castle’s work, however, did not include physiological
measures. Hence our research extends our understanding of the
negative health and social outcomes associated with relocation
to another domain.
Our study design, using longitudinal analysis to examine
physiological, psychological, and behavioral variables simulta-
neously, was ideal for studying the ways in which psychologi-
cal perceptions along with social opportunities and established
community affect outcomes of relocation. The psychosocial
data we derived from the interviews and journals provided
insight into the women’s motivations and challenges regarding
relocation, while the cortisol sampling illuminated their
physiological responses to these challenges.
In one significant finding about the relationship between
relocation and stress, the four women in the present study who
exhibited flattened diurnal salivary cortisol rhythms, an indica-
tor of allostatic load, all considered their recent move to be a
significant stressor. Although the number of cases is small, this
finding could partially explain earlier findings of relocation
stress syndrome and the increased mortality following
0
5
10
15
20
25
30
35
Month 6 Month 2 Month 3 Month 4 Month 5 Month 1
Relocation after long illness. Poor sleep; dependence on pain killers.
Christmas holiday. Feeling isolated. Ate dinner in dining hall for first time.
Hospitalized for pulmonary hypertension.
Preparing for holidays. Adjusting to size of apartment. Seekingcompanionship.
Discharged with congestive heart failurediagnosis. Began receiving oxygen at home.
Urinary tract infection.
Saliv
ary
Cor
tisol
(nm
ol/L
)
Evening/NadirMorning/Peak
Figure 4. Profile of allostatic load: The case study of Edna. Figure illustrates peak and trough cortisol values over the 6-month study periodmapped to major life events. Sun and moon symbols represent the mean peak and evening values, respectively, for adult females over the ageof 60 (Aardal & Holm, 1995; Edwards et al., 2001). Dashed lines above and below the mean peak and evening symbols show the 95% CIs for thepeak and evening values.
Ewen and Kinney 9
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
relocation. In fact, these women were exhibiting characteristics
of HPA-axis allostatic load, or exhaustion of the HPA-axis
feedback mechanism, at the time of the move. This finding
demonstrates the utility of using a physiological measure of
stress along with psychological and behavioral measures to
explore the effects of potential stressors, like relocation, in the
lives of older adults.
In applying the model of allostasis to this population and the
stressor of relocation, mortality and comorbidities would serve
as indicators of allostatic load. The three women we selected as
case exemplars of the processes related to the allostatic model,
in fact, all experienced health events over the study period,
including a broken bone, shingles, a series of infections, and
complications of chronic health conditions. None of the women
died within the period. Only Liz, the exemplar of homeostasis,
did not experience the onset or exacerbation of a systemic
illness, as her only experience with a health event was a broken
bone in Month 3. By mapping data from the journals and inter-
views to the cortisol data for these three cases, we were able to
illustrate that increased perceptions of stress were related to
incidents of acute illness. It would have been even more
informative if we could have followed the women for a full
year, as did the studies that Castle analyzed (2001), yet even
in our 6-month study period, the sequelae of comorbid health
conditions were evident in the cases representing allostasis and
allostatic load.
The three cases in our study also provide a clear example of
the relationship between perceived social support and ability to
adjust. Although all three women reported making some friend-
ships within the facility, each approached them differently: Liz,
our exemplar of homeostasis, integrated herself into the extant
structure and received satisfaction from her relationships;
Alison, our exemplar of allostasis, found her friendships to
be a source of both support and stress; and Edna, our exemplar
of allostatic load, was unable to use her potential relationships
to create a support structure of any kind. Regardless of the
differences among the ways in which they approached these
relationships, social interaction and connectedness was an
important and common theme for all three women. It is
interesting to note the divergence between our homeostatic
exemplar on one hand and our allostatic and allostatic load
exemplars on the other in regard to social connectedness: the
two women who were socially isolated and experienced little
or no social support in their new surroundings also suffered
multiple health maladies and demonstrated salivary cortisol
patterns indicative of increased stress. Loss of personal and
social resources may be one explanation as to why older adults
appear to be more vulnerable to the negative effects of stress
(Cairney & Krause, 2008).
Limitations
Consistent with many prior studies on relocation and adapta-
tion, our sample size was small and we lacked a control group
(Castle, 2001). Therefore, we used the primary data collection
as our baseline measure, which left the data right-censored.
While the small sample size could be viewed as a limitation,
it also allowed us to collect detailed, in-depth data across
psychosocial and physiological domains.
A consistent problem noted in the cortisol literature is
assuring that samples are collected at the predetermined times
(Kudielka, Broderick, & Kirschbaum, 2003). Our participants
recorded the times of awakening and sample collections in their
journals. Although we had labeled each vial with a specific col-
lection time, it is possible that participants were not compliant
with the predetermined sampling schedule and/or in using the
appropriate vial. The aberrant profiles in Figure 1C may be
indicative of such a data collection error. Use of a time-
stamped collection protocol is recommended, but it is quite
expensive and was not feasible for this study. Edwards, Clow,
Evans, and Hucklebridge (2001) found that single-sample
measurement of cortisol was reliable when the sampling was
synchronized to awakening, which was our aim. However,
saliva sampling only occurred on 1 day per month, which may
not be optimal for accuracy of the diurnal curve.
Implications for Nursing and Nursing Research
In discussing the difficulty of determining the degree of
relationship between ‘‘stress’’ and ‘‘illness,’’ McEwen (1998)
asserted that the concept of stress is subjective and does not
take into account the enormous individual differences that exist
in coping with the environment. In this study, we explored how
these individual differences might affect older adult women’s
ability to adapt to the stressful life event of relocation. We used
a case study approach to describe exemplars of the primary
states described by the model of allostasis: homeostasis, allos-
tasis, and allostatic load. The longitudinal design and in-depth
data collection methods allowed for mapping of life events,
individual perceptions and coping abilities, and health impacts
directly onto the cortisol graphs, affording a unique perspective
on the role that the interactions among stress, perception, and
coping play in adaptation and health. This approach provided
insight into the transition and acclimation processes that occur
when older women move into a senior housing community,
illustrated the complex interplay among the physiological and
psychosocial components of the model of allostasis, and illumi-
nated aspects of the allostatic processes that prior research on
relocation did not explore. Our results provide support for the
application of the model of allostasis to significant events
requiring changes in behavior, lifestyle, and environment in
later life. Our study also provides preliminary evidence sup-
porting the acceptability and feasibility of collecting salivary
samples for cortisol analysis during significant life events in
this population.
Kirst and Peck (2010) lament the paucity of literature on
contextual interventions based upon population characteristics
and best practices with regard to relocation issues among older
adults. Although relocation to a new residence is, itself, stress-
ful, the adaptation and acclimation period may introduce or
exacerbate stresses associated with relocating. One of the most
exciting potential applications of the present study involves the
10 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
demonstrated ability to observe physiological reactivity to self-
reported stresses and coping abilities. Nurses, mental health
specialists, physicians, and researchers are likely to find this
method of combining self-reported stress and cortisol measures
useful in developing and implementing interventions for
helping older adults adapt to a new residence.
For instance, all three women in our case studies acknowl-
edged the importance of social connections to their well-
being; yet, they grappled to differing degrees with unwritten
social rules for resident conduct among the already-
established social cliques in the facilities to which they had
moved. Previous research has shown that social support offsets
the ill effects of stress (Krause, 2006; Shaw, Krause, Liang, &
Bennett, 2007), and social comparisons offer one interpretive
mechanism for understanding how individuals evaluate
themselves during times of stress (Ryff & Singer, 2008). The
cortisol profiles in our three case studies demonstrate that the
woman who was most successful in establishing social support
in her new residence was also able to maintain physiological
homeostasis. Further exploration of social belonging and sup-
port in a larger sample may lead to the development of inter-
ventions and policies for prospective and new residents of
senior housing communities. Such interventions might include
invitations for prospective residents to attend social events and
meals during which they can observe interpersonal dynamics,
cliques, and staff–resident interactions. New residents could
be paired with established residents for social introductions and
daily check-ins.
Future research on relocation outcomes would benefit from
using the methods we describe here: a longitudinal design
involving the triangulation of self-report, psychosocial, and
physiological measures. Optimally, data collection beginning
with potential participants on the housing waitlist would pro-
vide a better method for ascertaining the baseline physiological
measures as well as for indentifying the social and lifestyle
changes that naturally occur when moving into congregate
housing. This would also afford an opportunity for developing
a control group of peers who are considering a move yet are
currently aging in place within the community.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to
the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the
research, authorship and/or publication of this article: This research
was supported by National Institutes of Health (NIH) grant no. M01
RR02602 through the General Clinical Research Center at the Univer-
sity of Kentucky.
References
Aardal, E., & Holm, A. C. (1995). Cortisol in saliva—Reference
ranges and relation to cortisol in serum. European Journal of
Clinical Chemistry and Clinical Biochemistry, 33, 927–932.
Aldwin, C. M., & Werner, E. E. (2007). Stress, coping, and develop-
ment: An integrative perspective (2nd ed.). New York, NY:
Guilford.
Cain, A. E., Depp, C. A., & Jeste, D. (2009). Ecological momentary
assessment in aging research: A critical review. Journal of
Happiness Studies, 4, 35–52. doi: 10.1023/A:1023657221954
Cairney, J., & Krause, N. (2008). Negative life events and age-related
decline in mastery: Are older adults more vulnerable to the control-
eroding effects of stress? Journals of Gerontology: Series B:
Psychological Sciences and Social Sciences, 63, S162–S170.
Castle, N. (2001). Relocation of the elderly. Medical Care Research
and Review, 58, 291–333.
Clayton, A. M., & Thorne, T. (2000). Diary data enhancing
rigour: Analysis framework and verification tool. Journal of
Advanced Nursing, 32, 1514–1521. doi:10.1046/j.1365-2648.
2000.01609.x
Cohen, S., & Williamson, G. (1988). Perceived stress in a probability
sample of the U.S. In S. Spacapam & S. Oskamp (Eds.), The social
psychology of health: Claremont symposium on applied social psy-
chology (pp. 31–67). Newbury Park, CA: Sage.
Davis, P., Morris, J., & Grant, E. (1990). Brief screening tests versus
clinical staging in senile dementia of the Alzheimer type. Journal
of the American Geriatrics Society, 38, 129–135.
Deuschle, M., Gotthardt, U., Schweiger, U., Weber, B., Korner, A.,
Schmider, J., . . . Heuser, I. (1997). With aging in humans the
activity of the hypothalamus-pituitary-adrenal system increases
and its diurnal amplitude flattens. Life Science, 61, 2239–2246.
Edwards, S., Clow, A., Evans, P., & Hucklebridge, F. (2001). Explo-
ration of the awakening cortisol response in relation to diurnal cor-
tisol secretory activity. Life Sciences, 68, 2093–2103.
Eskin, M., & Parr, D. (1996). Introducing a Swedish version of an
instrument measuring mental stress (Reports from the Department
of Psychology, no. 813). Stockholm, Sweden: Stockholm
University.
Hinkelmann, K., Moritz, S., Botzenhardt, J., Muhtz, C., Wiedemann,
K., Kellner, M., & Otte, C. (2012). Changes in cortisol secretion
during antidepressive treatment and cognitive improvement in
patients with major depression: A longitudinal study. Psychoneur-
oendocrinology, 37, 685–692.
Hood, S. D., Melichar, J. K., Taylor, L. G., Kalk, N., Edwards, T. R.,
Hince, D. A., . . . Nutt, D. J., (2011). Noradrenergic function in
generalized anxiety disorder: Impact of treatment with venlafaxine
on the physiological and psychological responses to clonidine
challenge. Journal of Psychopharmacology, 25, 78–86.
Jacelon, C. S., & Imperio, K. (2005). Participant diaries as a source of
data in research with older adults. Qualitative Health Research, 15,
991–997. doi:10.1177/1049732305278603
Juster, R. P., McEwen, B. S., & Lupien, S. J. (2010). Allostatic load
biomarkers of chronic stress and impact on health and cognition.
Neuroscience and Biobehavioral Reviews, 35, 2–16.
Karlamangla, A. S., Singer, B. H., McEwen, B. S., Rowe, J. W., &
Seeman, T. E. (2002). Allostatic load as a predictor of functional
decline. Journal of Clinical Epidemiology, 55, 696–710.
Kirst, J., & Peck, S. (2010). Older adult relocation: Considerations for
nurse practitioners. The Journal for Nurse Practitioners, 6(3):206–
211.
Ewen and Kinney 11
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from
Krause, N. (1999). Assessing change in social support during late life.
Research on Aging, 21, 539–569.
Krause, N. (2006). Exploring the stress-buffering effects of church-
based and secular social support on self-rated health in late life.
Journals of Gerontology Series B Psychological Sciences and
Social Sciences, 61, S35–S43.
Krout, J. A., Moen, P., Holmes, H. H., Oggins, J., & Bowen, N. (2002).
Reasons for relocation to a continuing care retirement community.
Journal of Applied Gerontology, 21, 236–256.
Krout, J. A., & Wethington, E. (2003). Residential choices and experi-
ences of older adults: Pathways to life quality. New York, NY:
Springer.
Kudielka, B. M., Broderick, J. E., & Kirschbaum, C. (2003).
Compliance with saliva sampling protocols: Electronic monitoring
reveals invalid cortisol daytime profiles in noncompliant subjects.
Psychosomatic Medicine, 65, 313–319.
Kumari, M., Badrick, E., Sacker, A., Kirschbaum, C., Marmot, M., &
Chandola, T. (2010). Identifying patterns in cortisol secretion in an
older population. Findings from the Whitehall II Study.
Psychoneuroendocrinology, 35, 1091–1099.
Lantz, P. M., House, J. S., Mero, R. P., & Williams, D. R. (2005).
Stress, life events, and socioeconomic disparities in health: Results
from the Americans’ Changing Lives study. Journal of Health and
Social Behavior, 46, 274–288.
Mallick, M. J., & Whipple, T. W. (2000). Validity of the nursing
diagnosis of relocation stress syndrome. Nursing Research, 49,
97–100.
McDowell, I., & Newell, C. (1996). Measuring health: A guide to rat-
ing scales and questionnaires (2nd ed.). New York, NY: Oxford
University Press.
McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and
allostatic load. Annals of the New York Academy of Sciences, 840,
33–44.
McEwen, B. S. (2000). Allostasis and allostatic load: Implications for
neuropsychopharmacology. Neuropsychopharmacology, 22,
108–124.
McEwen, B. S. (2002). Sex, stress and the hippocampus: Allostasis,
allostatic load and the aging process. Neurobiology of Aging, 23,
921–939.
McEwen, B. S. (2003). Interacting mediators of allostasis and
allostatic load: Towards an understanding of resilience in aging.
Metabolism, 52, 10–16.
Mroczek, D. K., & Almeida, D. (2004). The effect of daily stress, per-
sonality, and age on daily negative affect. Journal of Personality,
72, 355–378.
Otte, C., Hart, S., Nevlan, T. C., Marmar, C. R., Yaffe, K., & Mohr, D. C.
(2005). A meta-analysis of cortisol response to challenge in human
aging: Importance of gender. Psychoneuroendocrinology, 30, 80–91.
Plat, L., Leproult, R., L’Hermite-Baleriaux, M., Fery, F., Mockel, J.,
Polonsky, K. S., & Van Cauter, E. (1999). Metabolic effects of
short-term elevations of plasma cortisol are more pronounced in
the evening than in the morning. Journal of Clinical Endocrinol-
ogy & Metabolism, 84, 3082–3092.
Rahe, R. H., Rubin, R. T., & Arthur, R. J. (1974). The three investiga-
tors study: Serum uric acid, cholesterol, and cortisol variability
during stresses of everyday life. Psychosomatic Medicine, 36,
258–268.
Ryff, C., & Singer, B. (2008). Know thyself and become what you are:
A Eudaimonic approach to psychological well-being. Journal of
Happiness Studies, 9, 13–39. doi:10.1007/s10902-006-9019-0
Schulkin, J. (2001). Allostasis, homeostasis, and the costs of biologi-
cal adaptation. Oxford, England: Cambridge University Press.
Schulkin, J. (2003). Allostasis: A neural behavioral perspective.
Hormones and Behavior, 43, 21.
Seeman, T., McEwen, B., Rowe, J., & Singer, B. (2001). Allostatic
load as a marker of cumulative biological risk: MacArthur studies
of successful aging. Proceedings of the National Academy of
Sciences, 98, 4770–4775.
Seeman, T., Singer, B., Rowe, J., & McEwen, B. (2001). Exploring
a new concept of cumulative biological risk—Allostatic load
and its health consequences; MacArthur Studies of Successful
Aging. Proceedings of the National Academy of Science, 98,
4770–4775.
Sephton, S., Sapolsky, R., Kraemer, H., & Spiegel, D. (2000). Diurnal
cortisol rhythm as a predictor of breast cancer survival. Journal of
the National Cancer Institute, 92, 994–1000. doi:10.1093/jnci/92.
12.994
Shaw, B. A., Krause, N., Liang, J., & Bennett, J. (2007). Tracking
changes in social relations throughout late life. Journals of Geron-
tology Series B Psychological Science Social Sciences 62,
S90–S99.
Smyth, J. M., & Stone, A. A. (2003). Ecological momentary
assessment research in behavioral medicine. Journal of Happiness
Studies, 4, 35–52.
Stalder, T., Evans, P., Hucklebridge, F., & Clow, A. (2010). Associa-
tions between psychosocial state variables and the cortisol awaken-
ing response in a single case study. Psychoneuroendocrinology,
35, 209–214.
Sterling, P., & Eyer, J. (1988). Allostasis: A new paradigm to explain
arousal pathology. In S. Fisher & J. Reason (Eds.), Handbook of
life stress, cognition and health (pp. 629–649). New York, NY:
John Wiley.
Van Cauter, E., Leproult, R., & Kupfer, D. J. (1996). Effects of gender
and age on the levels and circadian rhythmicity of plasma cortisol.
Journal of Clinical Endocrinology and Metabolism, 81,
2468–2473.
Vincennati, V., Pasqui, F., Cavazza, C., Pagotto, U., & Pasquali, R.
(2009). Stress-related development of obesity and cortisol in
women. Obesity, 17, 1678–1683.
Walker, C. A., Curry, L. C., & Hogstel, M. O. (2007). Relocation
stress syndrome in older adults transitioning from home to a
long-term care facility: Myth or reality? Journal of Psychosocial
Nursing and Mental Health Services, 45, 1–9.
Wrosch, C., Miller, G. E., Lupien, S., & Pruessner, J. C. (2008). Diur-
nal cortisol secretion and 2-year changes in older adults’ physical
symptoms: The moderating roles of negative affect and sleep.
Health Psychology, 27, 685–693.
Yehuda, R., & McEwen, B. S. (2004). Biobehavioral stress response:
Protective and damaging effects. New York: New York Academy
of Sciences.
12 Biological Research for Nursing 00(0)
at OhioLink on February 1, 2013brn.sagepub.comDownloaded from