The Antecedents of online customer satisfaction and customer ...
Antecedents to cardiac arrests in a teaching hospital intensive care unit
Transcript of Antecedents to cardiac arrests in a teaching hospital intensive care unit
C
Ac
TSa
b
a
ARRA
KAEICAC
1
aCoa
dl
i
H
0h
Resuscitation 85 (2014) 411–417
Contents lists available at ScienceDirect
Resuscitation
j ourna l h o me pa g e : www.elsev ier .com/ locate / resusc i ta t ion
linical Paper
ntecedents to cardiac arrests in a teaching hospital intensiveare unit�
homas H. Rozena,∗, Siobhan Mullaneb, Melissa Kaufmanb, Yu-Feng Frank Hsiaob,tephen Warrillowb, Rinaldo Bellomob, Daryl A. Jonesb
Alfred Hospital, Commercial Road, Melbourne, AustraliaAustin Hospital, Australia
r t i c l e i n f o
rticle history:eceived 26 July 2013eceived in revised form 7 November 2013ccepted 16 November 2013
eywords:ntecedentspidemiologyntensive careardiac arrestdvanced life support (ALS)ardiopulmonary resuscitation (CPR)
a b s t r a c t
Background: In hospital cardiac arrests (CA) treated with cardio-pulmonary resuscitation (CPR) outsideof the intensive care unit (ICU) have poor outcomes. Most are preceded by deranged vital signs. Thereare, however, limited studies assessing antecedents to CAs inside the ICU.Objectives: To study the antecedents to, and characteristics of CAs in ICU.Study population: We prospectively identified CA cases that occurred inside our ICU between January2010 and July 2012. Controls were obtained by sequentially matching ICU patients based on APACHE IIIdiagnosis, APACHE III score, age, gender and length of stay in ICU.Results: Thirty-six patients had a CA during the study period (6.28/1000 admissions). In the 12 h priorto CA, index patients had higher maximum (22 breaths/min vs. 18 breaths/min, p = 0.001) and minimumrespiratory rates (16 breaths/min vs. 12 breaths/min, p = 0.031), a lower median mean arterial pressure(65 mmHg vs. 70 mmHg, p = 0.029) and systolic blood pressure (97 mmHg vs. 106 mmHg, p = 0.033), ahigher central venous pressure (14 cm H2O vs. 11 cm H2O, p = 0.008) and a lower bicarbonate level(20.5 mmol vs. 26 mmol, p = 0.018) compared to controls. CA patients also had a higher maximum dose ofnoradrenaline (norepinephrine) (17.5 mcg/min vs. 8.0 mcg/min, p = 0.052) but there was no difference inany other levels of intensive care support. Two-thirds of CA’s occurred within the first 48 h of ICU admis-
sion. The initial monitored rhythm was non-shock responsive (pulseless electrical activity, bradycardiaor asystole) in 26/36 (72%). Return of spontaneous circulation was achieved in 29/36 (80.6%) patients,with 16/36 (44.4%) surviving to hospital discharge.Conclusions: In the period leading up to the CA inside ICU, there were signs of physiological instabilityand the need for higher doses of noradrenaline. Return of spontaneous circulation was achieved in 80%.However, in-hospital mortality was greater than 50%.. Introduction
In-hospital ward cardiac arrests (CA) that receive CPR are associ-ted with an in-hospital mortality of approximately 80%.1 In thoseAs that occur on general hospital wards (floors), a high proportionf patients have warnings,1 such as derangements in vital signs2
nd may occur despite medical review.3
Patients inside ICU often have severe acute diseases with organysfunction superimposed upon variable degrees of chronic under-
ying ill health. Despite invasive physiological supports in a highly
� A Spanish translated version of the summary of this article appears as Appendixn the final online version at http://dx.doi.org/10.1016/j.resuscitation.2013.11.018.∗ Corresponding author at: c/o: Intensive Care Unit, Austin Hospital, Studley Road,eidelberg, Victoria 3084, Australia.
E-mail address: [email protected] (T.H. Rozen).
300-9572/$ – see front matter © 2013 Elsevier Ireland Ltd. All rights reserved.ttp://dx.doi.org/10.1016/j.resuscitation.2013.11.018
© 2013 Elsevier Ireland Ltd. All rights reserved.
monitored area, such patients occasionally suffer CA’s,4 which areassociated with an in-hospital mortality of 52–100%4–16 despite ashort time to resuscitation.17–19
There is a considerable literature examining the antecedentsto CA’s occurring in general hospital wards. However, there isless literature on the epidemiology of CA’s in the ICU, particu-larly regarding the presence of instability leading up to the arrest.Patients in ICU are continuously monitored, and thus derangementsin vital signs may be detected earlier than in hospital wards. In addi-tion, ICU patients receive invasive organ support, which can modifyand reverse derangements in vital signs. Thus, derangements invital signs may not reliably warn of impending cardiac arrest in theICU. Instead, escalation of levels of support may be a more reliable
marker of clinical deterioration in such patients.We conducted a retrospective case–control study to assess thecharacteristics and outcomes of patients who suffered a CA in theICU of a tertiary hospital. Specifically, we assessed the 12 h period
4 scitati
lcwpm
2
2
rn
2
rb
2
a2cTdaccs
2
iiaamfiWt
sIaAoCpw
2
tA
2
li
12 T.H. Rozen et al. / Resu
eading up to CA for the presence of physiological instability andhanges in the level of ICU therapeutic support and compared thisith a matched control group. We also assessed the proportion ofatients who suffered a CA, and examined their timing, features,anagement and outcome.
. Methods
.1. Ethics
Ethics approval for this study was obtained from the hospitalesearch and ethics committee (Ethics number: H2012/04698). Theeed for patient consent was waived by the HREC.
.2. Study design
We conducted a retrospective case–control study of CA occur-ing in patients inside the intensive care unit of a teaching hospitaletween January 2010 and July 2012.
.3. Study setting
The Austin Hospital is a tertiary referral centre, which haspproximately 33,000 multi-day admissions per year. The ICU has0 beds, admits 2300 adult patients per year, and operates as alosed ICU where only ICU medical staff can prescribe therapy.he ICU treats both medical and surgical patients including car-iac and neuro-surgical patients and is a state referral centre forcute spinal care, liver transplantation, complex epilepsy, obstetricritical care, respiratory weaning and aortic vascular surgery. Allritical care therapies are available, including advanced circulatoryupports such as extracorporeal membrane oxygenation.
.4. Study population and inclusion criteria
Between January 2010 and July 2012, index cases were includedf they received CPR in the intensive care unit and had no lim-tation of medical therapy in place. Cardiac arrest was defineds cessation of cardiac mechanical activity as confirmed by thebsence of signs of circulation sufficient to necessitate the com-encement of external cardiac massage.11 We included only the
rst arrest for the single patient who had more than one event.e excluded all patients with documented limitations of medical
herapy.We obtained controls from the ICU patient database. We
equentially matched CA patients with controls using consecutiveCU admissions. Controls were selected as matches using their ICUdmission diagnosis (APACHE III diagnosis) first, followed by theirPACHE III score (±5), age (within same decile), gender and lengthf stay in ICU. One case could not be matched with a control as theA occurred en route to the ICU during a transfer from another hos-ital, and no pre-arrest physiological data or APACHE informationas available.
.5. Data sources and data capture
Data were obtained from the hospital clinical information sys-em database, the patient’s scanned medical record, and the ICUNZICS-AORTIC database.
.6. Participants
CA patients were identified from a prospectively maintainedist of patients who received cardio-pulmonary resuscitation (CPR)n the intensive care unit. This list was derived from routine shift
on 85 (2014) 411–417
reports, which documents daily unit activity and was completedby the nurse in charge at the conclusion of each ICU nurse shift.
We used standardised case report forms to collect data fromthe hospital electronic and the patients’ files. Data was manuallyentered into an Excel spreadsheet by two investigators who workedtogether to minimise data entry error.
2.7. Data collected
For each CA, data in three major categories were collected. First,we collected demographic data about each patient, including theadmission source, reason for admission and comorbidities. In addi-tion, we assessed the patient’s charts the 12 h before the cardiacarrest to assess the patient’s vital signs and level of intensive caresupports. Finally, we documented data about each cardiac arrest,including the initial rhythm of the arrest, the interventions, and theshort and long-term outcomes.
Once controls were identified, we assessed the Scanned MedicalRecord (SMR) to find the same day of admission, and the same timeinterval of the day (i.e. in the 12 h period prior to the arrest thatoccurred in the corresponding case) to collect data on physiologicalderangements and intensive care supports, as well as the outcomeof the hospital admission.
We collected data on pre-existing co-morbidities includ-ing ischaemic heart disease, congestive cardiac failure, dialysisdependence, home oxygen use, chronic obstructive pulmonarydisease (COPD), pulmonary fibrosis, obstructive sleep apnoea(OSA), long term non-invasive ventilation, neuromuscular disor-ders, spinal injuries, dementia, cirrhosis and chronic liver disease,diabetes, obesity and malignancy.
We recorded the worst values for electrolytes and arterial bloodgas, including serum lactate, derangements in potassium and cre-atinine in the 12 h prior the timing of the CA. We also collected dataon the extremes of vital signs for hypoxaemia (SpO2%), respiratoryrate and minute ventilation (L/min), blood pressure (mean arterialblood pressure [MAP] in mmHg and systolic blood pressure [SBP]in mmHg), heart rate (bpm) and urine output (mL in 4 h). We alsodocumented the presence and value of the lowest and highest cen-tral venous pressure (CVP) in the 12 h period prior to the timingof the arrest, as well as the CVP within 6 h after the timing of thearrest.
We analysed changes in Intensive Care supports prior to CA(particularly the highest value and the maximum change in prior12 h) including: (1) vasopressor or inotropic drug dose: we col-lected detailed information on vasoactive medication – what agentspatients were on, whether it was newly commenced in the prior12 h, the maximal dose and a change in the dose (looking at themaximum and minimum in a 12 h period), (2) requirements forinvasive and non-invasive respiratory support, (3) renal replace-ment therapy (RRT) in the 24 h preceding, and (4) pre-arrest“sentinel events” including airway manipulation, sedation in anon-intubated patient, bleeding, immediate complications of a pro-cedure, pericardial tamponade and documented delirium.
Finally, we recorded the outcomes of patients who had an arrestin the ICU: the time to return of spontaneous circulation (ROSC),death within 24 h and in ICU, in-hospital death and the timing (incalendar days) between the arrest and death, and discharge desti-nation and survival status.
The primary outcomes of our study were (1) the proportionof patients achieving return of spontaneous circulation, and thetiming of this, and (2) the proportion of patients who survived
to hospital discharge. In addition, we assessed differences in theseverity of derangement of vital signs, ICU supports, or laboratoryresults in the 12 h prior to the arrest, as well as predictors of CAamongst these variables.T.H. Rozen et al. / Resuscitation 85 (2014) 411–417 413
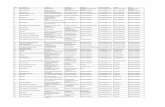
Table 1comparison of baseline characteristics of patients with CA with controls.
Cardiac arrests Controls p-Value
Number of patients 36 35Age: median (IQR) 67 (52.5–75.0) 65 (57.0–77.0) 0.87Gender male: number (%) 21 (58.3) 22 (62.9) 0.70ICU admission APACHE III 59(14–78) 54(14–71) 0.589Admission source: n (%)
Cardiac catheter lab 1 (2.8) 2 (5.7)
0.35Emergency Department 14 (38.9) 13 (37.1)Other hospital 9 (25.0) 3 (8.6)Theatre 6 (16.7) 10 (28.6)Ward 6 (16.7) 7 (20.0)
Emergency admission: n (%) 29 (80.6) 28 (80.0) 0.953Parent unit
Medical 20 (55.6) 20 (57.1)0.571Surgical 16 (44.4) 14 (40.0)
Other 0 1 (2.9)Place of residence
Home 34 340.611Nursing home 1 0
Supported accommodation 1 1Co-morbidity
Any: n (%) 29 (80.6) 23 (65.7) 0.16Number: median (IQR) 1.5 (1.0–3.0) 1.0 (0–2.0) 0.066
Days between ICU and hospital admission 0(0–1) 0(0–3) 0.30
2
buvrsMptsswtafDa
3
ti(d
3
iaywaT
Median (IQR)
.8. Statistical analysis
A data analysis plan was prospectively established and ratifiedy the investigators prior to analysis. Descriptive statistics weresed to describe overall cases (n) and proportions (%). Continuousariables were found to be skewed (non-Gaussian) and are thuseported as median and interquartile range [IQR]. Inferentialtatistics comparing continuous data was conducted using theann–Whitney U test, and comparison of categorical data and
roportions was conducted using the chi-sq. test. In all statisticalests, a two sided p-value of <0.05 was taken to indicate statisticalignificance. After conducting uni-variable analysis, we selectedignificant parameters to identify predictors of cardiac arrestithin the cohort. We used recursive partitioning to identify
he combination of significant univariate factors which mostccurately predicted a cardiac arrest. Various cut-off were chosenor each significant variable to optimise sensitivity and specificity.iagnostic sensitivity, specificity, PPV and NPV were calculatednd are presented as percentages.
. Results
There were 4814 patients admitted to the ICU a total of 5732imes during the study period. There were 316 deaths, giving ann-ICU mortality rate of 6.56% (316/4814). Of the 316 deaths, 29994.4%) had a “do not resuscitate [DNR]” designation at the time ofeath.
.1. Demographics of cases and controls
Between January 2010 and July 2012, 36 ICU patients fulfillednclusion criteria by receiving CPR for CA (CA arrest rate 6.28/1000dmissions). The median (IQR) age of all patients was 67 (52.5–75
ears), with 58.3% being male. The median (IQR) APACHE III scoreas 59 (14–78). Twenty-nine patients (80.6%) were emergencydmissions and 20 (55.6%) were admitted under a medical unit.he controls were well matched (Table 1).
3.2. Derangements in physiology prior to arrest
There were several differences in the presence of physiologicalderangement in CA patients compared with controls (Table 2). Thus,CA patients had a higher median maximum and minimum respira-tory rate, a lower median MAP, a lower systolic blood pressure and alower bicarbonate level in the 12 h prior to the event. Furthermore,a quarter of patients suffering cardiac arrest had a respiratory rateof more than 34 breaths/min and/or heart rate more than 130 bpm,a MAP lower than 56 mmHg, and a systolic blood pressure of lessthan 80 mmHg in the 12 hours prior to the arrest. The CVP wasconsistently higher in cases than controls (Table 2), but there wasno difference in the lowest oxygen saturation (p = 0.26), highestheart rate (p = 0.07), highest serum lactate level (p = 0.21), low-est pH (p = 0.46), highest potassium (p = 0.16), lowest potassium(p = 0.186), urine output (p = 0.393) or highest creatinine (p = 0.60).
3.3. Changes in intensive care support prior to arrest
CA patients had a higher maximum dose of noradrenaline(norepinephrine) (17.5 mcg/min vs. 8.0 mcg/min, p = 0.052), butthere was no difference in the proportion of patients with endo-tracheal intubation (p = 0.38), mechanical ventilation (p = 0.55),renal replacement therapy (p = 0.82) or vaso-active medications(p = 0.56). The total number of these supports was also similar(p = 0.43). There was no statistically significant difference in anynewly started therapies in the prior 12 h (data not shown). Addi-tionally, there was no statistically significant difference in theproportion of patients who were on vaso-active drugs, or on eachspecific agent or in variations in the dose in the preceding 12 h.
3.4. Peri-arrest sentinel events
There was no difference in the incidence of airway manipula-tion (p = 0.12), administration of sedation in non-intubated patients(p = 0.49), bleeding (p = 0.36), delirium (p = 0.49), immediate com-
plications of a procedure (p = 0.20) or presence of pericardialtamponade (p = 0.61). However, when all of these sentinel eventswere combined, there was a trend towards higher incidence inthose who had a CA (18/36 vs. 10/35, p = 0.07).414 T.H. Rozen et al. / Resuscitation 85 (2014) 411–417
Table 2Antecedents to cardiac arrests in the ICU.
Variable (in 12 h before arrest) Missing data (controls/arrests) Controls Arrests p-Value
Physiological derangementLowest respiratory rate (breaths/min) 0/1 12 (10–16) 16 (12–20) 0.031Highest respiratory rate (breaths/min) 0/1 18 (14–20) 22 (19–34) 0.001Lowest MAP (mmHg) 0/5 70 (65–80) 65 (56–70) 0.029Lowest SBP (mmHg) 0/1 106 (90–115) 97 (80–106) 0.033Highest HR (bpm) 0/1 100 (85–110) 110 (90–130) 0.068Lowest HCO3 (mmol/L) 1/2 26.0 (20–28.6) 20.5 (17.7–26) 0.018Highest HCO3 (mmol/L) 1/2 28.0 (22.7–30) 23.5 (23–30) 0.055
Level of supportOn adrenaline n/N (%) 7/19 (36.8) 6/21 (28.6) 0.58On noradrenaline n/N (%) 16/19 (84.2) 18/21 (85.7) 0.89On milrinone n/N (%) 5/19 (26.3) 2/21 (9.5%) 0.13On vasopressin n/N (%) 0/19 (0) 1/21 (4.8) 0.34Maximum dose noradrenaline (mcg/min) 8.0 (5.0–10.0) 17.5 (5.0–24.3) 0.052
Details of CVP* measurement in entire cohortLowest CVP (mmHg) in 12 h pre-arrest 12/9 8.0 (7.0–8.0) 9.0 (8.0–13.5) 0.013Highest CVP (mmHg) in 12 h pre-arrest 12/9 11.0 (9.0–12.0) 14.0 (11.0–17.5) 0.008
Details of CVP measurement in patients on vasoactive medications
3
oa2d
avsmp
(s(opl(
3
(b9t
o5s2frto
3
ci
Lowest CVP (mmHg) in 12 h pre-arrest 5/2
Highest CVP (mmHg) in 12 h pre-arrest 5/2
* CVP, central venous pressure.
.5. Timing of cardiac arrests
The timing of CAs was not uniform. Two-thirds of arrestsccurred within less than 48 h of admission (ten on the day ofdmission to ICU, twelve on day 1 post admission, nine on days–7 and five after day 7). However, CA’s occurred at all times ofay, and days of week (Fig. 1).
Compared with those who had an early CA, patients who had CA after 48 h of admission were more likely to be on RRT (100%s. 4.8%, p = 0.001), with a trend for higher median [IQR] APACHEcore ((107.0 [63.5–139.5] vs. 79 [66.0–89.0]); p = 0.096) and loweraximum heart rate ((100.0 [88.8–114.0] vs. 130 [92.5–137.5]),
= 0.061).In contrast, there was no difference in gender distribution
p = 0.91), age (p = 0.96), admission source (p = 0.51), elective admis-ion status (p = 0.27), intubation status (p = 0.47), initial rhythmp = 0.88), highest respiratory rate (p = 0.93), lowest MAP (p = 0.83),r highest PEEP (p = 0.26). Finally, the in-hospital mortality ofatients who suffered a CA after 48 h (8/14 [57.1%]) was simi-
ar to that of patients who suffered an early CA (12/22 [54.5%])p = 0.88).
.6. Details of initial rhythm and therapies
Most (26/36 [72%]) initial rhythms were non-shockable, 14/3638.9%) were pulseless electrical activity (PEA), 8/36 (22%) severeradycardia and 4/36 (11.1%) asystole. Of the shockable rhythms,/36 (25%) were ventricular tachycardia (VT) and 1/36 (2.8%) ven-ricular fibrillation (VF).
Amongst therapies administered during the CA, 30/36 (83.3%)f patients had adrenaline boluses, 10/36 (27.8%) had DC-shock,/36 (13.9%) received an amiodarone bolus, 5/36 (13.9%) receivedodium bicarbonate and 17/36 (47.22%) had atropine. Additionally,/36 (5.6%) of patients subsequently received pericardiocentesisor pericardial tamponade. The two cases of CA with shockablehythms that did not receive DC-shock both had VT that revertedo a perfusing, non-shockable rhythm in less than 30 s of initiationf CPR.
.7. Patient outcomes
In 29/36 (80.6%) patients sustained return of spontaneous cir-ulation (ROSC) was achieved and the median (IQR) time to ROSCn these patients was 4 (2–8) min.
8.0 (7.0–8.5) 9.0 (8.0–14.0) 0.03711.5 (10.0–13.0) 14.0 (13.0–18.0) 0.021
Overall, 12/36 (33.3%) patients died within 24 h of the arrest,5/36 (13.9%) died in ICU more than 24 h post arrest and 3/36 (8.3%)died in hospital after ICU discharge. Thus, 16/36 (44.4%) patientswere discharged from hospital alive. Overall, 6/36 (16.6%) weredischarged directly home and 10/36 (27.8%) were discharged toanother hospital/rehabilitation facility.
There were no differences between survivors to non-survivorsat hospital discharge, including gender (p = 0.74), age (p = 0.96),APACHEIII (p = 0.48), CA during daytime (p = 0.15) and initialrhythm (p = 0.30).
3.8. Predicting arrest
From the above variables, we assessed the predictive value of thesimultaneous presence of at least two of four high risk antecedents:(1) a lowest MAP of 65 mmHg or less, (2) a high respiratory rate of20 breaths/min or more, (3) a HCO3 of 20 mmol/L or less, and (4)any noradrenaline infusion (Fig. 2).
Amongst the cohort, 31 CA patients and 35 controls had 2 ormore of these variables recorded. In these patients, such criteriahad a sensitivity of 74.2%, a specificity of 68.6%, a positive predictivevalue of 67.6%, a negative predictive value of 75%, and an accuracyof 71%.
4. Discussion
4.1. Summary of major findings
We conducted a two and a half year retrospective case–controlstudy to assess the characteristics, antecedents and outcomes ofpatients who suffered a CA while in the ICU of a tertiary hospi-tal. We found that a CA occurred in approximately one in every200 patients and that return of a sustained viable rhythm andoutput was achieved in 80% of cases. However, 64% of patientsdied in hospital. We also found that patients who had a CAwere more likely to have markers of physiological instabilityin the period prior to the CA than controls including a higherlevel of vasopressor support. The presence of two or more
of MAP ≤ 65 mmHg, RR ≥20 breaths/min, HCO3 ≤ 20 mmol/L andthe presence of a noradrenaline infusion were of some use-fulness in identifying patients at greater risk of a CA in ourICU.T.H. Rozen et al. / Resuscitation 85 (2014) 411–417 415
circa
4
twwlestrir
Fig. 1. Diagram illustrating the
.2. Comparison with previous studies
The CA rate in our ICU was 6.28/1000 admissions. This is athe lower end of the reported range of ICU CA rates9,10,15,16,20
ith rates of resuscitated cardiac arrest (as distinct from deathsithout resuscitation) likely reflecting local culture related to
imitation of medical treatment orders and end of life care. Nev-rtheless, the population studied is the biggest ICU cohorts studiedo far aside from one large registry review.14 In our hospital,
wo prior studies have assessed CA rates in ward patients withates of 1.12 per 1000 during 201121 and 1.26 per 1000 dur-ng 2004.22 This suggests that patients in ICU are at increasedisk of CA compared to ward patients. Compared with previousFig. 2. Decision tree linking key predict
dian rhythm of cardiac arrests.
studies, a similar proportion of patients in our study had non-shockable rhythms.14 In other literature, non VT/VF CA’s in ICUwere found to be associated with a higher mortality,4,5,8,15,16 how-ever this could not be assessed in our cohort due the rarity ofVT/VF.
ROSC was obtained and sustained in 80.6% of CA patients andtook only 4 min (IQR, 2–8 min) to achieve. This is shortest time inthe literature, with previous papers reporting a median durationof CPR before ROSC of 8–20 min.4,12,16 Our ROSC rate is also the
highest in the literature, with published ROSC rates ranging from29.8 to 80.5%.4,8,9,12,16 A longer time to ROSC has been pre-viously associated with poorer outcomes, particularly beyond20 min.4,8,9,12,16ive variables with cardiac arrests.
4 scitati
Iina
tthrkt
sasigrahor4
4
patfithaaatcmehaavtitht
4
tcIiwmc
coao
1
1
1
1
1
1
1
1
16 T.H. Rozen et al. / Resu
There was no difference in the circadian rate of CA in this study.n previous literature, incidents on evenings or weekends14 andncidents later in the patient’s stay9 had a worse outcome. We didot detect a statistically significant difference in outcomes associ-ted with these variables.
Patients who suffer CAs on the ward have deranged vitals prioro the arrest.23–25 Similarly, our ICU CA patients had higher respira-ory rates, lower blood pressures and lower bicarbonate levels, andigher noradrenaline doses. When these indices were combined, atisk patients could be, to a degree, identified before the CA. To ournowledge, there have been no prior studies of predictors of CA inhe ICU.
We found no predictors of mortality after CA. In contrast, othertudies have shown that sepsis12,16 and hypotension12 have beenssociated with a worse prognosis, as have higher APACHE 2cores,8,12 higher simplified acute physiology score (SAPS II),5,9
ncreasing age4,9,14 and, in one instance, decreased age,13 emer-ency surgical patients9 and being female.4,5 One other studyevealed that use of vasoactive medications prior to a CA wasssociated with an odds ratio of survival of 0.55.14 Survival toospital discharge after CA in ICU in our study was 44.4%. Onlyne other study had a higher published survival, with literatureeporting of survival to hospital discharge ranging from 0% to7.3%.5,8,9,12,13,15,16
.3. Implications for clinicians
Despite invasive support, our CA patients had a lower bloodressure than matched controls. This may relate either to underppreciation and sub-optimal treatment of hypotension, or refrac-ory hypotension despite resuscitation or both. Alternatively, thesendings may reflect a higher level of metabolic burden and acuity inhese patients – particularly when viewed in conjunction with theirigher respiratory rates, lower bicarbonate levels and greater nor-drenaline doses. As many CA’s occurred within the first 12 h of ICUdmission, optimal assessment and stabilisation may not have beenchieved despite strong attempts. In all comparisons conducted,he documented CVP measurements were higher in the cases thanontrols, including those on vaso-active medications. This findingay argue against the presence of significant hypovolemia. How-
ver, a proportion of patients on vaso-active medications did notave a CVP documented in the 12 h prior to the time of the arrest,nd/or within 6 h after the timing of the arrest. Successful ROSC waschieved and sustained in the vast majority. Yet only a minority sur-ived with most deaths being hours or days later. This suggests thathe CA reflected extreme illness severity rather than being itself themmediate cause of death. Finally, we were able, for the first time,o describe physiological antecedents that might help identify veryigh risk patients and perhaps allow implementation of therapieso prevent such CA or redirect strategies to end of life care.
.4. Study strengths and weaknesses
Our study has a number of strengths. To our knowledge it ishe first to scrutinise antecedents to cardiac arrest in the intensiveare unit and the first to identify possible predictors of arrest in theCU. Additionally, cases were identified prospectively from nurs-ng shift reports designed specifically to identify sentinel events
ithin the intensive care unit, and it is unlikely that any cases wereissed. Cases were well matched with controls at baseline for all
o-variates assessed.Our study has the limitations of a relatively small, single centre,
ase–controlled study, and sub-optimal documentation at the timef CPR. Furthermore, in the context of higher noradrenaline beingssociated with CA, this study did not have data to permit analysisf measures of LV filling or function prior to arrest. We are not
1
1
on 85 (2014) 411–417
able to comment on whether the higher noradrenaline dosage wasa reflection of more severe disease, or represented a strong effortto normalise hypotension. No other studies have yet been able toprovide such data.
A further limitation of our study relates to the incidence ofmissing data and small sample size. Thus, variables that were notdifferent between groups may simply have failed to detect dif-ferences due to lack of statistical power. Finally, although someof the differences were statistically different, they were, in someinstances, perhaps of uncertain clinical importance.
5. Conclusions
Cardiac arrests within our ICU were uncommon and associatedwith rapid ROSC in most cases, which was sustained for hours ordays. Despite such successful immediate resuscitation efforts, two-thirds of patients eventually died. In the period leading up to theCA there were signs of physiological and biological instability, andincreasing doses of noradrenaline. When two or more of these werepresent the risk of CA was particularly high. This information mayprove useful in identifying very high risk patients and prevent aproportion of these events in the future and in other ICU’s.
Conflict of interest statement
None identified.
References
1. Buist M, Bernard S, Nguyen TV, Moore G, Anderson J. Association betweenclinically abnormal observations and subsequent in-hospital mortality: aprospective study. Resuscitation 2004;62:137–41.
2. Hillman KM, Bristow PJ, Chey T, et al. Antecedents to hospital deaths. Intern MedJ 2001;31:343–8.
3. Trinkle RM, Flabouris A. Medical reviews before cardiac arrest, medical emer-gency call or unanticipated intensive care unit admission: their nature andimpact on patient outcome. Crit Care Resusc 2011;13:175–80.
4. Kutsogiannis DJ, Bagshaw SM, Laing B, Brindley PG. Predictors of survival aftercardiac or respiratory arrest in critical care units. CMAJ 2011;183:1589–95.
5. Myrianthefs P, Kalafati M, Lemonidou C, et al. Efficacy of CPR in a general, adultICU. Resuscitation 2003;57:43–8.
6. Bedell SE, Delbanco TL, Cook EF, Epstein FH. Survival after cardiopulmonaryresuscitation in the hospital. N Engl J Med 1983;309:569–76.
7. Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital-widecode rates and mortality before and after implementation of a rapid responseteam. JAMA 2008;300:2506–13.
8. Chang S-H, Huang C-H, Shih C-L, et al. Who survives cardiac arrest in the inten-sive care units? J Crit Care 2009;24:408–14.
9. Enohumah KO, Moerer O, Kirmse C, Bahr J, Neumann P, Quintel M. Outcome ofcardiopulmonary resuscitation in intensive care units in a university hospital.Resuscitation 2006;71:161–70.
0. Galhotra S, DeVita MA, Simmons RL, Dew MA. MERIT. Mature rapid responsesystem and potentially avoidable cardiopulmonary arrests in hospital. Qual SafHealth Care 2007;16:260–5.
1. Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resusci-tation outcome reports: update and simplification of the Utstein templates forresuscitation registries. Resuscitation 2004;63:233–49.
2. Peterson M, Geist L, Schwartz D, Konicek S, Moseley P. Outcome after cardiopul-monary resuscitation in a medical intensive care unit. Chest 1991;100:168–74.
3. Rabinstein AA, McClelland RL, Wijdicks EFM, Manno EM, Atkinson JLD. Car-diopulmonary resuscitation in critically ill neurologic-neurosurgical patients.Mayo Clin Proc 2004;79:1391–5.
4. Tian J, Kaufman DA, Zarich S, et al. Outcomes of critically ill patients who receivedcardiopulmonary resuscitation. Am J Respir Crit Care Med 2010;182:501–6.
5. Wallace K, Ewer MS, Price KJ, Feeley TW. Outcome and cost implications ofcardiopulmonary resuscitation in the medical intensive care unit of a compre-hensive cancer center. Support Care Cancer 2002;10:425–9.
6. Yi H-J, Kim Y-S, Ko Y, Oh S-J, Kim K-M, Oh S-H. Factors associated with survivaland neurological outcome after cardiopulmonary resuscitation of neurosurgicalintensive care unit patients. Neurosurgery 2006;59:838–46.
7. Scapigliati A, Ristagno G, Cavaliere F. The best timing for defibrillation in shock-able cardiac arrest. Minerva Anestesiol 2013;79:92–101.
8. Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillationafter in-hospital cardiac arrest. N Engl J Med 2008;358:9–17.
9. Spearpoint KG, McLean CP, Zideman DA. Early defibrillation and the chainof survival in in-hospital adult cardiac arrest, minutes count. Resuscitation2000;44:165–9.
scitatio
2
2
2
2
T.H. Rozen et al. / Resu
0. Chan P, Khalid A, Longmore L. Hospital-wide code rates and mortalitybefore and after implementation of a rapid response team. JAMA 2008;300:2506–13.
1. Vetro J, Natarajan DK, Mercer I, et al. Antecedents to cardiac arrests in a hos-pital equipped with a medical emergency team. Crit Care Resusc 2011;13:162–6.
2. Jones D, Bellomo R, Bates S, et al. Long term effect of a medical emergency teamon cardiac arrests in a teaching hospital. Crit Care 2005;9:R808–15.
2
2
n 85 (2014) 411–417 417
3. Buist MD, Jarmolowski E, Burton PR. Recognising clinical instability in hospitalpatients before cardiac arrest or unplanned admission to intensive care. A pilotstudy in a tertiary-care hospital. Med J Aust 1999;171:22–5.
4. McQuillan P, Pilkington S, Allan A, et al. Confidential inquiry into quality of carebefore admission to intensive care. BMJ 1998;316:8–1853.
5. Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons foravoidable in-hospital cardiac arrest in a district general hospital. Resuscitation2002;54:115–23.