Use of complementary and alternative medicine among people living with diabetes: literature review
Alternative medicine or alternative patients: a qualitative study of patient-oriented...
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Alternative medicine or alternative patients: a qualitative study of patient-oriented...
http://mdm.sagepub.com
Medical Decision Making
DOI: 10.1177/0272989X03261567 2004; 24; 64 Med Decis Making
Opher Caspi, Mary Koithan and Michael W. Criddle Processes with Respect to Complementary and Alternative Medicine
Alternative Medicine or "Alternative" Patients: A Qualitative Study of Patient-Oriented Decision-Making
http://mdm.sagepub.com/cgi/content/abstract/24/1/64 The online version of this article can be found at:
Published by:
http://www.sagepublications.com
On behalf of:
Society for Medical Decision Making
can be found at:Medical Decision Making Additional services and information for
http://mdm.sagepub.com/cgi/alerts Email Alerts:
http://mdm.sagepub.com/subscriptions Subscriptions:
http://www.sagepub.com/journalsReprints.navReprints:
http://www.sagepub.com/journalsPermissions.navPermissions:
http://mdm.sagepub.com/cgi/content/refs/24/1/64SAGE Journals Online and HighWire Press platforms):
(this article cites 54 articles hosted on the Citations
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
10.1177/0272989X03261567 ARTICLEMEDICAL DECISION MAKING/JAN–FEB 2004CASPI, KOITHAN, CRIDDLEDECISION PSYCHOLOGYPATIENTS’ DECISION PATHS FOR CAM DECISION PSYCHOLOGY
Alternative Medicine or “Alternative” Patients:A Qualitative Study of Patient-Oriented Decision-
Making Processes with Respect toComplementary and Alternative Medicine
Opher Caspi, MD, PhD, Mary Koithan, RN, PhD, Michael W. Criddle, BS
Background. Theory and clinical practice suggest thatcomplementary and alternative medicine (CAM) decision-making processes may differ from those used in conventionalmedicine. If so, understanding the differences could improvepatient-provider communication around treatment options.Objectives. To examine patient-oriented decision-makingprocesses relative to CAM use. Population. Adults withchronic rheumatological disorders who utilize allopathicmedicine only, CAM only, or both. Method. An exploratory,cross-sectional naturalistic design with thematic and contentanalyses. Results. Three distinct decision paths were devel-oped, differing substantially on the importance of provider
trust, disease severity/prognosis, willingness to experiment,intuitive/spiritual factors, and outcomes evidence. Conclu-sions. These divergent decision paths indicate the possibilityof “alternative patients,” not just “alternative therapies.”Since informed decisions, tailored to the patient, would likelylead to sustainable improvements in health care outcomes,the findings may facilitate providers’ capacity to effectivelyadvise patients about treatment alternatives and CAM use.Key words: complementary and alternative medicine; deci-sion making; qualitative methods. (Med Decis Making2004;24:64–79)
Many health care decisions require trade-offs. Adiagnostic test or a medical treatment may re-
lieve suffering or reduce the likelihood of future mor-bid events but at the cost of side effects and inconve-nience. Thus, for many instances in which diagnosticand treatment decisions must be made, rational peoplemight choose any one of several options.1 Examples
abound—hormone replacement therapy in postmeno-pausal women, elective surgery, aggressive end-of-lifecare, anticoagulation for atrial fibrillation, and most re-cently, the inclusion of complementary and alternativemedicine (CAM) for treating various illnesses. There-fore, for medical decisions with more than 1 reasonableoption, patient participation in decision making is of-ten necessary to optimally match management deci-sions with patient preferences.2
In recent years, there has been a call in health care toenhance informed decision-making processes, shiftingmedical consultation from a unidirectional, dutifuldisclosure of alternatives, risks, and benefits by thephysician (a paternalistic approach) to a more mean-ingful dialogue between physician and patient.3,4 How-ever, involving patients in clinical decisions is a chal-lenging task, mainly because sharing information andsharing decisions are not synonymous.5 Indeed, a re-cent comparative analysis found that 35% of Ameri-cans felt excluded from medical decision making.6 Todevelop more equal partnerships between health care
64 • MEDICAL DECISION MAKING/JAN–FEB 2004
Received 14 October 2002 from the Program in Integrative Medicine(OC, MWC) and the College of Nursing (MK), University of Arizona, Tuc-son. Financial support for this study was provided in part by a grantfrom the National Institutes of Health (5T35HL007479-19). The fundingagreement ensured the authors’ independence in designing the study,interpreting the data, and writing and publishing the report. Revisionaccepted for publication 10 October 2003.
Address correspondence and reprint requests to Opher Caspi, MD,PhD, research assistant professor, Program in Integrative Medicine,Department of Medicine, College of Medicine, University of Arizona–Health Sciences Center, PO Box 245153, Tucson, AZ 85724-5153; e-mail: [email protected].
DOI: 10.1177/0272989X03261567
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
professionals and patients, providers need training inthe special skills required to ensure that shared deci-sion making occurs, and patients need decision aidsthat would provide information about treatment op-tions and outcomes relevant to their own health statusand the process by which they make health care deci-sions. Health decision aids are designed to facilitateshared decision making by helping patients and theirphysicians choose among reasonable clinical options.2
However, a preliminary requisite for the developmentof such user-friendly, high-value decision-making aidsis proper understanding of patients’ perceptions, valu-ations, and preferences as they relate to health care.Unfortunately, such an understanding is only infre-quently available. The emerging field of CAM is a casein point. The requisite knowledge about the nature ofdecision processes and the factors that underlie thosedecisions, which help patients navigate the complexmaze of alternative therapeutics, is to a large extent,lacking.
WHAT IS CAM?
CAM is not a homogenous field. Rather, it is a cate-gorical term that covers a broad range of more than 100healing philosophies, approaches, and therapeuticmodalities that allopathic medicine does not com-monly study, understand, accept, use, or make avail-able.7,8 CAM therapies may be used instead of conven-tional therapies (therefore “alternative”) or inconjunction with them to supplement or augment thetherapeutic outcome (hence “complementary”). WhileCAM appears to be primarily used for conditions forwhich conventional (allopathic) medicine currently isunable to offer a complete cure (e.g., cancer, back pain,allergies, rheumatological disorders), the vast majorityof CAM users do not rely solely on CAM for treatmentof their medical condition(s) but rather use it in con-junction with conventional medical treatments.9
Interest in CAM is peaking worldwide.10 One of thebest reflections of this increased interest is the ever-growing number of patients,11 medical students,12,13
health care practitioners,14,15 third-party insurers,16 andhealth care policy makers,17 who constantly make in-quiries into issues associated with the incorporation ofvarious CAM modalities into the current health caresystem. This interest is also reflected in a growing bodyof medical research that examines 2 important epide-miological aspects of CAM use: 1) the patients who useCAM (the “who” aspect)18,19 and 2) the reasons that leadthem to use it (the “why” aspect).20,21 However, while
studies exist that describe the means by which patientsarrive at conventional medical decisions, thus far therehave been no systematic studies examining the deci-sion paths (i.e., the temporal sequences of the stagesand subroutines of the decision-making process) thatpatients use to arrive at CAM health care decisions (the“how” aspect).
The dissimilar philosophical underpinnings ofCAM, along with its extreme diversity, create a realityin which patients, who for whatever reasons are inter-ested in CAM, typically face a plethora of modalitiesand practitioners among which to decide. Whatcomplicates things even more is the fact that in CAM-related decisions, which notoriously involve multiplepotential treatment options, there is only limited clini-cal evidence supporting any of the options available.22
Of substantial concern is that many patients are utiliz-ing alternative treatments without being informed oftheir risks and efficacy.23 Investigators have docu-mented evidence of adverse interactions between CAMand conventional medications24,25 and expressed theconcern that CAM users may defer effective availableconventional interventions.26 These treatment lapsesmay occur because of a lack of pertinent informationexchange on CAM between provider and patient27 and/or because patients utilize limited sources of informa-tion on CAM in their health care decision-making pro-cess.28 Thus, if CAM information is not being commu-nicated appropriately to patients or is otherwiseunavailable to patients during the decision-makingprocess at the point of care, the potential for health careoversights may increase.
The lack of mutual awareness about CAM interven-tion options between patients and practitioners begsthe question of whether decision making with respectto CAM differs from decision making with respect toallopathy. If so, an understanding of these different de-cision paths would empower health care providers tobetter tailor communication and advice regardingCAM according to the needs of the patient. As there islittle extant literature about the nature of decision mak-ing in patients who use CAM either in conjunctionwith allopathy or in lieu of it, we conducted a prelimi-nary study that sought to explore and describe patients’decision paths related to CAM use. Specifically, 3research questions were addressed:
1. What processes do patients use when making deci-sions about health care alternatives?
2. What information is central to decision making rela-tive to CAM use?
DECISION PSYCHOLOGY 65
PATIENTS’ DECISION PATHS FOR CAM
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
3. What are the similarities and differences in the decision-making processes used by patients who elect to useCAM and those who decline its use?
METHODS
Design Overview
Three basic assumptions underpin this study andprovide rationale for the design and study methodsused to address the research questions.
First, we assumed that the ways in which patientscome to use CAM involve decision processes that canbe specified and explicated. To this end, we used natu-ralistic inquiry and qualitative methods to gain accessand elicit data descriptive of these complex humanprocesses.29,30 Naturalistic investigation was first iden-tified by Lincoln and Guba31 as a form of inquiry thatincorporates the axioms of the naturalistic paradigm: 1)realities are multiple, constructed, and holistic; 2)knower and known are inseparable; 3) hypotheses aretime and context bound; 4) entities are continuouslyinteractive; and 5) inquiry is value bound. They identi-fied an investigational “flow of activities” that seeks to“study things in their natural [uncontrolled] set-tings . . . in order to interpret the meanings of phenom-ena.” As such, we conducted individual open-endedinterviews with persons who either have used CAM orconsidered to use CAM but declined to 1) elicit de-scriptions about the processes inherent in health caredecision making, 2) describe factors that affected theseprocesses, and 3) understand more fully how patientsmake decisions regarding the type of health care theyseek. Thematic analysis and content analysis strategieswere used to examine the transcripts of these inter-views from which rudimentary descriptive models ofthe decision-making processes began to emerge.
Second, we assumed that the decision paths pa-tients use to choose CAM may differ from the decisionpaths used to choose allopathic health care interven-tions. To this end, 3 distinct groups of patients wereconsidered: 1) patients who have considered usingCAM but in the end decided not to use it (the allopathicgroup), 2) patients who use CAM but not allopathicmedicine (the alternative group), and 3) patients whouse both CAM and allopathic medicine (the comple-mentary group). This consideration allowed us to ex-amine if differences exist in the decision-makingpathways of these 3 groups.
Third, we assumed that the decision paths patientsuse to choose CAM may differ as a function of personaland contextual factors. To this end, we were trying to
understand how these factors shape the decision paths.Because of the preliminary nature of the present study,we decided to focus our effort on a specific group of pa-tients (those with chronic rheumatological disorders,such as osteoarthritis, rheumatoid arthritis, andfibromyalgia) who are likely to use both conventionalmedicine and various CAM modalities. Chronicrheumatological disorders serve as an archetypicalmedical condition for which CAM is used. They arewidely prevalent in the United States, have poorly un-derstood etiologies, are lacking definitive cures,32 andare typified by substantial pain and discomfort, vari-able disease course, and often adversely affect func-tional status. Indeed, some two-thirds of rheumatologypatients report routine use of CAM,33 a substantiallyhigher rate than the roughly 40% “general national av-erage.”19 The most commonly reported CAM therapiesbeing used by this population include exercise, dietarymanipulations and supplements, herbs, copper brace-lets, acupuncture, chiropractic, and massage.34,35
Across surveys, rheumatology patients perceive CAMto be moderately helpful yet not more effective thenallopathy.36,37 Moreover, some rheumatological disor-ders are treated with immunosuppressive drugs thatmay interact with CAM,33 but data on patients’ percep-tions of the safety of specific CAM modalities are lim-ited.36,38 These characteristics suggest that rheumato-logy patients constitute a large health care populationthat may facilitate the examination CAM-relatedpatient decision paths.
In addition, we were interested primarily in the rou-tine, ongoing use of either CAM or allopathy ratherthan in one-time experimentation with either. To in-crease consistency across subjects, we were interestedin patterns of treatments that patients used explicitly totreat their chronic rheumatological condition ratherthan treatments used for other problems. For example,if a patient routinely used vitamin C to combat acommon cold but no other CAM therapies to allevi-ate arthritis-related suffering, the patient was not con-sidered a CAM user. If, on the other hand, the patientroutinely used 1 or more CAM modalities (for instance,glucosamine) to specifically fight her rheumatologicaldisorder, she would be considered a CAM user.
All study procedures and protocols were approvedby the University of Arizona Institutional ReviewBoard (IRB). Consistent with IRB regulations, after clar-ifying any questions subjects may have had, all subjectswho voluntarily agreed to participate in the study wererequired to sign an informed consent. No monetary orother forms of compensation were offered. Other thanthe interviewer who knew the patients, all other data
66 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
were collected and analyzed by an anonymousindividual.
Subjects
Since our goal for this study was one of descriptionand exploration, we used purposive sampling31,39 to ac-cess subjects who were able and willing to fully de-scribe their decision-making processes relative to CAMuse. Adult patients with confirmed chronicrheumatological disorders were directly recruited ei-ther from the Arizona Arthritis Center, Arizona HealthSciences Center, Tucson, Arizona, or through non-MDpractitioner initiatives in community-based CAMpractices located in Tucson, Arizona, who explainedthe study to all potential eligible subjects. Since thiswas an initial exploratory study, we sought primarily tounderstand the decision-making process used by self-governing individuals rather than examine a morecomplicated process that might involve minor chil-dren and adult parents. In addition, we chose not to in-clude newly diagnosed patients because we did notwant to potentially create more confusion by “suggest-ing” more therapeutic options or additional emotionalstress that often accompanies a new diagnosis. Accord-ingly, inclusion criteria included 1) adult patients (age18 years) who suffer from any type of confirmedchronic (6 months) rheumatological disorder, 2)willingness and ability to communicate in English, and3) willingness and ability to participate in the study.
Once identified, participants were presented with alist of commonly used CAM modalities and asked 2 ini-tial questions: 1) “Have you used any of the followingtherapies to specifically treat your rheumatologicaldisorder more than once in the last year?” and 2) “If yes,did you use the therapy in lieu of or in addition to thetherapy that your physician has recommended toyou?” These questions were meant to assist us in ex-ploring similarities and differences in CAM-relateddecision-making processes among members of the 3distinct groups of patients outlined above (allopathic,alternative, and complementary).
Data Collection Methods
To ensure the trustworthiness of the design, we usedthe data collection and analysis framework suggestedby Lincoln and Guba.31 In-depth, open-ended inter-views were used as the method of data collection. Eachinterview lasted approximately 1 to 1½ h and was con-ducted at a time and place that was convenient, acces-
sible, and agreeable to both participant and inter-viewer. All interviews were audio recorded and tran-scribed for later analysis and quality control.
One interview was conducted with each partici-pant. Although prompting questions were used to fo-cus these interviews, the content and direction of theinterviews were driven by the participants’ responses.This type of nonstructured interviewing is particularlyuseful when little is known about the phenomenon ofconcern and when the researchers are interested in un-covering breadth of information, the “hows [sic] of peo-ple’s lives and the constructive work involved in pro-ducing order in everyday life.”40(p646) We began eachinterview with a grand tour or broad, general question.This 1st question was, “Describe what you do currentlyfor your health care treatment and how you make deci-sions about these health care treatments.” Participantswere allowed to respond as they chose using the interac-tive interviewing style of Spradley41 and Silverman.42
Prompts were used to encourage further explicit de-scription of the decision-making process or to clarifyareas of confusion. Table 1 presents a few examples ofthe prompts used.
During the interview, the interviewer kept fieldnotes to remind himself of key ideas or concepts identi-fied by the participant, in addition to areas that re-mained unclear or underdeveloped. Toward the end ofthe interview, the interviewer summarized the decision-making processes that were identified by the partici-
DECISION PSYCHOLOGY 67
PATIENTS’ DECISION PATHS FOR CAM
Table 1 Exemplar Interview Prompts and ClarifyingQuestions
What led you to decide to use alternative medicine?What sources of information do you often rely on when
making decisions about health care treatments?What were the things you have considered when deciding
to use or not use alternative medicine?How do you decide who or what you trust related to health
care information?Could you explain what you specifically did when you
consulted with friends before making a decision to useor not to use alternative medicine?
What are your expectations of the health care treatmentsyou select?
Do you feel that you make health-related decisions any waydifferently than other decisions in your life?
When you say that there’s “nothing to lose,” what do youmean?
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
pant and asked if this summary accurately portrayedwhat the participant experienced and if there were ad-ditional key points or changes that the participantwould like to make. Using this confirmatory interview-ing technique, the interviewer had the opportunity toclarify problematic areas without leading the partici-pant in a particular direction or biasing the final prod-uct because of misunderstandings. Following the inter-views, the data were transcribed into text for thepurpose of analysis.
Coding and Analysis
Thematic and content analysis strategies were usedto identify and develop core concepts and categoriesthat eventually comprised the key components andphases of the decision-making processes used by theparticipants. Once all of the data were collected, 2 re-searchers independently reviewed the transcripts aswholes to try to extract an understanding of the data foreach individual participant and for the data set fromeach of the 3 groups (i.e., allopathic, alternative, andcomplementary). Individual data units, representa-tive of critical incidents, critical junctures, and theprocesses/characteristics/influences inherent in thoseinstances, were then considered from the emic per-spective (using the participants’ own words anddescriptors to explain the phenomenon). Data units(word phrases and sentences), representative of centralor fundamental concepts or processes, were thencoded in a textual assessment database generated usinga combination of MS Word and MS Excel. Once thisinitial coding was complete, the 2 researchers met andagreed through consensus on the emic codes thatwould be moved forward in the process of theorygeneration.
Having generated the emic codes for each individualparticipant and each decision incident, all members ofthe research team met to compare the codes withinstudy groups to find meaningful relationships amongthe codes and to generate etic thematic categories (the-oretical and conceptual descriptors that are more ab-stract and generalizable). These categories were thenused to address the first 2 research questions and toidentify core categories that provide the basic descrip-tion of the different decision-making processes used bythe groups. Each of these core categories was then fullyexplored within the data, initial definitions were iden-tified, and inherent subprocesses were described. Theteam then developed rudimentary explanatory modelsof decision making for each of the 3 study groups. Oncethese 3 models were identified, we then compared thecategories and themes both across individual subjects
and then across groups to derive convergent anddivergent core categories and processes to address the3rd research question.
RESULTS
Participants’ Characteristics
Twelve adult patients (5 males and 7 females, agerange = 39–68 years) with confirmed chronicrheumatological disorders participated in this prelimi-nary study. Nine of them were directly recruited fromthe Arizona Arthritis Center, Arizona Health SciencesCenter, Tucson, Arizona, and 3 were recruited throughnon-MD practitioner initiatives in community-basedCAM practices located in Tucson, Arizona. All partici-pants defined themselves as white (non-Hispanic). Nosignificant differences were found among the 3 studycohorts in terms of education, age, or gross annual in-come. Four subjects had a graduate degree, 4 had an un-dergraduate degree, and 4 graduated from high school.In terms of income, 3 reported a gross annual incomebelow $25,000, 5 between $25,000 and $50,000, and 1between $50,000 and $80,000 (3 subjects declineddisclosing their income).
Descriptive Models of CAM HealthCare-Related Decision Making
Three unique rudimentary descriptive models of de-cision making emerged from the within-group analy-sis. These models address the first 2 research questionsand provide insight into the processes that patients usewhen making decisions about health care alternativesand the information that each group considers centralto those decisional processes.
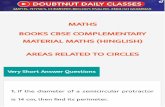
Decision paths for the allopathic group. Five partici-pants who used only allopathic treatments to addresstheir chronic rheumatological conditions provideddata about their health care decision-making pro-cesses. Several convergent patterns emerged from thedata, including the basic social process used to makehealth care treatment decisions. Figure 1 presents a de-scriptive model for this group and summarizes key fea-tures of their CAM-related decision processes.
All participants agreed that they are continuouslyappraising 2 conditional parameters, 1) current func-tional status and 2) their current sense of well-being,that then influence their decision to identify treatmentoptions and select their preferred treatment strategies.Participants stated that they would seek professionalcare and treatment when they perceive themselves to
68 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
have increasing disability and dysfunction. Theywould then identify viable treatment options by con-sidering 3 conditional and treatment aspects: 1) poten-tial consequences of the treatment, including harmfulside effects; 2) perceived severity of the presenting di-agnosis and/or symptoms; and 3) prognosis. If a treat-ment is deemed “relatively safe or essentially harm-less,” they would be more likely to agree to try thatremedy. If the condition was considered life threaten-ing, those in this group would consider alternativetherapies to be “too great a risk” and would insteadseek out more conventional, allopathic treatment strat-egies. However, participants indicated that they mightbe willing to consider alternative therapies as a preven-tative measure or when they perceive themselves as“hopeless”; they stated that they may be willing to “tryanything,” including alternative therapy, if they “hadnothing to lose.”
Trust in the allopathic health care system and pro-viders also seemed to be consistent across allopathicparticipants, whereas those from the other 2 groupswere more skeptical. Once a decision had been made toseek out care and treatment options, participantswould immediately turn to the conventional physicianfor an advice. His or her opinion and recommendationweighed heavily in the decision-making process andserved as a mediating interpersonal process affectingthe basic social process of decision making. “I don’t un-derstand the arthritis, so I leave it in the hands of thedoctor. He has a huge amount of experience andschooling.”
In this group of allopathic-only patients, the pa-tient’s role in decision making appears to be a relativelypassive one. Participants consistently stated that theytrusted their physician to make correct treatmentchoices. Although they stated that they required evi-
DECISION PSYCHOLOGY 69
PATIENTS’ DECISION PATHS FOR CAM
Decision-Making Process
Key Features
Appraise functional status
Appraise well-being
Identify TreatmentOptions
Make TreatmentSelection
Assess Potential Consequences Assess Diagnosis
Severity
Consider Prognosis
Provider Opinion and Choice
� Seeks health care with increasing disability and dysfunction � Trusts allopathic provider and provider’s decisions� Relative passivity in the decision-making process� Little active information seeking by client/patient� Will consider alternative therapies as prevention or if condition is hopeless
or there is little risk in therapy
Figure 1 A descriptive model for complementary and alternative medicine–related decision processes for the allopathic group.
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
dence or logic supporting a treatment to try it, whenquestioned about the process of validating the recom-mendations of their physicians, they were unable toidentify either a process that was used or what evenconstituted logic. Rather, participants consistentlystated, “Having my MD’s approval to try something isall that I would need. I don’t need any other informa-tion.” When questioned about the type of evidence thatshe would require, one subject stated, “[The] evidencethat I need is my physician telling me that it works.”This type of thinking may be considered consistentwith an external locus of control (i.e., responsibility forverification of treatment validity is assigned or dele-gated to an outside other who is perceived to be in-formed).43 In addition, this group did not seem toactively search for information about any therapy.
Participants in this group sustained their decision toexclusively use allopathic interventions by 1) consid-ering the perceived outcomes of current treatment and2) continuous symptom appraisal. They were notlikely to entertain changes in their treatment choice ifoutcomes were perceived to be positive. “I neverthought about trying any other thing. The medicineseemed to be doing the job.” Contrarily, when the pre-scribed therapy failed, participants stated that theymight be more open to alternative treatments, thusonce again considering treatment options using thesame approach. “He had me on antibiotics for almost ayear and a half and it wasn’t getting any better, soI . . . [might consider] a homeopathic practice that mymother-in-law suggested.” In addition, if participantsperceive their condition to be deteriorating, theywould be more open to suggestions of CAM if approvedby their allopathic physician. This suggests that the ba-sic process described by the participants is redundantand recurrent in nature.
Decision paths for the alternative group. Three par-ticipants who used only alternative treatments to ad-dress their chronic rheumatological conditions wereinterviewed. Several emerging patterns were found inthese data, suggesting a 2nd distinct decision-makingprocess. Figure 2 presents a descriptive model for thisgroup and summarizes key features of their CAM-related decision processes.
In this group, the initial decision to try alternativetherapies was not based on perceptions about severityof the condition, disability, or appraisal of potentialconsequences. Rather, the initial decision to considerand identify treatment options was based on 1) per-sonal testimonials, 2) repeated suggestions that they trya particular modality, or 3) repetitive endorsements of aspecific treatment. “On 2 or 3 specific occasions I heard
about this specific [alternative] treatment, then I readbooks that talked about the same thing. . . . So I was ex-posed several times and ran across it several times . . .so it all worked together as signs . . . so it was an avenuethat I decided to look into.”
The most notable finding in this group was that par-ticipants appear to be willing to experiment with treat-ment modalities once the options were identified. Thisexperimentation was done before making a final treat-ment decision and was used to justify and test the“rightness” of a treatment for them individually. Twoparticipants specifically identified that prior to the de-cision, they receive a “spiritual sign” or an “intuitivefeeling” that signals that the treatment is “right forthem.” “Running into something else that confirmswhat I’ve already thought and heard by chance or fate.Then I decide to use it.” For these participants, this signwas a necessary precursor to the initial decisionalevent. Therefore, it appears that this group may ascribelocus of control to a powerful other (God/spirit) orchance rather than to an external (physician) orinternal (self) source.
Several contextual phenomena serve as backgroundto the alternative decision-making process. This groupassumed that allopathic physicians “don’t have all theanswers,” that a single provider does not possess privi-leged knowledge. They consistently identified that“we can’t put our lives in other people’s hands whenthey don’t have the whole picture.” Subjects in thisgroup also had a more skeptical view of the allopathichealth care system. Two identified specifically thatprevious failures with allopathy underpin their ap-proach to therapy. Also, they seemed more comfortablewith uncertainty. They stated that they did not need toknow specific proof of potential benefits or how a treat-ment or modality “works in the body” to try it. “It needsto make sense to me personally and spiritually, not if itmakes sense scientifically or if there is a scientific ex-planation in books.” Finally, participants sustained thedecision to use alternative therapy by evaluatingwhether “balance in mind-body-spirit” or “balance be-tween the inner and outer person” had been achieved.Therefore, while participants in this group may decideto experiment with a variety of modalities, they subse-quently decided to continue use of specific therapiesbased on perceived holistic healing. “I use my mindand spirit to decide if I want to try [a therapy], then afterI try something I use my mind-body-spirit to evaluatehow I responded. If there is continued imbalance, Imove on.”
Members of this group differed in their need for in-formation. Whereas some did not actively seek infor-mation about health care choices, others took a very ac-
70 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
tive role and placed a much higher value on the“literature.” There was also divergence when consider-ing the influence of friends, family, and allopathic phy-sicians on the decision-making process. Two usedfriends and family as information conduits only, whilethe 3rd commented that he would be more likely to usea therapy if it were recommended by a trusted other.While physician input was not shunned, it was also notconsidered necessary. One commented, “I would onlytalk to him if it was something drastic.”
Decision paths for the complementary group. Fourparticipants who used both allopathic and alternativetreatments to address their rheumatological conditionswere interviewed. Convergent patterns within thisgroup were again identified, leading to a 3rd distinctdecision-making process. Figure 3 presents a descrip-tive model for this group and summarizes key featuresof their CAM-related decision processes.
Participants of this group required multiple sourcesof data prior to making any decision. The participantsdescribed a consistent sequential process of informa-tion gathering that would occur as a precursor to the ac-tual decision. Friends, family, or close associates whooffered opinions and personal testimonials often initi-ated treatment suggestions. These were met with bothinterest and skepticism. Participants would then con-sult the Internet for further information. Web siteswould be scrutinized for credibility, with participantsoften reviewing the credentials of those responsible forthe site. Web sites that were most commonly identifiedincluded WebMD (http:///www.webmd.com), theAmerican Medical Association (http://www.ama-assn.org), Discovery Health (http://health.discovery.com),the US Food and Drug Administration (FDA) (http://www.fda.gov/), and the Arthritis Foundation (http://www.arthritis.org). Search engines were also fre-quently used. Some participants would consult medi-
DECISION PSYCHOLOGY 71
PATIENTS’ DECISION PATHS FOR CAM
Decision-Making Process
Key Features
Personal
Testimonials
Repetitive Endorsements/ Suggestions
Identify Treatment Options
Experiment with options
Make Treatment Selection
InherentSkepticism of
system
Prior negative system experiences
Comfort with uncertainty
IntuitiveRightness of
Fit
� Considers intervention based on convincing repetitive suggestions and personal testimonials
� Inherent skeptic of both the current health care system and alternatives� Experiments with many treatment modalities prior to decision� Inherent comfort with uncertainty� Accepts personal responsibility for choices and decisions/active
participant in decision-making process� Intuitive “rightness of fit” is a significant mediator of the process
Figure 2 A descriptive model for complementary and alternative medicine–related decision processes for the alternative group.
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
cal literature or access published information, such asthe Journal of the American Medical Association, theMerck Manual, and the FDA cross-references. Specifi-cally, they were looking for convergence among find-ings relative to a specific treatment modality. If therewas enough evidence, they then made the decision totry a particular therapy. All were very sensitive to mar-keting efforts, assigning less credibility to sources thatwere “trying to get your money.”
All participants stated that they required a logicalexplanation before making decisions to use eitherallopathic or alternative therapies and that “scientificfacts” are more influential on the process than is “per-sonal testimony.” “Scientific facts are more importantthan other people’s experiences. Some people don’t en-
joy a particular therapy even though it may be effective.But there’s proof there in writing that it’s better foryou.” They all recognized that there is individual vari-ation in the effect of a treatment and stated that they didnot expect similar results for similar treatments. “Otherpeople’s systems respond differently to a treatment, soyou can’t put too much value on other peoples’ suc-cesses.” Yet logic and evidence was tempered by theparticipants’ belief system. Treatments had to logicallyfit and the evidence had to “make sense” given theparticipant’s own values and philosophical views.
These participants sustained their health care deci-sions by evaluating the effectiveness of symptom relief,the congruency of the treatment with a personal valuesystem, and cost. Pain was considered a priority symp-
72 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
Decision Making Process
Key Features
Personaltestimonials
of close associates
IdentifyTreatmentOptions
ResearchTreatment Options
MakeTreatmentSelection
Interest
Skepticism
Assesscredibility of siteand information
Assessconvergenceof findings
InternetLiterature
Strengthof
evidence
Perceived logic of treatment & evidence
Consistency with belief in system
� Testimony by personal friends and close associates initiates care seeking� Credibility of evidence is carefully scrutinized, mediated by intellectual
curiosity and skepticism.� Decisions based on perceived logic of treatment and outcomes; cognitive
process of weighing evidence � Examination of treatment includes consideration of fit between evidence,
therapy and personal belief system� Active participation in the decision-making process
-
Figure 3 A descriptive model for complementary and alternative medicine–related decision processes for the complementary group.
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
tom in this evaluative/decision-making process.“When I rub this [herbal treatment] on my knees, itheats up the muscles and joints for 4 days, where I don’thave the immense pain that I had. I still use it when Ineed to.” Cost and strangeness were mentioned as bar-riers to ongoing CAM use. “Even though acupuncturedid relieve my pain for days afterward, I didn’t go backbecause I couldn’t afford it.” “The [alternative] treat-ment progressed to crystals being waved over yourface . . . that is when I said this is too weird. I don’t be-lieve in this kind of hocus-pocus, medicine man kindof stuff . . . so I quit.” Again, these statements indicatethat this is a redundant rather than linear socialprocess.
Divergent themes also arose. When participantswere asked if they would follow the same basicdecision-making process even in times of desperation,this group seemed to follow a less consistent sequentialpathway. One stated that he would still proceed withcaution, while others stated that they would “throwlogic out the window.” “It’s that feeling of hopeless-ness; I’m willing to go past my comfort . . . outside of mybelief system . . . use something that may be unproven.”
Participants also disagreed about decision parame-ters. Some participants looked more to conventionaltreatment for severe pain and disability. Others wouldbe very practical and try multiple approaches(allopathic and alternative) to alleviate severe symp-toms, with an attitude that “it can’t hurt.” However, noone stated that alternative therapies would ever be fa-vored over allopathic therapies, simply because theywere alternative or “not conventional.” Neither didthey suggest that there was a specific sequence of inter-vention types (trying allopathic treatments first and re-serving alternatives for failed symptom relief). It ap-pears, therefore, that these participants did not relegatealternative therapies to a secondary status. Rather, al-ternatives were considered as 1 of 2 options when mak-ing health care decisions, and evidence of effectivenesswas considered paramount to any decision beingmade.
Similarities and Differences in DecisionProcesses between Participant Groups
The third research question was addressed as wecompared themes and categories across the 3 partici-pant groups (allopathic, alternative, and complemen-tary). A defining characteristic of the sampled patientswho use only allopathic means for their rheumatolo-gical condition(s) was trust in their physicians to makehealth-related decisions for them. Indeed, for this
group, allopathic physicians seemed to be the ultimateauthority regarding health information and diseasetreatment. This contrasted noticeably with the alterna-tive group, which, although not necessarily considerednegatively, did not assign any special authority toallopathy or its practitioners. Rather, the ultimate au-thority to decide was reserved for the patient himself,and this decision was centered on a personal belief sys-tem, not a professional opinion. A treatment approachthat was congruent with that belief system, regardlessof scientific backing, was considerably more likely tobe undertaken than one that was not. The range of thesefindings is consistent with the literature. This depend-ency on the physician is not new. Previous research hasfound that many patients are strongly influenced bytheir physicians’ recommendations, so much so thatthey want their physicians to take much of the respon-sibility for their medical decisions, whereas others pre-fer to take an active role in the decision-makingprocess.44–46
The complementary group, like the alternativegroup, did not defer the decision to an outside author-ity. However, unlike the alternative group, these pa-tients seemed to give the most sway to scientific evi-dence. If a treatment had been documented in theliterature to be effective, especially by controlled scien-tific studies, and multiple sources confirmed the re-sults, patients in the complementary group were likelyto try it. Information seeking also separated this groupfrom the other two. Patients in the allopathic and alter-native groups were more passive absorbers of informa-tion, through their physicians in the former and bychance, coincidence, or “fate” in the latter. However,members of the complementary group went out of theirway to gather information before making a decision.They did this by surfing the Internet, searching booksand journals in the library, asking their physician or an-other expert, and so forth. One potential explanationfor this information-seeking behavior is that the utili-tarian value of the various CAM modalities was hard todetermine. Pierce suggested that patient-oriented deci-sion making can be either immediate or deliberative,depending on the salience of the alternatives and theirrespective attributes. A salient alternative is one that isclear to the decision maker and appears to be the mostpreferable at that moment. Alternatives that are not im-mediately salient tend to stimulate a need in the deci-sion maker for more information so that he or she willbe able to better evaluate its characteristics.47
The fact that information and scientific backing wasimportant may also suggest that the complementarygroup was uncomfortable with uncertainty. They
DECISION PSYCHOLOGY 73
PATIENTS’ DECISION PATHS FOR CAM
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
wanted to be sure that a treatment was safe and likely toproduce positive results before trying it. This furtherdistinguishes the complementary group from the alter-native group, which seemed much more comfortablewith uncertainty and more likely to experiment withunproven therapies. Perhaps it could be better ex-plained by looking at it from the alternative group’sperspective. An intuitive or spiritual confirmation,congruency with personal belief system, and/or com-ing across something by chance or “fate” may work to-gether to serve the same purpose that documented evi-dence serves for the complementary group and that aphysician’s approval serves for the allopathic group: Ithelps to reduce the uncertainty about making adecision to try something else/new.
Another feature that separates the 3 groups is therole of perceptions of disease severity and disability inthe decision-making process. The clearest distinctionlay between the allopathic and alternative groups. Forpatients in the allopathic group, disease severityseemed to be a very important factor. If they perceivedthemselves to be more debilitated or their condition tobe graver, they would seek only allopathy. However,they may consider alternative treatments as a preven-tive measure. Most in this group also agreed that if theyhad exhausted allopathic means and perceived theirsituation to be hopeless, they may be willing to try al-ternative treatments as a last resort. In the alternativegroup, perceptions about severity and disability didnot seem to play a major role. It was unclear from thedata what role these perceptions played for the com-plementary group, although some in this group agreedthat if they felt desperate or hopeless, they might followa less systematic approach and would be more likely totry a therapy that has no scientific or logical backing.
DISCUSSION
The recent mainstreaming of CAM brings with it notonly a renaissance for many old healing philosophiesand techniques but also some unique challenges forcontemporary medicine. For example, valid concernshave been raised with respect to the best models forCAM integration into the health care delivery sys-tem,48–51 the empirical base for such an integration,52
the extent to which CAM should be regulated,53 and thecompetency and scope of education of integrative phy-sicians.54 The present study focuses on yet anotherchallenge: understanding the ways by which patientsmake CAM-related health care decisions.
Our study suggests that at least in patients who suf-fer from chronic rheumatological disorders, those pa-tients who use CAM in lieu of allopathic medicine mayuse decision-making processes that are distinct fromthe ones employed by those who use only allopathicmedicine. It also suggests that patients who combineallopathic and alternative forms of treatment use yetanother unique approach to health-related decisionmaking.
Decision making is a process that combines desires(utilities, personal values, goals, ends, etc.) and beliefs(expectations, knowledge, means, etc.) to choose acourse of action.55 Evidence exists that individualswho do participate actively in their treatment decision-making process tend, in general, to be more satisfiedand more compliant with their treatment plan andoverall do better after treatment than those who assumea passive role.45,56 However, patients may vary in theirdesire for involvement in decision making in consulta-tions.46 Evidence also exists that patients’ preferencesfor involvement in medical decision making relate tothe nature of the decisions, type of illness, and illnessseverity.57 However, it is less known how the numberand diversity of multiple therapeutic alternative op-tions affect patients’ desire and ability to take an activepart in shared decision making. In that sense, the con-temporary integration of CAM into the health care sys-tem poses an interesting question with respect to theimpact of an expanded armamentarium of therapeuticoptions on patients’ decision-making process. This isbecause, on one hand, this integration promises theo-retically an improved package of medical care for theconsumer,58,59 yet, on the other hand, it may add morecomplexity in terms of making choices.
Redelemeier and Shafir60 have shown in a study un-related to CAM that in complex medical situations thatoffer multiple alternatives, the introduction of addi-tional options can paradoxically increase decision dif-ficulty and hence the tendency to choose a distinctiveoption or maintain the status quo. This may be in partbecause cognitive biases appear when people have dif-ficulty deciding between conflicting alternatives, facesituations of substantial uncertainty, or consider out-comes that have long-term consequences.61,62 It is alsolikely that when patients are presented with more than1 therapeutic option, the framing and representation ofthe problem and its alternative solutions become veryimportant.63 Patients may decide one way or anotherdepending on factors such as the extent to which atreatment option is perceived to be congruent withtheir beliefs, values, and preference; prior thought and
74 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
preconceptions about the problem and the potentialsolutions; and an affective response to either comfort orthreat. In making choices among a number of alterna-tives, patients do not necessarily consider all the attrib-utes of all the alternatives.64 Tversky suggested adeterministic, elimination-by-aspects model in which
the selection of an aspect eliminates all the alternativesthat do not include the selected aspect, and the processcontinues until a single alternative remains. If a se-lected aspect is excluded in all the available alterna-tives, no alternative is eliminated and a new aspect isselected. Consequently, aspects that are common to allthe alternatives under consideration do not affectchoice probabilities.65
Barthelemy and Mullet, on the other hand, suggested aselection-by-aspect model in which attributes or as-pects are both ruled in and out simultaneously ratherthan sequentially.66 A few examples of such attributesor aspects that appear to be salient in CAM-related de-cision making are the cost of the treatment, whether thetreatment makes sense, and the empirical or evidencebase of the various alternatives. Consistent with theprominence hypothesis, it has been suggested thatchoosing an alternative on the basis of its most impor-tant attribute is easy to justify to oneself and others,does not require trade-offs between attributes, and re-duces mental effort.67 For example, often the most sa-lient attribute of an alternative is the emotional re-sponse (repulsion or attraction) it elicits in the decisionmaker’s mind. In these cases, the amount of informa-tion provided may be less important than its emotionalimpact. Thus, for example, negative information tendsto be weighed more heavily than positive informationin the comparison of 2 choice options.68
Our data suggest that at least in patients who sufferfrom chronic rheumatological disorders, the most sa-lient attributes or aspects on which patients base theirdecision of whether to use CAM are fairly distinct foreach of the 3 groups. To explain why there exist suchdifferences among these 3 groups, the temptation maybe to say that patients who are using alternative medi-cine are doing so because they have had negative expe-riences with the allopathic system or that they perceivethat the system has failed them. Therefore, they are try-ing a different approach. Although 2 of the 3 alternativegroup members suggested that they have had such ex-periences with allopathy, this per se does not seem toaccount for most of the differences. Moreover, failure ofthe allopathic system was not mentioned among mem-bers of the complementary group as a major reason forturning to alternative treatments. Rather, the differ-
ences among the groups seem to be rooted in personalvalue systems and appear to be more intrinsic to the pa-tient than extrinsic. Does this suggest that some pa-tients are, by nature, “alternative” patients and there-fore more likely to follow a decision pattern that willresult in the use of alternative medicine?
Sirois and Gick69 divided CAM users into 2 groupsbased on the frequency and length of their use of com-plementary therapies. They found that in general,health-aware behaviors and dissatisfaction with con-ventional medicine were the best predictors of overalland initial/infrequent CAM use and that more frequenthealth-aware behaviors were associated with contin-ued CAM use. Medical need also influenced the choiceto use CAM and was the best predictor of committedCAM use, with the established CAM clients reportingmore health problems than the new/infrequent CAMgroup. Openness to new experience was associatedwith CAM use in general but was most notable in thedecision to initially try or explore using CAM. Theirfindings support the utility of the 3 components (pre-disposing, enabling, and need factors) of Andersen andNewman’s sociobehavioral model70 for explaining whysome people choose CAM. They concluded that “CAMclients need to be looked at in more sophisticatedways, rather than being treated simply as a homoge-nous group with similar beliefs, motivations andneeds.”(70,p1025)
Astin studied the sociodemographic and personalfactors that underlie motivations to use CAM.20 Hetested 3 theories to explain this use: 1) dissatisfactionwith conventional treatment, 2) need for personal con-trol over health care decisions, and 3) philosophicalcongruence with worldviews. Using multivariate re-gression model analysis, he found that higher educa-tion, valuing subculture ideals, transformational expe-rience changing one’s worldview, poorer overallhealth, holistic health philosophy, and any of the con-ditions of anxiety, back problems, chronic pain, or uri-nary tract problems were determinants of CAM use.Pawluch and others71 found an association of CAM usewith a holistic health philosophy and valuation of un-conventional lifestyles, lending support to Astin’sfinding that CAM users have had a changed worldview.Other researchers have found that use of CAM is asso-ciated with lower health-related quality of life andlower health protective behaviors.72,73 AlthoughMontibrand,28 using the Health Locus of Control, iden-tified a desire for control over treatments in patientswho use CAM, Ramos-Remus and others7 found thatCAM users were no more likely to be “internals” (i.e.,patients who believe they influence events by theirown actions) than patients who were not CAM users.
DECISION PSYCHOLOGY 75
PATIENTS’ DECISION PATHS FOR CAM
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
Using the health belief model as a theoretical frame-work, Brown and Segal74 examined the relationshipsbetween health beliefs and the use of conventionalmedicine and CAM in hypertensive persons. Theyfound that behaviors consistent with the health beliefmodel (i.e., perceived severity and perceived benefits)were determinants of CAM use. A sociodemographicsurvey in Canada found no significant differences be-tween patients who used “accepted CAM practices”such as chiropractic and acupuncture and those whoused “rejected CAM practices” such as homeopathy.The authors of that survey concluded that patients whosought rejected alternative health care providers arebest understood as desperate pragmatists rather thangullible fools who are uninformed about orthodoxmedicine’s assessment of what is appropriate for theirhealth problems.75
We do not claim or suppose our categorizing of thesedifferent patients as allopathic, alternative, and com-plementary to be exhaustive or absolute. There arelikely varying degrees to which patients in each groupfollow the patterns described above. Some may employa decision-making process that does not clearly fit intoany one category but contains components of multiplecategories. Furthermore, other subcategories clearlyexist. For example, in the complementary group, theremay be those who use allopathic medicine to supple-ment alternative therapy and those who use alternativetreatments as an adjunct to allopathic medicine. Themain point is that different kinds of patients use differ-ent resources, thought processes, and belief systems toarrive at decisions. As a result, different patients mayrequire different kinds of information from their healthcare providers to comfortably make an informeddecision regarding their health. One size does not fitall.
There are some limitations to this study. A cross-sectional study does not offer the benefit of observingthe patients’ health care decision making over time.Since decisions are contextual and reflect situation-be-havior combinations,53 it is important to have longitu-dinal studies in which patients make decisions acrosssituations. Although our sample size of 12 participantsmay at first glance appear inadequately small, the datawe elicited from the participating subjects were ex-tremely rich (more than 100 decision incidents). This isbecause, as is customary in qualitative research, actualsample size is “not dependent on the numbers of par-ticipants or subjects, but rather on the numbers of inci-dents that those subjects can provide.”76 Therefore, thenumber of participants (n) is not the critical question
when considering adequacy of the sample. Instead, ifone is able to sample participants who have experi-enced multiple incidences of the critical element orphenomenon of interest, every participant can providehundreds of “data bits.”39,77,78 Although our small sam-ple clearly does not permit any firm generalizations tobe made, our findings provide the basis for future re-search in which a much larger confirmatory samplingwill be used to validate and verify any emergent theoryrelated to CAM-related decision making.
Along the same lines, the participants were limitedto southern Arizona and may not be a good representa-tion of the population in general. Only patients withchronic rheumatological conditions were included.Although a convenient group to study when consider-ing CAM, our findings among these patients may not begeneralizable to other patient populations. The open-ended nature of the interview process, although usefulfor eliciting descriptive information from participants,allows more room for investigator bias than does a stan-dardized interview. Efforts were made to ask similarquestions of all participants, but again, as the explor-atory nature of the study indicated, questions evolvedas the study progressed. Those who participated laterin the study may have been asked questions in a differ-ent way than those who participated earlier in thestudy. In addition, some different and/or additionalquestions were presented to later participants based oninformation obtained from earlier participants. Be-cause the same information was not obtained from allpatients, the validity of comparing them to each otheris limited.
CONCLUSIONS, IMPLICATIONS,AND FUTURE DIRECTIONS
Notwithstanding the preliminary and exploratorynature of our findings, we believe that our study mayhave some important implications in the way we thinkabout advising patients with respect to CAM utiliza-tion. Specifically, the following 3 points are worthmentioning.
1. Different patients may utilize markedly differentdecision-making paths to arrive at health care–relateddecisions. Some of the aspects of these paths that mayvary include value and belief systems, what informa-tion resources are used and deemed credible, how toassign credibility to a source, and degree of activesearching for information. As a consequence, differentpatients may appreciate different forms of informationwhen making decisions regarding their health. In ad-
76 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
dition, these differences in decision paths may ex-plain why some patients are more likely to use CAM.
2. Health care providers should be sensitive to these dif-ferences and seek to tailor the information they pro-vide to patients according to those patients’ needs.Clearly, to do this, the provider must not only beknowledgeable in CAM but also be sensitive to the pa-tient’s desire and belief system. The practice of medi-cine requires good rapport and mutual respect be-tween patient and practitioner so that an alliance maybe forged around a common agenda. This is virtuallyimpossible when a practitioner is judgmental and crit-ical and stifles patient inquiry and partnership. It isimportant for practitioners to understand patients’reasons for using and refusing particular healing mo-dalities and for identifying particular modalities as ei-ther central or peripheral to their life. This requires notonly a consideration of the meaning of an illness forthe afflicted but also the meaning of healing modali-ties viewed not only individually but also in relationto other modalities. Assessing health practices(broadly defined) requires placing them in context. La-beling a health practice alternative may be misleadingif it is integrated within one’s life as normal practice.What may be alternative for one individual could bemainstream for another. For example, for many pa-tients, routine use of mind-body practices such asmeditating is not alternative at all. Thus, the medicalpractitioner must consider the patient’s viewpoint andexperience. Not to do so may compromise thetherapeutic relationship, impede compliance, andlead to treatment failure.79
3. To better understand how decision-making processeswork in different patients and how health care provid-ers may recognize these differences, more researchthat cuts across disease processes and geographical ar-eas needs to be conducted. Although patient partici-pation in decision making is increasingly being re-garded as desirable ethically in terms of patientautonomy and self-determination, legally with respectto informed consent requirements, and socially fromthe perspective of consumer rights advocates and pa-tient charters, the reality is that there is a lack of a gen-eral accepted definition of what is a “good” decision.80
Thus, better understanding of what is involved in thedecision of whether to use CAM is much needed sothat physicians will provide not only better advice totheir patients but also advice that patients will valuebecause it fits into their natural process of decisionmaking. Decisions are never taken in a vacuum but in asocial context with varying degrees and types of socialinfluence. Therefore, we advocate that future researchshould use a naturalistic approach to decision makingrather than a normative one.81 To this end, future re-search should further identify and describe the basic
social, social-psychological, and social-structural pro-cesses inherent in these decision-making processes.We hope that this would lead to the development of agrounded theory that explicates and differentiatesthese decision-making processes to determine thetype of health care interventions (allopathic,alternative, and complementary) that patients seek.
Our quest to find out whether some patients are, bynature, “alternative” patients is by no means a conten-tion that there is an implicit hierarchy in terms of cor-rectness. Rather, it reflects the fact that what decisionmakers themselves bring to the situation must also beconsidered. Our study shows clearly that patients varyin their expectations, beliefs, experience, appraisal ofthe situation, affective state, motivation, and goals.Hence, providing patients with just the evidence is notenough since “evidence does not make decisions, peo-ple do.”82 Thus, the use of evidence is most successfulwhen patient and societal factors such as choice,efficiency, and equity are factored into the decision-making process, whether at the clinical, system, or pol-icy level. Global evidence still needs localized decisionmaking.83 As the late John Eisenberg put it, “World-wide access to evidence-based clinical decision mak-ing must coexist with respect for individual decisionmaking shaped by local culture and circumstances.This is the balance between globalizing the evidenceand localizing the decisions that will improve deliveryof health care worldwide.”84
REFERENCES
1. Deyo RA. Tell it like it is. Patients as partners in medical decisionmaking. JGIM. 2000;15:752–4.2. Barry MJ. Health decision aids to facilitate shared decision mak-
ing in office practice. Ann Int Med. 2002;136:127–35.3. Braddock CH, Edwards KA, Hasenberg NM, Laidley TL,
Levinson W. Informed decision making in outpatient practice: time toget back to basics. JAMA. 1999;282:2313–20.4. Deyo RA. A key medical decision maker: the patient. BMJ.
2001;323:466–7.5. Gwyn R, Elwyn G. When is a shared decision not (quite) a shared
decision? Negotiating preferences in a general practice encounter.Soc Sci Med. 1999;49:437–47.6. Ferriman A. Patients need to be more involved in care decisions.
BMJ. 2001;323:10.7. Ramos-Remus C, Watters CA, Dyke L, Suarez-Almazor ME, Rus-
sell AS. Assessment of health locus of control in the use ofnonconventional remedies by patients with rheumatic disease. JRheumatol. 1999;26:2468–74.8. National Center for Complementary and Alternative Medicine.
Understanding complementary and alternative medicine. What iscomplementary and alternative medicine? Available from: http://nccam.nih.gov/health/whatiscam/. Accessed 25 September 2002.
DECISION PSYCHOLOGY 77
PATIENTS’ DECISION PATHS FOR CAM
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
9. Wootton JC, Sparber A. Surveys of complementary and alterna-tive medicine: part I: general trends and demographic groups. J AltComp Med. 2001;7:195–208.10. Ernst E. Prevalence of use of complementary/alternative medi-cine: a systematic review. Bull of WHO. 2000;78:252–7.11. Harris P, Rees R. The prevalence of complementary and alterna-tive medicine use among the general population: a systematic reviewof the literature. Comp Ther Med. 2000;8:88–96.12. Halliday J, Taylor M, Jenkins A, Reilly D. Medical students andcomplementary medicine. Compl Ther Med. 1993;1(Suppl):32–3.13. Hopper I, Cohen M. Complementary therapies and the medicalprofession: a study of medical students’ attitudes. Altern Ther HealthMed. 1998;4:68–73.14. Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A reviewof the incorporation of complementary and alternative medicine bymainstream physicians. Arch Int Med. 1998;158;2303–10.15. Winslow LC, Shapiro H. Physicians want education about com-plementary and alternative medicine to enhance communicationwith their patients. Arch Intern Med. 2002;162:1176–81.16. Pelletier KR, Astin JA, Haskell WL. Current trends in the integra-tion and reimbursement of complementary and alternative medicineby managed care organizations (MCOs) and insurance providers:1998 update and cohort analysis. Am J Health Promot. 1999;14;125–33.17. White House Commission on Complementary and AlternativeMedicine Policy Final Report (March 2002). Available from: http://whccamp.hhs.gov/finalreport.html. Accessed 25 September 2002.18. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR,Delbanco TL. Unconventional medicine in the United States. N Engl JMed. 1993;328:246–52.19. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternativemedicine use in the United States, 1990-1997: results of a follow-upnational survey. JAMA. 1998;280:1569–75.20. Astin JA. Why patients use alternative medicine: results of a na-tional study. JAMA. 1998;279:1548–53.21. Vincent C, Furnham A. Why do patients turn to complementarymedicine? An empirical study. Br J Clin Psychol. 1996;35:37–48.22. Ernst E, Pittler MH, Stevinson C, White A, Eisenberg D, editors.The Desktop Guide to Complementary and Alternative Medicine: AnEvidence-Based Approach. Edinburgh, UK: Mosby; 2001.23. Sampson W. The braid of the “alternative medicine” movement.Scientific Review of Alternative Medicine. 1998;2:4–11.24. Piscitelli S. Preventing dangerous drug interactions. J AmPharma Ass. 2000;40:44–5.25. Ruschitzka F, Meier PJ, Turina M, Luscher TF, Noll G. Acute hearttransplant rejection due to Saint John’s wort. Lancet. 2000;355:548–9.26. Angell M, Kassier JP. Alternative medicine—the risks of untestedand unregulated remedies. N Engl J Med. 1998;339:839–41.27. Wynia MK, Eisenberg DM, Wilson IB. Physician-patient commu-nication about complementary and alternative medical therapies: asurvey of physicians caring for patients with human immunodefi-ciency virus infection. J Alt Comp Med. 1999;5:447–56.28. Montibrand MJ. Freedom of choice: an issue concerning alter-nate therapies chosen by patients with cancer. Oncol Nurs Forum.1993;20:195–210.29. Streubert HJ, Carpenter DR. Qualitative Research in Nursing: Ad-vancing the Humanistic Imperative. Philadelphia: Lippincott, Wil-liams & Wilkins; 1999.30. Thorne S. Nursing Praxis: Knowledge and Action. ThousandOaks, CA: Sage; 1997.31. Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA:Sage; 1985.
32. Lawrence R, Helmick CG, Arnett FC, Deyo RA, Felson DT,Giannini EH. Estimates of the prevalence of arthritis and selectedmusculoskeletal disorders in the United States. Arthritis Rheum.1998;41:778–99.33. Rao JK, Mihaliak K, Kroenke K, Bradley J, Tierney WM,Weinberger M. Use of complementary therapies for arthritis amongpatients of rheumatologists. Ann Intern Med. 1999;131:409–16.34. Chandola A, Young Y, McAlister J, Axford JS. Use of complemen-tary therapies by patients attending musculoskeletal clinics. J RoyalSoc Med. 1999;92:13–6.35. Camara K, Danao-Camara T. Awareness of, use and perceptionsof efficacy of alternative therapies by patients with inflammatoryarthropathies. Hawaii Med J. 1999;58:329–32.36. Boisset M, Fitzcharles MA. Alternative medicine use by patientsin a universal health care setting. J Rheumatol. 1994;21:148–52.37. Ernst E. Usage of complementary therapies in rheumatology: asystemic review. Clin Rheumatol. 1998;17:301–5.38. Cronan TA, Kaplan RM, Kozin F. Factors affecting unprescribedremedy use among people with self-reported arthritis. Arthritis CareRes. 1993;6:149–55.39. Glaser B, Strauss A. The Discovery Of Grounded Theory: Strate-gies for Qualitative Research. New York: Aldine de Gruyter; 1967.40. Fontana L, Frey D. Constructivist methodology. In: Denzin NK,Lincoln YS, editors. Handbook of Qualitative Research. 2nd ed.Thousand Oaks, CA: Sage; 2000.41. Spradley AP. The Ethnographic Interview. New York: Holt,Rinehart and Winston; 1979.42. Silverman D. Analyzing talk and text. In: Denzin NK, Lincoln YS,editors. Handbook of Qualitative Research. 2nd ed. Thousand Oaks,CA: Sage; 2000. p. 821–34.43. Wallston KA, Stein MJ, Smith CA. Form C of the MHLC scales: acondition-specific measure of locus of control. J Pers Assess.1994;63:534–53.44. Gurmankin AD, Baron J, Hershey JC, Ubel PA. The role of physi-cians’ recommendations in medical treatment decisions. Med DecisMaking. 2002;22:262–71.45. Guadagnoli E, Ward P. Patient participation in decision-making.Soc Sci Med. 1998;47:329–39.46. McKinstry B. Do patients wish to be involved in decision makingin the consultation? A cross sectional survey with video vignettes.BMJ. 2000;321:867–71.47. Pierce PF. When the patient chooses: describing unaided deci-sions in health care. Human Factors. 1996;38:278–87.48. Coates JR, Jobst KA. Integrated health care: a way forward for thenext five years? A discussion document from the Prince of Wales’sInitiative on Integrated Medicine. J Alt Comp Med. 1998;4:209–47.49. Dalen EJ. ’Conventional” and “unconventional” medicine. Canthey be integrated? Arch Intern Med. 1998;158:2179–81.50. Integration of complementary and alternative medicine: a healthservices research perspective. RFA: AT-01-001. Available from: http://grants2.nih.gov/grants/guide/rfa-files/RFA-AT-01-001.html. Ac-cessed 25 September 2002.51. Faass N, editor. Integrating Complementary Medicine intoHealth Systems. Gaithersburg, MD: Aspen; 2001.52. Caspi O, Maizes V, Bell IR. The integrative medicine perspective:concepts, clinical application, implications for evidence-based prac-tice, and medical education. In press.53. Lewis JD, Strom BL. Balancing safety of dietary supplementswith the free market. Ann Intern Med. 2002;136:616–8.54. Weeks J. What makes a physician an expert in CAM? Med Econ.2000;77:109–10, 117.55. Hastie R. Problems for judgment and decision making. Ann RevPsychol. 2001;52:653–83.
78 • MEDICAL DECISION MAKING/JAN–FEB 2004
CASPI, KOITHAN, CRIDDLE
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from
56. Reaby LL. Breast restoration decision making: enhancing theprocess. Cancer Nurs. 1998;21:196–204.57. Mansell D, Poses RM, Kazis L, Duefield CA. Clinical factors thatinfluence patients’ desire for participation in decisions about illness.Arch Intern Med. 2000;160:2991–6.58. Snyderman R, Weil AT. Integrative medicine: bringing medicineback to its roots. Arch Intern Med. 2002;162:395–97.59. Bell IR, Caspi O, Schwartz GRE, et al. Integrative medicine andsystematic outcomes research: issues in the emergence of a newmodel for primary health care. Arch Intern Med. 2002;162:133–40.60. Redelmeier DA, Shafir E. Medical decision making in situationsthat offer multiple alternatives. JAMA. 1995;273:302–5.61. Kahneman D, Slovic P, Tversky A, editors. Judgment under Un-certainty: Heuristics and Biases. New York: Cambridge UniversityPress; 1982.62. Bell DE, Raiffa H, Tvesrky A, editors. Decision Making. NewYork: Cambridge University Press; 1988.63. Redelmeier DA, Rozin P, Kahneman D. Understanding patients?Decisions: cognitive and emotional perspectives. JAMA.1993;270:72–6.64. Becker GM, DeGroot MH, Marschak J. Stochastic models ofchoice behavior. Behav Sci. 1963;8:41–55.65. Tversky A. Elimination by aspects: a theory of choice. PsycholRev. 1972;79:281–99.66. Barthelemy JP, Mullet E. A model of selection by aspects. ActaPsychologica. 1992;79:1–19.67. Tversky A, Sattath S, Slovic P. Contingent weighting in judgmentand choice. Psychol Rev. 1988;95:371–84.68. Bockenholt U, Albert D, Aschenbrenner M. The effects of attrac-tiveness, dominance, and attribute differences on information acqui-sition in multiattribute binary choice. Organizational Behavior andHuman Decision Processes. 1991;49:258–81.69. Sirois FM, Gick ML. An investigation of the health beliefs andmotivations of complementary medicine clients. Soc Sci Med.2002;55:1025–37.70. Andersen R, Newman JF. Societal and individual determinantsof medical care utilization in the United States. The Milbank Memo-rial Fund Quarterly. 1973;51:95–124.
71. Pawluch D, Cain R, Gillet J. Ideology and alternative therapy useamong people living with HIV/AIDS. Health Canadian Soc.1994;2:63–84.72. Brugmann M, Kugler J, Galm O, Fabry U, Osieka R, Neuser J. Psy-chological determinants for the use of complementary medicine inoncology patients [abstract 247]. Paper presented at the 6th AnnualConference of the International Society for Quality of Life Research,Barcelona, Spain, November 1999.73. Delate T, Griffis DL, Coons SJ. Determinants of the use of comple-mentary and alternative medicine by persons with HIV. In press.74. Brown CM, Segal R. Ethnic differences in temporal orientationand its implications for hypertension management. J Health SocBehav. 1996;37:350–61.75. Fries CJ, Menzies KS. Gullible fools or desperate pragmatists? Aprofile of people who use rejected alternative health care providers.Can J Pub Health. 2000;91:217–9.76. Strauss A, Corbin J. Basic of Qualitative Research. Newbury Park,CA: Sage; 1990.77. Glaser B. Theoretical Sensitivity. San Francisco: University ofCalifornia San Francisco Press; 1978.78. Chamaz K. Grounded theory: objectivist and constructivistmethods. In: Denzin NK, Lincoln YS, editors. Handbook of Qualita-tive Research. 2nd ed. Thousand Oaks, CA: Sage; 2000.79. Campbell SM, Roland MO, Buetow SA. Defining quality of care.Soc Sci Med. 2000;51:1611–25.80. Broadstock M, Michie S. Process of patient decision making: the-oretical and methodological issues. Psychol Health. 2000;15:191–204.81. MacPhail-Wilcox B, Bryant HD. A descriptive model of decision-making: review of idiographic influences. J Res Develop Ed.1988;22:7–22.82. Haynes RB, Devereaux PJ, Guyatt GH. Physicians? And patients?Choices in evidence based practice. BMJ. 2002;324:1350.83. Schneider EC, Eisenberg JM. Strategies and methods for aligningcurrent and best medical practices. The role of information technolo-gies. West J Med. 1998;168:311–8.84. Eisenberg JM. Globalize the evidence, localize the decision:evidence-based medicine and the international diversity. Health Af-fairs. 2002;21:166–8.
DECISION PSYCHOLOGY 79
PATIENTS’ DECISION PATHS FOR CAM
© 2004 Society for Medical Decision Making. All rights reserved. Not for commercial use or unauthorized distribution. at PENNSYLVANIA STATE UNIV on April 16, 2008 http://mdm.sagepub.comDownloaded from