What the phlebologist should know about local anesthetics
Transcript of What the phlebologist should know about local anesthetics
Review Article
What the phlebologist should knowabout local anesthetics
Stefan De Hert1, Luc De Baerdemaeker1 andMarianne De Maeseneer2,3
Abstract
An increasing number of phlebological interventions are performed under local and tumescent anesthesia. Although the
modern local anesthetic agents are generally perceived as being effective and safe drugs, the administration of these drugs
may be associated with a number of adverse events. It is therefore mandatory that everyone who uses these compounds
has insight into the pharmacological actions of these drugs and is capable of recognizing and adequately treating potential
adverse events. The present narrative review summarizes the current knowledge on mechanisms of action of the most
important local anesthetic drugs and reviews the potential adverse effects as well as their treatment.
Keywords
Anaesthesia, pharmacology, physiology
Introduction
Local anesthesia refers to a reversible anesthetic tech-nique in which a part of the body is made insensitive topain in order to perform surgical or procedural inter-ventions without discomfort to the patient. In contrastto general anesthesia, which implies a period of uncon-sciousness, the patient under local anesthesia is awareof what is going on. By definition, local anesthesiarefers to blocking of nociception of a small localizedarea of the body such as a part of the skin and sub-cutaneous tissue. However, local anesthetics are alsoused to block entire nerve pathways in the case of locor-egional anesthesia or even to block pain sensation in anentire part of the body such as with epidural and/orspinal anesthesia. The latter may be associated with avariable degree of motor block.
Whereas locoregional anesthetic techniques are pri-marily the field of expertise of anesthesiologists, the useof local anesthetic infiltrations to facilitate minor pro-cedures belongs to the daily practice of every physicianperforming surgery. The introduction of tumescentanesthesia, in which pain perception is blocked inlarger parts of the body by subcutaneous infiltrationof higher volume solutions of local anesthetic agents,has broadened even more the use of these agents indaily surgical practice. Nowadays, an increasingnumber of phlebological interventions are performedunder local or tumescent anesthesia.
While local anesthesia is generally perceived as beingsafer than general anesthesia, the use of local anestheticdrugs may be associated with local and systemic toxiceffects, the severity of which may greatly depend on thetype of drug used and the amount administered.Therefore, it is mandatory that every clinician usingthese compounds is aware of the pharmacology, themechanisms of action and the potential side effects ofthese drugs.
The present review summarizes the current know-ledge on local anesthetic agents when used in dailypractice for treatments under local or tumescent anes-thesia. This review does not include the different locor-egional techniques since these constitute a specificanesthesiological issue, not belonging to the usual prac-tice of the phlebologist. Moreover, only the local
1Department of Anesthesiology, Ghent University Hospital, Ghent,
Belgium2Department of Dermatology, Erasmus Medical Center, Rotterdam, The
Netherlands3Faculty of Medicine and Health Sciences, University of Antwerp,
Antwerp, Belgium
Corresponding author:
Stefan De Hert, Department of Anesthesiology, Ghent University
Hospital, De Pintelaan 185, B-9000 Ghent, Belgium.
Email: [email protected]
Phlebology
2014, Vol. 29(7) 428–441
! The Author(s) 2013
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/0268355513501303
phl.sagepub.com
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
anesthetic agents that are relevant for phleblogicalpractice will be discussed.
Peripheral nerve conduction
Anatomy of the peripheral nerve
A typical peripheral nerve consists of several axon bun-dles (Figure 1). Each axon has its proper connectivetissue layer which covers the endoneurium. Each axonbundle is covered by a second connective tissue layer,the perineurium, while the entire nerve is surrounded bya separate outer sheath, the epineurium. Most largemotor and sensory fibers are surrounded by severallayers of myelin that consist of the plasma membranesof Schwann cells that are wrapped around the axonduring its outgrowth. Myelin facilitates the speed ofaction potential conduction throughout the axon mem-brane by insulating it from the surrounding conductingmedium. Thereby it forces the current to propagatethroughout the neural membrane to the nodes ofRanvier, which are periodic interruptions in themyelin sheath. Table 1 summarizes the classificationof the peripheral nerves according to the fiber sizeand the physiologic properties.
As a general rule small nerve fibers are more suscep-tible to local anesthetics than large fibers. However,other factors like myelinization and relative positionof the fibers within a nerve (mantle vs. core) may alsoplay a role. About three nodes of Ranvier need to beblocked in order to block the transmission of the actionpotential. The smallest nerve fibers are non-myelinated
and are blocked more readily than the myelinatedfibers. However, at similar size, myelinated fibers areblocked before non-myelinated fibers. In general, auto-nomic fibers, small non-myelinated C fibers (mediatingpain, warm temperature and touch), and small myelin-ated Ad fibers (mediating pain and cold temperature)are blocked before Aa, Ab, and Ag fibers (motor, pro-prioception, touch and pressure).
In order to reach their site of action, local anestheticsneed to diffuse through the connective tissue layers toreach the axon plasma membrane. Like all biologicalcell membranes, the axon plasma membrane consists ofa phospholipid bilayer with long hydrophobic fattyacid tails that project in the center of the membraneand polar hydrophilic heads which face the cytoplasmintracellularly and the interstitial fluid outside the cell.Within this phospholipid layer, proteins are localizedserving various functions such as acting as receptorsfor signal transduction or as ion channels that regulateelectrical balance over the cell membrane and initiatepropagation of the action potential.
Physiology of nerve conduction
The neural membrane maintains an electrical trans-membrane gradient of 60 to 90mV. In resting condi-tions, chemical and electrical gradients are establishedacross the nerve cell membrane by various ion channels(leak channels or non-gated channels: found in theplasma membrane throughout the neuron, alwaysopen and responsible for the resting membrane poten-tial; ligand-gated channels: open or closed in response to
Figure 1. Schematic representation of the anatomical structure of a peripheral nerve.
De Hert et al. 429
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
the binding of a chemical messenger to a specific recep-tor in the plasma membrane; and voltage-gated chan-nels: open or closed in response to changes inmembrane potential and responsible for the initiationand propagation of action potentials).
The resting membrane potential depends on the con-centration gradient of different ions (primarily sodiumand potassium ions) across the plasma membrane andthe presence of ion channels in the plasma membrane.Sodium ions are more concentrated at the outside ofthe cell, whereas potassium ions are more concentratedat the inside. As a consequence, there is a driving forceto push sodium into the cell and potassium outwards.The cell membrane is to a certain extent permeable toions but in resting conditions, the number of openpotassium channels exceeds by far the number ofopen sodium channels. As a consequence, the cell mem-brane is about 25 times more permeable to potassiumthan to sodium. The concentration gradient across themembrane is mainly maintained actively by the Naþ/Kþ pump which transports three sodium ions out of thecell and two potassium ions into the cell per molecule ofadenosine triphosphate (ATP) hydrolyzed.
During the action potential a large, rapid depolariza-tion occurs during which the membrane potential actu-ally reverses from approximately �70mV to þ30mV.Once initiated, the action potential is propagated alongthe entire length of the axon without any decrease instrength. The generation of an action potential isbased on an acute change in the plasma membrane per-meability for sodium. This causes the transmembranepotential to rise which is called ‘‘depolarization’’.
The depolarization of a section of the plasma membranecreates a difference in potential with the adjacent areas.This generates an electrical current, resulting in thedepolarization of these adjacent areas and a wave ofdepolarization runs along the axon.
The second phase of an action potential is the ‘‘repo-larization’’, during which the membrane potentialreturns to its resting levels. Within 1ms after the risein sodium permeability, this decreases rapidly, at whichtime, potassium permeability increases and potassiummoves across its electrochemical gradient outside thecell (Figure 2).
These acute changes in permeability are caused byopening and closing of the voltage-gated sodium andpotassium channels located in the plasma membraneof the axon. In myelinated axons, these channels areconcentrated at the nodes of Ranvier, whereas in thenon-myelinated fibers, the sodium channels are distrib-uted evenly along the axon. The voltage-gated sodiumchannels consist of a pore forming a-subunit and 1 or 2b-subunits. The sodium conducting part of the channelis the a subunit, a single polypeptide protein with a rela-tive molecular mass of about 260,000. The a-subunit iscomposed of four domains (D1-4) which contain six hel-ical transmembrane segments (S1-6) (Figure 3).1–4
Upon nerve stimulation, a series of conformationalchanges occur running through four functional states:resting, activated, inactivated and deactivated. Thesodium channel can conceptually be viewed as havingtwo functional gates: an outer gate and an inner gate,the position of which varies according to the membranepotential. In the resting state (�70 to �90mV) the
Table 1 Classification of the peripheral nerve fibers.
Fiber type
Sensory
classification Function
Diameter
(mm)
Conduction
(m/s)
Local
anesthetic
activity Myelinisation
Aa Motor 12–20 70–120 þ yes
Aa type Ia Proprioception 12–20 70–120 þþ yes
Aa type Ib Proprioception 12–30 70–120 þþ yes
Ab type II Proprioception 5–12 30–70 þþ yes
Touch pressure
Ad type III Pain 2–5 12–30 þþþ yes
Cold temperature
Touch
Ag Motor (muscle spindle) 3–6 15–30 þþ yes
B Preganglionic <3 3–14 þþþþ some
Autonomic fibers
C dorsal root type IV Pain, touch 0.4–1.2 0.5–2 þþþþ no
Warm and cold temperature
C sympathetic Postganglionic 0.3–1.3 0.7–2.3 þþþþ no
Sympathetic fibers
430 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
outer gate is closed but the inner gate is open. On nervestimulation the outer gate opens, leading to the rapidinflux of sodium along the electrochemical gradient(activated state)(Figure 4). Upon complete depolariza-tion, the inner gate closes, blocking further sodiuminflux (inactivated state) and the resting potential isrestored by the opening of voltage-gated potassiumchannels. The model for the latter channels describes
only a single gate that opens more slowly in response todepolarization than the sodium channels so that atapproximately the same time sodium inactivationgates close (1 to 2ms after depolarization to threshold),the potassium channels begin to open. Potassium chan-nels are composed of four separate polypeptide chains,each containing one domain. When the membranepotential reaches about �60mV, the outer gate of the
Figure 3. Schematic representation of the voltage-gated sodium channel a-subunit. This subunit consists of four domains each
containing six segments which span the neural membrane.
Figure 2. The ionic fluxes during a neuronal action potential. The rapid depolarization is caused by a rapid increase in sodium
permeability (P Na) that allows sodium to enter the cell. Repolarization occurs due to the slower increase in potassium permeability
(P K) resulting in an increased outflow of potassium out of the cell as compared to resting conditions.
De Hert et al. 431
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
sodium channel closes and this channel is then in thedeactivated state. During the inactivated and deacti-vated state, the nerve is refractory to stimulation.Resting ion balance is then restored by the activeNaþ/Kþ pump.
Mechanisms of action of local anesthetics
Local anesthetics reversibly block the propagation ofthe action potentials in the axons by inhibiting theinflux of sodium. After diffusion from the site of injec-tion through the neural membrane into the axoplasm,they enter the sodium channel and prevent these fromassuming the active ‘‘open’’ state. This inhibition isobtained by a reversible binding with the D4-S6 partof the a-subunit of the voltage-gated sodium channel(Figure 3).2–4 This site of action is intracellular andtherefore the local anesthetics need to diffuse acrossthe lipophilic lipoprotein layer.
Chemistry
The local anesthetic molecule consists of three differentcomponents: a lipophilic aromatic ring, an intermediate
ester or amide chain and a hydrophilic terminal amine(Figure 5). The linking chain is used to classify theagents as an ester or amide. All local anestheticagents used in phlebological practice are amino-amide
Figure 4. The hypothetical model for the operation of the voltage-gated sodium channels. These channels are schematically rep-
resented as having two gates: an activation gate and an inactivation gate. At rest (a), the sodium inactivation gate is open and the
activation gate is closed but is capable of opening in response to a depolarizing stimulus. Following a depolarizing stimulus (b) to the
threshold potential, both the activation and the inactivation gates are open and sodium can move through the channel. Approximately
1 ms after the depolarizing stimulus (c), the inactivation channel closes and remains closed until the cell has repolarized to the resting
state.
Figure 5. Basic structure of the local anesthetics. All local
anesthetics contain three different parts: a lipophilic part, a
linkage part and a hydrophilic part. The chemical composition of
these different parts determines the pharmacological properties
of the different compounds.
432 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
linked ester from which lidocaine is the prototype(Figure 6). The aromatic ring is responsible for thelipid solubility of the compound. Lipid solubility canbe further enhanced by aliphatic substitutions at spe-cific locations (designed with R in Figure 5). Increasedlipid solubility enhances diffusion through the nervesheaths and the neural membranes. The terminalamine may exist in a tertiary form, which is lipid sol-uble or in a quaternary form, which is positivelycharged (cation) and makes the molecule water soluble.The structure of the terminal amine allows the localanesthetic to exist either in a lipid-soluble or a water-soluble configuration.
To be stable in solution, the local anesthetic shouldbe formulated as a hydrochloride salt. In this form, themolecules are in a quaternary, water-soluble state at themoment of injection. In this configuration, however,the local anesthetic is not able to pass into the neuronand therefore the molecule needs to be converted to itstertiary lipid-soluble configuration. This tertiary config-uration passes readily through the cell membranes;hence, the speed of onset of local anesthesia willdepend on the relative concentration of unchargedlocal anesthetic molecules injected at a physiologicalpH of 7.4 (Figure 7). The proportion of the chargedcationic form with respect to the unchanged baseform depends on the dissociation constant (pKa¼ thevalue at which 50% of either form of the molecule ispresent in the solution) of the molecule and this pro-portion can be calculated from the Henderson-Hasselbach equation:
log cation=uncharged½ � ¼ pKa localanestheticð Þ
� pH solution,7:4forplasmað Þ
Local anesthetics are weak bases (pKa between 7.6and 8.9) and therefore a greater proportion of the mol-ecules exist in their quaternary, water-soluble form(cation) when injected into normal tissue. Esters tendto have a higher pKa value than amides. As a conse-quence, the higher the pKa of the local anesthetic is, thefewer molecules are available in their lipid-soluble con-figuration which will slow down onset of anestheticaction.5–8 Another consequence is that when the anes-thetic is injected in an acidic environment (pH< 7.4)such as is the case for inflamed tissues, it will favorthe quaternary water-soluble configuration even fur-ther. This has been suggested as a possible explanationfor the difficulties encountered when trying to anesthe-tize inflamed or infected tissue. Conversely, theco-administration of sodium bicarbonate to increasethe pH of the local anesthetic solution will shift theconfiguration of the molecule towards a higher
concentration of the tertiary lipid-soluble configur-ation, which will enhance onset of anesthetic action.
Of note, once the tertiary molecules have entered theneuron, they re-ionize to the quaternary form, which is
Figure 6. Chemical structure of the different local anesthetic
agents discussed in this review.
De Hert et al. 433
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
the configuration that is actually responsible for theblocking of the sodium channel.
Stereoisomerism
Some local anesthetics exhibit stereoisomerism. Twomolecules are described as stereoisomers of each otherif they are made of the same atoms, connected in thesame sequence, but the atoms are positioned differentlyin space (differentiated according to the direction inwhich they deflect polarized light: left (S) or right (R)).Their physicochemical properties are usually similar buttheir effects on biological receptors may differ substan-tially. Stereoisomerism is found for bupivacaine, prilo-caine, ropivacaine, etidocaine and mepivacaine. Thesedrugs are usually marketed as racemic mixtures (equalconcentrations of both isomers), but the more recentlyintroduced local anesthetic agent levobupivacaine(S-bupivacaine) and ropivacaine (S-ropivacaine) onlycontain the S-stereoisomer. Whereas the local anestheticactivity is similar to the racemicmixture, the toxic profileof these isomers is significantly lower.
Pharmacology
Local anesthetics vary in their relative potency, time ofonset and duration of action. Differences in relativepotency and time of action onset essentially relate to a
difference in lipid-solubility of the particular local anes-thetic molecule. With higher lipid solubility, the relativepotency is increased and the time of onset is faster.The property of lipid solubility is determined by thearomatic ring and its substitutes, together with thestructure of the tertiary amine. Lipid solubility is quan-tified in the laboratory by measurement of the relativedistribution of the local anesthetic between a referenceaqueous phase and a non-aqueous solvent phase. Thedistribution of the substance between the two phasesallows for calculation of the solvent partition coeffi-cient. The higher this partition coefficient, the higherthe lipid solubility. Local anesthetics with higher lipidsolubility usually require lower concentrations of thedrug to achieve a similar anesthetic block.
Duration of action is related to differences of thedrugs in their affinity for protein. Local anestheticsbind to plasma and tissue proteins. The higher the pro-tein binding, the longer the anesthetic action. Durationof action also depends on the time that the local anes-thetic remains in the vicinity of the target tissue, whichare the neural fibers. Therefore, vasoconstrictors aresometimes associated to the local anesthetic in orderto slow down absorption and dissipation of the localanesthetic but also to decrease perioperative bleeding.This may be of particular importance with those anes-thetics that exhibit intrinsic vasodilating propertiessuch as for instance lidocaine.
Figure 7. Schematic representation of the local anesthetic action. When injected, the local anesthetic exists as an equilibrium
between its quaternary salt form (B-Hþ) and its tertiary base (B) form. The relative amount of both forms depends on the pKa of the
compound and the pH of the surrounding tissue. Only the B-form is lipid soluble and can penetrate the surrounding membranes of the
axon. This penetration is essential for the local anesthetic to perform its action. Upon diffusion in the axoplasma, the base form gains a
hydrogen ion (Hþ) and is ionized in its quaternary form (B-Hþ) which is responsible for the actual blockade of the sodium channel.
434 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
Clearance of the drug depends on the type of localanesthetic. Esters usually undergo rapid hydrolysis bynon-specific esterases. The metabolites have no localanesthetic effects but they may exhibit allergenic prop-erties. Amides on the contrary are mostly eliminated byhepatic metabolism and only a small fraction by renalclearance. Therefore, dose reduction is advised inpatients with liver disease. The rate of metabolism dif-fers between agents.
Physicochemical properties of the most importantlocal anesthetic agents used in phlebological practiceare summarized in Table 2.9,10
Main local anesthetic compounds used inphlebological practice
This part summarizes some properties of the main localanesthetic drugs used in clinical practice (Table 2)(Figure 6).
Amide local anesthetics
Lidocaine [2-diethylamino-N-(2,6-dimethylphenyl)-ethana-
mide]. Lidocaine is probably the most widely usedlocal anesthetic over the world. It produces a rapidonset of sensory nerve blockade, which may be asso-ciated with motor blockade when used in a locoregionaltechnique.11,12 Higher concentrations (5%) have beenassociated with neurotoxicity13 and some laboratorydata also suggest local neurotoxic effects at lowerconcentrations.14
Lidocaine is also a class Ib anti-arrhythmic agentthat can be used to treat ventricular arrhythmias.
Bupivacaine [1-butyl-N-(2,6-dimethylphenyl)-piperidine-2car-
boxamide]. Bupivacaine is a potent agent with a slowonset and a prolonged action duration.15 It is a popularanesthetic for longer lasting procedures. Compared tothe other local anesthetics, bupivacaine is markedly car-diotoxic. Systemic exposure to excessive quantities of
bupivacaine mainly results in central nervous systemand cardiovascular effects. For this reason, bupivacaineis contraindicated for intravenous regional anesthesiabecause of potential risk of tourniquet failure and sys-temic absorption of the drug.
Prilocaine [N-(2-propylaminopropionyl)-O-toluidine].
Prilocaine has a similar rapid onset of action than lido-caine but the anesthetic effect lasts longer.11 Tissueuptake and metabolism are fast and as a consequenceplasma levels decline swiftly.
Ortho-toluidine, one of the metabolites of prilocainebreakdown, is capable of converting ferrous iron toferric iron in hemoglobin, thereby causing methemoglo-binemia. Neonates are at particular risk because theirred blood cells are deficient in the enzyme, methemo-globin reductase. For this reason, prilocaine is bestavoided in pregnant women. Treatment of methemo-globinemia consists of administration of high oxygenconcentration together with intravenous methyleneblue (1mg/kg). Methylene blue is capable of reducingthe heme group from methemoglobin to hemoglobin.Of note, large doses (>7mg/kg) of methylene blue mayitself cause methemoglobinemia.
Prilocaine, together with lidocaine, is a basic com-pound of EMLA (Eutectic Mixture of LocalAnesthetics) cream. EMLA is used to provide topicalanesthesia. It penetrates the skin easily and is frequentlyapplied in pediatrics to reduce the pain of vein punctureor in adult patients if repetitive injections are needed tointroduce the local anesthetic over a substantial area,such as with tumescent anesthesia. Large doses maycause methemoglobinemia16 and therefore applicationon open wounds or inflamed skin should be avoided.
Levobupivacaine [(S)-1-butyl-N-(2,6-dimethylphenyl)piperidine-
2-carboxamide]. Bupivacaine is a racemic mixture oftwo isomers. While the two isomers have equal anes-thetic properties, the S-isomer has a safer profile withregard to potential adverse effects.17,18 Despite this
Table 2 Physicochemical properties of the main local anesthetic agents used in phlebological practice.
Agent MW pKa
Speed of
onset
Partition
coefficient Potency
Protein
binding (%) Duration Toxicity
Maximum
dose plain
(m/kg)
Maximum
dose with
VC (mg/kg)
AMIDES
Lidocaine 234 7.7 fast 43 intermediate 64 intermediate low 5 7
Bupivacaine 288 8.1 slow 346 high 95 long high 2 3
Prilocaine 220 7.9 fast 25 intermediate 55 intermediate low 5 8
Levobupivacaine 288 8.1 slow 346 high 96 long intermediate 2.5 3
Ropivacaine 274 8.1 slow 115 intermediate 94 long intermediate 2.5 4
MW: molecular weight; VC: vasoconstriction.
De Hert et al. 435
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
safer profile, there have been reports of adverse eventsmainly related to intravascular injection resulting inmassive overdose.19
Ropivacaine [N-n-propyl-2,6-pipecoloxylidide]. Ropivacainewas already synthesized in 1957 but was only intro-duced in clinical practice in the mid 1990s.20 It has asimilar onset and duration of action as bupivacaine butis less potent. In low concentrations it appears to have adifferential sensory/motor block when used as agent forlocoregional analgesia, with some degree of motorsparing.
The commercial form of ropivacaine is the purifiedS-isomer.21 This formulation has been claimed to causeless toxicity as bupivacaine,22 but still events of sys-temic toxicity have occurred.23,24
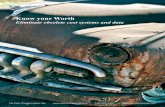
Tumescent local anesthesia
Tumescent anesthesia refers to the practice of injecting avery dilute solution of a local anesthetic agent, possiblycombined with a number of additives, into tissue, until itbecomes firm and tense (Figure 8).25,26 Initially, thistechnique was applied in the field of plastic surgery,especially for liposuction, where it has gained wideacceptance.26–30 With the introduction of less invasivetechniques for treatment of varicose veins and chronicvenous insufficiency, such as endovenous thermalablation with laser, radiofrequency energy or steam,this local anesthetic technique has also found itszindications in phlebology.31–34 So-called ‘classic’ surgi-cal procedures, consisting of high ligation at the junctionand stripping of the saphenous trunk, can perfectly be
performed in local tumescent anesthesia as well.32,33
Also in other peripheral vascular and endovascularinterventions, the usefulness of tumescent local anesthe-sia is explored.35
Lidocaine still is the most popular local anestheticagent used for tumescent anesthesia. The concentrationused for tumescent anesthesia ranges between 0.05 and1.5%, though higher concentrations may be needed forsurgery of more sensitive body areas. Other possiblelocal anesthetics include prilocaine,36 bupivacaine37
and ropivacaine.38 However, the use of prilocaine as atumescent agent when used at doses of 2.5mg/kg hasbeen associated with a 10% incidence of methemoglo-binemia (related to the production of its metaboliteO-toluidine).39 Bupivacaine has a slow rate of elimin-ation and carries the risk of potential severe side effects,reason why the American Society of Plastic Surgeonshas urged caution against its use.40 In addition, bupi-vacaine produces only a minimally prolonged durationof analgesia compared to lidocaine.41 Ropivacaine isless cardio- and neurotoxic than bupivacaine.42
For tumescent anesthesia, the local anesthetic isdiluted with a crystalloid solution, either normalsaline or compound sodium lactate. Some recommendcompound sodium lactate because it may cause less of aburning sensation on injection and causes a lowersodium load.43
Epinephrine may be added to the solution because itprolongs the local anesthetic effect; it slows the rate ofabsorption of the local anesthetic, permitting the use ofhigher doses, and it induces vasoconstriction whichmay reduce peri-procedural blood loss. The majorityof local anesthetics are weak vasodilators (with the
Figure 8. Duplex ultrasound of the great saphenous vein (GSV) at the medial side of the right thigh – transverse images. Left panel:
preoperative image showing an enlarged GSV (diameter 1.53 cm) in the saphenous compartment. The arrow points at the vein wall.
Right panel: perioperative image at the same site after introduction of a radiofrequency catheter (seen as central white dot with
acoustic shadow) and application of tumescent anesthesia (black halo) around the GSV (arrow) which has clearly shrunk.
436 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
exception of cocaine and ropivacaine that have weakvasoconstrictive properties) and this effect may enhanceperiprocedural bleeding, if no epinephrine is asso-ciated.44 In order to limit the incidence of importantsystemic side effects such as tachycardia and/or hyper-tension, it is recommended not to exceed a total dose ofepinephrine of 0.07mg/kg.40
Sodium bicarbonate is added to the mixture for sev-eral reasons. Alkalinisation of the mixture hastens theonset of the anesthetic block. It shifts the equilibriumtowards the uncharged lipid soluble moiety and there-fore enhances diffusion through the lipid layer (seeabove). In addition, because the commercially availablelocal anesthetic solutions are slightly acidic and maycause pain on injection, the addition of sodium bicar-bonate neutralizes the pH to a more physiologicalrange and will reduce the discomfort of injection.45
Finally, it has been suggested that the dissolvedcarbon dioxide which is created during the bufferingprocess of the local anaesthetic may enhance theeffect of the local anesthetic.46 Tumescent local anes-thetic mixtures usually contain 10mEq NaHCO3/L ofsolution. Too much alkalinisation may decrease aminesolubility and therefore results in local anesthetic pre-cipitation, which may be harmful to local tissues. Inparticular, care should be taken with bupivacainesince it may precipitate when alkalized.47
Adverse effects
Although the modern local anesthetic agents are gener-ally perceived as being very safe, every caregiver shouldbe aware of the fact that all of these compounds maypotentially cause adverse events. These adverse eventscan result from allergic reactions to the drug or may becaused by local or systemic toxicity.
Allergic reactions
Since the introduction of the amide local anesthetics,the number of allergic reactions to local anesthetics hasdeclined dramatically. Indeed, allergy to amides is con-sidered to be extremely rare and it is estimated that lessthan 1% of the reported cases of allergic reactions toamide local anesthetics are truly immune systemmediated responses.48 It is difficult to estimate the realincidence of allergic reactions to local anesthetics, notonly because of the inconsistency in methods of con-firmation but also because in many cases there has beenno confirmation of the presence of IgE to the offendingdrug by immunoblot testing.49
Local anesthetics are too small (<300Daltons) tobe antigenic by themselves but they may bind ashaptens to plasma or tissue proteins and then act asantigen. Usually, up to 14 days are required to develop
antibody production. Once sensitization has occurred,exposure, even to minimal fractions of the antigenicagent can invoke an antigen–antibody reaction. Thesereactions may vary from mild contact dermatitis to full-blown anaphylactic shock with bronchospasm, generaledema and cardiovascular collapse requiring promptresuscitation.
Allergic reactions attributed to local anesthetics arefrequently caused by other compounds in the solutionsuch as preservatives (methylparaben) or antioxidants(sulfites).50 Methylparaben is included to prevent bac-terial growth and sulfites are added to prevent the oxi-dation of vasopressors and are therefore only present invials containing the combination of local anestheticwith some kind of vasopressor. Latex allergy shouldalso be included in the list of differential diagnoses ofreactions to local anesthetics.51
When an allergic reaction to local anesthetics is sus-pected the patient should be referred for confirmationof the diagnosis. This type of investigation should beperformed by experienced individuals and should notbe attempted casually by every clinician.48 Skin pricktesting may be performed in those patients who haveexhibited mild symptoms but in those patients with ahistory of anaphylaxis, an in vitro testing is indicated.In the event a local anesthesia is required in a patientwith reported allergy to local anesthetics before ade-quate medical clearing was obtained, prilocaine withoutvasopressors was reported to be a good alternative.8 Ingeneral, esters are more likely to produce an allergicreaction than amides and by avoiding solutions thatcontain vasopressors, the allergenic bisulfites that areincluded as antioxidants are also avoided. Finally,alternatives such as the non-ester, non-amide, topicallocal anesthetic, dyclonine52 or the use of benzyl alco-hol as local anesthetic,53 have been described.
Toxic effects
Local anesthetics may also cause toxic effects. These areeffects that can directly be attributed to the agent admin-istered and are not mediated by an immunological cas-cade of events. These direct toxic effects can eithermanifest as a systemic toxic effect or as a local toxiceffect.
Systemic toxic effects. When local anesthetics areabsorbed in the systemic circulation, they may causeadverse central nervous system (CNS) effects and/oradverse cardiovascular effects.
The most frequent and prominent early warningsigns and symptoms of local anesthetic systemic toxicity(LAST) are CNS symptoms.54 About 60% of thepatients who develop LAST experience a typical pres-entation with evidence of progressively more severe
De Hert et al. 437
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
neurological symptoms, often prior to cardiovascularcollapse.55 These neurological symptoms are generallyexcitatory, possibly due to inhibition of inhibitory neu-rons via GABA (gamma-aminobutyric acid) receptors,and may include perioral and tongue paresthesia, ametallic taste, and dizziness, further developing toslurred speech, diplopia, tinnitus, restlessness, muscletwitching and finally convulsions. At higher plasmalevels there is a widespread sodium channel blockadewith general neuronal depression leading to coma.Occasionally, patients will rapidly progress to seizureswithout prior evidence of the CNS symptoms andrarely LAST may present as sudden cardiac arrest with-out any pre-emptive signs. Imminent cardiovasculartoxicity can be heralded by the development of brady-cardia with long PR-interval and widened QRS com-plexes followed by varying degrees of conduction block,the appearance of multifocal ectopic beats, re-entrancearrhythmias, tachycardia and ventricular fibrillation.
The plasma levels of local anesthetic drugs at whichtoxicity of respectively the cardiovascular system andthe CNS (cardiovascular/CNS ratio) occur may varysubstantially among the agents. Drugs like bupivicaine,ropivacaine and levobupivacaine have a lower ratio(signs of cardiovascular system toxicity occur atplasma levels close to the levels of CNS toxicity)while the less potent anesthetic agents such as lidocaineand mepivacaine have a higher ratio (signs of cardio-vascular system toxicity occur at substantially higherplasma levels than the levels of CNS toxicity). It hastherefore been suggested that, for these latter drugs,cardiovascular versus CNS toxicity ratios may permitseizure activity to serve as a marker of local anestheticoverdose. This may trigger caregivers to initiate therapyto avoid cardiovascular toxicity.54
The mechanisms by which cardiovascular symptomsand cardiac arrest occur also differ between the differ-ent local anesthetic agents. Local anesthetics with ashort clinical action duration and lower potency (suchas lidocaine) tend to depress cardiac contractility usu-ally without producing important cardiac arrhythmias.More potent local anesthetics with a longer actionduration (such as bupivacaine, levobupivacaine andropivacaine), on the contrary primarily produce cardiacarrhythmias, with less effects on cardiac contractility.As a consequence, optimal cardiovascular supportingtherapy may differ according to the local anestheticthat is responsible for the toxic effects. Inotropicdrugs may prove to be appropriate in case of lido-caine-induced cardiac toxicity but not for bupiva-caine-induced toxicity because of their propensity toinduce or exacerbate cardiac arrhythmias.
Treatment of toxic effects is generally supportive.56,57
Minor CNS symptoms usually do not need treatment assymptoms will subside swiftly if no additional local
anesthetic is administered. In the presence of seizures,patients should be protected of harming themselves andadequate ventilation and oxygenation should be pro-vided, if necessary with tracheal intubation. Seizuresusually can be terminated with small doses of short-acting barbiturates (midazolam 1 to 5mg) or propofol(50 to 100mg). Of note, propofol may induce cardiovas-cular instability and should not be used when the patientis hemodynamically unstable.
Lipid emulsion therapy has become a cornerstone inthe treatment of LAST, though failures to rescue havealso been described with this treatment. Themechanismsby which lipid emulsion counteracts LAST are still notelucidated but one theory suggests that the lipid emul-sion acts as a ‘‘lipid sink’’ within the systemic circulation;thereby allowing lipid-soluble drugs to dissolve in lipidmicelles, which are then gradually removed by the liver.The general agreement is that lipid emulsion therapyshould be initiated early during an episode of LAST inorder to prevent progression of mild symptoms to seiz-ures, coma, and cardiac arrest. The therapy consists ofinfusing a 20% lipid emulsion intravenously in bolus at adose of 1.5mL/kg over 1min, followed by a continuousinfusion at 0.25mL/kg/min. In case of persistent cardio-vascular collapse, the bolus dose can be repeated once ortwice. If blood pressure remains low, the infusion ratecan be doubled to 0.5mL/kg/min. The infusion shouldbe continued for at least 10min after circulatory stabilityhas been obtained. The recommended maximal dose ofthe lipid emulsion is 10mL/kg over the first 30min.56,57
The use of inotropics and/or vasopressors in case ofLAST is under discussion, since data on the effective-ness of medical supportive therapy are conflicting.Although there is currently no consensus, it is suggestedthat for the treatment of cardiac arrest from bupiva-caine the lipid emulsion therapy can be supplementedby a small (1 mg/kg) dose of epinephrine, combined withchest compression and mechanical ventilation.Additional epinephrine can be administered based onthe initial response to the drug.54
Local toxic effects. Direct cytotoxicity of the local anes-thetics has been described at the level of the neuronsand the muscles. Microscopic analysis has revealed thatlocal anesthetics potentially damage cell ultrastructureand can cause a local inflammatory reaction.58,59 Asmost of these observations come from laboratory stu-dies using high concentrations of local anesthetics andprolonged exposure, the clinical implications of a directlocal cytotoxic effect of local anesthetics remain debat-able. It is suspected that complaints of postproceduralparesthesia are rather primarily caused by direct nervedamage with puncture. General preventive measuresmay include ultrasound-guided puncture and avoidanceto use concentrated solutions.
438 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
Local anesthetic ‘‘resistance’’
There are sporadic reports in literature about localanesthetic resistance. While one is easily tempted toattribute such resistance to a technical failure or topoor quality of the injected solution, it should beremembered that inflammation may interfere withthe quality of local anesthetic block.60 However,even in the absence of inflammation, resistance toanalgesic effects of local anesthetics have beenreported. Except for a number of case reports, thereis only one study that systematically tested patients forresistance to local anesthetics.61 In this study, 250patients out of a total of 1198 patients interviewed,reported a history of suboptimal analgesia after localanesthetic infiltration and were tested for hypoesthesiaafter local anesthesia with lidocaine, mepivacaine andbupivacaine. Ninety patients were found to be hypoes-thetic only to mepivacaine, and an additional 43patients only to lidocaine. The remaining were hypoes-thetic to bupivacaine or to all local anesthetics tested.It was therefore suggested that in case of reportedresistance to local anesthetics, mepivacaine might bean alternative to be considered.
The underlying mechanisms for this reported resist-ance to local anesthetics remain to be determined.Resistance to local anesthetic has been reported inEhler Danlos type III patients62 and also in redheads,related to variation in the MC1R gene.63,64 This sug-gests that such resistance might have an underlyinggenetic reason and it was therefore postulated thatreceptor mutation at the level of the sodium channelmight be implied. It has also been suggested that suchresistance could be acquired after previous exposure totoxins,65 but this hypothesis has not been exploredfurther.
Conclusion
The use of local anesthesia allows to perform a varietyof phlebological procedures and avoids general anes-thesia. However, the administration of local anestheticscarries a potential risk of adverse events. Therefore, athorough understanding of the mechanisms of action,the risk profile of the different agents and the targetedtherapy for adverse events is mandatory knowledge foreveryone applying these agents in clinical practice.
Conflict of interest
None declared.
Funding
This research received no specific grant from any fundingagency in the public, commercial, or not-for-profit sectors.
References
1. AgnewWS, Levinson SR, Brabson J, et al. Purification of
the tetrodotoxin-binding component associated with the
voltage-sensitive sodium channel from electrophorus elec-
tricus electroplax membranes. Proc Natl Acad Sci USA
1978; 75: 2606–2610.2. Vassilev PM, Scheuer T and Catterall WA. Identification
of an intracellular peptide segment involved in sodium
channel activation. Science 1988; 241: 1658–1661.
3. Scholz A. Mechanisms of (local) anaesthetics on voltage-
gated sodium and other ion channels. Br J Anaesth 2002;
89: 52–61.4. Yu FH, Yarov-Yarovoy V, Gutman GA, et al. Overview
of molecular relationships in the voltage-gated ion chan-
nel superfamily. Pharmacol Rev 2005; 57: 387–395.5. McLure HA and Rubin AP. Review of local anaesthetic
agents. Minerva Anesthesiol 2005; 71: 59–74.6. Becker DE and Reed KL. Essentials of local anesthetic
pharmacology. Anesth Prog 2006; 53: 98–109.
7. Heavner JE. Local anesthetics. Curr Opin Anaesthesiol
2007; 20: 336–342.8. Becker DE and Reed KL. Local anesthetics: review of
pharmacological considerations. Anesth Prog 2012; 59:
90–102.
9. Cartwright PD and Fyhr P. The manufacture and storage
of local anesthetics. Reg Anesth 1988; 13: 1–22.10. Strichartz GR, Sanchez V, Arthur GR, et al.
Fundamental properties of local anesthetics II.
Measured octanol:buffer partition coefficients and pKa
values of clinically used drugs. Anesth Analg 1990; 71:
158–170.11. Eriksson E. Review of the properties of two new local
anaesthetics, prilocaine and lidocaine. Acta Anaesthesiol
Scand 1966; 25(Suppl.): 54–58.
12. Holmdahl MH. Xylocaine (lidocaine, lignocaine), its dis-
covery and Gordh’s contribution to its clinical use. Acta
Anaesthesiol Scand 1998; 42(Suppl. 113): 8–12.13. Hiller A, Karjalainen K and Rosenberg P. Transient
neurological symptoms after spinal anaesthesia with
hyperbaric 5% lidocaine or general anaesthesia. Br J
Anaesth 1999; 82: 575–579.
14. Kanai Y, Katsuki H and Takasaki M. Lidocaine disrupts
axonal membrane of rat sciatic nerve in vivo. Anesth
Analg 2000; 91: 944–948.15. Lund PC, Cwik JC and Vallesteros F. Bupivacaine –
a new long-acting anesthetic agent. A preliminary clin-
ical and laboratory report. Anest Analg 1970; 49:
103–113.
16. Hahn I, Hoffmann R and Nelson L. EMLA-induced
methaemoglobinaemia and systemic topical anaesthetic
toxicity. J Emerg Med 2004; 26: 85–88.
17. McClellan K and Spencer C. Levobupivacaine. Drugs
1998; 56: 355–362.
18. McLeod G and Burke D. Levobupivacaine. Anaesthesia
2001; 56: 331–341.19. Breslin DS, Martin G, Macleod DB, et al. Central ner-
vous system toxicity following administration of levobu-
pivacaine for lumbar plexus block. A report of two cases.
Reg Anesth Pain Med 2003; 281: 144–147.
De Hert et al. 439
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
20. McClure JH. Ropivacaine. Br J Anaesth 1996; 76:300–307.
21. Markham A and Faulds D. Ropivacaine. A review of its
pharmacology and therapeutic use in regional anaesthe-sia. Drugs 1996; 52: 429–449.
22. Feldman HS, Arthur GR, Pitkanen M, et al. Treatmentof acute systemic toxicity after rapid intravenous injec-
tion of ropicvacaine and bupivacaine in the consciousdog. Anesth Analg 1991; 73: 373–384.
23. Klein SM, Pierce T, Rubin Y, et al. Successful resuscita-
tion after ropivacaine-induced ventricular fibrillation.Anesth Analg 2003; 97: 90–93.
24. Dernedde M. Grand mal convulsions after an accidental
injection of ropivacaine. Anesth Analg 2004; 98: 521–523.25. Conroy PH and O’Rourke J. Tumescent anaesthesia.
Surgeon 2013; 11: 210–221.
26. Klein JA. Tumescent technique for regional anesthesiapermits lidocaine doses of 35 mg/kg for liposuction.J Dermatol Surg Oncol 1990; 16: 248–263.
27. Hanke CW, Bernstein G and Bullock S. Safety of tumes-
cent liposuction in 15,336 patients: national surveyresults. Dermatol Surg 1995; 21: 459–462.
28. Matarasso A and Hutchinson OHZ. Liposuction. JAMA
2001; 285: 266–268.29. Habbema L. Safety of liposuction using exclusively
tumescent local anesthesia in 3,240 consecutive cases.
Dermatol Surg 2009; 35: 1728–1740.30. Habbema L. Efficacy of tumescent local anesthesia with
variable lidocaine concentration in 3430 consecutive casesof liposuction. J Am Acad Dermaotol 2010; 62: 988–994.
31. Creton D, Rea B, Pittaluga P, et al. Evaluation of thepain in varicose vein surgery under tumescent local anaes-thesia using sodium bicarbonate as excipient without any
intravenous sedation. Phlebology 2012; 7: 368–373.32. Rass K, Frings N, Glowacki P, et al. Comparable effect-
iveness of endovenous laser ablation and high ligation
with stripping of the great saphenous vein. ArchDermatol 2012; 148: 49–58.
33. Rasmussen L, Lawaetz M, Bjoern L, et al. Randomized
clinical trial comparing endovenous laser ablation andstripping of the great saphenous vein with clinical andduplex outcome after 5 years. J Vasc Surg 2013; 58:421–426.
34. Kendler M, Simon JC and Wetzig T. Local anesthesiawith lidocaine and prilocaine, using the tumescent tech-nique, for the radiofrequency ablation of lower extremity
varicose veins. Int J Dermatol 2013; 52: 739–744.35. Haines WY, Deets R, Lu N, et al. Tumescent anesthesia
reduces pain associated with balloon angioplasty of
hemodialysis fistulas. J Vasc Surg 2012; 56: 1453–1456.36. Rudlof K, Ruffert H, Wehner M, et al. Tumescent anaes-
thesia for dermatological surgery. Plasma concentrationsof lignocaine and prilocaine. Der Anaesthesist 2007; 56:
785–789.37. Swanson E. Prospective study of lignocaine, bupivacaine
and adrenaline levels and blood loss in patients undergo-
ing liposuction and abdominoplasty. Plast Reconstr Surg2012; 130: 702–722.
38. Breuninger H, Hobbach PS and Schimek F. Ropivacaine:
an important anesthetic agent for slow infusion and other
forms of tumescent anesthesia. Dermatol Surg 1999; 20:
459–464.
39. Schmittner MD, Faulhaber J, Kemler B, et al. Influence
of high dose tumescent local anaesthesia with prilocaine
on systemic interleukin (IL)-6, IL-8, and tumour necrosis
factor-a. Eur Acad Dermatol Venereol 2010; 24:
1400–1405.
40. Iverson RE and Lynch DJ American Society of Plastic
Surgeons Committee on Patient Safety. Practice advisory
on liposuction. Plast Reconstr Surg 2004; 11: 1478–1490.41. Howe NR and Williams JM. Pain of injection and dur-
ation of anesthesia for intradermal infiltration of ligno-
caine, bupivacaine, and etidocaine. J Dermatol Surg
Oncol 1994; 20: 459–464.42. Cederholm I. Preliminary risk-benefit analysis of ropiva-
caine in labour and following surgery. Drug Saf 1997; 16:
391–402.
43. Sood J, Jayaraman L and Sethi N. Liposuction: anaes-
thesia challenges. Indian J Anaesth 2011; 55: 220–227.
44. Llanos S, Dagnino B, Ponce D, et al. Effect of subcuta-
neous lignocaine infiltration on blood loss secondary to
corporal lipoaspiration: a prospective, randomized,
double-masked clinical trial. Aesthetic Plast Surg 2009;
33: 738–742.
45. Cepeda MS, Tzortzopoulou A, Thackrey M, et al.
Adjusting the pH of lidocaine for reducing pain on
injection. Cochrane Database Syst Rev 2010; (12):
CD006581.46. Bokesch PM, Raymond SH and Strichartz GR.
Dependence of lidocaine potency on pH and pCO2.
Anesth Analg 1987; 66: 9–17.
47. Bourget P, Bonhomme L and Benhamou D. Factors
influencing precipitation of the pH-adjusted bupivacaine
solutions. J Clin Pharm Ther 1990; 15: 197–204.48. Finucane BT. Allergies to local anesthetics – the real
truth. Can J Anesth 2003; 50: 869–874.49. Speca SJ, Boynes SG and Cuddy MA. Allergic reactions
to local anesthetic formulations. Dent Clin North Am
2010; 54: 655–664.50. Schatz M. Adverse reactions to local anesthetics.
Immunol Allergy Clin North Am 1992; 12: 585–609.51. Rae SM, Milne MK and Wildsmith JA. Anaphylaxis
associated with, but not caused by, extradural bupiva-
caine. Br J Anaesth 1997; 78: 224–226.52. Bacon GS, Lyons TR and Wood SH. Dyclonine hydro-
chloride for airway anesthesia: awake endotracheal intub-
ation in a patient with suspected local anesthetic allergy.
Anesthesiology 1997; 86: 1206–1207.53. Jolliffe VML and Sinclair RD. Excision biopsy in a
patient with suspected local anaesthetic allergy: use of
0.9% saline with benzyl alcohol as local anaesthesia.
Clin Exp Dermatol 2012; 37: 862–864.
54. Wolfe JW and Butterworth JF. Local anesthetic systemic
toxicity: update on mechanisms and treatment. Curr Opin
Anesthesiol 2011; 24: 561–566.55. Di Gregorio G, Neal JM, Rosenquist RW, et al. Clinical
presentation of local anesthetic systemic toxicity: a review
of published cases, 1979 to 2009. Reg Anaesth Pain Med
2010; 35: 181–187.
440 Phlebology 29(7)
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from
56. Neal JM, Bernards CM, Butterworth JF, et al. ASRApractice guidelines on local anesthetic systemic toxicity.Reg Anesth Pain Med 2010; 35: 152–161.
57. Weinberg GL. Treatment of local anesthetic systemic tox-icity (LAST). Reg Anesth Pain Med 2010; 35: 188–193.
58. Borgeat A and Aguirre J. Update on local anesthetics.Curr Opin Anaesthesiol 2010; 23: 466–471.
59. Nouette-Gaulain K, Capdevila X and Rossignol R. Localanesthetic ‘‘in-situ’’ toxicity during peripheral blocks:update on mechanisms and prevention. Curr Opin
Anaesthesiol 2012; 25: 589–595.60. Hargreaves KM and Keiser K. Local anesthetic failure in
endodontics: mechanisms and management. Endodontic
Topics 2002; 1: 26–29.61. Trescot AM. Local anesthetic ‘‘resistance’’. Pain
Physician 2003; 6: 291–293.
62. Arendt-Nielsen L, Kaalund S, Bjerrinp P, et al.Insufficient effect of local analgesics in Ehler Danlostype III patients. Acta Anaesthesiol Scand 1990; 34:
358–361.63. Liem EB, Lin CM, Suleman MI, et al. Anesthetic require-
ment is increased in redheads. Anesthesiology 2004; 101:279–283.
64. Liem EB, Joiner TV, Tsueda K, et al. Increased sensitiv-ity to thermal pain and reduced subcutaneous lidocaineefficacy in redheads. Anesthesiology 2005; 102: 509–514.
65. Panditrao MM, Panditrao MM, Khan MI, et al. Doesscorpion bite lead to development of resistance to theeffect of local anaesthetics. Indian J Anaesth 2012; 56:
575–578.
De Hert et al. 441
by Marianne Demaeseneer on December 28, 2014phl.sagepub.comDownloaded from