So much time for so little: Italy's pharmaceutical industry and doctors' information needs
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of So much time for so little: Italy's pharmaceutical industry and doctors' information needs
Time for a smoke? One cigarette reduces your life by 11 minutes
Editor—Studies investigating the impact onmortality of socioeconomic and lifestyle fac-tors such as smoking tend to report deathrates, death rate ratios, odds ratios, or thechances of smokers reaching different ages.These findings may also be converted intodifferences in life expectancy. We estimatedhow much life is lost in smoking onecigarette.
Our calculation is for men only andbased on the difference in life expectancybetween male smokers and non-smokersand an estimate of the total number of ciga-rettes a regular male smoker might consumein his lifetime. We derived the difference inlife expectancy for smokers and non-smokers by using mortality ratios from thestudy of Doll et al of 34 000 male doctorsover 40 years.1 The relative death rates ofsmokers compared with non-smokers werethreefold for men aged 45-64 and twofoldfor those aged 65-84,1 as corroborated else-where.2 Average life expectancy from birthfor the whole population or subgroups canbe derived from life tables. Applying therates of Doll et al to the latest interim lifetables for men in England and Wales, withadjustment for the proportion of smokersand non-smokers in each five year agegroup,3 we found a difference in life expect-ancy between smokers and non-smokers of6.5 years.
We used the proportion of smokers byage group, the median age of starting smok-ing, and the average number of cigarettessmoked per week in the 1996 generalhousehold survey.4 We calculated that if aman smokes the average number ofcigarettes a year (5772) from the medianstarting age of 17 until his death at the ageof 71 he will consume a total of 311 688cigarettes in his lifetime.
If we then assume that each cigarettemakes the same contribution to his death,each cigarette has cost him, on average, 11minutes of life:
6.5 years = 2374 days, 56 976 hours, or3 418 560 minutes
5772 cigarettes per year for 54 years =311 688 cigarettes
3 418 560/311 688 = 11 minutes percigarette.
This calculation is admittedly crude—itrelies on averages, assumes that the healtheffects of smoking are evenly spreadthroughout a smoker’s lifetime, presupposesthat the number of cigarettes smokedthroughout a lifetime is constant, andignores the difficulties in classifying peopleas either lifetime smokers or non-smokers.5
However, it shows the high cost of smokingin a way that everyone can understand.
The first day of the year is traditionally atime when many smokers try to stop, and on1 January 2000 a record number might beexpected to try to start the new millenniummore healthily. The fact that each cigarettethey smoke reduces their life by 11 minutesmay spur them on. The table shows somebetter uses for the time they save.Mary Shaw Economic and Social Research Councilresearch fellowRichard Mitchell research fellowDanny Dorling readerSchool of Geographical Sciences, University ofBristol, Bristol BS8 1SS
Competing interests: Drs Shaw and Mitchell arenon-smokers. Dr Dorling is a smoker (20 cigarettesa day).
1 Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortalityin relation to smoking: 40 years’ observations on maleBritish doctors. BMJ 1994;309:901-11.
2 Phillips AN, Wannamethee SG, Walker M, Thomson A,Davey Smith G. Life expectancy in men who have neversmoked and those who have smoked continuously: 15 yearfollow up of large cohort of middle aged British men. BMJ1996;313:907-8.
3 Office for National Statistics. 1997 mortality statistics:general. London: Stationery Office, 1999. (Series DH1No 30.)
4 Office for National Statistics. General household survey.Living in Britain. London: Stationery Office, 1996.
5 Suidicani P, Hein HO, Gyntelberg F. Mortality andmorbidity of potentially misclassified smokers. Int JEpidemiol 1997;26:321-7.
Stumbling into occupationalhealth: the influenzaconundrumEditor—In his editorial Smith describeshow the British government has decided onaccess to treatments.1 The occupationalhealth service of the NHS has had a similar,albeit less sophisticated, experience withrespect to advising on the immunisation ofstaff against influenza this winter. The lack ofa recognised body to give authoritativeadvice on occupational health has led topiecemeal arrangements by trusts.
The chief medical officer has advisedthat routine immunisation of healthcareworkers is not recommended in the UnitedKingdom as part of national policy but thatsome health trusts may offer influenzavaccine to staff as part of their planning forwinter.2
Subsequently, NHS employers havebeen advised that “Ministers had concludedthat the immunisation of staff should beregarded as an acceptable part of winterplanning arrangements.”3 The purpose ofthis planning measure is to reduce staffillness. No additional funds will be madeavailable.
I surveyed trusts’ current arrangementsby contacting NHS occupational physicians
Opportunities gained in stopping smoking by amount smoked
Amount smoked Life lost Opportunity gain
One cigarette 11 minutes Telephone call to friend; read of newspaper; brisk walk;or fairly frantic sexual intercourse
Pack of 20 cigarettes 3 hours 40 minutes Long film (for example, Titanic); two football matches;one shopping trip; Eurostar journey from London toParis, including visit to cafe; running in Londonmarathon; or tantric sex
Carton of 200 cigarettes 1.5 days Visit to friends or family; one very serious shoppingtrip; Wagner opera; flying round the world; or romanticnight away
Advice to authorsWe prefer to receive all responses electronically,sent either directly to our website or to theeditorial office as email or on a disk. Processingyour letter will be delayed unless it arrives in anelectronic form.
We are now posting all direct submissions toour website within 24 hours of receipt and ourintention is to post all other electronicsubmissions there as well. All responses will beeligible for publication in the paper journal.
Responses should be under 400 words andrelate to articles published in the precedingmonth. They should include <5 references, in theVancouver style, including one to the BMJ articleto which they relate. We welcome illustrations.
Please supply each author’s currentappointment and full address, and a phone orfax number or email address for thecorresponding author. We ask authors to declareany competing interest. Please send a stampedaddressed envelope if you would like to knowwhether your letter has been accepted or rejected.
Letters will be edited and may be shortened.
Letters
Website: www.bmj.comEmail: [email protected]
53BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
throughout the United Kingdom on anemail network. Of 14 replies from England,Scotland, and Northern Ireland, five trustswere not offering vaccinations, three wereadopting a low key response, three wereactively targeting groups of staff such asaccident and emergency staff, and threewere offering vaccinations to all their staff.The large scale vaccination programmeswere being funded either by the trust or bylocal purchasers.
What is the explanation? The case thatroutine influenza vaccinations will reducestaff absences remains to be made. Indeed, arecent review of NHS staff absences duringthe influenza epidemics of 1993-4 and1996-7 found that absenteeism was notaffected.4 Preventing nosocomial infectionof susceptible patients merits study but hasnothing to do with the millennium holiday.The main focus of risk assessment, there-fore, seems to be the prospect of embarrass-ment should planning go awry. Some trustsare responding by minimising the risk ofbeing criticised, others are taking pro-fessional advice and acting accordingly.Scotland and Northern Ireland areinterested observers. This is a curiousexample of postcode prescribing but afamiliar example of postcode occupationalhealth in the NHS.John Harrison senior lecturer in occupationalmedicineDepartment of Environmental and OccupationalMedicine, Medical School, Newcastle upon TyneNE2 [email protected]
1 Smith R. Stumbling into rationing. BMJ 1999;319:936.(9 October.)
2 Department of Health. Influenza immunisation. CMO’supdate 23. London: DoH, 1999.
3 Department of Health. Immunisation of NHS staff againstinfluenza for winter 1999-2000 including the millenniumperiod. London: DoH, 1999. (HSC 1999/214.)
4 Nguyen-Van-Tam J, Granfield R, Pearson J, Fleming D,Keating N. Do influenza epidemics affect patterns ofsickness absence among British hospital staff? Infect ControlHosp Epidemiol 1999;20:691-4.
Lack of funding will inhibitevidence based commissioningof cancer treatmentsEditor—We welcome the appointment ofa cancer tsar to improve the treatment ofpatients with cancer in the NHS.1 However,more resources and greater transparencyin their allocation will be necessaryto improve survival rates in the UnitedKingdom in relation to its comparableEuropean neighbours.2
We have previously reported our effortsin evidence based commissioning of cancerservices for 1997-8.3 Since then we haverepeated the exercise in the 1998-99 and1999-2000 contracting rounds. However,most available growth monies have beenabsorbed by large increases in activity andpay awards. Little money has been left fornew expensive cancer drugs, despite strongevidence of their cost effectiveness and theincreasing willingness of clinicians to setpriorities between cancer treatments. We
conclude that a randomised controlled trialof evidence based medicine versus shroudwaving (as standard practice) is urgentlyrequired.
This process of evidence based commis-sioning was comparatively resource inten-sive. Unless there is some perceived benefitfor clinicians and commissioners of care, itwill wither on the vine. We do not expect allcost effective new treatments to be fundedautomatically. However, there should bescope for the evidence to have a greaterimpact on the system and for the emergingNational Centre for Clinical Excellence tobe able to say yes as well as no to costlytreatments.June So chief pharmacistJ Howard Scarffe professor of medical oncologyChristie Hospital NHS Trust, Manchester M20 4BX
Elizabeth Rous consultant in public health medicineManchester Health Authority, Gateway House,Manchester M60 7LP
Robbie Foy clinical research fellowScottish Programme for Clinical Effectiveness inReproductive Health, Department of Obstetricsand Gynaecology, University of Edinburgh,Edinburgh EH3 [email protected]
1 In brief. NHS to have cancer tsar. BMJ 1999;319:1152.(30 October.)
2 Sikora K. Cancer survival in Britain. BMJ 1999;319:461-2.(21 August.)
3 Foy R, So J, Rous E, Scarffe H. Commissioner and special-ist perspectives of prioritising new cancer drugs: impact ofthe evidence threshold. BMJ 1999;318:456-9.
Decisions to withdrawtreatment
Values histories are more useful thanadvance directives
Editor—Winter and Cohen recognise oneof the problems with advance directiveswhen they correctly state: “The advancerefusal of treatment is legally bindingprovided certain conditions are met. . . . Aproblem still exists unless they are preciselyworded.”1
Traditional advance directives arebecoming less and less useful, partly as aresult of lack of data on when treatmentbecomes futile in different clinical scenarios.When advance directives were first intro-duced, the application of standard “heroicmeasures,” often without reasonable expec-tation of result, was far more common thanit is today. In that situation, a generaladvance directive about refusing, say, cardio-pulmonary resuscitation, was an appropri-ate statement of common sense. Thesituations facing modern intensive careunits are far more complex. The tendencytowards precise wording in advance direc-tives to make them legally binding has madeit difficult for them to keep up with the paceof medical technology.2
An alternative approach that is findingincreasing favour, either as an adjunct to theadvance directive or as a stand alone instru-ment, is the “values history.” Values historiesrelate to the declarant’s values rather than
instructions. Patients’ values are recorded asa basis for decisions on medical treatment(rather than including explicit instructionson specific treatments). They identify corevalues and beliefs in the context of terminalcare that are important to the patient.3 4
Values histories take a goal based ratherthan prescriptive approach, giving guidanceon a policy to be implemented rather thanthe medical means to the end. The legalpersuasiveness of them is less strong, butthey may be useful adjuncts when a personis seeking to have an advance refusalrespected or they may provide valuableguidance in their own right.5 In general,the trend towards greater use of values inadvance statements is more useful topatients and intensive care doctors than isthe trend towards increasingly specificwording of treatments to be refused. Useof values histories should therefore beencouraged.
Further details on values histories maybe obtained from the Living Will andValues History Project, BM 718, LondonWC1N 3XX.Chris Docker directorVoluntary Euthanasia Society of Scotland,Edinburgh EH1 [email protected]
1 Winter R, Cohen S. ABC of intensive care: withdrawal oftreatment. BMJ 1999;319:306-8. (31 July.)
2 Docker C. Living wills/advance directives. In: McLean S,ed. Contemporary issues in law, medicine and ethics. Aldershot:Dartmouth, 1996:179-214.
3 Gibson J. Values history focuses on life and deathdecisions. Med Ethics 1990;5:1-2, 17.
4 Lambert P, Gibson J, Nathanson P. The values history: aninnovation in surrogate medical decision-making. Law MedHealth Care 1990:18:202-12.
5 Docker C. Living wills. In: Finance and law for the elderlyclient. London: Butterworths-Tolley (in press).
Treatment can sometimes be withdrawnat home
Editor—In their article on withdrawal oftreatment in the intensive care unit Winterand Cohen rightly emphasise theimportance of ensuring the comfort ofdying patients as well as caring for thefamily.1 The intensive care unit can be noisyand stressful for grieving relatives. It maybe difficult to provide a comfortable andprivate environment for families andpatients who are terminally ill.
In appropriate circumstances it is possi-ble to take patients to their home and with-draw treatment there. Since 1996 we havetaken six patients from our unit home to die.The table gives details of the last fourpatients.
In all cases the relatives found thisapproach helpful. Relatives often state that,given the choice, the patient would prefer todie at home rather than in hospital. More-over, relatives seemed better able to copewith their grief in the familiar surroundingsof their homes.
There are several conditions that shouldbe satisfied before a patient in intensive carecan be taken home to die. There has to bemedical consensus that continued intensivetherapy is futile, and withdrawal of ventila-tion or cessation of inotropes should
Letters
54 BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
preferably lead quickly to death. Organdonation should not be an option, and thepatient’s death should not require referralto the coroner. Ideally the patient shouldlive locally. An intensive care nurse anddoctor need to be available to accompanythe patient and to manage the process ofwithdrawal of treatment once at thepatient’s home. Transport needs to bebooked in advance.
A clear drug palliation plan should beformulated that uses opiates and benzodi-azepines to ensure that the patient is sedatedand absolutely comfortable. It is essential todiscuss the plan with the patient’s generalpractitioner so that ongoing care for thefamily can be instigated. Under certaincircumstances the general practitioner mayissue a death certificate.
Once all the conditions are satisfied thepossibility of taking the patient home can beoffered to the family. The process should bediscussed in detail and they should be told ofthe risk of death during transfer. It is essen-tial that all family members agree before thepatient is transferred.
We believe that when intensive care isdeemed futile, consideration should begiven to withdrawing treatment in thepatient’s home.Paul Frost consultant in intensive careon behalf of medical and nursing staff from thedepartment of intensive care medicine,Middlemore Hospital, Auckland, New Zealand
1 Winter B, Cohen S. ABC of intensive care: withdrawal oftreatment. BMJ 1999;319:306-8. (31 July.)
Most decisions are based on subjectiveappraisal
Editor—Winter and Cohen’s review ofwithdrawal of treatment in intensive caretouched on several issues that continue topose vexing problems to intensive care doc-tors.1 These ethical problems apply to bothadult and paediatric intensive care. We agreewith the authors that death in intensive careoften follows a process of withholding orwithdrawal of treatment and that theseissues are becoming increasingly commonas well as complex.
In a prospective audit of deaths overnine months in a paediatric intensive careunit in the United Kingdom, we found that44 (84%) of the 52 deaths resulted from aprocess of withholding or withdrawal oftreatment. Withdrawal of active treatment,such as inotropes or renal replacementtherapy or extubation from mechanicalventilation, was by far the commonestprocess. These decisions were often made
on the basis that death was imminent orthat prolonging treatment was futile. Acombination of worsening severity ofillness, minimal response to aggressivetreatment, and poor future quality of lifewere often the stated reasons for with-drawal. However, our objective analysis ofthese deaths using severity of illnessmeasurements with the paediatric risk ofmortality (PRISM II) score, showed that 22(50%) of these children had mortality risks> 50% and only 10 (23%) had mortalityrisks > 80%. Twenty (45%) had conditionsthat were associated with extremely poorlong term prognosis. Therefore it seemsthat most decisions concerning futility oftreatment were based on subjectiveappraisal of the child’s deteriorating condi-tion. A study in a paediatric intensive careunit in Malaysia has shown that personalbias of the intensive care doctor and thepatient’s sociocultural background mayinfluence these decisions.2 The concept offutility may differ quite substantially amongintensive care doctors and also amongpatients.
We disagree with Winter and Cohen thatit is easier to withhold a treatment than towithdraw it once it has been instituted. Weoften find ourselves in situations where theinappropriateness of intensive care andlimitations of treatment have not beendiscussed with the family before referral tothe intensive care team. In the current auditall the patients had received mechanicalventilation and a variable period of aggres-sive intensive care before treatment waswithdrawn.
With advances in critical care these ethi-cal dilemmas are expected to intensify. Untilsuch a time that objective criteria for futilitybecome sufficiently accurate for individualpatient prognostication, we agree with theauthors that the principles that guide inten-sivists on end of life decision making shouldbe based on beneficence and non-maleficence to our patients.1 3
Adrian T Goh visiting fellow paediatric intensive [email protected]
Quen Mok consultant paediatrician in intensive carePaediatric Intensive Care Unit, Great OrmondStreet Hospital for Children, London WC1N 3JH
1 Winter B, Cohen S. ABC of intensive care: withdrawal oftreatment. BMJ 1999;319:306-8. (31 July.)
2 Goh AYT, Lum LCS, Chan PWK, Bakar F, Chong BO.Withdrawal and limitation of life support in paediatricintensive care. Arch Dis Child 1999;80:424-8.
3 Royal College of Paediatrics and Child Health.Withholdingor withdrawing life saving treatment in children.A framework forpractice. London: RCPCH, 1997.
Courts can help resolve disagreement indifficult cases
Editor—In the same issue as Winter andCohen’s article on withdrawing treatment inintensive care,1 Clare Dyer reported on arecent Court of Appeal case involving thetreatment of a 12 year old child.2 3 Oneimportant aspect of the case was the viewexpressed by the court and by MichaelWilks, chairman of the BMA’s ethicscommittee, that if there was fundamentaldisagreement between the parents and doc-tors an application to the family division ofthe High Court could be an appropriate wayforward. This is an important point to bearin mind when faced with the problems iden-tified by Winter and Cohen.1
The idea of futility is a quagmire.4
Despite this I would agree that in most casescareful and sensitive discussion does lead toa resolution of any disagreement. As therecent case2 shows, however, the disagree-ment sometimes cannot be resolved withoutthe benefit of the views of the court. Doctorsshould be sensitive to the existence of suchsituations and be aware that a short noticeapplication to the court is a potential courseof action in these cases.Raj Mohindra specialist registrar, general medicineHeatherwood Hospital, Ascot SL5 [email protected]
1 Winter B, Cohen S. ABC of intensive care: withdrawal oftreatment. BMJ 1999;319:306-8. (31 July.)
2 R v Portsmouth Hospitals NHS Trust ex parte Carol Glass.Times 26 July 1999.
3 Dyer C. Mother fails to win right to control treatment forson. BMJ 1999;219:278. (31 July.)
4 Zucker MB, Zucker HD, eds. Medical futility and the evalua-tion of life sustaining interventions. New York: CambridgeUniversity Press, 1997.
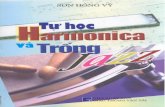
So much time for so little:Italy’s pharmaceutical industryand doctors’ information needsEditor—Two local experiences in northernItaly may be relevant to the discussion follow-ing the recent editorial by Griffith on doctors’reasons for not seeing drug representatives.1
In 1992, eight general practitioners fromGuastallae evaluated the amount of timespent with pharmaceutical representatives.On average, each doctor had 435 visits peryear from 102 different companies andspent a total of 58 hours every year talkingto pharmaceutical representatives. Toreduce this time, four doctors allowed up totwo visits per day, and four allocated a singleweekly session, allowing up to eight visits,but this approach did not lead to the desiredresults (table).
In 1994, four of these general practition-ers contacted 102 drug companies, asking toreceive information based on systematicevaluation of available evidence rather thanglossy booklets and favourable trials only.Nothing changed except that staff specialistsjoined the visit. In 1996, drug companieswere asked to send their representatives onlywhen invited or when relevant informationwas available in advance. Most representa-tives stopped visiting doctors’ surgeries, and
Details of four patients who had intensive treatment withdrawn at home
Age (years) and sex Diagnosis APACHE II score Length of stay (hours) Ventilated
51, male Cellulitis, septic shock 33 79 No
54, female Pneumonia 32 19 Yes
61, male Cardiac arrest outsidehospital
24 52 Yes
58, male Cerebellar haemorrhage 24 436 Yes
Written consent was obtained from relatives for publication of patients’ details.APACHE=acute physiological and chronic health evaluation.
Letters
55BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
only three out of 102 agreed to answer spe-cific questions.
In 1992, four general practitioners fromImola, after the publication of a drug formu-lary,2 asked 105 drug companies to submitonly clinically relevant information andanswer doctors’ specific questions. This put acomplete stop—which still persists—to visitsfrom drug representatives.
We analysed some typical “informationpackages” and found that “drug oriented”information is often flawed, biased, ormisleading3 4: protocols of ongoing studiesare used as evidence of clinical benefits;unpublished data on file are quoted asreliable references; pharmacological ormolecular effects are overemphasised; andall this is almost regularly accompanied byan invitation to gather your own experienceswith this drug and then judge. This is notpatient oriented information drawn from asystematic evaluation of available evidence.
Transforming advertising into reliableinformation is probably impossible. Pharma-ceutical companies are well equipped to pro-duce and disseminate information abouttheir drugs, and they are one of the mainsources of information for doctors. Healthauthorities should arrange a similar system,using dedicated professionals to provide doc-tors with valid and unbiased information.Interventions of this sort should be includedin the current effort by Italy’s health service toproduce and implement practice guidelines.Local centres could be used to make thisinformation easily available to doctors and todetermine and evaluate the best strategies fordissemination and implementation.5
Emilio Maestri general practitionerGilberto Furlani general practitionerGuastalla, Reggio Emilia, Italy
Fabio Suzzi general practitionerImola, Bologna, Italy
Annalisa Campomori pharmacistGiulio Formoso epidemiologistNicola Magrini headUnit of Drug Evaluation and Evidence-BasedPrimary Care, Centro per la Valutazione dellaEfficacia della Assistenza Sanitaria (CeVEAS), 41100Modena, [email protected]
1 Griffith D. Reasons for not seeing drug representatives.BMJ 1999;319:69-70. (10 July.)
2 Magrini N, Vaccheri A, Suzzi F, Montanaro N. 150 farmaciper il medico di famiglia. Rome: Il Pensiero ScientificoEditore, 1993.
3 Ziegler Mg, Lew P, Singer BC. The accuracy of drug infor-mation from pharmaceutical sales representatives. JAMA1995;273:1296-98.
4 Herxheimer A. Basic information that prescribers are notgetting about drugs. Lancet 1987;8523:31-3.
5 Thorsen T, Mäkelä M, eds. Changing professional practice.Theory and practice of clinical guidelines implementation.Copenhagen: Danish Institute for Health Services Research,1999.
Effect of temazepam onventilatory response atmoderate altitudeEditor—Dubowitz’s study of the effect oftemazepam on oxygen saturation at highaltitude found that benzodiazepines do nothave a depressant effect.1 He explains thediscrepancy between his findings and thoseof previous studies by the fact that otherstudies have investigated the effect oflong acting benzodiazepines.2 Dubowitz’sprobands were investigated after altitudeacclimatisation while walking to Everest basecamp, whereas climbers in Europe mainlyengage in short periods of mountaineering.We therefore evaluated the effect of 10 mgtemazepam on respiration in non-acclimatised Alpine climbers at moderatealtitude.
We performed a randomised, doubleblind, placebo controlled, crossover trial inseven healthy men aged 21 to 27. Partici-pants at 171 m altitude were randomised toreceive either 10 mg temazepam or placebo.Three days later the men were given thesame medication and taken by cable car to3000 m. The procedure was repeated afterone week, with the men crossed to the otherarm of the study. Arterial blood sampleswere obtained from the ear lobe before andone hour after temazepam or placebo wastaken.4 Arterial oxygen partial pressure andcarbon dioxide partial pressure were ana-lysed on an IL Synthesis 25 blood gasanalyser (Instrumentation Laboratory,Milan, Italy). Differences in blood gasconcentrations before and after temazepamor placebo at each altitude were analysed bypaired t tests.
The table shows the results of bloodgas analysis before and after temazepam.At 171 m blood gas concentrations didnot change significantly after temazepam.At 3000 m the arterial oxygen pressuredecreased and carbon dioxide pressureincreased significantly after temazepam.The mean decrease in arterial oxygenconcentration between altitudes was 0.77(95% confidence interval − 8.02 to − 3.69)kPa (P < 0.01) and the mean increase inarterial carbon dioxide concentration was0.3 (0.46 to 4.11) kPa (P < 0.05). Placebo didnot affect blood gas concentrations at eitheraltitude.
Although we did not measure respira-tion directly, our data indicate that a lowdose of a short term benzodiazepine canimpair respiration at moderate altitude.These findings seem to contradict Dubow-itz’s conclusion. Treatment with temazepamat stable conditions after altitude acclimati-sation may not impair respiration, but initialstages of acute respiratory adaptation tohypoxia at altitude are inhibited. Similarresults were found after 50 g alcohol atmoderate altitude.5 Caution in the use ofbenzodiazepines to treat sleep disorders ataltitude is therefore necessary, especially inthe initial stages of altitude acclimatisation.Georg Röggla head of [email protected]
Berthold Moser studentDepartment of Internal Medicine, MunicipalHospital of Neunkirchen, Neunkirchen, Austria
Martin Röggla lecturerDepartment of Emergency Medicine, University ofVienna, Austria
1 Dubowitz G. Effect of temazepam on oxygen saturationand sleep quality at high altitude: randomised placebocontrolled crossover trial. BMJ 1998;316:587-9.
2 Röggla G, Röggla M, Wagner A, Seidler D, Podolsky A.Effect of low dose sedation with diazepam on ventilatoryresponse at moderate altitude. Wien Klin Wochenschr1994;106:649-51.
3 Hills M, Armitage P. The two-period cross-over clinicaltrial. Br J Clin Pharmacol 1979;8:7-20.
4 Spiro SG, Dowdeswell IR. Arterialised ear lobe blood sam-pling for blood gas tensions. Br J Dis Chest 1976;70:263-8.
5 Röggla G, Röggla H, Röggla M, Binder M, Laggner AN.Effect of alcohol on acute ventilatory adaptation to mildhypoxia at moderate altitude. Ann Intern Med1995;122:925-927.
Guidelines are needed if drugtesting of those arrested by thepolice becomes compulsoryEditor—The prime minister’s announce-ment at the last Labour Party conference thatthe government proposes to introducecompulsory drug and DNA testing forpeople arrested for indictable offences beforethey have been convicted will raise someimportant ethical issues for healthcare pro-fessionals if it does eventually become law.1 Aspointed out in the Economist,2 the upshot ofcompulsory DNA testing might be that everyalleged shoplifter could be held down forciblywhile a mouth swab is taken.2 Collecting sweatfor a drug test by wiping the forehead of arestrained and resisting subject with a swabwould be no more dignified.
Interactions between drug representatives andeight general practitioners in Guastalla, Italy, in1992-3
Mode of access
No ofvisitsperyear
Meanduration
(min)
TotalGP time(hours/year)
Unrestricted (1992) 435 7 58
Maximum two visits/day(1993)
400 8 55
Group appointment (6-8visits per week) (1993)
340 10 50
Arterial oxygen (PaO2) and carbon dioxide (PaCO2) concentrations (kPa) of seven men before and onehour after 10 mg temazepam at 171 and 3000 m
Case No
PaO2 PaCO2
171 m 3000 m 171 m 3000 m
Before After Before After Before After Before After
1 12.2 12.2 9.3 8.6 4.5 4.3 4.3 4.4
2 11.2 11.6 8.6 8.4 4.7 4.9 4.4 4.7
3 12.1 12 8.9 8.2 4.4 4.5 4.4 4.7
4 11 11.4 9.1 4.9 4.9 4.8 4.0 4.3
5 10.9 11 8.5 8.1 4.7 4.4 4.1 4.4
6 12.5 12.2 9.1 8.1 4.5 4.8 4.4 4.7
7 12 12.2 9.4 8.4 4.4 4.5 4.0 4.8
Mean (SD) 11.7 (0.63) 11.8 (0.48) 9 (0.29) 8.3 (0.2) 33.4 (1.4) 34.6 (1.8) 4.2 (0.19) 4.5 (0.2)
Letters
56 BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
The BMA has issued helpful guidelinesfor police surgeons who have been asked toexamine people in police custody whenconsent for such examination is notforthcoming.3 I hope that similar guidelineswill be produced for medical practitionerswho may be asked to participate incollecting body fluids for drug testing fromarrested people without their consent and inanalysing, interpreting, and using the resultsin samples obtained in this way.A R W Forrest professor of forensic toxicologyDepartment of Forensic Pathology, University ofSheffield, Sheffield S3 [email protected]
1 Another fine mess [editorial]. New Law Journal 1999;149:1429.
2 Tony Blair and liberty [editorial]. Economist 1999;353(8139):19-20.
3 Pownall M. Doctors should obtain informed consent forintimate body searches. BMJ 1999;318:310.
Incidence of venousthromboembolism in users ofcombined oral contraceptives
Methods for identifying cases andestimating person time at risk must bedetailed
Editor—Lawrenson et al reported a crudeincidence of venous thromboembolism of38 per 100 000 women who used combinedoral contraceptives, based on informationderived from the General Practice ResearchDatabase, without describing how theyderived their estimate.1 This estimate isclosely similar to the incidence reported in aprior publication of theirs, which was basedon a different automated medical database.2
In their letter they provide no details on thevalidity and specificity of the diagnosis ofvenous thromboembolism or the presenceof medical risk factors and no informationon the person time at risk for current usersof oral contraceptives.
An incidence must be based on persontime at risk. Despite apparent deficiencies,the authors provide an incidence that isroughly twice as high as the incidence thatcolleagues and I reported in a paper derivedfrom the General Practice Research Data-base; we included only idiopathic cases ofvenous thromboembolism (those possiblyrelated directly to use of oral contracep-tives).3 Lawrenson et al conclude that ourreported estimate was substantially lowerthan the true incidence.
On the basis of their previous publi-cation,2 Lawrenson et al seem to haveincluded both outpatients and inpatientswith any one of five computer recordeddiagnoses as patients with venous thrombo-embolism, without documentation fromclinical records. The five diagnoses include acomputer recorded diagnosis of thrombo-phlebitis. Colleagues and I found that,on the General Practice Research Database,over 90% of subjects with this computerrecorded diagnosis alone were treatedas outpatients, so clinical histories werenot available; we did not find any of the
remaining patients with this diagnosis tohave idiopathic deep vein thrombosis afterreview of clinical histories.3 Thus weconcluded that many young women with acomputer diagnosis of thrombophlebitis donot have documented idiopathic deep veinthrombosis.
The results from the General PracticeResearch Database provided in Lawrensonet al’s letter are uninterpretable because,firstly, it is unclear whether the general prac-titioners reported incidence according tonumber of users rather than person time atrisk, and, secondly, presumably the diagnosisof venous thromboembolism was not vali-dated from clinical records. By contrast,cases of venous thromboembolism that wereported were validated as idiopathic fromclinical records.3
An interpretation of estimates of theincidence of venous thromboembolismrelated to current use of oral contraceptivesrequires that the method for identifying rel-evant cases as well as the method forestimating person time at risk be clearlydetailed,4 as in our paper.3 In the absence ofsuch information, comparison of rates of ill-ness between different reports is unjustifiedand surely misleading.Hershel Jick associate professor of medicineBoston Collaborative Drug Surveillance Program,Boston University School of Medicine, 11 MuzzeyStreet, Lexington, MA 02421, USA
Competing interests: None declared.
1 Lawrenson RA, Whalley A, Simpson E, Farmer RDT. DoHseems to have underestimated incidence of venous throm-boembolism in users of combined oral contraceptives. BMJ1999;319:387. (7 August.)
2 Farmer RD, Lawrenson RA, Thompson CR, Kennedy JG,Hambleton IR. Population-based study of risk of venousthromboembolism association with various oral contra-ceptives. Lancet 1997;349:83-8.
3 Jick H, Jick SS, Gurewich V, Myers MW, Vasilakis C. Risk ofidiopathic cardiovascular death and nonfatal venousthromboembolism in women using oral contraceptiveswith differing progestogen components. Lancet 1995;346:1589-93.
4 Jick H, García Rodríguez LA, Pérez Gutthann S. Principlesof epidemiologic research on adverse and beneficial drugeffects. Lancet 1998;352:1767-70.
Risk is particularly high with first use oforal contraceptives
Editor—Lawrenson et al show that the riskof venous thromboembolism during use oforal contraceptives might be higher thanestimated by the Medicines Commission ofthe United Kingdom’s Department ofHealth.1 That is especially likely for first use.
In a paper that was published at aboutthe same time Herings et al found anincidence of 90 per 100 000 woman years inthe first episode of use of third generationoral contraceptives; for second generationcontraceptives the figure was 24 per100 000; for the youngest ages and duringthe first year of use the incidences becamehigher than 100 per 100 000.2 These dataare in line with those found in earliercase-control studies.
A stratified analysis of the World HealthOrganisation’s study found a 21.6-foldincrease in the risk of venous thrombosisamong first ever users of third generationoral contraceptives during the first year ofuse (relative to never use); this relative risk
was 9.1 for second generation oral contra-ceptives.3 In the Leiden study we found four-fold to sevenfold risk increases for thirdversus second generation oral contracep-tives among younger women (most newusers would be young); this was over andabove an overall threefold to fourfold riskincrease for second generation oral contra-ceptives.4
Jick et al found 9.2-fold and 5.6-foldincreases in risk between third and secondgeneration oral contraceptives during thefirst six months of use.5 Multiplying thesecumulative relative risks with an overallbaseline incidence of, say, 5 per 100 000woman years yields incidences of the orderof magnitude found by Herings et al,2
thereby confirming the suspicion that theincidences are higher than generallybelieved, especially in young and first timeusers.Jan P Vandenbroucke professor, department ofclinical [email protected]
Kitty W M Bloemenkamp registrar, department ofobstetrics, gynaecology and reproductive medicineFrits R Rosendaal professor, thrombosis andhaemostasis research centreFrans M Helmerhorst lecturer, department ofobstetrics, gynaecology and reproductive medicineLeiden University Medical Centre, PO Box 9600,2300 RC Leiden, Netherlands
Competing interests: Professors Vandenbrouckeand Rosendaal have no competing interests. DrBloemenkamp has been involved in, and DrHelmerhorst has supervised, studies sponsored orassigned by various pharmaceutical companies thatmanufacture oral contraceptives, but none of thesecompanies has funded their studies on thecomparative merits of second and third generationoral contraceptives.
1 Lawrenson RA, Whalley A, Simpson E, Farmer RDT. DoHseems to have underestimated incidence of venous throm-boembolism in users of combined oral contraceptives. BMJ1999;319:387. (7 August.)
2 Herings RMC, Urquhart J, Leufkens HGM. Venousthromboembolism among new users of different oral con-traceptives. Lancet 1999;354:127-8.
3 Poulter NR, Farley TMM, Chang CL, Marmot MG, MeirikO. Safety of combined oral contraceptive pills. Lancet1996;347:547.
4 Bloemenkamp KWM, Rosendaal FR, Helmerhorst FM,Büller HR, Vandenbroucke JP. Enhancement by factor VLeiden mutation of risk of deep-vein thrombosisassociated with oral contraceptives containing third-generation progestagen. Lancet 1995;346:1593-6.
5 Jick H, Jick SS, Gurewich V, Myers MW, Vasilakis C. Risk ofidiopathic cardiovascular death and non-fatal venousthromboembolism in women using oral contraceptiveswith differing progestagen components. Lancet 1995;346:1589-93.
Authors’ reply
Editor—Our letter in response to theDepartment of Health’s statement calcu-lated an incidence of idiopathic venousthromboembolism of 36.5 per 100 000exposed woman years in users of combinedoral contraceptives. This was based on astructured review of published papers andcompared well with the findings from ourrecent study, for which we used the GeneralPractice Research Database. That studyincluded only cases of diagnosed venousthromboembolism with supporting evi-dence of anticoagulation treatment. Furtherinformation from general practitionersshowed that in 83% of cases there wassupportive evidence (venograms, Dopplerultrasound scans, or lung scans).
Letters
57BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
We have argued that general practition-ers in the United Kingdom do not treatpatients with anticoagulants without thesupport of diagnosis by a hospital consult-ant.1 The general practitioners’ responsesindicated that all our cases had beenreferred to hospital, although for a fifth thishad not been recorded on the General Prac-tice Research Database. We believe that thestrategy used by Jick et al of requiring acomputer record of hospital admission ledto a 20% underestimate of cases.2 In all ourstudies of combined oral contraceptives wehave used person time at risk for calculatingincidences, based on a 28 day pack. Jick et alused 30 days, which would have led to a fur-ther 7% error.
Vandenbroucke et al cite a further studyby Herings et al that supports our assertionof a higher incidence of venous throm-boembolism than that reported by theDepartment of Health. Their letter citesexamples of higher incidences of venousthromboembolism among users of thirdgeneration compared with second genera-tion combined oral contraceptives. We agreethat new users of combined oral contracep-tives seem to be at an increased risk of idio-pathic venous thromboembolism; this isimportant when considering the riskascribed to third generation combined oralcontraceptives.
In our studies we have compared usersof levonorgestrel 150 ìg plus ethinyloestra-diol 30 ìg with users of formulations ofcombined oral contraceptives containingdesogestrel and gestodene and found nodifference in risk of venous thromboembo-lism between the formulations. Interestingly,a further analysis has shown that, despite alarge change in prescribing practice sinceNovember 1995 from third to secondgeneration formulations, the overall risk ofvenous thromboembolism in users ofcombined oral contraceptives has notchanged.3
The key point of our letter was that thetrue rate of venous thromboembolism inusers of combined oral contraceptives isprobably nearer 37 per 100 000 exposedwoman years and that the figures quotedby the Department of Health are under-estimates.R A Lawrenson senior lecturer in public healthA Whalley research officerE Simpson research officerR D T Farmer professor of pharmacoepidemiology andpublic healthEuropean Institute of Health and Medical Sciences,University of Surrey, Guildford GU2 5RF
Competing interests: The department in which theauthors work has received funding from Organonand Schering for investigating venous thrombo-embolism in women using oral contraceptives.
1 Farmer RDT, Lawrenson RA. Third generation oralcontraceptives and venous thrombosis. Lancet1997;349:732-73.
2 Jick H, Jick SS, Gurewich V, Myers MW, Vasilaskis C. Risk ofidiopathic cardiovascular death and nonfatal venousthromboembolism in women using oral contraceptiveswith differing progestagen components. Lancet 1995;346:1589-93.
3 Farmer RDT. The impact of the 1995 “pill scare” in the UK.Pharmacoepidemiol Drug Safety 1999;8(suppl 2):S187.
Some patients are happy fordoctors to make decisionsEditor—I agree with Bastian that therelationship between doctors and theirpatient is fundamentally changing and thatmany patients should be more closelyinvolved in the decision making regardingtheir health needs.1 I do, however, not acceptBastian’s statement that doctors do not havea sophisticated understanding of the consul-tation process and wish to raise a point thatis often overlooked by many people in con-sumer organisations.
An appreciable body of patients in thecommunity is more than happy to offloadthe decision making about their treatmentto the doctor. Many of these patients areintelligent, motivated people who approachthe medical profession for advice based onknowledge and experience. As an anaesthet-ist I have spent much time discussing withpatients the pros and cons of one form ofperioperative analgesia versus another, and,almost invariably, when I ask the patientabout their preference the response is,“Whatever you think best, doctor” or “Whichone would you have?”
Every patient we see is unique andshould be treated as such. Some patientsclearly gain reassurance from the medicalprofession adopting the politically incorrectpaternalistic approach, and these peoplemust not be forgotten.Ian Taylor specialist registrar in anaesthesiaPrincess Margaret Hospital, Swindon SN1 4JU
1 Richards T. Australia’s consumer champion. BMJ 1999;319:730. (18 September.)
Long term vascularcomplications of Coxiellaburnetii infection
Cardiovascular risk factors cannot beignored
Editor—In their paper on the potential forinfection by Coxiella burnetii to be a risk factorfor cardiovascular disease Lovey et al suggestthat the established mode of transmission ofC burnetii is unlikely to be associated with riskfactors for cardiovascular disease. They alsosay that the unavailability of baseline data onsuch risk is unlikely to influence theirfindings.1 However, in an outbreak of Q feverpneumonia affecting 147 patients in theUnited Kingdom in 1989 (not referred to byLovey et al) we found that of 110 patients inwhom smoking history was available for thetime of the infection, 60 were currentsmokers, 28 were ex-smokers, and only 22had never smoked.2 3
A subsequent case-control study in thiscohort confirmed smoking to be a risk factorfor Q fever.4 Follow up of 87 (59%) patients inclinic nine years after the original outbreakidentified 31 (35%) as current smokers (meanage 51.2 (SD 10.2)), with a mean smokingburden of 33.0 (15.8) pack years. In this groupone patient had had a cerebrovascular
accident and three had ischaemic heartdisease. Thirty five (40%) patients wereex-smokers (mean age 57.0 (13.4)), with amean smoking burden of 26.4 (18.8) packyears. In this group one had had acerebrovascular accident and six had ischae-mic heart disease. Only 17 (20%) patients(mean age 53.8 (9.1)) had never smoked, andnone of these had vascular disease.
These results suggest that smoking is arisk factor for Q fever and show that in ourpatients it has been the current orex-smokers who have developed cardiovas-cular disease. It is therefore essential thatcurrent and past cigarette smoking areadded to a reanalysis by the Geneva groupbefore C burnetii can be taken as theexplanation of the excess cardiovascularmorbidity and mortality observed.Martin Wildman research fellow in [email protected]
Jon G Ayres professor of respiratory medicineHeartlands Research Institute, BirminghamHeartlands Hospital, Birmingham B9 5SS
1 Lovey P, Morabia A, Bleed D, Peter O, Dupuis G, Petite J.Long term vascular complications of Coxiella burnetiiinfection in Switzerland: cohort study. BMJ 1999;319:284-6. (31 July.)
2 Smith DL, Ayres JG, Blair I, Burge PS, Carpenter MJ, CaulEO, et al. A large Q fever outbreak in the West Midlands:clinical aspects. Respir Med 1993;87:509-16.
3 Hawker JI, Ayres JG, Blair I, Evans MR, Smith DL, SmithEG, et al. A large outbreak of Q fever in the West Midlands:windborne spread into a metropolitan area? Commun DisPublic Health 1998;1:180-7.
4 Ayres JG, Flint N, Smith EG, Tunnicliffe WS, Fletcher TJ,Hammond K, et al. Post-infection fatigue syndromefollowing Q fever. Q J Med 1998;91:105-23.
Authors’ reply
Editor—The data reported by Wildmanet al cannot be interpreted as evidence thatsmoking is a risk factor for Q fever. Theprevalence of current smoking in these 110patients was unusually high (55%), evencompared with the general local populationof East Birmingham (35%).1 2 These patientshad mostly been admitted to hospital andbeen identified on the basis of a recent diag-nosis of pneumonia or fever of unknownorigin. Smokers may therefore have beenoverselected simply because they were moreseverely affected by respiratory disease. Thisoverrepresentation of smokers among casesmay in turn explain the positive associationof smoking and Q fever observed in thestudy by Ayres et al, in which 71 patientswith Q fever were compared with patients ingeneral practice who were free of febrile ill-ness.3 By comparison, in the Swiss outbreakof 1983, 191 patients had fever, but 224others were identified by serum analysis ofthe general population (n = 3036).4 Q feverpneumonia affected only 68 patients (36%of the patients with symptoms and 16% ofthe whole group). Only 8 of the 415 patients(2%) were admitted to hospital.
Wildman et al also argue that cardio-vascular disease does not occur in patientsinfected with Q fever who never smoked.Three cases of ischaemic heart disease in 31smokers may, however, not be different fromno cases in 17 people who have neversmoked. Their numbers (31 + 35 + 17) do
Letters
58 BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com
not add up to 87, nor the proportions(35 + 40 + 20) to 100%.
Overall, the direct evidence for apossible confounding effect of smoking onthe relation between Q fever and coronaryheart disease and stroke is weak. Moreover,smoking does not seem to have been astrong confounder in other studies thatinvestigated the infectious origin of cardio-vascular disease.5 We therefore think itunlikely that a confounding effect ofsmoking, if it exists, could be strong enoughto fully explain the observed associationbetween acute infection with Coxiella burnetiiand the incidence of coronary heart diseaseand stroke.Pierre-Yves Lovey senior resident, department ofinternal [email protected]
Alfredo Morabia director, division of clinicalepidemiologyUniversity Hospital of Geneva, Rue Micheli duCrest 24, 1211 Geneva 14, Switzerland
1 Smith DL, Ayres JG, Blair I, Burge PS, Carpenter MJ, CaulEO, et al. A large Q fever outbreak in the West Midlands:clinical aspects. Respir Med 1993;87:509-16.
2 Hawker JI, Ayres JG, Blair I, Evans MR, Smith DL, SmithEG et al. A large outbreak of Q fever in the West Midlands:windborne spread into a metropolitan area? Commun DisPublic Health 1998;1:180-7.
3 Ayres JG, Flint N, Smith EG, Tunnicliffe WS, Fletcher TJ,Hammond K, et al. Post-infection fatigue syndromefollowing Q fever. Q J Med 1998;91:105-23.
4 Dupuis G, Petite J, Péter O, Vouilloz M. An importantoutbreak of human Q fever in a Swiss Alpine valley. Int JEpidemiol 1987;16:282-7.
5 Nieto FJ, Adam E, Sorlie P, Farzadegan H, Melnick JL,Comstock GW, et al. Cohort study of cytomegalovirusinfection as a risk factor for carotid intimal-medial thick-ening, a measure of subclinical atherosclerosis. Circulation1996;94:922-7.
Internet helps communicationbetween doctors and patientsEditor—I found the articles by Jadad andShepperd et al on using the internet to pro-vide patients with information helpful.1 2
The internet is beginning to transformhealth care, but there is fear that cliniciansmay remain ill prepared unless action istaken now. Jadad was unable to identify myarticle on this subject.3 I have developed theconcept of cyberclinics in rheumatology andosteoporosis with active participation ofpatients and am now able to offer consulta-tion and advice on the net.3 4
The internet can provide vast amountsof information, but the material is variablein quality. I have created one of the firstdepartmental websites in rheumatologyand osteoporosis (www.smuht.man.ac.uk/rheumat/), which features information that Ihave written personally or selected (afterstudying it online) and consider reliable sothat patients can access this informationwith confidence. A further point raised byJadad—strategies to increase “health lit-eracy” in general—is also important. I haverecently held a “road show” to demonstrateto patients the basic aspects of computersand the internet, and how the internet canbe used to access information relating tohealth care. Patients were able to participateand gain hands-on experience. My overallimpression was that even elderly people
would accept such new technology if theywere shown how to use it.
Jadad mentioned email, which isanother facility I offer to my patients andlocal practitioners for rapid response to anyqueries or anxieties they may have and toavoid delays caused by post and telephones.5
It is vital to ensure equal access totechnology and information. Even compara-tively poor countries may be able to affordtelecommunications facilities as the costs arecoming down, but they paradoxically remainunable to afford clinical expertise because ofa lack of trained specialists in such countries.Cyberclinics of the type I have developedmay enable patients from these countries toobtain medical advice in a more costeffective way than in many other formats oftelemedicine currently available, which canbe constrained by cost and technical failure.Badal Pal consultant rheumatologistDepartment of Rheumatology, WythenshaweHospital, Manchester M23 [email protected]
1 Jadad AR. Promoting partnerships: challenges for theinternet age. BMJ 1999;319:761-3. (18 September.)
2 Shepperd S, Charnock D, Gann B. Helping patients accesshigh quality health information. BMJ 1999;319:764-6.(18 September.)
3 Pal B, Laing H, Estrach C. A cyberclinic in rheumatology.J R Coll Phys London 1999;33:161-2.
4 Pal B. Cyber/virtual clinic in osteoporosis? A question-naire based feasibility study towards a rapid consultationand advisory service [abstract]. Ann Rheum Dis 1999:(suppl) No 1010.
5 Pal B. Email contact between doctor and patient. BMJ1999;318:1428.
New guidelines for urgentreferral of patients with cancerare waste of energyEditor—Guidelines have recently been sentout by the Department of Health for wideconsultation in the United Kingdom.1 Theaim is try to reduce mortality from cancer inthe United Kingdom by guaranteeing thatall patients who present to their generalpractitioner with symptoms possibly due tocancer are seen in a hospital clinic withintwo weeks. But there is no evidence whatso-ever that delay in diagnosis is a largeproblem in the United Kingdom. Efforts toimplement the so called two week policy aremisplaced. The guidelines themselves repre-sent a reasonable distillation from basicmedical textbooks, but they are patronisingto doctors, who have the longest universitytraining of any professional group. Mostcopies are likely to end up in the bin.
Those in the United Kingdom know thatit continues to lag behind its Europeanneighbours in cancer survival. Politiciansmust be educated about this rather than beallowed to continue with their obsessionabout waiting list targets. The whole exerciseis reminiscent of the man who loses his keyson the dark side of the road and looks forthem under the light across the street. In theUnited Kingdom the shortage of cancerspecialists is more than 500; £1.2bn isneeded to bring radiotherapy equipment upto date; and an extra £170m a year is neededfor chemotherapy. Facilities for good
psychosocial care are few, and people relyheavily on the charity sector for palliativecare. The Calman-Hine network is only par-tially and patchily implemented, with littlenew funding. There is still gross inequity inthe quality of cancer care in the UnitedKingdom. And there is no National CancerCentre to set the gold standard.
Ominously for the NHS are the clearsigns that there will be major improvementsin cancer treatment over the next decade.Next year will see the licensing of herceptinfor breast cancer by the European Medi-cines Evaluation Agency. This will be theforerunner of sophisticated targeted treat-ments that will require integrated molecularand therapeutic solutions. The humangenome project, scheduled for completionin 2003, will lead to new ways of predictingwhich people are at high risk of developingcancer. In the United Kingdom the basiccancer services need urgently to be put inorder to meet these new challenges, allowingBritish patients to reap the benefits of globalprogress. If the NHS cannot do it the privatesector will—but at a price.
The National Cancer Forum is a deriva-tive of the Calman-Hine group and isconvened irregularly. At its most recentmeeting this topic was raised, but the forumwas told that “ministers have gone too fardown the road on this one.” Why? It hasnever been on the agenda of the forum.During my two years with the World HealthOrganisation I have visited many countriesin different economic environments.Nowhere does a state health departmenthave a two week policy or send out such gra-tuitous advice to doctors—yet many havebetter outcomes for cancer care.
Although streamlining the diagnosticprocess and improving treatment resourcesmakes good sense, these new targets are awaste of energy. Along with NHS Direct andits latest variant—its interactive website—theyare simply window dressing. A significanteffort to improve the quality of cancer care isessential if we are really going to make animpact and save lives.Karol Sikora global vice presidentClinical Research (Oncology), Pharmacia andUpjohn, via Robert Koch, Milan 20152, [email protected]
1 Department of Health. Referral guidelines for suspectedcancer—consultation document. London: DoH, 1999. (HSC1999/241.) (www.doh.gov.uk/cancer)
Correction
Breast feeding and obesityTwo biometricians should have beenincluded with Johannes Hebebrands asauthors of the second letter in this cluster.They are Frank Geller and Andreas Ziegler,both from the Institute of Medical Biometryand Epidemiology at Philipps-University ofMarburg at Marburg in Germany.
Letters
59BMJ VOLUME 320 1 JANUARY 2000 www.bmj.com