Limitations in the Diagnosis of Childhood Teratoid Lesions on Fine Needle Aspiration Cytology
Rationale and design of the INFUSE-AMI study: A 2 × 2 factorial, randomized, multicenter,...
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Rationale and design of the INFUSE-AMI study: A 2 × 2 factorial, randomized, multicenter,...
Rationale and design of the INFUSE-AMI study:A 2 × 2 factorial, randomized, multicenter, single-blindevaluation of intracoronary abciximab infusion andaspiration thrombectomy in patients undergoingpercutaneous coronary intervention for anteriorST-segment elevation myocardial infarctionC. Michael Gibson, MS, MD,a ,j Akiko Maehara, MD,b,j Alexandra J. Lansky, MD,b,j Jochen Wohrle, MD,c,j
Tom Stuckey, MD,d,j Rajesh Dave, MD,e,j David Cox, MD,f,j Cindy Grines, MD,g,j Dariusz Dudek, MD,h,j
Gabriel Steg, MD, i,j Helen Parise, ScD, i,j Steven D. Wolff, MD, PhD,b,j Ecaterina Cristea, MD,b,j andGregg W. Stone, MDb,j Boston, MA; New York, NY; Ulm, Germany; Greensboro, NC; Harrisburg, and Allentown, PA;Royal Oak, MI; Krakow, Poland; and Paris, France
Background Whether thrombus aspiration and local glycoprotein IIb/IIIa administration reduce infarct size in patientswith ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI) has not beenestablished in multicenter studies.
Design INFUSE-AMI is a multicenter, open-label, controlled, single-blind randomized study enrolling 452 subjects withanterior STEMI and an occluded proximal or mid–left anterior descending artery with thrombosis in myocardial infarction 0, 1,or 2 grade flow undergoing primary PCI with bivalirudin anticoagulation. Subjects are randomized in a 2 × 2 factorial to oneof the following 4 arms: (1) local infusion of abciximab using the ClearWay RX Local Therapeutic Infusion Catheter (ClearWay,Atrium Medical Corp, Hudson, NH) after aspiration with a 6F Export Aspiration Catheter (Medtronic, Inc, Minneapolis, MN),(2) local infusion of abciximab using the ClearWay RX Infusion Catheter and no aspiration, (3) no local infusion of abciximaband aspiration with a 6F Export Aspiration Catheter, or (4) no local infusion of abciximab and no aspiration. The primary endpoint is infarct size (percentage of total left ventricular mass) at 30 days measured by cardiac magnetic resonance imaging.Other secondary end points include microvascular obstruction by cardiac magnetic resonance imaging at 5 days, ST-segmentresolution, angiographic myocardial perfusion, thrombus burden, angiographic complications, and clinical events through1-year follow-up. Safety end points include major and minor bleeding.
Summary INFUSE-AMI is testing the hypothesis that the intracoronary administration of an abciximab bolus with orwithout thrombus aspiration before stent implantation compared to no infusion with or without thrombus aspiration reducesinfarct size among patients undergoing primary PCI for anterior STEMI who are treated with bivalirudin. (Am Heart J2011;161:478-486.e7.)
BackgroundIn patients with ST elevation myocardial infarction
(STEMI), primary percutaneous coronary intervention
From the aCardiovascular Division, Department of Medicine, Beth Israel Deaconess MedicalCenter, Harvard Medical School, Boston, MA, bColumbia University Medical Center and theCardiovascular Research Foundation,NewYork,NY, cClinic of InternalMedicine II, Universityof Ulm, Ulm, Germany, dLeBauer Cardiovascular Research Foundation, UNC School ofMedicine, Greensboro, NC, eHarrisburg Hospital, Harrisburg, PA, fLehigh Valley Hospital,Allentown, PA, gWilliam Beaumont Hospital, Royal Oak, MI, hJagiellonian UniversityMedicalCollege Institute of Cardiology, Krakow, Poland, and iHopital Bichat-Claude BernadSer-vice de Cardiologie, Paris, France.j For the INFUSE-AMI Investigators.
(PCI) results in lower rates of reinfarction, stroke, anddeath than fibrinolytic therapy.1,2 This is because, at leastin part, of the fact that primary PCI more frequently
Mauricio G. Cohen, MD served as guest editor for this article.Clinical trial registration:ClinicalTrials.gov no. NCT00976521.Submitted August 27, 2010; accepted October 1, 2010.Reprint requests: C. Michael Gibson, MS, MD, 185 Pilgrim Road, Deaconess 319 Boston,MA 02215.E-mail: [email protected]/$ - see front matter© 2011, Mosby, Inc. All rights reserved.doi:10.1016/j.ahj.2010.10.006
Gibson et al 479American Heart JournalVolume 161, Number 3
restores normal epicardial coronary blood flow (throm-bosis in myocardial infarction [TIMI] 3 flow) (90% forprimary PCI vs 50%-60% for fibrinolytic therapy).3-7
However, studies with contrast echocardiography, Dopp-ler, positron emission tomography, and technetium Tc99m macroaggregated microspheres and angiographyhave demonstrated that despite restoration of TIMI 3epicardial flow after primary percutaneous transluminalcoronary angioplasty, normal myocardial perfusion isachieved in only 30% to 50% of patients.8-15 Persistentimpairment of myocardial perfusion on angiography hasbeen associated with more than a doubling of mortality at30 days, even in patients with TIMI 3 flow.15 Impairedmyocardial perfusion after recanalization of the infarctartery may be caused by myocardial edema, microvascu-lar spasm, loss of microvascular integrity, or distalthromboemboli with capillary plugging.16
It has been hypothesized that protection of the distalmicrocirculation during primary PCI should result inimproved TIMI 3 flow and myocardial perfusion. Theseimprovements should in turn result in reduced infarct sizeand preserved left ventricular function, which wouldultimately lead to reduced mortality. To date, there isinsufficient evidence supporting either the routine use ofdistal protection devices in capturing atherothromboticemboli or the use of adjunctive systemic pharmacother-apy, such as abciximab, to reduce thromboemboli.4-6
Proximal aspiration devices have been shown toimprove myocardial perfusion and improve ST-segmentresolution when used in STEMI patients.17-20 The TAPAS,a single-center randomized trial, showed that whencompared to conventional therapy, the Export AspirationCatheter (Medtronic, Inc, Minneapolis, MN) significantlyreduced cardiac death (3.6% vs 6.7%, P = .02) as well asdeath and myocardial infarction (MI) (5.6% vs 9.9%, P =.009).20 To date, these favorable single-center results havenot been replicated in multicenter trials.21 If thrombect-omy during primary PCI is indeed effective in reducingmortality, the mechanism presumably must be by afavorable effect on reducing infarct size. However,studies of aspiration have yielded mixed results; in onestudy, infarct size was paradoxically increased withaspiration,22 whereas, in a second smaller study, therewas a non significant trend toward a decrease in infarctsize with aspiration.23 Even in the TAPAS trial, there wasno significant reduction in infarct size as assessed by serialenzyme measures.24
Abciximab is a potent inhibitor of platelet aggregationthat may also promote the disaggregation of freshthombus at high local drug concentrations.25 In additionto its antiplatelet (glycoprotein [GP] IIb/IIIa mediated)properties, abciximab also exhibits anti-inflammatoryeffects by inhibiting smooth muscle cell migration andproliferation, thereby suppressing platelet, white cell,and endothelial-mediated mechanisms.26-28 Abciximabcan be delivered via the intravenous (IV) or the
intracoronary route. The systemic IV administration ofGP IIb/IIIa receptor inhibitors in STEMI patients under-going PCI and stenting of native vessels have demonstrat-ed mixed results in the RAPPORT, Munich, ADMIRAL,and CADILLAC trials.1,4-6 Furthermore, the increased riskof bleeding and thrombocytopenia in patients treatedwith systemic abciximab may reduce the efficacy of thismethod of agent administration.In small to modest sized studies, the intracoronary
administration of abciximab has been associated withimproved postprocedural coronary flow, myocardialperfusion, myocardial salvage, and left ventricular func-tion when compared to systemic administration of thedrug or placebo.28-36 The rationale for intracoronaryadministration of abciximab is based on the hypothesisthat local administration yields a higher rate of GPreceptor occupancy than systemic administration there-by improving disaggregation of downstream micro-thrombi.37-40 By potentiating the local anti-inflammatoryeffects of abciximab, reperfusion injury may also beminimized thereby resulting in greater myocardialsalvage. Moreover, intracoronary administration of abcix-imab has not been associated with increased bleedingcomplications or risks of immune response.40
The effect of intracoronary abciximab may be poten-tiated by its site-specific delivery via a rapid exchangetherapeutic infusion balloon catheter (the ClearWay RXInfusion Catheter, Atrium Medical Corp, Hudson, NH).41
The catheter has a novel occlusion, containment, andinfusion platform. The balloon occludes antegrade bloodflow while medications are infused through the micro-porous polytetrafluoroethylene (PTFE) material of theballoon. This mode of delivery achieves local drugconcentrations that are orders of magnitude higher thanthat achieved systemically as well as a longer local dwelltime of several minutes rather than that achieved with atransient bolus over seconds. As a result, drug bioavail-ability at the site of the thrombus may be maximized,leading to greater dissociation of bound fibrinogen fromthe GP IIb/IIIa receptors thereby leading to superiorthrombus disaggregation in the artery and the microvas-culature. Indeed, as compared to administration via aguide catheter, abciximab delivery via the ClearWaycatheter has been associated with a significant reductionin thrombus burden and with improved flow.42,43
Finally, the multicenter, prospective HORIZONS-AMItrial randomized 3,602 patients with STEMI undergoingprimary PCI to unfractionated heparin plus a GP IIb/IIIainhibitor versus the direct thrombin inhibitor bivalirudinalone (with the use of GP IIb/IIIa inhibitors reserved forrefractory ischemic or thrombotic procedural complica-tions). Compared to heparin plus a GP IIb/IIIa inhibitor,bivalirudin resulted in reduced rates of major and minorbleeding, thrombocytopenia, and blood transfusions andsignificantly improved survival at 30 days 1 year.44,45
However, stent thrombosis was increased with bivalir-
480 Gibson et alAmerican Heart Journal
March 2011
udin within the first 24 hours (though not at 30 days or1 year) possibly because of lack of potent antiplateletcoverage early before maximal thienopyridine effect. Thecombination of bivalirudin with abciximab was notevaluated in HORIZONS-AMI, and it is hypothesized thatthis combination of agents may further improve clinicaloutcomes by improving myocardial perfusion andlimiting stent thrombosis. Moreover, an intracoronaryabciximab bolus alone in patients undergoing primarystenting with bivalirudin might have these favorableeffects while minimizing bleeding compared to thestandard IV bolus and 12-hour abciximab infusion.Thus, the early localized intracoronary infusion of a
potent antiplatelet agent, such as abciximab, in STEMIpatients treated with bivalirudin before primary PCI aswell as the use of catheter-based aspiration offers thepotential to reduce thrombus burden, distal emboliza-tion, no reflow, and stent thrombosis. Taken together, itis hypothesized that these effects would in turn improvemicrocirculatory function and reduce infarct size withoutincurring a significant increase in bleeding. We describeherein the design of the INFUSE-AMI study, a 2 × 2factorial, randomized, multicenter, single-blind evalua-tion of intracoronary abciximab infusion and aspirationthrombectomy in patients undergoing primary PCI.
Study objectivesIn the INFUSE-AMI trial, patients with anterior STEMI
undergoing primary PCI treated with bivalirudin as afoundation anticoagulant are randomized in a 2 × 2factorial to one of the following 4 arms: (1) localinfusion of abciximab using the ClearWay RX InfusionCatheter after aspiration with a 6F Export AspirationCatheter, (2) local infusion of abciximab using theClearWay RX Infusion Catheter and no aspiration, (3) nolocal infusion of abciximab and aspiration with a 6FExport Aspiration Catheter, or (4) no local infusion ofabciximab and no aspiration.The primary objective of the study is to demonstrate
that in patients with a large amount of myocardium at risk(anterior STEMI), administration of an intracoronarybolus of abciximab before stent implantation via theClearWay catheter compared to no abciximab bolus(standard of care) results in reduced infarct size measuredby cardiac magnetic resonance imaging (MRI) at 30 days(range −7/+14 days, ie, between 23 and 44 days), reducedmicrovascular obstruction (MVO) by cardiac MRI at 5 ± 2days (ie, between 3 and 7 days), enhanced ST-segmentresolution, improved angiographic myocardial perfusion,reduced thrombus burden and angiographic complica-tions, and no increase in major and minor bleeding.Subjects with and without thrombus aspiration will becombined for this analysis.The major secondary objective of the study is to
demonstrate that among subjects undergoing primary
PCI for anterior STEMI, thrombus aspiration compared tono thrombus aspiration before stent implantation (usingthe same catheter and technique as in TAPAS) results inreduced infarct size and MVO measured by cardiac MRI,enhanced ST-segment resolution, improved myocardialperfusion, reduced thrombus burden and angiographiccomplications, and reduced MVO by cardiac MRI at 5 ± 2days (ie, between 3 and 7 days). Subjects with andwithout abciximab administration will be combined forthis analysis.
Study population and patient selectionThis is a multicenter, open-label, controlled, single-
blind randomized study with up to 452 subjects ≥18years enrolled in up to 50 US and European sites.Magnetic resonance imaging will be performed in allpatients at 30 days. In addition, a cardiac MRI substudy at5 days to evaluate MVO will be performed, with up to160 subjects at up to 30 sites. Study participants mustexperience clinical symptoms consistent with acute MI(eg, chest pain, arm pain, etc) for at least 30 minutes andbe unresponsive to nitroglycerin. They must present tothe hospital with an anterior MI with an electrocardio-gram showing at least 1 mm of ST-segment elevation in≥2 contiguous leads in V1 to V4 or new left bundle-branch block. Study subjects must have an anticipatedsymptom onset to balloon or aspiration time of ≤5hours, a time frame chosen such that myocardial salvagemay still be achievable.46 All patients will provideinformed written consent.In addition, subjects will undergo preprocedure
(baseline) angiography as the final assessment of studyeligibility. The infarct must be located in the proximalor mid–left anterior descending (LAD) coronary artery,with TIMI 0, 1, or 2 grade flow at the time of initialdiagnostic angiography (before wire passage). Based onthe coronary anatomy, there must be an indication forprimary PCI with plans to treat only 1 epicardialcoronary artery.Major general exclusion criteria include prior MI or
known prior systolic dysfunction (known ejectionfraction b40% by any prior measure or regional wallmotion abnormalities); a history of bypass surgery(coronary artery bypass graft); impaired renal function(creatinine clearance b30 mL/min per 1.73 m2 [or b51.99cm3/min, estimated with the Cockcroft-Gault formula])or on dialysis; known platelet count b100,000 cells/mm3
or N700,000 cells/mm3 or an hemoglobin (Hgb) b 10g/dL; gastrointestinal or genitourinary bleeding withinthe last 2 months or major surgery within 6 weeks; activebleeding or a history of bleeding diathesis or coagulo-pathy (including heparin-induced thrombocytopenia) orrefusal to receive blood transfusions if necessary;previous coronary stent implantation in patients whosecoronary angiography demonstrates stent thrombosis to
Gibson et al 481American Heart JournalVolume 161, Number 3
be the cause of the STEMI; any previous angioplasty orstenting procedures in the LAD artery; another medicalillness (eg, cancer, known malignancy, or congestiveheart failure); a history of intracerebral mass, aneurysm,arteriovenous malformation, or hemorrhagic stroke; or astroke or transient ischemic attack within the past6 months or any permanent residual neurologic defect.Specific angiographic exclusion criteria include coro-
nary anatomy that may require coronary artery bypassgraft surgery within 30 days; anticipated multivesselintervention during the index procedure (planned,staged procedures are permitted with strong recommen-dation to be performed after the 30-day end points andMRI are completed); severe vessel tortuosity, diffusedisease, or severe calcification that may impede success-ful delivery of the ClearWay RX Infusion Catheter or theExport Aspiration Catheter; the presence of features thatare highly unfavorable for PCI; MI caused by thrombosiswithin or adjacent to a previously implanted stent;severe mitral regurgitation or a ventricular septal defect(VSD) as demonstrated by left ventriculography; or anunprotected left main stenosis N40% or that will requireintervention. The online Appendix A contains additionalexclusion criteria.
Randomization and treatment protocolSubjects who meet all clinical eligibility criteria and
who sign the consent form must undergo protocol-specified laboratory tests before the index procedure(online Appendix B). Once all the criteria are met,subjects receive a 324 mg chewed or 250 to 500 mg IVloading dose of aspirin and 600-mg p.o. clopidogrel or 60-mg p.o. prasugrel per local investigator discretion.Subjects then undergo emergent left ventriculographyand coronary arteriography before being screened forangiographic eligibility criteria. Bivalirudin bolus andinfusion are started before PCI, initiated either in theemergency department or in the catheterization labora-tory. Up to 5000 U of IV heparin may be administeredbefore arrival in the catheterization laboratory but nonethereafter. Appendix C contains detailed dosing informa-tion regarding the bivalirudin bolus and infusion.The study coordinator/investigator then calls the
Interactive Voice Response System for randomization,and the subject is randomized in a 2 × 2 factorial to oneof the following 4 arms: (1) local infusion of abciximabusing the ClearWay RX Infusion Catheter after aspirationwith a 6F Export Aspiration Catheter, (2) local infusionof abciximab using the ClearWay RX Infusion Catheterand no aspiration, (3) no local infusion of abciximab andaspiration with a 6F Export Aspiration Catheter, or (4)no local infusion of abciximab and no aspiration.Randomization is stratified by time from symptoms toangiogram b3 hours versus ≥3 hours and by whetherthe infarct lesion is in the proximal or mid-LAD (before
or after the first septal perforator, respectively) viastratified block randomization.Once randomization is assigned, the subject is
officially enrolled in the study. All subjects will haveclinical follow-up at discharge (in-hospital), an officefollow-up visit at 30 days (range −7/+14 days, ie,between 23 and 44 days), and an office/telephonefollow-up visit at 12 months (±28 days). At each of these3 time points, both safety and effectiveness are to beevaluated. All patients will undergo cardiac MRI imagingat 30 days (range −7/+14 days, ie, between 23 and44 days). The first 160 patients enrolled at selected siteswill also be evaluated by cardiac MRI at 5 ± 2 days (ie,between 3 and 7 days).Online Appendix D outlines the screening and enroll-
ment process in greater detail.
Primary and secondary end pointsThe primary end point is infarct size (percentage of
total left ventricle [LV] mass) at 30 days (range −7/+14days, ie, between 23 to 44 days) measured by cardiacMRI, comparing the pooled, randomized, active (abcix-imab) infusion (with or without thrombus aspiration)to the pooled noninfusion arms (with or withoutthrombus aspiration).The major secondary end point is infarct size (grams
and percentage of total LV mass) at 30 days (range −7/+14days, ie, between 23 and 44 days) measured by cardiacMRI, comparing the pooled, randomized aspiration arms(with or without local infusion of abciximab) to thepooled no aspiration arms (with or without local infusionof abciximab).Other secondary end points are being examined across
both pooled arms. They include the following:
1. Incidence of final TIMI 3 flow and corrected TIMIframe counts;
2. Final myocardial perfusion measured by angio-graphic myocardial blush grade;
3. Thrombus area after infusion or aspiration beforestent implantation;
4. Incidence of complete ST-segment resolution 60 ±30 minutes after the last angiogram;
5. Major adverse cardiac events (MACE);6. Major adverse cardiac and cerebrovascular events;7. Net adverse clinical events (which is MACE +
bleeding) in-hospital at 30 days and 12 months postindex procedure;
8. Major or minor bleeding in-hospital at 30 days and12 months post index procedure;
9. New onset severe heart failure;10. Rehospitalization for heart failure.
Online Appendix E contains additional secondaryend points.
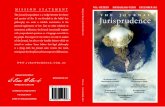
Figure 1
The upper left panel shows an area of MVO, which appears as a black area inside an area of delayed enhancement. The bottom right panel showscontiguous slices from the base to the apex of each infarct area, which will be analyzed as shown in the upper right where the white area will besummed across multiple slices as total infarct volume.
482 Gibson et alAmerican Heart Journal
March 2011
Cardiac MRI substudy end pointsThe primary end point for the cardiac MRI substudy is
MVO size (grams and percentage of total LV mass andpercentage of total infarct mass) at 5 ± 2 days(ie, between 3 and 7 days) from the time of the indexprocedure measured by cardiac MRI (Figure 1).Secondary end points for the cardiac MRI substudy
include the following:
1. Left ventricular ejection fraction (%), left ventricularend-diastolic volume (mL), and left ventricular end-systolic volume (mL) at 30 days (range −7/+14 days,ie, between 23 and 44 days) and at 5 ± 2 days (ie,between 3 and 7 days) from the time of the indexprocedure measured by cardiac MRI;
2. Myocardial stunning score at 30 days (range −7/+14days, ie, between 23 and 44 days) evaluated bycardiac MRI, comparing acute phase MRI at 5 ± 2days (ie, between 3 and 7 days) and MRI at 30 days(range −7/+14 days, ie, between 23 and 44 days);
3. Infarct size (grams and percentage of total LV mass)at 5 ± 2 days (ie, between 3 and 7 days) from the
time of the index procedure measured by cardiacMRI. Online Appendix E contains additional sub-study secondary end points.
Primary and secondary endpoint definitionsFor the primary end point, infarct size is defined as
the percentage of total LV mass. Infarct size as asecondary end point will also be measured in grams inaddition to being defined as the percentage of total LVmass. These end points are computed from myocardialdelayed enhancement images (Figure 1). Thrombosis in
myocardial infarction 3 flow is defined as antegradeflow into the terminal coronary artery segment througha stenosis that is as prompt as antegrade flow into acomparable segment without a stenosis, with contrastmaterial clearing as rapidly from the distal segment asfrom an uninvolved segment.47 Myocardial perfusionmeasured by angiographic myocardial blush grade has ascoring system of 0, 1, 2, or 3.48 Blush 0 indicates anabsence of opacification or staining, blush 1 signifies a
Gibson et al 483American Heart JournalVolume 161, Number 3
minimal contrast opacification, blush 2 indicates areduced but clearly evident blush in the infarct zonecompared to the ipsilateral or contralateral noninvolvedepicardial vessel(s), and blush 3 signifies myocardialcontrast filling equal to or greater than that seen in thenoninvolved epicardial vessel(s). Complete ST-segment
resolution is defined as ≥70% ST resolution in patientswithout left bundle-branch block.49,50
Major adverse cardiac events is the composite of death,reinfarction, new onset severe heart failure, or rehospi-talization for heart failure. Major adverse cardiac and
cerebrovascular events is defined as combined eventsconsisting of ischemia resulting in target vessel revascu-larization, death, reinfarction (Q wave and non–Qwave), and stroke. Net adverse clinical events is thecomposite of all deaths, MIs (Q wave and non–Q waveMI), ischemic target lesion revascularizations (TLRs),and major bleedings. Severe heart failure is defined asheart failure requiring intubation, intra-aortic balloonpump insertion, 100% oxygen by face mask, documen-ted PaO2 b60 mm Hg or radiographic evidence ofpulmonary edema, or heart failure necessitating rehos-pitalization. Major or minor bleeding is defined using theTIMI scale, HORIZONS scale, GUSTO scale, thrombocy-topenia, and transfusions.See online Appendix F for additional end point
definitions.
Statistical considerationsThis is a single-blind clinical study. The physician
performing the procedure as well as the staff presentduring the index procedure will not be blinded, but thesubjects and family members, the sponsor and biostatis-ticians performing the analysis, clinical event committee/data safety monitoring board (CEC/DSMB), and all corelaboratories will be blinded to the treatment arms of thisstudy. Unblinding will occur only after the database hasbeen locked for the analysis of the primary end point or toprotect subject rights, welfare, or well-being.The study is powered for infarct size determination at
30 days. Evaluating 408 subjects would provide 80%power to demonstrate a relative 25% reduction in infarctsize from 24% to 18% (SD 21%). Assuming approximately10% lost to follow-up, 452 subjects will be randomized.The cardiac MRI substudy is powered for MVO size as a
percentage of total LV mass determination at 5 days.Enrolling a total of 152 subjects would provide 99%power to demonstrate a 50% reduction in MVO from 4%(SD 3%) to 2% (SD 1.5%). Assuming a 5% dropout, 160 willbe enrolled in the substudy.There are 2 analysis sets defined for this study: the
Intent to Treat (ITT) Analysis Set and the Per ProtocolAnalysis Set. All subjects who have enrolled into thestudy, regardless of whether treatment is actuallyreceived, are counted in the ITT Analysis Set. The
Per Protocol Analysis Set will include all enrolledsubjects who receive the intended treatment with nomajor protocol deviations. Major protocol deviationsinclude, but are not limited to, enrollment of a subjectwhose informed consent was not properly obtained,who did not meet all the inclusion or exclusioncriteria, or who did not receive treatment according totheir randomized assignment.The primary and all secondary end points will be
summarized for each treatment arm as well as withineach of the 4 randomized groups. As an additionalanalysis, the primary end point will also be evaluatedusing the Per Protocol set.For both the main study and cardiac MRI substudy, no
imputation of or adjustments for missing data will beperformed for the primary analyses. All available data willbe presented, following intention to treat principles. Fortime-to-event analyses, subjects will be censored at theirlast known follow-up.For the main study, secondary infarct size analyses will
be done with missing infarct size data imputed using thefollowing baseline variables to best match missing cases:baseline left ventricular ejection fraction (LVEF), proxi-mal versus mid-LAD occlusion, the presence of collat-erals, time to reperfusion, age, and sex. An additionalsecondary analysis will be done in which all patients withmissing infarct size data who died before the end of thecardiac MRI assessment period (ie, before 44 days) will beassigned an imputed infarct size equal to the largestinfarct size value measured in either arm in the study.All statistical analyses will be performed using SAS
System (SAS Institute, Inc, Cary, NC) statistical software(version 9.1 or higher), unless otherwise noted. Forboth the main study and the cardiac MRI substudy, themean, SD, median, interquartile range (IQR), andminimum and maximum values of continuous variableswill be presented. Groups will be compared using theWilcoxon rank sum test. The primary end points for thestudy and substudy (infarct size and MVO size,respectively) are known to be non-normally distributedand will be reported as medians with IQRs andminimum and maximum values. For these primary endpoints, data will only be analyzed in subjects completingthe cardiac MRI study in whom the imaging data arereceived at and analyzable by the core laboratory. Forcategorical variables, the frequencies and percentagewithin each category will be calculated. Groups will becompared using the χ2 or Fisher exact test, asappropriate. Time-to-event data will be summarizedusing Kaplan-Meier methods and compared betweengroups using the log-rank test. Data will be summarizedfor each of the treatment arms independently, infusionand aspiration, as well as separately for each of the 4categories of the 2 × 2 randomization.Baseline demographic and clinical variables will be
summarized for each of the 4 randomized groups and
484 Gibson et alAmerican Heart Journal
March 2011
combined within each of the infusion and aspirationtreatment arms for both the ITT and Per Protocolpopulations in the main study and for just the ITTpopulation in the substudy cohort.For the primary analyses in both the main study and
substudy, a test of the interaction of the 2 treatment armswill be done using standard analysis of variance models.In addition, interaction testing for the secondary endpoints in the main study and substudy will be performedfor the 2 treatment arms of the 2 × 2 factorial usinganalysis of variance and logistic regression.Because there is a single primary end point of interest in
this study and substudy, no adjustments for multiplecomparisons are necessary. In addition, no adjustment forcovariates is planned for the primary analyses but may beperformed for secondary analyses in the main study.Furthermore, as this is a multicenter study, heterogeneityof the treatment effects with respect to sites will beexplored, and the results will be reported for both themain study and the substudy. Sites with b10 subjects willbe combined for this analysis.
Statistical hypotheses for trial objectivesThe following hypotheses corresponding to the trial
objectives will be tested.• Main study (based primarily on the ITT analysis set
and then additionally on the Per Protocol set)In subjects undergoing primary PCI for anterior STEMItreated with a bivalirudin monotherapy anticoagula-tion strategy, the pooled, randomized, active (abcix-imab) infusion arm (with or without thrombusaspiration) is superior to the pooled control noninfu-sion arm (with or without thrombus aspiration) in thereduction of infarct size measured by cardiac MRI at30 days.
Formal assumptions and hypotheses:A, population of infarct sizes at 30 days in thecontrol arm (24%)B, population of infarct sizes at 30 days in the activeinfusion arm (18%)204 subjects in each armα Error = 5% 2 sidedPower 80%Reduction 25%
Hypotheses:H0: A = BHa: A ≠ BThe hypothesis will be tested using the nonparametricWilcoxon rank sum test. Given the fact that infarctsize is non-normally distributed, infarct size will bereported as medians with IQR.
• Magnetic resonance imaging substudy (based on theITT analysis set)
In subjects undergoing primary PCI for anteriorSTEMI treated with a bivalirudin monotherapyanticoagulation strategy, the pooled, randomized,active (abciximab) infusion arm (with or withoutthrombus aspiration) is superior to the pooledcontrol noninfusion arm (with or without thrombusaspiration) in the reduction of MVO size as apercentage of total LV mass at 5 days.
Formal assumptions and hypotheses:A, population of MVO sizes at 5 days in the controlarm (4%)
B, population of MVO sizes at 5 days in the activeinfusion arm (2%)
72 subjects in each arm
α Error = 5% 2 sided
Power ≥99%
Reduction 50%
Hypotheses:H0: A = B
Ha: A ≠ BThe hypothesis will be tested using the nonparametricWilcoxon rank sum test.
Prespecified subgroups for analysisThe following subgroups of interest are prespecified
for analysis in the main study: proximal LAD versus mid-LAD infarct lesion location, less than the baselineangiographic LVEF versus greater than or equal to themedian (core laboratory analysis), less than the time fromsymptom onset to balloon or aspiration versus greaterthan or equal to the median, the presence of collaterals atbaseline (as determined by the angiographic corelaboratory) (yes or no), groups pooled by infusion andthrombectomy randomization, and in the 4 randomizedgroups individually (infusion with aspiration, infusionwithout aspiration, no infusion with aspiration, noinfusion without aspiration).
Interim analysisA pooled (blinded) interim analysis will be performed
once 200 subjects have reached the 30-day end point forsample size re-estimation in the main study. If the lost–to–follow-up rate is higher than expected, no action willbe taken. The sample size may be increased if a smallerpooled mean infarct size than expected or larger SDthan expected is determined; otherwise, no action willbe taken. The sample size will not be adjusteddownward. No differences between treatments will beexamined at this time. Thus, no adjustment to α isnecessary for this re-estimation.
Gibson et al 485American Heart JournalVolume 161, Number 3
ConclusionINFUSE-AMI will enroll patients undergoing primary
PCI for anterior STEMI and baseline TIMI 0 to 2 flowtreated with a bivalirudin monotherapy anticoagulationstrategy in the early hours of infarct evolution, a timeduring which myocardial salvage should be possible. Itis sufficiently powered to provide definitive data prima-rily regarding the efficacy of an intracoronary infusion ofan abciximab bolus before stent implantation comparedto no infusion, with or without thrombus aspiration, onMVO at 5 days and infarct size determination at 30 days.The trial will also provide important information regard-ing the efficacy of thrombus aspiration to reduce infarctsize. Secondary angiographic, electrocardiographic, andclinical end points will assess additional measures of thesafety and efficacy of these 2 approaches in patients withSTEMI and a large amount of myocardium at riskundergoing a PCI for primary reperfusion.
References1. Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary
coronary angioplasty and intravenous thrombolytic therapy for acutemyocardial infarction. A quantitative review. JAMA 1997;278:2093-8.
2. Stone GW, Brodie BR, Griffin JJ, et al. Clinical and angiographicfollow-up after primary stenting in acute myocardial infarction: theprimary angioplasty in myocardial infarction (PAMI) stent pilot trial.Circulation 1999;99:1548-54.
3. Grines CL, Cox D, Stone GW, et al. A randomized trial of primaryangioplasty compared to heparin-coated stent implantation for acutemyocardial infarction. N Engl J Med 1999;341:1949-56.
4. Marso SP, Miller T, Rutherford BD, et al. Comparison of myocardialreperfusion in patients undergoing percutaneous coronary interven-tion in ST-segment elevation acute myocardial infarction with versuswithout diabetes mellitus (from the EMERALD trial). Am J Cardiol2007;100:206-10.
5. Brener SJ, Barr LA, Burchenal JE, et al. Randomized, placebo-controlled trial of platelet glycoprotein IIb/IIIa blockade with primaryangioplasty for acute myocardial infarction: ReoPro and primaryPTCA organization and randomized trial (RAPPORT) investigators.Circulation 1998;98:734-41.
6. Montalescot G, Barragan P, Wittenberg O, et al. Platelet glycoproteinIIb/IIIa inhibition with coronary stenting for acute myocardialinfarction. N Engl J Med 2001;344:1895-903.
7. Stone GW, Grines CL, Cox D, et al. A prospective, multicenter,international randomized trial comparing four reperfusion strategiesin acute myocardial infarction: principal report of the controlledabciximab and device investigation to lower late angioplastycomplications (CADILLAC) trial. J Am Coll Cardiol 2001;37:648A.
8. Kondo M, Nakano A, Saito D, et al. Assessment of “microvascularno-reflow phenomenon” using technetium-99 m macroaggregatedalbumin scintigraphy in patients with acute myocardial infarction.J Am Coll Cardiol 1998;32:898-903.
9. Belli G, Pezzano A, De Biase AM, et al. Adjunctive thrombusaspiration and mechanical protection from distal embolization inprimary percutaneous intervention for acute myocardial infarction.Catheter Cardiovasc Interv 2000;50:362-70.
10. Schröder R, Wegscheider K, Schröder K, et al. Extent of earlyST-segment elevation resolution: a strong predictor of outcome inpatients with acute myocardial infarction and a sensitive measure tocompare thrombolytic regimens. J Am Coll Cardiol 1995;26:1657-64.
11. The GUSTO Angiographic Investigators. The effects of tissueplasminogen activator, streptokinase, or both on coronary-arterypatency, ventricular function, and survival after acute myocardialinfarction. N Engl J Med 1993;329:1615-22.
12. Anderson JL, Karagounis LA, Califf RM. Meta analysis of five reportedstudies on the relation of early coronary patency grades with mortalityand outcomes after acute myocardial infarction. Am J Cardiol 1996;78:1-8.
13. Ito H, Okamura A, Iwakura K, et al. Myocardial perfusion patternsrelated to thrombolysis in myocardial infarction perfusion gradesafter coronary angioplasty in patients with acute anterior myocardialinfarction. Circulation 1996;93:1993-9.
14. Neumann FJ, Blasini R, Schmitt C, et al. Effect of glycoprotein IIb/IIIareceptor blockade on recovery of coronary flow and left ventricularfunction after the placement of coronary-artery stents in acutemyocardial infarction. Circulation 1998;98:2695-701.
15. Costantini CO, Stone GW, Mehran R, et al. Frequency, correlates,and clinical implications of myocardial perfusion after primaryangioplasty and stenting, with and without glycoprotein IIb/IIIainhibition, in acute myocardial infarction. J Am Coll Cardiol 2004;44:305-12.
16. De Lemos JA, Antman EM, Gibson CM, et al. Abciximab improvesboth epicardial flow and myocardial reperfusion in ST-elevationmyocardial infarction: observations from the TIMI 14 study.Circulation 2000;101:239-43.
17. Galiuto L, Garramone B, Burzotta F, et al. Thrombus aspirationreduces microvascular obstruction after primary coronary interven-tion: a myocardial contract echocardiography sub-study of theREMEDIA trial. J Am Coll Cardiol 2006;48:1355-60.
18. Silva-Orrego P, Colombo P, Bigi R. Thrombus aspiration beforeprimary angioplasty improves myocardial reperfusion in acutemyocardial infarction: the DEAR-MI study. J Am Coll Cardiol 2006;48:1552-9.
19. De Luca L, G Sardella G, Davidson CJ. Impact of intracoronaryaspiration thrombectomy during primary angioplasty on the leftventricular remodeling in patients with anterior ST elevationmyocardial infarction. Heart 2006;92:951-6.
20. Vlaar PJ, Svilaas T, van der Horst IC, et al. Cardiac death andreinfarction after 1 year in the Thrombus Aspiration duringPercutaneous coronary intervention in acute myocardial infarctionStudy (TAPAS): a 1-year follow-up study. Lancet 2008;371:1915-20.
21. Inaba Y, Chen JA, Mehta N, et al. Impact of single or multicentrestudy design on the results of trials examining the efficacy ofadjunctive devices to prevent distal embolisation during acutemyocardial infarction. EuroIntervention 2009;5:375-83.
22. Kaltoft A, Bøttcher M, Nielsen SS, et al. Routine thrombectomy inpercutaneous coronary intervention for acute ST-segment-elevationmyocardial infarction: a randomized, controlled trial. Circulation2006;114:40-7.
23. Sardella G, Mancone M, Bucciarelli-Ducci C, et al. Thrombusaspiration during primary percutaneous coronary interventionimproves myocardial reperfusion and reduces infarct size: the EXPIRA(thrombectomy with export catheter in infarct-related artery duringprimary percutaneous coronary intervention) prospective, random-ized trial. J Am Coll Cardiol 2009;53:309-15.
486 Gibson et alAmerican Heart Journal
March 2011
24. Svilaas T, Vlaar PJ, van der Horst IC, et al. Thrombus aspirationduring primary percutaneous coronary intervention. N Engl J Med2008;358:557-67.
25. Collet JP, Montalescot G, Lesty C, et al. Disaggregation of in vitropreformed platelet-rich clots by abciximab increases fibrin exposureand promotes fibrinolysis. Arterioscler Thromb Vasc Biol 2001;21:142-8.
26. Simon DI, Xu H, Ortlepp S, et al. 7E3 monoclonal antibody directedagainst the platelet glycoprotein IIb/IIIa cross reacts with the leukocyteintegrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1.Arterioscler Thromb Vasc Biol 1997;17:528-35.
27. Schwartz M, Nordt T, Bode C, et al. The GPIIb/IIIa inhibitorabciximab (c7E3) inhibits the binding of various ligands to theleukocyte integrin Mac-1 (CD11b/CD18, alphaMbeta2). Thromb Res2002;107:121-8.
28. Kupatt C, Habazettl H, Hanusch P, et al. C7E3Fab reduces postischemic leukocyte-thrombocyte interaction mediated by fibrinogen:implications for myocardial reperfusion injury. Arterioscler ThrombVasc Biol 2000;20:2226-32.
29. Thuraisingham S, Tan KH. Dissolution of thrombus formed duringdirect coronary angioplasty with a single 10 mg intracoronary bolusdose of abciximab. Int J Clin Pract 1999;53:604-7.
30. Bailey SR, O'Leary E, Chilton R. Angioscopic evaluation of site-specific administration of ReoPro. Cathet Cardiovasc Diagn 1997;42:181-4.
31. Bartorelli AL, Trabattoni D, Galli S, et al. Successful dissolution ofocclusive coronary thrombus with local administration of abciximabduring PTCA. Catheter Cardiovasc Interven 1999;48:211-3.
32. Shlaifer JD, Horgan W, Malkowski MJ. Acute antithromboticocclusion of the left main coronary artery in a hypercoagulablepatient treated with intracoronary abciximab. Clin Cardiol 2001;24:788.
33. Barsness GW, Buller C, Ohman EM, et al. Reduced thrombus burdenwith abciximab delivered locally before percutaneous intervention insaphenous vein grafts. Am Heart J 2000;139:824-9.
34. Wohrle J, Grebe OC, Nusser T, et al. Reduction of adverse cardiacevents with intracoronary compared with intravenous bolus appli-cation of abciximab in patients with acute myocardial infarction orunstable angina undergoing coronary angioplasty. Circulation2003;107:1840-3.
35. Kakkar AK, Moustapha A, Hanley HG, et al. Comparison ofintracoronary vs. intravenous administration of abciximab incoronary stenting. Catheter Cardiovasc Interv 2004;61:31-4.
36. Thiele H, Schindler K, Friedenberger J, et al. Intracoronary comparedwith intravenous bolus abciximab application in patients with ST-elevation myocardial infarction undergoing primary percutaneouscoronary intervention. The randomized leipzig immediate percuta-neous coronary intervention abciximab IV versus IC in ST-elevationmyocardial infarction trial. Circulation 2008;118:49-57.
37. Deibele AJ, Jennings LK, Tcheng JE, et al. Intracoronaryeptifibatide bolus administration during percutaneous coronary
revascularization for acute coronary syndromes with evaluation ofplatelet glycoprotein IIb/IIIa receptor occupancy and plateletfunction: the Intracoronary Eptifibatide (ICE) trial. Circulation2010;121:784-91.
38. Gibson CM, Zorkun C, Kunadian V. Intracoronary administration ofabciximab in ST-elevation myocardial infarction. Circulation 2008;118:6-8.
39. Kunadian V, Zorkun C, Williams SP, et al. Intracoronary pharma-cotherapy in the management of coronary microvascular dysfunction.J Thromb Thrombolysis 2008;26:234-42.
40. Romagnoli E, Burzotta F, Trani C, et al. Rationale for intracoronaryadministration of abciximab. J Thromb Thrombolysis 2007;23:57-63.
41. Saraf S, Ong PJ, Gorog DA. ClearWay RX—Rapid exchangetherapeutic perfusion catheter. EuroIntervention 2008;3:639-42.
42. Capodanno D, Prati F, Pawlowsky T, et al. ClearWay RX system toreduce intracoronary thrombus in patients with acute coronarysyndromes according to optical coherence tomography afterabciximab intracoronary local infusion trial (COCTAIL): studyrationale and design. J Cardiovasc Med (Hagerstown) 2010;11:130-6.
43. Prati F, Ramazzatti V, Gil R, et al. COCKTAIL study: optimal treatmentof intracoronary thrombosis with local abciximab infusion throughthe ClearWay system. San Francisco: Transcatheter CardiovascularTherapeutics—TCT Conference; Sept 21-25; 2009.
44. Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin duringprimary PCI in acute myocardial infarction. N Engl J Med 2008;358:2218-30.
45. Mehran R, Lansky AJ, Witzenbichler B, et al. Bivalirudin in patientsundergoing primary angioplasty for acute myocardial infarction(HORIZONS-AMI): 1-year results of a randomised controlled trial.Lancet 2009;374:1149-59.
46. Gersh BJ, Stone GW,White HD, et al. Pharmacological facilitation ofprimary percutaneous coronary intervention for acute myocardialinfarction: is the slope of the curve the shape of the future? JAMA2005;293:979-86.
47. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase Ifindings. TIMI Study Group. N Engl J Med 1985;312:932-6.
48. van 't Hof AW, Liem A, Suryapranata H, et al. Angiographicassessment of myocardial reperfusion in patients treated with primaryangioplasty for acute myocardial infarction: myocardial blush grade.Zwolle Myocardial Infarction Study Group. Circulation 1998;97:2302-6.
49. Schröder R, Dissmann R, Bruggemann T, et al. Extent of early STsegment elevation resolution: a simple but strong predictor of outcomein patients with acute myocardial infarction. J Am Coll Cardiol 1994;24:384-91.
50. The ISAM Study Group. A prospective trial of intravenousstreptokinase in acute myocardial infarction (ISAM). Mortality,morbidity, and infarct size at 21 days. N Engl J Med 1986;314:1465-71.
Gibson et al 486.e1American Heart JournalVolume 161, Number 3
Appendix A. Additional exclusion criteria
Exclusion Criteria:
• A known hypersensitivity or contraindication toabciximab, aspirin, bivalirudin, clopidogrel, ticlopi-dine or prasugrel
• A known hypersensitivity or allergy to stainless steel,nickel, cobalt chromium, nitinol, or titanium
• A known hypersensitivity or allergy to contrastmedia (e.g. rash) that cannot effectively be con-trolled by premedication with steroids and/ordiphenhydramine
• A hypersensitivity or allergy to any of the compo-nents of the device (structural, drug or polymercomponents)
• True prior anaphylaxis to contrast media• Pregnancy, nursing, or plans of pregnancy in the oneyear period following the index procedure. Femalesubjects of child-bearing potential must have anegative pregnancy test done prior to the indexprocedure
• Definite planned use of aspiration, atherectomy,thrombectomy and/or distal protection cathetersprior to PTCA or stent implantation (other than insubjects randomized to thrombus aspiration)
• Receival of N5000 units of heparin prior topresentation to the catheterization laboratory
• Receival of heparin after arrival in the cardiaccatheterization laboratory prior to randomization
• Intended intracoronary infusion of supersaturatedoxygen (if this technology becomes available beforecompletion of enrollment)
• Any scheduled elective surgical procedures thatwould necessitate an interruption of antiplateletagents during the first twelve monthspost-enrollment
• Current use of coumadin or coumarin• Presentationwith cardiogenic shock (SBPb80mmHgfor N30 minutes, or requiring IV pressors or emer-gency IABP for hypotension treatment) or cardiopul-monary resuscitation prior to randomization
• Any organ transplant or being on a waiting list forany organ transplant
• Prior administration of thrombolytic therapy, GPIIb/IIIa inhibitors, low molecular weight heparinor fondaparinux for this admission (subjectsreceiving prior unfractionated heparin may beenrolled)
• Contraindications to undergo MRI imaging includeany of the following:
• A cardiac pacemaker or implantable defibrillator• Non-MRI-compatible aneurysm clip• Neural stimulator (e.g., TENS-Unit)• Any implanted or magnetically activated device(e.g., insulin pump)
• Any type of non-MRI-compatible metallic earimplant
• Metal shavings in the orbits• Any metallic foreign body, shrapnel, or bullet in alocation which the physician feels would presenta risk to the subject
• Any history indicating contraindication to MRI,including claustrophobia or allergy to gadolinium
• Inability to follow breathhold instructions or tomaintain a breathhold for N15 seconds
• Irregular cardiac rhythm not expected to resolveafter treatment of the acute cardiac condition(e.g., chronic atrial fibrillation)
• Known hypersensitivity or contraindication togladolinium contrast
• Known history of substance abuse (alcohol, cocaine,heroin etc.) that may cause non-compliance with theprotocol, confound the data interpretation or isassociated with a limited life expectancy of less thanone year
• Any significant medical condition which in theInvestigator's opinion may interfere with the sub-ject's optimal participation in the study
• Current participation in another investigational drugor device study, which has not completed theprimary endpoint follow-up period
• Previous enrollment in this study
486.e2 Gibson et alAmerican Heart Journal
March 2011
Appendix B
Schedule of events
Procedure/Test
Pre-procedure Procedure Post-procedureuntil dischargeCardiac MRIsub-study
(5 ± 2 days)
30 days(range -7 days/
+14 days)office visit
1 year(±28 days)office visit/
telephone call
Unscheduledvisits
Subject Medical / ClinicalHistory (age, sex,risk factors, anginastatus, cardiac history)
✓
Subject Informed Consent
✓ General Inclusion /Exclusion Criteria✓
Angiographic Inclusion /Exclusion Criteria
✓
Pregnancy Test (if applicable)
✓ Cardiac Enzymes (CK/CKMBor Troponin I or T if CK andCKMB are not available)✓
✓ ✓3 ✓3WBC
✓ Hgb, Hct, platelet count,creatinine✓
✓5Body weight and height,blood pressure,tobacco use history,diabetes mellitus status,other medical history
✓
✓1NYHA Class
✓4 ✓ Killip Class ✓ Cardiac MRI ✓1 ✓ ECG ✓ ✓2 ✓ ✓ ✓3Coronary Angiogramand LeftVentriculography
✓
Study Procedure( ± intracoronaryinfusion, ± aspiration)
✓
Per-protocol medications
✓ ✓ ✓ ✓ ✓ ✓ Dual Anti-platelet Medication ✓ ✓ ✓7 ✓ ✓ ✓ Concomitant CardiacMedications✓
✓ ✓ ✓ ✓ ✓Adverse Events8
✓ ✓ ✓ ✓ ✓ ✓1 If missed at baseline.2 ECG to be performed 60 ± 30 minutes after the last angiogram.3Required only if cardiac events.4Collected prior to MI.5Measured the day after the procedure and then daily until the nadir value for Hgb, Hct, platelet count and the peak value for serum creatinine is reached or the patient is discharged.6Only for subjects enrolled in cardiac MRI sub-study.7 Post-procedure DAPT is according to current recommended standards as published by the AHA/ACC/ESC, which recommends a minimum of 12 months DAPT for patients receivinga DES.8An adverse event is any untoward medical occurrence in a subject or clinical investigation subject administered a study product and which does not necessarily have a causalrelationship with this treatment. An adverse event (AE) can therefore be any unfavorable and unintended sign (including an abnormal laboratory finding), symptom, or diseasetemporarily associated with the use of a medicinal (investigational) product whether or not related to the study product. Elective procedures for a pre-existing condition are notconsidered AEs. Abnormal laboratory values will not be considered AEs unless: 1) the PI determined that the value is clinically significant, 2) the abnormal lab value requiredintervention, or 3) the abnormal lab value required subject termination from the study.
Gibson et al 486.e3American Heart JournalVolume 161, Number 3
Appendix C. Dosing information on thebivalirudin bolus and infusionIf angiography shows TIMI 0, 1 or 2 flow in an occluded
proximal or mid LAD and all other angiographic criteriaare met, a bivalirudin bolus and infusion is started(bivalirudin may be started prior to angiography if this isstandard of local practice):
• Bivalirudin is administered as a bolus 0.75 mg/kgIV plus an infusion of 1.75 mg/kg/h, not titrated to
Appendix D. Enrollment and procedure p
452 pts with anterior MI with anticipated
(Short-form or full) Informed consent in
Aspirin 324 mg chewed or 250-500 mg IV, clo
Emergent left ventriculography (mandatory
TIMI 0, 1, or 2 flow in occlude
YeBivalirudin bolus and infusion (note: bivalirudin may bcath lab per local practice). If unfractionated heparin w
and start the bivalirudin 30 minutes later, or just prioshould receive bivaliru
Call IVRandomize (stratify by time from symptom to ang
(Subject is considered formally enrolled after randomconsented but not randomized becau
Aspiration (Export®) No aspiration Active infusion Active infusion
ACT (adjusted for renal insufficiency as per thepackage IFU).
• If pre-procedural unfractionated heparin was admin-istered, bivalirudin should be started 30 minutesafter the last heparin dose, but in all cases prior toPCI (even if b30 minutes after the last heparin dose).
• Bivalirudin is typically terminated at the end of theprocedure unless prolonged antithrombin is needed(e.g., for an intra-aortic balloon pump), in whichcase the infusion is reduced to 0.25 mg/kg/hr.
• Routine post-PCI bivalirudin use is not permitted.
rocess
symptom to balloon time <5 hours
ER, baseline 12-lead EKG obtained
pidogrel 600 mg po or prasugrel 60 mg po
pre PCI) and coronary arteriography
d proximal or mid LAD? Not enrolled
s No e started pre or post randomization, and in ER or
as given prior to bivalirudin, withhold the heparinr to PCI, whichever occurs first (i.e., all subjects din prior to PCI)
RS io <vs. ≥3 hours and proximal vs. mid-LAD) ization – a screening log will be kept for patients se of angiographic exclusions)
Aspiration (Export®) No aspiration No infusion No infusion
If randomized to active infusion, cross lesion with a 1.0 or 1.5 mm ClearWay™ RX Infusion Catheter. If the lesion iscrossed or penetrated by at least 1mm, infuse abciximab (0.25 mg/kg body weight, infused at a rate of 10 cc overapproximately 60 seconds) through the ClearWay™ RX Infusion Catheter. If the lesion cannot be crossed with theClearWay™ RX Infusion Catheter, withdraw the device and dilate lesion with 2.0 mm balloon PTCA catheter. Cross thelesion with 1.5 mm ClearWay™ RX Infusion Catheter and infuse abcixmab. If the lesion still cannot be crossed, theClearWay™ RX Infusion Catheter may be inflated just proximal to the lesion and drug infused from this location(0.25 mg/kg body weight, infused at a rate of 10 cc over approximately 60 seconds). If the lesion length is longer than thelength of the ClearWay™ RX Infusion Catheter (20 mm), the ClearWay™ RX Infusion Catheter should be placed in themost proximal part of the lesion and abciximab infused from this location (0.25 mg/kg body weight, infused at a rate of 10cc over approximately 60 seconds). Once infusion is complete, pull negative on inflation syringe and remove theClearWay™ RX Infusion Catheter.If randomized to no active infusion, either pre-dilate or aspirate as randomized.
486.e4 Gibson et alAmerican Heart Journal
March 2011
All patients must have either pre-dilatation with a PTCA catheter or the ClearWay™ RX Infusion Catheter or aspirationprior to stent implantation. Exception: Direct stent implantation without balloon dilatation or aspiration is allowable peroperator discretion in subjects randomized to no abciximab without aspiration in whom TIMI 2 flow is present atbaseline, or in whom TIMI 2 or 3 flow is present after intracoronary guidewire passage allowing full delineation of thelesion length and reference vessel diameter.Stent implantation is recommended as per standard of care.Bail-out abciximab allowed only for presence of “giant” thrombus or sustained no reflow.
Appendix E. Additionalsecondary endpoints
Additional Secondary Endpoints for
INFUSE-AMI Trial
• Composite angiographic complications at any timeduring the procedure (e.g. new thrombus, forma-tion, transient or sustained no reflow or slow flow,distal embolization, side branch loss, acute closure)and requirement for bail-out nitroprusside, calciumchannel blocker or adenosine administration, orunplanned use of thrombectomy, aspiration or distalprotection devices
• Acute success (clinical device and clinical procedure)• Stent thrombosis (ARC definite and/or probable)
Additional Secondary Endpoints for the Cardiac
MRI Sub-study
• Transmural extent of infarction (%) at 30 days(range -7 days/+14 days; i.e., between 23 and44 days) and at 5 ± 2 days (i.e., between 3 and7 days) from the time of the index proceduremeasured by cardiac MRI
• Change of infarct size (grams and percentage of totalLV mass), change of LVEF (%), change of LVEDV(ml), change of LVESV (ml) between the two MRItime points for sub-study patients.
Gibson et al 486.e5American Heart JournalVolume 161, Number 3
Appendix F. Additional secondaryendpoint definitions
1. Additional Endpoint Definitions for INFUSE-AMI Trial
● ACUTE CLOSURE / ABRUPT CLOSURE
Occurrence of new severely reduced flow (TIMI grade0 or 1) within the target vessel during the indexprocedure that persists and requires rescue by anon-assigned treatment strategy (including emergencysurgery), or results in myocardial infarction or death.Abrupt closure requires proven association with amechanical dissection of the treatment lesion or instru-mented vessel, coronary thrombus, or severe spasm.Abrupt closure does not connote “no reflow” (due tomicrovascular flow limitation), in which the vessel ispatent but had reduced flow. Abrupt closure also doesnot connote transient closure with reduced flow in whichthe index treatment application reversed the closure.
• Subabrupt Closure
Abrupt closure that occurs after the indexprocedure is completed (and the subject left thecatheterization laboratory) and before the 30-dayfollow-up endpoint.
• Threatened Abrupt Closure
Defined as a grade B dissection and ≥50% diameterstenosis or any dissection of grade C or higher.
● ACUTE SUCCESS
Classified as follows:
• Lesion Success
Lesion success is defined as achievement of a finalin-stent residual diameter stenosis of b50%(by QCA) and TIMI-3 flow using anypercutaneous method.
• Procedure Success
Procedure success is defined as achievement of afinal in-stent diameter stenosis of b50% (by QCA)using the assigned device and with any adjunctivedevices and TIMI-3 flow, without the occurrence ofcardiac death, Q wave or non-Q wave MI, or repeatrevascularization of the target lesion during thehospital stay.
● DISSECTION
National Heart, Lung, and Blood Institute (NHLBI)
Dissection Classification System:
A. Minor radiolucencies within the lumen duringcontrast injection with no persistence after dyeclearance.
B. Parallel tracts or double lumen separated by aradiolucent area during contrast injection with nopersistence after dye clearance.
C. Extraluminal cap with persistence of contrast afterdye clearance from the lumen.
D. Spiral luminal filling defects.E. New persistent filling defects.F. Non-A-E types that lead to impaired flow or total
occlusion.
Note: Type E and F dissections may representthrombus.
● MYOCARDIAL INFARCTION (MI)
(Per ARC Circulation 2007:115: 2344-2351)
Myocardial infarction classification and criteria for diagnosis
Classification
Biomarker criteria⁎ Additional criteriaPeriproceduralPCI
Troponin N3 × URL or CK-MB N3 × URL
Baseline value bURL
PeriproceduralCABG
Troponin N5 × URL or CK-MB N5 × URL
Baseline value bURL andany of the following: newpathologic Q waves orLBBB, new native or graftvessel occlusion, imagingevidence of loss of viable
myocardium
Spontaneous Troponin NURL or CK-MBNURL
Sudden death Death before biomarkersobtained or beforeexpected to be elevated
Symptoms suggestive ofischemia and any of the
following: new STelevation or LBBB,
documented thrombus byangiography or autopsy
Reinfarction
Stable or decreasingvalues on 2 samples and20% increase 3 to 6 hoursafter second samplediagnose recurrent MI.
If biomarkers increasing orpeak not reached theninsufficient data to
diagnose recurrent MI.
URL=Upper Reference Limit (defined 99th percentile of normal reference range);LBBB=Left Bundle-branch Block⁎Baseline biomarker value requiring before study procedure and presumes a typicalrise and fall
– Periprocedural MI After PCI
The periprocedural period includes the first 48 hoursafter PCI.– Periprocedural MI After CABG
The periprocedural period includes the first 72 hoursafter coronary artery bypass grafting (CABG).– Spontaneous MI
MI after the periprocedural period may be secondary tolate stent complications or progression of native disease.Performance of ECG and angiography supports adjudi-cation to either a target or non-target vessel in most cases.With the unique issues and pathophysiological mech-
anisms associated with these later events as well as thedocumented adverse impact on short-and long-term
486.e6 Gibson et alAmerican Heart Journal
March 2011
prognosis, a more sensitive definition than for peripro-cedural MI of any elevation of troponin above the upperrange limit is used. All late events that are not associatedwith a revascularization procedure simply asspontaneous.– Electrocardiographic Classification
Within this category it is distinguished:– Q-wave MI (QMI)
Development of new pathological Q waves in 2 ormore contiguous leads (according to the Minnesota codeas assessed by the ECG core lab) with or without post-procedure CK or CK-MB levels elevated above normal.– Non Q-wave MI (NQMI)
All MIs not classified as Q waves.– Relation to the Target Vessel
All infarcts that cannot be clearly attributed to a vesselother than the target vessel will be considered related tothe target vessel.
● NO REFLOW
An acute reduction in coronary flow (TIMI grade 0-1) inthe absence of dissection, thrombus, spasm, or high-grade residual stenosis at the original target lesion. Alsosee “Acute Closure.”
● STENT THROMBOSIS
(Per ARC Circulation 2007:115:2344-2351):Stent Thrombosis should be reported as a cumulative
value at the different time points and with the differentseparate time points. Time 0 is defined as the time pointafter the guiding catheter has been removed and thesubject left the Catheterization lab.
Timing
Acute stent thrombosis⁎:
0 - 24 hours post stent implantation Subacute stent thrombosis⁎: N24 hours – 30 days post stent implantation Late stent thrombosis†: 30 days - 1 year post stent implantation Very late stent thrombosis†: N1 year post stent implantation⁎Acute/subacute can also be replaced by early stent thrombosis. Early stentthrombosis (0 - 30 days) - this definition is currently used in the community.† Including “primary” as well as “secondary” late stent thrombosis; “secondary” latestent thrombosis is a stent thrombosis after a target segment revascularization.
Categories (Definite, Probable, and Possible)
a. Definite stent thrombosis
Definite stent thrombosis is considered to haveoccurred by either angiographic or pathologicconfirmation.
Angiographic confirmation of stent thrombosis⁎
The presence of an intracoronary thrombus thatoriginates in the stent or in the segment 5 mm proximalor distal to the stent and presence of at least 1 of thefollowing criteria within a 48-hour time window:
• Acute onset of ischemic symptoms at rest• New ischemic ECG changes that suggest acuteischemia
• Typical rise and fall in cardiac biomarkers (refer todefinition of spontaneous MI)
• Nonocclusive thrombus• Defined as a (spheric, ovoid, or irregular) non-calcified filling defect or lucency surrounded bycontrast material (on 3 sides or within a coronarystenosis) seen in multiple projections, or persis-tence of contrast material within the lumen, or avisible embolization of intraluminal materialdownstream.
• Occlusive thrombus• TIMI 0 or TIMI 1 intrastent or proximal to a stentup to the most adjacent proximal side branch ormain branch (if originates from the side branch).
Pathological confirmation of stent thrombosisEvidence of recent thrombus within the stent deter-
mined at autopsy or via examination of tissue retrievedfollowing thrombectomy.
⁎ The incidental angiographic documentation of stentocclusion in the absence of clinical signs or symptomsis not considered a confirmed stent thrombosis(silent occlusion).
b. Probable stent thrombosis
Clinical definition of probable stent thrombosis isconsidered to have occurred after intracoronary stentingin the following cases:
○ Any unexplained death within the first 30 days†
○ Irrespective of the time after the index procedure,any MI that is related to documented acute ischemiain the territory of the implanted stent withoutangiographic confirmation of stent thrombosis and inthe absence of any other obvious cause
† For studies with ST-elevation MI population, one mayconsider the exclusion of unexplained death within30 days as evidence of probable stent thrombosis.
c. Possible stent thrombosis
Clinical definition of possible stent thrombosis isconsidered to have occurred with any unexplained deathfrom 30 days after intracoronary stenting until end ofstudy follow-up.For this protocol, the primary definition of stent
thrombosis is ARC definite or probable stent thrombosis –the ARC possible definition will not be consideredstent thrombosis.
2. Additional Endpoint Definition for the Cardiac MRISub-study
• TRANSMURAL EXTENT
Transmural extent of infarction (%) is calculated bycardiac MRI by dividing the infarct area by the total areaof pre-defined segment.
Gibson et al 486.e7American Heart JournalVolume 161, Number 3
Cardiac MRI Sub-study Endpoint Definitions
MVO size, the sub-study primary endpoint, is defined aslate hypo-enhancement within a hyper-enhanced regionon a late enhancement image.Secondary endpoints are defined in the following
manner. Left ventricular end-diastolic volume (LVEDV) isthe maximum left ventricular volume in milliliters at theend diastolic phase, while left ventricular end-systolicvolume (LVESV) is the minimum left ventricular volumein milliliters at the end systolic phase. Left ventricularejection fraction (LVEF) is the percentage that is equalto (LVEDV-LVESV)/LVEDV⁎100.Myocardial Stunning is evaluated per pre-specified
segment by MRI analysis. The function between theacute phase and 30 days will be compared andcategorized as score 0=no change, score 1=mildrecovery (recovered, but not completely), score2=marked recovery (recovered completely). Then, thetotal myocardial stunning score at 30 days will besummed for total segments.
Bleeding Definitions:
TIMI Major Bleeding is defined as intracranial hemor-rhage or is associated with a decrease in Hgb N5 g/dL
(or N15% of hematocrit), corrected by re-operation forbleeding or use of any blood product transfusion. TIMIMinor Bleeding is defined as observed blood loss (e.g.gross hematuria or hematemesis, heme-positive coffeeground emesis, heme-positive melena, hematoma orretroperitoneal bleeding) associated with a hemoglobindecrease of N3 g/dL (or a hematocrit decrease of N9%), ora hemoglobin decrease N4 g/dL (or N12% of hematocrit)with no bleeding site identified. HORIZONS majorbleeding is defined as any of the following: intracranialbleeding, intraocular bleeding, retroperitoneal bleeding,access site hemorrhage requiring surgery or a radiologicor interventional procedure, hematoma ≥5cm in diame-ter at the puncture site, reduction in hemoglobinconcentration of ≥4g/dL without an overt source ofbleeding, reduction in hemoglobin concentration of≥3g/dL with an overt source of bleeding, re-operation forbleeding, or the use of any blood product transfusion.The GUSTO classification defines bleeding as severe orlife-threatening, moderate, or mild, using intracranialhemorrhage and/or bleeding that requires interventionfor hemodynamic compromise, requires blood transfu-sion without compromise, or bleeding that meets noneof the above.