Needs-Based Planning for Persons With Schizophrenia Residing in Board-and-Care Homes
Transcript of Needs-Based Planning for Persons With Schizophrenia Residing in Board-and-Care Homes
Needs-Based Planning for PersonsWith Schizophrenia Residing in
Board-and-Care Homes
by Janet Durbin, Paula Qoering, Jeanette Cochrane,Dianne Macfarlane, and Tess Sheldon
Abstract
Data available from a recent planning project pro-vided an opportunity to examine impairment and ser-vice needs of individuals with schizophrenia spectrumdiagnoses living hi a large board-and-care program.When first implemented, this minimum-support custo-dial program was assumed to be adequate for dis-charged long-term inpatients with schizophrenia andother chronic mental illnesses. However, the needsassessments indicated considerable heterogeneity inresident level of Impairment When a validated plan-ning template was applied to assign residents to anappropriate level of care, almost one-quarter wereassigned to independent living with minimal support,one-third to community living with intensive support,and 40 percent to residential or inpatient treatmentThe authors conclude that this program is not able tomeet the varying needs of residents. Despite a commondiagnosis, many can function in more independent set-tings, while others need more treatment and rehabili-tation than they are currently provided.
Keywords: Residential care, schizophrenia, levelof care, planning, mental health.
Schizophrenia Bulletin, 30(1): 123-132,2004.
The mental health reform movement of recent decades inOntario and throughout North America has set out a num-ber of priority goals for system reform, including deliveryof care in the least restrictive setting and greater involve-ment of consumers and families in developing the servicesystem and managing their own care. The reform move-ment has been fueled in part by changing perceptions ofthe course of severe and persistent mental illness, and thecapabilities of individuals suffering from severe condi-tions such as schizophrenia and major mood disorders.These changing perceptions have been accompanied bythe development of new psychopharmacologic interven-tions and emphasis on integration of individuals with
mental disorders into full community living (Pandiani etal. 1996; Jibson and Tandon 1998). While newer modelsof care reflect these goals, a number of older models per-sist. In the area of residential care a body of literature isemerging supporting approaches that emphasize normalhousing, give consumers choice and control, and promotecommunity integration (Srebnik et al. 1995; Parkinson etal. 1999; Fakhoury et al. 2002; Wong and Solomon 2002).Yet more custodial approaches, such as board-and-carehomes where only basic care services are provided, rou-tines are rigid, and staff make most decisions, remain partof the care continuum in many jurisdictions (Randolph etal. 1991; Trainor et al. 1993; Nelson et al. 1997). Thisraises the question of whether there continues to be a rolefor these more custodial/maintenance approaches, andwhere current residents of these programs would best beserved.
In the province of Ontario, a long-standing board-and-care home program called Homes for Special Care(HSC), operated by provincial psychiatric hospitals, isunder review. This program was established in 1964 toprovide a low-support, community-based residential careoption for hospital patients ready for discharge. Theseindividuals, many of whom suffered from schizophrenia,were expected to experience an illness course ofinevitable chronicity and as such, to require no more thancustodial care. However, views on the life course of indi-viduals with psychotic disorders have changed during thelast several decades, in part because of longitudinal stud-ies that have demonstrated improvement and recovery insymptoms, self-care, and social and community function-ing (Harding et al. 1987; McGlashan 1988; Breier et al.1991; Harding and Zahniser 1994; Huber 1997). In thiscontext, the HSC program has been criticized for beingcustodial, doing little to promote resident choice, growth,
Send reprint requests to Janet Durbin, M.Sc., Centre for Addiction andMental Health, 33 Russell Street, Tower 301, Toronto, Ontario M5S2S1; e-mail: [email protected].
123
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Schizophrenia Bulletin, Vol. 30, No. 1, 2004 J. Durbin et al.
and independence (Trainor 1996; Trainor and lives 1999).Yet patient-level information has not been available todescribe the level of impairment of HSC residents andassess whether other approaches to treatment and supportcan more appropriately meet their needs. As a result of aplanning project to evaluate the service needs of provin-cial psychiatric hospital patients, assessments of function-ing and level of care recommendations became availablefor a sample of HSC residents. In this article, we use thesedata to learn more about the current functioning and ser-vice needs of a particularly vulnerable subgroup of HSCresidents, those with schizophrenia spectrum disorders.The goals of this article are as follows:
1. Review evidence about housing approaches forindividuals with mental illness, including those withschizophrenia spectrum disorders.2. Describe current levels of impairment and serviceneeds of a sample of HSC residents with a schizo-phrenia spectrum diagnosis.3. Discuss alternative approaches to providing treat-ment and support for this subgroup based on assess-ment data and current knowledge about evidence-based practices.
Review of Housing Approaches andEvidence
Housing became a major concern in the 1960s with recog-nition that deinstitutionalization was discharging manyindividuals into the community without providing ade-quate housing or support (Lamb 1984). This period saw aproliferation of boarding home programs that providedsafe, secure housing in the community but few opportuni-ties for growth and community integration (Randolph etal. 1991; Trainor et al. 1993). During the 1970s and1980s, the linear residential continuum approach becamepopular, offering varying levels of support to individualsliving in small, homelike settings. However, optimismabout this model dissipated in the face of high costs andclient resistance to repeated uprooting in order to meetchanging levels of need (Ridgway and Zipple 1990;Geller and Fisher 1993).
In keeping with the current emphasis on providingcare in the least restrictive setting, on community integra-tion, and on respect for client preferences, interest hasshifted to models that separate support services and hous-ing components. Support is perceived as portable and fol-lows the client wherever he or she chooses to live. Theclient is a full tenant in regular housing, and eligibility foraccommodation is not affected by service needs (Carling1993; Pyke and Lowe 1996; Parkinson et al. 1999).
While evidence indicates that living in more normal-ized settings with flexible support benefits many individu-als, there is a subgroup whose symptoms and behaviorsmake independent community living inappropriate(Trieman et al. 1998;Wasylenki et al. 2000). For thisgroup, high-support residential treatment facilities (RTFs)are emerging as a more appropriate community-basedalternative to hospitalization. These facilities offerenriched treatment and rehabilitation in small, secure set-tings with skilled staff and a high ratio of staff to patients(Shepherd 1995; Rothbard et al. 1997; Trainor and lives1999). RTFs are intended to provide an alternative toinstitutional care but are not a replacement for more inde-pendent housing options (Fields 1990). This is consistentwith Bachrach's view (1994) that an array of residentialopportunities are needed to respond to varying levels ofneed. A recent review of best practices in housing supportunder mental health reform recommended that systems ofcare offer a range of housing alternatives, including resi-dential treatment, but give priority to community-based,supported housing models (Health Canada 1997).
Evidence from numerous studies reinforces the needfor a range of housing support options for individualswith schizophrenia. A growing body of research on dein-stitutionalization demonstrates that long-term psychiatricinpatients, including many with schizophrenia spectrumdiagnoses, are discharged into various types of housing,including supervised community residences and moreindependent situations. At followup, researchers havefound low rates of rehospitalization (Okin et al. 1995),stability of placement (McGrew et al. 1999), and high lev-els of satisfaction (Leff et al. 1996). A recent review of theeffectiveness of assertive community treatment (ACT)and intensive case management found that these high-sup-port interventions can help very ill individuals sustainindependent living situations and increase communitytenure (Mueser et al. 1998). In the reviewed studies, thepercentage of individuals with schizophrenia spectrumdiagnoses ranged from 30 percent to 84 percent.
Program Description
In the 1960s, psychiatric hospitals in Ontario assumedresponsibility for operating community residences forlong-term inpatients who no longer required active treat-ment but lacked lodging and possessed very limited com-munity living skills. The underlying assumption of theHSC program was that people with serious and persistentmental illnesses never improved or recovered, andrequired only custodial care. Meals, housekeeping, andlaundry services were provided; residents were notinvolved in house decisions; and care was not titrated toneed. On-site supervision was provided by operators who
124
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Needs-Based Planning in Board-and-Care Homes Schizophrenia Bulletin, Vol. 30, No. 1, 2004
received minimal reimbursement and had no special train-ing. A hospital fieldworker was assigned to each HSC res-ident to help with adjustment and management problemswithin the home. Psychiatric consultation was availablebut not routinely accessed.
The HSC program has remained unchanged, despitethe impact of mental health reform on other parts of thecare system. A recent review identified numerous weak-nesses in the model (Trainor 1996) related to its mainte-nance rather than growth orientation, inadequate funding,and isolation from the rest of the community and care sys-tem.
Data Collection and Measures
The Ontario Ministry of Health recently commissioned aseries of needs-based planning projects to identify ser-vices and supports required by current users of provincialpsychiatric hospital services. In each facility, needs dataare obtained on a cross-sectional sample of patients. Aclinical staff member who knows the patient or residentwell completes the assessment based on personal knowl-edge and chart information. Using a standardized assess-ment tool, the most recent version of the Colorado ClientAssessment Record (CCAR) (Ellis et al. 1991), staff rateimpairment across 21 domains related to symptoms, riskbehaviors, and social and community functioning. Aglobal impairment rating assesses overall severity, and aglobal strengths rating assesses overall resources, such asthe patient's economic and skill base, and support fromfamily and friends.
All ratings are scored on an ordinal scale from one tonine (slight to severe problem) and pertain to the preced-ing 3 to 4 weeks. Ratings in the "slight" range indicatethat problems are intermittent or persist at a low level andthat intervention may be required in the future. Ratings inthe "moderate" range indicate that problems persist at amoderate level or become severe on occasion and thatintervention is required. "Severe" end ratings indicatethat problems are subacute but chronic, or acute andsevere. Intervention is required and may include hospital-ization. In a tool requiring clinical judgment, reliability isa concern. Rater consistency was enhanced throughavailability of a manual that provided individualized doc-umentation for each rating domain, outlining its scopeand defining five anchor points along the nine-pointresponse continuum. In addition, all raters (i.e., HSC,inpatient, and outpatient staff) participate in a full-daytraining session to maximize consistent interpretation ofitems and to calibrate ratings. Given the heterogeneity ofstaff completing CCAR assessments, the authors con-ducted an interrater reliability study at one facility toassess whether variation in training and skills influenced
rating consistency. When possible, two raters were askedto independently assess the same patient. Out of 571patients in the assessment sample, 219 cases had 2 rat-ings submitted.1 Intraclass correlations were found toexceed 0.70 for all CCAR domains, regardless of disci-pline or years of experience (Goering et al. 1999). Usinga similar version of the CCAR, Ward et al. (1998)reported moderate to high intraclass correlations thatexceeded 0.50 for 17 out of 18 ratings.
The assessment package also includes a ServiceNeeds Profile in which, for each of a number of treatmentand rehabilitation areas, clinicians rate current serviceneeds (in terms of frequency of contact) and whether theamount of support currently received is less dian needed,more than needed, or appropriate. Clinicians also reportpatient sociodemographic characteristics, primary andsecondary diagnoses, and previous hospitalizations (basedon patient charts). At each facility, the methodology wasreviewed and ethics approval obtained. Because comple-tion of the CCAR did not require a patient interview andconfidentiality was protected in all reporting, patient con-sent was not required.
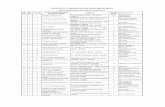
To link needs assessment data with a recom-mended package of services, a planning template wasdeveloped based on best practice evidence and consul-tation with local stakeholders. Figure 1 presents thealgorithm and criteria by which patients were linked toone of five levels of care, based on assessed need. Thelevels are broadly defined as self-management (level1), community support (level 2), intensive communitysupport (level 3), residential treatment (level 4), andinpatient care (level 5), with higher levels providingmore supervision, individualized support, and frequentcontact (table 1). Patient need is based on ratings insix CCAR domains (security/management issues, sui-cide/danger to self, violence/danger to others, globalseverity rating, self-care/basic needs, and globalstrengths rating). Consistent with the goal of helpingpatients achieve desired outcomes in the least restric-tive setting, only those with the most severe ratings(related to security, self- and other harm, and self-care) are assigned to levels 4 and 5 (i.e., inpatient careor residential treatment). Those with lower levels ofimpairment are assigned to independent living situa-tions with varying levels of support. Final placementsconsider patient strengths (resources and support fromfamily and friends), assigning those with more per-sonal resources to a lower level of support.Correlations between the assigned level of care andindependent measures of patient severity and service
1 Raters in the reliability study were not randomly selected but, withsuch a large sample, represent a wide range of staff skills and experience.
125
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Schizophrenia Bulletin, Vol. 30, No. 1, 2004 J. Durbin et al.
Figure 1. Placement algorithm linking CCAR ratings of need to level of care.
L*f«Dd:
LcvcfcrfCuv
i d f i i m u w t out KtttfeaMH LatmtvtCM rcaldtaibkl trataoit hptr t r i
Rittat catcf*rksi Al6tma)mM except r m n x u R » • • ! ! •
Low m Dooc*mik] prooWfnMod - modcr̂ e problemHi m •cvcre to extreme problem
HI - biyfa 10 vny WgkMod * inodentvLow- nmetD tow
Note.—CARR = Colorado Client Assessment Record.
need support the validity of the template for placingthose who require more services into a higher level ofcare (Durbin et al. 2001).
Sample Description
Data were collected from three psychiatric hospitalslocated in the southwestern, central western, and easternregions of the province. At each facility, a sample wasdrawn of all inpatients on a specified census day and arandom selection of outpatients and HSC residents, strati-fied by program. A minimum sample of 30 per programwas sought where possible. Because of variation in pro-gram size, overall, 15 percent of outpatients and 20 per-cent of HSC residents were sampled. Assessments werereturned for 95 percent HSC residents with a schizophre-nia spectrum diagnosis formed the study group (88 out of
115 assessed HSC residents), and outpatients with schizo-phrenia not living in HSCs (277 out of the 603 assessedoutpatients) formed the comparison group. These outpa-tients were enrolled in a variety of facility services,including rehabilitation programs, community treatmentteams, and specialty clinics but excluding forensic pro-grams.
The two groups are described in table 2. Over one-quarter of the HSC residents are 65 years of age orolder. Most have never married (83%), and their educa-tion is limited. More than 40 percent have a seconddiagnosis, and 98 percent are taking psychotropic med-ications. Thirty-six percent have been hospitalized atleast once in the past 2 years. In comparison, the outpa-tients are younger, are more likely to be married or liv-ing with family, and have more education. Yet the HSCresidents are less likely to have been recently hospital-ized, suggesting a more stable group.
126
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Needs-Based Planning in Board-and-Care Homes Schizophrenia Bulletin, Vol. 30, No. 1, 2004
Table 1. Level of care continuum
Level of care Description
Individual is capable of self-management, resides in the community, accesses familyphysician or psychiatric services periodically, and may intermittently use communityservices and supports.
Individual resides in the community, needs assistance approximately weekly to iden-tify needs and access community services and supports, and can obtain psychiatriccare from an outpatient clinic or private office
Individual lives in the community, needs intensive assistance (i.e., up to daily visitsand 24-hour availability of support) to obtain needed mental health treatment andrehabilitation services and access other community services.
Individual needs 24-hour support and access to treatment and rehabilitation servicesin a securable setting and may access some services and supports in the community.
Individual needs 24-hour care provided by a multidisciplinary team of highly trainedexperts in a securable setting with the capacity to do comprehensive assessmentand treatment.
Note.—Services and supports available to all levels: acute Inpatient care, crisis services, psychiatric services, consumer and family Initia-tives, primary medical care, housing support, and rehabilitation services (e.g., income support, vocational and educational support,leisure and recreational activities).
1: self-management
2: community support
3: intensive community support
4: residential treatment
5: inpatient care
Table 2. Demographic and Illness characteristics
CharacteristicHSC sample
(n = 88)1
28.9
26.1
82.8
0.0
53.7
36.4
97.7
40.9
Outpatient sample(n = 277)1
38.7
7.2
67.6
26.1
39.3
54.6
99.3
48.7
% female
% > 65 yrs o ld "
% never married"
% living with family/relative/spouse"
% whose highest level of education was primary school or less*
% hospitalized at least once in last 2 yrs**
% prescribed psychotropic medication
% with more than 1 diagnosis
Note.—HSC = Homes for Special Care.1 Sample sizes per characteristic vary slightly because of missing responses.
Results of x2test: HSC vs. outpatient sample: * p< 0.05; " p< 0.001
Assessment Results
Mean CCAR ratings are reported in table 3. Regardingclinical functioning, ratings suggest that HSC residentscontinue to experience moderate impairment in most symp-tom areas. Risk behaviors are slight in most domains, withthe exception of security management, where ratersassessed a moderate need for supervision related to medica-tion compliance and behavior management Impairment insocial and community functioning ranges from mild tomoderate but is most pronounced in the area of self-careand meeting basic needs. Residents were rated as having
few family problems, but this likely reflects lack of familycontact rather than positive relations. Regarding strengths,residents are severely impoverished, lacking economicresources, job skills, and personal support from family andfriends. Compared with the outpatient group, this HSCcohort is significantly more impaired in self-care manage-ment and has more safety management problems and fewerstrengths. While overall levels of impairment are slight tomoderate, there is considerable variation among residents.
Table 4 summarizes clinician ratings of patient needfor specific services. Regarding treatment, clinicians esti-mate a high level of need among HSC residents for med-
127
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Schizophrenia Bulletin, Vol. 30, No. 1, 2004 J. Durbin et al.
ication monitoring and assessment/diagnosis, most of these are receiving less than needed. Regarding rehabilita-which is being met. However, of the 62 percent of resi- tion, the need for support with activities of daily livingdents estimated to need psychotherapy/counseling, half (ADL), social/recreational activities, housing support, andare not receiving the required care. Few HSC residents are income assistance is estimated to be very high, with mostestimated to need substance abuse treatment, but half of of this need rated as being met. Estimated need for voca-
Table 3. Impairment among HSC residents with schizophrenia spectrum diagnoses
Impairment Rating1:CCAR Domain (Mean, SD)
CCAR Domain None-slight (1-3.49) Moderate (3.5-6.49) Severe (6.5-9.0)
Symptoms Depression (3.4, 2.0) Emotional withdrawal (4.0, 2.1)Hyper affect (2.9, 2.3) Anxiety (3.8, 2.3)Danger to self (2.0,1.8) Attention problems (4.0, 2.3)
Thought processes (4.4, 2.2)Cognitive problems (4.4, 2.2)Resistiveness (4.5, 2.2)
Risk behaviors Substance abuse (1.8, 1.7 ) Security management (4.6, 2.5)"Antisocial (2.6, 2.0)Legal (1.3, 1.3)Danger to others (2.0, 1.9)Aggressiveness (3.1,2.6)
Functioning Medical/physical (2.6,2.2) Self-care/basic needs (5.9,2.3)**Family context (2.2, 2.2) Interpersonal (4.3, 2.4)+Family relationships (2.3, 2.3)+ Role performance (4.6, 3.2)
Global ratings Severity (5.1, 1.8) Strengths (6.6, 1.7)*
Note.—CCAR = Colorado Client Assessment Record; HSC = Homes for Special Care; SD = standard deviation.1 Ratings range from 1 to 9, with higher ratings indicating more Impairment.Results of x2 test: HSC versus outpatient sample:HSC more impaired than outpatient sample: * p < 0.01 ** p < 0.001
HSC less Impaired than outpatient sample: + p < 0.01
Table 4. Service need among HSC residents and outpatients with schizophrenia spectrum diagnoses
Service area
TreatmentMedication managementAssessment/diagnosisPsychotherapy/counselingSubstance abuse programming
RehabilitationSelf-care/ADLVocationalEducationalSocial/recreationalHousing supportIncome/financial assistance
HSC
99876220
964433969895
> Needing Service1
Outpatients
9898**77**23
76"533592
7 1 "79"
%Wtth
HSC
0155053
369651415
Unmet Need for Service2
Outpatients
9**7
2 1 "59
29**5157
57"18"23*
Note.—ADL - activities of daily living; HSC = Homes for Special Care.1 Need Is a dichotomous variable (none vs. any); denominator» total sample.2 Denominator = individuals who need service.
Results of x2 test: HSC residents vs. outpatients: * p < 0.01; ** p < 0.001
128
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Needs-Based Planning in Board-and-Care Homes Schizophrenia Bulletin, Vol. 30, No. 1, 2004
tional and educational support is lower, but about two-thirds of residents are not adequately supported in theseareas. Compared with the outpatients, fewer HSC resi-dents are perceived to need treatment (i.e., assessment andpsychotherapy), but rates of unmet need are higher. Thisfinding is consistent with the assertion that HSC residentshave limited access to psychiatric care and may reflect theprogram's emphasis on custodial, not growth-oriented,services (Trainor 1996). Regarding rehabilitation, moreHSC residents than outpatients are rated as needing sup-port for self-care/ADL, maintaining housing, and securingincome. However, more outpatients are rated as having anunmet need for these services. Both groups lack voca-tional support. Many outpatients also lack adequatesocial/recreational opportunities.
Table 5 describes the recommended level of care basedon the planning template. Despite setting a high thresholdfor assignment to more restrictive levels of care, about 40percent of HSC residents were assigned to residential orinpatient treatment. This is not surprising, given their lim-ited skills in self-care, few strengths, and significant needfor security management. These residents require moresupport than is currently provided. At the same time, overhalf of HSC residents were assigned to independent livingsituations, with one-third perceived as requiring intensivecommunity support and one-quarter requiring up to weeklyassistance to identify needs and access services. These indi-viduals have the potential to live more independently,despite current placement in congregate-care situationswith limited opportunities for growth. While a greater por-tion of the outpatients were assigned to independent set-tings (76% versus 57%), there is much more overlap insupport needs among these two groups than current percep-tions of HSC residents would have predicted.
Discussion
A series of provincial planning projects have providedvaluable information about the clinical and functional sta-
Table 5. Level of care assignment
Level of care*
1: self-management
2: community support
3: intensive communitysupport
4: residential treatment
5: inpatient care"
HSC residents(n = 86),%
4.7
19.8
32.6
39.5
3.5
Outpatients(n = 267), %
9.0
27.3
40.1
22.5
1.1
' X 2 -13.2, £#=4, p = 0.01.
" Unstable estimates because of small cell size.
tus of a sample of HSC residents. These individuals wereplaced in board-and-care programs with an expectation ofan unremitting illness course and continued low function-ing. The CCAR needs assessments show that, as a group,the individuals remain moderately troubled by psychiatricsymptomatology, have difficulty meeting basic needs,require close supervision related to behavior and medica-tion management, and have few personal resources. Otherstudies of residents in intermediate care facilities reportsimilar profiles (Segal and Kotler 1993; Anderson andLyons 2001). Yet, consistent with the findings of longitu-dinal research (McGlashan 1988; Harding and Zahniser1994), within this group there is considerable heterogene-ity. When a planning template based on best practices wasapplied to assign residents to an appropriate level of care,almost one-quarter were assessed as able to live indepen-dently in the community with minimal support, one-thirdwere assigned to community living with intensive sup-port, and about 42 percent were assessed as requiringhigh-support residential or inpatient treatment.
These findings underscore the weaknesses inherent incongregate residential programs that have a custodial ori-entation and treat all residents more or less uniformly. TheHSC program is ill-equipped to respond to the diversity ofresident needs evident in these assessments. Without moreresources and highly trained on-site staff, the program isnot positioned to provide intensive treatment and rehabili-tation to those who are experiencing extreme difficulty.Without an emphasis on integration and linkage withcommunity resources such as case management, crisisintervention, psychiatric treatment, and self-help, the pro-gram is not positioned to promote more independence andmeet die needs of the higher functioning subgroup. As aresult, few residents are receiving the support tiiey need toachieve a better quality of life.
The incongruence between support needed and sup-port received is also reflected in the Service NeedsProfile, where clinicians identified high levels of unmetneed for psychotherapy/counseling, substance abusetreatment, and vocational and educational support.Minimal unmet need was identified in areas of self-care,social recreation, and income assistance. This may bemisleading, as clinicians were asked to rate amount ofsupport rather than appropriateness or quality of support.We know that the HSC program has little capacity tocustomize support to individual need so that, for exam-ple, residents are provided with meals even if interestedin and capable of cooking for themselves. Similarly, res-idents lack opportunities to develop money managementskills, as almost all are under the Public Trustee andreceive only a small comfort allowance (Trainor 1996;Trainor and lives 1999).
Given past undue pessimism regarding the prognosisof individuals with schizophrenia, one wonders about the
129
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Schizophrenia Bulletin, Vol. 30, No. 1, 2004 J. Durbin et al.
potential iatrogenic effect of long-term residence in a cus-todial setting. Residents have limited self-care and inter-personal skills, and almost no family involvement orfriendship support. Most have never married. In theabsence of longitudinal studies of comparison groupsexposed to different interventions, we cannot assesswhether the constraints of living in a restricted settinghave stunted social and skill development. We canobserve whether level of functioning improves for indi-viduals who are transferred to more independent set-tings. However, many residents are older and havealready missed opportunities to create more normalizedlives.
Under mental health reform, treatment close to homeis a priority. Unfortunately, many HSC residents wereseparated from home communities and family when firstadmitted to the psychiatric hospital, a separation that con-tinued when they were discharged to the HSC program.While our data show that many residents suffer fromimpoverished social networks, reconnection with familymay not be possible after so many years. Still, if effortsare made to move residents into more independent livingsituations, their preferences related to locating closer tofamily need to be explored.
Use of the CCAR and planning template provided astandardized method for assessing resident needs andidentifying appropriate service responses that can benefitboth system planning and individual placement (Bachrach1996). In Ontario, results from planning projects are pro-viding each region with similar evidence on which to basenew service development. Common themes include theneed for more intensive community support programssuch as ACT and for initiatives (mental health and generalcommunity) to help consumers develop richer social livesand obtain real jobs. A future repeated application of themethodology could help to assess system progress inthese important areas.
Several study limitations need to be noted. Thepatient sample was drawn from three psychiatric hospitalsand may not be broadly representative of HSC residentsand outpatients with schizophrenia. In addition, HSChomes vary considerably in size and quality of support,characteristics that could not be incorporated into thesampling strategy. Regarding study measures, diagnosticclassifications were based on information recorded inpatient charts rather than current psychiatric assessmentsor structured interviews. The Service Needs Profile is nota standardized tool, and ratings were based on subjectiveimpressions of service need rather than objective criteria.While we have found considerable consistency across set-tings in areas where unmet need was greatest, explicit rat-ing criteria would help to increase the reliability of ratingsand clarify interpretation.
The level of care continuum used in this projectexcludes low-intensity residential support as an option,assuming that individuals who do not require intensiveresidential treatment can manage independently in thecommunity if needed support (including wraparoundservices such as ACT) is available. While we haveassessed the concurrent validity of the level of care tem-plate, we recognize that prospective studies are neededto evaluate the appropriateness of the recommendedlevel of care, compared with other options. It is possiblethat some individuals need a type of support that fallsbetween levels 3 and 4—that is, a low-intensity super-vised setting combined with community-based treatmentand rehabilitation.
Conclusion
Clinician ratings of a sample of HSC residents with schizo-phrenia spectrum diagnoses demonstrate a range of func-tional levels within a group previously felt to have anunremitting illness and poor prognosis. The current HSCprogram, a custodial model of care with minimal flexibility,is not positioned to respond to this diversity, yet many indi-viduals have lived in HSC programs for decades. A bestpractices planning template has suggested alternativeapproaches for meeting the housing, treatment, and supportneeds of these individuals. Some require a higher level ofresidential support Others could live more independentlyin the community if appropriate services and support wereavailable. While this study demonstrates the inadequacy ofboard-and-care homes for meeting resident needs, researchmust continue on the effective housing and support combi-nations for people with different levels of need.
References
Anderson, R., and Lyons, J. Needs-based planning forpersons with serious mental illness residing in intermedi-ate care facilities. Journal of Behavioral Health ServicesResearch, 28(1): 104-110, 2001.
Bachrach, L. Residential planning: Concepts and themes.Hospital and Community Psychiatry, 45:202-203, 1994.
Bachrach, L. The state of the state mental hospital in1996. Psychiatric Services, 47(10):1071-1078, 1996.
Breier, A.; Schreiber, J.L.; Dyer, J.; and Pickar, D.National Institute of Mental Health longitudinal study ofchronic schizophrenia. Archives of General Psychiatry,48:239-246,1991.
Carling, P.J. Housing and supports for persons with men-tal illness: Emerging approaches to research and practice.Hospital and Community Psychiatry, 44:439-449, 1993.
130
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Needs-Based Planning in Board-and-Care Homes Schizophrenia Bulletin, Vol. 30, No. 1, 2004
Durbin, J.; Cochrane, J.; Goering, P.; and Macfarlane, D.Needs-based planning: Evaluation of a level of care plan-ning model. Journal of Behavioral Health ServicesResearch, 28:67-80, 2001.
Ellis, R.; Wackwitz, J.; and Foster, M. Uses of an empiri-cally derived client typology based on level of function-ing: Twelve years of the CCAR. Journal of Mental HealthAdministration, 18:88-100, 1991.
Fakhoury, W.K.H.; Murray, A.; Shepherd, G.; andPriebe, S. Research in supported housing. SocialPsychiatry and Psychiatric Epidemiology, 37:301-315,2002.
Fields, S. The relationship between residential treatmentand supported housing in a community system of ser-vices. Psychosocial Rehabilitation Journal, 13:105—113,1990.
Geller, J.L., and Fisher, W.H. The linear continuum oftransitional residences: Debunking the myth. AmericanJournal of Psychiatry, 150(7): 1070-1076, 1993.
Goering, P.; Macfarlane, D.; Cochrane, J.; Durbin, J.; andPalmer, H. Comprehensive Assessment Project: HamiltonPsychiatric Hospital Final Report. Toronto, Canada:Clarke Consulting Group, 1999.
Harding, CM., and Zahniser, J.H. Empirical correction ofseven myths about schizophrenia with implications fortreatment. Ada Psychiatrica Scandinavica, 90:140-146,1994.
Harding, CM.; Zubin, J.; and Strauss, J.S. The Vermontlongitudinal study of persons with severe mental illness:II. Long-term outcome of subjects who retrospectivelymet DSM—III criteria for schizophrenia. American Journalof Psychiatry, 144:727-735, 1987.
Health Canada. Review of Best Practices in MentalHealth Reform. Ottawa, Canada: Ministry of Supply andServices Canada, 1997.
Huber, G. The heterogeneous course of schizophrenia.Schizophrenia Research, 28:177-185, 1997.
Jibson, M., and Tandon, R. New atypical antipsychoticmedications. Journal of Psychiatric Research,32:215-228, 1998.
Lamb, H.R. Deinstitutionalization and the homeless men-tally ill. Hospital and Community Psychiatry,35(9):899-9O7, 1984.
Lehman, A.F.; Slaughter, J.G.; and Myers, C.P. Quality oflife in alternative residential settings. PsychiatricQuarterly, 62(l):35-49, 1991.
Leff, J.; Dayson, D.; Gooch, C ; Thornicroft, G.; andWills, W. Quality of life of long-stay patients dischargedfrom two psychiatric institutions. Psychiatric Services,47:62-67, 1996.
McGlashan, T. A selective review of recent NorthAmerican long-term follow-up studies of schizophrenia.Schizophrenia Bulletin, 14(4):515-542, 1988.
McGrew, J.H.; Wright, E.R.; Pescosolido, B.A.; andMcDonel, E.C. The closing of Central State Hospital:Long-term outcomes for persons with severe mental ill-ness. Journal of Behavioral Health Services Research,26:246-261, 1999.
Mueser, K.T.; Bond, G.R.; Drake, R.E.; and Resnick, S.Models of community care for severe mental illness: Areview of research on case management. SchizophreniaBulletin, 24(l):37-74, 1998.
Nelson, G.; Hall, G.B.; and Walsh-Bowers, R. A compara-tive evaluation of supportive apartments, group homes,and board-and-care homes for psychiatric consumer/sur-vivors. Journal of Community Psychology, 25:167-188,1997.
Okin, R.L.; Borus, J.F.; Baer, L.; and Jones, A.L. Long-term outcome of state hospital patients discharged intostructured community residential settings. PsychiatricServices, 46:73-78, 1995.
Pandiani, J.; Murtaugh, M.; and Pierce, J. The mentalhealth care reform debate: A content analysis of positionpapers. Journal of Mental Health Administration,23(2):217-225, 1996.
Parkinson, S.; Nelson, G.; and Horgan, S. From housingto homes: A review of the literature on housingapproaches for psychiatric consumer/survivors. CanadianJournal of Community Mental Health, 18(1):145-164,1999.
Pyke, J., and Lowe, J. Supporting people, not structures:Changes in the provision of housing support. PsychiatricRehabilitation Journal 19:5-12, 1996.
Randolph, F ; Ridgway, P.; and Carling, P. Residentialprograms for persons with severe mental illness:A nation-wide survey of state-affiliated agencies.Hospital and Community Psychiatry, 42(11):1111-1120, 1991.
Ridgway, P., and Zipple, A. The paradigm shift in residen-tial services: From the linear continuum to supportedhousing approaches. Psychosocial Rehabilitation Journal,13:11-31, 1990. Special issue: Supported housing: Newapproaches to residential services.
Rothbard, A.; Richman, E.; and Hadley, T."Unbundling" of state hospital services in the commu-nity: The Philadelphia state hospital story.Administration and Policy in Mental Health,24(5):391-398, 1997.
Segal, S.P., and Kotler, P.L. Sheltered care residence: Tenyear personal outcomes. American Journal ofOrthopsychiatry, 63:80-91, 1993.
131
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from
Schizophrenia Bulletin, Vol. 30, No. 1, 2004 J. Durbin et al.
Shepherd, G. The "ward-in-a-house": Residential care forthe severely disabled. Community Mental Health Journal,31(l):53-69, 1995.
Srebnik, D.; Livingston, J.; Gordon, L.; and King, D.Housing choice and community success for individualswith serious and persistent mental illness. CommunityMental Health Journal, 31(2):139-151, 1995.
Trainor, J. Homes for Special Care Review. Toronto,Canada: Ontario Ministry of Health, 1996.
Trainor, J., and lives, P. Residential Treatment Facilities:A Review With Development Recommendations. Toronto,Canada: Clarke Consulting Group, 1999.
Trainor, J.; Morrell-Bellai, T.L.; Ballantyne, R.; andBoydell, K. Housing for people with mental illnesses: Acomparison of models and an examination of the growthof alternative housing in Canada. Canadian Journal ofPsychiatry, 38:494-501, 1993.
Trieman, N.; Hughes, J.; and Leff, J. The TAPS project42: The last to leave hospital—a profile of residual long-stay populations and plans for their resettlement. AdaPsychiatrica Scandinavica, 98:354-359, 1998.
Ward, J.; Dow, M.; Penner, K.; Saunders, T.; and Halls, S.A Manual for Using the Florida Version of the FunctionalAssessment Rating Scale. Tampa, FL: Florida MentalHealth Institute, 1998.
Wasylenki, D.; Goering, P.; Cochrane, J.; Durbin, J.; andPrendergast, P. Tertiary mental health services: I. Key
concepts. Canadian Journal of Psychiatry, 45:179-184,2000.
Wong, Y.I., and Solomon, PL. Community integration ofpersons with psychiatric disabilities in supportive inde-pendent housing: A conceptual model and methodologicalconsiderations. Mental Health Services Research,4(1): 13-28, 2002.
The Authors
Janet Durbin, M.Sc, is Assistant Professor, Department ofPsychiatry, University of Toronto, Toronto, Ontario; andScientist, Health Systems Research and Consulting Unit,Centre for Addiction and Mental Health, Toronto, Ontario.Paula Goering, Ph.D., is Professor, Department ofPsychiatry, University of Toronto; and Director, HealthSystems Research and Consulting Unit, Centre forAddiction and Mental Health. Jeanette Cochrane, B.A., isdeceased. Formerly Lecturer, Department of Psychiatry,University of Toronto; and Consultant, Health SystemsResearch and Consulting Unit, Centre for Addiction andMental Health. Dianne Macfarlane, M.A., is AssistantProfessor, Department of Psychiatry, University of Toronto;and Senior Consultant, Health Systems Research andConsulting Unit, Centre for Addiction and Mental Health.Tess Sheldon, M.Sc, entered law school. Formerly ProjectCoordinator, Health Systems Research and Consulting Unit,Centre for Addiction and Mental Health.
132
by guest on May 22, 2011
schizophreniabulletin.oxfordjournals.orgD
ownloaded from