Gastroenteritis - Bacterial (1 of 15) - NET
-
Upload
khangminh22 -
Category
Documents
-
view
0 -
download
0
Transcript of Gastroenteritis - Bacterial (1 of 15) - NET
B126
Gastroenteritis - Bacterial (1 of 15)
Yes
No
1Patient presents w/ signs & symptoms suggestive of acute gastroenteritis
2DIAGNOSIS
Do the history, physical exam & lab results support bacterial
infection?
3ASSESS THE SEVERITY
OF DEHYDRATION
ALTERNATIVE DIAGNOSIS• Consider viral or parasitic
gastroenteritis- Please see
Gastroenteritis - Viral or Gastroenteritis - Parasitic disease management chart for further information
TOXININDUCED FOOD POISONING
TRAVELER’S DIARRHEA
A Rehydrate & maintain hydration
A Rehydrate & maintain hydration
B Patient educationC Empiric antibiotics
TREATMENT See page 5
TREATMENT See page 6
4MANAGEMENT DECISION
BLOODY DIARRHEA
WATERY DIARRHEA
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B127
Gastroenteritis - Bacterial (2 of 15)
1 BACTERIAL GASTROENTERITIS
• Diarrhea: Change in normal bowel movements characterized by increase in frequency, water content or volume of stools or w/ bloody stools- Usual stool output is 10 g/kg/day
• Acute diarrhea: Diarrhea lasting ≤14 days duration- Chronic diarrhea is a diarrhea lasting >14 days
• Infectious diarrhea: Diarrhea of infectious origin & is usually associated w/ symptoms of nausea & vomiting (N/V) & abdominal cramps
2 DIAGNOSIS
• Initial clinical evaluation of the patient w/ acute diarrhea should focus on assessment of the severity of the illness, the need for rehydration & the identifi cation of likely causes on the basis of history & clinical fi ndings
• A careful clinical evaluation is needed in order to provide a cost-eff ective evidence-based approach to initial diagnostic tests & treatment
Clinical HistorySymptoms• Determine abrupt or gradual onset, duration & progression of symptoms• Onset & frequency of bowel movement • Amount of stool excreted• If dysenteric symptoms are present (eg fever, tenesmus, blood/pus in stool)Associated Symptoms• Frequency & intensity of N/V, abdominal pain, cramps, myalgia, headache, altered sensorium Symptoms of Volume Depletion• � irst• Tachycardia• Orthostasis• Decreased urination• Decrease in skin turgor• LethargyEpidemiological Risk Factors• Travel to developing/underdeveloped areas• Daycare attendance• Ingestion of unsafe foods (eg unpasteurized dairy products, undercooked meats, seafood)• Swimming/drinking untreated fresh water• Poor personal & public hygiene (eg seldom practice of handwashing) • Visit to farm or contact w/ pets w/ diarrhea• Knowledge of other ill persons• Recent or regular medications (eg antibiotics)• Underlying medical conditions (eg AIDS, immunosuppressants)Physical Exam• Vital Signs
- Orthostatic pulse, blood pressure changes, rate of breathing, presence of fever • Other signs of volume depletion
- Dry mucous membranes, decrease in skin turgor• Abdominal tenderness• Altered sensorium• Accurate body weight to estimate fl uid loss• Other fi ndings may include excessive irritability, cyanosis, petechial rash Lab Tests• � e majority of patients presenting w/ acute gastroenteritis do not require laboratory tests• Consider CBC, blood culture, fecalysis, stool culture & sensitivity, electrolytes, BUN, creatinine & bicarbonate
in patients w/ evidence of systemic illness, fever, bloody stools & moderate to severe dehydration • If considering to give IV rehydration, electrolytes, glucose & creatinine should be ordered • Further stool studies are indicated when patient has a history of traveling abroad, or diarrhea that does not
improve within 7 days or that occurred in a gastroenteritis outbreak
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B128
Gastroenteritis - Bacterial (3 of 15)
3 ASSESSMENT OF THE SEVERITY OF DEHYDRATION
Goals• To provide a starting point for treatment• To segregate which patients can safely be sent home for therapy, which ones should remain for observation
during therapy & which ones immediately need intensive therapy- Consider admitting patient to the hospital if w/ severe dehydration, failed rehydration, serious alternative
diagnoses, or concerns regarding caregiver’s ability to administer rehydration therapy or to identify signifi cant symptoms requiring a return visit
Dehydration AssessmentMinimal or No Dehydration• Consists of <3% loss of body weight (<5% in infants)• Normal heart rate (HR), respiratory rate (RR) & pulse volume• Normal eyes w/ presence of tears, moist mucous membranes• Normal capillary refi ll• Normal to decreased urine output• Patient is well & alertMild to Moderate Dehydration• Consists of 6% loss of body weight (5-10% in infants)• Normal to increased heart rate, respiratory rate• Normal to decreased pulse volume• Slightly sunken eyes w/ decreased tears, sticky mucous membranes• Delayed capillary refi ll• Decreased urine output• Patient may appear normal, listless or fatiguedSevere Dehydration• Consists of >9% loss of body weight (>10% in infants)• Tachycardia w/ bradycardia especially in severe cases, deep respirations• � ready to absent pulse• Deeply sunken eyes w/ absence of tears, parched mucous membranes• Poor capillary refi ll• Minimal urine output• Patient may appear lethargic to comatose
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B129
Gastroenteritis - Bacterial (4 of 15)
4 MANAGEMENT DECISION
• Management of acute diarrhea may be decided upon the history & presentationToxin-Induced Food Poisoning• Should be suspected in those w/ vomiting as the major presenting symptomBacterial Toxin-Induced Food Poisoning• Incubation period varies depending on causative agent• Diarrhea may follow vomiting & is usually not so severe• Abdominal pain may also be present & is usually colicky in nature• Most patients are afebrile & not severely dehydrated unless vomiting or diarrhea is intenseTraveler’s Diarrhea• Usually considered in a person who normally resides in an industrialized region & who travels to developing/
underdeveloped countries • May also refer to illness that occurs within 7-10 days after returning home• Patient often feels weak & w/ orthostatic symptomsEtiology • Causes of acute traveler’s diarrhea will vary from one geographical area to another• Enterotoxigenic E coli is one of the most frequently identifi ed organisms• Campylobacter infections seem to predominate as the cause of traveler’s diarrhea in North Africa & Southeast
Asia• Other common bacterial causes:
- Enteroaggregative E coli (EAEC), Salmonella, Shigella sp, Campylobacter jejuniMain Presentation: Watery Diarrhea• Semi-formed to loose-watery stools without the presence of blood• Often clinical presentation of enterotoxin-induced diarrhea• Cholera
- Cholera is highly suggested by severe profuse watery diarrhea & dehydration- Other clinical features: Very abrupt onset of acute diarrhea w/ rapid progression to severe dehydration, the
presence of muscle cramps but no fever or abdominal pain- Stools are usually greenish-yellow, clear, watery w/ little food residue- Dark-fi eld microscopy (DFM) & stool culture should be done in all cases- Microscopic exam of stool may also reveal shooting bacteria, but not WBC or RBC- If cholera is confi rmed in nonendemic areas, it should be reported to health authorities - Any case of watery diarrhea in endemic areas during outbreaks or seasonal epidemics should be treated as
cholera & stool cultures should be done in all cases to confi rmEtiology• Severe dehydration w/ severe watery diarrhea is most likely caused by Vibrio cholerae subgroup O1• Vibrio O139, other non-O1 vibrios & occasionally Vibrio parahaemolyticus, Aeromonas sp & enteropathogenic
Escherichia coli can cause a similar clinical picture (though diarrhea by these organisms usually causes milder forms of diarrheal illness)
Main Presentation: Bloody Diarrhea• Bloody diarrhea is considered if macroscopic exam of stools contains blood • Patients often have fever that may last >2 days & may be high (>38.5°C)• May initially suff er w/ watery diarrhea that rapidly changes to bloody diarrhea & dysentery• Mild dehydration • RBC & WBC are found on microscopic exam of the stools• Dysentery
- Suggested by frequent passage (10-30x/day) of small-volume stools that consist of blood, mucus & pus- Patient usually suff ers abdominal cramps & tenesmus
Etiology• Shigella sp & Campylobacter jejuni
- Shigella dysenteriae & Shigella fl exneri may cause a more severe disease w/ high fever- Shigella boydii & Shigella sonnei cause a milder disease
• Salmonella enteritidis, Yersinia enterocolitica, C diffi cile, Balantidium coli, Plesiomonas, enterohemorrhagic E coli (EHEC) & enteroinvasive E coli (EIEC) can produce bloody diarrhea
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B130
Gastroenteritis - Bacterial (5 of 15)
Yes No
Yes
No
PATIENT W/ MAIN PRESENTATION OF WATERY DIARRHEA
Severe dehydration?
Improvement?
A Rehydrate & maintain hydrationB Patient education
A Maintain hydrationB Patient education
5DIAGNOSTIC TESTS
• Stool exam• Stool microscopy (DFM)• Stool culture/sensitivity
NO FURTHER TREATMENT
STOOL EXAM CULTURE & SENSITIVITY
F Antibiotics• Consider if
pathogen identifi ed
D Empiric antibiotics for cholera• While waiting for
sensitivity results
5 DIAGNOSTIC TESTS
• Stool Exam: Stools typical of cholera are typically greenish-yellow, clear, watery & w/ little food residue (rice-watery stools)
• Stool Microscopy: - May reveal bacteria w/ darting motility- No WBC or RBC
• DFM & Stool Culture/Sensitivity: Should be performed in both non-endemic & endemic areas
D Empiric antibiotics for cholera• If typical cholera
symptoms in ongoing epidemic
No
Is stool
microscopy suggestive of
cholera?
Yes
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B131
Gastroenteritis - Bacterial (6 of 15)
No
No
No
Yes
Yes
Yes
PATIENT W/ MAIN PRESENTATION OF BLOODY DIARRHEA
Does stool exam reveal protozoal cysts,
trophozoites &/or other parasites?
Is entero-hemorrhagic E coli
(EHEC) suggested by stool exam?
STOOL EXAM CULTURE & SENSITIVITY
AVOID ANTIMOTILITY DRUGS & ANTIBIOTICS
A Maintain hydrationB Patient educationE Empiric antibiotics
• If available, follow local sensitivity patterns & treat for Shigella sp
Improvement in 3-5 days?
NO FURTHER TREATMENT
F Pathogen-specifi c treatment of bacterial diarrhea• If culture & sensitivity is known, modify antibiotic
regimen accordingly• Repeat stool exam for culture & parasitic investigation
MANAGEMENTPlease see
Gastroenteritis - Parasitic disease
management chart for further information
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B132
Gastroenteritis - Bacterial (7 of 15)
Not all products are available or approved for above use in all countries.Specifi c prescribing information may be found in the latest MIMS.
A REHYDRATE & MAINTAIN HYDRATION• Dehydration is the primary cause of morbidity & mortality; thus, treatment goals include prevention of
dehydration, treatment of dehydration when present, & reduction of the severity & duration of symptoms Principles of Treatment • ORT encompasses 2 phases of treatment:
- Rehydration phase: Electrolytes & water are administered as ORS to replenish fl uid losses- Should be performed rapidly within 3-4 hours
- Maintenance phase: Restoration of ongoing fl uid & electrolyte losses, & adequate dietary intake • Age-appropriate diet (including solids) for rapid realimentation is recommended once adequate degree of
hydration is attained • Breastfeeding should be continued especially for breastfed patients• Changes in formula milk or avoidance of milk-based products is not necessary Oral Rehydration Solutions (ORS) • � e formula recommended by the World Health Organization (WHO)
- Concentration of 75 mEq/L sodium, 75 mmol/L glucose w/ total osmolarity of 245 mOsm/L, or ½ teaspoon of salt & 6 teaspoons of sugar in 1 L of water
- Lower osmolarity that is proportionally reduced sodium & glucose concentrations - � e formulation has been shown to reduce vomiting & the need for IV fl uids
• � e WHO-recommended amount to be given based on weight & age are as follows:
Weight Age Amount (within the fi rst 4 hours)
<5 kg (11 lb) <4 months 200400 mL5-7.9 kg (11 lb -17 lb, 7 oz) 4-11 months 200400 mL
8-10.9 kg (17 lb, 10 oz - 24 lb) 12-23 months 600800 mL11-15.9 kg (24 lb, 4 oz - 35 lb) 2-4 years 8001200 mL
16-29.9 kg (35 lb, 4 oz - 65 lb, 15 oz) 5-14 years 12002200 mL30 kg (66 lb, 2 oz) or more ≥15 years 22004000 mL
• First-line treatment for patients w/ acute diarrhea accompanied by mild-moderate dehydration • May also be considered in mild-moderately dehydrated patients w/ vomiting or severe diarrhea • Severe vomiting, abdominal ileus & in state of hemodynamic shock are contraindications to ORSIV Fluids or Nasogastric (NG) ORS• Given for 4-6 hours or until adequate hydration is achieved• IV fl uids are recommended in the following patients:
- Severely dehydrated - In whom oral hydration has failed due to severe vomiting- Patients in shock or altered mental status- Patients w/ intestinal ileus or intestinal obstruction
• Nasogastric ORS may be given to moderately dehydrated patients who cannot tolerate oral administration of ORS & to children who are too weak & refuse to drink that may cause insuffi cient hydration if only by oral intake
• NG feeding allows continuous ORS administration at a slow & steady amount• Rehydrated state should be maintained by continuous replacement of lossesDietary � erapy• Depends on age & diet history• Breastfed patients should continue nursing on demand while formula-fed patients must continue their usual
full-strength milk- Based on several trials, feedings w/ diluted formula is associated w/ protracted symptoms & delayed nutritional
recovery• Lactose-free formulas are recommended in patients w/ documented & persistent lactose intolerance • Intake of patient’s usual diet is recommended• Foods high in simple sugars should be avoidedMild Dehydration• Administer 50-100 mL of ORS to children <2 years old, 100-200 mL to children 2-10 years old, or unlimited
amount for children >10 years old, after each loose stool, or 20 mL/kg body weight/hour to replace estimated fl uid defi cit
• Several trials support the use of NG ORS feeding even in patients w/ continuous vomiting or w/ presence of oral ulcers
• Continue breastfeeding or resume age-appropriate feeding• Rapid IV hydration may also be administered
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B133
Gastroenteritis - Bacterial (8 of 15)
Not all products are available or approved for above use in all countries.Specifi c prescribing information may be found in the latest MIMS.
B PATIENT EDUCATION• Bacterial gastroenteritis is contagious • Good hygiene (eg handwashing & housekeeping) is needed especially during outbreaks
- Handwashing should also be observed in caregivers having contact w/ patient’s feces to minimize potential transmission
• Early refeeding w/ age-appropriate foods is benefi cial• Breastfeeding in young children helps decrease the incidence of acute gastroenteritis & hospital admissions
from diarrhea
C EMPIRIC ANTIBIOTICS FOR TRAVELER’S DIARRHEAEmpiric treatment of traveler’s diarrhea has been the best approach, but its usefulness is being undermined by growing antibiotic resistance in many parts of the worldGeneral � erapy Principles• � e objectives of antimicrobial treatment of traveler’s diarrhea are shortening illness & returning travelers to
normal activities• Eradication of enteropathogens from stool does not predict the clinical benefi ts of antimicrobial therapy• Traveler’s diarrhea is typically short-lived & self-limited, but many organisms that cause the infection can be
treated w/ antibiotics• Choice of therapy should depend on epidemiologic dataEmpiric AntibioticsAzithromycin• May be the treatment of choice for C jejuni infection for patients 2-8 years of age• Reported eff ective against traveler’s diarrhea in Southeast AsiaCo-trimoxazole [Sulfamethoxazole (SMZ) & Trimethoprim (TM)]• Historically the drug of choice for treatment of traveler’s diarrhea• Resistance of enterotoxigenic E coli (ETEC) & Salmonella sp to this drug limits its usefulness
PREVENTION OF TRAVELER’S DIARRHEA• Traveler should avoid:
- Undercooked food except peeled fruits or vegetables- Non-bottled beverages & unpasteurized dairy products
Water Purifi cation • Travelers who are going to be living in rustic circumstances overseas will need to make arrangements for a
safe water supplyProphylactic Antibiotics• Eff ective but cannot be recommended unless the complications of diarrhea in a traveler or severe dehydration
in a person w/ an underlying medical condition cause the benefi ts of antibiotic prophylaxis to outweigh the risks• May also be given to asymptomatic people whose stools have been tested positive for Salmonella enterica
subspecies enterica serovar typhimurium to reduce spread of infectionProbiotics • May decrease the incidence of diarrhea in travelers• Eg Lactobacillus sp, Saccharomyces boulardii, Bi� dobacterium sp
A REHYDRATE & MAINTAIN HYDRATION (CONT’D)Moderate to Severe Dehydration• Start patient on rapid IV rehydration• Administer 20 mL/kg body weight of IV lactated Ringer’s solution or normal saline solution (0.9% NaCl) until
pulse, perfusion & mental status return to normal, followed by 100 mL/kg body weight of ORS for 4 hours or 5% dextrose ½ normal saline IV at 2x maintenance fl uid rates - Alternatively, give 100 mL/kg body weight. � en, for infants <1 year, give 30 mL/kg/body weight within the
1st hour, followed by 70 mL/kg/body weight within 5 hours. For children >1 year, 30 mL/kg/body weight IV fl uid may be given within the 1st 30 minutes, followed by 70 mL/kg/body weight within 2.5 hours
- Administration of ORS may encourage early resumption of feeding - Study shows that giving of ORS may lead to rapid resolution of acidosis compared to IV fl uid
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B134
Gastroenteritis - Bacterial (9 of 15)
Not all products are available or approved for above use in all countries.Specifi c prescribing information may be found in the latest MIMS.
D EMPIRIC ANTIBIOTICS FOR CHOLERA• Rehydration is the mainstay of therapy• When antibiotics are administered to cholera patients, there is reduction of stool volume loss & a shorter
clinical course• Antibiotics administered should follow recent sensitivity data for V cholera, if availableEmpiric Antibiotics• Doxycycline & Tetracyclines are preferred agents against V cholera
- Not recommended in patients <8 years of age• Co-trimoxazole, Erythromycin & Ciprofl oxacin are alternative drugs
E EMPIRIC ANTIBIOTICS FOR BLOODY DIARRHEA• Antipropulsives should be avoided as these drugs may increase the severity by delaying excretion of organisms
& facilitating invasion of the mucosa• Usage of antibiotics should be judicious & not for all casesEmpiric Antibiotics• Antibiotics may reduce the duration of illness & shorten the carrier stage• Initiation of empiric antibiotics may be considered in special situations:
- Infants <3 months old w/ manifestations of bacterial infection- Immunocompetent patients exhibiting signs & symptoms of Shigella infection (fever, abdominal pain,
hematochezia)- Recently traveled & w/ fever of ≥38.5°C & other signs of septicemia
• Once EHEC or Shiga toxin-producing E coli (STEC) has been excluded by stool exam, empiric therapy w/ antibiotics can be started
• Broad-spectrum antimicrobials should be started in patients w/ signs & symptoms pointing to sepsis as soon as specimens have been collected- Antibiotic therapy should be tailored once results become available
• Antibiotics following the local sensitivities for Shigella sp may be used as empiric therapy before waiting for culture & sensitivity results
• Ciprofl oxacin or any 3rd generation cephalosporin (eg Ceftriaxone, Cefotaxime) may be used as empiric therapy for infants <3 months of age, & patients w/ CNS manifestations, or Azithromycin in pediatric patients, depending on location & antimicrobial susceptibility data, & travel history- � ere are reports on resistance to Ciprofl oxacin in some countries (please refer to local guidelines for
recommended antibiotics)• � ere is widespread resistance to the following drugs: Ampicillin, Co-trimoxazole, Chloramphenicol, Nalidixic
acid, Tetracycline, Gentamicin & 1st- & 2nd-generation cephalosporins
PREVENTION OF CHOLERA/CAREGIVER EDUCATION• V cholera is spread through contaminated food & water• Prevention depends on interruption of fecal-oral transmission• Travelers to regions w/ cholera should follow precautions for the prevention of traveler’s diarrhea• Water can be treated w/ chlorine or iodine, by fi ltration or by boiling
ADJUNCTIVE THERAPYProbiotics• Eg Bacillus clausii, Bi� dobacterium spp, Lactobacillus spp, Saccharomyces boulardii• Have been shown to reduce the intensity & duration of diarrhea of acute infectious diarrhea in children • Bacillus clausii contributes to the recovery of the intestinal microbial fl ora altered during the course of microbial
disorders of diverse origin- It is capable of producing various vitamins, in particular group B vitamins, hence it contributes to correcting
the consequent vitamin disorders caused by antibiotics & chemotherapeutic agents in general• Bi� dobacterium spp is the most commonly used probiotic that is used to improve the health of the host when
given in adequate amounts• Lactobacillus spp is a lactic acid bacteria used as an adjunct to rehydration therapy in children w/ acute
gastroenteritis• Saccharomyces boulardii is a yeast that is used as an adjunct to rehydration therapy in children w/ acute
gastroenteritis- It is an intestinal replacement fl ora which acts as an antidiarrheal microorganism in the digestive tract- It transits in the digestive tract without colonizing it, rapidly attaining signifi cant intestinal concentrations
which are maintained at a constant level throughout the administration period
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B135
Gastroenteritis - Bacterial (10 of 15)
1Ciprofl oxacin is not recommended in patients <18 years of age, except in cases when potential benefi ts outweigh the risks.2Tetracycline & Doxycycline are contraindicated in patients <8 years of age.
Not all products are available or approved for above use in all countries.Specifi c prescribing information may be found in the latest MIMS.
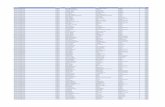
F PATHOGEN-SPECIFIC TREATMENT OF BACTERIAL DIARRHEAPathogen Preferred Agent(s) Alternative Agent(s) Remarks
Aeromonas/Plesiomonas spp
Antibiotics not usually requiredAeromonas sp: Antibiotics may be indicated in patients prone to septicemia (eg cirrhosis, immunocompromised patients) Plesiomonas sp: Antibiotics may be required in severely ill or immunocompromised patients
Co-trimoxazole Ciprofl oxacin1
ChloramphenicolAminoglycosides
Campylobacter spp
Antibiotics not usually required; may be used in severely ill patients or traveler’s diarrhea
• A self-limiting condition
• Early treatment can shorten the duration of the illness & prevent any relapse
ErythromycinAzithromycinCiprofl oxacin1
Tetracycline or Doxycycline2
EHEC 0157:H7 Antibiotics & antipropulsives are contraindicated; may increase the chance of developing hemolytic uremic syndrome
Salmonella spp CefotaximeCeftriaxone
AmpicillinCo-trimoxazoleCiprofl oxacin1
Chloramphenicol
• Ceftriaxone may be considered in suspected septicemic cases
• Follow available local epidemiologic data
Shigella spp CefotaximeCeftriaxoneCiprofl oxacin1
Co-trimoxazole
Azithromycin • A self-limiting condition
Yersinia spp Co-trimoxazoleTetracycline or Doxycycline2
Ciprofl oxacin1
Antipseudomonal aminoglycosides3rd generation cephalosporins (eg Cefotaxime)
ADJUNCTIVE THERAPY (CONT’D)Zinc• Zinc supplementation given during an episode of diarrhea may decrease the duration & severity of diarrheal illnessAntiemetic Agents• Eg Ondansetron• May be used in patients >4 years of age to decrease vomiting or help avoid the need for IV fl uid, but may
increase episodes of diarrhea Antisecretory Agent (Racecadotril)• May be used as an adjunctive therapy in acute diarrhea
- Studies showed decreased diarrhea duration & reduced stool output following administration of Racecadotril in children w/ acute diarrhea
Bovin Colostrum• Contains antimicrobial peptides (lactoferrin, lactoperoxidase), immune-regulating & infl ammatory cytokines,
& growth factors that may help provide passive immunity by enhancing diff erent immune functions (eg phagocytosis, antigen presentation, antimicrobial activity via antigen chelation, infl ammation control) in the gastrointestinal tract- Studies showed that bovine colostrum improved clinical symptoms (eg reduced stool frequency, reduced
occurrence & duration of diarrhea) in children w/ infectious diarrhea - Clinical benefi t in the prevention & management of infectious diarrhea is currently undergoing clinical trials
Investigational Agents • Human milk, gelatin tannate & other probiotics are being studied to conclude their use in the management of
gastroenteritis
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B136
Gastroenteritis - Bacterial (11 of 15)
All dosage recommendations are for children w/ normal renal & hepatic function unless otherwise stated.Not all products are available or approved for above use in all countries.
Products listed above may not be mentioned in the disease management chart but have been placed here based on indications listed in regional manufacturers’ product information.
Specifi c prescribing information may be found in the latest MIMS.
Dosage Guidelines
ANTIBACTERIAL COMBINATION
Drug Dosage Remarks
Co-trimoxazole [Sulfamethoxazole (SMZ) & Trimethoprim (TMZ)]
8-12 mg/kg/day PO divided 12 hrly based on TM
Adverse Reactions • GI eff ects (N/V, anorexia, diarrhea, glossitis, stomatitis, rarely
antibiotic-associated diarrhea/colitis); Dermatologic eff ects (rash, pruritus, photosensitivity); Hypersensitivity reactions can range from mild (eg rash) to severe/life-threatening (eg Stevens-Johnson syndrome, toxic epidermal necrolysis); Urogenital eff ect (crystallization in the urine)
• Rarely hematologic eff ects which may be more common if given for long periods or w/ high doses; Rarely hepatic eff ects, renal eff ects; Aseptic meningitis has occurred
Special Instructions• Maintain adequate fl uid intake• Contraindicated in patients <2 mth of age & patients w/
sulfonamide allergy• Use w/ extreme caution or not at all in patients w/ hematological
disorders especially megaloblastic anemia due to folic acid defi ciency• Use w/ caution in patients w/ renal impairment or severe hepatic
dysfunction, folate defi ciency (may consider administration of Calcium folinate), G6PD defi ciency
ANTIDIARRHEALS
Drug Dosage Remarks
Antidiarrheal MicroorganismsBacillus clausii 2-3 vials PO 24 hrly Special Instructions
• Given in interval between antibiotic dosesLactobacillus spp (L reuteri, L acido-philus, L rhamnosus, L sporogenes)
450 mg PO 24 hrly Special Instructions• Should be taken w/ food
Lyophilized Saccharomyces boulardii
250 mg PO 12-24 hrlyPrevention of traveler’s diarrhea:Must be taken 5 days before travel
Adverse Reactions• Dermatological eff ects (rash, urticaria, pruritus); Other
eff ects (fl atulence, angioedema)Special Instructions• Use w/ caution in patients w/ diarrhea of >2 days • Contraindicated in patients w/ allergies to yeast &
immunocompromisedAntipropulsiveLoperamide1 Initial dose:
>6 yr: 2 mg POSubsequently after each loose stool: 6-8 yr: 1 mg PO≥9 yr: 2 mg POMax dose: 2-5 yr: 3 mg/day6-8 yr: 4 mg/day9-12 yr: 6 mg/day
Adverse Reactions• GI eff ects (abdominal pain, nausea, constipation, rarely
paralytic ileus); Hypersensitivity reactionsSpecial Instructions• Do not use in patients w/ ileus, abdominal distension, acute
IBD, antibiotic-associated colitis, or any other condition for which inhibition of peristalsis must be avoided
• Use w/ caution in patients w/ hepatic impairment
1Combination w/ Simeticone (Simethicone) is available. Specifi c prescribing information may be found in the latest MIMS.
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B137
Gastroenteritis - Bacterial (12 of 15)
ANTIDIARRHEALS (CONT’D)
Drug Dosage Remarks
Intestinal AdsorbentsBismuth subsalicylate
3-6 yr: 87 mg PO every 30 min-1 hr as required6-9 yr: 175 mg PO every 30 min-1 hr as required9-12 yr: 262 mg PO every 30 min-1 hr as requiredMax dose: 8 doses/24 hr
Adverse Reactions• Long-term use may produce tinnitus; allergic reactions in
salicylate-sensitive patients; black discoloration of the tongue/black stools from nonabsorbable Bismuth salts
Special Instructions• Use w/ caution in patients w/ gout, renal insuffi ciency & those
taking anticoagulants, Probenecid, Methotrexate, Aspirin-containing drugs
• Brushing the teeth & tongue, rinsing mouth w/ water after each dose may help prevent tongue discoloration
Dioctahedral smectite
<1 yr: 3 g/day PO in 2-3 divided doses1-2 yr: 3-6 g/day PO in 2-3 divided doses>2 yr: 6-9 g/day PO in 2-3 divided doses
Adverse Reactions• GI eff ect (rarely constipation)Special Instructions• Should be taken alone & not w/ other drugs as it aff ects
absorption of these substances
Other AntidiarrhealsRacecadotril Day 1: 1.5 mg/kg/dose
PO w/ 1 initial dose then 3 divided doses dailySubsequent days:3 divided doses dailyMax duration: 7 days
Adverse Reactions• GI eff ects (nausea, constipation); Other eff ects (headache,
drowsiness)Special Instructions• Ensure adequate hydration• Contraindicated in patients w/ bloody/purulent stool &/or
fever, prolonged uncontrolled vomiting, fructose intolerance, sucrase-isomaltase defi ciency, glucose-galactose malabsorption
Other Intestinal AntiinfectivesNifuroxazide Infant <6 mth: 250 mg
PO 12 hrlyChildn & infant >6 mth: 250 mg PO 8 hrly Max duration: 7 days
Adverse Reactions• GI eff ects (abdominal pain, diarrhea, green pigment on
tongue, feces & urine); Other eff ects (allergic reactions, reduction of normal microbial fl ora, cerebral disturbances)
Special Instructions• Ensure adequate hydration• Use w/ caution in patients w/ neurological disorder• Contraindicated in patients w/ bloody or mucoid stools, fever,
vomiting
All dosage recommendations are for children w/ normal renal & hepatic function unless otherwise stated.Not all products are available or approved for above use in all countries.
Products listed above may not be mentioned in the disease management chart but have been placed here based on indications listed in regional manufacturers’ product information.
Specifi c prescribing information may be found in the latest MIMS.
Dosage Guidelines
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B138
Gastroenteritis - Bacterial (13 of 15)
All dosage recommendations are for children w/ normal renal & hepatic function unless otherwise stated.Not all products are available or approved for above use in all countries.
Products listed above may not be mentioned in the disease management chart but have been placed here based on indications listed in regional manufacturers’ product information.
Specifi c prescribing information may be found in the latest MIMS.
Dosage Guidelines
ELECTROLYTES
Drug Dosage Remarks
Sodium chloride, Trisodium citrate, Potassium chloride, Glucose (NaCl, KCl, Trisodium citrate, Glucose anhydrous)
<2 yr: 1 sachet (5.125 g) PO for the 1st 2 hr, then up to 8 hrly2-5 yr: 1 sachet (5.125 g) PO 3x for the 1st 2 hr, then up to 4 hrly>5 yr: 1 sachet (5.125 g) PO 4x for the 1st 2 hr, then up to 3 hrly
Adverse Reactions• Hypernatremia, Na & water retention, N/VSpecial Instructions• Dissolve 1 sachet in 250 mL water• Use in caution in patients w/ renal impairment,
severe dehydration, severe & prolonged diarrhea, glucose malabsorption, vomiting, inability to drink
CEPHALOSPORINS
Drug Dosage Remarks
� ird Generation Cefi xime >6 mth: 1.5-3 mg/kg PO 12 hrly
Severe infections: 6 mg/kg PO 12 hrlyAdverse Reactions• Hypersensitivity reactions (urticaria,
pruritus, rash, severe reactions eg anaphylaxis can occur); GI eff ects (diarrhea, N/V, rarely antibiotic-associated diarrhea/colitis); Other eff ects (Candidal infections, inj site infl ammation)
• High doses may be associated w/ CNS eff ects (encephalopathy, convulsions); Rarely hepatic, renal & hematologic eff ects have occurred
• Prolonged prothrombin time (PT), prolonged activated partial thromboplastin time (APTT), &/or hypoprothrombinemia (w/ or without bleeding) have been reported & occurs most frequently w/ N-methylthiotetrazole (NMTT) side chain containing cephalosporins
Special Instructions• May be taken w/ food to decrease gastric
distress• Ceftriaxone is contraindicated in
hyperbilirubinemic neonates• Avoid simultaneous administration of
Ceftriaxone w/ IV Ca-containing soln• Use suspension containing sodium
benzoate w/ caution in neonates as this has been associated w/ gasping syndrome
• Use w/ caution in patients allergic to Penicillin, there may be 10% chance of cross sensitivity; & patients w/ renal impairment & GI disease especially w/ history of colitis
Cefoperazone 50-200 mg/kg/day IM/IV divided 12 hrlyCefotaxime Neonates <7 days:
1.2-2 kg: 100 mg/kg/day IM/IV divided 12 hrly >2 kg: 100-150 mg/kg/day IM/IV divided 8-12 hrly Neonates >7 days:1.2-2 kg: 150 mg/kg/day IM/IV divided 8 hrly>2 kg: 150-200 mg/kg/day IM/IV divided 6-8 hrly Infants & childn:100-200 mg/kg/day IM/IV divided 6-8 hrly
Ceftazidime 30-100 mg/kg/day IM/IV divided 8-12 hrlyMax dose: 6 g/day IM/IV divided 8 hrly Neonates & infants:25-60 mg/kg/day IM/IV divided 12 hrly
Ceftibuten 9 mg/kg PO 24 hrlyMax dose: 400 mg/day
Ceftriaxone ≤2 wk: 20-50 mg/kg IM/IV 24 hrly3 wk-12 yr: 20-80 mg/kg IM/IV 24 hrly
Fourth GenerationCefepime >2 mth & ≤40 kg: 50 mg/kg IM/IV
8-12 hrly
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B139
Gastroenteritis - Bacterial (14 of 15)
All dosage recommendations are for children w/ normal renal & hepatic function unless otherwise stated.Not all products are available or approved for above use in all countries.
Products listed above may not be mentioned in the disease management chart but have been placed here based on indications listed in regional manufacturers’ product information.
Specifi c prescribing information may be found in the latest MIMS.
Dosage Guidelines
PENICILLINS
Drug Dosage Remarks
Aminopenicillins w/ or without Beta-lactamase InhibitorsAmoxicillin (Amoxycillin) 40-50 mg/kg/day PO divided 8 hrly
High-dose: 80-90 mg/kg/dayAdverse Reactions• Hypersensitivity reactions (rash,
urticaria, pruritus, severe reactions eg anaphylaxis can occur); GI eff ects (diarrhea, N/V, rarelyantibiotic-associated diarrhea/colitis); Other eff ect (Candidal infections)
• Rarely hematologic, renal & hepatic eff ects; High doses may be associated w/ CNS eff ects (encephalopathy, convulsions)
Special Instructions• Avoid in patients w/ Penicillin
allergy• Use w/ caution in patients w/ renal
impairment
Amoxicillin/clavulanic acid (Co-amoxiclav, Amoxicillin/clavulanate)
≥3 mth: 25-50 mg/kg/day PO divided 8 hrly based on Amoxicillin orNeonates: 25-30 mg/kg IV 8-12 hrly≥3 mth: 25-30 mg/kg IV 6-8 hrly
Ampicillin 50-100 mg/kg/day PO divided 6 hrly or100-200 mg/kg/day IM/IV divided 6 hrly
Ampicillin/sulbactam [Sultamicillin (Ampicillin & Sulbactam), Sultamicillin: Pro-drug of Ampicillin/sulbactam, the 2 drugs are linked chemically w/ a double ester]
<30 kg: 25-50 mg/kg/day PO divided 12 hrly based on Ampicillin or150-300 mg/kg/day IM/IV divided 6-8 hrly
OTHER ANTIBIOTICS
Drug Dosage Remarks
Rifaximin >12 yr: 200 mg PO 8 hrly x 3 daysor400 mg PO 12 hrly x 3 days
Adverse Reactions• CNS eff ects (dizziness, headache, N/V); GI eff ects (pseudomembranous
colitis, abdominal pain, bloating, constipation, diarrhea, urgency to evacuate feces, involuntary & painful/ineff ective straining); Other eff ects (fever, overgrowth of nonsusceptible organisms)
Special Instructions• Contraindicated in patients w/ infectious/traveler’s diarrhea w/ fever &/or
bloody stools, & children <12 yr
MACROLIDES
Drug Dosage Remarks
Erythromycin 30-50 mg/kg/day PO divided 6-12 hrly
Adverse Reactions• GI eff ects (N/V, abdominal discomfort, diarrhea & other GI
disturbances, antibiotic-associated diarrhea/colitis, stomatitis, infantile hypertrophic pyloric stenosis); Other eff ects (Candidal infections, headache)
• Hypersensitivity reactions are uncommon (urticaria, pruritus, rash, rarely anaphylaxis); Rarely cardiotoxicity, hepatotoxicity; Dose-related tinnitus/hearing loss have occurred w/ some macrolides
• Azithromycin tend to cause less GI disturbances than ErythromycinSpecial Instructions• May take w/ food to decrease gastric distress• Use w/ caution in patients w/ hepatic dysfunction
Advanced MacrolideAzithromycin 10 mg/kg PO 24 hrly
x 3 daysor10 mg/kg PO 24 hrly x 1 day followed by 5 mg/kg PO 24 hrly x 4 days
© MIMS Pediatrics 2020
© MIM
S
GAST
ROEN
TERI
TIS
- BAC
TERI
AL
B140
Gastroenteritis - Bacterial (15 of 15)
All dosage recommendations are for children w/ normal renal & hepatic function unless otherwise stated.Not all products are available or approved for above use in all countries.
Products listed above may not be mentioned in the disease management chart but have been placed here based on indications listed in regional manufacturers’ product information.
Specifi c prescribing information may be found in the latest MIMS.Please see the end of this section for the reference list.
Dosage Guidelines
TETRACYCLINES
Drug Dosage Remarks
Doxycycline >8 yr & ≤45 kg:4.4 mg/kg/day PO divided 12 hrlyFollowed by 2.2 mg/kg/day PO divided 12 hrly
Adverse Reactions• GI eff ects (N/V, diarrhea, antibiotic-associated diarrhea/colitis has
occurred, discoloration of teeth, dysphagia, esophageal ulceration has occurred when taken w/ an insuffi cient amount of liquid); Other eff ects (Candidal infections, interference w/ skeletal development & bone growth, photosensitivity)
• Rarely renal dysfunction, hepatotoxicity, hematologic eff ects, intracranial pressure w/ headache & visual disturbances; Hypersensitivity reactions have occurred
Special Instructions• Avoid long exposure to sunlight or tanning beds• Take w/ plenty of fl uid while sitting or standing & before retiring to bed• Use w/ caution in renal or hepatic impairment
Tetracycline >8 yr: 25-50 mg/kg/day PO divided 6 hrly
VACCINES, ANTISERA & IMMUNOLOGICALS
Drug Dosage Remarks
Killed bivalent whole cells of Vibrio cholerae O1 & O139
>1 yr: 2 doses of 1.5 mL PO given at 2-wk interval
Adverse Reactions• GI eff ects (abdominal pain, loose stools,
N/V, dry mouth); Other eff ects (fever, rash, pruritus, weakness, cough, vertigo)
Special Instructions• Transient increases in viral load in
immunization of HIV-infected patients• Contraindicated in patients w/ acute illness
or hypersensitivity to formaldehyde• Not be used as replacement for cholera
therapy
Vibrio choleraeO1 Inaba & Ogawa classic & El Tor strains, recombinant cholera toxin B
Cholera:2-6 yr: 3 doses PO administered at 1-wk interval, booster dose within 6 mth>6 yr: 2 doses PO administered at 1-wk interval, booster dose within 2 yrETEC: 2 doses PO administered at 1- to 6-wk interval
SUPPLEMENTS & ADJUVANT THERAPY
Drug Dosage Remarks
Bovine colostrum ≥12 mth: 1 sachet/day (7 g) PO x 3 days
Special Instructions• Mix the contents of 1 packet w/ 30 mL water in a cup• Use w/ caution in patients w/ allergy to milk &/or egg
Lactobacillus spp (L casei, L acidophilus, L rhamnosus, L bulgaricus)/ Bi� dobacterium spp (B breve, B infantis)/Strepto-coccus thermophilus1
1 sachet (1 g) PO 24 hrly x 4-7 days
Special Instructions• Contents of the sachet may be added to food/water/
milk/juice• Use in caution in patients w/ allergy to fi sh, soya or
milk
1Various combination products are available. Please see the latest MIMS for specifi c formulations.
© MIMS Pediatrics 2020
© MIM
S