Final Report — Towards optimal allied health and nursing service provision in VACS funded...
Transcript of Final Report — Towards optimal allied health and nursing service provision in VACS funded...
Final Report — Towards optimal allied health and nursing
service provision in VACS funded specialist clinics
MARCH , 2010
FOR THE
DEPARTMENT OF
HEALTH , VICTORIA
H u m a n C a p i t a l A l l i a n c e
2
Towards Optimal Allied Health and Nursing Service Provision in VACS Funded Specialist Clinics
This report was prepared by:
Human Capital Alliance (International) Pty Ltd PO Box 2014, Normanhurst NSW 2076 Australia
Suite 2, 2a Pioneer Ave, Thornleigh NSW 2120 Ph: +61 2 9484 9745 Fax: +61 2 9484 9746
The Final Report was written by: Rosalie Boyce, Sharon Kendall, Mark Mattiussi, Meredith McIntyre, Lee Ridoutt, Joanne Bagnulo and Adrian Schoo.
Disclaimer
This report has been prepared by Human Capital Alliance (International) for the Department of Health, Victoria. Human Capital Alliance (International) prepares its reports with diligence and care and has made every effort to ensure that evidence on which this report has relied was obtained from proper sources and was accurately and
faithfully assembled. It cannot, however, be held responsible for errors and omissions or for its inappropriate use.
H u m a n C a p i t a l A l l i a n c e
3
Contents
1. EXECUTIVE SUMMARY .................................................................................................. 6
OVERVIEW ............................................................................................................... 6
METHODOLOGY ...................................................................................................... 7
DISCHARGE PERFORMANCE .................................................................................... 8
BETTER USE OF ALLIED HEALTH SKILLS ................................................................ 8
OTHER ALLIED HEALTH CLINICS ........................................................................... 9
GROUP CLINICS ...................................................................................................... 10
CONCLUSION .......................................................................................................... 11
LIST OF RECOMMENDATIONS ................................................................................ 12
2. INTRODUCTION ......................................................................................................... 16
PURPOSE OF THE REVIEW ...................................................................................... 16
BACKGROUND ........................................................................................................ 16
PAST REVIEWS AND REPORTS ................................................................................ 20
METHODOLOGY ..................................................................................................... 21
ABOUT THIS REPORT ............................................................................................. 22
3. IMPROVING THE RATE OF DISCHARGE ............................................................................. 23
BACKGROUND ....................................................................................................... 23
POSSIBLE WAYS FORWARD ..................................................................................... 27
FUNDING SYSTEM CHANGES ................................................................................. 27
NON FUNDING SYSTEM APPROACHES ................................................................... 29
SUMMARY OF RECOMMENDED APPROACH............................................................ 32
4. BETTER USE OF ALLIED HEALTH / NURSING SKILLS .............................................................. 34
BACKGROUND ....................................................................................................... 34
CURRENT SITUATION ............................................................................................ 35
BROAD OPPORTUNITIES ........................................................................................ 37
PRIORITY OPPORTUNITIES ................................................................................... 40
POSSIBLE WAYS FORWARD ..................................................................................... 43
FUNDING SYSTEM CHANGES ................................................................................. 44
NON FUNDING SYSTEM APPROACHES ................................................................... 46
5. RATIONALISATION OF ‘OTHER’ CODED CLINICS ................................................................. 50
BACKGROUND SITUATION ..................................................................................... 50
PATTERNS OF ‘OTHER’ SERVICE DELIVERY .......................................................... 53
POSSIBLE WAYS FORWARD ..................................................................................... 57
6. GROUP CLINICS ......................................................................................................... 61
BACKGROUND ........................................................................................................ 61
CURRENT SITUATION ............................................................................................ 62
A WAY FORWARD .................................................................................................... 64
ANOTHER WAY FORWARD ..................................................................................... 64
H u m a n C a p i t a l A l l i a n c e
4
NON FUNDING APPROACHES ................................................................................ 68
7. DISCUSSION ............................................................................................................. 70
BACKGROUND ....................................................................................................... 70
OVERVIEW OF RECOMMENDATIONS ...................................................................... 71
ALTERNATIVE PATHWAYS ..................................................................................... 73
COST IMPLICATIONS OF RECOMMENDATIONS...................................................... 75
8. REFERENCES ............................................................................................................. 77
APPENDIX A: METHODOLOGY DETAILS .............................................................................. 79
THE QUESTIONNAIRE SURVEY .............................................................................. 79
SITE VISIT INTERVIEW CONSULTATIONS .............................................................. 80
FOCUS GROUP DISCUSSIONS ................................................................................... 81
LITERATURE REVIEW ............................................................................................ 82
APPENDIX B: GROWTH IN MEDICAL SPECIALIST TRAINEES ....................................................... 83
APPENDIX C: ALLIED HEALTH OUTPATIENT OOS TARGETS ..................................................... 84
APPENDIX D: SURVEY RESPONDENTS ................................................................................. 85
APPENDIX E: SURVEY INSTRUMENT .................................................................................. 86
APPENDIX F: STAKEHOLDER CONSULTATIONS .................................................................... 103
APPENDIX G: INTERVIEW SCHEDULE FOR KEY HEALTH SERVICE CONTACTS .............................. 105
APPENDIX H: INTERVIEW SCHEDULE FOR KEY INTEREST GROUPS ........................................... 107
H u m a n C a p i t a l A l l i a n c e
5
Table of Abbreviations BSBC Better Skills, Best Care
CAHE Centre for Allied Health Evidence COAG Council of Australian Government DHS Department of Human Services, Victoria
DRG Diagnostic related group EAL Early Assessment and Linkage EPC Enhanced Primary Care FEES fibre optic endoscopic evaluation of the swallow
FTE Fulltime equivalent HACC Home and Community Care MDC Multidisciplinary care MDS Minimum Dataset
OAHKS Osteoarthritis Hip and Knee Service OIIS Outpatient Innovation and Improvement Strategy OOS occasions of service OWL Orthopaedic Waiting List SVR Surgical Voice Restoration VACS Victorian Ambulatory Classification and Funding System VINAH Victorian Integrated Non-Admitted Health
H u m a n C a p i t a l A l l i a n c e
6
1. Executive Summary
Overview
Since its inception in 1997 the Victorian Ambulatory Classification and Funding System (VACS) has been continually evolving. Recent reviews have focused attention on areas of
possible change. This Review builds on previous internal and external change efforts and was initiated under the Victorian Government’s Outpatient Innovation and Improvement Strategy
(OIIS) in 2006-07. The aim is to improve access to public hospital outpatient services and to address some of the issues identified in the Auditor General’s report (June 2006) Access to specialist medical outpatient care. The purpose of this review was to:
� determine and map the current allied health and advanced nursing practice service provision in acute hospital settings;
� identify opportunities and barriers for further advancement of scope of practice and to provide advice on the required changes to the VACS funding model to support the implementation of extended and advanced allied health roles;
� explore the potential for provision of current specialist clinic allied health services
in alternate settings;
� improve current discharge performance; and
� analyse the possibility of delivering more outpatient services through group rather than individual patient encounters without any loss of efficiency.
The review focuses on allied health and nursing elements of total outpatient services. In
terms of the VACS funding arrangements, this means the scope of the review is limited to funding codes 601 to 611 which include 601, Audiology; 602, Nutrition; 603, Optometry; 604, Occupational Therapy; 605, Physiotherapy; 606, Podiatry; 607, Speech
Pathology; 608, Social Work; 609, Other Allied Health Services; 610, Cardiac Rehabilitation; and 611, Hydrotherapy. The proportion of total outpatient service activity in the VACS allied health coded areas
can vary from as low as 17% to as high as 51% in different health services and overall is just under 30%.
Between the financial years 2001/02 and 2007/08, overall growth in occasion of service activity in the allied health VACS code categories increased by only 9%, but certain VACS code activity grew by almost half while others shrank by almost as much. In absolute terms the largest growth areas were ‘Other Allied Health Services’ (609) and ‘Optometry’
(603), although the latter was off a low base. The largest areas of reduction were ‘Audiology’ (601), ‘Social Work’ (608) and ‘Speech Pathology’ (607). The ‘Other Allied Health Services’ category has grown 13% and over 20,000 occasions of service since 2001 to now account for almost one third of all VACS allied health occasions of service. As a general rule, an ‘other’ category within any taxonomy should not exceed 5% of the total count. Many of the 609 category services are new nursing models of
practice, including advanced practice. Target allied health activity levels are set each year for each health service and funded accordingly. Many of the health services report that there are significant discrepancies
H u m a n C a p i t a l A l l i a n c e
7
between the activity targets budgeted under the VACS and the actual demand for these services. In the 2007/08 financial year more than half of the health services exceeded their targets for allied health coded VACS activity. Overall in that year though, the VACS
funded services activity in the 600 series codes for all health services was 588,3821 outpatients which fell short of the total target set by 6,543, or just over 1% of the
funded target2. In the 2008 / 2009 financial year the total actual activity in the 600 series VACS code area was 556,970 outpatients, again marginally short (approximately 6%) of the set total target activity of 594,248. Total allied health activity has varied considerably from year to year over the last eight years.
Methodology
The methodology employed for this Review to meet the objectives of this report included four main forms of data collection as follows:
� a survey questionnaire completed by all VACS funded services;
� interviews and focus group meetings with representatives from health services, outpatient services and clinic managers;
� focus group meetings with nurse and allied health leaders from outpatient
settings; and
� an extensive literature review of speciality allied health and nursing services currently in use or being trialled in Australia or overseas (i.e. the United
Kingdom, Canada).
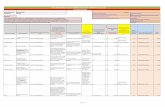
Table 1.1: Review objectives and required research method
Review objectives Survey Interviews Focus
groups
Literature
review Mapping of current allied health and
advanced practice nurse service provision across the selected VACS
funded health services
Understand the potential for provision of
current specialist clinic allied health services in alternate settings
Identification of opportunities for allied health enhanced practitioners and
advanced practice nurses to provide
specialist clinic services
Analysis of ‘group’ encounters for allied health services
Analysis of new and ongoing treatment
sessions and discharge destinations
Identification of potential for
reclassification of 609 VACS clinics
Source: Project Plan
Ongoing open discussion with the Department and the project steering group led to some adjustment and refinement of the method during the project.
1 Victorian-Public hospitals and mental health services: policy and funding guidelines 2007-08 2 Figures based on a count of all patients including the majority categorised as ‘Public’ and a much smaller but still significant number categorised as ‘DVA’ or Department of Veterans Affairs.
H u m a n C a p i t a l A l l i a n c e
8
Discharge performance
The ratio of ‘new’ patients to ‘review’ patients varies considerably between VACS codes
and also between different health services. The proportion of new patients at the average clinic could range from as low as 14% (hydrotherapy) to as high as 70% (audiology). At least 20%, or one fifth of current allied health patient consultations, are estimated by outpatient service providers to be able to be diverted to alternative care settings. There
is much interest in realising this movement of patients and thus significantly increasing the capacity of Victorian specialist outpatient clinics. Funding system changes and educational or administrative changes could facilitate this shift through a ‘package’ of measures to influence change. This package of funding, administrative and educational
measures should drive clinics into the desired direction, help them self-assess when they are not performing as they could, and help them to develop and implement clinic specific initiatives to optimise performance. Recommended interventions include:
� introduction of a differential VACS payment for ‘new’ and ‘review’ patient occasions of service which favours ‘new’ patient services;
� development of a generic discharge protocol that prohibits ongoing patient review in the absence of a re-referral process generated by a community-based service provider;
� introduction of a ‘discharge activity’ payment that supports a more active
referral process from the outpatient environment to community care;
� development of a basic benchmarking system within VACS health services
allowing comparison of like clinics within health service categories, with at least two discharge performance indicators; and
� creation of a separate fund within the Department to support an internal (to VACS funded health services) peer consultancy program for at least 3-5 years.
These measures have been designed to improve the rate of discharge from allied health outpatient clinics without encouraging inappropriate discharge of patients who should be in specialist outpatient services or for whom there are no realistic referral options available in the short term. The objective is to facilitate appropriate discharge of patients who no longer need hospital-based care.
Better use of allied health skills
The current deployment of allied health professionals and nurses into advanced practice activity is characterised by:
� significant variation between VACS code areas of activity and within codes between health services in the types and levels of advanced practice undertaken
by allied health professionals and nurses;
� with the exception of some centrally organised projects (for instance the ‘Better Skills Best Care’ Program), an ad hoc (rather than strategic) approach to
expansion of allied health or nurse activity that has prevailed; and
� a clinician led expansion of allied health and nursing roles at a local level based on the skill, knowledge, experience and expertise of the individual clinicians in
response to patient demand and local contextual pressures.
Much currently labelled ‘extended’ scope of practice is on closer analysis ‘advanced’ practice and, as such, within accepted scope of practice. Depending on the complexity of
the caseload practice may require operating in novel settings and with greater independence, although in consultation with other professionals. The introduction of
H u m a n C a p i t a l A l l i a n c e
9
‘advanced’ practice requires: (1) proving the competence exists to undertake the advanced practice work (this may or may not require credentialed evidence); and (2) obtaining the support of medical specialists if advanced practice involves performing
work which was previously the exclusive domain of medical specialists. Many examples of advanced practice already in VACS funded health services provide proof that this can be achieved.
In terms of the health professional resources devoted to delivering advanced activities as a proportion of total specialist allied health outpatient clinic services there is variation between the VACS code activities. In some areas of VACS activity the contribution of
advanced practice to total activity is minor (for example hydrotherapy, cardiac rehabilitation, audiology) while in some other areas of activity ‘advanced’ practice accounts for just under half of total activity (podiatry, speech pathology, physiotherapy).
The Review recommends a range of measures aimed at increasing the level and pace of the introduction of advanced nursing and allied health practice innovation into Victorian outpatient clinics. The measures would help support innovation, and assist individual
clinicians and clinical teams and their management infrastructure to become informed about innovations. Specific recommendations include the following interventions:
� new innovative clinics that are clinically validated by the Clinical Panel and
satisfy other key criteria (a well argued business case, well developed clinical pathways, strong local support from medical practice and health service executive, and proven competence of nurse and allied health practitioners)
should be supported by temporary supplements to the relevant health service’s VACS targets;
� weighted VACS allied health clinic payments should be progressed;
� introduction of multidisciplinary care (MDC) payment codes would support developments in advanced practice in areas where it has the best chance of flourishing and providing benefit;
� development of generic protocols and clinical pathway guidelines for those
advanced practice developments at one health service that have proven valuable and worthy of broader implementation; and
� a program of meetings of health service based teams of nurse and allied health
clinic practitioners, along with key and relevant medical practitioners and outpatient service managers, where advanced practice innovations can continually be showcased in an environment of collegiate discourse.
Other allied health clinics
The ‘Other Allied Health’ coded activity (609) area last year accounted for just over one
third of total VACS allied health activity (601 to 611 including 609). Analysis of available clinic survey and Clinics Schedule data allows several major clinic sub-groupings to be discerned including:
� specialist nurse – led clinics that tend to run parallel with or otherwise in support of specialist medical or surgical clinics. Some of these clinics are specifically to prepare patients for an operation or support patients post-operatively;
� allied health clinics of disciplines not covered under other 600 codes. The main discipline / service area categories are psychologists, orthoptists, orthotists / prosthetists;
� procedural clinics where a particular set service is provided and the clinics essentially help prepare patients for the procedure which can be a single
H u m a n C a p i t a l A l l i a n c e
10
occasion of service (e.g. a scope procedure) or a longer term course of treatment (e.g. to treat cancer); and
� multidisciplinary clinics (involving only allied health and/or nursing professionals
but no medical specialists). The case for separating these categories from the broader ‘Other’ code can be waged on
the following possible grounds:
� more information about actual outpatient services activity is able to be elicited
for planning and policy development purposes;
� inappropriate outpatient activity can be more easily identified; and
� opportunities for advanced practice within a multidisciplinary care setting (for
instance within a medical or surgical VACS code area) are lost. On the basis of available evidence of the prevalence of current clinic types reported within 609 coded activity a reasonable case could be mounted to introduce the following
new VACS clinic classifications:
� Stomal Therapy;
� Diabetes Education;
� Psychological Services;
� Orthotics and Prosthetics;
� Post-operative wound management;
� Urology services (post-operative); and
� Nurse-led Oncology care. The creation of new codes in the VACS classification has no implications to cost. Health service activity targets will not change; rather existing activity will simply be re-labelled. This might change if recommendations to introduce cost weightings for allied health services were adopted. It is difficult to know how the identified new clinic categories might be weighted and if they will fall on average above or below the current unweighted
rate of payment ($61 per occasion of service).
Group clinics
Several of the health services (20%) claim not to conduct group outpatient activities at all, while many of the others restrict group activities to a narrow band of VACS funded areas. None of the surveyed health services for instance offered group activities for 601 (Audiology), 606 (Podiatry) and 607 (Speech Pathology). Within the VACS codes, group
processes were relatively prominent only for nutrition, physiotherapy and ‘Other Allied Health’ categories.
Group clinics are not well perceived because stakeholders argue group sessions are not cost effective as funding does not take into account the actual time and resources required for the proper organisation, set up and conduct of group sessions. Moreover, many group clinics are claimed to have a ‘group’ and ‘individual’ component (generally an
assessment or monitoring of a care plan) and so services find it easier and more financial to count group participants as individual occasions of service.
Despite the general negative attitude, most outpatient clinicians acknowledge there are some circumstances in which the evidence supports the efficacy of group processes. It seems there are genuine clinical advantages for group sessions where they include elements of peer support and shared learning. Some examples of these are cardiac rehabilitation groups which provide peer support and child health groups where new
H u m a n C a p i t a l A l l i a n c e
11
parents learn from, and support, each other. The Review recommends developing criteria for decision making to aid service providers in identifying circumstances that are appropriate for group processes and for individual occasions of service encounters and
promoting these criteria to health services. Shifting behaviour towards more appropriate use of group clinical processes requires an overhaul to the VACS payment methodology. The current VACS group clinic payment that
is the same as an individual occasion of service infers that group processes have a single purpose only, to increase efficiency of resource (labour) use. This approach is placing group clinics on a pathway to eventual extinction.
To support the use of group clinics where clinically indicated, group activity payment needs to be determined such that the payment is higher than an individual occasion of service, but not so high as to encourage inappropriate use of group processes. The most attractive approach is to set payment levels for group activity within each VACS allied health code developed through cost weight methodology. This would be in keeping with recommendations made for other areas of proposed change.
An alternative would be to define and develop a new set of codes for group activity within VACS. A taxonomy based on purpose appears the most useful way to classify group activity. It is most consistent with an understanding of the worth of group processes.
Different group purposes could include:
� information provision / preparation for treatment;
� education / shared learning;
� peer support;
� assessment; and
� combined or similar courses of treatment / therapy / exercise.
There are several ways purposes can be combined to create different group activity types, each of which would have a different cost implication. A possible classification and payment approach based on a limited number of most feasible group activity types and input cost estimates developed by an expert panel is discussed in Chapter 6.
Whatever changes are implemented, the challenge will be to shift health services from claiming the individual Allied Health VACS codes to the new group codes and specific clinical group activity target setting. Auditing may be required to facilitate this shift in
behaviour.
Conclusion
The introduction of the VACS classification and funding arrangements has achieved some of its architects’ expectations, especially improved fairness in funding allocation, a better description of services provided (which supports better planning and service management) and some efficiencies. However VACS needs to continue to evolve to
provide the right types of incentives for service improvement and efficient delivery. In the area of the Allied Health VACS Codes growth in nursing led clinics under the ‘Other
Allied Health’ code, the flat payment for all occasions of service, and issues around group activities and discharge of patients from services have resulted in diminished value of service data and growing inefficiencies in service planning and decision making.
H u m a n C a p i t a l A l l i a n c e
12
This Review has provided a series of suggestions for improvement that are detailed above under each of the main areas of proposed change viz. clinic discharge; growth in the area of new and advanced nursing and allied health practice including support for
multidisciplinary teams; reduction in the number and proportion of clinics covered under the 609 ‘Other Allied Health’ code; and group clinic services. In total there are 18 separate recommendations which are listed in the following section.
This rather daunting list can be grouped into several broad categories of proposed action as follows:
� introduction of new VACS classification codes by splitting existing 600 series code categories into subunits as a matrix and / or by creating specifically targeted new code categories;
� changing basic elements of the VACS funding arrangement to encourage certain types of health service behaviour;
� development of protocols and guidelines to better inform clinic practitioners
and managers of desired, evidence based practice approaches; and
� building of infrastructure to support the desire for, and the capacity for, dissemination of innovative models of outpatient service delivery.
The cost of implementing the recommendations is qualitatively assessed but this will depend on the pathways adopted, especially whether the preferred pathway to establish cost weighted payments for Allied Health VACS codes is adopted.
List of recommendations
Recommendation 1:
� To require all VACS funded health services to collect and report data on ‘new’ and ‘review’ patients at each clinic from financial year 2010/11.
� To complete data definitions for the outpatient component of VINAH in respect
to patient status (‘new’ or ‘review’, probably by using episode start and other date comparisons).
� To introduce a differential VACS payment in financial year 2011 /12 for ‘new’
and ‘review’ patient occasions of service which favours ‘new’ patient services, where ‘new’ is defined as the occasion when an assessment and treatment plan is developed.
Recommendation 2:
� To develop guidelines that limit the number of allied health occasions of
service for any one patient for all patients referred to outpatient specialist services from a general practitioner. The rules pertaining in the primary care setting under Medicare funding arrangements could easily be copied. These guidelines would place limits on the maximum number of occasions of service but not preclude earlier discharge. After reaching the limit a further referral must be sought from the general practitioner.
� To develop guidelines for all other types of patient journey (for instance those
from inpatient care) that limit the number of initial patient occasions of service to an agreed and appropriate number based on available evidence. Continued treatment beyond this limit would be contingent on gaining a general practitioner (or specialist) referral.
H u m a n C a p i t a l A l l i a n c e
13
� To develop and formally establish service entry protocols will not allow acceptance of referrals (and VACS payments not be honoured) unless the approved patient journey pathway has been followed.
Recommendation 3:
� Following the more universal implementation of data collection requirements, to introduce a benchmarking ‘service’ that provided at least six monthly data at the individual clinic level on the ‘new’ to ‘review’ patient ratio and the average number of occasions of service of patients visiting each clinic on a
nominated ‘census’ week. The scope of this service will depend on the extent to which data collection is limited (for instance it may be constrained to review of Allied Health VACS Codes activity).
� To establish agreed sub-classes within the VACS classification system, to allow meaningful comparison within and between health services. For instance, a distinction may need to be drawn between ‘specialist’ allied health clinics and the more routine ‘treatment’ type clinics.
� To publish benchmark results such that clinics can identify their performance within their health service and within same class clinic categories across all health services (for instance all hydrotherapy treatment clinics).
� To annually audit a selection of clinics that have below average indicators, initially through processes internal to health services but later through external processes if performance issues persist for more than 12 months.
Recommendation 4:
� To establish a budget to be administered by a relevant branch within the
Department of Health that would support the operation of a ‘peer consultant’ workforce, that properly supported identifying the right consultants and administering arrangements for their consultancy activity with relevant clinics, and reimbursed health service employers sufficiently to ‘back fill’
temporary vacancies when peer consultants are engaged in consultancy activities.
Recommendation 5:
� To implement within the next two years advanced practice service models that optimally utilise higher order skills of nurses and allied health professionals.
Recommendation 6:
� To allocate separate occasions of service targets for advanced practice clinics
newly approved by the Clinical Panel which the Panel itself could determine (or approve on application). The target approval would apply for two financial years only, after which it would need to be supported through an allocation
from the total target amount.
Recommendation 7:
� To renew efforts to find appropriate cost weightings for allied health clinics.
Most likely this research work will need to be done collaboratively at a national level and therefore borrow concepts from existing funding models (for instance in South Australia) and be undertaken through Council of
Australian Government (COAG) arrangements.
H u m a n C a p i t a l A l l i a n c e
14
Recommendation 8:
� To examine the examination a multidisciplinary clinic code and payment
where allied health contributes to a medically driven clinic.
� To investigate a new VACS code that covers multidisciplinary care provided only by allied health practitioners and nurses in the absence of any medical practitioner input.
Recommendation 9:
� To develop centrally, through an appropriate forum of relevant Departmental officers and innovative health service providers, a strategic investment plan in worthy (promising) advanced practice models in a similar way to the current
BSBC model. In priority order these can be supported from a separate fund to become operational.
Recommendation 10:
� To increase the number and quality of current collaborative activities in a way that enhances regular interaction between health service and clinic level decision makers and practitioners.
Recommendation 11:
� To develop a state outpatient services training plan that (1) identifies skill
needs for support of implementation of desired advanced practice innovations (2) prioritises investment in those skills where a deficit is perceived to be a barrier to implementation.
� To ascertain the need for skills to be certified.
� To negotiate with appropriate professional associations and / or training and education institutions to undertake skills assessment, recognition and
certification where it is considered necessary or prudent.
Recommendation 12:
� To introduce a number of new VACS codes within the 600 ‘Allied Health’ series. This would include at least codes for:
− Stomal Therapy
− Diabetes Education − Psychological Services − Orthotics and Prosthetics − Post-operative wound management
− Urology services (post-operative) − Nurse-led Oncology care
Recommendation 13:
� To develop criteria for assessing the suitability of clinics on the basis of stated
aims and models of care for an outpatient services setting.
� To conduct an audit of all 609 VACS coded clinics and assess them against the prescribed criteria.
H u m a n C a p i t a l A l l i a n c e
15
� To seek an explanation from health services where clinics do not appear to satisfy the criteria for suitability.
� To install the prescribed criteria to ensure future applications for new clinics
are subjected to a structured assessment of validity to belong within an outpatients services environment.
Recommendation 14:
� To use group coding (and funding) only in cases where evidence-based practice suggests group interaction to be appropriate and to confer clinical
advantages.
Recommendation 15 (preferred option):
� To introduce a funding arrangement based on cost weightings for group activity in each of the allied health VACS code areas if appropriate. Cost weightings to be developed using a similar methodology to that required for
individual occasions of service.
Recommendation 16 (contingency option):
� To increase the payment for group clinics according to payment on the primary purpose/s of the clinic. A limited number of payment options to be developed (say no more than 10) based on the most common types of group clinic purpose or purpose combinations.
� To develop an agreement on the payment levels associated with each group activity type from a reasonable assessment of the inputs required. An expert panel of experienced outpatient clinic allied health and nursing clinicians to be
convened to create this consensus.
Recommendation 17:
� To introduce any new group activity payment first as a shadow funding
arrangement while changes to the VACS funding model are settled.
Recommendation 18:
� To develop criteria for decision making to aid service providers in identifying circumstances which are appropriate for group processes and those which are better suited to individual OOS encounters.
� To provide examples and descriptions of successful group clinics and group activity best practice.
� To initiate a broad promotion and education campaign in regard to group
clinic processes targeting health service outpatient administrators and clinic leaders.
H u m a n C a p i t a l A l l i a n c e
16
2. Introduction Purpose of the Review
This review was initiated under the Victorian Government’s OIIS, which commenced in 2006-07 with the aim of improving access to public hospital outpatient services and
addressing some of the issues identified in the Auditor General’s report (June 2006) Access to specialist medical outpatient care. The purpose of this review was to determine and map the current allied health and advanced nursing practice service provision in acute hospital settings, to identify opportunities and barriers for further advancement of
this scope of practice and to provide advice on the required changes to the VACS funding model to support the implementation of extended and advanced allied health roles, group encounters and multidisciplinary teams.
This Review has provided the following reports prior to this Final Report:
� A description of current and allied health service provision in specialist clinics at selected VACS funded Victorian public hospitals — this report attempted primarily to gain a better understanding of the current activity and the role of allied health and nurse labour in VACS funded hospital outpatient
services with a particular focus on the 600 series VACS funded clinics.
� Identification of opportunities for enhanced practitioners in specialty clinics and the requisite qualifications and scope of practice — this report
focused on the Review objective requiring the identification of opportunities for allied health enhanced practitioners and advanced practice nurses to provide specialist clinic services. The report is mostly based on a review of the literature although qualitative data from consultations in VACS funded health services and
broader stakeholder groups were also drawn upon where appropriate.
The review focuses on allied health and nursing elements of total outpatient services. In
terms of the VACS funding arrangements, this means the scope of the review is limited to funding codes 601 to 611 which include 601, Audiology; 602, Nutrition; 603, Optometry; 604, Occupational Therapy; 605, Physiotherapy; 606, Podiatry; 607, Speech Pathology; 608, Social Work; 609, Other; 610, Cardiac Rehabilitation; and 611,
Hydrotherapy. During the course of the Review a strong interest in the 609 VACS category “Other allied health services” emerged, partly because it was thought that this code might include clinics that should be in alternate care delivery settings and partly because it covered too much of total activity for an ‘other’ category.
Background
Funding arrangements
VACS was introduced in 1997 with the aim of providing a case mix model for outpatient services. The VACS arrangement is used to fund the outpatient services in 19 Victorian public health services.
H u m a n C a p i t a l A l l i a n c e
17
Typically outpatient services include (DHS, 2008):
“ … a number of visits within a short time frame and may overlap with other public
and private inpatient and community-based services. These services essentially
provide specialised consultations, pre and post-hospital care, and other general
medical and allied health services. Hospital outpatient services are important for
teaching and training, and the development of innovative service models. They play
a special role in particular areas and for particular population groups, for example
persons from non-English speaking backgrounds.”
VACS hospitals report patient attendances as either bundled encounters or occasions of service. Encounters refer to visits within one of the 35 VACS weighted medical and surgical clinics and include allowances for the costs of ancillary services such as pathology, radiology and pharmacy which occur in the 30 days either side of the clinic visit. Occasions of service refer to visits within one of the eleven VACS allied health unweighted categories (the 600 series) and the VACS Code 550 for Emergency Medicine. The current VACS Categories and Weights 2009-10 can be found in Appendix 4 of the
Victorian Health Services Policy and Funding Guidelines 2009-10, Part 2 Policy and
Funding Details – Technical Guidelines. For the 2009-10 fiscal year the payments for VACS are $173 per weighted encounter and $61 per allied health occasion of service. The Department of Health routinely calculates the VACS weights for the 35 different bundled
encounter categories provided by the participating VACS Hospitals (that have been able to provide robust and timely data) and this is then used to review the base weighted encounter payment and the relative clinic code weightings.
Activity targets are provided each year for health services with VACS Weighted Encounters and Allied Health Occasions of Service being provided as separate targets for each service. Budgets can then be modelled on the revenue associated with these targets
in conjunction with other revenue target and funding sources for the health services. Targets for all clinics are not set on costing data alone but rather the activity history of a health service with adjustments to take into account service demand and capability.
Outpatient activity Many of the health services report that there are significant discrepancies between the outpatient activity targets budgeted for under the VACS and the actual demand for these
services. In the 2007 / 08 financial year slightly more than half the health services exceeded their targets (see Appendix C) for allied health coded VACS activity. Overall in that year though, the VACS funded services activity in the 600 series codes for all health services was 588,382 outpatients which fell short of the total target set by 6,543, or just
over 1% of the funded target. In the 2008 / 2009 financial year the total actual activity in the 600 series VACS code area was 556,970 outpatients, again marginally short (approximately 6%) of the set total target activity of 594,248. Total activity has varied
considerably from year to year over the last eight years as shown in Figure 2.1 on page 15 making any effort to assess observations on the balance between actual and target patient totals difficult. Indeed in five of the last eight years for which data is available actual patient numbers have exceeded the target for which funding was available
although in three of the last four years actual patient numbers have been below targets. When considering the implementation of new models of allied health and nursing care in ambulatory settings and how incentives in the funding system can assist in uptake of the
new models the nuances of the current model must be considered. If health services are exceeding their activity (revenue) targets and no new activity or revenue is being proposed then there is no incentive in the current system to support the implementation
of new clinics (under new models of care) unless they substitute for presently funded activity. Under this arrangement there will also be the requirement to reduce the FTE
H u m a n C a p i t a l A l l i a n c e
18
establishment of one type of clinician when substituting with another to support the new model of care.
Figure 2.1: Total occasions of service (OOS) activity in the VACS 600 series
(Allied Health) codes Financial Years 2001/02 to 2008/09 with percentage
change from previous year
500000
510000
520000
530000
540000
550000
560000
570000
580000
590000
600000
610000
2001/02 2002/03 2003/04 2004/05 2005/06 2006/07 2007/08 2008/09
-8
-6
-4
-2
0
2
4
6
8
10
OOS % change
Source: Victorian Public hospitals and mental health services: policy and funding
guidelines 2001/02 -2008/09
To some extent substitution of activity between VACS codes appears to have already been the norm. Between the financial years 2001/02 and 2007/08, overall growth in OOS activity in the allied health VACS code categories was only 9.3%, yet certain VACS code activity grew by almost half while others shrank by almost as much. In absolute terms
the biggest growth areas were ‘Other Allied Health Services’ (609) and ‘Optometry’ (603) although the latter was off a low base, and the biggest areas of reduction were ‘Audiology’ (601), ‘Social Work’ (608) and ‘Speech Pathology’ (607). This is
demonstrated in Table 2.1. Apart from the apparent dynamism in service activity between VACS categories, another feature of Table 2.1 is the growth in the ‘Other Allied Health Services’ category. It has
grown 13% and over 20,000 OOS, to now account for just over one third of all VACS allied health occasions of service. Total outpatient encounters vary considerably between health services ranging from
under 40,000 per year to larger services with over 130,000 encounters per year. All health services have medical (101-115) and surgical (201-209) outpatient clinics but some health services have only limited (or no) clinics in the VACS codes of 300 (Dental,
Orthopaedics, Orthopaedic applications, Psychiatry and Behavioural Disorders), 400 (Family Planning, Obstetrics / Gynaecology) or 500 (Paediatric) codes. All health services have outpatient clinic activity in the VACS codes 601 to 611, but not for all codes.
H u m a n C a p i t a l A l l i a n c e
19
Table 2.1: Trends in OOS activity by VACS allied health codes, 2001/02 to 2007/08
Code Category 2001/2002 2007/2008 % Change
between
time
periods
601 Audiology 16,184 10,034 -38%
602 Nutrition 35,270 44,600 +26%
603 Optometry 895 7,830 +774%
604 Occupational Therapy 62,363 70,051 +12%
605 Physiotherapy 142,197 150,052 +6%
606 Podiatry 12,110 11,985 -1%
607 Speech Pathology 19,589 14,530 -26%
608 Social Work 88,350 65,721 -26%
609 Other Allied Health Services 152,715 204,286 +34%
610 Cardiac Rehabilitation 4,415 3,262 -27%
611 Hydrotherapy 4,096 6,031 +47%
TOTAL 538,184 588,382 +9.3%
Source: AIMS data (2009)
In Figure 2.2 below the proportion of total outpatient encounters (again gathered through the VACS AIMS data collection process) able to be attributed to codes 601 to 611 (allied health) for all VACS funded health services is shown.
Figure 2.2: VACS funded outpatient service codes 601 to 611 as a proportion of
total outpatient services in selected health services, 2008 and 2009 financial
years
0
10
20
30
40
50
60
%
o
f
t
o
t
a
l
s
e
r
v
i
c
e
s
A B C D E F G H I J K L M N O P Q R S
Health services
2007-08 2008-09
Source: AIMS data (2009)
As shown in Figure 2.2, the allied health (and other) proportion of total outpatient services can vary from as low as 17% to as high as 51% in different services. There does
not seem to be an obvious pattern in this variation, other than that, the smaller and less
H u m a n C a p i t a l A l l i a n c e
20
specialised hospitals have a lower proportion. This could be a reflection of available allied health staffing resources.
New clinics In the event that a new clinic is proposed by participating health services or the expansion of current clinics is required then there is an established pathway to be followed. This pathway involves the use of the Clinical Panel which is a panel of eminent clinicians from a range of specialties, representatives from the field and Departmental representatives whose role it is to preside over decisions regarding the classification and
use of the VACS eligible clinics3. The role only concerns the clinical verification of clinics as appropriate for inclusion in the VACS model, (e.g. whether a clinic is appropriate for
the category for which it has been submitted or should be in another category). Where there has been a request for additional funding for a new clinic, the Panel's decision will inform its consideration.
The Clinical Panel meets and advises if there is sufficient clinical evidence to support the new clinic, if an expanded clinic meets the relevant guidelines and also whether the clinic is best provided as ambulatory care or alternatively in the community.
Past reviews and reports
Significant intellectual capital has been invested through work that has already been undertaken in the area of VACS funding and allied health clinics: this Review seeks to
build on selected themes from this past work. The past efforts which this Review has most considered are:
� Auditor General Victoria (2006) Access to specialist medical outpatient care,
Auditor Generals Office, Victoria
� Healthcare Management Advisors (2006) VACS clinical verification and activity audit. Department of Human Services, Victoria
� Victorian Government Department of Human Services (2006) Care in your community: A Planning Framework for Integrated Ambulatory Health Care, Melbourne, Victoria
� SANO Consulting (2008) Development and Pilot of a Generic Outpatient Care
Pathway Template Department of Human Services, Victoria
� Aspex Consulting (2008) Review of the Victorian Ambulatory Classification &
Funding System. Final Report and Implementation Plan. Department of Human Services, Victoria
� Victorian Government Department of Human Services (2008) Review of the
Victorian Ambulatory Classification & Funding System and the DHS response to
Aspex Consulting Review, Melbourne, Victoria
� Victorian Government Department of Human Services (2008) Victorian
Ambulatory and Classification System (VACS) and Funding Model A profile for
1997/98 – 2008/09, Funding Health & Information Policy Branch, (Funding Policy) of the Metropolitan Health and Aged Care Services, Melbourne Victoria
� Victorian Government Department of Human Services (2009) Victorian health
services policy and funding guidelines 2009–10 Part 1: Highlights, Melbourne, Victoria
� Victorian Government Department of Human Services (2009) Victorian health
services policy and funding guidelines 2009–10 Part 2: Policy and funding details Policy and program initiatives, Melbourne, Victoria
3 The Panel has no responsibility for the approval of VACS targets or funding requests related to those clinics, but does inform the process.
H u m a n C a p i t a l A l l i a n c e
21
� Victorian Government Department of Human Services (2009) Victorian Public Hospital Specialist Clinics: Strategic Framework, Melbourne Victoria
There are many common themes within these reports pertinent to improving on the current allied health VACS classification and funding arrangements. These include:
� the absence of high quality, detailed patient level data;
� that there is no agreed international, national or local classification system for outpatients that is comparable to the current inpatient classification system;
� reinforcing our finding of the increasing use of the VACS Clinic Code 609 “Other Allied Health”, which has grown to be a very heterogeneous group of clinics;
� that any proposed change to the classification system for the VACS Clinic Code
609 will need to be cognisant of AHCA/National Health Care Agreement reporting requirements;
� specialist nurse clinics should be allocated to a new VACS category that
distinguishes them (professionally) from Allied Health Professionals;
� there are currently accepted practices where endorsed nurse practitioners and midwives are eligible to claim medical VACS for their clinic consultations as they
are viewed as substitution;
� the potential for telephone screening including Early Assessment and Linkage (EAL) clinics should be trialled though it was considered prudent that the
payment for these should be captured as a part of the bundled VACS encounter;
� that the application of weights should be considered for those non weighted OOS (Allied Health VACS codes 601 to 611 including group clinics), Multidisciplinary
Care (MDC) Services and Care Planning Conferencing (CPC);
� any sudden change to Allied Health Cost Weights may have significant funding implications within and between health services and it would be prudent to implement a shadow funding arrangement in the first instance; and
� that funding for group clinics consider the different types of group clinics in light of the number of providers per group; a group with individual treatment plans for participants; and classes where all participants receive identical attention
from one provider.
Methodology
The methodology employed for this Review, in so far as the main tasks and activities are
concerned, included four main forms of data collection viz.:
� a survey questionnaire completed by all VACS funded services;
� interviews and focus group discussions with health service, outpatient service and clinic managers;
� focus group discussions with nurse and allied health leaders from outpatient
settings; and
� an extensive literature review of speciality allied health and nursing services currently in use or being trialled in Australia or overseas (i.e. the UK, Canada,
etc.).
The methodology was fixed after initial consultations with the Department set the parameters for the Review and was laid out in the Project Plan. Ongoing open discussion
with the Department and the project steering group led to appropriate adjustment and refinement of the method. Descriptions of each of the above processes of data collection are provided in Appendix A. Table 2.2 below summarises the relationship between
methods of data collection and analysis and the objectives of the Review.
H u m a n C a p i t a l A l l i a n c e
22
Table 2.2: Relationship between methods of inquiry and review objectives
Review objectives Survey Interviews Focus
groups
Literature
review Mapping of current allied health and
advanced practice nurse service
provision across the selected VACS
funded health services
Understand the potential for provision of
current specialist clinic allied health services in alternate settings
Identification of opportunities for allied
health enhanced practitioners and advanced practice nurses to provide
specialist clinic services
Analysis of ‘group’ encounters for allied
health services
Analysis of new and ongoing treatment
sessions and discharge destinations
Identification of potential for
reclassification of 609 VACS clinics
Source: Project Plan
About this report
This report provides a consolidated view of the current allied health service provision in
VACS funded specialist clinics and identifies opportunities for more efficient and effective utilisation of outpatient clinics. In terms of the VACS funding arrangements, this means the scope of the Review is limited to funding codes 601 to 611 which include 601, Audiology; 602, Nutrition; 603, Optometry; 604, Occupational Therapy; 605,
Physiotherapy; 606, Podiatry; 607, Speech Pathology; 608, Social Work; 609, Other; 610, Cardiac Rehabilitation; and 611, Hydrotherapy. In Chapter 3 the report addresses ways to improve efficiency within the current clinics through improved discharge. Chapter 4 builds on improving capacity of the current workforce with extension of the current roles of allied health and nursing practitioners into advanced and extended roles. Chapter 5 looks at the provision of outpatient services
provided under the 609 or ‘other’ funding category. Chapter 6 expands on Group sessions and describes possible methodologies for enhancing the uptake of groups including VACS funding system changes and the report concludes with the discussions in Chapter 7 that attempt to overview the broad intent of recommendations throughout the
report.
H u m a n C a p i t a l A l l i a n c e
23
3. Improving the rate of discharge Background
In an earlier report for this project (HCA, 2009a) based on survey data it was noted that the ratio of ‘new’ patients to ‘review’ patients varied considerably between VACS code areas of activity and also within codes between different health services. The proportion
of new patients at the average clinic could range from as low as 14% (hydrotherapy) to as high as 70% (audiology). In Table 3.1 below, the ‘average’ proportion of new patients at each clinic is provided, calculated by adding all viable responses and dividing by the total number of valid respondents. In some cases extreme outlier values were excluded
from the analysis. A median statistic was examined, but after outlier values were excluded there was little difference between mean and median statistics. The range of
values for new patient proportions is also provided in Table 3.14.
Table 3.1: Average the number of reviews per patient within the 601-611 VACS
codes
VACS
Code VACS descriptor Average % New
Patients per clinic
Range of new patient
clinic ratios
601 Audiology 70.1%* 1:2 to 10:1
602 Nutrition 47.1% 1:5 to 4.5:1
603 Optometry 33%% 1:5 to 1.1
604 Occupational Therapy 36.5% 1:8 to 1:0 (only new)
605 Physiotherapy 30.5% 1:18 to 12:1
606 Podiatry 11.1% 1:12 to 1:4
607 Speech Pathology 37.1%* 1:8 to 4:1
608 Social Work 52.7% 1:8 to 6:1
610 Cardiac Rehabilitation 22.7% 1:10 to 2:1
611 Hydrotherapy 13.6% 1:10 to 1:4
Source: Survey of health services * One outlier value removed from the analysis since it was distorting the figures
Several stakeholders noted that an average statistic in regard to the proportion of new
patients per clinic was potentially meaningless if allied health clinics were distributed bi-modally. They argued this could be the case with clinics falling into two distinct groups:
A. specialist clinics that largely undertook assessment and referral tasks such as a
health service physiotherapy clinic described as a “… Screening clinic for patients on waiting list for Orthopaedic and Neurosurgical outpatient clinic
consultation” (AIMS Clinics Schedule) these clinics would predominantly only
see new patients; and
B. regular treatment clinics that would be providing ongoing support and would
have a very high proportion of review patients.
4 Note, the statistics for the ‘Other Allied Health’ category 609 have not been included because the variation within this category is too great rendering a mean or median figure somewhat irrelevant.
H u m a n C a p i t a l A l l i a n c e
24
The survey data does not allow realistic examination and validation of this position; however the significant range in new to review patient ratios for some allied health codes noted in Table 3.1 suggests this might be a possibility. Selected VACS code areas of
activity taken from the AIMS data, suggest that the bulk of health services have only one clinic per allied health VACS code.
Clearly though, some health services, mostly the teaching hospitals, have greater
differentiation of clinic type within selected allied health areas, and have some genuinely specialist clinics. Examples, again using descriptions extracted from the AIMS Clinic Schedule, of such clinics are:
Orthopaedic Education Clinic - Limb Review Clinic - Education (OREDCL) This
clinic provides pre-operative education to every elective limb reconstruction patient.
Each session lasts 2 - 3 hours and is conducted by nursing and allied health staff.
The purpose of the service is to improve pre-operative planning, increase patient
knowledge of the procedure and facilitate timely discharge.
Orthopaedic Assessment Clinic (ORTALL) This clinic provides an assessment and
triaging service for new patients referred to the Orthopaedic Department's
outpatient clinics with lower acuity conditions who would otherwise wait an
indefinite amount of time for a clinic appointment. The clinic is held five times per
week and is serviced predominantly by an orthopaedic physiotherapist however
there is some level of orthopaedic registrar involvement.
Clinical Nutrition (456C) For clients with a number of complex metabolic
problems. Each week there is a different focus such as eating disorders, body
composition, osteoporosis and nutritional support. Clients are seen by
endocrinologists, clinical nutrition physician, dietician a nurse and psychologist.
Generally, the pattern in new to review patient ratios reflects the number of times
patients are called back for review or to maintain their treatment process (see Figure 3.1 below). In most cases, review patients need to be discharged before new patients can be accepted.
Figure 3.1: Average the number of reviews per patient within the 601-611 VACS
codes
Source: Survey of health services * One outlier value removed from the analysis since it was distorting the figures
The issue of poor discharge rates has been a concern for many years (for instance see
the Aspex Consulting report, 2005), especially from those clinics that provide more
H u m a n C a p i t a l A l l i a n c e
25
routine treatment to patients with chronic illness or which provide a service to the more general patient population.
There is a strong consensus that a better patient throughput could be achieved. The survey results showed that health services could identify a number of opportunities to shift the patient workload (of existing review patients) to alternative service providers. Respondents estimated that between 3% and 90% of current patient consultations,
depending on the VACS area of activity could in theory be provided by alternative sectors of the health system (especially primary health care providers and community health). Overall, an estimated average of at least 20% or one fifth of current patient
consultations are believed by outpatient service providers to be able to be moved to alternative care settings. The proportion of outpatient consultations that participants thought could be offered in alternative settings by VACS code is shown in Table 3.2 below.
Table 3.2: Potential for moving current patient load to alternative care settings
VACS descriptor Range of clinic opinions on % of current
consultations that could be offered by
alternate providers
Audiology (601) 3 – 30%
Nutrition (602) 5 – 50%
Optometry (603) 0 – 40%
Occupational Therapy (604) 0 – 30%
Physiotherapy (605) 5 – 90%
Podiatry(606) 10 – 30%
Speech Pathology (607) 10 – 80%
Social Work(608) 10 – 20%
Cardiac Rehabilitation (610) 5%
Hydrotherapy(611) 15 – 20%
Source: Survey of health services
If there is so much potential for improvement in patient throughput the obvious question is why is greater referral to alternative settings (sub-acute and community) not
happening? Why is discharge of patients being delayed?
Some health services stakeholders consulted argued that some reluctance to discharge could be attributed to the attitude of certain outpatient service providers. Hesitation on
the part of the hospital-based services to refer to community service settings could be due to concern that some patients would experience an inferior service. This is reflected in the observations of one health service interview subject, who noted:
“There is an insufficient critical mass of appropriate expertise available in
community settings particularly for patients requiring specialised management for
acute conditions.”
Of course, there are times when this reason for non referral is appropriate; there are clearly a range of services delivered through outpatients clinics that are sufficiently specialised that they cannot feasibly be delivered in more generalist community services.
Such services include those that target complex or rare conditions requiring high levels of practitioner expertise, specialised equipment and / or immediate access to diagnostic support facilities. For allied health clinics, close access to specialist medical practitioner consultation can also be a factor.
H u m a n C a p i t a l A l l i a n c e
26
Some of the examples provided by health services in the survey responses that would satisfy these conditions were:
� most patients require review and maintenance of their prosthetic or orthotic device for a long period of time. Once the device needs to be replaced or their condition changes a new prosthesis or orthosis may need to be provided.
Therefore the majority of these patients will require long term service provision;
� if the patient is not stable from a wound management perspective and requires multidisciplinary specialist management. Patient may be discharged after a
single visit. Wounds with a longer healing time will be assessed at six weeks and if not healed then ten weeks;
� UV light therapy equipments costs for purchasing UV light machine are prohibitive for the community. Discharged upon completion of treatment; and
� because of chronic complications a prostatectomy for benign hypertrophy is only done when the patient’s urine stream is at a certain decreased level. A single visit may be all that is necessary, but many visits may be required if the
appropriate conditions for the procedure are not satisfied. Separating out legitimate reasons for retaining patients in the outpatient clinic
environment from less valid ‘attitude-based’ concerns about the quality of community services is not easy. It is further complicated because at times, the result of staff and other limitations, the quality of community services is compromised. Some evidence of this cited in the survey responses were:
� Long waiting lists at community services because of a paucity of appropriate allied health or nursing resources. These waiting lists could require a discharged
patient to potentially have a significant ‘gap’ in service continuity with likely poor health outcomes. One health service interview subject consulted noted:
“... there is a three month and longer waiting list to access community
services [in my area] due to the insufficient number of specialist services
available, a situation that is further complicated by low staff retention due
to feelings of isolation and lack of support.”
� A corollary of long waiting lists is tight admissions criteria. Several clinic stakeholders consulted complained that attempts to discharge to an alternative service in the community are often blocked by the tight criteria set down by the service provider for admission.
� The cost of alternative services to the patient is also perceived as a main barrier
to discharge from VACS clinics. The outpatient clinic population is typically drawn from the lower socioeconomic levels of the community and these patients need access to bulk billing services. Outpatient clinic stakeholders argue in such cases
discharge needs to be facilitated by the service as patients are unable to navigate the system without help. In some cases, for instance especially in rural regions, discharge to community services will require a significant co-payment on the part of the patient, which is often likely to lead to a cessation of
treatment altogether. As one health service interview subject observed:
“There is a lack of funding for public patients to access private services. For
example EPC [enhanced primary care Medicare Item numbers] funded
under Medicare does not cover acute conditions and five visits for all allied
health per year does not meet the needs of patients with chronic
conditions.”
H u m a n C a p i t a l A l l i a n c e
27
Sometimes it is clear that patients, as consumers of the health care system, prefer to access their services from specialist outpatient clinics, and this has nothing to do with cost but rather a perception of quality. They perceive the human resources, equipment
and facilities at an acute care centre to be superior to those they might obtain closer to where they live.
Possible ways forward
The Victorian Public Hospital Specialists Clinics Strategic Framework (2009) strongly advocates providing health care in the setting that best matches patient needs:
“To ensure people receive care in the most effective setting and ensure timely
access, comprehensive protocols should be in place for triage, assessment and
discharge of patients, and patients should be discharged to community-based
settings when clinically appropriate, or where there is capacity for a primary or
community provider to more appropriately provide care” (p. 9)
While the use of protocols is important, these must be sensitive to the needs of different
patient groups. There are some patients who will need to be retained by the outpatient clinic because it has the most appropriate resources to manage their care. Measures designed to influence or improve the rate of discharge from allied health outpatient
clinics must ensure that they do not encourage inappropriate discharge of these patients or other patients for whom there are no realistic referral options available in the short-term. Rather, the objective should be to facilitate appropriate discharge of patients who no longer need hospital-based care and who are being retained for reasons such as
patient or clinician preference. The options open to influence change fall into two broad categories:
� funding system changes; and
� educational or administrative changes.
Funding system changes
Qualitative data collected through the consultation process for this Review, along with opinion from past reviews (e.g. HMA, 2006), does not suggest the design of the funding
arrangements particularly affects the behaviour of clinics at the operational level. Rather the more common view is that behaviour is generally historically underpinned (that is clinics do what they have always done) and motivated in the best interests of the patient or at least in maintaining some degree of service delivery status quo. This is testimony of
the sort of willingness, at least based on anecdotal and self-reported survey evidence, of outpatient clinics to put the interests of patients above financial considerations. Nevertheless, this report supports the view that while an imperfect relationship exists
between financial signals and service behaviour, some influence does still prevail. All other funding models, including case mix models for inpatient services, have been designed for and are considered to contribute to influencing clinical practice and
administration. Why should funding of outpatient services be different? Accordingly, a number of changes to the VACS funding arrangements are considered. The idea of creating a separate payment schedule for ‘new’ and ‘review’ occasions
of service is not new. To incentivise an increase in the willingness of clinics to take on more new patients (and by implication discharge review patients earlier), the payment for ‘new’ patient occasions of service would naturally be larger than for review patients.
H u m a n C a p i t a l A l l i a n c e
28
A larger payment they hypothesised could be supported on cost and clinical grounds, since it was (and according to our consultations still is) widely considered that new patient consultations take longer and generally require more higher order assessment
and diagnosis competencies.
They also mooted a separate VACS payment for a successful discharge, again higher than would be the case for an ordinary allied health occasion of service. This approach
would be to incentivise the discharge process rather than as above, incentivise the taking on of new patients. A related approach would be to provide a disincentive to keep review patients by progressively discounting the payment made for review patient
occasions of service, essentially making each successive review occasion of service more of a revenue loss. Alternatively an arbitrary cap on the number of funded visits could be applied, and after reaching the cap the VACS payment reduces to zero (or at least the clinic is requested to justify retaining a patient beyond what is considered to be acceptable practice).
An alternative to trying to incentivise earlier discharge, or at least de-incentivise delayed
discharge, would be to provide funding support to the discharge process itself. A separate payment for ‘discharge’ activity might be provided which would cover the cost of a conferencing clinic (possibly in the absence of the patient), the development of a care plan and administration of the referral to an appropriate alternative service. If there were
a moderate incentive to refer patients and this was buttressed by funding support for a considered discharge process or plan, then higher levels of appropriate discharge might be achieved.
A final option would be to bundle up a number of occasions of service for a particular patient and fund a single ‘episode’ of treatment associated with a coherent patient
diagnosis5. In this option, the funding arrangement would provide a ‘lump sum’ payment along the lines of a WEIS payment for a particular DRG related inpatient service. This
approach effectively caps total payment encouraging discharge when costs begin to drag on (with diminishing reimbursement outcomes). However, if the cost weights for an episode are developed reasonably, the impact on behaviour should be more subtle than with the blunter discharge incentives noted above which would still have unweighted
occasion of service payments associated with a real or de facto capping mechanism. The problem though with this approach is that there could be difficulties collecting the degree of linked patient level data to be able develop the ‘price’ estimates and subsequently to
fund the model.
For different reasons, none of the above suggested changes to the current VACS funding arrangements are entirely satisfactory. Indeed, according to the Aspex Consulting report,
all changes aimed at influencing discharge behaviour run the risk of encouraging inappropriate discharge.
The suggestion that shows most promise though is one based on a revised payment structure for ‘new’ and ‘review’ patients. Of course proper costing of the ‘new’ versus ‘review’ patient population occasions of service would need to be undertaken, but it seems counter-intuitive that review occasions of service could be more costly on average
than new patient occasions of service unless the first visit is not when a thorough assessment, triage and treatment plan is undertaken — a situation that may pertain in
some clinics and health services6. While detractors of this suggestion will note the
5 This would require a definition of the episode based on pathways and can’t be substantiated without good patient level data 6 This is most likely to be the case in some medical and surgical clinics where patients are referred, especially from general practitioners, for specialist consultation but without the necessary ‘work up’ of required pathology and medical imaging tests. In such cases the ‘new’ or initial occasion of service may simply be to order requisite tests, and the follow up or second visit is when the true assessment, diagnosis and treatment plan development occurs. This circumstance is less likely to present in allied health clinics.
H u m a n C a p i t a l A l l i a n c e
29
absence of comprehensive quality patient level reporting across the health services, our own survey efforts were able to elicit data on this issue from health services. Of course, as with all survey data, it can be subjective and difficult to validate. There appears to be
no reason intrinsically though why this minimum amount of data could not be collected and provided regularly and at only a limited ‘compliance’ cost to health services and individual clinics.
Indeed the Victorian Public Hospital Specialist Clinics Strategic Framework (2009) notes the importance of reporting linked patient level data as a key reform agenda item for the purposes of sustainability and efficiency of the outpatient system. The Framework
document cites the National Health and Hospitals Reform Commission (2008) to identify several benefits of improved patient level data including to support continuum of patient care and to utilise health care services more optimally. The Framework describes preparation for state-wide rollout of a minimum data set the Victorian Integrated Non-
Admitted Health (VINAH) Minimum Dataset (MDS).
VINAH has been developed to incorporate the Community Rehabilitation Centre Minimum Dataset, the Specialist Clinics (outpatient) Minimum Dataset and HARP into a single
dataset. The new dataset is designed to enable the Department to meet its State and Commonwealth accountability obligations under the Commonwealth – State Agreement, and provide important data to inform service planning. The VINAH MDS has still not completed its definitions in the area of outpatient services. However, it is clear that data
on episode (or occasion of service) start date (and end date for that matter) will be part of the MDS along with other potentially useful related data such as health condition, plan of treatment and referral destination.
Recommendation 1:
� To require all VACS funded health services to collect and report data on ‘new’
and ‘review’ patients at each clinic from financial year 2010/11.
� To complete data definitions for the outpatient component of VINAH in respect to patient status (‘new’ or ‘review’, probably by using episode start and other date comparisons).
� To introduce a differential VACS payment in financial year 2011 /12 for ‘new’ and ‘review’ patient occasions of service which favours ‘new’ patient services, where ‘new’ is defined as the occasion when an assessment and treatment
plan is developed.
Non funding system approaches
Change to the VACS payment arrangements is a potentially blunt instrument when seeking to influence health services’ behaviour and comparatively quite a ‘radical’ step. A more conservative approach is to try to influence allied health clinic behaviour through a range of information provision, education and consulting type interventions.
First, it is important to remove or at least significantly reduce the level of variation between health services (within areas of VACS code activity and too for specific types of patient presentations) in approaches to care for essentially the same types of service
requirement. Clinicians value their independence and the capacity to make autonomous clinical judgements based on the ‘unique’ circumstances of each patient presentation. Yet clearly patient populations can be grouped into relatively homogenous categories, and
equally clearly there will be more optimal and efficient ways of addressing these group needs.
H u m a n C a p i t a l A l l i a n c e
30
As the Sano Report (SANO Consulting, 2008) notes: “There is currently significant variation in provision of outpatient services across
Victoria’s public hospital outpatient services... [there is a] … need for development
of evidenced care pathways to support optimal and consistent protocols for patient
management in outpatient services. Literature both nationally and internationally
supports the view that evidence based care pathways are being increasingly utilised
to support standardisation and integration across the continuum of care.
Standardised care pathways have been shown to improve the patient’s experience
and health outcomes by facilitating timely and effective patient care.” (p. 4)
A key expectation within the Victorian Public Hospital Specialist Clinics Strategic Framework is that health services will develop and implement ‘patient journey standards’. These derive from a significant body of work undertaken in the United Kingdom (Laitner and Normanton, 2007) and attempt to ensure the patient’s journey through any part of the health system (outpatient services in this case) is managed in the most timely, efficient and effective manner. Standards encompass the entire journey,
from referral to discharge. It is almost certain that patient journey standards will be included as performance benchmarks in future Australian Health Care Agreements for outpatient services delivery.
Initial work in this area to develop a generic ‘Outpatient Care Pathway Template’ has been focused on high volume medical / surgical specialist clinic areas (urology, orthopaedics, maternity, ophthalmology and colonoscopy) some of which have significant multidisciplinary (allied health and nursing) input. There remains a gap though between
this development and more specific and appropriate standards to guide and inform specific types of clinic work.
An increased layer of detail is required that equates to protocol based care, and again is advocated by the Specialist Clinics Strategic Framework and is alternatively termed clinical practice guidelines or care pathways. Discharge protocols, although only one part of the patient journey, could be given development priority.
A generic discharge protocol could be developed in the interim that would apply in most circumstances where community-based service alternatives should be possible. In
Queensland for instance a general protocol which mirrors that within the Medical Benefits Schedule, has been put in place to limit the longevity of a referral from a GP to outpatient clinics to 12 months (Duckett, 2007), after which the patient must return for another referral. While most referrals from general practitioners are likely to be directed
to medical and surgical clinics, many of these will increasingly be seen first in pre-appointment specialist allied health clinics or anyway end up as long review / treatment ‘tails’ in allied health VACS clinics. Even if there are limited resources in the community to which the GP can subsequently refer (probably therefore leading to a re-referral back
to outpatients), seeking the GP to consider the options would still be good practice.
Such practice is also in line with allied health services funded by the Commonwealth
under the Enhanced Primary Care (EPC) Program for allied health services (Medicare Benefit Item numbers 10950 – 10970) or under Better Access for mental health services. In both cases the number of occasions of service funded from a single referral is capped and the longevity of the referral is limited to 12 months following the completion of a GP
Management Plan (Item 721 or 725). Given the possibility of future Commonwealth / State funding directions, it is feasible that a referral from a GP for allied health services using one of the above items could be to an outpatient clinic service, particularly in rural areas where private practice resources are scarce and the hospital represents the best prospect of developing and retaining a stable allied health workforce.
H u m a n C a p i t a l A l l i a n c e
31
Recommendation 19:
� To develop guidelines that limit the number of allied health occasions of
service for any one patient for all patients referred to outpatient specialist services from a general practitioner. The rules pertaining in the primary care setting under Medicare funding arrangements could easily be copied. These
guidelines would place limits on the maximum number of occasions of service but not preclude earlier discharge. After reaching the limit a further referral must be sought from the general practitioner.
� To develop guidelines for all other types of patient journey (for instance those
from inpatient care) that limit the number of initial patient occasions of service to an agreed and appropriate number based on available evidence. Continued treatment beyond this limit would be contingent on gaining a
general practitioner (or specialist) referral.
� To develop and formally establish service entry protocols will not allow acceptance of referrals (and VACS payments not be honoured) unless the
approved patient journey pathway has been followed.
An additional approach might be to introduce stronger benchmarking practice. National Health and Hospitals Reform Commission (2008) advocates for a careful
selection of a (small number of) high-value performance indicators and benchmarks generally, and this advice would apply well in the Victorian outpatient services setting. Benchmarks for discharge performance that measure for instance the average number of
review occasions of service per patient or the ‘new’ to ‘review’ patient ratio are not that hard to implement; the data is possible to be collected both accurately and routinely. Queensland for instance has instituted several discharge benchmark measures.
Clinics that consistently vary from benchmark performance standards or averages (both poorer and better performing clinics) could be the subject of specific audits to verify performance levels, identify factors underpinning the performance levels, and in the case
of verified poor outcomes, initiate a process of change. Recommendation 3:
� Following the more universal implementation of data collection requirements,
to introduce a benchmarking ‘service’ that provided at least six monthly data at the individual clinic level on the ‘new’ to ‘review’ patient ratio and the average number of occasions of service of patients visiting each clinic on a
nominated ‘census’ week. The scope of this service will depend on the extent to which data collection is limited (for instance it may be constrained to review of Allied Health VACS Codes activity).
� To establish agreed sub-classes within the VACS classification system, to
allow meaningful comparison within and between health services. For instance, a distinction may need to be drawn between ‘specialist’ allied health clinics and the more routine ‘treatment’ type clinics.
� To publish benchmark results such that clinics can identify their performance within their health service and within same class clinic categories across all health services (for instance all hydrotherapy treatment clinics).
� To annually audit a selection of clinics that have below average indicators, initially through processes internal to health services but later through external processes if performance issues persist for more than 12 months.
It would seem appropriate for change to be facilitated by peer consultants, well regarded clinicians and managers from the same type of clinic (likely from another health service) who have proven that they can manage improved performance in rates of
H u m a n C a p i t a l A l l i a n c e
32
appropriate discharge7 and have the capacity to articulate these changes to their peers in other services. Such exchanges should not be left to informal information exchanges, but should be planned, centrally managed and separately funded. A consultancy episode might require several days research and consultation plus follow-up distance and face-to-
face support. The investment in this consultancy would provide a rich return on investment if only a small percentage shift in discharge rate was achieved; a targeted approach to the discharge rate at the Austin Hospital for instance reported by Aspex
Consulting yielded a 35% increase in the discharge rate and 22% increase in the ‘new’ patient proportion of total outpatient occasion of service.
Recommendation 4:
� To establish a budget to be administered by a relevant branch within the Department of Health that would support the operation of a ‘peer consultant’
workforce, that properly supported identifying the right consultants and administering arrangements for their consultancy activity with relevant clinics, and reimbursed health service employers sufficiently to ‘back fill’ temporary vacancies when peer consultants are engaged in consultancy activities.
Summary of recommended approach
A ‘package’ of measures designed to influence change is usually more effective than a
single intervention in achieving desired outcomes. The package needs to be implemented jointly with a program in community-based health services designed to increase service capacity. We would recommend a package of funding, administrative and educational
measures that drive clinics towards the right broad direction, put parameters around the direction they should be taking, helps them self-assess when they are not performing as they should (or allow a third party to make the same judgements), and help them to develop and implement clinic specific initiatives to achieve a better performance.
7 The ‘peer consultants’ also would be identified through the benchmarking process or through existing networking forums.
H u m a n C a p i t a l A l l i a n c e
33
Recommended Approach
An appropriate ‘package’ could therefore include the following interventions:
Step A Financial year
2009-2010
Develop data collection & reporting processes, get definitions right, prior to the commencement of the 2010-11 financial year.
Step(s) B & C
Financial year
2010-2011 (could happen at the same
time)
Introduce data collection & reporting processes. Development of a basic benchmarking system within
VACS health services allowing comparison of like clinics within health service categories, with at least two discharge performance indicators. Targeted audits would be undertaken of consistently poor performers.
Development of a generic discharge protocol that prohibited ongoing patient review beyond agreed limits
in the absence of a (re-)referral process generated by a community-based service provider. This will often be the patient’s GP, but might also include the community health service.
Step D Financial year
2010-2011 (later the
same year as steps B&C)
Creation of a separate fund within the Department to support an internal (to VACS funded health services) peer consultancy program for at least 3-5 years. The
cost of consultancy would largely be to backfill peer consultant positions when they are providing advice and support to their fellow clinic colleagues.
Step E Financial
year 2010-2011
Consider options for differentiating between funding for new and review OOS. Isolate clinic types where the difference is negligible. Undertake a trial application of
the new payment arrangements.
Step F Financial
year 2011-2012
Introduction of a differential VACS payment for ‘new’
and ‘review’ patient occasions of service which favours ‘new’ patient services, where ‘new’ is defined as the occasion when an assessment and treatment plan is developed. Some clinics will not be suitable for this type
of payment approach (e.g. hydrotherapy clinics, education clinics), so appropriate business rules will need to be developed and an appropriate cost weight differential established.
Step G Financial
year 2011-2012 (later the
same year as step E)
Consider introduction of a ‘discharge activity’ payment that supports a more active referral process from the outpatient environment to community care. One would hope over time this payment will be of diminishing necessity.
H u m a n C a p i t a l A l l i a n c e
34
4. Better use of allied health /
nursing skills
Background
There are increasingly articulate summaries emerging in the literature of the current deployment of allied health professionals and nurses into advanced practice activity within outpatient services and strong cases being proposed for further expanding the utilisation of allied health and nursing skills (e.g. Aitken, Faulkner, Bucknall & Parker, 2001; Laurant, Reeves, Hermens, Braspenning, Grol & Sibbald, 2004; McPherson, Kersten, George, Lattimer, Breton, Ellis, 2006; Kersten, McPherson, Lattimer, George, Breton & Ellis, 2007; School of Public Health, 2008; Centre for Allied Health Evidence
Review Team, 2008). This issue was also explored at length through the survey of health services and consultations with stakeholders.
The survey and stakeholder consultations revealed some confusion over the terms
‘advanced’, ‘enhanced’ and ‘extended’ practice. A simple taxonomy was introduced to ameliorate this confusion as follows:
‘Typical Activity’, used to describe the functions that are required to be
performed by health professionals working in a particular clinic service. This term takes into consideration the full scope of practice for which each health professional group is qualified to practice. The description of typical activity
includes practice from both ends of the scale of expertise, from a beginning level practitioner to an experienced specialist practitioner.
‘Advanced practice’ describes practice at the highest level of expertise within
the scope, inclusive of complex decision making and crisis management skills. Clinicians practicing at the advanced level are generally required to have undertaken appropriate specialty training.
In this taxonomy, ‘enhanced’ practice is considered as equivalent to advanced practice. Advanced practice, a subset essentially of the ‘typical’ practice universe, was important for advancing knowledge at the apex of practice.
‘Extended’ practice was determined to be potentially outside this universe. While closely aligned with advanced practice, the extended practice role integrates selected extensions of practice, such as initiation of diagnostics,
referral to medical specialists, admitting and discharge privileges, limited prescribing and approval of work certificates, all of which are outside the scope of ‘typical’ practice for most allied health and nursing professions. Even though
these ‘extensions’ often only constitute a small part of the overall function of an extended practitioner, they differentiate extended practice from other advanced clinical practice. Only a limited number of allied health clinicians are currently able to refer to medical specialists and have the authority to approve work
certificates, even less have prescribing rights. Nurse practitioners, in Victoria are recognised as engaging in extended practice, and this is acknowledged in the VACS funding arrangements which support medical practitioner substitution in obstetric clinics.
H u m a n C a p i t a l A l l i a n c e
35
The relationship between advanced and extended scope of practice is well illustrated in a broad descriptive taxonomy of new areas of practice being undertaken by
physiotherapists provided by Kerston et.al. (2007) summarised in Table 4.1 below.
Table 4.1: Example of physiotherapy advanced & extended practice
Intervention type
Example of physiotherapy advanced or
extended scope role
Non-invasive assessment
� Physiotherapists assessing (and managing) patients with mechanical low back pain, foot and shoulder disorders
� Physiotherapy extended scope practitioners in orthopaedic outpatient clinics assessing and diagnosing patients
Invasive assessment
� Physiotherapists referring patients for arthroscopy of the knee
Non-invasive treatment
� Physiotherapists managing paediatric rheumatology and orthopaedic patients
Invasive treatment
� Physiotherapists can inject, refer patient for
further investigations or list them for surgery
� Physiotherapists prescribe medication
Direct access to therapist rather than medical consultant service
� Physiotherapists forming part of the A&E triage team seeing patients as emergencies
� Initial assessment and management
undertaken by post-fellowship junior orthopaedic surgeons, or by specially trained physiotherapists working in an extended role
(orthopaedic physiotherapy specialists)
Source: Adapted from Kerston et al., (2007)
In Table 4.1 only the invasive treatment activities could be considered true examples of extended practice beyond the scope of accepted physiotherapy practice. All other areas of activity are within current scope of practice and especially notable because of the additional responsibility associated with more autonomous decision making and less or
no medical specialist supervision. Kersten et al., (2007) reported that non-invasive assessment (47%), followed by non-invasive treatment (37%) of patients were the most frequent types of practice undertaken in advanced practice physiotherapy settings. Invasive assessment and treatment were much less frequently reported.
Current situation
Putting aside unresolved issues about terminology, the current situation is characterised
by:
� significant variation between VACS code areas of activity and within codes
between health services in the types and levels of advanced practice undertaken by allied health professionals and nurses;
� an ad hoc (rather than strategic) approach to expansion of allied health activity
as allied health professionals or nurses (or both) have ‘drifted’ into new activities
H u m a n C a p i t a l A l l i a n c e
36
over time in response to immediate needs, generally to resolve a shortage of specialist medical practitioners8; and
� a clinician led expansion of roles both in allied health and nursing at a local level
based on the skill, knowledge, experience and expertise of the individual clinicians in response to immediate needs, such as patient demand and local contextual pressures.
Much of the initial expansion of advanced skills utilisation has been in the medical and surgical VACS code areas. Local workforce concerns about the availability of medical specialists, and a desire to increase career options for allied health and nursing as part of retention strategies, have been key drivers of change. In these code areas allied health and nursing labour is used increasingly as part of multidisciplinary team care in support of, in parallel with, or in partial substitution of one or more medical practitioner
specialists. In cases where the multidisciplinary care can be provided in ‘seriatim’ or parallel or in other ways as separate entities, separation into a distinct VACS code (600 to 611) is possible.
As noted earlier, much of what is often identified as ‘extended’ scope of practice is on closer analysis ‘advanced’ practice still within traditional scope of practice but possibly
operating in novel settings and often with greater practice independence. Some examples of current advanced practice identified through the survey of health services were:
� advanced scope physiotherapy that would historically have seen a medical specialist at an outpatient specialist clinic that can be carried out by enhanced
scope physiotherapists (Grade 4 Physiotherapists);
� diabetes management clinics (VACS code 602,606,609) run by credentialed diabetes nurse educators, dieticians, psychologists and podiatrists; and
� fibre optic endoscopic evaluation of the swallow (FEES) service (VACS code 607
Speech Pathology) - Speech Pathologists manage this service in conjunction with ENT support.
Importantly, introduction of ‘advanced’ practice generally requires few barriers to be overcome. These barriers normally consist of proving the competence exists to undertake the advanced practice work (this may or may not require credentialed evidence) and obtaining medical specialist support if advanced practice invokes performing work which was previously the exclusive domain of medical specialists. Proof of the above lies in the many examples of advanced practice able to be demonstrated from current VACS funded
services9. Still, in terms of the health professional resources devoted to delivering advanced activities as a proportion of total specialist allied health outpatient clinic
services, there is significant variation between the VACS code activities (see Figure 4.1 below).
In some areas of VACS activity the contribution of advanced practice to total activity is minor or nil (for example hydrotherapy, cardiac rehabilitation, audiology) while in some other areas of activity ‘advanced’ practice accounts for just under half of total activity (podiatry, speech pathology, physiotherapy). A conclusion from Figure 4.1 is that a
significant capacity exists to broaden the contribution of allied health and nursing advanced skills to total outpatient activity if the required resources (for instance appropriate competence) exist.
8 Some centrally supported efforts have tried to drive innovation in this area more strategically by supporting and promoting local initiatives or by helping initiate new projects (for example the ‘Better Skills Better Care’ Program), however these efforts have not yet achieved system wide outcomes. 9 The more pertinent question is why advanced practice has not been more uniformly adopted in relevant clinics across the health services.
H u m a n C a p i t a l A l l i a n c e
37
Figure 4.1: ‘Advanced’ or ‘enhanced’ practice as a proportion of total allied health outpatient activity
0
5
10
15
20
25
30
35
40
45
%
601 602 603 604 605 606 607 608
VACS Codes
Source: Survey of health services
Broad opportunities
An inventory of current advanced / extended practice can be identified either in existing VACS clinics (through the survey of health services) or in the literature (that is practiced in another part of Australia or more commonly overseas). The majority of roles currently
undertaken in VACS clinics would be classified as ‘advanced’ practice. In essence all of these advanced roles would be reclassified into extended scope if barriers to the supply, prescribing and administration of medicines were removed or if access to ordering and interpreting diagnostic techniques or injecting therapies were authorised. Table 4.2, on
page 34, highlights role-related opportunities for advanced / extended practice for selected allied health professions and nursing. It is acknowledged that some of these roles are currently performed in VACS clinics.
Table 4.2 underplays the complexity of the role responsibilities inherent in advanced/extended practice. Advanced/extended practice requires clinical expertise and the exercise of professional judgement that surpasses the scope of practice typical of graduate practitioners. A hallmark of advanced / extended practice is the ability to integrate complex diagnostic inputs and tasks into a seamless care package for the patient – exercising advanced clinical reasoning and investigative skills. Nevertheless, and confirming earlier comments in this Chapter of the report, the majority of
opportunities highlighted in Table 4.2 are consistent with the definition of the ‘advanced practice’ category.
H u m a n C a p i t a l A l l i a n c e
38
Table 4.2: Identified areas of opportunity for advanced / extended practice
Discipline / Areas of
practice
Advanced/Extended practice
Audiology � Counselling, fitting and management of BAHAs � Balance testing � Facial nerve testing � Specialised hearing testing
Physiotherapy
(Orthopaedic, emergency care, general trauma, rheumatology, cardio-respiratory, neurology,
burns care, women's health, and gerontology)
� First contact practitioners (embodied in private practice role)
� Assessment and management of new referrals � Psychosocial interventions to reduce symptom
chronicity and enduring disability � Continence/pelvic floor management
� Orthotic prescription, splinting, plastering � Parenteral medication administration/ injecting � Direct referral for surgery
� Applying complex clinical reasoning � Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path .
Occupational therapy
(emergency care,
Outpatients)
� Mobility and balance assessments � Removal of sutures � Fabrication of soft and dynamic splints
� Triaging patients for Hand Therapy. Treatment of more complex hand conditions
� Applying complex clinical reasoning
� Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path � Application of ultrasound � Triage and management of simple procedures (e.g.
Dupuytren’s release, carpal tunnel, digital fractures) � Neuro-developmental assessment
Speech pathology � FEES � Voice therapy using fibre optic video laryngeal
endoscopy � Assessing and recommending to other prescribers
� Advanced dysphagia management � Video fluoroscopy counselling � Stroboscopic Voice Analysis Clinic
� Head and neck surgery including management of oral cancer, swallowing, saliva & communication
� Objective assessment of swallowing disorders � Surgical Voice Restoration (SVR) management
� Use of EMG and neuromuscular electrical stimulation for treatment of facial weakness and dysphagia
� Supply or prescribe or administer (making use of Patient Specific Directives and Patient Group Directives)
� Laryngeal endoscopy / Nasendoscopy � Laryngectomy management including insertion of
voice prostheses following total laryngectomy and management of issues related to their use
H u m a n C a p i t a l A l l i a n c e
39
Table 4.2: Identified areas of opportunity for advanced / extended practice (cont.)
Discipline / Areas of
practice
Advanced/Extended practice
� Management of tracheostomised +/- ventilator dependent patients with regards to swallowing and communication
� Applying complex clinical reasoning � Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path
Nutrition / dietetics
(Gastroenterology,
nephrology)
� Management of eating disorders and PEG � Assessment and treatment including enteral feeding,
education, close monitoring of nutritional status � Manage community-based patients with Stage III
kidney disease � Remove percutaneous and endoscopic gastrostomy
tubes
� Treatment of metabolic disease (inborn errors of metabolism) where diet is the principal therapeutic intervention
� Nasogastric tube insertions and the management of
initiation and conclusion of parenteral nutrition � Supply or prescribe or administer (making use of
Patient Specific Directives and Patient Group
Directives) � Applying complex clinical reasoning � Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path
Podiatry
(Orthopaedic)
� Collaborative clinic caseload reviews between podiatry and orthopaedic surgeons
� Application of total contact casts
� Sharp debridement of extensive foot ulcers � Neurovascular assessment � Pressure offloading � Surgical procedures
� Supply or prescribe or administer (making use of Patient Specific Directives and Patient Group Directives)
� Applying complex clinical reasoning � Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path
Nurse practitioner � Referral to medical specialists � Initiation of diagnostics � Interpretation of diagnostic findings � Admitting and discharge privileges
� Treatment planning & implementation � Limited prescribing � Approval of work certificates
H u m a n C a p i t a l A l l i a n c e
40
Table 4.2: Identified areas of opportunity for advanced / extended practice (cont.)
Discipline / Areas of
practice
Advanced/Extended practice
Advanced practice
nursing May be Division 1 or in
some incidences Division 2 (cardiology, respiratory, Gastroenterology,
radiotherapy / oncology, Ophthalmology, Diabetes, Urology,
Haematology)
� Triage assessment / diagnostic work-up / specialist referrals
� Wound checks & debridement - diagnostics (radiology
and pathology) � Management of chronic leg wounds � Insulin dosage adjustment, insulin pumps, initiation &
titration
� Stomal Therapy - stoma care � Pre-op counselling / Information, reassurance and
support
� Nurse-led on-treatment review / Surveillance for recurrent symptoms
� Pre-operative cataract assessment and post-operative care clinic
� Fitting of temporary prosthetics � Bone & Soft Tissue -complex treatment plans � Gastro-Intestinal Nurse –complex treatment plans
� Education, assessment, consultations and follow-up � BCG Therapy for Bladder Cancer �
Diabetes educators
(e.g. nurse
practitioners, specialist
nurses [Div 1 or Div 2],
dieticians)
� Referral to specialist care � Applying complex clinical reasoning � Interpreting multiple clinical diagnostic inputs � Utilise diagnostic tests to plan care path � Supply or prescribe or administer (making use of
Patient Specific Directives and Patient Group Directives)
Social work � Complex bereavement training � Child protection training
Source: Survey of health services
Priority opportunities
A broader analysis of the more fertile opportunities for expanding advanced practice identifies three major areas where nursing and allied health professions can work at the apex of typical practice, possibly within a guideline framework in dedicated allied health or nurse-led clinic services. These are all areas of service delivery which are recognised
as current concerns. The areas, all within the VACS funded outpatient services arrangements, are:
� Pre-appointment in specialist clinics
� Preparing patients for outpatient treatment
� Pre-specialist surgical admission clinics
These are discussed briefly below.
H u m a n C a p i t a l A l l i a n c e
41
Pre-appointment in specialist clinics is when a traditional patient journey involving a referral to a specialist medical practitioner has an initial prior visit to an allied health professional or nurse. There are problems with a traditional consultant-focused model
of care that might be overcome with pre-appointment clinics. A good current example of this type of opportunity for using advanced practitioners is the Osteoarthritis Hip and Knee Service (OAHKS) and the Orthopaedic Waiting List
(OWL) programs, both of which use an initial assessment by an advanced practitioner physiotherapist to triage patients into specialist referral or more conservative management treatment streams. In addition to benefits obtained from reducing the
patient workload on medical specialists, comprehensive pre - specialist consultation work-up managed by specialist nurses or allied health professionals makes any ultimate appointment with the specialist more productive. The comparatively common need for a second appointment with the medical consultant because all the necessary diagnostic information is not available at the time of the first visit is negated. The diagnostic process and time required to first treatment is thus more efficient (so long as the resources for the triage process itself do not become a limiting factor and
create their own waiting lists). It is important to note a significant number of patients are effectively managed through this process and the interventions initiated mean they do not proceed to specialist medical clinics. Specialist clinics would include but are not limited to;
� Neurology (physiotherapist);
� Orthopaedic (nurse / physiotherapist);
� Cardiac (nurse / physiotherapist);
� Respiratory (nurse / physiotherapist);
� Oncology (nurse);
� Renal (nurse / dietician);
� Gastroenterology (nurse / dietician);
� Endocrine (nurse);
� Urology/Haematuria (nurse)
Another model could look at the development of pathways for specific conditions. In the UK there is an ICT solution called “Map of Medicine” which is utilised at the point of referral to ensure that appropriate clinical pathways including the availability of
relevant clinical investigations have been followed before a specialist appointment is allocated. Preparation for treatment is particularly pertinent when a patient, generally with a
chronic illness, has been referred for a potentially long course of treatment. More generally the Victorian Public Hospital Specialist Clinics Strategic Framework (2009) emphasises the importance of the concept of ‘patient-centred care’. They note that patient-centred approaches have been shown to increase patient satisfaction and
engagement, and as a consequence improve health outcomes. They argue:
“Informed patient choice is integral to patient-centred care increasingly the
community wishes to have involvement and influence over their health, including
decision making and management of their conditions.” (p. 11)
Situations that most require the provision of comprehensive information to patients
prior to engaging in treatment and ongoing through the treatment management phase would be in areas such as:
� Chemotherapy (specialist nurse)
� Radiotherapy (specialist nurse)
H u m a n C a p i t a l A l l i a n c e
42
� Renal dialysis (specialist nurse)
� Cardiac rehabilitation (specialist nurse / physiotherapist)
� Endoscopic (specialist nurse)
� Endocrine (specialist nurse)
� Respiratory (Specialist nurse/ physiotherapist)
� Diabetes (specialist nurse / dietician) These requirements are time consuming and once the treatment plan has been
determined do not need to be undertaken by medical staff. Depending on the degree of complexity of the consultations the role of specialist nurse could be undertaken by Division 1 or Division 2 nurses. A relevant example of this would be the role of practice nurses in General Practice, where nurses for both divisions undertake consultative roles with patients with chronic conditions. Pre-specialist surgical admission clinics. Comprehensive pre-operative work-up is
required for the majority of elective specialty surgical cases pre-hospitalisation to reduce the cost of hospitalisation while the necessary investigations are completed. Pre-admission clinics have contributed to the significant fall in average length of stay
experienced in all Australian public hospitals over the last few decades. Required investigations generally include pathology laboratory tests, a range of medical imaging procedures and cardiac function tests. The ‘work-up’ process also typically includes information and education about the preparation required for the day of surgery,
length of stay and post-operative expectations. Surgical pre-admission clinics are currently funded under a separate VACS code (209) and they account for approximately 17% of total VACS funding of weighted surgical activity (based on 2007/08 AIMS data).
Specialist nurses working at the apex of typical practice within a protocol based framework would be able to manage pre-admission nurse-led clinics efficiently. Areas
would include preparation for:
� All forms of cardiac surgery
� Surgery to remove cancerous tumours
� Orthopaedic surgery
� Urology
� Gynaecology
The three area's described above all essentially function within a multidisciplinary team
model (and would therefore be categorised currently within a medical or surgical VACS
clinic)10, where all members of the team are used to the fullest efficiency and respected for the skill set that they bring to the service.
We contend an appropriate model needs to be established which accepts allied health
professionals and nurses as potentially making up a multidisciplinary team with a medical specialist being available but not necessarily integral. Thus the model could include specialist allied health-led and nurse-led clinics into which patients are referred for
continuing treatment by the medical specialist as part of the treatment plan. These clinics could be offered from primary care locations within the community with efficient communication processes across the team for example regular team meetings or case management conferences.
10 The pre-surgical admission clinics could be conducted as a nurse-led clinic presumably with medical specialists (at least registrars) on call.
H u m a n C a p i t a l A l l i a n c e
43
Interestingly also, the three areas of opportunity to expand deployment of advanced allied health and nursing practitioners can all be accomplished without recourse to extended practice options. In particular, the use of protocol driven assessments,
investigations were conducted. The degree of complexity of each pre-specialist surgical admission clinic would dictate the appropriate clinician involvement. In some cases, the pre-specialist surgical admission clinic might be more efficient if led by a nurse practitioner, in others there may be a requirement for an anaesthetist and in others a
specialist nurse or allied health clinician. From a funding perspective though a precedent has been set that midwives are able to claim the medical VACS for their antenatal clinics when they are a substitute for doctors. Similar circumstances prevail in clinics with a
nurse practitioner. This sets the ‘price’ of such clinics therefore quite high and potentially reduces the incentive to substitute if a medical practitioner is just as available.
Possible ways forward
There are good reasons to enhance the role of allied health and nursing practitioners into a broader range of outpatient services by deploying more of their advanced competencies:
From a service provision perspective, although sufficient evidence has yet been gathered to develop a sufficiently strong case (for or against), intuitively one would expect a positive cost/benefit outcome from increased deployment of advanced allied
health and / or nursing skills11. This of course will depend on the results of such deployment; and the degree to which other forms of labour (possibly more costly) are
able to be used more effectively and efficiently. This in turn will depend on the actual allied health and nursing workforce competence levels (sufficient to deliver expected levels of care), the availability of labour, and labour cost relativities remaining
favourable (an issue to be discussed below).
From a patient perspective increased use of advanced practice allied health and nursing labour should enhance the patient journey experience by delivering reduced
waiting times, more personalised and patient-centred attention and potentially more convenient and accessible service locations and settings. Available evidence suggests there is no decrease in quality or safety of service through greater use of advanced
allied health and nurse practitioners, even when this results in substitution for medical specialists, if practice is confined within agreed protocols.
Finally, from a practitioner perspective, there are potentially valuable workforce
capacity building and human resource management ‘by-products’. Advanced practice can slow down the leakage from many health professions by addressing factors such as lack of career opportunities, under utilised skill sets and not being respected as a professional. The cost of attracting and inducting new staff is huge, not only in direct
costs but also loss of health service provision. Second, advanced nurse and allied health practitioners are well suited to be a crucial part in inter-professional practice in a client-centred health care system (e.g., as in the UK via managed clinical networks).
Recommendation 5:
� To implement within the next two years advanced practice service models that optimally utilise higher order skills of nurses and allied health professionals.
11 Of course if the VACS funds the advanced practice at the medical rates, for instance if a nurse practitioner is deployed given the obstetric VACS precedent, it would be harder to demonstrate a cost benefit.
H u m a n C a p i t a l A l l i a n c e
44
Funding system changes
In discussing how opportunities for advanced practice could be better and more
vigorously pursued we can look first at possible changes to the VACS funding model, all of which have already been mooted in past reviews:
� The way targets are currently set separately for medical / surgical and
allied health In 2009/10 funding caps were set separately for VACS medical
/ surgical weighted encounters and allied health occasions of service at each health service. On average the proportion of allied health occasions of service funded was approximately 30% of total occasions and service encounters. The
Aspex Consulting (2008) report recommended that the funding cap arrangement be changed and, while maintaining an overall target figure, a single target for all outpatient activity at a health service be established. They argued that the
current arrangement:
“... has the disadvantage of discouraging service substitution and/or diversion
between medical and allied health categories in some instances. For example,
it may prevent the greater use of allied health clinics and encourage medical
clinics to maximise funding where the targets are misaligned with the
direction of clinical practice changes that the hospital is seeking and/or the
policy direction of DHS. Therefore, the two-target approach may have
perverse incentives.” (p. 98)
We are not sure that moving towards a single target for each health service
would necessarily impact on advanced allied health practice positively. In theory the increased flexibility would allow freer flow of activity between VACS codes, and thus more support for innovation (or at least fewer barriers to suggested changes). A new allied health clinic could be mooted for instance and supported
(after approval). Or advanced allied health skills could be incorporated as an additional pathway within a medical VACS clinic and some of the ‘target’ total shared more generously with this clinic. Just how a single versus the old two way
target approach would affect deployment of advanced allied health practitioners though is unknown. If the Department therefore, wishes to reduce the uncertainty of ‘market’ like effects, it could be more prescriptive and allocate a specific activity target to any newly approved model.
Recommendation 6:
� To allocate separate occasions of service targets for advanced practice clinics
newly approved by the Clinical Panel which the Panel itself could determine (or approve on application). The target approval would apply for two financial years only, after which it would need to be supported through an allocation from the total target amount.
� The introduction of cost weights for allied health VACS clinics — in 08/09 all
allied health clinic occasions of service (601 to 611) attract a single payment of $59. A flat payment is known to be low for some types of service and high for several others but the assumption is that on average the payment will be
appropriate. It appears to be calculated on the basis of funding a reasonable rate of pay for the average duration of an occasion of service. It was noted in consultations that the payment equates to employing a practitioner for $130,000 per year (including on costs).
H u m a n C a p i t a l A l l i a n c e
45
A flat payment structure for allied health services contrasts with the output based payment for weighted medical and surgical VACS activity. The justification for this has been that no acceptable classification structure for allied health
services has been developed and a paucity of patient level data on allied health encounters undermines an ability to construct valid cost weights.
Nevertheless the Aspex Consulting (2008) review recommended adoption of
weighted payments and noted: “As a sound funding principle, allied health categories should be weighted, and
funds should be provided on the basis of weighted encounters in the same way
as medical categories.” (p. 97)
Aspex Consulting argued that the relative weights for allied health activity should be developed across all VACS categories (this would have the immediate advantage of not requiring a separate base rate) on the basis that the allied health contribution was part of the same patient journey. More importantly for
this review they contended that this was important so as not to compromise a viable substitution and diversion approach which would be the case if true cost relativities were not maintained. Based on calculations from data they had collected during the study, they estimated allied health cost weights would range
from 0.2 to 0.6 of the standard VACS weight. This would provide for a payment variation of approximately between $35 and $104 per occasion of service. A ‘break even’ weight for the current flat fee would be 0.34.
At (perceived) properly weighted payments for occasions of service, health services and clinics are more likely to pursue deployment of advanced allied health and nurse labour clinic options.
The search for valid and efficient cost weightings could be facilitated by consideration of different levels of service within VACS codes, for instance by differentiating between ‘specialist’ and routine ‘treatment’ clinics.
Recommendation 7:
� To renew efforts to find appropriate cost weightings for allied health clinics. Most likely this research work will need to be done collaboratively at a national level and therefore borrow concepts from existing funding models
(for instance in South Australia) and be undertaken through Council of Australian Government (COAG) arrangements.
� Introduction of multidisciplinary clinic VACS code and payment — currently medical and surgical VACS weighted payments allow for a certain degree of contribution from allied health and nursing professionals into the completion of the encounter. Most services consulted during this review expressed the view, that the allied health contribution to medical and surgical VACS clinics was undervalued. Some were not even aware that allied health costs were taken into account in determining the weights. Given that they also observed that the
introduction of nurse and allied health labour into a multidisciplinary team environment could improve the efficiency and effectiveness of medical specialist labour use but rarely reduced the actual cost (due to indivisibilities of labour or
simply an increase in cleared service demand), then adding allied health labour to a medical VACS clinic might only be perceived as an additional cost.
H u m a n C a p i t a l A l l i a n c e
46
The introduction of multidisciplinary clinic VACS codes and payments might more explicitly recognise the different team contributions in overt payment arrangements. This could have the effect of encouraging more advanced allied
health contribution to multidisciplinary team efforts. The implementation of MDC VACS codes will require the differentiation of the allied health input already included in the medical and surgical VACS encounter weights.
Recommendation 8:
� To examine the examination a multidisciplinary clinic code and payment where allied health contributes to a medically driven clinic.
� To investigate a new VACS code that covers multidisciplinary care provided only by allied health practitioners and nurses in the absence of any medical practitioner input.
Non funding system approaches
A range of factors that act as enabling influences for, or barriers to, change processes
were identified through the literature and consultations. The most important factors vital to the success of change in practice (to advanced or extended practice options) appeared to be:
� (Relevant) medical specialist support;
� A clear role definition;
� Strategies to ensure rigorous establishment and evaluation of clinical competencies as part of a wider risk management plan; and
� Separate and independent health service governance structures in Victoria12. Additional non funding encouragement could therefore be provided through several other initiatives including:
� Active promotion of examples of advanced practice that have recognised worth, where a reasonable (even if not complete) evidence base has been established through evaluation or other forms of evidence, can be undertaken. The
target for these promotional activities should be those examples that fit within the three broad areas of practice noted above, have only been introduced at a few services, and have a strong case that can already be made for their promotion. The
success of the OAHKS model has lead to its implementation in many health services. A more concerted promotional effort to support the dissemination of other ‘good bet’ examples of advanced practice or even more speculative examples of practice could achieve much faster rates of innovation expansion. The Department
can, and should, exert more pressure on dissemination reducing the level of discretion afforded to health services to adopt new practice.
To facilitate the promotional process:
• A peer consultancy service can be established similar to that described earlier
for improving discharge performance. A separate fund would be established to underpin the use of practitioners who have successfully implemented innovative advanced practice models in consulting to health services who are just considering, or just starting to implement the same service model. Some times when implementing a new innovation some ‘hand holding’ is required.
12 This same infrastructure can challenge rapid dissemination of initially proven developments
H u m a n C a p i t a l A l l i a n c e
47
• Investment can be made in more speculative examples of advanced practice along the lines of the original phases of the ‘Better Skills, Best Care’ (BSBC) program. In this phase the BSBC program funded a number of innovative pilots
based on submissions from health services, some of which could not, in retrospect, be justified. This time, the pilots should be chosen more centrally to pre-specified criteria that emphasised a search for practice models that were highly promising but lacked an evidence base to push their claims.
• The same investment program could identify practice models that were slightly ahead of ‘speculative’ status and around which a growing evidence base was forming, but dissemination was meeting resistance because of the lack of care
pathways or protocols.
Recommendation 9:
� To develop centrally, through an appropriate forum of relevant Departmental officers and innovative health service providers, a strategic investment plan in worthy (promising) advanced practice models in a similar way to the current
BSBC model. In priority order these can be supported from a separate fund to become operational.
� In the recent past a few isolated gatherings of practitioners in workshops and seminars (for example events organised under the Patient Flow Collaborative II - Outpatients) have been organised centrally. These workshops bring practitioners
together where they discuss informally their specific circumstances and begin to disseminate best practice through the most potent form of communication, word of mouth. Gatherings such as these have proven in other fields to be the most
powerful means of promoting adoption of innovation. An intense period (1-2 years) of shorter but more regular meetings of health service based teams of nurse and allied health clinic practitioners along with key and relevant medical practitioners and outpatient service managers would cost comparatively little yet potentially yield much if conducted within a broader promotional program.
Recommendation 10:
� To increase the number and quality of current collaborative activities in a way that enhances regular interaction between health service and clinic level
decision makers and practitioners.
� Despite the above promotion efforts there will still be allied health practitioners,
clinic managers and medical specialists who will resist change. The rallying point for resistance will be patient safety and quality service concerns. These can be addressed through establishing:
• As noted above, a stronger business case and evidence base for the practice
models being promoted and developing ‘ready-made’ care pathways and protocols;
• The necessary allied health and nurse labour competencies to adequately perform the advanced practice activities at the level of the protocol base or practice guidelines.
H u m a n C a p i t a l A l l i a n c e
48
Recommendation 11:
� To develop a state outpatient services training plan that (1) identifies skill
needs for support of implementation of desired advanced practice innovations (2) prioritises investment in those skills where a deficit is perceived to be a barrier to implementation.
� To ascertain the need for skills to be certified.
� To negotiate with appropriate professional associations and / or training and education institutions to undertake skills assessment, recognition and certification where it is considered necessary or prudent.
Similar to the earlier discussion of discharge processes, a ‘package’ of measures aimed at increasing the level of introduction of advanced nursing and allied health practice innovation into Victorian outpatient clinics is required. We would recommend measures that help financially support innovation or at least do not hinder it, that assist individual
clinicians and clinical teams and their management infrastructure become better informed about innovations, and offer them ground level support to develop and implement specific initiatives in their clinics.
An appropriate ‘package’ could evolve as shown below.
H u m a n C a p i t a l A l l i a n c e
49
Recommended Approach
Step A Financial
year 2009/10
Development of generic protocols and clinical pathway guidelines for those advanced practice developments at one health service that have proven valuable and worthy
of broader implementation. These protocols would still be amenable to local service and clinic modification, but could potentially reduce the time required for new practice adoption.
Development of an intense period (2-3 years) of short (half day) but more regular meetings of health service
based teams of nurse and allied health clinic practitioners along with key and relevant medical practitioners and outpatient service managers where advanced practice innovations can continually be
showcased in an environment of collegiate discourse. Step(s) B & C
Financial year
2010/11
Introduction of MDC and EAL payment codes would support developments in advanced practice in areas that it has the best chance of flourishing and providing
benefit. The implementation of these codes will require the differentiation of the allied health input from the current medical and surgical codes which currently
include funding allocations for allied heath input. All new clinics that are validated by the Clinical Panel and satisfy other key criteria (e.g. a well argued
business case, well developed clinical pathways, strong local support from medical practice and health service executive, and proven competence of nurse and allied
health practitioners) should be supported by temporary supplements to individual health service VACS targets. Thus, additional target funding could be provided for say two years to a new clinic (or for an existing clinic that
wanted to introduce a pre-admission stream), after which the previous VACS target growth trend would be resumed and the new clinic activities funded by productivity gains or the reduction of services in another
clinic13. Step D Financial
year
2010/11 (Later in the
year)
Weighted VACS allied health clinic payments should be progressed. Again acknowledging the challenge of
developing appropriate cost weights around which a reasonable consensus can be built, in the first instance ‘shadow’ costs should be implemented for the first year or two. These weighted payments will have to be congruent with the current medical and surgical VACS encounter weights.
Step E Financial
year 2011/12
Implement new cost weightings if proven appropriate.
13 Neither of the two proposed target suggestions preclude actions which derive from ‘target shifting’ (moving target allocation from one clinic to another) or from innovations within existing clinics and targets.
H u m a n C a p i t a l A l l i a n c e
50
5. Rationalisation of ‘Other’
coded clinics Background situation
The ‘609 Other’ VACS code activity accounted for approximately one third of total allied
health coded activity in the last financial year. Usually, ‘other’ categories in any taxonomies account for less than 5% of whatever is being counted, and therefore identifiable categories in their own right are generally extracted from the ‘other’ category until only genuinely exceptional cases remain. The 609 category within the VACS
classification does encompass a heterogeneous collection of clinics from which sub-categories can be clearly delineated. Given the fixed payment for an occasion of service for all allied health VACS coded activity though, there has been little incentive in the past
to act on breaking up the 609 category.
A case for greater differentiation now needs to be waged on the following grounds:
� more information about actual outpatient services activity is able to be elicited for planning and policy development purposes;
� it is a necessary measure for recommendations made earlier in this report for cost weighting of allied health coded activity. For accurate cost weight data to be collected and interpreted relatively homogeneous classes of activity need to be examined;
� inappropriate outpatient activity can be more easily identified. There is agreement within health services that some activity would be better located in care settings such as the community or primary health care. The current undifferentiated 609 categorisation enables services that appear not to be
appropriate for implementation within the specialist outpatient clinic setting to ‘hide’ amongst a varied number of other more legitimate outpatient services activity (see examples later in this section); and
� opportunities for advanced practice within a multidisciplinary care setting (for instance within a medical or surgical VACS code area) are lost. Alternatively, a 609 clinic prevails which potentially or actually overlaps the activities of another
clinic.
The 609 category is already used by some health services as a means to organise and record better activity in existing allied health codes. For instance, in the VACS Clinic Schedule one health service described a new 609 activity thus:
“Activity in this service was previously recorded under the VACS clinic name of
Physiotherapy. This is not a new activity but has been separated on our system
to allow for better management and analysis of activity in the Physiotherapy
Department.”
To more appropriately categorise activity in this VACS category it is a must to first establish what activity it does currently cover. A list of 609 VACS coded outpatient services activity types identified by surveyed health services is provided in Table 5.1 below. Each clinic is described in terms of clinic type, staffing type and typical activity.
The list represents a compilation of the range of services provided and gives a strong insight into the very eclectic nature of the clinics included under the 609 category.
H u m a n C a p i t a l A l l i a n c e
51
Table 5.1: A listing and description of staff type and ‘typical’ activity within the 609 VACS code
VACS Clinic
name � Staffing Type Typical Activity
Hand Clinic / Therapy
� Occupational Therapist
� Physiotherapist
Hand therapy, splinting exercise, wound and scar management - assessment, Intervention, & education Art therapy
RECG ECG - Repatriation
� Cardiology
Technologist
Performing & Interpreting ECG’s
BSTN (Bone and Soft Tissues
Clinical Nurse)
� Specialist Nurse Patient orientation, physical assessment and wound
management. Reiterating complex treatment plans to patients, education about
treatment, discussion of completed screening tools.
Antenatal / Postnatal
� Midwife (Adult,
Teenage, Genetic)
Antenatal classes, breastfeeding
Diabetes Head
and Neck Nephrology / Obesity Clinic
� Dietician Nutrition assessment, management
& review
General and Specialty Clinical Psychology
� Psychologist (Menopause, Cystic Fibrosis, Breast, Oncology, Couple)
Psychological assessment and treatment: Family & relationships - depression & anxiety
Prosthetics & Orthotics
� Orthoptist Provision of an orthotic or prosthetic device. Preliminary assessment pre-
opthalmologist consultation, medications and prescription of glasses, intraocular pressure,
anterior segment and pupil function preceding dilation. Visual field analysis (computerised and manual)
Binocular vision and paediatric assessment/management
Lymphoedema � Occupational Therapist
� Physiotherapist
Compression management,
exercise/massage, education, lifestyle issues
Stomal Therapy � Stomal Therapy Nurse Stoma siting. Stoma/wound
assessment and treatment. Education stoma care and lifestyle management. Interventions such
as hernia management. Pre-post-operative information review & support.
Medical illustration
� Medical photographers Variety of medical photographic techniques
H u m a n C a p i t a l A l l i a n c e
52
Table 5.1: A listing and description of staff type and ‘typical’ activity within the 609 VACS code (cont.)
VACS Clinic
name � Staffing Type Typical Activity
BNC (Breast Clinical Nurse Coordinator) Breast Care Liaison
� Specialist Nurse Screening for supportive needs/coordinating complex care needs. Facilitating referrals to other services. Symptom assessment & education. Diagnostic work-up. Fine needle aspirations of seromas, end of treatment education. Fitting
prosthetics.
CVAD - Oncology � Specialist Nurse Haematology assessment. Patient triage
Wound management & Vascular
� Podiatrist Podiatric assessment, treatment and review
Wound Clinic � Specialist Nurse (Vascular, Burns, Plastics, Seroma)
Complex/ Chronic wound assessment, management & referral
Pulmonary Rehabilitation
� Occupational therapist, Physiotherapist,
Exercise Physiologist, Nursing & Social Work
Assessment, Therapy & Education (CPAP)
GIN (Gastro-
Intestinal Nurse) � Specialist Nurse Screening for supportive needs.
Coordinating complex care needs. Facilitating referrals. Assessment of symptoms. Diagnostic work-up & cancer education
Lower urinary tract surveillance
� Nursing Prostate cancer surveillance clinic, following all stable patients to monitor for biochemical recurrence (rise in PSA), urinary function (incontinence- and erectile dysfunction
Pain clinic � Physiotherapist/ Psychologists
Assessment treatment management plan
GYNC
(Gynaecology Nurse) Coordinator
� Specialist Nurse Diagnostic work-up. Screening for
supportive needs. Coordinating complex care needs. Facilitating referrals. Symptom assessment
and education.
Diabetics Clinic � Specialist Nurse (adult, paediatric)
Follow – up and review. Education for self-management. Insulin
initiation, titration and adjustment during stabilisation, insulin pumps and continuous glucose monitoring. Goal setting. Healthy lifestyle
H u m a n C a p i t a l A l l i a n c e
53
Table 5.1: A listing and description of staff type and ‘typical’ activity within the 609 VACS code (cont.)
VACS Clinic
name � Staffing Type Typical Activity
Urology � Specialist nurse Post-operative review. Uro-flow rate measurement. Bladder scanning. Complex catheterisation, self-catheterisation, self-dilatation. Continence advice.
Dermatology � Specialist nurse Allergy testing
Infectious Diseases
� Specialist nurse Follow-up of test results
Central Venous
Access/ infusion � Specialist nurse
Maintenance of venous access
Source: Survey of health services
Currently, the ‘Other’ category is the only outlet for establishing and growing nurse-led involvement in outpatient services delivery.
The survey of health services found the average consultation time of most 609 clinics varies in length between 30 and 60 minutes with some extending to 90 minutes. It was consistently reported during interviews with key-stakeholders that the majority of patient appointments in this category include an intervention or treatment that necessitates an
extended appointment time.
Patterns of ‘other’ service delivery
A study of existing 609 coded clinics listed in the VACS Clinic Schedule generates a similar list to that above but also allows a pattern of service provision across the health services to be discerned. The relative prevalence of clinics in each of these broad clinic types is illustrated in Table 5.2 below.
From the survey data and listed clinics in the 609 category the following groupings can be isolated:
� Specialist nurse – led clinics that tend to run parallel with or otherwise in support of specialist medical or surgical clinics. Some of these clinics are specifically to
prepare patients for an operation or support patients post-operatively;
� Allied health clinics of disciplines not covered under other 600 codes. The main discipline / service area categories are psychologists, orthoptists, orthotists /
prosthetists;
� Procedural clinics where a particular set service is provided (although calibrated to the specific individual patient needs). This includes endoscopy, radiotherapy and chemotherapy; and
� Multidisciplinary clinics (involving only allied health and/or nursing professionals but no medical specialists).
H u m a n C a p i t a l A l l i a n c e
54
Table 5.2: Distribution of 609 clinics across the health services by clinic type (N = 19)
Source: VACS Clinic Schedule, 2009
Specialist nurse-led clinics are the most common forms of 609 Other Allied Health VACS clinics with all health services having at least one such clinic. Nurse-led clinics are able to be sub-categorised into three main areas as follows:
� Specialist Nurse consultant services where the nurse functions in a similar capacity to that in the allied health disciplines. These specialist nurses are characterised by closer alliance to the specialist discipline than to nursing in
general and invariably have a separate professional association. For example:
• Diabetes education
Clinic type
Total number
of health
services with
clinic type
Specialist nurse clinics
Stomal Therapy Nurse Clinic 15
Diabetes Education Clinic 16
Antenatal / post natal education, infant clinic 8
Sexual Health 4
Dermatology/ Skin clinic 4
Respiratory + VRSS 3
Continence 3
MS Nurse Clinic 3
Other (less than 3 health services with clinic - includes Lymphedema Management clinic, Enuresis Clinic, Injection,
Infection control clinic, Epilepsy nurse- led clinic, Hepatitis Nurse Consultant clinic)
Other allied health clinics
Psychological Services / Neuropsychology 9
Orthotics and Prosthetics 9
Medical photography 3
Nutrition clinic 1
Procedural clinics
Breast Care Nurse Clinic / Oncology clinic 8
Cardiac Health/ Assessment / ECG clinic / Heart Failure Service
7
Other (less than 3 health services with clinic — includes Growth hormone management, Endoscopy education, Sleep Apnoea)
Pre & Post – operative care clinics
Dressings/ plaster/ wound management 7
Urology Nurse Clinic 7
Nurse pre-admission 2
Liver transplant nurse clinic 1
H u m a n C a p i t a l A l l i a n c e
55
• Stomal therapy • Dermatology
� Some of the above categories are already included in the South Australian outpatient clinics classification model as separate codes.Post-operative care as in management that in the past, under a regime of longer inpatient hospital stays,
would have been undertaken prior to discharge. Examples include:
o Orthopaedic Nurse-Led (ORTHO) - Review of orthopaedic patients post-operative wounds. Ongoing wound management. Removal of sutures. Post-operative patient education on exercise and wound care.
o Vascular Nurse-Led (Vascular) - Wound management of chronic ulcers, varicose vein bandage changes, patient assessment and patient referral
to community services. o Urology Nurse-Led (Urology) - Supra Public Catheter changes, bladder
wash outs, urodynamics, voiding flow measures, patient assessment, patient referral to community services.
o HOC Nurse-Led (HOC) - PICC line dressing change, Hickman's catheter dressing change, injections, patient education, venipuncture, patient assessment, patient referral to community services.
� Pre-operative care and preparation. Currently there are a small number of nurse-led pre-admission clinics.
An extended range of procedural clinics are included in the 609 category. The clinics help prepare patients for the procedure that can be a single occasion of service (e.g. a scope procedure) or a longer term course of treatment (e.g. cancer treatment). The
clinics in this broad category include:
� Chemotherapy, radiotherapy
� Endoscopy, colonoscopy, oesophagoscopy14
� Renal dialysis
An example of such a clinic (located at the Bendigo Health Service) is described in the VACS Clinic Schedule:
Renal Clinic — The Renal clinic is a new clinic that will service clients with
chronic kidney disease. A dietician, a social worker and a renal resource nurse
will service the clinic. Clients will be seen individually, and have individual self-
management plans developed according to their needs. The clinic will work
closely with the Renal General Outpatients clinic, the HARP CDM Renal Care
Coordinator and the clients general practitioner.
In the SA outpatient services classification these procedures have their own code and
weighted cost. It can be argued that surgical and medical VACS codes cover this area of activity already.
Approximately 75% of health services have an allied health clinic that involves an allied
health discipline not covered by existing Allied Health VACS Codes. The larger teaching hospitals (A1 category) are more likely to have a clinic conducted by a discipline not covered by a VACS code.
14 There is no evidence from any data source that scope procedures are actually performed by nurses. However given advanced speech pathologists transition to the conduct of scoping procedures, one might expect nurses to follow.
H u m a n C a p i t a l A l l i a n c e
56
The main disciplines covered in this way are:
� Psychology (almost half the services have clinics);
� Prosthetics / Orthotics (a similar number of services have clinics); and
� Orthoptics.
In comparable other classification systems such as the South Australian MMSS, all allied health disciplines are covered and have a separate code. The VACS 600 code categories could be extended to include relevant disciplines. Currently all allied health service
activity is remunerated at a fixed rate and it makes little or no difference whether the clinic is coded 609 or otherwise, although there are benefits in coding outpatient service activity more precisely.
In the survey data, and less obviously in the Clinic Schedule data, some 609 clinic activity is accounted for where combinations of allied health professionals offer collaborative clinic services. Combinations include psychologists and social workers
with other allied health professionals and nurses. At least three variations of multidisciplinary team options have been recommended none of these were without at least one medical specialist. An example of a multidisciplinary allied health clinical service is hand therapy that might include physiotherapists and occupational therapists. Another
collaboration example is between a clinician who deals with the physical aspects of the disease (e.g. nurse, physiotherapists) and a clinician that deals with the psychosocial aspects of patients or their carers (e.g. social worker, psychologist), for example patients
with oncology or degenerative disease, or in rehabilitation settings.
There are a number of seemingly different and ‘one-off’ type clinics (although the actual activity could be similar in approach and intent to the above 609 VACS code area clinic
types). This genuine ‘other’ group of clinics includes:
� Halo Washing;
� Chaplaincy Services (similar intent to psychology clinics);
� Koori Lifestyle Education Clinic;
� Multicultural services;
� Women’s wellness clinic;
� Mock MRI; and
� Community Outreach.
Some 609 clinics appear not to be appropriate for implementation within the specialist
outpatient clinic setting. A more appropriate setting for these clinics is community health or a low dependency ‘step-down’ care facility. The following descriptions from the Clinic Schedule for rural health services are examples that illustrate this:
� Teenage antenatal classes — classes are run by a midwife. They cover antenatal
education, early parenting education, basic life skills and building on self-esteem.
� Infant massage classes — The Infant massage classes are run by a Midwife /
Registered Infant Massage Therapist. Massage is used to enhance the parent
infant attachment. The classes also provide education around early parenting.
This clinic would seem more appropriate in a residential parenting support
service or again in community health.
� Breastfeeding classes — The Breastfeeding classes are an education class for
parents around the benefits of breastfeeding and about support services
available with an aim to increase successful initiation & establishment of
breastfeeding.
H u m a n C a p i t a l A l l i a n c e
57
� Parenting classes — Early Parenting classes provided antenatally covering
feeding, bathing, support services, parenting, baby care, father support, SIDS
and support group information.
� Antenatal classes — (25% public) Antenatal classes are provided by a Midwife /
Childbirth Educator. They cover pregnancy, labour, birth, support services, baby blues, contraception, what happens in hospital, pain relief. It also includes a tour
of the maternity department.
Possible ways forward
The capacity for planning and policy development will be enhanced when potential overlap and duplication between specifically coded outpatient service activity and ‘other’ clinic activities and the possibility of inappropriate outpatient activity can be reduced.
The main way to address the problem is simply to judiciously introduce more VACS classification codes. On the basis of available evidence of the prevalence of current clinic types reported within 609 coded activity, a reasonable case can be mounted to introduce some or all of the following clinic classifications (See Table 5.3).
Table 5.3: Potential new clinic classifications derived from current 609 ‘Other’
clinic activity
Clinic classification Example / description
Stomal therapy • Services provided include: Counselling &
Emotional support, Information & education. Equipment / Appliance prescription and training. Education & training in changing and trouble-shooting of stoma bags. Wound assessments
and dressings
Diabetes Education • People with diabetes who have been identified as requiring further diabetes education following
inpatient stay or medical review in endocrinology outpatients. Treatment provided = diabetes education, initiation of blood glucose monitoring,
insulin commencement etc.
Antenatal / post natal education, infant services15
• General gynaecological women's health assessment for women over the age of 45 years
• Provision of pregnancy testing services with advice and referral as appropriate
• Education about childbirth and parenting
15 One might argue that these activities should be included with codes 401 to 404, although all these codes require the presence of a specialist medical practitioner.
H u m a n C a p i t a l A l l i a n c e
58
Table 5.3: Potential new clinic classifications derived from current 609 ‘Other’ clinic activity (Cont.)
Clinic classification Example / description
Psychological Services (possibly
including services currently labelled as ‘chaplaincy’). There are three variants of this type of clinic …
• Patients initially seen in various wards and
requiring review visits to complete the psychological intervention: e.g. adjusting to loss of limb, acute anxiety, compliance to medication
• Sexual dysfunction secondary to physical
problems/medication; psychological approaches as part of management; relationship problems and sexual difficulties often interact and it is important for a complete approach to intervene
with the relationship • Support for patients and their carers and family
(in collaboration with another allied health
practitioner or nurse) undergoing longer term treatment for a serious illness with attendant impacts on living circumstances
Orthotics and Prosthetics • Patients attend for measurements and fitting of orthotics and prosthetics
Orthoptics • Visual acuity, visual fields, HESS, 'A' scan
(testing)
Post-operative wound management
• Review of patient’s post-operative wounds. Ongoing wound management. Removal of
sutures. Post operative patient education on exercise and wound care.
Urology services (post operative) • Supra Public Catheter changes, bladder wash
outs, urodynamics, voiding flow measures, patient assessment, patient referral to community services.
Oncology care • Provide ongoing information, support and coordination of care to patients diagnosed with cancer
Cardiac Service16 • Multidisciplinary program to rehabilitate patients with chronic heart or lung disease. Targets patients who have recently had a hospital
admission or are at risk of an admission related to their condition. The patient will be reviewed by a nurse, social worker, physiotherapist or occupational therapist according to the client
need. Intended to improve patient capacity to self care and manage their condition without the need to a full rehabilitation program.
Source: Survey of health services
It is difficult to estimate the effect introduction of the above codes would have on the
VACS data since no activity data was available for analysis at the individual clinic level. However, it is likely that introduction of nurse-led clinics (stomal therapy and diabetes education) and specialist allied health clinics (psychology services and orthotics / prosthetics) alone would take up to three quarters of the current 609 code activity.
16 A similar situation can be argued as for ante and post natal services.
H u m a n C a p i t a l A l l i a n c e
59
This would reduce the ‘Other’ category to just over 8% of total allied health VACS coded activity. These new codes are in line with those used in other Australian jurisdictions, and overall health service activity targets will not change (rather existing activity will simply
be re-labelled). If payment for occasions of service remains at the flat rate for all allied health VACS activity, a cost neutral outcome will result.
The introduction of cost weightings for allied health services (as recommended) might
still result in a cost neutral outcome, however it is difficult to know how the identified new clinic categories might be weighted and if they will fall on average above or below the current unweighted rate of payment ($61 per occasion of service).
Recommendation 12:
� To introduce a number of new VACS codes within the 600 ‘Allied Health’
series. This would include at least codes for:
− Stomal Therapy
− Diabetes Education − Psychological Services − Orthotics and Prosthetics − Post-operative wound management
− Urology services (post-operative) − Nurse-led Oncology care
The proposed changes to the VACS classification should more clearly expose any clinics that appear to be more appropriately delivered in a primary health care, community
health or stepped down care setting. In addition. a once off audit only of ‘609 Other’ clinics, particularly after the bulk of the clinic activity has been reclassified, is recommended, focusing on examination of the validity of clinics within an outpatient
services setting.
Recommendation 13:
� To develop criteria for assessing the suitability of clinics on the basis of stated aims and models of care for an outpatient services setting.
� To conduct an audit of all 609 VACS coded clinics and assess them against the
above criteria.
� To seek an explanation from health services where clinics do not appear to satisfy the criteria for suitability.
� To install the above criteria to ensure future applications for new clinics are subjected to a structured assessment of validity to belong within an outpatients services environment.
H u m a n C a p i t a l A l l i a n c e
60
Recommended Approach
A ‘package’ of measures designed to influence change is likely to be more effective than a single intervention in achieving desired outcomes. An appropriate ‘package’
could therefore include the following interventions:
Step A Financial
year 2009/0
Seek agreement on new categories of outpatient
activity to be coded separately under a revised Victorian Ambulatory and Classification System. Revise the VACS Reporting Forms to reflect the new categories agreed.
Step(s)
B & C
Financial
year 2010/11
Introduce the agreed new categories into the
targeting and funding process. Advise health services of the opportunities and the obligations for new clinic classification and data collection.
Draft criteria for auditing health services and the appropriateness of existing (remaining) 609 clinics within the outpatient setting. Embedding the criteria into the deliberations of the Clinical Panel.
Step D Financial
year
2011/12
Conduct of an audit of 609 clinics, identification of clinics that should be in an alternative setting,
consultation with health services on ‘suspect’ clinics.
H u m a n C a p i t a l A l l i a n c e
61
6. Group clinics
Background
Most stakeholders were cautious in their attitude toward group clinics. Several of the surveyed health services (4 or 20%) claimed not to conduct group outpatient activities at
all, while many of the others restrict group activities to a narrow band of VACS funded areas. For instance, none of the surveyed health services offered group activities for 601 (Audiology), 606 (podiatry) and 607 (speech pathology). Within the VACS codes, group processes were relatively prominent only for nutrition, physiotherapy and ‘Other Allied
Health’ categories.
Stakeholders argued that group sessions are not cost effective, as funding does not take
into account the actual time and resources required for the proper organisation, set up and conduct of group sessions. A proportion of stakeholders were of the opinion that all patient encounters should be counted individually. Since most VACS allied health clinics are for post hospital support, they argued that 99% of patients receive individual
assessment, treatment and management. A possible exception is cardiac rehabilitation where evidence-based practice suggests some group interaction to be appropriate, although it was pointed out by the stakeholders that the bulk of the patients’ cardiac
rehabilitation is still managed on a one-to-one basis with the clinician. A study supportive of the above argument conducted in Tasmania on means of weighting allied health costs, found that only 0.5% of total allied health encounters were group encounters, and the average per-patient cost for these was 70% of the costs of a 1-to-1 encounter.
Despite the widespread ambivalence expressed in regard to group clinic funding, a majority of stakeholders still conceded a clinical case can be made for group therapy in certain circumstances. For instance, group sessions are useful in areas where clusters of patients have similar educational needs — such as preparation for chemotherapy or renal dialysis, cardiac rehabilitation or diabetes lifestyle. Another example is a lymphoedema clinic, which is predominantly a group education clinic held in concert with the medical
VACS clinic, and is counted as one encounter. One could argue that information provision / education is best delivered one-to-one since it can perfectly adjust for different patient learning capabilities, style and pace.
There are genuine clinical advantages for group sessions where they include elements of peer support and shared learnings. Examples of these are cardiac rehabilitation which provides peer support and child health groups where new parents learn from and support
each other.
Recommendation 14:
� To use group coding (and funding) only in cases where evidence-based practice suggests group interaction to be appropriate and to confer clinical advantages. A further recommendation on this issue is provided below.
H u m a n C a p i t a l A l l i a n c e
62
Current situation
Group sizes in clinics range from 2 to 20 patients, with cardiac rehabilitation and social
work clinics obtaining greater average patient group sizes of 10 or more. Although group outpatient clinics run from one to six hours, clinical sessions normally average around 90 minutes.
A survey of health services detailed the current types of group clinics as shown in Table 6.1. Most of these groups appear educational in purpose, although they are also likely to satisfy the ‘clinical’ criterion of providing peer support.
Table 6.1: Clinic names / types of group clinics by VACS code
VACS
Code
Types of clinic
Current Suggested
602
Nutrition
Mental health cooking group;
Obesity Clinic
Nutrition-gestational diabetes
groups. The groups would include input from a diabetes education specialist, dietician and
physiotherapist
604
Occupational therapy
Juvenile Arthritis clinic; hand clinic Paediatric groups (gross motor,
fine motor), post carpal tunnel and hand surgery patients. Symptom management (stress, fatigue, sleep problems, breathlessness,
return to work preparation).
605
Physiotherapy
Pregnancy fitness; Pelvic floor and
abdominal exercise; Pilates; Pre-natal Back Care; TENS information; Maternal weight
management; Gestational Diabetes Exercise; Mother and baby exercise and education; Vulval Clinic initial education
session; Chronic Pelvic Pain relaxation group; Polycystic Ovarian Syndrome Exercise Group; Childbirth Education; Menopause exercise; OA knee group; Ankle group TNH
Exercise groups for Type 2
diabetes, shoulder and menopause patients, ‘Living with cancer’ exercise and education groups,
pelvic floor, back pain and continence education groups
608 Social work
Group activity led by social workers in all areas of clinical practice including maternity,
gynaecology, oncology and neonates. These groups could include: • open, closed, support and/or
education groups for patients accessing a range of clinical services who experience
H u m a n C a p i t a l A l l i a n c e
63
Table 6.1: Clinic names / types of group clinics by VACS code (Cont.)
VACS
Code
Types of clinic
Current Suggested
complex psychosocial issues and are marginalised or disadvantaged, including antenatal support groups,
parents with disabilities, culturally and linguistically diverse persons, victims of violence;
• therapeutic groups for children with diagnosed terminally ill family members;
• information sessions regarding specific psychosocial issues, community services, and so on.
Community partnerships could be accessed to deliver groups, assisting with the transition to the
community from the acute sector.
609
Other
Cardiac Rehabilitation clinics,
continence clinics; dialysis clinic, multidisciplinary diabetes clinic; nurse-led gestational diabetes clinic; Pastoral Care; an end of treatment breast cancer clinic; Hand therapy group; Lymphoedema group; Preparation for chemotherapy clinic
Physiologists - exercise groups for
oncology, shoulder, renal, ante and post natal patient groups
Source: Survey of health services
A review of new group clinic suggestions from the survey data suggests a similar pattern as shown in Table 6.1. There are a number of other allied health group activities that often include one-to-one consultation time with each patient. Common practice for a group component that all patients require (for instance, education) is followed by one-to-one consultation time within the group session. A secondary benefit is time for patients to talk amongst themselves, thus satisfying peer support objectives. Generally these ‘group’ activities are counted as individual occasions of service and recorded as such for
VACS funding purposes (generating several as opposed to a single VACS payment). Although there are a range of legitimate group processes, only some are counted for VACS payment purposes. There is difficulty in finding a generic definition of a ‘group’ for
the purpose of classification and funding as demonstrated in a comment from one interview subject:
“Need to differentiate between true groups where all patients have exactly the
same condition and all do the identical program at the same time and the more
common multiple patient model. In this model such as hydrotherapy, pulmonary rehabilitation etc, patients all have their own individual goals and their
interventions are provided concurrently. Any one visit may last up to 90 minutes.
H u m a n C a p i t a l A l l i a n c e
64
Patients benefit from interaction with other patients with similar conditions. There are often multiple therapists present”.
A way forward
In an earlier Chapter it was recommended that cost weightings be introduced for allied health VACS code activity similar to that prevailing for medical and surgical VACS codes.
Ideally if this recommendation were adopted then two separate weights for some of the 11 allied health categories would be introduced — one weight for single patient encounters and one for group sessions that involve multiple patients at the same
session17. The payment for group sessions would be expected to be weighted higher than for individual occasions of service first because of the greater potential workload (and therefore cost) and second because group activity weightings would need to be high enough to provide an incentive for group, rather than individual, sessions where clinically warranted.
Recommendation 15 (preferred option):
� To introduce a funding arrangement based on cost weightings for group
activity in each of the allied health VACS code areas if appropriate. Cost weightings to be developed using a similar methodology to that required for individual occasions of service.
Like all cost weights, weightings for allied health group activity would represent a range
of possible cost outcomes depending on a range of group characteristics. Some of the more important are considered below.
Another way forward
Contingency should be provided for the ‘ideal’ option of cost weighted payments not being adopted and an alternative way of considering (1) the basis on which different groups can be logically defined; and (2) how group activity could be determined such
that the payment is higher than an individual occasion of service, but not so high as to
make group processes too attractive18. Ideally, any increase in group activity should be at the expense of individual occasions of service so the increased costs of groups is balanced by the decrease in total cost of individual patient payments (with the only net
result being an improvement in clinical outcomes).
There is several ways that groups can be defined. The most obvious means of classification include:
� different sized groups. The survey data indicated that many groups are small (numbering less than six), although some larger groups are formed in cardiac
rehabilitation and hydrotherapy. Groups can be classified as small (2-6), medium (7-12) and large (>12). When considering the appropriate size of the group, smaller groups are preferable if an individual patient assessment or treatment
17 Information systems would obviously need to be modified to allow capture of group allied health sessions. Currently, all allied health (indeed all VACS) groups are counted as a single patient encounter 18 Thus promoting group clinics in circumstances where the evidence is not supportive.
H u m a n C a p i t a l A l l i a n c e
65
element is required, whereas a larger group is preferred when there is an element of shared learning between the group participants.
� different group process duration. Some group clinics might be only for an hour,
whereas others are for a whole session (half day or 4 hours). Others can take all day. The survey results indicated the average session duration to be around one and a half hours. Group clinics though could be classified on the basis of duration,
say < 1 hour; 1-2 hours; 3-4 hours; > 4 hours.
� different group activity purposes. A possible list of purposes is:
o Information provision / preparation for treatment o Education / shared learning o Peer support o Assessment
o Combined or similar courses of treatment / therapy / exercise
Many group processes are a combination of purposes (e.g. education + assessment + therapy), and this makes it difficult to find an appropriate funding basis.
There are two broad ways that groups could be funded differently from the current flat fee, and in recognition of the additional cost (and value) of group clinics:
1. An input based approach – that is the cost of labour required for delivery of the
service divided by the number of clinics the labour can provide to obtain the unit ‘price’ per patient. This is essentially what has occurred to develop a unit price for
allied health VACS clinic payments per occasion of service (for an individual patient). Input based models have found favour elsewhere. For instance, the Home and
Community Care funding arrangements for allied health care provide for a ‘person hour’ of direct service received by a single service consumer. Each person hour attracts a set fee. HACC services provide for two different group activity fees; one for a ‘core’ planned activity group, and another for a ‘high’ planned activity group. The latter is calculated on the basis of 20% of a full hour of individual consumer service delivery for each group activity participant. The total ‘person hours’ is calculated by summing the individual hours spent in a session by all consumers — if more than five consumers attend a group for an hour then the payment for a group activity becomes
greater than an individual occasion of service.
Without too much change to the existing VACS funding arrangements, a discounted
individual payment for attendance at a group clinic could be devised along the above lines.
2. An output based approach – output funding arrangements pay on the basis of a
completed service. The cost weights for medical and surgical VACS payments are output based as is much of the payment for inpatient services in the Victorian health system.
Within an output based funding arrangement there are many alternative ways of establishing the payments. Examples based on the group definitions discussed above include:
− A block payment for various group clinic attendance ‘output’ bands (i.e. 1-6 attendees = rate A; 7-12 attendees = rate B; 13-20 = rate C, etc.). The payment arrangement could be a flat amount for each different group size;
presumably the payment per unit patient would diminish as group sizes got larger.
H u m a n C a p i t a l A l l i a n c e
66
The payment could instead (or as well) take into account the duration of group sessions. If the information management systems supporting the booking and claiming of allied health VACS payments was sufficiently sophisticated the
system could be designed in such a way as to monitor the length of the session and number of attendees.
− Payment on the basis of different types of groups. Different groups could be broadly defined as noted above such as ‘Education’ or ‘Treatment’. Examples of
each include antenatal classes as education and cardiac rehabilitation and hydrotherapy groups as treatment groups. The need for this type of differentiation was a consistent message from the focus group interviews.
Payments for different group types need to vary according to the amount of work required for each group participant. For instance, education groups could largely be counted as a single person (since the work is largely the same for one
or many participants19) and therefore be paid at or close to the current rate of a
single occasion of service plus a small administration charge for preparation and set up – booking appointments, room booking, session preparation etc. At the other end of the spectrum, a treatment group with a mixture of one-to-
one and true group activities, could be close to the equivalent of 75% (or other figure) of the OOS for each individual patient in the group. Thus the payment for a ‘treatment’ group might be calculated on an agreed percentage of an individual OOS payment multiplied by the number of group participants.
As noted earlier, our research has shown that there are many different purposes for group activities but these invariably encompass one or more of education, peer support,
treatment and assessment. A significant array of different group activity types could be constructed from different permutations of these specific group purposes — each of these separate combinations of clinic activities in theory should be included in any proposed funding methodology given the varied cost implications of each purpose combination.
Possible payment options and examples of how prices may be set for a range of the most realistic group clinic purpose combinations are described in Table 6.2 below. Of course the multiplier amounts shown in Table 6.2 above are completely arbitrary and
intended only to demonstrate first the main types of group activity forms and second how a more appropriate payment for group activity might be constructed. Developing actual values for the multiplier factors in Table 6.2 would be best achieved through an
expert panel of outpatient allied health and nursing clinicians. All this assumes that a cost weight study approach is not to be pursued.
Recommendation 16 (contingency option):
� To increase the payment for group clinics according to payment on the primary purpose/s of the clinic. A limited number of payment options to be
developed (say no more than 10) based on the most common types of group clinic purpose or purpose combinations.
� To develop an agreement on the payment levels associated with each group
activity type from a reasonable assessment of the inputs required. An expert panel of experienced outpatient clinic allied health and nursing clinicians to be convened to create this consensus.
19 No doubt many educationalists and trainers will argue this approach, noting that only for truly didactic education sessions would the proposal hold true. Most education sessions would presumably allow for some individual instruction and checking of understanding, although this may have only a limited impact on the session duration.
H u m a n C a p i t a l A l l i a n c e
67
Table 6.2: Possible Combination group payments
Type of group
VACS payment Rationale
Education only (frequent justification for group process) or ... Peer support only (probably
unlikely although may be appropriate in social work or psychology clinics)
OOS x 1.3 Equivalent to single OOS but with allowance for costs of preparation & administration.
The inclusion of a time dimension may also add value to this measure
Education + peer support OOS x 1.4 Allows for the additional work required to coordinate the shared learning from peer support
Treatment only, e.g. hydrotherapy
OOS x 2 This category might need a greater multiplier if more staff resources are required though it
could equally be claimed, as it is under the current system, as a collection of individual occasions
of service.
Education + Treatment or ...
Peer Support + Treatment
OOS x 2.3
Assessment / care planning + Education or ...
Assessment / care planning + Peer Support
OOS x 2.3 It is presumed that the ‘assessment’ component will
require limited time and might be more like a monitoring of progress against the care plan.
One would expect any significant assessment process, for instance one from which the care plan was
developed, to be considered as an individual OOS.
Assessment / care planning + Treatment
OOS x 3 Assumption that each assessment is approximately 15% of the standard VACS allied health code OOS (that is around
10 minutes). This would mean that groups of six (approximately the average group size) would attract the equivalent of an
additional individual OOS payment.
Due to the significant implications within and between health services that may result from changes to the VACS funding model for group activity, the implementation of a
shadow funding arrangement say in the first year would be prudent. This will allow the impact of proposed changes to be properly tested and the outcomes of changes on health service revenue fully demonstrated.
H u m a n C a p i t a l A l l i a n c e
68
Recommendation 17:
� To introduce any new group activity payment first as a shadow funding
arrangement while changes to the VACS funding model are settled.
Non funding approaches
Any change to the VACS model which reduces the revenue obtained by health services will need to be carefully managed. The Review’s consultation data suggests that attempting to move health services away from claiming individual occasions of service for participants in many current group activities will be challenging. Therefore, as well as the fine tuning the VACS funding model to give greater incentive to the use of group clinics, there is a need for promotion of group clinic processes.
Accordingly, guidelines need to be developed and promoted that identify the clinical circumstances in which group processes are at least equal if not superior to individual patient occasions of service. These could be broad guidelines that (1) offered a range of
decision making criteria against which practitioners could test specific clinic circumstances, (2) provided examples and descriptions of successful group clinics and (3) provided thoughts on group activity best practice including group size, session duration, session conduct and adult education principles. Alternatively, if a strong enough evidence
base exists, more prescriptive (advisory) parameters, which specified specific types of clinics within VACS code classifications as always being more appropriate for group processes, could be developed.
Recommendation 18:
� To develop criteria for decision making to aid service providers in identifying
circumstances which are appropriate for group processes and those which are better suited to individual OOS encounters.
� To provide examples and descriptions of successful group clinics and group activity best practice.
� To initiate a broad promotion and education campaign in regard to group clinic processes targeting health service outpatient administrators and clinic leaders.
The current VACS group clinic payment that is the same as an individual occasion of service logically infers that group processes have a single purpose, to increase efficiency
of resource (labour) use. The Review findings indicate that if a more suitable funding methodology is not found to fund group clinics then their continued decline in use (and subsequent substitution with individual appointments) will become common practice for all but those groups whose sole purpose is to provide education.
The most appropriate way to halt and possibly even reverse the trend is to appeal to outpatient health service provider and managers’ understanding of group activity not just as a means of efficient resource use but more as a means of promoting better patient
health outcomes. A renewed and appropriately directed interest in the group clinic as an important clinical intervention must still be supported though by changes in the VACS funding arrangements for group clinics. If the Department adopts the recommendation
offered by this review, and moves to appropriately weighted allied health VACS payments for individual occasions of service, then the optimum approach would be to calculate cost weights for group clinics within each of the Allied Health VACS Codes. If this pathway is not chosen, then group clinic payments at the very least will have to be changed to
H u m a n C a p i t a l A l l i a n c e
69
Recommended Approach
better account for the costs to health services of preparing for, setting up and conducting group clinics.
Step
A
Financial
year 2009/10
Develop guidelines based on a review of available
evidence to help health service management determine the clinical circumstances under which group activities promote superior patient outcomes.
Seek agreement on defined categories of group activity and devise a way of allocating these categories a code each in a revised Victorian Ambulatory and Classification
System. Revise the VACS Reporting Forms to reflect the new categories agreed.
Convene an expert panel of experienced outpatient clinic allied health and nursing clinicians to develop an
agreement on the payment levels associated with each new group activity VACS code.
Step
B
Financial
year 2010/11
Disseminate guidelines on group activity process decision
making and promote group activity aggressively. Introduce new group activity VACS codes and collect data on group activity. Allocate shadow prices to codes and analyse the cost implications of a full implementation of new group activity payments.
Ensure relevant group clinic parameters (e.g. group size, duration, type, etc.) are included in the VINAH minimum data set.
Step
C
Financial
year 2010/11
If possible, undertake a study of cost weights for group
clinic activity in each of the allied health VACS code areas. Compare the cost implications of weighted group clinic payments on the VACS funding arrangements with a
payment system based on defined group types and expert group assessed payment levels (see above).
Step
D
Financial
year 2011/12
Introduce a new system of payments for allied health and
nursing group clinics.
In the timeline suggested above, given actual introduction of new funding arrangements for group clinics is not until financial year 2011 / 12, the challenge will be to shift health services from claiming the individual Allied Health VACS Codes to proposed new group codes. Specific target setting for group clinic activity and auditing may be required to
facilitate this shift in behaviour. Monitoring of the appropriateness of health service claiming of individual and group sessions can be instituted though this will require clear criteria for group activity, the setting of an individual minimum time treatment / assessment occasions of service, and information systems which can accurately track the length of group sessions and the number of participants in each session.
H u m a n C a p i t a l A l l i a n c e
70
7. Discussion Background
The Department of Human Services introduced a funding model for outpatient services based on the Victorian Ambulatory Classification System (VACS) on 1 July 1997 for the 17 major metropolitan and Geelong hospitals and on 1 July 1998 for Ballarat and Bendigo
hospitals. The new model, while acknowledged as not being perfect, began to address major issues of inequality in funding between health services that had arisen because of entrenched historical funding levels. It was also appropriate to the context of the time in that it did was easy to understand, comparatively simple to implement especially in so
far as it did not require patient level data. In introducing the VACS classification and funding arrangements its proponents were
aiming to:
� “Improve fairness in terms of allocation of funding across hospitals.
� Maintain service efficiencies.
� Create a profile or broad description of services provided by acute public
hospitals.
� Provide incentives to maintain and restructure hospital outpatient services to
improve services for patients.
� Identify possible ‘gaps’ and duplications and enable more detailed service
planning.” (DHS, 2008). Since its introduction, the VACS system has evolved incrementally largely as a result of internal reflection and analysis and in response to external reviews. A history of the
development of the VACS system is provided in Appendix 2 to Victorian Ambulatory and
Classification System (VACS) and Funding Model: A profile for 1997/98 – 2008/09 (DHS, 2008) and some key points in its development (real and potential) are highlighted earlier
in this Report. Most would agree that the introduction of the VACS classification and funding arrangements has achieved some of its architects’ expectations, especially improved
fairness in funding allocation, a better description of services provided (which supports better planning and service management) and some efficiencies. At the same time, there are difficulties in providing the right types of incentives (and not provide perverse incentives) to maintain commitment to service improvement and efficient delivery. This has especially been the case in the area of the Allied Health VACS Codes where growth in nursing led clinics under the ‘Other Allied Health’ code, the flat payment for all occasions of service, and controversy around group activities and discharge of patients from
services have resulted in diminished value of service data and growing inefficiencies in service planning and decision making. In analysing and assessing possible future changes to VACS, the following advice can be used as a benchmark:
“The value of an outpatient classification system lies in its ability to define and
reflect service patterns, while ensuring flexibility and innovation. The accuracy and
stability of the system is also important for funding purposes. The extent of data
collected must be administratively appropriate, as well as precise and clinically
meaningful.” (DHS, 2008)
H u m a n C a p i t a l A l l i a n c e
71
In previous sections of this report a range of recommended actions have been listed (18 in all) under each of the areas in which change in outpatient services delivery has been identified as desirable — the area of clinic discharge; growth in the area of new and
advanced nursing and allied health practice including support for multidisciplinary teams; reduction in the number and proportion of clinics covered under the 609 ‘Other Allied Health’ code; and group clinic services.
Overview of recommendations
The recommendations represent a series of potentially overlapping and interrelated
suggestions for improvement and can be grouped into several broad categories of proposed action as follows:
� introduction of new VACS classification codes by splitting existing 600 series
code categories into subunits as a matrix and / or by creating specifically targeted new code categories;
� changing basic elements of the VACS funding arrangement to encourage certain types of health service behaviour;
� development of protocols and guidelines to better inform clinic practitioners and managers of desired, evidence based practice approaches;
� support for dissemination of innovative models of outpatient service delivery.
Within the area of proposed changes to the VACS classification codes and associated payments, we have suggested a number of modifications. Technically the classification codes and payment arrangements are independent. In practice these are
intimately linked; one cannot introduce a new code for instance without considering the attendant payment issues. Classification changes recommended include:
� the development of differential rates of payment for ‘new’ and ‘review’ patient occasions of service as a means of improving discharge rates. It is suggested that this measure should also have applicability to medical and surgical VACS encounters.
� payment classifications for discharge and or discharge planning support could also be considered to incentivise discharge from the clinic environment.
� new classification codes to better account for and understand current ‘Other
Allied Health’ activity. At least six to seven new codes are recommended. These new codes would be subject in the same way as existing 600 series allied health codes, to the other recommendations on new and review patients, discharge planning, group clinic processes, and multidisciplinary care.
� the requirement to consider separate VACS payment classifications within the current Allied Health codes to support the provision of group sessions.
� the implementation of VACS codes to cater for Multidisciplinary Care Services
requires a clear distinction to be drawn between the allied health and nursing input in VACS weighted medical surgical clinics to those proposed within the 600 series for Multidisciplinary Care Service. For the purposes of this Review they
are seen to be quite different entities, although the opportunity exists for reconciliation within these categories during the implementation of desired new codes.
If all the recommendations on the classification system are adopted, and depending on the approach taken to modelling payment, then between 18 and 30 new codes could be added. Since the introduction of VACS few new codes have been created and calls for
new codes in recent reviews are mostly still being considered. Clearly there is concern
H u m a n C a p i t a l A l l i a n c e
72
around the expansion of VACS codes which Jackson and Sevil (1997) capture well by suggesting classification systems.
“… walk a tightrope between maintaining simplicity and accurately characterising
resource use. The former objective is maximised by reducing the number of
categories employed, and the latter by increasing the number of categories. “ (p.13)
This Review in particular supports the expansion of pre-screening services in support of specialist medical consultations and elective hospital admissions to improve the ‘front’
end experience of the patient journey and the introduction of new codes that might influence discharge and referral behaviour. The establishment of new clinics or changing the way existing clinics operate is a continuing process of change evident in most outpatient services. Stressors within the service, such as increasing patient demand, stimulate the need for these changes. The content for change though is important to get right; hence we have suggested that
clinical protocol and guidelines be developed for evidence based innovative clinic models and discharge processes. Innovation will be easier to adopt if the conditions for adoption are made simpler through generic protocols provided as a package to health services rather than an expectation that they will develop them locally. This will also
facilitate standardisation of evidence based practice across the health services. The more immediately required protocols and guidelines include:
� guidelines on the number of visits to a particular outpatients clinic that an
individual patient should make before being discharged. Upon reaching the limit triggers the requirement for a new referral from a general practitioner or specialist;
� service entry protocols that prescribe an accepted patient journey prior to entering outpatient clinic care, failing which the new patient is not accepted; and
� guidelines on the use of group clinics and the conditions under which group clinic
processes are likely to promote superior clinical outcomes to individual occasions of service.
While all the above suggestions are aimed at promoting the use of and creating a more supportive environment for better utilisation of allied health and nursing resources through optimal deployment of their skills, improved patient throughput and better use of group clinic processes, the innovations still need to be disseminated if a cost benefit is to
be realised on investment. An infrastructure that facilitates dissemination is therefore required. The literature is replete with knowledge on how to disseminate ideas quickly and turn ideas into practice adoption. Accepted wisdom dictates that word of mouth is
the most powerful means of pushing ideas; and this normally translates into fostering greater levels of communication between innovators and early adopters of innovations and the rest of the adopting population (in this case outpatient services clinicians and their management). There are already a number of collaborative and communication
events and more frequent practice based workshops and showcases would be warranted. It is a challenge, given the complex nature of the innovations we are canvassing to translate the innovation into the unique context of a specific service / clinic setting and
navigate the many potential barriers to implementation. We suggest those introducing new processes can be assisted by hands-on consulting, and that clinicians who have already successfully introduced change would make the best ‘consultants’. Such a system of peer consultants need funding support, the system cannot be expected to flourish on goodwill alone. We have therefore recommended that consideration be given to the creation of a separate fund within the Department to support an internal (to VACS funded health services) peer consultancy program for a number of years. The cost of
H u m a n C a p i t a l A l l i a n c e
73
consultancy would largely be to backfill peer consultant positions when they are providing advice and support to their fellow clinic colleagues.
In support of these movements and to help disseminate innovative practice further and faster, we have supported several recommendations from previous reviews to change the basic elements of the VACS funding arrangement. This includes introducing cost weights for VACS allied health coded clinics to better value actual service delivery
(including for group clinics). The weightings will need to be applied to the new VACS payment classifications described above.
We understand that these measures could impact on total VACS funding requirements, something which in the short term at least would be difficult to support. Without undertaking the necessary cost weight data collection and analysis it is impossible to provide actual weights to each VACS code or to estimate the direction this will take total VACS funding obligations. It is assumed that increases in some individual allied health VACS code payments could potentially be balanced by decreases in others — the key will
be whether average cost weight is lower, higher or close to the same as the current flat
payment for allied health occasions of service of $61. Caution is advised, and the use of shadow funding arrangements is suggested to ensure that any changes do not have significant unintended impacts to health services or Departmental funding arrangements.
There is also a requirement to ensure that during the setting of new weights for allied health and nursing in any new typology that the relativities are maintained between allied health, nursing and medical clinics and across any matrix that may be superimposed.
We have also suggested changes which could be applied to the setting of activity targets to promote and support the implementation of new models of care. Primarily these include the setting of clinic specific targets through temporary target extensions to
support innovative new clinics. We understand this would not be cost neutral and instead add a layer of cost (albeit marginal) on to the total VACS funding. We believe that this measure should quicken the pace of delivering greater efficiencies into the outpatient
services system in the medium term, thus providing a good return on investment. An alternative to accepting this cost would be to dissolve the differentiation between allied health and specialist medical clinic targets to allow more flexibility at a local level in
the implementation of new models. It is possible to organise any changes to activity targets for health services in such a way to ensure that the result is cost neutral if this is a desired outcome.
Alternative pathways
In the context of all of the above recommendations the major issue will be whether to
introduce cost weights to allied health activity or not. This is a significant decision that will impact on the total VACS funding costs and the way (and even whether) other recommendations are implemented.
While agreeing that this view will not perhaps be universally accepted, one can assume that calculating and assigning cost weights to each allied health code would improve the efficiency with which these services were provided as health services would be presented with better ‘pricing’ signals (consistent with actual resource use). Despite this argument,
cost weights for allied health services may nevertheless be considered too risky, either in terms of uncertainty in regard to the total VACS funding budget implications or the difficulty associated with modelling allied health service costs. Jackson and Sevel (1997) for instance noted in the early days of VACS implementation that cost data from allied
H u m a n C a p i t a l A l l i a n c e
74
health clinics was too unreliable to support extensive analysis, a view that was supported more recently by Aspex Consulting (2008).
In Table 7.1 below, the implications for all recommendations of pursuing, or not pursuing, a cost weight approach to payment modelling is considered. Table 7.1: Implications on recommendations of adopting (or not) a cost weight
approach to determining allied health VACS coded payments
Recommendation Cost weighting pathway
adopted
Cost weighting pathway
NOT adopted
‘New’ / ‘review’ patient code and payment options
This is the ideal way to deal with this issue. More exact
price placed on the ‘new’ and ‘review’ differential
Difficult to reduce the flat payment for a ‘review’
occasion of service so likely higher rate for ‘new’ OOS is required to establish a
differential. This would add to total costs unless mechanisms to lower volumes of ‘review’ patients are imposed
New Discharge planning
VACS code
Ideal way to calculate
payment
Would probably adopt
similar methodology to cost weight to develop appropriate payment option
New VACS codes from within ‘Other Allied Health’
area of activity
Ideal way to calculate payment
A flat payment arrangement, as currently
exists for all allied health OOS, could be introduced
Wiser and more appropriate use of group processes
Ideal way to calculate payment and ensure appropriate ‘price’ differential is obtained to
support sound clinical considerations for the use of group clinics
Fall back payment arrangements are able to be developed which could incentivise the appropriate
use of group processes. Need to determine a means of differentiating between different types of group
activity (e.g. purpose, size, duration)
H u m a n C a p i t a l A l l i a n c e
75
Table 7.1: Implications on recommendations of adopting (or not) a cost weight approach to determining allied health VACS coded payments (Cont.)
Recommendation Cost weighting pathway
adopted
Cost weighting pathway
NOT adopted
Introduction of multidisciplinary clinic (MDC) codes and payments
Ideal way to calculate payment
Much multidisciplinary activity, current or proposed, is within or associated with the medical
and surgical VACS codes. It is difficult to see how MDC activity could be costed independently of a cost
weighting approach. Collaborative activity which
only involves nurses and allied health practitioners could be separately costed on the basis of labour inputs (essentially the basis for the current flat allied health payment)
Setting activity targets for specific (innovative) clinics
outside the broader health service allocation
Independent of the means of calculating code payments
Development and dissemination of practice protocols and guidelines
Independent of the means of calculating code payments
Investment in increased capacity for dissemination of innovative practice
Independent of the means of calculating code payments
Construction of peer consultant capability
Independent of the means of calculating code payments
Cost implications of recommendations
Irrespective of whether a cost weight approach to allied health VACS activity payments is undertaken, most recommended areas of change can be pursued. In Table 7.2 below, the cost implications of the different recommendations of the Review for the total VACS
funding arrangements are crudely assessed.
H u m a n C a p i t a l A l l i a n c e
76
Table 7.2: Cost implications of recommendations
Recommendation Cost implications
Cost weighting pathway
adopted
Cost weighting pathway
NOT adopted
‘New’ / ‘review’ patient code and payment options
Difficult to assess. Cost of increasing payment for ‘new’ patients could be
offset by reduction in cost for ‘review’ patients if volumes are reduced.
Likely increase in cost since the only change will be to increase the payment for
‘new’ occasions of service.
New Discharge planning VACS code
Increased cost, the total dependent on the cost weighting
Increased cost
New VACS codes from within ‘Other Allied Health’ area of activity
Could be an increased cost if cost weight of new coded services are on average greater than current flat
payment
Cost neutral. Because in a flat payment arrangement, activity will simply be re-labelled but not change in
cost
Wiser and more appropriate use of group processes
Difficult to assess. Depending on the cost weight calculated, a group activity could result in a reduced cost compared with
the widespread current practice of counting each group participant as an OOS
Increases in cost could be made marginal by adjusting group payment to close to cost of a single OOS x average group size; indeed
careful adjustment could reduce costs
Introduction of multidisciplinary clinic (MDC) codes and payments
Increased cost, the total dependent on the cost weighting
Difficult to assess. Cost of collaborative activity which only involves nurses and allied health practitioners could increase in cost since presumably these are
currently counted as a single occasion of service.
Setting activity targets for specific (innovative) clinics outside the broader health
service allocation
Increased marginal cost depending on cost weight of new clinic activity
Increased marginal cost equivalent to projected clinic throughput multiplied
by the flat OOS payment
Development and
dissemination of practice protocols and guidelines
One-off cost associated with development, monitoring,
review and modification
Investment in increased capacity for dissemination of innovative practice
Short term marginal cost
Construction of peer consultant capability
Short term marginal cost until broader dissemination of innovation achieved
H u m a n C a p i t a l A l l i a n c e
77
8. References Applied Economics (2005) Assessing the Effects of the Proposed Medical Specialist Training Model on Service Delivery in Public Hospitals and Related Issues. Australian Department of Health and Ageing
Aitken, R., Faulkner, R., Bucknall, T. & Parker, J. (2001) National Review of Nursing Education: Aspects of Nursing Education: The Types Of Skills And Knowledge Required To
Meet The Changing Needs Of The Labour Force Involved In Nursing - Literature Review,
Commonwealth Department of Education and Training, Report submitted by Victorian Centre for Nursing Practice Research, School of Postgraduate Nursing, The University of Melbourne
Aspex Consulting (2008) Review of the Victorian Ambulatory Classification & Funding
System. Final Report and Implementation Plan. Department of Human Services, April 2008.
Auditor General Victoria (2006) Access to specialist medical outpatient care, Auditor Generals Office, Victoria
Centre for Allied Health Evidence Review Team (2008) A Systematic Review of the
Literature on Extended Scope of Practice Physiotherapy, Centre for Allied Health Evidence (CAHE), University of South Australia, Adelaide.
Duckett S (2007) “Outpatient Services in Queensland: Is Reform or Revolution Needed?”, Presentation to the: Improving the Delivery of Services for Outpatients Conference, Brisbane, September 2007, Accessed on 30/11/07 at: http://www.changechampions.com.au/Outpatients%2007.htm HCA (2009a) Description of Current Allied Health and Nursing Specialist Clinics at VACS Funded Victorian Public Hospitals, prepared for the Victorian Government Department of
Human Services HCA (2009b) Allied Health and Nursing - Developments in New Roles and Advanced
Practice, prepared for the Victorian Government Department of Human Services Healthcare Management Advisors (2006) Victorian Ambulatory Classification System
(VACS) clinical verification and activity audit. Department of Human Services, Victoria
Jackson, T. and Sevil, P. (1997) The Refinement of Relative Resource Weights for Non-
Admitted Patients. Centre for Health Program Evaluation, Technical Report 7, Melbourne
Kersten, P., McPherson, K., Lattimer, V., George, S., Breton, A., & Ellis, B. (2007) ‘Physiotherapy extended scope of practice: who is doing what and why?’ Physiotherapy, vol. 93 no. 4, pp235-242.
Laitner, S and Normanton, S (2007) The 18 Weeks Commissioning Pathway Template. NHS, UK
Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. (2004) ‘Substitution of doctors by nurses in primary care’ Cochrane Database of Systematic Reviews 2004, vol. 4 no. 2
H u m a n C a p i t a l A l l i a n c e
78
McPherson, K., Kersten, P., George, S., Lattimer, V., Breton, A., Ellis, B., et al. (2006) ‘A systematic review of evidence about extended roles for allied health professionals’, Journal of Health Services & Research Policy, vol. 11 no 4, pp240-247.
National Health and Hospitals Reform Commission (2008) Beyond the Blame Game:
Accountability and performance benchmarks for the next Australian Health Care
Agreement. Report of the NHHRC, April
Victorian Government Department of Human Services (2005) Victorian Ambulatory
Classification System (VACS) audit report, Summary of recommendations from
Healthcare Management Advisors Pty Ltd, Melbourne, Victoria Victorian Government Department of Human Services (2006) Care in your community: A
Planning Framework for Integrated Ambulatory Health Care, Melbourne, Victoria
Victorian Government Department of Human Services (2007) Review of the Victorian Ambulatory Classification System: Report on Consultancy Findings, Melbourne, Victoria
Victorian Government Department of Human Services (2008) Review of the Victorian Ambulatory Classification & Funding System and the DHS response to Aspex Consulting
Review, Melbourne, Victoria
Victorian Government Department of Human Services (2008) Victorian Ambulatory and
Classification System (VACS) and Funding Model A profile for 1997/98 – 2008/09, Funding Health & Information Policy Branch, (Funding Policy) of the Metropolitan Health
and Aged Care Services, Melbourne Victoria Victorian Government Department of Human Services (2009) Victorian health services
policy and funding guidelines 2009–10 Part 1: Highlights, Melbourne, Victoria Victorian Government Department of Human Services (2009) Victorian health services policy and funding guidelines 2009–10 Part 2: Policy and funding details Policy and
program initiatives, Melbourne, Victoria Victorian Government Department of Human Services (2009) Victorian Public Hospital
Specialist Clinics: Strategic Framework, Melbourne Victoria SANO Consulting (2008) Development and Pilot of a Generic Outpatient Care Pathway
Template Stage one Final Report, prepared for the Victorian Government Department of
Human Services, School of Public Health (2008) Report of Systematic Literature Review on Workforce
Models for Allied Health Professionals, Queensland University of Technology, Brisbane.
H u m a n C a p i t a l A l l i a n c e
79
Appendix A: Methodology details
The questionnaire survey
An emailed survey of nurses and allied health professionals providing specialty clinic services within the 600 series of all VACS funded health services provided the Review with data on specialty clinic service type, levels of staff expertise, scope of practice and
within that ‘advanced practice’, models of care provision, discharge issues and estimated
resource allocation including fulltime equivalent (FTE). The survey was distributed to 1720 VACS funded services. After allowing respondents more time than originally provided to form their response, all (one hundred percent) of the services participated by completing
and returning surveys for their services. A complete list of the services who participated in the survey is listed in Appendix D.
A letter of introduction to services participating in the survey listed the purpose of the
survey as being to:
1. Determine the type of allied health and nursing service provision currently
undertaken in acute hospital settings within the 601-611 VACS codes.
2. Examine the profile of clinicians working within these codes.
3. Explore the types of services that could be provided in alternative settings, and the barriers to discharge of patients from the acute service to these
alternative settings.
4. Determine what level of enhanced scope of practice is occurring in 601 - 611 codes.
5. Examine what opportunities exist for developing enhanced practice models if the appropriate circumstances were created.
6. Explore what group activity is occurring in the 601-611 VACS codes.
7. Examine what opportunities exist for conducting more group sessions if the
appropriate circumstances were created.
The survey consisted of 4 sections:
A. Section A (pages 2-6)– Tables provided relate to 601-611 VACS codes (excluding 609)
B. Section B (pages 7-10)– Tables provided relate to the 609 VACS code
only C. Section C (pages 11-12)– Tables provided relate to group services with the
601-611 VACS codes (including 609) D. Section D (pages 13 -16)– Short answer & comments regarding enhanced
practice in 601-611 VACS codes (including 609)
The survey template is included as Appendix E.
20 17 separate health services were included in the survey process (see Appendix D), however 20 completed survey forms were received by the researcher as Southern Health completed 3 surveys ( one for each of their campuses: Casey, Monash Medical Centre and Dandenong) and Eastern Health completed 2 surveys (one for each of their campuses: Box Hill and Maroondah)
H u m a n C a p i t a l A l l i a n c e
80
Survey respondents’ feedback as provided through their survey forms was entered into a database and analysed. There were some obvious issues with data quality given that each survey response was in fact a collation of many clinic responses at the
health service level. There is the possibility that some clinics’ data was not collated and therefore a health service’s data could have under-reported total allied health VACS activity at that service. There was no simple way of checking and validating the data. However the surveyed health services provided details for a total of 423,714
allied health OOS21. AIMS data, as noted in the earlier Chapter, indicated there were 530,256 service encounters in the VACS codes 601 to 611 (including 609) during the financial year 2008/2009 which equates to 357,316 when the 609 coded activity is removed. This would suggest that if anything the survey data over-estimated the clinic activity. As well, for the same reason that AIMS data is at times questioned, the survey data could have suffered from a wrong interpretation by clinic level respondents of the
intent of a particular question or the appropriate way to count activity or resources. Where possible, data was cleaned using common sense and logical rules prior to analysis.
The findings of the survey were reported in both descriptive and quantitative form.
Site visit interview consultations
In addition to the survey process, face-to-face interviews with lead nurse and senior allied health professionals working in specialty clinics located in major health services, specialist health services and major regional health services were undertaken. The interviews allowed for a more complete description of the full requirements of the
various allied health and nursing roles including:
• detailed information related to model of care provision;
• existing protocols and guidelines used to define the scope of practice of each role;
• rules around the employment of group versus 1:1 intervention process; • the perceived potential to expand the allied health contribution to the specific
specialty clinics services; • identifying potential barriers to such expansion; • data on cost factors, especially those associated with servicing patients through
group interventions. Interviews were undertaken with other key service delivery decision makers in selected services. These interview subjects were identified by the lead nurse and/or
allied health contacts, and included specialist clinic managers and relevant medical specialists. These interviews established, at a practical level:
• the perceived potential to expand the allied health contribution to the specific
specialty clinics services;
• identified potential barriers to such expansion;
• data on cost factors, especially those associated with servicing patients through
group interventions.
21 Note that AIMS data indicated there were 588382 service encounters in the VACS codes 601 to 611 (including 609) during the financial year 2007/2008 which compares with the survey findings of 423,714, minus the 609 coded activity.
H u m a n C a p i t a l A l l i a n c e
81
As well, interviews were conducted with selected individuals in the Department who were able to provide specific information on the VACS arrangements or provide policy insights to outpatient services delivery. These individuals included:
• Katy Fielding-Manager, Nurse Workforce Policy & Programs, Nurse Policy
Branch • Kathleen Philip-Manager, Workforce Innovation, Service & Workforce Planning
Branch • Terese Barton- Senior Policy Analyst, Funding Models, Metropolitan Health and
Aged Care Services
• John Bayliss-McCulloch- Manager Reform and Innovation, Funding, Health and Information Policy Metropolitan Health and Aged Care Services
• Jacqueline Martin- Senior Policy Adviser, Workforce Innovation, Service & Workforce Planning
• Christine Brackwell- Nurse Policy Branch
For a complete list of stakeholder interviewees see Appendix F. The stakeholder
interview schedules are included as Appendix G and H.
Focus group discussions
Stakeholder consultations, in the form of detailed focus group discussions with
representatives of key stakeholder groups were held for the purpose of determining the potential to expand allied health specialty clinics services, potential barriers to such expansion, and what specialty services are best placed to be offered in alternative settings.
Two main focus group discussions were held (1) with allied health mangers of outpatients services (the Allied Health Leaders Forum) and (2) with nurse managers of outpatients services (the NUMs Benchmarking Group). The names of attendees at
each of these discussion groups are provided in Appendix F. Additional focus group discussions were planned particularly with specialist medical practitioner stakeholders and possibly also general practitioner representative groups, but these were ultimately
deemed to be unnecessary at this point in time. The focus group discussions largely centred on the initial response to and analysis of the survey questionnaire. In this way, specific issues that seem to be emerging from
the survey data could be explored and validated or better understood. Some of the key questions were:
� Levels of expertise and scope of practice – trying to understand advanced practice roles not captured by survey – for instance roles not funded by VACS or being performed in non 600 series (medical and surgical) VACS coded clinics;
� VACS Funding service shortfall – exploring the cost of providing service in excess of the standard VACS payment because of additional work (e.g. education) or resource / consumable requirements;
� Potential for service to be offered by alternate providers. The following statement was provided by a health service survey respondent and the
proposition was put to participants for their feedback on wether they felt the statement was accurate and widespread and relevant to health service providers at large, or if they thought it was a one off happening specific only to the health service provider who completed the survey:
H u m a n C a p i t a l A l l i a n c e
82
‘There is considerable unmet demand for [allied health] in the general population. This is because access to publicly funded services is very limited and Medicare EPC funding is very limited also. This results in many patients
presenting to public hospital specialist clinics with conditions which could be easily managed by [allied health profession] in the community in the acute stages’.
� Opportunities for allied health enhanced practitioners and advanced practice nurses to provide specialist clinics;
� Group processes, their value and when they should be used.
Literature review
A wide ranging literature review of what specialty allied health and/or advanced nursing services are currently in use or being trialled in other jurisdictions in Australia and in the UK, Canada and other countries with similar health systems looked at potential for expansion. A systematic review of the literature ensured an effective
search strategy and rigour in the approach. Effort was made to collect and collate existing documentation previously gathered by the Department, various stakeholders and HCA itself. This was supplemented by an
extensive search of the web and relevant abstract databases. Any comprehensive literature search in this area (with so many key search criteria and many labour categories) would, and indeed did, uncover a large number of literature sources. To
manage the volume of papers an initial data reduction strategy was employed to isolate 'high-value' literature sources relevant to the project objectives. In particular, the strategy was to identify existing systematic reviews and interrogate them against each other for their overlap (temporal overlap, discipline overlap and content overlap)
and their gaps. 'High-value' was defined in terms of the project purpose by reference to a range of factors (Boyce, 2009) which included robustness of study design, relevance to project objectives, inclusion of multiple allied health professions and or multiple cases, inclusion of evaluation measures, particularly patient-centred health outcomes, included a critical analysis of what constituted advanced practice or extended scope of practice, and explicitly discussed limitations in the study design. Seven ‘high-value’ papers were identified.
H u m a n C a p i t a l A l l i a n c e
83
Appendix B: Growth in medical
specialist trainees
Medical Course Completions / Graduate supply: Historical and Projected Time
Series - 1995 to 2015
0
500
1000
1500
2000
2500
c
o
m
p
l
e
t
i
o
n
s
1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015
Year of course completion
Domestic International
H u m a n C a p i t a l A l l i a n c e
84
Appendix C: Allied Health
Outpatient OOS Targets Actual and target Allied Health Outpatient OOS for 2007-0822 are provided in the Table below.
Health service Actual Target Difference
(Target – actual)
Alfred Hospital 41,518 40,415 -1,103
Austin & Repatriation Med Centre 77,723 50,838 -26,885
Ballarat Health Services 10,843 10,973 130
Barwon Health 32,235 33,500 1,265
Bendigo Healthcare Group 15,703 18,468 2,765
Box Hill Hospital 11,197 11,133 -64
Dandenong Hospital 25,212 14,568 -10,644
Monash Medical Centre 32,720 46,874 14,154
Frankston Hospital 16,882 17,762 880
Mercy Public Hospital 24,833 27,727 2,894
Northern Hospital 25,265 25,175 -90
Peter MacCallum Cancer Institute 26,366 23,793 -2,573
Royal Children's Hospital 68,196 68,458 262
Royal Melbourne Hospital 27,365 26,287 -1,078
Royal Victorian Eye and Ear 67,641 67,477 -164
Royal Women's Hospital 28,929 25,251 -3,678
St Vincent's Hospital 24,420 22,218 -2,202
Sunshine / Western Hospital 31,334 36,212 4,878
588,382 567,129
Source: AIMS data (2009)
22 This is the last year for which complete actual OOS are available. Totals include both ‘Public’ and ‘Department of Veterans Affairs’ outpatients.
H u m a n C a p i t a l A l l i a n c e
85
Appendix D: Survey respondents
Services AUSTIN HEALTH ALFRED HEALTH BALLARAT HEALTH BARWON HEALTH BENDIGO HEALTH CARE GROUP
EASTERN HEALTH (Box Hill Hospital & Maroondah Hospital) SOUTHERN HEALTH (Dandenong Hospital & Monash Medical centre plus VACS held at Moorabbin Hospital) PENINSULA HEALTH (Frankston Hospital)
MERCY HEALTH & AGED CARE (Mercy Public Hospital Heidelberg)
PETER MacCALLUM CANCER CENTRE
ROYAL CHILDRENS HOSPITAL
ROYAL MELBOURNE HOSPITAL
ROYAL VICTORIAN EYE AND EAR HOSPITAL
ROYAL WOMENS HOSPITAL
ST VINCENT'S HOSPITAL
WESTERN HEALTH (Footscray Hospital & Sunshine Hospital)
NORTHERN HEALTH
H u m a n C a p i t a l A l l i a n c e 86
Appendix E: Survey Instrument
Section A – 601- 611 VACS codes 1:1 contacts (EXCLUDING 609 “other”)
Question 1: Describe the current activity of allied heath resources in each of the selected VACS codes at your service by completing the following table. (Space has been provided for only one OOS under each allied health discipline. Insert more rows if the space provided is insufficient, for clarity please ‘label’ each separate OOS reported upon.)
VAC
S
Code
VACS descriptor Primary
purpose
How
many
(OOS)
per
year
Total clinical time spent
face-to-face with patients
per OOS
Approximate clinician EFT and grading
(e.g., 0.6 EFT of grade 2 physio)
601
Audiology
( ) consultation ( ) education ( ) treatment
EFT____ Grade & Discipline_____ EFT ____ Grade & Discipline_____
602 Nutrition
( ) consultation ( ) education
( ) treatment
EFT____ Grade & Discipline_____ EFT ____ Grade & Discipline_____
603 Optometry
( ) consultation ( ) education ( ) treatment
EFT____ Grade & Discipline_____ EFT ____ Grade & Discipline_____
604 Occupational
Therapy
( ) consultation ( ) education ( ) treatment
EFT____ Grade & Discipline_____ EFT ____ Grade & Discipline_____
H u m a n C a p i t a l A l l i a n c e 87
VAC
S
Code
VACS descriptor Primary
purpose
How
many
(OOS)
per
year
Total clinical time spent
face-to-face with patients
per OOS
Approximate clinician EFT and grading
(e.g., 0.6 EFT of grade 2 physio)
605 Physiotherapy
( ) consultation ( ) education ( ) treatment
EFT____ Grade & Discipline_____ EFT ____Grade & Discipline ______
606 Podiatry
( ) consultation ( ) education
( ) treatment
EFT____ Grade & Discipline_____ EFT ____Grade & Discipline______
607 Speech Pathology
( ) consultation
( ) education ( ) treatment
EFT____ Grade & Discipline_____
EFT ____Grade & Discipline______
608
Social Work
( ) consultation ( ) education
( ) treatment
EFT____ Grade & Discipline_____ EFT ____Grade & Discipline______
610 Cardiac
Rehabilitation
( ) consultation ( ) education ( ) treatment
EFT____ Grade & Discipline_____ EFT ____Grade & Discipline______
611 Hydrotherapy
( ) consultation
( ) education ( ) treatment
EFT____ Grade & Discipline_____
EFT ____ Grade & Discipline______
H u m a n C a p i t a l A l l i a n c e 88
Section A – 601-611 VACS codes 1:1 contacts (EXCLUDING 609 “other”)
Question 2: For each of the selected 1:1 VACS codes at your service, please nominate the type and level of staff and provide an example of ‘typical’ activity within the each code. Please note if you believe this to be ‘enhanced practice’, and the profile of staff performing the enhanced activity. Under each VACS code you may allow for more than one OOS– (please add rows if further space is required).
VACS
code
VACS
descriptor
Description of
typical activity Description of
enhanced practice
activity (if any)
Qualifications and
/or additional
training required to
complete the
advanced tasks
required
Approximate EFT and grade of staff
performing enhanced practice
activity
(e.g. 0.2 EFT grade 3 OT)
601 Audiology EFT______ Grade & Discipline_________ EFT ______ Grade &
Discipline_________
602 Nutrition EFT______ Grade & Discipline_________
EFT ______ Grade & Discipline_________
603 Optometry EFT______ Grade &
Discipline_________ EFT ______ Grade & Discipline_________
604 Occupational Therapy
EFT______ Grade & Discipline_________ EFT ______ Grade & Discipline_________
605 Physiotherapy EFT______ Grade & Discipline_________ EFT ______ Grade &
Discipline_________
606 Podiatry EFT______ Grade &
H u m a n C a p i t a l A l l i a n c e 89
Discipline_________ EFT ______ Grade &
Discipline_________
607 Speech Pathology
EFT______ Grade & Discipline_________
EFT ______ Grade & Discipline_________
608 Social Work EFT______ Grade &
Discipline_________ EFT ______ Grade & Discipline_________
610 Cardiac Rehabilitation
EFT______ Grade & Discipline_________ EFT ______ Grade & Discipline_________
H u m a n C a p i t a l A l l i a n c e 90
Section A – 601-611 VACS codes 1:1 contacts (EXCLUDING 609 “other”) Question 3: For each of the selected 1:1 VACS codes at your service, please nominate the new patient vs. review patient ratio, suggest the average number of reviews per patient, and suggest any barriers to discharge. Within each VACS code you may allow for more than one OOS (please add rows if further space is required).
VACS
code VACS descriptor
New:
Review
ratio
Average
number of
reviews per
patient
Are there any barriers to discharge from this clinic? (if
yes, please list what these are)
601 Audiology
602 Nutrition
603 Optometry
604 Occupational Therapy
605 Physiotherapy
606 Podiatry
607 Speech Pathology
608 Social Work
610 Cardiac Rehabilitation
611 Hydrotherapy
H u m a n C a p i t a l A l l i a n c e 91
Section A – 601-611 VACS codes 1:1 contacts (EXCLUDING 609 “other”) Question 4: Stakeholders at several services have described how selected interventions have potential to offer more efficient / effective service by alternate providers (i.e. community or sub-acute). If services were available in the community, what % of your work could be done in the community by a community provider? For only those “600” VACS codes at your service where this has been done in the last 2-3 years or would like to in the near future, please indicate the potential for change to a community provider (if the appropriate services existed in the community and there were no barriers to discharge). N.B. This question is not about outreach VACS codes, but alternative providers. Under each VACS code you may allow for more than one OOS-(please add rows if further space is required).
VACS
code VACS descriptor
% of
consultations that
could be offered
by alternate
providers
Suggest alternate
provider (eg, GP,
Community Health
Centres, Sub-Acute)
Rationale for being able to provide this
consultation in an alternate setting
601 Audiology
602 Nutrition
603 Optometry
604 Occupational Therapy
605 Physiotherapy
606 Podiatry
607 Speech Pathology
608 Social Work
610 Cardiac Rehabilitation
611 Hydrotherapy
H u m a n C a p i t a l A l l i a n c e 92
Section B - 609 VACS code (“other allied health” – includes nursing services)
The clinics that are funded under the 609 VACS code are of special interest.
Question 5a: Please list all the 609 NURSING clinics operating at your service and for each listed service complete the following table.
Nursing resource requirements Enhanced activity
Clinic
name
Generalis
t Nurse
input
(Note Div 1
or 2)
How
many
clinics
per
year
What is
the
average
clinical
time spent
with
patients
per clinic
Descriptio
n of
typical
activity
Description
of enhanced
activity (if
any)
Specialist
qualifications and /or
additional training
required for nurse to
complete the advanced
tasks
Grade and
approximate EFT of
staff performing
enhanced practice
activity (e.g. 0.6 EFT
of Grade 3 nurse or
0.8 EFT of Div 2
nurse)
Wound
clinic
� Div 1 � Div 2
EFT_____ Grade______ EFT_____ Grade______
� Div 1
� Div 2
EFT_____ Grade______
EFT_____ Grade______
� Div 1
� Div 2
EFT_____ Grade______
EFT_____ Grade______
H u m a n C a p i t a l A l l i a n c e 93
Section B - 609 VACS code (“other allied health” – includes nursing services)
Question 5b: Please list all the 609 ALLIED HEALTH VACS OOS operating at your service and for each listed service complete the following table.
Allied Health resource requirements Enhanced activity
VACS
descriptor
/
name
Allied
health
input:
discipline
(e.g., orthoptist)
How
many
OOS
per
year
What is
the
average
clinical
time spent
with
patients
per OOS
Descriptio
n of
typical
activity
Descriptio
n of
enhanced
activity (if
any)
Specialist
qualifications
and /or
additional
training
required to
complete the
advanced tasks
Approximate EFT and Grade of
staff performing Enhanced
activity (if any) (e.g. 0.4 EFT
grade 2 orthoptist)
EFT_____ Grade & Discipline______
EFT_____ Grade & Discipline______
EFT_____ Grade &
Discipline______ EFT_____ Grade & Discipline______
EFT_____ Grade & Discipline______ EFT_____ Grade & Discipline______
EFT_____ Grade & Discipline______ EFT_____ Grade & Discipline______
H u m a n C a p i t a l A l l i a n c e 94
Section B – 609 VACS code (“other allied health” – includes nursing services)
Question 6: For each of the“609” VACS codes at your service, please nominate the new vs. review ratio, suggest the average number of reviews per patient, and suggest any barriers to discharging from the clinic. Within each VACS code you may allow for more than one description– (please add rows if further space is required).
609 - Other
Allied Health
Services
(includes
nursing):
E.g. orthoptics
New vs.
Review
ratio
Average number of
reviews per patient
Are there any barriers to discharge from this service? (if yes,
please indicate what they are)
H u m a n C a p i t a l A l l i a n c e 95
Section B - 609 VACS code (“other allied health” – includes nursing services)
Question 7: Stakeholders at several services have described how selected codes have potential to offer more efficient/ effective services by an alternate provider (e.g. community or sub-acute). If services were available in the community, what % of your work could be done in the community by a community provider? For only those 609 VACS codes at your service where this has been done in the last 2-3 years or would like to in the near future, please indicate the potential for change to a community provider. (if the appropriate services existed in the community and there were no barriers to discharge).
N.B. This question is not about outreach services, but alternative providers
Within each 609 VACS code you may allow for more than one description--(please add rows if further space is required).
609 Other
Allied Health
Services
(includes
nursing)
(e.g. orthopist)
% of consultations that
could be offered by
alternate providers
Suggest alternate provider (e.g.
GP, Community Health Centres,
Sub-Acute)
Rationale for being able to provide this
consultation in an alternate setting
H u m a n C a p i t a l A l l i a n c e 96
Section C - Groups
Please provide a definition of “group” as it is applied in your specialist clinics (outpatients):________________________
______________________________________________________________________________________________________
Question 8: In the table below, please describe the current type and the amount of GROUPS within each of the VACS categories at your service. You can provide separate details within each VACS Code area: (please add rows if further space is required). This question applies to all categories from 601-611
VACS
Code
VACS
descripto
r
Purpose of
group
Average patient
number of patients
per group
Individual or
group care
plans
Average duration of
group (please
include set up,
service and
completion tasks)
Approximate EFT
and actual % of
time clinician
spends doing
group
601 Audiology ( ) consultation
( ) education ( )
treatment
( ) individual ( ) group
602 Nutrition
( ) consultation ( ) education ( )
treatment
( ) individual ( ) group
603 Optometry
( ) consultation ( ) education
( ) treatment
( ) individual
( ) group
604 Occupational Therapy
( ) consultation ( ) education
( ) treatment
( ) individual
( ) group
H u m a n C a p i t a l A l l i a n c e 97
VACS
Code
VACS
descripto
r
Purpose of
group
Average patient
number of patients
per group
Individual or
group care
plans
Average duration of
group (please
include set up,
service and
completion tasks)
Approximate EFT
and actual % of
time clinician
spends doing
group
605 Physiotherapy
( ) consultation ( ) education
( ) treatment
( ) individual
( ) group
606 Podiatry
( ) consultation ( ) education ( ) treatment
( ) individual ( ) group
607 Speech Pathology
( ) consultation ( ) education
( ) treatment
( ) individual
( ) group
608 Social Work
( ) consultation ( ) education ( )
treatment
( ) individual ( ) group
609 Other Allied Health Services
( ) consultation ( ) education ( ) treatment
( ) individual ( ) group
610 Cardiac Rehabilitation
( ) consultation ( ) education ( )
( ) individual ( ) group
H u m a n C a p i t a l A l l i a n c e 98
VACS
Code
VACS
descripto
r
Purpose of
group
Average patient
number of patients
per group
Individual or
group care
plans
Average duration of
group (please
include set up,
service and
completion tasks)
Approximate EFT
and actual % of
time clinician
spends doing
group
treatment
611 Hydrotherapy
( ) consultation ( ) education
( ) treatment
( ) individual
( ) group
H u m a n C a p i t a l A l l i a n c e 99
Section D – Short answers
Question 9a: Stakeholders at several services have described how selected VACS codes/clinics are more efficient/ effective due to increased input and scope of practice of specialist nurses & allied health practitioner. Are you considering any 601-611 VACS codes/clinics at your service where you could operate increased scope of practice? If so please identify which code/clinic and nominate which clinicians would provide this service. Please provide a description of activities that would constitute enhanced practice.
H u m a n C a p i t a l A l l i a n c e 100
Section D – Short answers
Question 9b: If appropriate conditions were created, please indicate if there is a possibility of increasing groups. Please list the groups and which clinicians would provide this service
H u m a n C a p i t a l A l l i a n c e 101
Section D – Short answers
Question 10: Please provide details of any high cost consumables required to provide patient care within the 601-611 VACS code/clinics including 609 (e.g. dressing products for wound clinic)
H u m a n C a p i t a l A l l i a n c e 102
Section D – Short answers
Question 11: Please provide any comments or suggestions you may have relating to the review of 601-611 VACS codes/ clinics (including 609).
H u m a n C a p i t a l A l l i a n c e
103
Appendix F: Stakeholder
Consultations Name Position
Bendigo Health Care Group
Dan Douglas Manager Allied Health Out Patent Services
Robert Porter Business Director Surgical Services
Leanne Anderson Project Officer Out Patent Services
Carol Ann Lever Nurse Unit Manager Out Patient Services
Ballarat Health
Wendy Hubbard Executive Director Allied Health
Janine Harris Services Director Outpatients
Dr Mark Yates Internal Medical Services Director
Austin Health
Dr Paul Mitchell CSU Medical Director Outpatients
Melinda Cosgriff Chair, Specialist Clinics Nurse Unit Managers
Benchmarking Group
Belinda Rickard Outpatient Improvement Lead
Wendy Driver Outpatient Nurse Unit Manager
Cathy Niall Director of Physiotherapy
Tony McHugh Mental Health Manager
Umit Agis Mental Health Community Manager
Rhy Gould Management CSU Director Outpatients
Dr John Ferguson Chief Medical Officer
Melbourne Health
Dr Peter Bradford Executive Director Clinical Governance and Medical Services
Leonie Carberry Nurse Unit Manager Outpatient Services
Debbie Munroe Senior Physiotherapist
Denise Heinjus Adjunct Professor, Executive Director of Nursing
Western Health
Silvio Pontonio Allied Health Leaders Executive Director, Community Integration and Allied Health
Natasha Toohey Allied Health Leaders Director, Community Integration and Allied Health
Southern Health
Emma Geor Occupational Therapy Manager
Sharon Dadson Director of Nursing Outpatient Services
Greg Young General Manager Acute Ambulatory Services
Kim Griffiths Occupational Therapist, Hand Therapy Team
Project Steering Group Members
Lyndell Keating Allied Health Managers Group
Allied Health Leaders Forum
Wendy Hubbard Exec Director Sub-acute and Community (Chief Allied Health Officer) - Ballarat Health Services
Janne Williams Director of Allied Health – RASP – Southern Health
Athina Georgiou Director of Allied Health – Acute – Southern Health
Lyndell Keating Director of Allied Health – Alfred Hospital
H u m a n C a p i t a l A l l i a n c e
104
Lauren Andrew Director of Allied Health – Royal Children’s Hospital
Debbie Schulz Director of Allied Health – Barwon Health
Gayle Sammut Director of Allied Health – Goulburn Valley Health
Janine Holland Director of Allied Health – Wangaratta Health
Jackie Martin Allied Health Team Leader, Senior Policy Adviser – Department of Human Services
NUMs Benchmarking Group
Melinda Cosgriff NUMs Benchmarking Group Chair
Wendy Driver Austin Health
Melanie Koscik Southern Health
Marie Wintle Box Hill Hospital
Michelle Morrow Mercy Health & Aged Care
Shay Morrissey Peter MacCallum Cancer Centre
Leonie Carberry Royal Melbourne Hospital
Natalie Smyth Western Health
Leanne Shea Ballarat Health
Eng Byrne William Angliss Hospital
Julie Swanson Western Health
Paula Henessey
Lisa Adair Barwon Health
Philomena O'Neill St Vincents Hospital
H u m a n C a p i t a l A l l i a n c e
105
Appendix G: Interview Schedule
for Key Health Service Contacts
Part 1 - Determine the type of allied health and advanced nursing service
provision currently undertaken in acute settings.
Questions 1 How many VACS funded outpatient clinics are operating in the Health Network? Identify specific AH specialties that might be separately categorised from within the 609 "other" group (eg, orthoptists, psychologists) What is the % of nurse-led & AH led clinics What % of clinics have a significant proportion of AH & nursing contribution
For each VACS funded outpatient clinic describe the service provided and by whom?
How much of the service is consultation only?
What time periods are allowed for each consultation? How long is the average consultation where an intervention is required? What interventions are employed?
Identify allied health-led and managed VACS funded clinics. Identify nurse-led and managed VACS funded clinics. Identify medical-led and managed VACS funded clinics. Identify mixed skill VACS funded clinics.
Identify the staff EFT and skill mix required to run each clinic Identify any specific high cost consumables that are required for these clinics?
Provide contact information for each clinic manager
Part 2 - Identify interventions that need to occur in acute settings, and those
that can be provided in alternate settings.
Questions 2 For each VACS funded outpatient clinic identify interventions that can only be undertaken in an acute care setting? What are the barriers to providing these in a non-hospital based environment?
Identify the interventions that could be provided in an alternative setting. What is the typical destination of the patient after treatment at this clinic? Who determines readiness for discharge? (doctor, nurse, AH?)
Part 3 - Identify the barriers of providing services in alternate settings and
make recommendations for addressing these barriers
Questions 3
Do you know of any new innovative models for specialty clinics that should be considered if relocation is an option?
Part 4 - Provide recommendations for the business rules around group allied
health sessions.
Questions 4 What model of service should be considered for allied health and nurse-led
specialist clinics?
H u m a n C a p i t a l A l l i a n c e
106
What is the likely composition of the new model (staff mix/skills, duration, number of patients per session, individual or group care plans/programs)
What are the key factors to be considered in a funding model (under the VACS framework) to support the implementation of these clinics? Is there a place for group sessions in specialist clinics for patients with similar health needs. Nominate what types of clinics you think would be suitable for
group sessions.
Part 5 - Define the role of allied health and advance nurse practitioners in
specialist clinics, examine the level of competency and the appropriate
funding arrangements needed to support opportunities for enhanced
scope of practice in specialist clinics.
Questions 5 From your experience what do you believe is the role of allied health and
advanced nurse practitioners in specialist clinics? What level of competency is required for each health professional providing a specialist clinic service? What if any additional educational requirement or training do you believe are
needed for nurses and allied health to undertake these roles?
What funding arrangements are needed to support opportunities for enhanced scope of practice in specialist clinics?
What pre-requisite qualifications would be required to meet the level of competency?
What level of competency would they require relating to the role they are performing?
What grade/level does the nurse/AH clinician need to be employed at?, eg could
intervention be provided by a grade 2 physio/grade 2 nurse (or Div 2 nurse)? or would they need to be grade 4 physio, or grade 4 nurse?
What governance arrangements needed to support enhanced practice: are there issues for the service around professional indemnity etc?
Would these services be directly substitutable for med/surg led clinics?
Is there an opportunity to better manage access and waitlists for the clinic by utilising AH & nursing clinicians in enhanced models of care?
H u m a n C a p i t a l A l l i a n c e
107
Appendix H: Interview Schedule
for Key Interest Groups
Questions re survey findings:
1. Mapping of VACS allied health and advanced nursing clinics 2. Levels of Expertise & Scope of practice - Enhanced scope of practice roles not
captured by survey – roles not funded by VACS Sample Statement #1: Many enhanced nursing practices currently performed in outpatients do not come under 609 VACS therefore the scope of this survey has not captured all advanced
nursing practices. E.g. management of plasters including manipulation & training of junior medical staff, family planning counselling, pre-clinic cardiology assessments , complex wound care management, infectious diseases patient education, to name a few.
3. VACS Funding service shortfall - Cost of providing service in excess of VACS
payment including 10% base and 7% education
Sample Statement #3: VACS does not give sufficient funding to cover the time and consumables needed to provide podiatry services to High Risk and complex patients. Consultation/treatment time is generally 45-60 minutes or longer per patient and
consumables can be quite expensive. All this time and product expense is still cheaper than an inpatient stay.
4. Potential for service to be offered by alternate providers Sample Statement #5: There is considerable unmet demand for physiotherapy in the general population. This is because access to publicly funded services is very limited and Medicare
EPC funding is very limited also. This results in many patients presenting to public hospital specialist clinics with conditions which could be easily managed by physiotherapists in the acute stages.
5. Opportunities for allied health enhanced practitioners and advanced practice nurses to provide specialist clinics. Sample Statement #1:
The funding structure of allied health VACS (601 -611) does not support substitution of current medical VACS funded clinics. The establishment of nurse-led services is prohibited by the cost of such services.
6. Groups
7. Other
Sample Statement #4: This survey does not seem to capture the resources required to manage discipline specific outpatient services, i.e. all OP services provided by Nutrition and planned, coordinated and evaluated by the Departmental manager. The cost of educational resources such as printed material is also not accounted for.
H u m a n C a p i t a l A l l i a n c e
108
Questions re areas not captured by survey findings:
Services funded by multiple sources Medical VACS considered income. Allied Health VACS services considered a cost.
Barriers to changing VACS funded services
Allied health and advanced nursing contribution to medical VACS in excess of 15%