Does midtrimester cervical length ≥25 mm predict preterm birth in high-risk women?
Transcript of Does midtrimester cervical length ≥25 mm predict preterm birth in high-risk women?
Does Mid-trimester Cervical Length ≥ 25 mm Predict Preterm Birthin High-Risk Women?
John Owen, MD, MSPH1, Jeff M. Szychowski, PhD2, Gary Hankins, MD3, Jay D. Iams, MD4,Jeanne S. Sheffield, MD5, Annette Perez-Delboy, MD6, Vincenzo Berghella, MD7, Deborah A.Wing, MD8, and Edwin R. Guzman, MD9 for the Vaginal Ultrasound Trial Consortium1Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University ofAlabama, Birmingham (AL)2Department of Biostatistics, University of Alabama, Birmingham (AL)3Department of Obstetrics and Gynecology, University of Texas Medical Branch, Galveston (TX)4Department of Obstetrics and Gynecology, The Ohio State University Medical Center, Columbus(OH)5Department of Obstetrics and Gynecology, University of Texas Southwestern Medical Center,Dallas (TX)6Department of Obstetrics and Gynecology, College of Physicians and Surgeons, ColumbiaUniversity, New York, (NY)7Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Thomas JeffersonUniversity, Philadelphia (PA)8Department of Obstetrics and Gynecology, University of California, Irvine, Irvine (CA)9Department of Obstetrics and Gynecology, Saint Peter’s University Hospital, New Brunswick (NJ)
AbstractObjective—To assess pregnancy outcome along a continuum of cervical lengths ≥25 mm.
Study Design—Planned secondary analysis of a randomized cerclage trial of women with priorspontaneous preterm birth 170–346/7 weeks. Outcomes of women who maintained cervical lengths≥25 mm were analyzed. Women with cervical lengths <25 mm randomized to no cerclage comprisedan internal comparison group.
Results—Of 1014 screened, 153 had cervical length <25mm, and 672 had cervical length ≥25 mm.Birth <35 weeks occurred in 16% of the ≥25 mm cohort. The relationship between cervical lengths≥25 mm and birth gestational age was null (p=0.15). In the <25 mm group, progressively shortercervical lengths predicted birth <35 weeks (p<0.001); this relationship was null in the ≥25 mm group(p=0.17).
Conclusion—The continuum of cervical lengths ≥25 mm measured between 160/7 and 226/7 weeksdoes not predict gestational length in women with prior spontaneous preterm birth.
© 2010 Mosby, Inc. All rights reserved.Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customerswe are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resultingproof before it is published in its final citable form. Please note that during the production process errors may be discovered which couldaffect the content, and all legal disclaimers that apply to the journal pertain.Oral abstract presentation at the annual Society of Maternal-Fetal Medicine Meeting, February, 2010 in Chicago, IL.
NIH Public AccessAuthor ManuscriptAm J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
Published in final edited form as:Am J Obstet Gynecol. 2010 October ; 203(4): 393.e1–393.e5. doi:10.1016/j.ajog.2010.06.025.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Keywordscervical length; prior preterm birth; vaginal sonography; preterm birth prediction
A prior spontaneous preterm birth is one of the strongest historical predictors of recurrence,and sonographic evaluation of the cervix, especially shortened cervical length, has consistentlybeen shown to be an effective predictor of preterm birth (1). Though not recommended forroutine use in low-risk or unselected populations (2), cervical length screening appears to havethe most clinical utility in high-risk populations (3,4). Previous reports have described theassociation between shortened cervical length below a prescribed cutoff and the risk of pretermbirth (4,5,6). The use of a 25 mm cutoff in the midtrimester has been utilized by investigatorsand clinicians to identify women at the highest risk of preterm birth. This cutoff threshold valueis the lower 10th percentile in both unselected (7) and high-risk (3) populations. The 25 mmthreshold has also been utilized as the basis for cerclage intervention trials (8,9,10,11)
Systematic reviews (4,5,6) confirm a consistent relationship between short cervix and earlierbirth in various populations, but, using the native reports which populated the reviews, theseinvestigators primarily sought to summarize and compare sensitivities, specificities andlikelihood ratios for preterm birth at various cervical length and gestational age thresholds.None specifically evaluated the continuum of cervical lengths above a specified threshold forthe prediction of preterm birth, as the outcomes of patients with longer cervical lengths weresimply pooled in order to calculate the screening test characteristics. Iams and colleagues inthe NICHD MFM units network (7) evaluated nearly 3000 unselected women at 24 weeks’gestation and found increasing relative risks of preterm birth with cervical shortening usingthe upper quartile > 40 mm as the referent group; however, the trend in rates of preterm birthassociated with cervical lengths above the 25 mm threshold was not formally evaluated.
To improve clinical decision making, patient selection for intervention trials and ourunderstanding of the preterm birth syndrome (12), the risks of preterm birth associated withlonger cervical lengths in high-risk women requires further characterization. Our nullhypothesis was that the continuum of cervical lengths above a 25 mm cervical length thresholdwould not be associated with pregnancy duration in women with prior preterm birth.
METHODSThis is a planned secondary analysis of a randomized clinical trial performed by a consortiumof 15 U.S. Centers between January, 2003 and November, 2007 (Owen, 2009). Multiparouswomen carrying a singleton and who had experienced at least one prior spontaneous pretermbirth between 170/7 and 336/7 weeks’ gestation, confirmed by a review of the patient’s medicalrecords, underwent serial vaginal sonographic assessment of cervical length. Exclusion criteriawere fetal anomaly, planned history-indicated cerclage for a clinical diagnosis of cervicalinsufficiency, and clinically significant maternal-fetal complications. Other details of the studyprotocol are described elsewhere (11)
Sonologists underwent a uniform certification process by a single investigator (J.O.) to ensureuniformity in sonographic equipment, measurement technique, completion of study forms, andadherence to protocol. Specifics of this sonographic evaluation based on the technique of Iamshave been previously described (7): the cervical length at each visit was measured along aclosed endocervical canal, where minimal degrees of apparent dilation (i.e. echolucency alongthe entire canal) less than 5 mm were considered closed. Fundal pressure was also applied for30 seconds by the sonologist as a provocative maneuver, and each scan included an evaluationperiod of at least 5 minutes to detect spontaneously occurring cervical shortening. The shortest
Owen et al. Page 2
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
cervical length for each examination that clearly displayed the internal and external cervicalos with equivalent thickness of the anterior and posterior cervix was recorded as the cervicallength, regardless of whether the measurement was obtained with pressure or was the result ofspontaneous dynamic shortening. Managing physicians were masked to the results of thesonographic evaluations except in cases of complete placenta previa, oligohydramnios or fetaldeath.
The first sonographic assessment was scheduled in the gestational age window 160/7 to 216/7
weeks’ gestation. Subsequent evaluations were scheduled every 2 weeks. If the cervical lengthwas observed to be 25–29 mm, scans were scheduled weekly. If on any evaluation the cervicallength was < 25 mm, the woman became eligible for randomization to cerclage or to a no-cerclage group. Women with a cervical length that remained at least 25 mm at the finalsonographic evaluation, scheduled to be no later than 226/7 weeks, were ineligible forrandomization and comprised the ≥ 25 mm cohort. We also compared their outcomes to aninternal control group of women who qualified for the trial based on a cervical length < 25 mmand were randomized to no cerclage. The protocol and consent forms received localinstitutional review board approval at all centers.
Categorical variables were analyzed with chi-square or the Mantel-Haenszel test of trend, whilecontinuous variables were compared using a t-test or Wilcoxon rank-sum test. Linearregression modeled the association between 2 continuous variables. Differences in time to birthwere assessed by Kaplan-Meier curves and the log-rank test. Multivariable Cox proportionalhazard models considered possible confounders for time to birth. An alpha level of 0.05 wasselected to represent statistical significance. Analyses were performed using SAS 9.2 (Cary,NC).
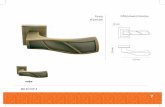
RESULTSA total of 1014 eligible women gave consent and underwent their initial sonographicassessment of cervical length. From this cohort, we observed 318 (31%) who experiencedcervical length shortening less than 25 mm. Sixteen patients did not consent to randomization,and 302 (95%) entered the randomized trial; 153 were assigned to the no-cerclage cohort. Ofthe 696 who underwent their initial scan and failed to shorten to < 25 mm, delivery outcomeswere available in 672 (96.6%); these comprised the ≥ 25 mm cohort (Fig. 1). Selectedcharacteristics of the 2 study cohorts are shown in Table 1. As anticipated, the cohorts differedwith regard to several characteristics.
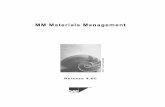
The rates of birth < 35 weeks were 42% in the < 25 mm internal comparison cohort and 16%in the ≥ 25 mm cohort (p < 0.0001). There was a non-significant association between cervicallength (predictor variable) and birth gestational age in the ≥ 25 mm cohort using a linearregression model (p = 0.15). Figure 2 depicts the relationship between cervical length groupsand birth < 35 weeks, both in the < 25 mm internal comparison cohort and also in the ≥ 25 mmcohort: the relationship between cervical length group and birth < 35 weeks in the < 25 mminternal comparison cohort, assessed with a test of trend, was statistically significant (p < 0.001)while the analogous comparison in the ≥ 25 mm cohort was not significant (p = 0.17). Themean gestational ages at birth were 26, 31, 33, and 35 weeks in the < 10 mm, 10–14 mm 15–19 mm and 20–24 mm groups respectively that comprised the internal control, no-cerclagecohort. The corresponding birth gestational ages in the failed-to-shorten cohort for cervicallength groups 25–29 mm, 30–34 mm, 35–39 mm, 40–44 mm, 45–50 and ≥ 50 mm groups were,37, 37, 37, 38, 38 and 38 weeks respectively.
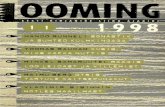
Finally, we chose to examine the relationship between cervical lengths near the 25 mm cutoff,i.e. 25–29 mm and longer cervical lengths of 30 mm or greater. As depicted in Figure 3, the
Owen et al. Page 3
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Kaplan-Meier survival analysis, comparing the 25–29 mm and ≥ 30 mm subgroups andconsidering the event time to birth (i.e. percent undelivered), was statistically significant (log-rank test p = 0.02). However, in a multivariable Cox proportional hazards model, controllingfor maternal race, age, cervical length at 1st sonogram, gestational age at 1st sonogram, cervicallength at last sonogram, gestational age at last sonogram, and number of sonographicevaluations, the relationship between these 2 cervical length subgroups became once again,null (p = 0.38).
COMMENTIn this large population of multiparous women, chosen to be homogeneous for the strongesthistoric risk factor for recurrent preterm birth, a mid-trimester cervical length threshold of 25mm appeared to be a good, if imperfect discriminator of preterm birth risk. Although this cohortremained at increased risk for preterm birth < 35 weeks’ gestation (16%) compared to anunselected population (2.7%) (7), the continuum of cervical lengths at or beyond 25 mm hadno appreciable impact on preterm birth risk or length of gestation as estimated with severaldifferent statistical models. Conversely, shorter lengths, as exemplified in the < 25 mm, no-cerclage cohort, clearly show the oft-demonstrated inverse relationship with preterm birth risk.
We included a < 25 mm internal comparison group to emphasize the disparity in the risk ofpreterm birth on either side of the 25 mm cervical length threshold. Not only is the rate ofpreterm birth < 35 weeks substantially higher (42% vs. 16%), but there was a strong correlationin the trend toward higher preterm birth rates in the < 25 mm group as the cervix shortensfurther; women with the shortest cervical lengths < 10 mm had > 90% chance of preterm birth< 35 weeks. An analogous trend in the continuum of risk was not observed in the ≥ 25 mmcohort (Figure 2). Not surprising is the observation that the 2 cohorts differed in several aspects,as shown in Table 1. Many of these characteristics, in addition to shorter cervical lengths,including Black race, abortion history and earlier gestational age of the prior (i.e. qualifying)preterm birth are themselves, well-known risk factors for preterm birth. That women in the ≥25 mm cohort underwent more sonograms and had their final sonogram at a later gestationalage, is simply a reflection of their failure to shorten in the temporal scanning window.
Possible limitations to our study include that our observations were censored by trial design at226/7 weeks gestation. Thus, it is possible that some women continued to experience cervicalshortening after the observation window ended and that pathologic shortening was associatedwith some of the observed preterm births. Another explanation for the apparent increasedpreterm birth risk in this population who failed to demonstrate cervical shortening < 25 mm,is that some of these early births may have been due to other components of the preterm birthsyndrome and that did not involve premature cervical shortening (Romero, 1994). Since wedid not collect more detailed delivery information in the ≥ 25 mm cohort beyond date ofdelivery, we could not determine whether the preterm births were indicated or, if spontaneous,whether they were associated primarily with premature membrane rupture, labor or cervicalinsufficiency. However, by design, we specifically excluded women with known conditionsthat would put them at risk for maternal-fetal complications and indicated preterm birth. Ofnote, in the no-cerclage comparison cohort, the overall rate of preterm birth < 37 weeks was59%, while the reported rate of indicated preterm birth only 4%. Thus we believe it is unlikelythat, had we limited our analysis to spontaneous preterm birth in the failed-to-shorten cohort,our results would have been different. Similarly, we did not have information on ancillarypreterm birth prevention strategies such as the use of progesterone (13), which may also haveexplained some of the observed variance in birth outcomes. Finally, as our null findings didnot demonstrate an association between cervical lengths ≥ 25 mm and pregnancy duration,there was a concern about statistical power. From the observed data we determined that asample of 672 women would have 80% power to detect a linear regression coefficient as small
Owen et al. Page 4
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
as 0.05, (considering birth gestational age as the dependent variable and cervical length as thepredictor), if such a relationship actually exists. This would imply that for each additional mmof cervical length, mean gestational age would increase by 0.05 weeks. Our observed regressioncoefficient was 0.03, p = 0 .15.
One of the interesting clinical findings in this study is the 16% rate of preterm birth < 35 weeksin these 672 high-risk women whose mean earliest prior spontaneous preterm birth was 26.6weeks. Women who fail to shorten to < 25 mm by 226/7 weeks can be reassured that the riskis low. Since ultrasound-indicated cerclage has been shown to improve pregnancy outcomesin women with prior spontaneous preterm birth and cervical length < 25 mm (11,14), and sinceless than one third of these women experience cervical shortening < 25 mm (3,11), we believeit is appropriate to screen women with a prior preterm birth history using serial sonography inorder to limit history-indicated cerclage.
In summary, women at increased risk for recurrent preterm birth but who maintain a cervicallength of at least 25 mm may still have an increased risk of recurrence. Nevertheless, whethera woman’s cervical length is near the threshold, or appreciably longer, her absolute risk appearsto be stable. Whether this biologic relationship holds in other populations of women with norisk factor (e.g. nulliparas) or other historic risk factors cannot be estimated from our data.However, in women with prior spontaneous preterm birth, a cervical length threshold of 25mm appears to be a clinically relevant discriminator of preterm birth risk. Further researchinitiatives may better define the pathways and mechanisms of preterm birth in women who failto exhibit cervical shortening in the midtrimester. Future intervention trials in women with thispreterm birth risk factor should consider using a cervical length threshold of 25 mm to identifythe population at highest risk.
AcknowledgmentsWe wish to acknowledge other members of the Vaginal Ultrasound Trial Consortium: Susan Ramin, MD, MarkTomlinson, MD, Eric Knudtson, MD, Robert Egerman, MD, Richard Silver, MD, Helen How, MD, Mike Gordon,MD.
Source of funding: The Eunice Kennedy Shriver National Institute of Child Health and Development provided fundingvia grant U01 HD039939; from the same agency, Dr. Owen also received support via grant 5K24 HD43314-5.
REFERENCES1. Spong C. Prediction and prevention of recurrent spontaneous preterm birth. Obstet Gynecol
2007;110:415.2. Anonymous. American College of Obstetricians and Gynecologists. Assessment of risk factors for
preterm birth. Practice bulletin Number 31. 2001 October;3. Owen J, Yost N, Berghella V, et al. for the National Institute for Child Health and Human Development
Maternal Fetal Medicine Unit Network. Mid-trimester endovaginal sonography in women at high riskfor spontaneous preterm birth. JAMA 2001;286:1340–1348. [PubMed: 11560539]
4. Crane JM, Hutchens D. Transvaginal sonographic measurement of cervical length to predict pretermbirth in asymptomatic women at increased risk: a systematic review. Ultrasound Obstet Gynecol 2008May;31(5):579–587. [PubMed: 18412093]
5. Honest H, Bachman LM, Coomarasamy A, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervicaltransvaginal sonography in predicting preterm birth: a systematic review. Ultrasound Obstet Gynecol2003;22:305–322. [PubMed: 12942506]
6. Leitich H, Brunbauer M, Kaider A, Egarter C, Husslein P. Cervical length and dilation of the internalos detected by vaginal ultrasonography as markers for preterm delivery: A systematic review. Am JObstet Gynecol 1999;181:1465–1472. [PubMed: 10601930]
Owen et al. Page 5
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
7. Iams JD, Goldenberg RL, Meis PJ, et al. for the National Institute of Child Health and HumanDevelopment Maternal Fetal Medicine Unit Network. The length of the cervix and the risk ofspontaneous premature delivery. N Engl J Med 1996;334:567–572. [PubMed: 8569824]
8. Rust OA, Atlas RO, Jones KJ, Bernham BN, Balducci J. A randomized trial of cerclage versus nocerclage among patients with ultrasonographically detected second-trimester preterm dilatation of theinternal os. Am J Obstet Gynecol 2000;183:830–835. [PubMed: 11035321]
9. Althuisius SM, Dekker GA, Hummel P, Bekedam DJ, van Geijn HP. Final results of the cervicalincompetence prevention randomized cerclage trial (CIPRACT): Therapeutic cerclage with bed restversus bed rest alone. Am J Obstet Gynecol 2001;185:1106–1112. [PubMed: 11717642]
10. Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a shortcervix found on transvaginal ultrasound: A randomized trial. Am J Obstet Gynecol 2004;191:1311–1317. [PubMed: 15507959]
11. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birthprevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol2009;201 375.e1-8.
12. Romero R, Mazor M, Munoz H, Gomez R, Galasso M, Sherer DM. The preterm labor syndrome.Ann HY Acad Sci 1994;734:414–429.
13. Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, Moawad AH, et al. Prevention of recurrentpreterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med 2003;348:2379–2385.[PubMed: 12802023]
14. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix onultrasonography, Meta-Analysis of Trials Using Individual Patient-Level Data. Obstet Gynecol2005;106(1):181–189. [PubMed: 15994635]
Owen et al. Page 6
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Figure 1. Flow of participants
Owen et al. Page 7
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Figure 2. Relationship between cervical length groups and birth < 35 weeksRates of preterm birth < 35 weeks by cervical length group in both the < 25 mm, no-cerclage,internal comparison cohort and ≥ 25 mm, failed-to-shorten cohort
Owen et al. Page 8
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Figure 3. Kaplan-Meier survival curves of cervical length groupsProbability of delivery across gestation in the ≥ 25 mm cohort, comparing women with cervicallengths 25–29 mm and those with cervical lengths 30 mm or greater.
Owen et al. Page 9
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Owen et al. Page 10
Table 1
Characteristics
< 25mm(n =153)
≥ 25mm(n =672)
p-value
Maternal age (y) 26.6 ± 5.1 26.7 ± 5.3 0.72
Number of prior births (n) 2 (1, 4)† 2 (1, 4)† 0.33
One or more prior induced abortion - no. (%) 25 (16) 62 (9) 0.01
Body mass index (kg/m2) 29.9 ± 7.5 28.7 ± 7.1 0.07
Race/ethnicity* - no. (%) <0.00 01
Black (non-Hispanic) 93 (61) 217 (32)
White (non-Hispanic) 28 (18) 128 (19)
Hispanic 17 (11) 208 (92)
Asian 0 (0) 11 (2)
Other 15 (9.8) 108 (16)
Marital Status - no. (%)
Single/never married 99 (65) 337 (50) 0.002
Married 42 (27) 294 (44)
Divorced 10 (6.5) 36 (5.4)
Widowed 1 (0.7) 4 (0.6)
Other 1 (0.7) 1 (0.2)
Prior cerclage - no. (%) 12 (7.8) 17 (2.5) 0.001
Years of education (n) 11.9 ± 2.4 11.6 ± 4.4 0.35
Gestational age of qualifying birth (wks) 24.9 ± 4.7 26.8 ± 4.4 < 0.0001
Gestational age at first vaginal sonogram (wks) 17.4 ± 1.4 17.8 ± 1.4 0.002
Cervical length at first vaginal sonogram (mm) 29.5 ± 12.9 40.6 ± 10.1 < 0.0001
Gestational age at randomization or final sonogram (wks) 19.5 ± 2.0 21.3 ± 1.4 < 0.0001
Cervical length at randomization or final sonogram (mm) 19.5 ± 5.3 37.9 ± 8.2 < 0.0001
Total number of vaginal sonograms (N) 2 (1, 4)† 3 (1, 4)† < 0.0001
Continuous data are expressed as a mean ± 1 standard deviation except as noted.
†Median and interdecile range
Am J Obstet Gynecol. Author manuscript; available in PMC 2011 October 1.