Children of Mothers With Borderline Personality Disorder: Identifying Parenting Behaviors as...
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Children of Mothers With Borderline Personality Disorder: Identifying Parenting Behaviors as...
Personality Disorders: Theory, Research, andTreatment
Children of Mothers With Borderline PersonalityDisorder: Identifying Parenting Behaviors as PotentialTargets for InterventionStephanie D. Stepp, Diana J. Whalen, Paul A. Pilkonis, Alison E. Hipwell, and Michele D.LevineOnline First Publication, March 28, 2011. doi: 10.1037/a0023081
CITATIONStepp, S. D., Whalen, D. J., Pilkonis, P. A., Hipwell, A. E., & Levine, M. D. (2011, March 28).Children of Mothers With Borderline Personality Disorder: Identifying Parenting Behaviors asPotential Targets for Intervention. Personality Disorders: Theory, Research, and Treatment.Advance online publication. doi: 10.1037/a0023081
Children of Mothers With Borderline Personality Disorder:Identifying Parenting Behaviors as Potential Targets for Intervention
Stephanie D. SteppUniversity of Pittsburgh School of Medicine
Diana J. WhalenUniversity of Pittsburgh
Paul A. Pilkonis, Alison E. Hipwell, and Michele D. LevineUniversity of Pittsburgh School of Medicine
Children of mothers with Borderline Personality Disorder (BPD) should be considereda high-risk group given the wide array of poor psychosocial outcomes that have beenfound in these children. This article describes the parenting strategies that might explainthe transmission of vulnerability from mothers with BPD to their offspring, frominfancy through adolescence. We conclude that oscillations between extreme forms ofhostile control and passive aloofness in their interactions with their children may beunique to mothers with BPD. We provide an overview of interventions that arecurrently recommended for mothers and family members with BPD, namely attachmenttherapy and psychoeducational approaches. On the basis of an integration of theempirical findings on parenting and child outcomes, as well as from the review ofcurrent approaches to intervention, we conclude with recommendations for treatmenttargets. We argue that mothers with BPD need psychoeducation regarding childdevelopment and recommended parenting practices and skills for providing consistentwarmth and monitoring, including mindfulness-based parenting strategies.
Keywords: mothers with borderline personality disorder, parenting, parent–child interventions,parent skills training
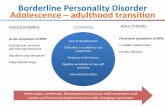
Borderline Personality Disorder (BPD) ischaracterized by a pattern of intense and stormyrelationships, uncontrollable anger, poor im-pulse control, affective instability, identity andcognitive disturbances, and recurrent suicidalbehavior. Individuals with BPD are likely toface a host of negative outcomes, includingpoor treatment response and poor social, occu-pational, and academic outcomes (Bagge et al.,2004; Bender et al., 2001; Skodol et al., 2002).The day-to-day life of those with this disorder isfraught with high levels of misery, which oftenendures even after symptoms of impulsivity and
suicide behaviors remit (Zanarini, Frankenburg,Hennen, & Silk, 2003). In clinical settings, 75%of those carrying a BPD diagnosis are women(Skodol & Bender, 2003), and there are esti-mated to be over 6 million women in the UnitedStates diagnosed with BPD (Freidel, 2004).There are likely a large number of women withBPD who are also mothers, which when com-bined with the extensive functional impairmentsassociated with this disorder represents a prob-lem of enormous public concern. Thus, it issomewhat surprising that the effects of maternalBPD on children’s outcomes have been the fo-cus of little empirical attention or treatmentdevelopment efforts. Given that parenting im-pacts both the mother and the child, we feel thatdeveloping a parenting intervention specificallyfor this high-risk population is a particularlyimportant endeavor.
Our overall aim for this work is to reviewparenting mechanisms that might explain thetransmission of psychosocial vulnerability frommothers with BPD to their offspring, from in-
Stephanie D. Stepp, Paul A. Pilkonis, Alison E. Hipwell,and Michele D. Levine, Department of Psychiatry, Univer-sity of Pittsburgh School of Medicine; Diana J. Whalen,Department of Psychology, University of Pittsburgh.
Correspondence concerning this article should be ad-dressed to Stephanie D. Stepp, University of PittsburghSchool of Medicine, Western Psychiatric Institute andClinic, 3811 O’Hara St., Pittsburgh, PA 15213. E-mail:[email protected]
Personality Disorders: Theory, Research, and Treatment © 2011 American Psychological Association2011, Vol. ●●, No. ●, 000–000 1949-2715/11/$12.00 DOI: 10.1037/a0023081
1
fancy through adolescence. We first reviewgene-environment interaction models to explainthe transgenerational transmission of the disor-der. Second, we review evidence that suggestschildren of mothers with BPD should be con-sidered a high-risk group given the wide arrayof poor psychosocial outcomes that have beenfound in these children. Next, we highlight par-enting practices that may explain the transmis-sion with a focus on particular parenting mech-anisms that might be especially relevant formothers with BPD across key developmentalmilestones. Finally, we discuss implications forinterventions with mother–child dyads and pro-vide recommendations regarding points of in-tervention for this population.
Transgenerational Transmission of BPD
There is good evidence for the transgenera-tional transmission of this disorder (for areview, see White, Gunderson, Zanarini, & Hud-son, 2003). For instance, family studies assess-ing the rates of BPD diagnoses and related traitsin first-degree relatives have found a 4- to 20-fold increase in prevalence or morbidity risk forBPD compared with the general population(e.g., Barnow, Spitzer, Grabe, Kessler, & Frey-berger, 2006; Zanarini, Gunderson, Marino,Schwartz, & Frankenburg, 1988). Research sup-ports an even stronger familial aggregation ofcore features of BPD, namely affective instabil-ity and impulsivity, compared with the fullydiagnosed disorder (Silverman et al., 1991).These features have been found to aggregateseparately, suggesting that they may be inher-ited independently. Given the familial aggrega-tion of these traits in BPD, it is not surprisingthat relatives of probands with BPD are also atincreased risk for related psychiatric disorders,including Major Depressive Disorder (MDD),Substance Use Disorders, and Antisocial Per-sonality Disorder (Riso, Klein, Anderson, &Ouimette, 2000; Schulz, Soloff, Kelly, Morgen-stern, Franco, & Schulz, 1989; Zanarini et al.,1988).
Given the high rate of family transmissionwith the disorder and associated features, off-spring of parents with BPD may inherit genespredisposing them to a difficult temperament,emotional reactivity, and/or impulsivity. Twinstudies offer evidence for the genetic transmis-sion of BPD. In a large, multinational commu-
nity-based adult twin sample, Distel and col-leagues (2007) reported a heritability estimateof 42% for BPD features. Torgensen (2000)reported a much higher heritability estimate of69% for the diagnosis of BPD in a relativelysmall twin sample of clinic-referred adult par-ticipants. The discrepancy in heritability esti-mates is likely because of differences in samplesize and sample ascertainment across the twostudies. In addition, genetic influences may bestronger for individuals with more extremeforms of the disorder (i.e., those that are clini-cally referred and carry the diagnosis). Thus,findings from the population-based study sug-gest a relatively strong influence for both ge-netic and unique environmental experiences inaccounting for variation in BPD features.
Gene-environment interaction models dem-onstrate the importance of an individual’sunique social environment in moderating theeffects of genes on the development of psycho-pathology and other maladaptive outcomes (Ca-cioppo, Berntson, Sheridan, & McClintock,2000). Parenting serves as an important envi-ronmental context for offspring of mothers withBPD. Theoretical models (Fruzzetti, Shenk, &Hoffman, 2005; Linehan, 1993) posit that inval-idating parenting experiences transact with achild’s genetic vulnerabilities to put them at riskfor poor psychosocial outcomes, including BPDand related psychopathology. Children lower inemotional reactivity may be more likely tomaintain a positive parent–child relationshipbecause their caregivers are willing to respondpositively to their emotional expressions. Incontrast, negative parent– child relationshipscan exacerbate both the internalizing and exter-nalizing symptoms in youth who are alreadyemotionally dysregulated (Feinberg et al., 2007;Huh, Tristan, Wade, & Stice, 2006). Warm andaccepting parenting can shield a child from neg-ative outcomes associated with genetic andphysiological vulnerabilities (Eley et al., 2004).Alternatively, children with certain genetic andphysiological factors may be protected from theeffects of social environments characterized byabuse, neglect, and conflict (Kaufman et al.,2006). Although it is impossible to modify achild’s genetic vulnerabilities, parenting prac-tices may be modified and thus offer an envi-ronmental context ripe for intervention.
Several lines of evidence suggest that indi-viduals with BPD would face heightened chal-
2 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
lenges in parenting, which could have a delete-rious effect on the child’s development. First,Hobson and colleagues (1998) demonstratedthat individuals with BPD displayed dysfunc-tional moment-to-moment relatedness with apsychotherapist, including hostility and intense,idealizing, and devaluing exchanges when com-pared with individuals with dysthymia. If thesepatterns of interaction are typical betweenmothers with BPD and their children, then theimpact on the child’s social-emotional develop-ment would be substantial. Second, individualswith BPD tend to have attachment styles clas-sified as disorganized and unresolved (Levy,2005). These attachment styles may influencethe manner in which a mother relates to herchild; specifically, mothers with unresolvedtrauma may relate to their child in a manner thatoscillates between hostility and passivity (Main& Hesse, 1990). Evidence suggests that mater-nal BPD impacts infant affect and early markersof self- and emotion regulation skills (Crandell,Patrick, & Hobson, 2003; Hobson, Patrick,Crandell, Garcıa-Perez, & Lee, 2005; Newman,Stevenson, Bergman, & Boyce, 2007). In sum,findings from moment-to-moment interpersonalexchanges and attachment strategies highlightthat parenting styles oscillating between hostilecontrol and passive, devaluating behaviors maylead to poor regulation in infants among moth-ers with BPD. On the basis of the biosocialtheory (Linehan, 1993), mothers with BPD mayinadvertently create these invalidating environ-ments for their own children by modeling theirparents’ strategies; indeed, these parenting strat-egies may be “passed down” from generation togeneration.
What Characterizes Children of MothersWith BPD?
Despite concerning epidemiological evidenceregarding the heritability of BPD features, fewstudies, relative to other forms of maternal psy-chopathology, such as depression, have directlyexamined outcomes of the offspring of motherswith BPD. We now turn to reviewing the avail-able findings regarding a broad array of psy-chosocial outcomes of children, from infancythrough adolescence, whose mothers haveBPD.
Outcomes During Infancy andEarly Childhood
Three studies have been conducted using in-fants of mothers with BPD (Crandell et al.,2003; Hobson et al., 2005; Newman et al.,2007). Newman and colleagues (2007) foundthat infants of BPD mothers (n � 14) aged 3to 36 months were less attentive and less inter-ested in interactions with their mother during afree-play interaction compared with infants ofhealthy control mothers (n � 20). The authorsspeculate that this could lead to avoidant inter-action patterns between the children and theirmothers. The still-face paradigm has also beenused to examine infant outcomes. Crandell andcolleagues (2003) found that during the still-face paradigm, 2-month-old infants of motherswith BPD demonstrated more dazed looks,more gaze aversion, and less overall responsive-ness toward the mother than infants of motherswithout a psychiatric disorder. The authors in-terpreted these results as suggestive of emo-tional dysregulation in the face of an interper-sonally stressful situation. Furthermore, afterthe still-face paradigm, the mother-infant dyadsshowed less recovery in their interactions as theinfants continued to show increasing negativeaffect and less-satisfying reengagement withtheir mothers. When this same group of infantswas 12 months old, 80% presented with behav-ioral patterns consistent with disorganized at-tachment to their mothers (Hobson et al., 2005).Infants were rated as having more behavioraldisorganization and poor mood toward astranger when engaging in the still-face proce-dure. Recovery time from the still face proce-dure was longer, suggesting greater affectivedysregulation.
Macfie and Swann (2009) examined mother–child attachment relationships in preschool andearly school age (4–7) children of mothers withBPD. The investigators administered 5 itemsfrom the MacArthur Story Completion Task(Bretherton, Oppenheim, Buchsbaum, Emde, &The MacArthur Narrative Group, 1990) and 5items from the Story-Stem Battery (Bretherton,Ridgeway, & Cassidy, 1990) to 30 preschool-aged children whose mothers had BPD, and 30healthy comparison 4- to 7-year-olds. The storystems elicit responses concerning the attach-ment relationship in increasingly stressful inter-personal situations, such as parental discipline,
3CHILDREN OF MOTHERS WITH BPD
parental comfort, and parental fighting. Thesenarratives representations are hypothesized toreflect the child’s actual experiences and inter-nal working models of the caregiver, the self,and emotional coherence or regulation. Usingthese open-ended narrative paradigms, findingsrevealed poorer emotion regulation in the chil-dren’s narratives as characterized by increasedlikelihood to talk about fantasies as well asmaterial of a traumatic nature. Role reversal(e.g., child tells fighting parents to: “Stop that!Go to your room!”) was also significantly morelikely to be present in the narratives of childrenwith a BPD mother. The children also exhibitedgreater fears of abandonment, where attemptsare made to resolve an anticipated loss in theirstories. More negative parent–child relationshipexpectations, such as the relationships charac-terized by danger and/or unpredictability werealso found in the preschooler’s narratives. Last,the children of BPD mothers also showed moreincongruent (e.g., the child cleans his or herroom then ruins it) and shameful self- represen-tations (e.g., the child says he or she is bad) inthe narratives.
We posit that these constructs may be relatedto a variety of psychosocial outcomes. First, achild who demonstrates fear of abandonment inhis or her parent–child narratives and/or nega-tive expectations of parental relationships maydemonstrate that same fear of abandonment inother relationships, making it difficult to formand maintain stable and meaningful interactionswith others. Second, children demonstrating ashameful and incongruent sense of self in his orher narratives may continue to show identitydisturbances into adolescence and adulthood.Disturbances in identity formation are one hall-mark feature of BPD and have been associatedwith self-injurious behavior and dissociativesymptoms (Ogawa et al., 1997; Yates, 2004).Early deficits in emotion regulation have alsobeen shown to be associated with later internal-izing and externalizing disorders in childhood(Eisenberg et al., 2001; Suveg, Hoffman, Ze-man, & Thomassin, 2009).
Outcomes for School-Aged andAdolescent Children
School-aged and adolescent children whohave mothers diagnosed with BPD are at riskfor both internalizing and externalizing prob-
lems. For instance, employing a wide age-rangeof children (4–18 years), those with maternalhistory of BPD (n � 21) had more BPD symp-toms during childhood (as assessed with theadult symptomatology), attention-deficit/hyperactivity disorder (ADHD), and other dis-ruptive behavior disorders (Feldman, Zelkow-itz, Weiss, Vogel, Heyman, & Paris, 1995)compared with children of control mothers(n � 23).
Abela and colleagues (1995) studied 6- to14-year-old children of mothers with comorbidMDD and BPD (n � 15) compared with moth-ers with only MDD (n � 87). Children of moth-ers with both disorders showed higher levels ofdepressive symptoms and were 6.8 times morelikely to have had at least one episode of MDD.These children also reported more cognitive andinterpersonal vulnerability, such as a negativeattributional style, ruminative response style,dysfunctional attitudes, self-criticism, insecureattachment style, and excessive reassuranceseeking. These results held even when control-ling for the mothers’ concurrent depressivesymptoms, suggesting that there are unique vul-nerabilities associated with having a motherwith BPD. In a small pilot study, 21 children ofmothers with BPD have also been found to havemore psychiatric diagnoses, such as ADHD andhigher rates of BPD symptoms in childhoodwhen compared with 23 children of controlmothers (Weiss, Zelkowitz, Feldman, Vogel,Heyman, & Paris, 1996). These results heldeven after controlling for childhood trauma,demonstrating some specificity for these find-ings. This study also rated the children of moth-ers with BPD as higher on global ratings ofimpairment. After controlling for other contrib-uting factors (depressive symptoms and child-hood trauma), maternal BPD remained a sig-nificant factor related to poor outcomes forschool-aged and adolescent children.
Consistent with outcomes during the school-age period, adolescents aged 11 to 18 yearswhose mothers had BPD (n � 23) exhibitedmore attention problems, delinquency, and ag-gression than adolescents whose mothers hadno psychiatric disorders (n � 168; Barnow etal., 2006). This same group of adolescents alsoreported more anxiety, depression, and low self-esteem than adolescents of mothers with majordepressive disorder, other personality disorders,and healthy controls. In a community sample of
4 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
mothers with 15-year-olds (n � 354), maternalBPD symptoms were related poor psychosocialoutcomes in the adolescents, including lowersocial self-perception, greater fearful attach-ment cognitions, more chronic stress in themother-adolescent relationship, and greater ma-ternal hostility (Herr, Hammen, & Brennan,2008). These findings held even after control-ling for both adolescent and maternal depres-sive symptoms suggesting that maternal BPDand depressive symptoms may be separate andunique risk factors.
These studies have shown that, from infancythrough early adolescence, maternal BPDplaces children at risk for a range of emotionaland behavioral problems. However, several ofthese studies are limited by the wide age rangein the offspring, as well as the variety of co-morbid conditions in the mothers. In addition,these studies did not account for the bidirec-tional influences inherent in mother–child rela-tionships. Specifically, in addition to the role ofmaternal characteristics on the development ofchild psychopathology, the child’s characteris-tics also exert an influence on his or her lateroutcomes. The effect of parenting practices onchildhood outcomes is more salient during in-fancy and early childhood. As children developmore autonomy in the selection of their envi-ronment during adolescence, the effect of peersand other social influences may exert a uniqueeffect on the child’s functioning. During thistime, parenting practices continue to play animportant role in emotion socialization and pro-vide appropriate monitoring and supervision toensure healthy child outcomes (Steinberg &Morris, 2001).
What Parenting Mechanisms Are Involvedin the Transmission of Vulnerability?
Despite its place as a major construct in Line-han’s theory, the role of parental invalidation inthe transmission and development of BPD re-mains largely untested. In normative samples,parental criticism or invalidation of children’semotions has been associated with social andemotional difficulties in early childhood (e.g.,Eisenberg, Fabes, & Murphy, 1996) and psy-chological distress in adulthood (Krause, Men-delson, & Lynch, 2003). On the basis of thistheory, we hypothesize that mothers with BPDmay invalidate the emotions of their children,
especially when the mother inaccurately per-ceives these emotions. This may in turn lead tochildren who deny or question their emotionsand emotional responses. This chronic invalida-tion of emotional experiences may disrupt theadaptive development of emotion processingsystems. It is likely that mothers with BPD, as aresult of their own difficulties understandingtheir feelings, lack of skills to manage their ownemotions, and their own childhood history ofparental invalidation would have a hard timemodeling appropriate emotion socializationstrategies. Mothers with BPD may thus teachtheir children maladaptive ways of expressingand managing emotions.
Invalidating environmental factors that corre-late with BPD include neglect and abuse (Ban-delow et al., 2005; Bornovalova, Gratz, Delany-Brumsey, Paulson, & Lejuez, 2006), which mayoccur within the family of origin. However, thespecific invalidating parenting practices thatmay play a role in the development of BPD hasreceived little empirical attention. We first re-view studies examining the parenting practicesamong mothers with BPD, and then, given thelittle empirical attention that has been given tothis topic, we discuss the evidence related toparenting of those with other personalitydisorders.
Mothers With BPD
The still-face paradigm has been used to in-vestigate parenting behaviors of mothers withBPD. Crandell and colleagues (2003) found thatthe mothers with BPD were more likely to becharacterized as intrusively insensitive based onratings of their speech and behavior during boththe free play period before the still face para-digm and the recovery period afterward com-pared with healthy controls. The authors laterreplicated these findings in another sample ofinfant-mother dyads (Hobson et al., 2005). Hob-son and colleagues (2009) also investigated therelationship between 1-year-old infants andtheir mothers with BPD. Using videotaped in-teractions of the Strange Situation paradigm, theauthors found that mothers with BPD displayeddysregulated affective communication towardtheir infants, including critical and intrusive be-haviors, role confusion, and frightened/frighten-ing behaviors. In addition, the mothers showedmore frightening and disorienting behavior than
5CHILDREN OF MOTHERS WITH BPD
mothers with depression or without a personal-ity disorder.
Consistent with some of the findings from theobservational studies with infants, Macfie andSwan (2009) argue that role-reversal during thetoddler period is particularly relevant for chil-dren of mothers with BPD. During the toddlerperiod, children begin to develop a sense ofautonomy. However, this milestone might bediscouraged in toddlers of mothers with BPD,who might prefer the toddler to stay close inorder to meet the mother’s needs. Mothers withBPD may be frightened that their child mightabandon them. This may result in role-reversal;that is, the child’s taking on an adult role ofpeer, friend, or parent. In line with this theory,disorganized attachment during infancy, whichis also a likely outcome for infants of motherswith BPD (e.g., Hobson et al., 2005), has beenshown to predict role-reversal during the tod-dler period (Macfie, Fitzpatrick, Rivas, & Cox,2008) and early childhood (Main, Kaplan, &Cassidy, 1985).
The work on parenting behaviors has alsoincluded an assessment of parenting perceptions(Newman et al., 2007). Mothers with BPD werefound to be less sensitive and demonstrated lessstructuring in their interaction with their infantswhen compared with psychiatrically healthymother–infant dyads. These mothers also per-ceived differences in their parenting ability, re-porting they were less satisfied, less competentand more distressed with their parenting abili-ties. Of interest, the authors noted that the levelsof distress and perceived difficulties with par-enting roles may be a factor contributing toneglect and abuse.
Both neglect and emotional underinvolve-ment by caretakers, an extreme form of emo-tional invalidation, appear to contribute to thedevelopment of BPD. Feldman and colleagues(1995) reported that children (aged 4–18) ofBPD mothers were exposed to environmentalinstability in the form of frequent changes inhousing and schooling, removal from the home,and maternal suicide attempts.
In sum, parenting behaviors that have beenfound to characterize mothers with BPD includeinsensitive forms of communication, such ascritical, intrusive, and frightening commentsand behaviors. In addition, these mothers maybe likely to engage in role confusion with theirchildren and may reinforce their children for
taking on the role of a parent or friend. Finally,mothers with BPD report experiencing highlevels of distress in roles as parents whichcould lead to abuse out of frustration andhopelessness.
Mothers With Personality Disorders
Other studies have examined the effect ofgeneral personality pathology on parenting.Conroy and colleagues (2009) recruited a com-munity sample of 200 mothers 8 weeks’ post-partum to participate in at-home assessmentsand observations. The authors found significantmain effects of depression and personality dis-orders on infant care practices scores even aftercontrolling for infant irritability, suggesting thatwomen with depression and women with a per-sonality disorder reported engaging in fewerrecommended infant care practices (e.g., “babyis placed supine to sleep at night,” “baby isnever exposed to cigarette smoke”) and lowerobservational ratings of maternal involvementcompared with mothers without depression andwithout a personality disorder. When examiningthe effect of personality disorder on infant careat the personality disorder cluster level (A, B,and C), there was a main effect for cluster Bpersonality disorder status (which includesBPD, histrionic, narcissistic, and antisocial) oninfant care practices but not on maternal in-volvement observational ratings. The lack ofassociation between cluster B personality disor-der status and maternal sensitivity observationalratings is inconsistent with findings from otherstudies. This discrepancy may be because of thelack of diagnostic specificity as a result ofgrouping personality disorders into clusters.In addition, the observational ratings werebased on one 3-min videotaped play in-teraction, which may not have been able todetect differences in maternal sensitivity andresponsiveness.
In addition, the Children in the CommunityStudy (CIC; e.g., Cohen, 1996) has provided alongitudinal prospective account of parenting,parental psychopathology, and child outcomes,and was one of the first to look at child rearingin parents with Axis II disorders, but not spe-cifically BPD. In 10 recent papers using datafrom late childhood and early adolescence, theyhave shown that: (a) parental personality disor-der is associated with problematic parenting; (b)
6 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
maladaptive parenting is predictive of later per-sonality disorder symptoms in offspring; and (c)parental personality disorder is associated withsymptoms and disorders in offspring (Berg-Neilsen, Vikan, & Dahl, 2002; Bezirganian, Co-hen, & Brook, 1993; Cohen, 1996; Cohen,Crawford, Johnson, & Kasen, 2005; Johnson,Cohen, Brown, Smailes, & Bernstein, 1999;Johnson, Cohen, Chen, Kasen, & Brook, 2006;Johnson, Cohen, Gould, Kasen, Brown, &Brook, 2002; Johnson, Cohen, Kasen, & Brook,2006; Johnson, Cohen, Kasen, Smailes, &Brook, 2001; Johnson, Cohen, Smailes, Skodol,Brown, & Oldham, 2001). This work illustratesthe importance of parenting in the transgenera-tional transmission of personality disorders.
What Parenting Challenges Are Specific toMothers With BPD?
One of the challenges faced when studyingthis topic area is how to disentangle parentingpractices that might be unique to mothers withBPD from those that are related to other formsof psychopathology, such as depression. Fromthe studies reviewed, we posit that maternalparenting strategies characterized by oscilla-tions between overinvolvement and underin-volvement to be specific to mothers with thisdisorder. We view these oscillations as extremeforms of inconsistencies. Inconsistencies inemotion socialization practices as well as indiscipline and monitoring strategies appear tocontribute to the development of BPD (Bezir-ganian et al., 1993). Mothers with BPD mayoscillate between overinvolved, intrusive be-haviors and withdrawn, avoidant behaviors.These behaviors may also manifest as oscilla-tions between hostile control and coldness. Forexample, mothers with BPD reported more ne-glectful and punishing responses to their ado-lescent’s emotional displays, even when con-trolling for current depressive symptoms(Whalen, Dahl, & Silk, 2009). These samemothers also reported almost equal amounts ofreward, a supportive emotion socialization strat-egy compared with depressed and healthy con-trol mothers, suggesting that mothers with BPDmay be more inconsistent in their emotion so-cialization strategies. Over time, this inconsis-tency may lead their adolescents to deny orquestion their emotional responses increasing
the potential for emotional vulnerability andfurther invalidation by others or self.
Furthermore, it seems that mothers with BPDmay engage in a greater number of negativeparenting behaviors, which may increase theiroffspring’s risk for psychopathology (e.g.,Johnson et al., 2006). The combined effects ofmaternal inconsistency across emotion social-ization as well as monitoring, for example, maycreate an environment invalidating enough tocontribute to the development of BPD in theoffspring. For example, Bezirganian and col-leagues (1993) reported clinical examples ofperceptions that mothers with BPD had abouttheir children. In one example a mother reportedthat she wished to, “place [her son] in thefreezer so that he could never grow old enoughto leave [me].” She went on to describe hernegative reactions, such as pouting and pleas forhis company, to his invitations to go out withfriends; however, she would always let himsocialize. These interactions were characterizedby inconsistency in that her verbal and emo-tional expressions conveyed one meaning, butthe end result of the interaction conveyed an-other. In addition, this type of interaction couldbe characterized as emotionally overinvolved inthat it inhibits the child’s autonomy in order tomeet the mother’s emotional needs. Motherswith BPD may find it difficult to balance appro-priate limit setting with the encouragement ofexploration and growth for their children. Itmay also be that mothers with BPD find itdifficult to adjust their parenting strategies tomatch the developmental needs of their chil-dren. For example, a discipline strategy thatworked well for a toddler may not have thesame impact on an adolescent.
Current Interventions
Based on our review, children of motherswith BPD are at risk for poor psychosocialoutcomes and the transmission of this vulnera-bility may be because of certain deficits in par-enting skills. Interventions designed specificallyfor mothers with BPD and their children do notexist. However, authors have made general rec-ommendations favoring attachment therapies(cf., Macfie, Fitzpatrick, Rivas, & Cox, 2008),especially during infancy through the preschoolperiod and/or psychoeducation-based interven-tions (cf. Gunderson, Berkowitz, & Ruiz-
7CHILDREN OF MOTHERS WITH BPD
Sancho, 1997) for family members of thosewith BPD.
Attachment-Based Interventions
Attachment-based interventions generally ap-proach preventing the transmission of insecureand/or disorganized attachment from parent(usually the mother) to the child in one of twoways: (a) individual psychotherapy with themother and (b) psychotherapy with the mother–infant (or toddler) dyad. Interventions designedwith the parent as the primary patient aim toprovide “corrective” attachment experiencesthrough interactions and experiences with thetherapist (e.g., Lieberman, Weston, & Pawl,1991; Lieberman & Zeanah, 1999). Duringindividual psychotherapy, the mother is encour-aged to talk about her own childhood experi-ences and link these events to her current rela-tionship with her child, allowing her to gaininsight into how she perpetuates the cycle ofinsecure and/or disorganized attachment. Thismode of improving attachment security via in-dividual psychotherapy with the mother has notbeen well manualized, which has impeded dis-semination and evaluation efforts.
The second approach of attachment-basedpsychotherapy intervenes at the level of therelationship between the mother and child(Stern, 1995). As with individual psychother-apy, mothers also discuss their developmentalhistory in terms of interactions and experienceswith caregivers. However, the difference withthis approach is that the therapist observes theinteractions between the mother and the child tofacilitate the mother linking her past experi-ences and own attachment style to that of hercurrent relationship with her child. There areseveral codified examples of this type of parent–infant relationship psychotherapy, includingWatch, Wait and Wonder (WWW; Muir, Lo-jkasek, & Cohen, 1999); Preschooler–ParentPsychotherapy (PPP; also referred to as infant-parent psychotherapy, and toddler–parent psy-chotherapy; e.g., Cicchetti, Rogosch, & Toth,2000); and Circle of Security (COS; Marvin,Cooper, Hoffman, & Powell, 2002). These in-terventions vary in terms of amount of psychoe-duction, with WWW providing the least parenttraining and COS providing the most structuredformat, specifically in regards to the skills nec-essary to provide a secure base for infants and
toddlers. For example, in COS, parents recordtheir interactions with their infant and are givenexplicit feedback in a group psychotherapy ses-sion regarding the techniques they use whileengaging with their child. These interventionshave been applied widely with maltreated chil-dren (e.g., Toth, Maughan, Manly, Spagnola, &Cicchetti, 2002), disadvantaged parent–childdyads (e.g., Hoffman, Marvin, Cooper, & Pow-ell, 2006) and depressed mothers (e.g., Cic-chetti, Toth, & Rogosch, 1999).
Newman and Stevenson (2008) describe theapplication of WWW with 20 mothers who hada diagnosis BPD. However, it was not modifiedfrom its original form. Although this applicationdid not involve an evaluation of this treatments’effectiveness in improving maternal–infant re-lationship outcomes, it is the only publishedpaper that we are aware of that describes atreatment application for mothers with BPD.WWW involved 12 to 14 therapy sessions overa 5-month period. The first half of the sessioninvolved the mother being invited by the ther-apist to follow her child’s lead in playing withtoys. The second half of the session involvedthe therapist discussing with the mother theactivities initiated by the child as well as themother’s understanding of the child’s behaviorduring the play session. They also describe thedifficulties parents expressed to their therapistsregarding everyday parenting skills, for exam-ple maintaining daily feeding and sleepingschedules for their infants. The authors electednot to address these issues but to stick strictly tothe WWW protocol, believing that this inter-vention would better serve the long-term out-comes for the child than would parent manage-ment training techniques.
Results regarding the efficacy of these inter-ventions in improving attachment security aremixed (see Lieberman & Zeanah, 1999, for areview). There is great variability regarding thetechniques employed across different attach-ment-based interventions, which has likely im-peded researchers’ ability to demonstrate theireffectiveness. Findings from a meta-analysis byvan Ijzendoorn, Juffer, and Duyvesteyn (1995)demonstrated that while attachment-based inter-ventions with mothers increased maternal sen-sitivity toward their infants and children, theyhad little impact on attachment security of themother or the child. More recent efforts haveincluded manualizing these interventions, espe-
8 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
cially for parent–child dyads, which has re-sulted in more evidence supporting their effec-tiveness in improving attachment security. Spe-cifically, PPP for depressed mothers (Cicchettiet al., 1999) and maltreated children (Toth et al.,2002), COS for disadvantaged parent–toddler orparent–preschool dyads in Head Start and EarlyHead Start Programs (Hoffman et al., 2006;Marvin et al., 2002), as well as WWW forhigh-risk mother–infant dyads (Cohen et al.,2002) have all demonstrated efficacy for im-proving attachment security and/or attachmentorganization in children.
Even though attachment-based interventionsare becoming codified and researchers seemeager to demonstrate their effectiveness in im-proving attachment security in high-risk parent–infant dyads, the utility of these interventionswhen offered alone for mothers with BPD andtheir children may be compromised. There ap-pears to be a gap between the objectives ofattachment-based interventions and the goals ofmothers with BPD when they seek professionalhelp. Findings from research regarding parent-ing practices and efficacy underscore this con-cern (Conroy et al., 2009; Newman et al., 2007).Attachment-based interventions applied withoutexplicit focus on parenting skills are unlikely toalleviate the distress and concerns they have forproviding basic needs for their children. It ap-pears that mothers with BPD may require psy-choeducation and parent skills training beforeaddressing parent–infant attachment strategies.
Psychoeducational Interventions
In contrast to attachment therapies where thepatient is primarily the individual with BPD,psychoeducational approaches typically provideinformation on a variety of issues relevant tofamily members of the afflicted, includingspouses, adult children, friends, and parents ofteens. Although none of these treatments havebeen developed specifically for mothers withBPD and their offspring, we review them herebecause of their relevance to a systems-basedapproach to the treatment of this disorder. Inaddition, many of the guiding principles of fam-ily psychoeducation, including forming supportnetworks with other individuals in the group(e.g., other mothers) as well as learning infor-mation about the targeted individual (e.g., in-fancy and toddlerhood developmental mile-
stones), will be relevant for a parent– childintervention for mothers with BPD.
Family-based psychoeducation programs forindividuals with serious mental illness have re-ceived extensive empirical support for reducingrelapse rates and reducing family stress andburden (for a review see Cohen et al., 2008).The impact of family psychoeducation for indi-viduals with BPD has lagged behind that ofother forms of serious mental illness, especiallyschizophrenia. Gunderson and colleagues(1997) advocate for a family psychoeducationalapproach to the treatment of BPD. They de-scribe the development of a pilot Multiple Fam-ily Group (MFG) program and reported im-provements in family communication andfamily burden after 6 months of treatment. Thereare three treatments that include family psy-choeducation as one component of the treat-ment model and have published at least oneempirical article on the effectiveness of the in-tervention for families with BPD: (a) FamilyConnections (FC; Fruzzetti & Hoffman, 2004),(b) Systems Training for Emotional Predictabil-ity and Problem Solving (STEPPS; Blum,Pfohl, St. John, Monahan, & Black, 2002), and(c) Multigroup Family Skills Training as part ofDialectical Behavior Therapy for adolescents(Miller, Rathus, & Linehan, 2006). The relativefocus on the family members and other supportpersons compared with the afflicted individualvaries among these treatments. FC focuses ex-clusively on family psychoeducation and theother programs focus solely on the individualwith BPD and include family members andother support persons in an ancillary fashion.
Overall, research supports FC to alleviatecaregiver stress and STEPPS and multifamilyskills training to improve patient outcomes. Weare not aware of research to date that has ex-amined the impact of family psychoeducationalapproaches on both caregiver stress and patientoutcomes. Furthermore, STEPPS and multifam-ily groups do not routinely collect informationfrom family members or friends involved in thetreatment, which limits our ability to determinethe effectiveness of these treatments for familyand friends involvement in treatment. Nonethe-less, these programs have implications for thedevelopment of parent–child interventions formothers with BPD, especially if the child is alsoexperiencing psychological problems. Motherswith BPD may benefit from information about
9CHILDREN OF MOTHERS WITH BPD
typical and atypical child development aswell as recommended parenting practices andbehaviors.
Implications for the Development of aParenting Intervention for Mothers
With BPD
On the basis of our review of parenting prac-tices of mothers with BPD, as well as the poorpsychosocial outcomes characterized by manyof their children, a parent–child treatment inter-vention specifically for mothers with BPD isneeded. An intervention for mothers and chil-dren should address the unique parenting chal-lenges that mothers with BPD experience,namely experiencing oscillations between hos-tile control and withdrawn behaviors as welloscillations between intrusiveness and coldness.It is also important for this intervention to ad-dress parenting behaviors that may be moreeffective given existing vulnerabilities (e.g.,temperament) in the child. In the next sections,we describe the targets for this intervention thatincorporates what we know about attachmentand family based interventions for BPD.
Psychoeducation RegardingChildhood Development
As discussed previously, we think that moth-ers with BPD may first need basic psychoedu-cation on appropriate developmental tasks andexpectations. Many mothers are unfamiliar withappropriate developmental milestones and mayhave difficulty coping with the normal behav-iors of infants, children, and adolescents. Thismay lead to maternal stress and a failure to meetthe child’s needs. By learning what happens asan infant grows into a toddler and a toddler intoa preschooler, mothers can be better preparedfor the challenges ahead and develop reasonableexpectations given the child’s current develop-mental state. For example, mothers with BPDmay believe that the cries of their infant daugh-ter or son reflect that they are a bad parent.Basic psychoeducation on an infant’s needs andcognitions may alter these beliefs and create amore positive relationship between the motherand child. Mothers may benefit from psychoe-ducation regarding basic parenting skills andpositive parenting, such as how to get a child to
go to bed, how to manage feeding, and non-physical discipline strategies. Learning this in-formation may help the mother take on thechild’s perspective and mothers may find it ben-eficial to know what signs to look for in thegrowth and development of their children. Withthe help of a therapist, mothers can assess andcelebrate their child’s growth and development.
Mothers can learn that each child is differentand possess his or her own needs. Instead ofpunishing or neglecting a younger child becausehe or she does not behave like an older sibling,mothers will be able to appreciate the child forhis or her unique qualities and developmentaltrajectory. Education on the developmentalmilestones also needs to extend beyond infancyand toddlerhood. Important physical, emotional,and cognitive changes occur throughout child-hood and adolescence. Knowledge about thesechanges may assist mothers in realizing thattheir role is still crucial for facilitating positiveoutcomes in older children even though theyare no longer physically dependent on theircaretaker.
Mothers can also learn that previous parent-ing experiences with their own caretakers canbe a trap, leading to ineffective parenting strat-egies with their current child. They may need tolearn how to identify oscillations between con-trolling, punitive parenting to more permissiveparenting practices by ignoring or withdrawing.
Skills To Promote Consistency inScheduling and Monitoring
As stated above, the importance of psychoe-ducation in developmental milestones extendsinto consistency in scheduling and monitoring.The studies reviewed above suggest that moth-ers with BPD may have difficulty maintaining astable and nurturing environment for their chil-dren. For example, Feldman and colleagues(1995) found that children of BPD motherswere exposed to several facets of environmentalinstability such as frequent changes in housingand schooling, removal from the home, andmaternal suicide attempts. In addition, researchsuggests that mothers with BPD may have dif-ficulties in scheduling and providing consistentfeeding and sleep–wake times (Conroy et al.,2009). An important intervention target formothers with BPD will learn the importance ofproviding a consistent and predictable routine
10 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
for their child that also consists of predictabletransition times, for example from play to sleeptime. Routines provide both a sense of structureand security to children. Routines assist chil-dren in learning that their environment or homeis a stable and safe place, and research haspromoted the protective effects of parental rou-tines and monitoring (Murphy, Marelich, Her-beck, & Payne, 2009). For example, the adoles-cents of mothers with HIV/AIDS who engagedin more family routines showed lower rates ofanxiety, depression, and conduct disorder (Mur-phy, Marelich, Herbeck, & Payne, 2009). Thefamily routine of meal time has been associatedwith fewer depressive symptoms, alcohol use,and marijuana use in adolescents (Eisenberg etal., 2004).
Parental monitoring of their children’s activ-ities and behaviors is a key feature of a stableand predictable home environment. Consistentmonitoring and supervision has been demon-strated to be an important factor to reduce child-hood injuries (e.g., Petrass, Blitvich, & Finch,2009). In addition, these parenting strategies arealso associated with less substance use as wellas fewer delinquent behaviors during adoles-cence and young adulthood (e.g., Clark, Kirisci,Mezzich, & Chung, 2008; Hoeve et al., 2007).Mothers with BPD may have difficulty consis-tently monitoring and supervising their child,vacillating between using harsh punishmentstrategies to control their children to laissez-faire, permissive strategies that provide littleguidance for their children. Thus, a related tar-get for intervention with this population will beto train mothers in how to effectively monitor,supervise and set limits with their child (cf.Koestner, Ryan, Bernieri, & Holt, 2006).
In sum, important intervention targets for thispopulation will be to assist mothers in settingroutines for their child as well as effective waysof adhering to them even during difficult cir-cumstances. Learning about the psychologicalimportance of routines (both for themselves andtheir children) as well as how to effectively startand maintain a schedule would be useful. Inaddition, learning how to consistently monitorand supervise their child based on their devel-opmental stage and individualized needs wouldalso be important. Increasing these skills willpromote parenting self-efficacy and decreasedistress regarding their role as a parent.
Skills to Promote Consistency in Warmthand Nurturance
Emotion related parenting practices are be-lieved to play a key role in the socialization ofemotion regulation in children (Morris et al.,2007). Several studies suggest that failing toregulate negative emotions may be associatedwith psychopathology during childhood and ad-olescence (e.g., Eisenberg et al., 2001).
Research suggests that parents possess a “me-taemotion philosophy” that guides responses totheir children’s emotional expressions (Gott-man, Katz, & Hooven, 1996). Parental discom-fort with emotional displays has been shown tobe associated with worse emotion regulationand behavior problems (Lunkenheimer, Shields,& Cortina, 2007). Given the research on mater-nal BPD reviewed, it appears that these mothersmay be likely to engage in parental emotion-dismissing behaviors, setting their children upfor difficulties in emotion regulation.
Maternal responses to their child’s emotionalexpression also play a significant role in teach-ing the child how to manage his or her ownemotions (Eisenberg et al., 1996; Morris et al.,2007). Mothers who respond positively to theirchildren’s emotional displays support thechild’s emotion regulation by encouraging theuse of more adaptive strategies, such as reap-praisal and problem solving. Supportive mater-nal responses can also assist children in prac-ticing strategies for managing emotions duringmore stressful social interactions with peers andadults.
Mothers with BPD may utilize nonsupportiveemotion socialization strategies and invalidatethe emotions of their children. Mothers whoinaccurately perceive their child’s emotions areparticularly likely to have invalidating re-sponses to their children’s emotional displays(Gottman, Katz, & Hooven, 1997). Criticizing,mocking, or punishing a child for his or heremotional expression may encourage the sup-pression of emotion and the use of avoidant oraggressive emotion regulation strategies (e.g.,Eisenberg et al., 1996). This may in turn lead tochildren who deny or question their emotionsand emotional responses. Several studies re-viewed above suggest that mothers with BPDmay engage in nonsupportive responses to theirchildren’s emotional displays (e.g., Johnson etal., 2006). When these children are later faced
11CHILDREN OF MOTHERS WITH BPD
with situations that provoke negative emotions,they may learn to suppress the emotional ex-pression while still experiencing heightenedphysiological arousal (Gross & Levenson,1997).
An important target for these mother–childdyads will be to facilitate mother’s respondingpositively and consistently to their children’semotional displays. It will also be important tohelp the mother plan how to consistently pro-vide warmth and nurturance even during timesof her own extreme emotional distress and urgesto avoid or control the child’s emotionalexpression.
Mindfulness-Based ParentingSkills To Facilitate Behavioral andEmotional Consistency
To engage in providing consistent behavioraland emotional support to their children, motherswith BPD may benefit from mindfulness-basedparenting strategies. Dumas (2005) describesthe habitual nature of many disagreements andconflicts that arise between parents and childrenand argues that mindfulness based parentingstrategies can help families become “unstuck”from such negative patterns. After 8 weeks ofmindfulness training with parents and adoles-cents with externalizing disorders, children re-ported a significant reduction in both internal-izing and externalizing symptoms and parentsreported an improvement in goal attainmentwith their child (Bgels, Hoogstad, van Dun, deSchutter, Restifo, 2005). The goal of self-awareness might help the mother with BPD gainobjectivity in difficult parenting situations, es-pecially when the child is experiencing a strongemotion or eliciting a strong emotion in themother. Self-awareness would also help moth-ers with BPD learn their own limits in parentingand when to ask for support and advice. This“metaskill” weaved throughout the interventionmight lead to an improvement in the ability toprovide a stable warm home environment.
Limitations
Despite the strong rationale for a specificparenting intervention for mothers with BPD,there are several factors that may limit interven-tion development. First, there is a lack of infor-
mation on this topic. For instance, we do noteven have accurate estimates regarding theprevalence of mothers with BPD. Second, werecognize that many children of mothers withBPD are resilient to poor outcomes and thatpositive outcomes may be because of the excep-tional parenting capabilities of some motherswith BPD. We also realize that a variety ofenvironmental factors, not only parenting prac-tices, put children at risk for the development ofBPD. However, we feel that mothers with BPD,because of specific aspects of their illness, mayface special challenges to parenting and thatincreased research in this area is sorely needed.The assumption underlying this review is thatparenting skills are amenable to change, andthat these changes may have profound positiveeffects on children’s outcomes, especially whenthese skills deficits are targeted during earlydevelopment.
Conclusions
In sum, genetic and environmental vulnera-bilities put children of mothers with BPD at riskfor BPD and related psychopathology. One en-vironmental context that may confer risk is par-enting. Mothers with BPD may encounterunique parenting challenges, especially in lightof the lack of efficacy they feel as parents. Theparenting strategy that might be most deleteri-ous to children of mothers with BPD may beoscillations between extreme forms of controland passivity that provide little consistency forthe child’s day to day experience. By addressingparenting skills, we expect to see improvementsin parent–child interactions, which will lead toreductions in the mother’s and child’s distress.Based on our thorough review of the literature,we outline several points for a parenting inter-vention, namely psychoeducation, consistencyin scheduling and monitoring, consistency inwarmth and nurturance, as well as the applica-tion of mindfulness-based parenting strategies.The development of an intervention for motherswith BPD is critical to ameliorate parentingproblems and promote the positive adjustmentof children. We hope that this review will gen-erate novel research questions regarding parent-ing strategies in mothers with BPD, as well asspur treatment development efforts for thispopulation.
12 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
References
Abela, J. R. Z., Hankin, B. L., Haigh, E. A. P.,Adams, P., Vinokuroff, T., & Trayhern, L. (2005).Interpersonal vulnerability to depression in high-risk children: The role of insecure attachment andreassurance seeking. Journal of Clinical Child andAdolescent Psychology, 34, 182–192.
Bagge, C. L., Nickell, A., Stepp, S., Durrett, C.,Jackson, K., & Trull, T. (2004). Borderline per-sonality disorder features predict negative out-comes two years later. Journal of Abnormal Psy-chology, 113, 279–288.
Bandelow, B., Krause, J., Wedekind, D., Broocks,A., Hajak, G., & Ruther, E. (2005). Early traumaticlife events, parental attitudes, family history, andbirth risk factors in patients with borderline per-sonality disorder and healthy controls. PsychiatryResearch, 134, 169–179.
Barnow, S., Spitzer, C., Grabe, H. J., Kessler, C., &Freyberger, H. J. (2006). Individual characteris-tics, familial experience, and psychopathology inchildren of mothers with borderline personalitydisorder. Journal of the American Academy ofChild & Adolescent Psychiatry, 45, 965–972.
Bender, D. S., Dolan, R. T., Skodol, A. E., Sanislow,C. A., Dyck, I. R., McGlashan, T. H., . . . Gunder-son, J. G. (2001). Treatment utilization by patientswith personality disorders. American Journal ofPsychiatry, 158, 295–302.
Berg-Nielsen, T. S., Vikan, A., & Dahl, A. A. (2002).Parenting related to child and parental psychopa-thology: A descriptive review of the literature.Clinical Child Psychology and Psychiatry, 7, 529–552.
Bezirganian, S., Cohen, P., & Brook, J. S. (1993).The impact of mother–child interaction on thedevelopment of borderline personality disorder.American Journal of Psychiatry, 150, 1836–1842.
Blum, N., Pfohl, B., St. John, D., Monahan, P., &Black, D. W. (2002). STEPPS: A cognitive-behavioral systems-based group treatment for out-patients with borderline personality disorder: Apreliminary report. Comprehensive Psychiatry, 43,301–310.
Bögels, S., Hoogstad, B., van Dun, L., de Schutter,S., & Restifo, K. (2005). Mindfulness training foradolescents with externalizing disorders and theirparents. Behavioural and Cognitive Psychother-apy, 36, 193–209.
Bornovalova, M. A., Gratz, K. L., Delany-Brumsey,A., Paulson, A., & Lejuez, C. W. (2006). Temper-amental and environmental risk factors for border-line personality disorder among inner-city sub-stance users in residential treatment. Journal ofPersonality Disorders, 20, 218–231.
Bretherton, I., Oppenheim, D., Buchsbaum, H.,Emde, R. N., & The MacArthur Narrative Group.
(1990). MacArthur Story Stem Battery (MSSB).Unpublished manuscript.
Bretherton, I., Ridgeway, D., & Cassidy, J. (1990).Assessing internal working models of the attach-ment relationship. In M. T. Greenberg, D. Cic-chetti, & M. Cummings (Eds.), Attachment in thepreschool years (pp. 273–308). Chicago, IL: Uni-versity of Chicago Press.
Cacioppo, J. T., Berntson, G. G., Sheridan, J. F., &McClintock, M. K. (2000). Multilevel integrativeanalyses of human behavior: Social neuroscienceand the complementing nature of social and bio-logical approaches. Psychological Bulletin, 126,829–843.
Cicchetti, D., Rogosch, F. A., & Toth, S. L. (2000).The efficacy of toddler-parent psychotherapy forfostering cognitive development in offspring ofdepressed mothers. Journal of Abnormal ChildPsychology, 28, 135–148.
Cicchetti, D., Toth, S. L., & Rogosch, F. A. (1999).The efficacy of toddler-parent psychotherapy toincrease attachment security in offspring of de-pressed mothers. Attachment and Human Develop-ment, 1, 34–66.
Clark, D. B., Kirisci, L., Mezzich, A., & Chung, T.(2008). Parental supervision and alcohol use inadolescence: Developmentally specific interac-tions. Journal of Development and Behavioral Pe-diatrics, 29, 285–292.
Cohen, A. N., Glynn, S. M., Murray-Swank, A. B.,Barrio, C., Fischer, E. P., McCutcheon, S. J., . . .Dixon, L. B. (2008). The family forum: Directionsfor the implementation of family psychoeducationfor severe mental illness. Psychiatric Services, 59,40–48.
Cohen, P. (1996). Childhood risks for young adultsymptoms of personality disorder: Method andsubstance. Multivariate Behavioral Research, 31,121–148.
Cohen, P., Crawford, T. N., Johnson, J. G., & Kasen,S. (2005). The children in the community study ofdevelopmental course of personality disorder.Journal of Personality Disorders, 19, 466–486.
Conroy, S., Marks, M. N., Schacht, R., Davies, H. A.,& Moran, P. (2009). The impact of maternal de-pression and personality disorder on early infantcare. Social Psychiatry and Psychiatric Epidemi-ology, 45, 285–92.
Crandell, L. E., Patrick, M. P. H., & Hobson, R. P.(2003). “Still-face” interactions between motherswith borderline personality disorder and their2-month-old infants. British Journal of Psychiatry,183, 239–247.
Distel, M. A., Trull, T. J., Derom, C. A., Thiery,E. W., Grimmer, M. A., Martin, N. G., . . .Boomsma, D. I. (2007). Heritability of borderlinepersonality disorder features is similar across threecountries. Psychological Medicine, 38, 1219–29.
13CHILDREN OF MOTHERS WITH BPD
Dumas, J. E. (2005). Mindfulness-based parent train-ing: Strategies to lessen the grip of automaticity infamilies with disruptive children. Journal of Childand Adolescent Psychology, 34, 779–791.
Eisenberg, M. A. Olson, R. E., Neumark-Sztainer,D., Story, M., & Bearinger, R. H. (2004). Corre-lations between family meals and psychosocialwell-being among adolescents. Archives of Pedi-atrics and Adolescent Medicine, 158, 792–796.
Eisenberg, N., Cumberland, A., Spinrad, T. L.,Fabes, R. A., Shepard, S. A., Resier, M., . . . Guth-rie, I. K. (2001). The relations of regulation andemotionality to children’s externalizing and inter-nalizing problem behavior. Child Develop-ment, 72, 1112–1134.
Eisenberg, N., Fabes, R. A., & Murphy, B. C. (1996).Parents’ reactions to children’s negative emotions:Relations to children’s competence and comfortingbehavior. Child Development, 67, 2227–2247.
Eley, T. C., Sugden, K., Corsico, A., Gregory, A. M.,Sham, P., McGuffin, P., . . . Craig, I. W. (2004).Gene-environment interaction analysis of sero-tonin system markers with adolescent depression.Molecular Psychiatry, 9, 908–915.
Feinberg, M. E., Button, T. M., Neiderhiser, J. M.,Reiss, D., & Hetherington, E. M. (2007). Parentingand adolescent antisocial behavior and depression.Archives of General Psychiatry, 64, 457–465.
Feldman, R. B., Zelkowitz, P., Weiss, M., Vogel, J.,Heyman, M., & Paris, J. (1995). A comparison ofthe families of mothers with borderline and non-borderline personality disorders. ComprehensivePsychology, 26, 157–163.
Freidel, R. O. (2004). Borderline personality disor-der demystified: An essential guide for understand-ing and living with BPD. New York, NY: Marlow& Company.
Fruzzetti, A. E., & Hoffman, P. D. (2004). FamilyConnections workbook and training manual. Rye,NY: National Education Alliance for BorderlinePersonality Disorder.
Fruzzetti, A. E., Shenk, C., & Hoffman, P. D. (2005).Family interaction and the development of border-line personality disorder: A transactional model.Development and Psychopathology, 17, 1007–1030.
Gottman, J. M., Katz, L. F., & Hooven, C. (1996).Parental meta-emotion philosophy and the emo-tional life of families: Theoretical models and pre-liminary data. Journal of Family Psychology, 10,243–268.
Gottman, J. M., Katz, L. F., & Hooven, C. (Eds.).(1997). Meta-emotion: How families communicateemotionally. Hillsdale, NJ: Erlbaum.
Gross, J. J., & Levenson, R. W. (1997). Hidingfeelings: The acute effects of inhibiting negativeand positive emotion. Journal of Abnormal Psy-chology, 106, 95–103.
Gunderson, J. G., Berkowitz, C., & Ruiz-Sancho, A.(1997). Families of borderline patients: A psy-choeducational approach. Bulletin of the Men-ninger Clinic, 61, 446–457.
Herr, N. R., Hammen, C., & Brennan, P. A. (2008).Maternal borderline personality disorder symp-toms and adolescent psychosocial functioning.Journal of Personality Disorders, 22, 451–465.
Hobson, P. R., Patrick, M. Crandell, L., Garcıa-Perez, R., & Lee, A. (2005). Personal relatednessand attachment in infants of mothers with border-line personality disorder. Development and Psy-chopathology, 17, 329–347.
Hobson, P. R., Patrick, M. P. H., Hobson, J. A.,Crandell, L. Bronfman, E., & Lyons-Ruth, K.(2009). How mothers with borderline personalitydisorder related to their year-old infants. The Brit-ish Journal of Psychiatry, 195, 325–330.
Hobson, R. P., Patrick, M. P. H., & Valentine, J. D.(1998). Objectivity in psychoanalytic judgements.British Journal of Psychiatry, 173, 172–177.
Hoeve, M., Smeenk, W., Loeber, R., Stouthamer-Loeber, M., van der Laan, P. H., Gerris, J. R., &Dubas, J. S. (2007). Long term effects of parentingand family characteristics on delinquency of maleyoung adults. European Journal of Criminol-ogy, 4, 161–194.
Hoffman, K. T., Marvin, R. S., Cooper, G., & Powell,B. (2006). Changing toddlers’ and preschoolers’attachment classifications: The circle of securityintervention. Journal of Consulting and ClinicalPsychology, 74, 1017–1026.
Huh, D., Tristan, J., Wade, J., & Stice, E. (2006).Does problem behavior elicit poor parenting?Journal of Adolescent Research, 21, 185–204.
Johnson, J. G., Cohen, P., Brown, J., Smailes, E. M.,& Bernstein, D. P. (1999). Childhood maltreat-ment increases risk for personality disorders dur-ing early adulthood. Archives of General Psychia-try, 56, 600–606.
Johnson, J. G., Cohen, P., Chen, H., Kasen, S., &Brook, J. S. (2006). Parenting behaviors associatedwith risk for offspring personality disorder duringadulthood. Archives of General Psychiatry, 63,579–587.
Johnson, J. G., Cohen, P., Gould, M. S., Kasen, S.,Brown, J., & Brook, J. S. (2002). Childhood ad-versities, interpersonal difficulties, and risk for sui-cide attempts during late adolescence and earlychildhood. Archives of General Psychiatry, 59,741–749.
Johnson, J. G., Cohen, P., Kasen, S., & Brook, J. S.(2006). Personality disorders evidence by earlyadulthood and risk for anxiety disorders duringmiddle school. Journal of Anxiety Disorders, 20,408–426.
Johnson, J. G., Cohen, P., Kasen, S., Smailes, E., &Brook, J. S. (2001). Association of maladaptive
14 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE
parental behavior with psychiatric disorder amongparents and their offspring. Archives of GeneralPsychiatry, 58, 453–460.
Johnson, J. G., Cohen, P., Smailes, E. M., Skodol,A. E., Brown, J., & Oldham, J. M. (2001). Child-hood verbal abuse and risk for personality disor-ders during adolescence and early adulthood.Comprehensive Psychiatry, 42, 16–23.
Kaufman, J., Yang, B., Douglas-Palumberi, H.,Grasso, D., Lipschitz, D., Houshyar, S., . . .Gelernter, J. (2006). Brain-derived neurotrophicfactor-5-HTTLPR gene interactions and environ-mental modifiers of depression in children. Biolog-ical Psychiatry, 59, 673–680.
Koestner, R., Ryan, R. M., Bernieri, F., & Holt, K.(2006). Setting limits on children’s behavior: Thedifferential effects of controlling vs. informationalstyles on intrinsic motivation and creativity. Jour-nal of Personality, 52, 233–248.
Krause, E. D., Mendelson, T., & Lynch, T. R. (2003).Childhood emotional invalidation and adult psy-chological distress: The mediating role of emo-tional inhibition. Child Abuse and Neglect, 27,199–213.
Levy, K. N. (2005). The implications of attachmenttheory and research for understanding borderlinepersonality disorder. Development and Psychopa-thology, 17, 959–986.
Lieberman, A. F., Weston, D. R., & Pawl, J. H.(1991). Preventative intervention and outcomewith anxiously attached dyads. Child Develop-ment, 62, 199–209.
Lieberman, A. F., & Zeanah, C. H. (1999). Contri-butions of attachment theory to infant-parent psy-chotherapy and other interventions with infantsand young children. In J. L. Cassidy & P. R.Shaver (Eds.), Handbook of attachment: Theory,research, and clinical applications (pp. 555–574).New York, NY: Guilford Press.
Linehan, M. M. (1993). Cognitive-behavioral treat-ment of borderline personality disorder. NewYork, NY: Guilford Press.
Lunkenheimer, E. S., Shields, A. M., & Cortina, K. S.(2007). Parental emotion coaching and dismissingin family interaction. Social Development, 16,232–248.
Macfie, J., Fitzpatrick, K. L., Rivas, E. M., & Cox,M. J. (2008). Independent influences upon mother-toddler role reversal: Infant-mother attachmentdisorganization and role reversal in mother’s child-hood. Attachment & Human Development, 10, 29–39.
Macfie, J., & Swan, S. A. (2009). Representation ofthe caregiver-child relationship and of the self, andemotion regulation in the narratives of young chil-dren whose mothers have borderline personalitydisorder. Development and Psychopathology, 21,993–1011.
Main, M., & Hesse, E. (1990). Parents’ unresolvedtraumatic experiences are related to infant disor-ganized/disoriented attachment status: Is fright-ened and/or frightening parental behavior the link-ing mechanism? In M. T. Greenberg, D. Cicchetti,& E. M. Cummings (Eds.), Attachment in thepreschool years: Theory, research, and interven-tion (pp. 161–182). Chicago: University of Chi-cago Press.
Marvin, R., Cooper, G., Hoffman, K., & Powell, B.(2002). The circle of security project: Attachment-based intervention with caregiver-pre-school childdyads. Attachment & Human Development, 4,107–127.
Miller, A. L., Rathus, J. H., & Linehan, M. M.(2006). Dialectical behavior therapy for suicidaladolescents. New York, NY: Guilford Press.
Morris, A. S., Silk, J. S., Steinberg, L., Myers, S. S.,& Robinson, L. R. (2007). The role of the familycontext in the development of emotion regulation.Social Development, 16, 361–368.
Muir, E., Lojkasek, M., & Cohen, N. J. (1999).Watch, Wait, and Wonder: A manual describing aninfant-led approach to problems in infancy andearly childhood. Toronto, ON: Hincks-DellcrestInstitute.
Murphy, D. A., Marelich, W. D., Herbeck, D. M., &Payne, D. L. (2009). Family routines and parentalmonitoring as protective factors among early andmiddle adolescents affected by maternal HIV/AIDS. Child Development, 80, 1676–1691.
Newman, L. K., & Stevenson, C. S. (2008). Issues ininfant-parent psychotherapy for mothers with bor-derline personality disorder. Clinical Child Psy-chology and Psychiatry, 13, 505–514.
Newman, L. K., Stevenson, C. S., Bergman, L. R., &Boyce, P. (2007). Borderline personality disorder,mother-infant interaction and parenting percep-tions: Preliminary findings. Australian and NewZealand Journal of Psychiatry, 41, 598–605.
Ogawa, J. R., Sroufe, L. A., Weinfield, N. S., Carl-son, E. A., & Egeland, B. (1997). Developmentand the fragmented self: Longitudinal study ofdissociative symptomatology in a nonclinical sam-ple. Developmental Psychopathology, 9, 855–879.
Petrass, L., Blitvich, J. D., & Finch, C. F. (2009).Parent/caregiver supervision and child injury: Asystematic review of critical dimensions for under-standing this relationship. Family and CommunityHealth, 32, 123–135.
Riso, L. P., Klein, D. N., Anderson, R. L., &Ouimette, P. C. (2000). A family study of outpa-tients with borderline personality disorder and nohistory of mood disorder. Journal of PersonalityDisorders, 14, 208–17.
Schulz, P. M., Soloff, P. H., Kelly, T., Morgenstern,M., Franco, R., & Schulz, S. C. (1989). A family
15CHILDREN OF MOTHERS WITH BPD
history of borderline subtypes. Journal of Person-ality Disorders, 3, 217–229.
Silverman, J. M., Pinkham, L., Horvath, T. B., Coc-caro, E. F., Klar, H., Schear, S., . . . Siever, L. J.(1991). Affective and impulsive personality disor-der traits in the relatives of patients with borderlinepersonality disorder. American Journal of Psychi-atry, 148, 1378–1385.
Skodol, A. E., & Bender, D. S. (2003). Why arewomen diagnosed borderline more than men? Psy-chiatric Quarterly, 74, 349–360.
Skodol, A. E., Gunderson, J. G., McGlashan, T. H.,Dyck, I. R., Stout, R. L., Bender, D. S., . . . Old-ham, J. M. (2002). Functional impairment in pa-tients with Schizotypal, Borderline, Avoidant, orObsessive-Compulsive Personality Disorder.American Journal of Psychiatry, 159, 276–283.
Steinberg, L., & Morris, A. S. (2001). Adolescentdevelopment. In S. T. Fiske, D. L. Schacter, & C.Zahn-Waxler (Eds.), Annual review of psychology(Vol. 52, pp. 83–110). Palo Alto, CA: AnnualReviews.
Stern, D. N. (1995). The motherhood constellation: Aunified view of parent–infant psychotherapy. NewYork: Basic Books.
Suveg, C., Hoffman, B., Zeman, J., & Thomassin, K.(2009). Emotion related predictors of anxious anddepressive symptoms in youth. Child Psychiatryand Human Development, 40, 223–239.
Torgensen, S. (2000). Genetics of patients with bor-derline personality disorder. Psychiatric Clinics ofNorth America, 23, 1–9.
Toth, S. L., Maughan, A., Manly, J. T., Spagnola, M.,& Cicchetti, D. (2002). The relative efficacy of twointerventions in altering maltreated preschool chil-dren’s representation models: Implications for at-
tachment theory. Development and Psychopathol-ogy, 14, 877–908.
van Ijzendoorn, M., Juffer, F., & Duyvesteyn, M.(1995). Breaking the intergenerational cycle ofinsecure attachment: A review of the effectives ofattachment based interventions on maternal sensi-tivity and infant security. Journal of Child Psy-chology and Psychiatry, 36, 225–248.
Weiss, M., Zelkowitz, P., Feldman, R. B., Vogel, J.,Heyman, M., & Paris, J. (1996). Psychopathologyin offspring of mothers with borderline personalitydisorder: A pilot study. Canadian Journal of Psy-chiatry, 41, 285–290.
Whalen, D. J., Silk, J. S., & Dahl, R. E. (2009). Theimpact of maternal borderline personality disorder onmaternal emotional socialization and adolescentemotional vulnerability. Manuscript in preparation.
White, C. N., Gunderson, J. G., Zanarini, M. C., &Hudson, J. I. (2003). Family studies of borderlinepersonality disorder: A review. Harvard Review ofPsychiatry, 11, 8–19.
Yates, T. M. (2004). The developmental psychopa-thology of self-injurious behavior: Compensatoryregulation in posttraumatic adaptation. ClinicalPsychology Review, 21, 35–74.
Zanarini, M. C., Frankenburg, F. R., Hennen, J., &Silk, K. R. (2003). The longitudinal course ofborderline psychopathology: 6-year prospectivefollow-up of the phenomenology of borderline per-sonality disorder. American Journal of Psychiatry,160, 274–283.
Zanarini, M. C., Gunderson, J. G., Marino, M. F.,Schwartz, E. O., & Frankenberg, F. R. (1988).DSM–III disorders in the families of borderlineoutpatients. Journal of Personality Disorders, 2,292–302.
16 STEPP, WHALEN, PILKONIS, HIPWELL, AND LEVINE