Body surface area determined by whole-body CT scanning: Need for new formulae? Clinical Physiology...
Transcript of Body surface area determined by whole-body CT scanning: Need for new formulae? Clinical Physiology...
ORIGINAL ARTICLE
Body surface area determined by whole-body CT scanning:need for new formulae?Chiara Villa1, Charlotte Primeau1, Ulrik Hesse2, Hans Petter Hougen1, Niels Lynnerup1 and Birger Hesse3
1Department of Forensic Medicine, University of Copenhagen, 2Health data and Information and Communication Technology, Statens Serum Institut,
and 3Clinic of Clinical Physiology, Nuclear Medicine and PET, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark
Summary
CorrespondenceChiara Villa, Laboratory of Biological
Anthropology, Department of Forensic Medicine,
University of Copenhagen, Frederik V’s Vej 11,
DK-2100 Copenhagen, Denmark
E-mail: [email protected]
Accepted for publicationReceived 11 August 2014;
accepted 26 June 2015
Key words
body mass index; body surface area; cadavers; CT
scans; males; overweight subject
Calculation of the estimated body surface area (BSA) by body height and weighthas been a challenge in the past centuries due to lack of a well-documented goldstandard. More recently, available techniques such as 3D laser surface scanningand CT scanning may be expected to quantify the BSA in an easier and moreaccurate way. This study provides the first comparison between BSA obtainedfrom post-mortem whole-body CT scans and BSA calculated by nine predictiveformulae. The sample consisted of 54 male cadavers ranging from 20 to 87 yearsold. 3D reconstructions were generated from CT scans using Mimics software,and BSA values were automatically extracted from the program. They werecompared with nine predictive equations from the literature. Remarkably, closecorrelations (r > 0�90) were found between BSA values from CT scans and thosefrom the predictive formulae. A mean BSA of the 54 cadavers of 1�84–1�87 m2
was calculated by all formulae except one, SD values varying between 0�171 and0�223 m2. T-tests revealed significant differences between mean BSA valuescalculated with CT and three of the formulae. Regression analyses showed inter-cepts >(0;0) and slopes <1�0 using all predictive equations, with the CT scandetermination as gold standard. It is concluded that DuBois and DuBois’ equationcan be safely used in normal-weight male subjects with high accuracy, but itseems likely that BSA is underestimated in underweight subjects and overesti-mated in overweight individuals. Creation of new formulae specific for over-weight subjects and children may be needed.
Introduction
Body surface area (BSA) is an important measurement in
many physiological and pharmacological applications, and in
several relations, it has been considered a better indicator of
metabolic mass than individual’s weight, height or body mass
index (BMI). The determination of BSA has been a challenge
in the past centuries, and many BSA formulae have been
developed over the years. The DuBois brothers (1916) were
the first who empirically measured and derived a BSA equa-
tion; their formula is still widely used even though it was
based on only nine subjects. In the following years, other
researchers proposed new equations based on larger numbers
of subjects and using more robust statistical techniques (Boyd,
1935; Gehan & George, 1970; Haycock et al., 1978; Mosteller,
1987; Shuter & Aslani, 2000). However, excellent correlations
and very similar results were demonstrated (Verbraecken et al.,
2006) and no improvement using new formulae compared to
the original one has been created.
On the other hand, criticism has been raised about the use
of the DuBois and DuBois equation in children and obese
patients; indeed, specific formulae have been derived for both
categories (Haycock et al., 1978; Livingston & Lee, 2001).
After about one century, new formulae are still being
developed, in particular using techniques such as 3D laser sur-
face scan and CT scanning that may be expected to quantify
the BSA in an easier and more accurate way. Surface scanning
has been extensively tested by Jones et al. (1994), Tikuisis
et al. (2001), Yu et al. (2003; 2010) and discussed in detail by
Daniell et al. (2012). Conversely, only one pilot study on eight
Clin Physiol Funct Imaging (2015) doi: 10.1111/cpf.12284
1© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
whole-body CT scans has been carried out in oncology
patients (Martinez-M€oller et al., 2007), and a formula derived
using parameters was obtained from a single abdominal CT
image (Geraghty & Boone, 2003). The reason for the very
limited number of studies is that healthy individuals should
not be exposed to the rather high radiation exposure from a
whole-body CT scan. On the other hand, CT scans of cadavers
is regularly performed before autopsy in many forensic
departments, with the advantage that an immense amount of
data in digital format is collected. Thus, BSA can be calculated
using postprocessing software.
The purpose of this study was to calculate the BSA using
whole-body CT scans of adult, male cadavers and to compare
the obtained results with those calculated using nine formulae
reported in the literature, to evaluate the necessity of creating
new formulae.
Materials and methods
The sample consisted of 54 whole-body CT scans of male
cadavers of Caucasian origin ranging from 20 to 87 years old
with a varying body mass index (BMI: three underweight
men (BMI <18�5 kg m�2); 32 normal-weight men (BMI
18�5–24�9 kg m�2); 19 overweight men (BMI ≥25 kg m�2).
There was only one obese person (BMI 30�9 kg m�2), and
we decided to group together with the overweight subjects.
All the information for each subject about age, nationality,
weight, height and BMI, as well as BMI group, is reported in
appendix 1. The bodies were scanned within three days from
the time of death and showed no or very limited signs of
decomposition. The scans were performed using a Siemens
Sensation 4 CT scanner with the following scan settings:
120 kV, 112�50 mAs, 3 mm slice thickness, 2 mm increment
and a B31f reconstruction algorithm. The whole-body scans
were performed in two or three (n = 11) parts. All bodies
were scanned in the supine position with the arms over the
head. The head and upper part of the body was scanned first
with the head first in, and then, the body was turned around
on the gantry couch, still in the supine position, and the
lower part of the body was scanned with feet first in. In cases
of three scannings, head, upper body and lower body were
scanned separately, with head first in for the first two scans,
then with feet first in for the lower body. Overlapping areas
were kept to allow registration of the CT scan image. Particu-
lar care was taken to ascertain that good overlapping of the
scans made it possible to accurately align the two (or three)
parts of the body in the computer model. Only, individuals
with intact skin and without post-mortem bloating were
included in the study.
3D visualization of the whole body was created using Mim-
ics software (Materialise Interactive Medical Image Control
System, NV Technologielaan Belgium Materialise), an image
processing software for 3D design and modelling. BSA values
were automatically extracted from the 3D reconstructions of
the bodies generated from the CT scans. All the internal
cavities filled with air were ‘closed’, and surfaces such as
regions between the legs, the arms and the chin, where differ-
ent skin areas are in contact, were separated (Fig. 1). Particu-
lar attention was also paid to the hands, because some
subjects were in a relaxed position while others held their
hands in a clenched fist or somewhere in-between resulting in
incorrect surface area determinations (Fig. 1). The surface of
the hands of 10 individuals (two underweight, four normal-
weight, four overweight subjects) was accurately segmented.
Independently of the BMI, the surface area of the segmented
hands was approximately 5% (ranges 4�0–6�0%) of the
remaining body surface area. Therefore, to calculate the BSA,
we used the surface area obtained from the 3D visualization
of the body without the hands and then added 5% of the val-
ues to obtain total BSA.
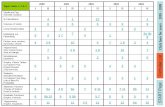
The BSA values of the 54 cadavers were also calculated from
their height and weight using nine equations (Table 1)
reported in the literature.
Statistics
The statistical analyses were performed using SPSS version
20 (IBM Corp., Chicago, IL, USA) and SAS version 9.3 (SAS
Institute Inc., Cary, NC, USA). We calculated mean BSA and
SD in m2 of the 54 cadavers from CT scans and estimated
their BSA values using the predictive formulae. Pearson’s
correlation coefficients and average differences (mean and
SD) were calculated between our CT scans and the formulae.
Student’s t-test was performed to evaluate the difference
between the BSA means; linear regression was used to esti-
mate regression lines. In addition, we used scatter plots of
the BSA from CT scans against BSA from the formulae and
Bland–Altman plots (1986) to visualize the agreement
between the methods.
Results
The mean value of BSA determined from CT scans was very
similar to that calculated using previously published predictive
formulae (Table 2): a mean BSA of the 54 male cadavers
between 1�84 and 1�87 m2 was determined by our CT
scanning and those calculated by all the formulae except one
(Yu et al., 2003). SD values varied between 0�171 and 0�223,and the lowest SD being calculated by our determinations.
Using Gehan and George’s formula, slightly higher BSA values
were calculated compared with the determination from our
CT scans, with the lowest average difference of 0�1%. Contrar-ily, the formula of Yu et al. (2003) consistently gave lower
BSA values (1�78 m2) with an average difference of 4�9%.Comparison with our BSA measurements the formula of Yu
et al. (2003) and also the formulae of Shuter & Aslani (2000)
and Tikuisis et al. (2001) gave statistically significant differ-
ences (Table 2). Appendix 1 reports the BSA values for each
subject obtained from CT scans and calculated using the nine
literature formulas.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al.2
Remarkably close correlations (r > 0�90) were found
between BSA values calculated from the CT scans and those
from the formulae in the literature (Table 2). However,
systematic variations are observed when our own BSA deter-
minations are compared with those calculated using the
formulae of Yu et al. (2003), Shuter & Aslani (2000), and to
some degree also using Tikuisis et al. (2001), cf. Fig. 2: the
majority of the BSA values lie to the left of the line of equal-
ity, that is line of perfect agreement (r = 1). Livingston and
Lee’s formula shows a slightly lower correlation (0�947) with
Table 1 BSA predictive equations used in the study.
References Year
Technique for
BSA determination Subjects
Different
BMI
Children/
Infants Equations
DuBois & DuBois (1916) 1916 Coating 9 Yes Yes BSA = 0�007184 9 H0�725 9 W0�425
Boyd (1935) 1935 Coating, surfaceintegration, triangulation
197 No Yes BSA = 0�017827 9 H0�5 9 W0�484
Gehan & George (1970) 1970 Coating, surfaceintegration, triangulation
401 No Yes BSA = 0�0235 9 H0�42246 9 W0�51456
Haycock et al. (1978) 1978 Linear geometry 81 Yes Yes BSA = 0�024265 9 H0�3964 9 W0�5378
Shuter & Aslani (2000) 2000 Coating andlinear geometry
42 No No BSA = 0�00949 9 H0�655 9 W0�441
Livingston & Lee (2001) 2001 Linear geometry 18 M29 F
Yes No BSA = 0�1173 9 W0�6466
Tikuisis et al. (2001) 2001 Surface scanning 395 M246 F
Yes No BSA = 0�0128 9 H0�6 9 W0�44(male)
Yu et al. (2003) 2003 Surface scanning 1814 M2137 F
No No BSA = 0�015925 9 (H 9 W)0�50
Yu et al. (2010) 2010 Surface scanning 135 M135 F
Yes No BSA = 0�00713989 9 H0�7437 9 W0�4040
BSA is expressed in square metre, height (H) in centimetre and weight (W) in kilogram.
(a) (b)
(c) (d)
Figure 1 3D visualizations of the hands andthe area of the chin/shoulder: (a) and (b)show the unsegmented touching skin surfaces;(c) and (d) show the same surfaces aftermanual editing. The arrows indicate the areaswhere manual separation of the surfaces wasperformed.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al. 3
our CT scans and has a large SD (0�2 m2): individuals with
BSA lower than 1�7 m2 were always overestimated and those
with BSA of ≥2�1 m2 underestimated.
The Bland–Altman plots (Fig. 3) visualize the agreements
between BSA determined by CT scans and those calculated by
the predicted formulae. If the individuals are divided into the
Table 2 BSA values obtained from CT scans and calculated using predictive equations.
Equations according to references
BSA (m2) Pearson’scorrelation
coefficient (r)
Average differencesfrom CT scans (m2) t-test
Mean BSA SD Mean (%) T P
CT scans 1�873 0�171 – – – –DuBois & DuBois (1916) 1�866 0�185 0�970* 0�006 (0�3) 0�046 0�995 0�324Boyd (1935) 1�860 0�191 0�970* 0�013 (0�7) 0�049 1�907 0�062Gehan & George (1970) 1�874 0�199 0�968* �0�002 (0�1) 0�055 �0�228 0�821Haycock et al. (1978) 1�868 0�205 0�967* 0�004 (0�2) 0�059 0�550 0�585Shuter & Aslani (2000) 1�839 0�183 0�971* 0�034 (1�8) 0�045 5�615 <0�001Livingston & Lee (2001) 1�854 0�223 0�947* 0�019 (1�0) 0�082 1�697 0�096Tikuisis et al. (2001) 1�858 0�182 0�971* 0�014 (0�7) 0�044 2�424 0�019Yu et al. (2003) 1�782 0�189 0�970* 0�091 (4�9) 0�048 14�016 <0�001Yu et al. (2010) 1�868 0�179 0�969* 0�005 (0�3) 0�045 0�801 0�427
This table shows the BSA (mean, SD), average differences (mean and SD), correlation coefficients and t-test results from comparison between BSAvalues from CT scans and BSA values calculated using predictive equations.*P < 0�001.
Figure 2 Scatter plots of BSA from CT scans (y-axis) and BSA from the predictive equations (x-axis), with line of equality.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al.4
BMI groups (underweight, normal-weight and overweight),
presented by increasing size of the circles, the differences are
obvious. As mentioned above, the BSA values calculated from
our CT scans are very closely correlated in the far majority of
moderately underweight and normal-weight subjects with val-
ues calculated by the other formulae mentioned above. In
other words, most of the formulae work well for average BSA
values. But regression analyses show that with a as the inter-
cept and b as the slope, all nine equations have intercepts
above (0;0) and slopes less than 1�0 (Table 3). This suggests
that very low BSA values, that is BSA of children, could be
overestimated and high BSA values probably underestimated
with other formulae if our determinations are correct. The
BSA values in the four overweight subjects are near or actually
outside the statistical limit of agreement (>mean � 2SD), sug-
gesting that BSA is overestimated by the predictive formulae.
The plot comparing the difference between our CT scans
and the calculations using the formula by Livingston & Lee
(2001) demonstrates that our underweight cadavers are signif-
icantly underestimated using their formula. Furthermore, the
regression analysis and the t-test both show that the formula
by Yu et al. (2003) deviates most from our CT results. The
visual impression from some of the plots in Fig. 2 also shows
a clear trend of a positive intercept and a reduced (<1) slope.
Figure 3 Bland–Altman plots of the difference in BSA as a function of the mean BSA based on CT scans and BSA based on the predictive equations.The solid line indicates the mean difference, and the two dotted lines indicate mean � 2SD. BMI groups are reflected in the size of the points.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al. 5
Discussion
This study provides the first comparison between BSA
obtained from post-mortem CT scans and BSA calculated by
predictive formulae reported in the literature, based on
different techniques including linear geometry, coating, trian-
gulation and more recent techniques like 3D surface scanning.
We found close agreement between the BSA values
determined in the adult male cadavers examined with our CT
scannings with Mimics software analyses, and values calculated
from the height and weight of the cadavers using existing for-
mulae, giving average differences of about 1% or less. As also
previously suggested (Livingston & Lee, 2001; Sardinha et al.,
2006; Verbraecken et al., 2006; Daniell et al., 2012), we
observed that BSA in the few overweight individuals is appar-
ently overestimated (Table 3). Livingston & Lee (2001)
developed a formula to improve the accuracy of overweight
subjects based on a population of 81 overweight or obese
subjects individuals. However, their formula did not improve
the accuracy of our four overweight subjects. On the contrary,
our determinations suggest significant disagreement with the
formula by Livingston & Lee (2001) both in overweight and
underweight subjects (Fig. 3), in line with the analysis of
Daniell et al. (2012), who found a similar discrepancy
between BSA values calculated by the Livingston and Lee
equation versus their 3D surface scanning.
The comparison between calculations from our CT scans
and the formulae of DuBois & DuBois (1916), Gehan &
George (1970) and Haycock et al. (1978), respectively, shows
very strong correlations and very low average differences
(0�3% or lower). Once again, in spite of the extremely limited
number of nine subjects examined in their study, the present
investigation confirms that the formula by DuBois and DuBois
produces accurate BSA values in normal-weight, male subjects.
Interesting is the comparison between the BSA generated
from the most recent techniques, that is the CT and the laser
scanners that may be anticipated to quantify BSA in a more
accurate way. We tested three formulae and found statistically
significant differences (P<0�05) between the BSA means for
two of the methods. Using the formula of Tikuisis et al.
(2001), BSA is underestimated in many subjects. The differ-
ences with the predictive formula reported by Tikuisis et al.
(2001) in their laser scanner study are very similar to our
results: they found an average difference of 0�32% with
DuBois & DuBois (1916), 0�54% with Boyd (1935) and
0�02% with Gehan & George (1970). Furthermore, in agree-
ment with our results they found an average difference of
around 1�6% with Shuter and Aslani’s formula. They reported
that their technic could be less accurate in some areas of the
body, including the upper arm, between the thighs and
around the ear, leading to an underestimation of BSA. The
lowest agreement was found with Yu et al. (2003); they
developed their formula also by laser surface scanning in a
Chinese population. The discrepancies between our data and
the values calculated from their formula were not unexpected
because high differences between BSA from surface scanner
and the predictive formulae were also reported by the authors
in relation to other predictive formulae: 3% with DuBois &
DuBois (1916), 2�1% with Shuter & Aslani (2000), 2�6% with
Boyd (1935), 5�7% with Gehan & George (1970) and 5�3%with Haycock et al. (1978). These differences could be due to
methodological differences in ancestry composition, resulting
in a significantly smaller mean body BMI and BSA. In a more
recent study, Yu and other colleagues (Yu et al., 2010) devel-
oped another formula based on Taiwanese subjects using a
more sophisticated laser scanner system and found an average
difference of 0�39% with DuBois and DuBois formula. We
also found much better agreement with the more recent study
and difference of 0�3%.Using whole-body CT scans, only one pilot study was
performed (Martinez-M€oller et al., 2007); the authors used the
whole-body CT of nine living subjects and reported,
differently from our results, a higher percentage of average
differences with DuBois and DuBois (2�2%) and Gehan and
George (2�5%). This may be due to their small sample size.
The use of the CT scans to calculate BSA has several advan-
tages compared with a surface scanner. The CT scanning does
not present any difficulty in areas where fat deposits artificially
enclose the space, like the regions between thighs or under
the upper arms: these areas can be easily corrected. Moreover,
no surfaces of the body cannot be properly scanned by a CT
scanner, nor is there any need to restore gaps in certain criti-
cal areas in the 3D models. These problems were reported by
Tikuisis et al. (2001) for areas such as ears, hands and feet
using a laser scanner.
Unfortunately, a true gold standard is very complicated to
create for BSA determination except by the hard and original
Table 3 CT scan as a function of the different formulae.
Estimate SE
DuBois & DuBois (1916) Intercept (a) 0�197 0�059Slope (b) 0�898 0�031
Boyd (1935) Intercept (a) 0�260 0�056Slope (b) 0�867 0�030
Gehan & George (1970) Intercept (a) 0�315 0�056Slope (b) 0�831 0�030
Haycock et al. (1978) Intercept (a) 0�367 0�055Slope (b) 0�806 0�029
Shuter & Aslani (2000) Intercept (a) 0�207 0�058Slope (b) 0�906 0�031
Livingston & Lee (2001) Intercept (a) 0�523 0�064Slope (b) 0�728 0�034
Tikuisis et al. (2001) Intercept (a) 0�175 0�058Slope (b) 0�914 0�031
Yu et al. (2003) Intercept (a) 0�306 0�055Slope (b) 0�879 0�031
Yu et al. (2010) Intercept (a) 0�143 0�062Slope (b) 0�926 0�033
CT scan = a + bx, a being the intercept, b the slope and x the valuecalculated from the different formulae.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al.6
way of DuBois & DuBois (1916). In our opinion, the surface
area measurement from the CT scanner is very accurate: CT
scanning can easily detect the edge of the body; the thin slice
thickness gives detailed information of the body surface; and
modern postprocessing software can easily create 3D of the
body, based on the differences of HU values between the air
and the skin. In addition, we think it is reasonable to assume
the errors of the CT scanner and the software are negligible.
In fact, BSA values in normal-weight subjects calculated in 3D
models from CT scans are very similar to those calculated with
other techniques. However, in the extremes cases (overweight
individuals), we find some fairly consistent trends suggesting
that the predictive formulae in the literature (including DuBois
& DuBois) may give erroneous results, a point of view that
has been repeatedly expressed in the literature. Thus, our
study strongly supports the need of modified formulae for
small and large BMI values.
Clinical impact of BSA calculations
The clinical importance of BSA estimations is obvious in
different areas of clinical medicine, such as standardization of
physiologic parameters like cardiac output and renal glomeru-
lar filtration rate, calculation of drug dosages and many other
areas including transplantation medicine, burn injuries and
critical care medicine.
Cardiac volumes, both cardiac output, stroke volume, and
end-diastolic and end-systolic chamber volumes, have been
normalized as the preferred parameter to body surface area
over several decades (Taylor & Tiede, 1952). Even left atrial
volume index has been shown and used as an important
prognosticator, for example in dialysis patients (Ozdogan
et al., 2010). A more recent interest has developed in sports
medicine for comparison of different types of training and
athletes regarding cardiac and left ventricular performance
assessed by normalized cardiac output and left ventricular vol-
umes (Erz et al., 2013). But obviously, the normalization may
be complicated by extreme BSA values in this population, as
recently discussed in a study on cardiac morbidity in obese
patients (Adler et al., 2013), where the authors conclude that
‘cardiac and stroke indices can be misleading relative to the
underlying raw values as a result of distortion by widely used
BSA formulae’. The same message is concluded by Adler et al.,
(2012) in their editorial about inappropriately indexed hemo-
dynamic measurements of body surface area extremes. In the
other end of the scale, that is in children, the same problems
have long been recognized, and they may get even worse in
obese children and adolescents (Ingul et al., 2010).
Accurate determination of renal function by measurement
of glomerular filtration rate (GFR) is important in several
clinical conditions such as optimal dosing of many drugs
including several cytostatic drugs, evaluation of renal disease
in children, determination of the need of dialysis in renal
insufficiency, etc. It is generally recommended to use a BSA
normalized plasma clearance measurement of a radionuclide
tracer (99mTc-labelled DTPA or 51Cr-EDTA) for accurate
determination (Fleming et al., 2004), but many attempts have
been carried out to replace the more cumbersome plasma
clearance measurement by determination of some plasma con-
centration for an estimated GFR (eGFR). Although less reliable
for a correct assessment of renal function, it has recently been
demonstrated that the clinical value of different eGFR formu-
lae is also significantly improved by normalization to BSA
(Mocroft et al., 2014). GFR normalized to BSA is furthermore
a strong predictor of development of cardiotoxicity of trastu-
zumab-based chemotherapy, independent of original cardiac
function (Russo et al., 2012). Again BSA has its shortcomings
in the extremes of the BSA curves, that is <1�6 m2 and
>2�0 m2, as recently shown (Redal-Baigorri et al., 2014). A
specific and unresolved normalization problem is related to
determination of children’s GFR, as discussed in several stud-
ies (e.g. reviewed by Filler et al., 2014).
The significance of BSA in cytostatic treatment is widely
accepted and repeatedly documented (e.g. Buzdar et al.,
2013), also for the introduction of new drugs or protocols
(e.g. Floquet et al., 2014). This has also been shown in
children (Camaione et al., 2013).
BSA is successfully applied in other areas as, for example
transplantation medicine, where both the donor and the
recipient BSA values were successfully included in the calcula-
tion of transplanted organ size (Fukazawa et al., 2013). In
anaesthesiology and critical care, medicine estimation of BSA
is frequently needed for determination of functions related to
body metabolism including ventilation, fluid requirements,
extracorporeal circulation and drug dosages (Current, 1998).
Also, for the treatment of burn injuries, BSA calculations
including the fraction of total burned surface areas are widely
used (Baryza et al., 2013).
Limitations
The sample used in our analysis was composed only of male
subjects of Caucasian origin. This means that the results
cannot be applied to women, to other ethnic groups, or to
children, without additional examinations. Indeed, Tikuisis
et al. (2001) found differences in BSA between sexes propos-
ing sex-based equations, and we found statistically, highly
significant differences with the formula developed from
Chinese population (Yu et al., 2003).
As in most other studies, we could include only few sub-
jects with high BMI. CT scanners, like MRI scanners, cannot
be used in many overweight and obese individuals, because
the typical 70 cm gantry diameter does not allow inclusion of
a total circumference of more than 58 cm, which is exceeded
in the majority of those individuals. Other techniques like a
laser scanner may be easier to use in subjects with a
BMI > 30.
If cadavers are subjected to decomposition processes, the
body surface could deviate from that of living subjects. We
carefully excluded subjects in whom putrefaction was
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al. 7
moderately advanced since that produces gas, which may
enlarge the abdomen and the scrotum. None of the cadavers
examined showed signs of putrefaction.
Finally, the surface of the hands was not determined in
each cadaver. Instead, we predicted the hand surface from the
determinations of ten subjects (as outlined in Material and
Methods). We found that the surface of two hands measured
close to 5% of the remaining body surface. Exactly, the same
percentage was reported by Tikuisis et al. (2001) and Yu et al.
(2010). In particular, the surface of the hands was accurately
measured by Yu et al. (2010) using an advanced laser scanner.
The maximum error due to this estimation of the surface of
the hands appears to be 1% of the total BSA, a small error
compared to the inaccuracy of a clinical BSA estimation based
on body height and weight.
In conclusion, we believe that our CT-based BSA calcula-
tions are more accurate than previous BSA determinations due
to the detailed information obtained of the body contour and
the well-documented software computation of the body sur-
face data. Nevertheless, we did not create a new formula, as
in agreement with several other groups, we found that the
widely employed DuBois and DuBois’ equation (1916) can
still be used quite accurately for the clinical determination of
BSA in normal-weight, Caucasian, male subjects. However,
our data suggest that BSA may be underestimated in under-
weight men and overestimated in overweight men. We do
not recommend the use of the modified formula developed
by Livingston & Lee (2001). New sex-specific formulae may
be needed, this demands further examinations in female pop-
ulation groups. New formulae should probably be developed
for overweight and obese subjects and for children.
Given the mechanical limitations of CT scanners in over-
weight subjects, surface laser scanning may be the best way to
generate new data in overweight subjects, although a signifi-
cant limitation of this method is related to the sometimes
large areas where fat deposits create closed spaces. Post-mor-
tem CT scanning may be an accurate technology to obtain sur-
face data in children and severely underweight adults and for
the examination of the influence of sex and different ethnics.
Acknowledgments
The authors would like to thank the Forensic Technicians at
the Section of Forensic Pathology (University of Copenhagen)
for helping with the data collection.
Conflict of interest
The authors have no conflict of interests.
References
Adler AC, Nathanson BH, Raghunathan K,
et al. Indexed hemodynamic measurementsmay be inappropriate at body surface
area extremes. Crit Care (2012); 16: 149.Adler AC, Nathanson BH, Raghunathan K,
et al. Effects of body surface area-indexedcalculations in the morbidly obese: a math-
ematical analysis. J Cardiothor Vasc An (2013);27: 1140–1144.
Baryza MJ, Hinson M, Conway J, et al. Five-year experience with burns from glass fire-
place doors in the pediatric population. JBurn Care Res (2013); 34: 607–611.
Boyd E. The Growth of the Surface Area of the HumanBody (1935). University of Minnesota Press,
MinneapolisBuzdar AU, Suman VJ, Meric-Bernstam F,
et al. Fluorouracil, epirubicin, andcyclophosphamide (FEC-75) followed by
paclitaxel plus trastuzumab versus paclitaxelplus trastuzumab followed by FEC-75 plus
trastuzumab as neoadjuvant treatment forpatients with HER2-positive breast cancer
(Z1041): a randomised, controlled, phase3 trial. Lancet Oncol (2013); 14: 1317–1325.
Camaione L, Elliott K, Mitchell-Van SA, et al.
Vancomycin dosing in children and youngadults: back to the drawing board. Pharma-
cotherapy (2013); 33: 1278–1287.
Current J. A linear equation for estimating the
body surface area in infants and children.Internet J Anesthesiol (1998); 2: 1–8.
Daniell N, Olds T, Tomkinson G. Technicalnote: Criterion validity of whole body sur-
face area equations: a comparison using 3Dlaser scanning. Am J Phys Anthropol (2012);
148: 148–155.DuBois D, DuBois EF. A formula to estimate
the approximate surface area if height andweight be known. Arch Intern Med (1916);
17: 863–871.Erz G, Mangold S, Franzen E, et al. Correla-
tion between ECG abnormalities and car-diac parameters in highly trained
asymptomatic male endurance athletes:evaluation using cardiac magnetic reso-
nance imaging. Int J Cardiovas Imag (2013);29: 325–334.
Filler G, Yasin A, Medeiros M. Methods ofassessing renal function. Pediatr Nephrol
(2014); 29: 183–192.Fleming JS, Zivanovic MA, Blake GM, et al.
Guidelines for the measurement ofglomerular filtration rate using plasma sam-
pling. Nucl Med Commun (2004); 25: 759–769.
Floquet A, Doussau A, Brouste V, et al.Pegylated liposomal doxorubicin and
cyclophosphamide in early recurrent ovar-
ian carcinoma: phase I dose-finding study.
Cancer Chemoth Pharm (2014); 73: 61–68.Fukazawa K, Yamada Y, Nishida S, et al.
Determination of the safe range of graft sizemismatch using body surface area index in
deceased liver transplantation. Transpl Int(2013); 26: 724–733.
Gehan EA, George SL. Estimation of humanbody surface area from height and weight.
Cancer Chemother Rep (1970); 54: 225–235.Geraghty EM, Boone JM. Determination of
height, weight, body mass index, and bodysurface area with a single abdominal CT
image. Radiology (2003); 228: 857–863.Haycock GB, Schwartz GJ, Wisotsky DH. Geo-
metric method for measuring body surfacearea: a height-weight formula validated in
infants, children, and adults. J Pediatr(1978); 93: 62–66.
Ingul CB, Tjonna AE, Stolen TO, et al. Im-paired cardiac function among obese ado-
lescents. Arch Pediat Adol Med (2010); 164:852–859.
Jones PR, Baker AJ, Hardy CJ, et al. Measure-ment of body surface area in children with
liver disease by a novel three-dimensionalbody scanning device. Eur J Appl Physiol
(1994); 68: 514–518.Livingston EH, Lee S. Body surface area pre-
diction in normal-weight and obese
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al.8
patients. Am J Physiol Endocrinol Metab (2001);
281: E586–E591.Martinez-M€oller A, Bundschuh R, Navab N,
et al. Determination of Body Surface Areafrom a whole-body CT scan and its impact
for SUV normalization. J Nucl Med Proc AnnMeeting Soc Nucl Med (2007); 48: 44.
Mocroft A, Ryom L, Reiss P, et al. A compar-ison of estimated glomerular filtration rates
using Cockcroft-Gault and the Chronic Kid-ney Disease Epidemiology Collaboration
estimating equations in HIV infection. HivMed (2014); 15: 144–152.
Mosteller RD. Simplified calculation of bodysurface area. N Engl J Med (1987); 317: 1098.
Ozdogan O, Kayikcioglu M, Asci G, et al. Leftatrial volume predicts mortality in low-risk
dialysis population on long-term low-saltdiet. Am Heart J (2010); 159: 1089–1094.
Redal-Baigorri B, Rasmussen K, Heaf JG. In-
dexing glomerular filtration rate to bodysurface area: clinical consequences. J Clin Lab
Anal (2014); 28: 83–90.Russo G, Cioffi G, Di LA, et al. Role of renal
function on the development of cardiotoxi-city associated with trastuzumab-based adju-
vant chemotherapy for early breast cancer.Intern Emerg Med (2012); 7: 439–446.
Sardinha LB, Silva AM, Minderico CS, et al. Ef-fect of body surface area calculations on
body fat estimates in non-obese and obesesubjects. Physiol Meas (2006); 27: 1197–1209.
Shuter B, Aslani A. Body surface area: Du Bois
and Du Bois revisited. Eur J Appl Physiol(2000); 82: 250–254.
Taylor HL, Tiede K. A comparison of the esti-mation of the basal cardiac output from a
linear formula and the cardiac index. J Clin
Invest (1952); 31: 209–216.Tikuisis P, Meunier P, Jubenville C. Human
body surface area: measurement and pre-diction using three dimensional body
scans. Eur J Appl Physiol (2001); 85: 264–271.
Verbraecken J, Van de Heyning P, De BackerW, et al. Body surface area in normal-
weight, overweight, and obese adults. Acomparison study. Metab, Clin Exp (2006);
55: 515–524.Yu C-Y, Lo Y-H, Chiou W-K. The 3D scanner
for measuring body surface area: a simpli-fied calculation in the Chinese adult. Appl
Ergon (2003); 34: 273–278.Yu CY, Lin CH, Yang YH. Human body sur-
face area database and estimation formula.Burns (2010); 36: 616–629.
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al. 9
Appendix
1Dem
ograph
icinform
ationof
the54
Caucasian,malecadavers
(sex,age,
nation
ality,
height,weigh
t,BM
IandBM
Igrou
p)andBSA(from
CTscansandusingpredictive
equation
s)of
each
subjectinclud
edin
thestud
y.
IDSex
Age
(years)Nationality
Height
(cm)
Weight
(kg)
BMI
(kgm
�2)
BMI
groups
Bodysurface
areacalculatedusing
CT
scans
DuBois
&DuBois
(1916)
Boyd
(1935)
Gehan&
George
(1970
)
Haycock
etal.
(1978
)
Shuter&
Aslani
(2000)
Livingston&
Lee
(2001)
Tikuisis
etal.
(2001)
Yuetal.
(2003)
Yuetal.
(2010)
1M
61Danish
165
4918
�0Und
erweigh
t1�5
531�5
221�5
041�5
051�4
891�4
971�4
531�5
181�4
321�5
332
M87
Danish
161
5320
�4Normal
1�566
1�546
1�543
1�551
1�538
1�525
1�528
1�549
1�471
1�554
3M
48Danish
176
4614
�9Und
erweigh
t1�5
701�5
531�5
061�4
971�4
771�5
181�3
951�5
351�4
331�5
684
M48
Danish
181
4714
�3Und
erweigh
t1�6
121�5
991�5
441�5
321�5
111�5
611�4
141�5
761�4
691�6
155
M39
Danish
174
5819
�2Normal
1�651
1�699
1�676
1�679
1�665
1�669
1�620
1�688
1�600
1�708
6M
49Spanish
162
5822
�1Normal
1�661
1�613
1�617
1�629
1�619
1�593
1�620
1�617
1�544
1�619
7M
59Danish
164
5420
�1Normal
1�664
1�579
1�572
1�578
1�565
1�556
1�547
1�579
1�499
1�588
8M
47Danish
170
5820
�1Normal
1�673
1�671
1�656
1�662
1�650
1�644
1�620
1�665
1�581
1�678
9M
41Danish
169
6021
�0Normal
1�678
1�688
1�679
1�687
1�677
1�662
1�656
1�684
1�604
1�694
10M
54Danish
179
6018
�7Normal
1�727
1�760
1�728
1�729
1�715
1�726
1�656
1�743
1�650
1�768
11M
66Danish
168
6422
�7Normal
1�728
1�727
1�727
1�740
1�732
1�704
1�727
1�726
1�651
1�731
12M
53Danish
167
6623
�7Normal
1�740
1�742
1�748
1�763
1�756
1�720
1�761
1�744
1�672
1�745
13M
73Danish
170
6422
�1Normal
1�743
1�742
1�737
1�749
1�740
1�717
1�727
1�739
1�661
1�747
14M
46Danish
177
6019
�2Normal
1�757
1�745
1�718
1�721
1�708
1�713
1�656
1�731
1�641
1�753
15M
74Danish
173
6722
�4Normal
1�769
1�799
1�792
1�804
1�796
1�772
1�778
1�793
1�715
1�802
16M
45Danish
165
7226
�4Overw
eigh
t1�7
701�7
921�8
121�8
351�8
321�7
731�8
631�7
991�7
361�7
9117
M51
Danish
164
6624
�5Normal
1�770
1�720
1�732
1�750
1�744
1�700
1�761
1�725
1�657
1�722
18M
48Danish
183
6419
�1Normal
1�780
1�838
1�802
1�804
1�791
1�802
1�727
1�817
1�723
1�845
19M
68Danish
173
5919
�7Normal
1�787
1�704
1�685
1�690
1�677
1�675
1�638
1�695
1�609
1�712
20M
62Danish
174
6722
�1Normal
1�802
1�807
1�797
1�808
1�800
1�779
1�778
1�799
1�719
1�810
21M
60Danish
170
6121
�1Normal
1�807
1�707
1�697
1�706
1�695
1�681
1�674
1�702
1�622
1�713
22M
27Polish
174
7123
�5Normal
1�809
1�852
1�848
1�863
1�857
1�825
1�846
1�845
1�770
1�853
23M
69Danish
170
6522
�5Normal
1�811
1�754
1�750
1�763
1�754
1�729
1�744
1�750
1�674
1�757
24M
54Danish
171
6923
�6Normal
1�832
1�806
1�807
1�822
1�816
1�782
1�813
1�803
1�730
1�808
25M
20Danish
178
6721
�1Normal
1�837
1�837
1�817
1�826
1�816
1�805
1�778
1�824
1�739
1� 841
26M
54Danish
171
7525
�6Overw
eigh
t1�8
551�8
711�8
811�9
021�8
991�8
481�9
131�8
711�8
031�8
7027
M45
Polish
182
6419
�3Normal
1�861
1�830
1�797
1�800
1�787
1�795
1�727
1�811
1�719
1�837
28M
55Danish
177
7122
�7Normal
1�864
1�875
1�864
1�876
1�869
1�845
1�846
1�864
1�785
1�877
29M
56Turkish
167
7426
�5Overw
eigh
t1�8
661�8
291�8
471�8
701�8
681�8
091�8
961�8
341�7
701�8
2830
M20
Danish
182
6820
�5Normal
1�868
1�878
1�851
1�857
1�847
1�844
1�796
1�860
1�772
1�883
31M
57Danish
178
6520
�5Normal
1�871
1�813
1�791
1�797
1�787
1�782
1�744
1�799
1�713
1�819
32M
84Danish
164
7829
�0Overw
eigh
t1�8
901�8
461�8
781�9
071�9
081�8
301�9
621�8
561�8
011�8
4233
M41
Danish
176
7724
�9Normal
1�905
1�933
1�933
1�952
1�948
1�906
1�946
1�926
1�854
1�931
34M
48Danish
180
7021
�6Normal
1�929
1�886
1�867
1�876
1�868
1�854
1�830
1�872
1�788
1�890
35M
35Danish
183
7622
�7Normal
1�948
1�977
1�959
1�971
1�965
1�944
1�929
1�960
1�878
1�978
36M
37Danish
174
7926
�1Overw
eigh
t1�9
631�9
381�9
461�9
681�9
661�9
131�9
781�9
341�8
671�9
3537
M44
Danish
175
8026
�1Overw
eigh
t1�9
771�9
561�9
641�9
861�9
841�9
311�9
951�9
521�8
841�9
53
(con
tinu
ed)
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al.10
Appendix
1(con
tinu
ed)
IDSex
Age
(years)Nationality
Height
(cm)
Weight
(kg)
BMI
(kgm
�2)
BMI
groups
Bodysurface
areacalculatedusing
CT
scans
DuBois
&
DuBois
(1916)
Boyd
(1935)
Gehan&
George
(1970
)
Haycock
etal.
(1978
)
Shuter&
Aslani
(2000)
Livingston&
Lee
(2001)
Tikuisis
etal.
(2001)
Yuetal.
(2003)
Yuetal.
(2010)
38M
48Danish
182
7221
�7Normal
1�979
1�924
1�903
1�912
1�904
1�891
1�863
1�908
1�823
1�927
39M
76Danish
180
8125
�0Overw
eigh
t1�9
832�0
072�0
032�0
222�0
201�9
772�0
111�9
961�9
232�0
0440
M36
Danish
179
8125
�3Overw
eigh
t1�9
861�9
991�9
982�0
182�0
161�9
702�0
111�9
891�9
181�9
9641
M64
Danish
178
9028
�4Overw
eigh
t1�9
972�0
822�0
962�1
252�1
282�0
562�1
522�0
762�0
162�0
7442
M51
American
181
8225
�0Overw
eigh
t2�0
042�0
262�0
212�0
402�0
381�9
952�0
272�0
131�9
402�0
2343
M57
Danish
174
8327
�4Overw
eigh
t2�0
251�9
791�9
932�0
192�0
191�9
552�0
431�9
771�9
141�9
7444
M34
Danish
192
7620
�6Normal
2�035
2�047
2�006
2�011
2�003
2�006
1�929
2�017
1�924
2�049
45M
45Danish
179
9228
�7Overw
eigh
t2�0
382�1
102�1
252�1
542�1
582�0
842�1
832�1
042�0
442�1
0146
M68
Danish
178
8526
�8Overw
eigh
t2�0
492�0
322�0
392�0
632�0
642�0
052�0
742�0
251�9
592�0
2747
M55
Danish
180
8626
�5Overw
eigh
t2�0
542�0
592�0
622�0
862�0
862�0
302�0
902�0
491�9
812�0
5348
M38
Danish
178
9830
�9Overw
eigh
t2�0
812�1
592�1
852�2
202�2
282�1
352�2
742�1
562�1
032�1
4749
M22
Danish
175
8327
�1Overw
eigh
t2�0
861�9
871�9
992�0
242�0
241�9
622�0
431�9
831�9
191�9
8250
M44
Danish
180
9228
�4Overw
eigh
t2�1
152�1
192�1
312�1
592�1
632�0
922�1
832�1
112�0
492�1
1051
M52
Danish
175
9129
�7Overw
eigh
t2�1
442�0
662�0
902�1
222�1
272�0
442�1
682�0
652�0
102�0
5752
M35
Icelandic
188
9627
�2Overw
eigh
t2�2
052�2
262�2
232�2
482�2
522�1
932�2
442�2
082�1
392�2
1753
M46
Danish
190
8924
�7Normal
2�207
2�172
2�154
2�172
2�171
2�136
2�137
2�149
2�071
2�167
54M
61Danish
197
102
26�3
Overw
eigh
t2�2
452�3
632�3
432�3
662�3
702�3
222�3
342�3
322�2
572�3
53
© 2015 Scandinavian Society of Clinical Physiology and Nuclear Medicine. Published by John Wiley & Sons Ltd
Body surface area from CT scans, C. Villa et al. 11