selulitis.pdf
Click here to load reader
-
Upload
dhisa-zainita-habsari -
Category
Documents
-
view
222 -
download
0
Transcript of selulitis.pdf

8/9/2019 selulitis.pdf
http://slidepdf.com/reader/full/selulitispdf 1/5
Correspondence: Emine Akçay, Mutlukoy Sitesi 1957. sk. No: 7, Umitköy, Ankara Turkey Email: [email protected]: 13 November 2013, Accepted: 31 December 2013
Copyright © Journal of Microbiology and Infec ous Diseases 2014, All rights reserved
Journal of Microbiology and Infectious Diseases / 2014; 4 (3): 123-127JMID doi: 10.5799/ahinjs.02.2014.03.0154
REVIEW ARTICLE
Preseptal and orbital cellulitis
Emine Akçay, Gamze Dereli Can, Nurullah Çağıl
Yıldırım Beyazıt Univ. Medical Faculty Atatürk Training and Research Hospital Dept. of Ophthalmology, Ankara, Turkey
ABSTRACT
Preseptal cellulitis (PC) is de ned as an in ammation of the eyelid and surrounding skin, whereas orbital cellulitis (OC)is an in ammation of the posterior septum of the eyelid a ecting the orbit and its contents. Periorbital tissues maybecome infected as a result of trauma (including insect bites) or primary bacteremia. Orbital cellulitis generally occursas a complication of sinusitis. The most commonly isolated organisms are Staphylococcus aureus , Streptococcus pneu-moniae , S. epidermidis , Haempphilus infuenzae , Moraxella catarrhalis and S. pyogenes. The method for the diagnosisof OS and PS is computed tomography. Using e ective antibiotics is a mainstay for the treatment of PC and OC. Thereis an agreement that surgical drainage should be performed in cases of complete ophthalmoplegia or signi cant visualimpairment or large abscesses formation.
This infections are also at a greater risk of acute visual loss, cavernous sinus thrombosis, meningitis, cerebritis, endo -phthalmitis, and brain abscess in children. Early diagnosis and appropriate treatment are crucial to control the infection.Diagnosis, treatment, management and complications of PC and OC are summarized in this manuscript. J MicrobiolInfect Dis 2014; 4(3): 123-127
Key words: infection, cellulitis, orbita, preseptal, diagnosis, treatment
Preseptal ve Orbital Sellülit
ÖZET
Preseptal selülit (PS) göz kapağı ve çevresindeki dokunun iltihabi reaksiyonu iken orbital selülit (OS) orbitayı ve onuniçeriğini etkileyen septum arkası dokuların iltihabıdır. Göz çevresi yapılar; travma (sıklıkla böcek ısırığı) veya primerbakteremiye bağlı olarak enfekte olur. Orbital selülit çoğunlukla sinüzite sekonder iltihabi olayın orbita içine ilerleme -siyle oluşur. Sıklıkla kültürlerden üretilen patojenler Staphylococcus aureus , Streptococcus pneumoniae , S. epidermidis ,Haempphilus infuenzae , Moraxella catarrhalis ve S. pyogenes ’dir. Tanıda OS ve PS’yi ayırt etmek için önerilen yöntembilgisayarlı tomogra k görüntülemedir. Uygun antibiyoterapi OS ve PS’de tedavinin ana basamağıdır. Cerrahi drenajtotal oftalmopleji, görsel kayıp veya büyük belirgin abse gelişiminde endikedir.
Bu enfeksiyonlar çocuklarda akut görme kaybı, kavernöz sinus trombozu, menenjit, serebrit, endoftalmi, beyin absesigibi komplikasyonlara neden olabilir. Bu nedenle bu enfeksiyonların erken tanınması ve doğru tedavi edilmesi oluşabi -lecek ciddi enfeksiyonların önlenmesi açısından çok önemlidir. Bu yazıda PS ve OS’nin tanı, tedavi, yönetim ve kompli -kasyonları özetlendi.
Anahtar kelimeler: Enfeksiyon, orbita, preseptal, selülit, tanı, tedavi
INTRODUCTION
Preseptal cellulitis (PC) and orbital cellulitis (OC)are serious infections of the adnexal tissues sur-rounding the eye. Although they can be seen at anyage, children are most commonly affected. 1,2 If nottreated appropriately, they can lead to sight-threat-ening complications such as acute visual loss andendophtalmitis and life-threatening complications,
such as the thrombosis of cavernous sinus, men-ingitis, cerebritis, and brain abscess. 3,4 Thereforecorrect diagnosis and early appropriate treatment isessential.
The purpose of this report is to discuss thepredisposing factors, clinical ndings, microbiologicdata, complications, and ef cacy of treatment in PCand OC in children.

8/9/2019 selulitis.pdf
http://slidepdf.com/reader/full/selulitispdf 2/5
Akçay E, et al. Preseptal and orbital cellulitis124
J Microbiol Infect Dis www.jmidonline.org Vol 4, No 3, September 2014
PATHOGENESIS AND CLASSIFICATION
Periorbital in ammation is classi ed according tothe severity and its location. The orbital septum di-vides two parts which the soft tissues of the eyelid
(preseptal space) from those of the orbit (postseptalspace) (Figure 1). PC is the infection of preseptalspace usually originates from trauma, or primarybacteremia. 5 In OC cases, the infection is localizedin the postseptal space and usually occurs as acomplication of sinusitis. Generally ethmoid sinususare predominating as the most common origin. 6 Al-though it is penetrated by the neural and vascularstructures, the orbital septum preserves enteringof the the infectious agents to the back of the or-bit. 7 The veins which drain the orbit, maxillary andethmoid sinuses and periorbital tissues create an
anastomotic network that lack a valve. Hence thevenous system allows the spread of infection fromone place to another leading to the cavernous si-nus involvement. The infection can spread from thetransition artery of the ethmoid and frontal bones. 6
Figure 1. Orbital septum is seen in the picture (arrow)(surgical photograph).
PRESEPTAL CELLULITIS
Preseptal cellulitis is an infection, which affects thetissue remaining in front of the orbital septum. It isseen more often than OC and generally is causedby bacteria. 8 There are two basic mechanisms inthe formation of PC. First one is spreading of a lo-cal infection to the eyelid. In this process sourceof infection is penetrating trauma around the eyesor an infection of the skin or subcutaneous tissue(acute dacryocystitis, hordeolum, infected chalazi-
on, severe conjunctivitis, impetigo, erysipelas). Theother reasons are eye surgery or insect bites. In thesecond mechanism it is originated from the focus ofinfection, which is far from orbit. General condition,co-morbidities of the patient as well as the anamne-
sis and physical examination are important clues todetermine the source of the infection. 4
EtiologyPreseptal cellulitis is generally seen in children es-pecially those that are 3-7 years old. 9 Bacteremiahas been reported in approximately 80% of childrendiagnosed with periorbital cellulitis. 10 H. infuenzae has been associated with preseptal cellulitis in chil-dren below the age of 4 years. In 1985 after theintroduction of H. infuenzae vaccine the microbio-logical spectrum of bacterial periorbital cellulitis haschanged. 10,11 Recent retrospective studies showedthe decreasing incidence of H. infuenzae in peri-orbital cellulitis. 12 Currently S. aureus and Strepto -
coccus species are the predominanting microor-ganisms as the cause of PC. 11 Among the etiologicagents causing preseptal cellulitis in children olderthan 4 years, S. aureus , S. epidermidis , S. pneu -
moniae , mixed anaerobic-aerobic bacterial oraseem to be the leading microorganisms. 13,14
Clinical fndings and diagnosisPreseptal cellulitis is clinically characterized by ery-thema, edema, and/or warmth of the periorbital tis-sues. High fever, fatigue and loss of appetite aredetermined especially in children. Clinical signs oforbital soft tissue involvement are not visible in PC. 5
Preseptal cellulitis diagnosis is made by clinicalexamination and it is the most valuable thing in thedifferential diagnosis of PC. 5 Various situations canmimic PC. Some of these are; OC, idiopathic orbitalin ammatory disease, thyroid orbitopathy, orbitaltrauma, allergic contact dermatitis, acute adnexalinfections, posterior scleritis, endophthalmitis, gran-
ulomatous vasculitic autoimmune diseases and tu-moral metastases. 6
In PC imaging with computed tomography (CT)is based on the clinical examination. If there is affer-ent pupillar defect, limitation of extraocular move-ments or pain exists, CT must be carried out. Also ifthe examination is dif cult, CT should be done. Axialand coronal sections of the orbit and sinuses shouldbe ne visualised for diagnosis. 1
TreatmentThe management of PC is mainly based on medicaltreatment, surgical approach is usually not neces-

8/9/2019 selulitis.pdf
http://slidepdf.com/reader/full/selulitispdf 3/5
Akçay E, et al. Preseptal and orbital cellulitis 125
J Microbiol Infect Dis www.jmidonline.org Vol 4, No 3, September 2014
sary. The children under 1 year of age should befollow up in the hospital. As the origin of the possibleinfection might be upper respiratory tract and si-nuses, initial empiric antibiotic therapy should coverthe ora there. If there is a focal trauma, treatment
should include S. aureus . Outpatient treatment withrst generation cephalosporin, amoxicillin-clavulan -
ic acid or ceftriaxone is suitable for mild cases ofolder children. If there is no response to the treat-ment in 48-72 hours, intravenous therapy must beapplied. In young children and severe cases, intra-venous treatment and close observation in hospitalis required. Using the second or third generationcephalosporins and penicillinase-resistant peni-cillins is important. If anaerobes plus S. aureus issuspected clindamycin + cephalosporin treatmentcan be an option. Chloramphenicol can be used inpatients allergic to penicillin. An additional one dayfollow up will be suitable after achieving clinical im-provement within 48-72 hours of antibiotic therapy.The total treatment must be completed 14 days withoral antibiotics. If the eyelid abscess is present,drainage of the abscess has to be done as well. 12
Complications
Meningitis is the most important complication of PCespecially in children who have H. in uenza celluli -tis secondary to bacteremia. 15
ORBITAL CELLULITIS
Orbital cellulitis is a serious infection of the posteriortissues to the orbital septum. Serious complicationssuch as intracranial abscess, meningitis, carotidartery occlusion, cavernous sinus thrombosis, andvisual loss can be observed. 16 It leads to a more se-vere infection than PC. The most common underly-ing factor for its development is a preceding ethmoidsinusitis and the microbiology of OC and abscesstends to re ect the underlying sinus involvement
and pathology.5
As the medial part of the orbit is verythin and due to its porous structure infections canextend easily to the neighborhood structures. 16 Fur-thermore, venuos system itself may one of the otherreason of the spreading of the infection as the lackof valve system of venos system in this reagion. 16
Also there are some exogenous and endogenouscauses of OC. Blunt or penetrating trauma of theorbita , the surgery of orbital and periorbital, struc-tures and dental procedures are some examples forexogenous causes. 16 Septisemi and endophtalmitisare the examples for endogenous causes of OC. 16
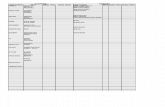
Chandler proposed a clinical classi cationwhich separates the orbital complications of acutesinusitis into 5 groups (Table 1). 17
Table 1. Orbital complications of acute sinusitis. Chandlerclassi cationGroups
Group 1: Preseptal cellulitis
Group 2: Orbital cellulitis
Group 3: Subperiosteal abscess
Group 4: Intraorbital abscess
Group 5: Cavernous sinus thrombosis
Etiology
Group A beta-hemolytic streptococci, S. aureus , S.
pneumoniae , H. infuenzae , M. catarrhalis , otherstreptococcal species, and anaerobic microorgan-isms are the micrororganisms which are respon-sible for OC in pediatric patients. 18,19 In the pre- H.
infuenzae type B. vaccine era, H. infuenzae typeB was the predominant organism isolated in chil-dren with positive blood cultures; it represented15% to 82% of all isolates depending on the patientpopulation. 20 Today, Streptococcus species are theleading microrganisms responsible for the OC. 20
Recent studies demonstrate that Staphylococcus and Streptococcus species are the most commonpathogens of the pediatric OC. In some populationmethicillin-resistant S. aureus is the increasing spe-cies responsible for pediatric OC. 21
Clinical fndings and diagnosis
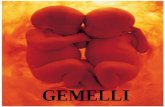
Cinical ndings of OC are pain, vision loss, restrict -ed motility, exophthalmus, proptosis and diplopia(Figure 2A). 12 Vision loss can be a seen as a compli-cation of involvement of optic nerve and retina dueto orbital compartment syndrome, vascular in ltra -tion, mass effect and optic neuritis. 18
Because of lack of orbital signs and symptomsin preseptal celulitis, this diagnosis can easily beexcluded. Mycotic OC, neoplasms thyroid eye dis-ease (Graves ophtalmopathy) and idiopathic orbitalin ammation should be considered in the differen -tial diagnosis of bacterial OC. Systemic autoim-mune congenital and traumatic disease can alsomimmic OC. 16
After clinical examination, complete bloodcount, blood cultures and computed tomography

8/9/2019 selulitis.pdf
http://slidepdf.com/reader/full/selulitispdf 4/5
Akçay E, et al. Preseptal and orbital cellulitis126
J Microbiol Infect Dis www.jmidonline.org Vol 4, No 3, September 2014
should be performed for clinical staging. Contrastagents should be used during CT imaging if it ispossible. Because it can increase the sensitivity andspesi ty of diagnosis of OC. Postseptal in amationmay be diffuse or localised in bacteriaal OC:. In ab-
scess formation localized involvement can be seenintra or extraconal region. Subperiostaeal abscessformation is an other complication which originatesbetween the bone and periorbita. CT images showslocalized in ammation in this abscess formation. 22
Treatment
The proper use of antibiotics is crucial in the treat-ment of PC and OC. Improvement can be achievedin clinical signs (Figure 2B). The general accep-tance of S. pneumoniae , S. aureus , other strep-tococci, and non-spore-forming anaerobes as the
main causative agents indicates the most appro-priate antibiotic regimen. 16 It is reasonable to useampicillin-sulbactam for the initial empiric therapy. 5 Other options may include nafcillin for Staphylo -
coccus or Streptococcus species . Clindamycin can
be used for S. pneumoniae , S. aureus , and anaer-obes, and cefotaxime for Gram negative organ-isms, nontypeable H. infuenzae , Moraxella, andresistant pneumococci. Most experts recommendthat children younger than 12–15 months with signsof systemic illness can be follow up in the hospitalfor parenteral therapy. In patients with OC, intrave-nous ampicillin-sulbactam therapy for initial 24–48hours seems reasonable, keeping in mind that thisregimen may require reevaluation. 23 Surgical drain-age followed by antibiotic therapy is mainstay in thepresence of subperiosteal or intraorbital abscess. 23
Figure 2. Ten years old patient with orbital cellulitis.A-The rst clinical examination. Edema, hyperemia and total ptosis seen in the left upper eyelid and periocular regionB- After medical treatment. Improved clinical ndings are seen in the picture
Complications
Systemic or local complications of OC were reportedin the literature. Ocular complications may includecorneal disease, retinitis, uveitis, exudative retinaldetachment, optic neuropathy, endophthalmitis, andglobe rupture. A motility defect, intracranial disease,cavernous sinus thrombosis, meningitis, sepsis,brain abscess are some of the catastrophic com-plications of OC which can lead to death. 3,4,8,16,19,22,25
CONCLUSION
Cellulitis of the orbital region in children, localized infront of the orbital septum, is a disease with a lowrisk of complications, provided that the patients aresubjected to proper medical treatment. However,the possibility of an extension of the in ammationin the retroseptal area makes multidisciplinary man-agement necessary in order to achieve cure and
minimize risk for an adverse visual defect. OC cancause serious ocular and neurological complica-tions. 26 Timely and appropriate use of imaging mo-dalities, antimicrobial therapy and surgery can leadto better outcomes. 27
REFERENCES
1. Handler LC, Davey IC, Hill JC, Lauryssen C. The acute orbit:differentiation of orbital cellulitis from subperiosteal abscessby computerized tomography. Neuroradiology 1991;33:15-18.
2. Schramm VL Jr, Curtin HD, Kennerdell JS. Evaluation oforbital cellulitis and results of treatment. Laryngoscope1982;92:732-738.
3. Krohel GB, Krauss HR, Winnick J. Orbital abscess presen-tation, diagnosis, therapy and sequelae. Ophthalmology1982;89:492-498.
4. Lessner A, Stern GA. Preseptal and orbital cellulitis. Infect DisClin North Am 1992;6:933-952.

8/9/2019 selulitis.pdf
http://slidepdf.com/reader/full/selulitispdf 5/5
Akçay E, et al. Preseptal and orbital cellulitis 127
J Microbiol Infect Dis www.jmidonline.org Vol 4, No 3, September 2014
5. Givner LB. Periorbital versus orbital cellulitis. Pediatr Infect DisJ 2002;21:1157-1158.
6. Wald ER. Periorbital and orbital infections. In: Long SS, Pick-ering LK, Prober CG, eds. Principles and Practice of Pediat-ric Infectious Diseases, 2nd ed. New York: Churchill Living-stone; 2003:508-513.
7. Coats DK, Carothers TS, Brady-McCreery K, Paysse EA. Ocu -lar Infectious Diseases. In: Feigin RD, Cherry JD, et al. eds.Textbook of Pediatric Infectious Diseases. 5th ed. Philadel-phia: WB Saunders Company; 2004;790-792.
8. Ambati BK, Ambati J, Azar N, et al. Periorbital and orbital cel-lulitis before and after the advent of Haemophilus in uenzatype B vaccination. Ophthalmol 1986;14:211-219.
9. Van Dissel JT, de Keizer RJW. Bacterial infections of the orbit.Orbit 1998;17:227-35.
10. Schwartz GR, Wright SW. Changing bacteriology of perior-bital cellulitis. Ann Emerg Med. 1996;28:617–620.
11. Donahue SP, Schwartz G. Preseptal and orbital cellulitis inchildhood. A changing microbiologic spectrum. Ophthalmol-ogy. 1998;105:1902–1905. discussion 1905-1906.
12. Botting AM, McIntosh D, Mahadevan M. Paediatric pre- andpost-septal peri-orbital infections are different diseases: Aretrospective review of 262 cases. Int J Pediatr Otorhinolar-yngol. 2008;72:377–383.
13. Rubinstein JB, Handler SD. Orbital and periorbital cellulitis inchildren. Head Nck Surg 1982;5:15-22.
14. Chaudhry IA, Shamsi FA, Elzaridi E, et al. Inpatient presep -tal cellulitis: experience from a tertiary eye care centre. Br JOphthalmol 2008 ;92:1337-1341.
15. Steinkuller PG, Jones DB. Preseptal and orbital cellulitis andorbital abscess. In:Linberg JV, Oculoplastic & Orbital Emer -gencies. Noorwalk: Appleton & Lange, 1990:51-66.
16. Jain A, Rubin PA. Orbital cellulitis in children. Int OphthalmolClin. 2001;41:71–86.
17. Chandler JR, Langenbrunner DJ, Stevens ER. The patho -genesis of orbital complications in acute sinusitis. Laryngo-scope. 1970;80:1414–1428.
18. Kloek CE, Rubin PA. Role of in ammation in orbital cellulitis.Int Ophthalmol Clin. 2006;46:57–68.
19. Nageswaran S, Woods C, Benjamin D, et al. Orbital cellulitisin children. Pediatr Infect Dis J. 2006;25:695–699.
20. Barone SR, Aiuto LT. Periorbital and orbital cellulitis in theHaemophilus in uenzae vaccine era. J Pediatr OphthalmolStrabismus 1997;34:293-296.
21. McKinley SH, Yen MT, Miller AM, Yen KG. Microbiology of pe-diatric orbital cellulitis. Am J Ophthalmol 2007;144:497-501.
22. Eustis HS, Mafee MF, Walton C, Mondonca J. MR imagingand CT of orbital infections and complications in acute rhino-sinusitis. Radiol Clin North Am. 1998;36:1165–1183.
23. Goldman RD, Dolansky G, Rogovic AL. Predictors for ad-mission of children with periorbital cellulitis presenting to
the pediatric emergency department. Pediatr Emerg Care2008;24:279-283.
24. Teele DW. Management of the child with red and swollen eye.Pediatr Infect Dis J 1983;2:258-262.
25. Primeggia J, Cyriac G, Kumar P. Invasive orbital aspergillosisin an apparently immunocompetent host without evidencesinusitis. J Microbiol Infect Dis 2012;2:113-116.
26. Georgakopoulos CD, Eliopoulou MI, Stasinos S, et al. Peri-orbital and orbital cellulitis: a 10-year review of hospitalizedchildren. Eur J Ophthalmol 2010;20:1066-1072.
27. Uy HS, Tuano PM. Preseptal and Orbital Cellulitis in a Devel-oping Country. Orbit 2007;26:33–37.