pleno14b
-
Upload
dewi-djasmi -
Category
Documents
-
view
111 -
download
1
Transcript of pleno14b

Planary Discussion3rd ScenarioMENGAPA ANAKKU TIDAK MAU LAHIR ?

• Ayu Sri Mega (0910311021)• Bikrulmal (0910313236)• Dewi Oktavia Djasmi (0910313188)• Fajar Normansyah (0910313205)• Fitrah Umi Muytasya (0910313201)• Nining Kurniawati (0910312066)• Nidya Purwadianti (0910311021)• Pratiwi Dian Pramana (0910312111)
GROUP 14 B

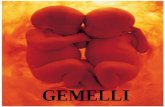
MODUL 3PERSALINAN DAN NIFAS PATOLOGISMENGAPA ANAKKU TIDAK MAU LAHIR ?
Ny. Distosiana (37 tahun) hamil anak pertama cukup bulan, diantar oleh Bidan ke Puskesmas Suliki dengan rujukan: partus tidak maju-maju setelah dipimpin Bidan mengedan selama 2 jam. Dari pemeriksaan dokter didapatkan fundus uteri 3 jari bawah prosessus xipoideus, tinggi fundus uteri 35 cm, pada pemeriksaan Leopold: janin letak kepala, His: 2-3x/50”/kuat, BJA 13-12-13, VT: Pembukaan lengkap, ketuban (-), sisa kehijauan, ubun-ubun kecil depan Hodge III-IV. Dokter memberikan antibiotik untuk mencegah infeksi, selanjutnya dokter merujuk pasien ke Rumah Sakit dengan diagnosis distosia kala II. Di rumah sakit, persalinan di terminasi dengan forsep ekstraksi. Bayi lahir dengan berat badan 3500 gram, panjang badan 50 cm, skor APGAR 7/8. Dokter melakukan manual plasenta dan repair ruptura perinei. Satu jam kemudian terjadi atonia uteri, dilakukan masase uterus dan diberikan oksitosin dan ampisilin.Pada hari ke dua post partum, pasien sering menangis yang tidak jelas sebabnya dan, pasien tidak mau menyusui bayinya.
Bagaimana anda menjelaskan yang terjadi pada Ny.Distosiana?

• Dystocia (antonym eutocia) is an abnormal or difficult childbirth or labour
• Forceps is an instrument that resembles a pair of tongs and can be used in surgery for grabbing, maneuvering, or removing various things within or from the body.
• Manual placenta removal is a procedure to remove a retained placenta from the uterus after childbirth.
Terminology

• Uterine atonic bleeding is massive bleeding during puerperium (the period from the end of the last stage of labor and the return of the uterus to its normal size after delivery: about 3-6 weeks in duration), and happens because of uterine contraction failure immediately after the placenta is delivered.
• Ampicillin is a beta-lactam antibiotic that has been used extensively to treat bacterial infections and also demonstrated activity against Gram-negative and positive organisms

• Uterine massage is an action used after the delivery of the placenta in which the provider or the woman places one hand on the fundus of the uterus through the woman's abdomen to rub or knead the uterus until it is firm. Sometimes blood and clots are expelled during uterine massage.
• Perineal repair is one of the most common surgical procedures performed when the perineum is torn naturally or cut during an episiotomy after a vaginal birth . Repair often involves the sewing together of torn or cut tissues to allow proper healing. In some rare instances, a perineal tear my occur during sexual activity.

• Oxytocin is a relatively short polypeptide hormone composed of nine amino acids. It is produced primarily in the hypothalamus and acts as a neurotransmitter in the brain. Physicians also sometimes administer the hormone intravenously to induce labor or strengthen contraction and to promote contraction of the uterus, thus helping to prevent hemorrhaging. During childbirth, oxytocin may even cause the involuntary ejection of milk, a reflex known as Ferguson's reflex.

1. why partus didnt show any improvement after being lead by the nurse for 2 hours?
2. what is the relationship between the mother's age and her first time pregnancy with partus hardship?
3. what is the interpretation from doctor's diagnosis?
4. why there is a feeling of defecating during partus?
5. why the doctor decided to terminate the process by extracting forceps?
Define Problem

7. why the placenta is being done manually and how is it done?what is the doctor's purpose giving the ampicillin and the oxytocin?
8. why did Mrs. distosiana cry in the 2nd day after the post partum?
9. why did the doctor repair the ruptura perinei and how is it being done?
10.what are the risk factors from atonia uteri?11.what are the consequence of forceps
extraction for the mother and the baby? 12.what is the interpretation after the labor?

1. Mrs. Distosiana suffered from dystocia. it is the condition of the old partus which is showed by 3 breakdowns :• Power (His) : atonia uteri, stiff uterus etc• Passage : a breakdown on the birth canal
such as tumor etc.• Passanger : abnormality from the baby's
position and shape2. age more than 35 years old weaken
the uterus. Nullipara affects the thick and stiff uterus' wall which end as dystocia.
Brainstorming

3. Interpretation: • fundus uteri is 3 fingers down from prosessus
xipoideus : normal • fundus' height is 35cm : matched with the gestation's
age• Leopold's inspection : the position of the baby's head :
normal• His: 2-3 times/50"/strong : His happen 2-3 times in 10
minutes for 50 seconds with strong contraction (Normal His: kala I)
• BJA 13-12-13 : Normal• VT : Complete opening : normal• the fetal membrane (-) : amnio membrane is not found• residual greenness : there is a possibility of meconium• small hair on Hodge III-IV : In PAP zone

4. Straining reflex caused by stimulation of the pressure of the bottom of the fetus (the normal delivery of the head) that suppress the anus and rectum. Additional power to push from the mother, with a contraction of the abdominal wall muscles and diaphragm, trying to extract the baby.
5. For the weak state of the mother after 2 hours of having obstructed labor that does not change, and the discovery of amniotic membrane that is not accompanied by the rest of the greenery which is an indication of the meconium which is feared will be the aspiration meconium resulting in fetal distress. Indications of the forceps is a state of fetal distress. In addition, there are indications Pinard, namely the head already in H-IV, a complete opening of the cervix, membranes have ruptured or 2 hours straining still unborn fetus.

6. Indications of manual removal of placenta is on the state of bleeding in the third stage of labor less than 400 cc that can not be stopped by uterotonic and massage, retensio placenta after 30 minutes the child was born, after a difficult childbirth, such as artificial high forceps, version extraction, perforation, and needed for the exploration of the birth canal and the umbilical cord cut.How:- stretch the umbilical cord with your fingers to form a cone- The tip of a finger through the umbilical cord, the left hand placed on the fundus- With a hand motion like water eroding, the placenta can be removed entirely (if possible), while the outside remains hand held fundus uteri participate lest pushed upwards

7. The purpose of ampicillin: to prevent infectionThe aim of oxytocin: to stimulate the uterus to contract so that bleeding can be stopped.
8. Mrs. Distosiana experienced maternity blues (postpartum blues) is caused by different predisposing factors, one of which is the rapid hormonal changes, especially progesterone levels dropped dramatically.
9. Perinei Ruptura is an effect of prolonged labor and wearing appliance assist labor like forseps. The object of repairing : to sew again natural muscle which ruptured and to prevent furthermore complication. Its way depended of its degree and will be studied in LO.

10.Many factors can contribute to the loss of uterine muscle tone, including:• overdistention of the uterus• ages• multiple gestations• Polyhydramnios• fetal macrosomia• prolonged labor• oxytocin augmentation of labor• grand multiparity (having given birth 5 or
more times)• Chorioamnionitis• halogenated anesthetics• uterine leiomyomata

11.Complications/dangers• Maternal-
• Injury-.• Extension of the episiotomy involving anus &
rectum or vaginal vault.• Vaginal lacerations and cervical tear if cervix
was not fully dilated.• Post partum haemorrhage –.
• Due to trauma, Atonic uterus or Anaesthetisia.• Shock –.
• Due to blood loss, dehydration or prolonged labour.
• Sepsis –.• Due to improper asepsis or devitalisation of
local tissues.

• Fetal-• Asphyxia.• Trauma-
•Intracranial haemorrhage.•Cephalic haematoma.•Facial / Brachial palsy.•Injury to the soft tissues of face & forehead.•Skull fracture
• Remote-cerebral palsy.• Foetal death-around 2%.

12.Interpretation of the newborn:o Infants born weighing 3500 grams (normal)o The body length of 50 cm (normal)o Apgar score of 7 / 8 (mild asphyxia)

Scheme

1. Labor and postpartum complications
2. Psychology Disorder During Pregnancy
3. Prolonged labor4. Perineal rupture and retained
placenta5. HPP and uterine atony6. Reference cases
Learning objective

I. Labor and postpartum complications
• A. Patologi persalinan* dystocia
1. his or power abnormalities2.abnormalities of location,
presentation and fetal position.3. pelvic disorder

* abnormalities of kala lll- which cause postpartum bleeding
uterine atony, injury of the birth canal, the release of some of the placenta in the uterus.
* injury and other events in labor- injury of vulva- injury of perineum- injury of vagina

2. Puerperal pathology* puerperal infectioninflammation caused by the entry of germs into the genital organ in time and parturition.
-bacteriology→ the organism that attacks the
former implantation or laceration due to childbirth.

causes :a. Streptococcus haemolyticus
aerobicusb. Sthaphyllococcus aureusc. Escheria colid. Clostridium welchi
*disorders and other diseases in childbed- abnormalities in the breast
a. Engorgement of the breast

→ the breast so hot and breast feels hard, the palpability ache. Body temperature does not rise.
b. Mastitis→ infection and inflammation of the breast,
especially in primipara. Infection occurs through wounds on the nipple, but also throught blood circulation.

II. Psychology Disorder During Pregnancy
• Psychiatric disorders are common in pregnant and postpartum women yet they often go undiagnosed and untreated.
• Approximately one-quarter of pregnant and postpartum women may have a psychiatric disorder.
• But the majority of these patients do not receive adequate treatment as part of their obstetric care.

Antenatal depression: 9–23% of pregnant women.
• Onset: •Before conception or during pregnancy•May progress to postpartum depression.
• Possible Features: •depressed mood or anhedonia lasting at
least 2 weeks•Loss of interest and pleasure, •sleep disturbance•appetite change•guilt•decreased concentration•suicidal ideation

• Management•For mild to moderate: counseling or
bright light therapy.•For depression with significant role
impairment, add treatment with antidepressant
Postpartum blues: 50–70% of postpartum women.
• Onset:•Peaks 3–5 days after delivery•Resolves <2 weeks

• Possible Features:•Crying spells•emotional lability•Irritability•Anxiety•Hypochrondriasis
• Management:•Reassure and educate•Encourage family to offer emotional and
social support.

Postpartum depression: 12–16% of postpartum women.
• Onset:• Within 6 months of delivery
• Possible features:• Classic depression symptoms lasting at least 2
weeks (same as antenatal depression above)• May also include intrusive thoughts or fears of
harming infant.• Management
• For mild to moderate: counseling or bright light therapy
• For depression with significant role impairment, add treatment with antidepressant
• Hospitalization when warranted.

Postpartum psychosis: 0.5% of postpartum women.• Onset:
• Within 3 weeks of childbirth• Women with bipolar disorder are at high risk.
• Possible features:• Delusions• Confusion• Hallucinations• Agitation• Insomnia• Disorganized thinking
• Management• Emergency referral to psychiatrist• Medical workup to rule out underlying etiology.

III. Prolonged laborDystocia Due To Abnormal Energy Inertia Uterine : his character is normal in
mean fundus contraction is stronger and early than other part. The abnormalities is located in uterus contraction which weaker, shorter, and rarely.
primary inertia uterine : occurs in the beginning of latent phase. From the outset there has been inadequate his so it’s often difficult to ensure.
secondary inertia uterine : arise after strong his progress for a long time. Occurs in the active phase of stage two and three.

His too strong : cause labor is complete in a short time under 3 hours, its named partus presipitatus. Short time labor can cause extensive injury in the birth canal, especially cervix, vagina, and perineum. In infant can lead to intracranial bleeding because this part put under pressure in a short time.

Incoordinate uterine action : his character is change. Increase uterine muscle tone and the contraction did not take place as usual because there is nosynchronization between its parts so his was not efficient in organizing the opening of the cervix. Beside that, because the increase uterine muscle tone causing pain is harder and longer for the mother and hypoxia in infant.


Problems with maternal soft tissue• A full bladder may impede the progress of labor,
as can myomata uteri, cervical edema, scar tissue, and congenital anomalies.
• Emptying the bladder may allow labor to continue; the other conditions may necessitate caesarean birth.
Dysfunctional uterine contractions• Contraction may be too weak, too short, too far
apart, ineffectual• Classification• A.) Primary: inefficient pattern present from
beginning of labor; usually prolonged latent phase.
• B.) Secondary: efficient pattern that changes to efficient or stops; may occur in any stage.

Assessment findings:• Progress of labor is slower than expected rate of dilatation,
effacement, descent for specific client.• Length of labor prolonged; prolonged latent phase (>20 hrs
in nullipara pt. or >4 h in a multipara pt), protacted active phase dilatation np. <1-2cm, mp <1.5cm; protacted descengt <1 cm per hr change in station in the nullipara pt. or <2 cm per hour in the mp pt.
• Maternal exhaustion/ distress• Fetal distress• Arrest of descent: no progress in fetal station greater than 1
hourintervention:• Individual as to cause• Provide comfort measures for client • Provide client, supportive descriptions of all actions taken• Administer analgesia if ordered• Monitor mother/ fetus continuously


Ineffective uterine
contraction or power
Maternal position and
during labor and birth
Previous psychological
response to past experience of
labor and delivery
Alteration of fetal size, position,
presentation, and number of fetuses.
Alteration in pelvic
structure
Insufficient contractions are producedCompromised
efforts due to analgesia
Occurrence of extended and painful labor
This interacts with the labor progress
Complications to the fetus:Neonatal asphyxiaFetal injuries and fracturesFetal distressComplications to the mother:Vaginal lacerationInfectionMaternal exhaustionPost partum hemorrhage
Maternal vaginal
laceration
Vaginal hemorrhage:
decrease blood volume
Acute pain
Poor dilatation and effacement of
the cervix
Poor descent of the fetus

Signs/ symptoms:
• Pain• Increase heart rate, pulse, body temp. • Increased BP• Diaphoresis• Body weakness• Exhausted appearance• SOB• Nasal flaring• Anxiety• Restlessness• Vaginal hemorrhage

Medical Management:• Treatment for contraction abnormalities involves
stimulation of labor through the use of oxytocin. An intrauterine pressure catheter may be used.
• Management for maternal passageway or fetal passage problems involves delivery in the safest manner for the mother and fetus.
• If the problem is related to the inlet or midpelvis, a CS delivery is indicated.
• If the size of the outlet is the problem, a forceps or vacuum extraction maybe perform.
Surgical Management:• Caesarean in necessary for delivery of the fetus

• Acute pain related difficulty in labor.• Promoting comfort:• Relaxation technique such as breathing techniques during labor• Changing position• Support person• Pain medications
• Anxiety related to threat of change in health status of self and fetus.
• Decreasing anxiety:• Give brief explanation to the women about the nature of contraction
associated with induce labor• Provide anticipatory guidance regarding use of meds, procedures
and equipment.• Prepare for caesarean if necessary
• Powerlessness• Provide rest period• Relaxation technique• Support person
Diagnosa

• Deficient knowledge related to measures that can be used to enhance labor and facilitate birth.
• Teach proper breathing techniques used during labor• Educate about the complication of the delivery• Explain client that caesarean is necessary due to
difficult labor.
• Ineffective individual coping related to inadequate support system.
• Support mechanism:• Stay with the patient during labor process• Encourage patient to discuss about her condition

IV. Perineal rupture and retained placenta
Perineal rupture is a obstetric tear that occurs in the perineum as a result of the inability of the pelvic muscles and soft tissues to accommodate the birth of a fetus.
Classification Ruptured Perineum 1) Spontaneous Ruptured Perineum That is the perineal wound that occurs because certain causes without tearing or deliberate action. These injuries occur during delivery and usually irregular.
2) Rupture of deliberate perineum (episiotomy) Perineal wound that is occurring because of cutting or tearing the perineum: episiotomy is an incision made in the perineum to enlarge the vaginal outlet

Perineal tear level can be divided into 4 levels:1. Level I Tear only occurs in vaginal mucous
membrane or skin of the perineum slightly. 2. Level II tear not only on the vaginal mucosa
but also on the bulbocavernosus muscle (muscle that forms the perineal body).
3. Level III Tear that occurs on the entire perineum until the sphincter ani muscles ( sphincter ani complex : external and internal)
4. Level IV Tear of the perineum until sphincter ani muscle and rectal mucosa

Causes of Occurrence of Perineal Rupture
Childbirth often causes injury to the birth canal. Injury on the birth occurred in: Basic pelvis / perineum, vulva and vagina, cervix uteri, and uterus. Whereas spontaneous rupture of the perineum caused by:
• Perineum rigid• Too fast fetal head through the pelvic floor• Big baby• Width perineum• Parity.

Diagnosis
1. Routine Inspection Almost all clinicians examining the perineum and periurethral after the delivery process to detect a tear that could arise. After all the deliveries, followed by routine rectal examination and inspection of the vaginal wall and cervix. Routine rectal examination aims to detect defects in rectal mucosa, rectal sphincter, and perineum by inserting one finger into the rectum. (-).

2. Peri-rule Is a standard tool to assess perineal rupture in level II objectively , made of plastic scale.
3. Endo Anal Ultrasound Is a radiological tool to use waves that are invasive and expensive and required special expertise. Endo anal ultrasound because ultrasound is sometimes overdiagnosis (+) but clinically

• Retained Placenta• Failure of placental delivery within 30
minutes after delivery of the foetus.• After delivery of the baby, the placenta
normally detaches from the inside of the uterus and is expelled, often with additional pushing efforts by the mother.
• Normally this occurs within a few minutes of delivery of the baby, but may take longer time

Causes• Retained separated placenta due to:
• Atony of the uterus: due to causes mentioned before.
• Constriction ring. • Rupture uterus: where the placenta
passes to the peritoneal cavity.• Retained non-separated placenta due to:
• Atony of the uterus.• Abnormal adherence of the placenta
which may be:

Causes
• Simple adhesion: Manual separation can be done easily.
• Morbid adhesion• Placenta accreta: There is deficient or absent
decidua basalis so that chorionic villi penetrate the superficial layer of the myometrium either partially (partial placenta accreta) or completely (complete placenta accreta).
• Placenta increta: The chorionic villi penetrate deeply in the myometrium.
• Placenta percreta: Penetration up to the peritoneal coat.

Clinical Manifestation
• Bleeding: occurs only if the placenta is separated partially or completely.
• Uterus: is lax in case of atony.• Vaginal examination may reveal:
• Constriction ring. • Rupture uterus.• Morbid placental adherence where there is
no plane of cleavage

Management• Uterine atony Massage with gentle cord traction if failed do,• Constriction ring
Deep anaesthesia and amyl nitrite inhalation are given before manual separation of the placenta
• Manual Removal of The PlacentaThe procedure is done under general anaesthesia.The right hand is introduced along the umbilical cord into the uterus.The lower edge of the placenta is identified and by a sawing movement from side to side the placenta is separated from its bed.

Management
Grasp the placenta and deliver it out.Examine the placenta and membranes for completeness.The left hand is supporting the uterus abdominally throughout the procedure

Complication
• Shock. • Postpartum haemorrhage. • Puerperal sepsis. • Subinvolution.• Retained parts with subsequent
haemorrhage, infection, placental polyp formation or choriocarcinoma.
• Complications of the methods used for its separation.

V. Hemorrhagic Post Partum anduterine atony
• HPP is bleeding more than 500ml in after pervaginam delivery or more than 1000ml after perabdominan delivery.
• Etiology :• Tone : atonia uteri• Trauma : the birth canal injury• Tissue : retensio placenta / retained
placenta• Thrombosis : Blood clotting disorders


Uterine Atony is abnormally large, roomy, flabby and without contraction directly after birth.Causes:
• Uterine inertia (primary and secondary)• Over-thinning of the uterus (twins, hydropsy)• Rupture of the uterus or cervix• Hypocalcemia
Clinical findings:• In rectal examination, the uterus found descended in the abdominal cavity, the uterus lack any contraction and filled with lochia• The cervix is dilated with small amount of lochia discharged from the vulva.• Secondary retention of placenta

“Tone: Think of Uterine Atony”
• Uterine atony causes 70% of hemorrhage• Assess and treat with uterine massage• Use medication early• Consider prophylactic medication...
Bimanual Uterine Exam• Confirms diagnosis of uterine atony.• Massage is often adequate for stimulating
uterine involution.

Medications for Uterine Atony
• 1. Oxytocin promotes rhythmic contractions.• Give IM or IU, not IV. (Can cause BP)• 40U/L at 250cc/h.• 2. Methergine 0.2mg (1 amp) IM• 3. Hemabate 0.25mg IM q 15min (max X8).

Medications: Methergine
• Causes tetanic uterine contraction.• May trap placenta.• Can cause Hypertension, especially IV.• Contraindicated in hypertensive patients and
those with pre-eclampsia.• Some authors skip Methergine altogether.

Prostaglandin F2 15-methyl
• Hemabate 0.25mg IM or IU.• Used to be called Prostin.• Controls hemorrhage in 86% when used
alone, and 95% in combination with above.
• Can repeat up to eight times.• Contraindicated in active systemic
diseases.• Can cause nausea/vomiting/diarrhea,
BP.

VI. Reference caseComplications of labor and factors impeding vaginal delivery such as:• prolonged labor or a failure to progress
(dystocia)• fetal distress• cord prolapse• uterine rupture• increased blood pressure (hypertension) in
the mother or baby after amniotic rupture• increased heart rate (tachycardia) in the
mother or baby after amniotic rupture

• placental problems (placenta praevia, placental abruption or placenta accreta)
• abnormal presentation (breech or transverse positions)
• overly large baby (macrosomia)• umbilical cord abnormalities (vasa
previa, multi-lobate including bi-lobate and succenturiate-lobed placentas, velamentous insertion)
• contracted pelvis

Other complications of pregnancy, preexisting conditions and concomitant disease such as• pre-eclampsia• hypertension [19]• multiple births• precious (High Risk) Fetus• HIV infection of the mother• Sexually transmitted infections such as
genital herpes (which can be passed on to the baby if the baby is born vaginally, but can usually be treated in with medication and do
• Bi-corniute uterus

Other• Lack of Obstetric Skill (Obstetricians
not being skilled in performing breech births, multiple births, etc. [In most situations women can birth under these circumstances naturally. However, obstetricians are not always trained in proper procedures])

THANK YOU!!