PENZUMIKAN
-
Upload
timotius-wira-yudha -
Category
Documents
-
view
27 -
download
10
description
Transcript of PENZUMIKAN
1
SKENARIO
Zumi, bayi laki-laki usia 9 bulan, dibawa ibunya ke dokter dengan keluhan batuk dan sukar
bernafas disertai demam, sejak dua hari yang lalu dan hari ini keluhannya bertambah berat.
Pemeriksaan Fisik
Keadaan umum: Tampak sakit berat, kesadaran kompos mentis.
RR 68*/menit, nadi 132*/menit – regulair, suhu 38,60C
Panjang badan 72cm, berat badan 8,5kg
Keadaan spesifik:
1. Kepala napas cuping hidung (+)
2. Thorax (paru) Inspeksi symmetris, retraksi intercostal, supraclavicula
Palpasi stem fremitus kiri = kanan
Perkussi redup pada basal kedua lapangan paru
Auskultasi peningkatan suara napas vesiculair, rhonchi basal harus nyaring,
tidak terdengar wheezing.
Pemeriksaan lain dalam batas normal.
Informasi tambahan: Tidak ada riwayat atopie dalam keluarga.
Pemeriksaan Laboratorium
1. Hb 11,9gr/Dl
2. Ht 34 vol%
3. WBC 18k/mm3
4. ESR 18mm/jam
5. PLT 220k/mm3
6. Diff count 0/2/1/75/20/2 STTR
7. CRP (-)
Pemeriksaan Radiologi
Thorax AP: infiltrat di perihilar kedua paru.
2
KLARIFIKASI ISTILAH
1. Batuk
2. Sukar bernafas
3. Tampak sakit berat
4. Napas cuping hidung
5. Retraksi intercostal Dorland 938: Gerakan menarik kembali atau keadaan tertarik
kembali.
6. Stem fremitus
7. Suara nafas vesiculair
8. Rhonchi basah halus nyaring
9. Wheezing Suara bersiul yang dibuat dalam bernafas, bunyi kontinu
seperti bersiul.
10. Atopie Predisposisi genetik untuk membentukr reaksi hyper-
sensitivitas terhadap antigen lingkungan umum (allergi atopik). Paling sering bermanifes-tasi
sebagai rhinitis allergika.
11. CRP
12. Infiltrat Diffusi atau penimbunan pathologik substansi di suatu
jaringan yang normalnya tidak terdapat pada jaringan tersebut atau dalam jumlah yang melebihi
normal.
IDENTIFIKASI MASALAH
1. Anamnesis
2. Pemeriksaan Fisik Umum
3. Pemeriksaan Fisik Spesifik
4. Pemeriksaan Laboratorium
5. Pemeriksaan Radiologi
6. Masalah Templat
3
ANALYSIS MASALAH
1. Zumi, ...
a. Preliminary
i. Anatomi (WAJIB)
ii. Histologi (WAJIB)
iii. Fisiologi (WAJIB)
b. Aetiologi
i. Batuk
ii. Sukar bernapas
iii. Demam
c. Mengapa keluhan Mr. Zumi bertambah berat?
d. Apa faktor usia berhubungan dengan keluhan yang dialami?
e. Bagaimana pertumbuhan dan perkembangan bayi pada kasus ini?
Sudah bisa mengucapkan M, B, P, ...
f. Bagaimana nutrisi pada bayi umur 9 bulan?
2. Pemeriksaan Fisik
a. Interpretasi dan mekanisme abnormal
i. Keadaan Umum dan Vital Sign (value untuk bayi)
ii. Panjang Badan, Berat Badan, BMI
b. Jenis-jenis suara nafas vesiculair
c. Apa saja immunisasi yang seharusnya sudah didapatkan oleh Zumi pada usia 9 bulan?
3. Keadaan spesifik
a. Interpretasi dan mekanisme abnormal
4. Pemeriksaan Laboratorium
a. Interpretasi dan mekanisme abnormal (value untuk bayi)
5. Pemeriksaan Radiologi
a. Interpretasi dan mekanisme abnormal, DISERTAI GAMBAR?
6. Masalah Templat
a. Clinical Diagnosis (Bronchopneumonie?)
b. Differential Diagnosis
c. Working Diagnosis
d. Definisi (WAJIB)
e. Aetiologi
f. Epidemiologi
g. Manifestasi Klinik
h. Patofisiologi (WAJIB)
i. Prevention
j. Tatalaksana
i. Farmakologik (WAJIB)
ii. Non-farmakologik
k. Komplikasi
l. Prognosis
m. Follow-up dan Monitoring
n. Edukasi
4
JAWABAN ANALYSIS MASALAH
1. Zumi, ...
a. Preliminary
i. Anatomi (WAJIB)
source: http://www.leeds.ac.uk/chb/lectures/anatomy7.html
Introductory Anatomy: Respiratory System
Dr D.R.Johnson, Centre for Human Biology
The word respiration describes two processes.
Internal or cellular respiration is the process by which glucose or other small
molecules are oxidised to produce energy: this requires oxygen and generates
carbon dioxide.
External respiration (breathing) involves simply the stage of taking oxygen
from the air and returning carbon dioxide to it.
The respiratory tract, where external respiration occurs, starts at the nose and
mouth. (Description of respiratory tract from nose to trachea here from
overheads) (There is a brief complication where the airstream crosses the path
taken by food and drink in the pharynx: air flows on down the trachea where
food normally passes down the oesophagus to the stomach. )
The trachea (windpipe) extends from the neck into the thorax, where it divides
into right and left main bronchi, which enter the right and left lungs, breaking up
as they do so into smaller bronchi and bronchioles and ending in small air sacs or
alveoli, where gaseous exchange occurs.
The lungs are divided first into right and left, the left being smaller to
accommodate the heart, then into lobes (three on the right, two on the left)
supplied by lobar bronchi.
Bronchi, pulmonary arteries and veins (which supply deoxygenated blood and
remove oxygenated blood), bronchial arteries and veins (which supply
oxygenated blood to the substance of the lung itself) and lymphatics all enter and
leave the lung by its root (or hilum). Lymph nodes blackened by soot particles
can often be seen here and the substance of the lung itself may be blackened by
soot in city dwellers or heavy smokers.
Each lobe of the lung is further divided into a pyramidal bronchopulmonary
segments. Bronchopulmonary segments have the apex of the pyramid in the
hilum whence they receive a tertiary bronchus, and appropriate blood vessels.
The 10 segments of the right lung and eight of the left are virtually self contained
units not in communication with other parts of the lung. This is of obvious use in
surgery when appropriate knowledge will allow a practically bloodless excision
of a diseased segment.
Gaseous exchange relies on simple diffusion. In order to provide sufficient
oxygen and to get rid of sufficient carbon dioxide there must be
a large surface area for gaseous exchange
a very short diffusion path between alveolar air and blood
5
concentration gradients for oxygen and carbon dioxide between alveolar air and blood.
The surface available in an adult is around 140m2 in an adult, around the area of
a singles tennis court. The blood in the alveolar capillaries is separated from
alveolar air by 0.6* in many places (1* = one thousandth of a mm) . Diffusion
gradients are maintained by
ventilation (breathing) which renews alveolar air, maintaining oxygen concentration near
that of atmospheric air and preventing the accumulation of carbon dioxide
the flow of blood in alveolar capillaries which continually brings blood with low oxygen
concentration and high carbon dioxide concentration
Haemoglobin in blood continually removes dissolved oxygen from the blood and
binds with it. The presence of this tennis court, separated from the outside air by
a very narrow barrier imposes demands on the respiratory tract.
Outside air:
varies in temperature. At the alveolar surface it must be at body temperature
varies from very dry to very humid. At the alveolar surface it must be saturated with water
vapour
contains dust and debris. These must not reach the alveolar wall
contains micro-organisms, which must be filtered out of the inspired air and disposed of
before they reach the alveoli, enter the blood and cause possible problems.
It is easy to see that the temperature and humidity of inspired air will increase as
it passes down a long series of tubes lined with a moist mucosa at body
temperature. The mechanisms for filtering are not so obvious.
Mucus
The respiratory tract, from nasal cavities to the smallest bronchi, is lined by a
layer of sticky mucus, secreted by the epithelium assisted by small ducted glands.
Particles which hit the side wall of the tract are trapped in this mucus. This is
encouraged by: (a) the air stream changing direction, as it repeatedly does in a
continually dividing tube. (b) random (Brownian) movement of small particles
suspended in the airstream.
The first of these works particularly well on more massive particles, the second
on smaller bits
Cilia
Once the particles have been sidelined by the mucus they have to be removed, as
indeed does the mucous. This is carried out by cilia on the epithelial cells which
move the mucous continually up or down the tract towards the nose and mouth.
(Those in the nose beat downwards, those in the trachea and below upwards).
The mucus and its trapped particles are and bacteria are then swallowed, taking
them to the sterilising vat of the stomach.
Length
The length of the respiratory tract helps in both bringing the air to the right
temperature and humidity but hinders the actual ventilation, as a long tract has a
greater volume of air trapped within it, and demands a large breath to clear out
residual air.
Protection
The entry of food and drink into the larynx is prevented by the structure of the
larynx and by the complicated act of swallowing. The larynx is protected by
6
three pairs of folds which close off the airway. In man these have a secondary
function, they vibrate in the airstream to produce sounds, the basis of speech and
singing. Below the larynx the trachea is usually patent i.e. open, and kept so by
rings of cartilage in its walls. However it may be necessary to ensure that this
condition is maintained by passing a tube (endotracheal intubation) to maintain
the airway, especially post operatively if the patient has been given a muscle
relaxant. Another common surgical procedure, tracheotomy, involves a small
transverse cut in the neck. If this is done with anatomical knowledge no major
structure is disturbed and the opening may be used for a suction tube, a ventilator,
or in cases of tracheal obstruction as a permanent airway.
Ventilation and perfusion
The gills of fish and the lungs of birds allow water and air receptively to flow
continually over the exchanging surface. In common with all mammals humans
ventilate their lungs by breathing in and out. This reciprocal movement of air is
less efficient and is achieved by alternately increasing and decreasing the volume
of the chest in breathing. The body's requirements for oxygen vary widely with
muscular activity. In violent exercise the rate and depth of ventilation increase
greatly: this will only work in conjunction with increase in blood flow, controlled
mainly by the rich innervation of the lungs.. Gas exchange can be improved by
breathing enriched air, which produces significantly reduced times for track
events. Inadequate gas exchange is common in many diseases, producing
respiratory distress.
Mechanism of breathing
In order to grasp the way in which we breathe we have to grasp the following
facts:
Each lung is surrounded by a pleural cavity or sac, except where the plumbing
joins it to the rest of the body, rather like a hand in a boxing glove. The glove has
an outer and inner surface, separated by a layer of padding. The pleura, similarly,
has two surfaces, but the padding is replaced by a thin layer of fluid.
Each lung is enclosed in a cage bounded below by the diaphragm and at the sides
by the chest wall and the mediastinum (technical term for the bit around the
heart). It is not usually appreciated that the lung extends so high into the neck. A
syringe inserted above a clavicle may pierce the lung.
Breathing works by making the cage bigger: the pleural layers slide over each
other and the pressure in the lung is decreased, so air is sucked in. Breathing out
does the reverse, the cage collapses and air is expelled. The main component
acting here is the diaphragm. This is a layer of muscle which is convex above,
domed, and squashed in the centre by the heart. When it contracts it flattens and
increases the space above it. When it relaxes the abdominal contents push it up
again. The proportion of breathing which is diaphragmatic varies from person to
person. For instance breathing in children and pregnant women is largely
diaphragmatic, and there is said to be more diaphragmatic respiration in women
than in men.
The process is helped by the ribs which move up and out also increasing the
space available. The complexity of breathing increases as does the need for
efficiency. In quiet respiration, say whilst lying on ones back, almost all
7
movement is diaphragmatic and the chest wall is still. This will increase thoracic
volume by 500-700ml. The expansion of the lung deforms the flexible walls of
the alveoli and bronchi and stretches the elastic fibres in the lung. When the
diaphragm relaxes elastic recoil and abdominal musculature reposition the
diaphragm again.
Deeper respiration brings in the muscles of the chest wall, so that the ribs move
too.
We must therefore understand the skeleton and muscular system of the thoracic
wall.
The 12 pairs of ribs pass around the thoracic wall, articulating via synovial joints
with the vertebral column - in fact two per rib. The ribs then curve outwards then
forwards and downwards and attach to the sternum via the flexible costal
cartilages. The first seven pairs of ribs (true ribs) attach directly, the next five
hitch a lift on each other and the last two float i.e. are unattached. Costal
cartilages are flexible. The first rib is rather different, short, flattened above and
below and suspended beneath a set of fairly hefty muscles passing up into the
neck, the scalene muscles. Between the ribs run two sets of intercostal muscles,
the external intercostals running forward and downwards, the internal
intercostals running up and back. These two muscle sheets thus run between ribs
with fibres roughly at right angles. When they contract each rib moves closer to
its neighbours. Because the lowest ribs float, and the first rib is suspended from
the scalene muscles contraction of the intercostal muscles tends to lift rib two
towards rib 1, and so on. The ribs are all, therefore pulled up towards the
horizontal, increasing anteroom-posterior and lateral thoracic diameters.
These movements are sometimes divided intopump handle movements, the rib
abducting on its vertebral joints and bucket handle movements, the rib rotating
on its axis around anterior and posterior attachments: these are not necessarily
helpful.
With more and more effort put into deeper and deeper breathing the scalene
muscles of the neck contract, raising the first rib and hence the rest of the cage,
then other neck muscles and even those of the upper limb become involved. A
patient with difficulty in breathing often grips a table edge in order to stabilise
the limbs so that their muscles can be used to help in moving the thoracic wall.
Problems.
The lungs sometimes fail to maintain an adequate supply of air. The earliest
cases of this are seen in infant respiratory distress syndrome. In premature infants
(less than about 2 lbs or 37 weeks the cells which make surfactant are not yet
active. Surfactant reduces the surface tension in the fluid on the surface of the
alveoli, allowing them to expand at the first breath, and remain open thereafter.
The sacs either fail to expand, or expand then collapse on expiration and result in
laboured breathing. In adults a similar syndrome is due to accidental inhalation
of water, smoke, vomit or chemical fumes.
Acute bronchitis is due to infection of the bronchial tree, which may have
impaired function due to fluid accumulation. Pneumonia involves the lung proper.
Lung cancers a malignancy that may spread to other tissues via the lymphatics in
the lung roots.
8
1. Dinding dada
Dinding dada pada bayi dan anak masih lunak disertai insersi tulang iga yang
kurang kokoh, letak iga lebih horizontal dan pertumbuhan otot interkostalis yang
belum sempurna menyebabkan pergerakan dinding dada terbatas.
2. Saluran nafas
Pada bayi dan anak relatif lebih besar dibandingkan dewasa. Besar trakea
neonatus sekitar 1/3 dewasa dan diameter bronkiolus ½ dewasa. Akan tetapi bila
terjadi sumbatan atau pembengkakan 1 mm saja, pada bayi akan menurunkan
luas saluran pernafasan sekitar 75%.
3. Alveoli
Jaringan elastis pada septum alveoli merupakan “elastic recoil” untuk
mempertahankan alveoli tetap terbuka. Pada anak, alveoli agak relatif lebih besar
dan mudah kolaps. Dengan makin besarnya usia bayi dan anak, jumlah alveoli
bertambah sehingga menambah “elastic recoil”.
ii. Histologi (WAJIB)
Overview of Respiratory Tract Histology
The lung is one of several organs that packs a large epithelial surface area into a
compact volume. The basic organizational pattern is that of a gland, in which a
branching tree of tubes provides continuity from the body's outside surface to a
vast number of epithelial cells. Indeed, the respiratory tract begins life as an
invagination of epithelial (endodermal) tissue, and embryonic lungs even have
the histological appearance of compound, exocrine glands. Only fairly late in
development do the cuboidal epithelial cells of the terminal alveoli assume the
thin squamous shape that characterizes the lining of mature gas-exchanging air
sacs. And some significant secretory function is retained, in the form of cuboidal,
surfactant-producing great alveolar cells.
Both in large glands and in the respiratory system, a system of conducting passageways
form a branching "tree", with functional units at the end of each twig.
o In the respiratory system, the tree's "trunk" is the trachea, larger branches are
called bronchi (singular "bronchus"), and smaller branches are
called bronchioles. (In a gland, the conducting passages are called "ducts".)
o In the lung, the epithelial cells at the ends of all the twigs form "respiratory units",
also called alveoli (singular, "alveolus"). (In a gland, the secretory units at the ends
of the twigs are also sometimes called "alveoli", which means a small hollow or
cavity.)
The pleural cavity is lined by mesothelium. This includes both the outer surface
of lung and the adjacent inner surface of the chest wall. (Simple squamous
9
mesothelial tissue also lines the other major body cavities, pericardial and
peritoneal.)
The conducting passageways of the respiratory system (nasal
cavity, trachea, bronchi and bronchioles) are lined
by pseudostratified columnar epithelial tissue, which
is ciliated and which includes mucus-secreting goblet
cells. Incoming particulates (dust, bacteria) adhere to the mucus, which is then
swept upward and away by the cilia.
Because the passage of air depends on wide open passageways,
the larger respiratory passages (trachea, and bronchi) are
supported by skeletal elements in the form of rings made
of cartilage. An extensive vascular plexus allows heat-exchange
to condition air before it reaches the delicate alveoli.
The respiratory or gas-exchange surface consists of millions of
small sacs, or alveoli, lined by a simple squamous
epithelium. This epithelium is exceedingly thin to facilitate
diffusion of oxygen and CO2. The alveolar walls also contain cuboidal
surfactant-secreting cells. The surfactant overcomes the tendency of alveolar
walls to adhere to one another (which would obliterate the air space).
As in any gland, each alveolus is enveloped by capillaries. In the lungs, the gas-
exchange function of this pulmonary vasculature is critical to organ function and
to life itself.
iii. Fisiologi (WAJIB)
The respiratory system is responsible for incorporating the oxygen in the
environment for the utilization of energy from the organic compounds and for
the elimination of carbon dioxide formed in the above process. This process can
be subdivided into:
1. Passage of air in between the lungs and the external environment
2. Exchange of gases in between the alveoli and the blood in the pulmonary capillaries
3. Transport of oxygen and carbon dioxide in blood
4. Diffusion of oxygen and carbon dioxide between the cells and the capillaries
5. Cellular respiration
10
1. Passage of Air in between the Lungs and the External Environment
Air flows as a bulk, in and out of the lungs through the upper respiratory tract to
come into contact with the blood in the pulmonary capillaries. The flow of air is
dependent on the differences of pressure created in between the environment and
the thoracic cavity due to the contraction of the respiratory muscles causing
movements of the chest wall and the diaphragm.
Learn more about lung mechanics......
Pulmonary Mechanics
Bulk flow of air in between the environment and the lungs is an important respiratory
function. Coordinated, active movements of the thorax and the diaphragm, result in
inspiration and expiration.
2. Gaseous Exchange at the Lungs
Oxygen diffuses along a partial pressure gradient from the alveolar air spaces in
to the pulmonary capillaries through the lining of the alveoli (simple squamous
epithelium), the thin interstitium and the endothelium of the pulmonary
capillaries, which is collectively known as the blood-gas barrier. Carbon-dioxide
diffuses in the opposite direction through the blood-gas barrier in to the alveoli.
3. Transport of Oxygen and Carbon-dioxide in Blood
Oxygen which enters the blood stream by simple diffusion through the alveolar
respiratory membrane is transported mainly bound to haemoglobin. A small
percentage of oxygen is transported dissolved in the plasma. Carbon-dioxide is
transported mainly in the dissolved form in plasma and the formed bicarbonate
ions are transported within the cytoplasm of the red blood cells.
4. Diffusion of Gases in between the Cells and the Capillaries
11
Oxygen is released from the haemoglobin to
which it is bound and diffuses along a
concentration gradient towards the cells in the
peripheral tissues. Carbon dioxide produced as
a byproduct of cellular respiration diffuses in
the opposite direction and is dissolved in the
plasma of the blood and the cytosol of the red
blood cells.
5. Cellular Respiration
The organic substances undergo oxidation by
losing electrons during the passage of
tricarbolic acid cycle and the electrone
transport chain. In the process oxygen acts as
an electrone and hydrogen acceptor and is converted to water. During the process,
carbon dioxide is produced as a byproduct.
The Physiological Anatomy of the Respiratory System
The respiratory system is made up of:
1. Upper respiratory tract (nose, pharynx and larynx)
2. Lower respiratory tract (trachea and the divisions of the airways)
1. The Upper Respiratory Tract
The upper respiratory tract is formed by the nose, pharynx and the larynx. The
upper respiratory tract is responsible for the conduction of air, which is in the
external environment, to the lower respiratory tract. In the process of conduction,
the air is filtered of any macro-particles, is humidified and warmed to the body
temperature. Large particles are prevented from reaching the lower respiratory
tract by adhesion to the mucus in the nasal cavity and the pharynx and the hair in
the nasal cavity. In addition, certain irritants are expelled by sneezing.
The pharynx is common to the digestive and the respiratory tracts and therefore,
is incorporated with a defense mechanism (gag-reflex) to prevent food from
entering the respiratory tract.
The larynx has an epiglottis (a covering cartilaginous flap) preventing aspiration.
It also has vocal cords responsible for phonation, which meet at the glottis, which
also can be closed tightly to prevent aspiration of substances. The glottis dilates
during inspiration and constricts during expiration. The larynx is supplied by a
12
sensory branch of the vagus nerve which can initiate the cough reflex, preventing
any aspirated and irritant substances (if inhaled accidentally) form reaching the
trachea.
2. The Lower Respiratory Tract
The lower respiratory tract commences at the trachea, which has a diameter of
2.5 cm and divides in to two bronchi, supplying air to each lung. The bronchi
further subdivide up to 16 divisions forming the conducting airways. The first
eleven divisions have a cartilaginous wall but the next five divisions, known as
bronchioles, is mainly muscular and therefore are subjected to collapse easily.
The 17
th to 19
th divisions of the lower respiratory tract, which are known as
respiratory bronchioles further divide to form alveolar ducts and alveolar sacs.
These alveolar sacs communicate with each other through Kohn’s pores. Each
lung comprises approximately 150 – 300 million alveoli and the total surface
area is larger than a tennis court (70m2). The alveoli have a conformation of a
honey-comb, which prevents collapse of individual alveoli and are lined by two
types of cells. The predominant type (known as type I alveolar cells) is a simple
squamous epithelium, across which the gases easily diffuse to the rich network of
pulmonary capillaries lying underneath the thin basement membrane. The second
type of cells is the type II alveolar cells, which secrete surfactant (a phospholipid
responsible for decreasing the surface tension in the alveoli, so that they would
be prevented from collapsing).
The alveoli are separated from each-other by a thin inter-alveolar septum, which
is formed only of pulmonary capillaries. The pulmonary capillaries bring poorly
oxygenated blood to the alveoli.
The physiology of the respiratory system and respiration is discussed in detail in
this series of hubs. However, the respiratory system preforms some non-
respiratory functions in addition to its main function. These will be discussed in a
separate hub.
13
b. Aetiologi
i. Batuk
Benda asing/ iritan pada saluran nafas bawah impuls aferen dari nervus vagus
ke otak respon inspirasi 2,5 L udara secara cepat epiglottis dan pita suara
menutup untuk menjerat udara dalam paru otot abdomen berkontraksi
mendorong diafragma serta otot pernafasan (mis, m. intercostalis internus) juga
berkontraksi pita suara dan epiglotis membuka tiba-tiba udara bertekanan
tinggi keluar dari paru-paru dengan cepat disertai dengan batuk.
ii. Sukar bernapas
Gangguan sistem pernafasan:
Penyakit saluran nafas: Asma bronkial, PPOK. Obstruksi.
Penyakit parenkim paru: Pneumonia, Acute Respiratory
Distress Syndrome, penyakit interstisial paru
Penyakit vaskular paru: emboli paru
Penyakit pleura: Pneumotoraks, efusi pleura
Gangguan sistem kardiovaskular
Gagal jantung kiri
Penurunan curah jantung
Anemia
Ankiektasis/psikosomatik
Gangguan pada sisitem neuromuskuloskeletal:
Polimiositis
Miastemia gravis
Sindrom Gullain-Barré
Kifoskoliosis
iii. Demam
Infection is the most common cause of fever in children. Common viral and
bacterial illnesses like colds, gastroenteritis, ear infections, croup, bronchiolitis,
and urinary tract infections are the most likely illnesses to cause fever.
(See "Patient information: The common cold in children (Beyond the
Basics)" and "Patient information: Nausea and vomiting in infants and children
(Beyond the Basics)" and "Patient information: Ear infections (otitis media) in
children (Beyond the Basics)" and "Patient information: Croup in infants and
14
children (Beyond the Basics)" and"Patient information: Bronchiolitis (and RSV)
in infants and children (Beyond the Basics)" and "Patient information: Urinary
tract infections in children (Beyond the Basics)".)
There is little or no scientific evidence to support the widespread belief that
teething causes fever. Although it is difficult to disprove this notion completely,
alternative causes of fever should always be sought and temperatures above
102°F (38.9°C) should never be attributed to teething.
Bundling a child who is less than three months old in too many clothes or
blankets can increase the child's temperature slightly. However, a rectal
temperature of 101ºF (38.5ºC) or greater is not likely to be related to bundling
and should be evaluated. (See 'Evaluation recommended'below.)
Some childhood immunizations can cause fever. The timing of the fever varies,
depending upon which vaccination was given. (See "Patient information:
Vaccines for infants and children age 0 to 6 years (Beyond the Basics)".)
c. Mengapa keluhan Mr. Zumi bertambah berat?
Keluhan Mr. Zumi bertambah berat karena pneumonia menyebabkan sekresi mukus
yang lebih banyak di dalam alveolus over time, jadi napas akan terasa lebih sesak.
d. Apa faktor usia berhubungan dengan keluhan yang dialami?
Faktor usia berhubungan dengan keluhan, yaitu pneumonia lebih sering terjadi di balita.
e. Bagaimana pertumbuhan dan perkembangan bayi pada kasus ini?
Sudah bisa mengucapkan M, B, P, ...
f. Bagaimana nutrisi pada bayi umur 9 bulan?
Bayi usia 9 – 12 bulan sudah mulai mengalami kemajuan dalam perkembangan
makan. Meskipun demikian orang tua harus memberi perhatian pada komposisi
makanan. Agar bayi memperoleh gizi yang cukup: tidak kurang atau berlebih.
Makanan penunjang ASI (MPASI) seperti apa yang bisa kita berikan untuk bayi yang
mulai memasuki 9 bulan? Pada saat itu Anda mulai bisa mengenalkan makanan dengan
tekstur yang lebih kental dan kasar seperti nasi tim. Gunanya agar bayi berlatih
mengunyah ketika gigi susunya mulai tumbuh.
Orang tua juga harus memberikan berbagai variasi makanan yang lengkap dan seimbang
gizinya untuk menunjang proses tumbuh kembang bayi. Selain itu juga untuk
memperkuat daya tahan tubuhnya dari berbagai serangan penyakit.
Hati-hati pada kelebihan atau kekurangan zat gizi tertentu karena kelebihan atau
kekurangan zat gizi ini bisa berpengaruh terhadap perrtumbuhan bayi. Misalnya,
kelebihan lemak pada bayi akan menyebabkan obesitas yang bisa memicu penyakit yang
15
berbahaya di kemudian hari. Dan, seterusnya. Berikut adalah sebuah contoh pola
pemberian makan untuk bayi usia 9 – 12 bulan:
Waktu Makanan/Minuman
05.00 ASI
07.00 Bubur Susu
09.00 Nasi Tim
10.00 ASI
12.00 Nasi Tim
14.00 ASI
16.00 Buah
17.00 Nasi Tim
19.00 ASI
Tengah
Malam ASI
Beri perhatian khusus:
Hindari kacang, kecuali dalam tekstur yang halus.
Periksa apakah masih ada duri ikan bila hendak memakan daging ikan. Perkenalkan ikan
setelah anak berusia 12 bulan.
Sedapat mungkin hindari daging yang berlemak dan garam yang dapat memicu terjadinya
obesitas, tekanan darah tinggi dan jantung (kecuali daging ayam rendah lemak bertekstur
lembut dan daging sapi cincang yang mengandung zat besi).
Hindari makanan pedas atau asam karena dapat memicu alergi pada usia ini. Makanan jenis
ini bisa diperkenal setelah anak berusia 12 bulan.
16
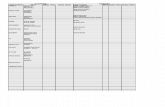
2. Pemeriksaan Fisik
a. Interpretasi dan mekanisme abnormal
i. Keadaan Umum dan Vital Sign (value untuk bayi)
Zumi, laki-
laki usia 9
bulan
Normal Interpretasi
Keadaan
umum:
Tampak
sakit berat
Sehat
Kesadaran:
Kompos
mentis
Kompos mentis Normal
RR: 68
x/menit
1 bulan – 1 th: 30 – 60
Rata2 waktu tidur: 30
Takipneu, kompensasi akibat
terjadinya gangguan aliran
udara akibat pemadatan
dialveoli karena peradangan
Nadi: 132
x/menit,
reguler
Istirahat (tidur): 80-150
Istirahat (bangun): 70-120
Aktif demam: s/d 200
Takikardi, karena adanya
demam dan adanya infeksi
menyebabkan pengaktifan
anti inflamasi salahsatunya
histamin yang salah satu dapat
menimbulkan vasokontriksi
PD.
Suhu: 38,6 0C
Normal : 36,5-37,2 oC
Sub Febris : 37,2-38˚C
Febris : >38-40˚C
Hyper Pirexia : >40˚C
Febris, karena adanya infeksi
shg merangsang pengeluaran
mediator inflamasi sprti IL1,
IL6, TNFα shg trjd
pningkatan suhu tubuh
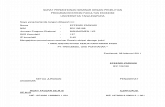
ii. Panjang Badan, Berat Badan, BMI
17
9 bulan kira-kira 37-38 minggu, dan seharusnya berat badan Zumi 6,5- 11,5kg.
Di sini terlihat bahwa berat badan Zumi normal.
b. Jenis-jenis suara nafas.
Jenis-jenis nafas vesikuler ?
Pada orang sehat dapat didengar dengan auskultasi suara napas :
1. Vesikuler
2. Trakeal
3. Bronkial
4. Bronkovesikuler
Untuk mendengar suara napas perhatikan intensitas, durasi dan pitch (nada) dari
inspirasi dibandingkan dengan ekspirasi.
Suara Napas Vesikuler.
Pada suara napas vesikuler, suara inspirasi lebih keras, lebih panjang dan pitchnya
(nada) lebih tinggi dari suara ekspirasi. Suara napas vesikuler terdengar hampir
diseluruh lapangan paru, kecuali pada daerah supra sternal dan interscapula. Suara
vesikuler dapat mengeras pada orang kurus atau post “exercise” dan melemah pada
orang gemuk atau pada penyakit-penyakit tertentu.
Suara Napas Bronkial / Trakeal
Pada suara napas bronkial, suara napas ekspirasi, intensitasnya lebih keras, durasinya
lebih panjang dan nadanya lebih tinggi dari suara inspirasi, terdapat pada daerah supra
sternal. Suara napas trakeal hampir sama dengan suara napas bronkial tetapi durasi
ekspirasi hampir sama antara ekspirasi dengan inspirasi, terdengar pada daerah trakea.
Ditemukanya bunyi napas bronkial pada daerah yang seharusnya suaran napas vesikuler,
hal ini dapat disebabkan oleh pemadatan dari parenkim paru seperti pada pneumonia dan
kompresive atelektase.
Suara Napas Bronkovesikuler
Pada bunyi napas bronkovesikuler, suara yang timbul adalah campuran antara suara
napas vesikuler dan bronkial. Jenis suara napas ini ditandai dengan ekspirasi lebih keras,
lebih lama dan nadanya lebih tinggi dari inspirasi. Jenis pernapasan ini, normal
didapatkan pada dada (?)
c. Apa saja immunisasi yang seharusnya sudah didapatkan oleh Zumi pada usia 9 bulan?
PAKE DATA SATRIA (DASAR) + OWEN (TAMBAHAN IDAI)
2 months
5-in-1 (DTaP/IPV/Hib) vaccine – this single jab contains vaccines to protect against five
separate diseases: diphtheria, tetanus, pertussis (whooping cough), polio and
Haemophilus influenzae type b (Hib, a bacterial infection that can cause severe
pneumonia or meningitis in young children)
Pneumococcal (PCV) vaccine
Rotavirus vaccine
3 months
5-in-1 (DTaP/IPV/Hib) vaccine, second dose
Meningitis C
Rotavirus vaccine, second dose
18
4 months
5-in-1 (DTaP/IPV/Hib) vaccine, third dose
Pneumococcal (PCV) vaccine, second dose
3. Keadaan spesifik
a. Interpretasi dan mekanisme abnormal
Jika kita melihat napas cuping hidung kita sudah harus berpikir bahwa diagnosis akan
arahnya ke pneumonia. Pneumonia lobair agak jarang, dan yang paling penting kita
perkirakan adalah adanya bronchopneumonia.
4. Pemeriksaan Laboratorium
a. Interpretasi dan mekanisme abnormal (value untuk bayi)
Di sini terlihat Leukocytosis, yang artinya terjadi infeksi. Lebih jelas lagi pada hitung
jenis kita dapatkan STTL (pergeseran ke kiri). ESR di sini 18 (≥ 15), yang artinya sudah
terjadi infeksi (biasanya acuut).
5. Pemeriksaan Radiologi
a. Interpretasi dan mekanisme abnormal, DISERTAI GAMBAR?
Infiltrat perihilair
19
6. Masalah Templat
a. Clinical Diagnosis (Bronchopneumonie?)
1. Anamnesis
- Apa keluhan yang dialami?
- Sejak kapan terjadi sesak napas?
- Sesak napas muncul hilang timbul atau terus-menerus?
- Sesak napas diperberat/dihilangkan dengan cara?
- Keluhan lain? (nafas cuping hidung, anak rewel, diare, demam)
- Sejak kapan terjadi gejala-gejala lain?
- Sudah pernah minum obat?
- Ada kontak dengan penderita?
- Riwayat sosial ekonomi keluarga?
- Lingkungan tempat tinggal?
2. Pemeriksaan Fisik
- Keadaan umum : sehat, sakit ringan, sakit sedang, sakit berat, kesadaran
- Respiratory rate
- Denyut nadi
- Suhu
- Nafas cuping hidung
- Inspeksi thoraks : retraksi otot-otot interkostal
- Palpasi thoraks: stem fremitus meningkat, bandingkan sisi kanan dan kiri
- Perkusi thoraks: redup pada basal (seharusnya sonor)
- Auskultasi thoraks: suara vesikular meningkat (ada kavitas, infiltrat), ada
ronki basah, tidak ada wheezing (menghilangkan diagnosis asma anak)
b. Differential Diagnosis
PRESENTASI Bronkopneumonia Bronkitis Bronkiolitis
Batuk + + +
Sukar bernafas + + +
Demam Demam tinggi Demam ringan Demam ringan/normal
USIA Infant/children Adult 1-2 tahun
Suara vesiculair Meningkat ? ?
Perkussi
Wheezing
c. Working Diagnosis
Bronchopneumonia (infant/children).
20
d. Definisi (WAJIB)
Bronkopneumonia adalah peradangan pada parenkim paru yang melibatkan bronkus atau
bronkiolus yang berupa distribusi berbentuk bercak-bercak (patchy distribution)
(Bennete, 2013). Pneumonia merupakan penyakit peradangan akut pada paru yang
disebabkan oleh infeksi mikroorganisme dan sebagian kecil disebabkan oleh penyebab
non-infeksi yang akan menimbulkan konsolidasi jaringan paru dan gangguan pertukaran
gas setempat (Bradley et.al., 2011)
e. Aetiologi
Infectious agents
Infectious agents are the most common cause of pneumonia in the cat and dog ( Table
19.1 ).
Viral infections include canine distemper virus (CD), canine adenovirus II (CAV2),
parainfluenza III (P13) and the upper respiratory tract viruses in cats. It is generally accepted
that viruses alone do not cause pneumonia, but rely on secondary bacterial infections.
Bacterial infections are generally secondary, although pneumonia has been associated with
the primary pathogens Bordetella bronchiseptica and B-haemolytic streptococci in dogs. In
cats Pasteurella spp may be primary bacterial pathogens.
The other bacterial invaders of the lungs are secondary pathogens, and are the major
aetiological agents in this disease. They include most of the agents found in the oropharynx
and may be regarded as part of the normal flora. However, the peripheral airways in normal
dogs and cats are sterile.
The most common secondary bacterial pathogens include staphylococci,
streptococci, Pasteurella, Klebsiella and Proteus spp,
and Escherichia coli. Pseudomonas spp do not constitute members of the normal upper
airway flora and they should always be regarded as pathogens.
Microaerophilic organisms such as Actinomyces and Nocardia spp can also cause
pneumonia.
Deciding whether or not an isolated organism is significant is qualitative. Heavy growths of
any of the organisms listed above suggest involvement in the disease process.
Mycoplasma agents and fungi are also secondary invaders; the mycotic pneumonias, such as
histoplasmosis and blastomycosis, are not found in the UK.
Several non-pneumonic conditions can progress to causing bronchopneumonia in
association with secondary bacterial invasion and proliferation. Chronic air-way conditions
such as chronic bronchitis, immotile cilia syndrome, tracheal collapse, chronic
tracheobronchitis and even acute tracheobronchitis, can predispose to pneumonia.
Non-infectious causes
21
While a variety of non-infectious agents can cause pneumonia this is usually due to
proliferation of secondary bacterial pathogens.
Non-specific irritants include smoke, acrolein and soot from house fires, although the acute
lung injury response to smoke inhalation is usually more serious than any secondary
bacterial bronchopneumonia that may develop.
Food and fluids can be inhaled and the degree of damage is related to the quantity of
material inhaled, its acidity and how easily it is removed from the lungs by normal
protective mechanisms.
Food inhaled because of swallowing defects, laryngeal paralysis or megoesophagus or in
young animals with cleft palate causes less damage than inhaled acidic gastric Contents.
Oral dosing with medications, particularly tasteless material such as liquid paraffin in cats,
and force feeding can result in bronchopneumonia. Once administration ceases, the
condition resolves itself as material is removed by macrophages and enters the lymphatic
drainage system.
Discrete foreign bodies such as grass seeds and small sticks can result in localised
bronchopneumonia, particularly if they lodge in smaller airways and are not removed within
a few days.
Inhaled allergens may also be involved in the development of eosinophilic pneumonia (see
PIE) in dogs and cats.
Airway and lung parasites such as Oslerus osleri in the dog and Aleurostrongylus abstrusus
in the cat (see Chapter 18 ) and migrating ascarid larvae in young animals might also
predispose to pneumonia.
Lung inflammation can also be caused by endogenous and exogenous toxins. Uraemic
pneumonitis has been reported in the dog, and paraquat causes interstitial lung damage and
interstitial fibrosis.
A sterile neutrophilic pneumonia has been seen by the authors, and auto-immunity
mechanisms in the aetiopathogenesis of pneumonia cannot be discounted
f. Epidemiologi
22
g. Manifestasi Klinik
The clinical presentation of bacterial pneumonia varies. Sudden onset of symptoms and
rapid illness progression are associated with bacterial pneumonias. Chest pain, dyspnea,
hemoptysis (when clearly delineated from hematemesis), decreased exercise tolerance,
and abdominal pain from pleuritis are also highly indicative of a pulmonary process.
The presence of cough, particularly cough productive of sputum, is the most consistent
presenting symptom. Although not diagnostic of a particular causative agent, the
character of the sputum may suggest a particular pathogen, as follows:
S pneumoniae is classically associated with a cough productive of rust-colored sputum.
Pseudomonas, Haemophilus, and pneumococcal species may produce green sputum.
Klebsiella species pneumonia is classically associated with a cough productive of red
currant-jelly sputum.
Anaerobic infections often produce foul-smelling or bad-tasting sputum.
Nonspecific symptoms such as fever, rigors or shaking chills, and malaise are common.
For unclear reasons, the presence of rigors may suggest pneumococcal pneumonia more
often than pneumonia caused by other bacterial pathogens.[27]
Other nonspecific
symptoms that may be seen with pneumonia include myalgias, headache, abdominal
pain, nausea, vomiting, diarrhea, anorexia and weight loss, and altered sensorium.[17]
h. Patofisiologi (WAJIB)
Normalnya, saluran pernafasan steril dari daerah sublaring sampai parenkim paru. Paru-
paru dilindungi dari infeksi bakteri melalui mekanisme pertahanan anatomis dan
mekanis, dan faktor imun lokal dan sistemik. Mekanisme pertahanan awal berupa filtrasi
bulu hidung, refleks batuk dan mukosilier aparatus. Mekanisme pertahanan lanjut berupa
sekresi Ig A lokal dan respon inflamasi yang diperantarai leukosit, komplemen, sitokin,
imunoglobulin, makrofag alveolar, dan imunitas yang diperantarai sel.
Infeksi paru terjadi bila satu atau lebih mekanisme di atas terganggu, atau bila virulensi
organisme bertambah. Agen infeksius masuk ke saluran nafas bagian bawah melalui
inhalasi atau aspirasi flora komensal dari saluran nafas bagian atas, dan jarang melalui
hematogen. Virus dapat meningkatkan kemungkinan terjangkitnya infeksi saluran nafas
bagian bawah dengan mempengaruhi mekanisme pembersihan dan respon imun.
Diperkirakan sekitar 25-75 % anak dengan pneumonia bakteri didahului dengan infeksi
virus.
Invasi bakteri ke parenkim paru menimbulkan konsolidasi eksudatif jaringan ikat paru
yang bisa lobular (bronkhopneumoni), lobar, atau intersisial. Pneumonia bakteri dimulai
dengan terjadinya hiperemi akibat pelebaran pembuluh darah, eksudasi cairan intra-
alveolar, penumpukan fibrin, dan infiltrasi neutrofil, yang dikenal dengan stadium
hepatisasi merah. Konsolidasi jaringan menyebabkan penurunan compliance paru dan
kapasitas vital. Peningkatan aliran darah yamg melewati paru yang terinfeksi
menyebabkan terjadinya pergeseran fisiologis (ventilation-perfusion missmatching) yang
kemudian menyebabkan terjadinya hipoksemia. Selanjutnya desaturasi oksigen
menyebabkan peningkatan kerja jantung.
Stadium berikutnya terutama diikuti dengan penumpukan fibrin dan disintegrasi
progresif dari sel-sel inflamasi (hepatisasi kelabu). Pada kebanyakan kasus, resolusi
23
konsolidasi terjadi setelah 8-10 hari dimana eksudat dicerna secara enzimatik untuk
selanjutnya direabsorbsi dan dan dikeluarkan melalui batuk. Apabila infeksi bakteri
menetap dan meluas ke kavitas pleura, supurasi intrapleura menyebabkan terjadinya
empyema. Resolusi dari reaksi pleura dapat berlangsung secara spontan, namun
kebanyakan menyebabkan penebalan jaringan ikat dan pembentukan perlekatan
(Bennete, 2013).
Secara patologis, terdapat 4 stadium pneumonia, yaitu (Bradley et.al., 2011):
1. Stadium I (4-12 jam pertama atau stadium kongesti)
Disebut hiperemia, mengacu pada respon peradangan permulaan yang berlangsung
pada daerah baru yang terinfeksi. Hal ini ditandai dengan peningkatan aliran darah dan
permeabilitas kapiler di tempat infeksi. Hiperemia ini terjadi akibat pelepasan mediator-
mediator peradangan dari sel-sel mast setelah pengaktifan sel imun dan cedera jaringan.
Mediator-mediator tersebut mencakup histamin dan prostaglandin. Degranulasi sel mast
juga mengaktifkan jalur komplemen. Komplemen bekerja sama dengan histamin dan
prostaglandin untuk melemaskan otot polos vaskuler paru dan peningkatan permeabilitas
kapiler paru. Hal ini mengakibatkan perpindahan eksudat plasma ke dalam ruang
interstisium sehingga terjadi pembengkakan dan edema antar kapiler dan alveolus.
Penimbunan cairan di antara kapiler dan alveolus meningkatkan jarak yang harus
ditempuh oleh oksigen dan karbondioksida maka perpindahan gas ini dalam darah paling
berpengaruh dan sering mengakibatkan penurunan saturasi oksigen hemoglobin.
2. Stadium II (48 jam berikutnya)
Disebut hepatisasi merah, terjadi sewaktu alveolus terisi oleh sel darah merah, eksudat
dan fibrin yang dihasilkan oleh penjamu ( host ) sebagai bagian dari reaksi peradangan.
Lobus yang terkena menjadi padat oleh karena adanya penumpukan leukosit, eritrosit
dan cairan, sehingga warna paru menjadi merah dan pada perabaan seperti hepar, pada
stadium ini udara alveoli tidak ada atau sangat minimal sehingga anak akan bertambah
sesak, stadium ini berlangsung sangat singkat, yaitu selama 48 jam.
3. Stadium III (3-8 hari berikutnya)
Disebut hepatisasi kelabu, yang terjadi sewaktu sel-sel darah putih mengkolonisasi
daerah paru yang terinfeksi. Pada saat ini endapan fibrin terakumulasi di seluruh daerah
yang cedera dan terjadi fagositosis sisa-sisa sel. Pada stadium ini eritrosit di alveoli
mulai diresorbsi, lobus masih tetap padat karena berisi fibrin dan leukosit, warna merah
menjadi pucat kelabu dan kapiler darah tidak lagi mengalami kongesti.
4. Stadium IV (7-11 hari berikutnya)
Disebut juga stadium resolusi, yang terjadi sewaktu respon imun dan peradangan
mereda, sisa-sisa sel fibrin dan eksudat lisis dan diabsorsi oleh makrofag sehingga
jaringan kembali ke strukturnya semula.
i. Prevention
*Penyakit bronkopneumonia dapat dicegah dengan menghindari kontak dengan
penderita atau mengobati secara dini penyakit-penyakit yang dapat menyebabkan
terjadinya bronkopneumonia ini.
Selain itu hal-hal yang dapat dilakukan adalah dengan meningkatkan daya tahan tubuh
kita terhadap berbagai penyakit saluran nafas seperti : cara hidup sehat, makan makanan
bergizi dan teratur ,menjaga kebersihan ,beristirahat yang cukup, rajin berolahraga, dll.
24
Melakukan vaksinasi juga diharapkan dapat mengurangi kemungkinan terinfeksi antara
lain:
- Vaksinasi Pneumokokus
- Vaksinasi H. influenza
- Vaksinasi Varisela yang dianjurkan pada anak dengan daya tahan tubuh rendah
- Vaksin influenza yang diberikan pada anak sebelum anak sakit.
*Vaksin Selain menghindari kontak menular, vaksinasi adalah modus utama dari
pencegahan. Vaksin memberikan kekebalan terhadap penyakit dengan merangsang
pembentukan antibodi dan dapat berupa dibunuh atau dilemahkan.
Vaksi Influenza virus (Fluzone) Vaksin influenza direkomendasikan untuk anak usia 6
bulan dan lebih tua. The 2 bentuk vaksin adalah (1) vaksin tidak aktif (berbagai produk),
diberikan sebagai suntikan intramuskular dan (2) vaksin dingin diadaptasi dilemahkan
(FluMist; MedImmune), diberikan sebagai obat semprot hidung, yang saat ini diberikan
hanya untuk orang yang berusia 2-49 tahun
13-valent vaksin pneumokokus konjugasi (PCV7, Prevnar) The 13-valent pneumococcal
conjugate vaksin (difteri CRM197 protein; Prevnar) berisi epitop sampai 13 strain yang
berbeda.
j. Tatalaksana
i. Farmakologik (WAJIB)
Pemilihan antibiotik dalam penanganan pneumonia pada anak harus
dipertimbangkan berdasakan pengalaman empiris, yaitu bila tidak ada kuman
yang dicurigai, berikan antibiotik awal (24-72 jam pertama) menurut kelompok
usia.
1. Neonatus dan bayi muda (< 2 bulan) :
a. ampicillin + aminoglikosid
b. amoksisillin - asam klavulanat
c. amoksisillin + aminoglikosid
d. sefalosporin generasi ke-3
2. Bayi dan anak usia pra sekolah (2 bl-5 thn)
a. beta laktam amoksisillin
b. amoksisillin - asam klavulanat
c. golongan sefalosporin
d. kotrimoksazol
e. makrolid (eritromisin)
3. Anak usia sekolah (> 5 thn)
a. amoksisillin/makrolid (eritromisin, klaritromisin, azitromisin)
b. tetrasiklin (pada anak usia > 8 tahun)
Karena dasar antibiotik awal di atas adalah coba-coba (trial and error) maka
harus dilaksanakan dengan pemantauan yang ketat, minimal tiap 24 jam sekali
sampai hari ketiga. Bila penyakit bertambah berat atau tidak menunjukkan
perbaikan yang nyata dalam 24-72 jam ganti dengan antibiotik lain yang lebih
tepat sesuai dengan kuman penyebab yang diduga (sebelumnya perlu diyakinkan
25
dulu ada tidaknya penyulit seperti empyema, abses paru yang menyebabkan
seolah-olah antibiotik tidak efektif).
ii. Non-farmakologik
Penatalaksanaan pneumonia khususnya bronkopneumonia pada anak terdiri dari
2 macam, yaitu penatalaksanaan umum dan khusus (IDAI, 2012; Bradley et.al.,
2011)
1. Penatalaksaan Umum
a. Pemberian oksigen lembab 2-4 L/menit sampai sesak nafas
hilang atau PaO2 pada analisis gas darah ≥ 60 torr.
b. Pemasangan infus untuk rehidrasi dan koreksi elektrolit.
c. Asidosis diatasi dengan pemberian bikarbonat intravena.
2. Penatalaksanaan Khusus
a. Mukolitik, ekspektoran dan obat penurun panas sebaiknya
tidak diberikan pada 72 jam pertama karena akan mengaburkan interpretasi
reaksi antibioti awal.
b. Obat penurun panas diberikan hanya pada penderita
dengan suhu tinggi, takikardi, atau penderita kelainan jantung
c. Pemberian antibiotika berdasarkan mikroorganisme penyebab
dan manifestasi klinis. Pneumonia ringan amoksisilin 10-25 mg/kgBB/dosis
(di wilayah dengan angka resistensi penisillin tinggi dosis dapat dinaikkan
menjadi 80-90 mg/kgBB/hari).
Faktor yang perlu dipertimbangkan dalam pemilihan terapi :
1. Kuman yang dicurigai atas dasas data klinis, etiologis dan epidemiologis
2. Berat ringan penyakit
3. Riwayat pengobatan selanjutnya serta respon klinis
4. Ada tidaknya penyakit yang mendasari
k. Komplikasi
Komplikasi yang paling berat dari pneumonia adalah gagal napas.
l. Prognosis dan SKDI
Dubia et bonam. SKDI bronchopneumonie paediatrik masuk ke 3B (tatalaksana darurat).
m. Follow-up dan Monitoring
Consider rawat inap. Jika pasien sudah sembuh, suruh follow-up untuk immunisasi dan
melihat apakah ada gejala sisa.
n. Edukasi
Beritahu orangtua pasien untuk kembali jika gejala menetap.
26
HYPOTHESIS
Zumi, bayi laki-laki usia 9 bulan, diduga menderita batuk, sukar bernafas, dan demam akibat
penyakit bronchopneumonie.
KETERKAITAN ANTAR MASALAH
[Type a quote from the document or
the summary of an interesting point.
Bronchopneumonia
Sesak napas Demam Batuk
27
LEARNING ISSUE
1. Anatomi dan Fisiologi Tractus Respiratorius
Saya tahu : Lumayan banyak
Saya tidak tahu : Banyak tentang detail
Saya mau buktikan : Sedikit
2. Diagnostik Fisik Paru
Saya tahu : Sedikit
Saya tidak tahu : Bagaimana pengerjaannya
Saya mau buktikan : Applikasi PDx paru
3. Bronchopneumonia
Saya tahu : Definisi
Saya tidak tahu : Penatalaksanaan
Saya mau buktikan : Pathofisiologi
30
Pharyng
Tuba auditiva [Eustachi]
Thyroid gland
Location = deep to sternothyroid, and sternohyoid m, @ level of C5-T1, isthmus located b/w 2nd &
3rd rings of trachea
Parts:
2 lobes – L and R, w. isthmus (small linking piece) b/w the two
Covered by fibrous capsule, which sends CT septa into gland (more info in HISTO)
Function: endocrine gland, produces
o thyroid hormone - controls rate of metabolism
o calcitonin – controls calcium level
CLINICAL NOTE -Tumor of thyroid gland can cause excess weight gain, or excess resorption of
Ca, causing bone fractures more likely
Blood supply:
o sup thyroid a (ext carotid a)
o inf thyroid a (thyrocervical trunk of subclavian)
o a run b/w fibrous capsule, and pretracheal cervical fascia
o both split into ant/post branches
Veins drain a venous plexus that covers ant surface of gland –> sup thyroid v, middle, inf thyroid
v
o sup & middle –> IJV
o inf thyroid –>brachiocephalic v
31
Lymph Drainage: network of lymph vessels –> prelaryngeal, pre tracheal, paratracheal l.n., inf
deep cervical l.n. –> brachiocephalic lymph nodes, thoracic duct
Innervation:
SNS: post ggl fibers from sup/mid/inf cervical ggl –> run via cardiac arterial plexus w/ thryroid
a –> cause VC (vaso constriction)
*NOTE- Thyroid reg. by hormones of hypophysis (pituitary)
Parathyroid glands:
Location: located just outside of fibrous capsule of thyroid gland
o Sup glands = 1 cm above entry of inf thyroid a, @ level of inf border of cricoid cart
o Inf glands = 1 cm below entry of inf thryoid a
Blood Supply: inf thryroid a, or br of esophageal, tracheal, laryngeal a
v –> venous plexus of thyroid gland
Lymph drainage: deep cervical and paratracheal l.n.
Nerves: see thyroid
Larynx:
Location: Bodies of C3 –> C6, leading from pharynx –> trachea
Function: regulate flow of air to and from lungs for vocalization = voice production, guard air
passages, so food and liquids don’t enter it
Part of Larynx: Cartilages, Membranes, Ligaments, Joints, Muscles
Cartilages:
o Thyroid - single hyaline cartilage
forms thelaryngeal prominence aka Adam’s apple,
32
has oblique line on lat surface of its lamina where inf pharyngeal constrictor,
sternohyoid, thryrohyoid attaches,
has a superior/inf horn
superior horn attaches to hyoid bone = thyrohyoid membrane
medial part of membrane = median thyrohyoid ligament
lateral part of membrane = lateral thyrohyoid ligament
o Cricoid cartilage - single hyaline cartilage
only one that encircles the entire larynx,
articulates w/ thryroid cartilage,
lower border of it marks end of pharynx/larynx
attaches to thyroid via median cricothyroid ligament
attaches to 1st ring of trachea via cricotracheal ligament
o Arytenoid (2) - paired hyaline/elastic cartilages,
shaped like pyramids w/ attachment to vocal ligaments and vocalis m to their vocal
processes (ant part of cart)
o Cunieform (2) - paired elastic cartilages that lie in aryepiglottic folds ant to corniculate
cartilages
o Corniculate (2) – paired elastic cart that lies on arytenoid cartilages, w/ aryepiglottic folds
of mucous membrane
o Epiglottis – single elastic cartilage, spoon shaped extension from sup/ant wall of larynx
Vallecula epiglottica – the areas b/w the the folds of the epiglottis, the median and
lateral glossoepiglottic folds
attached to thyroid cartilage via thyroepiglottic lig
Membranes & Ligaments of Larynx:
o Thyroid membrane – b/w hyoid and thyroid cart
o Cricothyroid ligament – thryroid and cricoid cartilage
o Quadrangular membrane – thyroid and arytenoid cart –> epiglottis, upper part of
aryepiglottic folds, inf margin of this membrane makes the ventricular folds
o Thryoepiglottic lig – epiglottis –> thyroid cart lamina
33
o Hyoepiglottic lig – epiglottis –> hyoid bone
o Conus elasticus - elastic membrane from cricoid cart –> line interconnecting inner surface
of thyroid cartilage and vocal process of arytenoid cartilage, closes off the laryngeal inlet,
except for at rima glottidis
Joints:
1. Cricothyroid Joint – tense vocal fold
o b/w inf horn of thyroid cartilage and lamina of cricoid cart
o fibrous capsule
o Movement: ant/post tilting of cricoid rt – when cart tips ant, tenses the cords, and post,
loosens cords, rotation & gliding of thyroid cartilage
o Associated Muscles = vertical and oblique cricothryroid m
2. Cricoarytenoid Joint
o b/w cricoid and base of arytenoid
o fibrous capsule
o Movement: Rotation, sliding, ant/post tilting – help tense and relax vocal folds
o Associate muscles = transverse arytenoid, post cricoarytenoid, lat cricoarytenoid, oblique
arytenoid, thryroarytenoid m vocalis m
Muscles of Larynx: – all innervated by recurrent laryngeal n, except cricothryroid = ext laryngeal
n, both from CN X
34
Intrinsic Muscles: move the laryngeal
parts, makes changes in the length and tension of the vocal folds
Adductors:
1. Lat cricoarytenoid
2. Oblique arytenoid
3. Transv arytenoid
4. Vocalis
Abductors:
1. Post cricoarytenoid m
Tensors of vocal fold:
1. Vertical and oblique cricothyroid m
2. Vocalis m
Relaxers of vocal fold:
1. Aryepiglottic
2. Vocalis m
3. Thyroarytenoid m
35
NOTE – ONLY 1 ABDUCTOR, so if inf laryngeal n is damaged, say bye to abducting – paralysis
of larynx
Extrinsic Muscles: move the larynx as a whole
Elevators of Larynx: (Mainly Suprahyoid m)
Digastric
1. Mylohyoid
2. Genioglossus
3. Stylohyoid
4. Stylopharyngeus
5. Thyrohyoid
Depressers of Larynx: (mainly infrahyoid m)
1. omohyoid
2. sternohyoid
3. sternohyoid
Cavity (Internal Structure) of Larynx:
3 parts:
1. Vestibule of larynx = laryngeal inlet –>the ventricular folds
o ventricular folds = mucus membrane folds elevated by lower free edge of quadrangular
membrane, run from thyroid cartilage above vocal ligament –> arytenoid cart
o laryngeal inlet = upper border of epiglottis, ary epiglottic folds, interarytenoid notch
2. Ventricle of larynx = b/w ventricular and vocal folds
o Vocal folds = from angle of thyroid –> vocal process of arytenoid cartilage,
IMPORTANT in voice production, b/c the control the stream of air thru rima
glottidis
alter the shape and size of rima glottidis, by movement of artyenoids to faciliate
respiration and phonation
Vocal folds made of:
36
vocal ligament = upper free edge of conus elasticus
vocal cords = fold of mucus membrane elevated by vocal lig
vocalis m = medial part of thyroarytenoid m
3. Subglottic (Infraglottic) space = rima glottidis –> lower border of cricoid cartilage
o Rima glottidis – narrow space b/w vocal folds
During inspiration = wide, expiration = narrow, wedge shaped
o Glottis = Rima glottidis + vocal folds + vocal processes
o Piriform recess = part of cavity of laryngopharynx on each side of laryngeal inlet
Breathing/Phonation (making noises):
The more tensed the vocal folds are, the more narrow the rima glottidis is.
Normal respiration – rima is narrow & wedge shaped
Forced respiration – wide and kite shaped
Phonation – narrow , slitlike
Whispering – almost not open
37
Blood Supply:
Arteries:
Sup laryngeal a – thru thyrohyoid membrane = internal surface of larynx
Inf laryngeal a – mucus mem and m. in inf part of larynx
enter w/ nerves of same name (Int br of sup laryngeal n/inf laryngeal n)
Veins: venis w/ arteries
Sup laryngeal v –> sup thyroid v –> IJV
Inf laryngeal v –> inf thyroid v, thyroid venous plexus –> L brachiocephalic v
Lymph Drainage:
Above vocal fold – upper deep cervical nodes
Below vocal fold – lower deep cervical nodes
Innervation: CN X
1. Superior Laryngeal n – splits into int laryngeal (SS, ANS) /ext laryngeal n (SM)
o = mucus membrane above vocal fold, taste buds on epiglottis
o enters w/ sup laryngeal a thru thryrohyoid mem
38
o int laryngeal n – SS to laryngeal mucosa above vocal folds
o ext laryngeal n - SM to inf constrictor m, cricothyroid m, runs w/ sup thyroid a
2. Recurrent Laryngeal n -
o (end branch of recurrent laryngeal n) all intrinsic m of larynx, except cricothyroid (ext
laryngeal br of CN X)
o SS = below vocal fold
o terminates in int laryngeal n @ just above lower border of cricoid cart
Pharynx
funnel shaped fibromuscular tube from base of skull –> to inf border of cricoid cartilage
Layers of Pharyngeal wall:
o Mucus membrane
o Submucosa
o Pharyngobasilar fascia
o Muscular layer
39
o Buccopharyngeal fascia
Has 3 parts:
Nasopharynx, Oropharnx, Laryngeopharynx
Nasopharynx: from base of occiput –> soft palate & isthmus of fauces
Structures w/in
1. Choana – post opening of nasal cavity
2. Pharyngeal fornix – angle b/w roof of nasopharynx and post wall of pharynx, location of
pharyngeal tonsils* (aka adenoids)
3. Opening of auditory tubes
- roof of auditory tube covered w/ torus tubarius
- ant bordered by salpingopalatine fold
- post bordered by salpingopharyngeal fold – has salpingopharyngeus m, opens pharyngeal
opening of auditory tube during swallowing
- around tube opening = tubal tonsils*
4. Pharyngeal recess – b/w salpingopharyngeal fold and post wall of pharynx
Oropharynx: b/w soft palate, root of tongue –> epiglottis
Structures w/in
1. Root of Tongue
2. Lingual tonsils*
3. Palatoglossal & palatopharyngeal folds – w/ tonsillar bed b/w,
o that holds palatine tonsils*
o tonsillar bed = formed by superior constrictor of pharynx, andpharyngobasilar fascia
Opening to Oropharynx = Faucial isthmus
o Exit of oral cavity –> pharynx
o bordered laterally by palatoglossal/palatopharyngeal folds
Isthmus of Pharynx (diff than Fauces)
o Narrowest part of pharynx b/w soft palate & post wall of pharynx
o b/w nasal and oral parts of pharynx
o closed by elevation and tightening of soft palate and contraction of sup constrictor of
pharynx & palatopharyngeus m
o Prevents food -> nasopharynx
Act of Swallowing:
1. Bolus of food pushed back by elevating tongue (styloglossus) into fauces
2. Palatoglossus & palatopharyngeus m contract to squeeze the bolus backward into oropharynx.
Tensor veli palatini & levator veli palatini eleavate soft palate & uvula to close entrance into
nasopharynx
3. Wall of pharynx raised by palatopharyngeus & stylopharyngeus to receive food, Suprahyoid m
40
elevate hyoid bone & laynx to close opening into larynx, passing over the epiglottis, prevent food
from entering respiratory pathway
4.Action of sup,mid,inf constrictor move food through oropharynx and laryngopharynx –> esoph,
where propelled by peristalsis
Blood Supply:
o tonsillar br of facial a
o asc pharyngeal a
o asc palatine br of facial a
o desc palatine a
o pharyngeal br of maxillary a
o br of sup/inf thyroid a
Innervation:
o lies on middle pharyngeal constrictor
o formed by pharyngeal br of CN IX, X, SNS br from sup cervical ggl
o Vagal br = all m of pharynx, w/ exception of stylopharygeus m (CN IX), and tensor veli
palatini (V2)
o Glossopharyngeal br = sensory fibers of pharyngeal mucosa
Laryngopharynx: epiglottis –> cricoid cartilage (C4-C6)
1. Piriform recess - b/w larynx (aryepiglottic fold) & lat wall of pharynx (medial surface of thyroid
cartilage & thyrohyoid membrane), contains sup laryngeal a, int laryngeal n
2. Med/Lat glossoepiglottic folds
3. Valleculae epiglottica – b/w med and lat glossoepiglottic folds on sup side of epiglottis
4. Post/lat walls = middle and inf constrictor m,
5. Internal wall = palatopharyngeus, stylopharyngeus m
Muscles: all innervated by Pharyngeal plexus, except stylopharyngeus m (IX)
41
Elevators:
o Stylopharyngeus m
o Palatopharyngeus m
o Salpingopharyngeus m
Constrictors:
Sup/middle/Inf constrictors
each one is thicker than the one above and cover the lower end of it
* To see Parapharyngeal space & Retropharyngeal space, refer to cards above
Histology: Pharynx, larynx and thyroid gland.
Slide #28 Larynx *H&E
42
Structures to Identify:
o vestibule
o true vocal folds
o false vocal folds
o cricoid cart
o vocal ligaments
o str columnar epith
o epiglottis
o rima glottidis
o quadrangular membrane
o vocalis m
o str. sq epith
o ventricles
o thryoid cartilage
o conus elasticus
o psuedo str. epith
Lower power:
can see greater horn of hyoid bone
hyaline cartilages:
cricoid cartilages
thyroid cartilages
b/w cartilages = laryngeal musc – str. musc fibers
on outer side of thyroid cart = infrahyoid m can be seen
Vertical section thru larynx:
show 2 vocal folds, supporting cartilages & muscles
vestibule –> vestibular folds –> ventricle –> true vocal fold —> subglottic region
Function:
conducts air
43
origin of speech
helps in swallowing
sound production & resonance
Mucosa:
false vocal fold = made by mucosa,
lined pseudostr. columnar epith w/ ciliae & goblet cells = respiratory epith
vocal fold= str. squamous non epith, more resistant to strain bacteria
vocal ligament located just deep to it
rich in a/v, esp capillaries
subglottic region = respiratory epith again
Lamina Propia
in LP = mixed glands (mostly mucus)
excretory ducts from glands, open @ epith
lymphatic nodules on ventricular side of fold
is thinner in area of vocalis m = no glands or a/v
Fibromuscular layer = quadrangular membrane
cartilages = become ossified to bone depending on age
cricoid cart = perichondrium + chondrons surrounded by matrix (PGs) + type II collagen fibers
ext pharyngeal m = responsible to move & elevate larynx during swallowing
44
musc = thyroarytenoid m
Adventia – external layer of CT
Slide #34 Thyroid Gland *H&E
Structures to Identify:
CT septa
follicles
colloid
follicular cells
parafollicular cells
arterioles
capillaries
venules
General Info:
unique exocrine gland b/c stores large amounts of secretory products extracellularly
has R & L lobe that are connected in middle via isthmus
CT septa separate thyroid gland into lobules
contain a/v, capillaries (from sup/inf thyroid a)
Follicular cells = prinicipal cells
follicular cells stores their secretory products in the cytoplasm
arranged into spherical shapes = follicles
45
surrounded by reticular fibers, and a/v – so thyroid hormones can enter blood
follicular epithelium = squamous, cuboidal, low columnar
structural and functional unit of thyroid gland
follicular cells can also release secretory products into lumen of follicles
stores their secretory products in the cytoplasm = colloid
made of thyroglobulin = GP w/ iodine acids
active thyroid hormones liberated from thyroglobulin
released into fenestrated capillaries that surround follicle
secretion of thyroid hormones = T3 + T4
o regulate cell & tissue base metabolism, heat production, influence body growth &
development
o inc fat/prot synthesis/degradation
o inc rate of carb use absorption
o inc heat production
o regulated by TSH
Production of Thyroid Hormones:
Thyroxine (3,5,3′,5′-tetraiodothyronine) is produced by follicular cells of the thyroid gland. It is
produced as the precursor thyroglobulin (this is not the same as TBG), which is cleaved by enzymes
to produce active T4.
Thyroxine is produced by attaching iodine atoms to the ring structures of tyrosine molecules.
Thyroxine (T4) contains four iodine atoms. Triiodothyronine (T3) is identical to T4, but it has one
less iodine atom per molecule.
Iodide is actively absorbed from the bloodstream by a process called ‘iodine trapping’ and
concentrated in the thyroid follicles. (If there is a deficiency of dietary iodine, the thyroid enlarges
in an attempt to trap more iodine, resulting in goitre.) Via a reaction with the enzyme
thyroperoxidase, iodine is covalently bound to tyrosine residues in the thyroglobulin molecules,
forming monoiodotyrosine (MIT) and diiodotyrosine (DIT). Linking two moieties of DIT produces
thyroxine. Combining one particle of MIT and one particle of DIT produces triiodothyronine.
* DIT + MIT → r-T3 (biologically inactive)
* MIT + DIT → triiodothyronine (usually referred to as T3)
* DIT + DIT → thyroxine (referred to as T4)
parafollicular cells
larger, pale staining cells
either peripherally, in follicular epith or w/in follicle
synthesize & secrete calcitonin =
o reg Ca2+ metabolism, and decreases its level in blood
46
o stimulate absorption of Ca2+ by bone
o regulated by concentration of Ca in blood
Embryology: Development of the pharynx, larynx and thyroid gland.
Pharynx:
Components of branchial/pharyngeal apparatus:
o Pharyngeal arches
o Pharyngeal pouches
o Pharyngeal clefts/grooves
Pharyngeal (branchial) arches:
o Derived from neural crest cells
o Resemble fish gills (branchia)
o Begin to develop early in the 4th week
o By end of 4th week, four pairs of arches are visible on the surface (not 5th and 6th ) and a
buccopharyngeal membrane ruptures forming communication between primitive oral cavity
and foregut
o Contribute to the formation of the neck as well as the face.
Pharyngeal Arch Derivatives:
Each arch has a core of mesenchymal tissue (mesoderm) covered bysurface ectoderm
(outside) and by endodermal epithelium (inside)
o Ectoderm -> skeletal
o Mesoderm -> muscles with accompanying nerve
o Arterial component (aortic arches) – each pharyngeal arch has an aortic arch running w. it
o Therefore, each arch carries nerve, muscle, bone and blood supply
First pharyngeal arch:
o Maxillary process (dorsal): Premaxilla, maxilla, zygomatic bone, portion of temporal bone
o Mandibular process (ventral): Contains Meckel’s cartilage which disappears except for
dorsal end (incus & malleus) and mandible
o Muscles of mastication, digastric (ant belly), mylohyoid, tensor tympani and tensor palatini
o Therefore, the accompanying motor nerve is the mandibular branch of trigeminal (V2) and
sensory are V1, V2, and V3
47
o 1st aortic arch practically disappears but forms the maxillary artery
Second pharyngeal arch:
o Reichert’s cartilage – stapes, styloid process, stylohyoid ligament, lesser horn and upper part
of the hyoid
o Muscles include: stapedius, stylohyoid, digastric (post belly), auricular, and those of facial
expression
o Facial nerve (CN VII)
o 2nd aortic arch – stapedial & hyoid arteries
Third pharyngeal arch:
o Cartilaginous contributions include greater horn and lower part of hyoid
o Sole muscle: stylopharyngeus
o CN IX (Glossopharyngeal nerve)
o 3rd aortic arch (quite large): common carotid, 1st portion of internal carotid (remainder
dorsal aorta), and external carotid
Fourth & sixth pharyngeal arch:
o Cartilaginous contributions to larynx derived from fusion: thyroid, cricoid, arytenoid,
corniculate, and cuneiform
o Muscles of 4th: cricothyroid, levator palatini, and pharyngeal constrictors are innervated by
SLN (CN X)
o Muscles of 6th: intrinsics of larynx are innervated by RLN (CN X)
o 4th aortic arch: L->arch of aorta & R->subclavian
o 6th aortic arch: L & R pulmonary with ductus arteriosus on left
Pharyngeal pouches (5):
o 1st:tubotympanic recess-> middle ear & eustacian tube -> TM
o 2nd palatine tonsil/fossa
o 3rd: inferior parathyroid (dorsal), thymus (ventral)
o 4th: superior parathyroid
o 5th: ultimobranchial body -> calcitonin producing C cells (parafollicular)
Pharyngeal clefts/grooves (4):
o 1st: external auditory meatus
48
o 2nd-4th : epicardial ridge and cervical sinus (disappears)
Larynx:
o Int lining from endoderm, as well as the laryngeal epithelium & glands
o musc & cartilage from 4th & 6th pharyngeal arch = thyroid, cricoid, arytenoid cartilages –
therefore innervated by CN X
superior laryngeal n – above the vocal fold
recurrent laryngeal n = below the vocal fold
o @ wk 4, on the ventral side of the primitive gut, a pocket forms that bulges out from the gut
= laryngotracheal diverticulum
o distal end of diverticulum to form lung bud
o then, 2 folds of tracheo-esophageal folds, push medially and push together to midline to
form a wall “septum”
ant (ventrally) = laryngealtracheal tube
post (dorsally) = esophageal tube
o opening of laryngeal diverticulum = orifice
Thyroid gland:
o endoderm lining @ midline of floor in pharynx – forms pocket =diverticulum
o @ 7th wk = this pocket moves downward – and passes ventral to hyoid & laryngeal cart
o remain connected to tongue by thyroglossal duct — remains foramen cecum
o functional @ 3rd month
49
PHYSICAL DIAGNOSTIC LUNG
History - Respiratory System
Cough
Duration of having cough.
Productive vs. non-productive.
Chest tightness (acute bronchitis).
Onset: environment (allergy, asthma).
Character:
• Bark-like (larynx).
• Whoop (whooping cough).
• Dry, with post-nasal drip (pharynx).
Exacerbating: night (CHF, asthma).
Sputum, hemoptysis
Volume.
Color:
• Yellow-green [purulent] (bronchiectasis, lobar pneumonia).
• Clear [serous].
• Grey [mucoid] (chronic bronchitis).
• Pink froth secretion (pulmonary edema).
• Red jelly (Klebsiella).
Viscosity (mucoid more viscous than purulent).
Foul smell (lung abscess, bronchiectasis).
Dyspnoea
Exertional: how far can you walk?
Orthopnoea: sleep with pillows?
Paroxysmal nocturnal dyspnoea: gasp at night?
Timing: worsened over the years (pulmonary fibrosis) vs. rapid onset (RTI).
Wheeze
Heard louder on expiration.
Prolonged expiration.
50
Precipitating factors.
Pt. could use term wheeze, when it's an inspiratory stridor, etc.
Chest pain
SOCRATES.
Character: stabbing.
Exacerbating: deep inspiration (pleurisy, rib fracture), anxiety.
Apnea
Do you snore?
Loudness of snoring.
Interruption of activity next day.
Hoarseness
Laryngitis attacks.
Voice hoarseness (CA, nerve palsy).
Sinus symptoms
Blocked sinuses sensation.
Number of times draining sinuses in day.
Post nasal drip.
Fever, night sweats
Fever (RTI, TB).
Timing: day or night.
Temperature reached, if known.
Sweating at night (TB).
Past medical, surgical history
RTIs: pneumonia, TB, bronchitis.
Asthma.
Measles, pertussis during childhood.
Laryngitis.
Lung CA.
51
HIV (PCP).
Surgery: for TB, tumor.
Family history
Condition in a relative, what age.
Asthma.
Emphysema, other COPDs.
CF.
TB.
MI, angina.
Social history
Smoking: ever smoked, how many per day, for how long, type [cigarette, pipe, chew].
Passive smoking in the home, workplace.
Alcohol (aspiration).
Occupation type:
• Farmer (farmer's lung).
• Construction, shipyard (asbestos).
• Miner, factory worker, stonemason (toxins).
• Animal worker (M. psitacci).
• Air conditioners (Legionella).
Occupation details:
• Tasks done at work.
• How long of exposure.
• Protection used.
• Illness in fellow workers.
Describe your home: stairs, etc.
Pets at home (allergy, M. psittaci).
Who is with you there at home.
Drug history
Drugs currently on, including delivery method.
• Steroids (TB risk).
• ACE inhibitors (cough).
• OCP (PE risk).
• Beta-blockers (bronchospasm).
52
OTCs, including antihistamines.
Ventilators.
Recreational drugs:
• Marijuana (cigarette-like).
• Cocaine (fibrosis).
• IV users (pulmonary edema, abscess).
Allergies, especially to inhaled substances.
Allergies to drugs, dyes.
Systems
Cardiovascular: (chest pain, dsypnoea).
Alimentary: GERD (chest pain cause, cough worse after eating).
Alimentary: fistula (cough worse after eating).
Nervous (respiratory depression).
Examination - Respiratory System
Environment
Table: inhalers, cigarettes.
Ventilator, O2 mask, nasal tube.
Sputum cup.
Pneumatic boots (PE risk).
General appearance
Ask pt. to sit over edge of bed, if well enough.
Colors:
• Cyanotic.
• Pink (emphysema, CO2 toxicity).
• White (anemia).
• Jaundiced (lung CA metastatic to liver).
• See Skin Colors Reference.
Dyspnea, wheeze, difficulties.
Breathing rate [normal: 14 breaths/min].
Using accessory muscles of respiration.
Edema.
53
Cough type. More detail later in Cough, Sputum exam below.
Thyroxicosis (goiter impinging on trachea).
Nails
Nicotine stains.
CLUBBING (Lung dz: hypoxia, lung cancer, bronchiectasis, CF).
• Emphysema, chronic bronchitis don't cause clubbing.
Leuconychia (hypoalbuminism 2° to cirrhosis).
Muehrke's lines (hypoalbuminism 2° to cirrhosis).
See Nails Reference.
Hands
Peripheral cyanosis.
CO2 flapping tremor (CO2 retention):
• Pt.does a policeman "stop" position with both hands.
• Unlike liver flap, both hands go down at once.
HPO (lung CA).
Erythema (CO2).
Tremor (asthma inhaler).
Veins (CO2).
Muscle wasting of hands: inspect, then ask pt. to adduct/abduct against Dr's resistance
(brachial plexus palsy 2° to lung CA).
Pallor of palmar creases (anemia 2° to blood loss).
Pulse: rate (asthma has tachycardia), rhythm, character, pulsus paradoxus (severe asthma).
See Pulse Reference.
Arms
Blood pressure, if relevant.
Eyes
Horner's syndrome (lung CA in apex):
• Ptosis.
• Miosis: partially constricted, but reacts normally to light.
• Anhydrosis: Dr's back of finger over each eyebrow to compare sweating.
Chemosis [tear that doesn't drop] (CO2 retention).
54
Eye fundus: papilloedema. See Fundus Examination.
Conjunctiva: pale (anemia).
Nose, sinuses
Deviated septum (nasal obstruction).
Nasal polyps (asthma).
Swollen turbinates (allergies).
Palpate sinuses for tenderness (sinusitis).
Mouth, voice
Lips blue: (peripheral cyanosis).
Pursed lips breathing (emphysema, but not chronic bronchitis).
Teeth: nicotine stains.
Teeth: broken, rotten (predisposition to pneumonia or lung abscess).
Tonsils: tonsils inflamed (upper RTI).
Pharynx: reddened (upper RTI)
Tongue: leucoplakia (smoking, spirits, sepsis, syphilis, sore teeth).
Under tongue (central cyanosis).
Voice: hoarseness (recurrent laryngeal nerve).
Voice: stridor (upper airway obstruction).
FET: listen for wheeze.
Cough, sputum
Productive cough (typical pneumonia, bronchiectasis, chronic bronchitis).
Dry cough (ACEi, asthma, atypical pneumonia, bronchial CA).
Bovine cough [lacks initial hard sound] (paralyzed vocal cords).
Sputum: colour, amount, consistency, blood, purulence.
• Red jelly sputum (Klebsiella).
• Rusty sputum (Strep pneumonia).
Neck
Expose pt's chest and neck, covering women's breasts with loose material.
Hypertrophied accessory muscles of inspiration.
55
Obese neck with receding chin (obstructive sleep apnea).
Signs of tracheostomy, other surgeries.
Goiter (trachea impingement).
Lymph nodes. See Nodes Reference.
JVP
Landmark is sternal notch to heads of SCM to earlobe.
Anything >3cm is significant.
See JVP Reference.
Trachea
Dr's middle finger on sternal notch.
Keeping middle finger on notch, put index on one side, then ring on other side.
Assess deviation (enlarged thyroid, intrathoracic dz).
If deviated, focus ensuing chest exam to upper lobe problem.
Chest: inspection
Ask. pt. to undress to waist.
Chest shape:
• Barrel chest (emphysema).
• Pigeon chest aka pectus carinatum (rickets).
• Funnel chest aka pectus excavatum (congenital defect).
Harrison's sulcus [depression above costal margin] (rickets, childhood asthma).
Asymmetry during respiration.
Spine curvature: kyphosis, scholiosis, lordosis, kyphoscliosis (polio, Marfan's).
Chest drains.
Scars.
Radiotherapy marks.
Veins (SVC obstruction).
Local swellings. If on breast, See Breast Examination.
Chest: palpation
Ask pt if any part tender: examine that last.
56
Ribs (fracture).
Chest: palpation: expansion
Pt leans forward, crossing arms to get scapula out of the way for palpation, percussion,
auscultation of back.
Pt lets their breath all the way out
Dr places palms on pt's back, thumbs together.
Pt breathes all the way in.
Dr records how far thumbs have spread, and whether 1 thumb moved less than the other.
Usual expansion is 4cm.
Alternatively: use a measuring tape.
Chest palpation: vocal fremitus
Ulnar edge of Dr's pronated, flattened hand slips into upper intercostal space.
Pt says "99".
Dr's hand moves to opposite side, and repeat down intercostal spaces.
Listening for a change in sensation:
Increased fremitus (pneumothorax helping conduction).
Decreased fremitus (consolidation preventing conduction).
Chest: percussion
Percuss by comparing left to right each time as move from top to bottom of lung.
Supraclavicular region.
Back.
Tidal percussion (diaphragm paralysis).
DDx:
• Dull: solid (liver, consolidated lung).
• Stony dull [very dull]: fluid (pleural effusion).
• Hyper-resonant: hollow (pneumothrorax, bowel).
Chest: auscultation
Have pt. cross arms. Ask pt. to "breath in and out, though your mouth, on your own time".
Breath sounds.
Adventitious sounds.
57
Chest: auscultation: resonance
Pt says "99" each time Dr listens to each part of chest
Clearly heard aegophony speech [bleating goat] means consolidation.
Muffled is normal.
If aegophony, assess "whispering pectoriloquy":
• Pt whispers "1,2,3,4".
• See if can hear whisper clearly with stethoscope (extreme consolidation).
Anterior chest
Palpate apex beat for presence, deviation. See Apex Beat Reference.
Pemberton's sign (SVC obstruction):
• Pt raises arms over head.
• Pt develops facial plethora, non-pulsatile JVP elevation and inspiratory stridor.
Heart
Pt. at 45º.
Have a quick listen to heart.
See Heart Auscultation in CVS examination.
See Heart Sound Reference.
Abdomen
Abdominal breathing: more than normal.
Palpate liver if RHF. See Liver Palpation in abdomen examination.
Legs
Peripheral cyanosis.
Ankle swelling (DVT, so PE risk).
Toenails and foot showing same symptoms as Fingernails and Hands.
58
BRONCHOPNEUMONIE INFANT-PAEDIATRIC
90% of pneumonia in children is viral. Of the 10% that is bacterial, 90% in children aged over three
months will be caused by pneumococcus; most of the remainder will be caused by H. influenzae. In
the younger child other organisms are implicated; they are considered under neonatal pneumonia.
Pneumonia in infants and children has a variety of aetiologies which can only be distinguished by
laboratory, and not clinical or radiological, findings. However, the epidemiology makes blind
treatment a practical proposition.
NICE note that clinical features suggestive of pneumonia , in a child less than 5 years, are:
tachypnoea
o RR > 60 breaths per minute age 0-5 months
o RR > 50 breaths per minute age 6-12 months
o RR > 40 breaths per minute age > 12 months
crackles in the chest
nasal flaring
chest indrawing
cyanosis
oxygen saturation <= 95%
The majority of lower respiratory tract infections in infants and children are preceded by upper
respiratory tract viral infections. Damage to epithelial surfaces and changes in the usual bacterial
flora permits secondary bacterial infection.
Other predisposition is from aspiration or debilitation.
Examples of different types of pneumonia in childhood:
viral - any child, especially younger than 1 year
Pneumococcal - older child, lobar, accounts for 90% paediatric bacterial pneumonia
Haemophilus - all ages
Staphylococcal - under 1 year, debilitated, weakened infants.
Mycoplasma - older children, ages 5 to 15.
59
Pneumocystis - in immunocompromised child (or adult)
In infants less than three months of age, the section on neonatal pneumonia should be consulted.
Several pathogens may co-exist in a sick child, one common combination is Chlamydia and
Cytomegalovirus.
clinical features
You have one open access page left.
UK healthcare workers and students can get
FREE subscriptions... click here.
Clinical diagnosis of pneumonia is based on:
fever
tachypnoea
intercostal or subcostal recession
nasal flaring
expiratory grunting
shortness of breath
anxiety
cyanosis
respiratory failure
Investigations to consider include:
chest radiology - if there is tachypnoea and crepitation
full blood count
C-reactive protein
blood cultures
urea and electrolytes
cough swab or sputum
blood gases may be indicated in the very sick patient
60
Findings such as a neutrophilia or a raised C-reactive protein level may be suggestive, but are not
diagnostic of a bacterial infection.
"GPs will often have to make a diagnosis based on clinical features alone since other diagnostic
tools such as chest Xray or sputum and blood culture may not be immediately available (1)." Ref:
Drugs and Therapeutics Bulletin (1997), 35 (12), 89-92.
The initial treatment of children with pneumonia, but with no obvious pathology such as immune
suppression, the most common cause of a baterial peumonia is Streptococcus pneumoniae and this
is usually sensitive to penicillin. Therefore the antibiotic of choice is penicillin V or amoxycillin (1)
(note that the broader spectrum of amoxycillin is probably not an advantage since penicillin V
covers the most likely organism, ie S. pneumoniae).
In children who are allergic to penicillin or if Mycoplasma pneumoniae is thought to be the
causitive organism (e.g. in the older school-aged child and adolescent) a macrolide such as
erythromycin is the first choice.
Failure to respond to this should raise the possibility of other factors:
mycoplasma - if used penicillin as first-line agent
structural anomoly, including a foreign body
tuberculosis
Ref: Drugs and Therapeutics Bulletin (1997), 35 (12), 89-92.
PEMBUATAN RESEP
dr. Mesyet
--------------------------------------
R/
Chloramphenicol Vial mL ??? No. ??? (or Gentamicin IM/IV)
R/
Paracetamol syrup fl No. I
S 4 dd 1 cth
R/
Ampicillin Vial mL ??? No. ???
61
PROGNOSIS
Sangat baik dengan pengobatan yang tepat dan cepat. Dengan pemberian antibiotika yang tepat dan
adekuat, mortalitas dapat ditemukan sampai kurang dari 1%. Anak dalam keadaan malnutrisi energi
protein dan yang datang terlambat menunjukkan mortalitas yang lebih tinggi.
Prognosis menjadi buruk pada kasus di bawah ini:
• Usia ektrim (anak dan lanjut usia)
• Mendapatkan pengobatan yang tidak tepat
• Shock (tekanan darah menurun)
• Pernapasan lebih dari 30 x/menit
• Mengenai lebih dari 1 lobus paru
• Darah putih yang rendah (< 5.000/l)
• Mempunyai penyakit lain (gangguan hati, gagal ginjal atau gangguan jantung)
• Penyakit menyebar keluar paru, misalnya mengenai selaput otak
STANDAR KOMPETENSI DOKTER INDONESIA
Tingkat Kemampuan 3B
Mampu membuat diagnosis klinik berdasarkan pemeriksaan fisik dan pemeriksaan tambahan (misal
labor sederhana dan x ray). Dokter dapat memutuskan dan memberikan terapi awal serta merujuk
kepada spesialis yang relevan dan menangani kasus gawat darurat.
62
There are four stages to pneumonia which an individual may go through after contracting the
condition.
The first stage will involve the body actually accumulated bacteria. The infection will continue to
grow as the number of bacteria increase. As a result, this will lead to the second
stage of pneumonia which is also known as the red hepatisation stage. At this stage, the alveolar
spaces in the lungswill start to become blocked with blood and this may even start appearing on the
surface of the lungs. These air sacs or alveoli will start to become more and more inflamed as they
become filled with fluid.
At the third stage, the red blood cells will begin to break up and this is also known as the gray
hepatization stage. The last stage occurs when fluids inthe lungs are broken down by enzymes and
this may also include pus.
The body’s natural reaction to trying to clear these fluids from the lungs is through coughing as it
becomes more difficult for the individual to breathe. As the lungs are becoming more filled, there is
less space for oxygen to be absorbed into the body and this could lead to further complications as
the body is unable to transport as much oxygen rich blood to its major organs.
For groups such as babies, young children, the elderly, smokers or those with a pre-existing lung
condition or weakened immune system, hospital treatment may be necessary. For those with a
milder form of pneumonia, it may be possible to treat the condition at home with a course
of antibiotics.
63
KERANGKA SYNTHESIS
Masuknya bakteri ke TR
(inhalasi, haematogen, aspirasi)
Mechanisme pertahanan diaktivkan Ternyata bakteri lebih kuat
Kehilangan effektivitas mechanisme pertahanan
Mengenai bagian steril dari TR (paru-paru)
Masuk ke alveoli
Multiplikasi
Kolonisasi Irritasi
Infeksi Mengeluarkan toxin Goblet cell
Inflammasi Okklusi jalan napas Mukus
Exudat Vasodilasi STTL Aktivasi receptor batuk
Blood flow Batuk Rhonchi basal nyaring
Fluid leakage + protein Pyrogen
Akummulasi cairan oedema Perubahan set point di hypothalamus
Mengisi Saccus alveolaris Febris
Restriksi Infiltrar parahilair
Hypoxia
Kompensasi tubuh
Dyspnoea Napas cuping hidung Hyperventilasi Retraksi interkostal
Hepatisasi
64
KESIMPULAN
Zumi, 9 bulan laki-laki, menderita bronchopneumonia infans dengan culprit paling possible
Streptococcus pneumoniae dengan gejala klinik dyspnoea, febris, dan batuk.
65
DAFTAR PUSTAKA
http://nurseonlineph.blogspot.com/2012/04/pathophysiology-of-pneumonia.html, diakses 26 Maret
2014, circa 09.00 WIB.
http://diseases-conditions.blurtit.com/33178/what-are-the-stages-of-pneumonia-, diakses 28 Maret
2014, 04.47 WIB.
http://www.gpnotebook.co.uk/simplepage.cfm?ID=1644560425&linkID=26813&cook=no, diakses
28 Maret 2014, 04.47 WIB.
Dorland, W. A. Newman.. 2002. Kamus Kedokteran Dorland edisi 29. Jakarta: EGC
Guyton dan Hall. 2003.Fisiologi kedokteran. Jakarta : EGC
Mansjoer, Arif, dkk. 2000. Kapita Selekta Kedokteran Edisi Ketiga Jilid 2. Jakarta: Media
Aesculapius
Price, Sylvia Anderson & Wilson. 2006. Patofisiologi: Konsep Klinis Proses-Proses Penyakit.
Jakarta: EGC
Sherwood, Lauralee. 2003. Fisiologi Manusia dari Sel ke Sistem. Jakarta: EGC
Staf pengajar IKA FK UI. 2005. Buku Kuliah Ilmu Kesehatan Anak. Jakarta: Infomedika.
Suyono, Slamet ,dkk. 1996. Buku Ajar Ilmu Penyakit Dalam. Jakarta: Balai penerbit FKUI
66
LAPORAN TUTORIAL BLOK XVI SKE C
“BRONCHOPNEUMONIE PAEDIATRIK-INFANT”
Disusun oleh
Kelompok IV
1. Preetibah Ratenavelu 04101401136
2. Maya Chandra Dita 04121401038
3. Fachra Afifah Aliati 04121401041
4. Octavia Ukhti Prakarsih 04121401052
5. Putri Septi Ramasari 04121401060
6. Vivi Miliarti 04121401061
7. Ayu Aprilisa Dahni P 04121401062
8. Iqbal Habibie 04121401063
9. Timotius Wira Yudha 04121401065
10. Owen Hu 04121401066
11. Ayu Novalia 04121401072
12. R Satria Surya C 04121401084
13. Ratri Shintya Dewi 04121401095
FAKULTAS KEDOKTERAN UNSRI
PALEMBANG 2014
67
KATA PENGANTAR
Penulis memuji dan bersyukur kepada Tuhan Yang Maha Esa atas selesainya laporan
Tutorial Blok XVI Skenario C ini. Penulis juga berterima kasih kepada seluruh pihak yang
mendukung terselesaikannya hasil diskusi ini, yang mohon maaf tidak bisa disebutkan satu-persatu.
Bronchopneumonie adalah penyakit yang sering mengenai anak-anak usia dini, apalagi juga
pada infant. Morbiditasnya dan child-year kenanya masih tinggi di Indonesia. Paparan dini terhadap
kasus ini akan membuat belajar menjadi lebih mudah.
Penulis menyadari bahwa hasil diskusi ini masih jauh dari apa yang dirasa cukup.
Kekurangan dari hasil diskusi ini akan diperbaiki di kala mendatang.
Penulis