efek histrectomy.pdf
-
Upload
santa-maria-pangaribuan -
Category
Documents
-
view
214 -
download
0
Transcript of efek histrectomy.pdf
-
8/10/2019 efek histrectomy.pdf
1/7
Arch Gynecol Obstet (2010) 282:97102
DOI 10.1007/s00404-010-1370-z
1 3
REPRODUCTIVE MEDICINE
EVect of previous uterine surgery on the operative hysteroscopic
outcomes in patients with reproductive failure:
analysis of 700 cases
Tarek Shokeir Yaser Abdel-Dayem
Received: 16 October 2009 / Accepted: 12 January 2010 / Published online: 3 February 2010
Springer-Verlag 2010
Abstract
Objective To determine the eVect of previous uterine sur-
gery according to whether the uterine cavity is opened or
not on the operative outcomes in a series of women under-
going surgical hysteroscopy guided by concomitant diag-
nostic laparoscopy for management of reproductive failure.
Methods Records of 700 consecutive major hysteroscopic
surgical procedures guided by concomitant diagnostic lapa-
roscopy and performed for women with previous pelvic
surgery were reviewed. All women were suVering from
reproductive failure. Patients were categorized according to
whether the uterine cavity was opened or not and according to
the type of hysteroscopic procedure performed. Analysis of
overall previous uterine surgery of any type combined and of
individual matched types of hysteroscopic procedure sepa-
rately was done. Patient age, American Society of Anesthesi-
ologists (ASA) patient classiWcation, surgical history,
perioperative change in serum sodium concentration and
hemoglobin level, Xuid balance, transfusion rate, rate of failed
hysteroscopic procedure, operative hysteroscopic time, com-
plication rate and hospital stay were assessed in each patient.
Results Of the 700 patients, 366 (52%) had never under-
gone uterine surgery, 105 (15%) had a history of uterine
surgery with cavity opened and 229 (33%) had uterine sur-
gery with cavity not opened. Overall previous uterine sur-
gery of any type was associated with an increased age, and
higher ASA score (P = 0.001). A history of uterine surgery
with cavity opened was associated with increased operative
time (P = 0.03) and increased hospital stay (P = 0.02).
No patients have required a transfusion. DiVerences in
perioperative serum sodium concentration and hemoglobin
level, the complication and failure rates in patients with and
without a history of uterine surgery did not attain signiW-
cance. Outcomes analysis of individual matched types
of hysteroscopic surgery showed similar results except for
hysteroscopic metroplasty. In these cases, previous uterine
surgery was not associated with increased age or ASA
score.
Conclusion Previous uterine surgery among young
women with reproductive failure whether the uterine cavity
is opened or not does not appear to aVect adversely the per-
formance and safety of subsequent major surgical hysteros-
copy guided by concomitant diagnostic laparoscopy.
Keywords Reproductive failure Hysteroscopic surgery
Uterine surgery
Introduction
Pelvic surgery, whether the uterine cavity is opened or not,
promotes the formation of adhesions. Autopsy studies show
intrapelvic adhesions in 7590% of patients with a history
of uterine surgery. In contrast, adhesions develop in only
10% of patients with no history of surgery [13]. In com-
pletely unpredictable fashion, adhesions may obscure tissue
planes, alter the position of anatomical landmarks and aYx
bowel to the anterior abdominal wall, making subsequent
laparoscopic access performed concomitantly during major
hysteroscopic surgical procedures subjectively more diY-
cult [4]. However, the role of adhesions in this regard
among women with reproductive failure remains controver-
sial. We have recently published a large retrospective
cohort study to better understand the risk of intraabdominal
T. Shokeir (&) Y. Abdel-Dayem
Department of Obstetrics and Gynecology,
Mansoura Faculty of Medicine,
Mansoura University Hospital, Mansoura, Egypt
e-mail: [email protected]
http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?- -
8/10/2019 efek histrectomy.pdf
2/7
98 Arch Gynecol Obstet (2010) 282:97102
1 3
adhesions at surgical laparoscopy for infertility. We reach to
the conclusion that preoperative risk factors for intraabdominal
adhesions should not contraindicate surgical laparoscopy
for infertility [5].
The severity and pattern of intrauterine adhesion (IUA)
development after uterine surgery are generally unrelated to
the type or number of previous uterine surgeries or whether
the uterine cavity is opened or not [6]. Previous uterine sur-gery may aVect subsequent hysteroscopy in several diVer-
ent ways. DiYcult uterine entry together with improper
uterine distention may hinder instrument manipulation dur-
ing the procedure. Adhesion lysis may increase the risk of
bleeding and uterine wall injury. In addition, the distortion
of normal anatomy may decrease the visibility during the
procedure. Concerns remain about potential adverse conse-
quences, such as morbidity and complications in some
cases. Technical considerations such as these have
prompted many initial reports in the infertility literature
citing previous uterine surgery, especially those with the
uterine cavity opened, as a potential risk factor to major
surgical hysteroscopy for the management of infertility and
reproductive failure [7, 8].
Because of the rapidity with which hysteroscopy guided
by concomitant laparoscopy has developed into an integral
and widely used component of surgery among women with
reproductive failure, evaluating the relative safety and
eYcacy of performing major surgical hysteroscopy in these
women with a history of uterine surgery represents a partic-
ular salient issue. Such information would prove useful in
developing suitable plans of care and counseling patients
on appropriate surgical options. However, there is a paucity
of published data assessing the potentially negative impact
of previous uterine surgery among patients with reproduc-
tive failure on the overall outcome of subsequent surgical
hysteroscopy for the management of these cases. Therefore,
the aim of this study is to determine the eVect of previous
uterine surgery according to whether the uterine cavity is
opened or not on the operative outcomes in a large series of
women with reproductive failure undergoing surgical hys-
teroscopy guided by concomitant diagnostic laparoscopy.
Materials and methods
From 2001 to 2008, the records of 700 consecutive major
hysteroscopic surgical procedures guided by concomitant
diagnostic laparoscopy and performed at a single tertiary
referral center (Mansoura University Hospital, Mansoura,
Egypt) were reviewed. All women had previous pelvic sur-
gery and, were suVering from reproductive failures (infer-
tility and/or recurrent pregnancy losses). Age, American
Society of Anesthesiologist (ASA) classiWcation, surgical
history, operative hysteroscopic time, pre-and postopera-
tive change in serum sodium concentration and hemoglobin
level, transfusion rate, failure rate, major complication rate
and hospital stay were assessed in each patient. In this
paper, major complications are deWned as any anesthetic
complications and/or those requiring laparotomy for man-
agement. Further, failed hysteroscopic procedure is deWned
as failure of uterine entry together with improper uterine
distention.Patients with previous pelvic surgery were grouped into
one of three categories as one-none uterine (Group A), two-
uterine with cavity opened (Group B) and three-uterine
with cavity not opened (Group C). Previous uterine surgery
was deWned as any type of open or closed uterine surgery
with the potential to cause intra-uterine adhesions, includ-
ing abdominal myomectomy, cesarean section, abdominal
repair of uterine perforation and abdominal operations for
correction of double uterus. Manipulated uterine cavitary
procedures, such as surgical or suction evacuations, and
dilatation and curettage (D & C) were considered also as
previous uterine surgery in our series. Previous none-uter-
ine surgery was deWned as any type of open abdominal,
Xank or pelvic surgery with the potential to cause intra-
abdominal and/or pelvic adhesions, including adnexal
surgery, gastrointestinal procedures, cholecystectomy,
urological procedures and appendectomy. Inguinal proce-
dures, superWcial abdominal surgery and endoscopic gas-
trointestinal, gynecologic or urological procedures were not
considered open intraabdominal surgery. Thus, unless
patients had undergone procedures that qualiWed as uterine
surgery, they were classiWed as having undergone non-uter-
ine surgery (Group A). These classiWcation criteria conform
to previously established standards in surgical and gyneco-
logic reports [5, 6, 9].
Patients were also categorized by the type of hystero-
scopic procedure performed for management of reproduc-
tive failure. To minimize any potential bias introduced by
variations in surgical technique among individual cases 399
cases in whom no associated laparoscopic surgical inter-
vention was performed were selected for further outcome
analysis. These include hysteroscopic lysis of IUAs in 116,
hysteroscopic polypectomy in 64, hysteroscopic myomec-
tomy in 131 and hysteroscopic metroplasty in 88. At our
institution, each of these four types is performed via a stan-
dard monopolar electrosurgical resectoscopic technique
(26 Fr resectoscope, Karl Storz, Germany) and using
glycine (1.5%) as a Xuid uterine distention medium. Fluid
balance was assessed using electronic suction irrigation
system (Endomat, Karl Storz, Germany). All hysteroscopic
operations were performed by the same surgeon.
In this article, deWnite criteria for each hysteroscopic
procedure have to be fulWlled for each patient before inclu-
sion in our study. Hysteroscopic myomectomy is deWned
as any procedure that primarily involves complete excision
http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?- -
8/10/2019 efek histrectomy.pdf
3/7
Arch Gynecol Obstet (2010) 282:97102 99
1 3
of a single or multiple submucous myomas, largest being
-
8/10/2019 efek histrectomy.pdf
4/7
100 Arch Gynecol Obstet (2010) 282:97102
1 3
Change in serum sodium concentration and hemoglobin
level was slightly higher in the groups with a history of
uterine surgery whether the uterine cavity was opened or
not versus no previous uterine surgery, but this diVerence
did not attain statistical signiWcance in the analysis. The
same Wnding was true for the complication rate and the rate
of failed hysteroscopic procedure. No patients in our series
have required a transfusion.
We also determined the outcome of the four speciWc hys-
teroscopic procedures in the groups with a history of uter-
ine surgery whether the cavity was opened or not versus no
previous surgery. As in the groups overall, there were no
observed diVerences in patients with uterine surgery versus
those with no history of uterine surgery for any measured
outcomes. Data regarding the failure rate (P = 0.25), com-
plication rate (P = 0.135), changes in hemoglobin and
serum sodium levels (P = 0.99 and P = 0.99, respectively),
hospital stay (P = 0.77) or operative hysteroscopic time
(P = 0.99) were comparable. However, for cases with hys-
teroscopic metroplasty previous uterine surgery was not
associated with increased age or ASA score.
On separate analysis of the individual matched types of
hysteroscopic surgery, diVerences in perioperative serum
concentration and hemoglobin levels, operative hystero-
scopic time, Xuid balance, the complication and failure
rates in patients with and without a history of uterine sur-
gery did not attain statistical signiWcance (P > 0.05).
Discussion
Hysteroscopy guided by concomitant laparoscopy has
assumed as an integral role within the reproductive logical
surgical armamentarium [12]. The importance of individu-
ally counseling patients with reproductive failure on the
potential risks of major hysteroscopic surgery guided by
laparoscopy, such as high operative blood loss, conversion
to an open procedure and operative complications, is para-
mount. Still, there remains a dearth of published material
on factors that may potentially inXuence patient outcome
after surgical hysteroscopy for reproductive failure, most
notably the surgical history. Although some groups main-
tain that previous uterine surgery remains a highly potential
risk factor to surgical hysteroscopy in this select patient
group, there are no supporting series in the recent literature
[8, 13]. To the best of our knowledge, this is the Wrst study
evaluating the eVect of previous uterine surgery according
to whether the uterine cavity is opened or not on the opera-
tive outcome in a large series of women with reproductive
failure who underwent major hysteroscopic surgery guided
by concomitant diagnostic laparoscopy.
The analysis of the current study was limited to four
common procedures in which no associated laparoscopic
operative intervention was performed, namely hystero-
scopic adhesiolysis, hysteroscopic myomectomy, hystero-
scopic metroplasty and hysteroscopic polypectomy. It was
done by the same surgeon and nearly the same technique
was performed to minimize the bias introduced by many
attending surgeons who performed the same type of surgery
using diVerent techniques in the individuals. Such variabil-
ity makes comparing operative time and the other outcome
parameters problematic. They also present a representative
sample of cases with diVerent levels of technical complex-
ity. Notably, the distribution of patients among the three-
uterine surgical history categories was the same for these
four procedures together with the series overall.
Patients with a history of previous uterine surgery of any
type were older. This Wnding is not surprising because older
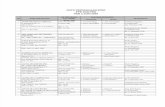
Table 2 Patient characteristics and operative hysteroscopic outcomes in 399 selected cases
Cases with no associated laparoscopic interventions
NSnon-signiWcant
* The Pvalues are for comparisons of groups B and C versus group A
Parameter Previous uterine surgery P*
None
(Group A; n = 206)
Cavity opened
(Group B; n = 53)
Cavity not opened
(Group C; n = 140)
Mean age SD 23 5.1 29.2 6.1 35.7 5.9 0.0001
Mean ASA score SD 1.97 0.82 2.30 0.66 2.40 0.65 0.0001
Mean hospital stay (days) 1.0 1.9 4.2 1.6 2.9 1.8 0.02
Mean operative time in minutes SD (min) 23 1.0 46 4.0 35 3.0 0.03
Mean change in serum Na SD (mEq/L) 0.06 3.63 0.64 3.56 0.60 3.50 NS
Mean fall in hemoglobin SD (g/dL) 0.67 0.62 0.82 0.78 0.84 0.70 NS
Percentage of complications 1.4 3.2 3.0 NS
Percentage of failed hysteroscopic procedure 1.2 2.3 2.2 NS
http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?- -
8/10/2019 efek histrectomy.pdf
5/7
Arch Gynecol Obstet (2010) 282:97102 101
1 3
patients lived longer and, therefore, are more likely to have
undergone surgery. They are also more likely to manifest
health problems that require surgical interventions. In fact,
patients with a history of uterine surgery in this series also
had a higher ASA score. A high ASA score reXects a
greater degree of medical co-morbidity and, therefore,
increased operative risk [1214]. In our series, outcome
analysis of individual matched types of hysteroscopic sur-gery showed similar results except for hysteroscopic metro-
plasty. In these cases, previous uterine surgery was not
associated with increased age or ASA score. In fact, we do
not have a possible explanation for this Wnding. However, a
large number of such cases in our series were presented
with recurrent miscarriage and bad obstetric history rather
than inability to conceive. Accordingly, we can assume that
previous uterine surgery as a risk factor alone cannot be
contributed to a higher morbidity, particularly there was no
signiWcant diVerence in the serum sodium concentration
and hemoglobin level, complication or failure rates in these
groups.
Previous uterine surgery with the uterine cavity opened
was associated with longer operative time and increased
hospital stay when compared with no history of surgery and
uterine surgery with the uterine cavity not opened. Longer
operative hysteroscopic time and relative increased compli-
cation rates (although statistically not signiWcant) were
likely associated with the increased diYculty and complex-
ity of hysteroscopic surgery in an anatomical region previ-
ously subjected to operative dissection. The reason for the
increased hospital stay in this particular group is unclear.
However, most of these cases were older and had a higher
ASA score. Therefore, we can speculate that in patients
undergoing surgical hysteroscopy guided by concomitant
laparoscopy, rather than a diagnostic procedure, increased
operative time independently predicted a longer hospital
stay.
In our results, the change in serum sodium concentration
and hemoglobin level as well as the complication rates
were slightly higher in the groups with a history of uterine
surgery whether the uterine cavity was opened or not versus
no previous uterine surgery but this diVerence did not attain
statistical signiWcance in the analysis. Association of con-
comitant IUA (more than stage I IUA), weakness of uterine
musculature, and complexity of surgical hysteroscopic
procedures performed in these cases could be a possible
explanation. However, a prospective randomized study
is required before any conclusions can be drawn regarding
this issue.
In our analysis, the most common previous uterine sur-
geries were not correlated to outcomes. This would have
been particularly interesting to know whether a higher inci-
dence of endoscopic reproductive surgery was performed
for patients with certain types of previous uterine surgery.
In surgical literature, however, it is well known that the
severity and pattern of adhesion development after abdomi-
nal surgery are generally unrelated to the type or number of
previous surgeries [35].
In this cohort study of combined surgical hysteroscopy
and diagnostic laparoscopy, successful laparoscopic access
to the peritoneal cavity was attained in all cases. Because
the natural history of formation of diVerent intraabdominaladhesions in relation to the presence or absence of preoper-
ative risk factors could not be determined exactly [6, 7], in
our study, no attempt was made to correlate the preopera-
tive risk factors of previous uterine or pelvic surgery with
the estimated adhesion severity seen at laparoscopy.
Rather, we analyzed the risk of previous uterine surgery
according to whether the uterine cavity is opened or not on
surgical hysteroscopy guided by concomitant diagnostic
laparoscopy.
The present study does provide some important issues
regarding the eVect of previous uterine surgery on the oper-
ative outcome in a large series of women suVering from
reproductive failure who undergo surgical hysteroscopy.
Accordingly, we support the concept that women with
reproductive failure and with a history of uterine surgery,
whether the uterine cavity is opened or not, may be coun-
seled that subsequent concomitant hysteroscopic and lapa-
roscopic procedures can be performed without signiWcantly
increased risk of operative blood loss, complications or fail-
ure. However, older patients with multiple co-morbidities
should be advised that there may be a higher probability of
increased operative risk and hospital stay.
From this paper, we can conclude that previous uterine
surgery whether the uterine cavity is opened or not among
young women with reproductive failure does not appear to
aVect adversely the performance or safety of subsequent
major surgical hysteroscopy guided by concomitant lapa-
roscopy.
ConXict of interest statement None.
References
1. Weibel MA, Majno G (1973) Peritoneal adhesion and their rela-
tion to abdominal surgery: a postmortem study. Am J Surg126:345
2. Davey AK, Maher PJ (2007) Surgical adhesions : a timely update,
a great challenge for the future. J Minimal Invasive Gynecol
14:1522
3. Baakdah H, Tulandi T (2005) Adhesion in gynecology complica-
tion, cost and prevention: a review. Surg Technol Int 14:185190
4. Brill AI, Nezhat F, Nezhat CH, Nezhat C (1995) The incidence of
adhesions after prior laparoscopy: a laparoscopic appraisal. Obstet
Gynecol 85:269
5. Shokeir T, Badawy A, Abo-Hashem H (2008) Preoperative risk
factors for intraabdominal adhesions should not contraindicate
surgical laparoscopy for infertility. JSLS 12:267272
http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?-http://-/?- -
8/10/2019 efek histrectomy.pdf
6/7
102 Arch Gynecol Obstet (2010) 282:97102
1 3
6. Gavai M, Berkes E, Fekete T, Lazar L, Takacs ZF, Papp Z (2008)
Analysis of perioperative morbidity according to whether the
uterine cavity is opened or remains closed during abdominal
myomectomy: results of abdominal myomectomy. Clin Exp Obstet
Gynecol 35:107112
7. Nappi C, Di Spiezio Sardo A, Greco E, Guida M, Bettocchi S,
Bifulco G (2007) Prevention of adhesions in gynecologic
endoscopy. Hum Reprod Update 13:379394
8. Christianson MS, Barker MA, Lindheim SR (2008) Overcoming
the challenging cervix: techniques to access the uterine cavity.
J Low Genit Tract Dis 12:2431
9. Schirmer BD, Dix J, Schmieg RE Jr, Aguilar M, Urch S (1995)
The impact of previous abdominal surgery on outcome following
laparoscopic cholecystectomy. Surg Endosc 9:1085
10. Wamsteker K, deKruif J (1993) Transcervical hysteroscopic
resection of submucous Wbroids for abnormal uterine bleeding:
results regarding the degree of intramural extension. Obstet Gynecol
82:736740
11. The American Fertility Society (1988) The American Fertility Soci-
ety ClassiWcation of adnexal adhesions, distal tubal occlusion, tubal
occlusion secondary to tubal ligation, tubal pregnancies, Mullerian
anomalies and intrauterine adhesions. Fertil Steril 49:944955
12. Kaminski P, Gajewska M, Wielgos M, Szymusik I, Ziolkowska K,
Bartkowiak R (2006) The usefulness of laparoscopy and hysteros-
copy in the diagnosis and treatment of infertility. Neuro Endocri-
nol Lett 27:813817
13. Bergeron ME, Beaudet C, Bujold E, Rheaume C, Quellet P,
Laberge P (2009) Glycine absorption in operative hysteroscopy:
the impact of anesthesia. Am J Obstet Gynecol 331:e1e5
14. Serocki G, Hanss R, Bauer M, Scholz J, Bein B (2009) The gyne-
cological TURP syndrome: severe hyponatremia and pulmonary
edema during hysteroscopy. Anaesthesist 58:3034
-
8/10/2019 efek histrectomy.pdf
7/7
Copyright of Archives of Gynecology & Obstetrics is the property of Springer Science & Business Media B.V.
and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright
holder's express written permission. However, users may print, download, or email articles for individual use.