Dengue Feverdownloads.hindawi.com/journals/focusissues/706761.pdf · 2012. 9. 11. · Editorial...
Transcript of Dengue Feverdownloads.hindawi.com/journals/focusissues/706761.pdf · 2012. 9. 11. · Editorial...

Dengue Fever
Journal of Tropical Medicine

Dengue Fever

Journal of Tropical Medicine
Dengue Fever

Copyright © 2012 Hindawi Publishing Corporation. All rights reserved.
This is a focus issue published in “Journal of Tropical Medicine.” All articles are open access articles distributed under the Creative Com-mons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original workis properly cited.

Editorial Board
Hans Peter Beck, SwitzerlandSukla Biswas, IndiaJoe Blaney, USAIb Christian Bygbjerg, DenmarkMaureen Coetzee, South AfricaCarlos E. P. Corbett, BrazilRodrigo Corra-Oliveira, BrazilLuis E Cuevas, UKAditya Prasad Dash, IndiaI. M. Elhassan, Saudi ArabiaBlaise Genton, Switzerland
Jean-Paul Gonzalez, FranceJoseph Hamburger, IsraelLukasz Kedzierski, AustraliaSusana A. Laucella, ArgentinaPeter Leggat, AustraliaSylvie Manguin, FranceWilbur Milhous, USALouis H. Miller, USAMathieu Nacher, French GuianaC. F. Ockenhouse, USAKenneth E. Olson, USA
John Henry Ouma, KenyaGerd Pluschke, SwitzerlandS. Pukrittayakamee, ThailandR. G. Ridley, USAGeorges Snounou, FrancePradya Somboon, ThailandShyam Sundar, IndiaMarcel Tanner, SwitzerlandThomas R. Unnasch, USADina Vlachou, UK

Contents
Increasing Role of Roof Gutters as Aedes aegypti (Diptera: Culicidae) Breeding Sites in Guadeloupe(French West Indies) and Consequences on Dengue Transmission and Vector Control, Joel Gustave,Florence Fouque, Sylvie Cassadou, Lucie Leon, Gabriel Anicet, Cedric Ramdini, and Fabrice SonorVolume 2012, Article ID 249524, 3 pages
Peritoneal Dialysis in Dengue Shock Syndrome May Be Detrimental, Chulananda D. A. Goonasekera,Bhagya G. Thenuwara, and Ranjith P. V. KumarasiriVolume 2012, Article ID 917947, 5 pages
Diffusion Pattern and Hotspot Detection of Dengue in Belo Horizonte, Minas Gerais, Brazil,Jose Eduardo Marques Pessanha Pessanha, Waleska Teixeira Caiaffa, Maria Cristina de Mattos Almeida,Silvana Tecles Brandao, and Fernando Augusto ProiettiVolume 2012, Article ID 760951, 11 pages
Comparative Evaluation of Permissiveness to Dengue Virus Serotype 2 Infection in Primary RodentMacrophages, Jeanette Prada-Arismendy, Veronica Rincon, and Jaime E. CastellanosVolume 2012, Article ID 950303, 7 pages
Dengue Virus Entry as Target for Antiviral Therapy, Marijke M. F. Alen and Dominique ScholsVolume 2012, Article ID 628475, 13 pages
Molecular Typing of Dengue Virus Circulating in Kolkata, India in 2010, Arindam Sarkar,Debjani Taraphdar, and Shyamalendu ChatterjeeVolume 2012, Article ID 960329, 5 pages
Effectiveness of Space Spraying on the Transmission of Dengue/Dengue Hemorrhagic Fever (DF/DHF)in an Urban Area of Southern Thailand, Suwich Thammapalo, Supaporn Meksawi,and Virasakdi ChongsuvivatwongVolume 2012, Article ID 652564, 7 pages

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 249524, 3 pagesdoi:10.1155/2012/249524
Research Article
Increasing Role of Roof Gutters as Aedes aegypti (Diptera:Culicidae) Breeding Sites in Guadeloupe (French West Indies) andConsequences on Dengue Transmission and Vector Control
Joel Gustave,1 Florence Fouque,2 Sylvie Cassadou,3 Lucie Leon,3
Gabriel Anicet,1 Cedric Ramdini,1 and Fabrice Sonor1
1 Service de Lutte Anti-vectorielle, Agence Regionale de la Sante de Guadeloupe, Le Raizet, 97110 Les Abymes, Guadeloupe2 Institut Pasteur de la Guadeloupe, Laboratoire d’Entomologie Medicale, Morne Joliviere, BP484, 97183 Les Abymes, Guadeloupe3 Cellule Inter Regionale d’Epidemiologie des Antilles et de la Guyane (CIRE), Agence Regionale de Sante de Guadeloupe, Bisdary,Rue des Archives, 97113 Gourbeyre, Guadeloupe
Correspondence should be addressed to Florence Fouque, [email protected]
Received 14 October 2011; Revised 27 January 2012; Accepted 30 January 2012
Academic Editor: Thomas R. Unnasch
Copyright © 2012 Joel Gustave et al. This is an open access article distributed under the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
During the past ten years, the islands of Guadeloupe (French West Indies) are facing dengue epidemics with increasing numbers ofcases and fatal occurrences. The vector Aedes aegypti is submitted to intensive control, with little effect on mosquito populations.The hypothesis that important Ae. aegypti breeding sites are not controlled is investigated herein. For that purpose, the roof guttersof 123 houses were systematically investigated, and the percentage of gutters positive for Ae. aegypti varied from 17.2% to 37.5%,from humid to dry locations. In the dryer location, most of houses had no other breeding sites. The results show that roof guttersare becoming the most important Ae. aegypti breeding sites in some locations in Guadeloupe, with consequences on denguetransmission and vector control.
Dengue fever (DF) is the most important arthropod-bornetransmitted disease worldwide with 50 to 100 millionDF infections, 500,000 dengue hemorrhagic fever (DHF)hospitalized cases, and 20,000 to 25,000 deaths [1]. In theAmericas, DF and DHF are endemic, and in 2010 more than50 countries reported 1,663,276 clinical DF cases, 48,954DHF cases, 1,194 deaths, and the cocirculation of the fourdengue serotypes [2]. Though suspected to be present since along time, dengue was first detected in Guadeloupe (FrenchWest Indies) around the 80s [3]. The disease was consideredrare until the first DEN-2 epidemic in 1992–1994 [4] andthe first report of DHF cases in 1995 [5]. The last epidemicstarted at the end of 2009 and continued all 2010 withabout 40,000 clinical DF cases, 418 severe DF cases, and5 deaths [6]. This epidemic was the largest one reportedfrom Guadeloupe. Dengue viruses are transmitted by themosquitoes Aedes aegypti L. 1762, and because no denguevaccine is available, the control of Ae. aegypti populations isthe only tool to avoid further DF and DHF epidemics. Untilrecently, the main Ae. aegypti breeding sites in Guadeloupe
were the 200 liters drums in urban and periurban situations[4]. The roof gutters were reported as Ae. aegypti breedingsites since a long time, but their mosquito production wasconsidered negligible compared to other ground breedingsites [7]. Consequently roof gutters are often neglected in theroutine survey of the mosquitoes breeding sites and are notincluded in the estimation of the Breteau Index [8]. However,an unpublished survey carried out in Guadeloupe in 1998found that about 30% of roof gutters were positive for Ae.aegypti and could produce huge numbers of mosquitoes.Roof gutters are still functioning when all accessible breedingsites have been controlled and may represent a reservoir forAe. aegypti. To better estimate the importance of roof guttersas breeding sites for Ae. aegypti populations in Guadeloupe,a survey was carried out in 2006 in 3 different environmentalareas of Guadeloupe.
The groups of houses investigated were chosen in resi-dential areas situated in different climatic zones of Guade-loupe: (i) in the city of Saint-Francois situated at the easternextremity of Grande-Terre (hot and dry climate, annual

2 Journal of Tropical Medicine
rainfall 1,300 mm, and mean annual temperature 25.6◦C),(ii) in the village of Saint-Claude situated in the inlandof Basse-Terre (cool and humid climate, annual rainfall4,463 mm, and mean annual temperature 24.2◦C), (iii) in thecity of Baie-Mahault situated in the northern part of Basse-Terre (intermediate climate, mean annual rainfall 1,679 mm,and mean annual temperature 26.4◦C). The climatic datawere provided by the French meteorological services. Foreach location, 40 houses (representing about 10% of the4,000 houses reported for each city) were selected randomlyto have their roof gutters investigated in January, February,and May 2006 in Saint-Francois, Baie-Mahault, and Saint-Claude, respectively. The presence of water and the mosquitoabundances (larvae and pupae) in the roof gutters wereestimated by direct observation, and samples were collectedfor mosquito identification. The height, length, form andmaterial of the roof gutter, and the presence of vegetalelements, detritus, and/or sediments were also reported. Themosquitoes were kept until adult emergence for their speciesidentification. The relation between Ae. aegypti larvae, andpupae presence and other water parameters were analyzedwith the Fisher exact test.
Among the 123 houses investigated, representing 520 mof roof gutters, 81 (65.8%) contained water, 35 (28.4%)were positive for Ae. aegypti larvae and 20 (16.3%) werepositive for Ae. aegypti pupae. All positive roof gutters werebreeding Ae. aegypti individuals. Culex sp. larvae were foundbreeding with Ae. aegypti in only one gutter. Larvae ofCeratopogonidae of the genus Dasyhelea were also observedin several roof gutters. The abundance of Ae. aegypti larvaeand pupae in roof gutters was highly variable, and importantdifferences were observed between the studied sites, with ahigh percentage of positive roof gutters in Saint-Francois:67% positive for larvae and 37% positive for pupae and alower percentage in Saint-Claude: 27% positive for larvaeand 17% positive for pupae. The dryer study site of Saint-Francois had the highest percentage of roof gutters positivefor Ae. aegypti larvae and pupae, the location of Baie-Mahault with intermediate climate had the intermediatevalue, and the more humid study site of Saint-Claude had thelowest percentage of positive roof gutters. This finding wasin agreement with previous observations (unpublished data)showing that roof gutters could serve as breeding “reservoirs”for Ae. aegypti in the dryer locations in Guadeloupe. Thehighest numbers of Ae. aegypti larvae and pupae were foundin roof gutters containing water with sediments and waterwith vegetal detritus. The exact test of Fisher estimates showthat the presence of Ae. aegypti pupae in roof gutters wassignificantly different between roof gutters with “clean” waterand roof gutters with sediments and/or vegetal detritus (P =0.0305, OR = 8.8 for sediments, P = 0.0135, OR = 11for vegetal detritus). For Ae. aegypti larvae no significantdifference was found, but the presence of sediments and/orvegetal was reported with the highest abundance of Ae.aegypti larvae (Figure 1). For densities higher than 100larvae/liter, the percentage of positive roof gutters containingsediments and/or vegetal detritus was about three to fourtimes higher than the percentage of positive roof gutterswith “clean” water. This finding indicates that Ae. aegypti
R2 = 0.8344
R2 = 0.7218
R2 = 0.9811
0
20
40
60
80
1 2 3
No larvaeLess than 10 larvae/liter
Between 10 and 100 larvae/literMore than 100 larvae/liter
(%)
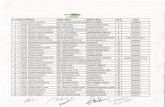
Figure 1: Graphical representation of the abundance of Ae. aegyptilarvae found in the roof gutters according to the type of waterduring investigations carried out in Guadeloupe between Januaryand May 2002. (Horizontal axis: 1 = clear water, 2 = water withsediments, 3 = water with vegetal detritus).
abundance is increasing with the presence of sedimentsand/or vegetal detritus (Figure 1), and on the contrary theabsence of Ae. aegypti larvae is found more often in “clean”waters. The mean size of the positive roof gutters was about6 m per house.
The main conclusion of this survey is the increasingimportance of roof gutters as Ae. aegypti breeding sitesin some locations in Guadeloupe. This type of breedingsites though recognized since about 50 years [7] is oftenneglected in the control operations due to the difficulty ofaccess and the low mosquito production. But, in Guadeloupethe situation is changing, although the survey was madeduring the dry season (from January to May), about two-third of the roof gutters contain waters and 44% werepositive for Ae. aegypti larvae. This type of containers wasthus representing kilometers of Ae. aegypti breeding sites.These results are in agreement with studies done in Australiawhere the production of Ae. aegypti by roof gutters wasestimated to account for 52.6% and 39.5% of the totalpopulation during wet and dry seasons, respectively, in urbanareas [9]. In the Americas, the oviposition of Ae. aegypti ingutters surrounding high-elevated apartments has also beenreported with consequences on dengue transmission [10].Unexpectedly, the highest percentage of positive roof gutterswas found in the driest area of Saint-Francois. This townwas an important dengue focus during the 2006-2007 and2009–2011 epidemics, but this town has one of the lowerBreteau Index of Guadeloupe. Our results show that theAe. aegypti densities in Saint-Francois are probably stronglyunderestimated, due to the absence of roof gutters investiga-tions during routine surveillance. It thus appears necessary tosystematically include roof gutters in the estimation of the Ae.aegypti indices. Following the present survey, the roof guttersBreteau indices of Saint-Francois, Baie-Mahault, and Saint-Claude were 40, 27, and 20, respectively. Furthermore, thepositive roof gutters must be treated as any other Ae. aegyptibreeding site. Another conclusion of the survey was the

Journal of Tropical Medicine 3
association between the presence of sediments and/or vegetaldetritus and the presence of Ae. aegypti in the roof gutters.The presence of vegetal detritus was significantly associatedwith the highest Ae. aegypti pupae densities pointing out therole of the roof gutters environment and exposition.
Finally, the increasing role of roof gutters as Ae. aegyptibreeding sites, demonstrated in this study, has consequenceson dengue transmission and prevention. Firstly, recom-mendations on the roof gutters construction (correct waterevacuation) and cleaning (suppression of tree branchesand other vegetal) must be implemented. Secondly, routinesurveillance and control of the roof gutters by the VectorControl Agencies are needed. Lastly, the presence of Ae.aegypti in the roof gutters must also be included in theinformation directed towards community participation, inparticular when dengue transmission is increasing or duringdengue epidemics.
Dengue viruses’ circulation in Guadeloupe has dramat-ically increased during the past years, and at the same timeurbanization is developing without any regards to diseasetransmission. Studies on the relation between housing, vec-tor development, diseases and community involvement arestrongly requested to better struggle against this mosquito-transmitted disease.
Conflict of Interests
No conflict of interests is declared.
Acknowledgments
The authors’ best thanks are due to Jean-Paul Delecolle forthe identification of the Ceratopogonidae and to the inhab-itants of the locations of Saint-Francois, Baie-Mahault, andSaint-Claude for their participation to the study. The studywas funded by the Direction de la Sante et du DeveloppementSocial (DSDS) of Guadeloupe, French Ministry of Health.
References
[1] D. J. Gubler, “Dengue/dengue haemorrhagic fever: history andcurrent status,” Novartis Foundation Symposium, vol. 277, pp.3–16, 2006.
[2] PAHO, “Number of Reported Cases of Dengue and SevereDengue (DS) in the Americas by Country: figures for 2010(to week noted by each country). Epidemiological Week /EW 52,” 2011, http://new.paho.org/hq/dmdocuments/2011/dengue cases 2010 May 20.pdf.
[3] F. X. Jousset, “Geographic Aedes aegypti strains and dengue-2 virus: susceptibility, ability to transmit to vertebrate andtransovarial transmission,” Annales de Virologie, vol. 132, no.3, pp. 357–370, 1981.
[4] J. Gustave, “The prevention of dengue in Guadeloupe,”Bulletin de la Societe de Pathologie Exotique, vol. 89, no. 2, pp.143–144, 1996.
[5] J. Nguyen, G. Sibille, F. Cazassus, R. Goursaud, and M. Strobel,“Dengue hemorrhagic fever : first case identified in Guade-loupe (FWI),” Medecine et Maladies Infectieuses, vol. 25, no.12, pp. 1223–1224, 1995.
[6] INVS, “Le point epidemiologique,” CIRE Antilles-Guyane, vol.2, pp. 1–2, 2011.
[7] M. E. Tinker, “Aedes aegypti larval habitats in Surinam,”Bulletin of the Pan American Health Organization, vol. 8, no.4, pp. 293–301, 1974.
[8] L. Sanchez, V. Vanlerberghe, L. Alfonso et al., “Aedes aegyptilarval indices and risk for dengue epidemics,” EmergingInfectious Diseases, vol. 12, no. 5, pp. 800–806, 2006.
[9] B. L. Montgomery and S. A. Ritchie, “Roof gutters: a keycontainer for Aedes aegypti and Ochlerotatus notoscriptus(Diptera: Culicidae) in Australia,” American Journal of TropicalMedicine and Hygiene, vol. 67, no. 3, pp. 244–246, 2002.
[10] D. D. Chadee, “Observations on the seasonal prevalence andvertical distribution patterns of oviposition by Aedes aegypti(L.) (Diptera: Culicidae) in urban high-rise apartments inTrinidad, West Indies,” Journal of Vector Ecology, vol. 29, no.2, pp. 323–330, 2004.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 917947, 5 pagesdoi:10.1155/2012/917947
Clinical Study
Peritoneal Dialysis in Dengue Shock SyndromeMay Be Detrimental
Chulananda D. A. Goonasekera, Bhagya G. Thenuwara, and Ranjith P. V. Kumarasiri
Department of Anesthesiology, Faculty of Medicine, University of Peradeniya, Peradeniya 20400, Sri Lanka
Correspondence should be addressed to Chulananda D. A. Goonasekera, [email protected]
Received 7 October 2011; Revised 8 January 2012; Accepted 9 January 2012
Academic Editor: Marcel Tanner
Copyright © 2012 Chulananda D. A. Goonasekera et al. This is an open access article distributed under the Creative CommonsAttribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work isproperly cited.
Dengue shock syndrome is the most severe form of Dengue that can be fatal. Nonresponders to standard therapy need intensivecare. This paper outlines the clinical features, complications, and outcomes of Dengue Shock Syndrome not responding to standardtherapies and needing supportive care in a tertiary referral intensive care unit of a developing country. Nearly one-third die within3 days of admission to ICU. Peritoneal dialysis predicts the worst outcomes.
1. Introduction
Dengue is an important arthropod-borne viral disease ofhumans [1]. Its presentation varies from a mild viralsyndrome to hemorrhagic fever and severe shock. Its severeforms (hemorrhagic fever and shock syndrome) may lead tomultiorgan involvement and death. Dengue Shock Syndrome(DSS) is characterized by a massive increase in systemiccapillary permeability with consequent hypovolemia [2]. Themortality rate in Dengue Shock Syndrome ranges from 6to 30 percent, most commonly reported in children. Fluidresuscitation is critical with added support for failing organs[3].
In the recent past, Sri Lanka has experienced a surge ofthe disease reaching epidemic proportions associated with aprobable change in the virus strain to a more virulent form[4, 5]. In this context we have also noted a rise in the numberof cases with severe forms of the disease needing intensivecare. The Peradeniya ICU is a tertiary referral centre and itattracts a large number of above patients with Dengue ShockSyndrome in the region who do not respond to standardtherapy with intravenous fluids, antibiotics, and supportivecare including inotropes.
2. Methods
We collected demographic data of all patients referred forintensive care between January 2009 and June 2010 (18
months) and analyzed their outcomes in relation to thecomplications of DSS that ensued during their ICU stayand the therapies given. The diagnosis of Dengue has beenestablished upon clinical grounds (WHO guidelines 2009)and treated accordingly by the referring physicians beforeadmission to the ICU. On admission to ICU, all have hadfever, vomiting 78%, abdominal pain 21%, cough 5%, andbody ache among 3% of cases. Eleven patients have hadserological tests and Dengue IgM was found to be positiveamongst 72% and IgG in 50% of the tested. They all havehad intravenous fluid therapies and antibiotics. During thecourse of therapy in ICU, 43.6% of cases received fresh frozenplasma, 21.8% cryoprecipitate, 32.7% blood, and 56.4%platelet transfusions. Furthermore, 36.4% of cases weremechanically ventilated for multiple reasons such as severerespiratory distress (FiO2 > 60%), RR > 40/min, myocardialfailure needing inotropes for persistent hypotension despiteadequate filling, that is, CVP above 12 cm of H2O. Thedecision for peritoneal dialysis was based on low urineoutput (<0.5 mL/kg/hour) detected over a period of time inan ICU as a trend despite resuscitation with fluids combinedwith a situation of fluid overload, high CVP, persistenthypotension, or severe ARDS. Neither the plasma creatinine(rather a delayed indicator of AKI) nor blood urea (notreliable in the presence of liver impairment) was used asa determining factor in implementing dialysis. Persistenthypotension in the presence of high CVP was interpretedas indication of myocardial involvement (with or without

2 Journal of Tropical Medicine
100908070605040302010
0
Cu
mu
lati
ve (
%)
0–5 6–10 11–15 16–20 21–40 41–60Age groups (years)
> 60
Figure 1: The cumulative age distribution of patients with Dengueshock syndrome needing intensive care.
Table 1: Was the death early or late in ICU?
Day No. of deaths %
1 08 50%
2 03 19%
3 03 19%
5 01 06%
15 01 06%
Total 16 100%
relative bradycardia, ECG changes) and was supported withinotropes, usually a combination of dobutamine and nor-adrenaline and with mechanical ventilation if oxygenationwas compromised.. Thus, our data is based on a group ofseverely ill patients diagnosed to be suffering from DengueShock Syndrome and continuing to deteriorate despiteintravenous therapies administered in the wards. Liver failureregime, that is, oral/NG metronidazole and lactulose wasintroduced in patients who were found to have raisedtransaminases. It should be noted that the number of ICUbeds available (10) in our hospital was approximately 1.5%of the total beds and this may have delayed the admission ofsome cases due to rationing.
3. Results
Between January 2009 and June 2010, 54 cases (25 male)diagnosed of Dengue Shock Syndrome were admitted fortreatment to the Peradeniya ICU, a tertiary referral center.Half of them were aged 20 or below as shown in Figure 1. Onadmission, all had received prior intravenous fluid therapies.Their mean (SD) PCV was 44.5% (5.5), WBC 7.7×109/L(4.6), Platelet count 22 109/L (17), respectively.
Of the 54, 16 died (mortality 29.6%). Most deaths (88%)occurred within 3 days of admission to the ICU (Table 1).The survivors needed intensive care for a median of 2 days(range 1–8) before being discharged to the referring wardsfor convalescence.
It is also noteworthy that 62.5% deaths occurred belowthe age 20 (see Table 2). Although we were unable to provethat risk of death was higher in children, a higher incidence
Table 2: Distribution of ICU deaths by age categories (∗1 missingdata).
Live discharges Deaths Total
≤20 years 16 10 26
>20 years 21 06 27
Total 37 16 53∗
χ2 = 1.66; df = 1; P = 0.198 (not significant).
of deaths (38% as opposed to 22%) was observed below thearbitrary cutoff age of 20 years.
To evaluate the risk of death according to the mani-festing complications we performed a bivariate analysis andcalculated the odds ratios (ORs) and confidence intervals(CI). OR and CI provide information on the strength(level of statistical significance) of association between thecomplications and the occurrence of deaths. Whereever thenumbers of subjects were too small, the Fisher’s exact testwas used to calculate the P value (Table 3).
We found that the complications of Dengue, namely,hemorrhage, pleural effusion, myocarditis, liver failure, andrenal failure were independently linked with a 7–11 timeshigher risk of death compared to those without (Table 3).However, the wide confidence intervals indicated the highervariability of this observation.
The effect of treatment modality on the outcome (death)was evaluated with chi-square test (see Table 4). Chi-squaretest is widely used to evaluate the association between thesepredictor and outcome variables.
The results revealed that the treatment modalities,namely, the use of inotropes, mechanical ventilation, peri-toneal dialysis, and the use of blood products were signif-icantly associated with higher occurrence of deaths amongthese patients (Table 4). However, the use of steroids had noassociation with death.
Thereafter a discriminant analysis was used to classify thecases according to the values of categorical dichotomous-dependent variables. This analysis assesses the relative im-portance of the independent variables in classifying thedependent variable.
The standardized canonical discriminant function coeffi-cients identified mechanical ventilation and peritoneal dial-ysis as therapeutic modalities significantly associated withthe deaths of dengue patients presenting with Dengue ShockSyndrome (Table 5).
A similar discriminant analysis was used to assess therelative importance of complications and outcome. Renalfailure and hemorrhage were identified as complications sig-nificantly associated with deaths in Dengue Shock Syndrome(Table 6).
4. Discussion
We have evaluated the mortality risk factors amongst across-section of patients in Dengue Shock Syndrome notresponding to standard therapies and as a consequence ina clinical scenario confounded by previous therapies beforeadmission to ICU. Dengue Shock Syndrome is a dangerous

Journal of Tropical Medicine 3
Table 3: Complications ensued and outcomes amongst patients with Dengue shock syndrome in ICU (∗Fisher’s exact test).
Complications Deaths Discharges Total OR CI P
HemorrhageYes 13 14 27
7.4 1.8–30.7 0.003No 3 24 27
Total 16 38 54
Pleural effusionYes 13 14 27
7.4 1.8–30.7 0.003No 3 24 27
Total 16 38 54
MyocarditisYes 8 6 14
5.3 1.4–19.8 0.02∗No 8 32 40
Total 16 38 54
Yes 10 0 10
Renal failure No 06 38 44 <0.001∗
Total 16 38 54
Liver failureYes 08 03 11
11.7 2.2–54.1 0.001∗No 08 35 43
Total 16 38 54
Table 4: Therapeutic modalities applied and outcomes of patients with Dengue Shock Syndrome receiving intensive care.
Therapies Deaths Discharges Total χ2 .df P
InotropesYes 15 12 27
17.41 1 <0.001No 01 26 27
Total 16 38 54
Mechanical ventilationYes 15 4 19
34.1 1 <0.001No 1 34 35
Total 16 38 54
Liver failure regimeYes 9 3 12
15.23 1 <0.001No 7 35 42
Total 16 38 54
Peritoneal dialysisYes 8 0 8
22.3 1 <0.001No 8 38 46
Total 16 38 54
Blood products1 14 11 25
15.2 1 < 0.0012 2 27 29
Total 16 38 54
SteroidsYes 7 13 20
0.353 1 0.553No 9 24 33
Total 16 37 53
complication of the dengue infection and is associated withhigh mortality. Almost one-third of our study group receivedblood transfusions to counter their bleeding manifestations.Thus, we were seeing the worst cases of the spectrum.
The pathogenesis of shock in dengue is complex. In-creased vascular permeability, together with myocardialdysfunction and dehydration due to capillary leakage, con-tribute to the development of shock, with resultant multi-organ failure. The onset of shock can be dramatic, and itsprogression relentless. The diagnosis is largely clinical andis supported by serology and identification of viral materialin the blood. No specific methods are available to predictoutcome and progression. As observed by Singhi et al. [6]the choice of fluids, inotropes, and techniques of organ
support and careful fluid management is the mainstay ofmanagement.
We have recorded a 30% mortality risk for this uniquegroup of patients with Dengue Shock Syndrome whohad received prior medical therapies and was admitted toIntensive Care with further deterioration. Unfortunately, thefact that 50% of the patients who succumbed did so withinthe first 24 hours of admission to the ICU indicates theirmoribund state upon referral to the ICU. It should be notedthat the presenting clinical status of these patients to theICU was confounded by a variety of treatment regimensthat were applied before admission to the ICU. For example,in a typical patient admitted with respiratory distress andhypoxia, the clinical picture would easily be modified by

4 Journal of Tropical Medicine
Table 5: Standardized Canonical Discriminant functions betweentherapeutic modalities and outcome (∗Wilk’s lambda = 0.315; df =2; P < 0.001).
VariablesCanonical discriminant function
coefficients
Mechanical ventilation 0.885∗
Peritoneal dialysis 0.566∗
Liver failure regime 0.474
Blood products 0.233
Steroids 0.215
Inotropes 0.192
Table 6: Standardized Canonical Discriminant functions betweencomplications and outcome.
VariablesCanonical discriminant function
coefficients
Renal failure .919∗
Liver failure .476
Pleural effusion .417
Hemorrhage .377∗
Myocarditis .368∗
Wilk’s lambda = 0.419; df = 02; P < 0.001.
overzealous hydration with colloids such as dextran orhetastarch prior to the ICU referral. In this study we have notbeen able to assess the influence of prior therapy on outcomedue to poor medical records received at the admission toICU. It is however the general impression of the authors,that the influence of prior therapies could be an importantdeterminant of outcome, especially because some patientswere noted to have had a cumulative dose of hetastarchexceeding 25 mL/kg suggesting overload contributing torespiratory distress more than the disease itself. This is a veryimportant aspect that cannot be overlooked in future studiesof this nature.
There is a general impression that fatal dengue iscommoner in the younger population compared to middleor old age [7, 8]. Although we recorded 62.5% deathsamongst patients aged 20 or below, we have no statisticalevidence to support the notion that mortality is higheramongst children. This is because our age distribution alsoindicated that 50% of the age cohort admitted for ICU carewas above the age of 20. Peradeniya ICU is multidisciplinaryand there are no age restrictions in its admission policy andhence we presume that our data represent the populationwith Dengue Shock Syndrome with no age bias.
In our study, from amongst the dead, 88% expired duringfirst three days of ICU care and the highest death ratewas reported on day 1 (50% of total deaths). A similarstudy during an epidemic of dengue hemorrhagic fever ineasternmost Indonesia showed a case fatality rate of 1.2%from a 172 suspected cases. They too observed that, thesurvivors needed a range of 1–8 days of ICU care [9] similarto the durations we observed. Another study from Mumbaiduring a dengue epidemic reported a case fatality rate of
16.6% amongst pediatric patients suffering from DengueShock syndrome [10].
Bleeding has been identified as one of the dreaded man-ifestations of concern that complicates the outcome ofdengue [11]. Although our canonical discriminant analysisindicated that hemorrhage and renal failure were the dreadedcomplications associated with death, from amongst its maintherapeutic modalities only peritoneal dialysis (PD) wasassociated with death. This suggested that the use of bloodproducts has effectively mitigated the effects of hemorrhageupon outcome. However, peritoneal dialysis did not showa similar effect suggesting that PD may not be the mostappropriate modality of therapy in these moribund patientswith multiorgan failure. It is also our clinical observationthat PD cycles in Dengue patients produced a relatively largefluid retrieval without the use of additional measures suchas dextrose in dialysate fluid. These large negative balanceswere corrected with the use of stored plasma intravenously.It is likely that these patients had ascites fluid that was alsoremoved by each dialysis cycle and this may have simulatedthe main problem of dengue, the “capillary leak.” Thus,peritoneal dialysis may have aggravated the clinical effects ofcontinuing “capillary leak” leading to worsened outcomes.We had no facility for Continuous Renal ReplacementTherapy (CRRT).
We also found that mechanical ventilation was alsoassociated with death. Only 21% of patients who receivedmechanical ventilation in the ICU recovered in this study (4out of 19). Since we had no facility for ECMO, it is difficultto comprehend whether mechanical ventilation is the bestsupportive mode of therapy to maintain oxygenation in DSS.
There was a significant relationship between dengue,complications, and the modes of therapies and outcome.Hemorrhage, pleural effusion, myocarditis, renal failure,and liver failure were all important predictors of the worstoutcomes. A study conducted in Thailand implied theimportance of detection of abnormal high transaminaseenzyme among the patients with dengue infection since theconsequently developed hepatic encephalopathy could beexpected [12]. In our study 9 out of 12 patients who weretreated with liver failure regime expired (75%).
Dengue induced Acute Kidney Injury (AKI) comprisingcreatinine increase, proteinuria, glomerulonephritis, andhaemolytic uremic syndrome has been reported [13, 14]and also dengue-haemorrhagic-fever-(DHF-) induced AKIeven in the absence of shock, haemolysis, or rhabdomyolysis[15]. In our study 8 out of 8 (100%) patients who weresuspected as having renal failure expired despite peritonealdialysis. Similar to our observation, Kuo et al. in the year2002 reported a Dengue outbreak in Taiwan and noted thatpatients with renal failure (RF) carry a high mortality rate,that is, the morality rate RF group versus non-RF group was28.6% against 1.2%; P < 0.001 [16].
Acute reversible myocardial dysfunction is the com-monest documented cardiac complication in dengue. Thevariable incidences of dengue myocarditis had been postu-lated to be due to variable immunopathogenesis secondaryto variations in serotypes. Dengue myocarditis is generallyreversible with favorable outcomes if diagnosed and treated

Journal of Tropical Medicine 5
early [17, 18]. In our study 15 out of 27 patients (55.55%)who were suspected of having dengue myocarditis weretreated with inotropes but they died during their ICU stay.
It has been reported that corticosteroids were no moreeffective than the placebo or the no treatment protocolfor reducing the number of deaths, the need for bloodtransfusion, or the number of serious complications [19] orin achieving a higher rise of the platelet count in dengueinfection [20]. We have observed the same. No specifictherapy has been shown to be effective in improving survival[21].
5. Conclusion
Our study indicates that during this dengue outbreak,patients in DSS who were not responding to standard ther-apies and admitted ICU had a 30% risk of death. Peritonealdialysis increases this risk to 100%.
Acknowledgments
The authors are grateful to all ICU staff for providing infor-mation for this study. They thank Mr. Mahes Salgado for hiscontribution in the preparation of the paper.
References
[1] D. J. Gubler, “Dengue and dengue hemorrhagic fever,” ClinicalMicrobiology Reviews, vol. 11, no. 3, pp. 480–496, 1998.
[2] T. N. Ngo, C. X. T. Phuong, R. Kneen et al., “Acute manage-ment of dengue shock syndrome: a randomized double-blindcomparison of 4 intravenous fluid regimens in the first hour,”Clinical Infectious Diseases, vol. 32, no. 2, pp. 204–213, 2001.
[3] S. Ranjit and N. Kissoon, “Dengue hemorrhagic fever andshock syndromes,” Pediatric Critical Care Medicine, vol. 12, no.1, pp. 90–100, 2010.
[4] G. N. Malavige, V. G. N. S. Velathanthiri, E. S. Wijewickrama etal., “Patterns of disease among adults hospitalized with dengueinfections,” QJM, vol. 99, no. 5, pp. 299–305, 2006.
[5] S. A. M. Kularatne, I. B. Gawarammana, and P. R. V.Kumarasiri, “Epidemiology, clinical features, laboratory inves-tigations and early diagnosis of dengue fever in adults: adescriptive study in Sri Lanka,” Southeast Asian Journal ofTropical Medicine and Public Health, vol. 36, no. 3, pp. 686–692, 2005.
[6] S. Singhi, N. Kissoon, and A. Bansal, “Dengue and denguehemorrhagic fever: management issues in an intensive careunit,” Jornal de Pediatria, vol. 83, no. 2, supplement, pp. S22–S35, 2007.
[7] T. K. Samsi, H. Wulur, D. Sugianto, C. R. Bartz, and R.Tan, “Some clinical and epidemiological observations onbiologically confirmed dengue haemorrhagic fever,” PaediatrIndones, vol. 30, no. 11-12, pp. 293–303, 1990.
[8] P. Gurugama, P. Garg, J. Perera, A. Wijewickrama, andS. Seneviratne, “Dengue viral infections,” Indian Journal ofDermatology, vol. 55, no. 1, pp. 68–78, 2010.
[9] N. C. Sukri, K. Laras, T. Wandra et al., “Transmission of epi-demic dengue hemorrhagic fever in easternmost Indonesia,”American Journal of Tropical Medicine and Hygiene, vol. 68, no.5, pp. 529–535, 2003.
[10] I. Shah, G. C. Deshpande, and P. N. Tardeja, “Outbreak ofdengue in Mumbai and predictive markers for dengue shocksyndrome,” Journal of Tropical Pediatrics, vol. 50, no. 5, pp.301–305, 2004.
[11] S. Shivbalan, K. Anandnathan, S. Balasubramanian, M. Datta,and E. Amalraj, “Predictors of spontaneous bleeding indengue,” Indian Journal of Pediatrics, vol. 71, no. 1, pp. 33–36,2004.
[12] V. Wiwanitkit, “Liver dysfunction in Dengue infection: ananalysis of the previously published Thai cases,” JAMC, vol.19, no. 1, pp. 10–12, 2007.
[13] P. Futrakul, V. Poshyachinda, and C. Mitrakul, “Renal involve-ment. And reticulo endothelial system clearance in denguehemorrhagic fever,” Journal of the Medical Association ofThailand, vol. 56, no. 1, pp. 33–39, 1973.
[14] V. Boonpucknavig, N. Bhamarapravati, and S. Boonpuck-navig, “Glomerular changes in dengue hemorrhagic fever,”Archives of Pathology and Laboratory Medicine, vol. 100, no. 4,pp. 206–212, 1976.
[15] E. Q. Lima, F. S. Gorayeb, J. R. Zanon, M. L. Nogueira, H. J.Ramalho, and E. A. Burdmann, “Dengue haemorrhagic fever-induced acute kidney injury without hypotension, haemolysisor rhabdomyolysis,” Nephrology Dialysis Transplantation, vol.22, no. 11, pp. 3322–3326, 2007.
[16] M. C. Kuo, P. L. Lu, J. M. Chang et al., “Impact of renal failureon the outcome of dengue viral infection,” Clinical Journal ofthe American Society of Nephrology, vol. 3, no. 5, pp. 1350–1356, 2008.
[17] D. M. Salgado, J. M. Eltit, K. Mansfield et al., “Heart andskeletal muscle are targets of dengue virus infection,” PediatricInfectious Disease Journal, vol. 29, no. 3, pp. 238–242, 2010.
[18] V. Wiwanitkit, “Dengue myocarditis, rare but not fatal mani-festation,” International Journal of Cardiology, vol. 112, no. 1,article 122, 2006.
[19] R. Panpanich, P. Sornchai, and K. Kanjanaratanakorn, “Cor-ticosteroids for treating dengue shock syndrome,” CochraneDatabase of Systematic Reviews, vol. 3, Article ID CD003488,2006.
[20] S. A. M. Kularatne, C. Walathara, S. I. Mahindawansa et al.,“Efficacy of low dose dexamethasone in severe thrombocy-topenia caused by dengue fever: a placebo controlled study,”Postgraduate Medical Journal, vol. 85, no. 1008, pp. 525–529,2009.
[21] S. Rajapakse, “Dengue shock,” Journal of Emergencies, Traumaand Shock, vol. 4, no. 1, pp. 120–127, 2011.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 760951, 11 pagesdoi:10.1155/2012/760951
Research Article
Diffusion Pattern and Hotspot Detection of Dengue inBelo Horizonte, Minas Gerais, Brazil
Jose Eduardo Marques Pessanha Pessanha,1, 2 Waleska Teixeira Caiaffa,1
Maria Cristina de Mattos Almeida,1, 2 Silvana Tecles Brandao,2
and Fernando Augusto Proietti1
1 Belo Horizonte Observatory for Urban Health (OSUBH), UFMG, 30130 Belo Horizonte, MG, Brazil2 Municipal Health Secretariat of Belo Horizonte, 30130 Belo Horizonte, MG, Brazil
Correspondence should be addressed to Jose Eduardo Marques Pessanha Pessanha, [email protected]
Received 15 September 2011; Revised 1 November 2011; Accepted 2 December 2011
Academic Editor: M. C. Field
Copyright © 2012 Jose Eduardo Marques Pessanha Pessanha et al. This is an open access article distributed under the CreativeCommons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided theoriginal work is properly cited.
This study considers the dengue occurrence in the city of Belo Horizonte over the last fifteen years. Approximately 186,000 casesregistered from 1996 to 2011 were analyzed. The home address of individuals whose dengue case was notified was used as a proxyfor exposure location. For determining possible outbreaks of disease and the specific patterns of dengue cases, spatial statisticsused included Kernel’s estimation. The occurrence of waves of dengue outbreaks was correlated with climatic and vector presencedata. Outbreaks had different durations and intensities: case clustering, thinned out both spatially and temporally. These findingsmay be useful for public health professionals responsible for fighting the disease providing some tools for improving evaluation ofinterventions such as vector control and patient care, minimizing the collective and individual burden of the disease.
1. Introduction
The most important arbovirus disease in humans, dengue,annually affects 80 million individuals in many countries,leading to 550,000 hospitalizations and 20,000 thousanddeaths [1]. The main vector is the mosquito Aedes aegypti, anarthropod with an extremely high capacity to adapt to urbanareas.
Since 1982, the reemergence of dengue has been reportedin urban centers in all Brazilian regions. The magnitude ofthis disease has led to high public federal, state, and munic-ipal investments in vector control, epidemiological surveil-lance, and patient care.
During the 1990s, the incidence of dengue increasedgreatly as a consequence of the dissemination of A. aegypti.Dispersion of the vector was followed by the disseminationof dengue virus serotypes 1 and 2 in twenty of the 27 statesof the country. Between 1990 and 2000, several epidemicsoccurred, mainly in the largest urban areas of the Southeastand the Northeast, where the majority of notified cases were
concentrated. The first great dengue epidemic occurred in1998, with approximately 528,000 cases [2].
In Brazil, the increase in the incidence of dengue cases in2002 and the emergence of a third serotype (DENV-3) ledto a prediction of an increased risk of dengue epidemics andan increase of the cases of dengue hemorrhagic fever (DHF).To face the expected risks for 2002, the Brazil Ministryof Health, in collaboration with the Pan-American HealthOrganization, carried out an international seminar in June2000 to evaluate the dengue epidemic and to prepare aNational Dengue Control Program (PNCD). However, thecurrent epidemiological situation shows that these programmeasures have not achieved the expected results. Epidemi-ological impact assessments of these interventions haveshown that their effectiveness has been extremely limited[3]. Regardless of each local health system, even when thesemeasures are well managed, their effectiveness is always low,given the intense viral circulation detected in the successiveepidemics and the results of serological surveys conducted inseveral Brazilian cities [4, 5].

2 Journal of Tropical Medicine
BeloHorizonte
Minas Gerais
MinasGerais
Brazil
South AmericaBelo Horizonte map
SD
HSCA
Northwest SDEast SD
South Central SD
Barreiro SD
West SD
Northeast SDPampulha SD
North SDVenda Nova SD
Figure 1: Belo Horizonte map.
0
1
2
3
4
5
6
7
8
9
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
Sum
mer
Fall
Win
ter
Spri
ng
1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
0
5
10
15
20
25
30
35
40
Cas
es n
um
ber
RainfallDengue cases
×103×102
(mm
3)
Figure 2: Dengue cases and rainfall by month, season, and year, Belo Horizonte, Minas Gerais state, Brazil, from 1996 to 2010.
The first dengue epidemic in Belo Horizonte (BH), theprincipal city of Brazil’s third metropolitan area, occurredin 1996, and since then, epidemics have occurred every year.Different from the subsequent epidemics, the 1996 epidemicstarted in the southern hemisphere’s fall. The only serotypeinitially identified was DENV-1. However, by the end of 1997,another epidemic of great intensity started, characterized bythe simultaneous circulation of DENV-1 and DENV-2. The
two serotypes continued to produce successive epidemicsevery year. In February 2002, DENV-3 was identified for thefirst time in BH, and now the three serotypes coexist [5].
The control measures, adopted in BH until the 1998epidemic, had only a limited role, without much impact onthe final numbers of cases [6]. This situation was repeatedin 1997 and only changed its stance in 1998, before thelargest epidemic in the city when DENV-1 and DENV-2 virus

Journal of Tropical Medicine 3
Table 1: Building larval index (BLI) in October larval foci survey, eggs average (EA) in September-October survey, and dengue incidencerates (DIR) per 100,000 inhabitants in subsequent years, by Sanitary District, Belo Horizonte city, 2004–2010.
Sanitary District
Year Barreiro South central East Northeast Northwest North West Pampulha Venda nova BH
2004 Building larval index 0.4 0.3 0.0 0.3 0.3 0.3 0.3 0.3 0.6 0.3
Eggs (average) 1.9 1.6 1.7 1.9 3.5 2.6 3.6 2.9 3.6 2.6
Dengue incidence rate 1.1 2.6 2.0 5.5 5.6 2.1 2.2 3.5 2.9 3.2
2005 Building larval index 0.5 0.8 0.4 0.5 0.5 0.6 0.9 0.6 0.8 0.6
Eggs (average) 3.2 4.0 3.3 3.8 3.7 4.6 7.1 4.1 8.6 4.7
Dengue incidence rate 7.6 6.0 5.6 17.9 81.5 5.7 44.3 46.3 5.7 26.1
2006 Building larval index 1.6 1.5 1.4 2.5 2.1 1.1 1.9 2.4 1.6 1.8
Eggs (average) 3.9 5.3 5.9 3.9 7.4 2.5 5.0 7.1 6.1 5.2
Dengue incidence rate 29.4 58.3 160.2 403.2 637.3 83.1 167.1 299.4 114.5 232.4
2007 Building larval index 0.1 0.4 0.4 0.6 0.3 0.2 0.4 0.4 1.0 0.4
Eggs (average) 1.8 4.1 3.6 2.4 4.8 5.9 4.6 3.8 5.7 4.0
Dengue incidence rate 45.0 71.8 369.7 2,545.8 477.5 529.0 139.2 528.7 217.9 558.6
2008 Building larval index 0.4 0.7 0.9 1.2 0.9 0.5 0.8 1.4 1.5 0.9
Eggs (average) 2.4 2.8 4.4 5.4 8.3 6.3 7.0 4.2 6.6 5.2
Dengue incidence rate 53.0 62.8 329.6 540.8 245.1 2,922.6 336.1 719.5 646.9 563.4
2009 Building larval index 1.4 1.5 2.8 2.4 2.1 2.7 2.3 2.4 3.2 2.3
Eggs (average) 11.0 6.1 7.7 9.8 11.8 14.1 14.2 12.9 26.2 12.3
Dengue incidence rate 678.1 273.3 1,837.1 1,823.3 2,511.9 4,371.3 2,316.0 3,802.2 5,111.5 2,375.3
2010 Building larval index 0.6 0.6 1.3 1.2 0.7 1.0 0.8 1.6 0.9 0.9
Eggs (average) 2.7 3.8 6.2 7.8 6.8 7.2 9.3 8.7 15.1 7.3
Dengue incidence rate 61.2 35.3 69.4 61.8 79.7 118.3 43.0 49.6 56.8 63.3
Pearson correlation BLI and DIR: r = 0.59, P < 0.001.Pearson correlation EA and DIR: r = 0.69, P < 0.001.
serotypes were both circulating. In 2002, it was observed thatthe spread of serotype 3 from the state where it was originallydetected presented a different pattern from that observedwith serotypes 1 and 2. Previously, the expansion of the newserotype (DENV-3) occurred slowly and some years elapsedbefore autochthonous cases occurred in other states. Duringthe first three months of 2002, the presence of the newserotype was detected in ten other states. In BH, the DENV-3serotype was isolated in only a few samples that year. It wouldbe theoretically possible to attribute these results to thecontrol measures proposed by the Brazil Ministry of Healthin 1996, the Program of Eradication of A. aegypti—knownas PEAa—which was only implemented in the municipalityin 1998. This program took into account the difficulties ofthe previous control strategy and proposed an even morecomplex objective, predicated on the assumption that thevector could be eradicated [7].
When compared to other large urban areas in SoutheastBrazil, the dengue epidemic cycle in BH has had its owncharacteristics [8]. Low epidemic intensity was observedfrom 1999 to 2005. This epidemic behavior was probablyonly interrupted when the resistance to the larvicidal agentbeing used was detected in BH in 2006 [9].
Currently, vector control is the only way to interruptdisease transmission, given that there is neither an effectivevaccine nor specific therapy [10]. Vector control, however, is
not a simple task, especially given the complexities of urbansettings. The failure of dengue control programs has beenpointed out by several authors [7, 11–13].
Spatial analyses are powerful tools in public healthdiagnosis and surveillance, allowing the identification ofcritical areas for intervention and the variables associatedwith the modulation of disease dynamics [14, 15]. Dengue,whose pattern is well known to be clustered in certainareas, is a health-related event for which spatial analysistechniques may be useful [16]. Spatial analyses and statistics,such as spatial autocorrelation analysis, cluster analysis, andtemporal analysis, are commonly used to highlight spatialpatterns of dengue cases and to test whether there is a patternof dengue incidence in a particular area [17, 18].
A geographic information system (GIS) can be used toidentify and assess potential compositional and contextualrisk factors associated to disease transmission such as socioe-conomic, climatic, demographic, and physical environment.GIS technologies have been applied in epidemiologic andpublic health studies for many years [19, 20], providinginformation useful for studying and modeling the spatial-temporal dynamics of dengue [21–23]. This paper aims toevaluate dengue dissemination in space and time, deter-mining possible outbreak waves of dengue cases correlatedwith climatic data and presence of the vector. This studymay contribute to implement interventions aimed at vector

4 Journal of Tropical Medicine
2001 2002 2003 2004 2005
2006 2007 2008 2009 2010
Proportional circleRange incidence rates
TI100000
até 100
300–1000
1000–5000
5000–10000
100–300
1
10
100
1000
10000
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
Years
Belo Horizonte cityBrazil
Den
gue
inci
den
ce/1
0000
0 in
hab
itan
ts
Figure 3: Dengue incidence point maps by city (proportional circle) and range incidence rates by municipalities areas, temporal dynamicsin space, Brazil, and incidence years comparative graphic, Belo Horizonte city, Brazil, 2001–2010.
control and patient care, minimizing the collective and indi-vidual burden of this disease.
2. Materials and Methods
2.1. Study Area. This ecological study was conducted in BeloHorizonte (BH), the capital of the state of Minas Gerais, inthe Southeast region of Brazil (19◦55′S 43◦57′W). Occupyingan area of 330.23 km2 [24] with 2,375,151 inhabitantsin approximately 600,000 households [25] (Figure 1), BHis Brazil’s sixth most populous city. Situated at altitudesranging from 700 to 1,200 meters (mean 858 meters), BHhas a tropical wet and dry climate with an average annualtemperature of approximately 21◦C [26].
Each one of 147 primary care units is responsible fora geographic area known as a health services catchmentarea (HSCA). The HSCAs are aggregated in nine SanitaryDistricts (SDs) named as North, Northeast, Northwest, East,South Central, West, Venda Nova, Pampulha, and Barreiro[27].
2.2. Dengue Cases. All dengue cases reported from 1996 to2011 (partial) to the municipal surveillance system—whichin turn are forwarded to Brazil’s national reporting system[28]—were used. The notification form contains, along withother information, each patient’s address and the date ofonset of dengue symptoms.

Journal of Tropical Medicine 5
1996 1997 1998 1999
2000
20042003
2001 2002
1996First cases
2002
Vector Case Vector Case Vector
Vector Case Vector CaseVector Case
Vector Case Vector Case
1999
Case
Green areas
100
Density of building with focspring larval survey
Hotspot dengue caseBelo Horizonte
High
LowOutros
∗
∗The green areas have no building
Figure 4: Temporal dynamics in space, foci of Aedes aegypti larvae in October survey and dengue outbreaks, between 1996 and 2004, BeloHorizonte/MG, Brazil.
2.3. Dengue Vectors. Dengue larvae vectors foci data reportedfor years 1996 to 2011 (partial) and eggs collected in ovitrapsfrom 2003 to 2010 were used in this study. The data wasobtained from the municipality vector reporting system—SCZOO [29] which contains the address for each larva focusand ovitrap and the dates of the survey.
The ovitraps—which cover a radius of 200 meters—areinstalled every two weeks [30]. The building larval index(BLI) as proposed by Connor and Monroe [31] measures thedensity of A. aegypti in urban areas and is estimated as theproportion of houses with A. aegypti larvae. It has been usedin Brazil since 2003 and in BH since 2004.
2.4. Climatic Data. Rainfall (mm) and temperature (degreesCelsius) for the years 2001–2010 were obtained from weatherstation of the 5th district of Brazil’s Meteorological Institute(INMET).
2.5. Spatial and Temporal Diffusion Pattern. Depending onthe analysis (see below), dengue incidence was calculated ona monthly or annual basis from 1996 to 2011.
Initially, monthly temporal trends of dengue incidencewere determined. Then the dengue incidence in a given yearfor each Sanitary District from 2005 to 2011 was correlated toSeptember-October vector data (the mean number of eggs inthe ovitraps of each SD and the BLI in the larvae foci survey)
from the previous year. We used the Pearson correlation coef-ficient to estimate the correlation between the monthly inci-dence of dengue and climate data for the years 2001 to 2010.
2.6. Spatial Analysis. All reported cases of dengue were ge-oreferenced using the patient household address. The vectordata was geocoded using the address of the larvae focibuilding and the locations of the ovitraps. Spatial statisticaltechniques used in this study included Kernel’s estimationin order to determine the possible outbreaks of disease andspecific patterns of distribution on the urban space.
2.7. Space and Time Analysis. To find how dengue spread inspace and time, we created map objects that change statuswith time [32].
2.8. Hotspot Detection. A “Hotspot” is defined as a conditionindicating some form of clustering in a spatial distribution[33]. Hotspot detection can be useful, even if the globalpattern is not clustered. Moreover, cases clusters that occurrandomly can also have an influence on the spread of aninfectious disease.
2.9. Software. TabWin 3.5 was used to make Brazil munici-palities maps (http://www.datasus.gov.br/), and R (R Devel-opment Core Team; http://www.r-project.org/) was used to

6 Journal of Tropical Medicine
00
1000
2000
3000
4000
5000
0.5 1 1.5 2 2.5 3 3.5
Building larval index
Inci
den
ce r
ate/
1000
00 in
hab
itan
ts
20102009
2008
2008
2005 2006 2007
2011
Vector Case Vector Case Vector Case
Vector Case Vector Case Vector Case
Green areas
Vector Case
2004
High
Low
Kernel’s estimationHotspot dengue casesBelo Horizonte
Highest intensity
Lowest intensity
−1000
y = 774.15x − 278.05r2 = 0.3596
r = 0.59
Figure 5: Temporal dynamics in space, foci of Aedes aegypti larvae Kernel’s estimation in October survey and dengue hotspot outbreaks,2004–2011, and regression linear graphic (incidence versus building larvae index), Belo Horizonte/MG, Brazil.
calculate the Pearson correlations and Kernel’s estimation.MAPIINFO 8.5 was used to make BH hotspots maps, andExcel 2003 was used to generate tables and figures.
3. Results
3.1. Spatial and Temporal Analysis of Dengue
3.1.1. Temporal Analysis. In this series of annual incidentdengue cases, five distinct periods were identified: (1)between April 1996, the first epidemic in BH, and July 1998,the most important epidemic; (2) between August 1998and December 2000 with incidence rates not exceeding 10cases per 100,000 inhabitants; (3) between January 2001 andAugust 2002, during which two new epidemics occurred; (4)between August 2002 and December 2005 again with lowdengue incidence rates; (5) the last period, between January
2006 and August 2010, during which the incidence rate wasprogressively higher (Figure 2).
The dengue temporal distribution with highest incidencein the rainy season presented a similar pattern duringthe period (Figure 2). Characteristically, dengue outbreaksgenerally occurred during the second part of the rainyseason, when humidity was higher than average [27].
In the period from 2005 to 2011, annual incidence ratesof dengue showed a statistically significant correlation withthe BLI according to Sanitary District (r = 0.60, P =0.0000002). For the mean values of eggs captured in theovitraps, the correlation was also statistically significant (r =0.69, P = 0.00000005) (Table 1).
Rainfall (RF) and temperature (TEMP) begin to increasein October, with dengue outbreaks occurring during themonths of January to May, the period of highest rainfalland humidity. The number of cases then fall through June,a period when RF and TEMP also decrease (Figure 2).

Journal of Tropical Medicine 7
Green areas
2003 2004 2004 2005
2011
2007
201020092007 2008 2008
20062005 2006
2009 2010
0
1000
2000
3000
4000
5000
0 5 10 15 20 25 30
Average eggs
Hotspot dengue caseBelo Horizonte
Highest intensity
Lowest intensity
Eggs density
1000
−1000
Inci
den
ce r
ate/
1000
00 in
hab
itan
ts
y = 166.41x − 457.13r2 = 0.4712
r = 0.59
Figure 6: Aedes aegypti eggs in ovitraps, September-October survey, and dengue outbreaks, temporal dynamics in space, 2003–2011, andlinear regression graphic (incidence versus mean number of eggs), Belo Horizonte, MG, Brazil.
Analyzing the climatic data for the years 2001 to 2010,monthly dengue incidence rates showed a statistically signif-icant correlation with the RF of the previous month (r =0.36, P = 0.00006) and the monthly minimum temperature(r = 0.29, P = 0.001).
3.1.2. Dengue Hotspot Detection. The maps that compriseFigure 3 illustrate the spatial and temporal evolution ofdengue in cities of Brazil and are accompanied by acomparative graph of annual incidence rates from 2001 to2011 for BH, Brazil. Figures 4 and 5 demonstrate the spatialcorrelation between dengue cases hotspots and the locationof Aedes aegypti larvae foci in BH. Figure 6 shows the sameobservation among dengue cases hotspots and the areas withthe greatest presence of Aedes aegypti eggs. The hotspot
analysis also found a higher risk of dengue in areas of thecity that are at lower elevations (Figures 7 and 8).
4. Discussion
Monitoring and planning control measures for dengueepidemics are vital for preventing or minimizing disease out-breaks. Information based on notified cases only, however,is insufficient, because many people who are infected mayeither be asymptomatic or do not become part of the officialstatistics even if they present symptoms [34].
The use of information on dengue incidences rates,mapping their patterns and dynamics of spread using spatialautocorrelation analysis, can be a valuable tool to analyzethe spatial patterns change over time. Therefore, instead of

8 Journal of Tropical Medicine
Weather point
Weather point
0
250
500
750
Nov
Dec Jan
Feb
Mar
Apr
May Jun
Jul
Agu Se
pO
ctN
ovD
ec
2009 2010
(mm
)
10
15
20
25
Rainfall (mm)
ano mês
Dados
Altitude range
1000 a 1600
900 a 1000
700 a 900
0
250
500
750
(mm
)
10
15
20
25
◦ C)
(
◦ C)
(
Temperature (◦C)
Fonte-gecoz/smsa/Belo Horizonte5◦district/inmet/Brazil N
ovD
ec Jan
Feb
Mar
Apr
May Jun
Jul
Agu Se
pO
ctN
ovD
ec
2009 2010
Rainfall (mm)
ano mês
Dados
Temperature (◦C)
Figure 7: Monthly minimum temperature and rainfall, from Nov/2009 to Nov/2010, weathers geographic points, and altitude range, BeloHorizonte/MG, Brazil.
1996 1997 1998 2001
2002 2007 201020092008
Hotspot dengue caseBelo Horizonte
High
LowOutros
Altitude range
1000 a 1600
900 a 1000
700 a 900
∗Green areas
∗The green areas have no building.
Figure 8: Dengue outbreaks, temporal dynamics in space, 1996–2011, and altitude range, Belo Horizonte/MG, Brazil.

Journal of Tropical Medicine 9
aiming to achieve a complete understanding of the transmis-sion process, it may be more efficient to improve the surveil-lance system and optimize disease control.
The heterogeneous intraurban distribution of dengueincidence according to Sanitary Districts for the years 2001to 2011 suggests the importance of analyzing transmission atthe SD level.
The degree of acquired immunity to the dengue virusmay vary across different areas of the municipality based onthe spatial distribution of previous outbreaks. Thus, SanitaryDistricts with larger proportions of susceptible individualsmay present higher incidences.
Our results indicate that continuous vector surveillanceusing ovitraps and larvae foci is necessary, so that a great-er number of areas with potential transmission can be iden-tified, permitting the prioritization and scheduling of vectorcontrol measures.
Certainly, the identification of high-risk areas, in a pro-cess of surveillance and control of the disease and themosquito, is an important step towards optimizing resources.Once such areas have been identified, interventions may pro-vide better results in decreasing incidences rather thanthrough the traditional approach of a uniform control stra-tegy for the city as a whole.
Determining whether greater vector presence or coeffi-cients of dengue incidence predominant in certain intrau-rban areas may be operationalized through the use of theconcept of persistence. For each SD, the number of months ofuninterrupted vector presence would be calculated, therebydetermining whether greater persistence occurs in specificSDs over the various periods of the year.
Temporal analysis of climatic factors (rainfall, tempera-ture, and humidity) revealed that dengue generally occurswhen average temperatures increase, when the rainy seasonhas started, and when the humidity is higher. Previously, areport from BH showed that rainfall and relative humiditydata from fifteen days before (t−1) showed very high corre-lation with dengue vector incidence in time t [30]. There areother studies in the literature reporting an important corre-lation between climate and dengue occurrences or denguevector abundance [35–37]. However, the occurrence of aresidual vector population or the occurrence of dengue casesin distinct intraurban areas in the cold and dry months, withmuch lower dengue incidence than in January to May, shouldbe taken into account for disease control.
Early detection and prediction of dengue outbreaksshould be goals for municipal surveillance systems. Iden-tifying locations and patterns of the vector population(species, density, and vector-control indices) should alsobe used to direct interventions with disease reduction asthe preferred outcome measure demonstrating impact, andovitraps index, house index, container index, and Breteauindex as proxy indicators of impact. With these strategies,information will be available in real time, which may uncoverother aspects about the relationship between vector andthe disease that could be revealed through spatial analyses[38, 39].
Other tools such as the industrial control chart—pro-posed by Rich and Terry [40], and adopted in several survey
vigilance systems—when applied to dengue require severalimprovements related to presentation and interpretation inorder to enhance its usefulness. The ability to demonstratetrends, analyzing only notified dengue cases at a potentiallyearlier time point, is limited. Heterogeneous internet accesslimits the use of query-based surveillance web tools to iden-tify disease and location outbreaks as candidates for interven-tions. Although this proposal is intriguing, so far the iden-tification of a given outbreak is usually too late for controlmeasures.
5. Conclusions
Our findings show that the strategies used in this studycan help public health officials to visualize and understandthe geographic distribution and trends of disease patternsand to prepare warnings and awareness campaigns. Denguespatial and temporal spread patterns and hotspot detectionmay constitute useful information for public health officialsto control and predict dengue dissemination from criticalhotspot areas. This may save time and cost and make pub-lic health department actions more efficient. Public healthofficers may employ the model to plan a strategy to con-trol dengue by analyzing the information received on dis-tribution and hotspots for various months. Some ancillaryfindings of the study such as influence of climate, which isseasonal and thus temporal, also contribute to knowledgeregarding its significance. The methodology is based on prin-ciples of spatial statistics and has the potential to be appliedto other epidemics. In the future, it will be important tohave regular daily statistics accumulated over several yearsto permit faster recognition of outbreak locations and beprepared to promptly implement appropriate public healthinterventions.
References
[1] World Health Organization, “DengueNet Implementation inthe Americas. Report of a WHO/PAHO/CDC Meeting, SanJuan, Puerto Rico, July 2002,” WHO HQ, Geneva, Switzerland,2003, http://www.who.int/csr/resources/publications/dengue/whocdscsrgar20038en.pdf.
[2] P. T. R. Vilarinhos, “Challenges for dengue control in Bra-zil: overview of socioeconomic and environmental factors as-sociated with virus circulation,” http://library.wur.nl/frontis/environmental change/10 vilarinhos.pdf.
[3] J. S. Koopman and I. M. Longini, “The ecological effects ofindividual exposures and nonlinear disease dynamics in pop-ulations,” American Journal of Public Health, vol. 84, no. 5, pp.836–842, 1994.
[4] M. C. M. Cunha, W. T. Caiaffa, C. L. Oliveira et al., “Fatoresassociados a infeccao pelo vırus do dengue no Municıpio deBelo Horizonte, Estado de Minas Gerais, Brasil: caracterısticasindividuais e diferencas intra-urbanas,” Epidemiol Serv Saude,vol. 17, no. 3, pp. 217–230, 2008.
[5] J. E. M. Pessanha, W. T. Caiaffa, E. G. Kroon, and F. A. Proietti,“Dengue fever in three sanitary districts in the city of BeloHorizonte, Brazil: a population-based seroepidemiologicalsurvey, 2006 to 2007,” Revista Panamericana de Salud Publica,vol. 27, no. 4, pp. 252–258, 2010.

10 Journal of Tropical Medicine
[6] P. R. Lopes Correa, E. Franca, and T. F. Bogutchi, “Aedesaegypti infestation and occurence of dengue in the city of BeloHorizonte, Brazil,” Revista de Saude Publica, vol. 39, no. 1, pp.33–40, 2005.
[7] J. E. M. Pessanha, W. T. Caiaffa, C. C. Cesar, and F. A. Proietti,“Evaluation of the Brazilian national dengue control plan,”Cadernos de Saude Publica, vol. 25, no. 7, pp. 1637–1641, 2009.
[8] Brazil. Ministry of Health, “Grafico da taxa de incidencia dedengue. Regiao Sudeste, 1990–2010,” http://portal.saude.gov.br/portal/arquivos/pdf/graf taxa inc dengue regiao sudeste90 09.pdf.
[9] Brazil. Tribunal de Contas da Uniao- TCU, “Audiencia Pub-lica Conjunta No: 1817/08 17/12/2008 Comissao Meio Ambi-ente/Comissao Fiscalizacao Financeira. Esclarecimentos sobremedidas adotadas pelo Ministerio da Saude em funcao dasrecomendacoes realizadas pelo Tribunal de Contas da Uniaono tocante ao controle da dengue,” http://www2.camara.gov.br/atividade-legislativa/comissoes/comissoes-permanentes/cmads/notastaq/nt17122008.
[10] World Health Organization (WHO), “Dengue guidelines fordiagnosis, treatment, prevention and control,” 2009.
[11] P. L. Tauil, “Critical aspects of dengue control in Brazil,” Cad-ernos de Saude Publica, vol. 18, no. 3, pp. 867–871, 2002.
[12] A. C. Figueiro, A. P. Soter, C. Braga, Z. M. A. Hartz, and I.A. Samico, “Analise da logica de intervencao do ProgramaNacional de Controle da Dengue,” Revista Brasileira de SaudeMaterno Infantil, vol. 10, supplement 1, 2010.
[13] C. Heintze, M. V. Garrido, and K. A. Velasco, “What docommunity-based dengue control programmes achieve? Asystematic review of published evaluations,” Transactions of theRoyal Society of Tropical Medicine and Hygiene, vol. 101, no. 4,pp. 317–325, 2007.
[14] N. A. Honorio, R. M. R. Nogueira, C. T. Codeco et al., “Spatialevaluation and modeling of dengue seroprevalence and vectordensity in Rio de Janeiro, Brazil,” PLoS Neglected TropicalDiseases, vol. 3, no. 11, article e545, 2009.
[15] R. Cordeiro, M. R. Donalisio, and V. R. Andrade, “Spatialdistribution of the risk of dengue fever in southeast Brazil,2006-2007,” BMC Public Health, vol. 11, article 355, 2011.
[16] P. V. Fulmali, A. Walimbe, and P. V. M. Mahadev, “Spread,establishment & prevalence of dengue vector Aedes aegypti(L.) in Konkan region, Maharashtra, India,” Indian Journal ofMedical Research, vol. 127, no. 6, pp. 589–601, 2008.
[17] J. S. Brownstein, H. Rosen, D. Purdy et al., “Spatial analysis ofWest Nile virus: rapid risk assessment of an introduced vector-borne zoonosis,” Vector Borne Zoonotic Dis, vol. 2, no. 3, pp.157–164, 2002.
[18] J. B. Siqueira, C. M. T. Martelli, I. J. Maciel et al., “Householdsurvey of dengue infection in central Brazil: spatial point pat-tern analysis and risk factors assessment,” American Journal ofTropical Medicine and Hygiene, vol. 71, no. 5, pp. 646–651,2004.
[19] C. Rotela, F. Fouque, M. Lamfri et al., “Space-time analysis ofthe dengue spreading dynamics in the 2004 Tartagal outbreak,Northern Argentina,” Acta Tropica, vol. 103, no. 1, pp. 1–13,2007.
[20] M. C. De Mattos Almeida, W. T. Caiaffa, R. M. Assuncao, andF. A. Proietti, “Spatial vulnerability to dengue in a Brazilian ur-ban area during a 7-year surveillance,” Journal of Urban Health,vol. 84, no. 3, pp. 334–345, 2007.
[21] D. A. T. Cummings, R. A. Irizarry, N. E. Huang et al., “Travell-ing waves in the occurrence of dengue haemorrhagic fever inThailand,” Nature, vol. 427, no. 6972, pp. 344–347, 2004.
[22] N. A. Maidana and H. M. Yang, “Describing the geographicspread of dengue disease by traveling waves,” MathematicalBiosciences, vol. 215, no. 1, pp. 64–77, 2008.
[23] A. Tran and M. Raffy, “On the dynamics of dengue epidemicsfrom large-scale information,” Theoretical Population Biology,vol. 69, no. 1, pp. 3–12, 2006.
[24] Instituto Brasileiro de Geografia e Estatıstica–IBGE, “Censodemografico e estatısticas,” http://www.ibge.gov.br/censo/div-ulgacao.shtm.
[25] Prefeitura Municipal de Belo Horizonte–PBH, http://portal-pbh.pbh.gov.br/pbh/ecp/comunidade.do?evento=portlet&pI-dPlc=ecpTaxonomiaMenuPortal&app=saude&tax=16010&la-ng=pt BR&pg=5571&taxp=0&.
[26] Brasil. Ministerio da Agricultura e Reforma Agraria. Secretar-ia Nacional de Irrigacao, Departamento Nacional de Meteo-rologia. Normais climatologicas (1961–1990). Brasılia, pp. 84,1992.
[27] Belo Horizonte. Prefeitura Municipal Secretaria Municipal deSaude, “Organizacao territorial dos servicos municipais desaude em Belo Horizonte,” pp. 1–6, 2003, http://www.pbh.gov.br/smsa/biblioteca/geepi/territoriosnasmsa.doc.
[28] Brasil. Secretaria de Vigilancia a Saude, Sistema de Informacaode Agravos de Notificacao—Sinan. Normas e Rotinas, Minister-io da Saude, Brasılia, Brazil, 2002.
[29] J. E. M. Pessanha and F. R. Carvalho, “A Criacao de um Sis-tema Informatizado com enfase na Padronizacao dos Meto-dos, para Auxiliar as Acoes de Controle de Zoonoses noMunicıpio de Belo Horizonte,” http://www.ip.pbh.gov.br/ANO1 N1 PDF/res ip0101pessanha.html.
[30] R. L. Vianello, J. E. M. Pessanha, and G. C. Sediyama, “Previsaode ocorrencia dos mosquitos da dengue em belo horizonte,com base em dados meteorologicos,” in Proceedings of the 14thCongresso Brasileiro de Meteorologia, Florianopolis, Brazil,2006.
[31] M. E. Connor and W. M. Monroe, “Stegomyia indices andtheir value in yellow fever control,” American Journal of Tropi-cal Medicine and Hygiene, vol. 3, pp. 9–19, 1923.
[32] S. Zhong, Y. Xue, C. Cao et al., “The application of space/timeanalysis tools of GIS in spatial epidemiology: a case studyof Hepatitis B in China using GIS,” in Proceedings of theIEEE International Geoscience and Remote Sensing Symposium(IGARSS ’05), vol. 8, pp. 1612–1615, July 2005.
[33] F. B. Osei and A. A. Duker, “Spatial and demographic patternsof Cholera in Ashanti region—Ghana,” International Journalof Health Geographics, vol. 7, article 44, 2008.
[34] S. B. Halstead, “Dengue in the Americas and Southeast Asia:do they differ?” Revista Panamericana de Salud Publica, vol.20, no. 6, pp. 407–415, 2006.
[35] N. Degallier, A. P. A. Travassos Da Rosa, P. F. C. Vasconceloset al., “Dengue fever and its vectors in Brazil,” Bulletin de laSociete de Pathologie Exotique, vol. 89, no. 2, pp. 128–136, 1996.
[36] M. R. Donalısio and C. M. Glasser, “Vigilancia entomologicae controle de vetores do dengue,” Revista Brasileira de Entomo-logia, vol. 5, no. 3, pp. 259–272, 2002.
[37] K. V. Schreiber, “An investigation of relationships between cli-mate and dengue using a water budgeting technique, Environ-ment Health Perspective,” International Journal of Biometeo-rology, vol. 45, no. 2, pp. 81–89, 2001.
[38] M. E. Beatty, A. Stone, D. W. Fitzsimons et al., “Best prac-tices in dengue surveillance: a report from the asia-pacific andamericas dengue prevention boards,” PLoS Neglected TropicalDiseases, vol. 4, no. 11, article e890, 2010.

Journal of Tropical Medicine 11
[39] G. T. Ai-leen and R. J. Song, “The use of GIS in ovitrap moni-toring for dengue control in Singapore,” http://www.searo.who.int/en/Section10/Section332/Section522 2536.htm.
[40] W. H. Rich and M. C. Terry, “The industrial “control chart”applied to the study of epidemics,” Public Health Reports, vol.61, pp. 1501–1511, 1946.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 950303, 7 pagesdoi:10.1155/2012/950303
Research Article
Comparative Evaluation of Permissiveness to Dengue VirusSerotype 2 Infection in Primary Rodent Macrophages
Jeanette Prada-Arismendy, Veronica Rincon, and Jaime E. Castellanos
Instituto de Virologıa, Universidad El Bosque, Carrera 7B Bis No. 132-11, Bogota, Colombia
Correspondence should be addressed to Jaime E. Castellanos, [email protected]
Received 19 October 2011; Accepted 19 December 2011
Academic Editor: Carlos E. P. Corbett
Copyright © 2012 Jeanette Prada-Arismendy et al. This is an open access article distributed under the Creative CommonsAttribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work isproperly cited.
Infection with dengue virus presents a broad clinical spectrum, which can range from asymptomatic cases to severe cases that arecharacterised by haemorrhagic syndrome and/or shock. The reason for such variability remains unknown. This work evaluatedthe in vitro permissiveness of mouse, rat, hamster, and guinea pig macrophages to infection by dengue virus 2 (DENV2). Theresults established that macrophages derived from the BALB/c mouse strain showed higher permissiveness to DENV2 infectionthan macrophages from other rodent species, although all rodent species studied had the C820T mutation in the oligoadenylatesynthetase 1b gene, indicating no relationship to the different in vitro susceptibilities of mouse cells at this locus. Other molecularmechanisms related to flavivirus susceptibility remain to be explored.
1. Introduction
Infection with dengue virus (DENV) causes dengue andsevere dengue (formerly dengue fever and dengue haemor-rhagic fever). DENV belongs to the Flaviviridae family,flavivirus genus. DENV is an enveloped virus, and its genomeconsists of a positive polarity, single-stranded RNA of around11 kb that encodes ten proteins. DENV can replicate in sev-eral types of cells, including dendritic cells, B and T lym-phocytes, endothelial cells, hepatocytes, and neuronal cells.However, monocytes/macrophages are the primary targetduring in vivo infection [1]. Viral entry into these cellsenables the virus to spread to different tissues and induces thepresentation HLA molecule-associated viral antigens. Thepresentation of viral antigens by macrophages to memory Tcells induces T cell activation and, consequently, the prolifer-ation and production of cytokines such as TNF-α, IFN, andIL-2. This set of cytokines and chemokines induces endothe-lial dysfunction and plasma leakage, both of which are char-acteristic of more severe manifestations of the disease [2].
Several studies have addressed the relationship betweenhuman genes and the susceptibility to dengue virus infection.For example, the HLA-A∗0203 allele correlated with denguefever (DF) in Thai children, while HLA-A∗0207 correlated
with dengue haemorrhagic fever (DHF). Moreover, thealleles HLA-B44, B62, B76, and B77 confer protection againstDHF in secondary infections [3]. Other polymorphismsassociated with DHF have been found in the genes for DC-SIGN1, TNF-α, Fc-γ receptors, vitamin D receptors, andmannose binding lectin [4, 5]. In addition to these hostfactors, there is evidence that DENV serotypes 2 and 3 causeDHF more frequently [6], supporting the belief that bothhost and virus factors can affect the clinical outcome ofpatients.
Recent studies have identified the oligoadenylate synthe-tase 1b (Oas1b) gene as being responsible for susceptibility/resistance to West Nile Virus (WNV) infection in mice, andit is therefore a potential candidate gene for the Flv locus[7, 8]. These seminal works found a non-sense mutation(C820T) in the Oas1b gene, exon 4, that was linked tosusceptibility to WNV infection. This mutation replaces anarginine with a stop codon, producing a truncated proteinlacking the C-terminal domain. Knock-in of a normal Oas1ballele induced resistance to Yellow Fever Virus infection ina susceptible mouse strain, which was comparable to theresistance observed in resistant congenic mice [9]. Theseresults led to the conclusion that the Oas1b gene conferredresistance against flavivirus infection. However, a neuronal

2 Journal of Tropical Medicine
cell line expressing the complete form of the Oas1b proteinshowed only a slight reduction in virus yield and was notsignificantly different from the same neuronal cell line ex-pressing the truncated form [10]. Likewise, transfectingcDNA from the complete Oas1b gene into susceptible em-bryonic fibroblasts did not induce a complete reversion to theresistant phenotype [11]. Together, these results suggest thatmurine resistance to Flavivirus infection is not completelyunderstood in vitro and that other cellular and animal mod-els should be studied. This work evaluated the permissivenessto DENV infection and evaluated the presence of the C820Tpolymorphism in the Oas1b gene obtained from differentrodent species, including three strains of mouse, rat, hamster,and guinea pig.
2. Materials and Methods
2.1. Animals and Cells. Experiments with animals were ap-proved by the Universidad El Bosque’s Ethics Committeefollowing the national legislation. Different 6–8-week-oldrodent species were used and were obtained from theColombian National Institute of Health’s animal facility. Theanimals used were BALB/c inbred mice (Mus musculus), NIHSwiss outbred mice, CD1 (ICR) Swiss outbred mice, Syrianhamsters (Mesocricetus auratus), Wistar rats (Rattus norvegi-cus), and Hartley strain guinea pigs (Cavia porcellus). Twomillilitres of 1.5% carboxymethylcellulose was injected in-traperitoneally into two animals from each species and thiswas done twice in different days. After 48 hours, the animalswere euthanized, and a peritoneal wash was made with RPMI1640 medium plus 10% foetal bovine serum, 100 U/mL peni-cillin, 10 μg/mL streptomycin, and 2,5 μg/mL amphotericin(complete medium-CM). The medium was collected andcentrifuged, and the cell pellet was then suspended in CM.Then, 200,000 cells were seeded into 12-well culture dishesand 10,000 cells were seeded in 24-well culture dishes usinground glass coverslips. Nonadherent cells were removed 48hours later, and the culture of adherent cells continued for afurther 5 days to allow for cytokine clearance. Adherent cellswere considered to be peritoneal macrophages, as previouslydescribed [12]. The cells were seeded in duplicate from eachanimal used.
2.2. Virus and Infection. The virus was obtained by infectingC6/36 HT cells with a DENV serotype 2 (COL-789) isolatedonated by Dr. Jairo Mendez from the Colombian Instituteof Health’s Virology Group and titrated on LLCMK-2 cells.The virus was placed in contact with the macrophages for 1hour at 37◦C at a multiplicity of infection (MOI) of 1 and0.1; it was then removed, fresh medium was added, and thecells were kept for 24, 48, and 72 hours, at which time theywere processed.
2.3. Plasmid Construction and qPCR. A capsid gene fragmentamplified from DENV2 RNA was used to construct a plas-mid as published previously [13], and a dilution having1010 copies/μL was prepared. RNA was extracted from infect-ed and uninfected macrophage supernatants and monolayersusing Trizol LS and Trizol reagents, respectively, (Invitrogen)
and reverse-transcribed using the M-MLV enzyme and ran-dom primers. The SYBR Green and the GeneAmp 5700sequence detection system (Perkin-Elmer Corporation) wereused for the real-time PCR assay. A DENV capsid gene frag-ment was amplified using DV2C-L and DV2C-R primers.Samples lacking cDNA were used as negative controls, andcDNA obtained from viral inoculums was used as positivecontrols. The data obtained from the monolayers were an-alysed using the relative quantification method based on theassumption of ideal amplification efficiency with a doublingproduct every cycle, followed by twofold changes in fluores-cence intensity (which could be calculated using the 2−ΔΔCT
formula) and β-actin as the housekeeping gene [14]. Abso-lute quantification was used for analysing the data obtainedfrom the supernatants by producing a six-point standardcurve (107–102 copies/μL) from the pDV2core plasmid (107–102 molecules) that was obtained as previously described[13]. This curve was simultaneously processed with thesamples and evaluated 24, 48, and 72 hours p.i. Data wereanalysed using ANOVA and a Least Significant Differencepost hoc test and P < 0.05 was considered significant. Twoindependent experiments were done, and two animals wereused from each species in each one. Independent duplicatesof cells were seeded for each animal (n = 8); each sample wasprocessed by duplicate in qPCR experiments.
2.4. Immunocytochemistry and TUNEL Assay. Infected andnoninfected cells were fixed with 4% paraformaldehydefor the same defined periods and then permeabilised with0.1% Triton X-100. Infected cells were detected by usingmonoclonal antiflavivirus antibody (Chemicon, MAB8744).Biotinylated anti-mouse IgG antibody was used as thesecondary antibody and detected with peroxidase-coupledstreptavidin, and 0.05% diaminobenzidine and 0.01% H2O2
were used as the developing reagents. Other cultures wereincubated with biotinylated dUTP and the TdT enzymefor detecting DNA fragmentation (as an apoptotic indi-cator); after being washed, samples were incubated withCy3-coupled streptavidin. The cultures were visualised andcounted in a Wild Leitz GmBH fluorescence microscope.One-way ANOVA was done, and when the overall ANOVAresulted in a P value less than 0.05, Least Significant Differ-ence (LSD) test was carried out for comparing infected cellcounts and values from viral RNA quantification.
2.5. Obtaining and Sequencing DNA. Brain DNA was ob-tained from each rodent species using phenol/chloroformextraction and precipitated with sodium acetate and ethanol.This DNA was used to amplify an Oas1b gene exon 4fragment using OAS-1bR: 5′-CTG GGA GTA TGG GAGTCG AG-3′ and OAS-1bL: 5′-GCT GTT GGT GCA GGTATT CA-3′ primers, which amplify the gene region betweennucleotides 771–925. The PCR product was purified andsequenced.
3. Results
3.1. Dengue Virus Replication Efficiency among DifferentRodent Macrophages. The number of viral copies released by

Journal of Tropical Medicine 3
1
10
100
1000
10000
24 h 48 h 72 h
Nu
mbe
r of
cop
ies/μ
g R
NA ∗∗ ∗∗ ∗∗
Balb/c
NIH
RatGuinea pigHamster
ICR
(a)
1
10
100
1000
10000
24 h 48 h 72 h
Nu
mbe
r of
cop
ies/μ
g R
NA ∗∗
(b)
Figure 1: qRT-PCR to obtain absolute quantification of viral copies yielded to supernatants from different rodent species’ peritonealmacrophages cultures. (a) Cells infected at a MOI 0,1 and (b) MOI 1. ∗∗P < 0.01.
the macrophages into the supernatant was quantified by real-time PCR analysis of the RNA obtained from the supernatantof cells infected for 24, 48, and 72 hours at two differentMOIs. Figure 1(a) shows that the viral copy number obtainedfrom BALB/c-derived macrophage supernatants infectedwith DENV at an MOI of 0,1 in all post-infection (p.i.)times was 4–25 times larger than that obtained from NIH-and ICR-derived mouse macrophages. The differences in thenumber of viral copies were significant at 24 and 48 hoursp.i. (P < 0.01), while the number of viral copies obtainedin BALB/c-derived macrophages was similar to that obtainedin NIH- and ICR-derived mouse macrophages at 72 hours.Similar findings were established in macrophages from tax-onomically different rodent species, such as rats, hamsters,and guinea pigs, where highly significant differences werefound (P < 0.01).
When the macrophages were infected at an MOI of 1(Figure 1(b)), significant differences were observed 24 hoursp.i. when BALB/c donors were compared to NIH mice, ham-sters, and guinea pigs (P < 0.01). No difference in the viralcopy number were found in the supernatants at 48 and 72hours p.i.
A larger number of viral RNA copies were found inBALB/c-derived macrophage supernatants from cells infect-ed with an MOI of 0.1 than with an MOI of 1 (Figure 1(a)versus Figure 1(b)). There were no differences among viralcopies when the infection was carried out at an MOI of 0.1or 1 in the other animals (P > 0.05). Relative RNA viralquantitation was carried out from macrophage monolayersand showed that the amount of virus found in cells was pro-portional to the amount of virus released to the supernatant.The relative viral RNA quantity was significantly larger inBALB/c macrophages, from 4-fold (BALB/c versus hamster)to 5400-fold (BALB/c versus ICR) higher at an MOI of0,1, and from 4-fold (BALB/c versus hamster) to 8100-fold(BALB/c versus ICR) at an MOI of 1 (P < 0.05, see Figure 2).Differences in relative expression levels were much moremarked than the differences found in the absolute quantifi-cation of the supernatants. The data obtained from the other
rodent species did not reveal any significant differences whencomparing different MOIs, nor when comparing the threep.i times. With the exception of the lower relative viral RNAlevels found in NIH mouse macrophages, the levels of viralRNA tended to decrease as the p.i. time increased (Figure 2).
3.2. Infected and Apoptotic Macrophages from DifferentRodents. Immunocytochemistry was used to detect viral an-tigens in macrophages from the six different rodent speciesstudied. As previously described [15], specific immunoreac-tivity was observed that corresponded to viral antigens in theinfected cell cytoplasm (having punctiform characteristics)in the perinuclear region. A significantly larger numberof infected macrophages was found in BALB/c-derivedmacrophages compared with other rodent macrophage cul-tures (Figure 3(c)). Approximately 43% of the macrophagesfrom BALB/c mice inoculated with an MOI of 1 showedevidence of infection 24 hours p.i., increasing to 100% at 48hours p.i.; an 81% infection of macrophages was reached atan MOI of 0.1, but only at 72 hours p.i. infection percentageswere much lower in cells from the other animals (seeTable 1). A large number of positively stained extracellularvesicles were also observed in BALB/c-derived macrophages(Figure 3(b)), but they were not observed in macrophagesfrom other species (Figure 3(c)). Macrophages inoculatedwith DENV at an MOI of 1 presented a high percentageof DNA fragmentation, as demonstrated by TUNEL. Highapoptotic percentages were found from 24 hours p.i. (88%)onwards and remained high up to 48 and 72 hours p.i. (91and 99%, resp.). In infected macrophages from rodent spe-cies other than BALB/c, the percentage of TUNEL-positivecells was similar to that found in control cells that had notbeen infected with DENV (Table 1). An interesting findingwas that the apoptotic percentages in macrophages fromBALB/c mice inoculated with DENV at an MOI of 0,1 didnot correlate with the percentages for DENV-positive cells.While 79% of the cells had become infected 48 hours after-infection, only 8% were apoptotic; the same phenomena oc-curred at 72 hours (81% versus 5%).

4 Journal of Tropical Medicine
Rel
ativ
e ex
pres
sion
of
vira
l RN
A
0.01
0.1
1
10
100
1000
10000
24 h 48 h 72 h
∗
∗∗∗
∗∗
Balb/c
NIH
RatGuinea pigHamster
ICR
(a)
Rel
ativ
e ex
pres
sion
of
vira
l RN
A
0.01
0.1
1
10
100
1000
10000
24 h 48 h 72 h
∗∗∗∗
∗∗
(b)
Figure 2: qRT-PCR to obtain relative quantification of viral copies obtained from monolayers from different rodents’ peritonealmacrophages cultures. The fold change of viral RNA was calculated from DENV-infected macrophage monolayers, normalising the dataobtained against noninfected control and against β-actin at 0,1 MOI (a) and at 1 MOI (b) and evaluated 24, 48, and 72 hours p.i. ∗P < 0.05,∗∗P < 0.01.
(a) (b)
(c)
Figure 3: Immunocytochemistry for DENV2-infected or noninfected macrophages. (a) Noninfected macrophage control. (b) Macrophagesfrom DENV-infected BALB/c mice at 1 MOI, 72 hours p.i. Observe the staining in almost all cells (arrows). Note the extracellular vesiclesimmunoreactive to viral antigen (arrow heads). (c) Hamster macrophages DENV-infected at MOI 1, 72 hours p.i. The stained cells show anintracytoplasmatic viral antigen distribution; the other animals showed a similar labelling pattern. The bars correspond to 40 μm.
3.3. Presence of the C820T Mutation. Analysing the sequencesfrom the Oas1b gene exon 4 fragment obtained from BALB/cmouse genomic DNA revealed that they were consistentwith those reported previously [7, 8]. The TGA stop codonmutation inserts a premature translation stop in the Oas1bgene in these mice. Interestingly, the other rodent speciesanalysed also had the C820T mutation, which leads to thetranslation of a truncated protein in all cases. The sequences
from this Oas1b fragment from guinea pigs, hamsters, andNIH and ICR mice had not been previously identified andwere reported to GenBank (Cavia porcellus accession numberEF081023, Rattus norvegicus accession number EF081022,Mus musculus NIH strain accession number EF081021, Musmusculus ICR strain accession number EF081020, Mesocrice-tus auratus accession number EF081019, Mus musculusBALB/c strain accession number EF081018).

Journal of Tropical Medicine 5
Table 1: Percentage of infected and positive TUNEL cultured macrophages from different rodents.
0.1 MOI 1 MOI
MOCK 24 h 48 h 72 h 24 h 48 h 72 h
TUNEL DENV+ TUNEL DENV+ TUNEL DENV+ TUNEL DENV+ TUNEL DENV+ TUNEL DENV+ TUNEL
BALB/c 4.0 13.2 5.2 79.8 8.2 81.4 5.0 43.4 88.6 100 91 86.8 99.2
ICR 13.0 26.6 9.2 21.8 17.0 22.6 13.6 13.2 4.6 25.6 23.6 34.2 17.0
NIH 8.0 5.8 5.0 12.2 9.4 15.6 31.0 9.2 9.4 13.8 29.2 17.2 9.2
Rat 2.0 24.4 4.6 17.8 5.2 23 7.4 20.6 5.6 13.6 4.2 8.0 6.3
Guineapig
5.2 5.2 3.2 12.4 8.6 24.4 4.6 5.2 6.0 17.8 8.0 29.6 3.8
Hamster 7.0 13.4 12.0 32.8 34.8 8.6 33.2 6.4 3.0 5.4 17.0 10 15.2
The data represent the percentage of DENV antigen positive over the total of cells counted. Note that only 43.4% of the cells were positive for viral antigen inBALB/c mouse macrophage infected with 1 MOI, 24 hours p.i., but almost all the cells presented DNA degradation. Two animals were used from each species;two groups of independent cells were seeded for each animal and two replicates were done for each of them in immunocytochemistry and TUNEL assays (n =8).
4. Discussion
Genetic markers for host susceptibility to infection couldprovide answers for questions concerning why not all indi-viduals infected by DENV become ill and why they do notall have similar symptoms if they do become ill. The clinicalmanifestations of dengue virus infection range from undif-ferentiated fever to severe systemic compromise, encephalitis,and haemorrhagic syndrome. The reason why infection withDENV (and the flavivirus in general) causes clinical mani-festations in only a small percentage of infected individualsremains unknown. However, it has been suggested that thehost’s genetic factors could be involved. The resistance ofsome mice strains to infection by some flavivirus has beendescribed since the beginning of the twentieth century ([11]reviewed in [16]), and it was initially found that flavivirusresistance to infection was inherited as a dominant trait [17].
It is known that the monocyte/macrophage system is theprimary in vivo cellular target for DENV, and the peritonealmacrophage model has also been used to study flavivirusresistance and susceptibility. In this work, it was found thatmacrophages from BALB/c mice had higher permissivenessto DENV2 infection using qPCR and immunocytochemistry.Sequence analysis of the Oas1b gene demonstrated that allfour rodent species studied had the C820T mutation, leadingto the supposition that the production of a truncated proteinby this genotype does not affect DENV susceptibility.
With the exception of BALB/c mice, all rodent strains andspecies of macrophages studied have a low capacity to sup-port DENV2 replication because infection with the virus didnot cause large amounts of RNA to assemble or be releasedas virions. This finding could contradict the suggestion of aprotective mechanism involving viral packaging, as has beenpreviously proposed [18]. The results found in NIH mouse-derived macrophages could suggest that these cells not onlyhave a cellular mechanism that reduces permissiveness butalso have a more efficient viral clearance process. Neverthe-less, it is important to clear that these results are only relevantfor dengue virus serotype 2; it is probable that differentresults could be found for other dengue serotypes.
Like other studies, we did find more viral copies insupernatants in any of the cultures that had been inoculatedwith an MOI of 0.1 relative to those with an MOI of 1. Brin-ton [19] suggested that this finding could be due to thepresence of defective interfering (DI) particles found ingreater amounts at a higher MOI. The production of DIparticles could be facilitated by some mechanism in resistantcells, while highly susceptible cells will mainly produceinfectious virus. In turn, this higher virus production leadsto greater cell death in highly susceptible cells. The theory issupported by the work done by Espina et al. [20], who usedhuman monocytes as their model. Despite the infected cellpercentage in BALB/c-derived macrophages is similar withboth MOIs, infection at an MOI of 1 induced a significantlyhigher number of TUNEL-positive cells. It seems that the in-fection of cells with a high MOI activates proapoptotic mo-lecular routes as a mechanism to block viral replication anddissemination during viral infection, thereby explaining thisfinding. However, the virus could be activating anti-apop-totic routes at a low MOI and improving cell survival. It hasbeen previously established that DENV induces apoptosisin different cell types (e.g., endothelial cells, hepatocytes,dendritic cells, monocytes, and neuroblastoma cells) [21].The proapoptotic mechanisms that are related to DENVinfection include apoptosis activation by the extrinsic route(via ligands such as TNF-α and Apo2/TRAIL) [22] andthe intrinsic route (described in neuroblastoma cells havingphospholipase A2 activation, superoxide anion production,cytochrome c release, followed by caspase 3 activation). Amechanism related to apoptosis has not been previouslyproposed in work studying resistance and susceptibility toflavivirus infection. The results of the present study displayeda clear relationship between lower susceptibility to infectionand decreased apoptosis. This finding suggests that the con-trol of apoptosis-inducing mechanisms may represent a ma-crophage protection strategy in addition to it control of viralreplication, a phenomenon that deserves more investigation.It would also be necessary to consider in the study ofthese cells susceptibility to dengue virus infection, the recentfindings of Kwan et al. [23], in which Monocyte-derived

6 Journal of Tropical Medicine
dermal macrophages were capable of internalizing liveDENV but they displayed an inherent resistance to viralgrowth because virus particles accumulate into poorly acidi-fied phagosomes, which prevents release of the nucleocapsidinto the cytoplasm, and therefore its later replication. Togeth-er, these results suggest an additional level of complexity inthe genetic control of flavivirus replication.
5. Conclusions
This work can conclude that BALB/c mice macrophages hadhigher permissiveness to DENV2 infection as it showedhigher viral copies when measuring by using qPCR and im-munocytochemistry. Besides, sequence analysis demon-strated that Balb/C, NIH, and ICR mice as well as rat, ham-ster, and guinea pig had the C820T mutation in Oas1b gene.It is needed to carry out more studies to clarify which isthe molecular pathway involved in this higher permissivenessand if it is related to some apoptotic pathway.
Author Contributions
J. Prada-Arismendy conducted cell culture, infection, andmolecular biology experiments and wrote the manuscript. V.Rincon collaborated in the molecular biology and real timePCR experiments. J. E. Castellanos edited the study, beingchief scientific advisor, and edited the manuscript. All au-thors read and approved the final manuscript.
Conflict of Interests
The authors declare that no conflicting financial interestsexist.
Acknowledgments
This work was supported by the Universidad El Bosque andInstituto Colombiano para el Fomento de la Ciencia y laTecnologıa (Colciencias, Project 130-8051-7588).
References
[1] K. Clyde, J. L. Kyle, and E. Harris, “Recent advances in de-ciphering viral and host determinants of dengue virus replica-tion and pathogenesis,” Journal of Virology, vol. 80, no. 23, pp.11418–11431, 2006.
[2] Y. C. Chen and S. Y. Wang, “Activation of terminally differen-tiated human monocytes/macrophages by dengue virus: pro-ductive infection, hierarchical production of innate cytokinesand chemokines, and the synergistic effect of lipopolysaccha-ride,” Journal of Virology, vol. 76, no. 19, pp. 9877–9887, 2002.
[3] H. A. F. Stephens, R. Klaythong, M. Sirikong et al., “HLA-Aand -B allele associations with secondary dengue virus in-fections correlate with disease severity and the infecting viralserotype in ethnic Thais,” Tissue Antigens, vol. 60, no. 4, pp.309–318, 2002.
[4] M. T. Fernandez-Mestre, K. Gendzekhadze, P. Rivas-Veten-court, and Z. Layrisse, “TNF-α-308A allele, a possible severityrisk factor of hemorrhagic manifestation in dengue feverpatients,” Tissue Antigens, vol. 64, no. 4, pp. 469–472, 2004.
[5] H. Loke, D. Bethell, C. X. T. Phuong et al., “Susceptibilityto dengue hemorrhagic fever in Vietnam: evidence of anassociation with variation in the vitamin D receptor and FCγreceptor IIA genes,” The American Journal of Tropical Medicineand Hygiene, vol. 67, no. 1, pp. 102–106, 2002.
[6] A. Balmaseda, S. N. Hammond, L. Perez et al., “Serotype-specific differences in clinical manifestations of dengue,” TheAmerican Journal of Tropical Medicine and Hygiene, vol. 74, no.3, pp. 449–456, 2006.
[7] T. Mashimo, M. Lucas, D. Simon-Chazottes et al., “A nonsensemutation in the gene encoding 2′-5′-oligoadenylate syn-thetase/L1 isoform is associated with West Nile virus suscepti-bility in laboratory mice,” Proceedings of the National Academyof Sciences of the United States of America, vol. 99, no. 17, pp.11311–11316, 2002.
[8] A. A. Perelygin, S. V. Scherbik, I. B. Zhulin, B. M. Stockman,Y. Li, and M. A. Brinton, “Positional cloning of the murineflavivirus resistance gene,” Proceedings of the National Academyof Sciences of the United States of America, vol. 99, no. 14, pp.9322–9327, 2002.
[9] S. V. Scherbik, K. Kluetzman, A. A. Perelygin, and M. A.Brinton, “Knock-in of the Oas1br allele into a flavivirus-induced disease susceptible mouse generates the resistantphenotype,” Virology, vol. 368, no. 2, pp. 232–237, 2007.
[10] M. Lucas, T. Mashimo, M. P. Frenkiel et al., “Infection ofmouse neurones by West Nile virus is modulated by theinterferon-inducible 2′-5′ oligoadenylate synthetase 1b pro-tein,” Immunology and Cell Biology, vol. 81, no. 3, pp. 230–236,2003.
[11] C. Lynch and T. Hughes, “The inheritance of susceptibility toYellow Fever encephalitis in mice,” Genetics, vol. 21, pp. 104–112, 1937.
[12] L. Pantelic, H. Sivakumaran, and N. Urosevic, “Differentialinduction of antiviral effects against west nile virus in primarymouse macrophages derived from flavivirus-susceptible andcongenic resistant mice by alpha/beta interferon and poly(I-C),” Journal of Virology, vol. 79, no. 3, pp. 1753–1764, 2005.
[13] J. Prada-Arismendy and J. E. Castellanos, “Real time PCR.Application in dengue studies,” Colombia Medica, vol. 42, pp.243–258, 2011.
[14] S. N. Peirson, J. N. Butler, and R. G. Foster, “Experimental val-idation of novel and conventional approaches to quantitativereal-time PCR data analysis,” Nucleic Acids Research, vol. 31,no. 14, article e73, 2003.
[15] J. A. Mosquera, J. P. Hernandez, N. Valero, L. M. Espina, andG. J. Anez, “Ultrastructural studies on dengue virus type 2infection of cultured human monocytes,” Virology Journal, vol.2, article 26, 2005.
[16] J. Prada-Arismendy and J. E. Castellanos, “Susceptibil-ity/Resistance genes to Flavivirus, implications on diseaseseverity,” Acta Biologica Colombiana, vol. 11, pp. 21–30, 2006.
[17] A. Sabin, “Nature of inherited resistance to viruses affectingthe nervous system,” Proceedings of the National Academy ofSciences, vol. 38, pp. 540–546, 1952.
[18] N. Urosevic, M. Van Maanen, J. P. Mansfield, J. S. Mackenzie,and G. R. Shellam, “Molecular characterization of virus-specific RNA produced in the brains of flavivirus-susceptibleand -resistant mice after challenge with Murray Valleyencephalitis virus,” Journal of General Virology, vol. 78, no. 1,pp. 23–29, 1997.
[19] M. A. Brinton, “Analysis of extracellular West Nile virus par-ticles produced by cell cultures from genetically resistant andsusceptible mice indicates enhanced amplification of defective

Journal of Tropical Medicine 7
interfering particles by resistant cultures,” Journal of Virology,vol. 46, no. 3, pp. 860–870, 1983.
[20] L. M. Espina, N. J. Valero, J. M. Hernandez, and J. A. Mos-quera, “Increased apoptosis and expression of tumor necrosisfactor-α caused by infection of cultured human monocyteswith dengue virus,” The American Journal of Tropical Medicineand Hygiene, vol. 68, no. 1, pp. 48–53, 2003.
[21] J. T. Jan, B. H. Chen, S. H. Ma et al., “Potential dengue virus-triggered apoptotic pathway in human neuroblastoma cells:arachidonic acid, superoxide anion, and NF-κB are sequen-tially involved,” Journal of Virology, vol. 74, no. 18, pp. 8680–8691, 2000.
[22] T. Matsuda, A. Almasan, M. Tomita et al., “Dengue virus-induced apoptosis in hepatic cells is partly mediated by Apo2ligand/tumour necrosis factor-related apoptosis-inducing lig-and,” Journal of General Virology, vol. 86, no. 4, pp. 1055–1065,2005.
[23] W. H. Kwan, E. Navarro-Sanchez, H. Dumortier et al., “Derm-al-type macrophages expressing CD209/DC-SIGN show in-herent resistance to dengue virus growth,” PLoS NeglectedTropical Diseases, vol. 2, no. 10, Article ID e311, 2008.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 628475, 13 pagesdoi:10.1155/2012/628475
Review Article
Dengue Virus Entry as Target for Antiviral Therapy
Marijke M. F. Alen and Dominique Schols
Department of Microbiology and Immunology, Rega Institute for Medical Research, Katholieke Universiteit Leuven,3000 Leuven, Belgium
Correspondence should be addressed to Dominique Schols, [email protected]
Received 26 September 2011; Accepted 10 November 2011
Academic Editor: Jean-Paul Gonzalez
Copyright © 2012 M. M. F. Alen and D. Schols. This is an open access article distributed under the Creative Commons AttributionLicense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properlycited.
Dengue virus (DENV) infections are expanding worldwide and, because of the lack of a vaccine, the search for antiviral products isimperative. Four serotypes of DENV are described and they all cause a similar disease outcome. It would be interesting to developan antiviral product that can interact with all four serotypes, prevent host cell infection and subsequent immune activation. DENVentry is thus an interesting target for antiviral therapy. DENV enters the host cell through receptor-mediated endocytosis. Severalcellular receptors have been proposed, and DC-SIGN, present on dendritic cells, is considered as the most important DENVreceptor until now. Because DENV entry is a target for antiviral therapy, various classes of compounds have been investigated toinhibit this process. In this paper, an overview is given of all the putative DENV receptors, and the most promising DENV entryinhibitors are discussed.
1. Introduction
Dengue virus (DENV) is a single-stranded, positive-senseenveloped RNA virus of the Flaviviridae family that is trans-mitted by Aedes aegypti and Aedes albopictus. There exist 4different serotypes of DENV. Each serotype shares around65% of the genome, and, despite of the differences, eachserotype causes nearly identical syndromes in humans andcirculates in the same ecological niche [1]. Dengue viruscauses clinical syndromes in humans, ranging from an acuteself-limited febrile illness (dengue fever, DF) to a severe andlife-threatening vascular leakage and shock (dengue hemor-rhagic fever/dengue shock syndrome, DHF/DSS) [2, 3]. Inthe last decade, due to a decline of vector control efforts,DENV has reemerged in tropical areas and is consideredas the most common arthropod-borne tropical disease thatendangers an estimated 2.5 billion people [4, 5]. Every year,50 million infections occur, including 500,000 hospitaliza-tions for DHF, mainly among children, with a case fatalityrate exceeding 5% in some areas. At present, diagnosis islargely clinical, treatment is supportive through hydration,and disease control is limited by eradication of the mosquito.Many efforts have been made in the search for a suitablevaccine, but the lack of an animal model and the need for
a high immunogenicity vaccine against all four serotypes anda low reactogenicity are posing huge challenges in the denguevaccine development [6, 7]. As there is no vaccine available,the search for antiviral products is imperative. Antiviralspreviously designed against flaviviruses have principallyfocused on inhibition of viral RNA replication. Ribavirin[8], mycophenolic acid [9], and adenosine analogues [10]are believed to act as inhibitors of the RNA-dependent RNApolymerase. Due to low efficacy of these types of compounds[9, 11, 12], more tolerable, highly potent DENV inhibitorsare urgently needed. In the past few years, progressionhas been made in unraveling the host cell pathways uponDENV infection. It is proposed that viral epitopes on thesurface of DENV can trigger cellular immune responses andsubsequently the development of a severe disease. Therefore,these epitopes are potential targets for the development of anew class of antiviral products, DENV entry inhibitors. Inhi-bition of DENV attachment and entry into the host cell caninhibit immune activation. The cellular immune response isbelieved to play an important role in antibody-dependentenhancement (ADE). This is a phenomenon where cross-reacting nonneutralizing antibodies generated to the firstDENV infection will recognize a heterologous DENV duringa secondary infection with another serotype. The DENV-Ab

2 Journal of Tropical Medicine
Target membrane
E-proteindimer
monomer
Fusion loop
Viral RNA
Domain IDomain IIDomain III
Fusion loopStem regionTransmembrane helices
E-proteintrimer
E-protein
Fusion loop
pH < 6.6
//
Outer/inner leaflet of DENV envelopeOuter/inner leaflet of target membrane
ne
monomer
oop
E-protein
Fusion loop
pH < 6.6
Viral RNA
E-proteintrimer
(b)(a)
(e)(d)(c)
Nucleocapsid
Figure 1: Schematic overview of the DENV membrane fusion process (modified figure from Stiasny et al., Amino Acids, 2009 [25]). (a)Prefusion conformation of the E-protein consists of homodimers on the virus surface. (b) Low endosomal pH triggers dissociation of the E-dimers into monomers which leads to the insertion of the fusion peptide with the endosomal target membrane. (c) A stable E-protein trimeris folded in a hairpin-like structure. (d) Hemifusion intermediate in which only the outer leaflets of viral and target cellular membranes havefused. (e) Formation of the postfusion E-trimer and opening of the fusion pore allow the release of the viral RNA into the cytoplasm.
complex enhances DENV access to Fc-receptor bearing cells[13, 14]. This results in the proliferation of T cells andthe production of proinflammatory cytokines that have anindirect effect on the vascular endothelial cells leading toplasma leakage and DHF [3, 4, 15].
This paper will focus on the entry process of DENV andon all identified cellular DENV receptors. A better under-standing of the role of the structural envelope proteinwould aid the research and development of entry inhibitorsagainst flaviviruses. Inhibition of virus attachment is avaluable antiviral strategy because it forms the first barrier toblock infection. Specific molecules preventing the interactionbetween the host and DENV envelope are discussed.
2. DENV Entry
2.1. Entry Process. The infectious entry of DENV in its targetcells, mainly dendritic cells [16], monocytes, and macro-phages, is mediated by the viral envelope glycoprotein E viareceptor-mediated endocytosis [17]. The E-protein is themajor component (53 kDa) of the virion surface and is ar-ranged as 90 homodimers in mature virions [18]. Recent
reports demonstrated that DENV enters its host cell viaclathrin-mediated endocytosis [19, 20], comparable withother flaviviruses [21, 22]. Evidence for flavivirus entry viathis pathway is based on the use of inhibitors of clathrin-mediated uptake, such as chlorpromazine. However, DENVentry via a nonclassical endocytic pathway independent fromclathrin has also been described [23]. It seems that theentry pathway chosen by DENV is highly dependent on thecell type and viral strain. In case of the classical endocyticpathway, there is an uptake of the receptor-bound virus byclathrin-coated vesicles. These vesicles fuse with early endo-somes to deliver their cargo into the cytoplasm. The E-protein responds to the reduced pH of the endosome with alarge conformational rearrangement [24, 25]. The low pHtriggers dissociation of the E-homodimer, which then leadsto the insertion of the fusion peptide into the target cellmembrane forming a bridge between the virus and thehost. Next, a stable trimer of the E-protein is folded intoa hairpin-like structure and forces the target membrane tobend towards the viral membrane, and eventually fusiontakes place [24, 26, 27]. The fusion results in the release ofviral RNA into the cytoplasm for initiation of replication andtranslation (Figure 1).

Journal of Tropical Medicine 3
Table 1: Susceptible cell types for DENV infection and putative DENV receptors.
Species Cell type Cell description DENV receptor(s) References
Monkey Vero Kidney epithelium cells Heparan sulfate (HS) [28, 29]
Glycoprotein (74 kDa) [30]
LLC-MK2 Kidney cells Glycosphingolipid [31]
Human Monocytes Primary myeloid cells CD14/LPS [32]
HSP70/HSP90 [33]
Fc-receptor [13, 14, 17]
Dendritic cells Primary myeloid cells DC-SIGN [34, 35]
Macrophages Primary myeloid cells Mannose receptor [36]
CLEC5A [37]
Huh Hepatocytes HS [38, 39]
HepG2 Hepatocytes Laminin receptor, GRP78, HS [40, 41]
HMEC-1 Dermal endothelium β3 integrin [42]
Hamster BHK Kidney fibroblast cells HS [43]
Glycosphingolipid [44]
CHO Ovary cells HS [28, 29]
Insect C6/36 A. albopictus larvae cells Laminin receptor (37/67 kDa) [45]
HSP related (45 kDa) [46, 47]
Prohibitin (35 kDa) [48]
CCL-125 A. Aegypti larvae cells Prohibitin (35 kDa) [48]
AP-61 A. pseudoscutellaris larvae cells Glycosphingolipid [31]
2.1.1. Human Cell DENV Attachment and Receptors. Prior tofusion, DENV needs to attach to specific cellular receptors.Because DENV can infect a variety of different cell typesisolated from different hosts (human, insect, monkey, andeven hamster), the virus must interact with a wide varietyof cellular receptors. In the last decade, several candidateattachment factor/receptors are identified (Table 1).
(1) Immune Cells (Monocytes, Dendritic Cells, and Macro-phages). Since 1977, monocytes are considered to be permis-sive for DENV infection [70]. More recent, phenotyping ofperipheral blood mononuclear cells (PBMCs) from pediatricDF and DHF cases resulted in the identification of monocytesas DENV target cells [71]. First, it was believed that mono-cytes are important during secondary DENV infections dur-ing the ADE process, because of their Fc-receptor expression.The complex formed between the nonneutralizing antibodyand the virus can bind to Fc-receptors and enhance infec-tion in neighbouring susceptible cells [13, 14, 17]. There isevidence for the expression of a trypsin-sensitive receptoron monocytes facilitating DENV infection [72]. Later, itwas shown that DENV can enter monocytes in a CD14-dependent manner, because lipopolysaccharide (LPS) caninhibit the infection [32]. After LPS binding, heat shockprotein (HSP) 70 and HSP90 are clustered around CD14,preventing them from interacting with DENV [33]. Thisindicates that HSP70 and HSP90 are part of a receptor com-plex in monocytes.
More detailed observation of the natural DENV infectionchanges the idea of monocytes being the first target cells.
Following intradermal injection of DENV-2 in mice, repre-senting the bite of an infected mosquito, DENV occurs toreplicate in the skin [73]. The primary DENV target cells inthe skin are believed to be immature dendritic cells (DCs)or Langerhans cells [16, 74–76]. Immature DCs are veryefficient in capturing pathogens whereas mature DCs are rel-atively resistant to infection. The search for cellular receptorsresponsible for DENV capture leads to the identification ofcell-surface C-type lectin DC-specific intercellular adhesionmolecule 3-grabbing nonintegrin (DC-SIGN; CD209) [34,35, 61, 77]. DC-SIGN, mainly expressed by immature DCas a tetramer, is a member of the calcium-dependent C-typelectin family and is composed out of four domains: a cyto-plasmic domain responsible for signaling and internalizationdue to the presence of a dileucine motif, a transmembranedomain, seven to eight extracellular neck repeats implicatedin the oligomerization of DC-SIGN, and a carbohydraterecognition domain (CRD) (Figure 2) [78]. The CRD recog-nizes high-mannose N-glycans and fucose-containing bloodgroup antigens [79, 80]. Importantly, DC-SIGN can binda variety of pathogens like human immunodeficiency virus(HIV) [81], hepatitis C virus (HCV) [82], Ebola virus [83],and several bacteria, parasites, and yeasts [84]. Many ofthese pathogens have developed strategies to manipulate DC-SIGN signaling to escape from an immune response [84].Following antigen capture in the periphery, DCs maturate byupregulation of the costimulatory molecules and migrate tosecondary lymphoid organs. Activated DCs are stimulatorsof naive T cells and they initiate production of cytokinesand chemokines [85]. Inhibition of the initial interaction

4 Journal of Tropical Medicine
Table 2: Overview of all described DENV entry inhibitors.
Class Compound Serotype∗ Cell line References
Fusion inhibitors 1OAN1 DENV-2 LLC-MK2 [49]
DN59 DENV-2 LLC-MK2 [50]
Compound 6 DENV-1-4 A549, BHK [51]
Tetracycline derivates DENV-2 BHK [52]
Doxorubicin derivate DENV-1, -2, -3 Vero, C6/36 [53]
NITD448 DENV-2 BHK, C6/36 [54]
Glycosidase inhibitors Castanospermine DENV-1-4 BHK [55, 56]
DENV-2 Huh-7 [55]
DNJ DENV-1 Mouse neuro 2a cells [56]
NN-DNJ DENV-2 BHK [57]
Alkylated iminocyclitol DENV-2 BHK [58]
OSL-9511 DENV-2 BHK [59]
CM-9-78 DENV-2 BHK [60]
CBAs Con A, WGA DENV-2 BHK [43]
HHA, GNA, UDA DENV-1-4 Raji/DC-SIGN, MDDC [61, 62]
DENV-1-4 Huh-7, U87/DC-SIGN Unpublished results
DENV-1-4 Raji/L-SIGN, U87/L-SIGN Unpublished results
PRM-S DENV-2 MDDC [62]
Heparan mimetics GAG DENV-2 Vero [28]
Heparin DENV-2 Vero [28, 29]
DENV-2 BHK [43]
DENV-2 Hepatocytes [38]
Suramin DENV-2 Vero, BHK [28, 63]
PI-88 DENV-2 BHK and in mice [63]
PPS DENV-2 BHK [63]
Fucoidan DENV-2 BHK [64]
Sulfated galactomannan DENV-1 C6/36 [65]
DL-galactan DENV-2, -3 Vero, HepG2 [66]
Carrageenan DENV-2, -3 Vero, HepG2 [66, 67]
α-D-glucan DENV-2 BHK [68]
Dextran sulfate 8000 DENV-2 Hepatocytes, Vero [66]
DS (MW > 500,000 Da) DENV-2 Raji/DC-SIGN [61]
Zosteric acid DENV-1-4 LLC-MK2 [69]∗
Serotype: The serotype mentioned is the serotype that has been tested and found susceptible to inhibition by the compound. Non-mentioned serotypes werenot tested or could not be inhibited by the compound.
between DENV and DC could prevent an immune response.DC-SIGN could be a target for antiviral therapy by interrupt-ing the viral entry process.
Besides DC, macrophages play a key role in the immuno-pathogenesis of DENV infection as a source of immunomod-ulatory cytokines [86]. Recently, Miller et al. showed that themannose receptor (MR; CD206) mediates DENV infectionin macrophages by recognition of the glycoproteins on theviral envelope [36]. MR is also present on monocyte-derivedDC (MDDC), and anti-MR antibodies can inhibit DENVinfection, although to a lesser extent than anti-DC-SIGNantibodies do [62]. MR differs from DC-SIGN in ligandspecificity and acts as an internalization receptor for DENVinstead of an attachment factor. Another C-type lectin,
CLEC5A (C-type lectin domain family 5, member A) ex-pressed by human macrophages can also interact with DENVand acts as a signaling receptor for the release of proin-flammatory cytokines [37]. However, whereas the DC-SIGN-DENV interaction is calcium-dependent, CLEC5A bindingto its ligand is not dependent on calcium. Mannan and fucosecan inhibit the interaction between CLEC5A and DENV,indicating that the interaction is carbohydrate-dependent[37]. However, a glycan array demonstrated that there is nobinding signal between CLEC5A and N-glycans of mammalsor insects [87]. The molecular interaction between CLEC5Aand DENV remains to be elucidated.
Immune cells, in particular dendritic cells, are the mostrelevant cells to use in the discovery of antiviral drugs against

Journal of Tropical Medicine 5
DC-SIGN
N - - C
DCA B
Figure 2: Structure of DC-SIGN. DC-SIGN, mainly expressed byhuman dendritic cells in the skin, is composed out of four domains:(A) cytoplasmic domain containing internalization signals, (B)transmembrane domain, (C) 7 or 8 extracellular neck repeats impli-cated in the oligomerization of DC-SIGN, and (D) carbohydraterecognition domain which can interact calcium-dependently with avariety of pathogens.
dengue virus, but the isolation of these cells and the charac-terization is labour intensive and time consuming.
(2) Liver Cells. The liver is an important target organ of den-gue, in particular in DHF and DSS, because liver enzymes areusually elevated [88] and apoptosis of hepatocytes has beenreported [89]. The interaction of DENV with liver cells hasbeen studied.
Heparan sulfate (HS), the most ubiquitous member ofthe glycosaminoglycan (GAG) family, present on humanhepatocytes, is described as a putative receptor for DENV[28, 29, 38, 43]. HS is also expressed by Vero cells, CHO cells,and BHK cells which are widely used in the study of denguevirus infection because of the easy cell growth conditions.HS very often acts as an attachment factor to concentratethe virus on the cell surface to facilitate binding to a secondreceptor. However, the contribution of HS to internalizeDENV appears to vary in a serotype-specific manner [39,90]. In Vero cells, a putative glycoprotein coreceptor is char-acterized of 74 kDa binding DENV-4 in a carbohydrate-dependent manner [30]. Another carbohydrate moleculecharacterized to interact with all four serotypes of DENV inBHK cells and insect cells is the terminal disaccharide of aglycosphingolipid, neolactotetraosylceramide [31, 44].
Besides HS [38, 39], glucose-regulated protein 78(GRP78) is identified as a possible liver receptor in hepato-cytes [40]. Wati et al. showed that GRP78 is also upregulatedin DENV-infected monocytes and acts as a chaperone forviral-protein production during DENV infection [91]. Livercells are important target cells during dengue virus infection,and the liver cell line Huh-7 has easy growth conditions. Ingeneral, liver cells are not widely used for studying denguevirus infection, but liver cells have more clinical relevancein contrast to monkey cells (Vero) or hamster cells (BHK)and should get more attention to use in screening discoveryprograms for antiviral drugs.
(3) Endothelial Cells. Liver/lymph node-specific ICAM-3grabbing nonintegrin (L-SIGN) is a DC-SIGN-related trans-membrane C-type lectin expressed on endothelial cells in
liver, lymph nodes, and placenta [92, 93]. Similar to DC-SIGN, L-SIGN is a calcium-dependent carbohydrate-bindingprotein and can interact with HIV [92], HCV [82], Ebolavirus [83], West Nile virus [94], and DENV [35]. Althoughendothelial cells [95] and liver endothelial cells [89] arepermissive for DENV and L-SIGN-expression makes unsus-ceptible cells susceptible for DENV infection, the in vivorole for L-SIGN in DENV entry remains to be established.Upregulation of β3 integrin has been observed followingDENV infection in human endothelial cells [42], and DENVentry is highly dependent on the expression of β3 integrin.This indicates that β3 integrin can act as an importantsecondary receptor for DENV entry in endothelial cells.
2.1.2. Mosquito Cell DENV Attachment and Receptors. DENVentry into mosquito cells is poorly understood. Previously,electron microscopic studies in the Aedes Albopictus mosqui-to cell line, C6/36, have shown that DENV penetrates directlyinto the cytoplasm by fusion at the plasma membrane [96].In contrast, experiments concentrating on cell fusion ofmosquito cells and virus inhibition with acidotropic agentshave provided evidence of viral uptake through receptor-mediated endocytosis [97]. Recently, according to overlayprotein-binding assays, two surface proteins on C6/36 cellswith molecular masses 80 en 67 kDa have been demonstratedto interact with all four serotypes of DENV [98]. This isin contrast with other reports, where a surface protein of45 kDa was identified as a receptor for DENV-4 in C6/36cells [46] which was later designated as a heat-shock-related protein (HSP related) [47]. Also, the 37/67 kDa pro-tein was identified as the laminin receptor expressed byC6/36 cells and hepatocytes [41, 45]. However, the bindingcapacity of DENV to interact with the laminin receptor isserotype-specific (only DENV-3 and DENV-4) and cell-type-dependent (only detected in larvae cells and not in adultmosquito cells). Recently, prohibitin is characterized as aDENV-2 receptor in insect cells [48]. However, it is unclearif this conserved eukaryotic protein plays a role in DENVinfection in mammalian cells.
3. The DENV Envelope
The DENV E-protein induces protective immunity, and fla-vivirus serological classification is based on its antigenic vari-ation. During replication, the virion assumes three confor-mational states: the immature, mature, and fusion-activatedform. In the immature state, the E-protein is arranged asa heterodimer and generates a “spiky” surface because thepremembrane protein (prM) covers the fusion peptide. Inthe Golgi apparatus, the virion maturates after a rearrange-ment of the E-protein. The E-heterodimer transforms to anE-homodimer and results in a “smooth” virion surface. Aftera furin cleavage of the prM to pr and M, the virion is fullymaturated and can be released from the host cell. Uponfusion, the low endosomal pH triggers the rearrangement ofthe E-homodimer into a trimer [99].
The E-protein monomer is composed out of β-barrelsorganized in three structural domains (Figure 3). The central

6 Journal of Tropical Medicine
Fusionpeptide
Asn153Asn67
CC
Asn67 Asn153
Figure 3: Location of the 2 N-glycans on the envelope protein ofDENV. The DENV E-protein dimer carries 2 N-glycans on eachmonomer at Asn67 and Asn153. β-strands are shown as ribbonswith arrows, α-helices are shown as coiled ribbons. Thin tubesrepresent connecting loops. Domain I is shown is red, domain IIis shown in yellow and contains the fusion peptide near Asn153.Domain III is shown in blue. Disulfide bridges are shown in orange.In green, the ligand N-octyl-D-glucoside is shown, which interactswith the hydrophobic pocket between domains I and II (modifiedfigure from Modis et al., PNAS, 2003) [100].
domain I contains the aminoterminus and contains twodisulphide bridges. Domain II is an extended finger-likedomain that bears the fusion peptide and stabilizes the dimer.This sequence contains three disulphide bridges and is richin glycine. Between domain I and domain II is a bindingpocket that can interact with a hydrophobic ligand, thedetergent β-N-octyl-glucoside. This pocket is an importanttarget for antiviral therapy because mutations in this regioncan alter virulence and the pH necessary for the induction ofconformational changes. The immunoglobulin-like domainIII contains the receptor-binding motif, the C-terminaldomain, and one disulphide bond [100, 101]. Monoclonalantibodies recognizing domain III are the most efficient ofblocking DENV [102, 103] and this domain is therefore aninteresting target for antiviral therapy.
Because DC-SIGN is identified as a receptor for DENVin primary DC in the skin and DC-SIGN recognizes high-mannose sugars, carbohydrates present on the E-proteinof DENV could be important for viral attachment. TheE-protein has two potential glycosylation sites: Asn67 andAsn153. Glycosylation at Asn153 is conserved in flaviviruses,with the exception of Kunjin virus [104] and is locatednear the fusion peptide in domain II [100, 101] (Figure 3).Glycosylation at Asn67 is unique for DENV [101]. The glyco-sylation at Asn67 is demonstrated to be essential for infectionof MDDC, indicating an interaction between DC-SIGN andthe glycan at Asn67 [105, 106]. Generally, the function ofglycosylation of surface proteins is proper folding of theprotein, trafficking in the endoplasmic reticulum, interactionwith receptors, and influencing virus immunogenicity [107].
There are some contradictions in terms of necessityof glycosylation of Asn67 and Asn153 during DENV viralprogeny. Johnson et al. postulated that DENV-1 and DENV-3have both sites glycosylated and that DENV-2 and DENV-4 have only one N-glycan at Asn-67 [108]. In contrast, astudy comparing the number of glycans in multiple isolatesof DENV belonging to all four serotypes led to the consensusthat all DENV strains have two N-glycans on the E-protein[109]. Nevertheless, mutant DENV lacking the glycosyla-tion at Asn153 can replicate in mammalian and insect cells,
indicating that this glycosylation is not essential for viralreplication [105, 110]. However, there is a change in pheno-type because ablation of glycosylation at Asn153 in DENVis associated with the induction of smaller plaques in com-parison to the wild type virus [105]. Asn153 is proximal tothe fusion peptide, and therefore deglycosylation at Asn153showed also an altered pH-dependent fusion activity anddisplays a lower stability [111, 112].
DENV lacking the glycosylation at Asn67 results in a re-plication-defective phenotype, because this virus infectsmammalian cells weakly and there is a reduced secretionof DENV E-protein. Replication in mosquito cells was notaffected, because the mosquito cells restore the N-glycosyl-ation at Asn67 with a compensatory site-mutation (K64N)generating a new glycosylation site [105, 113]. These data arein contrast with other published results, where was demon-strated that DENV lacking the Asn67-linked glycosylationcan grow efficiently in mammalian cells, depending on theviral strain and the amino acid substitution abolishing theglycosylation process [110]. A compensatory mutation wasdetected (N124S) to repair the growth defect without creat-ing a new glycosylation site. Thus, the glycan at Asn67 is notnecessary for virus growth, but a critical role for this glycan invirion release from mosquito cells was demonstrated [110].
Virions produced in the mosquito vector and humanhost may have structurally different N-linked glycans,because the glycosylation patterns are fundamentally differ-ent [109, 114]. N-glycosylation in mammalian cells is oftenof the complex type because a lot of different processingenzymes could add a diversity of monosaccharides. Glycansproduced in insect cells are far less complex, because of lessdiversity in processing enzymes, and usually contain morehigh-mannose and pauci-mannose-type glycans. DC-SIGNcan distinguish between mosquito and mammalian cell-derived alphavirus [115] and West Nile virus [94], resultingin a more efficient infection by a mosquito-derived virus, butthis was not the case for DENV [109].
4. DENV Entry Inhibitors
4.1. Fusion Inhibitors. By docking experiments and physic-ochemical algorithms using the structural data of the E-protein, small molecules and peptides targeting the hy-drophobic pocket are characterized as entry inhibitors ofDENV (Table 2) [49–51]. Nicholson et al. showed that twopeptide entry inhibitors, DN59 and 1OAN1, could inhibitADE in vitro, indicating that entry inhibitors could preventdevelopment of the more severe disease outcome of dengue,DHF/DSS [116]. Tetracycline derivates have been shownto interact with the hydrophobic pocket of the E-protein(Figure 3) and, due to steric hindrance, prevent conforma-tional rearrangements of the E-protein and subsequentlyprevent viral fusion [52]. A derivate of the antibiotic doxoru-bicin, SA-17, has a structure partially similar to tetracycline.SA-17 has been demonstrated to have antiviral activityagainst DENV serotype 1, 2, and 3 in Vero and C6/36 cellsand interferes with viral entry by binding to the hydropho-bic pocket of the E-protein without being virucidal [53].

Journal of Tropical Medicine 7
Recently, two fusion assays using C6/36 cells have been opti-mized to examine the antifusion activities of a variety ofcompounds. NITD448, selected in docking experiments, wasdemonstrated to inhibit DENV-2 fusion by binding to thehydrophobic pocket of the E-protein [54]. All these com-pounds can serve as lead compounds for further drug discov-ery and for further elucidation of the entry process of DENV.
4.2. Glycosidase Inhibitors. Because of the risk of ADE, it isvery important to achieve maximal protection to the sameextent against all four serotypes with one drug or vaccine.Inhibitors targeting host cell processes, as glycosylation pro-cesses, are interesting targets and could overcome this prob-lem. We will further focus on some α-glycosidase inhibitorsthat affect the modification of N-glycosylation of the viralproteins in the endoplasmic reticulum (ER).
The two lead compounds in inhibiting glycoproteinfolding are imino sugars deoxynojirimycin (DNJ) and cas-tanospermine (CSP) which mimic glucose (reviewed in[117]). CSP is a natural alkaloid derived from the black beanand is water soluble. CSP inhibits all four DENV serotypesby reducing the number of secreted particles, due to inappro-priate glycoprotein folding, and by decreasing the infectivityof the secreted DENV particles [55, 56]. DNJ exerts the samemechanism of action as castanospermine [56]. Because of thelow efficacy and cytotoxic effects, the development of iminosugars is limited. Alkylated iminocyclitol derivates, contain-ing an imino sugar head group and an N-alkyl side chain,proved to be more potent against DENV-2 and less cytotoxicthan DNJ [58]. N-alkylated derivates of DNJ (N-nonyl-DNJ(NN-DNJ)) have been shown to have increased antiviralpotency compared to DNJ, but cytotoxic effects were alsoincreased [57, 118]. However, NN-DNJ and a CSP derivateboth reduced significantly viremia in a dengue fever mousemodel [119]. Further optimization of the chemical structureof the imino sugar DNJ leads to the production of N-pentyl-(1-hydroxycyclohexyl)-DNJ (OSL-9511), an iminocyclitolwith a DNJ head group, which showed reduced cytotoxicityand retained antiviral activity against DENV [59]. Toimprove the antiviral efficacy, a hydroxyl group was removedand an oxygen atom was added. This resulted in a newcompound, CM-9-78, with exerted high anti-DENV activityand very low cytotoxicity [60]. Recently, the compound CM-9-78 and another variant CM-10-78 were tested in vivoand were shown to reduce viremia modestly by 2-fold. Toimprove the antiviral efficacy in vivo, a combination therapywas tested with ribavirin, a compound with a differentantiviral mechanism of action. Whereas ribavirin by itselfdid not reduce viremia [119], combination of CM-10-78 andribavirin demonstrated a clear enhancement in the reductionof viremia [120].
To conclude, there is a limited use of glycosidase in-hibitors because of their toxicity and low specificity, butthese compounds indeed help to understand the process ofthe E-protein glycosylation. In the last decade, not muchprogression has been made in the development of inhibitorstargeting host glycosidase enzymes by biochemical modifica-tions, but combination with other classes of inhibitors seemsto achieve the best antiviral efficacy.
4.3. Carbohydrate-Binding Agents (CBAs). The CBAs forma large group of natural proteins, and they can be isolatedfrom different organisms. Concanavalin A, isolated fromthe Jack bean, binds to mannose residues and wheat germagglutinin (WGA) binds to N-acetylglucosamine (Glc-NAc)residues. Both compounds can reduce DENV induced plaqueformation in BHK cells [43]. A competition assay, usingmannose, proved that the inhibitory effect of Con A was dueto binding α-mannose residues on the viral protein, becausemannose successfully competed with Con A [43]. Recently,three plant lectins, Hippeastrum hybrid (HHA), Galanthusnivalis (GNA), and Urtica dioica (UDA), isolated from theamaryllis, snowdrop, and stinging nettle, respectively, havebeen shown to inhibit DENV-2 infection in Raji/DC-SIGNcells [61]. Binding studies revealed that the CBAs act duringthe adsorption phase of the virus to the host cell. HHA andGNA have been shown to interact with mannose-residues[121, 122], and UDA can recognize specifically Glc-NAcresidues [123]. Mannose and Glc-NAc molecules are presentin the backbone of the high-mannose type glycans on theviral envelope protein. Because DC-SIGN can also recognizethese sugar molecules, the interaction between DC-SIGNand DENV E-glycoprotein is disrupted by HHA, GNA,and UDA. DC-SIGN, present on DC in the skin [16], isimportant during the first steps of a natural infection andthus forms an important target to focus on. The antiviralactivity profile of the CBAs has been extended using differentcell types. Recently, the antiviral activity of HHA, GNA, andUDA has been demonstrated in primary MDDC against allfour DENV serotypes, and, importantly, the potency of thethree CBAs was much higher in MDDC than in DC-SIGNtransfected cell lines, such as Raji/DC-SIGN [62]. Raji cellsand U87 cells transfected with L-SIGN, a DC-SIGN-relatedreceptor, can be infected with DENV and this infection canalso be inhibited with the three plant lectins (Figure 4 andunpublished data). However, since plant lectins are expensiveto isolate in large quantities and not orally bioavailable, thesearch for nonpeptidic small molecules is necessary. PRM-S is a highly soluble nonpeptidic small-size carbohydrate-binding antibiotic and proved to inhibit DENV-2 in MDDC[62]. These data indicate that targeting the initial interactionbetween the N-glycans on the DENV envelope and the hostcell is promising and that the CBAs have broad spectrumantiviral activity.
4.4. Heparan Mimetics. Because HS is a putative receptor forDENV, it is interesting to target the E-protein-HS interactionwith soluble GAGs and other highly charged polyanionsmimicking HS to prevent DENV entry (Table 2). GAG andheparin, a more highly sulfated protein than HS, can preventbinding of DENV to Vero cells and BHK cells [28]. DomainIII of the E-protein is responsible for the interaction withHS [124]. It has been widely assumed that domain III isconserved within each DENV serotype and it is a goodtarget for vaccines, because it contains epitopes recognizedby neutralizing antibodies [102, 103].
The pharmaceutical product suramin, a small polyanionmimicking the structure of HS, and persulfated GAGs canbind to the polyanion-binding site of the DENV E-protein

8 Journal of Tropical Medicine
U87 U87/DC-SIGN U87/L-SIGN
HH
A1μ
MIn
fect
edU
ninf
ecte
d
(a)
Relative red fluorescence
Rel
ativ
e ce
ll n
um
ber
Raji/L-SIGN
012
0
104103102101104103102101100
104103102101104103102101
012
0
100
012
0
100
012
0
100
VC
MFI: 12 80 nM
MFI: 48
MFI: 80 MFI: 1.4
16 nM
400 nM
(b)
Figure 4: Antiviral activity of HHA in DC-SIGN and L-SIGN transfected cell lines. (a) U87, U87/DC-SIGN, and U87/L-SIGN cells wereinfected with DENV-2 in the presence or absence of HHA. DENV-2 infection was analyzed by confocal microscopy using specific DENVantibodies as previously described [62]. The cell nucleus is shown in blue (Dapi) and DENV-2 infected cells are shown in green (anti-DENVAb + Alexa 488). (b) Raji/L-SIGN cells were infected with DENV-2 in the presence or absence of HHA, and viral infection was analyzed byflow cytometry using specific DENV antibodies. The open histogram represents uninfected cells. The upper left red histogram shows thevirus control (VC), and the mean fluorescence of intensity (MFI) is indicated in each panel. HHA was added at different concentrations(400–80–16 nM), and the MFI shows the dose-dependent inhibition of the DENV-2 infection in Raji/L-SIGN cells. Comparable antiviralactivity of HHA in Raji/DC-SIGN cells was obtained [61].
[125] and can inhibit DENV infection. Pentosan polysulfate(PPS) and the sulfated polysaccharide PI-88, which arecurrently in clinical trials for antitumor activity, inhibitDENV-2 infection in BHK cells. In IFN-α/γ receptor knock-out mice, a mouse model for DENV, PI-88 demonstrated anincrease in survival time [63] whereas suramin and PPS didnot show a beneficial effect in vivo.
Fucoidan, a sulfated polysaccharide isolated from marinealga, has specifically antiviral activity against DENV-2 inBHK cells and not against the other serotypes [64]. This is inagreement with others, where was demonstrated that sulfatedpolysaccharides from red seaweeds, carrageenan, and DL-galactan had antiviral activity against DENV-2 and DENV-3 but a very weak and no antiviral activity against DENV-4and DENV-1, respectively, in human hepatocytes and Verocells. The polysaccharides were not inhibitory in mosquitocells. Together with the fact that sulfated galactomannansare proved to be inhibitors of DENV-1 in C6/36 cells [65],these data indicate that the antiviral activity of sulfatedpolysaccharides is serotype- and cell-type-dependent [66].
Heparin analogues often have anticoagulant activitiesand this forms a major restriction factor for their use asantiviral product. Thus the search for polysaccharides withfewer side effects is imperative. DL-galactan from red sea-weed lacks cytotoxic effects and anticoagulant propertiesand exhibits a high antiviral activity against DENV-2 [126].Next, two α-D-glucans were isolated from a widely usedChinese herb with several therapeutic activities. These two
polysaccharides exhibit anti-DENV-2 activity in BHK cellsand sulfated derivates of one of the compounds provedeven to be more potent [68]. This is in accordance withprevious findings demonstrating that the antiviral activity ofpolysaccharides increases with molecular weight and degreeof sulfation [28, 125].
There are some contrasting data concerning the antiviralactivity of dextran sulfate. Dextran sulfate with molecularweight 8000 Da (DS8000) has been shown to have antiviralactivity against DENV-2 in human hepatocytes and Verocells [66]. This is in contrast with our data, where DS5000had no antiviral activity against DENV-2 in Raji/DC-SIGNcells and Vero cells [61]. High molecular weight DS (MW =500,000 Da) had no antiviral activity against DENV in Verocells [28, 61], but recently this compound had been shown toinhibit DENV-2 in human Raji/DC-SIGN cells [61]. Thesedata reinforce the idea that the entry process and therebythe antiviral activity of sulfated polyanions is cell-type- andserotype-dependent.
Another sulfated compound is the antiadhesive com-pound p-sulfoxy-cinnamic acid, zosteric acid, derived froma marine eelgrass. It showed to be nontoxic and inhibitoryagainst all four serotypes in LLC-MK2 cells [69]. It has beenshown that this compound promotes inappropriate virus-cell attachment and prevents virus entry.
In general, binding studies revealed that polysaccharidesact during virus adsorption and internalization [66, 127].The mechanism of action of carrageenan is by inhibition

Journal of Tropical Medicine 9
of a postadsorption process, namely, the release of the viralnucleocapsid into the cytoplasm, probably due to the inter-action with the E-protein [67]. The antiviral effect of HSmimetics is probably due to steric hindrance and the negativecharged sulfate groups, but there is a dose-limiting effectdue to their anticoagulant activity. The antiviral activity ofsulfated polyanions is cell-type- and serotype-dependent andthus not suitable for further clinical testing.
5. Conclusion
DENV is able to infect many types of host cells and thisresulted in the identification of several putative DENV recep-tors. DCs in the skin are believed to be the first target cells,and therefore DC-SIGN is assumed to be the most importantDENV receptor until now. The unraveling of the entryprocess of DENV into the host cell and the recent progressesin virtual screening and docking techniques have lead to thedevelopment of a new class of DENV inhibitors, entry in-hibitors. This class of compounds has great potential tobe used either alone or in combination therapy with viralreplication inhibitors. It has been shown that entry inhibitorscan prevent ADE in human cells and subsequently immuneactivation [116]. This indicates a very important featurefor further development of entry inhibitors and for futureclinical studies.
Acknowledgments
The work of the authors was supported by the KatholiekeUniversiteit Leuven (GOA no. 10/014 and PF/10/018) and theFWO (no. G.485.08).
References
[1] S. B. Halstead, “Dengue virus-mosquito interactions,” An-nual Review of Entomology, vol. 53, pp. 273–291, 2008.
[2] T. Solomon and M. Mallewa, “Dengue and other emergingflaviviruses,” Journal of Infection, vol. 42, no. 2, pp. 104–115,2001.
[3] J. G. Rigau-Perez, G. G. Clark, D. J. Gubler, P. Reiter, E. J.Sanders, and A. V. Vorndam, “Dengue and dengue haemor-rhagic fever,” Lancet, vol. 352, no. 9132, pp. 971–977, 1998.
[4] S. B. Halstead, “Dengue,” Lancet, vol. 370, no. 9599, pp.1644–1652, 2007.
[5] D. J. Gubler, “Dengue and dengue hemorrhagic fever,” Clini-cal Microbiology Reviews, vol. 11, no. 3, pp. 480–496, 1998.
[6] S. Murrell, S. C. Wu, and M. Butler, “Review of dengue virusand the development of a vaccine,” Biotechnology Advances,vol. 29, no. 2, pp. 239–247, 2011.
[7] S. S. Whitehead, J. E. Blaney, A. P. Durbin, and B. R. Murphy,“Prospects for a dengue virus vaccine,” Nature ReviewsMicrobiology, vol. 5, no. 7, pp. 518–528, 2007.
[8] R. Takhampunya, S. Ubol, H. S. Houng, C. E. Cameron,and R. Padmanabhan, “Inhibition of dengue virus replicationby mycophenolic acid and ribavirin,” Journal of GeneralVirology, vol. 87, no. 7, pp. 1947–1952, 2006.
[9] M. S. Diamond, M. Zachariah, and E. Harris, “Mycophenolicacid inhibits dengue virus infection by preventing replicationof viral RNA,” Virology, vol. 304, no. 2, pp. 211–221, 2002.
[10] Y. L. Chen, Z. Yin, S. B. Lakshminarayana et al., “Inhibitionof dengue virus by an ester prodrug of an adenosine analog,”Antimicrobial Agents and Chemotherapy, vol. 54, no. 8, pp.3255–3261, 2010.
[11] J. M. Crance, N. Scaramozzino, A. Jouan, and D. Garin,“Interferon, ribavirin, 6-azauridine and glycyrrhizin: antivi-ral compounds active against pathogenic flaviviruses,”Antiviral Research, vol. 58, no. 1, pp. 73–79, 2003.
[12] P. Leyssen, E. De Clercq, and J. Neyts, “Perspectives for thetreatment of infections with Flaviviridae,” Clinical Microbiol-ogy Reviews, vol. 13, no. 1, pp. 67–82, 2000.
[13] A. Takada and Y. Kawaoka, “Antibody-dependent enhance-ment of viral infection: molecular mechanisms and in vivoimplications,” Reviews in Medical Virology, vol. 13, no. 6, pp.387–398, 2003.
[14] S. C. Kliks, A. Nisalak, W. E. Brandt, L. Wahl, and D. S. Burke,“Antibody-dependent enhancement of dengue virus growthin human monocytes as a risk factor for dengue hemorrhagicfever,” American Journal of Tropical Medicine and Hygiene,vol. 40, no. 4, pp. 444–451, 1989.
[15] A. T. A. Mairuhu, J. Wagenaar, D. P. M. Brandjes, and E. C.M. Van Gorp, “Dengue: an arthropod-borne disease of globalimportance,” European Journal of Clinical Microbiology andInfectious Diseases, vol. 23, no. 6, pp. 425–433, 2004.
[16] S. J. L. Wu, G. Grouard-Vogel, W. Sun et al., “Humanskin Langerhans cells are targets of dengue virus infection,”Nature Medicine, vol. 6, no. 7, pp. 816–820, 2000.
[17] Z. Kou, M. Quinn, H. Chen et al., “Monocytes, but not T orB cells, are the principal target cells for dengue virus (DV)infection among human peripheral blood mononuclearcells,” Journal of Medical Virology, vol. 80, no. 1, pp. 134–146,2008.
[18] R. J. Kuhn, W. Zhang, M. G. Rossmann et al., “Structure ofdengue virus: implications for flavivirus organization, matu-ration, and fusion,” Cell, vol. 108, no. 5, pp. 717–725, 2002.
[19] E. G. Acosta, V. Castilla, and E. B. Damonte, “Functionalentry of dengue virus into Aedes albopictus mosquito cellsis dependent on clathrin-mediated endocytosis,” Journal ofGeneral Virology, vol. 89, no. 2, pp. 474–484, 2008.
[20] H. M. Van Der Schaar, M. J. Rust, Chen et al., “Dissecting thecell entry pathway of dengue virus by single-particle trackingin living cells,” PLoS Pathogens, vol. 4, no. 12, Article IDe1000244, 2008.
[21] J. J. H. Chu and M. L. Ng, “Infectious entry of West Nile virusoccurs through a clathrin-mediated endocytic pathway,”Journal of Virology, vol. 78, no. 19, pp. 10543–10555, 2004.
[22] M. Nawa, T. Takasaki, K. I. Yamada, I. Kurane, and T. Akat-suka, “Interference in Japanese encephalitis virus infection ofVero cells by a cationic amphiphilic drug, chlorpromazine,”Journal of General Virology, vol. 84, no. 7, pp. 1737–1741,2003.
[23] E. G. Acosta, V. Castilla, and E. B. Damonte, “Alternativeinfectious entry pathways for dengue virus serotypes intomammalian cells,” Cellular Microbiology, vol. 11, no. 10, pp.1533–1549, 2009.
[24] Y. Modis, S. Ogata, D. Clements, and S. C. Harrison, “Struc-ture of the dengue virus envelope protein after membranefusion,” Nature, vol. 427, no. 6972, pp. 313–319, 2004.
[25] K. Stiasny, R. Fritz, K. Pangerl, and F. X. Heinz, “Molecularmechanisms of flavivirus membrane fusion,” Amino Acids,vol. 41, no. 5, pp. 1159–1163, 2009.
[26] Y. Zhang, W. Zhang, S. Ogata et al., “Conformational changesof the flavivirus E glycoprotein,” Structure, vol. 12, no. 9, pp.1607–1618, 2004.

10 Journal of Tropical Medicine
[27] C. S. S. Martın, C. Y. Liu, and M. Kielian, “Dealing with lowpH: entry and exit of alphaviruses and flaviviruses,” Trends inMicrobiology, vol. 17, no. 11, pp. 514–521, 2009.
[28] Y. Chen, T. Maguire, R. E. Hileman et al., “Dengue virus in-fectivity depends on envelope protein binding to target cellheparan sulfate,” Nature Medicine, vol. 3, no. 8, pp. 866–871,1997.
[29] R. Germi, J. M. Crance, D. Garin et al., “Heparan sulfate-mediated binding of infectious dengue virus type 2 and yel-low fever virus,” Virology, vol. 292, no. 1, pp. 162–168, 2002.
[30] J. J. Martınez-Barragan and R. M. Del Angel, “Identificationof a putative coreceptor on Vero cells that participates indengue 4 virus infection,” Journal of Virology, vol. 75, no. 17,pp. 7818–7827, 2001.
[31] S. Wichit, A. Jittmittraphap, K. I. Hidari et al., “Denguevirus type 2 recognizes the carbohydrate moiety of neu-tral glycosphingolipids in mammalian and mosquito cells,”Microbiology and Immunology, vol. 55, no. 2, pp. 135–140,2011.
[32] Y. C. Chen, S. Y. Wang, and C. C. King, “Bacterial lipo-polysaccharide inhibits dengue virus infection of primaryhuman monocytes/macrophages by blockade of virus entryvia a CD14-dependent mechanism,” Journal of Virology, vol.73, no. 4, pp. 2650–2657, 1999.
[33] J. Reyes-Del Valle, S. Chavez-Salinas, F. Medina, and R. M.Del Angel, “Heat shock protein 90 and heat shock protein 70are components of dengue virus receptor complex in humancells,” Journal of Virology, vol. 79, no. 8, pp. 4557–4567, 2005.
[34] E. Navarro-Sanchez, R. Altmeyer, A. Amara et al., “Den-dritic-cell-specific ICAM3-grabbing non-integrin is essentialfor the productive infection of human dendritic cells bymosquito-cell-derived dengue viruses,” EMBO Reports, vol.4, no. 7, pp. 723–728, 2003.
[35] B. Tassaneetrithep, T. H. Burgess, A. Granelli-Piperno etal., “DC-SIGN (CD209) mediates dengue virus infection ofhuman dendritic cells,” Journal of Experimental Medicine, vol.197, no. 7, pp. 823–829, 2003.
[36] J. L. Miller, B. J. M. DeWet, L. Martinez-Pomares et al.,“The mannose receptor mediates dengue virus infection ofmacrophages,” PLoS Pathogens, vol. 4, no. 2, article e17, 2008.
[37] S. T. Chen, Y. L. Lin, M. T. Huang et al., “CLEC5A is criticalfor dengue-virus-induced lethal disease,” Nature, vol. 453,no. 7195, pp. 672–676, 2008.
[38] P. Hilgard and R. Stockert, “Heparan sulfate proteoglycansinitiate dengue virus infection of hepatocytes,” Hepatology,vol. 32, no. 5, pp. 1069–1077, 2000.
[39] Y. L. Lin, H. Y. Lei, Y. S. Lin, T. M. Yeh, S. H. Chen, andH. S. Liu, “Heparin inhibits dengue-2 virus infection of fivehuman liver cell lines,” Antiviral Research, vol. 56, no. 1, pp.93–96, 2002.
[40] S. Jindadamrongwech, C. Thepparit, and D. R. Smith, “Iden-tification of GRP 78 (BiP) as a liver cell expressed receptorelement for dengue virus serotype 2,” Archives of Virology, vol.149, no. 5, pp. 915–927, 2004.
[41] C. Thepparit and D. R. Smith, “Serotype-specific entry ofdengue virus into liver cells: identification of the 37-kilodalton/67-kilodalton high-affinity laminin receptor as adengue virus serotype 1 receptor,” Journal of Virology, vol. 78,no. 22, pp. 12647–12656, 2004.
[42] J. L. Zhang, J. L. Wang, N. Gao, Z. T. Chen, Y. P. Tian, andJ. An, “Up-regulated expression of β3 integrin induced bydengue virus serotype 2 infection associated with virusentry into human dermal microvascular endothelial cells,”
Biochemical and Biophysical Research Communications, vol.356, no. 3, pp. 763–768, 2007.
[43] S. L. Hung, P. L. Lee, H. W. Chen, L. K. Chen, C. L. Kao, andC. C. King, “Analysis of the steps involved in dengue virusentry into host cells,” Virology, vol. 257, no. 1, pp. 156–167,1999.
[44] C. Aoki, K. I. P. J. Hidari, S. Itonori et al., “Identification andcharacterization of carbohydrate molecules in mammaliancells recognized by dengue virus type 2,” Journal of Biochem-istry, vol. 139, no. 3, pp. 607–614, 2006.
[45] P. Sakoonwatanyoo, V. Boonsanay, and D. R. Smith, “Growthand production of the dengue virus in C6/36 cells andidentification of a laminin-binding protein as a candidateserotype 3 and 4 receptor protein,” Intervirology, vol. 49, no.3, pp. 161–172, 2006.
[46] J. S. Salas-Benito and R. M. Del Angel, “Identification of twosurface proteins from C6/36 cells that bind dengue type 4virus,” Journal of Virology, vol. 71, no. 10, pp. 7246–7252,1997.
[47] J. Salas-Benito, J. R. D. Valle, M. Salas-Benito, I. Ceballos-Olvera, C. Mosso, and R. M. Del Angel, “Evidence that the45-kD glycoprotein, part of a putative dengue virus receptorcomplex in the mosquito cell line C6/36, is a heat-shock-related protein,” American Journal of Tropical Medicine andHygiene, vol. 77, no. 2, pp. 283–290, 2007.
[48] A. Kuadkitkan, N. Wikan, C. Fongsaran, and D. R. Smith,“Identification and characterization of prohibitin as a recep-tor protein mediating DENV-2 entry into insect cells,”Virology, vol. 406, no. 1, pp. 149–161, 2010.
[49] J. M. Costin, E. Jenwitheesuk, S. M. Lok et al., “Structuraloptimization and de novo design of dengue virus entryinhibitory peptides,” PLoS Neglected Tropical Diseases, vol. 4,no. 6, article no. e721, 2010.
[50] Y. M. Hrobowski, R. F. Garry, and S. F. Michael, “Peptideinhibitors of dengue virus and West Nile virus infectivity,”Virology Journal, vol. 2, article 49, 2005.
[51] Q. Y. Wang, S. J. Patel, E. Vangrevelinghe et al., “A small-molecule dengue virus entry inhibitor,” Antimicrobial Agentsand Chemotherapy, vol. 53, no. 5, pp. 1823–1831, 2009.
[52] J. M. Yang, Y. F. Chen, Y. Y. Tu, K. R. Yen, and Y. L. Yang,“Combinatorial computational approaches to identify tetra-cycline derivatives as flavivirus inhibitors,” PLoS One, vol. 2,no. 5, article no. e428, 2007.
[53] S. J. F. Kaptein, T. De Burghgraeve, M. Froeyen et al., “Aderivate of the antibiotic doxorubicin is a selective inhibitorof dengue and yellow fever virus replication in vitro,”Antimicrobial Agents and Chemotherapy, vol. 54, no. 12, pp.5269–5280, 2010.
[54] M. K. Poh, A. Yip, S. Zhang et al., “A small molecule fusioninhibitor of dengue virus,” Antiviral Research, vol. 84, no. 3,pp. 260–266, 2009.
[55] K. Whitby, T. C. Pierson, B. Geiss et al., “Castanospermine,a potent inhibitor of dengue virus infection in vitro and invivo,” Journal of Virology, vol. 79, no. 14, pp. 8698–8706,2005.
[56] M. P. Courageot, M. P. Frenkiel, C. Duarte Dos Santos, V.Deubel, and P. Despres, “α-Glucosidase inhibitors reducedengue virus production by affecting the initial steps ofvirion morphogenesis in the endoplasmic reticulum,” Journalof Virology, vol. 74, no. 1, pp. 564–572, 2000.
[57] S. F. Wu, C. J. Lee, C. L. Liao, R. A. Dwek, N. Zitzmann, andY. L. Lin, “Antiviral effects of an iminosugar derivative onflavivirus infections,” Journal of Virology, vol. 76, no. 8, pp.3596–3604, 2002.

Journal of Tropical Medicine 11
[58] P. H. Liang, W. C. Cheng, Y. L. Lee et al., “Novel five-membered iminocyclitol derivatives as selective and potentglycosidase inhibitors: new structures for antivirals andosteoarthritis,” ChemBioChem, vol. 7, no. 1, pp. 165–173,2006.
[59] B. Gu, P. Mason, L. Wang et al., “Antiviral profiles of noveliminocyclitol compounds against bovine viral diarrhea virus,West Nile virus, dengue virus and hepatitis B virus,” AntiviralChemistry and Chemotherapy, vol. 18, no. 1, pp. 49–59, 2007.
[60] J. Chang, L. Wang, D. Ma et al., “Novel imino sugar deriva-tives demonstrate potent antiviral activity against flavivirus-esv,” Antimicrobial Agents and Chemotherapy, vol. 53, no. 4,pp. 1501–1508, 2009.
[61] M. M. F. Alen, S. J. F. Kaptein, T. De Burghgraeve, J. Balzarini,J. Neyts, and D. Schols, “Antiviral activity of carbohydrate-binding agents and the role of DC-SIGN in dengue virusinfection,” Virology, vol. 387, no. 1, pp. 67–75, 2009.
[62] M. M.F. Alen, T. de Burghgraeve, S. J.F. Kaptein, J. Balzarini,J. Neyts, and D. Schols, “Broad Antiviral activity ofCarbohydrate-binding agents against the four serotypes ofdengue virus in monocyte-derived dendritic cells,” PLoS One,vol. 6, no. 6, article e21658, 2011.
[63] E. Lee, M. Pavy, N. Young, C. Freeman, and M. Lobigs, “Anti-viral effect of the heparan sulfate mimetic, PI-88, againstdengue and encephalitic flaviviruses,” Antiviral Research, vol.69, no. 1, pp. 31–38, 2006.
[64] K. I. P. J. Hidari, N. Takahashi, M. Arihara, M. Nagaoka,K. Morita, and T. Suzuki, “Structure and anti-dengue virusactivity of sulfated polysaccharide from a marine alga,” Bio-chemical and Biophysical Research Communications, vol. 376,no. 1, pp. 91–95, 2008.
[65] L. Ono, W. Wollinger, I. M. Rocco, T. L. M. Coimbra, P. A. J.Gorin, and M. R. Sierakowski, “In vitro and in vivo antiviralproperties of sulfated galactomannans against yellow fevervirus (BeH111 strain) and dengue 1 virus (Hawaii strain),”Antiviral Research, vol. 60, no. 3, pp. 201–208, 2003.
[66] L. B. Talarico, C. A. Pujol, R. G. M. Zibetti et al., “Theantiviral activity of sulfated polysaccharides against denguevirus is dependent on virus serotype and host cell,” AntiviralResearch, vol. 66, no. 2-3, pp. 103–110, 2005.
[67] L. B. Talarico and E. B. Damonte, “Interference in denguevirus adsorption and uncoating by carrageenans,” Virology,vol. 363, no. 2, pp. 473–485, 2007.
[68] H. Qiu, W. Tang, X. Tong, K. Ding, and J. Zuo, “Structureelucidation and sulfated derivatives preparation of two α-d-glucans from Gastrodia elata Bl. and their anti-dengue virusbioactivities,” Carbohydrate Research, vol. 342, no. 15, pp.2230–2236, 2007.
[69] C. R. Rees, J. M. Costin, R. C. Fink et al., “In vitro inhibitionof dengue virus entry by p-sulfoxy-cinnamic acid and struc-turally related combinatorial chemistries,” Antiviral Research,vol. 80, no. 2, pp. 135–142, 2008.
[70] S. B. Halstead, E. J. O’Rourke, and A. C. Allison, “Dengueviruses and mononuclear phagocytes. II. Identity of bloodand tissue leukocytes supporting in vitro infection,” Journalof Experimental Medicine, vol. 146, no. 1, pp. 218–229, 1977.
[71] A. P. Durbin, M. J. Vargas, K. Wanionek et al., “Phenotypingof peripheral blood mononuclear cells during acute dengueillness demonstrates infection and increased activation ofmonocytes in severe cases compared to classic dengue fever,”Virology, vol. 376, no. 2, pp. 429–435, 2008.
[72] C. C. Daughaday, W. E. Brandt, J. M. McCown, and P. K.Russell, “Evidence for two mechanisms of dengue virus infec-tion of adherent human monocytes: trypsin-sensitive virus
receptors and trypsin-resistant immune complex receptors,”Infection and Immunity, vol. 32, no. 2, pp. 469–473, 1981.
[73] S. Taweechaisupapong, S. Sriurairatana, S. Angsubhakornet al., “Langerhans cell density and serological changesfollowing intradermal immunisation of mice with dengue 2virus,” Journal of Medical Microbiology, vol. 45, no. 2, pp. 138–145, 1996.
[74] M. Marovich, G. Grouard-Vogel, M. Louder et al., “Humandendritic cells as targets of dengue virus infection,” Journal ofInvestigative Dermatology Symposium Proceedings, vol. 6, no.3, pp. 219–224, 2001.
[75] D. H. Libraty, S. Pichyangkul, C. Ajariyakhajorn, T. P. Endy,and F. A. Ennis, “Human dendritic cells are activated bydengue virus infection: enhancement by gamma interferonand implications for disease pathogenesis,” Journal of Virol-ogy, vol. 75, no. 8, pp. 3501–3508, 2001.
[76] L. J. Ho, J. J. Wang, M. F. Shaio et al., “Infection of humandendritic cells by Dengue virus causes cell maturation andcytokine production,” Journal of Immunology, vol. 166, no. 3,pp. 1499–1506, 2001.
[77] P. Y. Lozach, L. Burleigh, I. Staropoli et al., “Dendriticcell-specific intercellular adhesion molecule 3-grabbing non-integrin (DC-SIGN)-mediated enhancement of dengue virusinfection is independent of DC-SIGN internalization sig-nals,” Journal of Biological Chemistry, vol. 280, no. 25, pp.23698–23708, 2005.
[78] D. A. Mitchell, A. J. Fadden, and K. Drickamer, “A novelmechanism of carbohydrate recognition by the C-type lectinsDC-SIGN and DC-SIGNR. Subunit organization and bind-ing to multivalent ligands,” Journal of Biological Chemistry,vol. 276, no. 31, pp. 28939–28945, 2001.
[79] H. Feinberg, D. A. Mitchell, K. Drickamer, and W. I. Weis,“Structural basis for selective recognition of oligosaccharidesby DC-SIGN and DC-SIGNR,” Science, vol. 294, no. 5549, pp.2163–2166, 2001.
[80] B. J. Appelmelk, I. Van Die, S. J. Van Vliet, C. M. J. E.Vandenbroucke-Grauls, T. B. H. Geijtenbeek, and Y. VanKooyk, “Cutting edge: carbohydrate profiling identifies newpathogens that interact with dendritic cell-specific ICAM-3-grabbing nonintegrin on dendritic cells,” Journal of Immunol-ogy, vol. 170, no. 4, pp. 1635–1639, 2003.
[81] T. B. H. Geijtenbeek, D. S. Kwon, R. Torensma et al., “DC-SIGN, a dendritic cell-specific HIV-1-binding protein thatenhances trans-infection of T cells,” Cell, vol. 100, no. 5, pp.587–597, 2000.
[82] S. Pohlmann, J. Zhang, F. Baribaud et al., “Hepatitis Cvirus glycoproteins interact with DC-SIGN and DC-SIGNR,”Journal of Virology, vol. 77, no. 7, pp. 4070–4080, 2003.
[83] A. Marzi, P. Moller, S. L. Hanna et al., “Analysis of the inter-action of Ebola virus glycoprotein with DC-SIGN (dendriticcell-specific intercellular adhesion molecule 3-grabbing non-integrin) and its homologue DC-SIGNR,” Journal of Infec-tious Diseases, vol. 196, no. 2, pp. S237–S246, 2007.
[84] Y. Van Kooyk and T. B. H. Geijtenbeek, “DC-SIGN: escapemechanism for pathogens,” Nature Reviews Immunology, vol.3, no. 9, pp. 697–709, 2003.
[85] J. Banchereau and R. M. Steinman, “Dendritic cells and thecontrol of immunity,” Nature, vol. 392, no. 6673, pp. 245–252, 1998.
[86] Y. C. Chen and S. Y. Wang, “Activation of terminally differen-tiated human monocytes/macrophages by dengue virus: pro-ductive infection, hierarchical production of innate cytokinesand chemokines, and the synergistic effect of lipopolysaccha-ride,” Journal of Virology, vol. 76, no. 19, pp. 9877–9887, 2002.

12 Journal of Tropical Medicine
[87] A. A. Watson, A. A. Lebedev, B. A. Hall et al., “Structuralflexibility of the macrophage dengue virus receptor CLEC5A:implications for ligand binding and signaling,” Journal ofBiological Chemistry, vol. 286, no. 27, pp. 24208–24218, 2011.
[88] Y. L. Lin, C. C. Liu, H. Y. Lei et al., “Infection of five humanliver cell lines by dengue-2 virus,” Journal of Medical Virology,vol. 60, no. 4, pp. 425–431, 2000.
[89] S. L. Seneviratne, G. N. Malavige, and H. J. de Silva, “Patho-genesis of liver involvement during dengue viral infections,”Transactions of the Royal Society of Tropical Medicine andHygiene, vol. 100, no. 7, pp. 608–614, 2006.
[90] C. Thepparit, W. Phoolcharoen, L. Suksanpaisan, and D. R.Smith, “Internalization and propagation of the dengue virusin human hepatoma (HepG2) cells,” Intervirology, vol. 47, no.2, pp. 78–86, 2004.
[91] S. Wati, M. L. Soo, P. Zilm et al., “Dengue virus infectioninduces upregulation of GRP78, which acts to chaperoneviral antigen production,” Journal of Virology, vol. 83, no. 24,pp. 12871–12880, 2009.
[92] S. Pohlmann, E. J. Soilleux, F. Baribaud et al., “DC-SIGNR, aDC-SIGN homologue expressed in endothelial cells, binds tohuman and simian immunodeficiency viruses and activatesinfection in trans,” Proceedings of the National Academy ofSciences of the United States of America, vol. 98, no. 5, pp.2670–2675, 2001.
[93] A. A. Bashirova, T. B. H. Geijtenbeek, G. C. F. Van Duijn-hoven et al., “A dendritic cell-specific intercellular adhesionmolecule 3-grabbing nonintegrin (DC-SIGN)-related pro-tein is highly expressed on human liver sinusoidal endothelialcells and promotes HIV-1 infection,” Journal of ExperimentalMedicine, vol. 193, no. 6, pp. 671–678, 2001.
[94] C. W. Davis, H. Y. Nguyen, S. L. Hanna, M. D. Sanchez, R.W. Doms, and T. C. Pierson, “West nile virus discriminatesbetween DC-SIGN and DC-SIGNR for cellular attachmentand infection,” Journal of Virology, vol. 80, no. 3, pp. 1290–1301, 2006.
[95] P. Avirutnan, P. Malasit, B. Seliger, S. Bhakdi, and M.Husmann, “Dengue virus infection of human endothelialcells leads to chemokine production, complement activation,and apoptosis,” Journal of Immunology, vol. 161, no. 11, pp.6338–6346, 1998.
[96] T. Hase, P. L. Summers, and K. H. Eckels, “Flavivirus entryinto cultured mosquito cells and human peripheral bloodmonocytes,” Archives of Virology, vol. 104, no. 1-2, pp. 129–143, 1989.
[97] V. B. Randolph and V. Stollar, “Low pH-induced cell fusionin flavivirus-infected Aedes albopictus cell cultures,” Journalof General Virology, vol. 71, no. 8, pp. 1845–1850, 1990.
[98] R. F. Mercado-Curiel, H. A. Esquinca-Aviles, R. Tovar, A.Dıaz-Badillo, M. Camacho-Nuez, and M. D. L. Munoz,“The four serotypes of dengue recognize the same putativereceptors in Aedes aegypti midgut and Ae. albopictus cells,”BMC Microbiology, vol. 6, article no. 85, 2006.
[99] R. Perera, M. Khaliq, and R. J. Kuhn, “Closing the dooron flaviviruses: entry as a target for antiviral drug design,”Antiviral Research, vol. 80, no. 1, pp. 11–22, 2008.
[100] Y. Modis, S. Ogata, D. Clements, and S. C. Harrison,“A ligand-binding pocket in the dengue virus envelopeglycoprotein,” Proceedings of the National Academy of Sciencesof the United States of America, vol. 100, no. 12, pp. 6986–6991, 2003.
[101] F. A. Rey, F. X. Heinz, C. Mandl, C. Kunz, and S. C. Harrison,“The envelope glycoprotein from tick-borne encephalitis
virus at 2 A resolution,” Nature, vol. 375, no. 6529, pp. 291–298, 1995.
[102] W. D. Crill and J. T. Roehrig, “Monoclonal antibodies thatbind to domain III of dengue virus E glycoprotein are themost efficient blockers of virus adsorption to vero cells,”Journal of Virology, vol. 75, no. 16, pp. 7769–7773, 2001.
[103] R. Rajamanonmani, C. Nkenfou, P. Clancy et al., “On amouse monoclonal antibody that neutralizes all four denguevirus serotypes,” Journal of General Virology, vol. 90, no. 4,pp. 799–809, 2009.
[104] J. H. Scherret, J. S. Mackenzie, A. A. Khromykh, and R. A.Hall, “Biological significance of glycosylation of the envelopeprotein of Kunjin virus,” Annals of the New York Academy ofSciences, vol. 951, pp. 361–363, 2001.
[105] J. A. Mondotte, P. Y. Lozach, A. Amara, and A. V. Gamarnik,“Essential role of dengue virus envelope protein N glycosy-lation at asparagine-67 during viral propagation,” Journal ofVirology, vol. 81, no. 13, pp. 7136–7148, 2007.
[106] E. Pokidysheva, Y. Zhang, A. J. Battisti et al., “Cryo-EM reconstruction of dengue virus in complex with thecarbohydrate recognition domain of DC-SIGN,” Cell, vol.124, no. 3, pp. 485–493, 2006.
[107] D. J. Vigerust and V. L. Shepherd, “Virus glycosylation: role invirulence and immune interactions,” Trends in Microbiology,vol. 15, no. 5, pp. 211–218, 2007.
[108] A. J. Johnson, F. Guirakhoo, and J. T. Roehrig, “The envelopeglycoproteins of dengue 1 and dengue 2 viruses grownin mosquito cells differ in their utilization of potentialglycosylation sites,” Virology, vol. 203, no. 2, pp. 241–249,1994.
[109] K. Hacker, L. White, and A. M. de Silva, “N-linked glycans ondengue viruses grown in mammalian and insect cells,” Jour-nal of General Virology, vol. 90, no. 9, pp. 2097–2106, 2009.
[110] E. Lee, S. K. Leang, A. Davidson, and M. Lobigs, “Both Eprotein glycans adversely affect dengue virus infectivity butare beneficial for virion release,” Journal of Virology, vol. 84,no. 10, pp. 5171–5180, 2010.
[111] F. Guirakhoo, A. R. Hunt, J. G. Lewis, and J. T. Roehrig,“Selection and partial characterization of dengue 2 virusmutants that induce fusion at elevated pH,” Virology, vol.194, no. 1, pp. 219–223, 1993.
[112] E. Lee, R. C. Weir, and L. Dalgarno, “Changes in the denguevirus major envelope protein on passaging and their local-ization on the three-dimensional structure of the protein,”Virology, vol. 232, no. 2, pp. 281–290, 1997.
[113] J. E. Bryant, A. E. Calvert, K. Mesesan et al., “Glycosylation ofthe dengue 2 virus E protein at N67 is critical for virus growthin vitro but not for growth in intrathoracically inoculatedAedes aegypti mosquitoes,” Virology, vol. 366, no. 2, pp. 415–423, 2007.
[114] K. M. Rogers and M. Heise, “Modulation of cellular tropismand innate antiviral response by viral glycans,” Journal ofInnate Immunity, vol. 1, no. 5, pp. 405–412, 2009.
[115] W. B. Klimstra, E. M. Nangle, M. S. Smith, A. D. Yurochko,and K. D. Ryman, “DC-SIGN and L-SIGN can act as attach-ment receptors for alphaviruses and distinguish betweenmosquito cell- and mammalian cell-derived viruses,” Journalof Virology, vol. 77, no. 22, pp. 12022–12032, 2003.
[116] C. O. Nicholson, J. M. Costin, D. K. Rowe et al., “Viral entryinhibitors block dengue antibody-dependent enhancementin vitro,” Antiviral Research, vol. 89, no. 1, pp. 71–74, 2011.
[117] A. C. Sayce, J. L. Miller, and N. Zitzmann, “Targeting a hostprocess as an antiviral approach against dengue virus,” Trendsin Microbiology, vol. 18, no. 7, pp. 323–330, 2010.

Journal of Tropical Medicine 13
[118] A. Mehta, S. Ouzounov, R. Jordan et al., “Imino sugarsthat are less toxic but more potent as antivirals, in vitro,compared with N-n-nonyl DNJ,” Antiviral Chemistry andChemotherapy, vol. 13, no. 5, pp. 299–304, 2002.
[119] W. Schul, W. Liu, H. Y. Xu, M. Flamand, and S. G. Vasudevan,“A dengue fever viremia model in mice shows reductionin viral replication and suppression of the inflammatoryresponse after treatment with antiviral drugs,” Journal ofInfectious Diseases, vol. 195, no. 5, pp. 665–674, 2007.
[120] J. Chang, W. Schul, T. D. Butters et al., “Combination ofα-glucosidase inhibitor and ribavirin for the treatment ofdengue virus infection in vitro and in vivo,” AntiviralResearch, vol. 89, no. 1, pp. 26–34, 2011.
[121] N. Shibuya, I. J. Goldstein, E. J. Van Damme, and W. J.Peumans, “Binding properties of a mannose-specific lectinfrom the snowdrop (Galanthus nivalis) bulb,” Journal ofBiological Chemistry, vol. 263, no. 2, pp. 728–734, 1988.
[122] H. Kaku, E. J. M. Van Damme, W. J. Peumans, and I. J.Goldstein, “Carbohydrate-binding specificity of the daffodil(Narcissus pseudonarcissus) and amaryllis (Hippeastrumhybr.) bulb lectins,” Archives of Biochemistry and Biophysics,vol. 279, no. 2, pp. 298–304, 1990.
[123] N. Shibuya, I. J. Goldstein, J. A. Shafer, W. J. Peumans, andW. F. Broekaert, “Carbohydrate binding properties of thestinging nettle (Urtica dioica) rhizome lectin,” Archives ofBiochemistry and Biophysics, vol. 249, no. 1, pp. 215–224,1986.
[124] J. J. Hung, M. T. Hsieh, M. J. Young, C. L. Kao, C. C. King, andW. Chang, “An external loop region of domain III of denguevirus type 2 envelope protein is involved in serotype-specificbinding to mosquito but not mammalian cells,” Journal ofVirology, vol. 78, no. 1, pp. 378–388, 2004.
[125] R. M. Marks, H. Lu, R. Sundaresan et al., “Probing theinteraction of dengue virus envelope protein with heparin:assessment of glycosaminoglycan-derived inhibitors,” Journalof Medicinal Chemistry, vol. 44, no. 13, pp. 2178–2187, 2001.
[126] C. A. Pujol, J. M. Estevez, M. J. Carlucci, M. Ciancia, A.S. Cerezo, and E. B. Damonte, “Novel DL-galactan hybridsfrom the red seaweed Gymnogongrus torulosus are potentinhibitors of herpes simplex virus and dengue virus,” Antivi-ral Chemistry and Chemotherapy, vol. 13, no. 2, pp. 83–89,2002.
[127] X. K. Tong, H. Qiu, X. Zhang et al., “WSS45, a sulfated α-D-glucan, strongly interferes with Dengue 2 virus infectionin vitro,” Acta Pharmacologica Sinica, vol. 31, no. 5, pp. 585–592, 2010.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 960329, 5 pagesdoi:10.1155/2012/960329
Research Article
Molecular Typing of Dengue Virus Circulating in Kolkata, Indiain 2010
Arindam Sarkar, Debjani Taraphdar, and Shyamalendu Chatterjee
ICMR Virus Unit, Kolkata, ID & BG Hospital Campus 57, Dr. S. C. Banerjee Road, Beliaghata, Kolkata 700010, India
Correspondence should be addressed to Shyamalendu Chatterjee, [email protected]
Received 7 September 2011; Revised 19 October 2011; Accepted 20 October 2011
Academic Editor: Aditya Prasad Dash
Copyright © 2012 Arindam Sarkar et al. This is an open access article distributed under the Creative Commons AttributionLicense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properlycited.
Dengue is one of the major public health threats in Kolkata. Every year, blood samples with dengue-like illness are referred tous from different medical colleges and hospitals in Kolkata for the detection of dengue infection in them. In 2010, a total of 378samples were referred to us for that purpose. All the samples were tested for the detection of IgM antibodies by ELISA method,followed by RT-PCR test for the detection of serotypes. Only 173 samples were ELISA positive. Out of 378 samples, 108 were RT-PCR positive. Out of 108 samples, 74 samples had monotypic infection with different serotypes of DENV and 33 samples had dualinfections with DENV-2 and DENV-3. Only one sample had the infection with DENV-1, DENV-2, and DENV-3. DHF was foundmainly among the patients, infected with multiple dengue serotypes. Only 3 dengue monotypic infected patients had suffered fromDHF.
1. Introduction
During the past few decades, dengue fever has graduallybecome one of the leading causes of morbidity and mortalityin tropical and subtropical areas throughout the world [1].The Dengue virus (DENV), a mosquito-borne member ofthe family Flaviviridae, circulates as four distinct serologicaltypes DENV 1, DENV 2, DENV 3, and DENV 4. Over all,two-fifth of the world population are living in areas, at riskfor dengue [2–4]. These four sero types offer cross protectionfor a very short period. Infection with any of these leadsto a mild self-limiting febrile illness (dengue fever, DF).A more severe form of the disease, dengue hemorrhagicfever/dengue shock syndrome (DHF/DSS), is responsible forhigh mortality rate, especially in children [5]. It has beenestimated that about 50 million cases of DF occur annually,with 10,000 infant deaths due to DHF/DSS. DHF/DSS hasbeen postulated to result from immune enhancement after asecond heterologous DENV infection [6].
In India, DENV was first isolated in 1946 and manyoutbreaks have been reported [7–10]. DHF was first reportedin Calcutta (Kolkata), West Bengal in 1963 [11], again in1964 [12]. Since then, there are numerous studies from theIndian subcontinent investigating DHF in various parts ofthe country [13–22]. But there are no studies investigating
the overall prevalence of the dengue serotype circulating inthe endemic zone, apart from the epidemic outbreak. Thepurpose of this paper is to present a comprehensive reporton the diagnosis of dengue infection amongst the febrilecases, available from January to December, 2010, in the city ofKolkata and also to identify the serotype presently circulatingin this region.
The incidence of DF in the rural West Bengal is onthe increase and is spreading to geographic regions notpreviously affected [23, 24]. It is widely known that dengue isendemic in Kolkata. The city has experienced several dengueepisodes in the past centuries [25]. Antibodies against GroupB-arthropod-borne viruses in more than 80% of the Kolkatapopulation have been recorded almost fifty years back, andthat is too possibly due to the infection by dengue viruses[26].
The present study aimed to identify the serotypes ofDENV in the population of Kolkata as well as to study thesociodemographic status in relation to DENV infection.
2. Materials and Methods
2.1. Study Area. Kolkata is one of the biggest metropolitancities in India. The present population of Kolkata is 44,86,679

2 Journal of Tropical Medicine
of which 23,62,662 are males and 21,24,017 are females [27].The city has an international sea and airport and one rail waystation (Sealdah) which is busiest in the world. The rail roadof this station covers a number of districts, situated at theborder of Bangladesh. Adjacent to the city, there is a thicklypopulated town, Howrah, which has one of the biggestterminating railway stations of the Eastern India. These tworail stations are the gateway of this city. The monsoon beginsin June and persists up to the end of October.
2.2. Patients and Clinical Specimens. Cases were mainlyreferred from outpatient department (OPD) and indoor ofI.D & B. G Hospital, attached to this unit, from differentmedical colleges as well as other hospitals in Kolkata alongwith a short history of the patients. A good number ofcases were referred to us by the private practitioners also.In the matter of selection of dengue fever (DF) cases, thefollowing criteria were initially considered: (1) high fever; (2)head ache; (3) retro-orbital pain; (4) nausea/vomiting; (5)malaise/joint pain; (6) generalized skin rashes [28]. In thepresent study two or more of these criteria, apart from fever,were fulfilled. The possibilities of bacterial and prokaryoticetiology in the collected samples were excluded throughinvestigations at the respective hospitals.
The case history and the investigations of the patientswere compiled. In the case of DHF, the history of illness wasrevealed by the sudden rise of high fever (38.3◦C–39.4◦C),headache, retro-orbital pain, conjunctival congestion, andfacial flashing. Fever sustained for 2–15 days. In additionto that, some cases had the history of hemorrhagic man-ifestation either with petechiae or with gum bleeding ormalena. In such cases, intermittent or biphasic course offever was recorded, where the first phase of fever persistedfor 2–7 days and the second bout of fever persisted for 2–3 days. No cases with the history of plasma leakage wereobserved. In the admitted cases, we found that fever was alsoaccompanied by generalized malaise and lumbosacral pain.Pulse rate was slow (60–70/min). Those patients representedrashes, appeared on 2–5 days of illness in limbs, sparingpalm, and souls. They were nonpruritic in nature andlasted 2–7 days. The hematological examination revealedgeneralized leucopenia, and platelet count was ≤105/cu mm.All the cases were nondiabetic and had no other physiologicalcomplications. Liver was either nonpalpable or just palpable.
All the samples were transported on dry ice to the ICMRVirus Unit. Sera were separated from the collected bloodsamples, were stored at −80◦C, and were tested within 1month from the date of collection. A total of 378 sampleswere thus received from the suspected cases and analyzed forthe detection of dengue viruses, if any.
2.3. Serology. To study the sociodemographic status in rela-tion to DENV infection, all the 378 samples were screenedfor the presence of dengue IgM antibodies by IgM captureenzyme-linked immunosorbent assay (ELISA): using a kit,prepared by the National Institute of virology, Pune, India,following the prescribed protocol [29]. Optical density (OD)was measured at 492 nm using an ELISA reader (TitertekMultiskan Plus, Lab systems Finland, Type-314).
2.4. RNA Extraction. To study the molecular typing ofDENV, attempts were made to isolate the RNA from all thesamples as well as from four different DENV serotype strains,which were used as positive control. Viral RNA was isolatedby using Qiagen viral RNA isolation kit (Qiagen, GmbH,Hilden, Germany) according to the manufacturer’s protocol.
2.5. RT-PCR. In this study, published primers by Lanciottiet al. were used [30]. In a single tube, viral RNA wasconverted to a DNA copy (cDNA) prior to enzymaticDNA amplification by the use of reverse transcriptase (RT)and the DENV downstream consensus primer D2-5′-TTG-CACCAACAGTCAATGTCTTCAGGTTC-3′ homologousto the genomic RNA of the four serotypes. Subsequent Taqpolymerase amplification was performed on the resultingcDNA with the upstream dengue virus consensus primer D1-5′-TCAATATGCTGAAACGCGCGAGAAACCG-3′. TargetRNA was amplified in 25 μL volumes containing the fol-lowing components: 800 mM deoxynucleotide triphosphates(dNTPs), 8 mM dithiothreitol, 0.24 μM each of primers D1and D2, 0.5 U of AMV RT (Promega, Madison, WI, USA),and 0.625 U of Dreamtaq DNA polymerase (Fermentas Inc.,USA). The reactions were allowed to proceed for 1 h at 42◦Cand then to proceed with 95◦C for 3 minutes for initialdenaturation followed by 35 cycles of denaturation (95◦Cfor 30 sec), primer annealing (55◦C for 1 min), and primerextension (72◦C for 2 min) along with final extension (72◦Cfor 5 min).
DENV serotyping was conducted by second-roundamplification (nested PCR) initiated with 10 u of dilutedmaterial (1 : 100 in sterile distilled water) from the initialamplification reaction. The total 20 μL of reaction mixturewas prepared using 2 μL of diluted first PCR products,0.8 mM dNTPs, 0.5 U of Dreamtaq DNA Polymerase and0.3 μM of primer D1 and 0.3 μM of dengue virus type-specific primers: TS1 5′-CGTCTCAGTGATCCGGGGG-3′, TS2 5′-CGCCACAAGGGCCATGAACAG-3′, TS3 5′-TAACATCATCATGAGACAGAGC-3′, and TS4 5′-CTC-TGTTGTCTTAAACAAGAGA-3′. Dithiothreitol and AMVRT were eliminated. The samples were subjected to initialdenaturation (95◦C for 3 min) followed by 20 cycles ofdenaturation (95◦C for 30 s), primer annealing (55◦C for1 min), and primer extension (72◦C for 1 min) along withfinal extension (72◦C for 5 min). The PCR products wereanalyzed by running a 1.5% agarose gel stained withethidium bromide.
3. Results
3.1. Serology. Out of 378 samples collected, only 173 sampleswere reactive to dengue IgM antibody by ELISA method.Maximum numbers of IgM positive cases were observedin the age group of 0–10 years in both male and femalepatients (Figure 1). Females were more affected (46.5%) thanthe males (45.1%). As regards the seasonal prevalence, it isevident from the result that although sporadic cases obtainedthroughout the year,dengue cases started from the month ofjuly and attained maximum number of cases in the month ofnovember (Figure 2).

Journal of Tropical Medicine 3
0
10
20
30
40
50
60
70
>50
Age group
Male (positivity %)
0–10 11–20 21–30 31–40 41–50
Female (positivity %)
IgM
per
cen
tage
pos
itiv
ity
Figure 1: Age and sex wise distribution of dengue IgM-positivecases in 2010.
0102030405060708090
100
Jan
uar
y
Febr
uar
y
Mar
ch
Apr
il
May
Jun
e
July
Au
gust
Sept
embe
r
Oct
ober
Nov
embe
r
Dec
embe
r
Month
IgM
pos
itiv
e ca
ses
No. positive
Figure 2: Monthly distributions of IgM-positive dengue cases in2010.
3.2. PCR Result. Out of 378 samples, 108 were RT-PCRpositive. Seventy-four samples (68.5%) had the DENVinfection by single different serotypes, of which 7 samples(9.5%) had the monotypic infection with DENV-1, 45samples (60.8%) had the monotypic infection with DENV-2and 22 samples (29.7%) had the monotypic infections withDENV-3 serotype. Both DENV-2 and DENV-3 serotypeswere detected in 33 samples (30.6%). Only one samplehad all the three serotypes, that is, DENV-1, DENV-2,and DENV-3. No DENV-4 serotype was detected in thosesamples. Out of 22 DHF cases, 3 were found with single-serotype infection and 18 cases with dual infections of DENV2 and DENV 3. Only a female patient of 24 years of agehad the infection with DENV-1, DENV-2, and DENV-3serotypes at a time and also suffered from DHF. Clinical dataregarding the death of the DHF cases was inadequate to reachany conclusion about the severity of illness. The specimencontaining DENV-1, DENV-2, and/or DENV-3 is identifiedby the detection of a DNA band of 482, 119, or 290 bp in size,respectively, on 1.5% agarose gel, loaded with nested PCR
482 bp
119 bp
290 bp
CS2
0
S18
S19
S17
S16
S15
S14 S1S13
S12
S11
S10 S9 S8 S7 S6 S5 S4 S3 S2 L
Figure 3: Results of dengue-specific RT-PCR followed by second-round nested PCR of RNA samples, showing band in 1.5% agarosegel electrophoresis stained with ethidium bromide. Lane L: 100 bpDNA ladder, Lane S1–S8 and S10: negative sample, Lane S9, S14and S20: sample positive for DEN-2 (119 bp), Lane S11–S13 andS16–S19: sample with dual infection of DEN-2 (119 bp) and DEN-3 (290 bp), Lane S15: sample with concurrent infection of DEN-1 (482 bp), DEN-2 (119 bp), and DEN-3 (290 bp), and Lane C:negative control.
products along with positive controls, stained with ethidiumbromide (Figure 3).
4. Discussion
The monitoring of DENV activity is required for publichealth importance, as the dengue fever and DHF/DSS areincreasing worldwide and are spreading in the places, whereit was previously not reported. The first isolation of DENVserotype 1 and 4 was reported from India in 1964 [31, 32]and serotype 3 in 1968 [18]. Although concurrent infectionwith more than one serotype of DENV in the same individualis uncommon, high percentage of concurrent infectionswith different DENV serotypes had been detected at anoutbreak in Delhi, India, in 2006 [33]. Kolkata is a dengueendemic zone; frequent outbreaks of DF and DHF have beenoccurring since last centuries. In Kolkata, dengue was firstdocumented in 1824 and several epidemics took place in thecity during the years 1836, 1906, 1911, and 1972, affecting40% of the city people [34]. The last large-scale dengueoutbreak has been recorded in the year 2005 [35]. In therural areas of West Bengal, dengue is gradually spreading andestablishes new reports [23, 24]. No continuous monitoringof the molecular detection of the dengue serotype has yetbeen attempted in the city of Kolkata, either in epidemic orin sporadic dengue outbreaks.
Out of 378 blood samples, initially 173 (45.76%) caseswere reactive to dengue IgM antibody. Agewise distributionrevealed that the highest number of dengue cases weredetected in the age group of 0–10 years, followed by 11–20 years and above (Figure 1). In the highest age group(above 50 years), the number of positive cases were too smalland only 16.6% dengue IgM positivity was found in themale individuals. In all the age groups, females were moreaffected than the males (Figure 1). As the vector mosquitoes

4 Journal of Tropical Medicine
(Aedes sp.) are domestic and peridomestics in nature, thefemales get more exposure than the males, as most of thetime they reside inside the house. During the year-roundstudy, although small number of samples from suspecteddengue cases were referred to us during the period fromJanuary to May, only a few were positive to dengue IgMantibody by ELISA method. It is evident from our study(Figure 2) that the dengue cases actually started from themonth of June and attained its peak in the month ofNovember during this year, which is the post-monsoonperiod. It may be explained by the fact that the stagnant freshwater during the rainy seasons (June to October) favouredthe breeding of the vector mosquitoes.
For the molecular detection, RT-PCR was performedwith all samples, of which 108 samples were positive by thatmethod. Forty-one samples were both ELISA and RT PCRpositive. A total of 74 samples had the monotypic infections,involving DENV 1, DENV 2, and DENV 3, of which DENV 2was predominated. All these were IgM negative. Conversely,33 samples had the dual infections with DENV 2 and DENV3, of which all the samples were IgM reactive. Only onesample produced prominent band against DENV1, DENV 2,and DENV 3 and also contained IgM antibody. The detectionof the viral RNA in presence of the IgM antibody may beexplained by the fact that, due to the consecutive infection,the IgM detected in those samples possibly appeared dueto the initial infection, which is evident by the intensity ofthe bands in gel electrophoresis (Figure 3). The hemorrhagicmanifestation was found mainly among the patients, infectedwith multiple dengue serotypes. Only 3 dengue monotypicinfected patients had suffered from DHF. DHF cases wereobserved mainly among the young and young-adult agegroups (0–30 years) which might be due to the absence ofimmunity against all serotypes of DENV in them.
Although the increasing trend of cocirculation of mul-tiple DENV serotypes suggests that Kolkata is becominga hyperendemic state, a large-scale monitoring on thecirculating strains of DENV is highly required to draw adefinite conclusion.
Funding
The authors received all sorts of financial help from theDepartment of Health and Family Welfare, Government ofWest Bengal, India, to carry out the work in the ICMR VirusUnit, Kolkata, India.
Acknowledgments
The authors express their sincere gratitude to all the staffmembers of ICMR Virus Unit, for their constant help andassistance to carry out the laboratory investigations andcompilation of data. They also gratefully acknowledge thehelp they received from N.I.V, Pune, India, for providingthem the specific ELISA kits for the detection of IgMantibody. The enthusiastic help obtained from the doctors ofthe medical colleges and hospitals, for providing them withthe clinically suspected samples for this study, is gratefullyacknowledged. They are indebted to the Officer-In-Charge,
ICMR Virus Unit, for allowing them to carry out the workin this department. A. Sarkar and D. Taraphdar contributedequally to this work.
References
[1] T. P. Monath, “Dengue,” in The Arboviruses; Ecology and Epi-demiology, T. P. Monath, Ed., vol. 2, pp. 224–260, CRC Press,Boca, Raton, Fla, USA, 1988.
[2] W. J. H. McBride and H. Bielefeldt-Ohmann, “Dengue viralinfections; pathogenesis and epidemiology,” Microbes and In-fection, vol. 2, no. 9, pp. 1041–1050, 2000.
[3] E. A. Henchal and J. R. Putnak, “The Dengue viruses,” ClinicalMicrobiology Reviews, vol. 3, no. 4, pp. 376–396, 1990.
[4] T. Solomon and M. Mallewa, “Dengue and other emergingflaviviruses,” Journal of Infection, vol. 42, no. 2, pp. 104–115,2001.
[5] World Health Organization, “Dengue and Dengue haemor-rhagic fever,” Fact sheet, pp. 117, 1996.
[6] S. B. Halstead, “Pathogenisis of dengue: challenges to molecu-lar biology,” Science, vol. 239, no. 4839, pp. 476–481, 1988.
[7] S. Balaya, S. D. Paul, L. V. D’Lima, and K. M. Pavri, “Inves-tigations on an outbreak of dengue in Delhi in 1967,” IndianJournal of Medical Research, vol. 57, no. 4, pp. 767–774, 1969.
[8] F. M. Rodrigues, M. R. Patankar, K. Banerjee et al., “Etiology ofthe 1965 epidemic of febrile illness in Nagpur city, Maharash-tra State, India,” Bulletin of the World Health Organization, vol.46, no. 2, pp. 173–179, 1972.
[9] V. S. Padbidri, C. N. Dandawate, and M. K. Goverdhan, “Aninvestigation of the aetiology of the 1971 outbreak of febrileillness in Jaipur city, India,” Indian Journal of Medical Research,vol. 61, no. 12, pp. 1737–1743, 1973.
[10] P. V. Karamchandani, “Study of 100 cases of dengue fever inMadras Penitentiary,” Indian Med Gazette, vol. 72, pp. 532–534, 1973.
[11] B. K. Aikat, N. R. Konar, and G. Banerjee, “Haemorrhagicfever in Calcutta area,” Indian Journal of Medical Research, vol.152, pp. 660–675, 1964.
[12] J. K. Sarkar, S. K. Chakravarty, and R. K. Sarkar, “Sporadiccases of haemorrhage and/or shock during dengue epidemics,”Transactions of the Royal Society of Tropical Medicine andHygiene, vol. 66, no. 6, pp. 875–877, 1972.
[13] S. N. Ghosh, K. M. Pavri, and K. R. P. Singh, “Investigationson the outbreak of dengue fever in Ajmer City, Rajasthan Statein 1969. Part I. Epidemiological, clinical and virological studyof the epidemic,” Indian Journal of Medical Research, vol. 62,no. 4, pp. 511–522, 1974.
[14] G. S. Chouhan, F. M. Rodrigues, B. H. Shaikh et al., “Clinicaland virological study of dengue fever outbreak in Jalore city,Rajasthan 1985,” Indian Journal of Medical Research, vol. 91,pp. 414–418, 1990.
[15] P. Seth, S. Broor, L. Dar, S. Sengupta, and M. Chakraborty,“Dengue outbraeak in Delhi laboratory diagnosis,” in DengueOutbreaks in Delhi, P. L. Sarma and O. P. Sood, Eds., pp. 28–30,Ranbaxi Science Foundation, Gurgaon, India, 1996.
[16] S. Broor, L. Dar, S. Sengupta, and M. Chakraborty, “Recentdengue epidemic in Delhi, India,” in Factors in the Emergenceof Arbo Virus Diseases, J. F. Saluzzo and B. Dodet, Eds., pp.

Journal of Tropical Medicine 5
123–128, Elsevier, Amsterdam, The Netherlands, 1996.
[17] S. Broor, L. Dar, S. Sengupta, I. Xess, and P. Seth, “The firstmajor outbreak of dengue hemorrhagic fever in Delhi, India,”Emerging Infectious Diseases, vol. 5, no. 4, pp. 589–590, 1999.
[18] R. M. Myers, M. J. Varkey, R. Reuben, and E. S. Jesudass,“Dengue outbreak in Vellore, southern India, in 1968, withisolation of four dengue types from man and mosquitoes,”Indian Journal of Medical Research, vol. 58, no. 1, pp. 24–30,1970.
[19] G. B. Banik, T. K. Pal, A. Mondal, M. S. Chakraborty, and S.K. Chakravarty, “Dengue haemorrhagic fever In Calcutta,”Indian Paediatr, vol. 31, pp. 685–687, 1994.
[20] T. Cherian, E. Ponnuraj, T. Kurruvila, C. Kirybakaran, T. J.John, and P. Raghupati, “An epidemic of dengue haemorrhagicfever & dengue shock syndrome in and around Vellore,” IndianJournal of Medical Research, vol. 106, pp. 1–3, 1994.
[21] H. Kaur, H. Prabhakar, P. Mathew, R. Marshalla, and M. Arya,“Dengue haemorrhagic fever outbreak in October-November1996 in Ludhiana, Punjab, India,” Indian Journal of MedicalResearch, vol. 106, pp. 1–3, 1997.
[22] M. Kurukumbi, J. P. Wali, S. Broor et al., “Seroepidemiologyand active surveillance of dengue fever/dengue haemorrhagicfever in Delhi,” Indian Journal of Medical Sciences, vol. 55, no.3, pp. 149–156, 2001.
[23] D. Taraphdar, A. Sarkar, M. K. Bhattacharya, and S. Chatterjee,“Sero diagnosis of dengue activity in an unknown febrileoutbreak at the Siliguri Town, District Darjeeling, WestBengal,” Asian Pacific Journal of Tropical Medicine, vol. 3, no.5, pp. 364–366, 2010.
[24] A. Sarkar, D. Taraphdar, and S. Chatterjee, “Investigations ofRecurrent outbreaks of unknown fever, establish rural dengueactivity in West Midnapore, a costal district in West Bengal,India,” Archives of Clinical Microbiology, vol. 1, no. 3, 2010.
[25] J. F. Siler, M. W. Hall, and A. P. Hitchens, “Dengue its history,epidemiology, mechanism of transmission, etiology, clinicalmanifestations, immunity and prevention,” Philippine Journalof Science, vol. 29, pp. 1–304, 1926.
[26] J. K. Sarkar and S. N. Chatterjee, “Survey of antibodies againstarthropod-borne viruses in the human sera collected fromCalcutta and other areas of West Bengal,” Indian Journal ofMedical Research, vol. 50, pp. 833–841, 1962.
[27] KMC 2010, “Data available from: department of censes,Kolkata Municipal Corporation,” Assessment year, 2010.
[28] T. P. Monath and T. F. Tsai, “Flaviruses,” in Clinical Virology, D.D. Richman, R. J. Whitley, and F. G. Hayden, Eds., pp. 1133–1186, Churchill Livingstone, New York, NY, USA, 1997.
[29] D. Cecilia, M. B. Kakade, A. B. Bhagat et al., “Detection ofdengue-4 virus in pune, western india after an absence of 30years—its association with two severe cases,” Virology Journal,vol. 8, no. 46, 2011.
[30] R. S. Lanciotti, C. H. Calisher, D. J. Gubler, G. J. Chang,and A. V. Vorndam, “Rapid detection and typing of dengueviruses from clinical samples by using reverse transcriptase-polymerase chain reaction,” Journal of Clinical Microbiology,vol. 30, no. 3, pp. 545–551, 1992.
[31] D. E. Carey, R. M. Myers, and R. Reuben, “Dengue types 1 and4 viruses in wild-caught mosquitoes in South India,” Science,vol. 143, no. 3602, pp. 131–132, 1964.
[32] R. M. Myers, D. E. Carey, F. M. Rodrigues, and C. E. Klontz,“The isolation of dengue type 4 virus from human sera in
south India,” The Indian Journal of Medical Research, vol. 52,pp. 559–565, 1964.
[33] P. Bharaj, H. S. Chahar, A. Pandey et al., “Concurrent infec-tions by all four dengue virus serotypes during an outbreak ofdengue in 2006 in Delhi, India,” Virology Journal, vol. 5, article1, 2008.
[34] A. K. Hati, “Studies on dengue and dengue haemorrhagicfever(DHF) in West Bengal State, India,” Journal of Commu-nicable Diseases, vol. 38, no. 2, pp. 124–129, 2006.
[35] A. K. Hati, “Dengue serosurveillance in Kolkata, facing anepidemic in West Bengal, India,” Journal of Vector BorneDiseases, vol. 46, no. 3, pp. 197–204, 2009.

Hindawi Publishing CorporationJournal of Tropical MedicineVolume 2012, Article ID 652564, 7 pagesdoi:10.1155/2012/652564
Research Article
Effectiveness of Space Spraying on the Transmission ofDengue/Dengue Hemorrhagic Fever (DF/DHF) in an Urban Areaof Southern Thailand
Suwich Thammapalo,1 Supaporn Meksawi,2 and Virasakdi Chongsuvivatwong3
1 Office of Disease Prevention and Control 12, Department of Disease Control, Ministry of Public Health, Songkhla 90000, Thailand2 Faculty of Health and Sports Science, Thaksin University, Phatthalung 93110, Thailand3 Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Songkhla 90112, Thailand
Correspondence should be addressed to Supaporn Meksawi, [email protected]
Received 10 September 2011; Accepted 1 November 2011
Academic Editor: Carlos E. P. Corbett
Copyright © 2012 Suwich Thammapalo et al. This is an open access article distributed under the Creative Commons AttributionLicense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properlycited.
Timely and extensive space spraying has been widely used to prevent the spread of dengue fever/dengue hemorrhagic fever(DF/DHF). Field evaluations on its effectiveness have been rarely reported. This study aimed to evaluate the timeliness, coverage,and effectiveness of space spraying for DF/DHF control using a geographic information system (GIS). Longitudinal monitoring ofDF/DHF cases and spray activities in Songkhla municipality was done between May 2006 and April 2007. After a case was detected,subsequent cases occurring within a 100 meter radius of the index case’s house and between 16–35 days of onset were considered aspotential secondary cases. During the study period, 140 cases of DF/DHF were detected. Of these, 25 were identified as secondaryinfections from 20 index cases. Where a secondary infection occurred, the mean attack rate was 2.7 per 1,000 population. Twosignificant predictors for being a secondary case were both related to the house of the index case, namely, absence of window screensand being constructed with corrugated iron sheets. Our findings suggest that space spraying in the study area was inadequate andoften failed to prevent secondary cases of DF/DHF. Control programs should target houses constructed with corrugated ironsheets.
1. Introduction
Dengue fever (DF), dengue hemorrhagic fever (DHF), ordengue shock syndrome (DSS) is one of the most importantmosquito-borne viral diseases caused by one of four closelyrelated, but antigenically distinct, virus serotypes (DENV-1,DENV-2, DENV-3, and DENV-4), of the genus Flavivirus.The virus is maintained in a cycle that involves humans andAedes aegypti, transmitted by an infected female mosquitothat is primarily a daytime feeder and mainly bites in themorning or late in the afternoon [1]. The transmission cyclestarts when the female Aedes mosquito takes blood from aperson during the viraemic phase (acute febrile) of illnessand then becomes infected with the dengue virus. After anextrinsic incubation period of 8 to 12 days [2], the salivaryglands of the mosquito become infected, and the virus istransmitted when the infective mosquito bites and injects the
salivary fluid into the blood of another person. Following anincubation period in humans (intrinsic incubation period)of 3 to 14 days (average of 4 to 7 days) [2], there is often asudden onset of the disease, with fever, headache, myalgias,loss of appetite, and a variety of nonspecific signs andsymptoms, including nausea, vomiting, and rash. Infectionwith dengue viruses may produce a spectrum of clinicalillnesses ranging from asymptomatic and nonspecific viralsyndrome to severe and fatal hemorrhagic disease. Viraemiais usually present at the time of or just before the onset ofsymptoms and lasts an average of 5 to 9 days after the onsetof illness. Symptoms caused by dengue infection may last3 to 10 days, with an average of 5 days [3], after the onsetof symptoms. This is the crucial period when the patientis most infective for the vector mosquito and contributesto maintaining the transmission cycle if the patient is notprotected against vector mosquito bites. Infection with one

2 Journal of Tropical Medicine
of four dengue virus serotypes does not provide long-termcross-protective immunity, so a person living in a dengue-endemic area can have four dengue infections from theirlifetime.
The trend of DF and DHF has increased epidemicdengue activity and increased incidence. DF and DHF aredistributed in most tropical and subtropical area, in which968,564 cases reported from 65 countries worldwide [4].Associated risk factors for DHF outbreaks have focused onenvironmental factor, housing conditions, and human den-sity. Environmental factors such as increased temperatures,numbers of rainy days, relative humidity, and rainfall [5, 6]have been found to be associated with DHF incidence. Thetransmission of dengue virus is sensitive with a seasonalvariation since temperature changes affect vector-borne viraldisease transmission and epidemic potential by the vector’sreproductive rate, biting rate, and length of the extrinsicincubation period (EIP) [7], which increases from 3 daysunder 32◦C to 14 days when the temperature is 20◦C [8].Other environmental factors, including housing conditionssuch as solid waste disposal problems, inadequate watersupply, and absence of window screens [9], are also knownto affect transmission rates. Virus transmission also increaseswith human population density. Urbanization in tropicalcountries has resulted in both a propagation of Ae. aegyptiand an increase in the number of susceptible human hosts. Incities, the movement of viraemic persons is a more importantmeans of transporting dengue viruses than movement of Ae.aegypti mosquitoes [10]. Vector control is the most effectivemethod for killing vectors as quickly as possible and toreduce vector density. Control methods include modificationor manipulation of environmental factors with a view topreventing or reducing vector proliferation and human-vector-pathogen contact.
Space spraying, spreading of microscopic droplets ofinsecticide in the air to kill adult mosquitoes, is an emergencycontrol measure when an outbreak of dengue has occurred[11]. The standard operational guidelines recommended byWHO for an area with a surveillance system in place is tospray within a radius of 100 meters of affected houses andwithin 24 hours after receiving the case notification. Sprayingshould also be repeated at 7–10 day-intervals. A parousrate, the number of gravid female mosquitoes capturedper house per person, of 10% or less within two daysafter spraying indicates that the spraying has been effective[12]. However, even with the implementation of widespreadspace spraying, the global DHF incidence has dramaticallyincreased. Songkhla province in southern Thailand is a highendemic area for DF/DHF even though space spraying fordengue prevention and control was implemented since 2002.The annual incidence rate of DF/DHF in Songkhla provincereported from the Bureau of epidemiology unit, Thailandduring January–April in the year 2009 was 55 per 100,000population compared to the national average of 11.7 per100,000 population [12]. This may reflect the failure ofoutbreak control programs. Evaluation of the effectivenessof space spraying in terms of coverage and timeliness is veryimportant, but very few studies have been done to date. Thisstudy aimed to evaluate the effectiveness of space spraying
for DF/DHF in Songkhla municipality, southern Thailandduring May 2006 to April 2007 and to determine the riskfactors for secondary DF/DHF cases.
2. Materials and Methods
The secondary transmission was evaluated by estimatedoverall reproduction number (secondary case) of DF/DHFusing a matrix model under the spatial-time condition ofcase.
2.1. Case Definitions
Primary Case. A new case that occurred in the communityduring the follow-up period.
Index Case. A primary case who infected another person liv-ing within a radius of 100 meters from the index case’s house(an estimated daily flying distance of Aedes mosquitoes [13]).
Secondary Case. A case who resided within a radius of 100meters from index case’s house and developed symptomsbetween 16 and 35 days after diagnosis of the index case(calculated the minimum lag time for developing secondarycase from summation of minimum of infectious period;Lmin = 5 days, extrinsic incubation period; EIPmin = 8days, and intrinsic incubation period; Imin = 3 days andthe maximum lag time from a summation of maximum ofinfectious period; Lmax = 9 days, extrinsic incubation period;EIPmax = 12 days, and intrinsic incubation period; Imax = 14days [2, 3]).
Coindex Case (Coprimary Case). A case that developedsymptoms within 16 days after diagnosis of an index case andcould be a possible source of infection for the secondary case.
Secondary Attack Rate. The number of secondary cases andsusceptible persons residing within a radius of 100 meters ofthe index case’s house during a specified time period.
2.2. Study Design. This is a longitudinal study monitoringcases of DF/DHF in an urban area of southern Thailand. Thestudy was conducted from 1 May 2006 to 30 April 2007.
2.3. Study Setting. The municipality of Songkhla, which wasselected to be the study site, is located at 07◦12
′N, 100◦36′E
on the east coast of southern Thailand, approximately1,000 kilometers south of Bangkok. The municipality covers9.3 km2 and lies on a small peninsular bordered by SongkhlaLake on the west side and the Gulf of Thailand on theeast. There were 27,898 households with a 2006 midyearpopulation of 92,032. The main occupations in this regionconsist of retail, fisheries, and government services. Thepopulation density on the north-eastern coast is low becausethis area contains beaches, government offices, schools andan airport. The central and western areas are denselypopulated by businesses involved in fisheries (western) andvarious types of retail stores (central).

Journal of Tropical Medicine 3
In the past 5 years, the annual number of cases inSongkhla municipality has varied from 66 to 1,352 caseswith an average annual incidence rate of 505 per 100,000population. Within this municipality, there is one generalhospital (Songkhla Hospital) containing 600 beds. This is thehospital where most serious DHF cases in the municipalityare admitted since the next closest tertiary care hospital is 30kilometers away.
2.4. Surveillance and Response Systems. All doctors takingcare of patients in all hospitals in Thailand are regularlyupdated on management of DF/DHF cases. Definitions ofsuspected, clinically diagnosed, and serologically confirmedcases follow the World Health Organization (WHO) guide-lines. Clinically diagnosed cases of DF, DHF, and DSS arecompiled weekly at each hospital with a standard form con-taining essential information on patients. These reports aresent to provincial health officers who take local control mea-sures and forward the information to the Department of Epi-demiology in Bangkok. Consequently, local health officersimplement control measures, such as space spraying, larvacontrol, and health education to reduce disease transmission.
2.5. Data Collection. Data collection was consisted of 3 parts.
(1) Hospital-Based Surveillance System for DF, DHF, and DSSCases. DF, DHF, and DSS cases were clinically diagnosed andserologically confirmed by physicians following the WHOguidelines. Each day, a field researcher verified all new casesadmitted to both inpatient and outpatient wards of SongkhlaHospital from 1 May 2006 to 30 April 2007 and notifiedthe response teams to carry out space spraying. The demo-graphic data of each patient, location of their house, onset ofillness, diagnosis date, and notification date were recorded.
(2) Monitoring the Activities of Space Spraying. Space spray-ing is usually performed for prevention of disease outbreaksor after notification of a case in order to interrupt diseasetransmission. In this study, we focus on spraying for DF/DHFafter a case notification. Information on case notificationdate, date of spraying, address of index case, and neighboringhouses which are sprayed were recorded by the rapidresponse teams.
(3) Graphical Information System (GIS) Data. A map ofSongkhla municipality at the household level was obtainedfrom The Songkhla Statistics Office. A house survey wascarried out to verify existing houses and update new ornonexistent ones. The updated map was digitized andcomputerized at the GIS southern center.
2.6. Statistical Analysis. The distances, Dij , between housesbelonging to pairs of cases in the study (one pair containsan index case and a nonindex case) were calculated using thefollowing formula:
Dij =√(
xi − x j)2
+(yi − y j
)2, (1)
Map of Songkhla municipality
Primary caseSecondary case100 meters radius from DF/DHF cases’ house
Figure 1: The distribution of DF/DHF case.
where xi and yi represent the coordinates of an index case’shouse and x j and y j represent the coordinates of a nonindexcase’s house.
Twenty cluster of an index case were used in thecalculation of relative secondary attack rate of 100 meterradius. Poisson regression was used to determine factorsassociated with the number of secondary DF/DHF cases withadjustment for age, sex, and whether or not an index case’shouse contained window screens. Variables with P-valuesless than 0.05 were considered significant. All analyses wereperformed using R software.
3. Results
3.1. General Characteristics of DF/DHF Cases. Occurrenceof DF/DHF cases in Songkhla municipality was foundthroughout the year, with a seasonal variation demonstratedand a peak occurrence in January. The highest number ofepisodes (2,818 and 16 times) were reported in January 2007,December, and November 2006, respectively, while the leastnumber of episodes (3 times) was found in April 2007.
140 cases (69 DF cases and 71 DHF cases) were reportedfrom Songkhla Hospital and the Provincial Health Officefrom 1 May 2006 to 30 April 2007. These DF/DHF cases werecomposed of 64 males (45.7%) and 76 females (54.3%). Themedian age was 10 years, and the most common age bracketwas 10–15 years (38.8%). All cases were identified underthe definition given above; 115 primary cases were classifiedinto 20 index cases and 95 primary cases (which included 6possible coindex cases). A further 25 secondary cases werealso identified (Figure 1). Secondary cases were composedof 13 (52%) DF and 12 (48%) DHF cases, 14 (56%) caseswere female, and the median age was 11 years. The primarycases were composed of 56 (48.7%) DF and 59 (51.3%) DHF

4 Journal of Tropical Medicine
Table 1: General characteristics of DF/DHF cases.
CharacteristicsType of case
P valuePrimary (%) Secondary (%)
Type of dengue
DF 56 (48.7) 13 (52.0) 0.94
DHF 59 (51.3) 12 (48.0)
Sex
Male 53 (46.1) 11 (44.0) 0.97
Female 62 (53.9) 14 (56.0)
Age group
Median 10 11 0.6
cases, 62 (53.9%) cases were female, and the median agewas 10 years (Table 1). There were no statistically significantdifferences in these general characteristics between primaryand secondary cases.
45.0% of index cases with secondary cases (group 1) and51.7% of index cases without secondary cases (group 2) werediagnosed as DHF. Most of the cases in both groups werefemale and the median age of group 2 was slightly higherthan group 1 (Table 2).
3.2. Distribution of DF/DHF Secondary Cases. On average,secondary cases developed symptoms 28 days (±5 days)after the notification date of the index case. The meandistance between the index cases houses and the houses ofthe secondary cases was 40 meters (range: 10.2–94.3 meters).
3.3. Secondary Attack Rate. The relative secondary attackrate ranged from 1 to 6.3 per 1,000 population, with anaverage of 2.7. The highest attack rate was found in Toa-Itcommunity which has a high population density. Most of theworkforce in this village consists of laborers, factory workers,or fishermen.
3.4. Environmental Characteristics of Index Case Houses.Table 3 shows a comparison of the environmental character-istics between the houses belonging to group 1 and group 2.Terraced houses were the most common type in both groups(group 1 = 70%, group 2 = 58.3%). Most houses of group1 were constructed with mixed concrete (35.5%) or woodand concrete (35.0%) while most houses of group 2 wereconstructed with concrete only (56.7%). 15% of group 1houses were constructed of corrugated iron sheets, but only5% in group 2. 85.0% of group 1 houses and 52.5% of group2 houses had no window screens, respectively.
Table 4 shows a comparison of house index and containerindex between the two groups of index cases. There wereplenty of breeding sites for Aedes mosquitoes found from thelarva survey, such as cement tanks in the toilet areas, waterjars, and discarded containers. The mean house index amonggroup 1 was 73.4 (sd = 17.4) and among group 2 was 66.9(sd = ±29.1). The mean container index for group 1 was30.8 (sd = 12.2) and among group 2 was 30.1 (sd = 19.5). Nostatistical differences between these two groups were found.
3.5. Coverage and Timeliness of DF/DHF Control Activities.Space spraying and larva control were implemented after acase was notified. Among houses in group 1 and group 2, dueto time constraints, only 40% and 40.8% were surveyed formosquito larva, respectively. Deltacide was used inside all ofthe houses from group 1. Among group 2 houses, incompletespray was the result due to operational difficulties. 94.2%were sprayed inside, and 5.8% were sprayed only in frontof the house. The coverage of spraying for houses ingroup 1 was 21.89 meters (1,788 m2) and 23.85 meters(1,506 m2) for houses in group 2, which is approximately 22times less than the coverage recommended by WHO (100meters or 31,428.4 m2). In terms of timeliness, spraying wasinitiated within a median of 17.3 hours after receiving casenotification for both groups.
3.6. Factors Affecting Occurrence of Secondary DF/DHF Cases.Univariate analysis demonstrated that factors associated withsecondary DF/DHF infection were age of index case, houseconstruction material and use of window screens (Table 5).
Multivariate Poisson regression confirmed the associa-tion for male gender (IDR = 2.7) and house constructed withcorrugated iron sheets (IDR = 4.0) after adjusting for age,and use of window screens (Table 6).
4. Discussion
Findings from this study showed ineffective space sprayingmeasures during the study period. WHO recommendationswere not properly followed, and this may have interferedin the final outcome. Twenty-five secondary infections wereidentified despite timely spraying. The relative secondaryattack rate was as high as 6.3 per 1,000 population withan average of 2.7 indicating a failure in outbreak control.The average spraying area was small compared with WHOrecommendations. Space spraying was implemented onlyonce after case notification. Incomplete spraying in terms ofboth coverage and time may cause Aedes mosquitoes to emi-grate from untreated areas into the previously sprayed areas.Koenraadt et al. [14] determined, that 7 days after insecticidespraying, 50% of the original number of mosquitoes werereestablished by extend around 50 meters or 15 meters within2 days of spraying.
The results of this study demonstrate that sex of thesecondary case and index case houses constructed withcorrugated iron sheets was significantly associated withsecondary infections. Males had a 2.7 times higher riskof being infected compared to females. This observationmerits further investigation with a larger sample and anal-ysis of sex-specific behaviors that might modify risk ofinfection. Houses constructed with corrugated iron sheetsplayed a significant role in transmission of DF/DHF in thecommunity. This type of housing material cannot preventmosquitoes from entering a house, where unsuspectingresidents are easy prey for hungry mosquitoes. Temperaturesinside houses constructed with corrugated iron are higherthan houses constructed with concrete or wood. It is knownthat the extrinsic incubation period (EIP) is shorter athigher temperatures; a 5-day decrease in the EIP may triple

Journal of Tropical Medicine 5
Table 2: General characteristics of DF/DHF cases classified by group of index cases.
CharacteristicIndex case group
P valueWith secondary cases (group 1) (%) Without secondary cases (group 2) (%)
Type of dengue
DF 11 (55.0) 58 (48.3) 0.76
DHF 9 (45.0) 62 (51.7)
Sex
Male 13 (35.7) 51 (42.5) 0.24
Female 7 (64.3) 69 (57.5)
Median age (yrs) 9 10.5 0.1
Table 3: Comparison of environmental characteristic of index case houses.
FactorIndex case group
P valueWith secondary cases (group 1) (%) Without secondary cases (group 2) (%)
House type 0.36
Terraced 14 (70.0) 70 (58.3)
Townhouse 0 (0.0) 4 (3.3)
Single house 3 (15.0) 22 (18.3)
Slum house 3 (15.0) 20 (16.7)
Apartment 0 (0.0) 4 (3.3)
Construction material 0.05
Concrete only 7 (35.0) 68 (56.7)
Concrete and wood 7 (35.0) 33 (27.5)
Wood only 3 (15.0) 13 (10.8)
Corrugated iron sheet 3 (15.0) 6 (5.0)
Window screens present 0.005
No 17 (85.0) 63 (52.5)
Yes 3 (15.0) 57 (47.5)
Garbage piles around house 0.71
No 18 (90.0) 111 (92.5)
Yes 2 (10.0) 9 (7.5)
Piped water
No 3 (15.0) 13 (10.8) 0.59
Yes (noncontinuous flow) 2 (10.0) 11 (9.2)
Yes (continuous flow) 15 (75.0) 96 (80.0)
Table 4: Comparison of house and container index.
FactorIndex case group
P valueWith secondary cases (group 1) (%) Without secondary cases (group 2) (%)
House index (hi)
0.36[0, 30] 0 (0.0) 10 (8.8)
[30, 100] 107 (100) 103 (91.2)
Median 72.5 70
Container index (ci)
0.89[0, 30] 9 (45.0) 56 (49.6)
[30, 100] 11 (55.0) 57 (50.4)
Median 31.3 29.9
the virus transmission rate [15]. The warmer temperaturesinside a corrugated iron house may allow vectors to surviveand reach maturity more rapidly thus promoting a quickertransmission of the virus compared to houses constructedwith other materials. Additionally, window screen was a
significant predictor for transmission in univariate analysisbut turned to be nonsignificant in multivariate analysis.This confounding could be explained by the association ofwindow screen and type of house or roof. Thus, the generalconstruction of house may be more important than whether

6 Journal of Tropical Medicine
Table 5: Univariate analysis of factors affecting incidence of secondary DF/DHF.
Variable IDR 95% CI P value
Male gender 2.21 0.88–5.54 0.08
Age of index case (years) 0.90 0.80–1.00 0.04
House type: ref. = single house
Terraced 1.90 0.50–6.60 0.3
Slum house 2.30 0.50–11.4 0.3
House material: ref. = concrete
Mixed concrete and wood 2.37 0.83–6.77 0.1
Wood 1.81 0.47–7.00 0.39
Corrugate iron sheet 5.04 1.30–19.5 0.02
Window screen (no versus yes) 4.10 1.20–14.1 0.01
Pipe water: ref. = continuous flowing
None 1.40 0.40–4.70 0.62
Noncontinuous flowing 1.00 0.20–4.20 0.97
Garbage pile near the house 1.60 0.40–7.10 0.53
House index 1.01 0.99–1.03 0.11
Container index 1.00 0.99–1.03 0.42
Time lag of spraying (hours) 0.99 1.00-1.01 0.51
Area of spraying (m2) 1.00 1.00-1.00 0.45
Table 6: Multivariate analysis of factors affecting incidence of secondary DF/DHF.
Variables Crude IDR (95% CI) Adj. IDR (95% CI) P-value
Age of index case (years) 0.9 (0.8–1) 0.9 (0.8–1) 0.10
Male gender 2.2 (0.9–5.5) 2.7 (1–7.2) 0.04
House construction: ref. = Concrete
Mixed concrete and wood 2.4 (0.6–5) 1.7 (0.6–5.4) 0.30
Wood 1.8 (0.5–7) 0.8 (0.2–3.4) 0.74
Corrugated iron sheets 5.0 (1.3–19.5) 4.0 (1.0–16.8) 0.05
No window screens 0.4 (0.1–1.2) 0.5 (0.1–1.8) 0.30
Time lag of spraying (hours) 1.0 (0.8–1.2) 1.0 (0.8–1.3) 0.90
Area of spraying (m2) 1.0 (1.0-1.0) 1.0 (1.0-1.0) 0.68
the house has window screen. The exact mechanism needsfurther investigation.
The first limitation in this study concerns the calculationof the number of secondary infections. We assumed thatthe minimum lag time or the minimum period in thedeveloping secondary case from summation of minimum ofinfectious period; Lmin, extrinsic incubation period; EIPmin,and intrinsic incubation period; Imin (Lmin + EIPmin +Imin) and the maximum lag time from a summation ofLmax, EIPmax, and Imax (Lmax + EIPmax + Imax). So, thevariation of number of secondary case may be due to thedistinction in each period of this assumption. Secondly, themovement of viraemic persons was not determined. Themovement of persons is a means of carrying or receiving thedengue virus to places that may encourage disease spreading;a case identified in the community could have been anindigenous one or an imported one.
5. Conclusion
Our findings suggest that space spraying in the study area wasinadequate and often failed to prevent secondary DF/DHF
infections. Our recommendations are to increase the sprayarea to cover a radius of 100 meters from the index case’shouse and to repeat spraying 7–10 days after the initial spray.Control programs should target houses constructed withcorrugated iron sheets.
Acknowledgments
The authors would like to thank the staff from The GISCenter of Prince of Songkhla University for their recommen-dation in the analysis. This study was supported by Grant No.1145 from SEARO, WHO.
References
[1] World Health organization, “Dengue/dengue haemorrhagicfever,” 2009, http://www.who.int/csr/disease/dengue/en/.
[2] World Health Organization, “Transmission of Dengue Virusby Aedes aegypti,” 2009, http://www.cdc.gov/ncidod/dvbid/dengue/slideset/set1/i/slide04.htm.
[3] World Health organization, “Monograph on Dengue/DengueHaemorrhagic Fever,” World health organization Regional

Journal of Tropical Medicine 7
Office for South East Asia, New Delhi, India, Regionalpublication, SEAR No. 22, 1993.
[4] World Health organization, “Impact of Dengue,” 2009, http://www.who.int/csr/disease/dengue/impact/en/index.html.
[5] S. Promprou, M. Jaroensutasinee, and K. Jaroensutasinee,“Climatic factors affecting dengue haemorrhagic fever inci-dence in Southern Thailand,” Dengue Bulletin, vol. 29, pp. 41–48, 2005.
[6] S. Thammapalo, V. Chongsuvivatwong, A. Geater, and M.Dueravee, “Environmental factors and incidence of denguefever and dengue haemorrhagic fever in an urban area,Southern Thailand,” Epidemiology and Infection, vol. 136, no.1, pp. 135–143, 2008.
[7] N. G. Gratz, “Emerging and resurging vector-borne diseases,”Annual Review of Entomology, vol. 44, pp. 51–75, 1999.
[8] D. M. Watts, D. S. Burke, and B. A. Harrison, “Effect of tem-perature on the vector efficiency of Aedes aegypti for dengue 2virus,” American Journal of Tropical Medicine and Hygiene, vol.36, no. 1, pp. 143–152, 1987.
[9] S. Thammapalo, V. Chongsuwiwatwong, A. Geater, A. Lim,and K. Choomalee, “Socio-demographic and environmentalfactors associated with Aedes breeding places in Phuket,Thailand,” Southeast Asian Journal of Tropical Medicine andPublic Health, vol. 36, no. 2, pp. 426–433, 2005.
[10] World Health Organization, “Dengue haemorrhagic fever:diagnosis, treatment, prevention and control,” 2nd edition,Geneva, Switzerland, 1997, http://www.who.int/csr/resources/publications/dengue/060-66.pdf.
[11] World Health Organization, “Dengue haemorrhagic fever:diagnosis, treatment, prevention and control,” 2nd edition,Geneva, Switzerland, 1997, http://www.who.int/csr/resources/publications/dengue/048-59.pdf.
[12] The Bureau of Epidemiology, “Annual report for diseasesurveillance of Thailand,” Bangkok, Thailand, 2009.
[13] R. Boyce, Yellow Fever and Its Prevention, E.P. Dutton and Co.,New York, NY, USA, 1911.
[14] C. J. M. Koenraadt, J. Aldstadt, U. Kijchalao, A. Kengluecha,J. W. Jones, and T. W. Scott, “Spatial and temporal patterns inthe recovery of Aedes aegypti (diptera: culicidae) populationsafter insecticide treatment,” Journal of Medical Entomology,vol. 44, no. 1, pp. 65–71, 2007.
[15] J. S. Koopman, D. R. Prevots, M. A. V. Marin et al.,“Determinants and predictors of dengue infection in Mexico,”American Journal of Epidemiology, vol. 133, no. 11, pp. 1168–1178, 1991.












![[SEBASTIAN BECK] Monografia](https://static.fdokumen.com/doc/165x107/579074ef1a28ab6874b239b3/sebastian-beck-monografia.jpg)