Volume-based vs Rate-based feeding - saspen
-
Upload
khangminh22 -
Category
Documents
-
view
2 -
download
0
Transcript of Volume-based vs Rate-based feeding - saspen
Learning Objectives
• Background• Definitions of volume- and rate-based enteral feeding • Discuss primary literature and other related research• Education and protocol implementation in the ICU • Compare and contrast the pros and cons to
volume-based vs. rate-based enteral feeding
Background
ICU SURVIVORS
• Frequently experience significant post-ICU morbidities:
-muscle weakness-loss of lean body mass-impairment in physical functioning
Stoppe et al. Critical Care 2019
Background
ICU SURVIVORS
which results in significant healthcare-associated
COSTsStoppe et al. Critical Care 2019
Background
ICU SURVIVORS
• Recent randomized trials demonstrate:-providing increased calories alone to ICU patientsmay not improve outcomes
• However, observational studies report that optimizing daily protein intake decreases infections, mechanical ventilationduration, time to discharge and mortality
Arabi YM, N Engl J Med 2015;372:398-408
Heyland DK, Nutrients 2018;10:462
Prieser J-C, Crit Care 2018;22:261
Stoppe et al. Critical Care 2019
Background
Optimal nutrition in critically ill patients is difficult to achieve
• Studies indicate these patients receive 50-70% of goal calories• Underfeeding may lead to malnutrition, increased infectious
complications, increased mechanical ventilation days, impairedimmune response, poor wound healing, and increased mortality,length of hospital stay and cost Rubinsin L, Crit Care Med 2004
Villet S, Clin Nutr 2005
Alberda C, Int Care Med 2009
Lewis SJ, J Gasto Sug, 2009
Haskins IN, JPEN 2015
Zheng YL, JPEN 2016
Compher C, Crit Care Med 2017
Background
Common reasons for NOT achieving our Nutrition Goals
• Delays in initiation of feeding OR NPO status• Frequent cessation of feeding for diagnostic testing and
multiple operative procedures• Aspiration concerns – GRV volumes• Malfunctioning Enteral access• Lack of feeding protocols (<60% protein delivered)• GIT complications McClave SA, Crit Care Med 1999
Drover JW, JPEN 2010
Peev MP, JPEN 2015
Background
ENTERAL NUTRITION (EN)
Remains the preferred route of feeding in ICU’s
Dhaliwal R: Canadian Crit Care Nutr guidelines, Nutr Clin Prac 2014
Kreymann KG: ESPEN guidelines on EN, Clin Nutr 2016
McClave SA, JPEN 2016
Reintam Blaser A: ESICM clin prac guidelines 2017
Background
WHY EN FEEDING PROTOCOLS?
PERMIT MORE TIMELY AND COMPLETE NUTRITION
J Krenitsky-Prac Gastro, Aug 2018
Definition
RATE BASED FEEDING (RBF)
McClaveSA, Crit Care Med 2014;42(12):2600-2610.McClaveSA, Nutr Clin Pract 2009;24:305-315.
–Traditional method of feeding–Consistently associated with failure to meet goals
–Low start and slow titration–Fixed rate
Definition
VOLUME BASED FEEDING (VBF)
–Establishes a 24 hour tube feeding goal volume
–Uses a nurse-driven algorithm to increase the EN infusion rate after interruptions (Max: 150ml/hr)
S Roberts-JPEN, March 2019;43(3):365-375M Bharal-J of Int. Care Soc, 2019
EXAMPLE OF VBF:
–Total 24 hour volume: 1800 ml(starting rate of 75 ml/hr)
–Patient fed 450 ml in 6 hours–EN put on hold for 5 hours
•New feeding goal: 1800-450=1350 ml•Time remaining: 24-6-5=13 hrs•Use the chart to locate new rate of 104 mL/hr
(1350/13)
https://criticalcarenutrition.com/pepup/study-tools
Protocol Implementation:
Education• In-services for all disciplines, pocket cards email
notification, FAQ binder, bedside VBF schedule, practice scenarios, bedside competencies
• May consider: posters, daily checklists, self-learning module
h
Main features of PEPuP Protocol
1. Three feeding options:• Volume-Based Feeds: Stable patients start EN at goal rate • Trophic Feeds: Unstable patients start at 10 mL/hour, re-assess daily• NPO: Re-assess daily 2. Volume-based feeding: target a 24-hour volume vs. traditional hourly volume
goal rate3. Nurse driven: adjust hourly rate to make up the 24-hour volume4. Semi-elemental/peptide-based 100% whey formula: start and progress to
polymeric5. Whey protein modular supplements (if required) and motility agents 6. Gastric residual volumes: tolerating higher thresholds (300ml)
Critical Care Nutrition, March 2016
Study design
• Multicentre Study• 2013, 24 ICU’s from Canada• Participated in the International Nutrition
Survey (INS)• 8 ICU’s – PEPuP and 16 ICU’s – Control sites• Nutrition practices and outcomes compared
Heyland DK, JPEN 39(6);Aug 2015:698-706
Data Collection
• Critically Ill patients, mechanically ventilated• At least a 72 hour ICU stay• Daily nutrition data – Max 12 days• Patient outcomes (60-days)
* ICU and hospital discharge* Duration of mechanical ventilation* Mortality
Heyland DK, JPEN 39(6);Aug 2015:698-706
Results
Heyland DK, JPEN 39(6);Aug 2015:698-706
Overall, 25 % of patients in both groupsdied by day 60 Median LOS in ICU and hospital was 11 days and 26.9 days respectivelyNO difference between groups
Results
Heyland DK, JPEN 39(6);Aug 2015:698-706
ENERGYPEPuP – 60.1%
vsControl – 49.9%
PROTEINPEPuP – 61%
vsControl – 49.7%
Conclusion
PEPuP Protocol
• Significant improvements in nutrition practices and nutrition outcomes
• NO difference in Patient OutcomesHeyland DK, JPEN 39(6);Aug 2015:698-706
A.S.P.E.N. Guidelines 2016: –“Based on expert consensus, we suggest that use of a volume-based feeding protocol or a top-down multi-strategy protocol be considered.”
Journal of Parenteral and Enteral Nutrition 40.2 (2016): 159-211
Literature
NutrClinPract. 2014 Oct;29(5):639-48JPEN J ParenterEnteral Nutr. 2015;39:707-712Critical Care Medicine: 2013 Dec; 41(12):2743–2753Haskins IN, J ParenterEnteral Nutr. 2015J Acad Nutr Diet. 2012 July;112(7):1073–1079Journal of Parenteral and Enteral Nutrition 40.2 (2016): 159-211
Results
B Taylor, Nutr in Clin Prac, Oct 2014;29(5):639-648
CALORIESFEED ME – 89%
vsRATE based – 63%
P<.0001
Results
B Taylor, Nutr in Clin Prac, Oct 2014;29(5):639-648
PROTEIN (g/kg)FEED ME – 1.26
vsRATE based – 1.13
P.36
Results
B Taylor, Nutr in Clin Prac, Oct 2014;29(5):639-648
Trend towards a longer LOS in
FEED ME15 vs 12.2 days
P.053
Study design
• Restrospective Study• Mechanically ventilated within 48 hrs• ICU stay ≥ 72 hrs• VBEN vs RBEN• EN-related and Glucose control outcomes
S Roberts, JPEN March 2019;43(3):365-575
Study design
BLOOD GLUCOSE
• Hyperglycaemia defined as BG >180 mg/dLbased on the first morning BG level
S Roberts, JPEN March 2019;43(3):365-575
Results
S Roberts, JPEN March 2019;43(3):365-575
ENERGYVBEN – 79.6%
vsRBEN – 67.6%
P<.001
PROTEINVBEN – 79.3%
vsRBEN – 68.6%
P<.001
Results
S Roberts, JPEN March 2019;43(3):365-575
HYPERGLYCAEMIANo difference
between 2 groupsP = .27
Literature
J Krenitsky, MS, RD-Practical Gastroenterology, Aug 2018
Exceeded Energyrequire-
ments at 30 kcal/kg in a large
obese
cohort
Background
ICU SURVIVORS
• Recent randomized trials demonstrate:-providing increased calories alone to ICU patientsmay not improve outcomes
• However, observational studies report that optimizing daily protein intake decreases infections, mechanical ventilationduration, time to discharge and mortality
Arabi YM, N Engl J Med 2015;372:398-408
Heyland DK, Nutrients 2018;10:462
Prieser J-C, Crit Care 2018;22:261
Stoppe et al. Critical Care 2019
Literature
PERFECT FEEDING PROTOCOL
Brierley-Hobson et al. Crit Care 2019 23:105
VBF Group
Volume ↑ 11.2% (p ≤ 0.001)
Energy ↑ 13.4%(p ≤ 0.001)
Protein ↑8.4%(p ≤ 0.02)
Literature
PERFECT FEEDING PROTOCOL
Brierley-Hobson et al. Crit Care 2019 23:105
VBF Group
↑ extubation rate with > 90% protein requirements met
compared to < 80 %
NOMORTALITYDIFFERENCE
Literature
OPTIMAL TIMING ???
• High protein intakes during the early phase of critical illness has been associated with detrimental effects
-? Increased production of glucagon -? Increased oxidation of amino acids-? Inhibition of AUTOPHAGY
Casaer MP, EPaNIC trial:a post hoc analysis Am J respir Cit Care Med 2013;187:247-55
Thiessen SE, Am J Respir Crit Care Med 2017; 196:1131-43
Wischmeyer PE, TOP-UP pilot trial Crit Care 2017;21:142
Patients at LOW
NUTRITIONAL RISK
Literature
OPTIMAL TIMING and DOSE???
• Several RCT’s however have demonstrated the safety of high-dose protein application, even in the early phase of critical illness in HIGH-RISK patients with prolongedICU stay
• More RCT’s are however needed to determine the optimal protein DOSE
Casaer MP, EPaNIC trial:a post hoc analysis Am J respir Cit Care Med 2013;187:247-55
Thiessen SE, Am J Respir Crit Care Med 2017; 196:1131-43
Wischmeyer PE, TOP-UP pilot trial Crit Care 2017;21:142
FUTURE Literature
EFFORT Trial
• Randomized • HIGH RISK patients
• Protein ≤ 1.2 g/kg/d OR ≥ 2.2 g/kg/d• VBF strategies• EN or PN protein supplemention
Brierley-Hobson et al. Crit Care 2019 23:105
Literature
Berger et al, ClinNutr2018; Singer et al, ClinNutr2018Sourced from R Blaauw: Consensus Guidelines, CNE 2019
NUTRITION AND STRESS RESPONSE
Late phase/ Post-acute phase(>7 days)• Rehabilitation and restoring
of losses =anabolismPICS (> 14 days)• Chronic critically ill• Decrease lean body massFeeding:• 25 30 kcal/kg• Monitor and increase as
needed
Late acute phase• Stabilization of metabolic
disturbances• Increased muscle wastingFeeding:• 80-100% EE• 20-25 kcal/kg
Literature
Criteria for Refeeding Hypophosphatemia:▪Serum PO4< 0.65 mmol/L OR▪Serum PO4drop > 0.16 mmol/L
Incidence in ICU is common 37-52%
WHAT ABOUT REEFEEDING?
Fuentes et al, 2016Olthof et al, 2017Ralib & Mat Nor, 2018
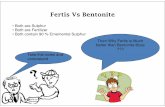
SUMMARY
VOLUME BASED RATE BASE
VS• Increased delivery of nutrition• Flexibility in protocol
design - ??protein supplementation• Nursing driven• Considerations for glucose control• May not be appropriate for all
patient populations• Extensive training necessary to
implement
• Historical use• Familiarity• Less nursing intensive• Easier glucose management• Consistently does not
meet minimum nutritiongoals
• Usually is slower to start and titrate
1. How to achieve nutrition goals by actual nutrition guidelines, Stoppe et al. Crit Care 2019;23:216
2. Full Force Enteral Nutrition: A New Hope, or the Dark Side? A Critical look at Enhanced Enteral Feeding protocols, J Krenitsky, Practical gastroenterology Aug 2018
3. Improving Enteral Delivery through the Adoption of the “Feed Early Enteral Diet adequately for maximum Effect (FEED ME)” protocol in a Surgical Trauma ICU: A QualityImprovement Review, Taylor B et al. Nutr. in Clin Prac Oct 2014;29:639-648
4. Safety and efficacy of volume-based feeding in critically ill, mechanically ventilated adultsusing the ‘Protein & Energy Requirements Fed for Every Critically ill patient every Time(PERFECT) protocol: a before-and-after study, Brierley-Hobson et al. Crit Care 2019;23:105
5. Volume-Based vs Rate-Based Enteral Nutrition in the Intensive Care Unit: Impact on NutritionDelivery and Glycemic Control, S Roberts et al. JPEN Mar 2019;43:3 365-375
6. Implementing the PEP uP Protocol in Critical Care Units in Canada: Results of a Multicenter,Quality Improvement Study, DK Helyland et al. JPEN Aug 2015;39:6 698-706
7. Enhanced protein-energy provision via the enteral route in critically ill patients: a single centerfeasibility trail of the PEP uP protocol, DK Heyland et al. Crit Care 2010
8. Volume based feeding versus rate based feeding in the critically ill: A UK study,M Bharal et al. J of Int. Care Society 2019
9. Volume- vs. rate-based tube feeding in burn patients: A Case-control study. C Sheckter et al.
Burns Open 2 (2018) 165-170
References